Abstract
Background
Osteoporosis is a highly prevalent disease with distinct sex pattern. We aimed to estimate the sex specific incidence, prevalence, and disability-adjusted life (DALYs) years of osteoporosis between 1990 and 2019, with additional predictions from 2020 to 2034.
Methods
We collected osteoporosis disease burden data from the Global Burden of Disease study covering the years 1990 through 2019 in 204 countries and territories. The data included information on the number of incident cases of osteoporosis, DALYs, age-standardized incidence rates (ASIR), age-standardized prevalence rates (ASPR) and age-standardized DALYs rates. Additionally, we performed an age-period-cohort analysis to forecast the burden of osteoporosis.
Results
The global number of incidence cases of osteoporosis, in 2019, reached 41.5 million cases. From 1990 to 2019, the low-middle socio-demographic index (SDI) region had the highest estimated annual percentage change in the world. Compared to males, female's ASIR and ASPR were all about 1.5 times higher than males for the same years in the same SDI regions. The projected global total number of incidence cases for osteoporosis between 2030 and 2034 is estimated to reach 263.2 million (154.4 million for females and 108.8 for males). Additionally, the burden in terms of DALYs is predicted to be 128.7 million (with 78.4 million for females and 50.3 million for males).
Conclusion
The global burden of osteoporosis is still increasing, mainly observed in high SDI countries. Females bear a burden 1.5 times higher than males in terms of incidence and DALYs. Steps should be taken to reduce the osteoporosis burden, especially in high SDI countries.
Key words: Osteoporosis, global burden of disease, sex, estimated annual percentage change, disability-adjusted life years
Introduction
Osteoporosis is a disease characterized by decreased bone mass, microarchitectural deterioration, and fragility fractures (1). Based on the aging of the world population, osteoporosis is a major public problem that has become increasingly prevalent (2) and highly prioritized in many countries due to its significant impact on public health. In the United States alone, approximately 10 million Americans are affected by osteoporosis, and an additional 34 million people have low bone mass, putting them at higher risk of developing the condition (3). As life expectancy continues to rise and lifestyle patterns undergo dramatic changes, including alterations in diet, occupation, reduced physical activity, and increased sedentary behavior, osteoporosis is expected to become even more prevalent in the near future. Consequently, the prevalence of osteoporosis is likely to continue increasing as these trends persist.
To date, several data have reported the global epidemiological trends of osteoporosis (4). Although osteoporosis affects both sexes, it is more prevalent in women, particularly postmenopausal women, due to hormonal changes that lead to bone loss. It's crucial to comprehend the sex-specific impact of osteoporosis to create effective preventive measures and treatments. Unfortunately, epidemiological data on the global sex-specific incidence of osteoporosis is limited. This study aims to analyze the sex-specific global trends of osteoporosis in incident cases, prevalence and disability-adjusted life years (DALYs).
Method
Study data
We obtained the disease burden data on osteoporosis from an online data source tool, the Global Health Data Exchange (GHDx) query tool (https://vizhub.healthdata.org/gbd-results/), which is the world's most comprehensive catalog of surveys, censuses, vital statistics, and other health-related data. We extracted data on osteoporosis from the Global Burden of Disease Study 2019 (GBD 2019) Data Resources, a study from 1990 through 2019 in 204 countries and territories; data on the annual number of osteoporosis incident cases, prevalence cases, DALYs, and the age-standard rate were collected. Simultaneously, we obtained the global population forecasts (2017–2100) data from GBD 2019 and standard population structure data from the Lancet (5).
DALYs and socio-demographic index
DALYs is a measurement unit that quantifies the burden of disease. DALYs means the total number of healthy years lost from disease onset to death. It consists of two parts: life lost years caused by early death and life lost years caused by disability due to disease (6).
As previously described (7), the Socio-demographic Index (SDI) is a composite index that encompasses three distinct components: lag-distributed income per capita, mean education level for individuals aged 15 years or older, and total fertility rate for individuals under the age of 25. The SDI values are constrained within a scale of 0 to 100. Using the SDI cutoffs derived from country-level estimates in 2019, the SDI quintiles are established. It's important to note that countries with populations less than 1 million are excluded from these calculations. Consequently, all locations are categorized into one of these quintiles based on their corresponding SDI value in 2019.
Statistical analysis
The concept of estimated annual percentage changes (EAPC) was introduced to describe the trend of the age-standard rate. The EAPC directly reflects the trend of the age-standard rate within a defined time interval. Therefore, we calculated the EAPC to quantify osteoporosis incidence trends. First, we assumed that the natural log of the age-standard rate is linear over time using the following formula.
Then, we calculated the EAPC as 100 × (exp (β) − 1), and we obtained the 95% confidence interval (CI) from the same linear regression model. When the EAPC and lower boundary of its 95% CI are both positive, the age-standard rate is deemed to be in an increasing trend. Conversely, if the EAPC and the higher boundary of its 95% CI are both negative, the age-standard rate is deemed to be in a decreasing trend. In addition, we forecast the osteoporosis cases of incidence and DALYs, and the age-standard rate of incidence and DALYs using age-period-cohort (APC) analysis. The outcome value of the APC model following a Poisson distribution was used for the analysis; this can be used to evaluate the character and quality of trends in the diseases8. Therefore, we applied APC analysis to investigate secular trends in the osteoporosis incidence rate and number of cases. All statistical analyses were performed using the R software (Version 4.2.1, R core team).
Result
Incidence burden of osteoporosis from 1990 to 2019
In 2019, the global incident cases of osteoporosis increased to 41.5 million (95% UI = 36.9–46.4), which is more than twice the number in 1990 (20.3 million, 95% UI = 18.1–22.8). However, the age-standard rate of incidence (ASIR) in 2019 (49.2 million, 95% UI = 43.9–51.2) did not differ much from that of 1990 (47.4 million, 95% UI = 42.2–53.1) (Table 1).
Table 1.
The global incident cases, age-standard incidence rate and estimated annual percentage change of osteoporosis by sociodemographic index (SDI) region, gender and location in 1990 and 2019
| Characteristics |
1990 |
2019 |
EAPC 1990–2019 (95%CI) |
|||
|---|---|---|---|---|---|---|
| Incidence cases, in thousand (95%UI) | ASIR_1990 per 100,000 (95%UI) | Incidence cases, in thousand (95%UI) | ASIR_2019 per 100,000 (95%UI) | |||
| SDI region | ||||||
| High | 5763.8 (5159.8–6483.0) | 600.5 (534.9–676.2) | 9477.8 (8494.7–10659.3) | 635.9 (568.4–714.8) | 0.25 (0.21–0.28) | |
| High-middle | 5317.9 (4723.7–6016.0) | 478 (426.6–538.4) | 9868.1 (8752.4–11070.9) | 496.8 (441.5–558.4) | 0.10 (0.07–0.13) | |
| Middle | 5182.9 (4583.7–5832.2) | 427.8 (379.5–479.8) | 12607.3 (11142.0–14162.6) | 458.5 (406.8–513.7) | 0.28 (0.25–0.31) | |
| Low-middle | 2911.9 (2586.2–3279.9) | 407.5 (363.1–456.8) | 6773.4 (6020.3–7604.4) | 441.3 (393.4–494.1) | 0.32 (0.30–0.33) | |
| Low | 1156.1 (1024.9–1309.0) | 403.1 (359.8–453.4) | 2721.1 (2420.6–3082.4) | 424 (378.6–476.5) | 0.18 (0.17–0.18) | |
| Gender | ||||||
| Both | 20341.7 (18125.0–22819.3) | 473.6 (422.0–531.4) | 41467.5 (36875.4–46438.4) | 492.2 (438.7–551.5) | 0.16 (0.15–0.18) | |
| Female | 11980.7 (10675.6–13509.9) | 548.3 (488.0–617.6) | 24370.6 (21703.1–27356.3) | 567.2 (504.9–636.3) | 0.20 (0.17–0.23) | |
| Male | 8360.9 (7451.1–9414.9) | 397.7 (354.2–446.1) | 17096.9 (15177.1–19174.7) | 415.2 (370.3–464.5) | 0.10 (0.08–0.13) | |
| Region | ||||||
| Global | 20341.7 (18125.1–22819.3) | 473.6 (422.0–531.4) | 41467.5 (36875.4–46438.4) | 492.2 (438.7–551.5) | 0.16 (0.15–0.18) | |
| Andean Latin America | 105.0 (93.3–117.8) | 447.8 (397.0–503.3) | 294.1 (263.3–327.2) | 494.5 (442.7–550.9) | 0.35 (0.34–0.37) | |
| Australasia | 131.1 (117.1–148.7) | 590.5 (524.1–673.4) | 259.2 (230.9–293.9) | 649.5 (577.7–733.9) | 0.28 (0.24–0.33) | |
| Caribbean | 119.3 (106.1–134.3) | 439.6 (390.6–493.8) | 243.3 (216.5–273.4) | 469.6 (418.1–526.9) | 0.25 (0.24–0.27) | |
| Central Asia | 200.0 (177.6–227.3) | 400.2 (357.3–452.7) | 369.4 (325.4–421.1) | 416.4 (371.1–473.1) | 0.13 (0.13–0.14) | |
| Central Europe | 566.7 (502.7–635.9) | 389.1 (347.1–437.4) | 739.8 (662.3–831.4) | 412.3 (368.3–462.6) | 0.19 (0.19–0.20) | |
| Central Latin America | 472.4 (419.9–534.6) | 483.7 (430.6–545.4) | 1319.3 (1169.7–1488.5) | 524.6 (465.9–590.8) | 0.29 (0.28–0.31) | |
| Central Sub-Saharan Africa | 118.9 (105.2–134.6) | 419.6 (373.4–473.8) | 306.4 (270.3–347.0) | 431.7 (383.8–485.6) | 0.07 (0.05–0.08) | |
| East Asia | 4760.4 (4192.2–5367.7) | 471.8 (417–530.5) | 11025.6 (9684.3–12460.9) | 509.1 (450.0–573.2) | 0.36 (0.29–0.43) | |
| Eastern Europe | 1547.4 (1361.6–1770.8) | 572.9 (505.7–656.6) | 1802.4 (1592.9–2052.4) | 590.2 (523.3–674.8) | −0.18 (−0.29–0.07) | |
| Eastern Sub-Saharan Africa | 382.2 (338.9–432.4) | 417.5 (371.7–471.2) | 927.3 (821.2–1049.6) | 436.7 (388.4–492.4) | 0.16 (0.16–0.17) | |
| North Africa and Middle East | 795.0 (705.5–895.7) | 393.5 (348.5–442.2) | 2292.2 (2035.5–2570.6) | 430.4 (382.2–481.9) | 0.28 (0.27–0.29) | |
| Oceania | 14.2 (12.5–15.9) | 374 (331.5–418.1) | 37.4 (32.7–42.1) | 396.2 (351.6–443.2) | 0.17 (0.13–0.21) | |
| High-income Asia Pacific | 1352.3 (1198.0–1526.1) | 643 (571.9–724.2) | 2088.9 (1879.6–2343.2) | 675.4 (601.8–759.9) | 0.47 (0.38–0.56) | |
| High-income North America | 2142.9 (1921.5–2423.6) | 692.5 (614.7–787.2) | 3751.7 (3316.0–4257.7) | 736.6 (654.2–833.0) | 0.14 (0.01–0.28) | |
| South Asia | 2717.7 (2413.0–3075.6) | 389 (346.5–436.8) | 6661.5 (5942.4–7491.3) | 421.9 (375.8–472.4) | 0.28 (0.27–0.29) | |
| Southeast Asia | 929.2 (819.6–1038.1) | 306.3 (271.7–340.7) | 2375.6 (2087.0–2662.4) | 336.2 (298.3–374.2) | 0.28 (0.27–0.29) | |
| Southern Latin America | 266.8 (237.1–303.0) | 571.3 (507.5–649.7) | 480.2 (428.6–543.0) | 617.8 (552.1–699.4) | 0.29 (0.25–0.32) | |
| Southern Sub-Saharan Africa | 152.5 (135.4–171.9) | 481.7 (430.1–541.9) | 334.4 (297.1–377.0) | 507.3 (453.4–571.0) | 0.18 (0.18–0.18) | |
| Tropical Latin America | 469.1 (414.0–526.7) | 445.9 (395.9–499.6) | 1230.5 (1087.8–1380.2) | 483.2 (428.6–541.7) | 0.29 (0.28–0.30) | |
| Western Europe | 2637.5 (2366.1–2958.9) | 526 (469.5–590.9) | 3785.5 (3372.1–4249.4) | 556 (497.1–622.2) | 0.25 (0.22–0.27) | |
| Western Sub-Saharan Africa | 460.2 (408.0–519.6) | 441.4 (392.7–497.5) | 1142.0 (1008.1–1293.4) | 464.6 (413.1–523.0) | 0.16 (0.12–0.20) | |
ASIR=age-standard incidence rate; UI=uncertainty interval; EAPC=estimated annual percentage change; CI=confidence interval
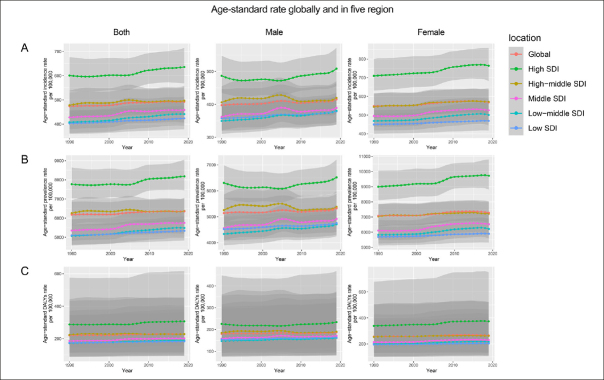
EAPC represents the tendency of the ASIR. From 1990 to 2019, the EAPC of high (0.25, 95% CI = 0.21–0.28), high-middle (0.1, 95% CI = 0.07–0.13), middle (0.28, 95% CI = 0.25–0.31), low-middle (0.32, 95% CI = 0.30–0.33) and low SDI regions (0.18, 95% CI = 0.17–0.18) were all positive (Table 1). The incidences increased in the vast majority of regions between 1990 and 2019, with the largest increase in the High-income Asia Pacific (EAPC = 0.47, 95% CI = 0.38–0.56) and the lowest increase in Central sub-Saharan Africa (EAPC = 0.07, 95% CI = 0.05–0.08). The tendency of the ASIR of osteoporosis declined only in Eastern Europe (EAPC = −0.18, 95% CI = −0.29 to 0.07) (Table 1). From 1990 to 2019, the ASIR of osteoporosis increased in all SDI regions, and even between 2005 and 2010, there was a slight decline in middle and high-middle SDI regions in males and both. In females, the ASIR of osteoporosis completely increased in all SDI regions (Fig 1a). As shown in Fig 2, a significant positive association was found between the SDI and the ASIR in 18 regions. In addition, the ASIR tended to be larger in higher SDI regions than in lower SDI regions (Fig 2).
Figure 1.
Age-standardized osteoporosis incidence (A), prevalence (B), and disability-adjusted life year (C) rates globally (red), and in high (green), high-middle (yellow), middle (purple), low-middle (baby-blue), and low (navy-blue) social-demographic index quintiles
Figure 2.

The correlation of osteoporosis age-standard rate of incidence in 2019 and the socio-demographic index
The blue line represents the average expected relationship between the socio-demographic index and the age-standard rate of incidences of osteoporosis based on values from all countries from 1990 to 2019. ASR: age-standardized rate; SDI: social-demographic index.
Regionally, Andorra, USA, and Iceland had the highest ASIR of males in 2019 (Fig 3a). However, for females, South Korea, Brunei, and Singapore had the highest ASIR in 2019 (Fig 3b).
Figure 3.

The age-standard incidence rate of osteoporosis in 2019 for males (A) and females (B) in 204 countries and territories
Countries with an extreme age-standard rate of incidence were lined out and shown in the partially enlarged map.
Prevalence and DALYs burden of osteoporosis between 1990 and 2019
Similar to the ASIR, between 1990 and 2019, the age-standard rate of prevalence (ASPR) and age-standard rate of DALYs showed an increasing trend globally (Fig 1b&c). The high SDI region had the highest ASPR every year, while the low SDI region had the lowest ASPR; however, in males, the low-middle SDI region had the lowest ASPR (Fig 1b). For males, DALY showed a decreasing trend from 1990 to 2005 and an increasing trend from 2005 to 2019 in the high SDI region. For females, DALY showed an upward trend in all SDI regions (Fig 1c).
Prediction of the incidence cases and the DALYs burden of osteoporosis from 2020 to 2034
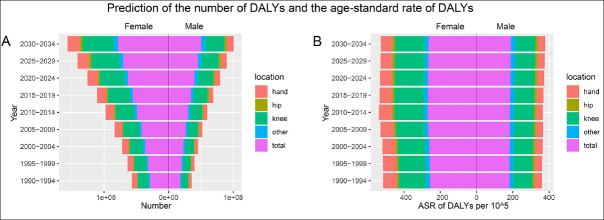
We divided the osteoporosis data into groups every five years, at the same time we marked the data with different locations of osteoporosis, including the hand, hip, and knee. Globally, the incident cases and the number of DALYs of osteoporosis showed a sharp upward trend from 1990 to 2034 (Fig Figure 4, Figure 5). For females, the total number of osteoporosis cases from 1990 to 1994 was 62.6 million; therefore, the total number of cases from 2030 to 2034 is projected to 154.4 million, which is about three times what it was from 1990 to 1994 (Table 2). For males, the number of cases from 1990 to 1994 was 43.9 million; therefore, the number of cases from 2030 to 2034 is projected to108.8 million (Table 2).
Figure 4.
Per five-year forecasts of the number of cases (A) (using scientific notation) and the age-standard rate of incidence of osteoporosis (B) at different locations of osteoporosis
Figure 5.
Per five-year forecasts of the number of disability-adjust life years (A) (using scientific notation) and the age-standard rate of disability-adjust life years of osteoporosis (B) at different locations of osteoporosis
Table 2.
The global incidence cases of osteoporosis from 1990 to 2019 and the prediction from 2020–2030
| Gender |
Year |
Position (number of incidence cases per 5 years, in thousand) |
||||
|---|---|---|---|---|---|---|
| Hand | Hip | Knee | Other | Total | ||
| Male | ||||||
| 1990–1994 | 7,408.9 | 1,848.2 | 30,033.8 | 4,655.0 | 43,946.0 | |
| 1995–1999 | 8,390.7 | 2,095.2 | 33,690.2 | 5,252.9 | 49,429.0 | |
| 2000–2004 | 9,254.4 | 2,391.7 | 38,736.9 | 5,996.4 | 56,379.3 | |
| 2005–2009 | 9,852.3 | 2,729.2 | 44,710.1 | 6,875.9 | 64,167.5 | |
| 2010–2014 | 10,217.7 | 3,108.6 | 50,713.6 | 7,855.6 | 71,895.4 | |
| 2015–2019 | 11,725.8 | 3,580.8 | 56,830.1 | 8,883.8 | 81,020.5 | |
| 2020–2024 | 13,375.6 | 4,056.2 | 63,343.7 | 9,998.8 | 90,820.6 | |
| 2025–2029 | 14,907.3 | 4,495.5 | 69,551.5 | 11,048.9 | 100,081.2 | |
| 2030–2034 | 16,298.7 | 49,037.7 | 75,490.2 | 12,043.1 | 108,815.8 | |
| Female | ||||||
| 1990–1994 | 12,382.0 | 2,005.2 | 43,833.0 | 4,429.4 | 62,649.6 | |
| 1995–1999 | 13,772.4 | 2,242.2 | 49,278.4 | 4,960.8 | 70,253.8 | |
| 2000–2004 | 15,417.7 | 2,531.1 | 56,674.7 | 5,622.6 | 80,246.1 | |
| 2005–2009 | 17,591.8 | 2,927.2 | 65,793.8 | 6,434.1 | 92,746.8 | |
| 2010–2014 | 19,620.1 | 3,411.0 | 75,556.3 | 7,356.3 | 105,943.8 | |
| 2015–2019 | 21,024.6 | 3,908.0 | 84,691.6 | 8,346.2 | 117,970.3 | |
| 2020–2024 | 22,439.2 | 4,452.0 | 94,421.8 | 9,415.1 | 130,691.3 | |
| 2025–2029 | 23,797.7 | 4,961.6 | 103,704.8 | 10,455.6 | 142,771.7 | |
| 2030–2034 | 25,220.8 | 5,444.0 | 112,550.8 | 11,467.2 | 154,380.1 | |
For females, the total number of DALYs attributed to osteoporosis between 1990 and 1994 was 28.5 million. However, the total number of cases for females from 2030 to 2034 is projected to 78.4 million. This projection represents an approximate threefold increase compared to the number of cases observed from 1990 to 1994 (Table 3). Similarly, for males, the number of cases from 1990 to 1994 was 17.9 million. According to the projections, the number of cases from 2030 to 2034 is estimated to reach 50.3 million (Table 3).
Table 3.
The global disability-adjust life years of osteoporosis from 1990 to 2019 and the prediction from 2020–2030
| Gender |
Year |
Position (number of DALYs per 5 years, in thousand) |
||||
|---|---|---|---|---|---|---|
| Hand | Hip | Knee | Other | Total | ||
| Male | ||||||
| 1990–1994 | 4,110.8 | 1,092.1 | 10,423.4 | 2,249.5 | 17,875.9 | |
| 1995–1999 | 4,581.1 | 1,242.6 | 11,704.2 | 2,558.7 | 20,086.6 | |
| 2000–2004 | 5,035.2 | 1,431.8 | 13,461.2 | 2,936.5 | 22,864.8 | |
| 2005–2009 | 5,426.6 | 1,654.8 | 15,757.4 | 3,399.5 | 26,238.3 | |
| 2010–2014 | 5,821.6 | 1,916.9 | 18,271.8 | 3,955.8 | 29,966.0 | |
| 2015–2019 | 6,891.1 | 2,255.8 | 20,920.8 | 4,586.5 | 34,654.1 | |
| 2020–2024 | 8,084.0 | 2,644.0 | 23,788.8 | 5,294.8 | 39,810.6 | |
| 2025–2029 | 9,309.7 | 3,038.7 | 26,679.0 | 6,017.7 | 45,057.6 | |
| 2030–2034 | 10,530.7 | 3,434.0 | 29,586.9 | 6,753.1 | 50,344.9 | |
| Female | ||||||
| 1990–1994 | 8,218.5 | 1,297.5 | 16,674.3 | 2,296.7 | 28,487.0 | |
| 1995–1999 | 9,026.5 | 1,453.9 | 18,733.8 | 2,579.6 | 31,793.8 | |
| 2000–2004 | 9,978.1 | 1,645.2 | 21,469.2 | 2,925.3 | 36,017.8 | |
| 2005–2009 | 11,475.8 | 1,904.5 | 25,150.5 | 3,359.1 | 41,889.9 | |
| 2010–2014 | 13,141.4 | 2,234.2 | 29,503.4 | 3,888.7 | 48,767.7 | |
| 2015–2019 | 14,492.3 | 2,599.8 | 33,849.5 | 4,500.2 | 55,441.8 | |
| 2020–2024 | 15,930.1 | 3,028.9 | 38,592.7 | 5,189.3 | 62,744.7 | |
| 2025–2029 | 17,507.4 | 3,490.4 | 43,465.3 | 5,918.9 | 70,410.6 | |
| 2030–2034 | 19,219.5 | 3,974.2 | 48,425.5 | 6,683.2 | 78,390.0 | |
Discussion
Based on GBD 2019, our study revealed sex-specific trends in global osteoporosis incidence, prevalence, and DALY. The analysis shows that global osteoporosis incidence cases more than doubled between 1990 and 2019. Compared to males, female's ASIR and ASPR were all about 1.5 times higher than males for the same years in the same SDI region; however, the age-standard rate of incidence remained largely unchanged.
Population aging and lifestyle changes have made osteoporosis a major global public health problem, not only in high SDI regions, such as North America and Europe but also in low SDI regions. Earlier epidemiological data indicates a notably higher prevalence of osteoporosis in Asian populations compared to white European or North American populations. In the latter regions, the prevalence ranges between 10% and 15% (9). Despite this, our study reported that the prevalence rates in low SDI regions are still lower than that in high SDI countries. The reasons for this result may be related to factors such as the high number of healthcare visits in high SDI areas and the long average life expectancy in the population.
Previous studies have reported a much higher prevalence rate among Chinese females (≥50 years) than males (40% vs. 22%)10. Similarly, previous studies have shown that American females are four times more likely to have osteoporosis than males (http://www.nof.org/osteoporosis/diseasefacts.htm). This may be related to specific hormonal regulations in women. Similar to our findings, there are some sex-related differences in the prevalence rate of osteoporosis. Our study showed that ASPR consistently increased in women from 1990 to 2019, while men showed a decreasing trend from 1990 to 2005. According to previous studies, the prevalence of osteoporosis among individuals aged 50 years and older is reported to be 55% for women and 68% for men in the UK (11). In the USA, nationally representative data collected from 1988 to 1994 showed a prevalence of 10.1% in people aged 50 years or older, 13–18% in older females, and 3–6% in older males (12). However, others estimate that nearly 20% of American males aged 50 years or older have osteoporosis of the hip, spine, or wrist (13). It is estimated that approximately 40% of white American women aged 50 years or older will experience a hip, spine, or wrist fracture at some time during the rest of their lives (10).
Changes in the incidence of osteoporosis are associated with many factors. Osteoporosis stands as the most prevalent systemic disease affecting the skeletal system. It arises due to a combination of biological, behavioral, and environmental factors. Among the biological factors, genetics, sex, age, and postmenopausal status play significant roles. Conversely, behavioral and environmental factors such as a low calcium diet, lack of exercise, limited outdoor activity, smoking, and excessive alcohol consumption also contribute to the development of osteoporosis (10). Some risk factors for osteoporosis have been discussed, such as bone mineral density (BMD), bone turnover (14), bone microarchitecture (15), skeletal geometry (16), and muscle mass (17). These factors primarily impact the skeletal system through pathophysiological or anatomical effects on bone structure and strength. While osteoporosis risk is higher in older populations, some of these factors can also influence younger adults, children, and even fetuses during the stages of bone size and density increase from early embryogenesis through in utero growth to infancy. Genetic and epigenetic influences, particularly on bone density, have been identified, including the role of maternal body size, lifestyle, and 25-OH Vitamin D status. These factors hold significant implications for developmental plasticity since the osteoporotic phenotype can be viewed as a result of the genotype and prevailing environment at all stages of life (18). Researchers are now looking for specific genetic loci to explore the potential for epigenetic osteoporosis and aging skeleton mechanisms to influence BMD (19, 20, 21), which may shed some light on the mechanistic study of osteoporosis. In addition, we need to consider the secondary causes of osteoporosis, such as endocrine regulation, inflammatory bowel disease, malabsorption syndromes, and nerve damage, which all contribute to osteoporosis and bone aging (22). Furthermore, many factors are particularly relevant to the elderly population.
In recent years, there has been a growing body of knowledge on the role of aging in the development of osteoporosis. Such mechanism such as genomic instability, inflammation, osteoblast/osteocyte apoptosis, epigenetic alterations, and dysfunction of proteostasis (e.g., autophagy)have been identified (23). This growing knowledge offers promising opportunities for future therapeutic approaches in the field.
Gerotherapeutics, which target the biological processes of aging, offer potential therapeutic targets for addressing age-related diseases, including osteoporosis. Some commonly researched drugs in this field include sodium-glucose cotransporter-2 inhibitors, metformin, acarbose, rapamycin/rapalogs, methylene blue, dasatinib (and quercetin), aspirin, and N-acetyl cysteine. Among these, metformin and rapamycin have been extensively studied (24). Therapies that target aging have the potential to delay or prevent various age-related diseases (25), including osteoporosis, providing significant benefits for geriatric treatment by employing single interventions that may slow multiple age-related diseases (26). As a result, potential geriatric therapies may reduce the burden of osteoporosis.
With the increasing prevalence of osteoporosis, more targeted and effective clinical assessment and treatment are needed. Evidence on optimal nutrition is still not fully substantiated, as the best measure of osteoporosis prevention for calcium and vitamin D supplementation remains undefined. There is a link between falls, muscle function, frailty, and multiple comorbidities, and interventions to reduce the risk of fracture due to osteoporosis may be possible using a combination of interventions that may be incorporated into a comprehensive geriatric assessment (27). However, in addition to risk assessment and case findings, effective interventions, such as the treatment of fractures complicating osteoporosis, are needed. Finally, even with the most effective treatments, the complications of osteoporosis are inevitable in older people; therefore, we need to ensure that the potentially devastating experience of rehabilitation is as good as possible. Perhaps, innovations such as databases for osteoporosis at various sites could improve the approach to patient care (28, 29). Compared with developed countries, the problem of population aging is more pronounced in emerging countries with relatively unsound social security systems. At the same time, the disease burden of diseases such as osteoporosis caused by population aging will become increasingly heavy. Although the results of present study suggest that the highest disease burden of osteoporosis is currently in high SDI regions. With the advancements of technology and society, developing countries such as the BRICS countries (Brazil, Russia, India, China and South Africa) located in the middle SDI regions may gradually join the high SDI region. Therefore, in the face of the upcoming disease burden of osteoporosis, corresponding preparations should be made.
Comparisons with previous studies
Several reviews have shown that the incidence rate or prevalence rate of osteoporosis is different between males and females. Chen et al. (30) shows that the prevalence of osteoporosis was significantly higher in women (25.41 %, 95 % CI: 21.54–29.49 %) than in men (15.33 %, 95 % CI: 11.8–19.21 %). And in every age group, HOLT et al.11 showed that the prevalence among people aged 50 years and older is 55% for women and 68% for men in the UK. Our study further assesses the sex stratified global incidence and prevalence and predictions of osteoporosis.
Conclusion
Between 1990 and 2019, the global burden of osteoporosis continually increased, despite decreases in ASPR and age-standardized DALY in the high SDI population at a given time. In recent years, the incidence of osteoporosis has continued to increase in higher SDI areas and to a lesser extent in lower SDI areas. This may be associated with the high average life expectancy and high rates of access to health care in high SDI countries. Therefore, steps should be taken to eliminate attributable risk factors to reduce the burden of osteoporosis, especially in countries with a higher SDI.
Acknowledgment
None
Contributor Information
Jing Zhang, Email: zhangjing666doc@163.com.
Xiao Liu, Email: kellyclarkwei@vip.qq.com, liux587@mail.sysu.edu.cn.
Author contribution
Z.C-Z: Methodology, Software, Formal Analysis, Data Curation, Writing - Original Draft. Methodology, Investigation, Data curation. Z.Q-T: Writing. Y.T-W: Methodology, Investigation. Y.F-W: Methodology, Investigation, Data curation. J.Y-M: Methodology, Investigation, J.T-L: Methodology, Data curation. P-Y: Methodology, Investigation. W.G-Z: Review & Editing. J-Z and X-L: Conceptualization, Methodology, Writing - Review & Editing, Supervision, Project administration, Funding acquisition.
Funding
This work was supported by the Natural Science Foundation of Jiangxi Province (No. 20212BAB216051 to J.Z., No. 20212BAB216047 to P.Y.); the Jiangxi Province Thousands of Plans (No. jxsq2023201105 to P.Y.); and the Hengrui Diabetes Metabolism Research Fund (No. Z-2017-26-2202-4 to P.Y.); and the National Natural Science Foundation of China (nos. 82160371 to J.Z. and nos. 82100869 to P.Y., nos. 82100347 to X. L. no. 21866019), National High Technology Research and Development Program of Guangzhou (nos. 20180304001 and nos. 2019GZR110406004 to J. F-W), Natural Science Foundation of Guangdong Province (nos. 2022A1515010582 and nos. 202201011395 to X. and Science and Technology Projects in Guangzhou (nos. 202102010007 to J.F-W), China Postdoctoral Science Foundation (Nos. 2021M703724).
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the https://vizhub.healthdata.org/gbd-results/, and no permissions were required to access the data.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict interest
The authors declare no competing financial interests.
References
- 1.Lane JM. Osteoporosis. Medical prevention and treatment. Spine (Phila Pa 1976) 1997;22(24):32s–37s. doi: 10.1097/00007632-199712151-00006. 9431642 10.1097/00007632-199712151-00006 Dec 15. [DOI] [PubMed] [Google Scholar]
- 2.Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006;194(2):S3–11. doi: 10.1016/j.ajog.2005.08.047. 16448873 10.1016/j.ajog.2005.08.047 Feb. [DOI] [PubMed] [Google Scholar]
- 3.Incidence & Prevalence Database (IPD) https://www.tdrdata.com/ipd/ipd_init
- 4.Salari N, Ghasemi H, Mohammadi L, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609. doi: 10.1186/s13018-021-02772-0. 34657598 8522202 10.1186/s13018-021-02772-0 Oct 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cousin E, Duncan BB, Stein C, et al. Diabetes mortality and trends before 25 years of age: an analysis of the Global Burden of Disease Study 2019. The Lancet Diabetes & Endocrinology. 2022;10(3):177–192. doi: 10.1016/S2213-8587(21)00349-1. 10.1016/S2213-8587(21)00349-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu M, Xia P, Tan Z, et al. Fibroblast growth factor-23 and the risk of cardiovascular diseases and mortality in the general population: A systematic review and dose-response meta-analysis. (2297-055X (Print)) [DOI] [PMC free article] [PubMed]
- 7.Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. 10.1016/S0140-6736(20)30925-9 Oct 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Bao J, Yu C, Wang J, Li C. Secular Trends of Breast Cancer in China, South Korea, Japan and the United States: Application of the Age-Period-Cohort Analysis. Int J Environ Res Public Health. 2015;12(12):15409–15418. doi: 10.3390/ijerph121214993. 26690183 4690929 10.3390/ijerph121214993 Dec 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cvijetić S, Grazio S, Kastelan D, Korsić M. [Epidemiology of osteoporosis] Arh Hig Rada Toksikol. 2007;58(1):13–18. doi: 10.2478/v10004-007-0002-x. 17424780 10.2478/v10004-007-0002-x Mar. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Tao Y, Hyman ME, Li J, Chen Y. Osteoporosis in china. Osteoporos Int. 2009;20(10):1651–1662. doi: 10.1007/s00198-009-0925-y. 19415374 10.1007/s00198-009-0925-y Oct. [DOI] [PubMed] [Google Scholar]
- 11.Holt G, Khaw KT, Reid DM, et al. Prevalence of osteoporotic bone mineral density at the hip in Britain differs substantially from the US over 50 years of age: implications for clinical densitometry. Br J Radiol. 2002;75(897):736–742. doi: 10.1259/bjr.75.897.750736. 12200242 10.1259/bjr.75.897.750736 Sep. [DOI] [PubMed] [Google Scholar]
- 12.Looker AC, Orwoll ES, Johnston CC, Jr., et al. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res. 1997;12(11):1761–1768. doi: 10.1359/jbmr.1997.12.11.1761. 9383679 10.1359/jbmr.1997.12.11.1761 Nov. [DOI] [PubMed] [Google Scholar]
- 13.Melton LJ., 3rd The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int. 2001;69(4):179–181. doi: 10.1007/s00223-001-1043-9. 11730244 10.1007/s00223-001-1043-9 Oct. [DOI] [PubMed] [Google Scholar]
- 14.Vilaca T, Gossiel F, Eastell R. Bone Turnover Markers: Use in Fracture Prediction. J Clin Densitom. 2017;20(3):346–352. doi: 10.1016/j.jocd.2017.06.020. 28716498 10.1016/j.jocd.2017.06.020 Jul–Sep. [DOI] [PubMed] [Google Scholar]
- 15.Vilayphiou N, Boutroy S, Sornay-Rendu E, Van Rietbergen B, Chapurlat R. Age-related changes in bone strength from HR-pQCT derived microarchitectural parameters with an emphasis on the role of cortical porosity. Bone. 2016;83:233–240. doi: 10.1016/j.bone.2015.10.012. 26525593 10.1016/j.bone.2015.10.012 Feb. [DOI] [PubMed] [Google Scholar]
- 16.Leslie WD, Lix LM, Morin SN, et al. Adjusting Hip Fracture Probability in Men and Women Using Hip Axis Length: the Manitoba Bone Density Database. J Clin Densitom. 2016;19(3):326–331. doi: 10.1016/j.jocd.2015.07.004. 26257267 10.1016/j.jocd.2015.07.004 Jul–Sep. [DOI] [PubMed] [Google Scholar]
- 17.Malkov S, Cawthon PM, Peters KW, et al. Hip Fractures Risk in Older Men and Women Associated With DXA-Derived Measures of Thigh Subcutaneous Fat Thickness, Cross-Sectional Muscle Area, and Muscle Density. J Bone Miner Res. 2015;30(8):1414–1421. doi: 10.1002/jbmr.2469. 25644748 10.1002/jbmr.2469 Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holroyd C, Harvey N, Dennison E, Cooper C. Epigenetic influences in the developmental origins of osteoporosis. Osteoporos Int. 2012;23(2):401–410. doi: 10.1007/s00198-011-1671-5. 21656266 10.1007/s00198-011-1671-5 Feb. [DOI] [PubMed] [Google Scholar]
- 19.Curtis EM, Murray R, Titcombe P, et al. Perinatal DNA Methylation at CDKN2A Is Associated With Offspring Bone Mass: Findings From the Southampton Women's Survey. J Bone Miner Res. 2017;32(10):2030–2040. doi: 10.1002/jbmr.3153. 28419547 10.1002/jbmr.3153 Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morris JA, Tsai PC, Joehanes R, et al. Epigenome-wide Association of DNA Methylation in Whole Blood With Bone Mineral Density. J Bone Miner Res. 2017;32(8):1644–1650. doi: 10.1002/jbmr.3148. 28394087 10.1002/jbmr.3148 Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu B, Wang CY. Osteoporosis: The Result of an ‘Aged' Bone Microenvironment. Trends Mol Med. 2016;22(8):641–644. doi: 10.1016/j.molmed.2016.06.002. 27354328 4969144 10.1016/j.molmed.2016.06.002 Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aspray TJ, Hill TR. Osteoporosis and the Ageing Skeleton. Subcell Biochem. 2019;91:453–476. doi: 10.1007/978-981-13-3681-2_16. 30888662 10.1007/978-981-13-3681-2_16 [DOI] [PubMed] [Google Scholar]
- 23.Farr JN, Almeida M. The Spectrum of Fundamental Basic Science Discoveries Contributing to Organismal Aging. J Bone Miner Res. 2018;33(9):1568–1584. doi: 10.1002/jbmr.3564. 30075061 10.1002/jbmr.3564 Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kulkarni AS, Aleksic S, Berger DM, Sierra F, Kuchel GA, Barzilai N. Geroscience-guided repurposing of FDA-approved drugs to target aging: A proposed process and prioritization. Aging Cell. 2022;21(4) doi: 10.1111/acel.13596. 35343051 9009114 10.1111/acel.13596 Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Niccoli T, Partridge L. Ageing as a risk factor for disease. Curr Biol. 2012;22(17):R741–R752. doi: 10.1016/j.cub.2012.07.024. 22975005 10.1016/j.cub.2012.07.024 Sep 11. [DOI] [PubMed] [Google Scholar]
- 26.Le Couteur DG, Barzilai N. New horizons in life extension, healthspan extension and exceptional longevity. Age Ageing. Aug 2 2022;51(8) doi: 10.1093/ageing/afac156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones D, Song X, Mitnitski A, Rockwood K. Evaluation of a frailty index based on a comprehensive geriatric assessment in a population based study of elderly Canadians. Aging Clin Exp Res. 2005;17(6):465–471. doi: 10.1007/BF03327413. 16485864 10.1007/BF03327413 Dec. [DOI] [PubMed] [Google Scholar]
- 28.Johansen A, Boulton C, Hertz K, et al. The National Hip Fracture Database (NHFD) -Using a national clinical audit to raise standards of nursing care. Int J Orthop Trauma Nurs. 2017;26:3–6. doi: 10.1016/j.ijotn.2017.01.001. 28237620 10.1016/j.ijotn.2017.01.001 Aug. [DOI] [PubMed] [Google Scholar]
- 29.Neuburger J, Currie C, Wakeman R, et al. Safe working in a 7-day service. Experience of hip fracture care as documented by the UK National Hip Fracture Database. Age Ageing. 2018;47(5):741–745. doi: 10.1093/ageing/afy074. 29796590 10.1093/ageing/afy074 Sep 1. [DOI] [PubMed] [Google Scholar]
- 30.Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1) doi: 10.1186/s12889-016-3712-7. 27716144 5048652 10.1186/s12889-016-3712-7 Oct 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the https://vizhub.healthdata.org/gbd-results/, and no permissions were required to access the data.