Abstract
Introduction
Given the lack of consensus on optimal treatment strategies for acute Achilles tendon rupture (ATR), understanding temporal trends, treatment choice and demographic characteristics is important. Previous research suggests increasing incidence with declining surgical treatment. Current trends in Sweden are not known.
Hypothesis/purpose
To assess how incidence rates, treatment trends and time from injury to surgery (TTS) of ATR have changed between 2002 and 2021 in Sweden, with particular attention to changes since 2012.
Study design
Descriptive epidemiology study.
Methods
We conducted a nationwide register-based study including all inpatients and outpatients ≥18 years of age with an ATR between 2002 and 2021 in Sweden.
Results
53 688 ATRs (78.5% men) were identified during the study period. 15 045 patients (81.5% men) were surgically treated within 30 days. The long-term incidence rate for ATR injury increased by 45%, from 28.8 in 2002 to 41.7 in 2021 per 100 000 person-years (p<0.0001). In the last 5 years of the study, there was a significant, continuing increase in ATR incidence by 21%, from 34.4 in 2017 to 41.7 in 2021 per 100 000 person-years (p<0.0001). The surgical incidence rates decreased from 13.4 to 6.0 per 100 000 person-years (p<0.0001). TTS increased from 0.6 days in 2002 to 5.1 in 2021 (p<0.0001).
Conclusion
The observed increase in incidence rates and decrease in surgical treatment of ATR emphasise the need for evidence-based treatment and rehabilitation protocols for non-operated patients of all ages. A significant increase in time from injury to surgery was observed throughout the study period.
Keywords: key terms
WHAT IS ALREADY KNOWN ON THIS TOPIC
Different regional and national studies indicate an increased incidence of Achilles tendon rupture (ATR) long-term (10–30 years), with northern European studies demonstrating a concurrent decrease in surgical treatment.
There is only one previous study regarding the incidence of ATR in Sweden, between 2001 and 2012, which suggests an increase in incidence rates between overall and per sex for three different age groups, with decreasing surgical treatment.
WHAT THIS STUDY ADDS
This study demonstrates a long-term rise since 2002 and an accelerated increase since 2017 in incidence rates of ATR, contrasting publications from Europe and Asia.
A simultaneous decreasing trend in the proportion of surgically treated ATR was observed, stabilised at a rate of around 14%–15% since 2017.
The time from diagnosis until surgical repair was investigated, demonstrating a continuous increase in time until surgical repair throughout the study period, which may have a negative impact on the outcomes of ATR patients.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Rising incidence underlines the need for evidence-based ATR treatment and rehabilitation decision-making to optimise patient outcomes.
This study suggests that the rising incidence could be due to increased activity levels at higher ages and activities associated with a higher risk of ATR, which warrants further examination.
The decline in primary surgical repair for ATR prompts surgeons to re-evaluate patient selection criteria, questioning if decisions are guided by scientific evidence or personal preference.
The impact of delayed surgical treatment on patient outcomes and whether this delay is due to economic pressures in Sweden’s healthcare system, such as staff shortages, requires further investigation.
Introduction
Acute Achilles tendon rupture (ATR) is a prevalent injury often occurring during physical or sporting activities. Numerous international studies over the past 30 years have demonstrated an overall increase in the incidence of ATR.1,7 However, recent studies between 2010 and 2017 suggest a plateau in ATR incidence rates.1 4 8 ATR incidence rates within the Swedish population were last reported up to 2012,2 and current rates are unknown.
Between 1997 and 2011, surgical treatment for acute ATR was favoured over non-surgical treatment as several studies demonstrated a reduced risk of re-rupture.9,11 Re-rupturing the Achilles tendon within the first year is considered a severe complication, as it prolongs rehabilitation and leads to an inferior patient-reported outcome.12 However, between 2012 and 2019, there was a shift in recommendations after studies demonstrated how non-surgical management with functional rehabilitation had comparable re-rupture rates and fewer overall complications compared with surgical treatment.13,15 Interestingly, most recent studies on ATR management again advocate for surgical repair over conservative management to prevent re-ruptures, reducing the risk of re-rupture by 64%–86%.16,19 Whether or not these fluctuating research trends can be observed in the clinical management of acute ATR in Sweden is unknown. Moreover, the current rate and demography of ATR patients chosen for surgical repair in Sweden are unknown.
While there remains uncertainty about which patients would benefit the greatest from surgical repair after ATR, a recent study suggests that the time to surgery (TTS), that is, the time from injury until surgical repair, may negatively impact patient outcome.20 Whether TTS has changed over the past 20 years remains unknown.
The present study investigated the long-term changes in ATR incidence rates, ATR treatment trends and TTS in Sweden between 2002 and 2021 and analysed more recent changes since 2012.
Materials and methods
Data were obtained from the Swedish National Patient Register (SNPR), a Swedish nationwide validated register which contains inpatient data since 1964 and outpatient data since 2001.21 Reporting data to the NPR is obligatory for all healthcare providers in Sweden, thus ensuring excellent national coverage. The NPR uses the International Classification of Disease (ICD-10) system based on patient-specific identity numbers to categorise patient morbidity and mortality.22 Thus, any person in Sweden with a personal identity number and seeking healthcare for any reason will be included in the NPR. In the present study, all patients with an Achilles tendon rupture (coded as S860 in ICD-10) from 2002 to 2021, 18 years of age or older, were requested from the register for analyses. Year of birth, age at rupture and sex were also collected from the SNPR. The first occurrence of S860 was regarded as the index case. Any subsequent occurrences in the same patient after 365 days were considered a new rupture. Surgical treatment of ATR was identified by the surgical procedural codes NHL19, NHL49 and NGL49 according to the NOMESCO Classification of Surgical Procedures Sweden.23 If any of these codes were recorded within 30 days in combination with S860, surgery was considered the primary treatment. TTS was defined as the days from the index case to the date when diagnostic and procedural codes were combined. This method was used to calculate the main results of TTS. Additionally, to explore potential influences of other primary diagnoses, difficulties in diagnosing ATR or misentries in the register, other ICD-10 diagnoses of other foot/ankle/lower limb pathologies registered within 14 days before the index case were examined for their impact on TTS. Twenty-two diagnostic codes were determined as relevant and were found in 986 (6.6%) of surgically treated patients. Fifty-four per cent of these patients (n=529) were initially diagnosed with M663/-H/-G (spontaneous rupture of flexor tendons/…of the ankle/…lower limb), 13% (n=131) were recorded as S932 (ruptured ligament in the foot), 10% (n=100) received M796/-D (pain in the extremity/… non-specific in the lower leg), 7% (n=66) as M662/-G/-H (spontaneous rupture of extensor tendon/…of the knee or lower leg/…of the ankle or foot), 4% (n=42) as M665 (spontaneous rupture of unspecified tendon). Another 12 diagnostic codes were recorded, representing the remaining 12% (n=118). The impact of a delay in ATR diagnosis is presented in a separate section in the results.
The STrengthening the Reporting of OBservational studies in Epidemiology checklist was used in preparation of the manuscript.
Statistics
As data for the number of ATRs were collected from the SNPR, another Swedish governmental agency, Statistiska Centralbyrån (Statistics Sweden), provided population data for incidence calculations. Based on 1 July, the midterm population was used to determine incidence rates for each year in the study. Data management was performed with R V.4.0.0 (R Centre for Statistical Computing, Vienna, Austria). Test of significance and 95% CIs for incidence rates were calculated with the MedCalc Statistical Software V.19.2.6 (MedCalc Software by Ostend, Belgium; https://www.medcalc.org; 2020). Significant changes in the median age of rupture were calculated with a Mann-Whitney U test. Significant changes and differences in mean days in delay for surgical repair were calculated using a paired and unpaired Student’s t-test when appropriate. An alpha of 0.05 was used in all statistical tests.
Results
Incidence of ATR
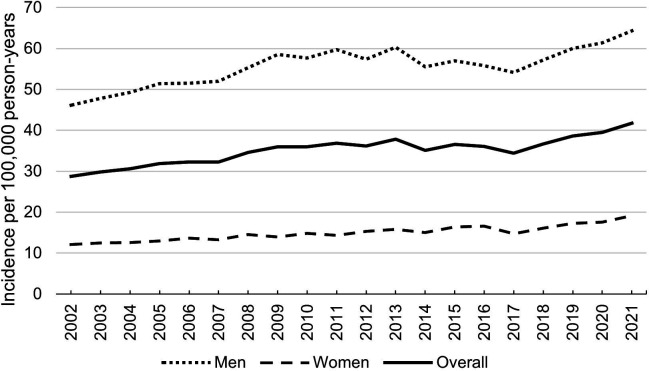
A total of 53 688 ATR cases were recorded in the SNPR between 2002 and 2021, corresponding to an overall incidence rate increase of 45% throughout the study period (p<0.0001) (figure 1, table 1). The overall incidence rate increased by 26% between 2002 and 2012, decreased by 4.8% between 2012 and 2017 and increased by 21% between 2017 and 2021 (figure 1, table 1).
Figure 1. Overall Achilles tendon rupture incidence rates per 100 000 person-years, stratified by sex.
Table 1. Incidence rates per 100 000 person-years and number of Achilles tendon ruptures.
| 2002 | 2012 | 2017 | 2021 | P value | ||
| Overall | Incidence rate (95% CI) | 28.8(27.5 to 30.1) | 36.1(34.9 to 37.5) | 34.4(33.1 to 35.7) | 41.7(40.4 to 43.2) | <0.0001,* 0.066,† <0.0001,‡ |
| N | 2025 | 2765 | 2753 | 3453 | ||
| Men | Incidence rate (95% CI) | 46.1(43.9 to 48.4) | 57.4(55.0 to 59.9) | 54.2(51.9 to 56.5) | 64.3(61.9 to 66.8) | <0.0001,* 0.058,† <0.0001,‡ |
| N | 1590 | 2173 | 2162 | 2663 | ||
| Women | Incidence rate (95% CI) | 12.1(11.0 to 13.3) | 15.3(14.1 to 16.6) | 14.7(13.6 to 16.0) | 19.1(17.8 to 20.5) | <0.0001,* 0.49,† <0.0001,‡ |
| N | 435 | 592 | 591 | 790 |
Comparison of 2002 and 2012.
Comparison of 2012 and 2017.
Comparison of 2017 and 2021.
N, number of Achilles tendon ruptures
The median age increased from 44 to 50 years between 2002 and 2021 (95% CI 43.8 to 44.2 and 49.7 to 50.3, p<0.0001). Men constituted 78% of all ATRs (n=42 140), and their incidence rate increased by 40% during the study period, 24% during 2002–2012 and 19% during 2017–2021 (figure 1, table 1). The male median age increased from 44 to 51 years (95% CI; p<0.0001) during the study period. ATR incidence for women increased by 58% over the whole study period, 26% from 2002 to 2012 and 30% from 2017 to 2021 (figure 1, table 1). The median age for women increased non-significantly from 46 to 49 years (p=0.10) throughout the study.
Age groups
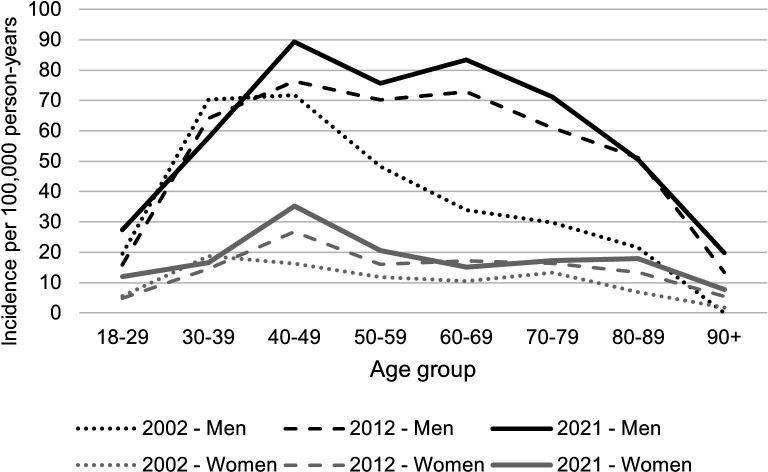
There were increasing incidence rates of ATR in most age groups throughout the study period, with decreasing rates only seen in the age group 30–39 years (table 2, figure 2).
Table 2. Age group ATR incidence rates and changes for men and women between 2002 and 2021 per 100 000 person-years.
| Age group (years) | Incidence rate | % change | P value | |
| 2002 (95% CI) | 2021 (95% CI) | |||
| Overall | ||||
| 18–29 | 12.7 (10.8 to 14.8) | 20.0 (17.8 to 22.4) | 57 | <0.0001 |
| 30–39 | 45.1 (45.1 to 41.5) | 37.8 (34.6 to 41.1) | −16 | 0.0029 |
| 40–49 | 44.5 (40.8 to 48.5) | 62.7 (58.5 to 67.2) | 41 | <0.0001 |
| 50–59 | 30.2 (27.2 to 33.4) | 48.5 (44.8 to 52.4) | 61 | <0.0001 |
| 60–69 | 22.0 (19.0 to 25.4) | 49.1 (45.1 to 53.4) | 123 | <0.0001 |
| 70–79 | 20.7 (17.5 to 24.4) | 43.4 (39.5 to 47.6) | 110 | <0.0001 |
| 80–89 | 12.4 (9.3 to 16.3) | 32.1 (27.2 to 37.6) | 159 | <0.0001 |
| 90+ | 1.3 (0 to 7.2) | 11.6 (6.2 to 19.8) | 795 | –* |
| Men | ||||
| 18–29 | 19.6 (16.3 to 23.3) | 27.4 (23.9 to 31.4) | 40 | 0.0024 |
| 30–39 | 70.4 (64.1 to 77.1) | 57.4 (52.4 to 63.5) | −18 | 0.0033 |
| 40–49 | 71.8 (65.2 to 78.9) | 89.2 (82.2 to 96.8)) | 24 | 0.0006 |
| 50–59 | 48.3 (43.0 to 54.0) | 75.6 (69.2 to 82.5) | 57 | <0.0001 |
| 60–69 | 34.0 (28.7 to 40.0) | 83.3 (75.9 to 91.3) | 145 | <0.0001 |
| 70–79 | 29.8 (24.0 to 36.5) | 71.2 (64.0 to 79.0) | 139 | <0.0001 |
| 80–89 | 21.5 (14.9 to 30.0) | 50.4 (41.2 to 61.0) | 134 | <0.0001 |
| 90+ | 0 (0 to 20.0) | 19.9 (8.0 to 40.9) | – | –* |
| Women | ||||
| 18–29 | 5.6 (3.9 to 7.7) | 11.9 (9.5 to 14.7) | 113 | 0.001 |
| 30–39 | 18.8 (15.5 to 22.5) | 16.7 (13.8 to 20.0) | −11 | 0.36 |
| 40–49 | 16.3 (13.2 to 20.0) | 35.2 (30.7 to 40.1) | 116 | <0.0001 |
| 50–59 | 11.8 (9.2 to 14.8) | 20.6 (17.3 to 24.4) | 75 | 0.0001 |
| 60–69 | 10.5 (7.7 to 14.0) | 15.0 (12.0 to 18.6) | 43 | 0.047 |
| 70–79 | 13.4 (10.0 to 17.6) | 17.3 (14.0 to 21.2) | 29 | 0.14 |
| 80–89 | 6.9 (4.1 to 10.9) | 17.9 (13.2 to 23.8) | 159 | 0.0003 |
| 90+ | 1.8 (0.033 to 7.2) | 7.8 (6.2 to 19.8) | 433 | –* |
A significance test was not performed because there was only 1one patient in the age group 90+ in 2002.
Figure 2. Achilles tendon incidence rates stratified by sex for the study period’s first, middle and last years.
Age groups between 18 and 79 years of both sexes demonstrated decreased proportions of surgical treatment of ATR. The overall number of injuries and proportion of surgical treatment per age group are presented in table 3.
Table 3. The number of ATR injuries and proportion of primary surgical treatment per age group for 2002 and 2021, with the percentage of change in ATR injuries and proportion of surgical treatment in the same period.
| Age group (years) | Number of ATR per year (% with primary surgical treatment) | % change, ATR injuries (surgical treatment) | |
| 2002 | 2021 | ||
| 18–29 | 163 (61) | 298 (29) | 83 (−53) |
| 30–39 | 575 (59) | 540 (20) | −6 (−67) |
| 40–49 | 522 (51) | 813 (15) | 56 (−70) |
| 50–59 | 378 (41) | 643 (13) | 70 (−68) |
| 60–69 | 191 (31) | 547 (9) | 186 (−70) |
| 70–79 | 143 (14) | 447 (9) | 213 (−39) |
| 0–89 | 52 (2) | 152 (3) | 192 (37) |
| 90+ | 1 (0) | 13 (0) | 1200 (–) |
ATR, Achilles tendon rupture
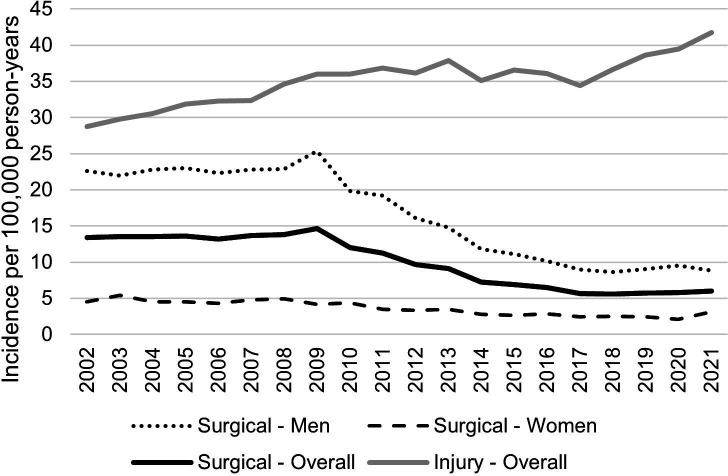
Incidence of surgical treatment of ATR
A total of 15 045 ATR surgical repairs were performed within 30 days of ATR diagnosis throughout the study period (82% men, n=12 269). The number of ATR surgeries decreased by 47%, from 942 surgeries in 2002 to 495 in 2021. This corresponded to a decrease in surgical treatment incidence rates from 13.4 in 2002 to 6.0 in 2021 per 100 000 person-years (95% CI 12.6 to 14.3 and 5.4 to 6.5, p<0.0001) (figure 3). The overall surgical treatment incidence rate was 13.4 in 2002, waning to 6.0 in 2021 per 100 000 person-years (95% CI 12.6 to 14.3 and 5.4 to 6.5, p<0.0001) (figure 3). The overall surgical incidence rate changed from 9.7 in 2012 to 5.7 in 2017 (95% CI 9.0 to 10.4 and 5.2 to 6.2, p<0,0001) and from 5.7 in 2017 to 6.0 in 2021 (p=0.45). The overall proportion of surgical-treated ATR cases decreased from 47% in 2002, 27% in 2012, 17% in 2017 and 14% in 2021.
Figure 3. Overall Achilles tendon injury and surgical incidence rates, overall and per sex, per year, per 100 000 person-years.
The male surgical incidence rate decreased from 22.6 in 2002 to 8.8 in 2021 per 100 000 person-years (95% CI 21.1 to 24.3 and 7.9 to 9.8, p<0.0001) (figure 3). Furthermore, surgical incidence rates changed from 16.1 in 2012 to 9.0 in 2017 (95% CI 14.9 to 17.4 and 8.1 to 10.0, p<0.0001) and from 9.0 to 8.8 in 2021 (p=0.85). The proportion of surgically treated men decreased from 49% in 2002, 28% in 2012, 17% in 2017 and 14% in 2021. For women, the surgical incidence rate decreased from 4.5 to 3.1 per 100 000 person-years throughout 2002–2021 (95% CI 3.8 to 5.3 and 2.6 to 3.7, p=0.001) (figure 3). For women, surgical incidence rates changed from 3.4 in 2012 to 2.4 in 2017 (95% CI 2.8 to 4.0 and 2.0 to 3.0, p=0.13) before reaching 3.1 in 2021 (p=0.063). The proportion of surgically treated women decreased from 37% in 2002, 22% in 2012 and 16% in 2017, reaching 16% in 2021.
Delay in ATR surgical repair
From 2002 to 2021, there was an overall increase in TTS of 719%, with TTS increasing from 0.6 days in 2002 to 5.1 days in 2021 (95% CI 0.5 to 0.8 and 4.6 to 5.6, p<0.0001) (online supplemental appendix 1). From 2012 to 2017, mean TTS increased from 2.9 days to 4.3 days (52%) (95% CI 2.6 to 3.2 and 3.9 to 4.9, p<0.0001), and from 2017 to 2021, mean TTS increased from 4.3 days in 2017 to 5.1 days in 2021 (16%) (p=0.043). Mean TTS in men changed from 0.5 to 5.0 days (900%) between 2002 and 2021 (95% CI 0.4 to 0.7 and 4.5 to 5.6, p<0.0001). Moreover, from 2012 to 2017, mean TTS increased from 2.9 to 4.4 (54%) (95% CI 2.6 to 3.2 and 3.9 to 5.0, p<0.0001), and from 4.4 to 5.0 days between 2017 and 2021 (14%) (p=0.17). In women, mean TTS increased from 1.1 to 5.2 days (373%) during the study period (95% CI 0.6 to 1.5 and 4.3 to 6.2, p<0.0001). Moreover, from 2012 to 2017, mean TTS increased from 3.0 to 4.3 days (44%) (95% CI 2.3 to 3.7 and 3.4 to 5.3, p=0.02) and from 4.3 to 5.2 days between 2017 and 2021 (22%) (p=0.15).
Delay of ATR diagnosis and surgical treatment
Out of the 15 045 patients surgically treated for ATR, 986 patients (6.6%) received a different initial injury diagnosis, which at a subsequent visit within 14 days was changed to S860. Using the time-point of the first different diagnosis rather than the initial recorded S860 for calculating TTS in those patients where this occurred resulted in an overall mean increase of 0.2 days for TTS per year.
Discussion
This nationwide register-based study on 53 688 ATR cases demonstrated a recent and long-term significant increase, with an overall increase of 45% in incidence rates between 2002 and 2021. A long-term decrease in surgical ATR treatment incidence rate, from 47% to stabilising around 15% in the last 5 years of the study, was found. Moreover, throughout the 20 years of the study, there was a 719% increase in the time from injury until surgical ATR repair, which could have a negative impact on patient-reported outcomes.20
The main finding of the present study is the significant long-term rise in incidence rates. The present Swedish data confirm those reported by other nationwide epidemiological studies of ATR. Colleagues from Finland4 reported a major increase in incidence rates from 17 in 1997 to 32 in 2019 (+87%), while Ganestam et al in Denmark1 reported a more modest increase in incidence rates from 27 to 31 between 1994 and 2013 (+16%). Moreover, a province in Canada and a sample of US hospitals showed marked and consistent increases in ATR incidence rates by 6%–10% per year.6 24 In contrast, recent East Asian studies (2009–2017) demonstrated moderate25 or no8 increases in ATR incidence, using data from health insurance claims. In fact, all recent European and Asian studies showed a plateau in ATR incidence after 2009. We could confirm such a plateau and even a 9% decrease in 2013–2017.
The data demonstrated a significant increase in ATR incidence of 21% from 2017 to 2021, marking a novel acceleration from the steadier long-term increase. The reasons behind the recent increase in incidence rates remain unclear. Still, they could be due to the notable surge in participation in the racquet sport Padel, as racquet sports increase the risk of ATR,26 with the number of unique individuals booking a court for Padel in Sweden increased from 33 990 to 540 000 between 2017 and 2021.27
The observed long-term rise in the ATR incidence rate is presumably related to increased participation in sports or recreational activities among women and people at older ages,28,30 evidenced by the higher incidence in women (58% vs 40% in men) and the shift in median injury age from 44 to 50 years. This observation is further substantiated by the fact that in 2002, the highest incidence was observed among patients aged 30–49 years, while by 2021, patients aged 40–80 years presented the highest increase and similar ATR incidence rates (figure 2). The transition to an increasingly older injury cohort seems to have been established by 2012, especially among those born between 1923 and 1952, who were aged 50–79 years in 2002 and thus 60–89 years of age in 2012. Both environmental and degenerative factors might explain this sharp increase. Degenerative changes, known to accumulate with increased age and metabolic conditions such as diabetes, increase the risk for ATR and could be an additional reason for the observed increase.31 The idea of degenerative changes within the tendon aligns with the staggering fivefold increase in ATR incidence in middle-aged Swedes (40–49 years in 2021) compared with when they were young adults (18–29 years in 2002; table 2). Similar findings were seen in Danish data comparing birth cohorts (69%–169% increase from 1994 to 2013).1 The 57% increase in ATR incidence in the youngest age group is intriguing and raises questions about whether this can be explained by altered sports habits alone or if intrinsic factors contribute. The decline in physical activity32 and rise in body mass index33 among younger Swedes may have compromised or subjected their tendons to an increased risk of rupture, as these are known risk factors for ATR.34 Future studies should try to separate intrinsic factors, including tendon quality, from factors related to sports trends. This might be achieved by cohort studies of register data spanning several decades.
The second main finding of this study was a major long-term decrease in primary surgical treatment of ATR of almost 50% overall and by two-thirds in age groups 30–69 years. The observed shift towards non-surgical treatment corroborates other studies in northern Europe and Canada at similar periods as the present study.1 2 4 6 Non-surgical treatment is favoured due to previous findings of comparable patient outcomes and fewer adverse events, although with a higher risk of re-rupture.1314 16,19 35 Contrastingly, recent data from both Japan and South Korea demonstrate an increase in surgical treatment by 5.4% and 28% from 2009 to 2017,8 25 explained by a higher degree of privately operated care in Japan and an inadequate outpatient healthcare structure for non-surgical early range mobilisation in South Korea. In the present study, the long-term decline in the rate of surgical treatment of ATR seems to have reached a plateau of around 15% of patients during 2017–2021. A long-term declining surgical trend might suggest that surgeons have either found a subset of patients preferred for surgical treatment, may have limited access to surgical options or appreciate the simplicity of non-surgical treatment with the knowledge of equivalent patient outcomes according to the recent meta-analyses. However, the smaller yet substantial decrease in surgical treatment of patients aged 18–29 years complies with the conception that younger individuals with more physical demands and fewer medical comorbidities would benefit more from surgical repair. To date, there is limited knowledge of how patient characteristics or other factors can guide surgeons in determining which patients would benefit most from surgical ATR repair. A shift towards non-surgical treatment for ATR possibly leads to an increased number of re-ruptures. However, this likely does not fully explain the sharp increase in incidence since 2017, as the decrease in surgical treatment was slight, from 17% to 14% during the same period. Moreover, as most re-ruptures occur within 1 year,36 37 subsequent entries in the register are likely contralateral ruptures and should be counted anew.
Perhaps the most notable finding of this study was the demonstration of a significant increase in the delay from injury to surgical treatment by 719%, from an average of 0.6 days to 5.1 days throughout the study period. To our knowledge, TTS has not previously been reported in a nationwide register study for ATR. However, increased TTS has previously been associated with impaired patient-reported outcomes and more complications, which suggest a possible disturbance in the healing process of the tendon if surgery is performed at a later stage of healing.20 An experimental study on Achilles tendon in a rat model verified how improved biomechanical and histological properties occurred if surgical repair was performed after 48 hours of injury.38 The underlying reasons for the increased TTS could be due to increasingly limited access to hospital emergency departments and in-hospital orthopaedic expertise and increasingly limited surgical resources following the underprioritisation of ATR for surgical treatment. Whether increased TTS impacts patient outcomes necessitates further verification but may warrant changes in practice guidelines when surgery on ATR patients should be performed. Furthermore, all comparisons between surgically and non-surgically treated ATR patients may require revision to consider TTS.
This study extends the knowledge of earlier registry studies, especially the results of Huttunen et al,2 which reported ATR incidence trends in Sweden between 2001 and 2012. Some differences exist between these studies. The discrepancy of slightly higher incidence rates could be attributed to methodological differences. The present study included ATR diagnosis from any of the 30 code positions in the register, not limited to primary or secondary positions. Re-entries were permitted 365 days after the first rupture, as patients with a previous ATR have an increased risk of contralateral rupture.39 40
Strength and limitations
The strength of the present study lies in its use of a nationwide register, setting it apart from other studies that rely on insurance or regional data. This enhances the reliability and generalisability of the results and limits selection bias related to socioeconomic, geographical or ethnic factors. The observed increases in TTS were corroborated by randomised controlled trials conducted at our clinic between 2010 and 2018 for operated ATR. Limitations of this study, as with any register-based study, are the retrospective design and the risk of misdiagnosis or incorrect entries in the register. However, the SNPR is reported to be of high quality,21 and any misclassification for the main outcome should not affect the results in any major way. The high quality of the SNPR further strengthens the findings, as the incidence rates were calculated based on the exact number of Swedish males and females in any specific year. Moreover, efforts were made to ensure correct coding in operated cases, which demonstrated how temporary diagnoses were used sparingly until definitive diagnosis. The SNPR does not distinguish between the left or right side, which may limit it for re-ruptures and contralateral injury estimations. Moreover, the SNPR do not contain patient outcome variables, such as questionnaires or functional tests, which are essential for assessing the impact of different treatment modalities. Incorporating such variables would enable data segmentation based on different patient characteristics, facilitating a deeper understanding of the significance of an individualised care protocol for ATR.
Clinical implications
The decreased surgery rate and the increased number of tendon ruptures demand increased resources to optimise and treat non-operated ATR patients of all ages. The marked delay of surgical cases shown in Sweden calls for the priority of diagnosis and surgery of these limited cases and underscores the need to research the impact of delayed surgical treatment on patient outcomes.
Conclusions
The incidence rate of ATR demonstrated both a long-term and a recent rise while an increasing median age at rupture. Concurrently, the rate of surgical treatment of ATR showed a steady decline to reach a plateau in the last 5 years of this study. Moreover, the time from injury to surgical treatment has significantly increased over the past 20 years.
supplementary material
Footnotes
Funding: Funding was received from the regional agreement on medical training and clinical research (ALF) dnr RS 2019-1054 to author LF-T and FoUI-960998 to author PWA.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study was approved by Stockholm regional ethics committee (Dnr: 2013/581-31, 2020/06182, 2022-04877-02). The study is based on register data and does not require patient consent.
Data availability free text: The data analysed in this study were extracted from the Swedish national patient register and are not publicly available but can be acquired via a third party. To obtain permission to access data, specific requirements must be met per Swedish law, including only reporting aggregated data in scientific articles as a precaution to safeguard the anonymity of the individuals in the dataset. For these reasons, data cannot be made generally available.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Simon Svedman, Email: simon.svedman@gmail.com.
Alejandro Marcano, Email: Alejandro.marcano@regionstockholm.se.
Paul W Ackermann, Email: paul.ackermann@ki.se.
Li Felländer-Tsai, Email: li.fellander-tsai@ki.se.
Hans Erik Berg, Email: hans.er.berg@regionstockholm.se.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.Ganestam A, Kallemose T, Troelsen A, et al. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. a nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24:3730–7. doi: 10.1007/s00167-015-3544-5. [DOI] [PubMed] [Google Scholar]
- 2.Huttunen TT, Kannus P, Rolf C, et al. Acute Achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419–23. doi: 10.1177/0363546514540599. [DOI] [PubMed] [Google Scholar]
- 3.Lantto I, Heikkinen J, Flinkkilä T, et al. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25:e133–8. doi: 10.1111/sms.12253. [DOI] [PubMed] [Google Scholar]
- 4.Leino O, Keskinen H, Laaksonen I, et al. Incidence and treatment trends of Achilles tendon ruptures in Finland: a nationwide study. Orthop J Sports Med. 2022;10:23259671221131536. doi: 10.1177/23259671221131536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:277–9. doi: 10.3109/17453679608994688. [DOI] [PubMed] [Google Scholar]
- 6.Sheth U, Wasserstein D, Jenkinson R, et al. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27 607 patients. Bone Joint J. 2017;99-B:78–86. doi: 10.1302/0301-620X.99B1.BJJ-2016-0434.R1. [DOI] [PubMed] [Google Scholar]
- 7.Suchak AA, Bostick G, Reid D, et al. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26:932–6. doi: 10.1177/107110070502601106. [DOI] [PubMed] [Google Scholar]
- 8.Yamaguchi S, Kimura S, Akagi R, et al. Increase in Achilles tendon rupture surgery in Japan: results from a nationwide health care database. Orthop J Sports Med. 2021;9:23259671211034128. doi: 10.1177/23259671211034128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 2010:CD003674. doi: 10.1002/14651858.CD003674.pub4. [DOI] [PubMed] [Google Scholar]
- 10.Lo IK, Kirkley A, Nonweiler B, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a quantitative review. Clin J Sport Med. 1997;7:207–11. doi: 10.1097/00042752-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Zhao HM, Yu GR, Yang YF, et al. Outcomes and complications of operative versus non-operative treatment of acute Achilles tendon rupture: a meta-analysis. Chin Med J (Engl) 2011;124:4050–5. [PubMed] [Google Scholar]
- 12.Westin O, Nilsson Helander K, Grävare Silbernagel K, et al. Patients with an Achilles tendon re-rupture have long-term functional deficits and worse patient-reported outcome than primary ruptures. Knee Surg Sports Traumatol Arthrosc. 2018;26:3063–72. doi: 10.1007/s00167-018-4952-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng S, Sun Z, Zhang C, et al. Surgical treatment versus conservative management for acute Achilles tendon rupture: a systematic review and meta-analysis of randomized controlled trials. J Foot Ankle Surg. 2017;56:1236–43. doi: 10.1053/j.jfas.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 14.Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soroceanu A, Sidhwa F, Aarabi S, et al. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94:2136–43. doi: 10.2106/JBJS.K.00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng H, Cheng X, Yang Y, et al. Rerupture outcome of conservative versus open repair versus minimally invasive repair of acute Achilles tendon ruptures: a systematic review and meta-analysis. PLoS One. 2023;18:e0285046. doi: 10.1371/journal.pone.0285046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meulenkamp B, Woolnough T, Cheng W, et al. What is the best evidence to guide management of acute Achilles tendon ruptures? A systematic review and network meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2021;479:2119–31. doi: 10.1097/CORR.0000000000001861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reda Y, Farouk A, Abdelmonem I, et al. Surgical versus non-surgical treatment for acute Achilles' tendon rupture. A systematic review of literature and meta-analysis. Foot Ankle Surg. 2020;26:280–8. doi: 10.1016/j.fas.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Seow D, Yasui Y, Calder JDF, et al. Treatment of acute Achilles tendon ruptures: a systematic review and meta-analysis of complication rates with best- and worst-case analyses for rerupture rates. Am J Sports Med. 2021;49:3728–48. doi: 10.1177/0363546521998284. [DOI] [PubMed] [Google Scholar]
- 20.Svedman S, Juthberg R, Edman G, et al. Reduced time to surgery improves patient-reported outcome after Achilles tendon rupture. Am J Sports Med. 2018;46:2929–34. doi: 10.1177/0363546518793655. [DOI] [PubMed] [Google Scholar]
- 21.Südow H, Sjödin L, Mellstrand Navarro C. Validity of distal radius fracture diagnoses in the Swedish National patient register. Eur J Med Res. 2023;28:335. doi: 10.1186/s40001-023-01314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . International statistical classification of diseases and related health problems, tenth revision. Geneva: World Health Organization; 1994. [PubMed] [Google Scholar]
- 23.NOMESCO NOMESCO classification of surgical procedures. 2011. [15-Oct-2023]. http://norden.diva-portal.org/smash/get/diva2:968721/FULLTEXT01.pdf Available. Accessed.
- 24.Lemme NJ, Li NY, DeFroda SF, et al. Epidemiology of Achilles tendon ruptures in the United States: athletic and Nonathletic injuries from 2012 to 2016. Orthop J Sports Med. 2018;6:2325967118808238. doi: 10.1177/2325967118808238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park HG, Youn D, Baik JM, et al. Epidemiology of Achilles tendon rupture in South Korea: claims data of the national health insurance service from 2009 to 2017. Clin Orthop Surg. 2021;13:539–48. doi: 10.4055/cios20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Larsson E. A narrative review of Achilles tendon ruptures in racket sports. Int J Racket Sports Sci. 2022 doi: 10.30827/Digibug.76979. [DOI] [Google Scholar]
- 27.Padelförbundet Sverige Statistik: Svenska Padelförbundet. 2023. https://svenskpadel.se/om-padel/statistik/ Available.
- 28.Calatayud J, López-Bueno R, Núñez-Cortés R, et al. Trends in adherence to the muscle-strengthening activity guidelines in the US over a 20-year span. Gen Hosp Psychiatry. 2023;84:89–95. doi: 10.1016/j.genhosppsych.2023.06.016. [DOI] [PubMed] [Google Scholar]
- 29.Leijon M, Midlöv P, Sundquist J, et al. The longitudinal age and birth cohort trends of regular exercise among adults aged 16-63 years in Sweden: a 24-year follow-up study. Popul Health Metr. 2015;13:18. doi: 10.1186/s12963-015-0049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vilhelmson B, Thulin E, Elldér E. Time change in the distribution of physical activity and its correlates among retired older Swedish adults: a repeated cross-sectional study from a national survey. BMC Public Health. 2022;22:2055. doi: 10.1186/s12889-022-14554-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paul W. Metabolic influences on risk for tendon disorders. Springer Cham; 2016. Advances in experimental medicine and biology. [Google Scholar]
- 32.Nyberg G, Kjellenberg K, Fröberg A, et al. A national survey showed low levels of physical activity in a representative sample of Swedish adolescents. Acta Paediatr. 2020;109:2342–53. doi: 10.1111/apa.15251. [DOI] [PubMed] [Google Scholar]
- 33.The Public Health Agency of Sweden Övervikt och Fetma. [10-Nov-2023]. https://www.folkhalsomyndigheten.se/faktablad/BMI-ULF-SILC/ Available. Accessed.
- 34.Ahn HS, Kim HJ, Suh JS, et al. The association of body mass index and waist circumference with the risk of Achilles tendon problems: a nationwide population-based longitudinal cohort study. Clin Orthop Surg. 2023;15:488–98. doi: 10.4055/cios22238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles' tendon rupture. N Engl J Med. 2022;386:1409–20. doi: 10.1056/NEJMoa2108447. [DOI] [PubMed] [Google Scholar]
- 36.Maempel JF, White TO, Mackenzie SP, et al. The epidemiology of Achilles tendon re-rupture and associated risk factors: male gender, younger age and traditional Immobilising rehabilitation are risk factors. Knee Surg Sports Traumatol Arthrosc. 2022;30:2457–69. doi: 10.1007/s00167-021-06824-0. [DOI] [PubMed] [Google Scholar]
- 37.Pajala A, Kangas J, Ohtonen P, et al. Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am. 2002;84:2016–21. doi: 10.2106/00004623-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Misir A, Kizkapan TB, Arikan Y, et al. Repair within the first 48 H in the treatment of acute Achilles tendon ruptures achieves the best biomechanical and histological outcomes. Knee Surg Sports Traumatol Arthrosc. 2020;28:2788–97. doi: 10.1007/s00167-019-05536-w. [DOI] [PubMed] [Google Scholar]
- 39.Arøen A, Helgø D, Granlund OG, et al. Contralateral tendon rupture risk is increased in individuals with a previous Achilles tendon rupture. Scand J Med Sci Sports. 2004;14:30–3. doi: 10.1111/j.1600-0838.2004.00344.x. [DOI] [PubMed] [Google Scholar]
- 40.Palma J, Villa A, Freundlich A, et al. Are patients presenting with an Achilles tendon rupture at greater risk of rupturing their contralateral tendon? A retrospective cohort study with minimum 2 years follow-up. Foot Ankle Orthop . 2018;3:2473011418S0009. doi: 10.1177/2473011418S00095. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data may be obtained from a third party and are not publicly available.