Abstract
Objective
To report on our initial experience in the management of war-related penile injuries; proper diagnosis and immediate treatment of penile injuries is essential to gain satisfactory results. Besides treating primary wounds and restoring penile function, the cosmetic result is also an important issue for the surgeon.
Patients and methods
The study was conducted in the Department of Urology at Benghazi Medical Center and comprised all patients who presented with a shotgun, gunshot or explosive penile injury between February 2011 and August 2017. The patient’s age, cause of injury, site and severity of injuries, management, postoperative complications, and hospital stay, were recorded.
Results
In all, 29 males with war-related penile injuries were enrolled in the study. The mean (SD) age of these patients was 31.3 (10.5) years. The glans, urethra, and corporal bodies were involved in four (13.7%), 10 (34.4%), and 20 (68.9%) of the patients, respectively. According to the American Association for the Surgery of Trauma Penis Injury Scale, Grade III penile injuries were the most common (11 patients, 37.9%). The most common post-intervention complications were urethral stricture with or without proximal urethrocutaneous fistula (eight patients, 27.5%), followed by permanent erectile dysfunction (five patients, 17.2%).
Conclusion
In patients who sustain war-related penile injuries the surgeon’s efforts should not only be directed to restoring normal voiding and erectile function but also on the cosmetic appearance of the penis.
Abbreviations: AAST, American Association for the Surgery of Trauma; IED, improvised explosive device
Keywords: Gunshot, Penis, Corporal bodies, Urethral injury, War-related penile injuries
Introduction
The global rise in terrorism, which is linked to easy access to the firearms and improvised explosive devices (IEDs), has led to an increase in the incidence of the external genital injuries, particularly in rebel areas [1], [2]. However, injuries caused by gunshots to the external genitalia are relatively rare compared with injuries to the other parts of the body because anatomical shielding provides protection against these injuries [3]. As IEDs and landmines are planted at ground level, the destructive impact of these explosive devices is mainly on the lower limbs, pelvis, and external genitalia [1]. To date, there is no single appropriate therapeutic strategy or surgical technique suitable to treat all types of penile injuries [4]. Thus, the type, severity, and location of penile injuries should be considered in the choice of surgical approach and surgical technique(s) [5]. Although penile injuries are usually not life-threatening, they can have a significant impact on the victims’ quality of life [6]. Despite good management and regular follow-up of external genital gunshot wounds, such wounds are fraught with the possibility of complications such as erectile dysfunction, urethral stricture, and infertility [7]. Therefore, the main therapeutic goals of penile injuries are to maintain or restore potency, fertility and natural urination strength, as well as to maintain the aesthetic shape of the penis [1], [2].
The aim of our present study was to report our initial experience in the management of war-related penile injuries; emphasising that we have limited experience in these types of injuries, as there was no single case of shotgun, gunshot or explosive penile injury recorded before 2011; the date of war in Libya.
Patients and methods
The study was conducted in the Department of Urology at Benghazi Medical Center. This descriptive case series was carried out in a proactive manner by immediate registration of all operated cases sustaining shotgun, gunshot or explosive injuries to the penis from February 2011 to August 2017. The patient’s demographic data, cause of injury, site and severity of primary penile injuries, surgical management as well as the surgical outcome, postoperative complications, and hospital stay, were recorded. These data were collected prospectively and analysed retrospectively. Patients who arrived dead or died during surgery were not enrolled in the study. Penile injuries were classified according to the cause of the penile injury, whether gun/shotgun bullets or shrapnel of explosive devises/projectiles. The causes of penile injuries due to gunshots were sub-classified according to the velocity of bullets into: low-velocity gunshot injuries (<350 m/s), medium-velocity gunshot injuries (350–500 m/s), and high-velocity gunshot injuries (>600 m/s) [8]. Penile injuries due to explosions were classified as: IEDs, personal landmine or explosion of a projectile. The proper assessment of penile injuries depends on clinical findings and imaging studies results, as well as on operative findings. Imaging studies, e.g. plain X-ray, are required to identify foreign bodies and/or bone fractures; however, a retrograde urethrogram can only be done in cases of superficial penile injuries, in which urethral injuries are not obvious. CT is usually performed to assess patients who sustain multiple serious injuries. The management of penile injuries depends on the severity of the injury, physical findings and haemodynamic stability of the patient; however, patients in shock underwent immediate laparotomy without any diagnostic imaging studies to treat life-threatening injuries. The grades of the penile injuries were classified according to American Association for the Surgery of Trauma (AAST) Penis Injury Scale [9] (Table 1).
Table 1.
AAST Penis Injury Scale.
| AAST Grade | Description of injury |
|---|---|
| I | Cutaneous laceration/contusion |
| II | Buck’s fascia (cavernous) laceration without tissue loss |
| III | Cutaneous avulsion |
| Laceration through glans/meatus | |
| Cavernosal or urethral defect <2 cm | |
| IV | Partial penectomy |
| V | Cavernosal or urethral defect >2 cm |
| Total penectomy |
All patients with penile injury underwent initial surgical repair by the same team and because the wounds were contaminated these patients received parenteral prophylactic and postoperative courses of antibiotics. All patients with Grade IV–V penile injuries required suprapubic urinary diversion, whereas, only six cases with Grade III penile injuries required a suprapubic cystostomy. Patients who presented with Grade I–II penile injuries were usually discharged immediately or within a few days, unless they were associated with other serious injuries that necessitated a longer hospital stay. Isolated Grade III penile injuries necessitated a hospital stay from 2 to 3 weeks. Severely injured patients were kept in hospital and then transferred to specialist centres abroad 2–3 months after preliminary repair of their penile injuries for further management of the penile and/or concomitant serious injuries. Permission for the study was granted by the Hospital Ethics and Research Committee. The statistical descriptive analysis was carried out using the Statistical Package for the Social Sciences (SPSS® Statistics for Windows, Version 22: IBM Corp., Armonk, NY, USA).
Results
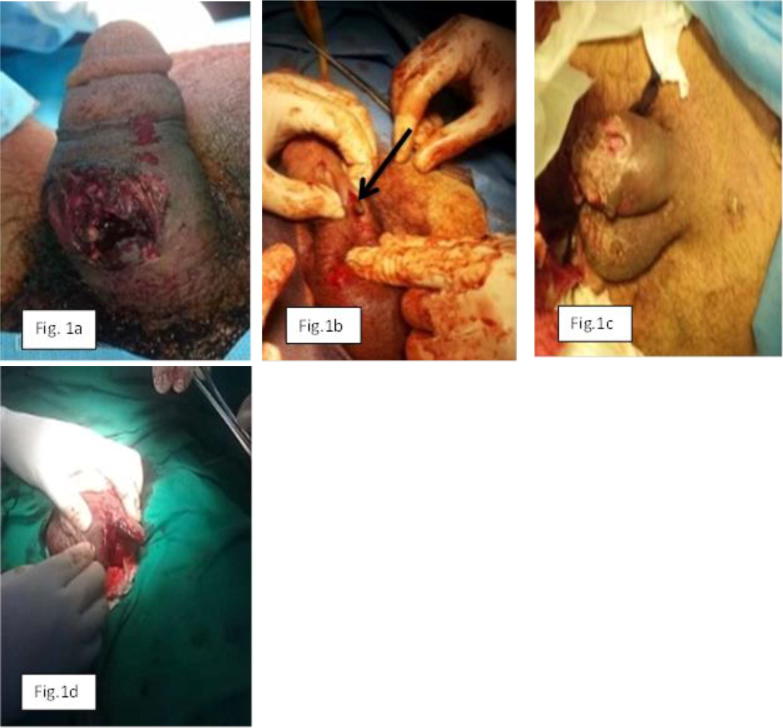
In all, 29 patients with war-related penile injuries were enrolled in the present study. The mean (SD, range) age of the patients was 31.3 (10.5, 16–62) years; with most injuries in the 21–40 years age-group. The causes of penile injuries were gunshots (18 patients, 62%), explosions (nine, 31%), and shotguns (two, 6.9%) (Fig. 1).
Fig. 1.
Grades of penile injuries. (a) Grade III shotgun injury to the penis; (b) Grade III medium-velocity gunshot injury to the penis (arrow); (c) Grade IV explosive injury to the penis; (d) Grade V high-velocity gunshot injury to the penis.
According to the AAST Penis Injury Scale, Grade III penile injuries were the most common (11 patients, 7.9%), followed by Grade II penile injuries (eight, 27.6%) (Table 2).
Table 2.
Penile injury grade and cause of injury.
| Cause of injury | Grade of penile injury, n (%) |
Total, n (%) | ||||
|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||
| Shotgun | 1 | – | 1 | – | – | 2 (6.9) |
| Low-velocity gunshot | 1 | – | 1 | – | – | 2 (6.9) |
| Medium-velocity gunshot | – | 2 | 4 | – | – | 6 (20.7) |
| High-velocity gunshot | – | 3 | 4 | 1 | 2 | 10 (34.5) |
| IED or personal landmine | 1 | 3 | 1 | 1 | 1 | 7 (24.1) |
| Explosion of a projectile | 1 | – | – | – | 1 | 2 (6.7) |
| Total | 4 (13.8) | 8 (27.6) | 11 (37.9) | 2 (6.9) | 4 (13.8) | 29 (100) |
The war-related penile traumas resulted in glanular laceration (four patients, 13.7%), corporal bodies injury (20, 68.9%), and urethral injury (10, 34.5%). In all, 17 (58.6%) patients had associated scrotal (14 patients), testicular (nine testicles in eight patients), abdominal (nine), chest (four), skeletal (four), head (three), and vascular (one) injuries. The associated skeletal injuries were amputation of both lower extremities (one), amputation of one leg (two), and fractured femur (one) (Fig. 2a and b).
Fig. 2.
(a) Shows a Grade I explosive injury to the penis associated with amputation of a right leg. (b) Shows a surgical repair of bilateral concomitant testicular injuries in a patient who sustained a Grade I gunshot injury to the penis.
Grade I penile injuries were treated by simple suturing or just dressing of the injured skin (four patients), whereas Grade II injuries were treated by debridement and haemostatic suturing of Buck’s fascia and skin (eight). The treatment of Grade III penile injuries comprised debridement and haemostatic suturing of the tunica albuginea and Buck’s fascia (one), debridement and haemostatic suturing of lacerated glans (four) or debridement and reconstruction of injured corporal bodies and/or injured urethra in addition to the suprapubic cystostomy (six). Patients with Grade IV penile injuries underwent partial penectomy with skin grafting due to extensive skin loss (two patients), whilst the patients who sustained Grade V penile injuries underwent primary and meticulous reconstruction of the corporal bodies with realignment of fragile urethra over a 18-F silicone catheter with suprapubic urinary diversion (four) (Fig. 3).
Fig. 3.
(a) and (b) shows a Grade V high-velocity gunshot injury to the penis that underwent immediate repair.
No obvious post-intervention complications developed in 18 of the 29 patients (62%) who sustained penile trauma, of these four had Grade I injuries, eight had Grade II, and six had Grade III penile injuries. However, the other eleven (37.9%) patients developed various complications related to their injuries, of these five had Grade III, two had Grade IV, and four had Grade V penile injuries (Table 3).
Table 3.
Complications after treatment of penile injury.
| Complication | Grade of penile injury, n |
Total, n (%) | ||||
|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||
| No residual complications | 4 | 8 | 6 | – | – | 18 (62) |
| Mild curvature of penis | – | – | 2 | – | – | 2 (6.8) |
| Severe curvature of penis | – | – | 1 | – | – | 1 (3.4) |
| Temporary erectile dysfunction | – | – | – | 1 | – | 1 (3.4) |
| Permanent erectile dysfunction | – | – | 1 | – | 4 | 5 (17.2) |
| Urethral stricture | – | – | 4 | – | 2 | 6 (20.6) |
| Urethral stricture with proximal urethrocutaneous fistula | – | – | – | – | 2 | 2 (6.8) |
In all, 16 (55.1%) patients with Grade I–III penile injuries (three, Grade I; seven, Grade II; and six, Grade III) were followed-up for 2–3 months and developed no obvious post-intervention penile injury-related complications. One case of isolated Grade III penile injury developed a urethral stricture after the preliminary repaired urethrocutaneous fistula, which required urethroplasty using a buccal mucosal graft through a perineal approach. Because the number of casualties exceeded the capacity of the only two active hospitals in our city during the period of the war; the other 12 cases of penile injuries (one, Grade I; one, Grade II; four. Grade III; two, Grade IV; and four, Grade V) were sent to advanced centres abroad at the expense of the government for further management of their severe penile and/or concomitant injuries. Stressing that all these patients were kept in the hospital for 1–3 months and the preliminary results of their penile reconstructive operations in terms of restoring the shape and contour of the penis were satisfactory.
Discussion
Male reproductive organs are protected by several defence mechanisms, such as size and mobility of these organs, as well as their anatomical location that provides shielding against penetration and blunt trauma [2], [10]. Gunshot injuries to the external genital organs; whether in the military battlefield or during peace time are relatively uncommon as compared with injuries to other parts of the body; however, most of the victims are young adults [7]. In the present study, the mean (SD, range) patient age was 31.3 (10.5, 16–62) years, with most of the penile injuries recorded in the 21–40 years age-group, representing 62% of the present recorded cases. Al-Azzawi et al. [11] reported that the mean (range) age of patients who sustained urethral and penile injuries during civil violence in Iraq was 29 (14–55) years, with most of the victims in the 20–39 years age-group, representing 78% of all their cases. Whereas, Dogo et al. [3] reported that the mean (range) age of victims of missile injuries to the external genitalia in Maiduguri-North Eastern Nigeria was 32.75 (5–70) years, with most of the victims aged 30–39 years. Indeed, other authors have reported that most victims are young adults, with a mean age of 30 years [12], [13] with predominance in those aged 18–28 years [14]. In Sana’a-Yemen and in Maiduguri-North Eastern Nigeria, patients aged <30 years represented 45% [15] and 38.6% [3] of all registered cases with war injuries to the external genitalia, respectively; whilst in the present study, 55.1% of penile injuries were recorded in this age group. The high rate of genital injuries in this age group reflects the problem of disability and productivity losses in afflicted countries. Injuries to the penis and urethra in the Iraq conflict were mainly caused by IEDs (56%) and pistols (44%) [11], whereas in our present study, penile injuries caused by explosions and firearms represented 34.4% and 68.9% of cases, respectively. This discrepancy may be explained by the fact that most of the victims of explosive injuries arrived dead or died during surgery, consequently they were not enrolled in our present study. The incidence of urethral injuries has been reported to range from 17% to 33% of patients that sustain penile gunshot traumas [16], whilst the incidence of associated urethral injuries recorded in our present series represented 34.4% of all penile injuries. In the present study, the corporeal bodies were involved in 68.9% of penile injuries, which correspond with the results of other studies reporting that the corporeal bodies were involved in 62% [10] and 81% [15] of penile wounds. However, we recorded combined corporal bodies and urethral injuries in nine (31%) patients, isolated injuries to the corporal bodies in 11 (37.9%), and isolated injury to the urethra in one (3.4%). Previous studies have reported that 70–93% of reproductive and urinary tract injuries are associated with abdominal, chest, and lower limb injuries [17], [18]; injury to major vessels is usually the leading cause of death in these casualties [11]. In the present study, 51.7% of the penile injuries were associated with abdominal, chest, lower limb and vascular injuries. In the present study, of nine associated testicular injuries (in eight patients), five testes were saved and in two previous studies the injured testes were saved in 44.5% [15], and 74.4% [6] of all cases who sustained genital injuries. Tissue damage in cases of gunshot injuries depends on the mass and the velocity of the bullets [19]. In the present study, seven patients had Grade I and II penile injuries that were caused by different weapons with different bullet sizes and velocities; the similarities of these injuries can be only explained by the differences in shooting distances. For the management of penile gunshot injuries, it is important to assess the amount of damage with respect to the shooting distance and bullet calibre, as well as the type of weapon [20]. Superficial or trivial penile lesions are managed non-operatively in 4.8–10% of cases who sustain war-related penile injuries [16], [21]. We treated four (13.7%) patients with Grade I penile injuries non-operatively and all of these cases developed no penile-injury related complications. Early surgical exploration, debridement of devitalised tissue, preservation of viable tissue, urinary diversion, removal of foreign bodies, securing haemostasis, and repair of injured tissue, are the principles for successful treatment of serious genital injuries [18], [22]. However, the treatment of genital and urinary tract injuries can be safely postponed for appropriate management of any life-threatening concomitant injuries [1]. Although the surgical approach to penile injuries depends on the site of injury; a lateral approach or sub-coronal degloving can provide good exposure for most penile injuries [22]. In the present study, the inlet of explosive IEDs and shrapnel at the lateral aspect of the scrotal neck provided good exposure to the injury in two cases of Grade V penile injury. Depending on the degree of penile and urethral damage, there are varieties of surgical management; including simple repair, closing the remaining penile stump of a partially amputated penis, and surgical re-anastomosis or total replacement with phallic reconstruction [23], [24]. We performed all types of reconstructive phallic surgeries including re-anastomosis of nearly amputated penis with intact neurovascular bundles in four cases of Grade V injuries to the penis. For surgical repair, adequate exploration and meticulous reconstruction of the corporal bodies is essential to prevent the development of complications, such as erectile dysfunction and penile curvature [16]. In the cases of urethral lesions, a primary surgical repair is the option of choice [25], whilst in the cases of extensive urethral defects, the treatment strategy of surgical repair in two stages should be considered [26], [27]. In our present series, those with a severely injured penis and fragile urethra underwent reconstructive surgery of the corporal bodies with the realignment of the injured urethra over silicone catheters, in order to perform urethroplasty at a later date. In severe penile injuries with extensive skin loss; a full-thickness skin grafting may be needed to complete the entire penile reconstruction process [28], [29]. A satisfactory cosmetic outcome with a normal penile erection was achieved in 50% of the patients, and mild penile curvature was recorded in 31% of the patients. Severe angulation and erectile dysfunction were recorded in 19% of cases with extensive corporal injuries [15]. In the present study, six (20.6%) patients developed either physiological erectile dysfunction responding to medical treatment (one patient, 3.4%) or permanent erectile dysfunction (five, 17.2%), and four (13.7%) developed either severe (one) or mild (three) penile curvature. However, 19 (65.5%) patients did not develop erectile dysfunction. In these types of debilitating injuries in addition to urologists, it is important to involve plastic surgeons, psychiatrists, and psychotherapists to complete the treatment of these patients [23].
Conclusion
The severity of gunshot injuries depends on the size and velocity of the bullet, as well as the distance between the trigger and target. Despite the immediate, comprehensive and primary meticulous repair of severe destructive penile and urethral war-related injuries, a normal erection and/or voiding function cannot be guaranteed. Severe shotgun, gunshot or explosive injuries to the penis are usually associated with a physical and emotional impact on the patient due to their postoperative complications; therefore the surgeons’ efforts should be focused on restoring the aesthetic shape of the penis, erectile function, and normal urethral urination. The present number of cases represents only the ‘tip of the iceberg’, and does not reflect the magnitude of the disaster in the whole of Libya.
Conflict of interest
The authors declare that they have no conflict of interest.
Source of Funding
The authors declare that this study received no financial support.
Trauma
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Phonsombat S., Master V.A., McAninch J.W. Penetrating external genital trauma: a 30-year single institution experience. J Urol. 2008;180:192–196. doi: 10.1016/j.juro.2008.03.041. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed A., Mbibu N.H. Aetiology and management of injuries to male external genitalia in Nigeria. Injury. 2008;39:128–133. doi: 10.1016/j.injury.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 3.Dogo H.M., Ibrahim A.G., Gana Y.L. Missile injuries to the external genitalia: a five-year experience in Maiduguri, North Eastern Nigeria. Int J Res Med Sci. 2016;4:2964–2966. [Google Scholar]
- 4.Morey A.F., Metro M.J., Carney K.J., Miller K.S., McAninch J.W. Consensus on genitourinary trauma: external genitalia. BJU Int. 2004;94:507–515. doi: 10.1111/j.1464-410X.2004.04993.x. [DOI] [PubMed] [Google Scholar]
- 5.Perovic S.V., Djinovic R.P., Bumbasirevic M.Z., Santucci R.A., Djordjevic M.L., Kourbatov D. Severe penile injuries: a problem of severity and reconstruction. BJU Int. 2009;104:676–687. doi: 10.1111/j.1464-410X.2008.08343.x. [DOI] [PubMed] [Google Scholar]
- 6.Waxman S., Beekley A., Morey A., Soderdahl D. Penetrating trauma to the external genitalia in Operation Iraqi Freedom. Int J Impot Res. 2009;21:145–148. doi: 10.1038/ijir.2008.59. [DOI] [PubMed] [Google Scholar]
- 7.Mahamat A.M., Sougui S., Ouchemi C., Ngaringuem O., Jalloh M., Niang L. Severe external genitalia lesion by firearm: a case report. Open J Urol. 2015;5:188–191. [Google Scholar]
- 8.Munsterman A.S., Hanson R.R. Trauma and wound management: gunshot wounds in horses. Vet Clin North Am Equine Pract. 2014;30:453–466. doi: 10.1016/j.cveq.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Moore E.E., Malangoni M.A., Cogbill T.H., Peterson N.E., Champion H.R., Shackford S.R. Organ injury scaling VII: cervical vascular, peripheral vascular, adrenal, penis, testis and scrotum. J Trauma. 1996;41:523–524. doi: 10.1097/00005373-199609000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Kunkle D.A., Lebed B.D., Mydlo J.H., Pontari M.A. Evaluation and management of gunshot wounds of the penis: 20-year experience at an urban trauma center. J Trauma. 2008;64:1038–1042. doi: 10.1097/TA.0b013e3180342036. [DOI] [PubMed] [Google Scholar]
- 11.Al-Azzawi I.S., Koraitim M.M. Urethral and penile war injuries: the experience from civil violence in Iraq. Arab J Urol. 2014;12:149–154. doi: 10.1016/j.aju.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hodonou R.K., Diallo A., Akpo E.C., Koura A., Hounassou P.P., Goudote E. [Injuries of the external male genital organs. Apropos of 20 cases] [Article in French] Ann Urol (Paris) 1997;31:318–321. [PubMed] [Google Scholar]
- 13.Cerwinka W.H., Block N.L. Civilian gunshot injuries of the penis: the Miami experience. Urology. 2009;73:877–880. doi: 10.1016/j.urology.2008.10.057. [DOI] [PubMed] [Google Scholar]
- 14.Bagga H.S., Tassian G.E., Fisher P.B., McCulloch C.E., McAninch J.W., Brever B.N. Product related adult genitourinary injuries treated at emergency department in the United States from 2002 to 2010. J Urol. 2013;189:1362–1368. doi: 10.1016/j.juro.2012.10.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghilan A.M., Ghafour M.A., Al-Asbahi W.A., Al-Khanbashi O.M., Alwan M.A., Al-Ba'dani T.H. Gunshot wound injuries to the male external genitalia. Saudi Med J. 2010;31:1005–1010. [PubMed] [Google Scholar]
- 16.Cavalcanti A.G., Krambeck R., Araujo A., Manes C.H., Favorito L.A. The penile lesion from the gunshot wound: a 43-case experience. Int Braz J Urol. 2006;32:56–63. doi: 10.1590/s1677-55382006000100009. [DOI] [PubMed] [Google Scholar]
- 17.Tucak A., Lukacević T., Kuvezdić H., Petek Z., Novak R. Urogenital wounds during the war in Croatia in 1991/1992. J Urol. 1995;153:121–122. doi: 10.1097/00005392-199501000-00043. [DOI] [PubMed] [Google Scholar]
- 18.Ochsner T.G., Busch F.M., Clarke B.G. Urogenital wounds in Vietnam. J Urol. 1969;101:224–225. doi: 10.1016/s0022-5347(17)62318-8. [DOI] [PubMed] [Google Scholar]
- 19.Tiguert R., Harb J.F., Hurley P.M., Gomes De Oliveira J., Castillo Frontera R.J., Triest J.A. Management of shotgun injuries to the pelvis and lower genitourinary system. Urology. 2000;55:193–197. doi: 10.1016/s0090-4295(99)00384-2. [DOI] [PubMed] [Google Scholar]
- 20.Brandes S.B., Buckman R.F., Chelsky M.J., Hanno P.M. External genital gunshot wounds: a ten-year experience, with fifty-six cases. J Trauma. 1995;39:266–271. doi: 10.1097/00005373-199508000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Öztürk M.İ., Ilktaç A., Koca O., Kalkan S., Kaya C., Karaman M.İ. Gunshot injury to the penis in a patient with the penile prosthesis: a case report Case Report. Ulus Travma Acil Cerrahi Derg. 2011;17:464–466. [PubMed] [Google Scholar]
- 22.Summerton DJ, Djakovic N, Kitrey ND, Kuehhas FE, Lumen N, Serafetinidis E, et al. Guidelines on Urological Trauma, EAU guidelines 2014. Available at: https://uroweb.org/wp-content/uploads/24-Urological-Trauma_LR.pdf. Accessed February 2018.
- 23.García-Perdomo H.A. Importance of defining the best treatment of a genital gunshot wound: a case report. World J Clin Cases. 2014;2:587–590. doi: 10.12998/wjcc.v2.i10.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charlesworth P., Campbell A., Kamaledeen S., Joshi A. Surgical repair of traumatic amputation of the glans. Urology. 2011;77:1472–1473. doi: 10.1016/j.urology.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 25.Husmann D.A., Boone T.B., Wilson W.T. Management of low-velocity gunshot wounds to the anterior urethra: the role of primary repair versus urinary diversion alone. J Urol. 1993;150:70–72. doi: 10.1016/s0022-5347(17)35399-5. [DOI] [PubMed] [Google Scholar]
- 26.Chapple C., Barbagli G., Jordan G., Mundy A.R., Rodrigues-Netto N., Pansadoro V. Consensus statement on urethral trauma. BJU Int. 2004;93:1195–1202. doi: 10.1111/j.1464-410x.2004.04805.x. [DOI] [PubMed] [Google Scholar]
- 27.Chang A.J., Brandes S.B. Advances in diagnosis and management of genital injuries. Urol Clin North Am. 2013;40:427–438. doi: 10.1016/j.ucl.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 28.McAninch J.W., Kahn R.I., Jeffrey R.B., Laing F.C., Krieger M.J. Major traumatic and septic genital injuries. J Trauma. 1984;24:291–298. doi: 10.1097/00005373-198404000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Summerton D.J., Campbell A., Minhas S., Ralph D.J. Reconstructive surgery in penile trauma and cancer. Nat Clin Pract Urol. 2005;2:391–397. doi: 10.1038/ncpuro0261. [DOI] [PubMed] [Google Scholar]