Abstract
For younger patients with extra-articular distal humerus fractures closed management is plagued with high rates of malunion, suboptimal functional outcomes, extended immobilization with loss of early motion, a delay in return to work, and a general period of lost productivity. Surgical management offers an appealing alternative. Maintaining respect for the triceps musculature and minimizing iatrogenic injury to the radial nerve are primary concerns with operative treatment. Accordingly, use of a triceps-sparing approach and single column plating may be the optimal treatment paradigm in the young patient presenting with an extra-articular distal humerus fracture.
Keywords: Extra-articular distal humerus fracture, Single column plating, Dual column plating, Sarmiento bracing
1. Introduction
The goals of care in the young active patient with extra-articular distal humeral fracture include uneventful fracture healing with optimized alignment. Further, return of pre-injury functionality is essential. Elbow motion should be preserved as well as muscle strength and endurance. Although closed management with a Sarmiento brace is an option for care, formal open reconstruction is preferred.
Traditional exposure for the operative treatment of distal humerus fracture is the triceps-splitting approach yet triceps-sparing method is gaining in popularity. Choice of approach is critical to prevent complications of surgery, which include radial nerve injury, stiffness, and muscle weakness. Lastly, fixation can involve single column plating, dual column plating, and even dual plating along one column.1
The purpose of this article is to demonstrate the merits of an optimized surgical care plan for these fractures, while also showing the limits of nonoperative treatment. Choice of surgical exposure, reduction technique, and internal fixation strategy can positively affect clinical outcome whilst minimizing complications for the distal humeral fracture in the younger more high demand patient. Best care paradigm for surgical reconstruction includes respect and care for the already traumatized soft tissue envelope, especially the triceps musculature and vulnerable radial nerve. In addition, achieving and maintaining optimal fracture alignment until union with low profile and well-contoured hardware is advisable.
1.1. Conservative treatment for the distal humerus fracture- functional bracing
In order to properly evaluate the relative merits of surgical intervention for this injury, nonoperative treatment and the resultant outcomes must be considered. This requires a thorough review of Sarmiento’s original functional bracing outcomes2, as well as other authors’ attempts to replicate his results in the years following.
1.1.1. Sarmiento functional bracing outcomes
Originally described by Sarmiento2, functional bracing has been shown to have a significant role in the treatment of humeral fractures for the general population2. Still, the younger high demand patient with a distal humeral fracture is perhaps not best served with this treatment method. The resultant outcomes of closed management in terms of nonunion, malunion, and adjacent joint function according to Sarmiento and others are typically not acceptable for this patient population. Further, inconvenience and short term morbidity with bracing makes this a less attractive option.
While Sarmiento’s series of 85 patients with distal third humeral fractures boasted a union rate of 96%, adjacent joint motion loss and malunion were significant.3 Malunion was noted in the vast majority of his patients, typically in the form of varus alignment. In active patients with high functional demands the loss of motion and malunion undoubtedly have a significant toll on their daily life and impede their ability to return to pre-injury activity level.
Consistent with these well documented yet infrequently discussed suboptimal outcomes by Sarmiento, newer literature has emerged further reaffirming the prevalence of unsatisfactory outcomes with bracing.
1.1.2. Nonunion with nonoperative treatment, post-Sarmiento
The 96% union rate reported by Dr. Sarmiento unfortunately has not been reproduced in further studies on functional bracing for distal humeral fracture. Ali et al. recently showed a 15% nonunion rate for distal third humerus fractures when treated with conservative treatment in 26 patients.4 Riera et al., in a larger study on humeral fractures, demonstrated a 12% nonunion rate in 162 patients.5 Ekholm et al. recently reported on a series of 78 patients treated conservatively with humeral fractures, 10% required secondary operation due to nonunion.6 Discrepancy in results between Sarmiento and others could be attributable to the substantial loss of follow-up noted in Sarmiento’s studies. Indeed, in Sarmiento’s largest series there was a 33% loss of follow-up.7
1.1.3. Malunion with nonoperative treatment
Although rates of nonunion with functional bracing are varied, malunion or deformity is commonplace, which is typically both functionally and cosmetically unacceptable for the young active patient. Sarmiento et al. reported varus malunion in eighty one percent of distal humerus fractures.3 In another study by Jawa et al. comparing conservative to operative management, distal humeral fractures treated in a brace had an average twelve-degree varus deformity.8 This was in contrast to their operative cohort that had minimal residual deformity after union. In a study of 21 patients treated with functional bracing for distal humeral fractures, Pehlivan found 38% of patients had varus angulation.9 Further, Riera et al. reported an 18% deformity rate in 162 humeral fractures treated in a functional brace.5
1.1.4. Functional outcomes with conservative treatment
Perhaps of greater importance to the young active patient is the ultimate functionality achieved after treatment and subsequent rehabilitation after distal humeral fracture. A concern with functional bracing is “cast disease” resulting in stiffness of adjacent joint especially the elbow but also the shoulder as well. Using a functional brace, specifically for distal humeral fractures, Sarmiento reported both shoulder and elbow dysfunction in a subset of his patients. At the shoulder, 45% of patients had a decrease in external rotation (range: 5 to 45 ° loss), and more than 15% lost abduction (range: 10 to 60 ° loss). At the elbow, 26% lost flexion (range: 5 to 25 ° loss) and 24% lost extension (range: 5 to 25°).3 In Ekholm’s study of 78 patients, 50% did not self-assess themselves as ‘fully recovered’ from their injury at final follow- up.6 Koch et al. reported on 67 patients and found that only 50% of their patients had ‘excellent’ functional outcomes defined as ‘normal, symmetric range of motion of shoulder and elbow; no pain’.10
1.1.5. Brace inconvenience
Beyond objective musculoskeletal data on the limitations of usage of the functional brace for the management of distal third humeral fracture, patient satisfaction can be compromised. Short term morbidity in terms of comfort, convenience, and early return to activity should be considered in the younger patient. Further, maturity and compliance as it relates to brace use is integral to its effectiveness, which can be especially challenging in the younger patient that potentially lacks the discipline and patience needed with this treatment. Sarmiento noted that compliance was the single most important factor leading to success with functional bracing.11, 12 Woon described some of the common pitfalls with brace wear including the tendency to remove the brace frequently, moving the arm excessively, loosening the straps for comfort and losing the intended sleeve-compression effect of the brace, as well as resting the elbow when upright and not allowing gravity to restore alignment.12 Jawa et al. reported that nearly 10% of patients with extraarticular distal humerus fractures treated with functional bracing had skin breakdown requiring brace discontinuation and transition to a sling.8
Other authors have reaffirmed these challenges associated with brace wear, as Jawa wrote:
‘With a fracture brace and sling, the pain and instability of the fracture make the arm relatively useless for at least 4 weeks…and up to 8 weeks…Even basic daily tasks are difficult on one’s own...Shoulder and elbow motion return but it can take weeks to months of uncomfortable stretching exercises. Some people have skin problems in the brace- particularly in hot, humid weather.’13
Clearly, the difficulties with brace wear and the younger patient’s desire to get back to a meaningful state of life in a timely manner can make bracing a less attractive if not inferior option compared to surgical fixation.
1.1.6. Secondary intervention after failed brace treatment
With these challenges of brace treatment comes the need to consider the significant consequences to failed brace management. Typically, operation is the only meaningful solution to correct nonunion, deformity, and stiffness (Fig. 1). As compared to operation in the acute setting, the rate of complication is higher and the functional result is less desirable.
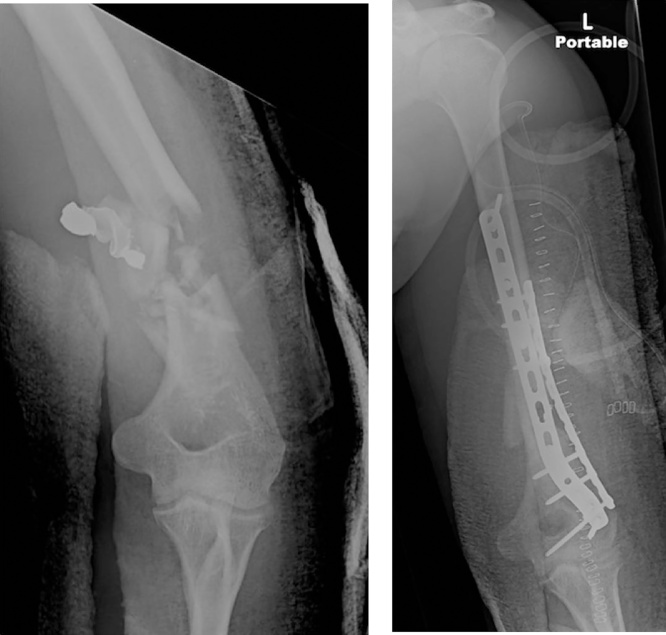
Fig. 1.
Malunion of open distal humerus fracture managed in Sarmiento brace initially. Anteroposterior (a) and lateral (b) radiographs with 13 ° varus and 27 ° procurvatum deformity. Patient desired correction of deformity and elbow contracture release secondary to pain, limited motion and cosmetic appearance. (c) Operative correction of malunion with opening wedge osteotomy, tricortical autograft, and dual column plating.
Working in scarified soft tissue envelope makes dissection more challenging and puts the radial nerve at increased risk for injury. In addition, callus can encase the nerve or place it under tension, putting the nerve at high risk.14 The incidence of radial nerve palsy after humeral shaft nonunion surgery has been reported from 4% to nearly 20%.14, 15, 16, 17, 18 Specifically for distal humerus nonunion surgery, Kakazu et al. noted a nearly 20% iatrogenic radial nerve palsy, whether patients initially were treated conservatively or with surgery.14
For the patient with loss of motion at the elbow after brace treatment several options exist. Static progressive and dynamic elbow splinting can be considered for a patient presenting within the first 6 months.19 For those who fail nonoperative treatment for their posttraumatic elbow stiffness, surgical contracture release is the next option. While this is met with good results, there is no doubt that it involves a demanding and long course of rehabilitation.19
The potential morbidity and ultimate functional result of operation in delayed fashion for the distal humeral fracture is certainly life altering. Aside from radial nerve concerns, the lost productivity, excess time off work, stiffness, and muscle wasting that occur during the extended course of a nonunion are difficult to quantify but certainly significant. This is especially true for the young patient that would otherwise be active, working, and productive.
1.2. Surgical treatment for the distal humerus fracture- patient selection
As compared to the limitations of functional bracing for extra-articular distal humeral fractures in the young patient, operation has been met with largely positive outcomes. Rigid fixation with earlier rehab and range of motion exercises translates into better adjacent joint motion and less stiffness. In a recent series of 30 patients, Maresca et al. noted full elbow ROM in 25 cases, extension loss of 5 ° in 4 cases, and extension loss of 10 ° in one patient.20 Decreased malunion rates have been shown with operative intervention, particularly avoidance of varus malalignment.8 Lastly, for the majority of younger patients, operative fixation can significantly improve patient satisfaction by offering a more expedient return to normalcy and activities of daily living.13
With these reported advantages in mind, there are several other factors to consider when evaluating the appropriateness of surgical treatment. These include host factors, fracture and injury characteristics, and radial nerve function.
1.2.1. Individualized care- consideration of host factors when evaluating surgical candidates
As with all orthopedic fractures, patient specific factors should be weighed heavily when managing these injuries. Certainly there are individuals for whom fracture bracing for over 2 months is impractical or even debilitating. Individuals who require use of their extremity for work and a quick return, those who are caregivers for the elderly or young, and those who have no assistance for activities of daily living are primary examples.13 Polytrauma is also a prime indication for operative treatment as described by Tingstad et al.21 This can expedite weight bearing through the extremity, allowing the patient with multiple extremity injuries to use the affected arm to assist in mobilization.
Aside from these situational factors, characteristics of the host themselves need to be taken into account. Humeral fractures occur in a bimodal distribution including the young and aged patient. Sarmiento’s focused studies initially did not take this into account and included a mix of both groups. Although union rates, malunion rates, and motion may not differ drastically between the young and elderly,3, 22 one outcome that inherently affects these two groups differently is the loss of time and loss of early function with conservative treatment. With functional bracing versus operative fixation there is a substantial loss of time to work, time to independence with daily activities, and lost productivity. Returning younger patients to work and recreation promotes productivity and quality of life. For this reason, along with their inherently higher functional demands, it’s typically indicated to fix the younger active patient versus the older lower demand patient.
Other host factors to consider include patients with morbid obesity, pendulous breasts, and poor compliance or tolerance of Sarmiento bracing. These patients should be offered surgical treatment due to the high likelihood of failure with bracing.23
1.2.2. Fracture and injury characteristics
Fracture characteristics and associated neurovascular injuries can further dictate the surgeon’s plan. Specifically, classic criteria for surgical treatment are open fractures, vascular injuries, brachial plexopathies, floating shoulders, floating elbows, segmental fractures, pathologic fractures, and high-velocity gun shot wounds.23 Historically, fractures of the humerus with more than 30 ° angulation in the coronal plane, 20 ° in the AP plane, or 3 cm of shortening qualify for operative treatment.23
1.2.3. Radial nerve injury and indications for surgery
Rates of radial nerve injury with humeral shaft fractures have been described as occurring anywhere from 2% to 17%.24 For distal 1/3 humeral shaft fractures these rates are even higher, with one study finding a 22% rate in Holstein-Lewis type fractures versus 8% in all other humeral shaft fractures.25 Indications for exploration of the nerve acutely include open fractures, vascular injuries, high velocity gun shut wounds, penetrating injuries, and other cases of suspected direct nerve laceration.
While the consensus in the literature appears to be that radial nerve palsy in isolation is not in an indication for operative treatment,26 it is inherently inconclusive. Intuitively, entrapment of the radial nerve in the fracture site is one potential cause of palsy that can be best addressed by open treatment and exposure of the nerve.
Still, proponents of initial observation site a high rate of spontaneous recovery without exploration. In a review of the literature, Shao et al. found a 70.7% rate of radial nerve recovery in patients treated nonoperatively without exploration. However, the mean time to onset of recovery for this group of patients was 7.3 weeks.27 This delayed recovery is in stark contrast to that reported by Pailhé et al., who after operative fixation and exploration of the nerve, noted radial nerve recovery occurred at an average of 3 days after surgery.28 They noted a similar overall recovery rate (75%). For a normally active patient, it can be devastating to have persistent or permanent radial nerve palsy. Regardless of whether nerve function could have eventually returned without surgery, the added value of an earlier nerve recovery and accordant earlier return to function within days, compared to months, makes a strong argument for operative treatment in an active individual. Additional advantages of operative fixation and early exploration include earlier nerve injury characterization and possible repair, less endplate loss, and less muscle atrophy.27
1.3. Techniques for operative intervention
Certainly, as detailed above, there are several reasons why surgical treatment is preferred for a significant number of patients with distal humeral fractures. With operative treatment of this injury however, come several controversies. These include how to minimize the notorious complications associated with surgical treatment, which approach is least morbid and most effective, and whether single plating is sufficient to achieve the goals of stable and reliable fixation.
1.3.1. Avoiding radial nerve dysfunction- triceps-splitting versus triceps-sparing approaches
Operations for distal humeral fracture have been met with significant apprehension as ORIF has been infamously linked to radial nerve palsy. The radial nerve is certainly vulnerable to injury given the close proximity to the fractured anatomy from either stretch or direct trauma. Beyond the initial injury itself, surgery has the potential to create temporary or permanent nerve palsy from a “second hit” phenomena. Unacceptable rates of iatrogenic radial nerve palsy have been reported in the literature for humeral shaft fractures treated operatively, ranging from 4 to as high as 19 percent.29, 30, 31, 32 More specifically, for extra-articular distal humerus fractures, this number has been quoted as high as 16%.8
However, respect and care for the radial nerve can have a profound impact on minimizing this devastating complication. In particular, surgical exposure through a lateral paratricipital approach has been shown to ultimately eliminate post-operative radial nerve palsy.
The two primary approaches to extra articular distal humeral fractures are the paratricipital, or triceps-sparing approach, and the triceps-splitting approach. The triceps-splitting approach is falling out of favor for a multitude of reasons. This approach involves dissection between the long and lateral head of the triceps to expose the medial head. The medial head is then split in the midline to provide bone exposure. This approach is commonly combined with a full thickness peel of the triceps insertion in a subperiosteal fashion over the olecranon for more distal exposure.33, 34
The triceps-sparing technique has several variants but perhaps the most widely accepted and broadly applied variant is that described by Schildhauer.35 Here, the extensor mechanism remains attached to the olecranon. A lateral window is developed between the lateral triceps and posterior border of the humerus and intermuscular septum. The radial nerve is identified and mobilized as needed (Fig. 2). Gerwin et al. found the radial nerve crossed the posterior aspect of the humerus on average 20.7 centimeters proximal to the medial epicondyle and 14.2 centimeters proximal to the lateral epicondyle.36 Laterally, the radial nerve divides with one branch innervating the medial head of the triceps and another branch that is the lower lateral brachial cutaneous nerve;36 this lower lateral brachial cutaneous nerve can be identified intraoperatively and traced back to the radial nerve proper. Lastly, Gerwin quantified that release of the lateral intermuscular septum to mobilize the radial nerve allowed access to 94% of the humeral shaft, versus with the triceps-splitting approach only 55% of the humeral shaft could be exposed.36
Fig. 2.
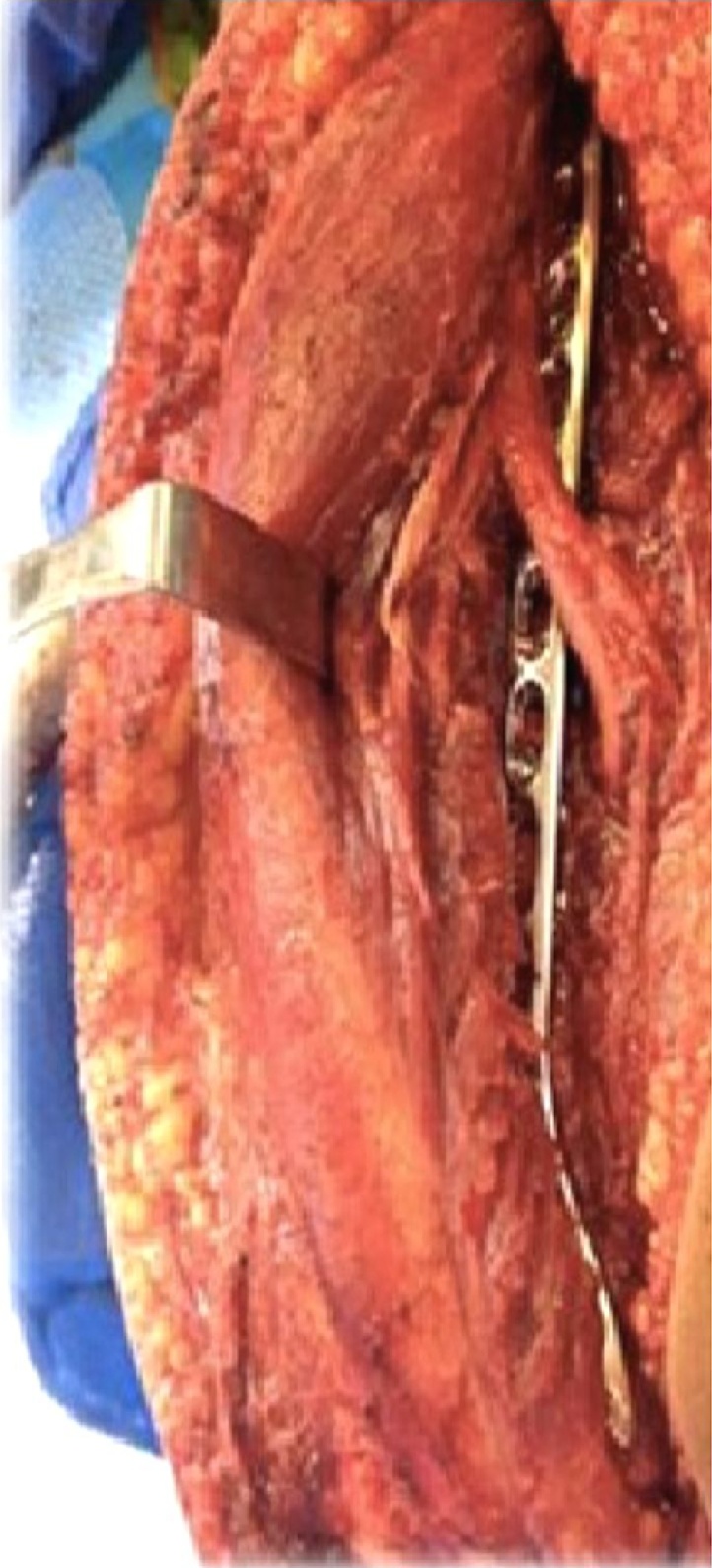
Lateral paratricipital exposure for distal humeral fracture reconstruction heralded for optimal fracture exposure for reduction and instrumentation. Limited iatrogenic muscle damage to triceps compared to splitting method. Radial nerve palsy avoided as release of the lateral intermuscular septum takes tension off of the nerve during fracture care.
The safety of the triceps-sparing approach for the radial nerve was shown by Meloy et al., who reported no new radial nerve palsies in a series of 45 patients treated with ORIF for extra-articular distal humeral fractures using the triceps-sparing technique.37 Voigt et al. further explored the benefits of a lateral paratricipital apparoch for minimizing the incidence of radial nerve palsy during distal humeral ORIF. Here, a cadaveric study demonstrated that the paratricipital approach with release of the intermuscular septum was found to have the lowest rates of strain across the radial nerve compared to a triceps-splitting technique and a paratricipital approach without release of the lateral intermuscular septum.26 Presumably, release of the radial nerve tether as it enters the anterior compartment at the level of the intermuscular septum protects the nerve from traction type injury during fracture manipulation and instrumentation.
1.3.2. Difference in functional outcomes with triceps-splitting versus triceps-sparing approaches
Return of motion and strength are critical for functional success after distal humeral reconstruction. The already traumatized triceps should be respected during operation. Choice of surgical approach will determine the extent of postoperative scarring and resultant muscle health, strength, and excursion.
The advantages of a triceps sparing vs splitting technique are not just limited to the preservation of radial nerve function. Less iatrogenic damage to the triceps with the sparing approach in terms of denervation and scarring improves clinical outcomes with regards to motion, strength, and endurance. While the triceps split has been shown to have favorable results compared to olecranon osteotomy,38, 39, 40 there are few studies that have directly compared triceps splitting versus sparing approaches. In one of these few studies, Illical et al. indeed found better outcomes when the lateral paratricipital approach was utilized versus a splitting technique for extra-articular distal humerus fractures. Better elbow range of motion and triceps strength was realized with the sparring versus splitting method.33
1.3.3. Avoiding hardware complications with distal humeral ORIF- single versus dual plating
Instrumentation after appropriate fracture reduction is a critical factor to consider. Although fracture pattern will dictate plate osteosynthesis strategy, the construct utilized must maintain stability to allow for immediate rehabilitation and uneventful union. Achieving stability of these distal fractures can be challenging considering the diminutive nature of the articular block and the considerable lever arm acting on the fixation construct.
In order to rigidly fix distal third humeral fractures, dual column plating has been accepted as the gold standard method. Dual column fixation provides multiple points of fixation in different planes into the distal humeral segment. Plates can be applied direct medial and lateral as well as posteromedial and posterolateral. Usage of fixed angle screws is also advantageous.
In a cadaveric study by Tejwani et al.41 dual plating was found to be significantly stiffer in bending compared to single column plating. With regards to different dual plating constructs, several recent cadaveric investigations have found parallel plating to be stiffer than orthogonal plating in simulated distal humerus fractures.42, 43, 44
Regardless of whether parallel dual plating or orthogonal dual plating is used however, the improved biomechanics associated with use of a second plate is associated with soft tissue irritability and the potential for nerve dysfunction. Rates of ulnar nerve neuritis have been unacceptably prevalent with this fixation strategy, in some reports as high as 51%.45, 46, 47, 48, 49, 50 This is more than likely related to exposure of the medial column and placement of an implant adjacent to the ulnar nerve. Furthermore, despite ulnar nerve decompression with dual plating, Chen et al. still reported neuritis in approximately 10% of cases.37, 45 In addition, dual plating theoretically involves more periosteal stripping, muscle dissection, blood loss, hardware related tension on neurovascular structures and increased operative times when compared to single column plating.37, 51
As an alternative to dual column plating, technological advances in precontoured fixed angle plates have produced a lateral single column locked plate designed to provide sufficient fixation into the articular block (lateral condyle) with a low profile design. This plate in most cases obviates the need to instrument medially (Fig. 3). Advantages include improvements in fracture biology as less periosteal stripping is required.37, 51 Further, less hardware irritation is a substantial advantage. Meloy et al.37 found equivalent union rates and alignment but fewer complications and increased elbow range of motion with lateral compared to dual column plating. A lateral paratricipital approach was used with direct anatomic reduction technique for extraarticular AO/OTA type 13A2 or 13A3 fracture patterns.
Fig. 3.
Clinical case of distal humerus fracture managed with direct reduction through lateral paratricipital exposure. Single column plating employed with a locked periarticular plate resulting in uneventful union without deformity.
Other clinical series have corroborated the clinical efficacy of single column locked lateral plating for extraarticular distal humerus fractures (Table 1). Levy et al. examined single-plate fixation using a customized 4.5 mm tibial plate to match the anatomy of the distal humerus.52 All 15 patients achieved uneventful union, with no reported complications. Cordero et al. reported on single plating using a fixed-angled pre-countoured implant and found a 97% union rate with minimal risk of iatrogenic complication such as nerve injury.53 In a series of 40 patients with distal humerus fractures treated with a triceps-sparing approach with a single precontoured posterolateral plate, Scolaro et al. found a 95% union rate and a nearly 90% patient satisfaction rate with their surgery despite 8 patients requiring reoperation.51 Fawi et al. reported a 100% union rate and 1 iatrogenic radial nerve palsy that recovered in their series of 23 patients treated with a single precountoured extra-articular locking plate.54 Capo et al. reported a 100% union rate with usage of a single locking compression plate in a series that included a large percentage of patients with gun shot wounds and other high-energy injuries.55
Table 1.
Single-column plating for Extra-Articular Distal Humerus Fractures.
| Author | Number of patients | Type of Fixation | Union Rate | Iatrogenic Radial Nerve Palsy | Malunion | Other |
|---|---|---|---|---|---|---|
| Meloy et al. 2013 | 45 | Precontoured anatomic locking | 97.8% | 0% | 0% | 1 hardware irritation, 1 hardware failure |
| Scolaro et al. 2014 | 40 | Precontoured anatomic locking | 95% | 0% | 0% | 20% reoperation |
| Capo et al. 2014 | 19 | Precontoured anatomic locking | 100% | 0% | 0% | 5.3% ulnar nerve palsy |
| Fawi et al. 2015 | 23 | Precontoured anatomic locking | 100% | 4.3% | 0% | 4.3% reoperation |
Despite this abundance of literature supporting single plating, fractures with significant comminution in the meta-diaphyseal region should be considered for a dual plating strategy. A single plate alone has not been as extensively tested as a bridging device. Certainly, supplemental plating medially will give more stability in these situations, however, to achieve the same goals and to avoid medially exposure and ulnar nerve irritation, Prasarn et al. described an alternative technique for dual plating. Here, orthogonal 90-90 plating with a posterolateral precountoured plate and a second direct lateral recon plate was utilized (Fig. 4). All patients went on to achieve union, no patient had more than 5 ° angulation, and there were no new radial nerve palsies.1
Fig. 4.
For unstable distal humerus fractures, such as this open variant with metaphyseal bone loss (a), dual column lateral plating is an alternative to exposure and instrumentation of the medial column (b).
Lastly, in addition to traditional single and dual column plating, alternative fixation methods have been shown to be viable options. Minimally invasive plate osteosynthesis (MIPO) provides the theoretical advantage of less soft tissue trauma and even less periosteal stripping. This was recently compared to traditional open reduction internal fixation in a large series of mid-distal humerus fractures, with findings of shorter union time and equivalent complication rates in the MIPO group.56, 57, 58
2. Summary
The young active patient with an extra-articular distal humerus fracture deserves thoughtful consideration for the best care paradigm for this injury. Surgery is typically the preferred option as closed management is plagued with extended immobilization with delayed rehabilitation, loss of early motion, skin irritation, and an understandable challenge in achieving patient compliance. In addition, lost time, including a delay in return to work, activity resumption, and a general period of lost productivity are difficult to quantify but certainly very real and meaningful to the young patient.
Minimizing iatrogenic radial nerve palsy is crucial when considering operative treatment. Using a triceps-sparing approach with release of the lateral intermuscular septum can minimize this risk. The argument for using a triceps-sparing approach rather than a triceps-splitting approach is further strengthened by the increased elbow range of motion as well as triceps strength that has been shown in using this muscle preserving approach.
With regards to singe versus dual-column plating, precontoured single column plating appears to afford equal union rates with decreased complication rates. However, strong caution is suggested in applying this strategy for comminuted AO type 13A3 fractures. Here dual plate fixation is advised to provide adequate stability. Lastly, newer fixation strategies such as MIPO have shown promise with their potential to minimize periosteal and soft tissue stripping, but further studies are needed to determine their safety and efficacy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Contributor Information
Mark S. Ayoub, Email: mayoub@fresno.ucsf.edu.
Ivan S. Tarkin, Email: tarkinis@upmc.edu.
References
- 1.Prasarn M.L., Ahn J., Paul O. Dual plating for fractures of the distal third of the humeral shaft. J Orthop Trauma. 2011;25(Jan (1)):57–63. doi: 10.1097/BOT.0b013e3181df96a7. [DOI] [PubMed] [Google Scholar]
- 2.Sarmiento A., Kinman P.B., Galvin E.G., Schmitt R.H., Phillips J.G. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(Jul (5)):596–601. [PubMed] [Google Scholar]
- 3.Sarmiento A., Horowitch A., Aboulafia A., Vangsness C.T., Jr. Functional bracing for comminuted extra-articular fractures of the distal third of the humerus. J Bone Joint Surg Br. 1990;72(Mar (2)):283–287. doi: 10.1302/0301-620X.72B2.2312570. [DOI] [PubMed] [Google Scholar]
- 4.Ali E., Griffiths D., Obi N., Tytherleigh-Strong G., Van Rensburg L. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg. 2015;24(Feb (2)):210–214. doi: 10.1016/j.jse.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Riera R., Maxson B., Infante A. The Post-Sarmiento Era: Is It Time to Rethink Expectations of Functional Bracing for Humeral Shaft Fractures?; Presented in Orthopaedic Trauma Association Meeting October; 2016. [Google Scholar]
- 6.Ekholm R., Tidermark J., Tornkvist H., Adami J., Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma. 2006;20:591–596. doi: 10.1097/01.bot.0000246466.01287.04. [DOI] [PubMed] [Google Scholar]
- 7.Sarmiento A., Zagorski J.B., Zych G.A., Latta L.L., Capps C.A. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(Apr (4)):478–486. doi: 10.2106/00004623-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Jawa A., McCarty P., Doornberg J., Harris M., Ring D. Distal third diaphyseal fractures of the humerus: a comparison of functional bracing and plate fixation. J Bone Joint Surg Am. 2006;88:2343–2347. doi: 10.2106/JBJS.F.00334. [DOI] [PubMed] [Google Scholar]
- 9.Pehlivan O. Functional treatment of the distal third humeral shaft fractures. Arch Orthop Trauma Surg. 2002;122:390–395. doi: 10.1007/s00402-002-0403-x. [DOI] [PubMed] [Google Scholar]
- 10.Koch P.P., Gross D.F., Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg. 2002;11(Mar–Apr (2)):143–150. doi: 10.1067/mse.2002.121634. [DOI] [PubMed] [Google Scholar]
- 11.Sarmiento A., Latta L. The evolution of functional bracing of fractures. J Bone Joint Surg Br. 2006;88:141–148. doi: 10.1302/0301-620X.88B2.16381. [DOI] [PubMed] [Google Scholar]
- 12.Woon C.Y. Cutaneous complications of functional bracing of the humerus: a case report and literature review. J Bone Joint Surg Am. 2010;92:1786–1789. doi: 10.2106/JBJS.I.01309. [DOI] [PubMed] [Google Scholar]
- 13.Ring D., Jawa A., Cannada L. Clinical faceoff are distal-third diaphyseal humerus fractures best treated nonoperatively? Clin Orthop Relat Res. 2016;474(Feb (2)):310–314. doi: 10.1007/s11999-015-4636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kakazu R., Dailey S.K., Schroeder A.J., Wyrick J.D., Archdeacon M.T. Iatrogenic radial nerve palsy after humeral shaft nonunion repair: more common than you think. J Orthop Trauma. 2016;30(May (5)):256–261. doi: 10.1097/BOT.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 15.Kumar M.N., Ravindranath V.P., Ravishankar M. Outcome of locking compression plates in humeral shaft nonunions. Indian J Orthop. 2013;47:150–155. doi: 10.4103/0019-5413.108899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abalo A., Dosseh E.D., Adabra K., Walla A., James Y.E., Dossim A. Open reduction and internal fixation of humeral non-unions: radiological and functional results. Acta Orthop Belg. 2011;77:299–303. [PubMed] [Google Scholar]
- 17.Bernard de Dompsure R., Peter R., Hoffmeyer P. Uninfected nonunion of the humeral diaphyses: review of 21 patients treated with shingling, compression plate, and autologous bone graft. Orthop Traumatol Surg Res. 2010;96:139–146. doi: 10.1016/j.rcot.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Martinez A.A., Cuenca J., Herrera A. Two-plate fixation for humeral shaft non-unions. J Orthop Surg. 2009;17:135–138. doi: 10.1177/230949900901700201. [DOI] [PubMed] [Google Scholar]
- 19.Mellema J.J., Lindenhovius A.L., Jupiter J.B. The posttraumatic stiff elbow: an update. Curr Rev Musculoskelet Med. 2016;9(Jun (2)):190–198. doi: 10.1007/s12178-016-9336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maresca A., Fantasia R., Cianforlini M., Giampaolini N., Cerbasi S., Pascarella R. Distal-third diaphyseal fractures of the humerus: choice of approach and surgical treatment. Musculoskelet Surg. 2016;100(Dec (Suppl 1)):97–104. doi: 10.1007/s12306-016-0418-z. [DOI] [PubMed] [Google Scholar]
- 21.Tingstad E.M., Wolinsky P.R., Shyr Y., Johnson K.D. Effect of immediate weight-bearing on plated fractures of the humeral shaft. J Trauma. 2000;1(2):278–280. doi: 10.1097/00005373-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Kozánek M., Bartoníček J., Chase S.M., Jupiter J.B. Treatment of distal humerus fractures in adults: a historical perspective. J Hand Surg Am. 2014;39(Dec (12)):2481–2485. doi: 10.1016/j.jhsa.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 23.McKee M., Larsson S. 7th ed. vol 1. 2010. Humeral shaft fractures; pp. 1013–1016. (Rockwood and Green’s Fractures in Adults). [Chapter 34] [Google Scholar]
- 24.Niver G.E., Ilyas A.M. Management of radial nerve palsy following fractures of the humerus. Orthop Clin North Am. 2013;44(Jul (3)):419–424. doi: 10.1016/j.ocl.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 25.Ekholm R.1, Ponzer S., Törnkvist H., Adami J., Tidermark J. The Holstein-Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. J Orthop Trauma. 2008;22(Nov–Dec (10)):693–697. doi: 10.1097/BOT.0b013e31818915bf. [DOI] [PubMed] [Google Scholar]
- 26.Voigt C., Illical E., Goyal K.S., Farrell D.J., Van Eck C.F., Tarkin I.S. Cadaveric investigation on radial nerve strain using different posterior surgical exposures for extraarticular distal humeral ORIF: merits of nerve decompression through a lateral paratricipital exposure. J Ortho Trauma. 2015;29(Feb (2)):e43–5. doi: 10.1097/BOT.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 27.Shao Y.C., Harwood P., Grotz M.R. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87:1647–1652. doi: 10.1302/0301-620X.87B12.16132. [DOI] [PubMed] [Google Scholar]
- 28.Pailhé R., Mesquida V., Rubens-Duval B., Saragaglia D. Plate osteosynthesis of humeral diaphyseal fractures associated with radial palsy: twenty cases. Int Orthop. 2015;39(Aug (8)):1653–1657. doi: 10.1007/s00264-015-2745-3. [DOI] [PubMed] [Google Scholar]
- 29.Wang X., Zhang P., Zhou Y. Secondary radial nerve palsy after internal fixation of humeral shaft fractures. Eur J Orthop Surg Traumatol. 2014;24:331–333. doi: 10.1007/s00590-013-1197-y. [DOI] [PubMed] [Google Scholar]
- 30.Zhang J., Moore A.E., Stringer M.D. Iatrogenic upper limb injuries: a systematic review. J Surg. 2011;81:227–236. doi: 10.1111/j.1445-2197.2010.05597.x. [DOI] [PubMed] [Google Scholar]
- 31.Wang J.P., Shen W.J., Chen W.M. Iatrogenic radial nerve palsy after operative management of humeral shaft fractures. J Trauma. 2009;66:800–803. doi: 10.1097/TA.0b013e31816142cf. [DOI] [PubMed] [Google Scholar]
- 32.Holstein A., Lewis G.M. Fractures of the humerus with radial-nerve paralysis. J Bone Joint Surg Am. 1963;45:1382–1388. [PubMed] [Google Scholar]
- 33.Illical E.M., Farrell D.J., Siska P.A., Evans A.R., Gruen G.S., Tarkin I.S. Comparison of outcomes after triceps split versus sparing surgery for extra-articular distal humerus fractures. Injury. 2014;45(Oct (10)):1545–1548. doi: 10.1016/j.injury.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 34.Ziran B., Smith W.R., Balk M.L., Manning C.M., Agudelo J.F. A true triceps-splitting approach for treatment of distal humerus fractures: a preliminary report. J Trauma. 2005;58:70–75. doi: 10.1097/01.ta.0000145079.76335.dd. [DOI] [PubMed] [Google Scholar]
- 35.Schildhauer T., Nork S.E., Mills W.J., Henley M.B. Extensor mechanism-sparing paratricipital posterior approach to the distal humerus. J Orthop Trauma. 2003;17:374–378. doi: 10.1097/00005131-200305000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Gerwin M., Hotchkiss R.N., Weiland A.J. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996;78(Nov (11)):1690–1695. doi: 10.2106/00004623-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Meloy G.M., Mormino M.A., Siska P.A., Tarkin I.S. A paradigm shift in the surgical reconstruction of extra-articular distal humeral fractures: single-column plating. Injury. 2013;44(Nov (11)):1620–1624. doi: 10.1016/j.injury.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Mejía Silva D., Morales de los Santos R., Ciénega Ramos M.A., González Pérez C. Functional results of two different surgical approaches in patients with distal humerus fractures type C (AO) Acta Ortop Mex. 2008;22(Jan–Feb (1)):26–30. [PubMed] [Google Scholar]
- 39.McKee M., Wilson T.L., Winston L., Schemitsch E.H., Richards R.R. Functional outcome following surgical treatment of intra-articular distal humerus fractures through a posterior approach. J Bone Joint Surg Am. 2000;82:1701–1707. doi: 10.2106/00004623-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 40.McKee M., Kim J., Kebaish K., Stephen D.J.F., Kreder H.J., Schemitsch E.H. Functional outcome after open supracondylar fractures of the humerus: the effect of the surgical approach. J Bone Joint Surg Br. 2000 Jul;82(5):646–651. doi: 10.1302/0301-620x.82b5.10423. [DOI] [PubMed] [Google Scholar]
- 41.Tejwani N.C., Murthy A., Park J., McLaurin T.I.M., Egol K.A., Kummer F.J. Fixation of extra-articular distal humerus fractures using one locking pate versus two reconstruction plates: a laboratory study. J Trauma. 2009;66(3):795–799. doi: 10.1097/TA.0b013e318181e53c. [DOI] [PubMed] [Google Scholar]
- 42.Taylor P.A., Owen J.R., Benfield C.P., Wayne J.S., Boardman N.D., 3rd Parallel plating of simulated distal humerus fractures demonstrates increased stiffness relative to orthogonal plating with a distal humerus locking plate system. J Orthop Trauma. 2016 Apr;30(4):e118–e122. doi: 10.1097/BOT.0000000000000477. [DOI] [PubMed] [Google Scholar]
- 43.Sabalic S., Kodvanj J., Pavic A. Comparative study of three models of extra-articular distal humerus fracture osteosynthesis using the finite element method on an osteoporotic computational model. Injury. 2013;44(Sep (Suppl 3)):S56–S61. doi: 10.1016/S0020-1383(13)70200-6. [DOI] [PubMed] [Google Scholar]
- 44.Caravaggi P., Laratta J.L., Yoon R.S. Internal fixation of the distal humerus: a comprehensive biomechanical study evaluating current fixation techniques. J Orthop Trauma. 2014;28(Apr (4)):222–226. doi: 10.1097/BOT.0b013e3182a6693f. [DOI] [PubMed] [Google Scholar]
- 45.Chen R.C., Harris D.J., Leduc S., Borrelli J.J., Jr, Tornetta P., III, Ricci W.M. Is ulnar nerve transposition beneficial during open reduction and internal fixation of distal humerus fractures? J Orthop Trauma. 2010;24(7):391–394. doi: 10.1097/BOT.0b013e3181c99246. [DOI] [PubMed] [Google Scholar]
- 46.Worden A., Ilyas A.M. Ulnar neuropathy following distal humerus fracture fixation. Orthop Clin North Am. 2012 Oct;43(4):509–514. doi: 10.1016/j.ocl.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 47.Vazquez O., Rutgers M., Ring D.C., Walsh M., Egol K.A. Fate of the ulnar nerve after operative fixation of distal humerus fractures. J Orthop Trauma. 2010;24(7):395–399. doi: 10.1097/BOT.0b013e3181e3e273. [DOI] [PubMed] [Google Scholar]
- 48.Wang K.C., Shih H.N., Hsu K.Y., Shih C.H. Intercondylar fractures of the distal humerus: routine anterior subcutaneous transposition of the ulnar nerve in a posterior operative approach. J Trauma. 1994;36:770–773. [PubMed] [Google Scholar]
- 49.McKee M.D., Jupiter J.B., Bosse G., Goodman L. Outcome of ulnar neurolysis during posttraumatic reconstruction of the elbow. J Bone Joint Surg Br. 1998;80:100–105. doi: 10.1302/0301-620x.80b1.7822. [DOI] [PubMed] [Google Scholar]
- 50.Ruan H.J., Liu J.J., Fan C.Y., Jiang J., Zeng B.F. Incidence, management, and prognosis of early ulnar nerve dysfunction in type C fractures of distal humerus. J Trauma. 2009;67 doi: 10.1097/TA.0b013e3181968176. 1397–40. [DOI] [PubMed] [Google Scholar]
- 51.Scolaro J.A., Voleti P., Makani A., Namdari S., Mirza A., Mehta S. Surgical fixation of extra-articular distal humerus fractures with a posterolateral plate through a triceps-reflecting technique. J Shoulder Elbow Surg. 2014;23(Feb (2)):251–257. doi: 10.1016/j.jse.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 52.Levy J.C., Kalandiak S.P., Hutson J.J., Zych G. An alternative method of osteosynthesis for distal humeral shaft fractures. J Orthop Trauma. 2005;18:43–47. doi: 10.1097/00005131-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 53.Cordero G.X., Daccarett M.S., Fehringer E.V. Presented at Orthopedic Trauma Association. 2011. Operative treatment of extra-articular distal humerus fractures utilizing single-column plating. [Google Scholar]
- 54.Fawi H., Lewis J., Rao P., Parfitt D., Mohanty K., Ghandour A. Distal third humeri fractures treated using the Synthes™ 3. 5-mm extra-articular distal humeral locking compression plate: clinical, radiographic and patient outcome scores. Shoulder Elbow. 2015;7(Apr (2)):104–109. doi: 10.1177/1758573214559320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Capo J.T., Debkowska M.P., Liporace F., Beutel B.G., Melamed E. Outcomes of distal humerus diaphyseal injuries fixed with a single-column anatomic plate. Int Orthop. 2014;38(May (5)):1037. doi: 10.1007/s00264-013-2213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Esmailiejah A.A., Abbasian M.R., Safdari F., Ashoori K. Treatment of humeral shaft fractures: minimally invasive plate osteosynthesis versus open reduction and internal fixation. Trauma Mon. 2015;20(Aug (3)):e26271. doi: 10.5812/traumamon.26271v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gallucci G., Boretto J., Vujovich A., Alfie V., Donndorff A., De Carli P. Posterior minimally invasive plate osteosynthesis for humeral shaft fractures. Tech Hand Up Extrem Surg. 2014;18(Mar (1)):25–30. doi: 10.1097/BTH.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 58.Xue Z., Jiang C., Hu C., Qin H., Ding H., An Z. Effects of different surgical techniques on mid-distal humeral shaft vascularity: open reduction and internal fixation versus minimally invasive plate osteosynthesis. BMC Musculoskelet Disord. 2016;26(Aug (17)):370. doi: 10.1186/s12891-016-1224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]