Abstract
Distal radius fractures are one of the most common types of fractures, accounting for around 25% of fractures in the pediatric population and up to 18% of all fractures in the elderly age group. Although the pediatric and elderly populations are at the greatest risk for this injury, distal radius fractures still have a significant impact on the health and well-being of young adults. Data from the past 40 years has documented a trend towards an overall increase in the prevalence of this injury. For the pediatric population, this increase can likely be attributed to a surge in sports related activities. The growth of the elderly population and a rise in the number of active elderly are directly responsible for the increase seen in this age group. Understanding the epidemiology of this fracture is an important step towards the improvement of the treatment strategies and preventative measures which target this debilitating injury.
Keywords: distal radius fracture, epidemiology, incidence, fragility fracture
Introduction
Distal radius fractures are one of the most common types of fractures, with over 640,000 cases reported during 2001 in the US alone.1 For reasons not fully understood, and likely multi-factorial, the incidence of this fracture appears to be on the rise in the US and abroad.2–5 Many of the societal effects of these fractures extend beyond the significant medical costs, including decreased school attendance, lost work hours, loss of independence and lasting disability. Fragmented care and coding discrepancies can make accounting for the true number of these fractures difficult, likely underestimating the rates typically quoted in the literature. When analyzing the incidence of distal radius fractures, there are three major populations to consider: children and adolescents, young adults, and the elderly. The pediatric and elderly populations are both considered at high risk for this injury, and the contributing factors will be examined in this paper. In addition to the 3 main age groups, gender and ethnicity may also be considered distinct risk factors within each of these populations. Understanding the epidemiology of distal radius fractures can help physicians choose the most appropriate treatment options for the fracture, as well as effectively target preventative measures towards at-risk populations.
Population Incidence
Overall
Chung and Spilson used data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) database and determined that 1.5% of all emergency department visits were due to hand and wrist fractures. Radius and ulna fractures consisted of 44% of these fractures.1 This study corresponds to a study by Larsen and Lauritsen showing that distal radius fractures accounted for 2.5% of all emergency department visits.6 These numbers vary more widely in earlier reports, but still represent a high incidence rate. In 1962, an analysis of fractures in Sweden documented the number of distal radius and ulna fractures to be as high 75% of all forearm fractures.7 A study by Knowelden et al. in 1964 found 32% of all fractures seen in women over the age of 35 in the distal end of the radius.8
Trends of increasing incidence
Current and past clinical data point to a rise in the incidence of distal radius fractures for the pediatric, adult, and elderly populations in recent years. This phenomenon has been a subject of debate as early as the 1960’s when Alffram and Bauer published their report on the increasing occurrence of distal radius fractures in a large Swedish city.7 A study from Rochester, Minnesota found a 17% increase in the incidence of this injury over a 40 year period.2 The incidence in Sweden almost doubled for the elderly population over a 30 year time span when compared to previous data from the same location. During the same study period as this increase, the incidence rates of shaft fractures of the radius and ulna remained the same, lending further validity to the increase in distal radius fractures as a legitimate trend.9 Although there is no single factor responsible for this phenomenon due to the absolute prevalence of distal radius fractures, any individual contributing factor is bound to have confounding variables.
Many theories have been proposed to determine the source of the increasing rates of distal radius fractures, but studies correlating a specific cause to the incidence of this injury must be carefully evaluated. The influence of lifestyle and environmental factors on the risk and incidence of distal radius fractures has recently been assessed to further examine the causes for the increasing rates. One study found a 30% greater risk for a distal radius fracture in urban women over rural women.10 Although the data indicated a significant difference between risk factors, it could not seem to determine the cause of this discrepancy, even after analyzing lifestyle and health factors. Others point to the impact of epigenetic influences on the development of diseases such as childhood obesity and osteoporosis as a basis for the increasing incidence of this fracture in different populations.11,12 It is possible that changing cultural dietary habits may be altering bone metabolism, affecting the overall incidence of distal radius fractures. Additionally, as the population ages and individuals strive to remain active, fractures due to relatively minor traumas have increased.7 Other theories will be discussed in further detail throughout the following sections.
Costs
As the incidence of distal radius fractures rises, the short and long term costs become apparent. Each year, fractures account for over half of the days patients spend in the hospital receiving treatment and care for upper extremity injuries.1,13 The costs of treating distal radius fractures in the pediatric population of the United States has been cited to be in upwards of $2 Billion per year.12 This is not surprising considering the overall prevalence of this injury. Chung et al. recently evaluated the costs that accompany this injury with respect to the elderly community. They found in 2007, Medicare paid $170 million in distal radius fracture related payments.14 Additionally, they projected that the future burden of Medicare could be $240 million if the current trend in the use of internal fixation continues. These costs did not include any secondary expenses associated with this injury such as prescription drugs, lost time at work, and loss of independence, which may be more significant than the direct costs. This data reveals the significant socioeconomic costs incurred as a direct result of distal radius fractures, and highlights the importance of analyzing preventative measures and treatment protocols for individuals who are at a high risk for or suffer from this injury.
Pediatric Incidence
Children and adolescents are at a particularly high risk for distal radius fractures, in part due to a rapidly developing skeletal structure. Studies have documented that up to 25% of fractures in children involve the distal end of the radius.15–18 A study by Landin estimated that until the age of 16, the risk of getting a fracture is 42% in boys and 27% in girls.15 In this analysis, fractures of the distal forearm accounted for approximately 21% of all fractures in the pediatric population. The indirect costs of this injury are incalculable in terms of medical costs, lost time from school, and even future work potential.
Increasing overall incidence
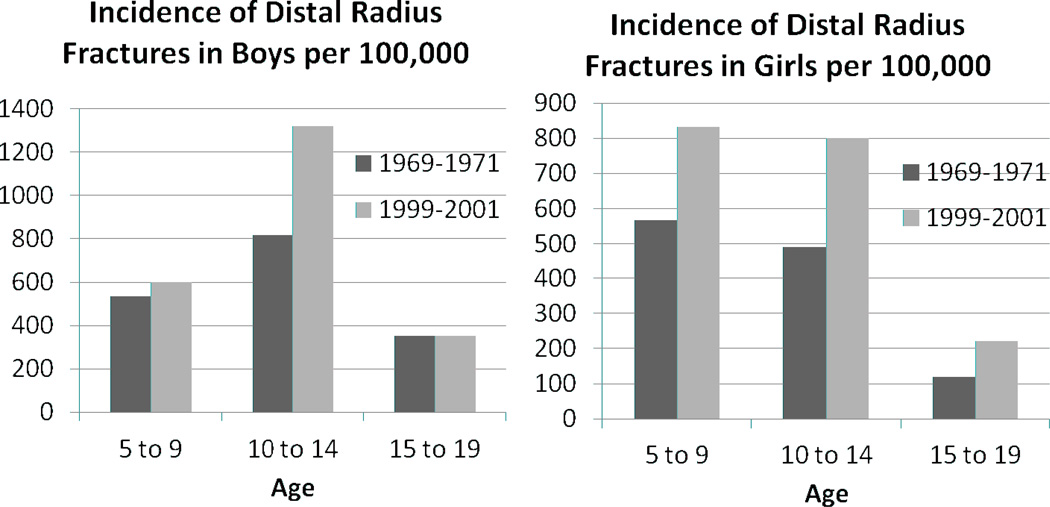
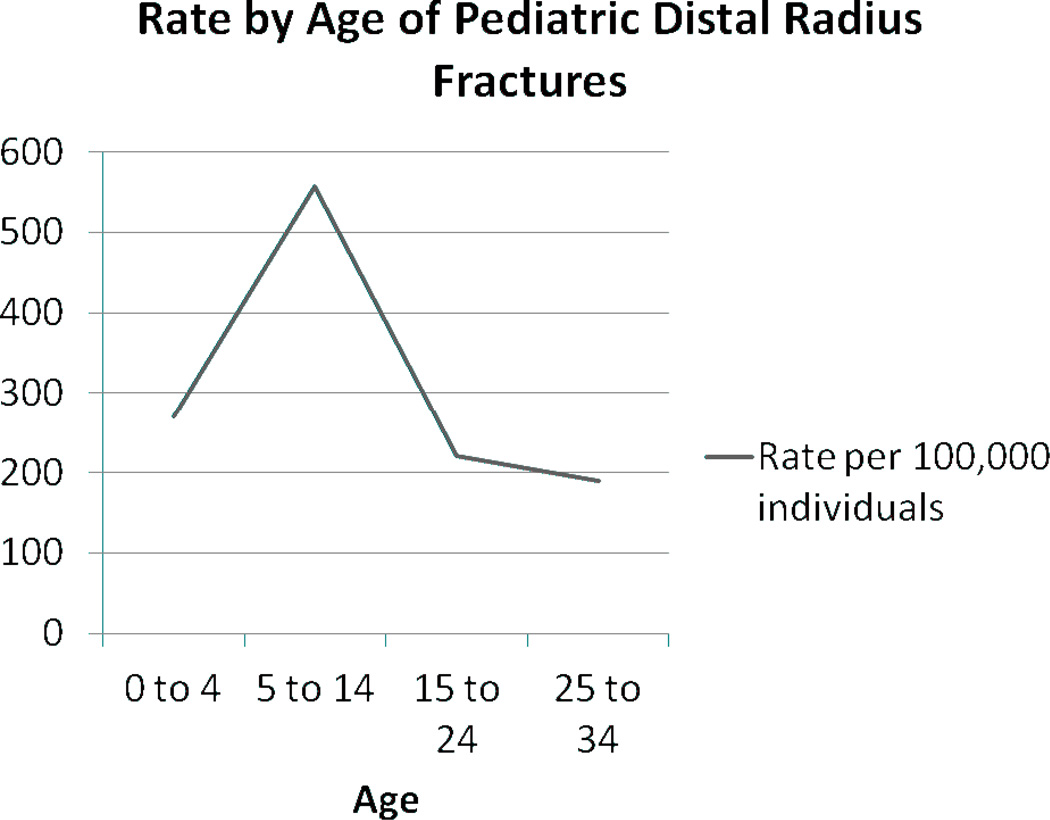
The incidence of distal radius fractures in children appears to be rising, but it is difficult to explain the exact cause of this steady increase over the past 40 years (Figure 1).3,19,20 Some studies suggest this could be the result of an overall increase in the participation of sports related activities in the pediatric population.3,12,19,21 Putter et al found an increase in sports related activities correlated with an increase in sports-related distal radius fractures (Figure 2). In another study, 23% of all sports fractures occurred in the distal part of the radius.22 However, Mathison and Agrawal attest that this increase may be due to an improved access to care and better detection of fractures.21
Figure 1.
The increasing incidence of distal radius fractures in boys and girls under the age of 20. The rise in incidence was statistically significant for both boys and girls.
Data from Khosla et al., Incidence of Childhood Distal Forearm Fractures Over 30 Years. Ref. 20
Figure 2.
A strong increase in the incidence of sports related fractures was found in the pediatric population, which may account for the rise in the overall incidence rates of distal radius fractures.
Data from Putter et al., Trends in Wrist Fractures in Children and Adolescents, 1997–2009. Ref. 3
Age and Bone Biology
Studies have revealed the average fracture incidence related to age to be higher in boys than in girls.12,15 In the 1960’s, the peak rate of fractures of the distal radius was found to occur during the start of puberty, between the ages of 10 to 14.7 A study in 1989 found the peak age to be specifically between 11.5–12.5 years old for girls and 13.5–14.5 years old for boys,23 while more recent data suggests that for girls the peak age is anywhere from 8–11 and for boys from 11–14.19 Using current data from the NHAMCS, Chung and Spilson recently documented this peak for the pediatric population, and noted a similar trend (Figure 3). After this peak rate of occurrence, the frequency of distal radius fractures consequently lowers, and is then only exceeded by the incidence rates in women 50 years of age and older.23 Although it might seem logical to attribute the causes of this peak rate during puberty to an increase in physical activity, it is known that activity levels tend to decrease as children progress through puberty.24 Rather, the peak rate of fractures appears to be closely correlated to the bone mineral density and bone mineral content of the distal radius during the pubescent growth spurt.
Figure 3.
This shows the combined peak rate of fractures of both boys and girls to be around 10 years old, corresponding to peak rates documented in other studies.
Data from Chung and Spilson, The Frequency and Epidemiology of Hand and Forearm Fractures in the United States. Ref. 1
Studies have confirmed a large dissociation between skeletal growth and mineralization during puberty, which may account for the increased fragility of bones seen during this stage of development.23,25–28 In an early study on the subject, Krabbe et al. found that during the pubescent growth spurt, children experience large, sudden advances in linear development, or bone lengthening, concurrent with very small increases in bone mineral content.25 The process of bone mineralization cannot keep up with the abrupt increase in new bone development, resulting in bones that are particularly susceptible to fracture. After puberty, linear development begins to slow, and bone mineral content begins to increase rapidly, creating stronger bones that are more resistant to trauma. Ryan et al. found a statistically significant higher proportion of injuries due to minor trauma in the 10–14 age group when compared to the 5–9 age group.12 This may suggest that a weakened skeletal structure due to low rates of bone mineralization during the adolescent growth spurt leaves even a minor trauma with the potential to cause a distal radius fracture.
Additionally, some suggest there may be a brief period of increased cortical porosity during the adolescent growth spurt to allow for efficient absorption of calcium required by the bones during this rapid stage of growth.29 Prior to mineralization, the increased bone porosity may contribute to the peak rate of distal radius fractures seen during this period of rapid physiological development.
Gender and Ethnicity
The incidence rate of distal radius fractures is known to be higher in boys than in girls. A study by Ryan et al. demonstrated a statistically significant difference between the incidence rates of boys and girls, with 64% of all fractures occurring in boys.12 Other studies have shown similar results.3,15,20,23 There is no evidence suggesting significant ethnic differences in the rates of pediatric distal radius fractures. One large study found no significant difference in the rate between urban and rural pediatric populations.19
Mechanism of Injury
The mechanism of injury in distal radius fractures in the pediatric population has been well documented. The main types of activities causing distal radius fractures in children are sports, car accidents, and playing. Khosla et al. found that from 1999 to 2001, 10% of all pediatric distal radius fractures in Olmsted County occurred while children were using playground equipment.19 Data from Ryan et al. documented 30% of distal radius fractures resulting from sports related injuries in the 10–14 age group, while sports were responsible for 47% of these fractures in the 15–17 age group. The most common mechanism of injury was fall related, with studies showing around 80% of injuries occurring in this fashion.12,30
Young Adult Incidence
The incidence of distal radius fractures in the adult population is significantly lower than in other age groups.31 As a result of this lower incidence, and the apparent random occurrence of fractures in this low risk group, little data is available on this population regarding the epidemiology of this injury. However, even at a low rate, the complications following this injury can result in lasting disability in previously young, healthy individuals. Although infrequent, these fractures are still the most common injury in the young adult population.32 Sports and car accidents are known to be one of the most common causes of distal radius fractures in young adults.
Gender and Ethnic differences
Research has shown that white women have higher rates of distal radius fractures in individuals above the age of 65, a trend not apparent in younger adults.33,34 Brogren et al. found that in the age group of 19–49, men and women had almost identical incidence rates. However, when looking at the age group from 19–65, women had almost double the rate when compared to men, likely owing to the onset of osteoporosis in women over 50 years old.31 A study by Chung and Spilson found that Caucasians represented 83% of all fractures but also had the largest proportion of emergency department visits.1 If other ethnic minorities are less likely to present themselves to the emergency room after an injury than Caucasians, this may account for the discrepancy in the published rates of ethnic differences in distal forearm fractures.
Elderly Incidence
Distal radius fractures account for up to 18% of all fractures in the over-65 age group.35 Numerous factors contribute to this risk, including architectural changes in the bone, increased activity levels, and metabolic bone disease. This fracture will prove to be a strain to the medical system over the next several decades due to the explosive growth of the elderly population.14
Most fractures occurring in the elderly are the result of trauma due to a low energy force, with a fall from a standing height the leading cause of injury.36,37 Many of the accidents causing these low energy fractures occur as an individual tries to stop a fall with a dorsally outstretched hand. Evidence has also shown that distal radius fractures seem to occur more often in cognitively intact individuals as opposed to those with significant dementia. Women with good neuromuscular control and faster walking speeds were found to be at higher risk for distal radius fracture, as they tend to “reach-out” to break a fall, rather than fall onto the side of their arm or leg, which would result in a proximal humerus or hip fracture.13,38
Age and Gender
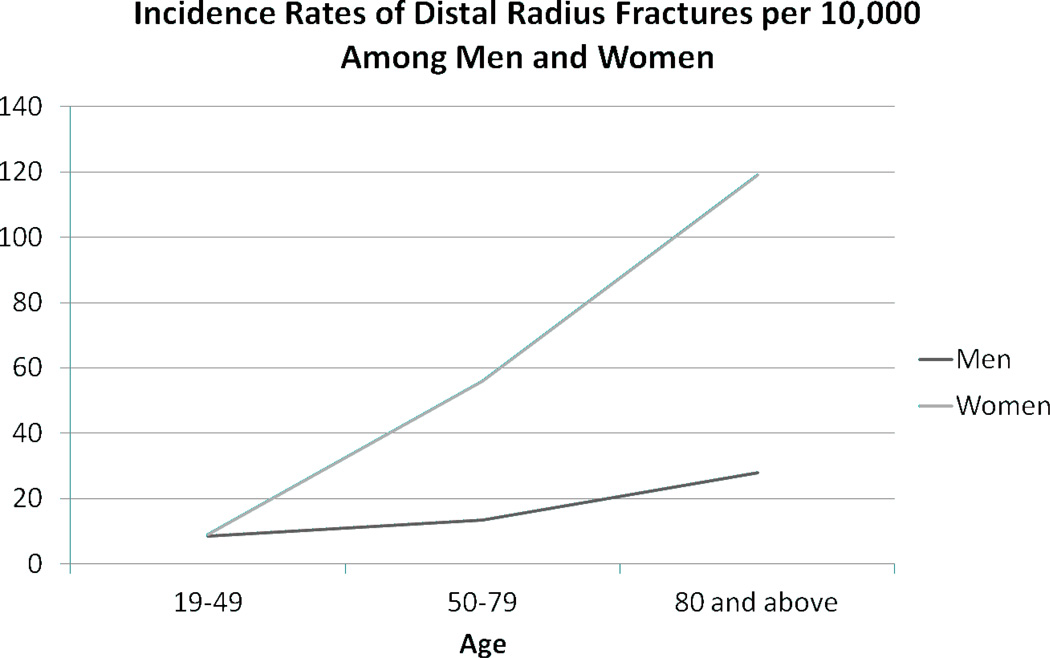
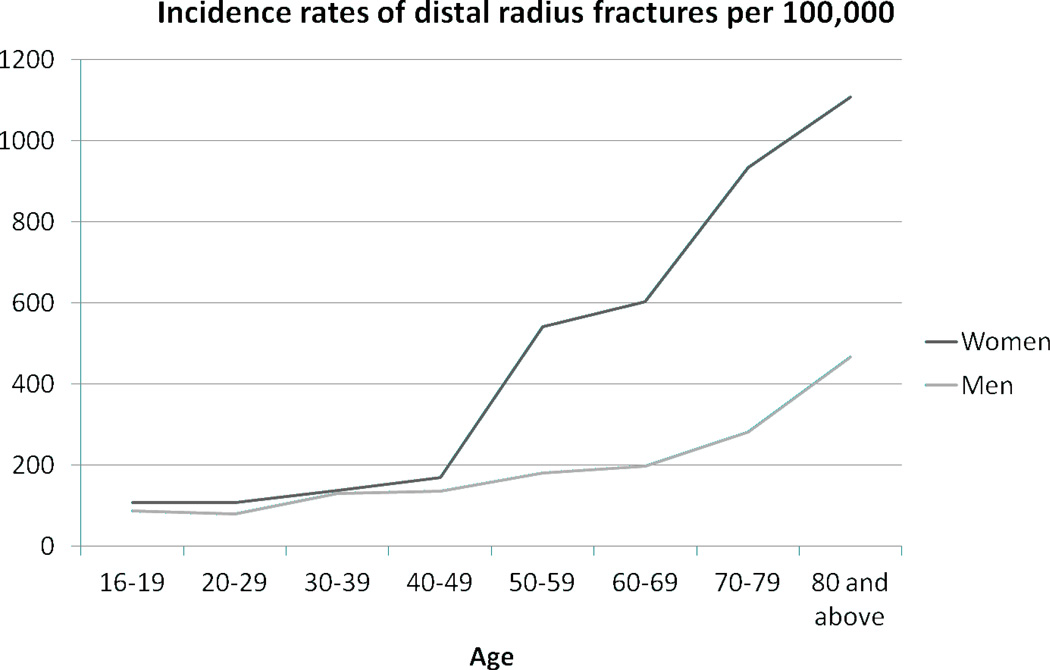
Age and gender have a pronounced effect on the incidence rates of distal radius fractures in the elderly community. Women are known to have a significantly greater risk of this injury than men in this age group, as compared to the opposite trend found in the pediatric population. Baron et al. found that one of the largest gender discrepancies occurred in the distal forearm, when looking at fracture rates in the over 65 age group.35 According to the data, the women in this study were approximately 4.88 times more likely than men to obtain a distal forearm fracture. This is in direct contrast to rate ratios in other regions of the upper extremity, where women had a risk factor of around only 3 times that of men. Brogren et al. also documented comparable differences between elderly men and women, finding women had a higher overall incidence, with almost 5 times more fractures in women than in men.31 They noted that the incidence for women increased rapidly from 50 years of age and older, almost doubling every 10 years until 90 years of age (Figure 4). The incidence in men remained low until 80 years of age, but despite this increase, still remained significantly lower than the rates seen in women. Flinkkila et al. took a closer look at this trend, breaking the age groups into 5 year increments, and found a similar trend (Figure 5).
Figure 4.
Incidence rate of distal radius fractures per 10,000 people in men and women aged 19 to 80. The increasing incidence was statistically significant when comparing the three age groups in both men and women.
Data from Brogren et al., Incidence and Characteristics of Distal Radius Fractures in a Southern Swedish Region. Ref. 32
Figure 5.
Incidence rate of distal radius fractures per 100,000 people in men and women aged 16 to 80. A statistically significant difference was documented between the overall incidence of men and women, with women having a higher rate of fracture.
Data from Flinkkila et al., Epidemiology and Seasonal Variation of Distal Radius Fractures in Oulu, Finland. Ref. 37
Osteoporosis
Osteoporosis and osteopenia are common degenerative bone diseases that plague the elderly population. They are caused by a reduced capacity to build and remodel bone. The World Health Organization defines osteoporosis as an individual with a bone mineral density −2.5 standard deviations or less than that of a matched adult, whereas osteopenia falls between osteoporosis and normal bone density for age matched controls.39 Low bone mineral density has been well documented in elderly women who suffer a distal radius fracture.40–45 A recent study by Øyen et al. found that decreased bone mineral density was a better predictor of the risk of distal radius fractures in women than in men, but a significant predictor in both men and women once osteoporosis was diagnosed.43
Clayton et al. recently documented the relationship between osteoporosis and the severity of distal radius fractures.46 This study indicated that less bone mineral density was correlated with more severe, intra-articular fractures. It also revealed that a decrease in bone mineral density is related to an increase in the probability of early instability after closed reduction, with a 66% chance in the osteoporosis group compared to only a 48% chance in the normal group. Additionally, they found that the probability of late carpal malalignment was 35% in the osteoporosis group but only 25% in the normal group.
Pediatric Outcomes
Age
In skeletally immature individuals, anatomic reduction of distal radius fractures is usually not required due to the potential for growth and remodeling, and operative intervention is seldom warranted. This fracture is rarely intra-articular, allowing for initial imperfect reductions to be well-tolerated. It is accepted that distal fractures have a more favorable prognosis than those in a more proximal aspect of an extremity. Observational studies indicate displacement of very distal fractures in patients of all ages is better tolerated than more proximal malunions in even very young children.47,48
Based on long-term functional outcomes of malunions in pediatric forearm fractures, Noonan et al. made a series of recommendations for reduction in pediatric patients presenting with this injury. For patients less than 9 years old, reduction could be accepted with complete displacement (bayonet apposition) and up to 1cm of shortening, 15 degrees of angulation, and 45 degrees of malrotation, without resulting in functional deficits. In children 9 years of age and older, 30 degrees of malrotation is acceptable, with 10 degrees of angulation for proximal fractures and 15 degrees for more distal fractures.49 Complete bayonet apposition is acceptable, especially for distal radius fractures, as long as angulation does not exceed 20 degrees and 2 years of growth remains.49
Complications
It is important to note that children with distal radius fractures have particularly low rates of complications,3,50 often attaining superior outcomes with casting alone. This results from the fact that the developing bone in children has a remarkable ability to remodel itself back into the correct anatomic orientation after trauma, even an injury as severe as a fracture. A recent study showed that only 17 out of 305 distal radius fractures in children had a complication.50 The tendency of surgeons to strive for perfect anatomic reduction in patients with distal radius fractures has caused debate over the appropriate treatment protocol for children with these injuries. A study by Do et al. compared the functional outcomes of children with distal radius fractures who underwent closed reduction and those who had only splint stabilization.51 The 34 children who had no attempted reduction had the same functional results at their follow-up visits as the 34 children who underwent reduction. In addition, they found the total cost for patients with attempted reduction to be 50% more than those without reduction, even though both groups achieved the same functional outcomes with no complications at their follow-up visits. A more recent study by Al-Ansari et al. showed that 0 out of 124 children with minimally angulated distal radius fractures required surgical intervention or manipulation of any type before a cast was applied.30
On occasion, pediatric distal radius fractures are accompanied by distal ulna fractures. Most studies to date have not separated outcomes from isolated distal radius fractures from those that include a distal ulna fracture (complete or incomplete).47 Synostosis is a rare but difficult to treat complication in this type of injury. Those most at risk are individuals with high energy trauma or those with a concomitant head injury.52 Re-fracture at the same site following a distal radius fracture is not infrequent if the immobilization is removed too early and the child returns to activities before the lamellar bone has fully remodeled. Outcomes following re-fracture have been documented as having worse clinical outcomes than fractures that have healed primarily.47,53 Specifically for girls with low bone mass density (BMD) and a previous distal forearm fracture, the risk of another distal radius fracture was shown to be 4 times greater than controls, since bone mineral deposition lags behind increases in body weight and bone length.54
Young Adult Outcomes
Once patients have reached skeletal maturity, most extra-articular distal radius fractures have good long-term functional results with conservative treatment if initially reduced to restore anatomic height and inclination. In a 30-year follow-up study of young adults in Sweden with distal radius fractures, they found that of the 28% of study participants who had extra-articular fractures (average age of 31 at time of fracture, range 18–40), only 37% had even minor complaints of pain, decreased mobility, or cosmetic deformity.55
It is difficult to obtain satisfactory results with intra-articular distal radius fractures in young adults. This is due to the development of symptomatic post-traumatic arthritis if treated non-operatively, with rates reported as high as 40%.55–57 In Knirk and Jupiter’s 1986 study of intra-articular fractures in young adults (average age at fracture of 28 years) treated either with cast immobilization or pins and plaster, they saw radiographic evidence of arthritis in 65% of patients at 7 years follow-up. Ninety-three percent of those with radiographic arthritis were symptomatic, which they asserted were most commonly the result of a malreduced die-punch fragment.58 Catalano et al studied 21 patients younger than the age of 45 years who had undergone internal fixation of displaced intra-articular fractures. At an average of 7 years, osteoarthrosis of the radiocarpal joint was radiographically apparent in 76% of wrists.59
The ability of young adults to return to work following a distal radius fracture may be one of the most objective parameters by which to assess the epidemiologic impact of these injuries on this population. In Knirk’s paper, only one of the 40 patients was unable to return to their prior occupation due to the residual effects of their distal radius fracture.60 In Catalano’s study, only 1 of 21 patients was unable to continue her current profession as a nurse.59 Although rates of post-traumatic arthritis may be high in these younger adults, data suggests that these reported symptoms may not significantly impact the livelihood of these patients.
Elderly Outcomes
Over the past decade, a multitude of studies have attempted to discover and understand the factors that define treatment options and optimize outcomes in the active elderly patient following a distal radius fracture. However, these factors are often interconnected and difficult to isolate for evaluation from an epidemiologic perspective. One of the major limiting factors in examining these outcomes is that few studies designate whether the fracture has intra-articular extension. This seems to be emerging as an important factor for regaining functional motion and strength, rather than absolute measures of fracture alignment and malunion.
Mortality and Functional Decline
Distal radius fractures can be a significant source of mortality and loss of independence in the elderly. In examining the functional status of a prospective cohort of 9,000 older women followed through the Study for Osteoporotic Fractures, women with a wrist fracture were 50% more likely than those without fractures to have a clinically important functional decline. This decline was practically defined by worsening ability to prepare meals, perform heavy housekeeping, climb 10 stairs, go shopping, and get out of a car.60 Mortality rates gathered from the Center for Disease Control and the National Death Index in patients with a distal radius fracture, compared to a standard US matched control group, were shown to be significantly higher than those of the standard US elderly population, an average of a 14% increase 7 years after the fracture.61 In this study, men with a distal radius fracture were found to be 2.65 times more likely to die in this time period than women with this fracture, likely due in part by the largest increase in incidence in men occurring in the over-80 year old age group. In practice, this information can be used to provide insight to the patient and family that a distal radius fracture in an elderly man portends worse outcomes than the same fracture in a woman.
Age
Previous radiographic parameters for acceptable reductions in displaced distal radius fractures had been developed using a sub-set of younger, more active patients. In Jarmeko et al’s study in 2007, they asserted that these factors had not been appropriately validated for the “elderly” in their study (average age of 68.5) and had little effect on self-reported functional outcomes in short-term follow-up in non-operative cases.62 In a retrospective study of 114 patients (average age of 79) who met operative criteria for unstable distal radius fracture, but for whom 63 declined surgery, Mattila found no significant differences at 5 years in functional outcomes or pain.63 A recent meta-analysis of more than 1,000 distal radius fractures comparing cast immobilization to any operative treatment in patients older than 60 has shown that despite worse radiographic outcomes associated with casting, functional outcomes were no different from those of surgically treated groups.
Increasing Rates of Operative Interventions
Over the past 10 years, there has been an increase in the use of surgical interventions for the treatment of distal radius fractures.63,64 Although this might appear to be directly correlated with the increased incidence of these fractures seen in recent years, no evidence is available to support such a claim. Matilla et al found that between 1998 and 2008, the use of surgical intervention for the treatment of distal radius fractures doubled.63 They also found an increase in the use of internal fixation over other techniques, which more than doubled over the 11 year period of the study.
A recent ten-year review of Medicare data conducted by Chung et al. documented trends in the treatment of distal radius fractures in the elderly.64 They found that closed fixation was the most prevalent form of fracture fixation, but the use of this treatment protocol has decreased from 82% to 70% over the past ten years. It was also documented that distal radius fractures are increasingly being treated by hand surgeons, with rates increasing from .8% to 3.9% during the study period. Additionally, hand surgeons were shown to be more likely to use internal fixation in the treatment of these fractures. In contrast, orthopaedic surgeons were found to be 5.7 times more likely than hand surgeons to use closed treatment. This coincides with a study by Koval et al. showing hand surgeons leaning towards the use of internal fixation over closed treatment.65 There is evidence that over 50% of fractures treated with closed reduction are plagued by malunion, which highlights the importance that distal radius fractures should be evaluated on a case by case basis.66,67
The increased tendency for surgical manipulation in recent years has been coupled with a shift in favor of open reduction and internal fixation over other treatment options. Although this new treatment is exciting, no conclusive evidence has shown it to be more effective than any other treatment protocol. It is not clear why this increase is occurring, but it may be because more distal radius fractures are being treated by hand surgeons. It also may be the result of increasingly successful marketing schemes directed towards surgeons, or even just the excitement that comes with the novelty of a new technology. Whatever the case, numerous studies have made it clear that there is no significant difference between the long term functional outcomes of ORIF and other therapeutic options for these fractures.68–71 Although some of these studies found that the volar locking plate did provide better short term outcomes, the long term results remained the same.
Seeking to answer some of these difficult surgical treatment questions in the elderly, the WRIST (Wrist and Radius Injury Surgical Trial) study group was formed in 2009, comprised of 19 centers across North America with participation from both plastic and orthopaedic hand surgeons.72 The group collaborated on the study design and pilot trials, and obtained NIH funding to investigate the outcomes of volar locking plates compared to other forms of surgical fixation through a multi-center clinical trial (MCCT). This MCCT design obtained through consensus structures a rigorous study protocol, collects a diverse patient sample, and recruits a large number of patients to detect smaller treatment effects.
A Dartmouth study of over 100,000 Medicare patients between 1998 and 2004 showed internal fixation rates close to doubling from 5% to 8% nationally across all ages. More interestingly, the type of operative fixation was extremely variable between hospital referral regions, with internal fixation ranging from .4% to 25% in some areas.73 These major differences in treatment rates are not unexpected given the variability in fracture patterns at the distal radius, numerous treatment options available, and the lack of consensus in the literature regarding treatment outcomes.
The most recent article to explore the use of internal fixation for distal radius fractures in the Medicare population examined regional variations, ethnic variability and treating physician characteristics to better understand the factors contributing to the changing trends.74 In 2007, they found nearly 86,000 Medicare patients suffered a closed distal radius fracture, of which 17% we treated with internal fixation. This is over two times the rate of internal fixation from a 6 year time period ending just 3 years prior to the study. They also found men were significantly less likely to receive internal fixation than women, as were blacks compared to whites. Like the Dartmouth study, they also saw nearly a 10-fold difference in the rates of internal fixation across different hospital referral regions. The study then examined these differences by region based on whether the patient was treated by a hand surgeon, finding significant positive correlations with the rates of internal fixation to the percentage of patients treated by a hand surgeon in each area.
Osteoporosis Treatment and Risk of Future Fracture
Distal radius fractures in the active elderly population can be one of the first indicators of underlying osteoporosis, and the event represents a prime point for intervention. In the year following a distal radius fracture, studies have shown 5 and10 times greater rates of vertebral fractures in women and men respectively, in accordance with a 60% increase in the rates of hip fractures for women over 70.75 It can be argued that the easiest distal radius fracture to treat is the one that does not happen, and a number of falls prevention initiatives in the active elderly have been both successful and cost-effective in preventing distal radius fractures.76,77 Other simple preventative measures include warnings for dangerous weather conditions and clearing or preventing accumulation of snow and ice in order to decrease the incidence of falls resulting in this injury.36
The elderly population has several options to aid in the prevention of distal radius fractures. One of the most important preventative measures includes the proper diagnosis and treatment of bone diseases such as osteoporosis and osteopenia. However, in a study of 111 patients in the military medical system to determine rates of osteoporosis follow up in the year following a distal radius fracture, it was discovered that only 66% received some sort of intervention for osteoporosis. One quarter of the patients were referred to endocrinology, 20% had a DEXA scan, while only 47% had been taking some sort of medication to treat their osteoporosis.78
The use of bisphosphonates in combination with supplements such as Calcium and Vitamin D has been shown to help decrease the risk of fractures due to osteopenia and osteoporosis. Bisphosphonates (BPs) are the most common therapy protocol for the treatment of bone resorption due to the effects of osteoporosis and other bone diseases.79–85 Osteoporosis is a leading risk factor for distal radius fractures, and the use of BPs has played an important role in reducing this risk. Research is currently providing new insights into the exact mechanism of action that gives BPs their anti-resorptive properties.86
Bisphosphonates are able to increase bone mineral calcium through the inhibition of osteoclastic bone resorption by altering upstream differentiation of osteocytes in addition to promoting the apoptosis of these osteoclasts.87 Due to the suppressive actions they have on bone remodeling, it was originally theorized that BPs would disrupt the healing process of fractures. It has been shown that this is not the case, and in fact BPs stimulate bone remodeling by promoting the recruitment and activity of osteoblasts and osteocytes, while decreasing apoptosis of these cells.88 This activity causes an increase in bone mineral density, which can result in up to a 50% decrease in the risk of future fractures.89 A recent study found less than a one week difference in the rate of distal radius fracture healing for those taking BPs and those not taking them (55 days versus 49 days), a difference felt to be not clinically significant90
Recent reports have highlighted that bisphosphonate treatment is not without risk, despite an estimated 30 million individuals prescribed bisphosphonate therapy per year in the US alone.91 Known esophageal irritation is common, but atypical sub-trochanteric femur fractures are increasingly being reported, primarily in the setting of long-term bisphosphonate use.92–94 Osteonecrosis of the jaw has also been reported to occur in up to .04% of osteoporotic patients on bisphosphonate therapy.95 The dose dependency effect is now more clearly defined, but the exact pathogenic role of bisphosphonates in these atypical bone events remains unclear. The physician must weigh the risks and benefits with the patient, but the absolute risk of atypical fracture associated with bisphosphonate use compared with the high risk of osteoporotic fractures is small, when compared to the beneficial effects of the drug.
The ability to efficiently and accurately diagnose osteoporosis is another important step that could help decrease medical costs and patient morbidity of those afflicted by this disease. It would not be cost effective to diagnose and treat everyone, so it is essential that only those at high risk for osteoporosis should be evaluated and treated.
Conclusion
Possessing a knowledge of the incidence and outcomes of distal radius fractures allows the physician to better counsel individual patients and determine the best management to optimize treatment. Although treatment outcomes for pediatric and young adults are fairly well defined for distal radius fractures, recent research in the elderly population has made decision-making for the patient and surgeon more complex. It is becoming increasingly difficult to define the difference between the active “older” adult that will continue to place high demands on an injured wrist, and the true “elderly” that may better adapt to an imperfect outcome. Large multi-center studies, such as the WRIST study, with long-term follow-up may be the only way to accurately delineate the best treatment options for an individual based on outcomes for a similar patient population.
Acknowledgements
Supported in part by grants from the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR062066) and from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2R01 AR047328-06) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Melton L, III, Amadio P, Crowson C, O'fallon W. Long-term trends in the incidence of distal forearm fractures. Osteoporosis Int. 1998;8:341–348. doi: 10.1007/s001980050073. [DOI] [PubMed] [Google Scholar]
- 3.de Putter CE, van Beeck EF, Looman CW, Toet H, Hovius SE, Selles RW. Trends in wrist fractures in children and adolescents, 1997–2009. J Hand Surg Am. 2011;36:1810–1815. e2. doi: 10.1016/j.jhsa.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Hagino H, Yamamoto K, Ohshiro H, Nakamura T, Kishimoto H, Nose T. Changing incidence of hip, distal radius, and proximal humerus fractures in Tottori Prefecture, Japan. Bone. 1999;24:265–270. doi: 10.1016/s8756-3282(98)00175-6. [DOI] [PubMed] [Google Scholar]
- 5.Thompson PW, Taylor J, Dawson A. The annual incidence and seasonal variation of fractures of the distal radius in men and women over 25 years in Dorset, UK. Injury. 2004;35:462–466. doi: 10.1016/S0020-1383(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 6.Larsen CF, Lauritsen J. Epidemiology of acute wrist trauma. Int J Epidemiol. 1993;22:911–916. doi: 10.1093/ije/22.5.911. [DOI] [PubMed] [Google Scholar]
- 7.Alffram PA, Bauer GC. Epidemiology of fractures of the forearm. A biomechanical investigation of bone strength. J Bone Joint Surg Am. 1962;44-A:105–114. [PubMed] [Google Scholar]
- 8.Knowelden J, Buhr AJ, Dunbar O. Incidence of Fractures in Persons over 35 Years of Age. A Report to the M.R.C. Working Party on Fractures in the Elderly. British J of Prev and Social Med. 1964;18:130–141. doi: 10.1136/jech.18.3.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bengner U, Johnell O. Increasing incidence of forearm fractures. A comparison of epidemiologic patterns 25 years apart. Acta Orthop Scand. 1985;56:158–160. doi: 10.3109/17453678508994345. [DOI] [PubMed] [Google Scholar]
- 10.Omsland TK, Ahmed LA, Gronskag A, et al. More forearm fractures among urban than rural women: the NOREPOS study based on the Tromso study and the HUNT study. J Bone Min Res. 2011;26:850–856. doi: 10.1002/jbmr.280. [DOI] [PubMed] [Google Scholar]
- 11.Holroyd C, Harvey N, Dennison E, Cooper C. Epigenetic influences in the developmental origins of osteoporosis. Osteoporos Int. 2011 doi: 10.1007/s00198-011-1671-5. [DOI] [PubMed] [Google Scholar]
- 12.Ryan LM, Teach SJ, Searcy K, et al. Epidemiology of pediatric forearm fractures in Washington, DC. J Trauma. 2010;69:S200–S205. doi: 10.1097/TA.0b013e3181f1e837. [DOI] [PubMed] [Google Scholar]
- 13.Kelsey J, Praemer A, Nelson L, Felberg A, Rice D. Upper Extremity Disorders: Frequency, Impact, and Cost. New York: Churchill Livingstone; 1997. [Google Scholar]
- 14.Shauver MJ, Yin H, Banerjee M, Chung KC. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36:1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 15.Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand Suppl. 1983;202:1–109. [PubMed] [Google Scholar]
- 16.Cooper C, Dennison EM, Leufkens HGM, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone and Mineral Res. 2004;19:1976–1981. doi: 10.1359/JBMR.040902. [DOI] [PubMed] [Google Scholar]
- 17.Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38:913–922. doi: 10.1016/j.injury.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 18.Ward WT, Rihn JA. The impact of trauma in an urban pediatric orthopaedic practice. J Bone Joint Surg Am. 2006;88:2759–2764. doi: 10.2106/JBJS.F.00046. [DOI] [PubMed] [Google Scholar]
- 19.Khosla S, Melton LJ, 3rd, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290:1479–1485. doi: 10.1001/jama.290.11.1479. [DOI] [PubMed] [Google Scholar]
- 20.Hagino H, Yamamoto K, Ohshiro H, Nose T. Increasing incidence of distal radius fractures in Japanese children and adolescents. J Orthop Sci. 2000;5:356–360. doi: 10.1007/s007760070043. [DOI] [PubMed] [Google Scholar]
- 21.Mathison DJ, Agrawal D. An update on the epidemiology of pediatric fractures. Pediatr Emerg Care. 2010;26:594–603. doi: 10.1097/PEC.0b013e3181eb838d. quiz 4–6. [DOI] [PubMed] [Google Scholar]
- 22.Wood AM, Robertson GA, Rennie L, Caesar BC, Court-Brown CM. The epidemiology of sports-related fractures in adolescents. Injury. 2010;41:834–838. doi: 10.1016/j.injury.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71:1225–1231. [PubMed] [Google Scholar]
- 24.Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000;32:1601–1609. doi: 10.1097/00005768-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Krabbe S, Christiansen C, Rodbro P, Transbol I. Effect of puberty on rates of bone growth and mineralisation: with observations in male delayed puberty. Arch Dis Child. 1979;54:950–953. doi: 10.1136/adc.54.12.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rizzoli R, Bonjour JP, Ferrari SL. Osteoporosis, genetics and hormones. J Mol Endocrinol. 2001;26:79–94. doi: 10.1677/jme.0.0260079. [DOI] [PubMed] [Google Scholar]
- 27.Henry YM, Fatayerji D, Eastell R. Attainment of peak bone mass at the lumbar spine, femoral neck and radius in men and women: relative contributions of bone size and volumetric bone mineral density. Osteoporosis Int. 2004;15:263–273. doi: 10.1007/s00198-003-1542-9. [DOI] [PubMed] [Google Scholar]
- 28.Faulkner RA, Davison KS, Bailey DA, Mirwald RL, Baxter-Jones AD. Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res. 2006;21:1864–1870. doi: 10.1359/jbmr.060907. [DOI] [PubMed] [Google Scholar]
- 29.Parfitt AM. The two faces of growth: benefits and risks to bone integrity. Osteoporos Int. 1994;4:382–398. doi: 10.1007/BF01622201. [DOI] [PubMed] [Google Scholar]
- 30.Al-Ansari K, Howard A, Seeto B, Yoo S, Zaki S, Boutis K. Minimally angulated pediatric wrist fractures: is immobilization without manipulation enough? CJEM. 2007;9:9–15. doi: 10.1017/s1481803500014676. [DOI] [PubMed] [Google Scholar]
- 31.Brogren E, Petranek M, Atroshi I. Incidence and characteristics of distal radius fractures in a southern Swedish region. BMC Musculoskelet Disord. 2007;8:48. doi: 10.1186/1471-2474-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 33.Griffin MR, Ray WA, Fought RL, Melton LJ., 3rd Black-white differences in fracture rates. Am J Epidemiol. 1992;136:1378–1385. doi: 10.1093/oxfordjournals.aje.a116450. [DOI] [PubMed] [Google Scholar]
- 34.Baron JA, Barrett J, Malenka D, et al. Racial differences in fracture risk. Epidemiology. 1994;5:42–47. doi: 10.1097/00001648-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Baron JA, Karagas M, Barrett J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Flinkkila T, Sirnio K, Hippi M, et al. Epidemiology and seasonal variation of distal radius fractures in Oulu, Finland. Osteoporos Int. 2011;22:2307–2312. doi: 10.1007/s00198-010-1463-3. [DOI] [PubMed] [Google Scholar]
- 37.Sigurdardottir K, Halldorsson S, Robertsson J. Epidemiology and treatment of distal radius fractures in Reykjavik, Iceland, in 2004. Comparison with an Icelandic study from 1985. Acta Orthop. 2011;82:494–498. doi: 10.3109/17453674.2011.606074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal Radius Fractures in Older Women: A 10-Year Follow-Up Study of Descriptive Characteristics and Risk Factors. The Study of Osteoporotic Fractures. J Amer Geriatric Soc. 2002;50:97–103. doi: 10.1046/j.1532-5415.2002.50014.x. [DOI] [PubMed] [Google Scholar]
- 39.WHO. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129. [PubMed] [Google Scholar]
- 40.Kanterewicz E, Yanez A, Perez-Pons A, Codony I, Del Rio L, Diez-Perez A. Association between Colles' fracture and low bone mass: age-based differences in postmenopausal women. Osteoporosis Int. 2002;13:824–828. doi: 10.1007/s001980200114. [DOI] [PubMed] [Google Scholar]
- 41.Lofman O, Hallberg I, Berglund K, et al. Women with low-energy fracture should be investigated for osteoporosis. Acta Orthopaedica. 2007;78:813–821. doi: 10.1080/17453670710014608. [DOI] [PubMed] [Google Scholar]
- 42.Oyen J, Rohde GE, Hochberg M, Johnsen V, Haugeberg G. Low-energy distal radius fractures in middle-aged and elderly women-seasonal variations, prevalence of osteoporosis, and associates with fractures. Osteoporos Int. 2010;21:1247–1255. doi: 10.1007/s00198-009-1065-0. [DOI] [PubMed] [Google Scholar]
- 43.Oyen J, Brudvik C, Gjesdal CG, Tell GS, Lie SA, Hove LM. Osteoporosis as a risk factor for distal radial fractures: a case-control study. J Bone Joint Surg Am. 2011;93:348–356. doi: 10.2106/JBJS.J.00303. [DOI] [PubMed] [Google Scholar]
- 44.Oyen J, Rohde G, Hochberg M, Johnsen V, Haugeberg G. Low bone mineral density is a significant risk factor for low-energy distal radius fractures in middle-aged and elderly men: a case-control study. BMC Musculoskeletal Disorders. 2011;12:67. doi: 10.1186/1471-2474-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Melton LJ, 3rd, Christen D, Riggs BL, et al. Assessing forearm fracture risk in postmenopausal women. Osteoporosis Int. 2010;21:1161–1169. doi: 10.1007/s00198-009-1047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clayton RAE, Gaston MS, Ralston SH, Court-Brown CM, McQueen MM. Association between decreased bone mineral density and severity of distal radial fractures. J Bone Joint Surg Am. 2009;91:613–619. doi: 10.2106/JBJS.H.00486. [DOI] [PubMed] [Google Scholar]
- 47.Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J of Ped Orthopedics. 1990;10:705. doi: 10.1097/01241398-199011000-00001. [DOI] [PubMed] [Google Scholar]
- 48.Fuller D, McCullough C. Malunited fractures of the forearm in children. J Bone Joint Surg Br. 1982;64:364. doi: 10.1302/0301-620X.64B3.7096406. [DOI] [PubMed] [Google Scholar]
- 49.Noonan KJ, Price CT. Forearm and distal radius fractures in children. J Am Acad Orth Surg. 1998;6:146–156. doi: 10.5435/00124635-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Randsborg P-H, Sivertsen EA. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthopaedica. 2009;80:585–589. doi: 10.3109/17453670903316850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Do TT, Strub WM, Foad SL, Mehlman CT, Crawford AH. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop Br. 2003;12:109–115. doi: 10.1097/01.bpb.0000043725.21564.7b. [DOI] [PubMed] [Google Scholar]
- 52.Vince K, Miller J. Cross-union complicating fracture of the forearm. Part II: Children. J Bone Joint Surg Am. 1987;69:654. [PubMed] [Google Scholar]
- 53.Arunachalam V, Griffiths J. Fracture recurrence in children. Injury. 1975;7:37–40. doi: 10.1016/0020-1383(75)90057-1. [DOI] [PubMed] [Google Scholar]
- 54.Goulding A, Grant AM, Williams SM. Bone and body composition of children and adolescents with repeated forearm fractures. J Bone and Min Research. 2005;20:2090–2096. doi: 10.1359/JBMR.050820. [DOI] [PubMed] [Google Scholar]
- 55.Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg Br. 1993;18:45–49. doi: 10.1016/0266-7681(93)90195-l. [DOI] [PubMed] [Google Scholar]
- 56.Cooney WP, Linscheid RL, Dobyns JH. External pin fixation for unstable Colles’ fractures. J Bone Joint Surg Am. 1979;61:840–845. [PubMed] [Google Scholar]
- 57.Green DP. Pins and plaster treatment of comminuted fractures of the distal end of the radius. J Bone Joint Surg Am. 1975;57:304–310. [PubMed] [Google Scholar]
- 58.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647–659. [PubMed] [Google Scholar]
- 59.Catalano LJ, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J. Displaced Intra-Articular Fractures of the Distal Aspect of the Radius. Long-Term Results in Young Adults after Open Reduction and Internal Fixation. J Bone Joint Surg Am. 1997;79:1290–1302. doi: 10.2106/00004623-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 60.Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional decline after incident wrist fractures—Study of Osteoporotic Fractures: prospective cohort study. BMJ. 2010;341 doi: 10.1136/bmj.c3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rozental TD, Branas CC, Bozentka DJ, Beredjiklian PK. Survival among elderly patients after fractures of the distal radius. J of Hand Surg. 2002;27:948–952. doi: 10.1053/jhsu.2002.36995. [DOI] [PubMed] [Google Scholar]
- 62.Jaremko J, Lambert R, Rowe B, Johnson J, Majumdar S. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiology. 2007;62:65–72. doi: 10.1016/j.crad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 63.Mattila VM, Huttunen TT, Sillanpaa P, Niemi S, Pihlajamaki H, Kannus P. Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma. 2011;71:939–942. doi: 10.1097/TA.0b013e3182231af9. [DOI] [PubMed] [Google Scholar]
- 64.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where's the evidence? J Bone Joint Surg Am. 2008;90:1855–1861. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 66.Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]
- 67.Strange-Vognsen HH. Intraarticular fractures of the distal end of the radius in young adults. A 16 (2–26) year follow-up of 42 patients. Acta Orthop Scand. 1991;62:527–530. doi: 10.3109/17453679108994488. [DOI] [PubMed] [Google Scholar]
- 68.Xu GGQ, Chan SP, Puhaindran ME, Chew WYC . Prospective randomised study of intra-articular fractures of the distal radius: comparison between external fixation and plate fixation. Annals of the Academy of Medicine, Singapore. 2009;38:600–606. [PubMed] [Google Scholar]
- 69.Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1568–1577. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]
- 70.Grewal R, Macdermid JC, King GJ, Faber KJ. Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg Am. 2011;36:1899–1906. doi: 10.1016/j.jhsa.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 71.Belloti JC, Tamaoki MJ, Atallah AN, Albertoni WM, dos Santos JB, Faloppa F. Treatment of reducible unstable fractures of the distal radius in adults: a randomised controlled trial of De Palma percutaneous pinning versus bridging external fixation. BMC Musculoskeletal Disorders. 2010;11:137. doi: 10.1186/1471-2474-11-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chung KC, Song JW. A Guide on Organizing a Multicenter Clinical Trial: the WRIST study group. Plastic and reconstructive surgery. 2010;126:515. doi: 10.1097/PRS.0b013e3181df64fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fanuele J, Koval K, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91:1313–1319. doi: 10.2106/JBJS.H.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chung KC, Shauver MJ, Yin H, Kim HM, Baser O, Birkmeyer JD. Variations in the Use of Internal Fixation for Distal Radial Fracture in the United States Medicare Population. J Bone Joint Surg Am. 2011;93:2154–2162. doi: 10.2106/JBJS.J.012802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cuddihy MT, Gabriel SE, Crowson CS, O'Fallon WM, Melton LJ., 3rd Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporosis Int. 1999;9:469–475. doi: 10.1007/s001980050172. [DOI] [PubMed] [Google Scholar]
- 76.Rizzo JA, Baker DI, McAvay G, Tinetti ME. The cost-effectiveness of a multifactorial targeted prevention program for falls among community elderly persons. Medical Care. 1996;34:954. doi: 10.1097/00005650-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 77.Kelsey JL, Prill MM, Keegan THM, et al. Reducing the risk for distal forearm fracture: preserve bone mass, slow down, and don’t fall! Osteoporosis Int. 2005;16:681–690. doi: 10.1007/s00198-004-1745-8. [DOI] [PubMed] [Google Scholar]
- 78.Freedman BA, Potter BK, Nesti LJ, Cho T, Kuklo TR. Missed opportunities in patients with osteoporosis and distal radius fractures. Clinical Orthopedics and Related Res. 2007;454:202. doi: 10.1097/01.blo.0000238866.15228.c4. [DOI] [PubMed] [Google Scholar]
- 79.Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD003376.pub3. CD001155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wells GA, Cranney A, Peterson J, et al. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD003376.pub3. CD003376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD004523.pub3. CD004523. [DOI] [PubMed] [Google Scholar]
- 82.Rodan GA, Fleisch HA. Bisphosphonates: mechanisms of action. J Clin Invest. 1996;97:2692–2696. doi: 10.1172/JCI118722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cummings SR, Karpf DB, Harris F, et al. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002;112:281–289. doi: 10.1016/s0002-9343(01)01124-x. [DOI] [PubMed] [Google Scholar]
- 84.Reid IR, King AR, Alexander CJ, Ibbertson HK. Prevention of steroid-induced osteoporosis with (3-amino-1-hydroxypropylidene)-1,1-bisphosphonate (APD) Lancet. 1988;1:143–146. doi: 10.1016/s0140-6736(88)92721-3. [DOI] [PubMed] [Google Scholar]
- 85.Saag KG, Emkey R, Schnitzer TJ, et al. Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-Induced Osteoporosis Intervention Study Group. N Engl J Med. 1998;339:292–299. doi: 10.1056/NEJM199807303390502. [DOI] [PubMed] [Google Scholar]
- 86.Lomashvili KA, Monier-Faugere MC, Wang X, Malluche HH, O'Neill WC. Effect of bisphosphonates on vascular calcification and bone metabolism in experimental renal failure. Kidney Int. 2009;75:617–625. doi: 10.1038/ki.2008.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hughes DE, Wright KR, Uy HL, et al. Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res. 1995;10:1478–1487. doi: 10.1002/jbmr.5650101008. [DOI] [PubMed] [Google Scholar]
- 88.Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;104:1363–1374. doi: 10.1172/JCI6800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 90.Rozental TD, Vazquez MA, Chacko AT, Ayogu N, Bouxsein ML. Comparison of radiographic fracture healing in the distal radius for patients on and off bisphosphonate therapy. J Hand Surg Am. 2009;34:595–602. doi: 10.1016/j.jhsa.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 91.Masoodi NA. Oral Bisphosphonates and the Risk for Osteonecrosis of th Oral Bisphosphonates and the Risk for Osteonecrosis of the Jaw e Jaw. British J of Medical Practitioners. 2009;2 [Google Scholar]
- 92.Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. New England Journal of Medicine. 2008;358:1304–1306. doi: 10.1056/NEJMc0707493. [DOI] [PubMed] [Google Scholar]
- 93.Rizzoli R, Åkesson K, Bouxsein M, et al. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European society on clinical and economic aspects of osteoporosis and osteoarthritis, and international osteoporosis foundation working group report. Osteoporosis International. 2011:1–18. doi: 10.1007/s00198-010-1453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. NEJM. 2011;364:1728–1737. doi: 10.1056/NEJMoa1010650. [DOI] [PubMed] [Google Scholar]
- 95.Cartsos VM, Zhu S, Zavras AI. Bisphosphonate use and the risk of adverse jaw outcomes: a medical claims study of 714,217 people. J of the Am Dental Assn. 2008;139:23–30. doi: 10.14219/jada.archive.2008.0016. [DOI] [PubMed] [Google Scholar]