Abstract
Background
The Health Information Technology for Economic and Clinical Health Act of 2009 introduced the Meaningful Use program to incentivize the adoption of electronic health records (EHRs) in the U.S. This study investigates the disparities in EHR adoption and interoperability between rural and urban physicians in the context of federal programs like the Medicare Access and CHIP Reauthorization Act of 2015 and the 21st Century Cures Act.
Methods
A cross-sectional analysis was conducted using the 2021 Quality Payment Program Experience Report Public Use File to compare EHR adoption and Promoting Interoperability scores (PISs) between urban and rural physician participants. Data were linked with the Certified Health IT Product List to assess certified EHR adoption and interoperability.
Results
The study included 209,152 physician participants, 12% of whom practiced in rural communities. EHR adoption was significantly higher in urban (74%) than in rural areas (64%). Epic Systems dominated the market in both settings. Multivariable logistic regression indicated lower odds of EHR adoption among rural physicians (OR: 0.79, CI: 0.76–0.82). Rural physicians also had lower PISs (β: –3.5, CI: –4.1 to –3.0). Factors like extreme hardship, small practitioner status, and location in a health professional shortage area significantly impacted EHR adoption and PISs.
Conclusions
Significant disparities exist in EHR adoption and interoperability between rural and urban physicians. These disparities highlight the need for targeted interventions to enhance EHR adoption and interoperability in rural settings to ensure equitable access to healthcare technologies and improved patient outcomes across all communities.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12168-5.
Keywords: EHR Adoption, Interoperability, Rural Healthcare, Meaningful Use, MACRA, Promoting Interoperability, Healthcare Disparities
Background
The 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act [1] represented a paradigm shift in healthcare delivery by emphasizing the adoption and meaningful utilization of electronic health records (EHRs) in the U.S. While HITECH transformed urban healthcare systems, its impact on rural healthcare still needs to be explored, particularly regarding technology adoption and utilization. The Meaningful Use (MU) program was central to this transformation, as it was designed to incentivize EHR systems’ adoption and meaningful utilization [2].
MU defines a set of criteria that healthcare providers (physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists) must meet to qualify for Medicare and Medicaid EHR Incentive Programs to ensure that the EHR they employ significantly enhances patient care and safety. Following the implementation of the MU program, several federal programs were established to further EHR adoption and promote interoperability. Notably, the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 introduced the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs), which altered how Medicare rewarded providers [3]. This shift underscored the role of technology in value-based care. Subsequently, the Promoting Interoperability program, launched in 2018 [3], focused on enhancing healthcare data exchange and patient access to health information. Concurrently, the 21st Century Cures Act [4], passed in 2016, emphasized EHR interoperability and preventing information blocking. It aimed to make EHRs more user-friendly and accessible by fostering seamless data exchange and patient access to health information. These programs collectively prompted a substantial leap in EHR adoption, information exchange, and patient engagement while dividing U.S. healthcare into pre- and post-MU eras.
Table 1 delineates the three stages of the MU program [5]. These stages were designed to promote EHR adoption across the spectrum but inadvertently contributed to a widening digital divide between rural and urban healthcare providers. Stage 1 focused on basic EHR adoption and health data collection. Stage 2 emphasized patient information exchange and care coordination via EHR systems, while Stage 3 advocated continuous monitoring and evaluation of healthcare outcomes through EHR utilization. Rural health clinics (RHCs) and critical access hospitals (CAHs) trailed behind urban counterparts in EHR adoption rates, particularly in the early stages, faced with financial constraints, limited technical support, and inadequate internet connectivity [2, 6–9].
Table 1.
Stages of meaningful use rollout in the United States
| Components [5] | Stage 1 (2011–2012): Data capture and sharing | Stage 2 (2014): Advanced clinical processes | Stage 3 (2016-): Improved outcomes |
|---|---|---|---|
| Goal | Encourage the adoption of EHRs and begin to detail their meaningful use | Expand upon Stage 1 criteria focusing on continuous quality improvement at the point of care and the exchange of information in the most structured format possible | To promote better health for populations, improve health outcomes, and prepare for advanced models of health delivery |
| Main Requirements |
• Electronically capture health information in a standardized format • Use that information to track key clinical conditions • Communicate that information for care coordination purposes • Use EHR to engage patients and their families • Report clinical quality measures and public health information |
• More rigorous health information exchange (HIE) • Increased requirements for e-prescribing and incorporating lab results • Electronic transmission of patient care summaries across multiple settings • More patient-controlled data |
• Improved quality, safety, and efficiency, leading to improved health outcomes • Decision support for national high-priority conditions • Patient access to self-management tools • Access to comprehensive patient data • Improving population health |
Table 1 outlines the three stages of the Meaningful Use (MU) program, designed to promote EHR adoption and meaningful utilization across healthcare settings. Each stage builds upon the previous one, improving clinical processes and health outcomes using EHRs
While MU has played a critical role in increasing EHR adoption, the disparities in rural versus urban settings, underscored by infrastructure and resource challenges [10], suggest a growing divide in the benefits of broad EHR adoption. In 2015, 44.5% of urban and 31.7% of rural hospitals had a comprehensive EHR, 39.7% of urban and 43.7% of rural hospitals had a basic EHR, and 15.8% of urban and 24.6% of rural hospitals had less than a basic EHR system [7]. EHR adoption increased dramatically after MU, with 95% of all hospitals, 93% of small rural hospitals and CAHs, and 97% of large hospitals having a certified EHR system by 2017 [11]. By 2021, 96% of hospitals had adopted certified EHRs, while 76% of office-based physicians had certified EHRs [12, 13], demonstrating MU’s impact on adoption rates.
While these and other studies [14, 15] have examined the disparities in EHR adoption between rural and urban healthcare providers, they have often overlooked the evolving challenges rural providers face in adapting to recent federal mandates and focused largely on hospital adoption. This study specifically explores whether rural physicians face significantly greater barriers to EHR interoperability than their urban counterparts. We hypothesized that rural physicians have lower EHR adoption rates and interoperability scores due to structural challenges, such as limited resources and support, alongside barriers like workforce shortages, financial constraints, and differing organizational priorities, collectively contributing to the rural–urban healthcare divide.
Methods
This cross-sectional study aimed to analyze disparities in EHR adoption and Promoting Interoperability scores (PISs) between urban and rural physicians as of 2021 by utilizing data from the 2021 Quality Payment Program (QPP) Experience Report Public Use File (PUF) [16]. The QPP PUF offers detailed insights at the taxpayer identification number (TIN)/National Provider Identifier (NPI) level concerning provider eligibility, payments, and compliance with EHR requirements and interoperability standards. A comparative analysis between urban and rural physician participants in the QPP was central to our study to uncover disparities in EHR adoption and advanced use as measured by PIS within these settings.
Data sources
The Centers for Medicare & Medicaid Services (CMS) plays a dominant role in shaping the practices and policies of physicians in the United States. Most physicians in the US are CMS providers, with estimates indicating that approximately 1% of physicians formally opted out in 2022—apart from Alaska and Colorado, where fewer than 2% of non-pediatric physicians opted out of Medicare while nearly 90% continued accepting new Medicare or Medicaid patients [17]. CMS’s influence is further underscored by its financial impact: in 2021, health expenditures accounted for 18.3% of the U.S. gross domestic product, or $12,914 per capita, with Medicare and Medicaid accounting for $1,634.8 billion of this $4,255.1 billion expenditure, or more than 38% [18]. As a result, CMS mandates such as MU are the de facto requirement for practicing physicians. Therefore, understanding trends and adoption rates at the CMS level is a reasonable proxy for population-level estimates at the office-based provider level.
Initiated under MACRA, the QPP attempts to shift Medicare payment methodology by emphasizing value over volume. It aims to reward healthcare providers for high-quality, efficient care through two primary tracks: the MIPS and Advanced APM programs. The PUF captures participation patterns and performance scores and provides crucial data on the PIS, a critical metric for assessing EHR adoption and interoperability.
The QPP provides a window into how providers meet EHR requirements and interoperability standards, which is crucial for our comparative analysis between urban and rural settings. In the context of the QPP PUF, a participant refers to an individual clinician or a group practice represented by an NPI or TIN, respectively. We linked the QPP data with the Certified Health IT Product List (CHPL) [19] maintained by the Office of the National Coordinator for Health Information Technology (ONC). The CHPL is an authoritative database of health IT products tested and certified under the ONC Health IT Certification Program. Through a shared certification identifier, this linkage provides a comprehensive view of certified health IT products’ capabilities, functionalities, and vendors.
Study population
We restricted our analysis to patient-facing physicians across U.S. states actively engaged in MIPS reporting, except those practicing exclusively at ambulatory surgical centers. Physicians with a certified EHR vendor indicated were included, while those without a corresponding vendor ID in the CHPL were excluded (Supplemental Figure 1). This analysis was restricted to general practitioners and selected specialties (see Supplemental Methods for a complete list of physician specialties included), which included those specialties with ≥ 50 physicians practicing in rural and urban settings in the QPP PUF to avoid comparing across specialties that are unequally represented in rural and urban communities.
Outcomes
We measured outcomes focused on adopting certified EHRs and the detailed assessment of the PIS [20] as stipulated by CMS. Certified EHR technology (CEHRT) is required to meet the 2015 Edition Cures Update criteria following CMS standards. CMS introduced the Promoting Interoperability Score (PIS) in 2018 as part of the MIPS program to replace the MU health IT requirements, focusing on enhancing health information exchange and patient access to data [21]. The PIS comprises four main objectives, each contributing to the total score:
Electronic prescribing focuses on using EHRs to manage and send prescriptions (10 points). Bonus points (5) are available for querying their respective prescription drug monitoring programs (PDMPs).
The health information exchange assesses the ability of EHR systems to exchange patient information with other healthcare providers, which includes support for electronic referral loops by sending health information (20 points) and receiving and reconciling health information (20 points).
Provider-to-patient exchange measures patient access to health information through the EHR system (40 points).
Public health and clinical data exchange involves EHR reporting capabilities to public health agencies (10 points), which can include any two of the following: syndromic surveillance, an immunization registry, electronic cases, a public health registry, a clinical data registry, or electronic reportable laboratory result reporting.
Additionally, the Protect Patient Health Information objective, including measures for Security Risk Analysis and Safety Assurance Factors for EHR Resilience (SAFER) Guides, is required [22]. The CMS performance-based scoring methodology applies to each measure, with a minimum requirement of 50 points for scoring satisfaction and a maximum of 100 points.
Variables
We identified the primary exposure as whether the physicians or practices had rural statuses, defined as practicing in a ZIP Code designated as rural by the Federal Office of Rural Health Policy [23] or a practice with more than 75% of the providers billing under this definition. We adjusted for factors influencing EHR adoption and interoperability, including small practitioner status (15 or fewer clinicians), facility- versus hospital-based, serving primary care health professional shortage areas (HPSAs) defined by the Health Resources and Services Administration, years in Medicare, U.S. Census division, provider specialty, and an extreme hardship designation.
Extreme hardship is an exemption CMS provides when a provider uses decertified EHR technology, has insufficient internet connectivity, or faces extreme financial hardship. Small practitioner status includes practices with 15 or fewer clinicians under one Taxpayer Identification Number (TIN). "Clinicians" refers to physicians, nurse practitioners (NPs), and physician assistants (PAs), among other eligible professionals, in both outpatient and inpatient settings. Facility-based providers deliver most of their services in facilities participating in the Hospital Value-Based Purchasing (VBP) program. In contrast, hospital-based providers deliver most of their services in hospital settings. These groups share similarities but differ in reporting and performance assessments. Facility-based providers may have lower PIS from exemptions or alternative scoring, especially in cases where facility-based scores were unavailable, as in the 2021 performance period due to the COVID-19 pandemic exemptions (see Supplemental Table 1 for a detailed review of each variable and potential limitations) [24].
Statistical analysis
We generated descriptive statistics and conducted Wilcoxon rank sum tests for continuous variables and Pearson’s chi-square tests for categorical variables to identify significant differences in EHR adoption rates between rural and urban physicians. We stratified EHR vendors by rurality and region to understand adoption patterns. Additionally, we used logistic regression to assess EHR adoption as a binary outcome, adjusting for listed covariates (Supplemental Table 2). Finally, we analyzed PIS using linear regression stratified by rurality to explore the relationship between rurality and EHR capacity, adjusting for baseline health system capacity and provider experience.
Table 2.
Descriptive statistics for 2021 quality payment program physician participants by rurality
| Characteristic |
Overall, N = 209,1521 |
Rural, N = 25,0311 |
Urban, N = 184,1211 |
p value2 |
|---|---|---|---|---|
| Practice Size | 288 (41, 1,131) | 120 (25, 342) | 344 (45, 1,290) | < 0.001 |
| Number of Medicare Patients | 17,396 (3,773, 48,936) | 6,825 (1,844, 17,362) | 20,765 (4,434, 51,604) | < 0.001 |
| Years in Medicare | 12 (8, 16) | 12 (8, 17) | 12 (8, 16) | < 0.001 |
| Practice Type | < 0.001 | |||
| Group | 187,628 (90%) | 21,936 (88%) | 165,692 (90%) | |
| Individual | 21,524 (10%) | 3,095 (12%) | 18,429 (10%) | |
| Small Practitioner Status | 39,458 (19%) | 5,238 (21%) | 34,220 (19%) | < 0.001 |
| Health Professional Shortage Area | 34,976 (17%) | 15,959 (64%) | 19,017 (10%) | < 0.001 |
| Hospital-Based | 64,239 (31%) | 9,178 (37%) | 55,061 (30%) | < 0.001 |
| Facility Based | 14,805 (7.1%) | 2,425 (9.7%) | 12,380 (6.7%) | < 0.001 |
| Extreme Hardship | 65,639 (31%) | 7,969 (32%) | 57,670 (31%) | 0.1 |
| Final MIPS Score | 98 (91, 100) | 97 (89, 100) | 98 (91, 100) | < 0.001 |
| Certified EHR Status | 153,119 (73%) | 16,127 (64%) | 136,992 (74%) | < 0.001 |
| Promoting Interoperability Score (PIS) | 90 (0, 100) | 80 (0, 100) | 92 (0, 100) | < 0.001 |
| Provider-to-Patient Exchange | 40 (40, 40) | 40 (39, 40) | 40 (40, 40) | < 0.001 |
| Health Information Exchange | 33 (12, 39) | 20 (10, 38) | 34 (12, 39) | < 0.001 |
| Electronic Prescribing Exchange | 10 (10, 10) | 10 (10, 10) | 10 (10, 10) | < 0.001 |
| Public Health/Surveillance Exchange | 10 (9, 10) | 10 (8, 10) | 10 (9, 10) | < 0.001 |
| US Census Region | < 0.001 | |||
| East North Central | 28,139 (13%) | 5,186 (21%) | 22,953 (12%) | |
| East South Central | 9,940 (4.8%) | 2,884 (12%) | 7,056 (3.8%) | |
| Middle Atlantic | 35,020 (17%) | 1,562 (6.2%) | 33,458 (18%) | |
| Mountain | 16,036 (7.7%) | 2,543 (10%) | 13,493 (7.3%) | |
| New England | 7,877 (3.8%) | 1,793 (7.2%) | 6,084 (3.3%) | |
| Pacific | 29,109 (14%) | 1,466 (5.9%) | 27,643 (15%) | |
| South Atlantic | 43,587 (21%) | 3,728 (15%) | 39,859 (22%) | |
| West North Central | 20,741 (9.9%) | 3,258 (13%) | 17,483 (9.5%) | |
| West South Central | 18,703 (8.9%) | 2,611 (10%) | 16,092 (8.7%) | |
1Median (IQR) for continuous variables; n (%) for categorical variables
2Wilcoxon rank sum test; Pearson’s Chi-squared test
Table 2 contains descriptive statistics of the 2021 Quality Payment Program (QPP) physician participants, stratified by rurality. This table presents key characteristics, including practice size, number of Medicare patients, certified EHR status, and Promoting Interoperability Scores, highlighting significant differences between rural and urban providers
We secondarily analyzed findings on adopting a certified EHR and PIS for primary care physicians to assess its impact on practice. CMS designates internal medicine, family medicine, general practice, pediatric medicine, and geriatric medicine as primary care specialties in Medicare Part B [25].
This analysis was deemed exempt by the University of Nebraska Medical Center Institutional Review Board since it did not involve human subjects and leveraged widely available data sources. Analyses were conducted in R version 4.2.3 using base stats, gtsummary [26], and ggstats [27] packages. P-values < 0.05 were considered statistically significant. All p-values were for 2-sided tests.
Results
Our study included 209,152 physician participants, 12% practicing in rural communities. Group practices accounted for most participants in rural (88%) and urban (90%) settings. Rural participants served fewer Medicare patients (median: 6,825 vs. 20,765; p < 0.001) and worked in smaller practices (median size: 120 vs. 344 participants; p < 0.001). Certified EHR adoption rates were significantly lower among rural physicians (64% vs. 74%; p < 0.001), underscoring disparities in digital integration (Table 2).
Small practitioners comprised 19% of QPP participants, slightly more in rural areas (21% vs. 19%; p < 0.001). Health professional shortage areas included 17% of participants, with a significant difference in distribution between rural (64%) and urban (10%) physicians (p < 0.001). Rural participants had higher representation in the East North Central and East South Central divisions, while urban participants were more prevalent in the South Atlantic and Pacific divisions.
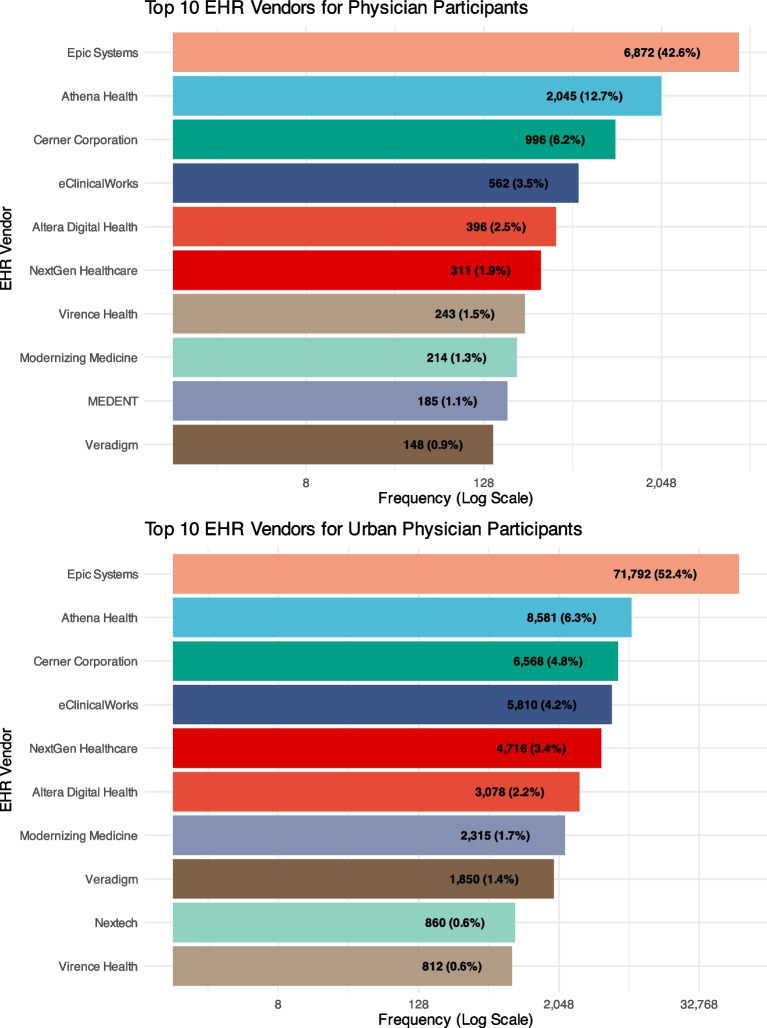
EHR adoption
Certified EHR adoption was higher in urban areas (74%) compared to rural settings (64%, p < 0.001). Across most specialties, urban participants demonstrated higher adoption rates than rural participants (Supplemental Figure 2), notably family practice, general practice, and internal medicine. Epic Systems Corporation was the dominant EHR vendor in both settings, with a 42.6% market share in rural areas, surpassing its closest competitors, Athenahealth (12.7%) and Cerner (6.2%). Among urban participants, Epic held a higher market share at 52.4%, while Athenahealth and Cerner had smaller shares at 6.3% and 4.8%, respectively. Although Epic and Athenahealth were prominent in rural and urban areas, Epic showed stronger dominance in urban settings (Fig. 1).
Fig. 1.
EHR vendors in use among Quality Payment Program physician participants with certified EHR by rurality. Figure 1 shows the distribution of EHR vendors among Quality Payment Program (QPP) physician participants with certified EHR systems, stratified by rural and urban settings. This figure highlights the dominant EHR vendors and their market shares in different geographic settings
EHR adoption across Census divisions varied significantly, revealing disparities in technology integration in different healthcare areas (Supplemental Figure 3 and Supplemental Table 2). Epic was the leading EHR vendor in most urban and many rural settings, with greater coverage in urban areas. Vendors like MEDENT and Nextech were region-specific.
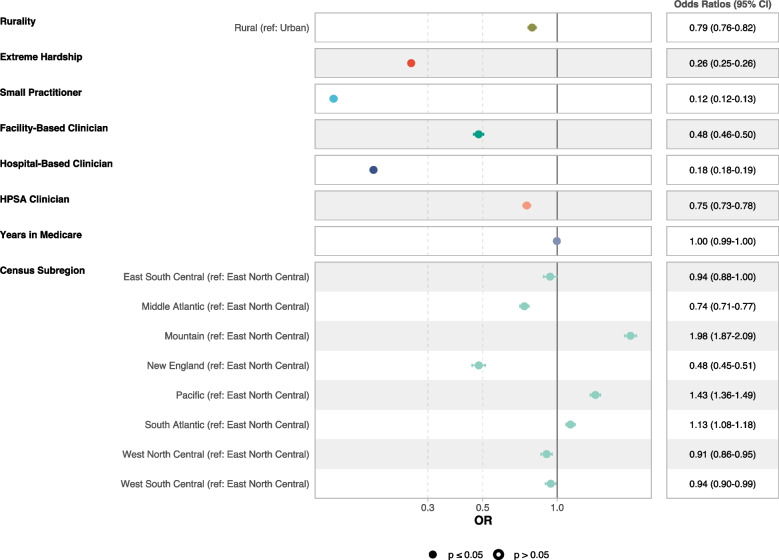
Multivariable logistic regression for certified EHR adoption
Multivariable logistic regression indicated rural physicians had 21% lower odds of adopting certified EHRs than urban physicians (OR: 0.79, CI: 0.76–0.82). Physicians facing extreme hardship (OR: 0.26, CI: 0.25–0.26) and those in small practices (OR: 0.12, CI: 0.12–0.13) had substantially lower odds of adoption (Fig. 2, Supplemental Table 3). Census divisions associated with lower odds included the Middle Atlantic, West North Central, and West South Central regions. In comparison, higher odds were observed in the Mountain, Pacific, and South Atlantic divisions relative to the East North Central division. Detailed model specifications for all physician specialties are available in Supplemental Table 3.
Fig. 2.
Multivariable logistic regression for having a certified EHR system among Quality Payment Program physician participants. Figure 2 shows results from a multivariable logistic regression analysis showing the odds of having a certified EHR system among QPP physician participants. The analysis accounts for various factors, including rurality, small practitioner status, and extreme hardship
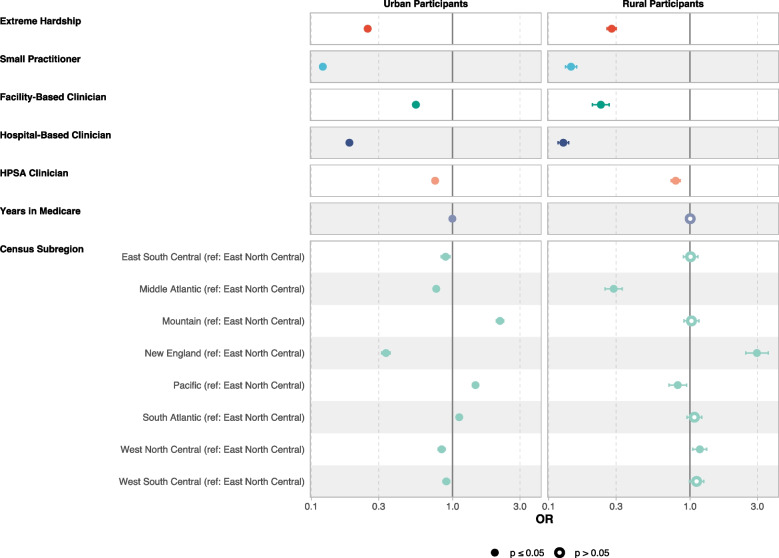
Models stratified by rurality revealed distinct factors associated with lower odds of EHR adoption (Fig. 3). Among urban physicians, extreme hardship (OR: 0.25, CI: 0.24–0.26) and small practitioner status (OR: 0.12, CI: 0.12–0.12) were associated with significantly lower odds of adoption. Facility-based (OR: 0.55, CI: 0.52–0.58) and hospital-based (OR: 0.19, CI: 0.18–0.19) settings were also associated with reduced odds. Physicians in health professional shortage areas (HPSAs) had lower odds of adoption (OR: 0.75, CI: 0.72–0.78).
Fig. 3.
Multivariable logistic regression for having a certified EHR system among Quality Payment Program physician participants, stratified by rurality. Figure 3 shows stratified multivariable logistic regression analysis examining the odds of having a certified EHR system among QPP physician participants, separated into rural and urban groups. The figure illustrates the distinct associations between various physician characteristics and EHR adoption within rural and urban settings
Among rural physicians, extreme hardship (OR: 0.28, CI: 0.26–0.30) and small practitioner status (OR: 0.14, CI: 0.13–0.16) were associated with significantly lower odds of EHR adoption. Facility-based (OR: 0.23, CI: 0.20–0.27) and hospital-based (OR: 0.13, CI: 0.12–0.14) settings also had markedly lower odds. Physicians in health professional shortage areas (HPSAs) experienced lower odds of adoption (OR: 0.79, CI: 0.74–0.85). Across most categories, rural physicians exhibited lower odds of adoption than urban physicians, with slightly less pronounced effects for extreme hardship and HPSA status but more severe barriers for facility- and hospital-based providers.
Promoting Interoperability Scores (PIS)
PIS was significantly higher for urban physicians (median: 92, IQR 0–100) compared to rural physicians (median: 80, IQR 0–100; p < 0.001, Table 2). Both groups achieved high scores for the provider-to-patient exchange measure (median: 40), though rural physicians showed slightly more variability (IQR 39–40 vs. 40–40; p < 0.001). Health information exchange scores displayed the greatest disparity, with rural physicians scoring a median of 20 (IQR 10–38) versus 34 (IQR 12–39) for urban physicians (p < 0.001). Scores for electronic prescribing exchange were uniformly high (median: 10 for both groups; p < 0.001). Public health reporting scores were slightly lower for rural physicians (median: 10, IQR 8–10) than for urban physicians (median: 10, IQR 9–10; p < 0.001).
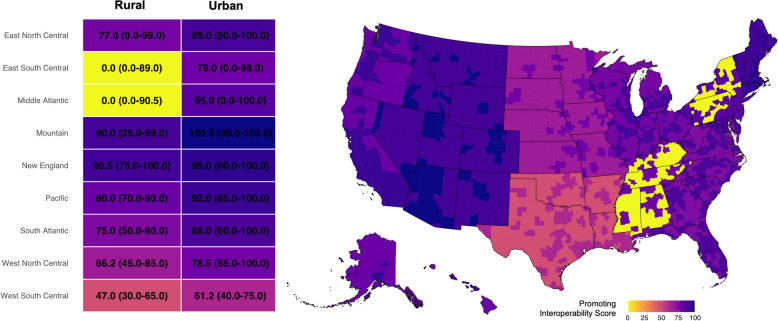
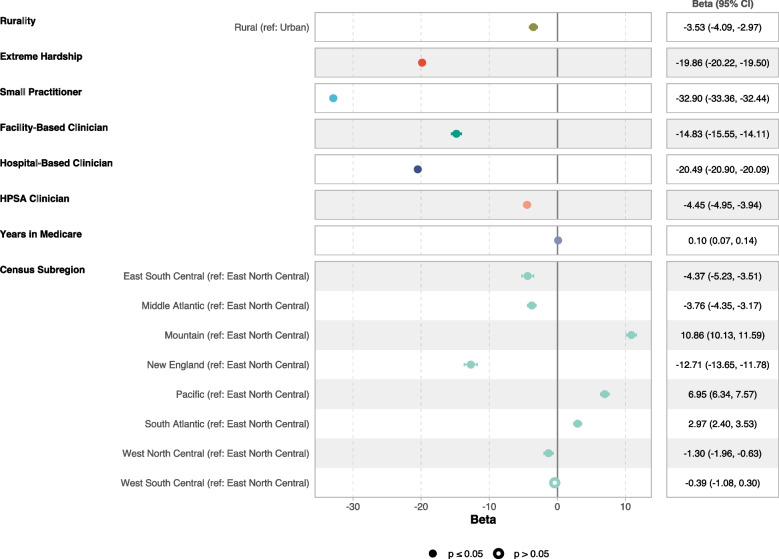
Multiple linear regression for promoting interoperability scores
Across all Census divisions except New England, rural areas were associated with consistently lower PIS scores compared to urban areas, highlighting geographical disparities in interoperability (Fig. 4). Multiple linear regression indicated that rural physicians had PIS scores 3.5 points lower on average than urban physicians (β = –3.5, CI: –4.1 to –3.0; Fig. 5). Extreme hardship (β = –20, CI: –20 to –19) and small practitioner status (β = –33, CI: –33 to –32) were associated with substantial negative differences in PIS scores, emphasizing the barriers faced by vulnerable physician groups. Detailed model specifications are in Supplemental Table 5.
Fig. 4.
Geographic distribution of average promoting interoperability score across U.S. census divisions by rurality. Figure 4 maps the geographic distribution of the median Promoting Interoperability Scores (PIS) across U.S. Census divisions, stratified by rurality at the county level. The accompanying heatmap provides the median PISs with interquartile ranges among rural and urban providers across the US. The map illustrates regional disparities in EHR interoperability, with rural areas exhibiting lower PIS than urban areas
Fig. 5.
Multiple linear regression for promoting interoperability score among Quality Payment Program physician participants. Figure 5 shows multiple linear regression analysis results showing the relationship between clinic characteristics and the Promoting Interoperability Score (PIS) among QPP physician participants. The analysis highlights the disparities in achieving interoperability goals between rural and urban settings
Stratified models revealed similarities and differences in PIS scores by rurality (Supplemental Figure 4). Among urban physicians, small practitioner status was associated with the largest differences in scores (β: –33, CI: –34 to –33), followed by hospital-based (β: –19, CI: –20 to –19) and facility-based physicians (β: –13, CI: –14 to –12). In rural settings, small practitioners (β: –30, CI: –32 to –29) and hospital-based physicians (β: –28, CI: –29 to –27) exhibited high negative associations with PIS scores, while extreme hardship was linked to more substantial score reductions than in urban areas (β: –17, CI: –18 to –16).
Regional variation indicated lower scores for Middle Atlantic physicians (urban: β: 0.77, rural: β: 0.29), while rural physicians in New England and the West North Central divisions demonstrated higher scores (β: 2.97, CI: 2.48–3.59; β: 1.17, CI: 1.05–1.32). Pacific division rural physicians had slightly lower scores (β: 0.82, CI: 0.71–0.95), contrasting with higher scores for urban physicians (β: 1.45, CI: 1.38–1.53). Detailed stratified models are available in Supplemental Table 6.
EHR adoption and PISs among primary care providers
Our secondary analysis of 57,697 primary care physicians (8,816 rural; 48,881 urban) showed lower certified EHR adoption rates overall, with urban physicians adopting at 68% and rural physicians at 56% (Supplemental Table 7). Logistic regression indicated that rural physicians had 10% lower odds of adoption compared to urban physicians (OR: 0.90, CI: 0.84–0.96). Other factors associated with lower odds of adoption included extreme hardship, small practitioner status, and facility-based practice (Supplemental Table 8).
Linear regression showed rural physicians had lower PIS scores than urban physicians (β: –1.4, CI: –2.4 to –0.46), reflecting a persistent interoperability gap in primary care (Supplemental Table 9). Associations with lower scores for hardship and small practice size mirrored broader trends.
Discussion
The transition from paper to EHRs has been a cornerstone of the movement toward an integrated, patient-centered healthcare model. EHR functionalities, including electronic documentation and decision-support tools, enhance clinical workflows and patient engagement while promoting advanced capabilities such as clinical decision-support systems, which reduce medication errors and improve adherence to evidence-based guidelines [28, 29]. EHRs improve care coordination by consolidating healthcare journeys and aiding complex patients [30]. Patient portals boost engagement and satisfaction, reduce redundancy, lower costs, and enhance the patient experience [31, 32]. Advanced EHR systems and interoperability are vital for population health strategies and public health responses [33]. However, the benefits of this digital transformation are unevenly distributed.
According to the 2014–2015 American Hospital Association’s Annual Survey Information Technology Supplement [34], while at least 75% of rural hospitals, small hospitals, and CAHs electronically sent care summaries, their overall engagement across all four domains was significantly lower, approximately 15–18%, compared to suburban and urban hospitals at 34%. They also found that smaller hospitals, CAHs, and rural hospitals often needed to catch up in having outside information electronically available at the point of care compared to their urban counterparts, which highlighted the challenges they faced in achieving comprehensive interoperability.
Furthermore, rural hospitals have shown lower readiness for Stage 2 MU, mainly due to limited resources and differences with information exchange initiatives [15]. In primary healthcare, urban providers have adopted computerized information management system (CIMS) functions more broadly than rural providers, suggesting an urban advantage in integrating advanced health technologies [35]. This trend is part of a broader digital “advanced use” divide, with CAHs lagging in adopting advanced EHR functionalities essential for performance measurement and patient engagement [7].
Our study identified high overall EHR adoption rates, with 74% of urban physicians and 64% of rural physicians using certified EHRs, but confirmed the growing divide in rural and urban settings. Even after controlling for variables such as practice size and hardship, rural physicians had 11% lower odds of adopting certified EHRs than urban physicians. This urban–rural divide in EHR adoption has significant implications for patient care, including diagnostic accuracy and preventive health measures, consistent with findings from other studies [36, 37].
Interoperability, the ability to efficiently exchange and use health information across different healthcare environments, is particularly lower in rural settings, as reflected by our study’s reduced PISs, which serve as a measure of how effectively providers meet CMS interoperability performance standards. Our regression models showed a significant PIS decrease among rural physicians, with a beta of –3.5 (CI: –4.1 to –3.0). This indicated that rural physicians face substantial challenges meeting interoperability performance requirements, such as provider-to-provider data exchange. This disparity was largely driven by differences in provider-to-provider data exchange. Hence, a substantial disparity existed in achieving interoperability goals between rural and urban settings. Physicians facing extreme hardship and those identified as small practitioners also exhibited pronounced PIS decreases.
Lower PISs in rural regions indicated challenges in seamless healthcare delivery and the potential for fragmented care, particularly in rural settings with lower EHR adoption rates [29]. These technological gaps exacerbate existing health disparities since rural populations contend with higher rates of chronic conditions and limited access to healthcare services [38]. These findings underscore the barriers that specific physician groups face in adopting and implementing EHR technologies to their full potential, particularly in terms of interoperability, which is crucial for the efficient exchange and use of health information across different healthcare environments.
While the difference in PISs between rural and urban physicians was statistically significant, the clinical significance was unclear since no studies have quantified the importance of this metric on care delivery. Thus, the relatively small difference in scores may not translate into clinically meaningful disparities in patient outcomes. However, the higher prevalence of extreme hardship, small practitioner status, and facility-based practice in rural areas may compound these providers’ challenges and potentially exacerbate healthcare disparities over time.
Our study highlights discrepancies between urban and rural healthcare physicians’ EHR adoption rates and interoperability capacity. These disparities reflect broader healthcare quality and outcome dichotomies and stem from rural physicians’ unique challenges, such as infrastructural inadequacies and workforce capacity constraints [2, 7, 39–41]. EHRs’ role in population health management is pivotal, yet their underutilization in rural areas risks creating data vacuums that hamper data-driven healthcare.
Underutilized EHRs and advanced health IT technology as defined by the QPP [3] in rural settings limit potential solutions to the provider shortage through telehealth and remote monitoring. Telehealth offers the potential to bridge the physical divide between rural dwellers and specialists [42, 43]. Telehealth also offers similar care for managing chronic diseases such as diabetes, with similar effectiveness in urban and rural settings [44, 45]. Additionally, EHRs are critical in public health initiatives, as they enable tracking disease patterns and tailoring health interventions, a capability especially critical in resource-limited rural areas [46].
While EHRs have transformative potential, our study highlights existing disparities in their availability and utilization. Both facility- and hospital-based clinicians had lower odds of EHR adoption, reflecting unique challenges. Implementation and certification decisions usually happen at the institutional rather than clinician level. These settings often qualify for CMS exemptions or alternative reporting, which may deprioritize certified EHR adoption. Addressing these disparities is essential for enhancing the quality of care and mitigating broader public health challenges, particularly in rural communities. Reduced EHR adoption in rural areas threatens to widen health disparities while excluding a significant portion of the population from the benefits of advanced health IT based on geographic location and proximity to urban centers.
Limitations
This study offers valuable insights into physician adoption of EHRs but has limitations. Focusing on CMS-associated physicians restricts the results’ generalizability across the healthcare landscape. Given the ubiquity of CMS participation, we anticipate that this limitation does not preclude comparison between rural and urban physicians since the distribution is likely non-differential and healthcare utilization and service availability across settings are similar in primary care [47]. The lack of detailed hospital data from sources like the American Hospital Association means the study captured physician-level rather than hospital-level insights into EHR adoption and interoperability. However, previous work has assessed hospital trends [48] while less has been uncovered at the physician level. Future studies should consider a more integrative approach by combining data from multiple sources to offer a comprehensive view of the EHR landscape and its implications for patient care and outcomes.
Certain healthcare entities, such as RHCs, are not required to report under the MIPS unless they bill for services under the Physician Fee Schedule (PFS). This might have impacted the representativeness of the data, as many RHCs exclusively use RHC payment methodologies and serve significant portions of rural populations [49]. The limited inclusion of RHCs in MIPS could have skewed our results, as these clinics serve approximately 62% of rural Americans and provide care to an average of 7,077 patients annually, primarily in remote areas with limited healthcare access [50]. The exclusions made during the selection process, particularly removing non-study specialties and participants with invalid EHR certification IDs, may have disproportionately affected rural physicians. These exclusions may have inadvertently resulted in a sample that underrepresents the extent of EHR adoption challenges in rural settings, where such issues prevail. Therefore, the results may reflect a slightly more favorable view of EHR adoption and interoperability in rural areas than is the case.
Conclusions
This study highlighted the significant disparities in EHR adoption and utilization across the rural spectrum. Given the transformative potential of EHRs to enhance patient care, these disparities challenge rural participation in an LHS. Addressing rural healthcare physicians’ unique challenges is vital to achieving equitable, patient-centered care across all communities. Equitable access to and effective use of EHRs and related technologies are key to enhancing healthcare outcomes and bridging the care delivery gaps between rural and urban settings. Future efforts should focus on developing and implementing strategies that support interoperability and advanced technology use in rural healthcare environments to ensure all communities benefit from healthcare informatics advancements.
Supplementary Information
Authors’ contributions
A Jerrod Anzalone: conceptualization, methodology, formal analysis, visualization, writing - original draft. Carol R. Geary: writing - review & editing. Ran Dai: writing - review & editing. Shinobu Watanabe-Galloway: writing - review & editing. James C. McClay: writing - review & editing. James R. Campbell: supervision, writing - review & editing.
Funding
Jerrod Anzalone, Ran Dai, and Shinobu Watanabe-Galloway are supported by the National Institute of General Medical Sciences, U54 GM115458, which funds the Great Plains IDeA-CTR Network. Shinobu Watanabe-Galloway is supported by the Pamela Buffett Cancer Center and its National Cancer Institute Cancer Center Support Grant, P30 CA036727. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Data availability
The data used in this study was obtained using public sources. Analyses and visualizations were performed using R and SQLite. The 2021 Experience Report Public Use File (PUF) and the Certified Health IT Product List are available freely online. All code used for data processing, analyses, and visualization is available in a public GitHub repository: https://github.com/Anzalone-Lab/Rural-Urban-EHR-Adoption-and-Interoperability.
Declarations
Ethics approval and consent to participate
This study was determined exempt by the University of Nebraska Medical Center Institutional Review Board since it does not involve human subjects and leverages widely available data sources.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Act H. Health Information Technology for Economic and Clinical Health. 2010.
- 2.Adler-Milstein J, Everson J, Lee SY. Sequencing of EHR adoption among US hospitals and the impact of meaningful use. J Am Med Inform Assoc. 2014;21(6):984–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System Policy Changes and Fiscal Year 2016 Rates; Revisions of Quality Reporting Requirements for Specific Providers, Including Changes Related to the Electronic Health Record Incentive Program; Extensions of the Medicare-Dependent, Small Rural Hospital Program and the Low-Volume Payment Adjustment for Hospitals. Final rule; interim final rule with comment period. Fed Regist 2015, 80(158):49325–49886. [PubMed]
- 4.Congress U: HR 34. 21st Century Cures Act. 2016. In: URL https://www.congress.gov/bill/114th-congress/house-bill/34/text:2017; 2017.
- 5.2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. In. Edited by Office of the National Coordinator for Health Information Technology (ONC) DoHaHSH; 2016: 62601–62759. [PubMed]
- 6.Adler-Milstein J, DesRoches CM, Kralovec P, Foster G, Worzala C, Charles D, Searcy T, Jha AK. Electronic Health Record Adoption In US Hospitals: Progress Continues. But Challenges Persist Health Aff (Millwood). 2015;34(12):2174–80. [DOI] [PubMed] [Google Scholar]
- 7.Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc. 2017;24(6):1142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to electronic health record adoption: a systematic literature review. J Med Syst. 2016;40(12):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vest JR, Kash BA. Differing Strategies to Meet Information-Sharing Needs: Publicly Supported Community Health Information Exchanges Versus Health Systems’ Enterprise Health Information Exchanges. Milbank Q. 2016;94(1):77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright A, Henkin S, Feblowitz J, McCoy AB, Bates DW, Sittig DF. Early results of the meaningful use program for electronic health records. N Engl J Med. 2013;368(8):779–80. [DOI] [PubMed] [Google Scholar]
- 11.Percent of Hospitals, By Type, that Possess Certified Health IT https://www.healthit.gov/data/quickstats/percent-hospitals-type-possess-certified-health-it
- 12.AHA Annual Survey Database™ Fiscal Year 2011. In.: American Hospital Association; 2008–2021.
- 13.National trends in hospital and physician adoption of electronic health records. https://www.healthit.gov/data/quickstats/adoption-electronic-health-records-hospital-service-type-2019-2021.
- 14.Sandefer RH, Marc DT, Kleeberg P. Meaningful use attestations among US hospitals: the growing rural-urban divide. Perspect Health Inf Manag. 2015;12(Spring):1f. [PMC free article] [PubMed] [Google Scholar]
- 15.Kim J, Ohsfeldt RL, Gamm LD, Radcliff TA, Jiang L. Hospital characteristics are associated with readiness to attain stage 2 meaningful use of electronic health records. J Rural Health. 2017;33(3):275–83. [DOI] [PubMed] [Google Scholar]
- 16.2021 QPP Experience Report Public Use File. In. Edited by Services CfMM; 2023.
- 17.Ochieng N, Rae M, Biniek J, Neuman T: Most office-based physicians accept new patients, including patients with Medicare and private insurance. In.; 2023.
- 18.Medicare Cf, Services M: CMS fast facts. In.: Retrieved November; 2021.
- 19.Certified Health IT Product List (CHPL) Open API. In. Edited by Technology OotNCfHI; 2023.
- 20.2021 Medicare promoting interoperability program scoring methodology fact sheet. In. Edited by (CMS) CfMMS; 2021.
- 21.Medicare Cf, Medicaid Services H: Medicare program; CY 2018 updates to the quality payment program; and quality payment program: extreme and uncontrollable circumstance policy for the transition year. Final rule with comment period and interim final rule with comment period. Federal register 2017;82(220):53568–54229. [PubMed]
- 22.Sittig DF, Classen DC, Singh H. Patient safety goals for the proposed Federal Health Information Technology Safety Center. J Am Med Inform Assoc. 2015;22(2):472–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Defining Rural Population. https://www.hrsa.gov/rural-health/about-us/what-is-rural.
- 24.Medicare Program; Hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and final policy changes and fiscal year 2021 rates; quality reporting and medicare and medicaid promoting interoperability programs requirements for eligible hospitals and critical access hospitals. In. Edited by HHS CfMMSC, vol. CMS-1735-F; 2020.
- 25.ACO #11-Percent of Primary Care Physicians Who Successfully Attest to an EHR Incentive Program. https://www.hhs.gov/guidance/document/aco-11-percent-primary-care-physicians-who-successfully-attest-ehr-incentive-program.
- 26.Daniel dS, Whiting K, Curry M, Lavery JA, Larmarange J: Reproducible summary tables with the gtsummary package. The R Journal. 2021;13(1):570–580.
- 27.Larmarange J: ggstats: Extension to'ggplot2'for Plotting Stats. 2023.
- 28.Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood). 2011;30(3):464–71. [DOI] [PubMed] [Google Scholar]
- 29.Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010;25(3):177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osborn CY, Mayberry LS, Wallston KA, Johnson KB, Elasy TA. Understanding patient portal use: implications for medication management. J Med Internet Res. 2013;15(7): e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103–17. [DOI] [PubMed] [Google Scholar]
- 33.Chan KS, Fowles JB, Weiner JP. Review: electronic health records and the reliability and validity of quality measures: a review of the literature. Med Care Res Rev. 2010;67(5):503–27. [DOI] [PubMed] [Google Scholar]
- 34.Patel V, Pylypchuk Y, Henry J, Searcy T. Variation in interoperability among US non-federal acute care hospitals in 2015. ONC Data Brief 2016;37.
- 35.Lintz J. Adoption of computerized information management systems (CIMS) functions: Urban versus rural primary healthcare providers. International Journal of Healthcare Management. 2021;14(4):1237–45. [Google Scholar]
- 36.Gill E, Dykes PC, Rudin RS, Storm M, McGrath K, Bates DW. Technology-facilitated care coordination in rural areas: What is needed? Int J Med Inform. 2020;137: 104102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52. [DOI] [PubMed] [Google Scholar]
- 38.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bahensky JA, Jaana M, Ward MM. Health care information technology in rural America: electronic medical record adoption status in meeting the national agenda. J Rural Health. 2008;24(2):101–5. [DOI] [PubMed] [Google Scholar]
- 40.Conn J. Stalled progress. EHR adoption lags for small, rural practices: studies. Mod Healthc. 2012;42(18):16. [PubMed] [Google Scholar]
- 41.Wittie M, Ngo-Metzger Q, Lebrun-Harris L, Shi L, Nair S. Enabling quality: electronic health record adoption and meaningful use readiness in federally funded health centers. J Healthc Qual. 2016;38(1):42–51. [DOI] [PubMed] [Google Scholar]
- 42.Bagchi AD. Expansion of telehealth across the rural–urban continuum. State and Local Government Review. 2019;51(4):250–8. [Google Scholar]
- 43.Chen J, Amaize A, Barath D. Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. J Rural Health. 2021;37(4):801–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Datta P, Eiland L, Samson K, Donovan A, Anzalone AJ, McAdam-Marx C. Telemedicine and health access inequalities during the COVID-19 pandemic. J Glob Health. 2022;12:05051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eiland L, Datta P, Samson K, Anzalone J, Donovan A, McAdam-Marx C. In-person and telehealth provider access and glycemic control for people with diabetes during the COVID-19 pandemic. J Diabetes Sci Technol. 2023;17(4):895–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holmgren AJ, Apathy NC, Adler-Milstein J. Barriers to hospital electronic public health reporting and implications for the COVID-19 pandemic. J Am Med Inform Assoc. 2020;27(8):1306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fraze TK, Lewis VA, Wood A, Newton H, Colla CH. Configuration and delivery of primary care in rural and urban settings. J Gen Intern Med. 2022;37(12):3045–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jiang J, Qi K, Bai G, Schulman K. Pre-pandemic assessment: a decade of progress in electronic health record adoption among US hospitals. Health Affairs Scholar. 2023;1(5):qxad056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MIPS Participation Fact Sheet. https://www.cms.gov/files/document/qppmipsparticipationfactsheetpdf.
- 50.Survey Emphasizes Scale and Significance of the RHC Program. https://www.narhc.org/News/30432/Survey-Emphasizes-Scale-and-Significance-of-the-RHC-Program.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study was obtained using public sources. Analyses and visualizations were performed using R and SQLite. The 2021 Experience Report Public Use File (PUF) and the Certified Health IT Product List are available freely online. All code used for data processing, analyses, and visualization is available in a public GitHub repository: https://github.com/Anzalone-Lab/Rural-Urban-EHR-Adoption-and-Interoperability.