Abstract
Introduction Preserving cranial nerve (CN) function during tumor removal at the jugular foramen is challenging. No anatomical study has better defined the relevant dural septations on the inner surface of the jugular foramen. This study was undertaken to elucidate this anatomy.
Methods Fourteen cadaveric heads (28 sides) were dissected, and relationships of the meningeal coverings of the jugular foramen and adjacent CNs documented. A classification scheme was created to better describe the dural septations of the inner surface of the jugular foramen.
Results Four types of dural septations were noted. Type I: 10 sides (36%) where a dural septation was seen between CNs IX anteriorly and X and XI posteriorly. Of these, the septum was ossified in 20%. Type II (32%) was defined as a jugular foramen with no dural septation. Type III (7%) was defined as septation between CNs IX and X anteriorly and XI posteriorly. Type IV (7 sides, 25%) or the chaotic form was defined as multiple septations within the jugular foramen that housed and divided CN rootlets.
Conclusions The dural septations defined here can be used in future studies to help correlate operative strategy to meningeal morphology within the jugular foramen.
Keywords: skull base, posterior fossa, cranial anatomy, meninges, jugular foramen, anatomy
Introduction
The jugular foramen is a canal between the occipital bone and the inferior and medial portion of the petrous pyramid of the temporal bone. It is an important route for arterial, venous, and nervous structures through the base of the skull. The dura mater at the inner aperture of the foramen forms a distinct compartment for housing the various venous structures and cranial nerves (CNs). These dural relationships are of potential interest in surgical treatment of various intrinsic and extrinsic lesions including paragangliomas, nerve sheath tumors, meningiomas, chordomas, chondrosarcomas, and other rare pathologic processes at the level of this foramen.
Preserving lower CN function when operating on jugular foramen schwannomas is very difficult. At the entrance into the pars nervosa of the jugular foramen, the lower CNs penetrate a thin periosteal layer where they are wrapped with perineurium, making their identification difficult even with operating room microscopy.1 The jugular foramen is often divided into an anteromedial nervous compartment and a posterolateral venous compartment. Through the jugular foramen, the glossopharyngeal, vagus, and accessory nerves extend within a sheath of connective tissue encompassing the dura mater to the pericranium. The inferior petrosal sinus or the glossopharyngeal nerve can either run together or each may run through its own bony canal.1
To date, no detailed anatomical study has been performed to better define the dural septations of the inner surface of the jugular foramen. Therefore, we undertook the following study in an attempt to elucidate this anatomy. Furthermore, such elucidation could assist the neurosurgeon during manipulation of the nerves entering the jugular foramen.
Materials and Methods
For the present study, we used 14 adult formalin-fixed cadaveric heads (28 sides). These specimens were derived from eight male and six female cadavers with an average age at death of 69 years (range: 38–88 years). In the prone position, large left and right retrosigmoid craniectomies were performed, and the dura mater was widely opened. Once the lower CNs were identified under magnification with an operating microscope (Zeiss Meditec, Germany), the nerves of the jugular foramen were transected as close to the brainstem and spinal cord as possible. Next, the tentorium cerebelli was excised along its petrous attachments, the spinal cord and midbrain transected, and the hindbrain removed. Under magnification, we reviewed the relationships of the meningeal coverings of the jugular foramen to the intraforaminal contents. Furthermore, a classification scheme was created to better describe the meningeal relationships of the jugular foramen. Random samples were submitted for hematoxylin and eosin staining to confirm their meningeal nature. Measurements of the length of the septations were made with microcalipers (Mitutoyo, Japan). Statistical analysis was performed using Statistica for Windows with significance set at p < 0.05.
Results
No pathology was identified in the region of the jugular foramen for any specimen. Four types of dural septations were noted. These included type I (10 sides [6 left and 4 right; 36%]) where a dural septation was seen between CN IX anteriorly and CNs X and XI posteriorly (Fig. 1). Of these, the septum was ossified on two (two right sides [20%]). Type II was seen on nine sides (three left and six right [32%]) and was defined as a jugular foramen with no meningeal septation (Fig. 2). Type III was observed on two right sides (7%) and was defined as a foramen with a septation between CNs IX and X anteriorly and CN XI posteriorly (Fig. 3). Type IV (seven sides [25%]) or the chaotic form of the foramen with multiple septations (average: 4, range: 3–7) within the jugular foramen that divided the various rootlets of the CNs (Fig. 4A, 4B). Type I foramina were seen more often in male specimens, but this did not reach statistical significance. Ossified types I and type III foramina were found only on right sides (p > 0.05). Ossification of the septations did not correlate with the age of the specimens. Type IV foramina were more common in females, but this did not reach statistical significance. Samples submitted for histologic confirmation were all confirmed to be meningeal in nature. Septations ranged in length from 0.5 to 1.1 mm (mean: 0.8 mm).
Fig. 1.

Left-side dissection of the type I dural septation (arrow) between cranial nerve (CN) IX (just above the arrowhead) anteriorly and CNs X and XI (just below the arrowhead) posteriorly. This is the traditionally illustrated septation of the jugular foramen. Note that the brainstem has not been removed.
Fig. 2.
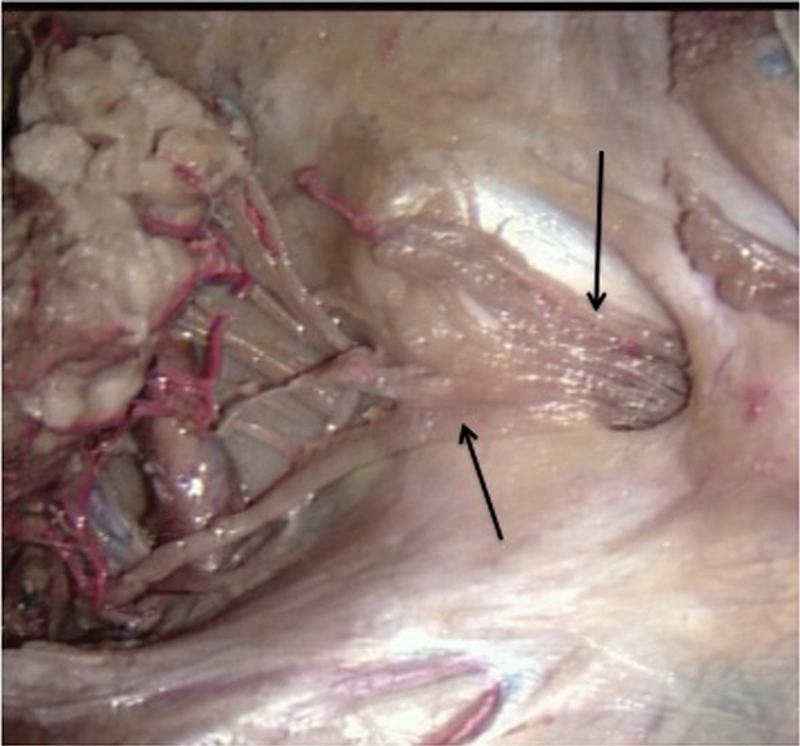
No meningeal septation (type II) in this right jugular foramen. The upper arrow points to cranial nerve (CN) IX and the lower arrow to CN XI. The transected brainstem giving rise to CNs IX, X, and part of XI is seen to the far left of the photograph.
Fig. 3.

A right-sided type III septation (arrow) between cranial nerves (CNs) IX and X anteriorly and CN XI posteriorly.
Fig. 4.

(A) Type IV septations (arrows) dividing the various rootlets of the cranial nerves (CNs) with CN IX labeled and zoomed (B) with septations labeled with arrows and CNs and their rootlets IX, X, and XI labeled.
Discussion
The current study has classified previously undescribed meningeal morphologies of the jugular foramen. The jugular foramen contains the posterolateral pars venosa and anteromedial pars nervosa, partially separated by the jugular spine of the temporal bone and sometimes completely by a fibrous or bony septum.2 3 4 5 6 7 This jugular dural fold is an important anatomical landmark for surgical intervention2 8 and corresponds to our type I jugular foramen meningeal relations in which two folds were ossified. Traditionally, the pars venosa has been described as housing the jugular bulb, the vagus and spinal accessory nerves, and the posterior meningeal branch of the ascending pharyngeal artery that runs between CNs X and XI. Conversely, the pars nervosa houses the glossopharyngeal nerve and the inferior petrosal sinus.3 5 7 9 10 The inferior petrosal sinus usually courses between CN IX and CNs X and XI, and it eventually joins the jugular bulb medially.3 7 9 In addition, the occipital artery gives rise to several meningeal branches that can pass through the jugular foramen.2
The dura mater covering the intracranial aperture of the jugular foramen contains a posterolateral compartment for the sigmoid sinus, an anteromedial compartment for the inferior petrosal sinus, and a neural compartment for CNs IX, X, and XI.2 4 The neural compartment forms two perforations, the glossopharyngeal and the vagal meati, which are usually described as separated by a dural septum of variable width. The glossopharyngeal nerve passes through the glossopharyngeal meatus that is described as funnel shaped; CNs X and XI pass through the vagal meatus that is larger with a variable shape.1 2 4 8 11 12 13
Clinical Application
Based on the difference in the internal dural sleeves of the jugular foramen as found in our study, various tumors of this region might behave differently regarding their growth patterns, which might be appreciated on preoperative imaging. For example, Macdonald et al14 differentiated primary jugular foramen meningiomas (arising within the jugular foramen) from secondary meningiomas (arising from outside of the jugular foramen) and found that these two types behave differently. Primary meningiomas were found to be centrifugal and extensive infiltration of the surrounding skull base, a permeative-sclerotic appearance to the bone margins of the jugular foramen, and prominent dural tails. Such tails might be found to grow into the foramen based on the type of meningeal arrangement. For example, in our study, a type II (Fig. 2) foramen with no dural septations would not inhibit such tumor tails. Therefore, in these cases, the tumor tails would be expected to fill the foramen. However, the dural septations as seen in our type IV foramina (Fig. 4A, 4B) would most likely inhibit significant growth into the jugular foramen.
Surgical approaches to the jugular foramen include the far-lateral (with transcondylar, supracondylar, and paracondylar trajectories), infratemporal fossa, and transjugular approaches, and various pathologies can involve this foramen. For example, for meningiomas of the foramen, although uncommon, surgery can be curative. Other pathologies of this region include neurinomas, schwannomas, and paragangliomas.
The internal meningeal arrangement at the jugular foramen as found in our study would be visualized with intradural procedures of this region and not extradural procedures such as the infratemporal approach. The various types of foramina as identified here might alter surgical approaches. For example, the type III jugular foramen were observed on 7% of sides in our study and were “reversed” compared with the traditionally described arrangement with a dural septation traveling between CNs IX and X anteriorly and CN XI posteriorly. The neurosurgeon should keep this pattern in mind because the traditional arrangement is often used to distinguish CN IX from CN X. Continuous with the glossopharyngeal and vagal meati, the dura mater forms the jugular dural fold that forms a lip over the glossopharyngeal meatus and covers the junction of the sigmoid sinus with the jugular bulb.4 8 For manipulation of the nerves of the jugular foramen, meningeal relations type II would make such maneuvers easier because no meningeal septation was found, and thus tethering of the nerves would be less likely. This is contrasted to type IV meningeal relations where the smaller rootlets of each of the CNs of the jugular foramen were septated and thus more tethered within the jugular foramen. Such significant tethering in the jugular foramina of this latter type would require additional dissection and would most likely increase the risks of CN injury following manipulation by the surgeon. Ossification of these septations would also make surgical manipulation more dangerous because there would be less give when moving the CNs exiting the jugular foramen.
Regarding the bony septation of the jugular foramen, 20% of the type I foramina, where a dural septation was seen between CN IX anteriorly and CNs X and XI posteriorly, were ossified. Others have also reported ossification of this dural septum that effectively creates a separate foramen for the glossopharyngeal nerve anteriorly, and the vagus and spinal accessory nerve posteriorly.15 In 300 Anatolian skulls, Hatiboğlu and Anil15 identified another bony septation in the foramen that created a separate canal for the transmission of the inferior petrosal sinus. This additional “foramen” was present in 5.6% of skulls on the right and in 4.6% on the left. Such a bony bar might be a result of the dural septation as seen in the type III foramen as described in our study (Fig. 3).
Conclusions
Surgery in and around the jugular foramen can be a challenge. Additional knowledge of the anatomy of this region and its anatomical variations can be useful to the neurosurgeon. The meningeal classification defined in this anatomical study can be used in future studies to help correlate operative strategy to morphology within the inner surface of the jugular foramen and aid in the terminology used to describe approaches or the pathology of this region.
Footnotes
Conflicts of Interest Aaron A. Cohen-Gadol has a consulting agreement with Carl Zeiss Meditec AG. The compensation from this arrangement is donated to a not-for-profit educational organization, The Neurosurgical Atlas. No other author has a conflict of interest.
References
- 1.Lang J Anatomy of the brainstem and the lower cranial nerves, vessels, and surrounding structures Am J Otol 1985(Suppl):1–19. [PubMed] [Google Scholar]
- 2.Katsuta T Rhoton A L Jr Matsushima T The jugular foramen: microsurgical anatomy and operative approaches Neurosurgery 1997411149–201.; discussion 201–202 [DOI] [PubMed] [Google Scholar]
- 3.Caldemeyer K S, Mathews V P, Azzarelli B, Smith R R. The jugular foramen: a review of anatomy, masses, and imaging characteristics. Radiographics. 1997;17(5):1123–1139. doi: 10.1148/radiographics.17.5.9308106. [DOI] [PubMed] [Google Scholar]
- 4.Rhoton A L Jr, Buza R. Microsurgical anatomy of the jugular foramen. J Neurosurg. 1975;42(5):541–550. doi: 10.3171/jns.1975.42.5.0541. [DOI] [PubMed] [Google Scholar]
- 5.Ozveren M F Türe U Ozek M M Pamir M N Anatomic landmarks of the glossopharyngeal nerve: a microsurgical anatomic study Neurosurgery 20035261400–1410.; discussion 1410 [DOI] [PubMed] [Google Scholar]
- 6.Shapiro R. Compartmentation of the jugular foramen. J Neurosurg. 1972;36(3):340–343. doi: 10.3171/jns.1972.36.3.0340. [DOI] [PubMed] [Google Scholar]
- 7.Tekdemir I, Tuccar E, Aslan A. et al. The jugular foramen: a comparative radioanatomic study. Surg Neurol. 1998;50(6):557–562. doi: 10.1016/s0090-3019(98)00048-2. [DOI] [PubMed] [Google Scholar]
- 8.Silverstein H, Willcox T O, Rosenberg S I, Seidman M D. The jugular dural fold—a helpful skull base landmark to the cranial nerves. Skull Base Surg. 1995;5(1):57–61. doi: 10.1055/s-2008-1058951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubinstein D, Burton B S, Walker A L. The anatomy of the inferior petrosal sinus, glossopharyngeal nerve, vagus nerve, and accessory nerve in the jugular foramen. AJNR Am J Neuroradiol. 1995;16(1):185–194. [PMC free article] [PubMed] [Google Scholar]
- 10.Weber A L, McKenna M J. Radiologic evaluation of the jugular foramen. Anatomy, vascular variants, anomalies, and tumors. Neuroimaging Clin N Am. 1994;4(3):579–598. [PubMed] [Google Scholar]
- 11.Ayeni S A, Ohata K, Tanaka K, Hakuba A. The microsurgical anatomy of the jugular foramen. J Neurosurg. 1995;83(5):903–909. doi: 10.3171/jns.1995.83.5.0903. [DOI] [PubMed] [Google Scholar]
- 12.Dichiro G, Fisher R L, Nelson K B. The jugular foramen. J Neurosurg. 1964;21:447–460. doi: 10.3171/jns.1964.21.6.0447. [DOI] [PubMed] [Google Scholar]
- 13.Kveton J F, Cooper M H. Microsurgical anatomy of the jugular foramen region. Am J Otol. 1988;9(2):109–112. [PubMed] [Google Scholar]
- 14.Macdonald A J, Salzman K L, Harnsberger H R, Gilbert E, Shelton C. Primary jugular foramen meningioma: imaging appearance and differentiating features. AJR Am J Roentgenol. 2004;182(2):373–377. doi: 10.2214/ajr.182.2.1820373. [DOI] [PubMed] [Google Scholar]
- 15.Hatiboğlu M T, Anil A. Structural variations in the jugular foramen of the human skull. J Anat. 1992;180(Pt 1):191–196. [PMC free article] [PubMed] [Google Scholar]


