Abstract
Aim
The aim of the present study was to describe the prescription of medications for attention‐deficit hyperactivity disorder (ADHD) in the UK between 1995 and 2015.
Methods
Using the Clinical Practice Research Datalink (CPRD), we defined a cohort of all patients aged 6–45 years, registered with a general practitioner between January 1995 and September 2015. All prescriptions of methylphenidate, dexamphetamine/lisdexamphetamine and atomoxetine were identified and annual prescription rates of ADHD were estimated using Poisson regression.
Results
Within a cohort of 7 432 735 patients, we identified 698 148 prescriptions of ADHD medications during 41 171 528 person‐years of follow‐up. Usage was relatively low until 2000, during which the prescription rate was 42.7 [95% confidence interval (CI) 20.9, 87.2] prescriptions per 10 000 persons, increasing to 394.4 (95% CI 296.7, 524.2) in 2015, corresponding to an almost 800% increase (rate ratio 8.87; 95% CI 7.10, 11.09). The increase was seen in all age groups and in both sexes but was steepest in boys aged 10–14 years. The prescription rate in males was almost five times that of females. Methylphenidate remained the most prescribed drug during the 20‐year study period, representing 88.9% of all prescriptions in the 6–24‐year‐old group, and 63.5% of all prescriptions in adults (25–45 years of age).
Conclusions
Prescription rates of ADHD medications have increased dramatically in the past two decades. This may be due, at least in part, to both an increase in the number of patients diagnosed with ADHD over time and a higher percentage of those patients treated with medication.
Keywords: attention‐deficit hyperactivity disorder, CPRD, methylphenidate, time trends, UK
What is Already Known about this Subject
Attention‐deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder in school‐aged children.
What this Study Adds
Prescription rates of ADHD medications have increased dramatically in the UK in the past two decades, particularly in children and adolescents.
This increase is likely to relate to both an increase in the number of patients diagnosed with ADHD over time and a higher percentage of patients treated with medications. Longer duration of use of ADHD drugs, as well as more frequent off‐label use, may also contribute to the increasing prescription rates.
Introduction
Attention‐deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder in school‐aged children, characterized by symptoms of inattention, impulsivity and hyperactivity 1. Symptoms may persist beyond childhood and some individuals are not diagnosed with ADHD until adulthood 2.
In the past few decades, an increased prevalence of ADHD and use of ADHD medications has been observed in several countries 3, 4, 5, 6, 7, 8, 9, including the UK 10, raising concerns about possible overdiagnosis and inappropriate prescription of ADHD medications. In this context, in July 2013 the National Institute for Health and Care Excellence (NICE) issued a reminder to avoid methylphenidate in children and young people with moderate ADHD 11, 12. Indeed, in the UK, pharmacological treatment of ADHD is only recommended for severe and persistent symptoms of ADHD in children and for the treatment of moderate symptoms when psychological interventions have been unsuccessful or are unavailable 13. Pharmacological treatment is the first‐line therapy for adults with ADHD with either moderate or severe levels of impairment but the only licensed drug for adults is atomoxetine, the others being used off‐label 13.
Longitudinal trends of ADHD medication prescription have not been updated recently, and trends in prescriptions over the last two decades have not been studied to date. This is important and needed as it allows a more accurate picture of long‐term trends, rather than possible insignificant short‐term changes. In addition, despite a growing interest in adults with ADHD, most studies have been restricted to children and little is known about the prescribing patterns of ADHD medication in adults. Moreover, studies have focused on cohorts of patients diagnosed with ADHD rather than on volumes of prescriptions regardless of a confirmed diagnosis of ADHD 10, 14, 15. This could lead to an underestimation of prescription rates, especially in primary care databases such as the Clinical Practice Research Datalink (CPRD) as a diagnosis is not systematically recorded with a prescription. Therefore, we aimed to describe the time trends in the prescribing of ADHD medications in UK primary care between 1995 and 2015 in children, adolescents and adults, focusing on different age groups, sex and different types of ADHD medications.
Methods
Data source
The present study was conducted using the UK CPRD database. This is one of the world's largest electronic databases of anonymized primary care medical records on a population of over 13 million patients enrolled with more than 680 general practices 16, 17. The geographic distribution of the practices, as well as the age and sex distributions of patients, broadly reflects that of the UK population. The CPRD contains information such as demographic data, medical diagnoses, procedures and referrals to specialists and hospitals that are documented by trained general practitioners (GP). Prescriptions dispensed by the GP are automatically recorded on the computerized patient file. Data completeness and quality of data, as well as consistency with medical files, are checked regularly, and have been shown to be valid 18, 19, 20.
Study population
We defined a cohort of all patients between 6 years and 45 years of age, with known sex and year of birth, and registered with a GP for at least 1 day between 1 January 1995 and 30 September 2015. Patients below 6 years of age were not included because NICE guidelines do not recommend drug treatment with ADHD medications in preschool children 13 and we expected prescription rates to be very low in this age group. Overall prescription rates were still provided for this age group but this information was not included in any of the other analyses. Patients with an unknown month of birth were assigned the date 1 July in their year of birth. For patients who registered with the general practice in the year of their birth, the date of registration was taken as their date of birth. Follow‐up started on 1 January 1995, patients’ 6th birthday, patients’ registration date with the general practice or the date that the practice started to contribute valid data to the CPRD (‘up to standard date’), whichever came later. Follow‐up ended at the patients’ 46th birthday, transfer out of the practice, death or the end of the study period (30 September 2015), whichever occurred first.
ADHD medications
We identified all ADHD medications listed in the British National Formulary (BNF). These drugs belong to the class of central nervous system stimulants (BNF chapter 4.4), and those licensed in the UK include methylphenidate, dexamphetamine (and lisdexamphetamine) and atomoxetine. Methylphenidate was licensed in the UK in 1972, atomoxetine in 2004 and dexamphetamine in 2008. Pemoline was an ADHD drug removed from the UK market in September 1997 owing to its associated liver toxicity; therefore it was not included in the present study. ADHD medications have virtually no other indications. Although unlicensed, methylphenidate can be used in the treatment of narcolepsy and in several other psychiatric disorders such as autism spectrum disorder 21.
Statistical analysis
For the entire study period, the follow‐up time for each patient in our cohort was classified in the following mutually exclusive age categories: 6–9 years, 10–14 years, 15–18 years, 19–24 years and 25–45 years. Patients changed age category on the day they completed the last year of a given age category. The person‐time denominator included all patients whether or not they were prescribed an ADHD medication. Based on the list of ADHD drugs defined in the previous section, we identified all corresponding prescriptions for all patients in the cohort during their follow‐up time. The number of ADHD prescriptions was calculated for each calendar year of follow‐up for each individual based on their age category. Prescription rates were calculated by dividing the total number of prescriptions in each calendar year by the total number of person‐years of follow‐up.
We calculated each calendar year's prescription rate and corresponding 95% confidence interval (CI) using Poisson regression. Annual prescription rates were also stratified by age, sex and different ADHD drugs. We estimated rate ratios (RR), adjusted for age and sex, comparing annual prescription rates with 2000 as the reference year, and then with the preceding calendar year as the reference. We also estimated the average annual change in prescription rates between 2000 and 2015, stratified by age and sex. All models included an overdispersion parameter to account for extra‐Poisson variation present in the data. The annual excess rate of prescriptions was calculated by means of a linear regression model with calendar time as a linear predictor in the model. For this analysis, the year 2000 was chosen as the starting point as prescription rates were low up to this point and started to increase linearly thereafter. In secondary analyses, we examined whether the increasing number of prescriptions over time may have been due, at least in part, to an increase in the number of newly diagnosed or newly treated patients. We estimated the number of patients with a first prescription for an ADHD drug (incident users) during the entire study period stratified by calendar year, age and sex. We also estimated the number of patients with a first ADHD diagnosis (incident cases) recorded in the CPRD during the study period, regardless of ADHD medications, to describe the trends in ADHD diagnosis over time. Among these newly diagnosed patients, we calculated the percentage being prescribed an ADHD drug within 1 year of ADHD diagnosis over time. In this last analysis, estimates were provided up to 2014 because no information was available for the last three months of 2015, which could have led to biased estimates. Finally, in order to confirm that most prescriptions were related to an ADHD diagnosis, we estimated the percentage of patients with an ADHD diagnosis recorded at any time during follow‐up among patients with at least one prescription for an ADHD medication. Confidence intervals were calculated using a significance level of 5%. All statistical procedures were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
The study protocol was approved by the Independent Scientific Advisory Committee of the CPRD (protocol number 15_231) and the Research Ethics Board of the Jewish General Hospital, Montreal, QC, Canada. This protocol was made available to the journal reviewers.
Results
Within a cohort of 7 432 735 patients, we identified 698 148 prescriptions of ADHD medications during 41 171 528 person‐years of follow‐up, yielding a rate of 169.6 (95% CI 156.4, 183.8) prescriptions per 10 000 persons per year. Most prescriptions were delivered to male patients (84.2%) and the majority were children and adolescents: 20.5% were aged 6–9 years, 48.5% were 10–14 years, 19.6% were 15–18 years, 6.2% were 19–24 years and 5.3% were 25–45 years of age.
Table 1 displays the prescription rates stratified by age and sex. The highest rate was seen in boys aged 10–14 years, with a prescription rate of 1239.4 per 10 000 persons per year (95% CI 1098.6, 1398.3). Prescription rates were much lower in girls, the highest rate being in those aged 10–14 years (203.9 per 10 000 persons per year; 95% CI 177.5, 234.2). As expected, prescription rates in children below 6 years of age were low, with an overall rate of 8.4 prescriptions per 10 000 persons per year (95% CI 6.7, 10.5) – 14.6 (11.1, 19.3) for boys, and 1.9 (1.4, 2.6) for girls. As shown in Figure 1, there was a steady increase in prescription rates from 1995, more marked in men compared with women, and from 2000 onwards. A similar steady increase was observed in all four UK regions (England, Wales, Scotland and Northern Ireland) (data not shown). The same time trends were noted when stratified by age, the steepest increase being in children and adolescents, particularly those aged 10–14 years (Figure 2). Overall, prescription rates increased by around 800% between 2000 and 2015 (RR 8.87; 95% CI 7.10, 11.09) (Table 2). Table 3 displays the yearly increase in prescription rates from 2000 to 2015 by age and sex. The yearly increased rate of ADHD prescriptions was 14% between 2000 and 2015, with an average of 23 additional prescriptions per 10 000 persons per year.
Table 1.
Person‐time, number of attention‐deficit hyperactivity disorder prescriptions and prescription rates in the UK Clinical Practice Research Datalink, 1995–2015
| Age group | Person‐years | Number of prescriptions | Prescription rate per 10 000 per year (95% confidence interval) |
|---|---|---|---|
| Overall | 41 171 528 | 698 148 | 169.6 (156.4, 183.8) |
| Boys/men | 20 994 364 | 587 929 | 280.0 (251.9, 311.4) |
| Girls/women | 20 177 163 | 110 219 | 54.6 (49.8, 60.0) |
| 6–9 years | 3 682 383 | 143 195 | 388.9 (333.8, 453.1) |
| Boys/men | 1 899 842 | 123 025 | 647.6 (559.0, 750.1) |
| Girls/women | 1 782 541 | 20 170 | 113.2 (95.7, 133.8) |
| 10–14 years | 4 559 005 | 338 547 | 742.6 (650.2, 848.1) |
| Boys/men | 2 371 698 | 293 954 | 1239.4 (1098.6, 1398.3) |
| Girls/women | 2 187 307 | 44 593 | 203.9 (177.5, 234.2) |
| 15–18 years | 3 539 915 | 136 557 | 385.8 (323.6, 459.9) |
| Boys/men | 1 855 452 | 115 526 | 622.6 (509.7, 760.6) |
| Girls/women | 1 684 463 | 21 031 | 124.9 (101.1, 154.2) |
| 19–24 years | 5 454 278 | 43 120 | 79.1 (67.1, 93.1) |
| Boys/men | 2 762 650 | 33 994 | 123.0 (99.8, 151.7) |
| Girls/women | 2 691 628 | 9126 | 33.9 (27.7, 41.6) |
| 25–45 years | 23 935 947 | 36 729 | 15.3 (14.3, 16.5) |
| Boys/men | 12 104 723 | 21 430 | 17.7 (15.9, 19.8) |
| Girls/women | 11 831 224 | 15 299 | 12.9 (11.8, 14.1) |
Figure 1.

Attention‐deficit hyperactivity disorder prescription rates in the UK Clinical Practice Research Datalink, 1995–2015, overall and stratified by sex.  , Boys/Men;
, Boys/Men;  , Girls/Women;
, Girls/Women;  , Overall
, Overall
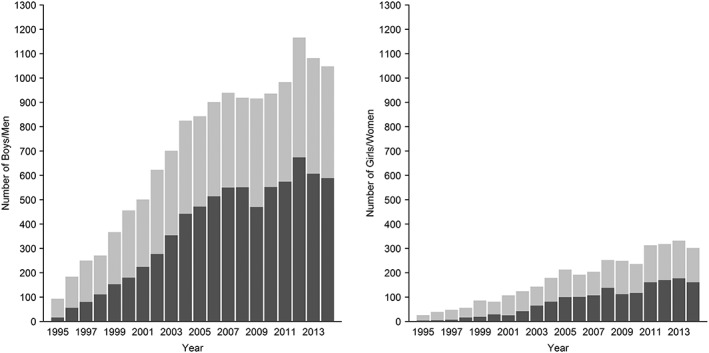
Figure 2.

Attention‐deficit hyperactivity disorder prescription rates in the UK Clinical Practice Research Datalink, 1995–2015, stratified by age group, among boys/men (A) and girls/women (B).  , 6–9;
, 6–9;  , 10–14;
, 10–14;  , 15–18;
, 15–18;  , 19–24;
, 19–24;  , 25–45
, 25–45
Table 2.
Time trends in attention‐deficit hyperactivity disorder prescription rates in the UK Clinical Practice Research Datalink, 1995–2015
| Year | Prescription rate per 10 000 [95% confidence interval (CI)] | Crude rate ratio compared with 2000 | Adjusted * rate ratio (95% CI) Compared with 2000 | Adjusted * rate ratio (95% CI) Compared with preceding year |
|---|---|---|---|---|
| 1995 | 4.8 (0.2, 112.6) | 0.11 | 0.12 (0.05, 0.31) | 1.00 (Ref for 1996 only) |
| 1996 | 13.0 (2.1, 80.1) | 0.30 | 0.32 (0.18, 0.56) | 2.63 (0.91, 7.57) |
| 1997 | 23.7 (6.7, 83.0) | 0.55 | 0.57 (0.37, 0.86) | 1.79 (0.94, 3.40) |
| 1998 | 31.0 (11.1, 86.6) | 0.73 | 0.73 (0.51, 1.06) | 1.30 (0.81, 2.08) |
| 1999 | 34.6 (14.3, 83.6) | 0.81 | 0.81 (0.58, 1.13) | 1.11 (0.75, 1.64) |
| 2000 | 42.7 (20.9, 87.2) | 1.00 | 1.00 (Reference) | 1.23 (0.88, 1.71) |
| 2001 | 50.4 (27.0, 94.0) | 1.18 | 1.17 (0.89, 1.54) | 1.17 (0.89, 1.54) |
| 2002 | 64.0 (37.8, 108.1) | 1.50 | 1.48 (1.14, 1.91) | 1.26 (0.99, 1.60) |
| 2003 | 86.3 (55.6, 133.9) | 2.02 | 1.97 (1.55, 2.52) | 1.34 (1.10, 1.63) |
| 2004 | 107.2 (73.0, 157.5) | 2.51 | 2.44 (1.93, 3.09) | 1.24 (1.04, 1.46) |
| 2005 | 127.5 (90.0, 180.8) | 2.98 | 2.89 (2.30, 3.65) | 1.19 (1.02, 1.38) |
| 2006 | 155.7 (113.6, 213.2) | 3.64 | 3.53 (2.81, 4.43) | 1.22 (1.06, 1.40) |
| 2007 | 189.8 (142.9, 252.1) | 4.44 | 4.31 (3.45, 5.38) | 1.22 (1.08, 1.38) |
| 2008 | 209.4 (159.6, 274.6) | 4.90 | 4.75 (3.81, 5.93) | 1.10 (0.98, 1.24) |
| 2009 | 225.0 (173.0, 292.7) | 5.27 | 5.13 (4.11, 6.39) | 1.08 (0.97, 1.20) |
| 2010 | 240.4 (186.0, 310.8) | 5.63 | 5.48 (4.39, 6.83) | 1.07 (0.96, 1.19) |
| 2011 | 268.9 (210.2, 344.0) | 6.29 | 6.11 (4.91, 7.61) | 1.12 (1.01, 1.24) |
| 2012 | 295.9 (233.5, 374.9) | 6.92 | 6.75 (5.43, 8.40) | 1.10 (1.00, 1.22) |
| 2013 | 322.6 (255.3, 407.6) | 7.55 | 7.36 (5.91, 9.15) | 1.09 (0.99, 1.20) |
| 2014 | 353.1 (278.8, 447.2) | 8.26 | 7.97 (6.41, 9.92) | 1.08 (0.98, 1.19) |
| 2015 | 394.4 (296.7, 524.2) | 9.23 | 8.87 (7.10, 11.09) | 1.11 (1.00, 1.24) |
Adjusted for age and sex
Table 3.
Annual changes in attention‐deficit hyperactivity disorder prescription rates in the UK Clinical Practice Research Datalink, 2000–2015
| Age group | Prescription rate per 10 000 in 2000 | Prescription rate per 10 000 in 2014 * | Yearly increase [95% confidence interval (CI)] from 2000 to 2015 | Excess annual rate † (95% CI) from 2000 to 2015 |
|---|---|---|---|---|
| Overall | 42.7 | 353.1 | 1.14 (1.12, 1.15) | 23.33 (22.06, 24.60) |
| Boys/men | 73.5 | 568.7 | 1.13 (1.11, 1.15) | 37.49 (35.78, 39.20) |
| Girls/women | 10.4 | 134.3 | 1.17 (1.15, 1.19) | 9.06 (7.99, 10.13) |
| 6–9 years | 173.6 | 621.1 | 1.09 (1.07, 1.10) | 35.03 (31.94, 38.11) |
| Boys/men | 296.1 | 1018.4 | 1.08 (1.07, 1.10) | 56.69 (51.06, 62.32) |
| Girls/women | 38.1 | 206.3 | 1.11 (1.09, 1.13) | 12.90 (11.92, 13.88) |
| 10–14 years | 196.0 | 1319.5 | 1.11 (1.09, 1.13) | 84.78 (79.01, 90.55) |
| Boys/men | 330.1 | 2184.6 | 1.11 (1.09,1.13) | 140.05 (129.18, 150.93) |
| Girls/women | 43.9 | 417.6 | 1.14 (1.12, 1.17) | 28.71 (27.05, 30.38) |
| 15–18 years | 38.6 | 859.4 | 1.18 (1.14, 1.21) | 62.92 (59.01, 66.83) |
| Boys/men | 68.1 | 1350.1 | 1.17 (1.14, 1.21) | 100.33 (94.10, 106.55) |
| Girls/women | 5.2 | 348.9 | 1.22 (1.19, 1.25) | 24.16 (20.72, 27.59) |
| 19–24 years | 5.9 | 274.0 | 1.30 (1.29, 1.32) | 19.39 (14.54, 24.25) |
| Boys/men | 5.6 | 423.1 | 1.31 (1.29, 1.34) | 30.71 (23.51, 37.90) |
| Girls/women | 6.3 | 123.8 | 1.28 (1.24, 1.31) | 7.99 (5.36, 10.62) |
| 25–45 years | 3.4 | 53.1 | 1.24 (1.22, 1.27) | 3.54 (2.37, 4.72) |
| Boys/men | 4.5 | 70.8 | 1.30 (1.26, 1.34) | 4.71 (2.95, 6.47) |
| Girls/women | 2.2 | 35.4 | 1.18 (1.16, 1.21) | 2.37 (1.77, 2.98) |
Rates are not presented for 2015 because data were available only up to 30 September 2015 and not for the entire year.
Estimated by linear regression, using year as a continuous variable.
As shown in Figure 3, most of the increase in ADHD drug prescriptions over time was related to methylphenidate, although a slight increase in the use of other drugs was also noted. This over‐representation of methylphenidate compared with other ADHD medications was evident in both sexes, particularly in children and young adults. In this age group (6–24 years), methylphenidate represented 88.9% of all prescriptions, atomoxetine 9.1% and dexamphetamine only 2%, with similar figures in both sexes. In adults (25–45 years of age), 63.5% of all prescriptions were for methylphenidate, 8.5% for atomoxetine, and 28% for dexamphetamine. The percentages varied slightly by sex so that in men, 67.6% of prescriptions were for methylphenidate 10.5% for atomoxetine and 21.9% for dexamphetamine, whereas in women this was 57.8%, 5.7% and 36.5%, respectively.
Figure 3.

Attention‐deficit hyperactivity disorder prescription rates in the UK Clinical Practice Research Datalink, 1995–2015, stratified by drugs.  , Methylphenidate;
, Methylphenidate;  , Atomoxetine;
, Atomoxetine;  , Dexamfetamine
, Dexamfetamine
Considering only the number of patients with a first prescription for an ADHD medication, there was a clear increase in the number of newly treated patients over the two decades in both sexes, particularly in young boys (Figure 4). Similarly, the number of patients with a first recorded diagnosis of ADHD in the CPRD increased steadily from 1995 to 2015 (Figure 5). Among these newly diagnosed patients, 16.8% were treated with an ADHD drug within 1 year of diagnosis in 1995, 38.9% in 2000, rising to 55.6% in 2014, when 56.2% of males and 53.3% of females newly diagnosed with ADHD were treated with an ADHD drug within 1 year of diagnosis (Figure 6). Overall, more than 80% of patients using ADHD medications had a diagnosis of ADHD recorded in their medical record during the study period (Appendix 1).
Figure 4.

Number of patients starting an attention‐deficit hyperactivity disorder (ADHD) medication per 100 000 persons per year in the UK Clinical Practice Research Datalink, 1995–2015, among boys/men (A) and girls/women (B).  , 6–9;
, 6–9;  , 10–14;
, 10–14;  , 15–18;
, 15–18;  , 19–24;
, 19–24;  , 25–45
, 25–45
Figure 5.

Number of patients with a first attention‐deficit hyperactivity disorder (ADHD) diagnosis per 100 000 persons per year in the UK Clinical Practice Research Datalink, 1995–2015, among boys/men (A) and girls/women (B).  , 6–9;
, 6–9;  , 10–14;
, 10–14;  , 15–18;
, 15–18;  , 19–24;
, 19–24;  , 25–45
, 25–45
Figure 6.
Number of patients with an attention‐deficit hyperactivity disorder prescription within 1 year of diagnosis in the UK Clinical Practice Research Datalink, 1995–2014.  , Treated;
, Treated;  , Untreated
, Untreated
Discussion
In the present large, population‐based study in UK primary care, we found a dramatic increase in the number of prescriptions of ADHD medications over the past two decades. Indeed, the prescription rates increased eightfold between 2000 and 2015. This rise in prescription rates was particularly pronounced in younger males, although an increased rate was observed in virtually every age group, as well as in female patients. Methylphenidate remained the most prescribed drug over the years, particularly in children and young adults.
A similar trend toward an increase in the number of prescriptions for ADHD medications over time has been observed elsewhere, with substantial variation between countries. In the USA, a 2.5‐fold increase in the use of methylphenidate in youths with ADHD was observed from 1990 to 1995 7. Between 1995 and 2010, a fourfold increase in ADHD medication visits was noted while the use of any stimulant medication increased from 4.0% of young people in 1996–1998 to 6.6% in 2010–2012 22, 23. The prevalence of school‐aged children on ADHD medication increased 14‐fold in Hong Kong between 2001 and 2013, from 0.072% to 1.027% 5. Given the 20‐year period of our study, the observed increase in prescription rates in the UK does not stand out compared with that in other countries. In addition, as the prescription rate of ADHD medications was virtually zero in the UK in 1990, a substantial increase occurred relatively quickly, whereas in countries where volumes of prescriptions were already high, the relative increase over time was less dramatic. In the UK, a few studies have reported an increase in ADHD diagnosis and treatment in the last decade. In the Health Improvement Network (THIN) database, the annual prevalence and incidence of pharmacologically treated ADHD increased from 2003 to 2008, with a twofold increase in prevalence for children and adolescents, and a 4–5‐fold increase for adults 10. Another study identified all patients aged 15–21 years within the CPRD with at least one prescription for an ADHD drug and found a sixfold increase in prevalence between 1999 and 2006 24. However, another recent study reported that both the incidence and prevalence of ADHD diagnosis rose from 1998 to 2007, and slightly decreased between 2007 and 2010 14. Studying trends in prescriptions for ADHD drugs up to 2015, our results indicate that, despite a slight decrease in prescribing around 2007–2009, overall prescription rates have risen continuously since 1995, particularly since 2000, with no clear signs of prescribing slowing down. These findings also underline the importance of looking at long periods when monitoring drug use, in order not to misinterpret a transient decrease in prescription rates as a signal of a sustained decline in drug use.
There may be several reasons to explain this continuous and important increase in the number of prescriptions of ADHD medications in the UK. ADHD may be increasingly diagnosed, leading to a rise in the number of treated patients, and thus more prescriptions issued over time. Previous studies have found the prevalence of ADHD to be lower in Europe, including the UK, than in North America, with reported figures around 8.8% in the USA 9, 25, against 3.5–5.6% in France 26, 5% in the Netherlands 27 and 3–5% in the UK 28. These inconsistent estimates may be explained by the use of tighter diagnostic criteria for ADHD in Europe, and the UK in particular. It has also been hypothesized that ADHD has been overdiagnosed in the USA, while possibly being under‐recognized in some other countries. Therefore, the continuous rise in prescriptions that we observed might relate to a better diagnosis and treatment of a previously unrecognized disease. Indeed, we found that the number of patients diagnosed with ADHD rose over the study period but our data do not allow any conclusion to be drawn on whether those ADHD diagnoses were appropriate or not. Physicians may also be more prone now than previously to initiate a pharmacological treatment for these patients. Indeed, the proportion of patients prescribed ADHD drugs around the time of diagnosis also increased over the two decades. In the UK, first‐line treatment of ADHD in children is a psychological intervention; pharmacological treatment is only recommended for severe and persistent symptoms and for the treatment of moderate symptoms when psychological interventions have been unsuccessful or are unavailable. Recent health resource restrictions, in particular regarding psychological services, may have led to the pharmacological treatment of patients who would otherwise have been referred for psychological interventions. Interestingly, an association has recently been reported between the incidence of ADHD diagnosis and socioeconomic deprivation in the UK, underlying the need for adequate service provision in deprived areas, as concluded by these authors 29. Pharmacological treatment may also be chosen over psychological intervention because parents or physicians are not willing to wait for improvement when a drug can provide a rapid benefit. Owing to concerns about the possible inappropriate prescription of ADHD medications, in July 2013 NICE issued a reminder to avoid prescribing methylphenidate in children and young individuals with moderate ADHD 11. In 2009, the European Medicines Agency also made recommendations for the safer use of Ritalin and other methylphenidate‐containing medicines 30. Indeed, while these drugs have a proven short‐term benefit in children with ADHD, there are concerns about their potential cardio‐ and cerebrovascular safety profile 31, and it is unknown whether these drugs have a long‐term benefit in patients with ADHD. Despite these concerns, we did not observe any decline in the number of prescriptions, including of methylphenidate, over the last few years. Methylphenidate remained the most frequently prescribed drug over the entire study period, with a continuous increase in the volume of prescriptions. However, it is possible that the NICE recommendations affected the prescribing behaviour of UK physicians and that these changes were not visible in our results because our data collection ended in September 2015 and longer follow‐up would have been needed to detect such a change. On the other hand, these recommendations may have induced a shift toward treating more severe patients without being perceived in overall prescribing trends. Moreover, without information on the severity and clinical profile of treated patients with ADHD, we cannot assess if there was a change over time in the clinical profile of treated patients.
Some other factors may have contributed to the increased usage of ADHD drugs over time observed in the present study. The duration of ADHD treatment may have increased, which would have manifested in our results as an increase in prescription rates. However, although this phenomenon could have contributed to the increasing volume of prescriptions, it is unlikely to have been the sole explanation for such a large and ongoing increase. More importantly, we showed a parallel increase in the number of patients issued a first ADHD medication over time, so the rise in prescription rates cannot be explained solely by the increasing duration of treatment. GPs may also have become more involved in the management of ADHD than in the past, and may more frequently dispense ADHD prescriptions that were previously prescribed by specialists, although, again, this is unlikely to be the full explanation for such an increase. The guidance for the diagnosis of ADHD is that it is made by specialists, and as these recommendations have not changed during the study period, the ADHD diagnoses recorded in the CPRD were probably made mostly by specialists, with these patients subsequently followed up by GPs. Therefore, the increasing trends both in ADHD prescriptions and diagnoses are not likely to reflect solely the major involvement of GPs in ADHD diagnosis currently. Finally, the off‐label use of ADHD medications for other conditions, as well as the abuse and misuse of ADHD drugs in adolescents and adults, may also be increasing over time. However, we suspect that the quantities involved in drug misuse represent a small part of the total usage 32.
As expected, prescription rates were much higher in boys compared with girls in every age group as ADHD is more prevalent in the former. Although there may be some pathophysiological explanation for the higher prevalence of ADHD in boys, it has been argued that this condition is underdiagnosed in girls because they experience fewer symptoms of disruptive behaviour than boys 33. We showed that the increase in prescription rates over time was steepest in males compared with females, both in children and adults, although the difference between sexes was more pronounced in children. When translated into a yearly percentage increase in prescriptions, there was a 17% increase in females and a 14% increase in males. This slightly higher annual percentage increase in females is due to a lower rate in 2000, the year of reference. However, not surprisingly, the number of additional prescriptions per year was much higher in males than females overall and in all age categories. Although prescription rates were much lower in adults than in children, the same trend toward an increased rate was noted over time, particularly for those aged 19–24 years, with a more modest rise in adults aged 25–45 years, similar to the findings in some other studies 34, 35. This underlines the importance of developing adult ADHD services to ensure adequate follow‐up and treatment of these patients. Indeed, a UK longitudinal study of ADHD patients aged 15–21 years from 1999 to 2006 suggested that treatment is sometimes be stopped prematurely in young adults 24. We found that methylphenidate was the most prescribed drug in adults, even though the only medication licensed for ADHD in this age group in the UK is atomoxetine. However, the NICE guidelines recommend methylphenidate as the first‐line drug in adults with ADHD 13. Therefore, the increased prescription rates may reflect, particularly in this age group, an increased off‐label use and possibly a rise in the misuse of ADHD drugs – a concern that has been raised previously but is difficult to confirm or to quantify 32, 36.
This study presents the most recent update of longitudinal time trends of ADHD drug prescriptions in the UK. We used the CPRD, a large and high‐quality database of primary care records, which has been used extensively in pharmacoepidemiology. The CPRD is broadly representative of the UK population, ensuring an accurate representation of the dynamics of ADHD prescriptions across the country. Moreover, we provide a comprehensive picture of prescribing trends both in children and adults, whereas many studies have focused exclusively on children. Previous studies defined cohorts of patients with an ADHD diagnosis or selected only patients with both a diagnosis and a treatment. This could lead to an underestimation of prescription rates as a diagnosis is not systematically recorded with a prescription in many databases. We therefore chose to study volumes of prescriptions regardless of associated diagnosis, rather than defining a cohort of patients with an ADHD diagnosis as we were primarily interested in ADHD medication overall, and not in ADHD. In the present study, there was no record of a diagnostic code for ADHD or for narcolepsy in around 20% of patients with a prescription for an ADHD medication. We only searched for specific codes of ADHD and not for symptoms such as poor concentration or behavioural problems. This may have reduced the percentage of patients identified with an ADHD diagnosis but ensured that we did not include those with unspecific symptoms. Moreover, our aim was to describe prescription trends of ADHD medications, not specifically to describe ADHD. Nevertheless, our results are likely to be an accurate reflection of prescription trends predominantly in relation to ADHD as we still found an ADHD diagnosis in around 80% of patients when using only specific diagnostic codes for ADHD. As previously noted, these medications may be used off‐label in various other conditions such as narcolepsy but, as expected, we found a minor percentage of all prescriptions associated with this diagnosis.
Interestingly, we found an increasing number of patients with a first diagnosis of ADHD over time, giving support to our findings of an increase in the number of prescriptions related to an ADHD diagnosis. Prescriptions are automatically recorded in the computerized file when issued by the GP, so the total count of prescriptions is accurate; however, we could not capture ADHD medications issued in hospitals or by specialists. Therefore, the number of ADHD medications and prescription rates are likely to have been underestimated in the present study and higher than we report here, although this does not preclude a valid description of prescribing trends over time. In addition, the first prescription of an ADHD drug issued by the GP and the first ADHD diagnosis recorded in the CPRD may not correspond to the first ever prescription and the real date of ADHD diagnosis, as diagnosis and treatment initiation are presumably made in secondary care; however, again, this does not preclude the accurate description of trends over time. It is unlikely that the severity of the disease affects the recording of the diagnosis because the CPRD contains the actual computerized medical file of patients, anonymized for research purposes. As gatekeepers of the health system, GPs see all patients with ADHD, regardless of severity, and record all medical histories in their files. Of note, we considered the extra‐Poisson variation from sex, age and calendar year in our estimation of the CIs. We did not take into account extra‐Poisson variation between practices, which may have slightly narrowed the CIs around the point estimates. Finally, as detailed information on diagnoses was not available, the severity of ADHD was unknown. Thus, it was not possible to assess whether prescriptions in children were issued for severe ADHD, as recommended by the NICE guidelines, or if the mental health impairment of treated patients has changed over time. We also have no insight into the potential misuse of these drugs in adolescents and adults.
In summary, prescription rates for ADHD medications have increased dramatically in the past two decades. This is likely to relate, at least in part, both to an increase in the number of patients diagnosed with ADHD over time and a higher percentage of patients receiving pharmacological treatment. A longer duration of use of ADHD drugs, as well as more frequent off‐label use, may also contribute to the increasing prescription rates. Further research is warranted to describe whether the clinical profile and mental health impairment of patients diagnosed and treated for ADHD have changed over time. It will also be important to attempt to quantify and monitor off‐label use of ADHD drugs in the future.
Competing Interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.”
CR is the recipient of a Chercheur‐Boursier Award from the Fonds de la recherche en santé du Québec (FRSQ).
Contributors
CR conceived the study. SD and SS critically reviewed the study protocol. SD analysed the data. J‐YS performed the literature review and helped to draft the manuscript. EF had an invaluable role in the interpretation of the data. All coauthors provided critical revisions to the manuscript. CR was responsible for drafting the manuscript and incorporating the suggestions of the coauthors and is the guarantor of the manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. The lead author (the manuscript's guarantor) affirms that the manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Appendix 1.
Number of patients using attention‐deficit hyperactivity disorder medications with a specific diagnosis in the UK Clinical Practice Research Datalink, 1995–2015

Renoux, C. , Shin, J. ‐Y. , Dell'Aniello, S. , Fergusson, E. , and Suissa, S. (2016) Prescribing trends of attention‐deficit hyperactivity disorder (ADHD) medications in UK primary care, 1995–2015. Br J Clin Pharmacol, 82: 858–868. doi: 10.1111/bcp.13000.
References
- 1. Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth edn. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- 2. Moffitt TE, Houts R, Asherson P, Belsky DW, Corcoran DL, Hammerle M, et al. Is adult ADHD a childhood‐onset neurodevelopmental disorder? Evidence from a four‐decade longitudinal cohort study. Am J Psychiatry 2015; 172: 967–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brault M‐C, Lacourse É. Prevalence of prescribed attention‐deficit hyperactivity disorder medications and diagnosis among Canadian preschoolers and school‐age children: 1994–2007. Can J Psychiatry 2012; 57: 93–101. [DOI] [PubMed] [Google Scholar]
- 4. Chai G, Governale L, McMahon AW, Trinidad JP, Staffa J, Murphy D. Trends of outpatient prescription drug utilization in US children, 2002–2010. Pediatrics 2012; 130: 23–31. [DOI] [PubMed] [Google Scholar]
- 5. Man KK, Ip P, Hsia Y, Chan EW, Chui CS, Lam MP, et al. ADHD drug prescribing trend is increasing among children and adolescents in Hong Kong. J Atten Disord 2014. DOI: 10.1177/1087054714536047 [DOI] [PubMed] [Google Scholar]
- 6. Ponizovsky AM, Marom E, Fitoussi I. Trends in attention deficit hyperactivity disorder drugs consumption, Israel, 2005–2012. Pharmacoepidemiol Drug Saf 2014; 23: 534–8. [DOI] [PubMed] [Google Scholar]
- 7. Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics 1996; 98: 1084–8. [PubMed] [Google Scholar]
- 8. Treceno C, Martin Arias LH, Sainz M, Salado I, Garcia Ortega P, Velasco V, et al. Trends in the consumption of attention deficit hyperactivity disorder medications in Castilla y Leon (Spain): changes in the consumption pattern following the introduction of extended release methylphenidate. Pharmacoepidemiol Drug Saf 2012; 21: 435–41. [DOI] [PubMed] [Google Scholar]
- 9. Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent‐report of health care provider‐diagnosed and medicated attention‐deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry 2014; 53: 34–46.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCarthy S, Wilton L, Murray ML, Hodgkins P, Asherson P, Wong IC. The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatr 2012; 12: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Institute for Health and Care Excellence . Avoid drug treatment for children and young people with moderate ADHD. 2013. [online]. Available at www.nice.org.uk/news/article/avoid‐drug‐treatment‐for‐children‐and‐young‐people‐with‐moderate‐adhd (last accessed 22 May 2016).
- 12. McClure I. Prescribing methylphenidate for moderate ADHD. BMJ 2013; 347: f6216. [DOI] [PubMed] [Google Scholar]
- 13. National Institute for Health and Care Excellence . Attention deficit hyperactivity disorder –diagnosis and management of ADHD in children, young people and adults. QS39. 2013. [online]. Available at http://publications.nice.org.uk/attention‐deficit‐hyperactivitydisorder‐qs39 (last accessed 22 May 2016).
- 14. Holden SE, Jenkins‐Jones S, Poole CD, Morgan CL, Coghill D, Currie CJ. The prevalence and incidence, resource use and financial costs of treating people with attention deficit/hyperactivity disorder (ADHD) in the United Kingdom (1998 to 2010). Child Adolesc Psychiatry Ment Health 2013; 7: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jick H, Kaye JA, Black C. Incidence and prevalence of drug‐treated attention deficit disorder among boys in the UK. Br J Gen Pract 2004; 54: 345–7. [PMC free article] [PubMed] [Google Scholar]
- 16. Garcia Rodriguez LA, Perez GS. Use of the UK General Practice Research Database for pharmacoepidemiology. Br J Clin Pharmacol 1998; 45: 419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015; 44: 827–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 2010; 69: 4–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jick SS, Kaye JA, Vasilakis‐Scaramozza C, Garcia Rodriguez LA, Ruigomez A, Meier CR, et al. Validity of the general practice research database. Pharmacotherapy 2003; 23: 686–9. [DOI] [PubMed] [Google Scholar]
- 20. Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract 2010; 60: e128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dalsgaard S, Nielsen HS, Simonsen M. Five‐fold increase in national prevalence rates of attention‐deficit/hyperactivity disorder medications for children and adolescents with autism spectrum disorder, attention‐deficit/hyperactivity disorder, and other psychiatric disorders: a Danish register‐based study. J Child Adolesc Psychopharmacol 2013; 23: 432–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Olfson M, Blanco C, Wang S, Laje G, Correll CU. National trends in the mental health care of children, adolescents, and adults by office‐based physicians. JAMA Psychiatry 2014; 71: 81–90. [DOI] [PubMed] [Google Scholar]
- 23. Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. N Engl J Med 2015; 372: 2029–38. [DOI] [PubMed] [Google Scholar]
- 24. McCarthy S, Asherson P, Coghill D, Hollis C, Murray M, Potts L, et al. Attention‐deficit hyperactivity disorder: treatment discontinuation in adolescents and young adults. Br J Psychiatry 2009; 194: 273–7. [DOI] [PubMed] [Google Scholar]
- 25. Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry 2003; 2: 104–13. [PMC free article] [PubMed] [Google Scholar]
- 26. Lecendreux M, Konofal E, Faraone SV. Prevalence of attention deficit hyperactivity disorder and associated features among children in France. J Atten Disord 2011; 15: 516–24. [DOI] [PubMed] [Google Scholar]
- 27. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007; 164: 942–8. [DOI] [PubMed] [Google Scholar]
- 28. Wong IC, Asherson P, Bilbow A, Clifford S, Coghill D, DeSoysa R, et al. Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) –a pharmacoepidemiological and qualitative study. Health Technol Assess 2009; 13: iii–v .ix–xi, 1–120 [DOI] [PubMed] [Google Scholar]
- 29. Hire AJ, Ashcroft DM, Springate DA, Steinke DT. ADHD in the United Kingdom: regional and socioeconomic variations in incidence rates amongst children and adolescents (2004–2013). J Atten Disord 2015. DOI: 10.1177/1087054715613441 [DOI] [PubMed] [Google Scholar]
- 30. European Medicines Agency . European Medicines Agency makes recommendations for safer use of Ritalin and other methylphenidate‐containing medicines in the EU 2009 [online]. Available at http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2009/11/news_detail_000218.jsp&mid=WC0b01ac058004d5c1 (last accessed 22 May 2016).
- 31. Westover AN, Halm EA. Do prescription stimulants increase the risk of adverse cardiovascular events?: a systematic review. BMC Cardiovasc Disord 2012; 12: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaye S, Darke S. The diversion and misuse of pharmaceutical stimulants: what do we know and why should we care? Addiction 2012; 107: 467–77. [DOI] [PubMed] [Google Scholar]
- 33. Staller J, Faraone SV. Attention‐deficit hyperactivity disorder in girls: epidemiology and management. CNS Drugs 2006; 20: 107–23. [DOI] [PubMed] [Google Scholar]
- 34. Castle L, Aubert RE, Verbrugge RR, Khalid M, Epstein RS. Trends in medication treatment for ADHD. J Atten Disord 2007; 10: 335–42. [DOI] [PubMed] [Google Scholar]
- 35. Pottegard A, Bjerregaard BK, Glintborg D, Hallas J, Moreno SI. The use of medication against attention deficit hyperactivity disorder in Denmark: a drug use study from a national perspective. Eur J Clin Pharmacol 2012; 68: 1443–50. [DOI] [PubMed] [Google Scholar]
- 36. Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry 2008; 47: 21–31. [DOI] [PubMed] [Google Scholar]


