Abstract
Background
Esophageal cancer poses a significant global burden, while its patterns and trends remain to be clarified. The aim of this study is to provide an update on the incidence and mortality rates of esophageal cancer and their trends in China based on data from the National Cancer Registry.
Methods
We extracted data from the National Central Cancer Registry (NCCR) of China from 2000 to 2016 and performed comprehensive quality control. We calculated age-standardized rates of China (ASR China) and world (ASR world) using the Chinese population in 2000 and the Segi's world standard population, and performed a joinpoint regression analysis to examine the trend in incidence and mortality of esophageal cancer. The annual percent change (APC) and weighted average APC (AAPC) over the entire study period were estimated to measure the changing trend. Subgroup analyses were conducted by sex, region and pathological type.
Results
A total of 487 eligible cancer registries were included in the data analysis and 22 registries with uninterrupted registration data were used for trend analysis. In 2016, there were an estimated of 184,500 incident cases of esophageal cancer and 142,300 deaths in China. The crude incidence, ASR China and ASR world were 25.25/100,000, 11.00/100,000 and 11.13/100,000, respectively. And the crude mortality, ASR China and ASR world were 19.38/100,000, 8.25/100,000 and 8.28/100,000, respectively. Esophageal squamous cell carcinoma (ESCC) was the most common histological type, accounting for 85.79% of all cases, followed by esophageal adenocarcinoma (EAC) (11.00%) and others (3.21%). There was a decreasing trend of ASR world in incidence and mortality during 2000–2016 with the AAPC of -4.6% (95% CI: -5.7%, -3.4%) and -4.6% (95% CI: -5.2%, -3.9%). The pattern and trend of esophageal cancer differ in sex, region and pathological type.
Conclusions
The burden of esophageal cancer in China remains high with sex, regional and subtype differences. The incidence and mortality of esophageal cancer have continued to decline over the past decade, which was due in part to the reductions in risk factor exposure and the implementation of screening.
Keywords: Esophageal cancer, Incidence, Mortality, Trends, China
1. Introduction
Esophageal cancer (EC) is the ninth most common cancer and the sixth most common cause of cancer death globally.1 There were an estimated 604,100 new cases of esophageal cancer and 544,076 deaths from esophageal cancer worldwide in 2020, and approximately half of them occurred in China.1,2 The two main histological subtypes of esophageal cancer are esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC).3 Globally, ESCC is the most common type of esophageal cancer, particularly in high-incidence areas of eastern Asia and in eastern and southern Africa, while EAC is the main type in western countries.3,4
In China, esophageal cancer has posed a large disease burden.5 The disability-adjusted life years (DALYs) caused by esophageal cancer ranks fourth among all cancers.6 Although the survival rate has increased from 20.9% to 30.3% in the past decade,7 the prognosis of esophageal cancer remains poor since most cases were diagnosed at a late stage.
This study estimated the incidence and mortality of esophageal cancer in China based on the latest data from the national cancer registry system, and analyzed the trends by sex, region, and histological types, to provide a reference for the prevention and control of esophageal cancer.
2. Materials and methods
The incident case and death records of esophageal cancer (coded as C15 according to International Statistical Classification of Diseases and Related Health Problems 10th Revision)8 were extracted from the National Central Cancer Registry (NCCR) of China and the population data were obtained from the National Bureau of Statistics of China. In 2019, 574 local cancer registries covered a population of 438 million in China (31.5% of the Chinese population), providing a representative data source for the analysis of cancer incidence and mortality.9
The data quality control was performed by NCCR according to the national criteria for Chinese cancer registration data, which was developed based on the relevant evaluation criteria of Chinese Guideline for Cancer Registration (2016) and International Agency for Research on Cancer (IARC)/International Association of Cancer Registries.10,11 Multiple indexes including the mortality to incidence (M/I) ratio, the percentage of cases morphologically verified (MV%), the percentage of death certificate-only cases (DCO%), and the stability of cancer trends over years were evaluated in consideration of completeness, comparability, validity and timeliness of registry data.10,11 For registers with unqualified data (MI<0.4 or MI>0.95, MV<40% or MV>95%, DCO>15%, or significant changes in historical data), NCCR organized expert group discussions to decide whether to include these registries based on more specific information. To ensure the accuracy and authenticity of the data, only high-quality data were included in the analysis.
The age-standardized rates of China (ASR China) and world (ASR world) were calculated using the Chinese population in 2000 and the 1966 Segi-Doll World standard population.12 The number of esophageal cancer incident and death cases in China in 2016 was estimated based on the incidence and mortality in cancer registry areas and the corresponding population data. The age-specific rates were calculated for each 5-year age group (0–4,…, 75–79, 80–84, and 85+) and compared by sex and area. The two main histological types of esophageal cancer were defined according to the third edition of the International Classification of Diseases for Oncology (ICD-O-3)13: ESCC: 8050–8078, EAC: 8140–8380. Cases with missing pathological type or morphology coded 8000–8010 were defined as unspecific cancers. Other esophageal cancers were those with any histology other than ESCC or EAC (excluding unspecified cancers). To estimate the incidence of each pathological type, we proportionally assigned the nonspecific cases to the three groups (ESCC, EAC, and other). Subgroup analysis was conducted by comparing the incidence and mortality by sex (male vs female), region (urban areas vs rural areas and seven administrative regions including North, Northeast, East, Central, South, Southwest, and Northwest) and pathological type (ESCC, EAC, and other).
A joinpoint regression analysis14 was performed to examine the trend in incidence and mortality of esophageal cancer using Joinpoint software (version 4.9.1.0; http://surveillance.cancer.gov/joinpoint) from the Surveillance Research Program of the US National Cancer Institute.15 To test whether the change in trend was statistically significant, a minimum of zero and a maximum of three connections were set. Trends of ASRs were expressed as annual percentage change (APC) for each identified linear segment and weighted average annual percentage change (AAPC) over the entire 2000–2016 period by age groups. Subgroup analyses by sex and region were performed for trends in age-standardized incidence and mortality and for trends in subtype-specific incidence. Data analysis was conducted using SAS software (Version 9.4, SAS Institute Inc).
3. Results
A total of 487 qualified cancer registries were included in the data analysis, covering 381,565,422 people (193,632,323 males and 187,933,099 females), representing 27.60% of the total population in China at the end of 2016. Of these, 200 registries were classified as urban areas and 287 were rural areas. A total of 87 registries were excluded due to poor quality, accounting for 13% of the population covered by the registries, and they were mainly distributed in rural areas in central and western China where cancer registration started relatively late. After quality control, the MV%, DCO% and M/I of esophageal cancer were 76.30%, 1.61%, and 0.77, respectively, suggesting good quality of the registered data.
Table 1 provided the estimated incidence and mortality of esophageal cancer in China in 2016. There were 252,464 new incident cases of esophageal cancer and 193,870 people died from esophageal cancer. The estimated crude incidence, ASR China and ASR world were 18.26/100,000, 11.00/100,000 and 11.13/100,000, respectively. The estimated crude mortality, ASR China and ASR world were 14.02/100,000, 8.25/100,000 and 8.28/100,000, respectively. Subgroup analysis showed that the ASR China incidence and mortality were about three times higher in males than in females, and about twice as high in rural areas as in urban areas (Fig. 1). Central China showed the highest incidence and mortality among the seven administrative regions, followed by East China and Southwest China (Supplementary Table 1).
Table 1.
Esophageal cancer incidence and mortality in China, 2016.
| Region | Sex | Incidence |
Mortality |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (104) | Crude rate (1/105) | Proportion (%) | ASR China (1/105) | ASR world (1/105) | Rank | Cases (104) | Crude rate (1/105) | Proportion (%) | ASR China (1/105) | ASR world (1/105) | Rank | ||
| All | Male | 18.45 | 26.05 | 8.26 | 16.56 | 16.81 | 5 | 14.23 | 20.10 | 9.30 | 12.63 | 12.73 | 4 |
| Female | 6.80 | 10.07 | 3.71 | 5.59 | 5.60 | 9 | 5.16 | 7.64 | 5.84 | 4.03 | 4.00 | 6 | |
| Total | 25.25 | 18.26 | 6.21 | 11.00 | 11.13 | 6 | 19.39 | 14.02 | 8.03 | 8.25 | 8.28 | 5 | |
| Urban | Male | 8.56 | 21.16 | 6.34 | 12.86 | 13.08 | 5 | 6.76 | 16.71 | 7.49 | 10.04 | 10.17 | 5 |
| Female | 2.59 | 6.67 | 2.26 | 3.57 | 3.57 | 12 | 2.01 | 5.17 | 3.80 | 2.61 | 2.59 | 8 | |
| Total | 11.15 | 14.06 | 4.47 | 8.17 | 8.28 | 7 | 8.77 | 11.06 | 6.13 | 6.27 | 6.32 | 5 | |
| Rural | Male | 9.89 | 32.59 | 11.19 | 21.88 | 22.18 | 4 | 7.47 | 24.61 | 11.89 | 16.35 | 16.42 | 4 |
| Female | 4.21 | 14.69 | 6.15 | 8.51 | 8.54 | 7 | 3.15 | 11.00 | 8.86 | 6.08 | 6.03 | 4 | |
| Total | 14.10 | 23.90 | 8.99 | 15.08 | 15.24 | 4 | 10.62 | 18.00 | 10.79 | 11.09 | 11.09 | 4 | |
Abbreviation: ASR, age-standardized incidence rate.
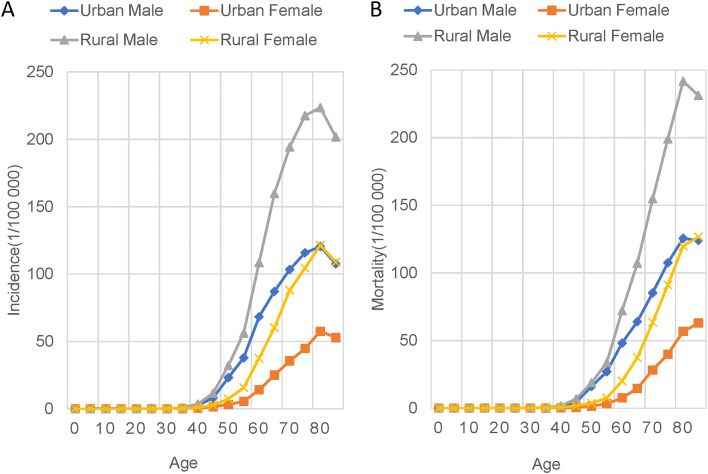
Fig. 1.
Age-specific incidence and mortality of esophageal cancer in China, 2016. EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma.
Fig. 1 showed the age-specific incidence and mortality. The incidence and mortality of esophageal cancer increases rapidly after the age of 40. In all age groups, the incidence and mortality rates were higher in males and in rural areas.
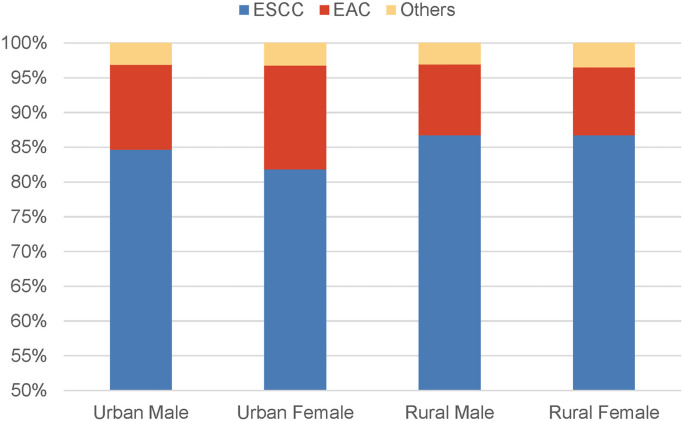
About 65.44% cases of esophageal cancer had morphological verification. Among those, ESCC was the most common histological type, accounting for 85.79% of all cases, followed by EAC (11.00%) and others (3.21%). The estimated age-standardized incidence rates of world for ESCC, EAC and other cancers were 9.55/100,000, 1.23/100,000 and 0.35/100,000, respectively (Supplementary Table 2). Fig. 2 and Supplementary Table 3 showed the distribution of the cases by pathological type, sex, and region. ESCC and EAC were similarly distributed among males and females, accounting for 85.8% and 11.2% of all esophageal cancer cases in males and 84.9% and 11.7% of all esophageal cancer cases in females, respectively. ESCC was slightly more prevalent in rural areas (90% vs 86.7% of cases), while EAC prevailed in urban areas.
Fig. 2.
Histological distribution of esophageal cancer in China, 2016. EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma.
A total of 22 registries with uninterrupted registration data were included in the trend analysis from 2000 to 2016. There was a decreasing trend of ASR world incidence and mortality during 2000–2016 with the AAPC of −4.6% (95%CI: −5.7%, −3.4%) and −4.6% (95%CI: −5.2%, −3.9%) (Table 2). In general, the decline in esophageal cancer incidence and mortality rates was more pronounced in females (−6.4% and −6.3% vs −3.9% and −4.1% per year) and in urban areas (−4.1% and −4.1% vs −2.9% and −3.5% per year). Analysis of age-specific incidence and mortality rates showed the sharpest decline (−10.8% and −10.0% annually) in younger age group (< 40 years) and the slowest decline (−3.5% and −3.3% annually) in older age group (>70 years) (Table 3).
Table 2.
Incidence and mortality trends (2000–2016) of esophageal cancer by sex and region in 22 cancer registration areas of China.
| Characteristics | Incidence, AAPC (95% CI) |
Mortality, AAPC (95% CI) | ||
|---|---|---|---|---|
| ESCC | EAC | All EC | All EC | |
| Sex | ||||
| Male | −3.7* (−4.0 to −3.3) | −3.8* (−6.2 to −1.2) | −3.5* (−3.9 to −3.2) | −3.7* (−4.1 to −3.4) |
| Female | −6.0* (−6.5 to −5.6) | −3.8* (−7.0 to −0.5) | −5.9* (−6.4 to −5.5) | −6.3* (−6.6 to −5.9) |
| Region | ||||
| Urban | −4.0* (−4.4 to −3.6) | −7.3* (−8.4 to −6.1) | −4.1* (−4.5 to −3.6) | −4.1* (−5.0 to −3.1) |
| Rural | −3.0* (−3.6 to −2.4) | 0.5 (−4.4 to 5.7) | −2.9* (−3.4 to −2.5) | −3.5* (−4.1 to −2.9) |
| Total | −4.3* (−4.7 to −3.9) | −3.8* (−6.0 to −1.4) | −4.2* (−4.6 to −3.8) | −4.4* (−4.7 to −4.1) |
Average annual percent change during 2000 to 2016 is significantly different from zero (P < 0.05).
Abbreviations: AAPC, average annual percent change; CI, confidence interval; ESCC, esophageal squamous cell carcinoma; EAC, esophageal adenocarcinoma; EC, esophageal cancer.
Table 3.
Incidence and mortality trends (2000–2016) of esophageal cancer by age group in 22 cancer registration areas of China.
| Characteristics | Trend 1 |
Trend 2 |
Trend 3 |
AAPC (95% CI) of 2000–2016 | |||
|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | ||
| Incidence | |||||||
| < 40 | 2000–2012 | −7.1* (−9.7 to −4.4) | 2012–2016 | −21.0* (−32.3 to −7.9) | −10.8* (−14.2 to −7.2) | ||
| 40–49 | 2000–2004 | −9.8* (−14.4 to −4.9) | 2004–2013 | −4.1* (−5.8 to −2.3) | 2013–2016 | −16.1* (−22.8 to −8.8) | −7.9* (−9.7 to −6.0) |
| 50–59 | 2000–2016 | −5.0* (−5.7 to −4.3) | −5.0* (−5.7 to −4.3) | ||||
| 60–69 | 2000–2005 | −5.8* (−7.1 to −4.5) | 2005–2009 | 0.2 (−2.8 to 3.4) | 2009–2016 | −5.5* (−6.3 to −4.7) | −4.2* (−5.0 to −3.4) |
| ≥ 70 | 2000–2016 | −3.0* (−3.6 to −2.4) | −3.5* (−3.8 to −3.3) | ||||
| Mortality | |||||||
| < 40 | 2000–2010 | −4.7* (−8.6 to −0.5) | 2010–2016 | −18.2* (−25.4 to −10.3) | −10.0* (−13.4 to −6.4) | ||
| 40–49 | 2000–2016 | −7.0* (−7.9 to −6.0) | −7.0* (−7.9 to −6.0) | ||||
| 50–59 | 2000–2016 | −4.6* (−5.2 to −4.1) | −4.6* (−5.2 to −4.1) | ||||
| 60–69 | 2000–2004 | −8.1* (−9.9 to −6.2) | 2004–2009 | −2.8* (−4.7 to −0.8) | 2009–2016 | −5.0* (−5.8 to −4.2) | −5.1* (−5.8 to −4.4) |
| ≥ 70 | 2000–2016 | −3.3* (−3.7 to −2.9) | −3.3* (−3.7 to −2.9) | ||||
Average annual percent change during 2000 to 2016 is significantly different from zero (P < 0.05).Abbreviations: AAPC, average annual percent change; APC, annual percent change; CI, confidence interval.
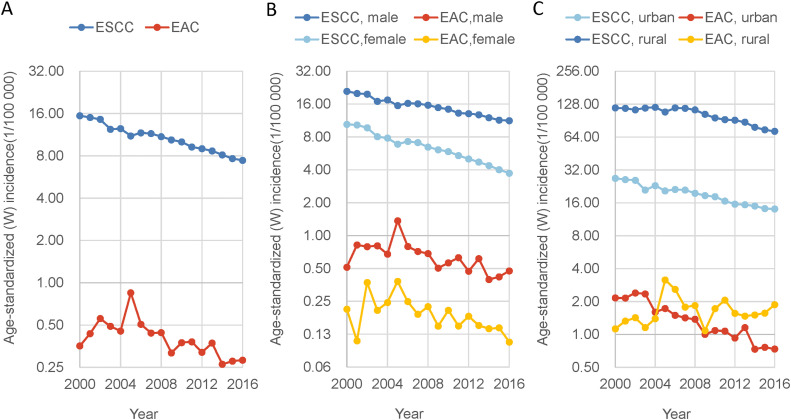
The incidence of both ESCC and EAC showed a decreasing trend from 2000 to 2016, with AAPC of −4.3% (95% CI: −4.7% to −3.9%) and −3.8% (95% CI: −6.0% to −1.4%), respectively (Table 2, Fig. 3). The incidence of ESCC had a greater decline in females than in males, and a greater decline in urban areas than in rural areas. The incidence of EAC had a similar declining trend in both sexes. There was a significant decline in EAC in urban areas, but no significant trend was observed in the incidence of EAC in rural areas.
Fig. 3.
Trends in age-standardized incidence of esophageal cancer by histological subtype during 2000–2016. EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma.
4. Discussion
This study provided the updated estimates of esophageal cancer incidence and mortality in China based on cancer registry data and analyzed the trends of esophageal cancer by sex, region, age group, and pathological type from 2000 to 2016. The results showed that, although the incidence and mortality rates of esophageal cancer have shown a decreasing trend since 2000, it is still one of the most common cancers in China and caused a huge disease burden. There were sex and regional differences in esophageal cancer incidence and mortality as well as their trends. The pattern and trend also differ by pathological type.
The incidence and mortality of esophageal cancer in China are higher than the global average level in both sexes. According to the GLOBOCAN report, the global incidence and mortality of esophageal cancer were 9.3/100,000 and 8.3/100,000 in males, and 3.6/100,000 and 3.2/100,000 in females.1 The incidence and mortality rate of esophageal cancer for the Chinese male population is 1.81 and 1.53 times those estimates, respectively. The corresponding figures for the female population are 1.56 and 1.25 times higher. Morgan et al.4 estimated the global burden of esophageal cancer based on the GLOBOCAN database, in which the incidence and mortality rates in China were 13.8/100,000 and 12.7/100,000, respectively, both higher than the estimates in this study. Notably, GLOBOCAN 2020 adopted data from 90 Chinese registries, whereas our study included data from 487 cancer registries, which may better reflect the true burden of esophageal cancer in China.
Sex and regional differences are partly due to differences in exposure to risk factors. The majority of esophageal cancer cases in China are ESCC, and its occurrence is closely related to behavioral factors. Wang et al.16 estimated the population attributable fraction of esophageal cancer to known risk factors and found that 45.8% of esophageal cancers (51.4% in men and 33.1% in women) in China could be attributed to smoking, alcohol consumption, and low fruit and vegetable intake. Wu et al. estimated that 48.5% of esophageal cancer in China were attributable to the lifestyle risk factors including smoking, high red meat consumption, high body mass index (BMI), alcohol consumption, low fruit intake, high processed meat consumption and low vegetable intake.17Yang et al. found that tobacco and alcohol use were the major risk factors for esophageal cancer death and DALYs in Chinese men, while high BMI and low-fruit diet were the main risk factors for Chinese women.18 In China, men drink and smoke more frequently than women, and urban and rural areas differ in terms of socioeconomic and lifestyle risk factors. Accumulating evidence from a large survey19, 20, 21, 22, 23 showed that urban residents had higher household income, education level and medical insurance coverage than rural residents. Urban residents also had a higher proportion of alcohol consumption, daily fresh fruit, dairy and meat intake, and higher BMI than rural residents, while the proportion of smoking was higher in rural areas than in urban areas. Therefore, current primary prevention strategies should consider sex and regional difference, and focus on eliminating various risk factors such as smoking and drinking and promoting a healthy lifestyle through health education to reduce the risk of esophageal cancer.
Overall, the incidence and mortality of esophageal cancer have shown a significant decreasing trend in both men and women, which is inconsistent with the results of previous studies. Rumgay et al.24 estimated the average annual percent change of esophageal cancer by subsite using data from the Cancer Incidence in Five Continents (CI5) database25 for the years 1975–2012 and found no significant decrease in ESCC and EAC in men in China, while the AAPCs for ESCC and EAC in women were −4.1(−6.8 to −1.3) and −6.0(−11.1 to −0.6), respectively. Differences in timing and coverage of data sources could explain this inconsistency. The study by Rumgay et al.24 used data from Chinese cancer registries adopted in CI5 from 1998 to 2012, including 35 cases of EAC and 497 cases of ESCC. Our study included data from 22 uninterruptedly reporting cancer registries up to 2016, for a total of 142,968 cases of esophageal cancer, which provided a greater stability and reliability to our findings.
The declines in incidence and mortality were differentiated by sex, region, and type of histology. The reductions in incidence and mortality were smaller in males than in females, which may be due to higher and poorly controlled of smoking and alcohol consumption in males. The difference in socioeconomic could explain part of the rural-urban differences in the decline in incidence and mortality. Compared with rural residents, urban residents had a higher income and education level and better access to healthcare, and are more likely to have early diagnosis and early treatment through screening. No significant decrease in the incidence of EAC in rural areas was observed, as the rural areas included in the analysis were mainly high-risk areas for ESCC, where the number of EAC cases is relatively low and trends are difficult to observe (Supplementary Table 2 and Supplementary Fig. 1).
Multiple factors have contributed to the decline in esophageal cancer incidence and mortality. In addition to the development of socioeconomic and medical technologies as well as the primary prevention measures targeting risk factors, population-based endoscopic screenings and the increasing use of endoscopy for diagnostic purposes have also played an important role in the prevention of esophageal cancer.26 Endoscopic screening can detect precancerous lesions and early cancers in advance, and reduce the risk of cancer through early diagnosis and early treatment, thus reducing the incidence and mortality of esophageal cancer.
Esophageal cancer is highly prevalent in the elderly people, with an average age of onset around 65 years. In the trend analysis, the incidence and mortality decreased more in the younger age groups than the older age groups, suggesting that the elderly population is the key population for the prevention and control of esophageal cancer. The recommended screening age in the current screening program in China is 40–69 years old.27 However, our study showed that the age-specific incidence of esophageal cancer peaked after the age of 70. Therefore, there is a need to optimize the screening strategy by increasing the starting and ending ages of screening, thus improving the detection rate of screening and reducing over-screening.
Although both MV% and DCO% in this study are relatively low compared to those in developed countries, they are reliable and reflect the characteristics of Chinese cancer registry data. In the Chinese cancer registries, the original pathological diagnosis results are required to define a case as a pathological diagnosis. However, medical resources related to cancer diagnosis and treatment in China are concentrated in large hospitals in urban areas, while the cases are reported by the cancer registries where the household registration is located. As a result, there will be a large number of out-of-town patients. This makes it difficult for the local cancer registries to obtain the patient's pathological diagnosis information, and these cases can only be classified as non-pathological when reported, which resulted in a relatively low MV%. At the same time, the China National Mortality Surveillance System requires additional reporting of the information on incidence and diagnosis for patients who died of cancer (judged according to ICD10). Therefore, when using death certificates as a source of information for cancer registries, the information on incidence and diagnosis is available for most patients, which in turn leads to relatively low DCO%.
A strength of our study is the use of nationwide, high-quality data from population-based cancer registries to ensure the validity, representativeness and comparability of the results. We also estimated the pattern and trend of esophageal cancer by age, sex, region and subtype, providing a more accurate reference for the prevention and control of esophageal cancer.
There are also several limitations. We based our estimates on the cancer registry system; therefore, any underreporting or lagging may have affected them. In addition, missing information on pathological types can also affect the estimate of incidence rates by subtype. As cancer registries expand and data quality improves, more accurate data will be available for future studies.
5. Conclusions
In conclusion, despite the declining trend in incidence and mortality, the burden of esophageal cancer in China remains high with sex and regional differences. Further research is needed to explore the underlying reasons contributing to these patterns and trends. Future prevention and control of esophageal cancer should focus on reducing exposure to modifiable risk factors and implementing individualized screening based on genetic and environmental factors.
Declaration of competing interest
The authors declare that they have no conflict of interests.
Acknowledgments
Acknowledgements
This study is supported by the National Natural Science Foundation of China (grant numbers: 81903403, 81974493), Beijing Natural Science Foundation (grant number: 7204294), National Science & Technology Fundamental Resources Investigation Program of China (grant number: 2019FY101101), and the Chinese Academic of Medical Sciences Innovation Fund for Medical Sciences (grant numbers: 2021-I2M-1-010, 2021-I2M-1–013). We sincerely thank the staffs of the population-based cancer registries for their efforts to make this study possible.
Author contributions
R.C. and W.W. designed the study. S.Z., S.W., K.S., H.Z., L.L conducted the data quality control. R.C. and R.Z. analyzed the data. W.W. and J.H. supervised the whole study. R.C. drafted the original manuscript. All authors reviewed the manuscript drafts and approved the final manuscript.
Footnotes
Given his role as Editor in Chief, Jie He had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Huan He.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jncc.2023.01.002.
Contributor Information
Wenqiang Wei, Email: weiwq@cicams.ac.cn.
Jie He, Email: hejie@cicams.ac.cn.
Appendix. Supplementary materials
References
- 1.Sung H., Ferlay J., Siegel R.L., et al. global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Arnold M., Abnet C.C., Neale R.E., et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159:335–349. doi: 10.1053/j.gastro.2020.02.068. e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lagergren J., Smyth E., Cunningham D., et al. Oesophageal cancer. Lancet. 2017;390:2383–2396. doi: 10.1016/S0140-6736(17)31462-9. [DOI] [PubMed] [Google Scholar]
- 4.Morgan E., Soerjomataram I., Rumgay H., et al. the global landscape of esophageal squamous cell carcinoma and esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: new estimates from GLOBOCAN 2020. Gastroenterology. 2022;163:649–658. doi: 10.1053/j.gastro.2022.05.054. e2. [DOI] [PubMed] [Google Scholar]
- 5.Zheng R., Zhang S., Zeng H., et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent. 2022;2:1–9. [Google Scholar]
- 6.Zhou M., Wang H., Zeng X., et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng H., Chen W., Zheng R., et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6:e555–e567. doi: 10.1016/S2214-109X(18)30127-X. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva: 1992. International Statistical Classification of Disease and Related Health Problems: 10th Revision. [Google Scholar]
- 9.Wei W., Zeng H., Zheng R., et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol. 2020;21:e342–e349. doi: 10.1016/S1470-2045(20)30073-5. [DOI] [PubMed] [Google Scholar]
- 10.Bray F., Parkin D.M. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45:747–755. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 11.Parkin D.M., Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45:756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 12.Doll R., Payne P., Waterhouse J. 1st ed. Springer; 1966. Cancer Incidence in Five Continents - A Technical Report. [Google Scholar]
- 13.World Health Organization . World Health Organization; 2000. International Classification of Diseases for Oncology (ICD-O) [Google Scholar]
- 14.Kim H.J., Fay M.P., Feuer E.J., et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.National Cancer Institute . National Cancer Institute; 2022. Join Point Regression Program. Version 4.9.1.0.https://surveillance.cancer.gov/joinpoint/ Accessed 31 AugustVolume 2022. [Google Scholar]
- 16.Wang J.B., Fan J.H., Liang H., et al. Attributable causes of esophageal cancer incidence and mortality in China. PLoS ONE. 2012;7:e42281. doi: 10.1371/journal.pone.0042281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Y., Li Y., Giovannucci E. Potential impact of time trend of lifestyle risk factors on burden of major gastrointestinal cancers in China. Gastroenterology. 2021;161:1830–1841. doi: 10.1053/j.gastro.2021.08.006. e8. [DOI] [PubMed] [Google Scholar]
- 18.Yang S., Lin S., Li N., et al. Burden, trends, and risk factors of esophageal cancer in China from 1990 to 2017: an up-to-date overview and comparison with those in Japan and South Korea. J Hematol Oncol. 2020;13:146. doi: 10.1186/s13045-020-00981-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Z., Chen J., Collins R., et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40:1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy M., Chen Y., Clarke R., et al. Socioeconomic differences in health-care use and outcomes for stroke and ischaemic heart disease in China during 2009–16: a prospective cohort study of 0.5 million adults. Lancet Glob Health. 2020;8:e591–e602. doi: 10.1016/S2214-109X(20)30078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Im P.K., Millwood I.Y., Guo Y., et al. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China Kadoorie Biobank. BMC Public Health. 2019;19:217. doi: 10.1186/s12889-019-6502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Z., Peto R., Zhou M., et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386:1447–1456. doi: 10.1016/S0140-6736(15)00340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qin C., Yu C., Du H., et al. Differences in diet intake frequency of adults: findings from half a million people in 10 areas in China. Chin J Epidemiol. 2015;36:911–916. [PubMed] [Google Scholar]
- 24.Rumgay H., Arnold M., Laversanne M., et al. International trends in esophageal squamous cell carcinoma and adenocarcinoma incidence. Am J Gastroenterol. 2021;116:1072–1076. doi: 10.14309/ajg.0000000000001121. [DOI] [PubMed] [Google Scholar]
- 25.Ferlay J., Colombet M., Bray F. International Agency for Research on Cancer; Lyon, France: 2018. Cancer Incidence in Five Continents, CI5plus: IARC Cancer Base No. 9. Lyon. [Google Scholar]
- 26.Chen R., Liu Y., Song G., et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut. 2021;70:251–260. doi: 10.1136/gutjnl-2019-320200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang G., Wei W. People's Medical Publishing House; 2020. Technical Protocols for Upper Gastrointestinal Cancer Screening and Early Diagnosis and Treatment (trial version in 2020) Beijing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.