Abstract
Purpose
Systemic chemotherapy still represents the gold standard in the treatment of irresectable colorectal liver metastases. Modern anticancer agents like the monoclonal antibody cetuximab have improved the outcome of patients in clinical studies. As hepatic arterial infusion (HAI) is capable to potentially increase the anticancer effect of cytostatics, we herein studied whether HAI of cetuximab (CE) as a single agent or in combination with oxaliplatin (OX) exerts increased anticancer effects compared to the systemic application (SYS) of the drugs.
Methods
WAG/Rij rats were randomized to eight groups and underwent 10 days after subcapsular hepatic tumor implantation either HAI or SYS of CE, OX, or the combination of both agents (CE + OX). Saline-treated animals served as controls. Tumor volume was measured at days 10 and 13 using three-dimensional ultrasound. On day 13, liver and tumor tissue was sampled for histological and immunohistochemical analysis.
Results
In controls, the tumor volume significantly increased from day 10 to 13. Application of OX alone via HAI or SYS did not inhibit tumor growth compared to controls. SYS of CE or CE + OX did also not reduce tumor growth. In contrast, HAI of CE and CE + OX significantly inhibited tumor growth. HAI of CE significantly reduced tumor vascularization as measured by the number of platelet endothelial cell adhesion molecule-1-positive cells and significantly increased the number of apoptotic tumor cells as measured by the cellular caspase-3 expression.
Conclusion
HAI of CE and CE + OX reduces tumor growth of colorectal rat liver metastases involving the inhibition of angiogenesis and induction of tumor cell apoptosis.
Keywords: Colorectal liver metastases, Locoregional chemotherapy, Hepatic arterial infusion, Systemic chemotherapy, Monoclonal antibody
Introduction
Colorectal cancer is one of the most common malignancies in the western world and has rising incidence in Asia either [1]. About 50 % of colorectal cancer patients develop liver metastases with a statistical 5-year survival of 10–20 % [2]. Today, due to novel and multimodal therapies, treatment options for hepatic colorectal metastases are manifold. However, the patient population is very inhomogeneous. In patients with irresectable liver metastases, the 5-year survival rate is almost zero. In contrast, patients with resectable metastases can even be healed by surgical treatment.
Systemic chemotherapy plays a key role in colorectal cancer patients, regardless of whether the therapeutic intention is curative or palliative. The response rate of the classic intravenous 5-fluorouracil/folinic acid chemotherapy regime is about 20 %. In the past years, it has been shown that by adding oxaliplatin or irinotecan (FOLFOX and FOLFIRI regimens) the response rate is doubled [3]. Cetuximab, a chimeric monoclonal IgG1 antibody directed against the ligand-binding domain of the epidermal growth factor receptor (EGF-R), belongs to a group of novel anti-cancer agents. Its additional application has led to a further improvement of the outcome of metastatic colorectal cancer treatment, albeit restricted to patients with wild-type K-ras status [4–6]. However, even with modern systemic chemotherapy regimens, the 2-year survival rate still does not exceed 40 % [7].
Despite an ongoing discussion about the oncological benefit of hepatic arterial infusion (HAI), it is known that HAI is capable of augmenting the antineoplastic effects of anticancer agents, and therefore, it is recommended from some centers [8–11]. A recent Cochrane review of Mocellin et al. concluded that the future of HAI seems to be linked to the delivery of novel cancer agents or drug combinations [12]. Accordingly, we herein studied in a rat liver metastasis model, whether HAI compared to SYS of cetuximab with or without the combination of oxaliplatin is capable of increasing the antitumor effect of these agents.
Materials and methods
Binding of cetuximab
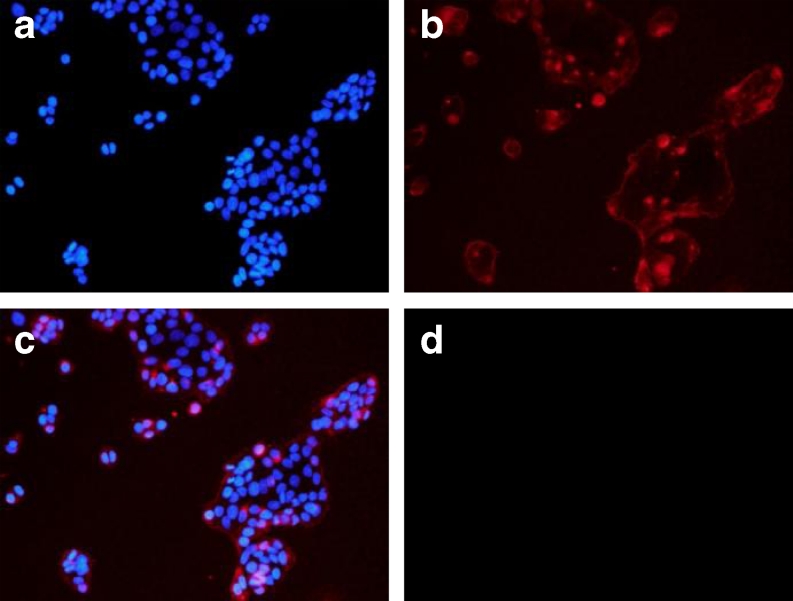
To analyze the specific binding of cetuximab to the surface of the cells of the rat colon carcinoma cell line CC531, in vitro immunocytochemical fluorescence staining was performed. After fixing with 4 % phosphate-buffered formalin and blocking of unspecific binding sites with 1 % donkey serum, CC531 cells were incubated with the primary antibody concentrate cetuximab for 2 h at 37 °C. A Cy-3-labeled donkey antihuman IgG antibody was incubated for 30 min at the concentration of 1:50 (Jackson by Dianova GmbH, Hamburg, Germany) and was used as secondary antibody. Cell nuclei were stained with 2 μg/mL bisbenzimide (Sigma, Taufkirchen, Germany). The cells were visualized by fluorescence microscopy (Fig. 1). In four separate experiments, the number of positively stained cells was counted in 20 high-power fields (each experiment) and is given in percent of all cells analyzed.
Fig. 1.
Immunocytochemical fluorescence microscopy of CC531 cells in vitro. a The staining of the nuclei of the cells (cells are stained blue). b The binding of cetuximab (stained red) on the CC531 cells; c the merge of a and b. d The negative control
In vitro cell viability analysis
To assess the effect of cetuximab on the viability of cultured CC531 cells, a water-soluble tetrazolium (WST)-1 assay was performed according to the manufacturer’s instructions (Roche, Mannheim, Germany). For this purpose, 1 × 104 cells per well were seeded in 100 μL RPMI medium with 20 % fetal calf serum,100 U/mL penicillin, and 0.1 mg/mL streptomycin (PAA, Cölbe, Germany) on a 9-well plate. After overnight culturing at 37 °C in a humidified atmosphere containing 5 % CO2, cells were treated with cetuximab in concentrations of 1, 10, 100, 1,000, 2,500, or 5,000 μg/mL for 24 h. WST-1 reagent (10 μL) was added, and the absorption was measured after 30 min at 450 nm and at 620 nm as reference, using a microplate reader. The measured data were corrected to the blank values without cells.
Drugs
Cetuximab was given in a dose of 125 mg/m2, and oxaliplatin, in a dose of 85 mg/m2. To calculate the body surface area, we used “Meeh’s formula,” assuming that it is proportional to the two-thirds power of the body weight. The formula reads as follows: A = K × W 2/3, where A represents the body surface area; K, an animal specific constant; and W, the body weight. In the present study, a K value of 9.1 was used [13].
Rat liver metastasis model
All experiments were approved by the local governmental ethic committee. Forty-eight male WAG/Rij rats with a mean body weight of 267.5 ± 5.9 g were used to perform the experiments. Animals were randomized in eight groups (n = 6 each) and kept in a temperature- and humidity-controlled 12-h light/dark cycle environment with free access to water and standard laboratory chow (Altromin, Lage, Germany). For the induction of colorectal liver metastases, a median laparotomy was performed under ether anesthesia. Using a 27 G needle (Omnicon F, Braun, Melsungen, Germany) 5 × 105 cells of the syngeneic CC531 colon carcinoma cell line were injected under the capsule of the lower surface of the left liver lobe. Laparotomy was closed by a one-layer running PDS 4–0 suture (Ethicon/Johnson & Johnson MEDICAL GmbH, Norderstedt, Germany).
Surgical procedure
Ten days after tumor cell implantation, animals were relaparotomized under ether anesthesia. For the HAI procedure, the gastroduodenal artery was cannulated (ID 0.28 mm, Portex, Hythe, UK). The tip of the catheter was positioned at the common hepatic artery. During the HAI procedure, the hepatic artery was not occluded and showed orthograde blood flow. After the HAI procedure, the catheter was removed, and the gastroduodenal artery was ligated. For the SYS procedure, the subhepatic vena cava was punctured with a 23-G needle (Troge Medical GmbH, Hamburg, Germany) according to previously published standards [14].
Experimental protocol
Animals were randomized to eight groups (n = 6 each) including four subgroups of animals undergoing HAI and four subgroups undergoing SYS. After tumor cell implantation (day 0), relaparotomy was performed on day 10, and animals received either cetuximab (CE), oxaliplatin (OX), or the combination of both (CE + OX) via HAI or SYS. Sham controls received an equivalent amount of 0.9 % saline solution (Braun, Melsungen, Germany). HAI or SYS procedure was performed for a time period of 1 min followed by ultrasound imaging. Three days later (day 13), animals underwent relaparotomy for final ultrasound imaging. Animals were sacrificed, and tissue samples were asserved for histological and immunohistochemical analysis. The body weight of the animals was measured on days 0, 10, and 13 to determine weight reduction due to the treatment.
Three-dimensional ultrasound imaging
For evaluation of the tumor volume, the 40-MHz ultrasound probe of the Vevo 770 high-resolution imaging system (VisualSonics, Inc., Toronto, Ontario, Canada) was used. Ultrasound imaging was performed on the liver surface on days 10 and 13. For three-dimensional imaging, parallel two-dimensional images were acquired in 50-μm intervals controlled by a stepping motor. The three-dimensional reconstruction was achieved by off-line outlining the tumor dimension every 200 μm on the two-dimensional images. Using these data, the integrated software of the ultrasound device produced a polygonal three-dimensional image and calculated the tumor volume.
Sampling and assays
Via puncture of the subhepatic vena cava, venous blood samples were taken at day 10 before drug administration and at day 13 before ultrasound imaging. As indicators of hepatocellular injury, aspartate aminotransferase (ASAT), alanine aminotransferase (ALAT) and glutamate dehydrogenase (GLDH) serum activities were determined using routine spectrophotometry.
Histology
Tissue specimens of the tumor and the surrounding liver parenchyma were fixed in 4 % phosphate-buffered formalin and embedded in paraffin. Histological analysis of hepatocellular injury, venular endothelial detachment and venular fibrin clotting, was performed using sections of 5 μm stained with hematoxylin–eosin. Hepatocellular injury was determined by analysis of hepatocellular vacuolization with a semiquantitative score: 0 = none; 1 = mild; 2 = moderate; and 3 = severe. Venular endothelial detachment was assessed by counting the number of venules with detachment of endothelial lining cells and is given in percent of all venules analyzed. Accordingly, the number of venules with fibrin clots was counted, and fibrin clotting is given in percent of all venules analyzed.
Immunohistochemistry
For immunohistochemistry tissue slides were deparaffinized, and proteins were unmasked with citrate buffer at a pH of 6. The endogenous peroxidases were blocked with 3 % H2O2 in methanol, and unspecific proteins were blocked with 3 % goat serum.
Cleaved caspase-3 (cysteine-aspartic proteases) as an indicator of apoptotic cell death was used. Five-micrometer sections of paraffin-embedded tumor-bearing liver specimens were incubated overnight at room temperature with a rabbit polyclonal anti-cleaved caspase-3 antibody (1:50, Cell Signaling Technology, Frankfurt, Germany). As secondary antibody, a peroxidase-conjugated goat anti-rabbit IgG antibody (1:100, Dianova, Hamburg, Germany) was used. 3.3′-Diaminobenzidine was used as chromogen. The sections were counterstained with hemalaun. Positively stained cells were counted in 25 high-power fields (HPF) per specimen and are given as number per HPF.
Proliferating cell nuclear antigen (PCNA) served as an indicator of cell proliferation. Five-micrometer sections of paraffin-embedded specimens were incubated for 18 h at 4 °C with a mouse monoclonal anti-PCNA antibody (1:50; Dako, Hamburg, Germany). For development of PCNA, a peroxidase-conjugated goat anti-mouse IgG antibody (1:100; Dianova) was incubated for 30 min. 3.3′-Diaminobenzidine was used as chromogen, and hemalaun was used for counterstaining. Sections were analyzed using a score ranging from 0 to 4 of PCNA-positive cells (0 ≤ 1 %, 1 = 1–10 %, 2 = 10–30 %, 3 = 30–50 %, 4 ≥ 50 % of PCNA-positive cells).
Platelet endothelial cell adhesion molecule-1 (PECAM-1; CD31) served as an indicator for vascularization. For immunohistochemical detection of PECAM-1 expression, a primary mouse anti-rat antibody (1:500; clone TLD-3 A12, Serotec) was used, and a peroxidase-conjugated goat anti-mouse antibody (Dianova) was used as secondary antibody. PECAM-1-positive blood vessels were given as number per HPF (counted in 25 HPF per section).
Statistical analysis
All values are expressed as mean ± SEM. After analysis of the normal distribution of data and homogeneity of variance, differences between the groups were calculated by one-way analysis of variance followed by the Student–Newman–Keuls test. The pairwise comparison was performed by Student’s t test. Overall statistical significance was set at p < 0.05. Statistical analysis was performed with the use of SigmaStat (SPSS, Inc., Chicago, USA).
Results
Binding of cetuximab
Specific in vitro binding experiments using immunocytochemical fluorescence staining showed that cetuximab binds to the surface of CC531 cells (Fig. 1). Quantitative analysis revealed 92.5 ± 0.4 % positively stained cells, indicating a high affinity of cetuximab to the CC531 cells.
In vitro cell viability after cetuximab exposure
After 30-min exposure of CC531 cells to 2,500 and 5,000 μg/ml cetuximab, the WST assay showed a significant reduction of cell viability to ~12 and ~3 % [optical density (OD) 0.034 ± 0.003 and 0.009 ± 0.002] compared to controls (OD 0.283 ± 0.011). Similar results were observed after 1-h exposure (OD 0.086 ± 0.001 and 0.012 ± 0.001 vs 0.446 ± 0.002). Cetuximab concentrations of <1,000 μg/ml did not significantly affect CC531 cell viability.
Metastatic tumor growth and general health conditions
After 10 days of tumor growth, all animals established a solitary tumor in the left liver lobe with a diameter of about 5 to 10 mm. Signs of extrahepatic disease were not observed. Animals were not affected systemically by the malignant process. Analysis of the body weight could not detect a significant difference of weight change from days 0 to 13 between HAI- and SYS-treated animals (Table 1). Of interest, SYS of CE, CE + OX, and OX showed significantly less weight gain compared to SYS Sham. In contrast, after HAI only, OX alone showed a reduced weight gain compared to sham (Table 1).
Table 1.
Body weight change (in percent) from days 0 to 13
| Group | HAI | SYS |
|---|---|---|
| Sham | −2.1 ± 0.4 | +7.3 ± 2.2 |
| CE | +1.2 ± 1.3 | −0.4 ± 1.0* |
| CE + OX | −2.0 ± 1.3 | −4.5 ± 1.2* |
| OX | −6.9 ± 1.9* | −4.3 ± 1.6* |
Weight change from days 0 to 13 in percent of the body weight at day 0. Animals were treated either with hepatic arterial infusion or systemic application of saline (Sham), cetuximab, the combination of cetuximab and oxaliplatin, or oxaliplatin alone. There were no statistically significant differences comparing HAI to SYS. Mean ± SEM
HAI hepatic arterial infusion, SYS systemic application, CE cetuximab, CE + OX combination of cetuximab and oxaliplatin, OX oxaliplatin
*p < 0.05 vs Sham of the corresponding group
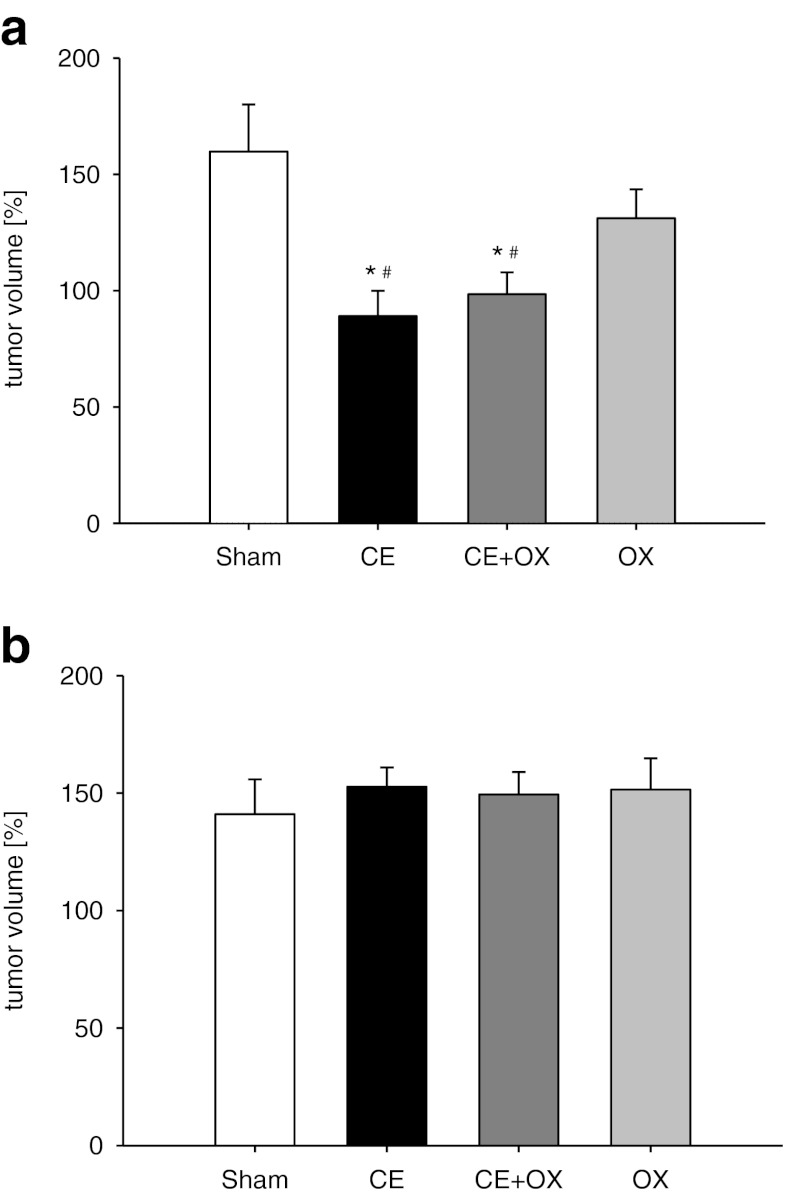
Metastatic tumor growth
From days 10 to 13, tumor size increased by more than 50 % in HAI controls (HAI Sham) and more than 40 % in SYS controls (SYS Sham) without significant difference when comparing the two groups (Fig. 2). Oxaliplatin given as monotherapy via HAI (HAI OX) showed a slight but not significant inhibition of tumor growth compared to HAI sham (Fig. 2), whereas SYS OX did not show any effect (Fig. 2). Of interest, HAI of cetuximab alone (HAI CE) or in combination with oxaliplatin (HAI CE + OX) significantly inhibited tumor growth compared to HAI sham and the corresponding SYS groups (Fig. 2).
Fig. 2.
a, b The tumor volume at day 13 in percent of the volume measured at day 10 after HAI (a) and SYS (b) of cetuximab (CE), oxaliplatin (OX), or the combination of both (CE + OX). Animals undergoing HAI or SYS with saline served as controls (Sham). Data are given as mean ± SEM; *p < 0.05 vs Sham; # p < 0.05 vs corresponding SYS
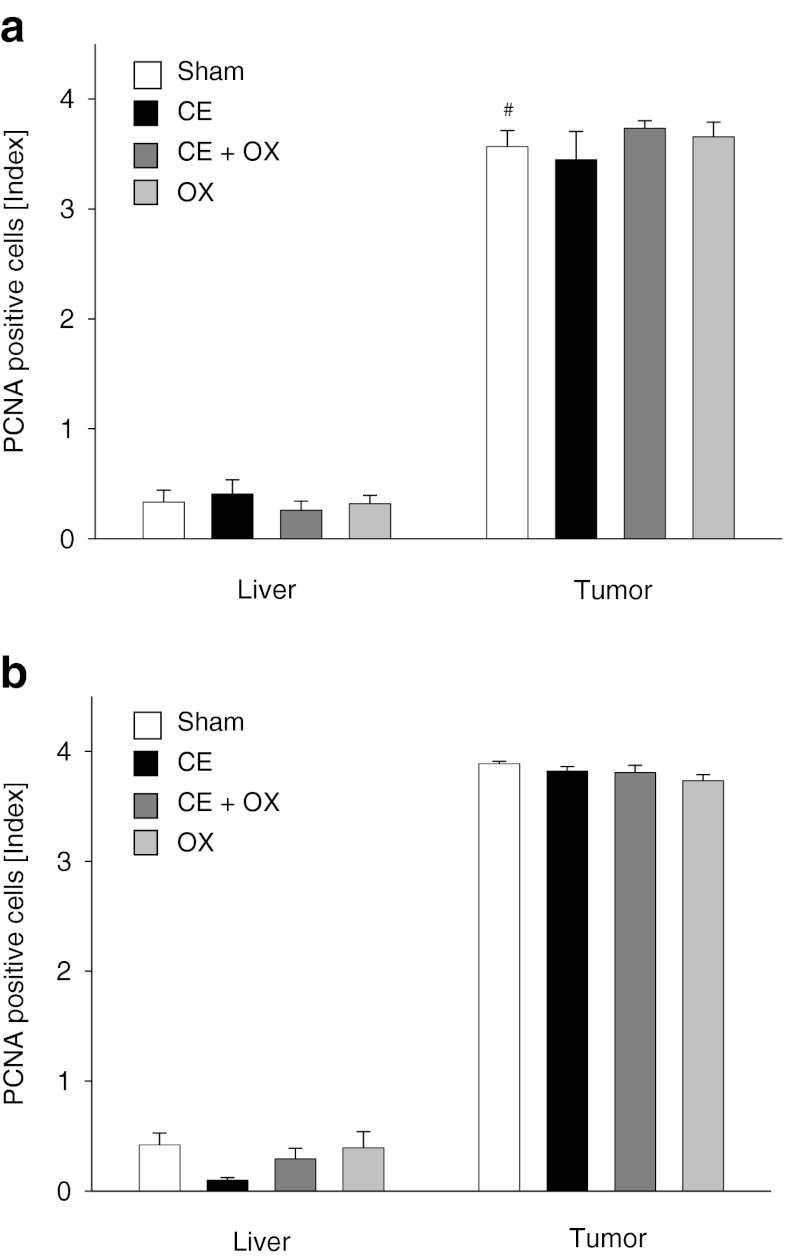
Tumor cell proliferation
In all groups, tumors showed a high proliferation rate as measured by PCNA-positive immunohistochemistry. There was no substantial difference in tumor cell proliferation between HAI- and SYS-treated animals (Fig. 3). The proliferation rate within the surrounding liver tissue was significantly lower compared to the tumor tissue. However, there were also no differences between the groups (Fig. 3).
Fig. 3.
a, b The data of the immunohistochemical analysis of proliferating nuclear cell antigen (score 0 = <1 %, 1 = 1–10 %, 2 = 10–30 %, 3 = 30–50 %, and 4 ≥ 50 % of PCNA-positive cells) of liver and tumor tissue of animals undergoing HAI (a) or SYS (b) with cetuximab (CE), oxaliplatin (OX), or the combination of both (CE + OX). Animals undergoing HAI or SYS with saline served as controls (Sham). Data are given as mean ± SEM; # p < 0.05 vs corresponding SYS
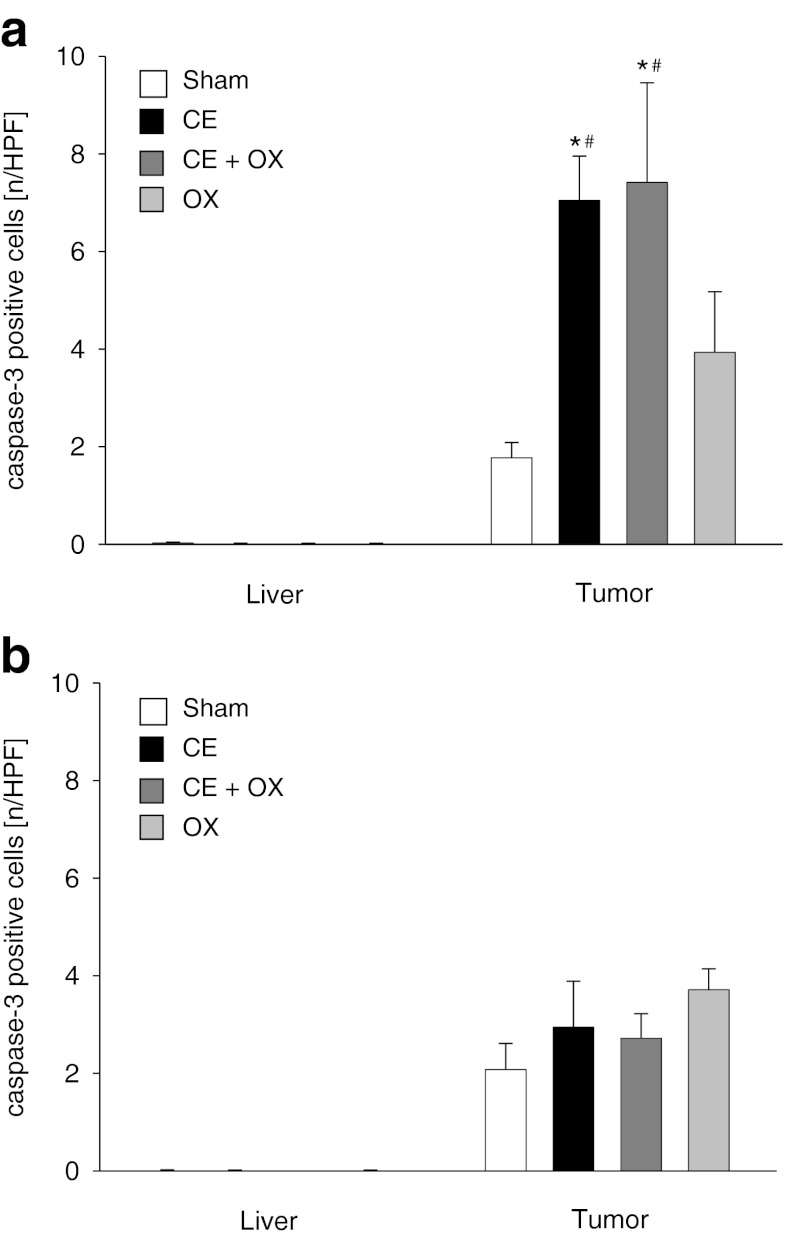
Apoptotic tumor cell death
Apoptotic cell death in the unaffected liver tissue was overall neglectable. Analysis of the number of apoptotic cells in the tumors revealed that sham controls and monotherapy with oxaliplatin did not show any relevant differences between HAI and SYS. Of interest, systemic application of the drugs did not show significant differences compared to SYS Sham (Fig. 4). In contrast, CE and CE + OX via HAI induced a significant three- to fourfold increase of apoptotic cell death compared to both HAI Sham as well as SYS CE and SYS CE + OX (Fig. 4).
Fig. 4.
a, b The quantitative analysis of cleaved caspase-3-positive cells of liver and tumor tissue (given as number per HPF) of animals undergoing HAI (a) or SYS (b) with cetuximab (CE), oxaliplatin (OX), or the combination of both (CE + OX). Animals undergoing HAI or SYS with saline served as controls (Sham). Data are given as mean ± SEM; *p < 0.05 vs Sham; # p < 0.05 vs corresponding SYS
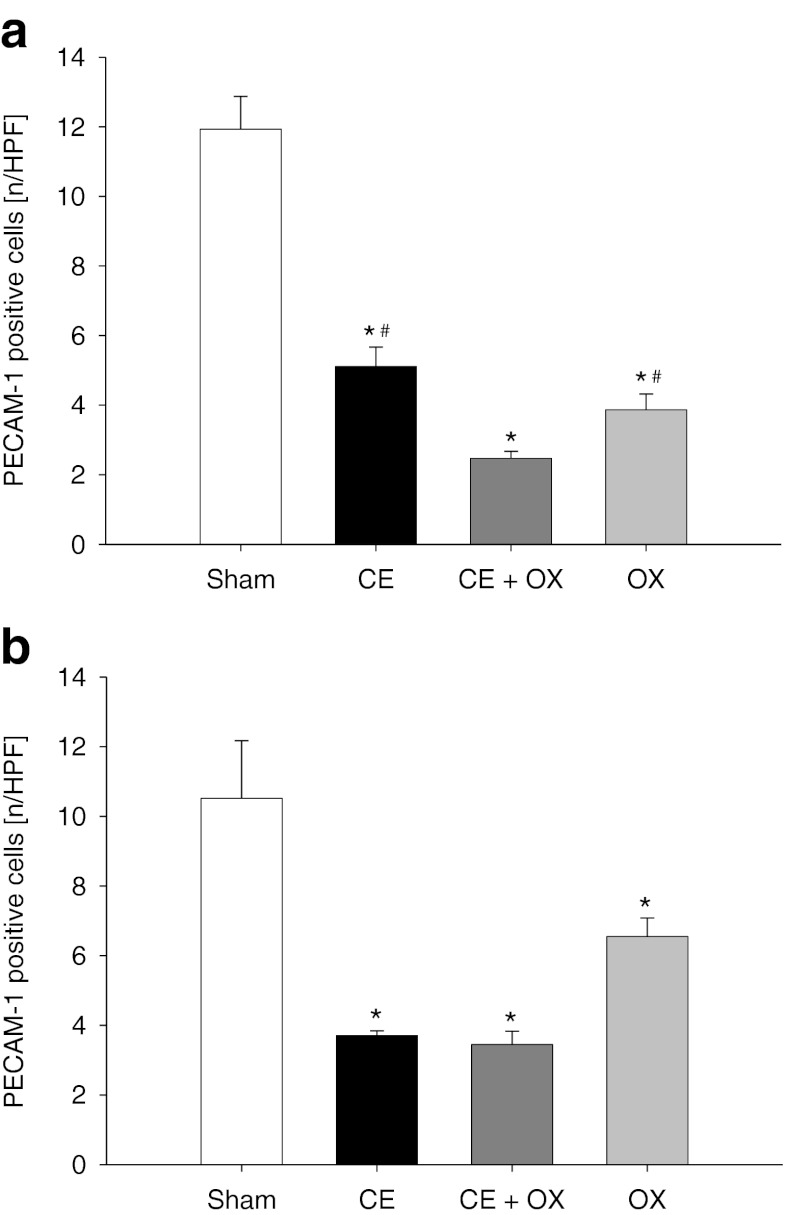
Tumor vascularization
In sham controls, the number of tumor vessels, indicated by PECAM-1-positive cells, was 11.9 ± 0.9 in HAI-treated tumors and 10.5 ± 1.7 per HPF in SYS-treated tumors. SYS OX reduced the number of blood vessels per HPF by about 40 %. HAI OX was even more effective and reduced the number of blood vessels by about 70 % compared to sham control. SYS or HAI of CE and, in particular, HAI CE + OX were also highly effective in reducing the number of tumor blood vessels (Fig. 5).
Fig. 5.
a, b The number of PECAM-1-positive blood vessels per HPF in tumors of animals undergoing HAI (a) or SYS (b) with cetuximab (CE), oxaliplatin (OX), or the combination of both (CE + OX). Animals undergoing HAI or SYS with saline served as controls (Sham). Data are given as mean ± SEM; *p < 0.05 vs Sham; # p < 0.05 vs corresponding SYS
Hepatocellular injury
Analysis of the liver enzymes ASAT and ALAT as indicators of hepatocellular injury at days 10 and 13 did not reveal significant differences between the HAI and SYS groups (data not shown). Analysis of the GLDH activity from days 10 and 13 showed a slight increase after HAI CE + OX and HAI OX (Table 2).
Table 2.
Liver enzyme GLDH (in units per liter) at days 10 and 13
| Group | Day 10 | Day 13 | ||
|---|---|---|---|---|
| HAI | SYS | HAI | SYS | |
| Sham | 22.3 ± 7.1 | 34.3 ± 10.3 | 35.0 ± 5.8 | 22.3 ± 6.5 |
| CE | 49.9 ± 9.7 | 23.2 ± 6.6 | 44.6 ± 8.4 | 22.9 ± 9.8 |
| CE + OX | 24.7 ± 6.4 | 38.6 ± 14.2 | 72.2 ± 5.1 | 20.8 ± 6.9* |
| OX | 30.5 ± 6.2 | 35.2 ± 5.9 | 59.8 ± 34.8 | 15.1 ± 2.9 |
Animals were treated either with hepatic arterial infusion or systemic application of saline (Sham), cetuximab, or oxaliplatin alone or the combination of cetuximab and oxaliplatin. HAI of cetuximab and oxaliplatin led to a significant increase of GLDH from days 10 to 13 compared to the systemic administration form (SYS CE + OX). Mean ± SEM
HAI hepatic arterial infusion, SYS systemic application, CE cetuximab, OX oxaliplatin, CE + OX combination of cetuximab and oxaliplatin, HAI CE + OX HAI of cetuximab and oxaliplatin
*p < 0.05 vs HAI
Histomorphological analysis of hepatocellular vacuolization, endothelial detachment, or vascular fibrin clotting did not reveal relevant differences between HAI and SYS after Sham, OX, CE, and CE + OX treatment (data not shown).
Discussion
The major finding of the present study is that cetuximab via HAI but not via SYS as monotherapy or in combination with oxaliplatin is effective to inhibit tumor growth of colorectal liver metastases in the rat. Colorectal cancer is the second leading cause of cancer death worldwide. About 20 % of the patients show synchronous hepatic metastases, and up to 30 % develop metachronous disease [15]. Therefore, the control of this hepatic disease remains a challenging issue. Systemic chemotherapy is a substantial part of the treatment of colorectal liver metastases. Moreover, hepatic arterial infusion is used in some centers with different results [8–11]. In a recent Cochrane review, Mocellin et al. concluded that the future of HAI seems to be linked to the use of novel anticancer agents or drug combinations [12]. Bouchahda et al. also claimed that the role of HAI should be revisited using modern therapeutic approaches [16]. Thus, HAI is moving again in the focus of scientific interest in clinical and experimental studies and plays an increasing role in the treatment of liver-limited metastatic colorectal cancer [7, 14, 17–19]. HAI, as locoregional chemotherapy, bears the advantage to increase the local concentration of tumoricidal agents within liver metastases. The rationale for HAI is that hepatic metastases receive their nutritive blood supply mostly from the hepatic arterial system, while the hepatic tissue is fed predominantly by the portal venous blood flow [20]. Moreover, whereas the portal vein via the Glisson Trias directly drains into the liver sinusoids, part of the arterial blood at first drains into the peribiliary plexus before entering the sinusoidal system [21]. Tumor vessels of hepatic metastases are supplied by this arterial blood flow [22], which leads to a prolonged exposure time of drugs applied via the arterial system. This probably caused the increased antitumor effect seen after HAI compared to SYS in the present study [23]. Moreover, hepatic arterial drug application can lead to high extraction rates of drugs via the first-pass effect and consecutively less side effects [7]. Therefore, agents with high extraction rates are particularly attractive for HAI. While in former clinical trials, HAI was predominantly performed with floxuridine or 5-FU, newer trials included oxaliplatin with encouraging results [8, 9, 14, 24, 25].
Oxaliplatin, plays a key role in chemotherapy of colorectal cancer because of a large spectrum of anticancer activity together with mild toxicity [26–28]. However, in the present study, a measureable reduction of tumor growth was only seen in animals treated by HAI of cetuximab alone or in combination with oxaliplatin. HAI or SYS of oxaliplatin alone did not inhibit tumor growth in the present liver metastasis model. This is not surprising because, from clinical findings, it is known that oxaliplatin monotherapy exerts only minimal antineoplastic effects [29]. Accordingly, in clinical studies, oxaliplatin is not given as a single drug, but only in combination with other antineoplastic agents [29]. The present study was conducted as a “proof of principle” study, where a single application of the drugs in a short time period was chosen to evaluate whether HAI of the drug in the fast growing CC531 metastases is superior to inhibit tumor growth compared to SYS.
Cetuximab, a novel anticancer agent, is a monoclonal human/murine chimeric anti-epidermal growth factor receptor antibody, who is selectively active in the subpopulation of wild-type K-ras. EGF-R is overexpressed in colorectal cancer and correlates with a poorer prognosis and higher resistance to systemic chemotherapy [30–32]. Deregulation of EGF-R is linked to inhibition of tumor proliferation, invasion, migration, angiogenesis, and resistance to apoptosis [33]. The tumor cell line CC531, which was used in the present study, also expresses the EGF-R on its surface. As shown by the present study, cetuximab binds to EGF-R on the surface of the CC531 tumor cells.
In a preclinical trial, Van Buren et al. demonstrated that, after partial hemihepatectomy, a monoclonal EGF-R antibody had no effect on liver regeneration [34]. This view is in line with the results observed in the present study, where neither HAI nor SYS of cetuximab induced relevant side effects.
In clinical trials, intravenous cetuximab shows its efficacy in the treatment of colorectal liver metastases both as a single agent in second-line treatments as well as in combination with irinotecan- or oxaliplatin-based therapy regimens in first-line treatments [4, 5, 35–38]. Accordingly, today, intravenous application of cetuximab is clinical standard in the treatment of colorectal liver metastases, albeit restricted to wild-type K-ras cases. However, Azzopardi and coworkers claim that these results are still inconclusive. Even in patients with wild-type K-ras an interindividual variability in response to cetuximab is observed [39]. In the present study, systemic application of cetuximab did not inhibit tumor growth. This is most probably due to the fact that the CC531 tumor cell line used exhibits a mutated K-ras gene in codon 12 (GGT to GAT), changing glycine to aspartic acid [40]. This is in line with the results of clinical studies, also demonstrating no significant effect of cetuximab on progression-free survival and overall survival in K-ras-mutated tumors [41]. Therefore, the results of our study are of particular interest because a comparable dose of cetuximab, when given via HAI, was not only capable of inhibiting the growth but also of decreasing the volume of the K-ras-mutated CC531 tumor. These in vivo results are supported by our in vitro analyses, demonstrating that, in high concentrations, cetuximab is capable of significantly reducing CC531 cell viability. Because the application of the mAb by HAI provides an increased concentration, this might explain the unexpected observation of an increased antitumor effect in the present study.
In conclusion, the present study shows that HAI of cetuximab alone or in combination with oxaliplatin is effective to inhibit tumor growth of colorectal liver metastases in the rat, whereas SYS was ineffective. Thus, HAI chemotherapy with cetuximab and oxaliplatin may represent a promising approach in the treatment of colorectal liver metastases.
Acknowledgments
We appreciate the excellent technical assistance of Janine Becker, Ruth Nickels, and Christina Marx.
References
- 1.Harrison S, Benziger H. The molecular biology of colorectal carcinoma and its implications: a review. Surgeon. 2011;9:200–210. doi: 10.1016/j.surge.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey JN, Nagorney DM, McWilliams RR. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27:3677–3683. doi: 10.1200/JCO.2008.20.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seehofer D, Neuhaus P. Current status of multimodal therapy for colorectal liver metastases. Zentralbl Chir. 2011;136:343–351. doi: 10.1055/s-0031-1271579. [DOI] [PubMed] [Google Scholar]
- 4.Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, D’Haens G, Pinter T, Lim R, Bodoky G, Roh JK, Folprecht G, Ruff P, Stroh C, Tejpar S, Schlichting M, Nippgen J, Rougier P. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1408–1417. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 5.Bokemeyer C, Bondarenko I, Makhson A, Hartmann JT, Aparicio J, de Braud F, Donea S, Ludwig H, Schuch G, Stroh C, Loos AH, Zubel A, Koralewski P. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27:663–671. doi: 10.1200/JCO.2008.20.8397. [DOI] [PubMed] [Google Scholar]
- 6.Garufi C, Torsello A, Tumolo S, Ettorre GM, Zeuli M, Campanella C, Vennarecci G, Mottolese M, Sperduti I, Cognetti F. Cetuximab plus chronomodulated irinotecan, 5-fluorouracil, leucovorin and oxaliplatin as neoadjuvant chemotherapy in colorectal liver metastases: POCHER trial. Br J Cancer. 2010;103:1542–1547. doi: 10.1038/sj.bjc.6605940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Power DG, Healey-Bird BR, Kemeny NE. Regional chemotherapy for liver-limited metastatic colorectal cancer. Clin Colorectal Cancer. 2008;7:247–259. doi: 10.3816/CCC.2008.n.032. [DOI] [PubMed] [Google Scholar]
- 8.Boige V, Malka D, Elias D, Castaing M, De Baere T, Goere D, Dromain C, Pocard M, Ducreux M. Hepatic arterial infusion of oxaliplatin and intravenous LV5FU2 in unresectable liver metastases from colorectal cancer after systemic chemotherapy failure. Ann Surg Oncol. 2008;15:219–226. doi: 10.1245/s10434-007-9581-7. [DOI] [PubMed] [Google Scholar]
- 9.Ducreux M, Ychou M, Laplanche A, Gamelin E, Lasser P, Husseini F, Quenet F, Viret F, Jacob JH, Boige V, Elias D, Delperro JR, Luboinski M. Hepatic arterial oxaliplatin infusion plus intravenous chemotherapy in colorectal cancer with inoperable hepatic metastases: a trial of the gastrointestinal group of the Federation Nationale des Centres de Lutte Contre le Cancer. J Clin Oncol. 2005;23:4881–4887. doi: 10.1200/JCO.2005.05.120. [DOI] [PubMed] [Google Scholar]
- 10.Elias D, Goere D, Boige V, Kohneh-Sharhi N, Malka D, Tomasic G, Dromain C, Ducreux M. Outcome of posthepatectomy-missing colorectal liver metastases after complete response to chemotherapy: impact of adjuvant intra-arterial hepatic oxaliplatin. Ann Surg Oncol. 2007;14:3188–3194. doi: 10.1245/s10434-007-9482-9. [DOI] [PubMed] [Google Scholar]
- 11.Kemeny NE, Melendez FD, Capanu M, Paty PB, Fong Y, Schwartz LH, Jarnagin WR, Patel D, D’Angelica M. Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2009;27:3465–3471. doi: 10.1200/JCO.2008.20.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mocellin S, Pasquali S, Nitti D (2009) Fluoropyrimidine-HAI (hepatic arterial infusion) versus systemic chemotherapy (SCT) for unresectable liver metastases from colorectal cancer. Cochrane Database Syst Rev CD007823 [DOI] [PubMed]
- 13.Benedict FG (1934) Die Oberflächenbestimmungen verschiedener Tiergattungen [Determination of body surface area in different animal species]. Ergebnisse der Physiologie und Experimentellen Pharmakologie 36:300–346
- 14.Sperling J, Schafer T, Ziemann C, Benz-Weisser A, Kollmar O, Schilling MK, Menger MD. Hepatic arterial infusion of bevacizumab in combination with oxaliplatin reduces tumor growth in a rat model of colorectal liver metastases. Clin Exp Metastasis. 2012;29(2):91–99. doi: 10.1007/s10585-011-9432-6. [DOI] [PubMed] [Google Scholar]
- 15.Reinacher-Schick AC, Bechstein WO. Colorectal liver metastases. Neoadjuvant chemotherapy: aspects of medical and surgical oncology. Internist. 2007;48:51–58. doi: 10.1007/s00108-006-1770-0. [DOI] [PubMed] [Google Scholar]
- 16.Bouchahda M, Levi F, Adam R, Rougier P. Modern insights into hepatic arterial infusion for liver metastases from colorectal cancer. Eur J Cancer. 2011;47(18):2681–2690. doi: 10.1016/j.ejca.2011.06.037. [DOI] [PubMed] [Google Scholar]
- 17.Bouchahda M, Adam R, Giacchetti S, Castaing D, Brezault-Bonnet C, Hauteville D, Innominato PF, Focan C, Machover D, Levi F. Rescue chemotherapy using multidrug chronomodulated hepatic arterial infusion for patients with heavily pretreated metastatic colorectal cancer. Cancer. 2009;115:4990–4999. doi: 10.1002/cncr.24549. [DOI] [PubMed] [Google Scholar]
- 18.Martin RC, Joshi J, Robbins K, Tomalty D, Bosnjakovik P, Derner M, Padr R, Rocek M, Scupchenko A, Tatum C. Hepatic intra-arterial injection of drug-eluting bead, irinotecan (DEBIRI) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi-institutional study. Ann Surg Oncol. 2011;18:192–198. doi: 10.1245/s10434-010-1288-5. [DOI] [PubMed] [Google Scholar]
- 19.Pohlen U, Buhr HJ, Berger G, Ritz JP, Holmer C. Hepatic arterial infusion (HAI) with PEGylated liposomes containing 5-FU improves tumor control of liver metastases in a rat model. Invest New Drugs. 2011;30(3):927–935. doi: 10.1007/s10637-011-9646-0. [DOI] [PubMed] [Google Scholar]
- 20.Breedis C, Young C. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30:969–985. [PMC free article] [PubMed] [Google Scholar]
- 21.Burkel W. The fine structure of the terminal branches of the hepatic arterial system of the rat. Anat Rec. 1970;167:329–349. doi: 10.1002/ar.1091670307. [DOI] [PubMed] [Google Scholar]
- 22.Gonda T, Ishida H, Yoshinaga K, Sugihara K. Microvasculature of small liver metastases in rats. J Surg Res. 2000;94:43–48. doi: 10.1006/jsre.2000.5978. [DOI] [PubMed] [Google Scholar]
- 23.Okuno K, Hirai N, Lee YS, Tarabar D, Ueno H, Yasutomi M. Superiority of hepatic arterial infusion in preventing catabolism of 5-FU compared with portal vein infusion revealed by an in vivo 19F NMR study. Cancer Chemother Pharmacol. 1998;42:341–344. doi: 10.1007/s002800050827. [DOI] [PubMed] [Google Scholar]
- 24.Del Freo A, Fiorentini G, Sanguinetti F, Muttini MP, Pennucci C, Mambrini A, Pacetti P, Della Seta R, Lombardi M, Torri T, Cantore M. Hepatic arterial chemotherapy with oxaliplatin, folinic acid and 5-fluorouracil in pre-treated patients with liver metastases from colorectal cancer. In Vivo. 2006;20:743–746. [PubMed] [Google Scholar]
- 25.Kern W, Beckert B, Lang N, Stemmler J, Beykirch M, Stein J, Goecke E, Waggershauser T, Braess J, Schalhorn A, Hiddemann W. Phase I and pharmacokinetic study of hepatic arterial infusion with oxaliplatin in combination with folinic acid and 5-fluorouracil in patients with hepatic metastases from colorectal cancer. Ann Oncol. 2001;12:599–603. doi: 10.1023/A:1011186708754. [DOI] [PubMed] [Google Scholar]
- 26.de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000;18:2938–2947. doi: 10.1200/JCO.2000.18.16.2938. [DOI] [PubMed] [Google Scholar]
- 27.Hebbar M, Tournigand C, Lledo G, Mabro M, Andre T, Louvet C, Aparicio T, Flesch M, Varette C, de Gramont A. Phase II trial alternating FOLFOX-6 and FOLFIRI regimens in second-line therapy of patients with metastatic colorectal cancer (FIREFOX study) Cancer Invest. 2006;24:154–159. doi: 10.1080/07357900500524397. [DOI] [PubMed] [Google Scholar]
- 28.Tournigand C, Cervantes A, Figer A, Lledo G, Flesch M, Buyse M, Mineur L, Carola E, Etienne PL, Rivera F, Chirivella I, Perez-Staub N, Louvet C, Andre T, Tabah-Fisch I, de Gramont A. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer—a GERCOR study. J Clin Oncol. 2006;24:394–400. doi: 10.1200/JCO.2005.03.0106. [DOI] [PubMed] [Google Scholar]
- 29.Omura K. Advances in chemotherapy against advanced or metastatic colorectal cancer. Digestion. 2008;77(1):13–22. doi: 10.1159/000111483. [DOI] [PubMed] [Google Scholar]
- 30.Ciardiello F, Tortora G. Epidermal growth factor receptor (EGFR) as a target in cancer therapy: understanding the role of receptor expression and other molecular determinants that could influence the response to anti-EGFR drugs. Eur J Cancer. 2003;39:1348–1354. doi: 10.1016/S0959-8049(03)00235-1. [DOI] [PubMed] [Google Scholar]
- 31.Gross ME, Shazer RL, Agus DB. Targeting the HER-kinase axis in cancer. Semin Oncol. 2004;31:9–20. doi: 10.1053/j.seminoncol.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 32.Ritter CA, Arteaga CL. The epidermal growth factor receptor-tyrosine kinase: a promising therapeutic target in solid tumors. Semin Oncol. 2003;30:3–11. doi: 10.1053/sonc.2003.50027. [DOI] [PubMed] [Google Scholar]
- 33.Ng M, Cunningham D. Cetuximab (Erbitux)—an emerging targeted therapy for epidermal growth factor receptor-expressing tumours. Int J Clin Pract. 2004;58:970–976. doi: 10.1111/j.1368-5031.2004.00369.x. [DOI] [PubMed] [Google Scholar]
- 34.Van Buren G, 2nd, Yang AD, Dallas NA, Gray MJ, Lim SJ, Xia L, Fan F, Somcio R, Wu Y, Hicklin DJ, Ellis LM. Effect of molecular therapeutics on liver regeneration in a murine model. J Clin Oncol. 2008;26:1836–1842. doi: 10.1200/JCO.2007.11.6566. [DOI] [PubMed] [Google Scholar]
- 35.Arnold D, Hohler T, Dittrich C, Lordick F, Seufferlein T, Riemann J, Woll E, Herrmann T, Zubel A, Schmoll HJ. Cetuximab in combination with weekly 5-fluorouracil/folinic acid and oxaliplatin (FUFOX) in untreated patients with advanced colorectal cancer: a phase Ib/II study of the AIO GI Group. Ann Oncol. 2008;19:1442–1449. doi: 10.1093/annonc/mdn150. [DOI] [PubMed] [Google Scholar]
- 36.Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype C, Chau I, Van Cutsem E. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351:337–345. doi: 10.1056/NEJMoa033025. [DOI] [PubMed] [Google Scholar]
- 37.Folprecht G, Lutz MP, Schoffski P, Seufferlein T, Nolting A, Pollert P, Kohne CH. Cetuximab and irinotecan/5-fluorouracil/folinic acid is a safe combination for the first-line treatment of patients with epidermal growth factor receptor expressing metastatic colorectal carcinoma. Ann Oncol. 2006;17:450–456. doi: 10.1093/annonc/mdj084. [DOI] [PubMed] [Google Scholar]
- 38.Lenz HJ, Van Cutsem E, Khambata-Ford S, Mayer RJ, Gold P, Stella P, Mirtsching B, Cohn AL, Pippas AW, Azarnia N, Tsuchihashi Z, Mauro DJ, Rowinsky EK. Multicenter phase II and translational study of cetuximab in metastatic colorectal carcinoma refractory to irinotecan, oxaliplatin, and fluoropyrimidines. J Clin Oncol. 2006;24:4914–4921. doi: 10.1200/JCO.2006.06.7595. [DOI] [PubMed] [Google Scholar]
- 39.Azzopardi N, Lecomte T, Ternant D, Boisdron-Celle M, Piller F, Morel A, Gouilleux-Gruart V, Vignault-Desvignes C, Watier H, Gamelin E, Paintaud G. Cetuximab pharmacokinetics influences progression-free survival of metastatic colorectal cancer patients. Clin Cancer Res. 2011;17(19):6329–6337. doi: 10.1158/1078-0432.CCR-11-1081. [DOI] [PubMed] [Google Scholar]
- 40.van Etten B, ten Hagen TL, de Vries MR, Ambagtsheer G, Huet T, Eggermont AM. Prerequisites for effective adenovirus mediated gene therapy of colorectal liver metastases in the rat using an intracellular neutralizing antibody fragment to p21-Ras. Br J Cancer. 2002;86(3):436–442. doi: 10.1038/sj.bjc.6600089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med Oct. 2008;359(17):1757–1765. doi: 10.1056/NEJMoa0804385. [DOI] [PubMed] [Google Scholar]