Abstract
Introduction:
Uterine lipoleiomyomas are a rare type of uterine myomas, which have been seldom diagnosed and are less known and still unusual. Histologically they are composed of smooth muscle cells with multiple fat cells and fibrous tissue. Their pathogenesis is still a stigmata and their preoperative diagnosis is still questionable.
Case report history:
A 39-year old woman presented at the University clinic for obstetrics and gynecology with complaints of a mild low abdominal and pelvic pain, increased frequency of vaginal bleeding and abdominal distension. Ultrasound examination showed dislocated uterus by a large semisolid tumor, located between the uterus and the urinary bladder. This mass was not well defined and had great vascularity. Pelvic computerized tomography revealed a large heterogeneous tumor located behind the bladder, measuring 8.5x7.5cm in size, making compression on the other pelvic organs.
Conclusion:
We should pay more attention on the preoperative imaging studies, in order to select patients who require surgery and further treatment more appropriately.
Keywords: uterus, pelvic tumor, myomas, imaging studies
1. INTRODUCTION
Uterine lipoleiomyomas are very rare, less known and unusual benign tumors. These kinds of lesions are occurring predominantly in obese perimenopausal and postmenopausal patients. They usually arise in the uterine corpus, mainly seen intramural. Rarely they can be diagnosed as subserosal or extremely rare located in the broad ligament. Specific types of uterine lipoleiomyomas are the subgroup of vascular lipoleiomyomas, which are extremely sporadic. Worldwide they are reported with an incidence of 0.03-0.2%, typically seen among postmenopausal women.
Histologically tumors known as lipoleiomyomas consist of bundles of bland, smooth muscle cells, mixed with multiple nests of mature fat cells and fibrous tissue (1-3). Uterine vascular lipoleiomyomas on the other hand have also a rich vascularization net, with vascular elements of different caliber, which originated from the small veins and arteries. Female genital tract is a rare site for occurrence of this type of vascular tumors. This tumor consists of three mesenchymal components seen in a variable proportions, mature adipose tissue, smooth muscle cells and anomalous tortuous thick-walled blood vessels, with heterogeneous morphologic subtypes (4).
The pathogenesis of the lipoleiomyomas is still unclear and not fully understood, both by the pathologists and gynecologists; although several studies have showed that they arise from metaplasia of pluripotent mesenchymal cells or by a direct metaplasia of smooth muscle cells. Uterine vascular lipoleiomymas were also found to be associated to some metabolic disorders as diabetes or hyperlipidemia and hypertriglyceridemia (5).
Lipoleiomymas are a diagnostic stigmata, their proper preoperative diagnosis is still questionable. Most of the patients are asymptomatic, but they can present with symptoms similar to regular myomas or ovarian cysts, including abdominal and/or pelvic pain, palpable pelvic mass and menstrual abnormalities. Other patients often present with hypermenorrhea.
Imaging studies in the preoperative period play an important role in identifying the nature of the tumor and its exact localization. We should always be aware that large tumors near the uterus can be mistaken in diagnosis, so unclear cases should always be confirmed on CT or MRI, which can specifically differ variant tumors. Imaging should differentially exclude: benign ovarian cysts, malignant ovarian cysts, pelvic lipomas, liposarcomas and other types of rare lipomatous uterine tumors. Most lipoleiomyomas are diagnosed in women with a history of uterine myomas.
Small asymptomatic lipoleiomyomas do not require any kind of surgical treatment, it is required and indicated in large masses and in patients complaining on menstrual abnormalities or low abdominal pain, also in diagnostically unclear cases (6, 7).
2. CASE REPORT HISTORY
A 39-year old woman presented at the University clinic for obstetrics and gynecology with complaints of a mild low abdominal and pelvic pain, increased frequency of vaginal bleeding and abdominal distension. She was diagnosed with a cystic formation in the right ovary 3 months before her visit at our clinic, since then the cyst was enlarged in size and caused additional symptoms to the patient. She was admitted to our clinic, at the department for operative gynecology for a further examinations and proper evaluation.
Gynecological history of our patient showed that she had her menarche at the age of 13 years, still with regular menstrual cycles and moderate intensity of menstrual bleeding. Her obstetric history revealed that she had two vaginal spontaneous deliveries. On detailed anamnesis she did not report any other medical condition, co-morbidities, previous surgeries or allergies. There was no family history for a malignancy of any type.
On physical examination she had normal vital signs, abdominal palpation showed mildly distended abdomen with a palpable solid mass filling mainly the right side of the pelvic cavity. No abdominal tenderness was observed. Gynecological examinations did not show any irregularities of the vulva, vaginal portion of the cervix, with no evident pathological findings detectable. Bimanual examination revealed palpable tumorous formation, mainly on the right side of the uterine body, with marked tenderness during mobilization.
All the laboratory standard hematological parameters were in referent ranges, blood count, liver function tests, coagulation parameters, urea, creatinine levels and serum electrolytes were in normal limits. Viral serology was negative and tumorous markers, such as cancer antigen 125 and carcinoembryonic antigen, were within their normal values. Cervicovaginal smear showed only inflammation.
The patient was examined with a modern ultrasound Voluson 8, both vaginally and abdominally. Transvaginal ultrasound showed posteriorly dislocated uterus with a total diameter of 5.4cm. Endometrial zone was with a diameter of 1.2cm, secretively changed, with no pathological findings. In front of the uterine body, posterior to the urinary bladder, predominantly on the right side, we detected a large semisolid tumorous formation. It was a large heteroechoic pelvic mass predominantly cystic, with a diameter of 7cmx8cm, septate, filled with thicker fluid in one part. After filling the urinary bladder with saline we excluded a vesical origin of the tumor. Doppler ultrasound study showed marked vascularity, but without pathologically changed Doppler waves. This not so well defined soft tissue lesion seemed to arise from the right ovary, but it had no distinct border with the uterus and it also seemed to spread into the right broad ligament. Left ovary was normal, right ovary was difficult to be properly showed and examined. In differential diagnosis we thought of ovarian tumor or uterine myoma.
Due to the diagnostic dilemma we also performed pelvic computerized tomography (CT). Pelvic CT showed a large tumorous heterogeneous tumorous formation which as localized behind the urinary bladder and in front of the uterus, mostly spread in the right broad ligament. The mass was oval with marked heterodensity, measuring 8.5x7.5cm in size (Figure 1). Centrally the tissue was solid, with small cystic multilocular and multifocal changes localized peripherally. In the post-contrast CT phase the tumorous formation showed high density in its central parts. The formation makes compression on the other pelvic organs but it does not infiltrate any of them. Uterus and ovaries were detected as normal. The CT did not detect enlarged lymph nodes, lymphadenopathy, or free liquid in the abdominal or pelvic cavity.
Figure 1.

Computerized tomography
Preoperative diagnosis of ovarian cystic tumor was made, although we could not exclude the possibility of degenerative uterine myoma.
Patient underwent surgery with a laparotomy via transverse abdominal incision. During operation, on inspection, we saw large white-yellowish cystic formation right in front of the uterine body, not connected to the right ovary anatomically. Macroscopically I looked like a cystic tumor localized in front of the uterine body, connected to the uterus in a small portion, but spread intraligamentary in a zone of 7cm (Figure 2, 3). The mass was totally extirpated and it was sent to a frozen section. It revealed mesenchymal tissues with highly vascularized structure, totally benign with no signs of malignancy. Due to the patients’ age and obvious benign characteristics of the tumor we did not perform hysterectomy or bilateral salpingo-oophorectomy.
Figure 2.

Intraoperative imaging
Figure 3.
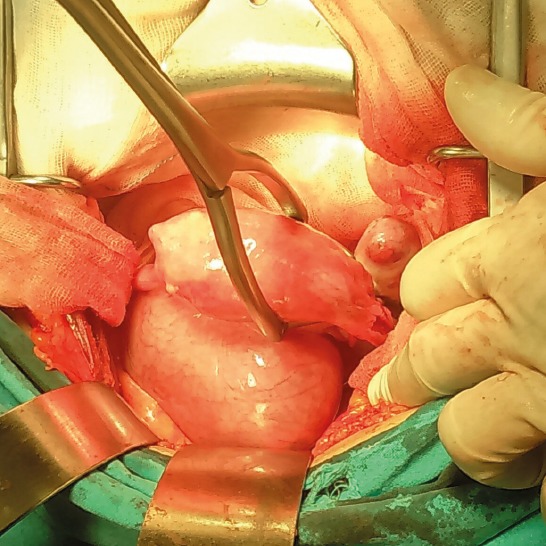
Intraoperative finding
Pathological examination of the operative material detected a well-structured nodule, measuring 8cmx8cm in diameter, with a grayish-white appearance. Macroscopically it as described as a solid tumorous tissue, with wide spread vascular net. It had a soft consistency on its cut surface. Histological examination showed a mixture of spindle-shaped smooth muscle cells, without nuclear atypia, admixed with nests of mature adipocytes. Between these muscle and adipose cells there very numerous vascular elements visible. The lipid cells very all mature, without any lipoblasts. The tumor was highly vascularized, with groups of muscle cells spread among the different sized blood vessels. All of the cells showed only benign characteristics, with no signs of malignancy, but with rare mitosis. Immunohistochemically cells were positive to Vimentin, focally positive to D-100 A4, diffusely positive to Demsin, SMA and Caldesmon, also they showed co-expression to CD100 in focus, while Calmetinin, CK, HMB45, Inhibin and S100 stayed negative. Ki67 showed very low proliferative index (<1%). Based on the above findings, the tumor was diagnosed as a benign vascular lipoleiomyoma.
The patient was hospitalized at our clinic for a total of 16 days, discharged after operation with no complications and in a stable clinical condition.
3. DISCUSSION
Lipomatous uterine tumors are an uncommon neoplasm seen in the female genital tract. Their incidence ranges from 0.03% in hysterectomy specimen to 0.2% among operative materials marked as uterine myomas. They can be located in the uterine body, cervix, broad ligament, retroperitoneum and ovaries. Pathologists categorized these tumors in three groups, pure lipomas, lipoleiomymas, angiomyolipomas or various mesodermal tissue component lesions and thirdly the rarest group including malignant neoplasms. There are different theories for vascular lipoleiomymas origin, including here misplacement of emryonic fat cells, direct metaplasia of smooth muscle cells or connective tissue into fat cells or proliferation of perivascular fat cells into blood vessel. Uterine lipoleiomyomas can be most frequently seen in postmenopausal women, aged between 50 and 70 years, making our case more unusual and unique. The majority of patients are without any symptoms, but some display symptoms of a presence of a typical uterine myoma. Imaging techniques like MRI and CT can play an important role in determining the intrauterine location and fatty nature of lipoleiomyomas, but most of these are incidental findings postoperatively on histopathology. MRI including fat suppression sequence is a useful technique to diagnose uterine lipoleiomyomas with its high sensitivity and specificity to fat and with its multi sectional ability to detect the precise location. Although, it is not often possible to differentiate uterine lipoleiomyoma with other lipomatous tumors. Differential diagnosis is often very difficult to make because the most of these lesions at the end appear to be ovarian tumors (8).
Uterine myolipomas was described first by Meis and Enzinger in the year 1991, all of them showing unique histological patterns. The differential diagnosis of these lipomatous masses in the pelvic cavity includes benign cystic teratomas, malignant degeneration of cystic teratoma, non-teratomatous lipomatous ovarian tumor, benign pelvic lipomas, liposaromas and lipoblastic lymphadenopathy. It has been reported in literature that lipomatous uterine tumors and endometrial carcinomas can be associated, especially lipoleiosarcomas arising in uterine lipoleiomyomas. The pathogenesis of these tumors remains still unknown, immunohistochemical and cytochemical studies only confirm the complex genesis of them, arising from mesenchymal immature cells (9).
Sonographycally uterine lipoleiomyomas appear as a hyperechoic mass with hypoechoic ring, which usually present the myometrial layer that surrounds the fatty tissue. CT describes this lesions more specific, as well structured, circumscribed, with fatty and non-fatty areas. On MRI lipomatous nature of the tissue is suggested by a high signal intensity on T1 images. These tumors should be managed surgically, both with hysterectomy or only extirpation of the tumor, due to several factors as patients’ age, severity of the symptoms, fertility desire, site of the mass and associated uterine myomas (10, 11).
Lipoliomyomas are usually intramural in location, but their well-defined lobular mass can be localized also submucosal or subserosal. They show a typical sonographycally seen halo around the lesion, which represents a flattened myometrial tissue. Lipoleiomyomas are very often diagnosed as a ovarian cystic tumors especially we face with a real diagnostic dilemma when the lesion is large in dimension making proper identification of the pelvic organs difficult, as was reported also in our case. In these cases final diagnosis is the histological study. Small asymptomatic lipoleiomymas should not be treated surgically (12, 13, 14). Lipomatous uterine tumors are very rare, and a total of 180 cases have been reported among the literature since today. All of them were diagnosed via MRI studies. MRI image with a fat-suppresion sequence is an important technique in the diagnosis of uterine lipoleiomymas, with high sensitivity and specificity. Although it is not always possible to differentiate uterine lipoleiomyoma from other uterine lipomatous tumors (angiomyolipoma, fibromyolipoma, myelolipoma, liposarcoma, and so on) on MRI, it is important to become familiar with the wide variety of MRI findings of this entity because a correct preoperative diagnosis is critical to determine appropriate treatment and to avoid unnecessary intervention (15).
It was reported that uterine lipomyomas may be linked to a different metabolic diseases, such as hyperlipidemia, hypothyroidism, and diabetes mellitus. Changes in lipid metabolism and other non-lipid mechanisms occurring during menopause may play an important role in the development of these tumors (14, 15).
Lipoleiomyomas are often misdiagnosed as an ovarian tumors. In our case, pelvic examination revealed huge pelvic mass with hard consistency similar to uterine myoma, but on the other hand ultrasonography and computed tomography finding showed pelvic mass separate from the uterus and were similar to ovarian mature cystic teratoma (6, 15).
4. CONCLUSION
Uterine vascular lipoleiomymas are very rare benign tumors, rarely seen among premenopausal women. Our case is the first of this kind described in our country. Differential diagnosis is very important, especially differing these tumors from cystis teratomas, degenerative myomas and uterine sarcomas. We should pay more attention on the preoperative imaging studies, in order to select patients who require surgery and further treatment more appropriately.
Footnotes
• Authors contributions: Vesna Chibisheva- data collection, data analyzes and study design, Vesna Antovska and Milka Trajanova-critical revision of article, Drage Dabeski and Ivana Kijajova-drafting the article, Rubens Jovanovic-laboratory work
• Conflict of interest: none declared.
REFERENCES
- 1.Rollasson TP, Wilkinson N. Non neoplastic conditions of myometrium and pure mesenchymal tumours of the uterus. In: Fox H, Wells M, editors. Haines and Taylor Obstetrical and gynaecological pathology. 5th ed. Edinburgh: Churchill Livingstone; 2003. p. 531. [Google Scholar]
- 2.Scurry JP, Carey MP, Targett CS, Dowling JP. Soft tissue lipoleiomyoma. Pathology. 1991;23:360. doi: 10.3109/00313029109063606. [DOI] [PubMed] [Google Scholar]
- 3.Gentile R, Zarri M, De Lucchi F, Bellone F, Lapertosa G. Lipoleiomyoma of the uterus. Pathologica. 1996;88:132–4. [PubMed] [Google Scholar]
- 4.Jungsuk A, Ha Na K, Hyun Yee C, Dong-Hae C, Na Rae K. Uterine vascular leiomyoma with a fat component mimicking angiomyolipoma: A case report. Journal of Women’s Medicine. 2010;3(3) [Google Scholar]
- 5.Hae Kyung K, Ju Hyun K, Sung Yeon H, Youn Seok C, Hoon Kyu O, Tae Sung LM. A usterine lipoleiomyoma of the broad ligament mimicking an ovarian tumor. Korean J Obstet Gynecol. 2012;55(10):787–90. [Google Scholar]
- 6.Izetbegovic S, Alajbegovic J, Mutevelic A, Pasagic A, Masic I. Prevention of diseases in gynecology. Int J Prev Med. 2013 Dec;4(12):1347–58. [PMC free article] [PubMed] [Google Scholar]
- 7.Ashish C, et al. Uterine lipoleiomyoma. The journal of practical medical imaging and management. 2004;24(6) [Google Scholar]
- 8.Hrgovic Z, Kulas T, Habek D, Izetbegovic S, Hrgovic I. New options in the diagnosis and management of uterine myomal. Med Arh. 2008;62(4):234–9. [PubMed] [Google Scholar]
- 9.Manjunatha HK, Ramaswamy AS. J Midlife Health. 2010:86–8. doi: 10.4103/0976-7800.76219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Avritscher R, Iyer RB, Am J Roentgenol. 2001;117(4) doi: 10.2214/ajr.177.4.1770856. [DOI] [PubMed] [Google Scholar]
- 11.Chawla A, et al. Uterine lipoleiomyoma. Applied Radiology. 2007;33(4) [Google Scholar]
- 12.Tsushiam Y, Kita T, Yamamoto K. Uterine lipoleiomyoma: MRI, CT and ultrasonic findings. British Journanl of Radiology. 1997:70. doi: 10.1259/bjr.70.838.9404215. [DOI] [PubMed] [Google Scholar]
- 13.Kazuhiro K, et al. MRI Findings of Uterine Lipoleiomyoma Correlated with Pathologic Findings. American Journal of Roentgenology. 2007:189. doi: 10.2214/AJR.07.2230. [DOI] [PubMed] [Google Scholar]
- 14.Hrgovic Z, Izetbegovic S. Primary prevention of cervical carcinomal. Med Arh. 2007;61(1):49–51. [PubMed] [Google Scholar]
- 15.Karaman E, et al. A Case of Giant Uterine Lipoleiomyoma Simulating Malignancy. Case Reports in Obstetrics and Gynecology. 2015 doi: 10.1155/2015/926961. [DOI] [PMC free article] [PubMed] [Google Scholar]


