Abstract
Chronic inflammation is a well-recognized tumor-enabling capability, which allows nascent tumors to escape immunosurveillance. A number of soluble and cellular inflammatory mediators take part in the various phases of cancer initiation and progression, giving rise to a fatal conspiracy, which is difficult to efficiently overcome. Tumor-associated macrophages (TAMs) are pivotal players of the tumor microenvironment and, because of their characteristic plasticity, can acquire a number of distinct phenotypes and contribute in different ways to the various phases of cancerogenesis. Tumor-associated neutrophils (TANs) are also emerging as important components of the tumor microenvironment, given their unexpected heterogeneity and plasticity. TAMs and TANs are both integrated in cancer-related inflammation and an ever better understanding of their functions can be useful to tailor the use of anticancer therapeutic approaches and patient follow-up.
Following the revision of the paradigm proposed by Hanahan and Weinberg (2000), it is now well recognized that chronic inflammation represents an enabling characteristic of cancer. Indeed, even if the presence of an immune infiltrate in and around the tumors was already known for a long time (Dvorak 1986), it was largely attributed to an effort of the immune system to combat tumors. In contrast, experimental evidence proved that cancer-related inflammation (CRI) had the unexpected effect of promoting tumorigenesis and progression, favoring nascent neoplasias to acquire all the hallmark capabilities of cancer, including the evasion from immunosurveillance. This revision has drastically changed the theoretical and therapeutic approach to cancer, expanding the focus from the tumor cell to the tumor microenvironment (TME).
Tumor-associated macrophages (TAMs) are a key component of the TME and are important mediators of the link between inflammation and cancer. These cells are present in different amounts and phenotypes in almost all tumor types and usually represent the main conductors of CRI. Indeed, they are characterized by plasticity, allowing them to acquire distinct phenotypes in response to different signals from the microenvironment.
In addition to macrophages, there is now evidence that neutrophils also can play several roles in the various phases of cancer development (Galdiero et al. 2013a). Indeed, contrary to what it has always been thought, they represent an unexpectedly heterogeneous population, with a spectrum of roles in CRI (Granot and Jablonska 2015).
In this review, we will recapitulate the main biological aspects of TAMs and tumor-associated neutrophils (TANs) and their roles in cancer initiation and progression. We will evaluate their role(s) as prognostic and predictive biomarkers in human cancers and we will explore the functions of these tumor-infiltrating immune cells as means or targets of old and new anticancer therapeutic approaches.
INFLAMMATION AND CANCER: A FATAL CONSPIRACY
Inflammation is an ancestral physiological response, working as a defense mechanism to combat pathogens, contain damage, and promote tissue repair. In acute inflammation, this reaction is self-limiting and sufficient to reestablish homeostasis. The resolution of inflammation is an active process, which includes cellular determinants and molecules that are locally active mediators, namely resolvins and protectins (Serhan 2010). When the inflammatory response is turned off, tissue remodeling is optimized to restore the local physiological conditions. In some circumstances, this mechanism is deranged and gives rise to chronic inflammation. This is the case of a nascent tumor, which prevents the resolution process, given the production of inflammatory molecules and recruitment of inflammatory cells, which persistently subverts the local tissue homeostasis (Dvorak 1986).
Chronic inflammation is now a well-recognized tumor-enabling capability, which can promote cancer development (Balkwill and Mantovani 2001; Hanahan and Weinberg 2011). About 20% of cancers are induced by chronic inflammation. Soluble and cellular inflammatory mediators are responsible for tumor initiation and progression (e.g., stomach, colon, skin, liver, breast, lung, and head/neck) (Al Murri et al. 2006; Bornstein et al. 2009; Barash et al. 2010; Grivennikov et al. 2010; Watanabe et al. 2012; Liang et al. 2013; Alam et al. 2016; Lund et al. 2016).
Tumor-related inflammatory responses vary depending on the context but, in general, tend to promote tumor progression (Mantovani et al. 2008; Galdiero et al. 2013b; Varricchi et al. 2017). Tumors can induce inflammatory reactions through several mechanisms. First, tumor and stromal cells release chemotactic factors that recruit macrophages and neutrophils (Bonavita et al. 2015). Moreover, the tumor can physically damage the normal tissue and release damage-associated molecular patterns, which activate granulocytes. These recruited cells release inflammatory molecules, amplifying the response. In addition, acidification of the TME has been associated with certain key features of cancer aggressiveness, including invasion, evasion from the immune system, increased angiogenesis, and resistance to therapy (Granja et al. 2017). Indeed, uncontrolled growth requires adaptations in energy metabolism to fuel cell proliferation. Thus, cancer growth leads to the production of high amounts of lactic acid, which is responsible for the acidification of the microenvironment. In contrast to normal mammalian cells, cancer cells present increased glycolysis independently of the oxygen levels (“aerobic glycolysis” or “Warburg effect”). As a consequence, high amounts of protons are generated and, to cope with this, cancer cells export protons to the microenvironment, allowing them to survive in the hostile environment that they have created (Granja et al. 2017). In addition, growing tumors increase oxygen consumption as a result of their increased metabolism (Stylianopoulos et al. 2012). The resulting hypoxia induces the production of cytokines and angiogenic growth factors, which give rise to neo-angiogenesis and lymphangiogenesis and recruit macrophages. These inflammatory processes persist as long as the tumor grows, thus giving rise to a fatal conspiracy increasingly difficult to overcome.
ROLES OF TAMs IN TUMOR GROWTH AND PROGRESSION
Macrophages are the most represented leukocytes in the TME (Mantovani et al. 2002). Classically viewed as terminally differentiated cells, they were thought to derive from circulating monocytes and to differentiate at sites of inflammation under the influence of growth factors, such as macrophage colony-stimulating factor (M-CSF) or granulocyte macrophage colony-stimulating factor (GM-CSF) (Allavena et al. 2008). However, several investigations have described, at least in mice, a self-renewing population of macrophages, derived from embryonic precursors that spread to tissues before birth and can locally proliferate and differentiate independently on bone marrow–derived monocytes (Davies et al. 2011; Jenkins et al. 2011; Robbins et al. 2013; Ginhoux et al. 2016). A few studies in atherosclerosis and cancer indicate that macrophage proliferation also exists in humans; however, their contribution to cancer development is still unclear (Bottazzi et al. 1990; Lutgens et al. 1999; Campbell et al. 2011).
During the last decades, increasing evidence has highlighted the multifunctional properties of macrophages, which are now considered highly plastic cells, which can modify their phenotype in response to microenvironmental signals, with classical M1 and alternative M2 polarization states as the reference paradigm (Galdiero et al. 2013b; Bonavita et al. 2015).
Chemotactic molecules involved in monocyte recruitment at the tumor site include CCL2 and CCL5, vascular endothelial growth factors (VEGFs), and M-CSF. Besides their chemotactic functions, these factors contribute to macrophage polarization toward specific phenotypes (Kitamura et al. 2015). In a transgenic mouse model in which CCL2 was overexpressed specifically in mammary epithelial cells, there was increased macrophage infiltration, increased expression of extracellular matrix (ECM) remodeling genes, such as matrix metalloproteases (MMPs) and lipoxygenase (LOX), and increased stromal density. In addition, CCL2 transgenic mice displayed an increased susceptibility to 7,12-dimethylbenz(a)anthracene (DMBA)-induced carcinogenesis, thus suggesting that CCL2 overexpression increases mammary stromal density and breast cancer risk (Sun et al. 2017). Also, M-CSF is a classical monocyte chemoattractant, which also favors macrophage survival and skewing toward a tumor-promoting “M2-like” phenotype (Pyonteck et al. 2013).
Tumor-infiltrating T and B cells as well as stromal cells can release factors activating classic M1 macrophages, able to recognize and eliminate nascent tumor cells in line with the “elimination phase” of the immunoediting (Dunn et al. 2002). However, if this process is not successful, tumors can evolve and, along with tumor progression, macrophage can divert through an M2/M2-like phenotype, which sustains many aspects of tumor growth and progression in line with the “escape phase” of the immunoediting (Dunn et al. 2002). This phenomenon can be driven directly by tumor cells or indirectly by “already corrupted” immune cells releasing M2-skewing molecules, such as interleukin (IL)-4, IL-13, immunocomplexes, transforming growth factor (TGF)-β, or M-CSF. Recently, in a murine model of breast cancer, overexpression of IL-23p19 was associated with increased tumor growth, pulmonary metastasis, and reduced survival. IL-23p19 overexpressing tumors displayed increased expression of MMP-9, CD31, and ki67, thus suggesting a higher ECM remodeling and proliferative activity. Moreover, tumors displayed decreased percentages of CD4+ and CD8+ T cells, as well as increased infiltration of M2-like macrophages expressing VEGF and TGF-β and neutrophils expressing IL-10 and VEGF. These findings suggested that IL-23 promoted infiltration of M2-like macrophages and neutrophils endowed with immunosuppressive capacity (Nie et al. 2017). M2 macrophages are classically characterized by a high production of chemokines, including CCL17, CCL22, or CCL24, involved in the recruitment of T helper (Th)2 cells, regulatory T cells (Tregs), eosinophils, and basophils, as well as a high production of IL-10. M2 macrophages produce low levels of IL-12 and are mainly involved in immunoregulatory networks, regulating tissue remodeling, and angiogenesis (Mantovani et al. 2013).
TAMs can acquire a wide range of activation states, depending on the tumor-related cellular and molecular network. Thus, the pathways of TAM activation vary among the various tumor types and, in some circumstances, within the same tumor (Ruffell et al. 2012). For example, in distinct tumor areas the variable access to oxygen is responsible for various levels of activation of metabolic pathways involved in tuning macrophage phenotypes (Movahedi et al. 2010; Henze and Mazzone 2016).
Despite the fine modulation of macrophage activation states in distinct tumors, M2-like polarization usually represents a common determinant. Indeed, TAMs display a number of M2-resembling functions, which ultimately are beneficial to cancer progression. Indeed, TAMs promote tumor cell growth through the production of growth factors such as epidermal growth factor (EGF), which induces breast cancer cell proliferation (Qian and Pollard 2010). In addition, TAMs produce high levels of reactive oxygen and nitrogen species, which contribute to DNA damage and genetic instability of cancer cells (Bonavita et al. 2015). Moreover, TAMs promote tumor-invasive behavior and metastatic progression. Indeed, they release proteolytic enzymes, such as MMPs, involved in ECM digestion and remodeling thus favoring tumor cell invasion (Allavena and Mantovani 2012). In addition to tissue remodeling, TAMs also promote angiogenesis and lymphangiogenesis, producing angiogenic/lymphangiogenic factors such as VEGF-A, VEGF-C, TGF-β, as well as proangiogenic chemokines such as CCL2 and CXCL8 (Hotchkiss et al. 2003; Murdoch et al. 2008; Granata et al. 2010; Schmidt and Carmeliet 2010). Tumor-associated hypoxia induces a proangiogenic program in TAMs, through the up-regulation of hypoxia-inducible factor (HIF)-1α, as well as through the production of adenosine, which in turn promotes the release of proangiogenic and lymphangiogenic factors by human macrophages (Granata et al. 2010). Finally, TAMs promote tumor progression by suppressing antitumor immunity. Indeed, TAMs produce immunosuppressive molecules (e.g., TGF-β, IL-10, indoleamine 2,3-dioxygenase [IDO], and arginase-1), which suppress adaptive T-cell immune responses and favor Treg recruitment and functions (Ruffell et al. 2012; Noy and Pollard 2014). In a mouse model of colitis-associated cancer (CAC), macrophages produced IL-17, which increased survival and immunosuppressive activity of granulocytic myeloid-derived suppressor cells (G-MDSCs) thus fostering tumor progression (Zhang et al. 2016). TAMs also express programmed cell death protein 1 (PD-1) ligands PD-L1 and PD-L2, which bind on T cells and activate the inhibitory PD-1 immune checkpoint in T cells (Kryczek et al. 2006; Wang et al. 2011). Moreover, TAMs could also express B7-H4 and VISTA, which likely exert similar functions (Deng et al. 2016; Wang et al. 2016b).
ROLES OF NEUTROPHILS IN TUMOR GROWTH AND PROGRESSION
Experimental models and epidemiological studies have shed new light on neutrophil roles in modulating tumor behavior. Indeed, TANs are pivotal players in CRI and can exert antitumoral or protumoral functions. Moreover, they are endowed with unsuspected plasticity (Fridlender et al. 2009; Mantovani 2009; Granot and Jablonska 2015). In murine models of cancer, neutrophils were driven by TGF-β to acquire a protumoral phenotype (Fridlender et al. 2009). Indeed, TGF-β inhibition led to the tumor infiltration of neutrophils with increased cytotoxicity against tumor cells, high expression of tumor necrosis factor α (TNF-α), CCL3, and intercellular adhesion molecule 1 (ICAM-1), and low levels of arginase-1. TGF-β inhibition also promoted a T-cell antitumor response, which involved neutrophils as effector cells (Fridlender et al. 2009). In this seminal paper, neutrophils were proposed to polarize in two distinct activation states: an antitumor N1 or a protumor N2 phenotype in response to signals derived from TME. In an in vivo model of melanoma and fibrosarcoma, mice lacking interferon (IFN)-β showed an infiltration of proangiogenic neutrophils, characterized by a high expression of CXCR4, VEGF-A, and MMP-9 (Jablonska et al. 2010). These results suggested a pivotal role for type I IFNs in polarizing neutrophils toward an N1 antitumor phenotype (Granot and Jablonska 2015).
Within the TME, CXC chemokines produced by tumor and stromal cells and associated with cancer growth and progression also retain neutrophil-recruiting functions (Keeley et al. 2010; Lazennec and Richmond 2010; Mantovani et al. 2011). For instance, murine models showed a central role for CXCR2 in promoting lung and pancreatic cancers (Keane et al. 2004; Ijichi et al. 2011). Indeed, inflammation-induced and spontaneous carcinogenesis were suppressed following CXCR2 abrogation or neutrophil depletion in mice (Jamieson et al. 2012). Moreover, CXCL17 promoted cancer growth together with the increased infiltration of a myeloid subset of CD11b+Gr1+F4/80− cells in a murine model of graft tumor (Matsui et al. 2012). In a conditional genetic murine model of lung cancer driven by K-ras activation and p53 inactivation, TAM and TAN precursors accumulated in the spleen and relocated from the spleen to the tumor, suggesting a role for the spleen as reservoir for tumor-promoting myeloid cells (Cortez-Retamozo et al. 2012). In humans, head and neck squamous cell carcinoma (HNSCC) cell lines produced CXCL8 and macrophage-inhibiting factor (MIF), which recruited neutrophils through the engagement of CXCR2 (Dumitru et al. 2011; Trellakis et al. 2011b). Hepatocellular carcinoma cells recruited neutrophils through the production of CXCL8 (Kuang et al. 2011).
Neutrophils play important roles in tumor initiation. Indeed, neutrophil-derived oxygen and nitrogen derivatives are responsible for DNA point mutations and promoted genetic instability (Gungor et al. 2010). Moreover, the MPO-derived hypochlorous acid HOCl activated MMPs and inactivated the tissue inhibitor of proteases (TIMP-1), thus promoting ECM remodeling as well as invasive and metastatic behavior of cancer cells (De Larco et al. 2004).
Granule proteins were also involved in tumor progression. For instance, neutrophil elastase (NE) taken up by lung cancer cells degraded the phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K) inhibitor, insulin receptor substrate 1 (IRS-1). This event unleashed PI3K activation and platelet-derived growth factor receptor (PDGFR) signaling, thus favoring tumor cell proliferation (Houghton et al. 2010). NE was also involved in neutrophil-related epithelial-to-mesenchymal transition (EMT) (Grosse-Steffen et al. 2012). On the contrary, NE taken up by breast cancer cells cleaved cyclin E, which was then presented in a truncated form in HLA-I context and efficiently activated a cytotoxic T lymphocytes–mediated antitumor response (Mittendorf et al. 2012). More recently, NE uptake increased the responsiveness of breast cancer cells to adaptive immunity by up-regulation of HLA class I (Chawla et al. 2016). Neutrophils released the cytokine oncostatin M, which up-regulated VEGF production in breast cancer cells, promoting tumor cell detachment and invasiveness (Queen et al. 2005). In bronchoalveolar carcinoma patients, hepatocyte growth factor (HGF) in broncholavage fluid correlated with neutrophil infiltration and was associated with poor prognosis (Wislez et al. 2003; Imai et al. 2005). In HNSCC patients, neutrophil infiltration correlated with the expression of Cortactin and with poor clinical outcome (Dumitru et al. 2013).
On the contrary, neutrophils also release TRAIL, which retains important antitumoral activities (Cassatella 2006; Hewish et al. 2010). Indeed, in bladder cancer, Mycobacterium bovis bacillus Calmette–Guerin (BCG) induced the release of TRAIL from neutrophils, which accounted for the anticancer effects of BCG (Kemp et al. 2005). Moreover, in chronic myeloid leukemia (CML) patients, IFN-α stimulation induced the release of TRAIL from neutrophils, which favored apoptosis of leukemic cells (Tecchio et al. 2004; Tanaka et al. 2007).
In surgically resected lung cancer patients, TANs produced the proinflammatory molecules CCL2, CCL3, CXCL8, and IL-6, stimulated T-cell proliferation, and IFN-γ release, mainly in a contact-dependent manner (Eruslanov et al. 2014). Neutrophils up-regulated the expression of costimulatory molecules (e.g., CD86 and OX40L), amplifying a positive feedback loop, which suggested an antitumor role for TANs in early stages human lung cancers (Eruslanov et al. 2014).
Neutrophils can also play a dual role in modulating metastatic behavior of cancer cells and angiogenesis. Melanoma-derived CXCL8 up-regulated β2-integrin expression on neutrophils, which interacted with ICAM-1 expressed by melanoma cells, allowing neutrophils to carry tumor cells to metastatic sites (Huh et al. 2010). Neutrophil extracellular traps (NETs) also captured circulating tumor cells and favored their engraftment to distant organ sites (Cools-Lartigue et al. 2013). In contrast, in a murine model of transplanted breast cancer, under the influence of granulocyte colony stimulating factor (G-CSF) and tumor-derived CCL2, neutrophils inhibited breast metastasis in the premetastatic lung in an H2O2-dependent manner (Granot et al. 2011).
Neutrophils are a major source of VEGF-A, which is also responsible for the angiogenic activity exerted by CXCL1 in vivo (Scapini et al. 2004). Neutrophils express high levels of MMP-9, which releases the active form of VEGF-A from the ECM (Nozawa et al. 2006; Kuang et al. 2011; Dumitru et al. 2012). Interestingly, neutrophils release MMP-9 in a TIMP-free manner, which further enhanced the proangiogenic and proinvasive activity of MMP-9 (Ardi et al. 2007). Unexpectedly, intratumoral delivery of MMP-9 decreased tumor growth and angiogenesis in a murine model of breast cancer, suggesting that MMP-9 also retains antiangiogenic functions (Leifler et al. 2013). In a tumor xenograft murine model, under the influence of G-CSF, neutrophils released the proangiogenic molecule Bv8, and its neutralization significantly impaired angiogenesis and tumor growth (Shojaei et al. 2007). Interestingly, tumors resistant to anti-VEGF therapy showed high infiltration of neutrophils and drug resistance was associated with G-CSF-induced Bv8 neutrophil expression (Shojaei et al. 2008, 2009). In contrast, neutrophils also express a number of antiangiogenic molecules. For example, NE cleaved VEGF and fibroblast growth factor 2 (FGF-2), giving rise to the angiostatin-like fragments from plasminogen, which suppressed VEGF- and FGF-2-induced angiogenesis (Scapini et al. 2004; Ai et al. 2007).
Neutrophil plasticity and heterogeneity have been highlighted by several recent observations in mice and in cancer patients. Indeed, circulating neutrophils are usually purified on a discontinuous density gradient (Ficoll). Following this separation, neutrophils are found in the high-density (HD) granulocytic fraction, whereas peripheral blood mononuclear cells (PBMCs) segregate in the low-density (LD) mononuclear fraction (Boyum 1968). However, an increasing number of studies shows that in chronic inflammatory conditions such as HIV, autoimmunity, and cancer, neutrophils could also be found in the LD fraction (Schmielau and Finn 2001; Rodriguez et al. 2009; Denny et al. 2010; Cloke et al. 2012). Moreover, the percentage of low-density neutrophils (LDNs) increases with cancer progression, and these cells retain T-cell-suppressive properties and include both mature and immature granulocytes (Mishalian et al. 2017). Immature granulocytes found in LD fraction have always been considered as G-MDSCs. MDSCs are a heterogeneous subset of myeloid cells, expanding in peripheral blood and spleen of tumor-bearing mice and cancer patients, and characterized by the capacity to suppress T-cell activation and proliferation (Gabrilovich and Nagaraj 2009; Peranzoni et al. 2010). Because G-MDSCs and neutrophils are both of myeloid origin, have similar morphological aspects and surface markers, as well as tumor-promoting properties, there is no clear consensus on the differences between these populations of cells. A transcriptomic analysis of peripheral neutrophils, TANs, and G-MDSCs in tumor-bearing mice found that TANs and G-MDSCs are distinct populations and that naïve neutrophils and G-MDSCs are more closely related to each other than to TANs (Fridlender et al. 2012). An interesting study performed on tumor-bearing mice as well as on breast and lung cancer patients showed that circulating neutrophils in cancer consist of two distinct subsets: mature segmented high-density neutrophils (HDNs) and LDNs. Within LDNs, two further subsets could be distinguished: a mature segmented one and a banded immature one, namely, G-MDSC. Both in tumor-bearing mice and cancer patients, the LDN fraction increased along with tumor progression (Sagiv et al. 2015). Although HDNs displayed antitumor functions, LDNs showed reduced chemotaxis, phagocytosis, oxidative burst, no significant cytotoxic activity against tumor cells, and significantly impaired T-cell activity and proliferation. These cancer-promoting activities were shared by both mature and immature (G-MDSCs) LDNs. Moreover, in this study, beyond this heterogeneity, the authors proposed an important plasticity, showing that HDNs can progress through the LDN transition under the influence of TGF-β and acquire T-cell-suppressive properties, thus suggesting that part of the LDN fraction is a subset of highly activated mature neutrophils but with reduced inflammatory properties. They also proposed that LDNs can switch to HDNs, but to a lesser extent than the opposite transition (Sagiv et al. 2015). These observations suggest that neutrophils are not terminally differentiated as previously thought. Indeed, they highlight the potential heterogeneity and plasticity of circulating neutrophils in cancer development and call for a rigorous reassessment of neutrophil characterization in cancer patients.
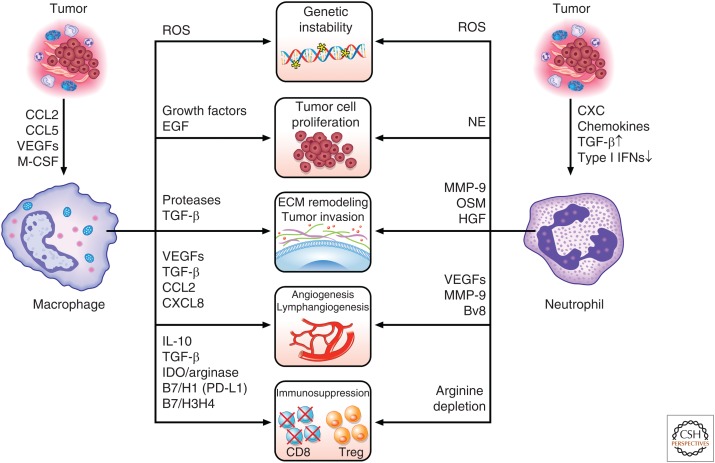
A schematic view of the roles of TAMs and TANs in CRI is summarized in Figure 1.
Figure 1.
Tumor-associated macrophages (TAMs) and tumor-associated neutrophils (TANs) as key regulators of the tumor-related inflammation. Neoplastic and stromal cells recruit macrophages and neutrophils, favoring their polarization toward a protumor phenotype. In turn, TAMs and TANs induce genetic instability (through the release of reactive oxygen species [ROS]), favor tumor growth (through the production of growth factors and neutrophil elastase [NE]), promote the remodeling of the extracellular matrix (ECM) and tumor cell invasive capabilities (through the release of proteases, transforming growth factor β [TGF-β], hepatocyte growth factor [HGF], and oncostatin M [OSM]), support angiogenesis and lymphangiogenesis (through the release of vascular endothelial growth factors [VEGFs], matrix metalloprotease (MMP)-9, and Bv8), and suppress antitumoral adaptive immunity (through arginine depletion and expression of suppressive soluble and membrane molecules, such as interleukin (IL)-10 and programmed cell death protein 1 ligand (PD-L1). See text for details. IDO, Indoleamine 2,3-dioxygenase; M-CSF, macrophage colony-stimulating factor; EGF, epidermal growth factor; Treg, regulatory T cell; IFN, interferon.
TAMs AND TANs AS PROGNOSTIC/PREDICTIVE BIOMARKERS IN CANCER PATIENTS
High TAM infiltration was associated with poor clinical outcome in a variety of human cancers (Bingle et al. 2002; Qian and Pollard 2010; Zhang et al. 2012). In breast cancer patients, a high macrophage infiltration was associated with high tumor grade and poor outcome (Campbell et al. 2011). Similarly, in bladder cancer patients, high TAM density correlated with advanced disease stage and poor survival (Hanada et al. 2000). In contrast, a positive correlation was found between TAM infiltration and patient survival in high-grade osteosarcoma patients (Buddingh et al. 2011) and TAMs positively correlated with tumor cell apoptosis and CD8+ infiltration in gastric cancer (Ohno et al. 2003). Some apparently controversial results can be explained considering that macrophages within a tumor are not homogeneous, and the TAM phenotype can vary within the same tumor. Moreover, there is a huge variability related on the techniques used to identify TAMs in tissues (CD68+, CD203+, CD206+, stabilin1+ cells, etc.), which may contribute to the variability of the results among different studies.
Interestingly, in follicular lymphoma patients, CD68+CD163+ TAM infiltration was associated with an adverse outcome in patients treated with first-line systemic treatment, including rituximab, cyclophosphamide, vincristine, and prednisone, but with favorable outcome in patients treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone. These results suggest that CD163+ macrophage density predicts the outcome in follicular lymphoma, but their prognostic impact is highly dependent on treatment received. This interesting study highlights the potential role of TAMs as a predictive marker of chemotherapy response (Kridel et al. 2015). Indeed, the vast majority of cancer patients are treated with old and new generation cytoreductive drugs or radiotherapy. This aspect is often neglected in epidemiological studies. Thus, the prognostic significance of TAM infiltration loses its value if it is not related to the administered therapy.
With regard to solid tumors, data on the predictive role of TAMs are missing. Indeed, most studies do not mention the therapeutic regimen administered to the patients, nor take account of this parameter in the statistical evaluation. The only study investigating the role of TAMs as predictors of chemotherapy response has been performed on pancreas cancer patients. This study revealed that TAM density correlated with a worse prognosis and increased distant metastasis only in patients who did not receive chemotherapy; indeed, gemcitabine administration restrained TAM protumour prognostic significance (Di Caro et al. 2016). Thus, TAMs retain important predictive significance in the response to chemotherapy in cancer patients and can be an additional tool to stratify patients for chemotherapy after surgery.
The relationship between TAN infiltration and prognosis in human cancer has been previously discussed (Donskov 2013). Neutrophil infiltration within human cancers has been correlated with poor clinical outcome in patients with metastatic and localized clear cell carcinomas, bronchioloalveolar carcinoma, liver cancer, colorectal carcinoma (CRC), and HNSCC (Wislez et al. 2003; Jensen et al. 2009; Kuang et al. 2011; Trellakis et al. 2011a; Rao et al. 2012). In addition, high neutrophil infiltration has been associated with high tumor grade in human gliomas and with aggressive pancreatic tumors (Fossati et al. 1999; Reid et al. 2011). In contrast, TANs have been associated with better prognosis in gastric cancer (Caruso et al. 2002) and CRC (Droeser et al. 2013; Galdiero et al. 2016). As discussed for TAMs, these apparently controversial results may depend on the type/subtype of tumors and on the techniques used to identify neutrophils within the tumors (e.g., hematoxylin–eosin stain versus immunohistochemistry) (Donskov 2013).
As for TAMs, studies evaluating the predictive value of TANs in human settings are missing. The only published comparison of the association of TANs with outcome in patients who received chemotherapy after tumor resection versus those who did not receive chemotherapy was performed on patients with CRC. In stage III patients, TAN infiltration was associated with better response to 5-fluorouracil (5FU)-based chemotherapy but with poor prognosis in patients treated with surgery alone (Galdiero et al. 2016). These results suggest a dual clinical significance of TANs, depending on the administration of chemotherapy, and make necessary a rigorous evaluation of the role of TAN density as a predictive factor for response to therapy in human cancer (Galdiero et al. 2016).
Several studies have evaluated the prognostic and predictive value of neutrophil-to-lymphocyte ratio (NLR) in peripheral blood of cancer patients. NLR is commonly used as a measure of systemic inflammation, and it has been shown to predict patient clinical outcome in a number of human cancers, such as rectal (Shen et al. 2017), esophageal (Nakamura et al. 2017), prostate (Gokce et al. 2016), pancreatic (Kadokura et al. 2016), and breast cancer (Ethier et al. 2017). Overall, a high NLR score was associated with worse survival and retained a more consistent prognostic value among patients with an advanced disease stage, who are also more likely to receive chemotherapy treatments or who are not operable (Guthrie et al. 2013). The advantage of this score is that it can be easily evaluated, but its prognostic power remains controversial. Indeed, NLR is not a specific biomarker because it might be confounded by other comorbidities (Di Caro et al. 2014). Moreover, it is important to remember that, because of the well-known heterogeneity of neutrophil subsets, circulating neutrophils may not faithfully mirror the tumor-related ones. Thus, further studies aimed at investigating circulating neutrophil-related markers that more likely reflect the TME are needed to identify more specific diagnostic biomarkers of tumor detection.
ROLES OF TAMs AND TANs IN ANTICANCER THERAPEUTIC RESPONSES
Given the protumor functions of TAMs, a number of therapeutic strategies have been evaluated based on their targeting. These approaches are designed to limit TAM recruitment, inhibit their protumor functions, and reeducate them toward an antitumor phenotype.
CCL2 inhibition reduced tumor growth and metastasis in experimental models of prostate, breast, lung, liver cancer, or melanoma. In combination with chemotherapy, anti-CCL2 antibodies improved the therapeutic efficacy of the drugs (Loberg et al. 2007; Lu and Kang 2009; Fridlender et al. 2011; Moisan et al. 2014). Anti-CCL2 antibodies have entered phase I and II clinical trials in patients with solid tumors, but showed controversial results (Pienta et al. 2013; Sandhu et al. 2013; Brana et al. 2015). M-CSF (CSF-1) is the main growth and differentiation factor for monocytes and macrophages and is expressed by several tumors. A number of small molecules and antibodies directed against CSF-1 receptor (CSF-1R) have been evaluated in preclinical settings and clinical trials (Manthey et al. 2009; Ries et al. 2014). The humanized antibody emactuzumab showed efficacy in patients with various malignancies and was promising in patients with diffuse-type tenosynovial giant-cell tumor (Ries et al. 2014). Pexidartinib, a small CSF-1R inhibitor did not show efficacy in glioblastoma patients (Butowski et al. 2016). However, when anti-CSF-1R drugs were combined with traditional anticancer therapy, the results were enhanced. For example, in a transgenic model of gemcitabine-resistant pancreatic tumor, the anti-CSF-1R inhibitor GW2580 enhanced the efficacy of gemcitabine through the elimination of TAMs, which were responsible for drug resistance (Weizman et al. 2014). In a transgenic model of breast cancer, inhibition of CSF-1/CSF-1R axis enhanced the therapeutic effect of paclitaxel, inhibited metastatic spreading, and increased intratumoral T-cell infiltration (DeNardo et al. 2011). Thus, targeting TAMs appears to be a promising complementary strategy to enhancing the therapeutic power of conventional anticancer therapies.
Trabectedin is an European Medicines Evaluation Agency (EMEA)-approved natural product with antitumor activity (Germano et al. 2010). Indeed, trabectedin activated the TRAIL-dependent apoptotic pathway selectively in monocytes, because of their low expression of TRAIL decoy receptors (Liguori et al. 2016). In murine models and human sarcoma patients, trabectedin treatment resulted in a reduction of TAM infiltration and angiogenesis (Germano et al. 2010), thus suggesting a promising role in TAM-targeted antitumor therapies.
TAM reeducation toward an antitumor phenotype represents a desirable goal. In this line, IFN-γ administration has been proposed in ovarian cancer patients (Colombo et al. 1992). This treatment led to the systemic antitumor cytotoxic activation and clinical response, but the real efficacy of IFN-γ immunotherapy is still poorly understood. In a murine model of pancreatic cancer, the fully human CD40 agonist antibody CP-870,893, in combination with gemcitabine chemotherapy, induced a switch in TAM phenotype from a tumor-promoting to an antitumor profile, with enhanced antigen-presenting activities that impaired tumor growth. In a phase II clinical trial in patients with advanced pancreatic cancer, 19% of patients had partial responses and 52% had a period of disease stabilization (Beatty et al. 2011).
Myeloid cells can also influence the effectiveness of chemotherapeutic drugs. Indeed, it is now well known that chemotherapeutic drugs exert their effects not only by acting on the tumor cell itself, but also on tumor-related immune cells. Actually, some chemotherapeutic drugs, such as doxorubicin, determine an “immunogenic cell death.” Tumor cell death induces the expression of “danger signals” (i.e., calreticulin, adenosine triphosphate [ATP], high-mobility group box 1 [HMGB-1]), which recruit and activate myeloid dendritic-cell-like cells. These cells are particularly efficient in capturing and presenting tumor cell antigens and give rise to an effective antitumor immune response (Galluzzi et al. 2012; Ma et al. 2013).
TAMs can also limit the effectiveness of chemotherapeutic drugs, such as paclitaxel and doxorubicin. For example, in murine models of breast and lung cancer, following chemotherapy M2-like macrophages accumulated in perivascular areas of tumors and favored tumor neo-angiogenesis in a CXCL12/CXCR4-dependant manner (Hughes et al. 2015). Anti-VEGF therapies are also associated with the accumulation of myeloid cells in perivascular areas as a consequence of the local hypoxia induced by the antiangiogenic therapy. In some circumstances, these cells activate an alternative program and produce proangiogenic molecules such as Bv8, which overcome the antiangiogenic effect of the drug (Murdoch et al. 2008; Shojaei et al. 2009). Thus, targeting TAMs can be an effective therapeutic strategy that is complementary to current chemotherapeutic and antiangiogenic therapies and can efficiently improve their effectiveness.
Immunotherapy using checkpoint inhibitors is an established part of the therapeutic strategies for an increasing number of cancers (Sharma and Allison 2015). Macrophages can express PD-L1 and PD-L2, which can be up-regulated under the influence of proinflammatory stimuli and hypoxia (Noman et al. 2014). The predictive power of these molecules on TAMs needs to be carefully evaluated. To what extent the expression of PD-L1 on macrophages can contribute to the therapeutic efficacy of immune checkpoint inhibitors is not yet understood.
The evaluation of TANs as therapeutic targets is still limited because a role of these cells in cancer development is a recent concept. Considering the tumor-promoting functions of TANs, targeting these cells could be desirable. However, their depletion could lead to deleterious “side effects.” Indeed, neutrophils play a pivotal role in host defense against infections and their depletion could give rise to immunosuppression. TAN neutralization could be obtained by inhibiting their recruitment or their effector molecules. In a murine model of fibrosarcoma and prostate cancer, TAN recruitment inhibition through CXCL8/IL-8 blockage significantly reduced angiogenesis and tumor growth (Bekes et al. 2011). In addition, in murine inflammation-driven and spontaneous carcinogenesis, CXCR2 deletion and/or inhibition blocked tumor development (Jamieson et al. 2012). Repertaxin, a small molecule inhibitor of CXCR1 and CXCR2, selectively targeted human breast cancer stem cells and inhibited tumor growth in xenograft murine models (Ginestier et al. 2010). More recently, the combination of repertaxin and 5-FU was shown to increase gastric cancer cell apoptosis and inhibited cellular proliferation, migration, and invasion (Wang et al. 2016a). Clinical trials are currently investigating the role of repertaxin in breast cancer patients, alone or in combination with chemotherapeutic drugs (paclitaxel) (www.clinicaltrials.gov).
The inhibitor of NE sivelastat efficiently suppressed breast cancer cell proliferation and enhanced the antitumor effect of trastuzumab, through restoring the expression of Her2/Neu (Nawa et al. 2012). Genetic deficiency and chemical inhibition of NE significantly reduced the incidence of ultraviolet-B-induced tumors in mice (Starcher et al. 1996). The NE inhibitor ONO-5046 inhibited both primary and metastatic growth of non-small-cell lung cancer (NSCLC) in severe combined immunodeficiency (SCID) mice (Inada et al. 1998). NE inhibitors are currently undergoing clinical trials for treatment of cystic fibrosis and respiratory diseases (www.clinicaltrials.gov), and these results could also be useful for cancer research.
CONCLUDING REMARKS
There is compelling evidence that cellular and humoral components of the TME have a large impact on cancer initiation and progression and on the resilience of most tumors in the face of therapy. Macrophages and neutrophils are both integrated within CRI and can take part in the various phases of tumor initiation and progression. Cancer cells as well as TAMs and neutrophils can release a plethora of protumorigenic and proangiogenic cytokines/chemokines. Targeting these mediators as well as blocking protumor functions could be useful for inhibiting tumor growth. On the other hand, fostering anticancer immune responses by blocking immunosuppressive molecules (e.g., TGF-β, IL-10, CTLA-4, PD-1, PD-L1), expressed either by cancer cells or by tumor-infiltrating immune cells, appears a promising therapeutic strategy in different tumors.
In conclusion, a deeper insight into the molecular mechanisms regulating the link between tumor-infiltrating immune cells and cancer cells could lead to the finding of new prognostic/predictive biomarkers, as well as a wider view of cancer immunotherapy, in an even more personalized therapeutic approach.
ACKNOWLEDGMENTS
This work is supported in part by grants from the Regione Campania CISI Laboratory Project, the CRèME Project, and the TIMING Project. We thank Fabrizio Fiorbianco for the figure. A.M. is supported by grants from the Associazione Italiana per la Ricerca sul Cancro (AIRC), an IG grant, and a 5X1000 grant, and by the Italian Ministry of Health.
Footnotes
Editors: Warren J. Leonard and Robert D. Schreiber
Additional Perspectives on Cytokines available at www.cshperspectives.org
REFERENCES
- Ai S, Cheng XW, Inoue A, Nakamura K, Okumura K, Iguchi A, Murohara T, Kuzuya M. 2007. Angiogenic activity of bFGF and VEGF suppressed by proteolytic cleavage by neutrophil elastase. Biochem Biophys Res Commun 364: 395–401. [DOI] [PubMed] [Google Scholar]
- Alam M, Khan M, Veledar E, Pongprutthipan M, Flores A, Dubina M, Nodzenski M, Yoo SS. 2016. Correlation of inflammation in frozen sections with site of nonmelanoma skin cancer. JAMA Dermatol 152: 173–176. [DOI] [PubMed] [Google Scholar]
- Allavena P, Mantovani A. 2012. Immunology in the clinic review series; focus on cancer: Tumour-associated macrophages: Undisputed stars of the inflammatory tumour microenvironment. Clin Exp Immunol 167: 195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allavena P, Sica A, Garlanda C, Mantovani A. 2008. The Yin–Yang of tumor-associated macrophages in neoplastic progression and immune surveillance. Immunol Rev 222: 155–161. [DOI] [PubMed] [Google Scholar]
- Al Murri AM, Bartlett JM, Canney PA, Doughty JC, Wilson C, McMillan DC. 2006. Evaluation of an inflammation-based prognostic score (GPS) in patients with metastatic breast cancer. Br J Cancer 94: 227–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardi VC, Kupriyanova TA, Deryugina EI, Quigley JP. 2007. Human neutrophils uniquely release TIMP-free MMP-9 to provide a potent catalytic stimulator of angiogenesis. Proc Natl Acad Sci 104: 20262–20267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkwill F, Mantovani A. 2001. Inflammation and cancer: Back to Virchow? Lancet 357: 539–545. [DOI] [PubMed] [Google Scholar]
- Barash H, E RG, Edrei Y, Ella E, Israel A, Cohen I, Corchia N, Ben-Moshe T, Pappo O, Pikarsky E, et al. 2010. Accelerated carcinogenesis following liver regeneration is associated with chronic inflammation-induced double-strand DNA breaks. Proc Natl Acad Sci 107: 2207–2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty GL, Chiorean EG, Fishman MP, Saboury B, Teitelbaum UR, Sun W, Huhn RD, Song W, Li D, Sharp LL, et al. 2011. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science 331: 1612–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekes EM, Schweighofer B, Kupriyanova TA, Zajac E, Ardi VC, Quigley JP, Deryugina EI. 2011. Tumor-recruited neutrophils and neutrophil TIMP-free MMP-9 regulate coordinately the levels of tumor angiogenesis and efficiency of malignant cell intravasation. Am J Pathol 179: 1455–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingle L, Brown NJ, Lewis CE. 2002. The role of tumour-associated macrophages in tumour progression: Implications for new anticancer therapies. J Pathol 196: 254–265. [DOI] [PubMed] [Google Scholar]
- Bonavita E, Galdiero MR, Jaillon S, Mantovani A. 2015. Phagocytes as corrupted policemen in cancer-related inflammation. Adv Cancer Res 128: 141–171. [DOI] [PubMed] [Google Scholar]
- Bornstein S, White R, Malkoski S, Oka M, Han G, Cleaver T, Reh D, Andersen P, Gross N, Olson S, et al. 2009. Smad4 loss in mice causes spontaneous head and neck cancer with increased genomic instability and inflammation. J Clin Invest 119: 3408–3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottazzi B, Erba E, Nobili N, Fazioli F, Rambaldi A, Mantovani A. 1990. A paracrine circuit in the regulation of the proliferation of macrophages infiltrating murine sarcomas. J Immunol 144: 2409–2412. [PubMed] [Google Scholar]
- Boyum A. 1968. Isolation of mononuclear cells and granulocytes from human blood. Isolation of monuclear cells by one centrifugation, and of granulocytes by combining centrifugation and sedimentation at 1 g. Scand J Clin Lab Invest Suppl 97: 77–89. [PubMed] [Google Scholar]
- Brana I, Calles A, LoRusso PM, Yee LK, Puchalski TA, Seetharam S, Zhong B, de Boer CJ, Tabernero J, Calvo E. 2015. Carlumab, an anti-C-C chemokine ligand 2 monoclonal antibody, in combination with four chemotherapy regimens for the treatment of patients with solid tumors: An open-label, multicenter phase 1b study. Target Oncol 10: 111–123. [DOI] [PubMed] [Google Scholar]
- Buddingh EP, Kuijjer ML, Duim RA, Burger H, Agelopoulos K, Myklebost O, Serra M, Mertens F, Hogendoorn PC, Lankester AC, et al. 2011. Tumor-infiltrating macrophages are associated with metastasis suppression in high-grade osteosarcoma: A rationale for treatment with macrophage activating agents. Clin Cancer Res 17: 2110–2119. [DOI] [PubMed] [Google Scholar]
- Butowski N, Colman H, De Groot JF, Omuro AM, Nayak L, Wen PY, Cloughesy TF, Marimuthu A, Haidar S, Perry A, et al. 2016. Orally administered colony stimulating factor 1 receptor inhibitor PLX3397 in recurrent glioblastoma: An Ivy Foundation Early Phase Clinical Trials Consortium phase II study. Neuro Oncol 18: 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MJ, Tonlaar NY, Garwood ER, Huo D, Moore DH, Khramtsov AI, Au A, Baehner F, Chen Y, Malaka DO, et al. 2011. Proliferating macrophages associated with high grade, hormone receptor negative breast cancer and poor clinical outcome. Breast Cancer Res Treat 128: 703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruso RA, Bellocco R, Pagano M, Bertoli G, Rigoli L, Inferrera C. 2002. Prognostic value of intratumoral neutrophils in advanced gastric carcinoma in a high-risk area in northern Italy. Mod Pathol 15: 831–837. [DOI] [PubMed] [Google Scholar]
- Cassatella MA. 2006. On the production of TNF-related apoptosis-inducing ligand (TRAIL/Apo-2L) by human neutrophils. J Leukoc Biol 79: 1140–1149. [DOI] [PubMed] [Google Scholar]
- Chawla A, Alatrash G, Philips AV, Qiao N, Sukhumalchandra P, Kerros C, Diaconu I, Gall V, Neal S, Peters HL, et al. 2016. Neutrophil elastase enhances antigen presentation by upregulating human leukocyte antigen class I expression on tumor cells. Cancer Immunol Immunother 65: 741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloke T, Munder M, Taylor G, Muller I, Kropf P. 2012. Characterization of a novel population of low-density granulocytes associated with disease severity in HIV-1 infection. PloS ONE 7: e48939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo N, Peccatori F, Paganin C, Bini S, Brandely M, Mangioni C, Mantovani A, Allavena P. 1992. Anti-tumor and immunomodulatory activity of intraperitoneal IFN-γ in ovarian carcinoma patients with minimal residual tumor after chemotherapy. Int J Cancer 51: 42–46. [DOI] [PubMed] [Google Scholar]
- Cools-Lartigue J, Spicer J, McDonald B, Gowing S, Chow S, Giannias B, Bourdeau F, Kubes P, Ferri L. 2013. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest 10.1172/JCI67484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortez-Retamozo V, Etzrodt M, Newton A, Rauch PJ, Chudnovskiy A, Berger C, Ryan RJ, Iwamoto Y, Marinelli B, Gorbatov R, et al. 2012. Origins of tumor-associated macrophages and neutrophils. Proc Natl Acad Sci 109: 2491–2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies LC, Rosas M, Smith PJ, Fraser DJ, Jones SA, Taylor PR. 2011. A quantifiable proliferative burst of tissue macrophages restores homeostatic macrophage populations after acute inflammation. Eur J Immunol 41: 2155–2164. [DOI] [PubMed] [Google Scholar]
- De Larco JE, Wuertz BR, Furcht LT. 2004. The potential role of neutrophils in promoting the metastatic phenotype of tumors releasing interleukin-8. Clin Cancer Res 10: 4895–4900. [DOI] [PubMed] [Google Scholar]
- DeNardo DG, Brennan DJ, Rexhepaj E, Ruffell B, Shiao SL, Madden SF, Gallagher WM, Wadhwani N, Keil SD, Junaid SA, et al. 2011. Leukocyte complexity predicts breast cancer survival and functionally regulates response to chemotherapy. Cancer Discov 1: 54–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J, Le Mercier I, Kuta A, Noelle RJ. 2016. A New VISTA on combination therapy for negative checkpoint regulator blockade. J Immunother Cancer 4: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denny MF, Yalavarthi S, Zhao W, Thacker SG, Anderson M, Sandy AR, McCune WJ, Kaplan MJ. 2010. A distinct subset of proinflammatory neutrophils isolated from patients with systemic lupus erythematosus induces vascular damage and synthesizes type I IFNs. J Immunol 184: 3284–3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Caro G, Marchesi F, Galdiero MR, Grizzi F. 2014. Immune mediators as potential diagnostic tools for colorectal cancer: From experimental rationale to early clinical evidence. Expert Rev Mol Diagn 14: 387–399. [DOI] [PubMed] [Google Scholar]
- Di Caro G, Cortese N, Castino GF, Grizzi F, Gavazzi F, Ridolfi C, Capretti G, Mineri R, Todoric J, Zerbi A, et al. 2016. Dual prognostic significance of tumour-associated macrophages in human pancreatic adenocarcinoma treated or untreated with chemotherapy. Gut 65: 1710–1720. [DOI] [PubMed] [Google Scholar]
- Donskov F. 2013. Immunomonitoring and prognostic relevance of neutrophils in clinical trials. Semin Cancer Biol 23: 200–207. [DOI] [PubMed] [Google Scholar]
- Droeser RA, Hirt C, Eppenberger-Castori S, Zlobec I, Viehl CT, Frey DM, Nebiker CA, Rosso R, Zuber M, Amicarella F, et al. 2013. High myeloperoxidase positive cell infiltration in colorectal cancer is an independent favorable prognostic factor. PloS ONE 8: e64814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumitru CA, Gholaman H, Trellakis S, Bruderek K, Dominas N, Gu X, Bankfalvi A, Whiteside TL, Lang S, Brandau S. 2011. Tumor-derived macrophage migration inhibitory factor modulates the biology of head and neck cancer cells via neutrophil activation. Int J Cancer 129: 859–869. [DOI] [PubMed] [Google Scholar]
- Dumitru CA, Fechner MK, Hoffmann TK, Lang S, Brandau S. 2012. A novel p38–MAPK signaling axis modulates neutrophil biology in head and neck cancer. J Leukoc Biol 91: 591–598. [DOI] [PubMed] [Google Scholar]
- Dumitru CA, Bankfalvi A, Gu X, Eberhardt WE, Zeidler R, Lang S, Brandau S. 2013. Neutrophils activate tumoral CORTACTIN to enhance progression of orohypopharynx carcinoma. Front Immunol 4: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. 2002. Cancer immunoediting: From immunosurveillance to tumor escape. Nat Immunol 3: 991–998. [DOI] [PubMed] [Google Scholar]
- Dvorak HF. 1986. Tumors: Wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 315: 1650–1659. [DOI] [PubMed] [Google Scholar]
- Eruslanov EB, Bhojnagarwala PS, Quatromoni JG, Stephen TL, Ranganathan A, Deshpande C, Akimova T, Vachani A, Litzky L, Hancock WW, et al. 2014. Tumor-associated neutrophils stimulate T cell responses in early-stage human lung cancer. J Clin Invest 124: 5466–5480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. 2017. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: A systematic review and meta-analysis. Breast Cancer Res 19: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati G, Ricevuti G, Edwards SW, Walker C, Dalton A, Rossi ML. 1999. Neutrophil infiltration into human gliomas. Acta Neuropathol 98: 349–354. [DOI] [PubMed] [Google Scholar]
- Fridlender ZG, Kapoor V, Buchlis G, Cheng G, Sun J, Wang LC, Singhal S, Snyder LA, Albelda SM. 2011. Monocyte chemoattractant protein-1 blockade inhibits lung cancer tumor growth by altering macrophage phenotype and activating CD8+ cells. Am J Respir Cell Mol Biol 44: 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridlender ZG, Sun J, Mishalian I, Singhal S, Cheng G, Kapoor V, Horng W, Fridlender G, Bayuh R, Worthen GS, et al. 2012. Transcriptomic analysis comparing tumor-associated neutrophils with granulocytic myeloid-derived suppressor cells and normal neutrophils. PloS ONE 7: e31524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Nagaraj S. 2009. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 9: 162–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galdiero MR, Bonavita E, Barajon I, Garlanda C, Mantovani A, Jaillon S. 2013a. Tumor associated macrophages and neutrophils in cancer. Immunobiology 218: 1402–1410. [DOI] [PubMed] [Google Scholar]
- Galdiero MR, Garlanda C, Jaillon S, Marone G, Mantovani A. 2013b. Tumor associated macrophages and neutrophils in tumor progression. J Cell Physio 228: 1404–1412. [DOI] [PubMed] [Google Scholar]
- Galdiero MR, Bianchi P, Grizzi F, Di Caro G, Basso G, Ponzetta A, Bonavita E, Barbagallo M, Tartari S, Polentarutti N, et al. 2016. Occurrence and significance of tumor-associated neutrophils in patients with colorectal cancer. Int J Cancer 139: 446–456. [DOI] [PubMed] [Google Scholar]
- Galluzzi L, Senovilla L, Zitvogel L, Kroemer G. 2012. The secret ally: Immunostimulation by anticancer drugs. Nat Rev Drug Discov 11: 215–233. [DOI] [PubMed] [Google Scholar]
- Germano G, Frapolli R, Simone M, Tavecchio M, Erba E, Pesce S, Pasqualini F, Grosso F, Sanfilippo R, Casali PG, et al. 2010. Antitumor and anti-inflammatory effects of trabectedin on human myxoid liposarcoma cells. Cancer Res 70: 2235–2244. [DOI] [PubMed] [Google Scholar]
- Ginestier C, Liu S, Diebel ME, Korkaya H, Luo M, Brown M, Wicinski J, Cabaud O, Charafe-Jauffret E, Birnbaum D, et al. 2010. CXCR1 blockade selectively targets human breast cancer stem cells in vitro and in xenografts. J Clin Invest 120: 485–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginhoux F, Schultze JL, Murray PJ, Ochando J, Biswas SK. 2016. New insights into the multidimensional concept of macrophage ontogeny, activation and function. Nat Immunol 17: 34–40. [DOI] [PubMed] [Google Scholar]
- Gokce MI, Tangal S, Hamidi N, Suer E, Ibis MA, Beduk Y. 2016. Role of neutrophil-to-lymphocyte ratio in prediction of Gleason score upgrading and disease upstaging in low-risk prostate cancer patients eligible for active surveillance. Can Urol Assoc J 10: E383–E387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granata F, Frattini A, Loffredo S, Staiano RI, Petraroli A, Ribatti D, Oslund R, Gelb MH, Lambeau G, Marone G, et al. 2010. Production of vascular endothelial growth factors from human lung macrophages induced by group IIA and group X secreted phospholipases A2. J Immunol 184: 5232–5241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granja S, Tavares-Valente D, Queiros O, Baltazar F. 2017. Value of pH regulators in the diagnosis, prognosis and treatment of cancer. Semin Cancer Biol 10.1016/j.semcancer.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Granot Z, Jablonska J. 2015. Distinct functions of neutrophil in cancer and its regulation. Mediators Inflamm 2015: 701067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granot Z, Henke E, Comen EA, King TA, Norton L, Benezra R. 2011. Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell 20: 300–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M. 2010. Immunity, inflammation, and cancer. Cell 140: 883–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse-Steffen T, Giese T, Giese N, Longerich T, Schirmacher P, Hansch GM, Gaida MM. 2012. Epithelial-to-mesenchymal transition in pancreatic ductal adenocarcinoma and pancreatic tumor cell lines: The role of neutrophils and neutrophil-derived elastase. Clin Dev Immunol 2012: 720768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gungor N, Knaapen AM, Munnia A, Peluso M, Haenen GR, Chiu RK, Godschalk RW, van Schooten FJ. 2010. Genotoxic effects of neutrophils and hypochlorous acid. Mutagenesis 25: 149–154. [DOI] [PubMed] [Google Scholar]
- Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. 2013. The systemic inflammation-based neutrophil-lymphocyte ratio: Experience in patients with cancer. Crit Rev Oncol Hematol 88: 218–230. [DOI] [PubMed] [Google Scholar]
- Hanada T, Nakagawa M, Emoto A, Nomura T, Nasu N, Nomura Y. 2000. Prognostic value of tumor-associated macrophage count in human bladder cancer. Int J Urol 7: 263–269. [DOI] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. 2000. The hallmarks of cancer. Cell 100: 57–70. [DOI] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. 2011. Hallmarks of cancer: The next generation. Cell 144: 646–674. [DOI] [PubMed] [Google Scholar]
- Henze AT, Mazzone M. 2016. The impact of hypoxia on tumor-associated macrophages. J Clin Invest 126: 3672–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewish M, Lord CJ, Martin SA, Cunningham D, Ashworth A. 2010. Mismatch repair deficient colorectal cancer in the era of personalized treatment. Nat Rev Clin Oncol 7: 197–208. [DOI] [PubMed] [Google Scholar]
- Hotchkiss KA, Ashton AW, Klein RS, Lenzi ML, Zhu GH, Schwartz EL. 2003. Mechanisms by which tumor cells and monocytes expressing the angiogenic factor thymidine phosphorylase mediate human endothelial cell migration. Cancer Res 63: 527–533. [PubMed] [Google Scholar]
- Houghton AM, Rzymkiewicz DM, Ji H, Gregory AD, Egea EE, Metz HE, Stolz DB, Land SR, Marconcini LA, Kliment CR, et al. 2010. Neutrophil elastase-mediated degradation of IRS-1 accelerates lung tumor growth. Nat Med 16: 219–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes R, Qian BZ, Rowan C, Muthana M, Keklikoglou I, Olson OC, Tazzyman S, Danson S, Addison C, Clemons M, et al. 2015. Perivascular M2 macrophages stimulate tumor relapse after chemotherapy. Cancer Res 75: 3479–3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh SJ, Liang S, Sharma A, Dong C, Robertson GP. 2010. Transiently entrapped circulating tumor cells interact with neutrophils to facilitate lung metastasis development. Cancer Res 70: 6071–6082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ijichi H, Chytil A, Gorska AE, Aakre ME, Bierie B, Tada M, Mohri D, Miyabayashi K, Asaoka Y, Maeda S, et al. 2011. Inhibiting Cxcr2 disrupts tumor-stromal interactions and improves survival in a mouse model of pancreatic ductal adenocarcinoma. J Clin Invest 121: 4106–4117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y, Kubota Y, Yamamoto S, Tsuji K, Shimatani M, Shibatani N, Takamido S, Matsushita M, Okazaki K. 2005. Neutrophils enhance invasion activity of human cholangiocellular carcinoma and hepatocellular carcinoma cells: An in vitro study. J Gastroenterol Hepatol 20: 287–293. [DOI] [PubMed] [Google Scholar]
- Inada M, Yamashita J, Nakano S, Ogawa M. 1998. Complete inhibition of spontaneous pulmonary metastasis of human lung carcinoma cell line EBC-1 by a neutrophil elastase inhibitor (ONO-5046.Na). Anticancer Res 18: 885–890. [PubMed] [Google Scholar]
- Jablonska J, Leschner S, Westphal K, Lienenklaus S, Weiss S. 2010. Neutrophils responsive to endogenous IFN-β regulate tumor angiogenesis and growth in a mouse tumor model. J Clin Invest 120: 151–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson T, Clarke M, Steele CW, Samuel MS, Neumann J, Jung A, Huels D, Olson MF, Das S, Nibbs RJ, et al. 2012. Inhibition of CXCR2 profoundly suppresses inflammation-driven and spontaneous tumorigenesis. J Clin Invest 122: 3127–3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins SJ, Ruckerl D, Cook PC, Jones LH, Finkelman FD, van Rooijen N, MacDonald AS, Allen JE. 2011. Local macrophage proliferation, rather than recruitment from the blood, is a signature of TH2 inflammation. Science 332: 1284–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H. 2009. Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol 27: 4709–4717. [DOI] [PubMed] [Google Scholar]
- Kadokura M, Ishida Y, Tatsumi A, Takahashi E, Shindo H, Amemiya F, Takano S, Fukasawa M, Sato T, Enomoto N. 2016. Performance status and neutrophil-lymphocyte ratio are important prognostic factors in elderly patients with unresectable pancreatic cancer. J Gastrointest Oncol 7: 982–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane MP, Belperio JA, Xue YY, Burdick MD, Strieter RM. 2004. Depletion of CXCR2 inhibits tumor growth and angiogenesis in a murine model of lung cancer. J Immunol 172: 2853–2860. [DOI] [PubMed] [Google Scholar]
- Keeley EC, Mehrad B, Strieter RM. 2010. CXC chemokines in cancer angiogenesis and metastases. Adv Cancer Res 106: 91–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp TJ, Ludwig AT, Earel JK, Moore JM, Vanoosten RL, Moses B, Leidal K, Nauseef WM, Griffith TS. 2005. Neutrophil stimulation with Mycobacterium bovis bacillus Calmette–Guerin (BCG) results in the release of functional soluble TRAIL/Apo-2L. Blood 106: 3474–3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitamura T, Qian BZ, Soong D, Cassetta L, Noy R, Sugano G, Kato Y, Li J, Pollard JW. 2015. CCL2-induced chemokine cascade promotes breast cancer metastasis by enhancing retention of metastasis-associated macrophages. J Exp Med 212: 1043–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kridel R, Xerri L, Gelas-Dore B, Tan K, Feugier P, Vawda A, Canioni D, Farinha P, Boussetta S, Moccia AA, et al. 2015. The prognostic impact of CD163-positive macrophages in follicular lymphoma: A study from the BC Cancer Agency and the Lymphoma Study Association. Clin Cancer Res 21: 3428–3435. [DOI] [PubMed] [Google Scholar]
- Kryczek I, Wei S, Zou L, Zhu G, Mottram P, Xu H, Chen L, Zou W. 2006. Cutting edge: Induction of B7-H4 on APCs through IL-10: Novel suppressive mode for regulatory T cells. J Immunol 177: 40–44. [DOI] [PubMed] [Google Scholar]
- Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu Z, Yin XY, Zheng L. 2011. Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol 54: 948–955. [DOI] [PubMed] [Google Scholar]
- Lazennec G, Richmond A. 2010. Chemokines and chemokine receptors: New insights into cancer-related inflammation. Trends Mol Med 16: 133–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifler KS, Svensson S, Abrahamsson A, Bendrik C, Robertson J, Gauldie J, Olsson AK, Dabrosin C. 2013. Inflammation induced by MMP-9 enhances tumor regression of experimental breast cancer. J Immunol 190: 4420–4430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J, Nagahashi M, Kim EY, Harikumar KB, Yamada A, Huang WC, Hait NC, Allegood JC, Price MM, Avni D, et al. 2013. Sphingosine-1-phosphate links persistent STAT3 activation, chronic intestinal inflammation, and development of colitis-associated cancer. Cancer Cell 23: 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori M, Buracchi C, Pasqualini F, Bergomas F, Pesce S, Sironi M, Grizzi F, Mantovani A, Belgiovine C, Allavena P. 2016. Functional TRAIL receptors in monocytes and tumor-associated macrophages: A possible targeting pathway in the tumor microenvironment. Oncotarget 7: 41662–41676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loberg RD, Ying C, Craig M, Day LL, Sargent E, Neeley C, Wojno K, Snyder LA, Yan L, Pienta KJ. 2007. Targeting CCL2 with systemic delivery of neutralizing antibodies induces prostate cancer tumor regression in vivo. Cancer Res 67: 9417–9424. [DOI] [PubMed] [Google Scholar]
- Lu X, Kang Y. 2009. Chemokine (C-C motif) ligand 2 engages CCR2+ stromal cells of monocytic origin to promote breast cancer metastasis to lung and bone. J Biol Chem 284: 29087–29096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund AW, Medler TR, Leachman SA, Coussens LM. 2016. Lymphatic vessels, inflammation, and immunity in skin cancer. Cancer Discov 6: 22–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutgens E, de Muinck ED, Kitslaar PJ, Tordoir JH, Wellens HJ, Daemen MJ. 1999. Biphasic pattern of cell turnover characterizes the progression from fatty streaks to ruptured human atherosclerotic plaques. Cardiovasc Res 41: 473–479. [DOI] [PubMed] [Google Scholar]
- Ma Y, Adjemian S, Mattarollo SR, Yamazaki T, Aymeric L, Yang H, Portela Catani JP, Hannani D, Duret H, Steegh K, et al. 2013. Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity 38: 729–741. [DOI] [PubMed] [Google Scholar]
- Manthey CL, Johnson DL, Illig CR, Tuman RW, Zhou Z, Baker JF, Chaikin MA, Donatelli RR, Franks CF, Zeng L, et al. 2009. JNJ-28312141, a novel orally active colony-stimulating factor-1 receptor/FMS-related receptor tyrosine kinase-3 receptor tyrosine kinase inhibitor with potential utility in solid tumors, bone metastases, and acute myeloid leukemia. Mol Cancer Ther 8: 3151–3161. [DOI] [PubMed] [Google Scholar]
- Mantovani A. 2009. The yin-yang of tumor-associated neutrophils. Cancer Cell 16: 173–174. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. 2002. Macrophage polarization: Tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 23: 549–555. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Allavena P, Sica A, Balkwill F. 2008. Cancer-related inflammation. Nature 454: 436–444. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Cassatella MA, Costantini C, Jaillon S. 2011. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol 11: 519–531. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Biswas SK, Galdiero MR, Sica A, Locati M. 2013. Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol 229: 176–185. [DOI] [PubMed] [Google Scholar]
- Matsui A, Yokoo H, Negishi Y, Endo-Takahashi Y, Chun NA, Kadouchi I, Suzuki R, Maruyama K, Aramaki Y, Semba K, et al. 2012. CXCL17 expression by tumor cells recruits CD11b+Gr1 high F4/80− cells and promotes tumor progression. PloS ONE 7: e44080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishalian I, Granot Z, Fridlender ZG. 2017. The diversity of circulating neutrophils in cancer. Immunobiology 222: 82–88. [DOI] [PubMed] [Google Scholar]
- Mittendorf EA, Alatrash G, Qiao N, Wu Y, Sukhumalchandra P, St John LS, Philips AV, Xiao H, Zhang M, Ruisaard K, et al. 2012. Breast cancer cell uptake of the inflammatory mediator neutrophil elastase triggers an anticancer adaptive immune response. Cancer Res 72: 3153–3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moisan F, Francisco EB, Brozovic A, Duran GE, Wang YC, Chaturvedi S, Seetharam S, Snyder LA, Doshi P, Sikic BI. 2014. Enhancement of paclitaxel and carboplatin therapies by CCL2 blockade in ovarian cancers. Mol Oncol 8: 1231–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Movahedi K, Laoui D, Gysemans C, Baeten M, Stange G, Van den Bossche J, Mack M, Pipeleers D, In't Veld P, De Baetselier P, et al. 2010. Different tumor microenvironments contain functionally distinct subsets of macrophages derived from Ly6Chigh monocytes. Cancer Res 70: 5728–5739. [DOI] [PubMed] [Google Scholar]
- Murdoch C, Muthana M, Coffelt SB, Lewis CE. 2008. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer 8: 618–631. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Yoshida N, Baba Y, Kosumi K, Uchihara T, Kiyozumi Y, Ohuchi M, Ishimoto T, Iwatsuki M, Sakamoto Y, et al. 2017. Elevated preoperative neutrophil-to-lymphocytes ratio predicts poor prognosis after esophagectomy in T1 esophageal cancer. Int J Clin Oncol 10.1007/s10147-017-100-5. [DOI] [PubMed] [Google Scholar]
- Nawa M, Osada S, Morimitsu K, Nonaka K, Futamura M, Kawaguchi Y, Yoshida K. 2012. Growth effect of neutrophil elastase on breast cancer: Favorable action of sivelestat and application to anti-HER2 therapy. Anticancer Res 32: 13–19. [PubMed] [Google Scholar]
- Nie W, Yu T, Sang Y, Gao X. 2017. Tumor-promoting effect of IL-23 in mammary cancer mediated by infiltration of M2 macrophages and neutrophils in tumor microenvironment. Biochem Biophys Res Commun 482: 1400–1406. [DOI] [PubMed] [Google Scholar]
- Noman MZ, Desantis G, Janji B, Hasmim M, Karray S, Dessen P, Bronte V, Chouaib S. 2014. PD-L1 is a novel direct target of HIF-1α, and its blockade under hypoxia enhanced MDSC-mediated T cell activation. J Exp Med 211: 781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noy R, Pollard JW. 2014. Tumor-associated macrophages: From mechanisms to therapy. Immunity 41: 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozawa H, Chiu C, Hanahan D. 2006. Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc Natl Acad Sci 103: 12493–12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno S, Inagawa H, Dhar DK, Fujii T, Ueda S, Tachibana M, Suzuki N, Inoue M, Soma G, Nagasue N. 2003. The degree of macrophage infiltration into the cancer cell nest is a significant predictor of survival in gastric cancer patients. Anticancer Res 23: 5015–5022. [PubMed] [Google Scholar]
- Peranzoni E, Zilio S, Marigo I, Dolcetti L, Zanovello P, Mandruzzato S, Bronte V. 2010. Myeloid-derived suppressor cell heterogeneity and subset definition. Curr Opin Immunol 22: 238–244. [DOI] [PubMed] [Google Scholar]
- Pienta KJ, Machiels JP, Schrijvers D, Alekseev B, Shkolnik M, Crabb SJ, Li S, Seetharam S, Puchalski TA, Takimoto C, et al. 2013. Phase 2 study of carlumab (CNTO 888), a human monoclonal antibody against CC-chemokine ligand 2 (CCL2), in metastatic castration-resistant prostate cancer. Invest New Drugs 31: 760–768. [DOI] [PubMed] [Google Scholar]
- Pyonteck SM, Akkari L, Schuhmacher AJ, Bowman RL, Sevenich L, Quail DF, Olson OC, Quick ML, Huse JT, Teijeiro V, et al. 2013. CSF-1R inhibition alters macrophage polarization and blocks glioma progression. Nat Med 19: 1264–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian BZ, Pollard JW. 2010. Macrophage diversity enhances tumor progression and metastasis. Cell 141: 39–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Queen MM, Ryan RE, Holzer RG, Keller-Peck CR, Jorcyk CL. 2005. Breast cancer cells stimulate neutrophils to produce oncostatin M: Potential implications for tumor progression. Cancer Res 65: 8896–8904. [DOI] [PubMed] [Google Scholar]
- Rao HL, Chen JW, Li M, Xiao YB, Fu J, Zeng YX, Cai MY, Xie D. 2012. Increased intratumoral neutrophil in colorectal carcinomas correlates closely with malignant phenotype and predicts patients’ adverse prognosis. PloS ONE 7: e30806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MD, Basturk O, Thirabanjasak D, Hruban RH, Klimstra DS, Bagci P, Altinel D, Adsay V. 2011. Tumor-infiltrating neutrophils in pancreatic neoplasia. Mod Pathol 24: 1612–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ries CH, Cannarile MA, Hoves S, Benz J, Wartha K, Runza V, Rey-Giraud F, Pradel LP, Feuerhake F, Klaman I, et al. 2014. Targeting tumor-associated macrophages with anti-CSF-1R antibody reveals a strategy for cancer therapy. Cancer Cell 25: 846–859. [DOI] [PubMed] [Google Scholar]
- Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, Figueiredo JL, Gorbatov R, Sukhova GK, Gerhardt LM, Smyth D, et al. 2013. Local proliferation dominates lesional macrophage accumulation in atherosclerosis. Nat Med 19: 1166–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC, Ernstoff MS, Hernandez C, Atkins M, Zabaleta J, Sierra R, Ochoa AC. 2009. Arginase I-producing myeloid-derived suppressor cells in renal cell carcinoma are a subpopulation of activated granulocytes. Cancer Res 69: 1553–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell B, Affara NI, Coussens LM. 2012. Differential macrophage programming in the tumor microenvironment. Trends Immunol 33: 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagiv JY, Michaeli J, Assi S, Mishalian I, Kisos H, Levy L, Damti P, Lumbroso D, Polyansky L, Sionov RV, et al. 2015. Phenotypic diversity and plasticity in circulating neutrophil subpopulations in cancer. Cell Rep 10: 562–573. [DOI] [PubMed] [Google Scholar]
- Sandhu SK, Papadopoulos K, Fong PC, Patnaik A, Messiou C, Olmos D, Wang G, Tromp BJ, Puchalski TA, Balkwill F, et al. 2013. A first-in-human, first-in-class, phase I study of carlumab (CNTO 888), a human monoclonal antibody against CC-chemokine ligand 2 in patients with solid tumors. Cancer Chemother Pharmacol 71: 1041–1050. [DOI] [PubMed] [Google Scholar]
- Scapini P, Morini M, Tecchio C, Minghelli S, Di Carlo E, Tanghetti E, Albini A, Lowell C, Berton G, Noonan DM, et al. 2004. CXCL1/macrophage inflammatory protein-2-induced angiogenesis in vivo is mediated by neutrophil-derived vascular endothelial growth factor-A. J Immunol 172: 5034–5040. [DOI] [PubMed] [Google Scholar]
- Schmidt T, Carmeliet P. 2010. Blood-vessel formation: Bridges that guide and unite. Nature 465: 697–699. [DOI] [PubMed] [Google Scholar]
- Schmielau J, Finn OJ. 2001. Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of T-cell function in advanced cancer patients. Cancer Res 61: 4756–4760. [PubMed] [Google Scholar]
- Serhan CN. 2010. Novel lipid mediators and resolution mechanisms in acute inflammation: To resolve or not? Am J Pathol 177: 1576–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P, Allison JP. 2015. The future of immune checkpoint therapy. Science 348: 56–61. [DOI] [PubMed] [Google Scholar]
- Shen J, Zhu Y, Wu W, Zhang L, Ju H, Fan Y, Zhu Y, Luo J, Liu P, Zhou N, et al. 2017. Prognostic role of neutrophil-to-lymphocyte ratio in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Med Sci Monit 23: 315–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojaei F, Wu X, Zhong C, Yu L, Liang XH, Yao J, Blanchard D, Bais C, Peale FV, van Bruggen N, et al. 2007. Bv8 regulates myeloid-cell-dependent tumour angiogenesis. Nature 450: 825–831. [DOI] [PubMed] [Google Scholar]
- Shojaei F, Singh M, Thompson JD, Ferrara N. 2008. Role of Bv8 in neutrophil-dependent angiogenesis in a transgenic model of cancer progression. Proc Natl Acad Sci 105: 2640–2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojaei F, Wu X, Qu X, Kowanetz M, Yu L, Tan M, Meng YG, Ferrara N. 2009. G-CSF-initiated myeloid cell mobilization and angiogenesis mediate tumor refractoriness to anti-VEGF therapy in mouse models. Proc Natl Acad Sci 106: 6742–6747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starcher B, O'Neal P, Granstein RD, Beissert S. 1996. Inhibition of neutrophil elastase suppresses the development of skin tumors in hairless mice. J Invest Dermatol 107: 159–163. [DOI] [PubMed] [Google Scholar]
- Stylianopoulos T, Martin JD, Chauhan VP, Jain SR, Diop-Frimpong B, Bardeesy N, Smith BL, Ferrone CR, Hornicek FJ, Boucher Y, et al. 2012. Causes, consequences, and remedies for growth-induced solid stress in murine and human tumors. Proc Natl Acad Sci 109: 15101–15108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Glynn DJ, Hodson LJ, Huo C, Britt K, Thompson EW, Woolford L, Evdokiou A, Pollard JW, Robertson SA, et al. 2017. CCL2-driven inflammation increases mammary gland stromal density and cancer susceptibility in a transgenic mouse model. Breast Cancer Res 19: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka H, Ito T, Kyo T, Kimura A. 2007. Treatment with IFNα in vivo up-regulates serum-soluble TNF-related apoptosis inducing ligand (sTRAIL) levels and TRAIL mRNA expressions in neutrophils in chronic myelogenous leukemia patients. Eur J Haematol 78: 389–398. [DOI] [PubMed] [Google Scholar]
- Tecchio C, Huber V, Scapini P, Calzetti F, Margotto D, Todeschini G, Pilla L, Martinelli G, Pizzolo G, Rivoltini L, et al. 2004. IFNα-stimulated neutrophils and monocytes release a soluble form of TNF-related apoptosis-inducing ligand (TRAIL/Apo-2 ligand) displaying apoptotic activity on leukemic cells. Blood 103: 3837–3844. [DOI] [PubMed] [Google Scholar]
- Trellakis S, Bruderek K, Dumitru CA, Gholaman H, Gu X, Bankfalvi A, Scherag A, Hutte J, Dominas N, Lehnerdt GF, et al. 2011a. Polymorphonuclear granulocytes in human head and neck cancer: Enhanced inflammatory activity, modulation by cancer cells and expansion in advanced disease. Int J Cancer 129: 2183–2193. [DOI] [PubMed] [Google Scholar]
- Trellakis S, Farjah H, Bruderek K, Dumitru CA, Hoffmann TK, Lang S, Brandau S. 2011b. Peripheral blood neutrophil granulocytes from patients with head and neck squamous cell carcinoma functionally differ from their counterparts in healthy donors. Int J Immunopathol Pharmacol 24: 683–693. [DOI] [PubMed] [Google Scholar]
- Varricchi G, Galdiero MR, Marone G, Granata F, Borriello F, Marone G. 2017. Controversial role of mast cells in skin cancers. Exp Dermatol 26: 11–17. [DOI] [PubMed] [Google Scholar]
- Wang L, Rubinstein R, Lines JL, Wasiuk A, Ahonen C, Guo Y, Lu LF, Gondek D, Wang Y, Fava RA, et al. 2011. VISTA, a novel mouse Ig superfamily ligand that negatively regulates T cell responses. J Exp Med 208: 577–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Hu W, Wang K, Yu J, Luo B, Luo G, Wang W, Wang H, Li J, Wen J. 2016a. Repertaxin, an inhibitor of the chemokine receptors CXCR1 and CXCR2, inhibits malignant behavior of human gastric cancer MKN45 cells in vitro and in vivo and enhances efficacy of 5-fluorouracil. Int J Oncol 48: 1341–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Heng X, Lu Y, Cai Z, Yi Q, Che F. 2016b. Could B7-H4 serve as a target to activate anti-cancer immunity? Int Immunopharmacol 38: 97–103. [DOI] [PubMed] [Google Scholar]
- Watanabe M, Kato J, Inoue I, Yoshimura N, Yoshida T, Mukoubayashi C, Deguchi H, Enomoto S, Ueda K, Maekita T, et al. 2012. Development of gastric cancer in nonatrophic stomach with highly active inflammation identified by serum levels of pepsinogen and Helicobacter pylori antibody together with endoscopic rugal hyperplastic gastritis. Int J Cancer 131: 2632–2642. [DOI] [PubMed] [Google Scholar]
- Weizman N, Krelin Y, Shabtay-Orbach A, Amit M, Binenbaum Y, Wong RJ, Gil Z. 2014. Macrophages mediate gemcitabine resistance of pancreatic adenocarcinoma by upregulating cytidine deaminase. Oncogene 33: 3812–3819. [DOI] [PubMed] [Google Scholar]
- Wislez M, Rabbe N, Marchal J, Milleron B, Crestani B, Mayaud C, Antoine M, Soler P, Cadranel J. 2003. Hepatocyte growth factor production by neutrophils infiltrating bronchioloalveolar subtype pulmonary adenocarcinoma: Role in tumor progression and death. Cancer Res 63: 1405–1412. [PubMed] [Google Scholar]
- Zhang QW, Liu L, Gong CY, Shi HS, Zeng YH, Wang XZ, Zhao YW, Wei YQ. 2012. Prognostic significance of tumor-associated macrophages in solid tumor: A meta-analysis of the literature. PloS ONE 7: e50946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Wang J, Wang W, Tian J, Yin K, Tang X, Ma J, Xu H, Wang S. 2016. IL-17A produced by peritoneal macrophages promote the accumulation and function of granulocytic myeloid-derived suppressor cells in the development of colitis-associated cancer. Tumour Biol 37: 15883–1589115891. [DOI] [PubMed] [Google Scholar]