Abstract
There is a rich history of cancer treatments which provides a number of important lessons for present and future cancer therapies. We outline this history by looking in the past, reviewing the current landscape of cancer treatments, and by glancing at the potential future cancer therapies.
Introduction
There are a number of rationally devised cancer treatments which were introduced over the last few centuries. Many cancer therapies introduced a long time ago are still relevant and are still used in oncology practice. We review cancer treatments by looking at therapies introduced before 1970, between 1970 and 2023, and the potential future cancer therapies. 1970 was selected as a demarcation mark because that year tamoxifen, the first important non-cytotoxic small molecule therapeutic, entered clinical trial with the intent to treat breast cancer1. Tamoxifen is a selective estrogen receptor modulator known in the 1970s as ICI-46474. The success of tamoxifen initiated the era of molecularly targeted cancer treatments.
Improvements in understanding of the complexity of cancer biology have been instrumental in advancing cancer treatments. Cancer is primarily driven by oncogenic somatic and/or germline alterations in oncogenes and tumor suppressor genes. There are many different tumor types, and the majority of tumors have multiple oncogenic alterations with significant degree of intra and inter tumor heterogeneity. Oncogenic alterations have multiple effects, including increase in proliferative signaling, resistance to cell death, bypassing replicative limit, increase in genome instability. Hanahan and Weinberg described these and other hallmarks of cancer, such as evasion of immune surveillance, and their implications for cancer treatments2.
Cancer treatments introduced prior to 1970
Surgery was the first rational cancer treatment. Surgery started to evolve into a modern form after anesthesia and antisepsis became available in 19th century3. Surgical techniques improved over time with better understanding of cancer biology, improvements of imaging capabilities, and surgical instruments. Improvements in early cancer detection contributed to the increase in the effectiveness of surgical procedures4. Surgical procedures in oncology have a variety of goals: preventive as for example removal of potentially pre-cancerous colorectal polyps, potently curative in cases of localized tumors, debulking larger tumors, and palliative. Surgeries have risks of mortality and morbidity; such risks vary by surgery type and extent. Minimally invasive surgeries, laser ablation, cryoablation, can help to minimize such risks. Some surgical procedures which were commonly used in the past, for example radical mastectomy, are now used only in a small subset of cases, after clinical trials proved that in the majority of cases less extensive surgery is equally effective and results in fewer side effects.
Interest in radiation as a treatment modality for cancer was initiated shortly after X-ray discovery in 1895 by Wilhelm Conrad Röntgen. Marie and Pierre Curie’s radioactivity research and isolation of radioactive elements helped to lay the foundation for using radiation as a treatment for cancer in the beginning of 20th century5. There are multiple types of cancer radiation treatments including: x-rays, proton beams, fast neutron therapy beams, radionuclide therapy (such as Iodine-131), brachytherapy and systemically delivered radionuclides conjugated to antibodies. Brachytherapy involves implanting sealed radioactive seeds and is usually done as an outpatient minimally invasive surgical procedure; however, brachytherapy can be employed as part of an extensive surgical procedure6. Radiation therapy is often administered as adjuvant therapy after initial surgical treatment, however radiation therapy can also be used with curative or palliative intent, and as neoadjuvant therapy prior to surgical treatment.
Radiation therapy is cytotoxic to cancer cells because it leads to DNA strand breaks leading to cell death. For therapeutic treatment radiation is delivered to the tumor mass and treatments are planned carefully to minimize normal tissue radiation exposure; however, such exposure is usually unavoidable and results in a number of side effects. Normal tissue fibrosis and potentially secondary malignancies as a late sequalae of radiation treatment are known. Radiation therapy to the head may cause cognitive decline, especially in young pediatric patients.
Anticancer chemotherapy development started in the first half of 20th century; based in part on observations of bone marrow and lymph nodes depletion in people exposed to mustard gas during World War I (WWI) chemical warfare and exposure to mustard gas after bombing of US naval ship loaded with mustard gas munition at Bari Harbor, Italy, in 1943 during WWII7. Initial articles on nitrogen mustard chemotherapy in patients for treatment of cancer were published in 19468. Nitrogen mustard (mechlorethamine) is a bi-functional alkylating agent, and its mechanism of action is based on producing DNA double strand crossing-links. Folate antagonists such as methotrexate were tested in children with acute leukemia a few years later9.
Purine antimetabolites were developed in 1950s10,11. In the same decade observation of preferential uptake of uracil by tumors in comparison with normal tissue triggered the development of the fluoropyrimidine 5-fluorouracil (5-FU)12. During this time, the search for new cancer therapies became more organized and scientific. In the mid-1960s, Skipper and his group reported on the criteria for “curability” and on the kinetics of leukemic cells in mice. The criteria described were derived directly from the behavior of bacterial cell populations exposed to antibacterial agents and were based on findings in mice bearing intraperitoneally implanted murine L1210 or P388 leukemia cells13. Rodent solid tumor models, some highly metastatic followed a few years later14,15. Tubulin inhibitors were developed in the beginning of the 1960s16, followed by new alkylating chemotherapies such as procarbazine17,18, and development of topoisomerase 1 and 2 inhibitors19. Exploration of combination chemotherapy regimens in the middle of 1960s propelled major improvement in the efficacy of cancer treatments shifting them from short term transient benefits to sustained remissions20,21,22. First combination chemotherapy regimens were primarily used in childhood leukemia and were followed by development of MOMP (mechlorethamine, vincristine (Oncovin), melphalan and prednisone) and MOPP (mechlorethamine, vincristine (Oncovin), procarbazine and prednisone) protocols for treatment of Hodgkin’s lymphoma23. Also, around the same time, clinical efforts started on integrating radiation therapy and combination chemotherapy regimens24.
Chemotherapy is most lethal to fast growing cells, which means that many side effects are especially noticeable in normal cells with high proliferation, such as hematopoietic cells, upper and lower gastrointestinal tract cells, and hair follicles25. Chemotherapy side effects may include nausea and vomiting, fatigue, oral and gastrointestinal mucositis, anemia, increased risk of infections, increased risk of cardiovascular disease, and central and peripheral neurotoxicity, among others. Many chemotherapies induce DNA damage, and as a result there is a risk of secondary malignancies.
In some tumor types, combination chemotherapy regimens are highly effective, for example in childhood leukemia. However, in many advanced non-pediatric malignancies, duration of remissions is limited. Due to critical normal tissue toxicities, dose reduction, treatment delay or in some cases, treatment cessation are necessary. In some relatively rare instances, local chemotherapy delivery such as intrathecal chemotherapy is a possibility, and it helps to limit systemic side effects.
Allogeneic hematopoietic stem cell transplantation (HSCT) for cancer treatment was first evaluated clinically in the 1950s26,27. In the 1960s, methods to identify and type human leukocyte antigens (HLA) were developed which enabled HLA matching between donor and recipient, and initiated major improvements in allogeneic HSCT28,29. Prior to allogeneic HSCT, high dose chemotherapy or a combination of chemotherapy and radiotherapy are administered to suppress the recipient immune system, in order to prevent graft rejection via graft versus host disease and treat the malignancy. The intensity of such pre-transplantation treatments is adjusted based on patients age, and other factors. Non-relapse related mortality two years after allogeneic HSCT has decreased from about 32% in 1980 to about 15% in 2016; infections, graft vs host disease, and multi-organ failure are main causes of mortality. Two-year overall survival after allogeneic HSCT has increased from about 46% in 1980 to about 62% in 2016, graft vs tumor activity is considered to be an important factor in improving overall survival30.
After observations of highly effective and durable responses to combination chemotherapy regimens and combined modality regimens with chemotherapy and radiation therapy in pediatric patients, there was some hope of obtaining the same level of clinical benefits for the majority of adult-onset malignancies. However, with time it became clear that while combination chemotherapy regimens and combination of chemotherapy with radiation therapy and surgery might result in highly effective and durable responses for some patients, especially with early-stage cancers, for the majority of patients remissions had limited duration. These observations required some re-thinking of the concept of cancer cell killing called the “log-kill hypothesis”. This hypothesis stated that when the growth of a tumor is exponential then when treated with effective anticancer drugs, the tumor shrinks by a constant fraction that is a constant logarithmic amount31.
At the end of 1960s first successful human tumor xenograft models were developed, taking advantage of immunocompromised strains of mice32. There are few advantages of using human tumor xenografts: malignant cells are of human tumors origin, a variety of tumor lines are available, the hosts are readily available, and statistically valid numbers of mice can be used in studies resulting in reasonably reproducible outcomes15. In some instances it is important to place tumor cells in the appropriate anatomical location, in such cases instead of subcutaneous tumor implants, human tumor xenografts can be implanted in the relevant orthotopic site33. Human tumor xenograft models, and later developed patient-derived xenografts (PDX), in which human cancers are directly engrafted into a immunocompromise mouse without in-vitro cell line creation, became important models for cancer treatments development and efficacy evaluation34.
Cancer treatments introduced between 1970 and 2023
Pharmacological hormone therapies that remove hormones or block their action have been under development since the 1960s. In 1970, tamoxifen, a selective estrogen receptor modulator, entered the first clinical trial with intent to treat breast cancer. Additional classes of pharmacological hormone treatments for breast cancer have been developed, including estrogen receptor degraders, aromatase inhibitors, and luteinizing hormone-releasing hormone (LHRH) agonists. Hormone therapies for breast cancer played a major role in significant decrease of breast cancer mortality35. Multiple classes of pharmacological hormone treatments for prostate cancer have also been developed, including androgen receptor antagonists, LHRH agonists, LHRH antagonists, and CYP17 inhibitors36. Side effects of hormone therapies may include the loss of bone density, blood clots, and insulin resistance, among others.
The development of treatments targeting genes with oncogenic alterations and related signaling pathways, based on advances in understanding of molecular cancer biology, was a major step in cancer treatment evolution. The first such treatment was trastuzumab, a monoclonal antibody against the extracellular domain of the transmembrane receptor ERBB2, also known as HER237. Trastuzumab (Herceptin) entered initial clinical trial in 1992 and was approved by FDA in 1998. In 2001 imatinib (Gleevec), an ABL1 kinase inhibitor, became the first FDA approved small molecule growth signal inhibitor for cancer treatment38. Many targeted treatments have been developed since then, including inhibitors of EGFR, BRAF, MAP2K1, ALK, etc. Most such treatments are based on presence of oncogenic alterations in relevant gene(s). Supplemental Table 1 lists genes with oncogenic alterations for which targeted treatments are available as monotherapy or part of combination therapy in at least one indication. For successful deployment of many targeted therapies, it is essential for patients and oncologists to have timely access to tumor sequencing data and properly performed analysis of such data, and it is also preferable to have access to well-structured molecular tumor board39,40,41. Some targeted molecular treatments are used for specific cancer subtypes, for example drugs targeting BCL-2, BTK, CDK4, SMO, HDAC, VEGF, JAK-2; this is especially the case for monoclonal antibodies targeting hematopoietic subtypes lineage markers such as CD20, CD52, and CD38.
The efficacy of targeted inhibitors varies significantly across tumor types. CML is one of the few indications in which targeted inhibitors transformed a previously almost uniformly lethal cancer into a manageable disease for the majority of patients with long term survival over 90%42. ABL1 inhibitors have been very successful in chronic phase CML, which can be detected early and is driven by a single genetic alteration - BCR-ABL fusion43. However, ABL1 inhibitors do not provide meaningful benefit in blast phase CML which is driven, in part, by additional genetic alterations in the tumor suppressors and/or transcription factors TP53, CDKN2A, CDKN2B, IKZF1 and RUNX1. There are essentially no successful therapies to substitute for the loss of function of these genes. Nearly all tumors are driven by multiple genetic alterations, however, currently only a subset of genetic alterations can specifically be targeted by drugs. The inability to target a number of key oncogenic alterations is one of major limitations of targeted inhibitors, in addition to acquired resistance to treatments after initial clinical benefits, as well as treatment-induced on target and off target toxicities.
Photodynamic therapy, also known as photochemotherapy, is based on a photosensitizer drug which is non-toxic until it is activated locally by light of a specific wavelength. Such an approach allows limited toxic exposure of normal tissues44. The first photosensitizer drug approved by FDA in 1994 was porfimer sodium. Currently there are multiple photosensitizer drugs approved for clinical use.
Antibody drug conjugates (ADC) have the potential of decreasing systemic toxicities due to preferential tumor delivery by binding to a protein found only on the cell surface of tumor cells, while delivering highly toxic payload which otherwise would not be possible to administer at sufficiently high concentration. The first ADC was approved in 2000 by FDA, targeting CD33, and at this point more than 10 ADCs have been approved for clinical use45. The toxic payload can be attached using cleavable or non-cleavable linkers. Non-cleavable linkers are associated with lower levels of systemic toxicity, while cleavable linkers might allow bystander killing due to toxic payload release into the tumor microenvironment.
An immune checkpoint inhibitor antibody targeting CTLA-4 was approved by FDA in 2011 and initiated renewed interest in immune system stimulation based treatments. In following years additional antibodies targeting immune checkpoint inhibitors such as PD-1, PD-L1, LAG-3 entered clinical practice46,47,48. Immune checkpoint inhibitors have provided significant, and often durable benefits for many cancer patients; however, the response rate is about 15% to 40% in most solid tumors and 40% to 60% in melanoma and tumors with high mutation rates due to impaired DNA repair such as for example mismatch repair (MMR) deficient tumors. Overall, about 10% to 15% of cancer patients benefit from immune checkpoint inhibitors. Acute and chronic immune-related toxicities are some of the potential side effects of immune checkpoint inhibitor treatments49.
Bispecific T-cell engagers (BiTEs) recruit T cells to tumor cells by simultaneously targeting CD3 molecule and tumor antigen50. The first BiTE was approved by FDA in 2014, it was designed to target CD19 which is expressed on B-cells. BiTEs targeting CD20, CD326 (EpCAM), BCMA, PMEL (GP100) have been later approved by FDA. It is interesting to note that PMEL, also known as SILV, has been previously identified by multiple groups as an ADC target in melanoma51,52. BiTEs therapy can also cause cytokine storm syndrome, neurotoxicity, and on-target off-tumor toxicity.
The first oncolytic virus therapy was approved by FDA in 2015, this particular therapy talimogene laherparepvec (T-VEC) is a genetically engineered herpes virus type 1 (HSV-1). T-VEC has two viral genes encoding for ICP34.5 and ICP47 removed, and the gene encoding human granulocyte-macrophage colony stimulating factor (GM-CSF) added53. ICP47 suppresses the immune response to viral infections, ICP34.5 blocks stress response to viral infections and its deletion prevents T-VEC from replication in normal cells and allows preferential replication in tumor cells which in some cases have disrupted stress response. Oncolytic virus therapy side effects are similar to symptoms due to viral infections.
In 2017 177Lu-DOTATATE became the first peptide receptor radionuclide therapy approved for clinical use54. In 2022 FDA approved 177Lu-PSMA-617 for the treatment of patients with prostate specific membrane antigen (PSMA) positive metastatic castration-resistant prostate cancer55. In the 1990s, intensity-modulated radiation therapy (IMRT) was developed. IMRT improves the ability to conform the treatment volume to tumor shapes and decreases radiation to neighboring normal tissues56. Volumetric modulated arc therapy (VMAT) was introduced in 2007; VMAT improves the IMRT delivery efficiency and shortens treatment times57.
In 2017 FDA approved chimeric antigen receptor T cell (CAR-T) therapy against B cell malignancies targeting CD19. Also, CAR-T therapy targeting BCMA has been later approved for clinical use. CAR-T is based on extracting patients T-cells, modifying them with chimeric receptor targeting particular tumor antigen, and infusing modified T-cells back into the patient58. First CAR-T cells were engineered in the 1990s, and first clinical use was in 2005, however administration did not result in clinical benefits. In order to increase the potency of CAR-T cells, several key modifications were introduced, including the addition of co-stimulatory domain, which helped to increase CAR-T cells expansion and persistence after infusion into patients59. There are multiple mechanisms of resistance to CAR-T therapies, including loss of targeted antigen and immunosuppressive response. CAR-T therapy in some instances can provide long term durable benefits, CAR-T therapy can also cause cytokine storm syndrome, neurotoxicity, and on-target off-tumor toxicity58.
Another important development was the introduction of genomic tests, which provide biomarkers driven assistance in guiding treatment decisions. Such genomic tests include PAM50 and Oncotype DX, which are used in breast cancer60. De-escalating and escalating treatments can therefore be potentially guided by genomic tests61.
In the last 60 years, cancer models have become better at modeling the biology of tumors, and cancer treatments have become more targeted, as shown in Figure 1.
Figure 1.

Trends in better cancer models and more targeted cancer treatments.
The advent of targeted therapies resulted in significant improvement in cancer treatment efficacy, increases in remissions duration, decreases in treatments toxicities, and marked by decreases in cancer mortality. For a few malignancies, like CML, where early detection is currently possible, targeted therapies provided the most transformational outcomes. However, due in part to multiple mechanisms of resistance, efficacy of targeted therapies is often limited.
Future of Cancer treatments
Surgery is likely going to continue to be an important cancer treatment modality for the foreseeable future, especially keeping in mind the likely increase in fraction of cancers detected early due in part to advances in circulating tumor-derived DNA (ctDNA) analysis62 and imaging technologies. The ctDNA analysis will likely need to include examination of ctDNA for oncogenic alterations, in addition to methylation and fragmentation analysis, to achieve clinically relevant levels of specificity. Approaches currently under development to better determine tumor margins should help to increase the efficacy of surgical procedures. Further improvements in minimally invasive procedures and other surgical techniques should help to decrease the morbidity and mortality of surgical procedures.
Radiation therapy is likely going to continue to be an important cancer treatment modality for the foreseeable future. New techniques such as flash radiotherapy63, the probable increase in use of unsealed radionuclide therapies, and improvements in minimizing radiation exposure to normal tissues are likely going to help to increase the efficacy and decrease the toxicities associated with radiation therapy.
Chemotherapy is likely going to continue to be an important cancer treatment modality for the foreseeable future, as demonstrate, in part, by unfortunate recent instances of shortages of a number of chemotherapeutic drugs. New formulations, better release control, local administration may help to increase efficacy and decrease toxicities of existing chemotherapeutic agents.
Allogeneic hematopoietic stem cell transplantation is likely going to continue to be an important cancer treatment modality for the foreseeable future. Improvements in HLA matching, managing infections, and managing graft vs host disease will likely help to continue the trend of decreases of non-relapsed related mortality.
Pharmacological hormone therapy is likely going to continue to be an important cancer treatment modality for the foreseeable future. Hormone therapies are an important part of treatment protocols for breast, endometrial, and prostate cancers.
Treatments targeting genes with oncogenic alterations and related signaling pathways are going to continue to be an important cancer treatment modality for the foreseeable future since cancer is a genetic disease driven by oncogenic alterations. There are number of new classes of targeted cancer treatments under development, for example: MAPK1 (ERK) inhibitors, PTPN11 (SHP2) inhibitors, KRAS G12D inhibitors and degraders, RAS(ON) inhibitors, ATR inhibitors, ATM inhibitors, PCNA inhibitors, MYC interaction inhibitors, MDM2/TP53 interaction inhibitors in TP53 WT tumors, spliceosome inhibitors, CLDN 18.2 targeting monoclonal antibodies. Recent efforts transitioning drug development thinking from the maximal tolerated drug dose (MTD) to the lower more precise biologically sufficient dose may help to decrease on-target and off-target normal tissue toxicities. Proteolysis-targeting chimeras (PROTACs) and molecular glue degraders might add additional approach for development of targeted cancer treatments64,65. MRT-2359 is an example of a molecular glue degrader targeting the translation termination factor GSPT1 which is under development. Using measurable/minimal residual disease (MRD) to personalize treatment duration might also help to improve effectiveness of treatments66.
Antibody drug conjugates are likely going to continue to be an important cancer treatment modality for the foreseeable future. There are more than 100 new ADCs under development, some of the targets are: CD20, CD22, CD123, CEACAM5, EphA3. The application of radioligands as the toxic payload is under development, and a possibility of simultaneously attaching different toxic payloads to antibody is being considered. Bispecific antibodies may also provide additional improvements. One of the inherent difficulties in ADC development is identifying cell surface targets with sufficiently high expression on tumor cells and sufficiently low expression on normal cells.
Immune checkpoint inhibitors are likely going to continue to be an important cancer treatment modality for the foreseeable future. TIGIT is one of the newer targets for immune checkpoint inhibitors67. Combinations of different immune checkpoint inhibitors, and combinations of immune checkpoint inhibitors with cancer vaccines may help to increase efficacy and the percentage of patients who might benefit from immune checkpoint inhibitors.
Bispecific T-cell engagers are likely going to continue to be an important cancer treatment modality for the foreseeable future. There are a number of new BiTEs under development, these are some of the targets: PSMA, EGFRvIII, CLDN18.2, GD2, DLL368,69. As with ADCs one of the inherent difficulties with BiTEs development is finding the targets with sufficiently high expression on tumor cells and sufficiently low expression on normal tissues cells.
Oncolytic virus therapy is likely going to continue to be available as a cancer treatment modality for the foreseeable future. There are multiple oncolytic virus therapies under development, for example BT-001, RP1, and Teserpaturev/G47Δ (conditionally approved for clinical use in Japan)70. Combining oncolytic virus therapies with immune checkpoint inhibitors is one of the potentially most promising strategies71, 72.
Chimeric antigen receptor T cell therapy is likely going to continue to be an important cancer treatment modality for the foreseeable future. There are several new CAR-Ts under development, these are some of the targets: CD20, CD22, DLL3, CLDN6, CLDN18.2. Currently a large infrastructure is necessary for CAR-Ts production, which makes CAR-T cells rather expensive, there are few efforts under development which might help to decrease cost of CAR-T cell treatments. Armored CAR-T cells can secrete cytokines or express cytokine receptors and may potentially increase efficacy, especially against solid tumors73. As with ADCs and BiTEs, one of the inherent difficulties in CAR-T cell development is on-target, off-tumor toxicity. Development of Boolean logic antigen engagement control for CAR-T cells might enable decrease in on-target off-tumor toxicity74. A recently developed 2-part approach might enable CAR-T cells to target all blood cancer malignancies. CAR-T cells are developed against an antigen present on all blood cancers, for example CD45, CAR-Ts CD45 is modified so CAR-Ts would not target each other; also, CD45 in hematopoietic stem cells is modified so CAR-Ts would not target them, and modified hematopoietic stem cells are used to repopulate patient bone marrow75.
Cancer vaccines have been in development for a few decades, recent technological developments allow reasonably efficient production of personalized cancer vaccines which might have clinical efficacy76, mRNA-4157 is an example of such a vaccine under development. There are a number of different cancer vaccines strategies under development, EO2401 vaccine is an example of an approach attempting to activate memory commensal specific T-cells that are cross-reactive against validated tumor associated antigens77.
The development of microRNA (miRNA), short hairpin RNA (shRNA), and short interfering RNA (siRNA) based cancer therapeutics development began in the beginning of 21th century78,79. The following are examples of such therapeutics under development: modified version of miR-34a, nano-formulated miR-12280. So far, the biggest challenge for small RNA therapeutics have been inability to provide clinically significant anti-tumor activity in clinical trials.
Pulsed electromagnetic field (PEMF) therapy research started after WWII. PEMF therapy has been approved by the FDA for bone growth simulation81. Over the last few decades PEMF therapy use has been investigated as potential cancer treatment, and translational efforts have reached the stage of clinical trials82.
Observations of preferential homing of some stem/progenitor cells and some bacteria to tumors have opened the possibility of new cancer treatment approaches, which for example may deliver a toxic payload or trigger/guide immune response83,84,85.
Initial observations of tumor Innervation have been documented at the end of 19th century and over the last few decades an increasing amount of evidence points to potential biological and clinical significance of tumor Innervation86. Targeting electrochemical communication between neurons and tumor cells might represent potential cancer treatment modality87.
There are a number of different gene therapy approaches under development. RZ-001 is an approach based on ribozyme-based RNA reprogramming. Targeting tumor-specific repeat sequences and tumor-specific junctions created by somatic structural alterations using CRISPR has been recently proposed88,89. Cancer treatment based on using somatic mutations as targets for insertion of sequences coding for peptides known to trigger immune response due to previous routine vaccination such as measles, mumps, rubella, etc., or coding for peptides triggering cell death is another potential gene therapy approach. This approach is illustrated in the Figure 2 using the example of TP53 somatic oncogenic mutation p.R273H and Hemagglutinin peptide KLWCRHFCV, which is known to be one of the targets of immune response to MMR vaccinations. Continuing improvements of efficiency of delivery of nanoparticles to different organs and continuing improvements in efficiency of gene editing are expected to make such approaches more likely to succeed as time goes by.
Figure 2.
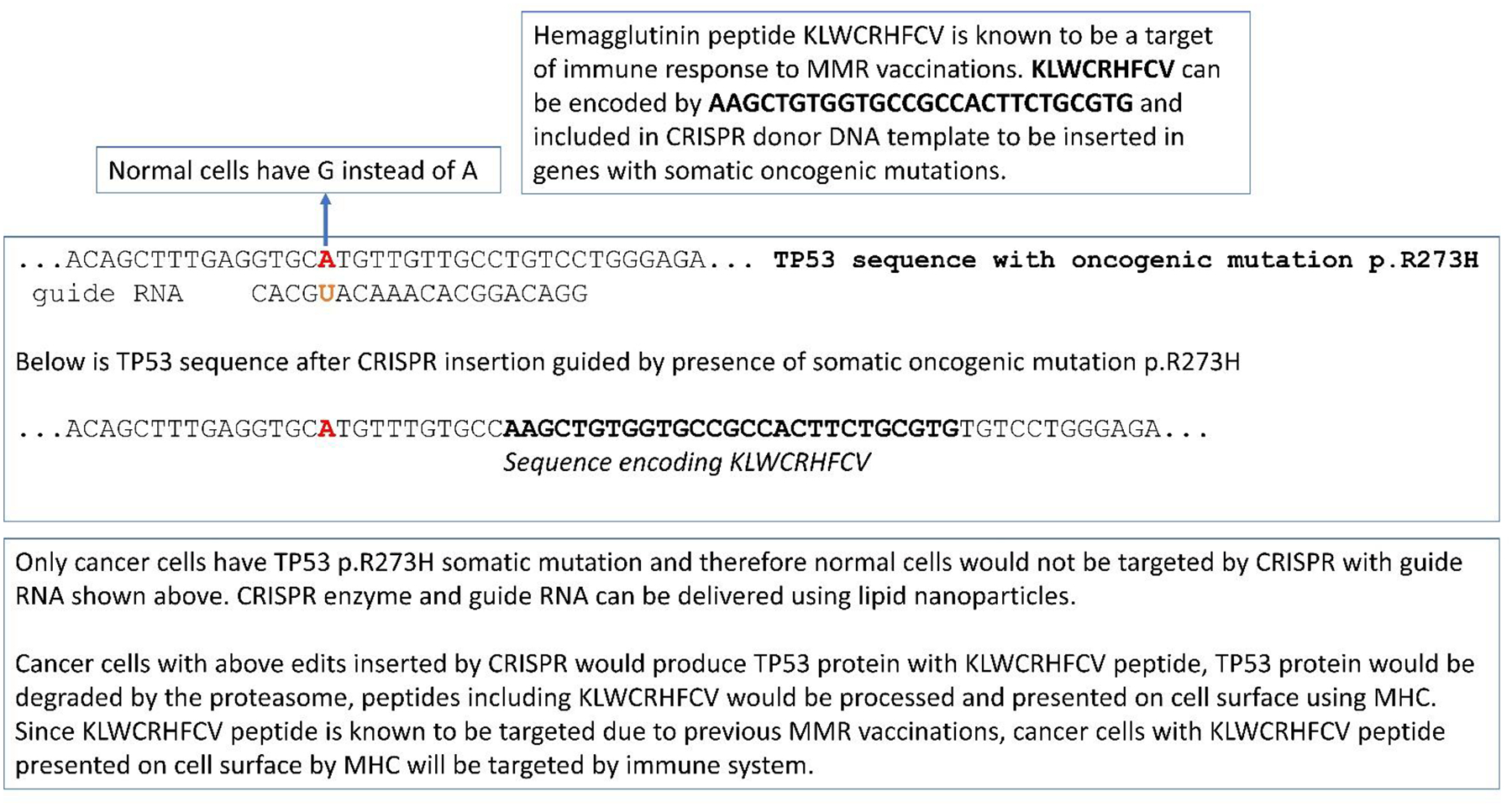
Using somatic mutations as targets for insertion of sequences coding for peptides known to trigger immune response due to previous routine vaccinations.
Computational biology has been playing an important role in fundamental biological research, biotechnology and drug development for well over 50 years. For example, it has been crucial for the development of genome sequencing and of many types of genomic analyses routinely used in clinical practice90. Advances in artificial intelligence, such as deep neural networks have potential to improve cancer treatments. For example, structure prediction of biomolecular interactions with DeepMind AlphaFold 3 has potential to improve and accelerate development of multiple types of cancer drugs, including small molecular drugs and antibody-based treatments91.
Multiple approaches are likely going to be needed for cancer treatment for the foreseeable future. As summarized in Table 1 all rational cancer treatment modalities introduced prior to 1970 are still in use today and likely will be in use for the foreseeable future, along with all other cancer treatment modalities in use today.
Table 1.
Cancer treatment modalities.
| Cancer treatment modality | Prior to 1970 | 1970 to 2023 | Future |
|---|---|---|---|
| Surgery | ✓ | ✓ | ✓ |
| Radiation therapy | ✓ | ✓ | ✓ |
| Chemotherapy | ✓ | ✓ | ✓ |
| Allogeneic hematopoietic stem cell transplantation | ✓ | ✓ | ✓ |
| Pharmacological hormone therapy | ✓ | ✓ | |
| Treatments targeting genes with oncogenic alterations and related signaling pathways | ✓ | ✓ | |
| Photodynamic therapy | ✓ | ✓ | |
| Antibody drug conjugates | ✓ | ✓ | |
| Immune check point inhibitors | ✓ | ✓ | |
| Bispecific T-cell engagers | ✓ | ✓ | |
| Oncolytic virus therapy | ✓ | ✓ | |
| Chimeric antigen receptor T cell therapy | ✓ | ✓ |
There is unfortunately still a large number of patients, especially those with metastasis, such as brain and liver metastasis who have exhausted all available treatments and have no viable clinical treatment option. The cost and availability of treatments, which are partly based on geographical location, are also important factors influencing patient outcomes92. Advances in early cancer detection may allow the treatment of more patients before the onset of metastatic disease and, hopefully, with a decreased number and decreased heterogeneity of oncogenic alterations. Additional cancer treatment modalities under development and improvements in existing cancer treatment modalities will be critical in improving clinical care of cancer patients.
Supplementary Material
Highlights.
History of cancer treatments.
The current landscape of cancer treatments.
Potential future cancer therapies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
The opinions expressed in this manuscript are the authors’ own and do not necessarily reflect the view of the National Cancer Institute, the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1.Cole MP, Jones CT & Todd ID A new anti-oestrogenic agent in late breast cancer. An early clinical appraisal of ICI46474. Br. J. Cancer 25, 270–275 (1971). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hanahan D & Weinberg RA Hallmarks of Cancer: The Next Generation. Cell 144, 646–674 (2011). [DOI] [PubMed] [Google Scholar]
- 3.Wyld L, Audisio RA & Poston GJ The evolution of cancer surgery and future perspectives. Nat. Rev. Clin. Oncol 12, 115–124 (2015). [DOI] [PubMed] [Google Scholar]
- 4.Crosby D et al. Early detection of cancer. Science 375, eaay9040 (2022). [DOI] [PubMed] [Google Scholar]
- 5.Lederman M The early history of radiotherapy: 1895–1939. Int. J. Radiat. Oncol 7, 639–648 (1981). [DOI] [PubMed] [Google Scholar]
- 6.Lim YK & Kim D Brachytherapy: A Comprehensive Review. Prog. Med. Phys 32, 25–39 (2021). [Google Scholar]
- 7.DeVita VT & Chu E A History of Cancer Chemotherapy. Cancer Res 68, 8643–8653 (2008). [DOI] [PubMed] [Google Scholar]
- 8.Goodman LS & Wintrobe MM Nitrogen mustard therapy; use of methyl-bis (beta-chloroethyl) amine hydrochloride and tris (beta-chloroethyl) amine hydrochloride for Hodgkin’s disease, lymphosarcoma, leukemia and certain allied and miscellaneous disorders. J. Am. Med. Assoc 132, 126–132 (1946). [DOI] [PubMed] [Google Scholar]
- 9.Farber S & Diamond LK Temporary remissions in acute leukemia in children produced by folic acid antagonist, 4-aminopteroyl-glutamic acid. N. Engl. J. Med 238, 787–793 (1948). [DOI] [PubMed] [Google Scholar]
- 10.Elion GB, Singer S & Hitchings GH Antagonists of nucleic acid derivatives. VIII. Synergism in combinations of biochemically related antimetabolites. J. Biol. Chem 208, 477–488 (1954). [PubMed] [Google Scholar]
- 11.Hitchings GH & Elion GB The chemistry and biochemistry of purine analogs. Ann. N. Y. Acad. Sci 60, 195–199 (1954). [DOI] [PubMed] [Google Scholar]
- 12.Heidelberger C et al. Fluorinated pyrimidines, a new class of tumour-inhibitory compounds. Nature 179, 663–666 (1957). [DOI] [PubMed] [Google Scholar]
- 13.Pittillo RF, Schabel FM, Wilcox WS & Skipper HE Experimental evaluation of potential anticancer agents. XVI. Basic study of effects of certain anticancer agents on kinetic behavior of model bacterial cell populations. Cancer Chemother. Rep 47, 1–26 (1965). [PubMed] [Google Scholar]
- 14.Schabel FM. Animal models as predictive systems. in Cancer chemotherapy-fundamental concepts and recent advances. 323–355 (Year Book Medical Publisher, 1975). [Google Scholar]
- 15.Teicher BA Tumor models for efficacy determination. Mol. Cancer Ther 5, 2435–2443 (2006). [DOI] [PubMed] [Google Scholar]
- 16.Johnson IS, Armstrong JG, Gorman M & Burnett JP THE VINCA ALKALOIDS: A NEW CLASS OF ONCOLYTIC AGENTS. Cancer Res 23, 1390–1427 (1963). [PubMed] [Google Scholar]
- 17.Brunner KW & Young CW A METHYLHYDRAZINE DERIVATIVE IN HODGKIN’S DISEASE AND OTHER MALIGNANT NEOPLASMS. THERAPEUTIC AND TOXIC EFFECTS STUDIED IN 51 PATIENTS. Ann. Intern. Med 63, 69–86 (1965). [DOI] [PubMed] [Google Scholar]
- 18.DeVita VT, Serpick A & Carbone PP Preliminary clinical studies with ibenzmethyzin. Clin. Pharmacol. Ther 7, 542–546 (1966). [DOI] [PubMed] [Google Scholar]
- 19.Tan C, Tasaka H, Yu KP, Murphy ML & Karnofsky DA Daunomycin, an antitumor antibiotic, in the treatment of neoplastic disease. Clinical evaluation with special reference to childhood leukemia. Cancer 20, 333–353 (1967). [DOI] [PubMed] [Google Scholar]
- 20.Freireich EJ, Karon M & Frei E III. Quadruple combination therapy (VAMP) for acute lymphocytic leukemia of childhood. Proc Am Assoc Cancer Res 5, (1964). [Google Scholar]
- 21.Frei E III. Potential for eliminating leukemic cells in childhood acute leukemia. Proc Am Assoc Cancer Res 5, (1963). [Google Scholar]
- 22.George P et al. A study of ‘total therapy’ of acute lymphocytic leukemia in children. J. Pediatr 72, 399–408 (1968). [DOI] [PubMed] [Google Scholar]
- 23.Devita VT, Serpick AA & Carbone PP Combination chemotherapy in the treatment of advanced Hodgkin’s disease. Ann. Intern. Med 73, 881–895 (1970). [DOI] [PubMed] [Google Scholar]
- 24.Moxley JH, De Vita VT, Brace K & Frei E Intensive combination chemotherapy and X-irradiation in Hodgkin’s disease. Cancer Res 27, 1258–1263 (1967). [PubMed] [Google Scholar]
- 25.Nurgali K, Jagoe RT & Abalo R Editorial: Adverse Effects of Cancer Chemotherapy: Anything New to Improve Tolerance and Reduce Sequelae? Front. Pharmacol 9, 245 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas ED, Lochte HL, Lu WC & Ferrebee JW Intravenous Infusion of Bone Marrow in Patients Receiving Radiation and Chemotherapy. N. Engl. J. Med 257, 491–496 (1957). [DOI] [PubMed] [Google Scholar]
- 27.Henig I & Zuckerman T Hematopoietic stem cell transplantation-50 years of evolution and future perspectives. Rambam Maimonides Med. J 5, e0028 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Rood JJ The detection of transplantation antigens in leukocytes. Semin. Hematol 5, 187–214 (1968). [PubMed] [Google Scholar]
- 29.Thomas ED et al. Marrow Transplantation for Acute Nonlymphoblastic Leukemia in First Remission. N. Engl. J. Med 301, 597–599 (1979). [DOI] [PubMed] [Google Scholar]
- 30.Penack O et al. How much has allogeneic stem cell transplant–related mortality improved since the 1980s? A retrospective analysis from the EBMT. Blood Adv 4, 6283–6290 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Norton L Cancer log-kill revisited. Am. Soc. Clin. Oncol. Educ. Book Am. Soc. Clin. Oncol. Annu. Meet 3–7 (2014) doi: 10.14694/EdBook_AM.2014.34.3. [DOI] [PubMed] [Google Scholar]
- 32.Rygaard J & Poulsen CO HETEROTRANSPLANTATION OF A HUMAN MALIGNANT TUMOUR TO “NUDE” MICE. Acta Pathol. Microbiol. Scand 77, 758–760 (1969). [DOI] [PubMed] [Google Scholar]
- 33.Bibby MC Orthotopic models of cancer for preclinical drug evaluation. Eur. J. Cancer 40, 852–857 (2004). [DOI] [PubMed] [Google Scholar]
- 34.Tentler JJ et al. Patient-derived tumour xenografts as models for oncology drug development. Nat. Rev. Clin. Oncol 9, 338–350 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meisel JL, Venur VA, Gnant M & Carey L Evolution of Targeted Therapy in Breast Cancer: Where Precision Medicine Began. Am. Soc. Clin. Oncol. Educ. Book Am. Soc. Clin. Oncol. Annu. Meet 38, 78–86 (2018). [DOI] [PubMed] [Google Scholar]
- 36.Arya M, Shergill IS, Grange P & Emberton M Hormone therapy: a revolution in understanding prostate cancer. Lancet Oncol 9, 1112 (2008). [DOI] [PubMed] [Google Scholar]
- 37.Schechter AL et al. The neu oncogene: an erb-B-related gene encoding a 185,000-Mr tumour antigen. Nature 312, 513–516 (1984). [DOI] [PubMed] [Google Scholar]
- 38.Druker BJ et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N. Engl. J. Med 344, 1031–1037 (2001). [DOI] [PubMed] [Google Scholar]
- 39.Enewold L & Thomas A Real-World Patterns of EGFR Testing and Treatment with Erlotinib for Non-Small Cell Lung Cancer in the United States. PLOS ONE 11, e0156728 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Horak P et al. Standards for the classification of pathogenicity of somatic variants in cancer (oncogenicity): Joint recommendations of Clinical Genome Resource (ClinGen), Cancer Genomics Consortium (CGC), and Variant Interpretation for Cancer Consortium (VICC). Genet. Med. Off. J. Am. Coll. Med. Genet 24, 986–998 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li MM et al. Standards and Guidelines for the Interpretation and Reporting of Sequence Variants in Cancer: A Joint Consensus Recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J. Mol. Diagn. JMD 19, 4–23 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Senapati J et al. Management of chronic myeloid leukemia in 2023 – common ground and common sense. Blood Cancer J 13, 58 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sonkin D & Simon R Early Detection Is as Important as Imatinib in CML Treatment Success. http://www.preprints.org/manuscript/201910.0207/v1 (2019) doi: 10.20944/preprints201910.0207.v1. [DOI] [Google Scholar]
- 44.Correia JH, Rodrigues JA, Pimenta S, Dong T & Yang Z Photodynamic Therapy Review: Principles, Photosensitizers, Applications, and Future Directions. Pharmaceutics 13, 1332 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shastry M et al. Rise of Antibody-Drug Conjugates: The Present and Future. Am. Soc. Clin. Oncol. Educ. Book e390094 (2023) doi: 10.1200/EDBK_390094. [DOI] [PubMed] [Google Scholar]
- 46.Bagchi S, Yuan R & Engleman EG Immune Checkpoint Inhibitors for the Treatment of Cancer: Clinical Impact and Mechanisms of Response and Resistance. Annu. Rev. Pathol. Mech. Dis 16, 223–249 (2021). [DOI] [PubMed] [Google Scholar]
- 47.Tawbi HA et al. Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. N. Engl. J. Med 386, 24–34 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ishida Y, Agata Y, Shibahara K & Honjo T Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J 11, 3887–3895 (1992). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson DB, Nebhan CA, Moslehi JJ & Balko JM Immune-checkpoint inhibitors: long-term implications of toxicity. Nat. Rev. Clin. Oncol 19, 254–267 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tian Z, Liu M, Zhang Y & Wang X Bispecific T cell engagers: an emerging therapy for management of hematologic malignancies. J. Hematol. Oncol.J Hematol Oncol 14, 75 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sonkin Dmitriy, Liu Yue, Pagliarini Raymond, Tschantz Bill, & Morrissey Michael. Identifying SILV as ADC target in melanoma. NVS-DFCI Jt. RETREAT (2010). [Google Scholar]
- 52.Chen Y et al. The melanosomal protein PMEL17 as a target for antibody drug conjugate therapy in melanoma. J. Biol. Chem 287, 24082–24091 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Franke V et al. High response rates for T‐VEC in early metastatic melanoma (stage IIIB/C-IVM1a). Int. J. Cancer 145, 974–978 (2019). [DOI] [PubMed] [Google Scholar]
- 54.Hofland J, Brabander T, Verburg FA, Feelders RA & De Herder WW Peptide Receptor Radionuclide Therapy. J. Clin. Endocrinol. Metab 107, 3199–3208 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sartor O et al. Lutetium-177–PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med 385, 1091–1103 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cho B Intensity-modulated radiation therapy: a review with a physics perspective. Radiat. Oncol. J 36, 1–10 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Otto K Volumetric modulated arc therapy: IMRT in a single gantry arc. Med. Phys 35, 310–317 (2008). [DOI] [PubMed] [Google Scholar]
- 58.Sterner RC & Sterner RM CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J 11, 69 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bourbon E, Ghesquières H & Bachy E CAR-T cells, from principle to clinical applications. Bull. Cancer (Paris) 108, S4–S17 (2021). [DOI] [PubMed] [Google Scholar]
- 60.Harris LN et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol 34, 1134–1150 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Curigliano G et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann. Oncol 28, 1700–1712 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Medina JE et al. Cell-free DNA approaches for cancer early detection and interception. J. Immunother. Cancer 11, e006013 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vozenin M-C, Bourhis J & Durante M Towards clinical translation of FLASH radiotherapy. Nat. Rev. Clin. Oncol 19, 791–803 (2022). [DOI] [PubMed] [Google Scholar]
- 64.Békés M, Langley DR & Crews CM PROTAC targeted protein degraders: the past is prologue. Nat. Rev. Drug Discov 21, 181–200 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mayor-Ruiz C et al. Rational discovery of molecular glue degraders via scalable chemical profiling. Nat. Chem. Biol 16, 1199–1207 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Munir T et al. Chronic Lymphocytic Leukemia Therapy Guided by Measurable Residual Disease. N. Engl. J. Med NEJMoa2310063 (2023) doi: 10.1056/NEJMoa2310063. [DOI] [PubMed] [Google Scholar]
- 67.Harjunpää H & Guillerey C TIGIT as an emerging immune checkpoint. Clin. Exp. Immunol 200, 108–119 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rudin CM et al. Emerging therapies targeting the delta-like ligand 3 (DLL3) in small cell lung cancer. J. Hematol. Oncol.J Hematol Oncol 16, 66 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhou S, Liu M, Ren F, Meng X & Yu J The landscape of bispecific T cell engager in cancer treatment. Biomark. Res 9, 38 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Frampton JE Teserpaturev/G47Δ: First Approval. BioDrugs 36, 667–672 (2022). [DOI] [PubMed] [Google Scholar]
- 71.Tian Y, Xie D & Yang L Engineering strategies to enhance oncolytic viruses in cancer immunotherapy. Signal Transduct. Target. Ther 7, 117 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Malfitano AM, Di Somma S, Iannuzzi CA, Pentimalli F & Portella G Virotherapy: From single agents to combinatorial treatments. Biochem. Pharmacol 177, 113986 (2020). [DOI] [PubMed] [Google Scholar]
- 73.Hawkins ER, D’Souza RR & Klampatsa A Armored CAR T-Cells: The Next Chapter in T-Cell Cancer Immunotherapy. Biol. Targets Ther 15, 95–105 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tousley AM et al. Co-opting signalling molecules enables logic-gated control of CAR T cells. Nature 615, 507–516 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wellhausen N et al. Epitope base editing CD45 in hematopoietic cells enables universal blood cancer immune therapy. Sci. Transl. Med 15, eadi1145 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lin MJ et al. Cancer vaccines: the next immunotherapy frontier. Nat. Cancer 3, 911–926 (2022). [DOI] [PubMed] [Google Scholar]
- 77.Maia A et al. 641 Strong immune response to therapeutic vaccination with EO2401 microbiome derived therapeutic vaccine + nivolumab: interim report of the EOGBM1–18/ROSALIE study. in Regular and Young Investigator Award Abstracts A671–A671 (BMJ Publishing Group Ltd, 2022). doi: 10.1136/jitc-2022-SITC2022.0641. [DOI] [Google Scholar]
- 78.Rupaimoole R & Slack FJ MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat. Rev. Drug Discov 16, 203–222 (2017). [DOI] [PubMed] [Google Scholar]
- 79.Padda IS, Mahtani AU & Parmar M Small Interfering RNA (siRNA) Therapy. in StatPearls (StatPearls Publishing, Treasure Island (FL), 2023). [PubMed] [Google Scholar]
- 80.Cuciniello R, Filosa S & Crispi S Novel approaches in cancer treatment: preclinical and clinical development of small non-coding RNA therapeutics. J. Exp. Clin. Cancer Res 40, 383 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Garland DE, Moses B & Salyer W Long-term follow-up of fracture nonunions treated with PEMFs. Contemp. Orthop 22, 295–302 (1991). [PubMed] [Google Scholar]
- 82.Vadalà M et al. Mechanisms and therapeutic effectiveness of pulsed electromagnetic field therapy in oncology. Cancer Med 5, 3128–3139 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Niess H et al. Genetic engineering of mesenchymal stromal cells for cancer therapy: turning partners in crime into Trojan horses. Innov. Surg. Sci 1, 19–32 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vincent RL et al. Probiotic-guided CAR-T cells for solid tumor targeting. Science 382, 211–218 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Raman V et al. Intracellular Salmonella delivery of an exogenous immunization antigen refocuses CD8 T cells against cancer cells, eliminates pancreatic tumors and forms antitumor immunity. Front. Immunol 14, 1228532 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baraldi JH, Martyn GV, Shurin GV & Shurin MR Tumor Innervation: History, Methodologies, and Significance. Cancers 14, 1979 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Venkatesh HS Targeting electrochemical communication between neurons and cancer. Sci. Transl. Med 15, eadi5170 (2023). [DOI] [PubMed] [Google Scholar]
- 88.Tan I-L et al. Targeting the non-coding genome and temozolomide signature enables CRISPR-mediated glioma oncolysis. Cell Rep 42, 113339 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yang H et al. KLIPP - a Precision CRISPR Approach to Target Structural Variant Junctions in Cancer. http://biorxiv.org/lookup/doi/10.1101/2023.05.10.540176 (2023) doi: 10.1101/2023.05.10.540176. [DOI] [Google Scholar]
- 90.International Human Genome Sequencing Consortium et al. Initial sequencing and analysis of the human genome. Nature 409, 860–921 (2001). [DOI] [PubMed] [Google Scholar]
- 91.Abramson J et al. Accurate structure prediction of biomolecular interactions with AlphaFold 3. Nature (2024) doi: 10.1038/s41586-024-07487-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gralow JR et al. Recommendations from the ASCO Academic Global Oncology Task Force. JCO Glob. Oncol 1666–1673 (2020) doi: 10.1200/GO.20.00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


