Abstract
The Sinding-Larsen-Johansson syndrome has a pathogenesis similar to that of the Osgood-Schlatter disorder and is the result of excessive force exerted by the patellar tendon on the lower pole of the patella. Clinically it is characterized by pain, which increases when the patellar is loaded during flexion, subpatellar swelling and functional limitation. The authors present a case of a 13-year-old boy who was a competitive youth team football player. He presented with anterior, spontaneous knee pain and swelling at the inferior pole of the patella. Ultrasonography (US) confirmed clinical diagnosis showing lesions typical of the Sinding-Larsen-Johansson syndrome. The patient was told to refrain from sports activity; after five months recovery was complete and US follow-up revealed no anomaly. The authors consider the case worthy of reporting because it is paradigmatic and to emphasize the role of US in the evaluation of the Sinding-Larsen-Johansson syndrome.
Keywords: Sinding-Larsen-Johansson syndrome, Knee, Ultrasound
Sommario
La sindrome di Sinding-Larsen-Johansson ha patogenesi simile alla malattia di Osgood-Schlatter, legata all'azione traumatica esercitata dal tendine rotuleo sul polo inferiore della rotula. Clinicamente è caratterizzata da dolore, che aumenta nell'appoggio in flessione, edema sottorotuleo e limitazione funzionale. Il caso in esame si riferisce ad un ragazzo di 13 anni che praticava il calcio, a livello agonistico. Clinicamente presentava dolore al ginocchio, anteriore, spontaneo e tumefazione in corrispondenza del polo inferiore del rotula. L'ecografia evidenziava le lesioni tipiche della sindrome di Sinding-Larsen-Johansson e confermava la diagnosi clinica; veniva prescritta l'astensione dall'attività sportiva. A distanza di cinque mesi si aveva la completa guarigione, con controllo ecografico che confermava l'assenza di lesioni.
Abbiamo ritenuto il caso meritevoli di segnalazione perché paradigmatico e per sottolineare il ruolo dell'ecografia nella valutazione della sindrome di Sinding-Larsen-Johansson.
Introduction
The Sinding-Larsen-Johansson syndrome has a pathogenesis similar to that of the Osgood-Schlatter disease and the two disorders sometimes occur simultaneously [1]. The Sinding-Larsen-Johansson syndrome is caused by increased tension and pressure due to repetitive traction by the patellar tendon on the lower pole of the patella (still partly cartilaginous in adolescents) during contraction of the quadriceps muscle. This leads to cartilage damage, swelling and pain, especially after exertion of force, and later to tendon thickening and fragmentation of the lower pole of the patella and sometimes to bursitis, i.e. inflammation of a bursa situated between the tendon and the patella. The syndrome is seen in adolescents typically between 10 and 14 years of age, but most often in males who play sports (football, running, volley ball, gymnastics) [2,3]. Clinically it is characterized by pain localized to the lower pole of the patella, which increases when the patellar is loaded during flexion, subpatellar edema and functional limitation. Ultrasound (US) can depict all the manifestations of this disorder: swelling of the cartilage, tendon thickening, fragmentation of the lower pole of the patella and bursitis [4–6].
Presentation of the case
The authors present a case of a 13-year-old boy who was a competitive youth team football player. He presented with anterior, spontaneous knee pain which was exacerbated during movement or after prolonged knee flexion and loading, and swelling at the inferior pole of the patella. Ultrasound (US) showed swelling of the cartilage, fragmentation of the lower pole of the patella, thickening of the patellar tendon at the proximal insertion (Fig. 1A) and the presence of a serous bursa distended with fluid situated between the patellar tendon and the lower pole of the patella (Fig. 1B). Sinding-Larsen-Johansson syndrome was diagnosed and the patient was told to refrain from sports activity, which was a difficult task in this particular case. The symptoms rapidly regressed and after 5 months the patient had completely recovered and US follow-up revealed no anomaly.
Figure 1.
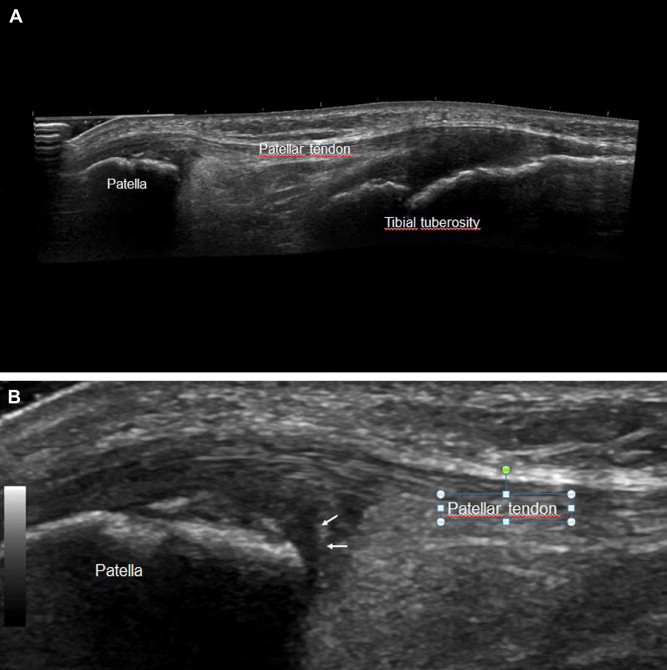
Sinding-Larsen-Johansson syndrome. US image shows swelling of the cartilage, fragmentation of the lower pole of the patella, patellar tendon thickening at the proximal insertion (A) and presence of a serous bursa (B) distended with fluid (arrows) located between the patellar tendon and the lower pole of the patella.
Discussion and conclusions
The Sinding-Larsen-Johansson syndrome is characterized by swelling of the cartilage, thickening of the patellar tendon with calcifications in the advanced stages, fragmentation of the lower pole of the patella (Fig. 1A) and bursitis affecting a serous bursa situated between the patellar tendon and the patella (Fig. 1B).
Clinically it is characterized by pain localized to the lower pole of the patella. In the acute painful phase, therapy is mainly rest and abstention from sports activity for at least 1–2 months, particularly football and running that may be replaced by swimming and other sports which exert less pressure on the quadriceps femoris muscle. The evolution is usually benign with spontaneous recovery; thanks to the physiological regeneration full recovery usually takes 12–24 months. When the patella is completely ossified the pain disappears and complications are rare [7].
US can evidence all manifestations of the Sinding-Larsen-Johansson syndrome (Fig. 1) [4–6] and should therefore be considered the examination of choice in the evaluation of this syndrome, also due to the absence of side effects which causes the method to be well-accepted by parents.
The authors consider the case worthy of reporting because it is paradigmatic and to emphasize the role of US in the evaluation of the Sinding-Larsen-Johansson syndrome.
Conflict of interest
The authors have no conflict of interest to disclose.
Appendix A. Supplementary data
References
- 1.Hagner W., Sosnowski S., Kaziñski W., Frankowski S. A case of Sinding-Larsen-Johansson and Osgood-Schlatter disease in both knees. Chir Narzadow Ruchu Ortop Pol. 1993;58(1):13–15. [PubMed] [Google Scholar]
- 2.Iwamoto J., Takeda T., Sato Y., Matsumoto H. Radiographic abnormalities of the inferior pole of the patella in juvenile athletes. Keio J Med. 2009 Mar;58(1):50–53. doi: 10.2302/kjm.58.50. [DOI] [PubMed] [Google Scholar]
- 3.Peace K.A., Lee J.C., Healy J. Imaging the infrapatellar tendon in the elite athlete. Clin Radiol. 2006 Jul;61(7):570–578. doi: 10.1016/j.crad.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 4.De Flaviis L., Nessi R., Scaglione P., Balconi G., Albisetti W., Derchi L.E. Ultrasonic diagnosis of Osgood-Schlatter and Sinding-Larsen-Johansson diseases of the knee. Skeletal Radiol. 1989;18(3):193–197. doi: 10.1007/BF00360969. [DOI] [PubMed] [Google Scholar]
- 5.Draghi F., Danesino G.M., Coscia D., Precerutti M., Pagani C. Overload syndromes of the knee in adolescents: sonographic findings. J Ultrasound. 2008;11:151–157. doi: 10.1016/j.jus.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barbuti D., Bergami G., Testa F. Ultrasonographic aspects of Sinding-Larsen-Johansson disease. Pediatr Med Chir. 1995 Jan-Feb;17(1):61–63. [PubMed] [Google Scholar]
- 7.Freedman D.M., Kono M., Johnson E.E. Pathologic patellar fracture at the site of an old Sinding-Larsen-Johansson lesion: a case report of a 33-year-old male. J Orthop Trauma. 2005 Sep;19(8):582–585. doi: 10.1097/01.bot.0000151817.55551.2d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


