Abstract
BACKGROUND—Infants with isolated totally anomalous pulmonary venous return often present severely decompensated, such that they are at high risk for surgical repair. On the other hand, if surgical repair can be safely accomplished, the outlook is usually good. Thus prenatal diagnosis would be expected to improve the prognosis for the affected child. OBJECTIVE—To describe the features of isolated totally anomalous pulmonary venous drainage in the fetus. DESIGN—Four fetuses with isolated totally anomalous pulmonary venous connection were identified and the echocardiographic images reviewed. Measurements of the atrial and ventricular chambers and both great arteries were made and compared with normal values. SETTING—Referral centre for fetal echocardiography. RESULTS—There were two cases of drainage to the coronary sinus, one to the right superior vena cava, and one to the inferior vena cava. Right heart dilatation relative to left heart structures was a feature of two cases early on, and became evident in some ratios late in pregnancy in the remaining two. CONCLUSIONS—Ventricular and great arterial disproportion in the fetus can indicate a diagnosis of totally anomalous pulmonary venous connection above the diaphragm. However, in the presence of an atrial septal defect or with infradiaphragmatic drainage, right heart dilatation may not occur until late in pregnancy. The diagnosis of totally anomalous pulmonary venous drainage in fetal life can only be reliably excluded by direct examination of pulmonary venous blood flow entering the left atrium on colour or pulsed flow mapping. Keywords: congenital heart disease; fetus; total anomalous pulmonary venous drainage; echocardiography
Full Text
The Full Text of this article is available as a PDF (150.7 KB).
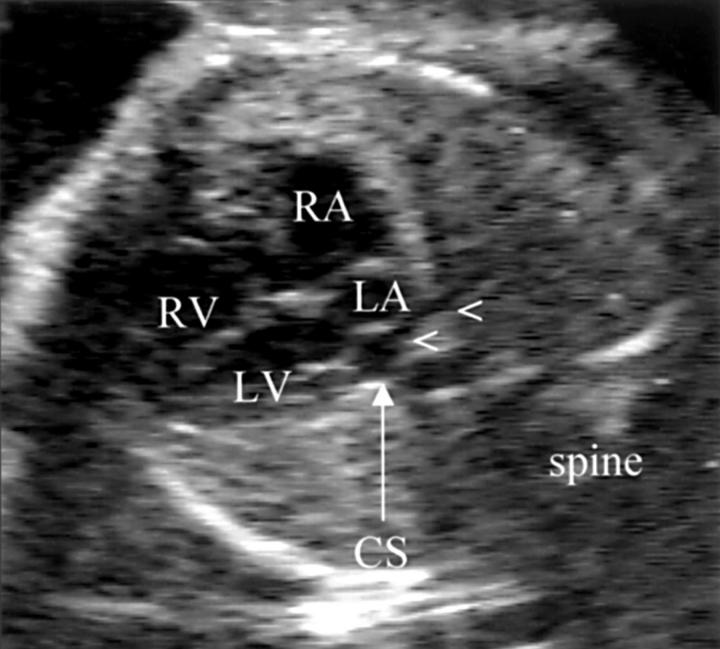
Figure 1 .
Case 1. On a four chamber view, the right atrium and ventricles appear dilated relative to the left sided structures. The pulmonary venous confluence (arrowheads) could be seen to drain to a dilated coronary sinus (CS). The pulmonary veins do not drain directly but appeared separated from the true left atrium by a membrane. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
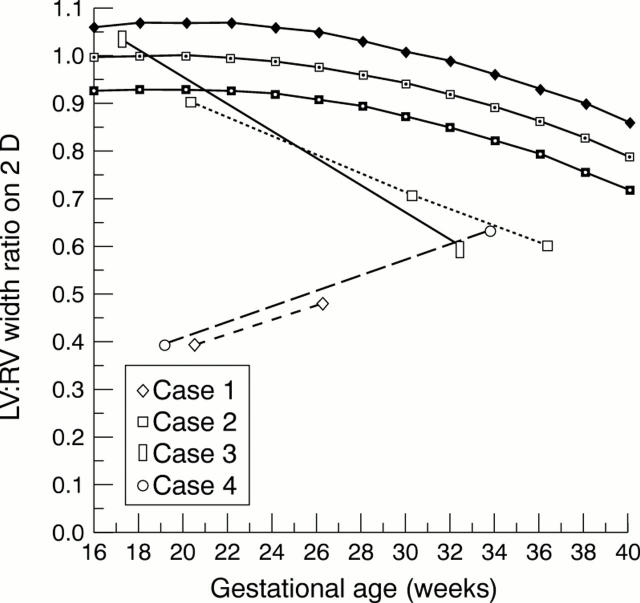
Figure 2 .
The ratio of the left ventricular to the right ventricular (LV:RV) cavity widths are shown in each case compared with the mean, 5th, and 95th centiles for normal hearts.
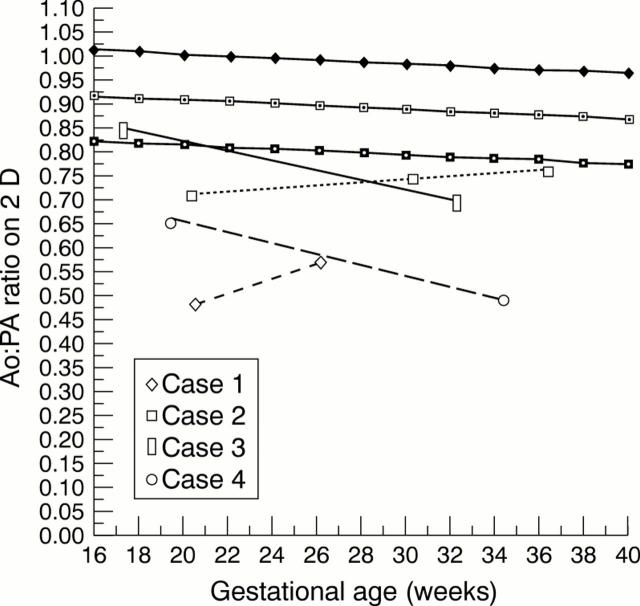
Figure 3 .
The ratio of the aorta to the pulmonary artery (Ao:PA) diameters are shown in each case compared with the mean, 5th, and 95th centiles for normal vessels.
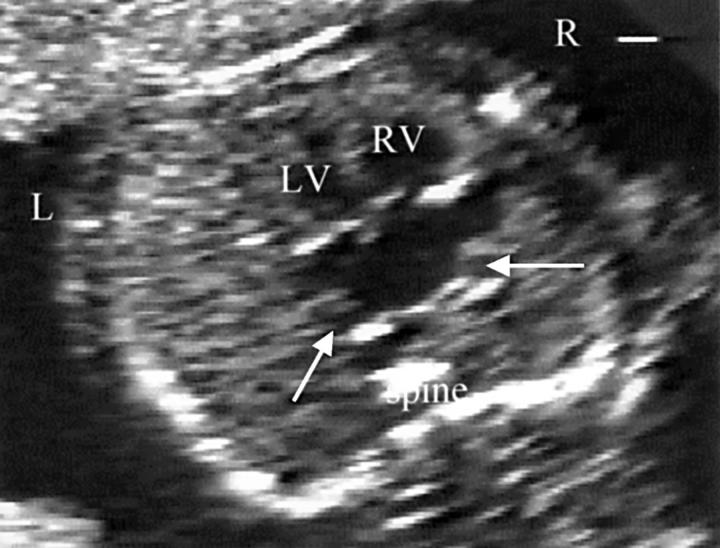
Figure 4 .
Case 2. The heart is unusually positioned in the thorax with the apex pointing almost directly anteriorly. There is a large secundum atrial septal defect. The ventricular chambers appeared equal at this gestational age of 20 weeks. The pulmonary veins on cross sectional imaging appear to drain normally. This emphasises the importance of colour flow mapping to confirm normal pulmonary venous drainage.
Figure 5 .
Case 3. This four chamber view showed normally proportioned ventricles and apparently normally connected pulmonary veins at the back of the left atrium at 18 weeks of gestation.
Figure 6 .
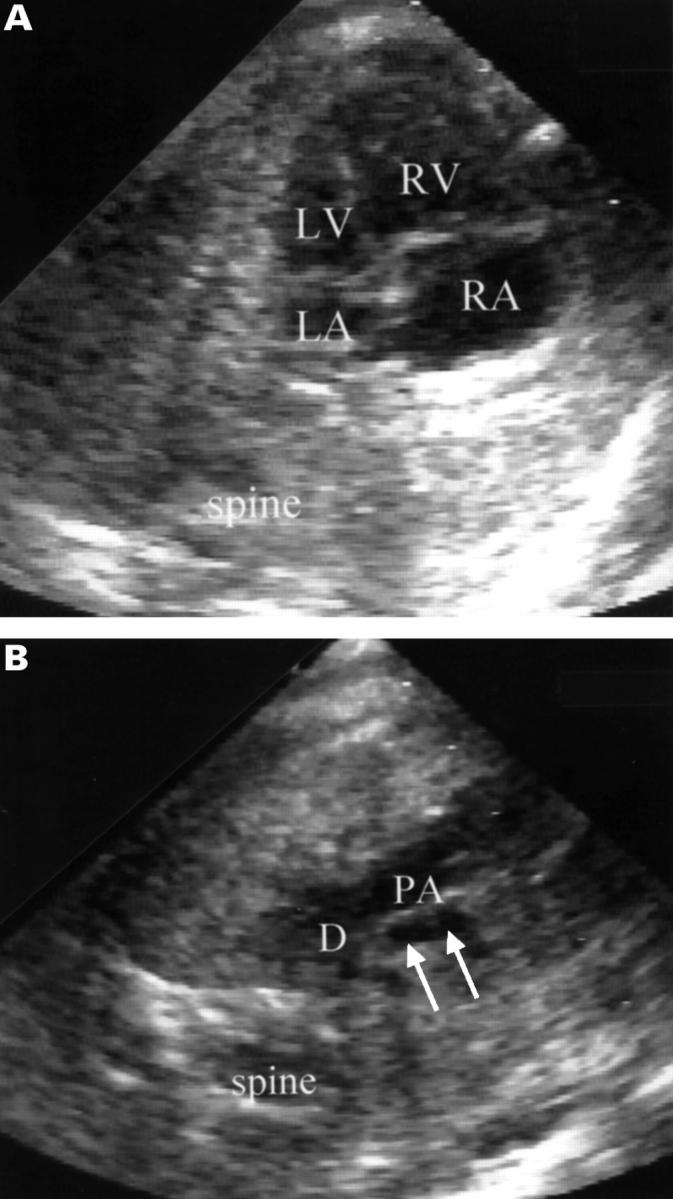
Case 4. (A) There is pronounced ventricular disproportion in this fetus with totally anomalous pulmonary venous drainage to the superior vena cava. (B) The family history of hypoplastic left heart syndrome, coupled with ventricular disproportion and the narrow transverse arch (arrows) compared with the duct (D), as shown here in a transverse view of the upper thorax, led us to suspect coarctation of the aorta. PA, pulmonary artery.
Figure 7 .
The heart is viewed in a four chamber projection. Colour flow mapping shows flow in both the left and right lower pulmonary veins (PVs) entering the left atrium in a normally connected fetal heart.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Better D. J., Kaufman S., Allan L. D. The normal pattern of pulmonary venous flow on pulsed Doppler examination of the human fetus. J Am Soc Echocardiogr. 1996 May-Jun;9(3):281–285. doi: 10.1016/s0894-7317(96)90141-8. [DOI] [PubMed] [Google Scholar]
- Bove E. L., de Leval M. R., Taylor J. F., Macartney F. J., Szarnicki R. J., Stark J. Infradiaphragmatic total anomalous pulmonary venous drainage: surgical treatment and long-term results. Ann Thorac Surg. 1981 Jun;31(6):544–550. doi: 10.1016/s0003-4975(10)61347-1. [DOI] [PubMed] [Google Scholar]
- Feller Printz B., Allan L. D. Abnormal pulmonary venous return diagnosed prenatally by pulsed Doppler flow imaging. Ultrasound Obstet Gynecol. 1997 May;9(5):347–349. doi: 10.1046/j.1469-0705.1997.09050347.x. [DOI] [PubMed] [Google Scholar]
- Lamb R. K., Qureshi S. A., Wilkinson J. L., Arnold R., West C. R., Hamilton D. I. Total anomalous pulmonary venous drainage. Seventeen-year surgical experience. J Thorac Cardiovasc Surg. 1988 Sep;96(3):368–375. [PubMed] [Google Scholar]
- Laudy J. A., Huisman T. W., de Ridder M. A., Wladimiroff J. W. Normal fetal pulmonary venous blood flow velocity. Ultrasound Obstet Gynecol. 1995 Oct;6(4):277–281. doi: 10.1046/j.1469-0705.1995.06040277.x. [DOI] [PubMed] [Google Scholar]
- Raisher B. D., Grant J. W., Martin T. C., Strauss A. W., Spray T. L. Complete repair of total anomalous pulmonary venous connection in infancy. J Thorac Cardiovasc Surg. 1992 Aug;104(2):443–448. [PubMed] [Google Scholar]
- Rasanen J., Wood D. C., Weiner S., Ludomirski A., Huhta J. C. Role of the pulmonary circulation in the distribution of human fetal cardiac output during the second half of pregnancy. Circulation. 1996 Sep 1;94(5):1068–1073. doi: 10.1161/01.cir.94.5.1068. [DOI] [PubMed] [Google Scholar]
- Sutton M. S., Groves A., MacNeill A., Sharland G., Allan L. Assessment of changes in blood flow through the lungs and foramen ovale in the normal human fetus with gestational age: a prospective Doppler echocardiographic study. Br Heart J. 1994 Mar;71(3):232–237. doi: 10.1136/hrt.71.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager S. B., Parness I. A., Spevak P. J., Hornberger L. K., Sanders S. P. Prenatal echocardiographic diagnosis of pulmonary and systemic venous anomalies. Am Heart J. 1994 Aug;128(2):397–405. doi: 10.1016/0002-8703(94)90494-4. [DOI] [PubMed] [Google Scholar]