Abstract
Summary
Rates of fracture worldwide are changing. Using the Clinical Practice Research Datalink (CPRD), age, and gender, geographical, ethnic and socioeconomic trends in fracture rates across the United Kingdom were studied over a 24 year period 1988-2012. Previously observed patterns in fracture incidence by age and fracture site were evident. New data on the influence of geographic location, ethnic group and socioeconomic status were obtained.
Introduction
With secular changes in age- and sex-specific fracture incidence observed in many populations, and global shifts towards an elderly demography, it is vital for health care planners to have an accurate understanding of fracture incidence nationally. We aimed to present up to date fracture incidence data in the UK, stratified by age, sex, geographic location, ethnicity and socioeconomic status.
Methods
The Clinical Practice Research Datalink (CPRD) contains anonymised electronic health records for approximately 6.9% of the UK population. Information comes from General Practitioners, and covers 11.3 million people from 674 practices across the UK, demonstrated to be representative of the national population. The study population consisted of all permanently registered individuals aged >=18 years. Validated data on fracture incidence were obtained from their medical records, as was information on socioeconomic deprivation, ethnicity and geographic location. Age and sex-specific fracture incidence rates were calculated.
Results
Fracture incidence rates by age and sex were comparable to those documented in previous studies and demonstrated a bimodal distribution. Substantial geographic heterogeneity in age and sex adjusted fracture incidence was observed, with rates in Scotland almost 50% greater than those in London and South East England. Lowest rates of fracture were observed in black individuals of both sexes; rates of fragility fracture in white women were 4.7 times greater than in black women. Strong associations between deprivation and fracture risk were observed in hip fracture in men, with a relative risk of 1.3 (95% CI 1.21-1.41) in Index of Multiple Deprivation category 5 (representing the most deprived) compared to category 1.
Conclusions
This study presents robust estimates of fracture incidence across the UK, which will aid decisions regarding allocation of healthcare provision to populations of greatest need. It will also assist the implementation and design of strategies to reduce fracture incidence and its personal and financial impact on individuals and health services.
Introduction
Osteoporosis is characterised by deterioration of bone mass and microarchitecture, resulting in increased bone fragility and propensity to fracture[1]. Worldwide, in the year 2000, there were estimated to be nearly 9 million osteoporotic fractures each year, of which 1.6 million were at the hip, 1.7 million at the forearm and 1.4 million were clinical (symptomatic) vertebral fractures[2]. The US Surgeon General’s report of 2004[3], consistent with data from the UK[4], suggested that almost one in two women and one in five men will experience a fracture in their remaining lifetime from the age of 50 years. The economic and personal costs of osteoporotic fracture are substantial, accounting for 37 billion Euros annually across the 27 countries of the European Union and 1,180,000 quality adjusted life years lost during 2010[5]. Owing to the ageing population, global costs of osteoporotic fracture are expected to increase by 25% during the period 2010 to 2025[5]. A similar increase is predicted in the United States, where osteoporosis is the 10th ranked major illness and is among the top 5% highest cost Medicare beneficiaries[3].
There is substantial variability in fracture incidence worldwide[6], and studies have demonstrated differences in fracture risk according to geography[2, 6, 7], ethnicity[7–9] and socioeconomic status[10–12]. The largest existing study of fracture epidemiology in England and Wales, published in 2001, sampled 5 million adults from the General Practice Research Database [GPRD, now known as the Clinical Practice Research Datalink (CPRD)] during the period 1988-1998[4]. In this analysis, it was not possible to stratify fracture incidence according to the geographic region, ethnicity and socioeconomic status; additionally secular changes in age- and sex- adjusted fracture incidence rates have been demonstrated worldwide in recent decades[13]. In this study, we aimed, using CPRD over the period 1988 to 2012, to provide current estimates of fracture incidence stratified by age, sex, geographic region, ethnic group and socioeconomic status.
Methods
Clinical Practice Research Datalink
The Clinical Practice Research Datalink (CPRD), previously known as the General Practice Research Database, contains the anonymised electronic records as collected by General Practitioners, who play a key role in the healthcare system of the UK, as they are responsible for primary healthcare and specialist referrals. The CPRD covers over 11.3 million individuals from 674 practices in the UK. Around 4.4 million individuals are active (alive, currently registered) and meet quality criteria, accounting for approximately 6.9% of the UK population. The cohort has been shown to be broadly representative of the UK population in terms of age, sex and ethnicity when compared with the UK census in 2011[14], and the body mass index distribution is comparable to that in the Health Survey for England in most patient subgroups[14]. Conversely, despite the large number of GP practices included, CPRD may not be representative of all practices in the UK in terms of geography and size[14]. Clinical data are stored and retrieved by means of READ codes for disease or causes of morbidity or mortality which are cross-referenced to the International Classification of Diseases, 9th edition (ICD-9). From the data collected we extracted information on patient demographics, clinical events, prescriptions, referrals, hospital admissions and their major outcomes.
Study Population
The study population consisted of all permanently registered individuals aged >=18 years who had a fracture recorded in their medical record during the period of time from the enrolment date of their practice in CPRD until the end of data collection. The data collection period was 1988 to 2012. Fractures were classified according to the International Classification of Diseases, ninth edition (ICD-9) categories. These included skull (ICD-9 categories 800-804), vertebra (805 or 806), rib (807), pelvis (808), clavicle (810), scapula (811), humerus (812), radius/ulna (813), carpus (814 to 817), femur/hip (820/821), patella (822), tibia/fibula/ankle (823 or 824), foot (825 or 826), or unspecified fractures (809, 818, 819, 827–829). These fracture outcomes were used individually, and then grouped as all fractures, fragility fractures (hip, spine, rib, humerus, radius/ulna or pelvis), and as the fracture definition used in the FRAX algorithm (hip, spine, radius/ulna or humerus). The validity of CPRD records for hip and vertebral fractures has been previously demonstrated[15], although such an investigation is awaited in the context of other fracture types. Thus 150 patients with a hip fracture and 150 with a vertebral fracture documented in CPRD were selected at random, and a questionnaire sent to the GP in order to validate the diagnosis. 91% of hip fractures and 88% of vertebral fractures were confirmed[15]. Since there is no standard approach for ethnic groups in the UK, we used the ethnicity classification as developed and tested by Mathur[16], for which a high level of concordance within and across NHS sources was found in an analysis of CPRD records of ethnicity: Within primary care in the UK, recording of ethnicity has been incentivised under the Quality and Outcomes Framework (QOF)11–13 between 2006/07 and 2011/12, dramatically improving the completeness of ethnicity data for newly registered patients. QOF results data show that over 90% of UK general practices are now recording ethnicity for all of their newly registered patients, and ethnicity is also recorded by hospital staff when an individual is admitted to hospital[16].
Statistical analysis
Age- and sex- specific fracture incidence rates were calculated by dividing the number of individuals with a fracture by the total person-years of follow-up. The total person-years was the sum of the number of individuals registered on the database at July 1 of each calendar year from 1988 to 2012. In CPRD, as in many similar datasets, differentiation of 2 distinct fracture events at the same site, from one fracture event recorded twice, is extremely difficult. In order to prevent double-counting, the incidence analyses were therefore based on the first-ever occurrence of a fracture at a particular location. If an individual had multiple records of fractures at the same location, only the first record was used in the incidence rate calculation. Socioeconomic status was classified according to the Index of Multiple Deprivation (IMD): The English Indices of Deprivation are comprised of a number of indicators covering different aspects (‘domains’) of material deprivation (housing, employment, income, access to services, education and skills, crime, living environment)[17]. Each domain index can itself be a composite score derived from two or more sub-domain indicators. In addition, a composite index, the Index of Multiple Deprivation (IMD), is calculated as a weighted sum of the domain indices. We used this measure incorporating 38 separate indicators, organised across seven distinct domains of deprivation, split into five categories with risk of fracture calculated for each category (IMD 2010: http://www.communities.gov.uk/communities/research/indicesdeprivation/deprivation10).
Results
Incidence by age, sex and fracture site
A total of 196,570 men aged 18 years or older sustained one or more fractures over 23,285,904 person-years of follow-up, compared with 263,592 women aged 18 years or older over 26,342,685 person-years of follow-up. When stratified by age [18-49 years (Table 1) and 50+ years (Table 2)], this equates to a fracture rate of 94.8 per 10,000 person-years of follow up (py) in men aged 18-49 years, in comparison to 54.3 per 10,000 py in women aged 18-49 years. In men aged 50+ years, the overall rate of fracture was reduced to 71.8 per 10,000 py whereas in women 50+ years it almost tripled to 155.4 per 10,000 py. When restricted to fragility fractures (hip, spine, rib, humerus, radius/ulna or pelvis) at 50+ years, the rates were 38.4 and 98.6 per 10,000 py in men and women respectively.
Table 1.
Fracture incidence rates in men and women aged 18-49 years, 1988-2012
| Men | Women | Both | ||||
|---|---|---|---|---|---|---|
| Fracture site | No. of cases | Rate per 10,000 py | No. of cases | Rate per 10,000 py | No. of cases | Rate per 10,000 py |
| Any | 121219 | 94.8 | 78265 | 54.3 | 199484 | 73.3 |
| Fragility | 37508 | 24.3 | 26813 | 17.2 | 64321 | 20.7 |
| FRAX | 29675 | 19.1 | 22865 | 14.6 | 52540 | 16.8 |
| Hip only | 990 | 0.6 | 530 | 0.3 | 1520 | 0.5 |
| Radius/ulna | 17420 | 11.0 | 14481 | 9.1 | 31901 | 10.1 |
| Carpus | 47901 | 30.9 | 17343 | 10.8 | 65244 | 20.7 |
| Tibia/fibula | 12011 | 7.4 | 5738 | 3.5 | 17749 | 5.5 |
| Ankle | 14551 | 8.9 | 9837 | 6.1 | 24388 | 7.5 |
| Foot | 20114 | 12.4 | 18924 | 11.8 | 39038 | 12.1 |
| Femur/hip | 2287 | 1.4 | 971 | 0.6 | 3258 | 1.0 |
| Ribs | 8662 | 5.2 | 3842 | 2.4 | 12504 | 3.8 |
| Humerus | 10024 | 6.2 | 7153 | 4.4 | 17177 | 5.3 |
| Skull | 17684 | 11.0 | 4595 | 2.8 | 22279 | 6.9 |
| Clinical vertebral | 2949 | 1.8 | 2078 | 1.3 | 5027 | 1.5 |
| Clavicle | 8377 | 5.1 | 2278 | 1.4 | 10655 | 3.3 |
| Pelvis | 1049 | 0.6 | 926 | 0.6 | 1975 | 0.6 |
| Patella | 1224 | 0.7 | 637 | 0.4 | 1861 | 0.6 |
| Scapula | 1409 | 0.8 | 480 | 0.3 | 1889 | 0.6 |
Table 2.
Fracture incidence rates in men and women aged 50+ years, 1988-2012
| Men | Women | Both | ||||
|---|---|---|---|---|---|---|
| Fracture site | No. of cases | Rate per 10,000 py | No. of cases | Rate per 10,000 py | No. of cases | Rate per 10,000 py |
| Any | 75351 | 71.8 | 185267 | 155.4 | 260618 | 116.3 |
| Fragility | 45660 | 38.4 | 128524 | 98.6 | 174184 | 69.9 |
| FRAX | 36561 | 30.3 | 119021 | 90.4 | 155582 | 61.7 |
| Hip only | 12411 | 9.9 | 40198 | 28.2 | 52609 | 19.6 |
| Radius/ulna | 10931 | 8.9 | 54081 | 39.7 | 65012 | 25.1 |
| Carpus | 12022 | 9.8 | 20961 | 14.7 | 32983 | 12.5 |
| Tibia/fibula | 5584 | 4.5 | 11911 | 8.3 | 17495 | 6.5 |
| Ankle | 8009 | 6.4 | 19688 | 13.9 | 27697 | 10.4 |
| Foot | 8298 | 6.7 | 19662 | 13.9 | 27960 | 10.5 |
| Femur/hip | 14263 | 11.3 | 45727 | 32.1 | 59990 | 22.4 |
| Ribs | 10047 | 8.0 | 9341 | 6.5 | 19388 | 7.2 |
| Humerus | 9829 | 7.9 | 30686 | 21.7 | 40515 | 15.2 |
| Skull | 3410 | 2.7 | 4266 | 3.0 | 7676 | 2.9 |
| Clinical vertebral | 5747 | 4.6 | 13485 | 9.4 | 19232 | 7.1 |
| Clavicle | 3770 | 3.0 | 4478 | 3.1 | 8248 | 3.1 |
| Pelvis | 2059 | 1.6 | 8842 | 6.1 | 10901 | 4.0 |
| Patella | 1088 | 0.9 | 2865 | 2.0 | 3953 | 1.5 |
| Scapula | 1167 | 0.9 | 1729 | 1.2 | 2896 | 1.1 |
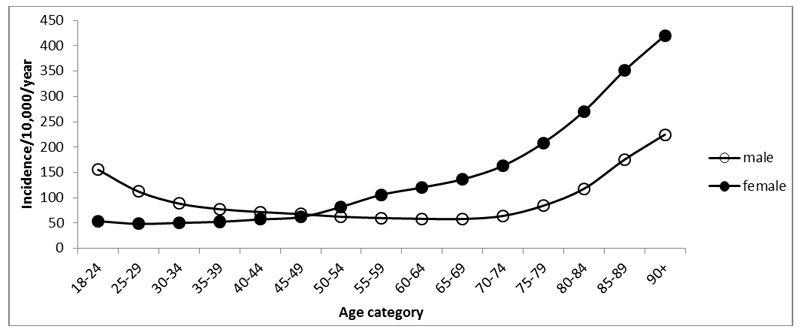
Figure 1 summarises the age- and sex- specific incidence rates for all fractures within the cohort. Fracture incidence was greater among men than women until age 50-54 years when the sex ratio reversed. In men aged 18-24 years, the annual fracture incidence was 155.3 per 10,000 py, gradually decreasing to a minimum of 58.2 per 10,000 py at age 60-64 years followed by a plateau and then a rise from age 75-79 years to an incidence of 224.8 per 10,000 py at 90+ years. Among women aged 18-24 years incidence was 54.0 per 10,000 py, increasing exponentially above 50 years such that, at 50-54 years the incidence was 82.0 per 10,000 py and above 90 years it was 420.4 per 10,000 py.
Figure 1.
Age- and sex-specific fracture incidence rate at any site among adults, 1988-2012
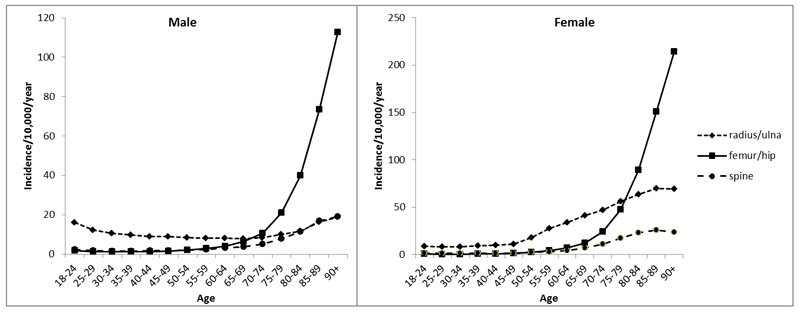
Figure 2, Online Supplementary Table 1 and Online Supplementary Figure 1 summarise the age- and sex- specific incidence rates for individual fracture types by 5 year age bands and clearly demonstrate heterogeneity across fracture sites. Fractures at the radius/ulna, humerus, clavicle, femur/hip, vertebrae and pelvis all tended to become more frequent at older ages with a tendency towards an exponential rise at ages above 70 years. This was particularly marked in women, and indeed the incidence of radius/ulna fractures remained relatively constant across all ages in men. Fractures of the carpus, skull, tibia/fibula and foot in men were more frequent at youngest ages and decreased with increasing age. These patterns contrasted to those in women where there was a gradual rise with age for fractures of the carpus and tibia/fibula but with fractures at the ankle and foot being most common around 50 to 60 years. Rib fractures appeared marginally more frequent in women than men at all ages and rising gradually with age in both sexes.
Figure 2.
Age and sex specific incidence rates of fracture at the femur/hip, radius/ulna, and spine 1988-2012
Regional variation in fracture incidence
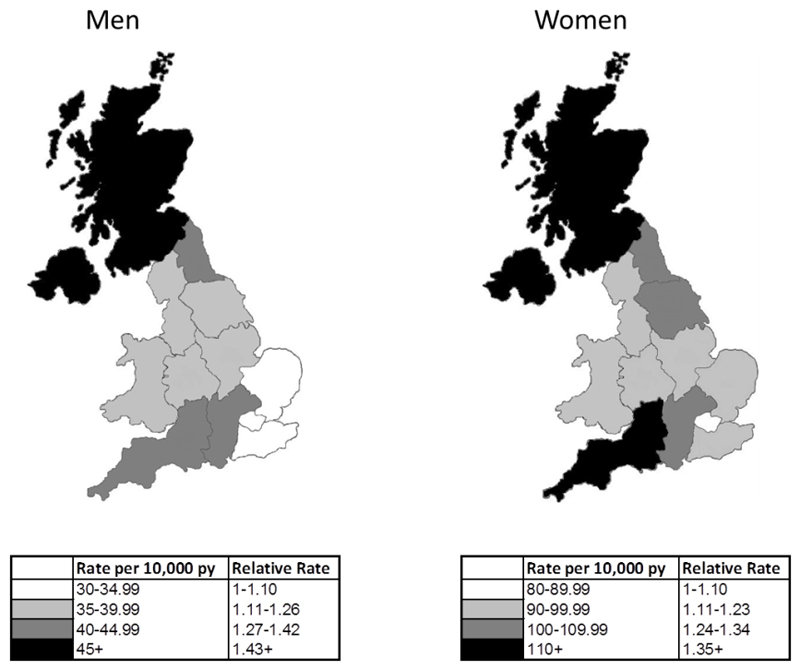
There was significant regional variation in the rates of fragility fractures, summarised in table 3, in which the incidence rates in men and women at 50+ years are stratified by region of the UK, ranked by incidence. The lowest incidence of fragility fractures was observed in London (82/10,000 py in women, 32/10,000 py in men), the East of England and South East coast, and highest in the South West, Northern Ireland and Scotland. Incidence of fragility fractures amongst women at 50+ years in Scotland (119/10,000 py) was 46% higher than that of London (Figure 3).
Table 3.
Regional variation in hip fracture incidence, and incidence of any fracture in men and women aged 50+ years in the UK, ranked in order of increasing incidence.
Regional variation in spine, wrist, and fragility fracture (spine, hip, wrist, rib, pelvis, and humerus) incidence is supplied in Online Supplementary Material Table 2.
| Men aged 50+ | Women aged 50+ | |||||
|---|---|---|---|---|---|---|
| Region | No of cases | Rate / 10,000 py |
Region | No of cases | Rate / 10,000 py |
|
|
Femur/ Hip |
London | 1052 | 9.06 | London | 3420 | 25.82 |
| East of England | 1272 | 10.21 | North West | 5367 | 29.13 | |
| West Midlands | 1233 | 10.70 | West Midlands | 3902 | 30.18 | |
| North West | 1742 | 10.75 | South East Coast | 4402 | 30.36 | |
| South East Coast | 1350 | 10.75 | East of England | 4315 | 30.93 | |
| East Midlands | 613 | 10.92 | Wales | 3919 | 31.93 | |
| Yorks & The Humber | 610 | 11.20 | East Midlands | 2012 | 32.34 | |
| Wales | 1227 | 11.31 | Yorks & The Humber | 2178 | 34.65 | |
| South Central | 1713 | 12.85 | North East | 988 | 35.01 | |
| North East | 316 | 12.89 | South Central | 5439 | 36.91 | |
| South West | 1547 | 14.17 | Scotland | 4372 | 37.12 | |
| Scotland | 1517 | 14.68 | South West | 4954 | 39.79 | |
| Northern Ireland | 574 | 15.57 | Northern Ireland | 1815 | 41.64 | |
| All fractures | London | 6079 | 59.12 | London | 15371 | 133.56 |
| East of England | 6951 | 65.30 | East of England | 17294 | 145.98 | |
| East Midlands | 3168 | 66.53 | West Midlands | 15933 | 148.96 | |
| South East Coast | 7225 | 67.24 | East Midlands | 7928 | 149.26 | |
| West Midlands | 6614 | 69.26 | South East Coast | 18610 | 150.53 | |
| South Central | 7833 | 71.61 | North West | 24386 | 158.93 | |
| Yorks & The Humber | 3321 | 72.04 | South Central | 19417 | 159.41 | |
| North West | 10049 | 74.93 | Wales | 16959 | 164.63 | |
| South West | 6923 | 76.34 | Yorks & The Humber | 8764 | 166.12 | |
| Wales | 6978 | 76.72 | South West | 17365 | 168.03 | |
| North East | 1596 | 80.94 | North East | 3966 | 173.33 | |
| Scotland | 6805 | 86.71 | Scotland | 16615 | 179.11 | |
| Northern Ireland | 2804 | 95.18 | Northern Ireland | 6488 | 183.34 | |
Figure 3.
Regional variation in fragility fracture (spine, hip, wrist, rib, pelvis, and humerus) incidence in men and women aged 50+ years within the UK. Relative rates of fracture are displayed in comparison to London.
Fracture incidence and ethnicity
There was considerable variation in the rates of fragility fracture and all fractures by ethnicity, as shown in table 4. Differences by ethnicity were more pronounced for fragility fractures than any type of fracture. The lowest rates of fracture were observed in black individuals of both sexes and thus rates of fragility fracture in white women were 4.7 times greater than in black women and 2.7 times greater in white men than black men. Men of mixed ethnicity had a fracture rate very similar to that of black men, whereas women of mixed ethnicity had more than double the fracture rate of black women. South Asian men had a higher fracture rate than those of black men and men of mixed ethnicity, whilst South Asian women had a lower fracture rate than women of mixed ethnicity. More pronounced differences in fracture incidence by ethnicity were observed when individual fragility fractures were considered. Hip fractures rates were 2.7 times greater in white men than black men (12.27 versus 4.57 per 10,000 py), and 5 times greater in white women than black women (32.61 versus 6.45 per 10,000 py respectively). Those of mixed or South Asian ethnicity had hip fracture rates of less than half that of individuals of white ethnicity.
Table 4.
Incidence of fragility fractures per 10,000 py by ethnicity in men and women 50+ years in the UK, 1988 to 2012.
| Men aged 50+ | Women aged 50+ | All persons aged 50+ | |||||
|---|---|---|---|---|---|---|---|
| Fracture type | Ethnicity | Number of cases | Rate per 10,000 py |
Number of cases | Rate per 10,000 py |
Number of cases | Rate per 10,000 py |
| All | Black | 206 | 39.17 | 369 | 57.84 | 575 | 49.40 |
| Mixed | 53 | 45.96 | 143 | 98.96 | 196 | 75.43 | |
| Other | 299 | 55.11 | 736 | 112.60 | 1035 | 86.52 | |
| S Asian | 577 | 57.21 | 946 | 91.05 | 1523 | 74.38 | |
| Unknown | 33627 | 66.02 | 84278 | 150.41 | 117905 | 110.23 | |
| White | 41584 | 78.83 | 102624 | 166.18 | 144208 | 125.94 | |
| Fragility | Black | 88 | 15.75 | 149 | 22.26 | 237 | 19.30 |
| Mixed | 22 | 17.37 | 77 | 50.12 | 99 | 35.32 | |
| Other | 170 | 28.88 | 496 | 70.98 | 666 | 51.73 | |
| S Asian | 289 | 26.85 | 491 | 44.46 | 780 | 35.77 | |
| Unknown | 20713 | 36.27 | 59328 | 97.53 | 80041 | 67.87 | |
| White | 25285 | 41.74 | 71081 | 104.03 | 96366 | 74.76 | |
|
Radius/ Ulna |
Black | 26 | 4.60 | 62 | 9.19 | 88 | 7.10 |
| Mixed | 3 | 2.32 | 31 | 19.79 | 34 | 11.89 | |
| Other | 37 | 6.13 | 206 | 28.59 | 243 | 18.36 | |
| S Asian | 78 | 7.13 | 200 | 17.76 | 278 | 12.52 | |
| Unknown | 4745 | 8.04 | 24402 | 38.43 | 29147 | 23.79 | |
| White | 6106 | 9.70 | 30278 | 42.28 | 36384 | 27.04 | |
| Spine | Black | 14 | 2.45 | 18 | 2.64 | 32 | 2.55 |
| Mixed | 7 | 5.36 | 7 | 4.38 | 14 | 4.82 | |
| Other | 27 | 4.42 | 51 | 6.86 | 78 | 5.76 | |
| S Asian | 53 | 4.79 | 80 | 6.98 | 133 | 5.90 | |
| Unknown | 2611 | 4.32 | 6143 | 9.20 | 8754 | 6.88 | |
| White | 3249 | 5.03 | 7701 | 10.13 | 10950 | 7.79 | |
|
Femur/ Hip |
Black | 26 | 4.57 | 44 | 6.45 | 70 | 5.59 |
| Mixed | 4 | 3.07 | 14 | 8.77 | 18 | 6.21 | |
| Other | 49 | 8.04 | 160 | 21.63 | 209 | 15.49 | |
| S Asian | 68 | 6.15 | 115 | 10.03 | 183 | 8.13 | |
| Unknown | 6718 | 11.16 | 22230 | 33.66 | 28948 | 22.93 | |
| White | 7901 | 12.27 | 24520 | 32.61 | 32421 | 23.23 | |
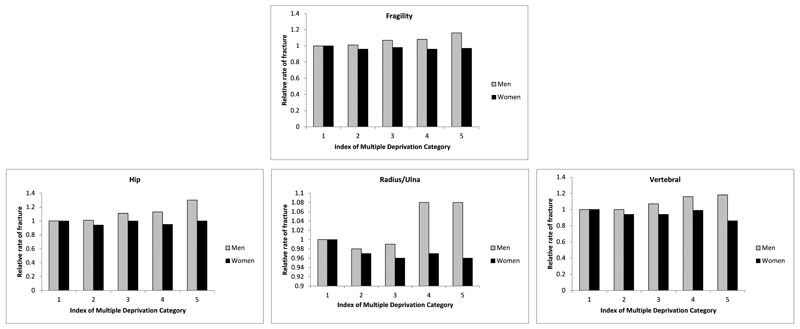
Fragility fracture incidence and socioeconomic deprivation
The relative risk of hip fractures, wrist and vertebral fractures increased with increasing levels of deprivation in men as shown in Figure 4, and Online Supplementary Table 2. The strongest association with deprivation and increased fracture risk was observed in hip fracture, with a relative risk of 1.3 (95% CI 1.21-1.41) in IMD category 5, representing the most deprived, compared to category 1. However, this trend was not observed in women, with no increase in relative risk of fracture in hip or wrist fractures. Indeed there was a trend towards decreased vertebral fracture risk with increasing levels of deprivation, with a relative risk of 0.86 (95% CI 0.79-0.94) in IMD category 5 compared to IMD category 1.
Figure 4.
Fragility, Hip, Radius/Ulna and Vertebral Fracture incidence relative rates to index of multiple deprivation (IMD) category 1 (least deprived) in men and women aged 50+ in the UK, 1988-2012.
Discussion
Summary of findings
In this population-based study, we have documented age- and sex- specific patterns of fracture consistent with those from our previous study in 2001, using the General Practice Research Database[4]. In our analysis to 2012, additional stratification demonstrated marked differences in fracture incidence according to the geographic location within the UK, ethnicity, and socioeconomic status.
Limitations
The CPRD is a large database of anonymised medical records from general practitioners, with a sample covering 6.9% of the UK population, and is broadly representative of the population in terms of age, sex and ethnicity. However there are some limitations which should be considered: firstly, although many fracture types are accurately recorded, vertebral and rib fractures often go undetected and it is likely that the rates for these fractures are underestimates. Secondly, owing to the temporal structure of CPRD, it was not possible to reliably distinguish second from first fractures of any particular type. Thus only first fractures are included and so the true impact of fractures is likely to be greater than that documented in our analysis. Thirdly, representativeness of the dataset when stratified by geographic region, ethnicity and socioeconomic status has not been documented, and variation in the density of sampling according to the strata may have influenced these results. In addition, primary care data on less widely reported measures such as ethnicity and social deprivation may be missing on some individuals with fractures. Indeed, there were a substantial number of individuals with “unknown” ethnicity, which may have led to a reduced recorded incidence of fractures in some minority ethnic groupings. Finally, the degree of trauma leading to a fracture is not reliably captured in CPRD and thus it was not possible to definitively categorise fractures into low or high trauma. However the expected variation with age and sex was observed for fracture types classically associated with bone fragility.
Comparison with European Populations
The incidence rates we report are broadly comparable to those documented in previous UK studies, which have been mostly confined to smaller, well defined populations in Leicestershire[18], Dundee[19], Oxford[19, 20], Cardiff[21] and Edinburgh[22]. Across Europe[6], the incidence of hip fracture in our study (32.1 per 10,000py in women aged 50+ years) is roughly equal to the incidence in Italy (33.4 per 10,000py), higher than that of the Netherlands (28.8 per 10,000 py) and Spain (22.8 per 10,000 py), lower than that of Scandinavian nations (for example: Norway 56.3 per 10,000 py).
Trends in fracture incidence by age and sex
Our findings are consistent with the vast majority of similar studies, which have suggested that fracture incidence is bimodal, with peaks in the second and third decades (predominantly in men) and in the elderly[22, 23]. These patterns attest to the role of trauma at younger ages, and bone fragility at older ages, in the pathogenesis of fracture. Such patterns demonstrated some specificity to individual fracture types. For example, rates of skull, carpus, clavicle, ankle and lower leg fracture, all classically associated with high trauma such as road traffic accidents, were particularly high in young males; in contrast hip fractures were uncommon at young ages in both sexes, and incidence rates increased exponentially with age. Sexual dimorphism of fractures was very pronounced in certain fractures, particularly of the distal forearm, which remained low throughout life for men but increased rapidly from the perimenopausal period in women (at age 60-64 years for example, rates were 8.1 per 10,000 py in men and 34 per 10,000 py in women). This pattern is similar to that observed in the EPOS study, in which the age-adjusted incidence, age 35 years at over, of distal forearm fracture was 36.8/10,000 py in women and 9.0/10,000 py in men[24]. In older women, the rate of femur/hip fractures was twice that of men (incidence in women aged 80-84 years, 89.4 per 10,000 py, compared to 40.1 per 10,000 py in men of the same age). Differences in bone structure, both in terms of macro- and microarchitecture, geometry and mineralisation, together with differences in lifestyle, comorbidities and falls risks by sex may account for such differences[25‒29].
Region and socioeconomic status
Stratification by region within the UK revealed substantial geographic heterogeneity in age- and sex- adjusted fracture incidence, with rates in Scotland almost 50% greater than those in London and the South-East. The observed patterns appear to match, at least in part, those of socioeconomic status across the country, with deprivation levels on average being higher in Northern England, Scotland and South Wales than in Southern and Eastern England[30]. Northern Ireland, Northern England, Scotland and Wales have a larger rural population than London, the South East of England and the East Midlands with the lowest incidence of fracture. Investigators in the US have shown that fracture risk was greater in the more rural, southern regions, compared with the more urbanised northern regions[31], with other European studies demonstrating the converse[32–34]. Rural or urban living is unlikely to be the underlying explanation for these regional differences, whereas deprivation and associated lifestyle factors may underlie this heterogeneity.
The strongest association with deprivation and increased fracture risk was seen in hip fracture in men, with a relative risk of 1.3 (95% CI 1.21-1.41) in IMD category 5 (representing the most deprived) compared to category 1. Our observed associations between socioeconomic status and fracture incidence in CPRD are consistent with evidence from other cohorts[7, 10–12]. High prevalence of adverse lifestyle habits such as smoking and excessive alcohol intake, together with poorer dietary quality, all cluster with lower socioeconomic status [7, 10, 11, 35], and given documented adverse effects on bone health[36], are likely to contribute to the geographic and socioeconomic variation in fracture incidence across the UK. A similar finding of greater association between deprivation and fracture risk in men than women has been documented in Australia[11], and possible explanations include the different magnitude of lifestyle habits between men and women, and greater frequency of traumatic events in men than women in low compared with high socioeconomic status groups. The prevalence of obesity is also greater amongst populations of lower, compared with higher, socioeconomic status but this would be expected to have diverging effects on fracture incidence dependent on fracture site. For example a recent meta-analysis demonstrated that obesity is protective for hip fracture but associated with increased risk of ankle fracture[37]. Indeed in a recent study from Spain, associations between socio-economic status and fracture hip fracture risk were substantially attenuated after adjustment for body mass index[12]. Although the majority of hip fractures occur as a result of falls indoors, rather than slipping on icy pavements[23], their incidence increases with latitude, and also varies with season, both attributes which suggest a potential role for vitamin D insufficiency in fracture pathogenesis, particularly at more northerly climes[6, 38].
Ethnicity
We observed marked differences in fracture incidence according to ethnicity. Our findings of lowest rates of fracture amongst black individuals and highest rates amongst white individuals, with the South Asian population experiencing an intermediate fracture rate, is consistent with those from elsewhere. A study of hip fracture rates in Dundee, Scotland, Malmo, Sweden and the black population of Johannesburg, South Africa, published in 1968 demonstrated similar differences in hip fracture rates by ethnicity, with fracture rates in Dundee females being approximately 8 times greater than black South African females[39]. Our findings were also mirrored by a Californian study of hip fracture rates, which demonstrated fracture rates of 14.1 per 10,000 py in white women over 50 years of age (32.6 per 10,000 py in the CPRD), 5.7 per 10,000 py in black women (6.45 per 10,000 py in the CPRD) and 8.5 per 10,000 py in Asian women (10.0 per 10,000 py in the CPRD)[40]. Amongst other ethnic groups, a Canadian study of first Nations people suggested higher risks of fracture within this ethnic group compared with non-First Nations people[41], and in Singapore, Chinese men and women had higher rates of hip fracture than did Indian or Malay individuals[42].
Differences in BMD by ethnicity have been demonstrated, as have differences in bone geometry and bone microarchitecture. Thus, for example, femoral neck BMD was shown to be 13.3% higher in black men than white men in a study of 1200 men from Boston, USA[43], resulting from variation in both peak bone mass and age related skeletal loss after peak bone mass has been attained. Lower BMD in Chinese than Malay or Indian men[44], and lower BMD in Chinese and Malay women compared with Indian women in Singapore[45], have been demonstrated; in a recent multi-cohort study, despite differences in both fracture rate and BMD by ethnicity, the relationship between BMD and fracture risk appeared relatively homogeneous across ethnic groups[9]. Studies using hip strength analysis[46] and CT scanning[47] have demonstrated differences in proximal femoral geometry (shorter, wider femoral neck in black than white individuals) which are associated with lower risk of hip fracture. More recently, use of high resolution pQCT has demonstrated differences in the bone microarchitecture of African American and Caucasian women. African American women had larger and denser bones than Caucasians, and although differences in trabecular thickness were observed, differences in cortical microarchitecture were most pronounced with higher cortical area, thickness and volumes in African Americans at both radius and tibia, and reduced cortical porosity at the tibia. These differences persisted after adjustment for bone mineral density assessed by DXA[48].
Differences in height and body composition between different ethnic groups may also partly explain the differences in fracture rates, with white individuals being generally taller than Asian and Black individuals, as demonstrated by data from the NHANES cohort[49]. Apparent differences in bone mineral content and bone mineral density between New Zealand Pacific Island and European children were explained by differences in height and weight in one study[50]. Body height has been shown to have an independent influence on hip fracture rates, with taller individuals at greater risk[51]. Distributions of populations of different ethnicity throughout the UK may also contribute to the finding that the lowest rates of fracture in the UK are present in London. In the 2011 census, the proportion of residents in the capital identifying themselves as of white ethnicity was 59.8%, in comparison with over 80% in other regions of England and Wales, therefore, as a population, being at lower risk of fracture[30].
Conclusion
In conclusion, we have documented up to date age- and sex- specific fracture rates for the UK. Previously noted trends in fracture incidence by age and site of fracture have been confirmed, and we also observed marked variation in fracture incidence by geographic location within the UK, ethnic group, and socioeconomic status. Understanding the reasons for variations in fracture rates will be important for allocation of healthcare provision, particularly in regions with the highest fracture rates and in populations most at risk in the UK and elsewhere in the world. It will also aid the implementation and design of strategies to reduce fracture incidence and its impact on individuals, health services and societies as a whole.
Supplementary Material
Highlights.
We used CRPD to document the epidemiology of fractures in the UK from 1988 to 2012, stratifying fracture incidence by age, sex, geographic location, ethnicity and socioeconomic status.
The incidence of any fracture was 94.8 per 10,000 person-years of follow up (py) in men aged 18-49 years, in comparison to 54.3 per 10,000 py in women aged 18-49 years. In men aged 50+ years, the overall rate of fracture was reduced to 71.8 per 10,000 py whereas in women 50+ years it almost tripled to 155.4 per 10,000 py.
There was substantial geographic heterogeneity in age- and sex- adjusted fracture incidence, with rates in Scotland almost 50% greater than those in London and South East England. Lowest rates of fracture were observed in black individuals of both sexes; rates of fragility fracture in white women were 4.7 times greater than in black women. Strong associations between deprivation and fracture risk were observed in hip fracture in men.
These findings may inform public health policy in UK and elsewhere.
Acknowledgements
CC and NCH are joint senior author. EMC is supported by the NIHR. The work was supported by a grant from the National Osteoporosis Society. This work was further supported by grants from the Medical Research Council, British Heart Foundation, Arthritis Research UK, National Institute for Health Research (NIHR) Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, and NIHR Musculoskeletal Biomedical Research Unit, University of Oxford.
Footnotes
Conflicts of Interest
All authors report no conflicts of interest.
References
- 1.Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. OsteoporosInt. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 3.Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville MD: 2004. [PubMed] [Google Scholar]
- 4.van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29:517–22. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- 5.Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden : A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239–56. doi: 10.1007/s00198-012-1964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cauley JA, Chalhoub D, Kassem AM, Fuleihan Gel H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10:338–51. doi: 10.1038/nrendo.2014.51. [DOI] [PubMed] [Google Scholar]
- 8.Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27:2325–32. doi: 10.1002/jbmr.1684. [DOI] [PubMed] [Google Scholar]
- 9.Shin MH, Zmuda JM, Barrett-Connor E, Sheu Y, Patrick AL, Leung PC, Kwok A, Kweon SS, Nam HS, Cauley JA. Race/ethnic differences in associations between bone mineral density and fracture history in older men. Osteoporos Int. 2014;25:837–45. doi: 10.1007/s00198-013-2503-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bacon WE, Hadden WC. Occurrence of hip fractures and socioeconomic position. J Aging Health. 2000;12:193–203. doi: 10.1177/089826430001200203. [DOI] [PubMed] [Google Scholar]
- 11.Brennan SL, Holloway KL, Williams LJ, Kotowicz MA, Bucki-Smith G, Moloney DJ, Dobbins AG, Timney EN, Pasco JA. The social gradient of fractures at any skeletal site in men and women: data from the Geelong Osteoporosis Study Fracture Grid. Osteoporos Int. 2015;26:1351–9. doi: 10.1007/s00198-014-3004-y. [DOI] [PubMed] [Google Scholar]
- 12.Reyes C, Garcia-Gil M, Elorza JM, Fina-Aviles F, Mendez-Boo L, Hermosilla E, Coma E, Carbonell C, Medina-Peralta M, Ramos R, Bolibar B, et al. Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone. 2015;73:127–31. doi: 10.1016/j.bone.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA. Secular trends in the incidence of hip and other osteoporotic fractures. OsteoporosInt. 2011;22:1277–1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, Smeeth L. Data Resource Profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015 doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Staa TP, Abenhaim L, Cooper C, Zhang B, Leufkens HG. The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf. 2000;9:359–66. doi: 10.1002/1099-1557(200009/10)9:5<359::AID-PDS507>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 16.Mathur R, Bhaskaran K, Chaturvedi N, Leon DA, vanStaa T, Grundy E, Smeeth L. Completeness and usability of ethnicity data in UK-based primary care and hospital databases. J Public Health (Oxf) 2014;36:684–92. doi: 10.1093/pubmed/fdt116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dedman D. Measures of area-based deprivation linked via patient postcode: Linkage Set 10: Documentation and Data Dictionary. London: 2014. [Google Scholar]
- 18.Donaldson LJ, Cook A, Thomson RG. Incidence of fractures in a geographically defined population. J Epidemiol Community Health. 1990;44:241–5. doi: 10.1136/jech.44.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knowelden J, Buhr AJ, Dunbar O. INCIDENCE OF FRACTURES IN PERSONS OVER 35 YEARS OF AGE. A REPORT TO THE M.R.C. WORKING PARTY ON FRACTURES IN THE ELDERLY. Br J Prev Soc Med. 1964;18:130–41. doi: 10.1136/jech.18.3.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buhr AJ, Cooke AM. Fracture patterns. Lancet. 1959;1:531–6. doi: 10.1016/s0140-6736(59)92306-2. [DOI] [PubMed] [Google Scholar]
- 21.Johansen A, Evans RJ, Stone MD, Richmond PW, Lo SV, Woodhouse KW. Fracture incidence in England and Wales: a study based on the population of Cardiff. Injury. 1997;28:655–660. doi: 10.1016/s0020-1383(97)00144-7. [DOI] [PubMed] [Google Scholar]
- 22.Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80:243–248. doi: 10.1302/0301-620x.80b2.7762. [DOI] [PubMed] [Google Scholar]
- 23.Harvey N, Dennison E, Cooper C. Osteoporosis: impact on health and economics. NatRevRheumatol. 2010;6:99–105. doi: 10.1038/nrrheum.2009.260. [DOI] [PubMed] [Google Scholar]
- 24.Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ, Reeve J, Banzer D, Benevolenskaya LI, Bhalla A, Bruges AJ, Cannata JB, et al. Incidence of limb fracture across Europe: results from the European Prospective Osteoporosis Study (EPOS) OsteoporosInt. 2002;13:565–571. doi: 10.1007/s001980200074. [DOI] [PubMed] [Google Scholar]
- 25.Clark MK, Sowers MF, Dekordi F, Nichols S. Bone mineral density and fractures among alcohol-dependent women in treatment and in recovery. Osteoporos Int. 2003;14:396–403. doi: 10.1007/s00198-003-1387-2. [DOI] [PubMed] [Google Scholar]
- 26.Hansen S, Shanbhogue V, Folkestad L, Nielsen M, Brixen K. Bone Microarchitecture and Estimated Strength in 499 Adult Danish Women and Men: A Cross-Sectional, Population-Based High-Resolution Peripheral Quantitative Computed Tomographic Study on Peak Bone Structure. Calcified Tissue International. 2014;94:269–281. doi: 10.1007/s00223-013-9808-5. [DOI] [PubMed] [Google Scholar]
- 27.Hind K, Gannon L, Whatley E, Cooke C. Sexual dimorphism of femoral neck cross-sectional bone geometry in athletes and non-athletes: a hip structural analysis study. J Bone Miner Metab. 2012;30:454–60. doi: 10.1007/s00774-011-0339-8. [DOI] [PubMed] [Google Scholar]
- 28.Zhang F, Tan LJ, Lei SF, Deng HW. The differences of femoral neck geometric parameters: effects of age, gender and race. Osteoporos Int. 2010;21:1205–14. doi: 10.1007/s00198-009-1057-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang VC, Do MT. Risk factors for falls among seniors: implications of gender. Am J Epidemiol. 2015;181:521–31. doi: 10.1093/aje/kwu268. [DOI] [PubMed] [Google Scholar]
- 30.ONS. UK Census. 2011 [Google Scholar]
- 31.Hinton RY, Lennox DW, Ebert FR, Jacobsen SJ, Smith GS. Relative rates of fracture of the hip in the United States Geographic, sex, and age variations. J Bone Joint Surg Am. 1995;77:695–702. doi: 10.2106/00004623-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Falch JA, Aho H, Berglund K, Duppe H, Finsen V, Hagstrom I, Jarvinen M, Johnell O, Kaastad TS, Lauritzen JB. Hip fractures in Nordic cities: difference in incidence. Ann Chir Gynaecol. 1995;84:286–290. [PubMed] [Google Scholar]
- 33.Rosengren BE, Ahlborg HG, Gardsell P, Sernbo I, Nilsson JA, Daly RM, Karlsson MK. Forearm bone mineral density and incidence of hip fractures in Swedish urban and rural men 1987-2002. Scand J Public Health. 2012;40:102–8. doi: 10.1177/1403494811425604. [DOI] [PubMed] [Google Scholar]
- 34.Kaastad TS, Meyer HE, Falch JA. Incidence of Hip Fracture in Oslo, Norway: Differences Within the City. Bone. 1998;22:175–178. doi: 10.1016/s8756-3282(97)00247-0. [DOI] [PubMed] [Google Scholar]
- 35.Benetou V, Orfanos P, Feskanich D, Michaelsson K, Pettersson-Kymmer U, Ahmed LA, Peasey A, Wolk A, Brenner H, Bobak M, Wilsgaard T, et al. Education, marital status, and risk of hip fractures in older men and women: the CHANCES project. Osteoporos Int. 2015;26:1733–46. doi: 10.1007/s00198-015-3054-9. [DOI] [PubMed] [Google Scholar]
- 36.Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57. doi: 10.1007/s00198-012-2074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johansson H, Kanis JA, Oden A, McCloskey E, Chapurlat RD, Christiansen C, Cummings SR, Diez-Perez A, Eisman JA, Fujiwara S, Gluer CC, et al. A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res. 2014;29:223–33. doi: 10.1002/jbmr.2017. [DOI] [PubMed] [Google Scholar]
- 38.Oden A, Kanis JA, McCloskey EV, Johansson H. The effect of latitude on the risk and seasonal variation in hip fracture in Sweden. J Bone Miner Res. 2014;29:2217–23. doi: 10.1002/jbmr.2250. [DOI] [PubMed] [Google Scholar]
- 39.Solomon L. Osteoporosis and fracture of the femoral neck in the South African Bantu. J Bone Joint Surg Br. 1968;50:2–13. [PubMed] [Google Scholar]
- 40.Silverman SL, Madison RE. Decreased incidence of hip fracture in Hispanics, Asians, and blacks: California Hospital Discharge Data. American Journal of Public Health. 1988;78:1482–1483. doi: 10.2105/ajph.78.11.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leslie WD, Derksen S, Metge C, Lix LM, Salamon EA, Wood Steiman P, Roos LL. Fracture risk among First Nations people: a retrospective matched cohort study. CMAJ. 2004;171:869–73. doi: 10.1503/cmaj.1031624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koh LK, Saw SM, Lee JJ, Leong KH, Lee J. Hip fracture incidence rates in Singapore 1991-1998. Osteoporos Int. 2001;12:311–8. doi: 10.1007/s001980170121. [DOI] [PubMed] [Google Scholar]
- 43.Araujo AB, Travison TG, Harris SS, Holick MF, Turner AK, McKinlay JB. Race/ethnic differences in bone mineral density in men. Osteoporos Int. 2007;18:943–53. doi: 10.1007/s00198-006-0321-9. [DOI] [PubMed] [Google Scholar]
- 44.Yang PL, Lu Y, Khoo CM, Leow MK, Khoo EY, Teo A, Lee YS, Das De S, Chong YS, Gluckman PD, Tai ES, et al. Associations between ethnicity, body composition, and bone mineral density in a Southeast Asian population. J Clin Endocrinol Metab. 2013;98:4516–23. doi: 10.1210/jc.2013-2454. [DOI] [PubMed] [Google Scholar]
- 45.Goh JC, Low SL, Das De S. Bone mineral density and hip axis length in Singapore’s multiracial population. J Clin Densitom. 2004;7:406–12. doi: 10.1385/jcd:7:4:406. [DOI] [PubMed] [Google Scholar]
- 46.Broy SB, Cauley JA, Lewiecki ME, Schousboe JT, Shepherd JA, Leslie WD. Fracture Risk Prediction by Non-BMD DXA Measures: the 2015 ISCD Official Positions Part 1: Hip Geometry. J Clin Densitom. 2015;18:287–308. doi: 10.1016/j.jocd.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 47.Shepherd JA, Schousboe JT, Broy SB, Engelke K, Leslie WD. Executive Summary of the 2015 ISCD Position Development Conference on Advanced Measures From DXA and QCT: Fracture Prediction Beyond BMD. J Clin Densitom. 2015;18:274–86. doi: 10.1016/j.jocd.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 48.Putman MS, Yu EW, Lee H, Neer RM, Schindler E, Taylor AP, Cheston E, Bouxsein ML, Finkelstein JS. Differences in skeletal microarchitecture and strength in African-American and white women. J Bone Miner Res. 2013;28:2177–85. doi: 10.1002/jbmr.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM, Jr, Hong S, Choi W. Scaling of adult body weight to height across sex and race/ethnic groups: relevance to BMI. Am J Clin Nutr. 2014;100:1455–61. doi: 10.3945/ajcn.114.088831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grant AM, Gordon FK, Ferguson EL, Williams SM, Henry TE, Toafa VM, Guthrie BE, Goulding A. Do Young New Zealand Pacific Island and European Children Differ in Bone Size or Bone Mineral? Calcif. Tissue Int. 2005;76:397–403. doi: 10.1007/s00223-004-0156-3. [DOI] [PubMed] [Google Scholar]
- 51.Meyer HE, Tverdal A, Falch JA. Risk factors for hip fracture in middle-aged Norwegian women and men. Am J Epidemiol. 1993;137:1203–11. doi: 10.1093/oxfordjournals.aje.a116622. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.