Abstract
Background
The principles that guide management of spinal cord injury (SCI) derive from injury resulting from blunt trauma, not gunshot wounds. Civilian gunshot-induced spinal cord injury (CGSWSCI) is a common, potentially serious cause of neurological deficit; there is disagreement about whether the same approaches used for SCI caused by blunt-force trauma should apply to gunshot-induced SCI.
Questions/purposes
We reviewed the literature to answer the following questions regarding presentation and outcome of gunshot wound-induced SCI: (1) Are there differences in recovery prognosis between complete SCI and other patterns of SCI in CGSWSCI. (2) Does the use of steroids improve neurological recovery? (3) Does surgery to remove the bullet affect neurological recovery in CGSWSCI? (4) Does surgery result in an increased risk of complications of treatment?
Methods
We performed a systematic literature review of articles related to civilian gunshot injuries to the spine. Information relating to incidence, pattern of neurological injury, associated injuries, treatment, neurological outcome, and associated complications was extracted. Three independent reviewers assessed the strength of evidence present in the literature by examining quality, quantity, and consistency of results.
Results
A total of 15 articles met the predetermined inclusion criteria. Complete SCIs are associated with the worst functional recovery regardless of treatment. Steroids do not appear to have any added benefit in terms of restoring sensory and motor function. There appears to be some neurologic benefit to surgical decompression with intracanalicular bullet retrieval in patients with an incomplete lesion and a cauda equina syndrome. Complication rates are greater in operated patients.
Conclusions
These findings should be interpreted with caution because of considerable heterogeneity among the studies in the literature on gunshot-induced SCI and because of generally poor-quality study design and a high associated risk of selection bias. Supportive management should be the primary method of care, whereas surgery should be an option in case of radiographic evidence of a static compression on the spinal cord. Future studies are necessary to develop better treatment guidelines for patients with gunshot wound-associated SCI.
Introduction
Traumatic injury caused by firearms is a major cause of morbidity and mortality, especially among persons younger than 44 years of age [3]. Civilian gunshot wound-associated spinal cord injury (CGSWSCI) alone accounts for 13% to 17% of all cases of spinal trauma [1, 6, 9, 10, 21, 25]. Many patients with a CGSWSCI require medical and surgical intervention. Damage to the cord is believed to result from three factors, namely (1) direct impact of the bullet; (2) the concussive effect of bullet impaction; and (3) temporary cavitations. Civilian spinal gunshot wounds (GSWs) are slightly different because these are generally caused by low-velocity (< 1000 ft/second) firearms, which cause damage mainly by a direct mass effect as a result of their low momentum [3]. Although civilian gunshot injuries are increasing in annual incidence, the rate of spinal cord injury (SCI) secondary to civilian GSW has decreased substantially over the last decade compared with prior decades [8]. It is therefore not surprising that the literature regarding CGSWSCI pertains more to military weaponry, because the proportion of these injuries in military personnel or in civilians in war zones far outweighs those in civilians in areas void of such weapons [3]. Additionally, military literature is not applicable to civilian injury as a result of different ballistic characteristics.
Indications for operative intervention have varied over the last 60 years with corresponding swings in the trends for treatment. After reviewing World War I SCIs, the British Medical Research Council concluded that CGSWSCI with progressive neurological deficit was an indication for operative decompression [31]. Later, during World War II, aggressive débridement, decompression, and intradural exploration was the favorable treatment option. Reports of up to 40% neurologic recovery with this management strategy were made; however, no nonoperative control data were available [12, 22, 27]. The accepted indication for operative intervention at the time was an incomplete lesion with static or progressive neurologic deficit and a complete lesion if there was any suspicion of the spinal cord being intact. Over time, this view has been challenged with a continuing debate whether conservative or aggressive management would be favorable.
Management of CGSWSCI centers on restoration of neurological function with prevention and management of gunshot injury-related complications. The treatment options include a decompressive laminectomy procedure, which relieves the pressure on the spinal cord and associated nerve roots [7]. Nonsurgical management involves spinal stabilization with or without steroid treatment to reduce spinal cord inflammation and improve recovery [19]. Current evidence present on the topic in the civilian and military literature is inconclusive regarding efficacy of either a conservative or invasive approach for optimal management of patients with CGSWSCI. Multiple factors like mechanism of injury, vital status, injured spinal level, degree of neurological deficit, and associated injury play a role in determining optimal management [3]. Therefore, it is important to try to develop clear recommendations regarding management of a patient with CGSWSCI.
This systematic review of the CGSWSCI literature was thus undertaken to provide answers to the following questions: (1) Are there differences in recovery prognosis between complete SCI and other patterns of SCI in CGSWSCI? (2) Does the use of steroids improve neurological recovery? (3) Does surgery affect neurological recovery in CGSWSCI? (4) Does surgery result in an increased risk of complications of treatment?
Materials and Methods
We conducted a systematic search of the literature in MedLine, Ovid, and EMBASE library from January 1975 to June 2012 using the Boolean terms “(spine) OR (spinal) AND (gunshot)”. Individual searches of the following journals were undertaken with the same Boolean operators to find articles from 2012 that would be too recent to be found in the databases: The Spine Journal (one article), Spine (zero), Spinal Cord (five), Journal of Spinal Cord Medicine (zero), Archives of Physical Medicine and Rehabilitation (one), Journal of Spinal Disorders & Techniques (one), British Journal of Neurosurgery (two), Injury and Journal of Trauma and Acute Care Surgery (eight). Reference lists of key articles were also systematically searched.
To answer our study questions, we attempted to identify studies specifically designed to evaluate the incidence and pattern of neurological injury after CGSWSCI. We then attempted to identify studies that reported associated complications. Lastly, we attempted to identify studies that examined the role of operative/conservative management on patients with CGSWSCI and reported neurological outcomes of the treatment provided.
Case reports, case series with fewer than 10 patients, articles on CGSWSCI from the military literature, editorials, review articles, case reports, and non-English-written studies were excluded. Articles were also excluded if patients with CGSWSCI were not analyzed separately from those who sustained SCI as a result of a blast or penetrating stab injury. Studies that did not describe the level or severity of SCI, neurological deficit, treatment approach, or neurologic deficit were also excluded.
Three independent reviewers reviewed each article (GSS, VP, AG). Most articles were excluded based on the information provided in the title or the abstract. Articles that could not be excluded unequivocally were identified and excluded only after consensus among the three reviewers. From the included articles, the following data were extracted: study design, number of subjects, mean age and length of followup, sex, SCI severity and spinal level, cord syndromes, associated injuries, operative and nonoperative interventions, complications, and neurological recovery. Level of evidence rating was assigned to each article independently by three reviewers using standard criteria for therapeutic studies [38]. Disagreements were resolved by a consensus among reviewers.
The incidence of neurological injury was reported as a proportion to the total number of patients with CGSWSCI. Neurological incidence rates were determined based on level of injury involved, namely cervical, thoracic, lumbosacral, whether the injury pattern resulted in complete injury or incomplete injury, if there was any bony involvement associated with neurological injury, an associated bullet in the canal, and instability present. Neurological recovery was documented on a nominal scale with the variables being significant or nonsignificant change in neurological outcomes because of different neurological recovery scoring systems used in various studies causing heterogeneity in data collection. Descriptive statistical analysis was performed for the data collected.
To determine the strength of the findings and recommendations of our systematic review, we analyzed the population of studies we included using guidelines proposed by van Tulder et al. [33]. We judged whether the body of literature represented a minimum standard for each of the three domains using the following criteria: for study quality, at least 80% of the studies reported needed to be rated as a level of evidence I or II; for study quantity, at least three published studies were needed, which were adequately powered to answer the study question; and for study consistency, at least 70% of the studies had to have consistent results. The overall strength of the body of literature was expressed in terms of the impact that further research may have on the results. An overall strength of “high” means that further research is very unlikely to change our confidence in the estimate of effect. The overall strength of “moderate” is interpreted as further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. A grade of “low” means that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate, whereas “very low” means that any estimate of effect is very uncertain [16].
Results
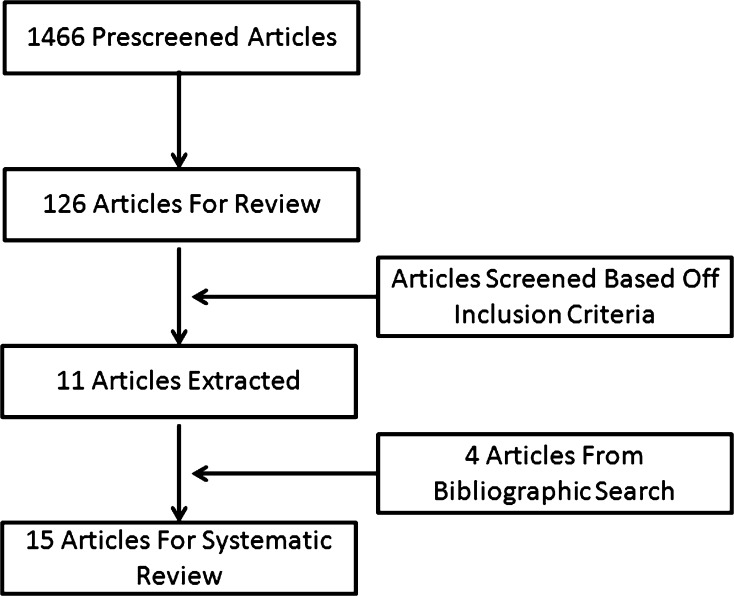
After excluding studies from which we could not extract data regarding isolated CGSWSCIs, we were left with 15 articles (Fig. 1; Table 1).
Fig. 1.
Flowchart demonstrating study selection criteria and the results of literature search.
Table 1.
Summary data of included studies
| Study | Level of evidence | Number of patients | Mean age (years) | Sex (% male) | Mean followup (months) | Severity of SCI | Level of SCI | Cord syndromes (number) | Nonoperative treatment (number) | Operative treatment (number) | Operative interventions (number) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Complete (number) | Incomplete (number) | Cervical (number) | Thoracic (number) | Lumbosacral (number) | ||||||||||
| Aryan et al., 2005 [2] | IV | 60 | 16 | NR | 12 | 34 | 26 | 12 | 31 | 17 | 60 | 0 | Nil | |
| le Roux and Dunn, 2005 [19] | IV | 49 | 28 | 78 | NR | 38 | 8 | 13 | 24 | 12 | NR | 17 | Bullet retrieval (11), stabilization (6) | |
| Heary et al., 1997 [13] | IV | 254 | 26 | 91 | 56 | 190 | 64 | 76 | 116 | 62 | 217 | 37 | Laminectomy (32), stabilization (5) | |
| Isiklar and Lindsey, 1997 [15] | IV | 37 | 28 | 92 | NR | 25 | 11 | 12 | 12 | 13 | 35 | 2 | Laminectomy and bullet retrieval (2) | |
| Levy et al., 1996 [20] | IV | 252 | 26 | 94 | NR | 109 | 143 | 51 | 158 | 43 | 227 | 25 | Laminectomy (16), stabilization (9) | |
| Turgut et al., 1994 [32] | IV | 16 | 29 | 81 | 5 | 7 | 9 | 3 | 8 | 5 | 3 | 13 | Laminectomy and débridement (13) | |
| Robertson et al., 1992 [25] | IV | 30 | 30 | 91 | 6 | 4 | 26 | 0 | 0 | 30 | Cauda equina (30) | 14 | 16 | Laminectomy and débridement (16) |
| Kupcha et al., 1990 [18] | IV | 28 | 32 | 89 | 46 | 21 | 7 | 28 | 0 | 0 | Brown-Sequard (3) | 23 | 5 | Laminectomy and bullet retrieval (3), laminectomy (1), anterior cervical decompression (1) |
| Waters and Adkins, 1991 [35] | III | 90 | 30 | 90 | 12 | 54 | 36 | 19 | 49 | 22 | 58 | 32 | Laminectomy and bullet removal (32) | |
| Cybulski et al., 1989 [7] | IV | 88 | 25 | 94 | NR | 29 | 59 | 0 | 0 | 88 | Conus medullaris (27), cauda equina (61) | 0 | 88 | Laminectomy, bullet fragment retrieval, débridement, and dural closure/graft (88) |
| Simpson et al., 1989 [28] | IV | 142 | 29 | 94 | NR | 94 | 48 | 38 | 77 | 27 | 111 | 31 | Laminectomy (34), bullet retrieval (20), intradural exploration (20) | |
| Benzel et al., 1987 [4] | IV | 35 | 30 | 77 | NR | 20 | 9 | 8 | 13 | 6 | Cauda equina (6) | 22 | 13 | Laminectony and débridement (11), anterior cervical decompression (1), anterior thoracic decompression (1) |
| Six et al., 1979 [29] | IV | 59 | NR | 78 | NR | 29 | 18 | 17 | 30 | 12 | Brown-Sequard (5), cauda equina (12) | 13 | 42 | Laminectomy (39), staged cervical traction and anterior fusion (3) |
| Stauffer et al., 1979 [30] | IV | 185 | NR | 82 | 36 | 106 | 79 | NR | NR | NR | 84 | 101 | Laminectomy (101) | |
| Heiden et al., 1975 [14] | IV | 38 | NR | NR | NR | 25 | 9 | 38 | 0 | 0 | Brown-Sequard (8), anterior cord (1) | 16 | 22 | Laminectomy and débridement (22) |
SCI = spinal cord injury; NR = not reported.
Question 1:
Are there differences in recovery prognosis between complete SCI and other patterns of SCI in CGSWSCI?
Of 15 articles included, a total number of 1363 subjects sustained CGSWSCI with a reported mean age of 27 years in 12 studies and constituting 87% of the male population in 13 studies. The reported rate of a complete lesion after a CGSWSCI ranged from 13% to 78%, whereas the reported rate of an incomplete lesion ranged from 16% to 87%. Complete deficit was reported to be more dependent on spinal injury level, violation of bone architecture by the bullet, and presence of a bullet in the canal. Based on data from 10 studies, CGSWSCI rate at the cervical level was 30% (315 of 1055), at the thoracic level was 49% (518 of 1055), and at the lumbosacral level was 21% (222 of 1055) [13, 17–25]. Of the cervical SCIs, two studies examining gunshot injuries to the cervical spine reported the rate of complete injury to be approximately 70% (46 of 66) [26, 27]. Two studies with data on lumbosacral injuries resulting in cauda equina and conus medullaris syndrome reported a 70% (85 of 121) rate of incomplete injury [6, 12].
Question 2:
Does the use of steroids improve neurological recovery?
Steroid administration was documented in four studies, three of which reported the association with neurological recovery [18, 20, 23]. Overall, no major clinical benefit was demonstrated with steroid administration. One study reported worsening neurological status after steroid administration [23], whereas another study reported increased incidence of complications after steroid administration [18].
Question 3:
Does surgery affect neurological recovery in CGSWSCI?
Surgery for CGSWSCI appeared to improve motor and sensory recovery in the lumbosacral spine, but not in the thoracic or cervical spine (Table 2). [13–15, 18, 20, 25, 28–30]. Studies in which surgery was performed reported weighted rate of neurologic recovery averaging 53% in patients with an incomplete deficit and 21.5% in patients with complete deficit (Fig. 2). Studies evaluating nonoperative management reported a weighted rate of neurologic recovery averaging 65.3% in patients with incomplete deficit and 12.7% in patients with complete deficit. Three studies demonstrated very poor improvement in neurological outcomes for patients with CGSWSCI who had a complete deficit compared with patients with an incomplete deficit irrespective of what treatment was given [28–30]. A few studies [4, 7, 14, 32] reported a favorable surgical outcome for patients who demonstrated radiographic evidence of compression with a progressive neurological deficit. One study [7] reported neurological outcome to be independent of timing of surgery after injury. Another study [2] reported a substantial but nonfunctional improvement in neurological outcome in patients solely treated nonoperatively after 1 year of a CGSWSCI. Neurological outcomes were reported to be similar in the operated group compared with the nonoperative group with an intracanalicular bullet. When looking at purely lumbosacral injuries with cauda equine syndrome, bullet removal was found to have a major effect on neurological recovery, especially when performed immediately and in case of injury resulting in an incomplete deficit [19, 25, 35]. le Roux et al. [19] reported a case of a bullet entering at L3 but was removed from S3. No other case of bullet migration was documented in other selected studies.
Table 2.
Summary of study neurological results stratified by treatment
| Study | Complete spinal cord injury (number) | Incomplete spinal cord injury (number) | Nonoperative treatment (number) | Neurological results (nonoperative) | Operative treatment (number) | Neurological results (operative) | Conclusion |
|---|---|---|---|---|---|---|---|
| Aryan et al., 2005 [2] | 34 | 26 | 60 | Significant (nonfunctional) neurological recovery in all patients: 53 patients autonomous, 19 ambulatory | 0 | In absence of instability, nonoperative care is supported in adolescent patient population | |
| le Roux and Dunn, 2005 [19] | 38 | 8 | NR | Minor recovery in ISCI more than CSCI; no recovery in thoracic CSCI | 11 | Some recovery evident postbullet retrieval from canal, especially if cauda equina involved | Nonoperative care is supported, because it appears that operative intervention does not affect natural history of GSWSCI |
| Heary et al., 1997 [13] | 190 | 64 | 217 | Frankel (≤ 2) grade improvement in 11 patients with ISCI; no improvement in CSCI; no difference with steroid administration | 32 | No statistically significant effect on neurological outcome with operative intervention | Bullet retrieval and operative intervention for CSCI were considered surgical contraindications unless progressive neurological deficit; no demonstrable support for steroid administration |
| Isiklar and Lindsey, 1997 [15] | 25 | 11 | 35 | Frankel (≤ 2) grade improvement in 3 of 23 patients with CSCI and 3 of 9 patients with ISCI | 2 | Frankel (≤ 2) grade improvement in 1 of 2 patients with CSCI and 0 of 2 patients with ISCI | Extent and level of initial neurologic injury are most important determinants of outcome; complete thoracic lesions fair worse; no demonstrable support for operative intervention |
| Levy et al., 1996 [20] | 130 | 106 | 227 | Frankel (≤ 3) grade improvement in 9 of 130 patients with CSCI and 24 of 106 patients with ISCI; no difference with steroid administration | 16 | Neurologic outcome of operative patients not quantified | Neurologic deficit at admission was most predictive of recovery; no demonstrable support for steroid administration, although no increased rate of complications in the treatment group |
| Turgut et al., 1994 [32] | 7 | 9 | 3 | No neurological recovery in 2 patients with CSCI and 1 patient with ISCI | 13 | Neurologic improvement in 4 of 5 patients with CSCI and 9 of 9 patients with ISCI | Operative intervention is mainstay of treatment for intracanalicular bullets |
| Robertson et al., 1992 [25] | 4 | 26 | 14 | No improvement in patient with 1 CSCI; 9 of 13 patients with ISCI improved and 4 of 13 had no change in neurologic status | 16 | Neurologic improvement in 3 of 3 patients with CSCI and 7 of 14 patients with ISCI; no change in neurologic status in 5 of 14 patients with ISCI and 1 worsened | Operative decompression of cauda equina did not alter early neurologic outcome, but may influence sensory more than motor recovery, thus benefitting patients with radicular pain as a result of neural compression; there may be an increased risk of complications with early surgery |
| Kupcha et al., 1990 [18] | 21 | 7 | 23 | Neurologic improvement in 9 of 18 patients with CSCI, 3 of 5 patients with ISCI, and 4 of 7 patients with retained intracanalicular bullets | 5 | Neurologic improvement in 2 of 3 patients with CSCI, 1 of 2 patients with ISCI, and 2 of 3 patients who had intracanalicular bullets retrieved | Surgical decompression did not improve neurologic recovery in patients with CSCI or ISCI, and recovery was not affected by retained intracanalicular bullet fragments |
| Waters and Adkins, 1991 [35] | 54 | 36 | 58 | Mean ASIA motor index score improved 2.1 points in 32 patients with CSCI and 11.4 points in 10 patients with ISCI | 32 | Mean ASIA motor index scores improved 6.5 points in 11 patients with CSCI and 13.8 points in 13 patients with ISCI | Bullet fragment removal made no major difference to pain reduction or recovery of sensation, but did improve motor recovery in patients with lesions between T12 and L4 |
| Cybulski et al., 1989 [7] | 29 | 59 | 0 | 88 | Neurologic improvement in 12 of 29 patients with CSCI and 19 of 46 patients with ISCI | Débridement and decompression recommended to enhance neurologic recovery while mitigating arachnoiditis, infection, and pain syndromes | |
| Simpson et al., 1989 [28] | 94 | 48 | 111 | Neurologic improvement in 12 of 80 patients with CSCI and 26 of 43 patients with ISCI | 31 | Neurologic improvement in 3 of 18 patients with CSCI and 8 of 19 patients with ISCI | No statistically significant difference in neurological outcome whether or not operative intervention was undertaken; higher incidence of complications with operative intervention |
| Benzel et al., 1987 [4] | 20 | 9 | 22 | No neurologic improvement in 17 patients with CSCI, neurologic improvement in 4 of 5 patients with ISCI | 13 | Neurologic improvement in 3 of 3 patients with CSCI and 10 of 10 patients with ISCI | Surgical decompression is recommended in patients with ISCI to improve radicular or myelopathic symptoms secondary to neural compression as evidenced by myelography |
| Six et al., 1979 [29] | 29 | 18 | 13 | Neurologic improvement in 1 of 6 patients with CSCI and 10 of 10 patients with ISCI | 39 | Neurologic improvement in 2 of 23 patients with CSCI, 8 of 8 patients with ISCI, and 8 of 12 patients with incomplete cauda equina syndrome | No major difference in the outcome between patients treated operatively and those treated conservatively; complete lesions portend worse functional recovery |
| Stauffer et al., 1979 [30] | 106 | 79 | 84 | Neurologic improvement in 1 of 56 patients with CSCI and 32 of 45 patients with ISCI | 101 | No neurologic improvement in 50 patients with CSCI, neurologic improvement in 26 of 34 patients with ISCI | Insufficient data regarding retained bullets; CSCIs are irreversible and ISCIs may recover partly or completely regardless of operative intervention |
| Heiden et al., 1975 [14] | 25 | 9 | 16 | Return of function in one or two cervical roots in some patients with CSCI, neurologic improvement in 4 of 6 patients with ISCI | 22 | Return of function in one or two cervical roots in some patients with ISCI, neurologic improvement in 3 of 3 patients with ISCI | No major difference in neurologic recovery with operative intervention in both CSCI and ISCI; operative intervention warranted if progressive neurological deficit |
CSCI = complete spinal cord injury; ISCI = incomplete spinal cord injury; GSWSCI = gunshot wound-induced spinal cord injury; ASIA = American Spinal Injury Association; NR = not reported.
Fig. 2.
Number of patients receiving operative versus nonoperative treatment for citations regarding a CGSWSCI by date of publication.
Question 4:
Does surgery result in an increased risk of complications of treatment?
Abdominal visceral injuries and hemopneumothoraces were the most common associated injuries with incidences of 24% and 20%, respectively (Table 3). The most common complications reported included neurogenic bladder (23 of 35 patients), urinary tract infections (20 of 64 patients), and chronic pain (seven of 26 patients) (Table 4). Complication rates were greater in the operative group of patients. For cervical spine injuries, Kupcha et al. [18] found no advantage to routine neck exploration for cervical spine CGSWSCI . Cybulski et al. [7] reported development of arachnoid adhesions (15%) and occult abscesses (17%) when decompression was delayed for greater than 2 weeks. Surgical indication for complications was required for late sequelae such as development of syringohydromelia, thecal migration of bullet fragments, and prolonged intractable pain. The overall strength of evidence for an effective recommendation with respect to all three questions is very low; that is, any estimate of effect is very uncertain (Table 5).
Table 3.
Overall incidence of reported associated injuries
| Associated injury | Incidence |
|---|---|
| Abdominal viscera | 23.7% (54/228) |
| Hemopneumothorax | 20.0% (17/86) |
| Vascular injury | 15.1% (13/86) |
| Pneumothorax | 12.0% (17/142) |
| Brachial plexus | 8.2% (4/49) |
| Esophagus | 6.1% (3/49) |
| Diaphragm | 5.4% (2/37) |
| Thoracic viscera | 4.2% (6/142) |
| Trachea | 4.1% (2/49) |
| Arteriovenous fistula | 2.6% (1/38) |
| Phrenic nerve damage | 15.4% (4/26) |
| Recurrent laryngeal nerve damage | 11.5% (3/26) |
Table 4.
Overall incidence of reported complications
| Complication | Incidence |
|---|---|
| Neurogenic bladder | 66.0% (23/35) |
| Cystitis/pyelonephritis | 31.2% (20/64) |
| Chronic pain | 27.0% (7/26) |
| Acute respiratory distress syndrome | 19.2% (5/26) |
| Autonomic dysreflexia | 19.2% (5/26) |
| Pneumonia | 13.3% (15/113) |
| Cutaneous fistula | 11.5% (3/26) |
| Central pain syndrome | 8.6% (3/35) |
| Posttraumatic syrinx | 7.7% (2/26) |
| Pyogenic discitis | 6.1% (3/49) |
| Deep venous thrombosis | 5.4% (14/260) |
| Spinal instability | 4.0% (13/325) |
| Wound infection | 4.0% (15/375) |
| Cellulitis | 3.8% (1/26) |
| Wound devitalization | 3.8% (1/26) |
| Brachial plexopathy | 3.8% (1/26) |
| Pleural effusion | 3.8% (1/26) |
| Cerebrospinal fluid fistula | 3.6% (12/334) |
| Pulmonary embolism | 3.1% (2/64) |
| Colonic perforation with abdominal sepsis | 2.7% (1/37) |
| Arachnoiditis | 2.6% (1/38) |
| Gastrointestinal hemorrhage | 2.6% (1/38) |
| Meningitis | 2.5% (5/198) |
| Sepsis | 2.5% (3/122) |
| Pseudomeningocele | 0.62% (1/160) |
Table 5.
Rating of overall strength of evidence
| Question | Strength of evidence | Conclusion | Quality | Quantity | Consistency |
|---|---|---|---|---|---|
| Are there differences in recovery prognosis between complete SCI and other patterns of SCI in CGSWSCI? | Very low | Initial complete deficit results in poor outcome regardless of intervention | No | Yes | No |
| Does the use of steroids improve neurological recovery? | Low | Steroid administration causes no additional benefit to neurological outcomes | No | Yes | Yes |
| Does surgery affect neurological recovery in CGSWSCI? | Low | Surgery for bullet removal does not improve outcomes except for lower lumbosacral cauda equine injuries | No | Yes | Yes |
| Very low | No significant difference is present between operative and nonoperative management CGSWSCI? | No | Yes | No | |
| Does surgery result in an increased risk of complications of treatment? | Low | Common complications include neurogenic bladder, urinary tract infection, and chronic pain | No | Yes | Yes |
| Very low | Surgery results in increased postoperative complications | No | Yes | No |
SCI = spinal cord injury; CGSWSCI = civilian gunshot-induced spinal cord injury.
Discussion
Management of acute SCI resulting from civilian firearms is complicated. Guidelines for managing SCI are derived from blunt force trauma, and so they may or may not apply to GSWSCI. Using the appropriate intervention that provides the best results is essential for achieving overall functional recovery of the patient. We therefore systematically reviewed the literature to determine: (1) Are there differences in recovery prognosis between complete SCI and other patterns of SCI in CGSWSCI? (2) Does the use of steroids improve neurological recovery? (3) Does surgery affect neurological recovery in CGSWSCI? (4) Does surgery result in an increased risk of complications of treatment?
The results of our specific review article are subject to a number of limitations. First, the 14 level IV studies and one level III study assigned based on level of evidence guidelines [38] do not adequately describe the general population of civilian firearm SCIs. All studies had a relatively small sample size, heterogeneous study design, and methodological flaws. Inclusion criteria of articles studied were sometimes directed toward a certain subset of the whole patient population, which could have resulted in a high degree of selection bias. Absence of a control group in most studies, lack of adjustment for confounding variables, along with combining the heterogeneous data of such studies in a systematic review introduced measurement bias. Similarly, assessment of neurological status was not uniformly performed in the included studies. Some studies defined recovery as improved American Spinal Injury Association (ASIA) or Frankel grades or ASIA motor/sensation numerical indices; others vaguely defined recovery as improved sensation or motor function. This resulted in greater subjectivity along with a loss of specificity regarding the diagnosis while distorting reported outcomes. All studies reported neurological recovery as the basis of a successful outcome. No study reported functional outcomes using different validated outcome measure questionnaires. Also, the rationale for a specific intervention often was unclear as commonly is the case in retrospective studies. Associated injuries that were not reported or addressed during an intervention might have added additional bias. Lastly, there was considerable heterogeneity in the literature. However, a more restrictive methodology on our part (for example, excluding level IV studies) would have left little, if any, literature to summarize.
Overall, in our review, we report complete SCIs after a CGSWSCI to portend the worst functional recovery. In our review of 15 studies, thoracic level of injury was the most common spinal level involved. Cervical injuries appeared to have a greater chance of resulting in a complete deficit compared with incomplete injuries. Rhee et al. [24] in a retrospective review comparing penetrating and blunt trauma to the cervical spine reported a neurological deficit presenting from a penetrating injury to be permanent and directly dependent on the mechanism of injury. Initial complete deficit in our review demonstrated a poor prognosis. Studies by Waters et al. [36, 37] with a 1-year followup of patients with traumatic SCI reported motor recovery to be substantially dependent on the initial level and degree of injury and not mechanism of injury or treatment. Another study reported the odds of paralysis among patients with a fragment in the spinal canal to be 12.99 times that of those without any fragment in the canal [6].
Studies in our review reported no significant benefit of the role of steroid administration after CGSWSCI and improvement in neurological deficit. A recent Cochrane review determined steroids to improve recovery in patients with acute SCI when given within 8 hours of injury, and the initial deficit was minimal [5]. However, GSW injury-related patient data were excluded from the review. Anecdotally, we believe that steroids may improve neurological outcome in those patients with CGSWSCI who present with initial minimal neurological deficit and the injury is the result of a concussive effect of the bullet rather than a compressive effect.
Our review concluded that operative intervention has no major benefit for improvement of neurological deficit after CGSWSCI.
However, there may be subgroups of patients with a CGSWSCI who might benefit from surgery. Despite no clear consensus on the appropriate indication for surgery in such patients in our review, studies suggested that patients whose neurological deficit was progressive who also had radiographic evidence of static compression indeed benefitted from a decompressive procedure [4, 7, 14]. This may have been from the presence of a bullet in the canal, bony material, expanding hematoma, or resultant mechanical instability. Gunshot wounds resulting in spinal column instability are different from blunt force spinal trauma because, in most gunshot injury cases, the posterior ligamentous complex remains intact despite anterior column destruction [37]. Different scoring systems were used in our selected studies to determine spinal stability [2, 15, 19]. However, no consensus exists on how to classify spinal instability after CGSWSCI. Lastly, if surgery is being considered, repeat imaging before taking the patient to the operating room is necessary because reports exist documenting migration of the bullet down the spinal canal [11, 23].
Increased incidence of an associated bowel perforation was reported in our review. Many studies, which did not meet our inclusion criteria, reported improved outcomes on nonoperative management of an abdominal spinal wound with 2-week parenteral antibiotic coverage even if there are retained bullet fragments in the spinal canal [16, 17, 26, 34].
In summary, we believe there may be some neurologic benefit to surgical decompression in patients with a progressive incomplete lesion and evidence of radiographic compression. However, complication rates are greater in operated patients. Similarly, there is no convincing evidence supporting the use of steroids in CGSWSCI. Larger, prospective studies with a matched cohort group are required to develop stronger recommendations for the management of these patients. The challenge here is the diversity of injury patterns in CGSWSCI, which makes crafting tight inclusion and exclusion criteria and performing a rigorous, controlled study difficult.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at the Rothman Institute & Thomas Jefferson University Hospital, Philadelphia, PA, USA
References
- 1.Aarabi B, Alibaii E, Taghipur M, Kamgarpur A. Comparative study of functional recovery for surgically explored and conservatively managed spinal cord missile injuries. Neurosurgery. 1996;39:1133–1140. doi: 10.1097/00006123-199612000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Aryan HE, Amar AP, Ozgur BM, Levy ML. Gunshot wounds to the spine in adolescents. Neurosurgery. 2005;57:748–752; discussion 748–752. [DOI] [PubMed]
- 3.Bartlett CS. Clinical update: gunshot wound ballistics. Clin Orthop Relat Res. 2003;408:28–57. doi: 10.1097/00003086-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Benzel EC, Hadden TA, Coleman JE. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20:281–285. doi: 10.1227/00006123-198702000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Bracken MB. Steroids for acute spinal cord injury. Cochrane Database Syst Rev. 2012;1:CD001046. [DOI] [PMC free article] [PubMed]
- 6.Chittiboina P, Banerjee AD, Zhang S, Caldito G, Nanda A, Willis BK. How bullet trajectory affects outcomes of civilian gunshot injury to the spine. J Clin Neurosci. 2011;18:1630–1633. doi: 10.1016/j.jocn.2011.02.047. [DOI] [PubMed] [Google Scholar]
- 7.Cybulski GR, Stone JL, Kant R. Outcome of laminectomy for civilian gunshot injuries of the terminal spinal cord and cauda equina: review of 88 cases. Neurosurgery. 1989;24:392–397. doi: 10.1227/00006123-198903000-00014. [DOI] [PubMed] [Google Scholar]
- 8.DeVivo MJ, Go BK, Jackson AB. Overview of the national spinal cord injury statistical center database. J Spinal Cord Med. 2002;25:335–338. doi: 10.1080/10790268.2002.11753637. [DOI] [PubMed] [Google Scholar]
- 9.Farmer JC, Vaccaro AR, Balderston RA, Albert TJ, Cotler J. The changing nature of admissions to a spinal cord injury center: violence on the rise. J Spinal Disord. 1998;11:400–403. [PubMed] [Google Scholar]
- 10.Gentleman D, Harrington M. Penetrating injury of the spinal cord. Injury. 1984;16:7–8. doi: 10.1016/0020-1383(84)90101-3. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S, Senger RL. Wandering intraspinal bullet. Br J Neurosurg. 1999;13:606–607. doi: 10.1080/02688699943880. [DOI] [PubMed] [Google Scholar]
- 12.Haynes WG. Acute war wounds of the spinal cord. Am J Surg. 1946;72:424–433. doi: 10.1016/0002-9610(46)90332-7. [DOI] [PubMed] [Google Scholar]
- 13.Heary RF, Vaccaro AR, Mesa JJ, Northrup BE, Albert TJ, Balderston RA, Cotler JM. Steroids and gunshot wounds to the spine. Neurosurgery. 1997;41:576–583; discussion 583–584. [DOI] [PubMed]
- 14.Heiden JS, Weiss MH, Rosenberg AW, Kurze T, Apuzzo ML. Penetrating gunshot wounds of the cervical spine in civilians. Review of 38 cases. J Neurosurg. 1975;42:575–579. doi: 10.3171/jns.1975.42.5.0575. [DOI] [PubMed] [Google Scholar]
- 15.Isiklar ZU, Lindsey RW. Low-velocity civilian gunshot wounds of the spine. Orthopedics. 1997;20:967–972. doi: 10.3928/0147-7447-19971001-14. [DOI] [PubMed] [Google Scholar]
- 16.Kihtir T, Ivatury RR, Simon R, Stahl WM. Management of transperitoneal gunshot wounds of the spine. J Trauma. 1991;31:1579–1583. doi: 10.1097/00005373-199112000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Wood GW, 2nd, Whittle AP. Low-velocity gunshot injuries of the spine with abdominal viscus trauma. J Orthop Trauma. 1998;12:514–517. doi: 10.1097/00005131-199809000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Kupcha PC, An HS, Cotler JM. Gunshot wounds to the cervical spine. Spine. 1990;15:1058–1063. doi: 10.1097/00007632-199015100-00014. [DOI] [PubMed] [Google Scholar]
- 19.le Roux JC, Dunn RN. Gunshot injuries of the spine—a review of 49 cases managed at the Groote Schuur Acute Spinal Cord Injury Unit. South Afr J Surg. 2005;43:165–168. [PubMed] [Google Scholar]
- 20.Levy ML, Gans W, Wijesinghe HS, SooHoo WE, Adkins RH, Stillerman CB. Use of methylprednisolone as an adjunct in the management of patients with penetrating spinal cord injury: outcome analysis. Neurosurgery. 1996;39:1141–1148; discussion 1148–1149. [DOI] [PubMed]
- 21.Lin SS, Vaccaro AR, Reisch S, Devine M, Cotler JM. Low-velocity gunshot wounds to the spine with an associated transperitoneal injury. J Spinal Disord. 1995;8:136–144. [PubMed] [Google Scholar]
- 22.Matson DD. Treatment of compound spine injuries in forward Army hospitals. J Neurosurg. 1946;3:114–119. doi: 10.3171/jns.1946.3.2.0114. [DOI] [PubMed] [Google Scholar]
- 23.Oktem IS, Selcuklu A, Kurtsoy A, Kavuncu IA, Pasaoglu A. Migration of bullet in the spinal canal: a case report. Surg Neurol. 1995;44:548–550. doi: 10.1016/0090-3019(95)00212-X. [DOI] [PubMed] [Google Scholar]
- 24.Rhee P, Kuncir EJ, Johnson L, Brown C, Velmahos G, Martin M, Wang D, Salim A, Doucet J, Kennedy S, Demetriades D. Cervical spine injury is highly dependent on the mechanism of injury following blunt and penetrating assault. J Trauma. 2006;61:1166–1170. doi: 10.1097/01.ta.0000188163.52226.97. [DOI] [PubMed] [Google Scholar]
- 25.Robertson DP, Simpson RK. Penetrating injuries restricted to the cauda equina: a retrospective review. Neurosurgery. 1992;31:265–269; discussion 269–270. [DOI] [PubMed]
- 26.Romanick PC, Smith TK, Kopaniky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am. 1985;67:1195–1201. [PubMed] [Google Scholar]
- 27.Schneider RC, Webster JE, Lofstrom JE. A follow-up report of spinal cord injuries in a group of World War II patients. J Neurosurg. 1949;6:118–126. doi: 10.3171/jns.1949.6.2.0118. [DOI] [PubMed] [Google Scholar]
- 28.Simpson RK, Jr, Venger BH, Narayan RK. Treatment of acute penetrating injuries of the spine: a retrospective analysis. J Trauma. 1989;29:42–46. [PubMed] [Google Scholar]
- 29.Six E, Alexander E, Jr, Kelly DL, Jr, Davis CH, Jr, McWhorter JM. Gunshot wounds to the spinal cord. South Med J. 1979;72:699–702. doi: 10.1097/00007611-197906000-00020. [DOI] [PubMed] [Google Scholar]
- 30.Stauffer ES, Wood RW, Kelly EG. Gunshot wounds of the spine: the effects of laminectomy. J Bone Joint Surg Am. 1979;61:389–392. [PubMed] [Google Scholar]
- 31.Tinsley M. Compound injuries of the spinal cord. J Neurosurg. 1946;3:306–309. doi: 10.3171/jns.1946.3.4.0306. [DOI] [PubMed] [Google Scholar]
- 32.Turgut M, Ozcan OE, Gucay O, Saglam S. Civilian penetrating spinal firearm injuries of the spine. Results of surgical treatment with special attention to factors determining prognosis. Arch Orthop Trauma Surg. 1994;113:290–293. doi: 10.1007/BF00443820. [DOI] [PubMed] [Google Scholar]
- 33.van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine. 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 34.Velmahos G, Demetriades D. Gunshot wounds of the spine: should retained bullets be removed to prevent infection? Ann R Coll Surg Engl. 1994;76:85–87. [PMC free article] [PubMed] [Google Scholar]
- 35.Waters RL, Adkins RH. The effects of removal of bullet fragments retained in the spinal canal. A collaborative study by the National Spinal Cord Injury Model Systems. Spine. 1991;16:934–939. doi: 10.1097/00007632-199108000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Waters RL, Adkins RH, Yakura J, Sie I. Profiles of spinal cord injury and recovery after gunshot injury. Clin Orthop Relat Res. 1991;267:14–21. [PubMed] [Google Scholar]
- 37.Waters RL, Sie IH. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:120–125. doi: 10.1097/00003086-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–3. doi: 10.1302/0301-620X.85B1.14063. [DOI] [PubMed] [Google Scholar]