Abstract
Background
Cervical cancer is the only cancer that can be eliminated worldwide. Tracking the latest burden of cervical cancer is critical toward the targets set by World Health Organization (WHO) to eliminate cervical cancer as a major public health problem.
Methods
All data were extracted from the Global Cancer Observatory (GLOBOCAN) 2022. Age-standardized incidence rate (ASIR) and mortality rates (ASMR) of cervical cancer were compared and linked to Human Development Index (HDI) between populations. The estimated annual percentage changes (EAPCs) were used to characterize the temporal trend in ASIR/ASMR, and demographic estimates were projected up to 2050.
Results
Globally, an estimated 662,044 cases (ASIR: 14.12/100,000) and 348,709 deaths (ASMR: 7.08/100,000) from cervical cancer occurred in 2022, corresponding to the fourth cause of cancer morbidity and mortality in women worldwide. Specifically, 42 % of cases and 39 % of deaths occurred in China (23 % and 16 %) and India (19 % and 23 %). Both ASIR and ASMR of cervical cancer decreased with HDI, and similar decreasing links were observed for both early-onset (0–39 years) and late-onset (≥40 years) cervical cancer. Both ASIR and ASMR of overall cervical cancer showed decreasing trends during 2003–2012 (EAPC: 0.04 % and -1.03 %); however, upward trends were observed for early-onset cervical cancer (EAPC: 1.16 % and 0.57 %). If national rates in 2022 remain stable, the estimated cases and deaths from cervical cancer are projected to increase by 56.8 % and 80.7 % up to 2050. Moreover, the projected increase of early-onset cervical cancer is mainly observed in transitioning countries, while decreased burden is expected in transitioned countries.
Conclusions
Cervical cancer remains a common cause of cancer death in many countries, especially in transitioning countries. Unless scaling-up preventive interventions, human papillomavirus (HPV) vaccination and cervical cancer screening, as well as systematic cooperation within government, civil societies, and private enterprises, the global burden of cervical cancer would be expected to increase in the future.
Keywords: Cervical cancer, Incidence, Mortality, Temporal trend, Future projection
1. Introduction
Globally, cervical cancer is the second most common cancer in terms of both incidence and mortality in women of reproductive age,1 with a particularly high burden in many countries with the lowest Human Development Index (HDI).2 The main cause of cervical cancer is persistent chronic human papillomavirus (HPV) infection,1 and a combination of HPV types 16 and 18 caused 71 % of cervical cancers worldwide.3 The natural history of cervical cancer is well understood, including a HPV infection, progression to precancer, and invasion to cancer. Other risk factors, including smoking, HIV infection, early sexual debut, oral hormonal contraceptives, and multiple sexual partners, collectively contributed a large number of cervical cancers.4 All these facts make cervical cancer a largely preventable disease.5
Randomized controlled trials and numerous population-based observational studies have consistently demonstrated that screening methods, such as conventional or liquid-based cytology, visual inspection with acetic acid, and high-risk HPV genotyping, significantly reduce the incidence of and mortality rates of cervical cancer.6, 7, 8, 9, 10, 11, 12 These benefits are particularly pronounced in organized screening programs. However, participation rates and screening coverage vary widely across countries due to major barriers related to socioeconomic status, health insurance, education level, and access to healthcare services in certain settings. Countries with a highHDI generally report lower incidence and mortality rates compared to those with a low HDI. This disparity reflects challenges such as a higher HPV infection rates and limited access to effective screening and vaccination programs in less developed regions.13
To address the global burden of cervical cancer, the World Health Organization (WHO) had launched the Global Initiative for Accelerated Elimination of Cervical Cancer in 2020.14 The initiative has set national 90–70–90 targets for 2030, including fully vaccinating 90 % of girls by age 15 with HPV vaccine, screening 70 % of women at age 35 and 45 with high-performance tests, and treating 90 % of women with precancerous lesions or invasive cancer.3,15,16 While significant progress has been made in some countries, particularly those undergoing transition, cervical cancer remains a major public health challenge worldwide.4
Given the fact that cervical cancer is currently the only cancer that can be eliminated worldwide, tracking the latest burden of cervical cancer is vitally important to inform policy development and evaluate the effectiveness of integrated interventions on the prevention and control of cervical cancer. Therefore, we aimed to describe the global distribution of cervical cancer cases and deaths on the basis of the latest estimates of GLOBOCAN 2022, including current status and temporal trends, as well as the future burden of cervical cancer up to 2050 in this study.
2. Materials and methods
2.1. Data sources
We obtained the estimated new cases and deaths from cervical cancer (International Classification of Diseases, 10th edition, code C53) by 18 age groups from 185 countries on the basis of the GLOBOCAN 2022 database (https://gco.iarc.fr/) released by the International Agency for Research on Cancer (IARC) under the WHO. To ensure data quality of current estimates, all country-level raw data of cervical cancer burden were aggregated and combined by the IARC according to uniform standards on assessments of completeness, comparability, validity/accuracy and timeliness.17 High-quality incidence data from the Cancer Incidence in Five Continents (CI5plus) database published by the IARC and mortality data from the WHO mortality database were used to describe temporal trends in the burden of cervical cancer.18 The demographic projected cases and deaths were used to present the future regional and national incidence and mortality of cervical cancer up until 2050.19
2.2. Regional and national data by the United Nations regions and HDI
Regional and national cervical cancer cases and deaths were presented by 20 aggregated world regions following the geographical definition of the United Nations (UN) (World Population Prospects, the 2019 revision, https://population.un.org/wpp/), and four-tiered HDI. The HDI is the most widely used summary measure of average socio-economic development index, which is assessed based on life expectancy, education and gross national income. According to the UN Development Program's Human Development Report 2021–22,20 all countries were classified into four levels of HDI: low (HDI <0.55), medium (HDI: 0.55–0.70), high (HDI: 0.70–0.79), and very high (HDI ≥0.80).21 Moreover, transitioning countries was used as a synonym for countries with low or medium HDI, while transitioned countries were used for those with high or very high HDI.
2.3. Statistical analysis
To achieve comparable incidence and mortality rates, regional and country-specific incidence and mortality rates of cervical cancer were standardized according to the 1966 Segi-Doll World standard population,22 thereby obtaining age-standardized incidence and mortality rates (ASIR and ASMR) per 100,000 women. Namely, the age-specific populations of different countries or regions were standardized according to the age distribution of the reference population, in order to eliminate the impact of differences in age distribution across populations on cervical cancer incidence and mortality rates. To characterize the age-stratified burden of cervical cancer, early-onset and late-onset cervical cancer were defined as whether the age at diagnosis of cancer is young or elder than 40 years old (0–39 versus ≥40 years). To clearly demonstrate the link between the ASIR/ASMR of cervical cancer and the HDI, simple linear regression was used to calculate the correlation between them, and the magnitude of correlation was measured with coefficients (r). Both the Kolmogorov-Smirnov (K-S) test and the Quantile-Quantile Plot were used to test the normality assumption of linear regression. The temporal trends in regional and national ASIR/ASMR of cervical cancer were characterized using the estimated annual percentage change (EAPC) on the basis of all available data from national registries with continuous monitoring.18 Based on the UN population projection data and the current estimates in 2022, the future incidence and mortality of cervical cancer for a given country or region up until 2050 were projected after assuming that national rates in 2022 remained stable and that the national population projections in population growth and ageing were correct in the prediction period 2022–2050.19
All statistical analyses were performed with R software (version 4.3.1) and the Global Cancer Observatory online, and P < 0.05 was considered statistically significant.
3. Results
3.1. Cervical cancer incidence and mortality rates by world region and country
Globally, an estimated 662,044 cases (age-standardized incidence rate: 14.12 per 100,000) and 348,709 deaths (age-standardized mortality rate: 7.08 per 100,000) from cervical cancer occurred in 2022, corresponding to the fourth cause of cancer morbidity and mortality in women worldwide. >85 % of new cases and 90 % of deaths from cervical cancer occurred in women aged 40 years and older, while the incidence and mortality rates of late-onset cervical cancer were approximately 10-fold and 20-fold higher than those of early-onset cancer. Both of them indicated that the global burden of cervical cancer was concentrated in this age group. (Table 1)
Table 1.
Estimated cases and deaths, and age-standardized incidence and mortality rates of cervical cancer by UN region and HDI in 2022.
| World regions | Incidence |
Mortality |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All ages |
0–39 years |
40–85+ years |
All ages |
0–39 years |
40–85+ years |
||||||||||||
| Numbers | ASR | Numbers | ASR | Numbers | ASR | Numbers | ASR | Numbers | ASR | Numbers | ASR | ||||||
| World | 662,044 | 14.12 | 105,794 | 3.52 | 556,250 | 36.66 | 348,709 | 7.08 | 32,593 | 1.07 | 316,116 | 19.84 | |||||
| Region | |||||||||||||||||
| Northern America | 15,654 | 6.35 | 3988 | 3.05 | 11,666 | 13.35 | 6692 | 2.18 | 594 | 0.44 | 6098 | 5.9 | |||||
| Eastern Asia | 167,528 | 13.43 | 18,124 | 2.99 | 149,404 | 35.63 | 62,094 | 4.29 | 2888 | 0.47 | 59,206 | 12.42 | |||||
| Eastern Africa | 58,145 | 40.42 | 11,884 | 7.26 | 46,261 | 110.91 | 39,476 | 28.87 | 5548 | 3.4 | 33,928 | 83.01 | |||||
| Middle Africa | 16,268 | 31.12 | 2682 | 4.43 | 13,586 | 87.83 | 11,293 | 22.86 | 1102 | 1.83 | 10,191 | 67.55 | |||||
| Northern Africa | 7686 | 6.5 | 572 | 0.56 | 7114 | 19.12 | 4425 | 3.8 | 79 | 0.08 | 4346 | 11.71 | |||||
| Southern Africa | 12,351 | 34.89 | 2559 | 8.16 | 9792 | 91.69 | 7114 | 20.36 | 1211 | 3.87 | 5903 | 55.38 | |||||
| Western Africa | 31,249 | 26.7 | 4102 | 2.97 | 27,147 | 77.12 | 18,306 | 16.29 | 1767 | 1.28 | 16,539 | 48.2 | |||||
| Caribbean | 4012 | 14.01 | 813 | 4.94 | 3199 | 33.29 | 2397 | 7.68 | 200 | 1.21 | 2197 | 21.42 | |||||
| Central America | 15,119 | 14.34 | 3453 | 4.6 | 11,666 | 35.04 | 7646 | 7.19 | 876 | 1.15 | 6770 | 20.02 | |||||
| South-Eastern Asia | 69,886 | 17.4 | 14,101 | 5.2 | 55,785 | 43.33 | 38,703 | 9.51 | 4044 | 1.47 | 34,659 | 26.58 | |||||
| South Central Asia | 153,944 | 15.1 | 19,921 | 2.33 | 134,023 | 42.23 | 95,962 | 9.51 | 8434 | 0.99 | 87,528 | 27.61 | |||||
| Western Asia | 5724 | 4.1 | 913 | 0.79 | 4811 | 11.14 | 3036 | 2.19 | 234 | 0.2 | 2802 | 6.42 | |||||
| Eastern Europe | 35,052 | 15.74 | 7835 | 7.34 | 27,217 | 33.61 | 16,669 | 6.27 | 1721 | 1.45 | 14,948 | 16.53 | |||||
| Northern Europe | 5659 | 8.17 | 1917 | 5.48 | 3742 | 13.91 | 2145 | 2.17 | 214 | 0.6 | 1931 | 5.5 | |||||
| Southern Europe | 7792 | 6.43 | 1178 | 2.58 | 6614 | 14.62 | 3740 | 2.21 | 171 | 0.36 | 3569 | 6.13 | |||||
| Western Europe | 9716 | 6.64 | 1899 | 2.98 | 7817 | 14.44 | 4396 | 2.14 | 241 | 0.37 | 4155 | 5.89 | |||||
| Australia-New Zealand | 1047 | 5.2 | 338 | 2.96 | 709 | 9.94 | 386 | 1.44 | 37 | 0.31 | 349 | 3.83 | |||||
| Melanesia | 1340 | 27.59 | 423 | 10.04 | 917 | 64.88 | 873 | 19.33 | 209 | 4.95 | 664 | 49.88 | |||||
| South America | 44,040 | 15.55 | 9109 | 5.14 | 34,931 | 37.69 | 23,471 | 7.84 | 3031 | 1.66 | 20,440 | 20.97 | |||||
| Micronesia | 54 | 18.6 | 16 | 7.88 | 38 | 41.4 | 33 | 10.92 | 0 | 0 | 33 | 34.11 | |||||
| Polynesia | 35 | 9.59 | 8 | 3.22 | 27 | 23.11 | 17 | 4.63 | 0 | 0 | 17 | 14.47 | |||||
| HDI | |||||||||||||||||
| Very HDI country | 107,148 | 9.26 | 23,237 | 4.11 | 83,911 | 20.2 | 48,363 | 3.33 | 4024 | 0.67 | 44,339 | 8.97 | |||||
| High HDI country | 265,503 | 14.08 | 37,826 | 3.47 | 227,677 | 36.64 | 118,418 | 5.87 | 9558 | 0.86 | 108,860 | 16.49 | |||||
| Medium HDI country | 200,389 | 18.02 | 28,858 | 3.14 | 171,531 | 49.65 | 123,222 | 11.21 | 11,477 | 1.24 | 111,745 | 32.39 | |||||
| Low HDI country | 89,004 | 23.76 | 15,873 | 3.83 | 73,131 | 66.12 | 58,706 | 16.29 | 7534 | 1.82 | 51,172 | 47.03 | |||||
Abbreviations: ASR, age-standardized rate per 100,000; HDI, Human Development Index; UN, United Nations.
Age-standardized incidence rate of cervical cancer varied up to 10-fold between the UN regions, with the highest incidence rate in Eastern Africa (40.42 per 100,000), followed by Southern Africa (34.89 per 100,000), Middle Africa (31.12 per 100,000), and Melanesia (27.59 per 100,000), and the lowest incidence rate in Western Asia (4.1 per 100,000) (Table 1). As shown in Fig. 1A, the highest country-specific age-standardized incidence rate was recorded in Eswatini (95.9 per 100,000), followed by Zambia (71.5 per 100,000) and Malawi (70.9 per 100,000, Supplementary Table 1). For early-onset cervical cancer, Melanesia (10.04 per 100,000, Table 1) and Malawi (23.7 per 100,000, Supplementary Table 1) recorded the highest regional and country-specific incidence rates, respectively. For late-onset cervical cancer, Eastern Africa (110.91 per 100,000, Table 1) and Eswatini (250.5 per 100,000, Supplementary Table 1) had the highest incidence rates.
Fig. 1.
The 20 countries with the highest ASIR and ASMR of cervical cancer in 2022. (A) Overall cervical cancer, (B) Early-onset cervical cancer, (C) Late-onset cervical cancer. ASIR, Age-Standardized Incidence Rates; ASMR, Age-Standardized Mortality Rates.
Age-standardized mortality rate of cervical cancer varied up to 20-fold between the UN regions, with the highest mortality rate in Eastern Africa (28.87 per 100,000), followed by Middle Africa (22.86 per 100,000), Southern Africa (20.36 per 100,000), and Melanesia (19.33 per 100,000), and the lowest mortality rate in Australia-New Zealand (1.44 per 100,000) (Table 1). As shown in Fig. 1A, the highest national cervical cancer mortality rate was observed in Eswatini (64.3 per 100,000), followed by Malawi (54.1 per 100,000), and Zambia (49.4 per 100,000, Supplementary Table 1). The highest regional mortality rate of early-onset and late-onset cervical cancer were observed in Melanesia (4.95 per 100,000) and Eastern Africa (83.01 per 100,000) (Table 1), respectively.
Both cases and deaths were estimated to be concentrated in Asia and Africa. More than one-quarter (25.3 %) of cervical cancer cases occurred in Eastern Asia, followed by South Central Asia (23.3 %) and South-Eastern Asia (10.6 %). Nearly three in ten (27.5 %) of cervical cancer deaths occurred in South Central Asia, followed by Eastern Asia (17.8 %), and Eastern Africa (11.3 %). Among young women, South Central Asia had the largest number of cases (18.8 %) and deaths (25.9 %) from early-onset cervical cancer. Among elder women, the top three largest number of late-onset cervical cancer were observed in Eastern Asia, South Central Asia and South-Eastern Asia. There was little difference in the estimated cervical cancer cases between South Central Asia and Eastern Asia, but the estimated deaths in South Central Asia were nearly twice that of Eastern Asia (Table 1).
In the country level, 42 % of cervical cancer cases occurred in China (23 %) and India (19 %) (Supplementary Fig. 1A), and 39 % of deaths occurred in the same two countries (China versus India: 16 % versus 23 %) (Supplementary Fig. 1D). After stratified by age at diagnosis, China had more cases of early-onset (14 %) and late-onset (24 %) cervical cancer than India (14 % and 20 %) (Supplementary Fig. 1B and 1C), while India had more deaths from early-onset (19 %) and late-onset (23 %) cases than China (7 % and 17 %) (Supplementary Fig. 1E and 1F). In addition, Indonesia and Brazil had the third and fourth heaviest burden (both cases and deaths) of cervical cancer globally, respectively (Supplementary Fig. 1A and 1D).
3.2. Link between HDI and cervical cancer burden
In 2022, >50 % of cervical cancer cases were diagnosed in countries with very high and high HDI, while <50 % of deaths occurred in the same countries. The greatest burden of cervical cancer cases was found in countries with high HDI, while the greatest burden of deaths was found in countries with medium HDI, accounting for 40.1 % of new cases and 35.3 % of deaths globally (Table 1).
The K-S test supported that the normality assumption between the incidence of early-onset cervical cancer and HDI (P = 0.09) (Supplementary Fig. 2B). Although the K-S test did not support that the normality assumption between other cervical cancer burden indicators and HDI (all other P values < 0.05), the Quantile-Quantile plots approximately support the normality assumption (Supplementary Fig. 2). Specifically, both the incidence and mortality rates of over cervical cancer decreased as HDI increased. As shown in Fig. 2, the incidence and mortality rate were 9.26 and 3.33 per 100,000 in countries with very high HDI, while they were 23.76 and 16.29 per 100,000 in countries with low HDI, respectively. A similar trend was observed for both early- and late-onset cervical cancer, with a more pronounced decline for late-onset cases.
Fig. 2.
Link between HDI and ASIR and ASMR of cervical cancer. (A) ASIR of overall cervical cancer. (B) ASIR of early-onset cervical cancer. (C) ASIR of late-onset cervical cancer. (D) ASMR of overall cervical cancer. (E) ASMR of early-onset cervical cancer. (F) ASMR of late-onset cervical cancer. ASIR, Age-Standardized Incidence Rates; ASMR, Age-Standardized Mortality Rates; HDI, Human Development Index.
3.3. Temporal trends in cervical cancer incidence and mortality
To ensure a robust and consistent analysis, we selected 30 countries with continuous and complete monitoring data during the study period for primary analyses to investigate the overall temporal trends in cervical cancer incidence and mortality. Based on the complete data from 30 countries, five countries demonstrated an increasing trend in the ASIR of cervical cancer. The countries with the largest increases included Bulgaria (EAPC: 1.6 % during 1993–2013), Latvia (EAPC: 1.4 % during 1983–2012), and Lithuania (EAPC:1.2 % during 1978–2012). In contrast, the largest decreases in ASIR were observed in Brazil (EAPC: −6.1 % during 1993–2012), Chile (EAPC: −5.5 % during 1998–2012), and Poland (EAPC: −4.6 % during 1998–2012) (Fig. 3A). Subcategory analysis showed that eight countries exhibited increasing trends in early-onset cervical cancer ASIR, while five countries demonstrated increasing trends in late-onset ASIR (Fig. 3B and C). These findings underscore potential disparities in healthcare access and early intervention programs across different regions. To provide a comparable temporal trends in cervical cancer incidence and mortality, sensitivity analyses of the EAPC were conducted based on incidence or mortality data within the same time period covered by all countries (2003–2010), and the global EAPCs of overall, early-onset, and late-onset cervical cancer ASIR were −0.04 %, 1.16 %, and −1.45 %, respectively (Supplementary Fig. 3).
Fig. 3.
EAPC of Age-Standardized Rate of cervical cancer, based on all available country-level data. (A) EAPC of overall cervical cancer ASIR. (B) EAPC of early-onset cervical cancer ASIR. (C) EAPC of late-onset cervical cancer ASIR. (D) EAPC of overall cervical cancer ASMR. (E) EAPC of early-onset cervical cancer ASMR. (F) EAPC of late-onset cervical cancer ASMR. ASIR, Age-Standardized Incidence Rates; ASMR, Age-Standardized Mortality Rates; EAPC, Estimated Annual Percentage Change.
For the age-standardized mortality rate (ASMR), four countries showed increasing trends. The countries with the largest increases included Spain (EAPC: 2.0 % during 1951–2017), Bulgaria (EAPC: 1.7 % during 1964–2018), and Latvia (EAPC: 0.7 % during 1980–2018). The largest decreases in ASMR were recorded in Chile (EAPC: −3.8 % during 1984–2018), Costa Rica (EAPC: −3.5 % during 1985–2017), and Canada (EAPC: −3.3 % during 1950–2017) (Fig. 3D). Further analysis showed that six countries showed an increasing trend in early-onset cervical cancer ASMR, while seven countries exhibited increasing trends in late-onset ASMR (Fig. 3E and F). These results would reflect significant variations in vaccination and screening coverage among regions. Consistent with the incidence trends, sensitivity analyses within the same time period for mortality (2003–2010) showed that the global EAPCs for cervical cancer ASMR were −1.03 % (overall), 0.57 % (early-onset), and −1.28 % (late-onset), as shown in Supplementary Fig. 3.
3.4. Demographic predicted cervical cancer cases and deaths up to 2050
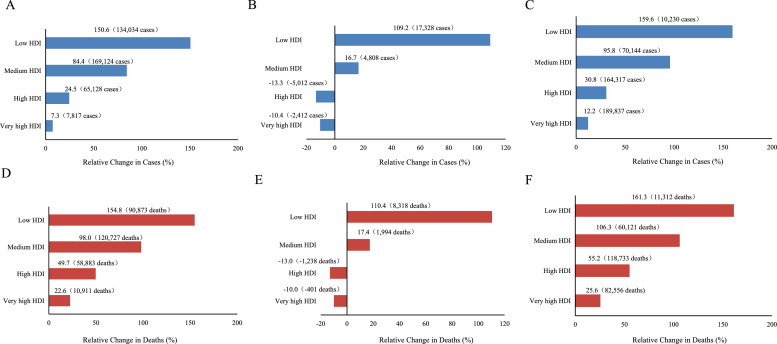
Based on the stable national changes in population growth and aging, the estimated cases of cervical cancer are projected to increase by 56.8 % from 2022 to 2050, with an estimated 1 million cases in 2050. Meanwhile, a total of 630,000 deaths were projected to occur in 2050, with an increase of 80.7 %. The highest absolute increases in cases and deaths from cervical cancer would occur in countries with medium HDI, with an estimated 169,124 cases and 120,727 deaths, respectively. The largest relative increases in cases and deaths would occur in countries with low HDI, with 150.6 % of increase in cases and 154.8 % of increase in deaths, respectively (Fig. 4A and D). However, projected cases and deaths from early-onset cervical cancer would increase in countries with low (109.2 % and 110.4 %) and medium HDI (16.7 % and 17.4 %) and decrease in countries with high and very high HDI (Fig. 4B and E).
Fig. 4.
Predicted percentage change in estimated cases and deaths from cervical cancer between 2022 and 2050 by HDI. (A) Change in overall cervical cancer cases. (B) Change of early-onset cervical cancer cases. (C) Change of late-onset cervical cancer cases. (D) Change of overall cervical cancer deaths. (E) Change of early-onset cervical cancer deaths. (F) Change of late-onset cervical cancer deaths. HDI, Human Development Index.
4. Discussion
This study provided a comprehensive and up-to-date overview of global, regional, and national patterns of cervical cancer in 2022. Globally, cervical cancer is the fourth most common cause of cancer incidence and mortality among women, and the disease is the most common cancer type and the leading cause of cancer death in several transitioning countries, mainly in sub-Saharan Africa as well as South America and South-Eastern Asia. Overall, incidence and mortality of cervical cancer vary widely by regions and countries, and they vary at least 10-fold among the 20 UN regions. If there were no effectively preventive and curative interventions to curb the current status of cervical cancer, the global burden of cervical cancer is expected to increase in the future, especially in transitioning countries.
The significant geographic disparities in cervical cancer burden largely reflected the marked regional and national differences in exposure to risk factors, including sexually transmittable infections (e.g. human deficiency virus and Chlamydia trachomatis), smoking, a higher number of childbirths, and long-term use of oral contraceptives),23 as well as inequalities in access to adequate screening, universal HPV vaccination, and effective cancer treatment facilities.24 Previous study showed that the HPV prevalence in cervical cancer could touch 99 %, which highly suggested HPV infection is a necessary cause of cervical cancer.25 Up until now, a total of 12 of the 448 known HPV types were classified as group I carcinogens by the IARC Monographs.26 Furthermore, numerous studies concluded that HPV testing is effective in detecting cervical precancer and in subsequently reducing the incidence of cervical cancer.5,12 However, many women in low-resource settings have not been vaccinated against HPV due to lack of essential laboratory infrastructure for vaccine development, along with the absence of essential cold chain storage facilities to keep the vaccine intact. These challenges, along with economic factors and competing health priorities, contribute to the low vaccination rates.27 Therefore, up until 2014, <3 % of women from less developed countries received the full course of HPV vaccine, which typically required multiple doses, compared with 33.6 % of women in more developed regions.28 Recent updates to the WHO guidelines, however, recommend a single-dose regimen for girls and boys aged 9–14 years, a change that could make it easier to scale up vaccination efforts in low-resource settings.29 Rapid roll-out of this updated HPV vaccination approach would be the most effective strategy to address current disparities in cervical cancer prevention.30
Although HPV testing alone would be the most effective in cervical cancer prevention given its balance of benefits against harms,5 several methods currently used in screening are also effective in reducing both the incidence and the mortality associated with cervical cancer.8, 9, 10, 11,31 In 2019, a total of 36 % of women aged 30–49 years have been screened in their lifetime worldwide, which was notably far from the target screening rate (70 %) proposed by the WHO.32 Specifically, 84 % of women from the high-income countries had been screened ever in lifetime, compared with 48 % in upper-middle-income countries, only 9 % in lower-middle-income countries, and 11 % in low-income countries.32 In China, the current largest populous country, although the regional cervical cancer screening coverage increased by 6 % during 2013–2018,33 the national screening coverage was 43.4 % in women aged 35–44 years and 36.8 % in women aged 35–64 years in 2018–2019. This screening coverage remained far below the target 70 % screening rate, and obvious disparity in lifetime screening coverage exists between urban and rural areas (41.1 % versus 32.4 %).34 The cost of cervical cancer screening in China varies depending on government subsidies and healthcare programs. While certain government-led initiatives, such as the National Cervical Cancer Screening Program, provide free or low-cost screening for rural women or other target groups, many women not covered by these programs must pay out-of-pocket. This financial burden can significantly limit access, especially in low-income areas, exacerbating the disparities in screening coverage. Moreover, systemic barriers to increasing screening coverage included a shortage in qualified healthcare personnel, equipment allocation, health education, and screening service quality control.33 These financial and systemic challenges underscore the importance of further policy interventions and investments to improve screening access and equity in China.
Consistent with previous studies,35 a broad decline in cervical cancer incidence and mortality has been observed in most countries over the last few decades. The dramatic declines would largely attributed to early implementation of organized screening programs, improvements in screening coverage, diagnosis and treatment, and the early initiation of HPV vaccination programs which recommended HPV vaccination at a younger age, typically between 9 and 14 years old, before individuals become sexually active,1,24 This timing maximizes the effectiveness of the vaccine in preventing HPV infections and related diseases. Moreover, the declines would also reflected the marked reduction of infection with high-risk HPV, which resulted from improved personal and genital hygiene, such as regular washing with mild soap and water, to reduce the risk of infections that could potentially increase the risk of cervical cancer. These changes, alongside declines in fertility and a decreased prevalence of sexually transmitted diseases associated with continuous rises in HDI,1,24,36 contributed to the observed reductions. All of these supported that both the incidence and the mortality of cervical cancer decreased with HDI, which is consistent with previous studies.13,36
However, an increased trend in incidence and mortality of cervical cancer was not only observed in some low-income countries (Uganda), but also observed in some high- or middle-income countries (e.g. Ireland, Bulgaria, Latvia, Lithuania, Israel, Ukraine, and Turkey), especially for young women. The exact reasons for the upward trend in these countries and young women remain unknown, and it would be a combined result of several factors. First, high exposure to high-risk HPV would likely play the key role. In 2023, the estimated prevalence of HPV16/18 among females with cervical cancer were 80.3 % in Bulgaria, 79.5 % in Israel, 74.2 % in Ireland, 74.0 % in Ukraine, and 70.0 % in Latvia, respectively.37 Secondly, increased use of improved screening tests and histological verification of cervical precancerous lesions could partially explain the steady increase in incidence over the past decades.38 In 2019, all of the cervical cancer screening coverages in these regions (68 % in Bulgaria, 61 % in Israel, 58 % in Latvia, 57 % in Ukraine) were relatively higher than the global average screening coverages (36 %).32 Thirdly, the HPV prevalence in younger women with normal cervical cytology was significantly higher than in elder women globally.37,39 The increasing HPV prevalence in younger women may be related to earlier age at first sexual activity, increased number of lifetime sexual partners, inadequate condom use, and more permissive sexual attitudes in the younger population.38,40,41 Additionally, the prevalence of high-risk HPV showed a bimodal U-shaped curve with age. Although almost all women have a HPV infection between the ages of 15 and 24, these HPV infections would quickly cleared up due to the relatively strong immunity of younger women.42, 43, 44 At the second peak after the age of 40, women's immunity has declined significantly and HPV virus clearance becomes more difficult. Therefore, it is vital important to provide additional evaluation (e.g., colposcopy with biopsy) for middle-aged and elder women even when cytology results are negative but HPV 16/18 testing is positive.45 Lastly, decreased screening activity in younger women, and increased immigrants from countries with limited cervical cancer screening and HPV vaccination may also collectively have an impact on the increased incidence of cervical cancer in high- or middle-income countries.46,47
Given the relatively high incidence rates and unfavorable trends of cervical cancer in many transitioning countries, the cervical cancer burden would continue to grow and many transitioning countries may not achieve the national 90–70–90 elimination goal without significantly scaling-up preventive interventions, HPV vaccination and cervical cancer screening.48 Additionally, fertility rates have steadily fallen in all countries since 1950 and would continue declining worldwide. Up until 2050, less than one-quarter of countries are expected to have fertility rates above replacement level, and the number would decline to only six by 2100.49 Alongside the falling fertility rates and longer life expectancy, several countries would further suffer the increased burden of cervical cancer due to the rapid aging.50 Moreover, the multifaceted impact of rapid aging on economic development and health services would be deeply perceived by both transitioning and transitioned countries, especially for the populous countries, including China and India.51 To mitigate or even reverse the increased burden, a sustainable and integral systematic cooperation within a broad range of stakeholders (government, civil societies, and private enterprises) and life-cycle management for the aging population are vitally important and urgently needed.27
Although this study provided an updated global landscape of cervical cancer burden, including the current status, temporal trend and demographic projections, some limitations also deserved attentions. First, high quality national data remained sparse in many countries, especially for transitioning countries, due to limited resources and underdeveloped statistical systems. This limitation might bias the estimated burden of cervical cancer in these regions. However, despite these challenges, the available data still provide valuable insights into global trends and disparities, forming a useful basis for policy making and resource allocation. Second, the current estimates cannot replace high-quality data with continuous monitoring collected by cancer registries and vital registries, which may also have an impact on the estimated cervical cancer burden. Thirdly, while temporal trend are assessed based on high-quality cancer registry data compiled in the CI5, we could not quantify the most recent trends in countries that have recently introduced HPV vaccination and routine screening.52 Thus, we could not observe the impact of these preventive interventions on the cervical cancer burden in those countries (such as China and Slovenia). These findings underscore the importance of strengthening cancer surveillance systems globally to improve the accuracy and comprehensiveness of future analyses. Finally, due to the lack of more detailed country-specific information on risk factors in GLOBOCAN, including smoking, alcohol consumption, obesity, HPV infection rates, HPV screening rates, and cervical cytology screening rates, it is difficult to provide a more detailed distribution of the burden of cervical cancer across populations.
5. Conclusions
Cervical cancer remains a common cause of death in many countries, especially in transitioning countries, which partly reflected the higher prevalence of high-risk HPV infection as well as limited access to screening and vaccination. The disease burden would continue to grow in the future, unless scaling-up preventive interventions, HPV vaccination and cervical cancer screening, as well as systematic cooperation within a broad range of stakeholders (government, civil societies, and private enterprises).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
This work was supported by the National Key R&D Program of China (grant number: 2021YFC2500400), National Natural Science Foundation of China (grant numbers: 82172894, 82073028, 82204121), and China Postdoctoral Science Foundation (grant number: 2023M742617). We thank the cancer registries worldwide who compiled and submitted their data for the GLOBOCAN project.
Author contributions
J.W., Q.J., Y.Z., Y.J. and Y.H. designed the study, guided the writing of manuscript, and reviewed manuscript. J.W., Q.J., J.L., X.L., H.D., Z.F., Y.L., and Y.Z. collected the data. J.W. and Q.J. processed the data, performed statistical analysis, and drafted the manuscript. W.J., Z.L., and Y.H. revised the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jncc.2024.11.006.
Contributor Information
Lei Yang, Email: younger2083@163.com.
Yubei Huang, Email: yubei_huang@163.com.
Appendix. Supplementary materials
References
- 1.Arbyn M., Weiderpass E., Bruni L., et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Das M. WHO launches strategy to accelerate elimination of cervical cancer. Lancet Oncol. 2021;22(1):20–21. doi: 10.1016/S1470-2045(20)30729-4. [DOI] [PubMed] [Google Scholar]
- 4.Yang M., Du J., Lu H., Xiang F., Mei H., Xiao H. Global trends and age-specific incidence and mortality of cervical cancer from 1990 to 2019: an international comparative study based on the Global Burden of Disease. BMJ Open. 2022;12(7) doi: 10.1136/bmjopen-2021-055470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouvard V., Wentzensen N., Mackie A., et al. The IARC perspective on cervical cancer screening. N Engl J Med. 2021;385(20):1908–1918. doi: 10.1056/NEJMsr2030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sankaranarayanan R., Nene B.M., Shastri S.S., et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360(14):1385–1394. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 7.Sankaranarayanan R., Nene B.M., Dinshaw K.A., et al. A cluster randomized controlled trial of visual, cytology and human papillomavirus screening for cancer of the cervix in rural India. Int J Cancer. 2005;116(4):617–623. doi: 10.1002/ijc.21050. [DOI] [PubMed] [Google Scholar]
- 8.Siebers A.G., Klinkhamer P.J.J.M., Grefte J.M.M., et al. Comparison of liquid-based cytology with conventional cytology for detection of cervical cancer precursors: a randomized controlled trial. JAMA. 2009;302(16):1757–1764. doi: 10.1001/jama.2009.1569. [DOI] [PubMed] [Google Scholar]
- 9.Klug S.J., Neis K.J., Harlfinger W., et al. A randomized trial comparing conventional cytology to liquid-based cytology and computer assistance. Int J Cancer. 2013;132(12):2849–2857. doi: 10.1002/ijc.27955. [DOI] [PubMed] [Google Scholar]
- 10.Sankaranarayanan R., Esmy P.O., Rajkumar R., et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster-randomised trial. Lancet Lond Engl. 2007;370(9585):398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- 11.Denny L., Kuhn L., De Souza M., Pollack A.E., Dupree W., Wright T.C. Screen-and-treat approaches for cervical cancer prevention in low-resource settings: a randomized controlled trial. JAMA. 2005;294(17):2173–2181. doi: 10.1001/jama.294.17.2173. [DOI] [PubMed] [Google Scholar]
- 12.Ronco G., Dillner J., Elfström K.M., et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet Lond Engl. 2014;383(9916):524–532. doi: 10.1016/S0140-6736(13)62218-7. [DOI] [PubMed] [Google Scholar]
- 13.Lin S., Gao K., Gu S., et al. Worldwide trends in cervical cancer incidence and mortality, with predictions for the next 15 years. Cancer. 2021;127(21):4030–4039. doi: 10.1002/cncr.33795. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2020. Accessed December 12, 2024. https://www.who.int/publications-detail-redirect/9789240014107
- 15.Simms K.T., Steinberg J., Caruana M., et al. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020-99: a modelling study. Lancet Oncol. 2019;20(3):394–407. doi: 10.1016/S1470-2045(18)30836-2. [DOI] [PubMed] [Google Scholar]
- 16.Brisson M., Kim J.J., Canfell K., et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet Lond Engl. 2020;395(10224):575–590. doi: 10.1016/S0140-6736(20)30068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferlay J., Ervik M., Lam F., et al. Global Cancer Observatory: cancer Today (version 1.1). Lyon, France: international Agency for Research on Cancer. Accessed December 12, 2024. https://gco.iarc.who.int/today.
- 18.Ervik M., Lam F., Laversanne M., et al. Global Cancer Observatory: cancer over time. Lyon, France: international Agency for Research on Cancer. Accessed December 12, 2024. https://gco.iarc.fr/overtime/en/about.
- 19.Ferlay J., Laversanne M., Ervik M., et al. Global Cancer Observatory: cancer Tomorrow (version 1.1). Lyon, France: international Agency for Research on Cancer. Accessed December 12, 2024. https://gco.iarc.fr/tomorrow.
- 20.United Nations Development Programme. Human Development Report 2021. Accessed December 12, 2024. https://hdr.undp.org/content/human-development-report-2021-22.
- 21.Kohler J.C., Bowra A. Exploring anti-corruption, transparency, and accountability in the World Health Organization, the United Nations Development Programme, the World Bank Group, and the Global Fund to Fight AIDS, Tuberculosis and Malaria. Glob Health. 2020;16(1):101. doi: 10.1186/s12992-020-00629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Say L., Chou D., Gemmill A., et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–e333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 23.Bray F., Laversanne M., Sung H., et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–263. doi: 10.3322/caac.21834. [DOI] [PubMed] [Google Scholar]
- 24.Singh D., Vignat J., Lorenzoni V., et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. 2023;11(2):e197–e206. doi: 10.1016/S2214-109X(22)00501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walboomers J.M., Jacobs M.V., Manos M.M., et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 26.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007;90:1–636. [PMC free article] [PubMed]
- 27.Yan H., Wang Q., Qiao Y. Cervical cancer prevention in China: where are we now, and what's next? Cancer Biol Med. 2024;21(3):213–217. doi: 10.20892/j.issn.2095-3941.2023.0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruni L., Diaz M., Barrionuevo-Rosas L., et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4(7):e453–e463. doi: 10.1016/S2214-109X(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 29.Kreimer A.R., Watson-Jones D., Kim J.J., Dull P. Single-dose human papillomavirus vaccination: an update. J Natl Cancer Inst Monogr. 2024;2024(67):313–316. doi: 10.1093/jncimonographs/lgae030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruni L., Diaz M., Barrionuevo-Rosas L., et al. Correction to Lancet Glob Health 2016; 4: e453-63. Lancet Glob Health. 2017;5(7):e662. doi: 10.1016/S2214-109X(17)30186-9. [DOI] [PubMed] [Google Scholar]
- 31.Sankaranarayanan R., Nene B.M., Dinshaw K.A., et al. A cluster randomized controlled trial of visual, cytology and human papillomavirus screening for cancer of the cervix in rural India. Int J Cancer. 2005;116(4):617–623. doi: 10.1002/ijc.21050. [DOI] [PubMed] [Google Scholar]
- 32.Bruni L., Serrano B., Roura E., et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. Lancet Glob Health. 2022;10(8):e1115–e1127. doi: 10.1016/S2214-109X(22)00241-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y., Guo J., Zhu G., Zhang B., Feng X.L. Changes in rate and socioeconomic inequality of cervical cancer screening in northeastern China from 2013 to 2018. Front Med. 2022;9 doi: 10.3389/fmed.2022.913361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang M., Zhong Y., Wang L., et al. Cervical cancer screening coverage - China, 2018-2019. China CDC Wkly. 2022;4(48):1077–1082. doi: 10.46234/ccdcw2022.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vu M., Yu J., Awolude O.A., Chuang L. Cervical cancer worldwide. Curr Probl Cancer. 2018;42(5):457–465. doi: 10.1016/j.currproblcancer.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Basu P., Ponti A., Anttila A., et al. Status of implementation and organization of cancer screening in The European Union Member States-summary results from the second European screening report. Int J Cancer. 2018;142(1):44–56. doi: 10.1002/ijc.31043. [DOI] [PubMed] [Google Scholar]
- 37.HPV Information Centre. Statistics. Accessed December 12, 2024. https://hpvcentre.net/datastatistics.php.
- 38.Orumaa M., Leinonen M.K., Campbell S., Møller B., Myklebust T.Å., Nygård M. Recent increase in incidence of cervical precancerous lesions in Norway: nationwide study from 1992 to 2016. Int J Cancer. 2019;145(10):2629–2638. doi: 10.1002/ijc.32195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang J., Deng Y., Boakye D., et al. Global distribution, risk factors, and recent trends for cervical cancer: a worldwide country-level analysis. Gynecol Oncol. 2022;164(1):85–92. doi: 10.1016/j.ygyno.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 40.Melesse D.Y., Mutua M.K., Choudhury A., et al. Adolescent sexual and reproductive health in sub-Saharan Africa: who is left behind? BMJ Glob Health. 2020;5(1) doi: 10.1136/bmjgh-2019-002231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Le Gall A., Mullet E., Rivière Shafighi S. Age, religious beliefs, and sexual attitudes. J Sex Res. 2002;39(3):207–216. doi: 10.1080/00224490209552143. [DOI] [PubMed] [Google Scholar]
- 42.Moscicki A.B., Hills N., Shiboski S., et al. Risks for incident human papillomavirus infection and low-grade squamous intraepithelial lesion development in young females. JAMA. 2001;285(23):2995–3002. doi: 10.1001/jama.285.23.2995. [DOI] [PubMed] [Google Scholar]
- 43.Li X., Xiang F., Dai J., et al. Prevalence of cervicovaginal human papillomavirus infection and genotype distribution in Shanghai, China. Virol J. 2022;19(1):146. doi: 10.1186/s12985-022-01879-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wei X., Zhang J., Mei Y., Dai Q., Yang X., Wang X. Prevalence and genotype distribution of HPV6/11/16/18 infections among 180,276 outpatient females from a women's and children's central hospital, 2015-2021, Chengdu, China. Sci Rep. 2023;13(1):22249. doi: 10.1038/s41598-023-48222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perkins R.B., Guido R.S., Castle P.E., et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24(2):102–131. doi: 10.1097/LGT.0000000000000525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel A., Galaal K., Burnley C., et al. Cervical cancer incidence in young women: a historical and geographic controlled UK regional population study. Br J Cancer. 2012;106(11):1753–1759. doi: 10.1038/bjc.2012.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jørgensen L., Gøtzsche P.C., Jefferson T. Increased incidence of cervical cancer in Sweden: an unlikely link with human papillomavirus (HPV) vaccination. BMJ Sex Reprod Health. 2019;45:303–304. doi: 10.1136/bmjsrh-2018-200245. [DOI] [PubMed] [Google Scholar]
- 48.Brisson M., Kim J.J., Canfell K., et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet Lond Engl. 2020;395(10224):575–590. doi: 10.1016/S0140-6736(20)30068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.GBD 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950-2021, with forecasts to 2100: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet Lond Engl. 2024;403(10440):2057–2099. doi:10.1016/S0140-6736(24)00550-6 [DOI] [PMC free article] [PubMed]
- 50.Vollset S.E., Goren E., Yuan C.W., et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet Lond Engl. 2020;396(10258):1285–1306. doi: 10.1016/S0140-6736(20)30677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gong J., Wang G., Wang Y., et al. Nowcasting and forecasting the care needs of the older population in China: analysis of data from the China Health and Retirement Longitudinal Study (CHARLS) Lancet Public Health. 2022;7(12):e1005–e1013. doi: 10.1016/S2468-2667(22)00203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.An J., Liu Y., Ma Y., et al. Real-world data of China: analysis of HPV vaccine coverage and post-vaccination adverse reaction monitoring in western Chinese provinces from 2018 to 2021. Hum Vaccin Immunother. 2024;20(1):2315653. doi: 10.1080/21645515.2024.2315653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.