Abstract
Introduction:
The role of ultrasonography in detection of pleural effusion has long been a subject of interest but controversial results have been reported. Accordingly, this study aims to conduct a systematic review of the available literature on diagnostic value of ultrasonography and radiography in detection of pleural effusion through a meta-analytic approach.
Methods:
An extended search was done in databases of Medline, EMBASE, ISI Web of Knowledge, Scopus, Cochrane Library, and ProQuest. Two reviewers independently extracted the data and assessed the quality of the articles. Meta-analysis was performed using a mixed-effects binary regression model. Finally, subgroup analysis was carried out in order to find the sources of heterogeneity between the included studies.
Results:
12 studies were included in this meta-analysis (1554 subjects, 58.6% male). Pooled sensitivity of ultrasonography in detection of pleural effusion was 0.94 (95% CI: 0.88-0.97; I2= 84.23, p<0.001) and its pooled specificity was calculated to be 0.98 (95% CI: 0.92-1.0; I2= 88.65, p<0.001), while sensitivity and specificity of chest radiography were 0.51 (95% CI: 0.33-0.68; I2= 91.76, p<0.001) and 0.91 (95% CI: 0.68-0.98; I2= 92.86, p<0.001), respectively. Sensitivity of ultrasonography was found to be higher when the procedure was carried out by an intensivist or a radiologist using 5-10 MHz transducers.
Conclusion:
Chest ultrasonography, as a screening tool, has a higher diagnostic accuracy in identification of plural effusion compared to radiography. The sensitivity of this imaging modality was found to be higher when performed by a radiologist or an intensivist and using 5-10MHz probes.
Key Words: Pleural Effusion, ultrasonography, radiography, diagnostic tests, routine
Introduction:
The role of ultrasonography in detection of pleural effusion was first discovered in the 1960s (1). One decade later the diagnostic value of A-mode ultrasonography in identification of pleural effusion was reported to be 95% (2). Thus, the impression that ultrasonography is not a suitable modality for detection of chest lesions was rejected at that time. Afterwards, various surveys were conducted evaluating the diagnostic accuracy of ultrasonography and radiography in identification of pleural effusion and most of them found a higher diagnostic value for ultrasonography compared to radiography (3-5). However, ultrasonography is still not considered as the first diagnostic tool for detection of pleural effusion and the majority of physicians use radiography for this propose (6).
Although a radiogram captured in lateral decubitus position with horizontal rays has a high sensitivity and specificity in detection of pleural effusion but it cannot be obtained from all the patients especially critically ill and trauma victims (4). Other views of chest radiogram have low sensitivities in this regard (7, 8). Vast improvements of technology have led to development of hand-held and pocket-size ultrasound devices (9, 10). A meta-analysis was performed in 2010 on four studies that reported the sensitivity and specificity of ultrasonography in detection of pleural effusion to be 93% and 96%, respectively (11). Yet, inclusion of few surveys and lack of sensitivity analysis and publication bias confirm the necessity of an update on this subject. Therefore, this study aims to conduct a systematic review of the available literature determining the diagnostic value of ultrasonography and radiography for detection of pleural effusion through a meta-analytic approach.
Methods:
Search strategy and selection criteria
This study was designed according to the consensus statement of Meta-analysis of Observational Studies in Epidemiology (MOOSE) (12). Extended systematic search was carried out in databases of Medline (via PubMed), EMBASE (via OvidSP), ISI Web of Knowledge, Scopus, Cochrane Library, and ProQuest based on the keywords obtained from Medical Subject Heading (MeSH) terms and EMTREE. The keywords included “Ultrasonography” OR “Sonography” OR “Ultrasound” OR “Chest Film” OR “Chest Radiograph” combined with “Pleural Effusion” OR “Effusion” OR “Pleural Free Fluid”. The directive was to find prospective and retrospective studies assessing the diagnostic value of ultrasonography or chest radiography in detection of pleural effusion. Two of the authors (M.Y, P.G) independently searched for sources and contacted the authors of relevant articles to obtain further articles and data. Only original articles were included. The studies that had used radiography as their reference test were excluded and only surveys in which a final diagnosis of pleural effusion had been confirmed by computed tomography scan or surgery were included. The search yielded three surveys which had compared the diagnostic value of pocket-size ultrasonography machines with high-end ones. Since these high-end ultrasonography machine had been performed by cardiologists and their results had been assessed by the final diagnosis proposed by two specialists as the reference test, these three surveys were also included in the meta-analysis.
Data extraction
The articles were entered into Endnote X7 software and after elimination of duplicates, two reviewers (M.Y, P.G) independently screened the articles. Full texts of the articles were studied and summarization was done. Quality of the surveys were evaluated according to the guidelines proposed by 14-Item Quality Assessment of Diagnostic Accuracy Studies (QUADAS2) tool (18). Each article was assessed regarding presence of various biases including selection, performance, recording, and reporting and they were classified as three grades of poor, fair or good. Only fair and good surveys were included in meta-analysis. Data on distribution of the study population regarding age and gender, sample size, the number of patients with/without pleural effusion according to reference tests, technique of ultrasonography, the specialty of the ultrasound device’s operator, sonographic definition of pleural effusion, probe’s frequency, blinding status, sampling method (consecutive, convenience) and finally number of true and false, positive and negative cases were gathered. A third author (M.H) was in charge of solving disagreements. In cases where data were not presented in the article web-based programs were used to compute true positive, false positive, true negative and false negative figures according to sensitivity and specificity. When available, data for each hemi-thorax were included in the analysis separately.
Statistical analysis
STATA 11.0 statistical software was used to analyze the data via MIDAS module. To evaluate the adequacy of ultrasonography and radiography in detection of pleural effusion, summary receiver operative curves (SROC), sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio with 95% confidence interval (95% CI) were calculated using a mixed-effects binary regression model. Heterogeneity between the included surveys was assessed through utilization of I2 and χ2 tests and a p value of less than 0.1 along with an I2 greater than 50% were considered as positive heterogeneity (19). Consequently, subgroup analysis was performed on sampling method (consecutive/ convenience), operator (emergency physician/ other specialists) or interpreting physician, frequency of the probe (1-5 MHz/ 5-10 MHz), type of ultrasound device (pocket-size/other) and sample size (less than 100 patients/ more than 100 patients).
Results:
Study characteristics
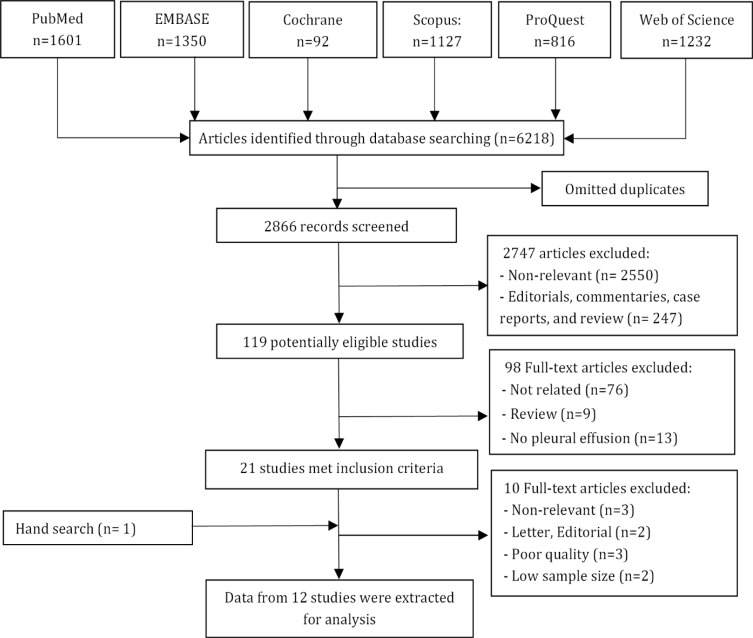
Search process and the number of articles obtained in each step are presented in Figure 1. Twenty one studies met the inclusion criteria. One survey was also found through manual search. After detailed evaluation of these surveys 12 studies were included in meta-analysis (3-5, 7-10, 13-17). The characteristics of included studies are presented in Table 1. The mean age of the subjects was 63.3 years (ranging from 14 to 101 years old) and 58.6% were male. All the studies were single-center (3-5, 7-10, 14-17)except one which was performed in two center (13). A total of 646 patients with pleural effusion and 912 subjects without it were evaluated. Diagnostic accuracy of both these modalities was assessed in nine surveys (3-5, 8-10, 13-17), radiography was evaluated individually in one study (7) and ultrasonography was assessed individually in two articles (10, 17). 11 articles were in English (3-5, 7-10, 13-15, 17) and one was in Farsi (16). The presence of heterogeneity was confirmed between the studies (P<0.1), but no publication bias was detected (Figure 2).
Figure 1.
Flowchart of the study
Table 1.
Charecteristics of included studies
| Study |
No. of patient
(+ / -) 1 |
Age
2
(years) |
Male (%) | Reference / Index | Transducer / Operator | Sampling | Weaknesses |
|---|---|---|---|---|---|---|---|
| Ma 1997 ( 5 ) | 26 / 214 | ≥ 18 | NR | CT/ US, CXR | 3.5-to 2.5-MHz / EP | Consecutive / Trauma |
Retrospective design |
| Kataoka 2000 ( 3 ) | 60 / 22 | 76.0 ± 12.9 | 38 | CT/ US, CXR | 3.5 MHz / Internist |
Consecutive / Critically ill |
Low sample size Only evaluating of CHF patient |
| Lichtenstein 2004 ( 4 ) | 100 / 284 | 58±15 | NR | CT/ US, CXR | 5 MHz / Intensivist |
Consecutive / Critically ill |
|
| Rocco 2008 ( 8 ) | 38 / 142 | 42±14 | 66.7 | CT/ US, CXR | 3.5 MHz / Intensivist |
Consecutive / Trauma |
Low sample size |
| Kitazono 2010 ( 7 ) | 117 / 83 | 54 (14-91) | 60 | CT/ CXR | NA / Radiologist |
Consecutive / Critically ill |
Retrospective design |
| Zanobetti 2011 ( 13 ) | 25 / 11 | 73 (21-101) | 51 | CT/ US, CXR | 5– to 8-MHz / EP | Consecutive / Critically |
CT was performed in some patients |
| Xirouchaki 2011 ( 14 ) | 63 / 21 | 57.1±21.5 | 81 | CT/ US, CXR | 5– to 9-MHz / Intensivist |
Convenience / Critically ill |
Low sample size |
| Schleder 2012 ( 15 ) | 35 /13 | NR | NR | Outcome / US, CXR | 5- to 9-MHz / Radiologist |
Consecutive / Critically ill |
Low sample size |
| Kasraei 2014 ( 16 ) | 27 / 7 | 18-70 | 53.8 | CT / US, CXR | 5- to 9-MHz / Radiologist |
Consecutive / Critically ill |
Low sample size Possibility of selection bias |
| Pocket-size ultrasonography | |||||||
| Dalen 2015 ( 10 ) | 39 / 85 | 74 (35–91) | 52 | High-end US / US | 1.7- to 3.8-MHz / Nurse | Consecutive / Heart failure |
Low sample size |
| Graven 2015 ( 9 ) | 95 / 23 | 67 (35-86) | 66 | High-end US / US, CXR | 1.7- to 3.8-MHz / Nurse | Convenience / Cardiac surgery |
Low sample size Possibility of selection bias |
| Stock 2015 ( 17 ) | 21 / 7 | 68 (24-94) | 42.8 | High-end US / US | 2- to 4-MHz / Internist |
Convenience / Surgery |
Low sample size Possibility of selection bias |
1, (+ / -): Number of patient with pleural effusion / number of patient without pleural effusion; 2, Number are presented as mean ± standard deviation or (range). CT: Computed tomography; CXR: Chest radiography; EP: Emergency physician; NA: Not applicable; NR: Not Reported; US: Ultrasonography
Figure 2.
Deeks’ funnel plot asymmetry test for assessment of publication bias. P values < 0.05 were considered as significant. Ultrasonography (A); Radiography (B). ESS: Effective sample sizes
Meta-analysis
Area under the curve of SROCs for ultrasonography and chest radiography in detection of pleural effusion were 0.98 (95% CI: 0.97-0.99) and 0.73 (95% CI: 0.69-0.77), respectively (Figure 3). Pooled sensitivity and specificity of ultrasonography in detection of pleural effusion were 0.94 (95% CI: 0.88-0.97; I2= 84.23, p<0.001) and 0.98 (95% CI: 0.92-1.0; I2= 88.65, p<0.001), respectively. Also, its pooled positive and negative likelihood ratios were calculated to be 53.96 (95% CI: 11.46-254.05; I2= 88.12, p<0.001) and 0.06 (95% CI: 0.03-0.12; I2= 84.44, p<0.001), respectively (Figure 4).
Figure 3.
Summary receiver operative curves (SROC) for ultrasound (A) and chest radiography (B) in detection of plural effusion. AUC: Area under the curve; SENS: Sensitivity; SPEC: Specificity
Figure 4.
Forest plot of screening performance characteristics of chest ultrasonography in detection of plural effusion. Sensitivity and specificity (A); Diagnostic likelihood ratio (DLR) (B). CI: Confidence interval
Pooled sensitivity and specificity of radiography in pleural effusion diagnosis were 0.51 (95% CI: 0.33-0.68; I2= 91.76, p<0.001) and 0.91 (95% CI: 0.68-0.98; I2= 92.86, p<0.001), respectively. In addition, its pooled positive and negative likelihood ratios were also found to be 5.60 (95% CI: 1.14-27.42; I2= 88.14, p<0.001) and 0.54 (95% CI: 0.35-0.84; I2= 84.44, p<0.001), respectively (Figure 5).
Figure 5.
Forest plot of screening performance characteristics of chest radiography in detection of plural effusion. Sensitivity and specificity (A); Diagnostic likelihood ratio (DLR) (B). CI: Confidence interval
Subgroup Analysis
Subgroups analyses were performed regarding study design, patients’ type (critically ill / other), operator of ultrasound machine, ultrasound model and sample size. The results showed that the sensitivity was higher when the procedure was performed via an intensivist or a radiologist, using 5-10 MHz transducers, whereas it was lower when carried out via pocket-size devices. On the other hand, the specificity of this modality was not influenced by any of these factors.
The diagnostic value of radiography was affected by the sample size and type of patients. In this regard, the sensitivity and specificity of chest radiography was found to be higher in studies with sample sizes of greater than 100 patients while both of these measures were calculated to be lower in critically ill patients (Table 2).
Table 2.
Subgroup analysis of diagnostic accuracy for chest radiography and ultrasonography in detection of plural effusion
| Covariate | No. of studies |
Bivariate random-effect model
|
|||||
|---|---|---|---|---|---|---|---|
|
Sensitivity
(95% CI) |
P |
Specificity
(95% CI) |
p | heterogeneity, I 2 | P * | ||
| Ultrasonography | |||||||
| Patient enrollment | |||||||
| Consecutive | 8 | 0.95 (0.90-0.99) | 0.08 | 0.97 (0.92-1.00) | <0.001 | 15.0 % | 0.31 |
| Nonconsecutive | 4 | 0.92 (0.84-1.00) | 1.00 (0.98-1.00) | ||||
| Operator | |||||||
| Radiologist/Intensivist | 6 | 0.97 (0.83-0.96) | <0.001 | 0.99 (0.98-1.00) | 0.34 | 68.0 % | 0.05 |
| Other physician | 6 | 0.90 (0.83-0.96) | 0.94 (0.86-1.00) | ||||
| Sample size | |||||||
| < 100 | 8 | 0.94 (0.89-0.99) | 0.22 | 0.96 (0.90-1.00) | <0.001 | 0.0 % | 0.38 |
| ≥ 100 | 4 | 0.94 (0.88-1.00) | 0.99 (0.98-1.00) | ||||
| Frequency | |||||||
| 1-5 MHz | 9 | 0.92 (0.86-0.97) | 0.04 | 0.98 (0.95-1.00) | 0.14 | 42.0 % | 0.18 |
| 5-10 MHz | 3 | 0.98 (0.95-1.00) | 0.99 (0.96-1.00) | ||||
| Patients | |||||||
| Critically ill | 7 | 0.94 (0.89-0.99) | 0.29 | 0.98 (0.95-1.00) | 0.12 | 15.0 % | 0.31 |
| Other | 5 | 0.93 (0.87-1.00) | 0.98 (0.94-1.00) | ||||
| Machine type | |||||||
| Pocket-size | 3 | 0.90 (0.80-1.00) | 0.09 | 0.92 (0.76-1.00) | 0.55 | 16.0 % | 0.30 |
| Other | 9 | 0.95 (0.91-0.99) | 0.97 (0.97-1.00) | ||||
| Radiography | |||||||
| Patient enrollment | |||||||
| Consecutive | 7 | 0.50 (0.30-0.71) | 0.93 | 0.81 (0.31-1.00) | 0.94 | 0.0 % | 0.77 |
| Nonconsecutive | 3 | 0.53 (0.13-0.92) | 0.93 (0.81-1.00) | ||||
| Operator | |||||||
| Radiologist/Intensivist | 6 | 0.50 (0.27-0.73) | 0.95 | 0.87 (0.65-1.00) | 0.95 | 0.0 % | 0.73 |
| Other | 4 | 0.51 (0.22-0.81) | 0.96 (0.84-1.00) | ||||
| Sample size | |||||||
| < 100 | 6 | 0.45 (0.22-0.67) | 0.44 | 0.79 (0.51-1.00) | 0.99 | 8.0 % | 0.34 |
| ≥= 100 | 4 | 0.60 (0.33-0.87) | 0.97 (0.90-1.00) | ||||
| Patients | |||||||
| Critically ill | 7 | 0.48 (0.26-0.69) | 0.62 | 0.82 (0.59-1.00) | 0.29 | 12.0 % | 0.32 |
| Other | 3 | 0.58 (0.25-0.91) | 0.98 (0.93-1.00) | ||||
P value < 0.1 was considered as significant for heterogeneity; CI: Confidence interval.
Discussion
The present meta-analysis showed that ultrasonography has high sensitivity (94%) and specificity (98%) in detection of pleural effusion. When the analysis was limited to the surveys in which the procedure was carried out by an intensivist or a radiologist, the presented sensitivity increased (98%). While, the diagnostic value of radiography was reported to be lower than ultrasonography (sensitivity 51%, specificity 91%). When we limited the analyses to studies in which the etiology of pleural effusion was trauma, surgery or congestive heart failure, sensitivity of radiography slightly increased (58%). On this basis it can be concluded that ultrasonography is a better diagnostic tool for pleural effusion compared to radiography.
In comparison with the results of the present study, Grimberg et al. reported similar results in their review of four articles. They found the sensitivity and specificity of ultrasonography to be 93% and 96% respectively while these figures for radiography were calculated to be 24% and 100% (11). Our results were almost similar to Grimberg’s et al. study. The higher sensitivity of radiography presented in this study might be due to inclusion of more surveys in the analyses. Grimberg’s survey lacked subgroup analysis which prevents us from further comparisons. In another meta-analysis Chavez et al. reviewed 10 articles aiming to evaluate the diagnostic value of ultrasonography in detection of pneumonia and they found a sensitivity of 94% and a specificity of 96% for this modality (20). These researchers stated that ultrasonography is a suitable diagnostic tool for ruling out pneumonia in patients referring to medical centers and emergency departments. Congruent with this survey we also found a considerable diagnostic value for ultrasonography in detection of pleural effusion.
One of the factors that influence sensitivity of ultrasonography is the operator of ultrasound device which has been verified by various surveys in the past years (21-24). An ultrasonography carried out by an intensivist or a radiologist is able to detect pleural effusion more effectively and precisely.
Pocket-size ultrasonography is a new technology recently being used in some medical centers and reported to be an effective modality in diagnostic procedures (25-27). This machine transmits high resolution pictures that help physicians to make more precise decisions regarding the patients’ pathology (28, 29). Accordingly, we found three studies which assess the diagnostic accuracy of pocket-size ultrasonography for pleural effusion (9, 10, 17), in two of which the procedure was performed by a trained nurse (9, 10) and in one it was carried out by an internal medicine specialist (17). The first two reported a sensitivity of approximately 92-98% and the latter survey found a sensitivity of 62% in detection of pleural effusion. This inconsistency might have been due to the different study populations. Graven et al. and Dalen et al. only included cardiac patients while Stock et al. evaluate patients with various diseases. Nevertheless, the sample sizes of all the three surveys were small and so further investigation is required for application of this ultrasonography device in clinical settings.
In this meta-analysis the extended search in databases and bibliographies yielded 12 relevant articles. Although few studies were included in this study, but the large sample population of 1554 subjects assured the validity of performed analyses to a great extent. Presence of no publication bias confirms this declaration. Heterogeneity between the articles was another limitation of this survey which was attempted to overcome through application of mixed-effects binary regression model and subgroup analysis. Simultaneous inclusion of retrospective and prospective surveys was probable limitation of this study, but the scatterplot developed to evaluate the outlier studies according to standardized predicted random effects showed that retrospective surveys were not the source of diversity between the included articles.
Conclusion:
The present meta-analysis found chest ultrasonography to have a considerably higher screening value in detection of pleural effusion compare to radiography. Being performed by an intensivist or a radiologist and using probes with frequencies of 5-10MHz improves the sensitivity of this imaging modality.
Acknowledgments:
None
Conflict of interest:
None
Funding support:
This research has been supported by Tehran University of Medical Sciences & health Services grant number: 93-02-38-25618.
Authors’ contributions:
All authors passed four criteria for authorship contribution based on recommendations of the International Committee of Medical Journal Editors.
References
- 1.Rozycki GS, Pennington SD, Feliciano DV. Surgeon-performed ultrasound in the critical care setting: its use as an extension of the physical examination to detect pleural effusion. J Trauma. 2001;50(4):636–42. doi: 10.1097/00005373-200104000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Rozycki GS, Cava RA, Tchorz KM. Surgeon-performed ultrasound imaging in acute surgical disorders. Curr Probl Surg. 2001;38(3):141–212. doi: 10.1067/msg.2001.112348. [DOI] [PubMed] [Google Scholar]
- 3.Kataoka H, Takada S. The role of thoracic ultrasonography for evaluation of patients with decompensated chronic heart failure. J Am Coll Cardiol. 2000;35(6):1638–46. doi: 10.1016/s0735-1097(00)00602-1. [DOI] [PubMed] [Google Scholar]
- 4.Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997;29(3):312–6. doi: 10.1016/s0196-0644(97)70341-x. [DOI] [PubMed] [Google Scholar]
- 6.Villena Garrido V, Cases Viedma E, Fernandez Villar A, et al. Recommendations of diagnosis and treatment of pleural effusion. Update. Arch Bronconeumol. 2014;50(6):235–49. doi: 10.1016/j.arbres.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Kitazono MT, Lau CT, Parada AN, Renjen P, Miller Jr WT. Differentiation of pleural effusions from parenchymal opacities: Accuracy of bedside chest radiography. Am J Roentgenol. 2010;194(2):407–12. doi: 10.2214/AJR.09.2950. [DOI] [PubMed] [Google Scholar]
- 8.Rocco M, Carbone I, Morelli A, et al. Diagnostic accuracy of bedside ultrasonography in the ICU: feasibility of detecting pulmonary effusion and lung contusion in patients on respiratory support after severe blunt thoracic trauma. Acta Anaesthesiol Scand. 2008;52(6):776–84. doi: 10.1111/j.1399-6576.2008.01647.x. [DOI] [PubMed] [Google Scholar]
- 9.Graven T, Wahba A, Hammer AM, et al. Focused ultrasound of the pleural cavities and the pericardium by nurses after cardiac surgery. Scand Cardiovasc J. 2015;49(1):56–63. doi: 10.3109/14017431.2015.1009383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dalen H, Gundersen GH, Skjetne K, et al. Feasibility and reliability of pocket-size ultrasound examinations of the pleural cavities and vena cava inferior performed by nurses in an outpatient heart failure clinic. Eur J Cardiovasc Nurs. 2015;14(4):286–93. doi: 10.1177/1474515114547651. [DOI] [PubMed] [Google Scholar]
- 11.Grimberg A, Shigueoka DC, Atallah AN, Ajzen S, Iared W. Diagnostic accuracy of sonography for pleural effusion: systematic review. Sao Paulo Med J. 2010;128(2):90–5. doi: 10.1590/S1516-31802010000200009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.Zanobetti M, Poggioni C, Pini R. Can chest ultrasonography replace standard chest radiography for evaluation of acute dyspnea in the ED? Chest. 2011;139(5):1140–7. doi: 10.1378/chest.10-0435. [DOI] [PubMed] [Google Scholar]
- 14.Xirouchaki N, Magkanas E, Vaporidi K, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med. 2011;37(9):1488–93. doi: 10.1007/s00134-011-2317-y. [DOI] [PubMed] [Google Scholar]
- 15.Schleder S, Dornia C, Poschenrieder F, et al. Bedside diagnosis of pleural effusion with a latest generation hand-carried ultrasound device in intensive care patients. Acta Radiol. 2012;53(5):556–60. doi: 10.1258/ar.2012.110676. [DOI] [PubMed] [Google Scholar]
- 16.Kasraei M, Abtahi H, Eyoobi Yazdi N, Safavi E, Firoozbakhsh S, Mohammady M. Diagnosis of pleural effusion by portable ultrasound and chest radiography in intensive care unit. Tehran Uni Med J. 2014;72(7):463–70. [Persian] [Google Scholar]
- 17.Stock KF, Klein B, Steubl D, et al. Comparison of a pocket-size ultrasound device with a premium ultrasound machine: diagnostic value and time required in bedside ultrasound examination. Abdom Imaging. 2015 doi: 10.1007/s00261-015-0406-z. [In press] [DOI] [PubMed] [Google Scholar]
- 18.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chavez MA, Shams N, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. 2014;15:50–9. doi: 10.1186/1465-9921-15-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abbasi S, Farsi D, Hafezimoghadam P, Fathi M, Zare MA. Accuracy of emergency physician-performed ultrasound in detecting traumatic pneumothorax after a 2-h training course. Eur J Emerg Med. 2013;20(3):173–7. doi: 10.1097/MEJ.0b013e328356f754. [DOI] [PubMed] [Google Scholar]
- 22.Bui-Mansfield LT, Chen DC, O'Brien SD. Accuracy of ultrasound of musculoskeletal soft-tissue tumors. Am J Roentgenol. 2015;204(2):W218–22. doi: 10.2214/AJR.14.13335. [DOI] [PubMed] [Google Scholar]
- 23.Fine D, Perring S, Herbetko J, Hacking C, Fleming J, Dewbury K. Three-dimensional (3D) ultrasound imaging of the gallbladder and dilated biliary tree: reconstruction from real-time B-scans. Br J Radiol. 1991;64(767):1056–7. doi: 10.1259/0007-1285-64-767-1056. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Jeong YK, Park KB, Park JK, Jeong AK, Hwang JC. Operator-dependent techniques for graded compression sonography to detect the appendix and diagnose acute appendicitis. Am J Roentgenol. 2005;184(1):91–7. doi: 10.2214/ajr.184.1.01840091. [DOI] [PubMed] [Google Scholar]
- 25.Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002–6. doi: 10.1016/j.amjcard.2005.05.060. [DOI] [PubMed] [Google Scholar]
- 26.Skjetne K, Graven T, Haugen BO, Salvesen O, Kleinau JO, Dalen H. Diagnostic influence of cardiovascular screening by pocket-size ultrasound in a cardiac unit. Eur J Echocardiogr. 2011;12(10):737–43. doi: 10.1093/ejechocard/jer111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tofield A. The use of pocket size imaging devices: a position statement by the European Association of Echocardiography. Eur Heart J. 2011;32(4):385–6. doi: 10.1093/eurheartj/ehr001. [DOI] [PubMed] [Google Scholar]
- 28.Andersen GN, Haugen BO, Graven T, Salvesen O, Mjolstad OC, Dalen H. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr. 2011;12(9):665–70. doi: 10.1093/ejechocard/jer108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mjolstad OC, Andersen GN, Dalen H, et al. Feasibility and reliability of point-of-care pocket-size echocardiography performed by medical residents. Eur Heart J Cardiovasc Imaging. 2013;14(12):1195–202. doi: 10.1093/ehjci/jet062. [DOI] [PMC free article] [PubMed] [Google Scholar]