SUMMARY
Coding of itch versus pain has been heatedly debated for decades. However, the current coding theories (labeled line, intensity and selectivity theory) cannot accommodate all experimental observations. Here we identified a subset of spinal interneurons, labeled by gastrin releasing peptide (Grp), that receive direct synaptic input from both pain and itch primary sensory neurons. When activated, these Grp+ neurons generated rarely-seen simultaneous robust pain and itch responses that were intensity-dependent. Accordingly, we propose a “leaky gate” model, in which Grp+ neurons transmit both itch and weak pain signals, however upon strong painful stimuli the recruitment of endogenous opioids works to close this gate, reducing overwhelming pain generated by parallel pathways. Consistent with our model, loss of these Grp+ neurons increased pain responses while itch was decreased. Our new model serves as an example of non-monotonic coding in the spinal cord and better explains observations in human psychophysical studies.
INTRODUCTION
Pain and itch are two distinct yet related sensations. Both pain and itch are detected by small-diameter dorsal root ganglia (DRG) neurons and transmitted to the spinal cord dorsal horn, yet trigger distinct behavioral responses. Pain generates a withdrawal response to avoid tissue damage, while itch elicits scratching to remove irritants. Pain can suppress itch, which is demonstrated when the mechanical pain generated by scratching relieves the itchy sensation (Davidson et al., 2009). Itch, however, can rarely suppress pain. On the cellular level, neurons responsive to itchy stimuli in both DRG and the spinal cord can also be activated by pain (Akiyama et al., 2009a; Davidson et al., 2007; Liu et al., 2009; Schmelz et al., 2003), begging the question how these two sensations are distinguished.
Debates about pain and itch coding have been on-going for decades. One major theory, the intensity theory, claims that poly-modal sensory neurons respond to both painful and itchy stimuli. The same group of neurons can be stimulated strongly or weakly to generate pain or itch sensations respectively (Lewis et al., 1927; Von frey, 1922). However, weaker painful stimuli or stronger itchy stimuli fail to turn into a different sensation, thus raising questions about the intensity theory (Handwerker et al., 1991; Ochoa and Torebjörk, 1989; Tuckett, 1982). Another major theory is the labeled line theory, which argues that different senses are coded by mutually exclusive populations (Norrsell et al., 1999; Schmelz et al., 1997). However, the fact that itch-responsive neurons are also activated by painful stimuli argues against the labeled line theory. A modified labeled line theory, termed the selectivity theory, incorporates the existence of poly-modal sensory neurons (Handwerker, 1992; McMahon and Koltzenburg, 1992). The selectivity theory suggests that itchy stimuli specifically activate itch-selective neurons to generate itch sensation, while painful stimuli activate both itch-selective neurons and a larger nociceptive population whose activation inhibits itch to produce only pain sensation.
Recent studies largely support this modified labeled line theory. In DRG, Han et al. confirmed the existence of “itch-selective” neurons by showing that the activation of the MrgprA3+ primary sensory neurons generated itch but not pain responses, while its ablation impaired itch and spared pain (Han et al., 2013). Further along this same labeled line, the “itch-selective” neurons in the spinal cord are proposed to be the gastrin releasing peptide receptor (GRPR) positive population. The loss of the GRPR+ neurons abolished most itch responses but spared pain responses (Sun et al., 2009). In addition, brain natriuretic peptide (BNP) is suggested to be the itch-specific neurotransmitter, signaling between itch-selective cells in DRG and itch-selective cells in the spinal cord (Mishra and Hoon, 2013). However, in human psychophysical studies, most chemical-induced itch sensations are accompanied by weaker nociceptive sensations (burning, pricking, stinging, etc.) (LaMotte et al., 2014; Liu, 2012; Sikand et al., 2011a, 2009). These mixed sensations raise questions about the “selectivity” of itch pathways.
Although we cannot deny the beauty of simplicity, the anatomical structure of the spinal cord dorsal horn seems to suggest a more complicated and integrative organization of sensory circuits than labeled lines. Unlike pseudo-unipolar DRG neurons, which all serve output functions, only a small subset of superficial dorsal horn neurons transmit signals further to the brain (Spike et al., 2003). The remaining majority are interneurons forming interlacing local circuitries whose functions remain largely elusive. Here we attempted to reveal the functions of dorsal horn circuits as they related to pain and itch. Second order neurons are the first step in the spinal circuitry, receiving direct synaptic input from DRG neurons. We identified a subset of second order neurons, positive for Grp, that receive direct synaptic inputs from both pain and itch primary sensory neurons. Surprisingly, the activation of the Grp+ neurons generated both pain and itch responses with the pain coding being intensity dependent. These data led us to this “leaky gate” model, which provides a refined theory for pain and itch coding in the spinal cord and better explains results from human psychophysics experiments.
RESULTS
Genetic labeling of itch second order neurons in the spinal cord
Previously, we discovered that axons of MrgprA3+ itch primary sensory neurons selectively terminate in lamina II of spinal cord (Han et al., 2013). To identify genetic markers of second order neurons which form synapses directly with MrgprA3+ neurons, we utilized transgenic mouse lines with Cre recombinase expression under specific neuronal gene promoters, generated using bacterial artificial chromosome (BAC)-based transgenic technology by the Gene Expression Nervous System Atlas (GENSAT) project (Gong et al., 2003). Upon screening all GENSAT Cre lines with expression in the spinal cord dorsal horn, we focused on a promising target, Grp. Grp has previously been implicated in itch transmission. Grp was reported to express in DRG but not in spinal cord and proposed to provide input to GRPR+ neurons (Sun and Chen, 2007). However, recent studies suggest that Grp instead expresses in spinal cord dorsal horn, not the DRG (Fleming et al., 2012; Solorzano et al., 2015).
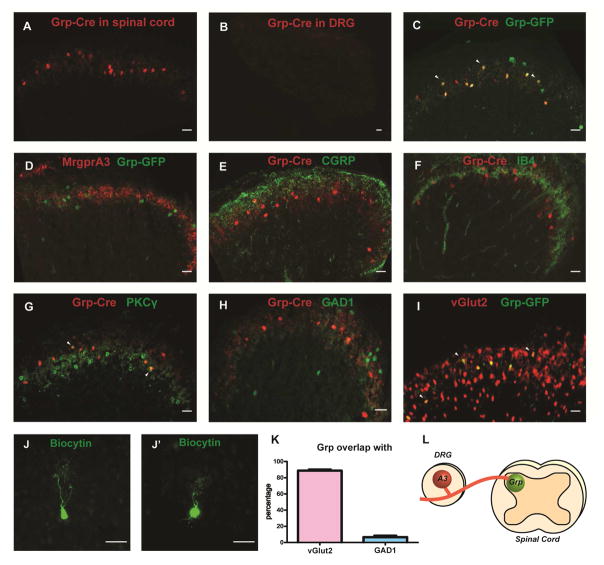
Consistent with the recent studies, we found that GrpCre expression was restricted to the superficial lamina of the spinal cord and we could not detect GrpCre expression in DRG (Figure 1A and 1B), when visualized with ROSA26LSL-tdTomato reporter line. Instead of attempting to reconcile the controversies regarding GRP expression, we focused more on utilizing the genetically labeled mouse lines to study the function of this subset of spinal cord neurons in pain and itch sensation. To further determine the laminar distribution of the Grp+ neurons in the dorsal horn, we performed immunostaining on GrpCre; ROSA26LSL-tdTomato spinal sections. Grp+ neurons were located deeper than the CGRP-labeled terminals in lamina II outer layer (Figure 1E), co-localized with IB4 positive fibers in lamina II dorsal inner layer (Figure 1F) and partially overlapped with PKCγ neurons (9.03%) in ventral inner layer(Braz et al., 2014; Solorzano et al., 2015) (Figure 1G and Figure S1E). Since there are no projection neurons (i.e. dorsal horn neurons sending their axons to the brain) in lamina II (Todd, 2010), GrpCre line thus labels a subset of interneurons (i.e. neurons whose axons remain and arborize in the spinal cord) in the lamina II inner layer. Regarding neurotransmitter types, more than 90% of Grp+ neurons expressed the glutamatergic excitatory marker (Figure 1H and 1K), vesicular glutamate transporter (vGlut2); while less than 10% of Grp+ neurons overlapped with the GABAergic inhibitory marker, GAD1 (Figure 1I). Therefore, Grp labels a subset of excitatory interneurons in lamina II inner layer.
Figure 1. Genetic labeling of itch second order neurons in the spinal cord.
(A and B) Spinal cord and DRG sections from GrpCre; ROSA26LSL-tdTomato mice, tdTomato fluorescence were visualized directly without staining. (C and D) GrpCre; ROSA26LSL-tdTomato;GrpEGFP and MrgprA3Cre; ROSA26LSL-tdTomato; GrpEGFP spinal sections stained with GFP antibody. (E–G) GrpCre; ROSA26LSL-tdTomato spinal sections stained with antibodies to CGRP, IB4 and PKCγ respectively. (H and I) GrpCre; ROSA26LSL-tdTomato; Gad1EGFP and vGlut2Cre; ROSA26LSL-tdTomato; GrpEGFP spinal sections stained with GFP antibody. White arrowheads in C, G, I indicate overlap. (J, J′) Biocytin labeled individual Grp+ neurons, categorized as vertical neurons. All scale bars represent 20 μm. (K) Percentage of Grp+ neurons expressing vGlut2 and Gad1. n= 15 hemisections from three mice per group. Data are represented as mean ± SEM. (L) Diagram summarizing the potential synaptic connections between MrgprA3+ DRG neurons and Grp+ neurons in the spinal cord. MrgprA3 also overlapped with Grp and post-synaptic marker, PSD95.
To check the prevalence of Grp+ neurons in the spinal cord, we stained for pan-neuronal marker, NeuN. Grp labeled only 4.24% of neurons in lamina II (Figure S1). Moreover, Grp+ neurons were all characterized as vertical neurons according to morphology (n=16) (Grudt and Perl, 2002) (Figure 1J and 1J′). Such a small group of genetically labeled neurons with uniform morphologies likely have uniform functions. Thus the GrpCre line from GENSAT serves as a great tool to investigate this small subset of spinal interneurons.
GENSAT has another Grp line with EGFP expression under the same promoter. 93% of neurons from GrpEGFP line were reported to express Grp mRNA (Solorzano et al., 2015). We crossed the EGFP line with GrpCre; ROSA26LSL-tdTomato. 90.3% of GrpCre positive neurons also expressed GrpEGFP (Figure 1C, Figure S1), while 64.1% of GrpEGFP neurons co-localized with GrpCre, showing that GrpEGFP line labeled most GrpCre positive neurons. We found that the distribution of GrpEGFP labeled neurons overlapped with MrgprA3 central terminals in the spinal cord (Figure 1D). Moreover, GrpEGFP co-localized with both MrgprA3 and post-synaptic marker PSD95 (Figure S1), suggesting that Grp+ neurons could form synaptic contacts with MrgprA3-labeled (diagramed in Figure 1L), itch-selective neurons in DRG (Han et al., 2013).
Grp+ neurons receive direct synaptic inputs from itch-selective primary neurons
Next, to directly examine the synaptic inputs to Grp+ neurons, we recorded from Grp+ neurons in spinal slices while electrically stimulating the dorsal root. All Grp+ neurons had monosynaptic input from C fibers (Figure S2), demonstrating that Grp exclusively labels second order neurons with direct synaptic input from DRG. We then tried to further determine the source of C fiber inputs onto Grp+ neurons. To determine whether Grp+ neurons receive direct synaptic input from MrgprA3+ neurons, we crossed MrgprA3Cre with Cre dependent Channelrhodopsin reporter line ROSA26LSL-ChR2 to selectively activate MrgprA3 fibers with blue light (as diagramed in Figure 2A).
Figure 2. Grp+ neurons receive monosynaptic itchy input.
(A) Left: diagram showing light activation of MrgprA3 peripheral fibers in behavioral tests; right: diagram showing light activation of MrgprA3 central terminals and recording of Grp+ neurons in the spinal cord. (B) 1Hz and 5Hz 100ms light stimulation triggered scratching bouts in five minutes. MrgprA3Cre; ROSA26LSL-ChR2 and ROSA26LSL-ChR2 control mice with light delivered to shaved nape regions (n=6). Data are represented as mean ± SEM. (C) From left to right: image of Grp+ neurons in spinal slice with electrode (black lines), representative traces of light-induced EPSCs in Grp+ neurons with monosynaptic input from MrgprA3+ neurons and percentage of Grp+ neurons with monosynaptic input from MrgprA3+ neurons. (D) Left: representative traces of light-induced EPSCs in lamina II Grp negative neurons with monosynaptic input, polysynaptic input and no synaptic input from MrgprA3+ neurons. Right: percentage of lamina II Grp negative neurons with monosynaptic input, polysynaptic input and no synaptic input from MrgprA3+ neurons.
To test the behavioral effect of light-mediated activation of the MrgprA3+ neurons, we shone blue light on the shaved nape regions of MrgprA3Cre; ROSA26LSL-ChR2 mice (as diagramed in Figure 2A). 1Hz 100ms light stimulation generated significant scratching compared with controls (Figure 2B, Supplemental video 1). Similar to chemical activation (Han et al., 2013), optogenetic activation generated only scratching but not wiping behavior, which confirmed the role of MrgprA3+ neurons as itch-selective neurons. 5Hz light stimulation, however, failed to elicit scratching above baseline (Figure 2B, see also Figure S3C). Consistently, 1Hz light stimulation reliably evoked action potentials in MrgprA3+ neurons, while 5Hz light stimulation failed to do so (Figure S3), suggesting that these neurons might not be able to fire at this higher frequency. Yet failure of 5Hz light to induce scratching could also be caused by failure in synaptic transmission in the central synapses or central terminals to follow at this frequency.
When we recorded from the Grp+ neurons while stimulating the MrgprA3 central terminals with light, 100% of the Grp+ neurons (16/16) received monosynaptic input from MrgprA3+ neurons (Figure 2C, see also Figure S3, monosynaptic connections inferred from no failure of EPSCs to 20 stimuli at 1Hz), showing that all sampled Grp+ neurons labeled a functionally unified population of second order neurons that appeared to receive direct itchy input from the periphery. When we recorded from surrounding Grp negative neurons, 25% of them (7/28) also received monosynaptic input, an additional 18% (5/28) received polysynaptic input and the remaining 57% (16/28) had no connection with MrgprA3+ neurons (Figure 2D), suggesting that Grp labels a subset of itch second order neurons in the spinal cord.
Grp+ neurons receive monosynaptic input from both itch and pain primary sensory neurons
We then checked whether Grp+ neurons receive input from nociceptors other than pruriceptors in DRG. However, it is hard to selectively activate nociceptors without also targeting the itch-selective neurons, given that they share many genetic markers. Therefore, we decided to use mono-synaptic rabies tracing (Wickersham et al., 2007) to systemically quantify the inputs to the Grp+ population. AAV helper virus (AAV8-LSL-TVA-EGFP-B19G) was injected into the spinal cord to enable expression of TVA receptor and rabies glycoprotein in Cre expressing neurons. Deficient rabies virus (ΔG-RV-GFP) then specifically infected TVA expressing Grp+ neurons, which also contained the rabies glycoprotein that allowed trans-synaptic labeling (as diagramed in Figure 3A).
Figure 3. Monosynaptic retrograde tracing from Grp+ neurons.
(A) Diagram showing monosynaptic retrograde tracing strategy from Grp+ neurons. (B) Rabies-labeled neurons overlap with IB4 in spinal cord. (C) Top panels: L4–6 DRG sections labeled with different markers (CGRP, IB4, NF200, MrgprC11 and TrpV1). Middle panels: rabies virus trans-synaptically labeled DRG neurons. Bottom panels: merge images. Arrowhead indicates overlap of markers and rabies-labeled DRG neurons. All scale bars represent 20 μm. (D) Percentage of rabies trans-synaptically labeled DRG neurons co-localize with different markers. Pooled results from more than 30 DRG sections of at least five mice for each marker.
Deficient rabies virus successfully infected Grp+ neurons in spinal cord lamina II, but not in Cre negative mice or when injected without the helper virus (Figure 3B and Figure S4), confirming the specificity of viral tracing. In DRG, rabies virus trans-synaptically labeled mostly small to medium diameter neurons. 64.1% of rabies-labeled DRG neurons expressed peptidergic marker calcitonin gene-related peptide (CGRP), 39.3% of rabies-labeled DRG neurons expressed non-peptidergic marker IB4, while very few (3.85%) expressed myelinated neuronal marker NF200 (Figure 3C and 3D). In addition, 50.0% of rabies-labeled neurons were positive for nociceptive marker, TrpV1; while an available MrgprC11 antibody, which marks most MrgprA3+ itch neurons (Han et al., 2013), labeled 22.3% of rabies-infected neurons, confirming that Grp+ neurons received monosynaptic input from itch-selective neurons (Figure 3D). Since the nociceptive neuron markers CGRP, IB4 and TrpV1 (which could also be expressed in some pruriceptors) labeled a larger percentage of rabies-infected DRG neurons than marker for itch neurons, we conclude that Grp+ neurons received monosynaptic input from nociceptive populations in addition to itch-selective neurons.
Painful stimuli strongly activate while itchy stimuli weakly activate Grp+ neurons
Since our results suggest that Grp neurons receive direct synaptic inputs from both itch and pain primary sensory neurons, we next tried to determine whether Grp+ neurons can distinguish between painful and itchy inputs. We performed DRG-attached spinal slice recordings and applied drugs on DRG cell bodies to mimic natural painful and itchy stimuli coming from the periphery (Figure 4A). Both pain- and itch-producing drugs applied directly on DRG triggered action potentials in Grp+ neurons (Figure 4C-F). Capsaicin evoked high frequency firing in Grp+ neurons; while the pruritogen SLIGRL produced only weak firing on the same recorded neurons even at very high doses. To ensure that limited penetration of peptide SLIGRL did not affect the responses of Grp+ neurons, we applied small molecule pruritogens, histamine and chloroquine. Similarly, histamine and chloroquine generated weaker firing in Grp+ neurons, comparing with capsaicin (p<0.001 and p<0.001 respectively, two-way ANOVA), which indicates that these neurons fire strongly in response to painful stimuli but weakly in response to itchy stimuli (diagramed in Figure 4B). Similar to our results, several previous studies showed spinal interneurons and projection neurons fired at higher frequencies in response to painful stimuli versus itchy stimuli (Akiyama et al., 2009b; Davidson et al., 2012, 2007).
Figure 4. Painful stimuli strongly activate while itchy stimuli weakly activate Grp+ neurons.
(A) Image of DRG attached spinal cord slice. Recording electrode on right and drug application electrode on left. (B) Diagram summarizing painful stimuli from DRG can strongly activate Grp+ neurons while itchy stimuli can only weakly activate Grp+ neurons. (C–F) Top panels: representative traces of action potentials from Grp+ neurons in responses to drugs. Bottom panels: Grp+ neurons in response to capsaicin (n=5, 0.5μM; n=5, 2μM; n=6, 5μM), SLIGRL (n=7, 100μM; n=6, 500μM), chloroquine (CQ, n=9, 3mM; n=10, 10mM) and histamine (n=5, 10mM; n=9, 50mM) application on DRG. Black bar indicates duration of drug application (n=6). Data are represented as mean ± SEM.
Coding of both pain and itch by Grp+ neurons
Although the itch neurons in DRG are responsive to both painful and itchy stimuli, activation of these neurons generates itch, not pain responses (Han et al., 2013). Similarly, Grp+ neurons appear to receive direct synaptic input from both pain and itch primary neurons. Using behavioral assays, we next determined what sensations are generated by the activation of Grp+ neurons. To specifically activate Grp+ neurons, we crossed GrpCre line to cre-dependent reporter line ROSA26LSL-TrpV1 in a global TrpV1 knockout background (GrpCre; ROSA26LSL-TrpV1; TrpV1−/−). In GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice, Grp+ neurons were the only cells with TrpV1 expression (as diagramed in Figure 5A), therefore TrpV1 agonist capsaicin can selectively activate Grp+ neurons. To test the functional expression of TrpV1, we injected AAV1-LSL-tdTomato virus into the spinal cord and recorded from tdTomato labeled Grp+ neurons. Labeled neurons from GrpCre; ROSA26LSL-TrpV1; TrpV1−/− but not from GrpCre; TrpV1−/− mice responded to capsaicin (Figure S5). Grp+ neurons with ectopic TrpV1 expression showed lower sensitivity to capsaicin compared with TrpV1+ DRG neurons. These neurons exhibited monotonically increased responses to a wide range of capsaicin doses (Figure S5), confirming the functional expression of TrpV1 in Grp+ neurons.
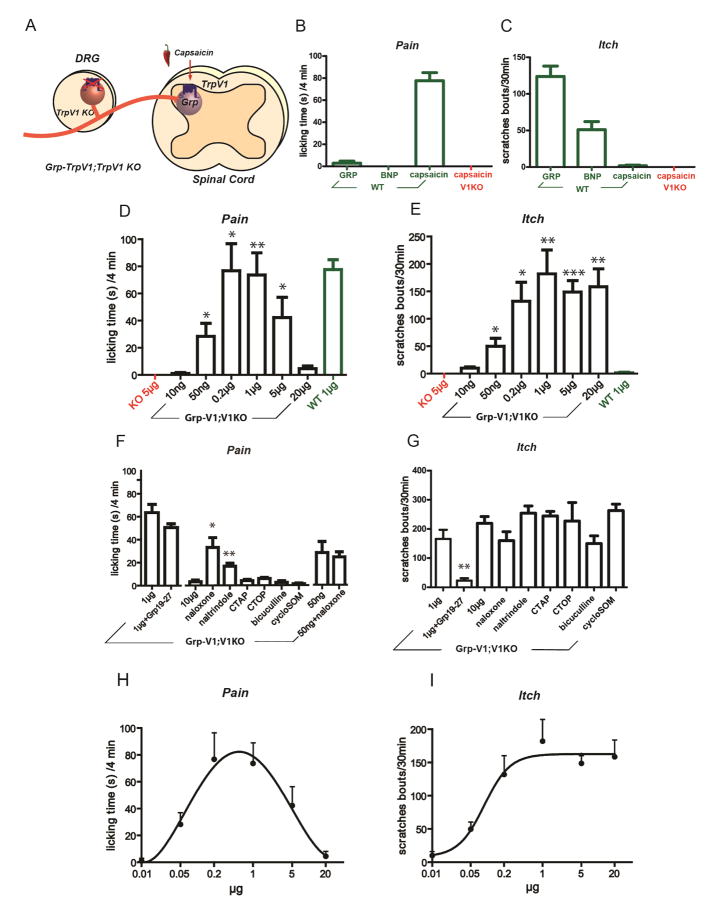
Figure 5. Intensity dependent coding of pain and itch by Grp+ neurons.
(A) Diagram showing the strategy of capsaicin-mediated specific activation of Grp+ neurons in GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice. (B and C) Pain-related licking time and itch-related scratching bouts in wild type (green bars) and TrpV1−/− mice (red bars) triggered by intrathecal delivery of 10μl capsaicin (1μg or 3.3nmol, n=6 for both genotypes), BNP (2.5mg/ml or 7.1nmol/site, n=8) and GRP peptides (200μM or 2nmol/site, n=8). (D and E) 10μl intrathecal capsaicin-triggered pain and itch responses in GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice (black bars, from left to right: 10ng or 0.03nmol, n=9; 50ng or 0.16nmol, n=6; 0.2μg or 0.67nmol, n=5; 1μg or 3.33nmol, n=6; 5μg or 16.7nmol, n=10; 20μg or 66.7nmol, n=6) together with responses in wild-type (green bars, 1μg or 3.33nmol, n=6) and TrpV1−/− mice (red bars, 5μg or 16.7nmol, n=6) from (B and C). (F and G) 10μl intrathecal capsaicin-triggered pain and itch responses in GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice with drugs. From left to right 1μg or 3.33nmol capsaicin without and with GRPR antagonist (Deamino-Phe19,D-Ala24,D-Pro26-psi(CH2NH)Phe27)-GRP (19–27), 200μM or 2nmol/site, n=6 and 5); 10μg or 33.3nmol capsaicin, n=8; 10μg or 33.3nmol capsaicin with naloxone (1μg or 3.33nmol, n=7), naltrindole (10μg or 24.1nmol, n=7), CTAP (5μg or 13.7nmol, n=6), CTOP (10μg or 9.43nmol, n=6), bicuculline (10μM or 0.1nmol, n=7), cycloSomatostatin (0.1mM or 1nmol, n=8) and for (F) 5μg/ml or 0.16nmol capsaicin without (n=6) and with naloxone (1μg or 3.33nmol, n=9). (H and I) Pain and itch dose-response curve fitting of (D and E). Data are represented as mean ± SEM. *: P < 0.05, **: P<0.01, ***: P<0.001, two-tailed unpaired Student’s t test. Abbreviations: WT short for wild type. KO short for TrpV1−/−. Grp-V1;V1KO short for GrpCre; ROSA26LSL-TrpV1; TrpV1−/−.
Drugs known to produce pain (capsaicin) and itch (gastrin releasing peptide, GRP and brain natriuretic peptide, BNP) were first tested intrathecally in wild-type mice. Previous studies reported mixed licking, biting and scratching responses to capsaicin (Hunskaar et al., 1985; Yaksh et al., 1979). Counting licking/biting and scratching separately, revealed that responses in mice were predominantly licking/biting with very few bouts of scratching (Hunskaar et al., 1986). To further distinguish licking, indicating pain and biting, indicating itch, behaviors were recorded with a high-definition camera and four side mirrors to enable views from all angles (Figure S5) (LaMotte et al., 2011). When played back at 1/4 normal speed, licking but not biting responses was detected following injections of capsaicin. Short-lasting licking responses (<5 minutes) directed to the lower back regions were predominantly observed, at a characteristic frequency of 5Hz, accompanied by minor scratching responses as previously reported (Figure 5B). Such responses were not seen in TrpV1−/− mice, ensuring specificity. GRP and BNP, nonetheless, produced scratching that lasted about 30 minutes after injection with minor licking responses (Figure 5C and Figure S5B).
Surprisingly, specific activation of Grp+ neurons in GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice by intrathecal injection of capsaicin generated both pain-related licking and itch-related scratching (Supplemental video 2); whereas injection of capsaicin generated no response in Cre negative control mice (ROSA26LSL-TrpV1; TrpV1−/−) and only pain-related licking in wild-type mice (Figure 5B and 5C), which confirms the specificity of the activation responses. The licking responses lasted only about 4 minutes after injection (similar to the licking responses in wild-type mice) and were not affected by intrathecal injection of a GRPR antagonist (Figure 5F); the scratching responses lasted more than 30 minutes and were effectively blocked by GRPR antagonist (Figure 5G), consistent with the critical role of GRPR neurons in itch transmission (Sun et al., 2009; Sun and Chen, 2007). Thus, the activation of Grp+ neurons can trigger both robust pain and itch responses, a phenomenon rarely observed. Grp+ neurons appear to receive monosynaptic inputs from both itch and pain neurons and code for both itch and pain, showing unexpected convergence of two related sensations in the spinal cord.
Intensity dependent coding of pain by Grp+ neurons
Next, we examined the relationship between neuronal activation and behavior by determining the behavioral effects of various doses of capsaicin. Itch responses monotonically increased until a plateau was reached and were fitted to the Hill equation (R2=0.97, Figure 5E and 5I). Pain responses, surprisingly, showed an inverted U relationship (Figure 5D). Increased amounts of capsaicin resulted in increased licking time that peaked and then decreased with higher capsaicin doses, so that weak and strong activation produced little pain behavior while medium range activation generated greatest pain responses. Not surprisingly, pain dose responses were fitted well with a polynomial equation (R2=0.99, Figure 5H). Given that high doses of capsaicin still caused robust itch responses, the inverted U pain responses were unlikely caused by desensitization. Thus, Grp+ neurons demonstrate intensity-dependent coding. Rather than generating itch sensation with weak activation and pain sensation with strong activation, as suggested by the original intensity theory, Grp+ neurons monotonically code for itch while pain is coded only by inputs of medium intensities.
We reasoned that the inverted U coding of pain could be generated by a combination of direct coding effects and another pain inhibition circuit. To uncover this pain inhibition mechanism, we attempted to “rescue” pain responses during strong activation of the Grp+ neurons. An opioid antagonist, naloxone, at a dose not eliciting pain itself, “rescued” the pain responses from almost zero to about half of the maximal level. Both bicuculline, a GABA A antagonist, and cyclo-somatostatin, the antagonist of anti-nociceptive somatostatin highly expressed in the surrounding region, failed to “rescue” the pain responses (Figure 5F). Successfully rescuing pain responses again confirmed that Grp+ neurons were not desensitized by high doses of capsaicin. To demonstrate that naloxone was not simply blocking the basal activity of the endogenous opioid system, independent of Grp activation, we co-injected naloxone with a low dose of capsaicin which can produce both medium pain- and itch-responses. No effect was observed on pain responses (Figure 5F), indicating that the endogenous opioid system was only recruited to inhibit pain during strong activation of the Grp+ neurons. Thus, the endogenous opioid system is at least partially responsible for the pain inhibition associated with strong activation of the Grp+ neurons and therefore, together with direct pain coding by the Grp+ neurons, generates this inverted U response curve.
We then determined which endogenous opioid peptide was employed to block pain by utilizing mu opioid antagonist CTAP and CTOP and delta opioid antagonist naltrindole. Naltrindole but not CTAP or CTOP induced a similar rescue effect as naloxone (Figure 5F), while none of the drugs affected itch responses (Figure 5G). These results suggest that Enkephalin, the endogenous ligand for delta opioid receptors, was recruited by Grp+ neurons to inhibit pain but not itch, consistent with previously reported enkephalin effects (Lee and Ko, 2015); on the contrary, another endogenous opioid, dynorphin was reported to inhibit itch but not pain (Kardon et al., 2014). Co-localization of Grp, enkephalin and synaptic marker PSD95 also suggests that enkephalin-expressing interneurons may be synaptically connected to Grp+ neurons (Figure S5). To directly test this, we utilized PenkCre line to label enkephalin-expressing neurons in the spinal cord and verified the expression of enkephalin in these inhibitory interneurons (Figure 6D and 6E), as previously reported (Fukushima et al., 2011; Todd et al., 1992). Patch-clamped recordings of GrpEGFP neurons were made in spinal cord slices from GrpEGFP; PenkCre; ROSA26LSL-GCaMP6 mice. Depolarization of a single GrpEGFP neuron triggered activation of enkephalin-expressing neurons, as monitored by GCaMP6 calcium imaging, in 50% of cases (5 out of 10 neurons, Figure 6C), confirming the synaptic connections between Grp+ neurons and enkephalin-expressing neurons. This percentage may be an underestimate, since some connections might be lost during sectioning. In addition, enkephalin release was detected by ELISA when GrpCre; ROSA26LSL-TrpV1; TrpV1−/− spinal cords were treated with high dose capsaicin but not with low dose or no capsaicin (Figure 6B). Furthermore, spinal cords from Cre negative control mice (ROSA26LSL-TrpV1; TrpV1−/−) treated with high dose capsaicin released a minimal amount of enkephalin, which confirms that the release of enkephalin is dependent on strong activation of the Grp+ neurons. Moreover, enkephalin requires strong depolarization for release (Cesselin et al., 1984; Neuman et al., 1984), consistent with the observation that only strong activation of the Grp+ neurons triggers pain inhibition.
Figure 6. Activation of enkephalin-expressing neurons triggered by stimulation of Grp+ neurons.
(A) Diagram showing calcium imaging of enkephalin-expressing neurons labeled by PenkCre while depolarizing GrpEGFP neurons in spinal slices. (B) Enkephalin release with different doses of capsaicin from GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice (black bars) and ROSA26LSL-TrpV1; TrpV1−/− control mice (blue bars) normalized to per g tissue used in ELISA. (C) Representative calcium imaging results showing enkephalin-expressing neurons before, during and after activation of GrpEGFP neurons (1Hz 50pA current injection). White lines (in pipet shape) indicated patch-clamped GrpEGFP neurons. Arrowheads indicated activated enkephalin-expressing neurons during Grp activation. Enkephalin-expressing neurons (PenkCre; Rosa26LSL-GCaMP6) were activated when 5 out of 10 Grp+ neurons were depolarized. (D) PenkCre labeled neurons co-localized with enkephalin and GAD1. Representative neurons magnified in upper right corner (Arrowheads indicated magnified cells). Scale bars represent 20μm.
Grp+ neurons form “leaky gate” to negatively regulate pain transmission
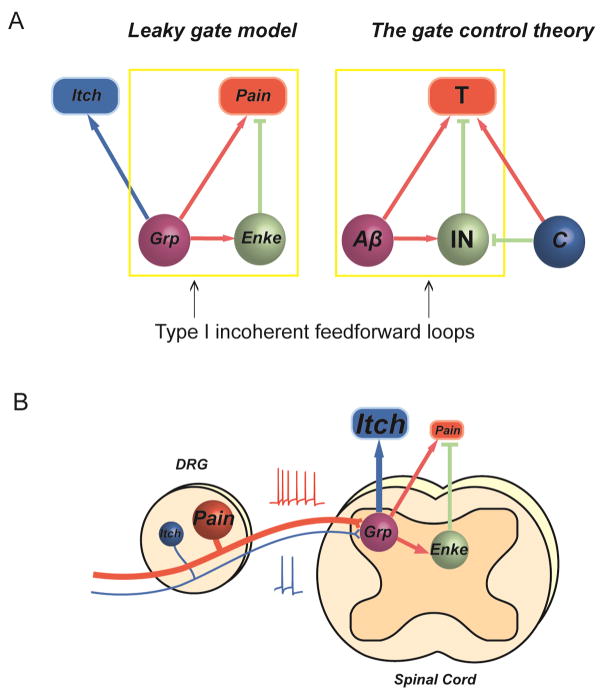
Activation of the Grp+ neuron population codes for pain but also inhibits pain through the release of enkephalin, which forms a type I incoherent feed forward loop (FFL) (summarized in Figure 7B), featuring non-monotonic output (Alon, 2007; Milo et al., 2002). Example of pain related type I incoherent FFL can be found in the gate control theory (Braz et al., 2014; Duan et al., 2014; Melzack and Wall, 1965; Wall, 1978). The gate control theory of pain proposes that nociceptive transmission neurons (T) receive both noxious input from C fibers and non-noxious input from Aβ fibers. Aβ input also indirectly inhibits nociceptive transmission neurons through inhibitory interneurons (IN), thus forming a type I incoherent feed forward loop, which can close the “gate” (T) and suppress painful input (Figure 7A). The somatostatin- and the dynorphin-expressing interneurons are recently implicated as transmission neurons and inhibitory interneurons in the gate control theory, respectively (Duan et al., 2014).
Figure 7. “Leaky gate” model in pain and itch transmission.
(A) Comparison of “leaky gate” model (left) and the gate control theory (right). Grp+ neurons directly code for pain and itch while inhibiting pain through enkephalin-expressing interneurons. Aβ fibers activate pain transmission neurons and also indirectly inhibit pain transmission neurons via inhibitory interneurons. Yellow rectangles indicate type I incoherent feed forward loop formed by Grp+ neurons and Aβ fibers respectively. (B) Diagram summarizing the role of Grp+ neurons in pain and itch coding. Grp+ neurons receive weak input from itchy stimuli and strong input from painful stimuli, and positively code for itch while negatively regulate pain transmission. Enke (Enkephalin), T (pain transmission neurons), IN (inhibitory interneurons).
Here, we present a model to explain our experimental observations and then provide more data to support the model. Similar to Aβ fibers in the gate control theory, we propose that Grp+ neurons utilize the type I incoherent feed forward loop as a “gate” to regulate pain transmission. When strongly activated, Grp+ neurons can trigger enkephalin release to close the “gate” to painful signals from both Grp+ neurons and potentially other pain- sensing neurons in the spinal cord, resulting in reduced pain sensation (summarized in Figure 7B). However, the Aβ and Grp gates have some fundamental differences. The Aβ FFL does not let any signals through the “gate”, at least under physiological conditions, so that non-noxious input does not elicit pain sensations; the Grp FFL allows weak pain signals to pass through the “gate” but suppresses strong pain signals. Therefore, we named it a “leaky” gate. We think the advantage of this “leaky gate” is that passing on weak signals ensures sensitivity to weak painful stimuli while inhibiting strong signals prevents overwhelming pain sensations.
Increased pain and decreased itch after ablation of Grp+ neurons
According to our “leaky gate” model, the Grp FFL functions as a “brake” to prevent strong pain signals from overwhelming the system. Therefore, we predicted that the loss of the Grp+ neurons should lead to an increase of pain responses. To directly test this prediction, we ablated Grp+ neurons with diphtheria toxin. Diphtheria toxin receptors (DTRs) were specifically expressed in Grp+ neurons with Cre dependent ROSA26LSL-DTR line together with ROSA26LSL-tdTomato allele to monitor ablation efficacy (Figure 8A). Diptheria toxin treatments successfully ablated more than 95% of the Grp+ neurons (Figure 8B and 8C). Cre negative mice (ROSA26LSL-DTR/LSL-tdTomato) treated with same doses of diphtheria toxin were used as controls. Ablated mice were healthy and had normal motor coordination in the rotarod test (Figure S6). In addition, CGRP and IB4 labeled lamina II regions showed no change after ablation, indicating that the loss of such a small population did not obviously affect the general organization of the local circuitries. The number of PKCγ positive neurons was reduced, consistent with the partial overlap between PKCγ and Grp+ neurons while the number of Pax2+ interneurons were comparable between ablated and control mice, confirming that diphtheria toxin treatment did not produce non-specific neurotoxicity (Figure S6).
Figure 8. Increased pain and decreased itch responses after the ablation of Grp+ neurons.
(A) Diagram showing ablation of Grp+ neurons in the spinal cord. (B) Representative images of GrpCre; ROSA26LSL-DTR; LSL-tdTomato spinal slices with and without diphtheria toxin treatments. All scale bars represent 20 μm. (C) Quantification of Grp+ neurons per five 20μm hemisections in GrpCre; ROSA26LSL-DTR; LSL-tdTomato (red) and ROSA26LSL-DTR; LSL-tdTomato control mice (blue) after diphtheria toxin treatments (n=5 mice). (D) Scratching bouts induced by histamine (100mM or 5μmol, n=6 vs. 8), serotonin (1mM or 50nmol, n=7 vs. 8), SLIGRL (1mM or 50nmol, n=7) and chloroquine (4mM or 200nmol, n=11 vs. 9) injection in the nape region (50μl) in GrpCre; ROSA26LSL-DTR; LSL-tdTomato (red) and ROSA26LSL-DTR; LSL-tdTomato control mice (blue). (E) Scratching bouts induced by injections of histamine (100mM or 5μmol, n=6) and chloroquine (4mM or 200nmol, n=6) in the nape region (50μl), with saline (50μl) or GRPR antagonist (50μl, Deamino-Phe19,D-Ala24,D-Pro26-psi(CH2NH)Phe27)-GRP (19–27), 200μM or 2nmol/site) pretreatments 10 minutes before injection and saline (50μl) induced scratching bouts (n=6) in GrpCre; ROSA26LSL-DTR; LSL-tdTomato (red) and ROSA26LSL-DTR; LSL-tdTomato control mice (blue). (F) Pain responses from capsaicin cheek injections (1mg/ml or 33nmol, n=8; 0.5mg/ml or 16.7nmol, n=7 vs. 6), capsaicin intraplantar injections (0.1mg/ml or 3.3nmol, n=6; 0.05mg/ml or 1.67nmol, n=6) and immersion assay (50°C, n=7 vs. 6; 52°C, n=7 vs. 6) in GrpCre; ROSA26LSL-DTR; LSL-tdTomato (red) and ROSA26LSL-DTR; LSL-tdTomato control mice (blue). (G and H) Pain responses from hot plate test (52°C, n=10; 55°C, n=7 vs. 6), Hargreaves test (n=8 vs. 7) and Von Frey test responses (n=11) in GrpCre; ROSA26LSL-DTR; LSL-tdTomato (red) and ROSA26LSL-DTR; LSL-tdTomato control mice (blue). Yellow shaded regions represent responses with strong stimuli. Data are represented as mean ± SEM. *: P < 0.05, **: P<0.01, ***: P<0.001, extended Welch’s t test for response ratio comparison between different temperatures in hot plate and tail immersion test and two-tailed unpaired Student’s t test for the rest. Abbreviations: Grp/DTR/tdt short for GrpCre; ROSA26LSL-DTR; LSL-tdTomato and DTR/tdt short for ROSA26LSL-DTR; LSL-tdTomato, CQ short for chloroquine, 5-HT short for serotonin.
First, we tested acute pain responses. Pain behavioral responses induced by injection of capsaicin into both the cheek and intraplantar surface of the hindpaw greatly increased after ablation (Figure 8E, yellow shaded). GrpCre; ROSA26LSL-DTR/LSL-tdTomato mice also had significantly shorter response latencies in all thermal pain assays including hot plate, Hargreave and tail immersion when compared with control mice (Figure 8E,F). Mechanical sensitivity tested by Von Frey filaments remained the same in both genotypes (Figure 8G). Thus, the loss of Grp+ neurons enhanced chemical and thermal pain, as predicted by the “leaky gate” model. We next examined itch responses. Scratching responses to multiple pruritogens including histamine (100mM or 5μmol/site), chloroquine (CQ, 4mM or 200nmol/site), SLIGRL (1mM or 50nmol/site) and serotonin (5-HT, 1mM or 50nmol/site) were all significantly reduced in GrpCre; ROSA26LSL-DTR/LSL-tdTomato mice, confirming the critical role of Grp+ neurons in itch coding (Figure 8D). Interestingly, GRPR antagonist significantly blocked histamine and chloroquine induced itch in control mice but did not further reduce scratching responses in Grp neuron ablated mice. This suggests that the residual itch responses after Grp neuron ablation is mediated by GRPR-independent pathway (Figure 8E).
Strong pain responses are more affected by the loss of Grp+ neurons
Unlike the gate control theory, only strong activation of the Grp+ neurons closes the “leaky gate” to inhibit pain. Therefore, the “leaky gate” model predicts that weak painful stimuli might trigger less or no inhibition. Accordingly, we compared chemical pain responses (capsaicin-induced cheek wiping) with two different doses. High dose capsaicin (1mg/ml) produced significantly more cheek wiping in ablated mice (Figure 8E, yellow shaded), while low dose capsaicin (0.5mg/ml) generated similar amounts of wiping in both ablated and control mice (Figure 8F), matching our prediction that weak pain triggers no inhibition from the Grp FFL. Similarly, intraplantar injection of high dose capsaicin (0.1mg/ml) induced significantly more licking/flinching responses, indicating pain, in ablated animals, while low dose (0.05mg/ml) triggered comparable responses. We also tested thermal pain using both hot plate and tail immersion, with two temperatures. Ablated mice showed reduced response latencies at both temperatures (Figure 8G,H). Therefore, we compared the ratios of ablated responses to control responses at the two temperatures, with a lower ratio meaning a larger increase in pain response after ablation. The ratios at high temperature were significantly lower than the ratios at low temperature in both tests, suggesting that thermal stimuli at higher temperatures resulted in larger increase in pain response after the loss of Grp+ neurons, consistent with the “leaky gate” model.
We also compared dose effect on itch responses, which are normally coded by the Grp+ neurons, between control and ablated mice. Ablated mice showed reduced itch responses to low doses of SLIGRL and CQ (Figure 8D), while high doses generated similar responses in both ablated and control mice (Figure S6). Thus, in contrast to pain, stronger itch responses are less affected by the loss of Grp+ neurons, potentially due to saturation or compensation from other itch second order neurons. These results confirm that the Grp FFL has distinct roles in pain and itch coding.
DISCUSSION
The selectivity theory depicts pain and itch coding in the spinal cord as the continuation of separate labeled lines from periphery with pain inhibiting itch through B5-I interneurons (Kardon et al., 2014) and NPY interneurons (Bourane et al., 2015). Here, we present experimental observations and a new leaky gate model to expand the current coding theory of pain and itch. In combination with selectivity theory, leaky gate model can provide better descriptions of pain and itch related phenomena. The data show that a subset of second order neurons with uniform morphologies, the Grp+ population, participates in the coding of both pain and itch sensations, which potentially represents the currently underappreciated crosstalk of different sensations in the spinal cord. Another feature of the Grp+ population is the intensity dependent coding of pain. The Grp+ neurons directly code for pain sensation and upon strong activation, indirectly inhibit pain via the recruitment of the endogenous opioid system. The classic intensity theory suggests that pain and itch sensations are differentially coded by strong and weak activation intensities. Here, we propose that the intensity-dependent pain coding by Grp+ neurons is a form of negative regulation of pain in the spinal cord. This novel intensity-dependent coding serves as a good example of the currently overlooked non-monotonic signal processing in spinal circuits.
Consistent with the intensity dependent coding of Grp+ neurons, we observed dose dependent behavioral changes after the loss of Grp+ neurons (Figure 8 and Figure S6), suggesting that testing of multiple doses in behavioral assays could help to identify currently overlooked non-linearity in pain and itch coding. Notably, the drug doses utilized in pain and itch behavioral tests in our study and in the pain/itch field were high compared with cellular studies. The specificities of these responses were largely established by previous work with respective pruritogen receptor knockouts (Han et al., 2006; Liu, 2011; Liu et al., 2009). However, receptor knockouts usually reduce but not abolish scratching responses, suggesting potential non-specific effects associated with high doses in behavioral tests. The number of activated neurons or ligand-bound receptors needed to trigger behavior responses remains an open question in the field. Yet the higher doses used in behavioral tests compared with cellular assays could be at least partially explained by dilution, tissue penetration and the differential receptor densities between nerve terminals and cell bodies. In addition, human psychophysical studies, in which subjects can orally report sensations, usually require lower doses (LaMotte et al., 2011; Sikand et al., 2011b)) compared to animal behavioral assays, indicating the relative low sensitivity of animal behavioral tests.
Grp+ neurons appear to receive monosynaptic input from both pain and itch sensing primary populations, yet painful stimuli strongly activates Grp+ neurons while itchy stimuli weakly activates them. The weaker pruritogen-mediated activation of Grp+ neurons could be due to factors including the weak activation of DRG neurons by itchy stimuli, weak synaptic connections, or a small percentage of itch responsive primary neurons. This weak activation by itchy stimuli is consistent with the failure to detect chloroquine induced c-fos activity in Grp+ neurons (Bell et al., 2016). Yet unlike enkephalin-expressing inhibitory interneurons, which require strong depolarization to release neuropeptides, the weak activation of Grp+ neurons by pruritogens seems sufficient to trigger GRP release from these excitatory interneurons. In addition to Grp+ neurons, some lamina II interneurons may receive monosynaptic itchy input. In lamina I, projection neurons and GRPR+ interneurons might also receive direct itchy input, warranting future research to further dissect related spinal cord circuits.
Pain detection systems need to be sensitive enough to protect the body from potential harm, but when exposed to strong painful stimuli, high sensitivity may generate too much pain and interfere with proper behavioral responses. Thus brakes are necessary. Brakes triggered by signals from Aβ mechanosensitive fibers makes gentle rubbing an effective way to relieve pain. The Grp FFL also functions as a brake for pain generated by Grp+ population and parallel pain pathways. It positively codes for pain while triggers enkephalin release only in response to strong activation, which is consistent with dependence of enkephalin release on strong depolarization. This prominent enkephalin mediated pain inhibition can completely block pain responses from the Grp+ population and further reduce pain coded by parallel pain pathways in the spinal cord, thus its high triggering threshold ensures sensitivity to weak painful input. Meanwhile, the pain inhibition mediated by Grp FFL cannot be triggered by itch, since itch stimuli only weakly activate Grp+ neurons, consistent with the fact that itch can rarely inhibit pain.
The ablation experiments showed that stronger pain responses had larger increases after the ablation of the Grp+ neurons, suggesting that the Grp FFL provides stronger inhibition on stronger painful input in physiological conditions, as predicted by the “leaky gate” model. Theoretically, weak enough painful stimuli would be positively coded by Grp+ neurons without triggering pain inhibition. Thus these pain responses might be weaker after the ablation of Grp+ neurons. However, given that the Grp+ neurons only represent a subset of pain responsive neurons in the spinal cord, the loss of these neurons may generate a more subtle change in behavior when compared with the loss of the strong pain inhibition effect mediated by the Grp FFL and thus be much harder to detect with animal behavioral tests. In a previous study, Mishra et al. ablated 70% of NPR1+ neurons, which were reported to be a subset of Grp+ neurons, with BNP conjugated saporin and found a significant change in histamine responses(Mishra and Hoon, 2013). We believe the partial loss of Grp+ neurons might not be sufficient to generate significant changes in pain responses; however, a trend of increase in pain responses from hot plate test was observed after the ablation of NPR1+ neurons.
The Grp+ neurons represent a subset of second order neurons that mediate pain and itch sensations in the spinal cord. Painful stimuli from the periphery can elicit both pain and itch responses via the Grp+ neurons. The itch responses are likely blocked by feed forward inhibition from parallel pain pathways, as noted by the selectivity theory. Similarly, itchy stimuli from the periphery can also trigger both itch and pain responses via the Grp+ neurons. We think this pain responses might be weak, as Grp+ neurons were only weakly activated by itchy stimuli. Indeed, in human psychophysical studies, most itchy substances induce itch sensation accompanied by weaker pain sensations, such as pricking and burning; while painful substances induce nociceptive but not itch sensations (LaMotte et al., 2014; Liu et al., 2012; Sikand et al., 2011a, 2009). Even if we cannot rule out the possibility that mechanical or other forms of itch can bypass or block the weak pain responses and result in pure itch sensation, the “leaky gate” model can explain the nociceptive sensations generated by itchy chemicals in human psychophysics studies.
In summary, Grp+ neurons positively code for itch while negatively regulating pain transmission with a “leaky gate.” This study, to our knowledge, experimentally demonstrates intensity-dependent coding of pain in the spinal cord for the first time. Our leaky gate model builds on current theories of pain and itch coding, and further refines them. It better explains observations in human psychophysical studies and serves as an example of non-monotonic coding and crosstalk of sensory information in the spinal cord. Further studies of the Grp+ related circuits in chronic pain and itch conditions might uncover relevant changes contributing to these pathological conditions.
STAR Methods
CONTACT FOR REAGENT AND RESOURCE SHARING
Further information and requests for resources and reagents should be directed to and will be fulfilled by the Lead Contact Xinzhong Dong (xdong2@jhmi.edu).
EXPERIMENTAL MODEL AND SUBJECT DETAILS Mouse lines
GrpCre and GrpEGFP mouse lines were acquired from MMRRC. MrgprA3Cre mouse line was previously generated by our group. ROSA26LSL-tdTomato, ROSA26LSL-ChR2, ROSA26LSL-DTR, ROSA26LSL-TrpV1, vGlut2Cre, GAD1EGFP and TrpV1−/− mouse lines were acquired from the Jackson laboratory. We used GrpCre, GrpEGFP, and MrgprA3Cre as hemizygotes or heterozygotes for all the experiments. All experiments were performed using protocols approved by the Animal Care and Use Committee of Johns Hopkins University School of Medicine.
All behavioral tests were performed with an experimenter blind to genotype. The mice were 2–4-month-old males that had been backcrossed to C57Bl/6 mice for at least six generations. The day before the behavioral tests, all mice were acclimated for at least 30 min to their testing environment. We housed 4–5 mice in each cage in the vivarium with 12h light/dark cycle and all the behavioral tests were performed in the morning.
METHOD DETAILS
Immunofluorescence
2–4 month old mice were anesthetized with pentobarbital and perfused with 20 ml 0.1 M PBS (pH 7.4, 4 °C) followed with 25 ml of fixative (4% formaldehyde (vol/vol) and 14% sat. picric acid (vol/vol) in PBS, 4 °C). Spinal cord and DRG were dissected from the perfused mice. DRG was post-fixed in fixative at 4 °C for 30 min, and spinal cord were fixed for 1 h. Tissues were cryoprotected in 30% sucrose (wt/vol) for more than 12 h and were sectioned with a cryostat. The sections on slides were dried at 37 °C for 40 min, and fixed with 4% paraformaldehyde at room temperature for 10 min. The slides were pre-incubated in blocking solution (10% normal goat serum (vol/vol), 0.2% Triton X-100 (vol/vol) in PBS, pH 7.4) for 1 or 2 h at room temperature, then incubated overnight at 4 °C with primary antibodies. Secondary antibody incubation was performed at room temperature for 2 h.
For primary antibodies, we used rabbit α-CGRP (T-4239, Peninsula, 1:1,000), rabbit α-NF200 (AB1982, Chemicon, 1:1,000), rabbit α-PKCγ (sc-211, Santa Cruz Biotechnology, 1:1,000), rabbit α-GFP (A-11122, Molecular Probes, 1:1,000), mouse α-Neuronal nuclei (MAB377, Chemicon, 1:200), mouse α-PSD95 (K28/43, NeuroMab, 1:500), rabbit α-PSD95 (EP1183Y, Millipore, 1:500), guinea pig α-TrpV1 (AB5566, Millipore, 1:200), rabbit α-MrgprC11 (made by our lab, 1:200), mouse α-GAD1 (MAB 5406, Millipore, 1:2000) and mouse α-Enkephalin (NOC1, Millipore, 1:100). For secondary antibodies, we used goat α-rabbit (A11008, Alexa 488 conjugated; A11011, Alexa 568 conjugated; A21245, Alexa 647 conjugated, Thermo Fisher), goat α-mouse (A11001. Alexa 488 conjugated; A11004, Alexa 568 conjugated; A21236, Alexa 647 conjugated, Thermo Fisher) and goat α-guinea pig (A11075, Alexa 568 conjugated). All secondary antibodies were diluted 1:500 in blocking solution. To detect IB4 binding, sections were incubated with Griffonia simplicifolia isolectin GS-IB4 (1:500; I21411, Alexa 488 conjugated; I21412, Alexa 568 conjugated, Thermo Fisher).
Electrophysiological recordings
To prepare spinal cord slices, 4 to 6 week-old mice were deeply anesthetized with 2% isoflurane (Abbott Laboratories, North Chicago, IL, USA). Spinal cord with dorsal root or DRG was rapidly removed and placed in ice-cold, low-sodium Krebs solution which contained: 95mM NaCl, 2.5mM KCl, 26mM NaHCO3, 1.25mM NaH2PO4-H2O, 6mM MgCl2, 1.5mM CaCl2, 25mM glucose, 50mM sucrose, 1mM kynurenic acid bubbled with 95% O2/5% CO2. Sagittal spinal cord slices (400μm) with dorsal roots or DRG attached were cut by a Vibratome (VT1200, Leica Biosystems, Buffalo Grove, IL, USA) and transferred to low-sodium Krebs solution without kynurenic acid for recovery at 34°C for 45 minutes and then at room temperature for an additional 1 hour before being used for recordings.
For electrophysiology recording, slices were stabilized with a nylon harp and submerged in a low-volume recording chamber (SD Instruments, San Diego, CA, USA), which was perfused with Krebs solution (125mM NaCl, 2.5mM KCl, 26mM NaHCO3, 1.25mM NaH2PO4-H2O, 1mM MgCl2, 2mM CaCl2, 25mM glucose) at a rate of 5ml/min bubbled with 95% O2/5% CO2. Whole-cell patch-clamp recording of Grp+ neuron was carried out under oblique illumination with an Olympus fixed-stage microscope system (BX51, Melville, NY, USA). Using a puller (P1000, Sutter, Novato, CA, USA), we fabricated thin-walled glass pipettes (World Precision Instruments, Sarasota, FL, USA) that had a resistance of 3–6 MΩ and were filled with internal solution (120mM K-gluconate, 20mM KCl, 2mM MgCl2, 0.5mM EGTA, 2mM Na2-ATP, 0.5mM Na2-GTP, and 20mM HEPES). The cells were voltage clamped at –70 mV. Membrane current signals were sampled at 10kHz and low-pass filtered at 2 kHz. We monitored R series and R input and discarded cells if either of these values changed by more than 20%.
DRGs were collected from mice, which were deeply anesthetized with 2% isoflurane (Abbott Laboratories, North Chicago, IL, USA) and put in cold DH10 medium (DMEM/F-12 with 10% fetal bovine serum and 1% penicillin/streptomycin, Gibco) and treated with enzyme solution (5mg/ml dispase and 1mg/ml collagenase Type I in HBSS without Ca2+ and Mg2+, Gibco) at 37°C. After trituration and centrifugation, cells were resuspended in DH10 with nerve growth factor (50ng/ml, Upstate) and glial cell line-derived neurotrophic factor (25ng/ml, R&D Systems), plated on glass coverslips coated with poly-D-lysine (100 μg/ml, Biomedical Technologies) and laminin (10μg/ml, Invitrogen), cultured at 37°C, and used after 20–40 hours. Whole-cell recording of MrgprA3 positive DRG neurons were performed with Axon 700B amplifier and pClamp 10 software (Molecular Devices, Sunnyvale, CA). The thin-walled glass pipettes were pulled by a puller (P1000, Sutter, Novato, CA, USA) with the resistance of 2–4 MΩ.
Dorsal roots stimulation was applied by a suction electrode at 500μA, sufficient to activate C-fibers, using a Master-9 Pulse Stimulator and Iso-Flex Stimulus Isolator (AMPI, Jerusalem, Israel). For light stimulation mediated by channelrhodopsin, the LED blue light (465 nm, 300 mW/cm2) was elicited by a high power LED illumination system(LEX2-B, Brainvision) through the Olympus fixed-stage microscope system (BX51, Melville, NY, USA). The LED illumination system was connected to an A/D converter (Digidata 1440, Axon CNS, Molecular Devices), and controlled by the pClamp10 software (Axon CNS). For DRG attached spinal cord slice Grp neurons recording, drugs were directly puffed on the DRG tissue using the DVD-8VC superfusion application system (ALA Scientific Instruments, Farmingdale, NY, USA). To differentiate monosynaptic and polysynaptic connections, 20 C-fiber-strength electrical stimulation or light stimulation at 1Hz were delivered, neurons with no failure in EPSCs were monosynaptically connected according to established criteria(Nakatsuka et al., 2000).
Calcium imaging of enkephalin-expression neurons was performed with a 700 Zeiss confocal microscope. PenkCre; Rosa26LSL-GCaMP6; GrpEGFP spinal slices were cut as described above. The GrpEGFP neurons were patched and depolarized by 1Hz 50pA current injection. Green fluorescence of patch neurons was monitored to exclude recording of active Penk+ neurons. Patched GrpEGFP neurons were labeled by Red fluorescent dye (Alex Fluor 568, life technologies). Images were acquired at 2.6Hz in frame-scan mode with a 256 × 256 pixel region of interest.
Biocytin Labeling
After 20 min in the whole-cell patch-clamp configuration, the biocytin-filled (0.5%) electrodes were withdrawn from the targeted neuron, and the slices were immersed in 4% paraformaldehyde for 15 min. Spinal slices were then washed with PBS (3 X 20 min) and incubated with Alexa-488 conjugated streptavidin (1:200, Life technologies) at 4°C overnight. After washing with PBS (3 X 20 min), the fluorescent signals of the spinal cord sections were collected as z-series images using a confocal microscope.
Rabies viral tracing
Mice were anesthetized by isoflurane and a laminectomy was performed at the T13-L1 level. A fine glass capillary was inserted into dorsal spinal cord. AAV helper virus, AAV8-LSL-TVA-EGFP-B19G (UNC vector core), was first injected (500nl, 50nl/min). AAV1-LSL-tdTomato virus (Upenn vector core) was similarly injected to visualize Grp+ neurons. EnvA pseudotyped rabies glycoprotein deficient GFP rabies virus (Courtesy of Dr. Fan Wang’s group, Duke University) was injected in the same spot three weeks later. Animals were perfused 7 days after rabies virus injection and processed for immunostaining.
ELISA
GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice and ROSA26LSL-TrpV1; TrpV1−/− littermate controls were deeply anesthetized with isoflurane, decapitated and the lumbar spinal cord was quickly removed to ice-cold, low-sodium Krebs solution which contain: 95mM NaCl, 2.5mM KCl, 26mM NaHCO3, 1.25mM NaH2PO4-H2O, 6mM MgCl2, 1.5mM CaCl2, 25mM glucose, 50mM sucrose, 1mM kynurenic acid bubbled with 95% O2/5% CO2.
Spinal cords were cut into three sagittal sections and then recovered in oxygenated ACSF for about 1h at 37°C. Three sections were subsequently incubated with 200μl oxygenated Krebs solution (125mM NaCl, 2.5mM KCl, 26mM NaHCO3, 1.25mM NaH2PO4-H2O, 1mM MgCl2, 2mM CaCl2, 25mM glucose) with capsaicin (2mg/ml, 5μg/ml and 0μg/ml, respectively) and proteinase inhibitor mix (1μM phosphoramidon, 1μM captopril and 0.1% BSA) for 15 minutes at 37°C. 100μl of ACSF from each sample was then used for the detection of Enkephalin release. ELISA detections of enkephalin were performed following manufacturer’s protocol (FEK02421, Phoenix Pharmaceuticals). Results were normalized to the weight of the tissue. At least six mice were used for each condition.
Behavioral testing
For ablation experiments, we injected 8-week-old GrpCre; ROSA26LSL-DTR;LSL-tdTomato mice and ROSA26LSL-DTR;LSL-tdTomato littermates with diphtheria toxin (intra-peritoneal, 35 μg per kg of body weight, Sigma) twice, separated by 72 h. Behavioral experiments were performed 4 weeks after the first toxin injection.
For back injections, pruritic compounds dissolved in saline were subcutaneously injected into the nape of the neck (50μl) with insulin syringes (26 Gauge). GRPR antagonist (Deamino-Phe19,D-Ala24,D-Pro26-psi(CH2NH)Phe27)-GRP (19–27), 200μM or 2nmol/site) or saline (50μl) were injected 10 minutes before pruritogen injection when indicated. Behavioral responses were video recorded for 30 min. The video recording was subsequently played back in slow motion and the number of bouts of scratching with the hindpaw and directed toward the injection site, were counted.
For the hot plate test, a clear plexiglass cylinder was placed on the plate and the mice were placed inside the cylinder. The onset of brisk hindpaw lifts and/or flicking/licking of the hindpaw was assessed at different temperatures.
For the tail immersion test, mice were gently restrained in a 50ml conical tube into which the mice voluntarily entered. The protruding one-third of the tail was then dipped into a water bath of varying temperatures. The latency to respond to the heat stimulus with vigorous flexion of the tail was measured.
For the Hargreaves test, mice were placed under a transparent plastic box (4.5 × 5 × 10 cm) on a glass floor. The infrared source was placed under the glass floor and the infrared light was delivered to the hindpaw. The latency for the animal to withdraw its hindpaw was measured.
For the Von Frey filament test, mice were placed under a transparent plastic box (4.5 × 5 × 10 cm) on a metal mesh. Von Frey filaments, each delivering a different bending force, were applied to the hind paw using the up-down method and the threshold force corresponding to 50% withdrawal was determined.
For the chemically induced pain test, 10μl of capsaicin and 7μl of capsaicin were injected in cheek and paw respectively and the numbers of front paw wipes or the time of licking/flinching responses were counted in 10 minutes.
For the rotarod test, each mouse was trained for 5 min at a constant speed of 4 rpm on the rotarod (Rotamex, Columbus Instruments). The first trial started at least 1h after training. Every day, each mouse received three trials, separated by 30 min, at speeds accelerating from 4 to 40 rpm (with a 4 rpm increase every 30 s). Each mouse was tested for three consecutive days. The trial was finished when the mouse fell off the rotarod. The latency to falling off the rotarod was recorded and used in subsequent analyses.
For specifc activation of Grp+ neurons, GrpCre; ROSA26LSL-TrpV1; TrpV1−/− mice were intrathecally injected with different amounts of capsaicin or capsaicin with naloxone (0.1mg/ml), naltrindole (0.2mg/ml), CTAP (0.5mg/ml), CTOP (1mg/ml), cycloSOM (0.1mM) and bicuculline (10μM). Lumber puncture were made with 30 gauge needles and drugs at 10μl of volume were delivered. Lower back regions of mice were shaved a day before injections. High definition videos were recorded from the top for 30 minutes with four mirrors to enable views of all angles. Video recordings were subsequently played back at 1/5 normal speed. The durations of licking directed to lower back region with a characteristic frequency of 5Hz were quantified in the first four minutes and bouts of scratching were counted in 30 minutes. ROSA26LSL-TrpV1; TrpV1−/− littermates were used as controls. Wild type and TrpV1−/− mice were also intrathecally injected with GRP, BNP and capsaicin. Licking and scratching behaviors quantified as reference.
For light mediated activation of MrgprA3+ neurons, MrgprA3Cre; ROSA26LSL-ChR2 mice with shaved nape regions were given 100 ms blue light at 1Hz or 5Hz and litter mate ROSA26LSL-ChR2 mice were used as controls. Scratching bouts were counted in 5minute time period. Sham operations without blue light were used to determine baseline scratch numbers.
QUANTIFICATION AND STATISTICAL ANALYSIS
Data are presented as mean ± s.e.m. n represents the number of mice analyzed. The distribution of the variables in each experimental group was assumed normal. Most statistical comparisons were conducted by two-tailed, unpaired Student’s t test. Two-way ANOVA followed by post hoc Student-Newmann-Keuls tests were used for comparison between capsaicin and pruritogen-induced responses. Extended Welch’s t test was used for the comparison of ratios of ablated responses and control responses, where student t tests and ANOVA tests could not apply. Power analysis was used to justify the sample size. No data was excluded. Differences were considered to be statistically significant for P < 0.05. Representative data are from experiments that were replicated biologically at least three times with similar results. Statistical analysis done with R.
Extension of Welch’s t test: μ1h: mean of log value of ablated responses, high dose; μ1l mean of log value of ablated responses, low dose; μ2h: mean of log value of control responses, high dose; μ2l: mean of log value of control responses, low dose. Null hypothesis H0: (μ1h - μ2h) - (μ1l - μ2l) = 0. Alternative H1: (μ1h - μ2h) - (μ1l - μ2l) > 0. Test statistics: , where μ̄ detonates the sample means of the subgroup. , where s2 denotes the sample variance and n is the sample size. Under H0, the test statistics follows t-distribution and the degrees of freedom,
Dose response curve fitting for capsaicin mediated activation:
Itch dose responses were fit with Hill equation:
Pain dose responses were fit with polynomial equation: y=0.469 − 3.882x + 11.38x2 − 1.904x3 + 0.08229x4
Supplementary Material
Acknowledgments
We thank Dr. Fan Wang at Duke University for deficient rabies virus. We thank C. Hawkins and the staff of Transgenic Mouse Core at Johns Hopkins University for assistance with transgenic mouse lines. We thank Dr. Hongzhen Hu at Washington University for allowing us to use their optogenetics apparatus. We also thank Dr. Pamela Colleen Lavinka and Dr. Dustin Green at Johns Hopkins University for manuscript editing and Dr. Zhixiang Lin at Stanford University for help with statistics. The work was supported by grants from the US National Institutes of Health to X.D. (R01DE022750 and R01NS054791). X.D. is an Investigator of the Howard Hughes Medical Institute.
Footnotes
AUTHOR CONTRIBUTIONS
S.S. and X.D. initiated the project. S.S. carried out the genetic manipulations, immunostainings and most of the behavioral experiments. C.G. and Q.L. contributed to optogenetics experiments. Q.X. and Y.G. performed electrophysiological recordings. Q.X. and S.S. performed virus-tracing experiments. S.S. and X.D. wrote the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akiyama T, Carstens MI, Carstens E. Excitation of mouse superficial dorsal horn neurons by histamine and/or PAR-2 agonist: potential role in itch. J Neurophysiol. 2009a;102:2176–83. doi: 10.1152/jn.00463.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akiyama T, Merrill AW, Carstens MI, Carstens E. Activation of superficial dorsal horn neurons in the mouse by a PAR-2 agonist and 5-HT: potential role in itch. J Neurosci. 2009b;29:6691–9. doi: 10.1523/JNEUROSCI.6103-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alon U. Network motifs: theory and experimental approaches. Nat Rev Genet. 2007;8:450–61. doi: 10.1038/nrg2102. [DOI] [PubMed] [Google Scholar]
- Bell AM, Gutierrez-Mecinas M, Polgár E, Todd AJ. Spinal neurons that contain gastrin-releasing peptide seldom express Fos or phosphorylate extracellular signal-regulated kinases in response to intradermal chloroquine. Mol Pain. 2016:12. doi: 10.1177/1744806916649602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourane S, Duan B, Koch SC, Dalet A, Britz O, Garcia-Campmany L, Kim E, Cheng L, Ghosh A, Ma Q, Goulding M. Gate control of mechanical itch by a subpopulation of spinal cord interneurons. Science (80-) 2015;350:550–554. doi: 10.1126/science.aac8653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braz J, Solorzano C, Wang X, Basbaum AI. Transmitting pain and itch messages: a contemporary view of the spinal cord circuits that generate gate control. Neuron. 2014;82:522–36. doi: 10.1016/j.neuron.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesselin F, Bourgoin S, Artaud F, Hamon M. Basic and Regulatory Mechanisms of In Vitro Release of Met-Enkephalin from the Dorsal Zone of the Rat Spinal Cord. J Neurochem. 1984;43:763–774. doi: 10.1111/j.1471-4159.1984.tb12798.x. [DOI] [PubMed] [Google Scholar]
- Davidson S, Zhang X, Khasabov SG, Moser HR, Honda CN, Simone DA, Giesler GJ. Pruriceptive spinothalamic tract neurons: physiological properties and projection targets in the primate. J Neurophysiol. 2012;108:1711–23. doi: 10.1152/jn.00206.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson S, Zhang X, Khasabov SG, Simone DA, Giesler GJ. Relief of itch by scratching: state-dependent inhibition of primate spinothalamic tract neurons. Nat Neurosci. 2009;12:544–6. doi: 10.1038/nn.2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson S, Zhang X, Yoon CH, Khasabov SG, Simone DA, Giesler GJ. The itch-producing agents histamine and cowhage activate separate populations of primate spinothalamic tract neurons. J Neurosci. 2007;27:10007–14. doi: 10.1523/JNEUROSCI.2862-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan B, Cheng L, Bourane S, Britz O, Padilla C, Garcia-Campmany L, Krashes M, Knowlton W, Velasquez T, Ren X, Ross SE, Lowell BB, Wang Y, Goulding M, Ma Q. Identification of spinal circuits transmitting and gating mechanical pain. Cell. 2014;159:1417–32. doi: 10.1016/j.cell.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming MS, Ramos D, Han SB, Zhao J, Son YJ, Luo W. The majority of dorsal spinal cord gastrin releasing peptide is synthesized locally whereas neuromedin B is highly expressed in pain- and itch-sensing somatosensory neurons. Mol Pain. 2012;8:52. doi: 10.1186/1744-8069-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukushima T, Tsuda M, Kofuji T, Hori Y. Physiological properties of enkephalin-containing neurons in the spinal dorsal horn visualized by expression of green fluorescent protein in BAC transgenic mice. BMC Neurosci. 2011;12:36. doi: 10.1186/1471-2202-12-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong S, Zheng C, Doughty ML, Losos K, Didkovsky N, Schambra UB, Nowak NJ, Joyner A, Leblanc G, Hatten ME, Heintz N. A gene expression atlas of the central nervous system based on bacterial artificial chromosomes. Nature. 2003;425:917–925. doi: 10.1038/nature02033. [DOI] [PubMed] [Google Scholar]
- Grudt TJ, Perl ER. Correlations between neuronal morphology and electrophysiological features in the rodent superficial dorsal horn. J Physiol. 2002;540:189–207. doi: 10.1113/jphysiol.2001.012890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han L, Ma C, Liu Q, Weng HJ, Cui Y, Tang Z, Kim Y, Nie H, Qu L, Patel KN, Li Z, McNeil B, He S, Guan Y, Xiao B, Lamotte RH, Dong X. A subpopulation of nociceptors specifically linked to itch. Nat Neurosci. 2013;16:174–82. doi: 10.1038/nn.3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han SK, Mancino V, Simon MI. Phospholipase Cbeta 3 mediates the scratching response activated by the histamine H1 receptor on C-fiber nociceptive neurons. Neuron. 2006;52:691–703. doi: 10.1016/j.neuron.2006.09.036. [DOI] [PubMed] [Google Scholar]
- Handwerker HO. Pain and allodynia, itch and alloknesis: An alternative hypothesis. APS J. 1992;1:135–138. doi: 10.1016/1058-9139(92)90043-C. [DOI] [Google Scholar]
- Handwerker HO, Forster C, Kirchhoff C. Discharge patterns of human C-fibers induced by itching and burning stimuli. J Neurophysiol. 1991;66:307–15. doi: 10.1152/jn.1991.66.1.307. [DOI] [PubMed] [Google Scholar]
- Hunskaar S, Fasmer OB, Hole K. Acetylsalicylic acid, paracetamol and morphine inhibit behavioral responses to intrathecally administered substance P or capsaicin. Life Sci. 1985;37:1835–1841. doi: 10.1016/0024-3205(85)90227-9. [DOI] [PubMed] [Google Scholar]
- Hunskaar S, Post C, Fasmer OB, Arwestrom E. Intrathecal injection of capsaicin can be used as a behavioural nociceptive test in mice. Neuropharmacology. 1986;25:1149–53. doi: 10.1016/0028-3908(86)90163-2. [DOI] [PubMed] [Google Scholar]
- Kaplan S, Bren A, Dekel E, Alon U. The incoherent feed-forward loop can generate non-monotonic input functions for genes. Mol Syst Biol. 2008;4:203. doi: 10.1038/msb.2008.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kardon AP, Polgár E, Hachisuka J, Snyder LM, Cameron D, Savage S, Cai X, Karnup S, Fan CR, Hemenway GM, Bernard CS, Schwartz ES, Nagase H, Schwarzer C, Watanabe M, Furuta T, Kaneko T, Koerber HR, Todd AJ, Ross SE. Dynorphin acts as a neuromodulator to inhibit itch in the dorsal horn of the spinal cord. Neuron. 2014;82:573–86. doi: 10.1016/j.neuron.2014.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMotte RH, Dong X, Ringkamp M. Sensory neurons and circuits mediating itch. Nat Rev Neurosci. 2014;15:19–31. doi: 10.1038/nrn3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMotte RH, Shimada SG, Sikand P. Mouse models of acute, chemical itch and pain in humans. Exp Dermatol. 2011;20:778–82. doi: 10.1111/j.1600-0625.2011.01367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Ko MC. Distinct functions of opioid-related peptides and gastrin-releasing peptide in regulating itch and pain in the spinal cord of primates. Sci Rep. 2015;5:11676. doi: 10.1038/srep11676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis T, Grant RT, Marvin HM. Vascular reactions of the skin to injury. Part X The intervention of a chemical stimulus illustrated especially by the flare. The response to faradism - Google Search [WWW Document] [accessed 7.31.15];Heart. 1927 URL https://www.google.com/search?q=Vascular+reactions+of+the+skin+to+injury+X.+The+intervention+of+a+chemical+stimulus+illustrated+especially+by+the+flare.+The+response+to+faradism&oq=Vascular+reactions+of+the+skin+to+injury+X.+The+intervention+of+a+chemical.
- Liu Q. Mechanisms of itch evoked by beta-alanine. J Neurosci. 2012;32:14532–14537. doi: 10.1523/JNEUROSCI.3509-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q. The distinct roles of two GPCRs, MrgprC11 and PAR2, in itch and hyperalgesia. Sci Signal. 2011;4:ra45. doi: 10.1126/scisignal.2001925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Sikand P, Ma C, Tang Z, Han L, Li Z, Sun S, LaMotte RH, Dong X. Mechanisms of itch evoked by β-alanine. J Neurosci. 2012;32:14532–7. doi: 10.1523/JNEUROSCI.3509-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Tang Z, Surdenikova L, Kim S, Patel KN, Kim A, Ru F, Guan Y, Weng HJ, Geng Y, Undem BJ, Kollarik M, Chen ZF, Anderson DJ, Dong X. Sensory neuron-specific GPCR Mrgprs are itch receptors mediating chloroquine-induced pruritus. Cell. 2009;139:1353–65. doi: 10.1016/j.cell.2009.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon SB, Koltzenburg M. Itching for an explanation. Trends Neurosci. 1992;15:497–501. doi: 10.1016/0166-2236(92)90102-E. [DOI] [PubMed] [Google Scholar]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–9. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Milo R, Shen-Orr S, Itzkovitz S, Kashtan N, Chklovskii D, Alon U. Network motifs: simple building blocks of complex networks. Science. 2002;298:824–7. doi: 10.1126/science.298.5594.824. [DOI] [PubMed] [Google Scholar]
- Mishra SK, Hoon MA. The Cells and Circuitry for Itch Responses in Mice. Science (80-) 2013;340:968–971. doi: 10.1126/science.1233765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatsuka T, Ataka T, Kumamoto E, Tamaki T, Yoshimura M. Alteration in synaptic inputs through C-afferent fibers to substantia gelatinosa neurons of the rat spinal dorsal horn during postnatal development. Neuroscience. 2000;99:549–56. doi: 10.1016/s0306-4522(00)00224-4. [DOI] [PubMed] [Google Scholar]
- Neuman B, Wiedermann CJ, Fischer-Colbrie R, Schober M, Sperk G, Winkler H. Biochemical and functional properties of large and small dense-core vesicles in sympathetic nerves of rat and ox vas deferens. Neuroscience. 1984;13:921–31. doi: 10.1016/0306-4522(84)90106-4. [DOI] [PubMed] [Google Scholar]
- Norrsell U, Finger S, Lajonchere C. Cutaneous sensory spots and the “law of specific nerve energies”: history and development of ideas. Brain Res Bull. 1999;48:457–465. doi: 10.1016/S0361-9230(98)00067-7. [DOI] [PubMed] [Google Scholar]
- Ochoa J, Torebjörk E. Sensations evoked by intraneural microstimulation of C nociceptor fibres in human skin nerves. J Physiol. 1989;415:583–99. doi: 10.1113/jphysiol.1989.sp017737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmelz M, Schmidt R, Bickel A, Handwerker HO, Torebjork HE. Specific C-Receptors for Itch in Human Skin. J Neurosci. 1997;17:8003–8008. doi: 10.1523/JNEUROSCI.17-20-08003.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmelz M, Schmidt R, Weidner C, Hilliges M, Torebjork HE, Handwerker HO. Chemical response pattern of different classes of C-nociceptors to pruritogens and algogens. J Neurophysiol. 2003;89:2441–8. doi: 10.1152/jn.01139.2002. [DOI] [PubMed] [Google Scholar]
- Sikand P, Dong X, LaMotte RH. BAM8-22 peptide produces itch and nociceptive sensations in humans independent of histamine release. J Neurosci. 2011a;31:7563–7. doi: 10.1523/JNEUROSCI.1192-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikand P, Shimada SG, Green BG, LaMotte RH. Sensory responses to injection and punctate application of capsaicin and histamine to the skin. Pain. 2011b;152:2485–2494. doi: 10.1016/j.pain.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikand P, Shimada SG, Green BG, LaMotte RH. Similar itch and nociceptive sensations evoked by punctate cutaneous application of capsaicin, histamine and cowhage. Pain. 2009;144:66–75. doi: 10.1016/j.pain.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solorzano C, Villafuerte D, Meda K, Cevikbas F, Bráz J, Sharif-Naeini R, Juarez-Salinas D, Llewellyn-Smith IJ, Guan Z, Basbaum AI. Primary afferent and spinal cord expression of gastrin-releasing peptide: message, protein, and antibody concerns. J Neurosci. 2015;35:648–57. doi: 10.1523/JNEUROSCI.2955-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spike RC, Puskár Z, Andrew D, Todd AJ. A quantitative and morphological study of projection neurons in lamina I of the rat lumbar spinal cord. Eur J Neurosci. 2003;18:2433–48. doi: 10.1046/j.1460-9568.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- Sun YG, Chen ZF. A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord. Nature. 2007;448:700–3. doi: 10.1038/nature06029. [DOI] [PubMed] [Google Scholar]
- Sun YG, Zhao ZQ, Meng XL, Yin J, Liu XY, Chen ZF. Cellular basis of itch sensation. Science. 2009;325:1531–4. doi: 10.1126/science.1174868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd AJ. Neuronal circuitry for pain processing in the dorsal horn. Nat Rev Neurosci. 2010;11:823–36. doi: 10.1038/nrn2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd AJ, Spike RC, Russell G, Johnston HM. Immunohistochemical evidence that Met-enkephalin and GABA coexist in some neurones in rat dorsal horn. Brain Res. 1992;584:149–156. doi: 10.1016/0006-8993(92)90888-G. [DOI] [PubMed] [Google Scholar]
- Tuckett RP. Itch evoked by electrical stimulation of the skin. J Invest Dermatol. 1982;79:368–73. doi: 10.1111/1523-1747.ep12529734. [DOI] [PubMed] [Google Scholar]
- Von frey M. Zur Physiologie der Juckempfindung [WWW Document] [accessed 7.31.15];Arch Neerl Physiol. 1922 URL https://www.google.com/webhp?sourceid=chrome-instant&ion=1&espv=2&ie=UTF-8#q=von+Frey+M.+Arch.+Neerl.+Physiol.+Vol.+7.+1922.+Zur+Physiologie+der+Juckempfindung%3B+pp.+142%E2%80%93145.
- Wall PD. The gate control theory of pain mechanisms. A re-examination and re-statement. Brain. 1978;101:1–18. doi: 10.1093/brain/101.1.1. [DOI] [PubMed] [Google Scholar]
- Wickersham IR, Lyon DC, Barnard RJO, Mori T, Finke S, Conzelmann KK, Young JAT, Callaway EM. Monosynaptic restriction of transsynaptic tracing from single, genetically targeted neurons. Neuron. 2007;53:639–47. doi: 10.1016/j.neuron.2007.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaksh TL, Farb DH, Leeman SE, Jessell TM. Intrathecal capsaicin depletes substance P in the rat spinal cord and produces prolonged thermal analgesia. Science. 1979;206:481–3. doi: 10.1126/science.228392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.