Abstract
The results of surgical treatment of posterior tibial tendon insufficiency (PTTI) may be different at different stages of the disease. No single study has compared the results at different stages. This comparison can be helpful to the patient and physician if the patient asks “What if I wait and the disease progresses, how will my results be different?” A preliminary study comparing results for stage IIa, stage IIb (advanced stage II), and stage III was performed followed by a larger study comparing IIa and IIb with 26 and 22 patients, respectively. American Orthopaedic Foot and Ankle Society (AOFAS) outcome scores as well as radiographs and functional questions were used. Nearly all patients, regardless of stage, felt they were helped by surgical treatment. However, the lowest AOFAS score was in stage III, the most advanced stage investigated in this study. In comparing stage IIa and IIb patients, stage IIb patients had a statistically higher incidence of lateral discomfort. Although statistically significant differences were not found in all comparisons, this study suggests that the results of surgical treatment for PTTI declines with increasing stage or severity of disease.
Key words: posterior tibial tendon insufficiency, adult acquired flatfoot
Introduction
Posterior tibial tendon insufficiency (PTTI) or the adult acquired flatfoot often causes a progressive flatfoot deformity [1]. Early in the course of the disease, osteotomies can be successful as part of the surgical treatment [2], whereas late in the course, fusions in the hindfoot are commonly required. Patients who are considering waiting on surgical treatment can ask “What if I wait and am treated when my deformity has progressed, will my outcome be different, and how will it be different?” No study has directly compared the results of patients treated at different stages.
Staging for PTTI has been commonly done with stages I–IV [1]. Stage I includes patients with “no deformity” from PTTI, stage II flexible deformity, stage III fixed deformity, and stage IV deformity at the ankle as well as the foot. Stage II admittedly encompasses a large number of patients with a varying amounts and types of deformity. Stage II is therefore subdivided in this study. Stage IIa patients have minimal abduction deformity through the proximal midfoot as determined by clinical and radiographic examination. Stage IIb have significant abduction noted to be more than minimal on clinical examination and more than 30% uncovering of the talonavicular head on the standing anteroposterior (AP) x-ray of the foot. Stage IIa patients are treated for the heel valgus with a medial heel slide, and in stage IIb, patients can be treated with a variety procedures, one of which is lateral column lengthening to correct the abduction [1–3]. Although lateral column lengthening is a commonly used procedure, some surgeons do not use it and choose a medial slide with other procedures and/or fusions in the foot [4–6]. There is evidence that lateral column lengthening increases pressure on the plantar lateral side of the foot, particularly if it is done through calcaneocuboid joint [7]. Stage III patients have fixed deformity, which minimizes or eliminates passive inversion of the triple joint complex (talonavicular, calcaneocuboid, and subtalar joints). Stage III is corrected by a talonavicular arthrodesis, most often part of a triple arthrodesis. Admittedly, comparing the results of treatment between these different stages means that comparison is being made between patients who presented different amounts of deformity and had different treatments. However, direct comparisons between these different groups is likely to be useful to answer the question, “What if I wait and have to be treated for more deformity, will there be differences in my outcome and what will they be?” The hypothesis of this study is that there are significant differences in outcome between the different stages. Confirmation or lack of confirmation of the hypothesis can be useful to both patients and physicians.
A preliminary study was first undertaken in stage IIa, IIb, and III patients to determine if there were indications of different results in these groups. A second study was then done with a larger number of patients to determine if a larger study would detect differences between stage IIa and stage IIb outcomes.
Materials and methods
For the first study, 23 patients were retrospectively reviewed with a minimum of 5 consecutive patients in each subgroup to include stage IIa, IIb, and III patients (Table 1). A total of four groups were used, with the third of four groups to include a second method of treating stage IIb patients. The groups consisted of group 1 (stage IIa), treated with a medial slide calcaneal osteotomy, group 2 (stage IIb), treated with a medial heel slide and lateral column lengthening proximal to the calcaneocuboid joint, group 3 (stage IIb) treated with a medial heel slide and a lateral column lengthening done through the calcaneocuboid joint with an arthrodesis of that joint, and group 4 (stage III), which consisted of patients with fixed deformity treated with a triple arthrodesis [1, 2, 5]. Groups 1–3 all had a flexor digitorum longus transfer as well as the bony procedures. Although there is variation in how surgeons treat different stages, the treatments listed are commonly used procedures for these stages. All patients were reviewed at a minimum 2-year follow-up and were operated on by the same surgeon, but with the review performed by a different observer.
Table 1.
Stages with defining characteristics of each stage and treatments used in this study
| Stage | Characteristic | Bony procedure |
|---|---|---|
| IIa | Deformity with increased heel valgus but minimal abduction through midfoot | Medial heel slide |
| IIb | Deformity with increased heel valgus and greater than 30% talar head uncoverage | Medial heel slide and lateral column lengthening (group 2, proximal to CC joint; group 3, at the CC joint) |
| III | Fixed deformity with no significant inversion through the triple joint complex | Triple arthrodesis |
The second study expanded the number of patients in groups 1 and 2 to look for differences between these two groups. The goal was to detect differences not detectable in the smaller study. This study included 26 consecutive patients in group 1, and 22 in group 2.
The outcome assessment included physical exams, x-rays, the American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scale and an additional functional question [8]. Patients frequently ask, “Will I be able to get exercise on my operated foot?” This question was, therefore, included. Finally, all patients were asked if surgery improved their ability to walk and if given the choice again whether they would have surgery. Patients did their final assessment at a minimum 2 years after their index procedure (average follow-up, 39.7 months).
X-ray measurements were made from AP and lateral views on pre- and postoperative films. Measurements included the lateral talometatarsal angle, plantar medial cuneiform to plantar fifth metatarsal base distance, and on the AP view, the AP uncoverage angle [3].
In the second study, the same patients used in groups 1 and 2 were included with the addition of consecutive patients to increase the number of patients. In addition to the AOFAS outcome scores, questions were added regarding stiffness and lateral discomfort or pain. A visual analog scale (1–10) was used for stiffness, and patients were asked to answer “yes” or “no” to presence of lateral discomfort or pain. These questions were added because of concerns of stiffness or lateral discomfort after the lateral column lengthening procedure.
Results
All patients in the preliminary study felt surgery improved their pain significantly. All except one patient believed surgery improved their ability to walk and would repeat the surgery. The exception was a patient from group 3 who had lateral pain pre- and postoperatively. Although the pain was improved, it was not improved adequately by the surgery.
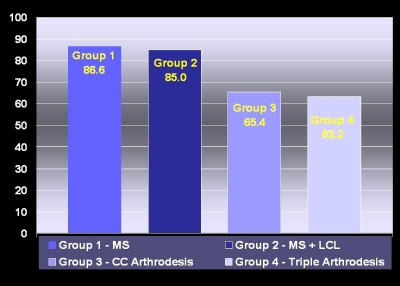
The results for the AOFAS hindfoot score in the preliminary study was 86.6 and 85.0 for the groups 1 and 2 (stages IIa and IIb), respectively, and 65.4 for group 3 (stage IIb) and 63.2 for group 4 (stage III) (Fig. 1). Preoperatively, these scores were 56 and 53 for groups 1 and 2 and 54 and 50 for groups 3 and 4. Despite large differences in AOFAS scores, there were not significant differences among the four groups in the small study. However, if group 4 (stage III) was compared to group 1 and group 2, there was a significantly inferior score (p < .05). If analysis was done grouping osteotomy procedures (groups 1 and 2) together and arthrodesis procedures (groups 3 and 4) together, there was a statistical difference between the osteotomy and arthrodesis groups.
Fig. 1.
AOFAS outcome scores for groups 1–4. Note the lower scores in stage III (group 4) and stage IIb (group 3), which was treated with a calcaneocuboid lengthening arthrodesis
The x-ray measurements showed statistically significant (p < .05) correction between the pre- and postoperative values for all four of the procedures. This was true for each one of the x-ray measurements. Differences between the groups for the amount of correction were not significantly different.
For the question of the ability to get enough exercise, only 1 patient in the 12 patients (14%) in groups 1 and 2 was not able to get enough exercise in comparison to 6 of 11 (55%) not able to get enough exercise in groups 3 and 4.
There were two complications in the preliminary study. The one dissatisfied patient mentioned above was in group 3 and had a non-union of the fusion. The patient was reoperated on with compression staples and went on to heal. One patient in group 2 had a delayed union with infection. This patient was treated with antibiotics and debridement and went on with an excellent functional result (no pain, no limitations with walking or the ability to get enough exercise).
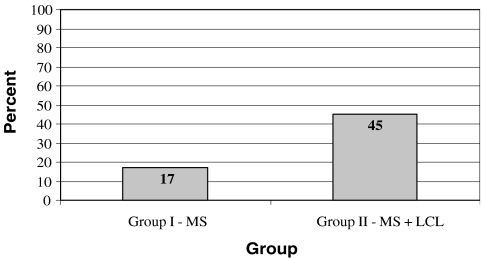
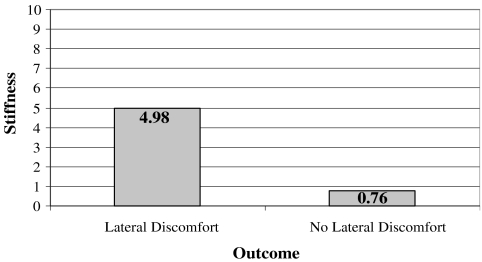
The results from the second study showed that the AOFAS hindfoot scale was 90.8 for the expanded group 1 and 84.7 for the expanded group 2, again no statistical difference. Statistical difference was found for lateral discomfort with 10 (45%) of 22 with lateral discomfort in group 2 vs 4 (17%) of 23 in group 1 (Fig. 2). No difference was found for stiffness, with 3.0 in group 1 vs 2.9 in group 2 (Fig. 3). However, if patients in group 2 with lateral discomfort were compared with those without lateral discomfort, there is a statistical difference, with average 4.98 stiffness with lateral discomfort patients vs 0.76 for those in group 2 without lateral discomfort (Fig. 4).
Fig. 2.
Percentage of patients with lateral discomfort in group 1 (stage IIa, treated with a medial slide osteotomy) vs group 2 (stage IIb, treated with a medial slide and lateral column lengthening)
Fig. 3.
Stiffness in Group 1 (MS) vs all Group 2 (MS and LCL) patients
Fig. 4.
Stiffness results comparing lateral column lengthening in patients who had lateral discomfort and those who did not
There were two complications in the second study in addition to those noted in the preliminary study. Two patients were revised to decrease the amount of lateral column lengthening because of the complaints of lateral weight bearing and stiffness. Revision improved these complaints in both patients satisfactorily.
Discussion
In the preliminary study, the lowest AOFAS score was 63.2, the score for group 4 (stage III treated with triple arthrodesis). These patients admittedly require arthrodesis because of fixed deformity. With the significant loss of motion pre- and postoperatively, it is not surprising that they have lower scores than stage II patients who were treated with procedures that preserve more motion. The number of patients is small, so the results should be considered indicative rather than definitive. It is, however, consistent with most of the literature. In the largest study of triple-arthrodesis patients, patients who had had a triple arthrodesis had a postoperative AOFAS score of 60.7, similar to the results in the preliminary study of 63.2 [9]. Despite the low outcome score, the patients, as in the present study, had a high satisfaction rate and felt that surgery increased their function.
The other low AOFAS score in the preliminary study was 65.4 in group 3 (stage IIb treated with calcaneocuboid arthrodesis). Like group 4, it was not statistically different from the other three groups. However, if group 4 was eliminated from the analysis, then group 3 was statistically different from groups 1 and 2. This trend to a lower score with the stage being the same for groups 2 and 3 suggest that it was the type of procedure (an arthrodesis of CC joint) that may have made for the poorer results. Indeed this procedure, a lengthening CC fusion, has become less frequently mentioned in the literature, possibly because of inferior results and difficulty in achieving union [6, 10].
The highest scores were in groups 1 and 2, which were the lowest stages and treated with osteotomies, not fusions. However, these two groups were different in their staging (stage IIa and IIb). There was no indication of differences in their results in the preliminary study with AOFAS scores of 86.6 and 85.0, respectively. However, there have been concerns of lateral discomfort or pain and stiffness after lateral column lengthening procedures such as used in group 2 [6, 9–11]. A second study with a larger number of patients was therefore done to compare groups 1 and 2.
In the second study, the AOFAS scores between groups 1 and 2 remained high (90.8 and 84.7, respectively). There was no statistically significant difference between these AOFAS scores. However, when asked about lateral discomfort, there was a statistical difference, with group 2 having a higher incidence of lateral discomfort (45%) in comparison to group 1 (17%) (Fig. 2). Two patients who were revised for lateral discomfort were included in the lateral discomfort group, although revision surgery resolved their discomfort. It should be noted that the other patients who had lateral discomfort did not feel the discomfort was disabling and were satisfied with their procedure. Although this discomfort was in most cases not disabling, it would be best to minimize its frequency. What is the origin of the lateral discomfort in these patients? Although this study cannot definitively answer this question, it does provide an indication. It does not point to the arthritis in the CC joint, originally thought to be a potential problem [12, 13]. These patients did not, by x-ray, have CC joint degenerative changes and did not point to the CC joint as the source of their discomfort. Instead, they commonly pointed to the plantar lateral border of their foot. This is consistent with the biomechanical study of plantar foot pressure after lateral column lengthening [7]. As stated in the results, patients with lateral discomfort had the highest incident of stiffness (4.98) in comparison to others in group 2 (0.76) (Fig. 4). This suggests that in these patients with lateral discomfort, the lateral column lengthening had resulted in more stiffness. This stiffness (with less eversion) could in turn lead to more lateral weight bearing. A goal for the future would be to treat stage IIb patients with a lower incidence of postoperative stiffness and lateral discomfort. This could be done by determining how to minimize stiffness with a lateral column lengthening or use other procedures which minimize stiffness yet still give adequate correction.
In summary, this study does indicate that there are differences in the results of treatment of PTTI by different stages of I, IIa, IIb, and III. Admittedly, these stages are treated with different procedures. The different procedures themselves can be contributing to the different results, as noted in the results of treatment in groups 2 and 3. For the treatments reviewed, this study suggests that patients who are treated at stage IIa are likely to have the best results. Improvement of results in the future will be to treat patients before procedures that stiffen the hindfoot are necessary and minimize the incidence of stiffness if lateral column lengthening or other procedures are to be used.
References
- 1.Myerson, MS (1996) Adult acquired flatfoot deformity. J Bone Jt Surg 78A (5):780–792.
- 2.Pomeroy GC, Pike RH, Beals TC, Manoli A (1999) Acquired flatfoot in adults. J Bone Jt Surg 81A:1173–1182. [DOI] [PubMed]
- 3.Sangeorzan BJ, Mosca V, Hansen ST, Jr (1993) Effect of calcaneal lengthening on relationships among the hindfoot, midfoot and forefoot. Foot Ankle Int 14:136–141. [DOI] [PubMed]
- 4.Hiller L, Pinney S (2003) Surgical treatment of acquired adult flatfoot deformity: what is the state of practice among academic foot and ankle surgeons in 2002? Foot Ankle Int 24:701–705. [DOI] [PubMed]
- 5.Graves SC, Stephenson K (1997) The use of subtalar and triple arthrodesis in the treatment of posterior tibial tendon dysfunction. Foot Ankle Clin 2:319–328.
- 6.Mann RA, Beamon DN, Horton GA (1998) Isolated subtalar arthrodesis. Foot Ankle Int 19:511–519. [DOI] [PubMed]
- 7.Thomas RL, Wells BC, Garrison RL, Prada SA (2001) Preliminary results comparing two methods of lateral column lengthening. Foot Ankle Int 22:107–119. [DOI] [PubMed]
- 8.Kitaoka HB, Alexander IJ, Adeloor RS, Nunley JA, Meyerson MS, Sanders M (1994) Clinical rating symptoms for the ankle–hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int 15:349–353. [DOI] [PubMed]
- 9.Pell RF, Myerson Ms, Schon LC (2000) Clinical outcome after primary triple arthrodesis. J Bone Jt Surg 82A:47–57. [DOI] [PubMed]
- 10.Tien TR, Parks BG, Guyton GP (2005) Plantar pressures in the forefoot after lateral column lengthening: a cadaveric study comparing the Evans osteotomy and a calcaneocuboid fusion. Foot Ankle Int 26:520–525. [DOI] [PubMed]
- 11.Pinney SJ, Lin SS (2006) Current concept review: acquired adult flatfoot deformity. Foot Ankle Int 27:66–75 [DOI] [PubMed]
- 12.Mosair-LaClair S, Pomeroy G, Manoli A (2001) Intermediate follow-up on the double osteotomy and tendon transfer procedure for state II posterior tibial tendon insufficiency. Foot Ankle Int 22:283–291. [DOI] [PubMed]
- 13.Pomeroy GC, Manoli A, II (1997) A new operative approach for flatfoot secondary to posterior tibial tendon insufficiency: a preliminary report. Foot Ankle Int 18:206–212. [DOI] [PubMed]