Abstract
Background/Aims:
Despite the benefits of laparoscopic surgery, which is being performed with increasing frequency, complications that do not occur during laparotomy are sometimes encountered. Such complications commonly occur during the initial trocar insertion, making this a procedural step of critical importance.
Methods:
In 2002, we experienced, upon initial trocar insertion, a serious major vascular injury (MVI) that led to hemorrhagic shock, and we thus modified the conventional closed entry method to an approach that we have found to be safe. We began developing the method by first measuring, in a patient undergoing laparoscopic cystectomy, the distance between the inner surface of the abdominal wall and the anterior spine when the abdominal wall was lifted manually for trocar insertion and when it was lifted by other methods, and we determined which method provided the greatest distance. We then devised a new approach, summarized as follows: The umbilical ring is elevated with Kocher forceps. The umbilicus is everted, and the base is incised longitudinally. This allows penetration of the abdominal wall at its thinnest point, and it shortens the distance to the abdominal cavity. A bladeless trocar (Step trocar) is used to allow insertion of the Veress needle. We began applying the new entry technique in July 2002, and by December 2014, we had applied it to 9676 patients undergoing laparoscopic gynecology surgery.
Results:
All entries were performed successfully, and no MVI occurred. The umbilical incision often resulted in an umbilical deformity, but in a questionnaire-based survey, patients generally reported satisfaction with the cosmetic outcome.
Conclusion:
A current new approach provides safe outcome with a minor cosmetic problem.
Keywords: Closed laparoscopy, Laparoscopic myomectomy, Major vascular injury, Umbilical deformity
Introduction
With the development of peripheral devices and new laparoscopic techniques, the indications for laparoscopic surgery continue to expand. It is no longer an exaggeration to say that laparoscopic surgery has become the gold standard for many surgical procedures. However, complications that do not occur during laparotomy are being encountered with increasing frequency,1 and effective measures for avoiding these complications are being devised.
Complications associated with laparoscopic surgery commonly occur during the initial trocar insertion,2,3 making this a procedural step that requires maximum caution. Accordingly, various measures and medical devices have been developed to facilitate the initial trocar insertion. The closed entry method, during which a Veress needle is used and the primary trocar is inserted blindly, is reported to confer a high risk of major vascular injury (MVI) in the retroperitoneum.3,4 Such MVIs can be life-threatening and should be prevented by all possible means.
Laparoscopic surgery was introduced at our hospital in July 1993, and over the next 9 years, we applied the closed insertion method in a total of 2440 patients undergoing laparoscopic gynecologic surgery. In July 2002, however, we experienced a serious MVI that led to hemorrhagic shock, and consequently, we modified the conventional closed entry method to an approach that we believe is safer. Herein, we describe the investigation we undertook to develop the modified method, the method itself, and results we have obtained thus far. In addition, because use of our new method resulted in umbilical deformities in some cases, we also investigated, by means of a questionnaire, patients’ satisfaction with the resulting umbilical irregularity, and we report our findings herein.
Methods and results
Preliminary investigation
As noted above, we used the conventional trocar insertion method (Fig. 1A and B) in all cases of laparoscopic gynecologic surgery performed between July 1993 and June 2002. MVI occurred in 5 (0.02%) of the 2440 patients. The 5 patients were all relatively slim (mean body mass index [BMI] = 19.3 ± 0.8). Despite the fact that all 5 MVIs resolved spontaneously during the post-surgical follow-up period, their occurrence, especially the MVI leading to hemorrhagic shock, prompted us to find a means by which the first trocar can be inserted more safely, even in slim patients and regardless of the surgeon’s level of experience.
Fig. 1.
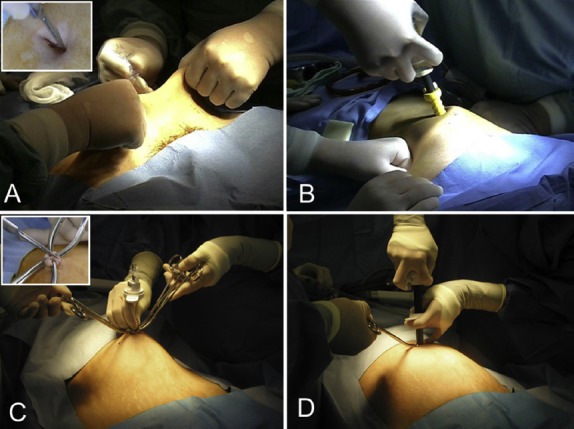
Conventional trocar insertion method and newly developed trocar insertion method. (A) When the conventional method is used, the skin is lifted manually, a Veress needle is inserted into the horizontal incision that has been made along the lower margin of the umbilical ring, and the abdomen is insufflated; (B) After removal of the Veress needle, the abdominal wall is pressed against from the left and right, and a “safety shielded trocar” is inserted. (C) When our new entry method is used, the umbilicus is lifted with Kocher forceps, and a Step Veress needle is inserted into the vertical incision that has been made at the base of the umbilicus; (D) After insufflation, the inner needle is removed, an 11-mm blunt-tip dilator is inserted to dilate the expandable sleeve, and the trocar is set in place.
Toward the development of a safe initial trocar insertion method, we first looked into ensuring an adequate space between the inner surface of the abdominal wall and the anterior surface of the lumbar spine where the retroperitoneal vessels reside. In a patient with a body mass index (BMI) of 19.9 and undergoing laparoscopic ovarian cystectomy and who provided informed consent, we measured the distance between the inner surface of the abdominal wall and the anterior surface of the lumbar spine when the abdominal wall was lifted manually for trocar insertion and also when the abdominal wall was lifted by other methods, and in so doing, we determined which method provides the greatest distance. We applied the 4-trocar method described by Roy et al,5 and we created a sterilized measuring device by attaching 1-cm-wide strips of vinyl tape at intervals of 1 cm to a cherry-tip dissector (Ethicon Co. Ltd., New Brunswick, NJ, USA). This device was inserted perpendicularly so that we could measure two distances: that between the upper surface of the abdominal wall and the anterior surface of the lumbar spine., and that between in inner surface of the abdominal wall and the anterior surface of the lumbar spine. After measuring the distance between the skin at the point of highest elevation and the surface of the lumbar spine before abdominal insufflation, we elevated the abdominal wall by 3 different methods (Fig. 2), and after each elevation, we performed an endoscopic examination via another trocar and measured the distance between the inner surface of the abdominal wall and the lumbar spine.
Fig. 2.
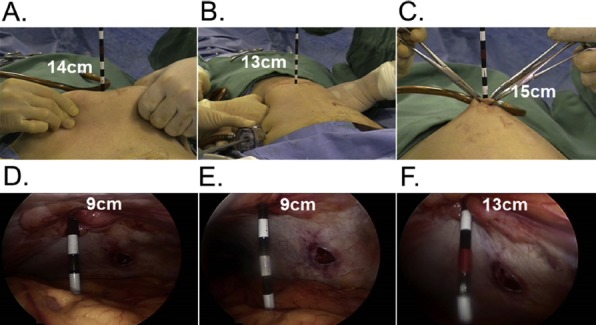
Preliminary study in which we measured distances from the abdominal wall to the anterior surface of the lumbar spine. We lifted the abdominal wall by 3 different methods: (A) by lifting the skin manually, (B) by pressing against the abdominal wall from the left and right after insufflation, (C) by lifting the umbilical ring with Kocher forceps. Measurements shown are taken from the external abdominal wall. (D, E, F) Corresponding measurements taken from the internal abdominal wall.
Results of our preliminary investigation
As shown in Table 1, by pinching the skin around the umbilicus for insertion of the insufflation needle or by compressing the skin on either side of the umbilicus for insertion of the trocar, we found that the abdominal wall is elevated very little. However, by grasping and elevating the umbilical ring with Kocher forceps, a distance of 13 cm between the inner surface of the abdominal wall and anterior surface of the lumbar spine is obtained, and the skin is elevated approximately 2 cm further. We also found that everting the umbilicus completely and incising the base of the umbilicus vertically allowed us to penetrate the abdominal wall at its thinnest point. This procedure also shortened the distance to the abdominal cavity.
Table 1.
Shortest distances from the abdominal wall to the anterior surface of the lumbar spine obtained in our preliminary study.
| A case of BMI = 19.9 | Conventional method | Lifting of the umbilicusc | |
|---|---|---|---|
| Veress needlea | Trocarb | ||
| External abdominal walld | 14 cm | 13 cm | 15 cm |
| Internal abdominal wall | 9 cm | 9 cm | 13 cm |
| External abdominal wall minus internal abdominal wall | 5 cm | 4 cm | 2 cm |
a Skin lifted manually.
b Abdominal wall pressure from the left and right after insufflation.
c Lifted with Kocher forceps.
d At the highest point on the skin.
Modified initial trocar insertion method
We devised a new closed entry method on the basis of these findings and now use the following technique for insertion of the first trocar: The umbilical ring is grasped with Kocher forceps, and the umbilicus is everted until its base is fully visible. A longitudinal incision is then made in the base of the umbilicus. After blunt dissection of the subcutaneous tissue, Kocher forceps are used to apply traction to the umbilical ring, and a radially expanding, bladeless Step trocar (Covidien, Minneapolis, MN, USA), used to facilitate introduction of the Veress needle, is inserted directly. The abdominal cavity is insufflated to 10 mmHg, the inner needle is removed, an 11-mm blunt-tip dilator is inserted to dilate the expandable sleeve, and the trocar is set in place (Fig. 1C and D). To avoid port-site hernia after wound closure, the tissues to the left and right of the fascia are sutured together, and 2–3 sutures are placed in the true dermis.
Application and outcomes of the modified closed entry technique
We began applying the modified closed entry technique in July 2002, and by December 2014, we had applied it to 9676 patients undergoing laparoscopic gynecology surgery at Juntendo University Hospital. For evaluation of the new entry method, we reviewed the records of all patients in whom it was applied. These patients were treated for benign gynecologic disorders, such as uterine fibroma, ovarian cyst, endometriosis, and adenomyosis. There were cases in which umbilical adhesions were anticipated, and in those cases, we entered the abdomen from a different site, but even when we approached from the ninth intercostal space6 and confirmed that umbilical adhesions were present, we used the elevation method described above for insertion of the Step trocar at the umbilicus. The new entry method is not difficult to learn. All 5 surgeons on our staff during the 2002–2014 study period performed a substantial number of the 9676 initial trocar insertions reported herein. Since we began using the new method, there have been no failed entry attempts, and we have not encountered an MVI. We found, however, that the vertical umbilical incision noted above often resulted in an umbilical deformity, a deformity that we do not encounter when we use a conventional horizontal incision along the lower margin of the umbilical ring.
Follow-up evaluation
Because of the umbilical deformities that occurred and the fact that the vertical incision is particular to our new entry method, we conducted a questionnaire-based survey regarding patients’ satisfaction with cosmetic outcomes. Patients surveyed were 177 women who, wishing to maintain their fertility, had undergone of 4-port laparoscopic myomectomy (LM) in the Department of Obstetrics and Gynecology, Juntendo University Hospital, between January 2013 and December 2014. Our new entry method was used in all 177 cases. The 177 women were those who had undergone second-look laparoscopy (SLL)7,8,9 6 months after LM. The SLL was performed in the Department of Gynecology, Asoka Hospital, one of our branch hospitals. We chose patients who underwent SLL because their visit to the department made it convenient for us to survey them. Before the SLL, the patients were shown diagrams (Fig. 3) representing possible shapes of the navel, and they were asked to indicate which shape most closely resembled the shape of their own navel after the surgery. The patients were also given a 4-item questionnaire, with 1 item that addressed the amount of pain the patient experienced in association with the LM and with the SLL. The remaining items addressed whether the postoperative appearance of the umbilicus resembled the preoperative appearance and the patient’s degree of satisfaction with the cosmetic outcome at the umbilicus. The questionnaire was completed by 69 of the 117 patients. We tabulated the responses anonymously. The questionnaire and its distribution were approved by the ethics committee of Asoka Hospital.
Fig. 3.
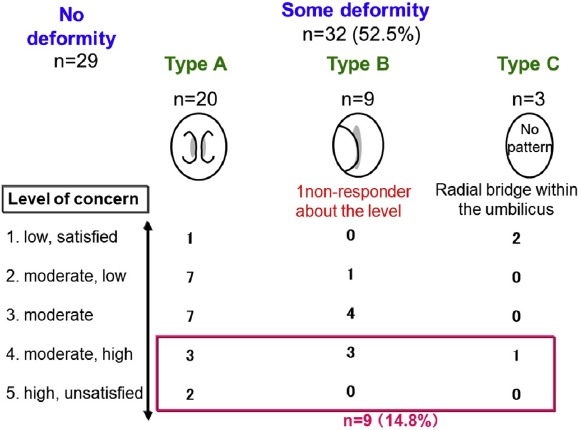
Diagrams shown to patients 6 months after laparoscopic myomectomy for self-evaluation of the umbilical scar. Survey period: January 2013–December 2014; 61 respondents, with 1 failing to mark the level of satisfaction. Type A deformity: Scaring at the midline. Type B deformity: Umbilical protrusion. The skin within the umbilicus protrudes. Type C: Atypical deformity.
Results of the follow-up investigation
Of the 69 questionnaire respondents, 61 answered questions about the postoperative umbilical appearance. Of these 61 patients, 29 (47.5%) reported that the postoperative umbilical appearance was the same as the preoperative appearance. Half of the 61 respondents (52.5%) reported that they had some kind of umbilical deformity (Fig. 3), with 20 (32.8%) reporting a central scar, 9 (14.8%) reporting an umbilical protrusion (acromphalus), and 3 (4.9%) reporting a radial bridge-like scar (Fig. 4). Of the 61 respondents, 9 (14.8%) reported that their wounds caused them moderately high (n = 7) or high concern (n = 2) (Fig. 3).
Fig. 4.
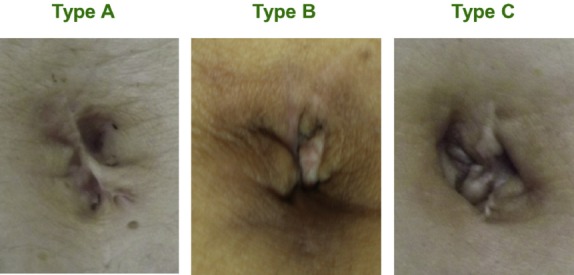
Actual examples of each type of umbilical deformity. Type A: Healing creates a central scar. Type B: Healing creates a protuberance (omphaloproptosis). Note that the umbilicus is collapsed and the skin protrudes. Type C: Healing is atypical, often resulting in a radial bridge-like scar.
Discussion
Major retroperitoneal vascular injury occurs during laparoscopic surgery at a reported frequency of 0.01–0.39%.10,11,12,13 We experienced retroperitoneal MVI at a frequency of 0.02%, which is within the reported range, but because retroperitoneal MVI is the most serious potential complication of gynecologic laparoscopic surgery and can be life threatening, we believe efforts should be undertaken to ensure that MVI does not occur at all. When MVI does occur, early detection and rapid conversion to laparotomy play an important role in the patient’s prognosis,10 but it is not uncommon for the diagnosis to be delayed because MVI is not usually accompanied by free intraperitoneal blood and because an expanding hematoma is not always recognized.14,15 The serious MVI we experienced before introducing our new trocar insertion method involved complete perforation of the left and right common iliac arteries and veins as well as injuries to the mesentery of the transverse colon and ileum. When repairing MVIs, surgeons should confirm that there are no other sites of injury; multiple MVIs are not uncommon,16,17 and sometimes there are injuries affecting both the anterior and posterior vessel walls.16,18,19 In addition, there are reported cases in which injudicious clamping of the vessels during repair has complicated the situation.15,18 In the case we experienced, we were able to diagnose the injury early and manage it appropriately, and we were fortunate to save the patient’s life.
Hurd et al performed a computed tomography (CT) analysis and found the mean distance between the bifurcation of the major vessels and the umbilicus to be 0.4 cm in non-obese women, 2.4 cm in overweight women, and 2.9 cm in obese women.20 The bifurcation of the major vessels is generally directly below the umbilicus or located somewhat caudally, but as BMI increases, the base of the umbilicus moves caudally away from the bifurcation, and the slimmer the individual, the closer the umbilicus is to the bifurcation of the major vessels, so caution is required during trocar insertion. In addition, Hurd et al reported a mean distance of 4 cm from the base of the umbilicus to the aorta (as measured on resting CT images) in non-obese women with a BMI < 25 kg/m2.21 In a patient in our department who underwent 3D-CT imaging for a genitourinary malformation, we found the distance from the base of the umbilicus to the aorta to be 3.5 cm; this patient’s height was 171 cm and weight was 57 kg (BMI = 19.4). Using 3D-CT, we confirmed that the bifurcation of the major vessels was below the umbilicus (Fig. 5). It is particularly important to ensure sufficient and effective elevation of the umbilicus, especially in slim patients. The traditional method involving manual lifting of the tissues around the umbilicus has been widely used.5,22 However, Roy et al reported using a method that involves grasping and elevating the umbilical ring. The mean maximum distance from the abdominal wall to the intra-abdominal organs, particularly the colon, was 6.8 cm when this method of trocar insertion was used,5 meaning that this amount of empty space must be created between the bowel and the abdominal wall simply to perform a puncture.
Fig. 5.
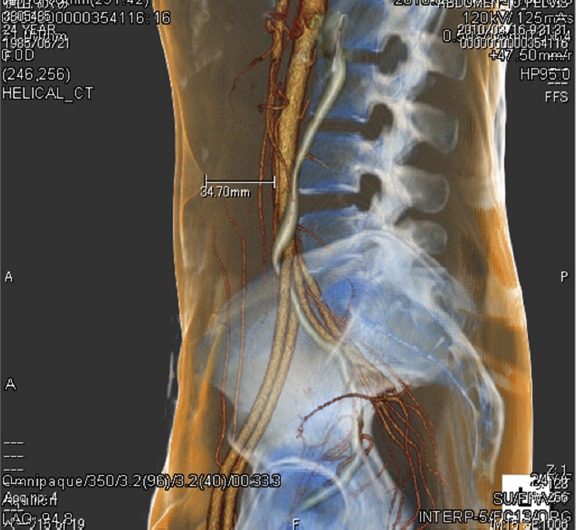
Three-dimensional computed tomography image obtained from a patient who was 171 cm in height and weighed 57 kg (BMI = 19.4).
The abdominal wall is thinnest at the base of the umbilicus, and there is not much subcutaneous adipose tissue, even in obese patients. Thus, trocar insertion methods involving incision of the base of the umbilicus and direct puncture have the advantage of little slippage, and the procedure is completed by accounting for the short distance between the skin and the intra-abdominal organs.5,21 In addition, in cases in which the base of the umbilicus is drawn inward,4 Kocher forceps can be used to firmly grasp the umbilical ring, making it easier to evert and expose the base of the umbilicus, thus making it possible to place the incision in the umbilical base with certainty.
Until recently, we have used a trocar known as a “safety shielded trocar,” which has a V-shaped flat linear blade tip and a spring-loaded blade shield, so the abdominal tissues are safeguarded when the trocar is not being used to puncture tissues. However, there is no evidence that shielded trocars reduce entry injuries,23 and, in September 1996, the United States Food and Drug Administration (FDA) advised that the term “safety shield” was inappropriate and that the trocars should be called “shielded cannulae.”16 We believe that it is important to use a “bladeless trocar,” that is, a trocar with no cutting blade, in addition to applying mechanical traction to the umbilical ring because it is still possible to come into contact with the intra-abdominal organs during trocar insertion. After traction is applied to the umbilical ring with Kocher forceps and the Step Veress insufflation needle (Covidien) is inserted, the inner needle is removed, and an 11-mm blunt-tip dilator is used to dilate the expandable sleeve, setting the trocar in place. With the Step trocar, there is no need for re-puncture after insufflation because it is left dilated and in place as a route for the insufflation needle. In addition, like other bladeless trocars, the Step trocar does not require any force or twisting to penetrate the peritoneum, so we believe it is safer than other types of trocars, with the exception of the Step trocar. VersaStep increases the procedural safety and can also reduce the time and pain associated with trocar insertion.24,25
In addition to the safety concerns that have arisen with the popularization of laparoscopic surgery, questions pertaining to wound cosmesis have emerged. The scar is noticeable when we use the closed method described herein, and we are starting to see umbilical deformities that were not seen when we used the conventional approach and made a horizontal incision in the umbilical ring. When an incision is made in the base of the umbilicus, the peritoneum and fascia on both sides are sutured during closure of the wound, but the epidermis, which has been elevated and rotated, does not easily bend inward. In our study patients, the incision was made for an 11-mm trocar, and it was commonly advanced through the surrounding subcutaneous tissues until the peritoneum or fascia was confirmed. We believe that the umbilical deformities result from residual skin, which, as a result of the suturing of deep layers, is hindered from inward return. However, results of our patient survey regarding umbilical deformities indicated that a midline scar extending vertically (Type A deformity) is more common than a protrusion (acromphalus) (Type B deformity). Despite the fact that sutures are placed perpendicularly to close the vertical incision, we know that the incisional scar shrinks in length, pulling on the surrounding tissues. We believe that atypical deformities, such as radial deformities (Type C deformity), occur when the residual skin contracts in several directions within the hollow of the umbilicus. Prevention is difficult. Fortunately, 2 of our 3 respondents with atypical scars indicated that they did not notice any deformity. Despite the fact that we have established a safe closed trocar insertion method, cosmesis after wound closure will present challenges going forward.
Conclusion
Due to technical advances in laparoscopic surgery, procedural steps once considered technically challenging can now be successfully managed, but this does not necessarily mean that vessel or even organ injury associated with adequate exposure will decrease in the future. It is important for surgeons to learn and adopt techniques aimed at avoiding complications. Although cosmetic challenges remain, our current method of initial entry, by which we insert a Step trocar via a longitudinal incision in the base of the everted umbilicus after applying traction to the umbilical ring, has thus far proven to be a fast, convenient, and safe insertion method.
Footnotes
Conflicts of interest statement: The authors have no conflicts of interest relevant to this article.
References
- 1.Peterson HB, Hulka JF, Phillips JM, Surrey MW. Laparoscopic sterilization. American Association of Gynecologic Laparoscopists' 1991 membership survey. J Reprod Med. 1993;38:574–576. [PubMed] [Google Scholar]
- 2.Munro MG. Laparoscopic access: complications, technologies and techniques. Curr Opin Obstet Gynecol. 2002;4:365–374. doi: 10.1097/00001703-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Nuzzo G, Giuliante F, Tebala GD, Vellone M, Cavicchioni C. Routine use of open technique in laparoscopic operations. J Am Coll Surg. 1997;184:58–62. [PubMed] [Google Scholar]
- 4.Bonjer HJ, Hazebroek EJ, Kazemier G, Giuffrida MC, Meijer WS, Lange JF. Open versus closed establishment of pneumoperitoneum in laparoscopy surgery. Br J Surg. 1997;84:599–602. [PubMed] [Google Scholar]
- 5.Roy GM, Bazzurini L, Solima E, Luciano AA. Safe technique for laparoscopic entry into the abdominal cavity. J Am Assoc Gynecol Laparosc. 2001;8:519–528. doi: 10.1016/s1074-3804(05)60614-7. [DOI] [PubMed] [Google Scholar]
- 6.Kumakiri J, Takeuchi H, Sato Y, et al. A novel method of ninth-intercostal microlaparoscopic approach for patients with previous laparotomy. Acta Obstet Gynecol Scand. 2006;85:977–981. doi: 10.1080/00016340600607065. [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kumakiri J, Takeda S. Influencing factors of adhesion development and the efficacy of adhesion-preventing agents in patients undergoing laparoscopic myomectomy as evaluated by a second-look laparoscopy. Fertil Steril. 2008;89:1247–1253. doi: 10.1016/j.fertnstert.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kumakiri J, Takeda S. Adhesionprevention effects of fibrin sealants after laparoscopic myomectomy as determined by second-look laparoscopy: a prospective, randomized, controlled study. J Reprod Med. 2005;50:571–577. [PubMed] [Google Scholar]
- 9.Kumakiri J, Kikuchi I, Kitade M, et al. Association between uterine repair at laparoscopic myomectomy and postoperative adhesions. Acta Obstet Gynecol Scand. 2012;91:331–337. doi: 10.1111/j.1600-0412.2011.01339.x. [DOI] [PubMed] [Google Scholar]
- 10.Saville LE, Woods MS. Laparoscopy and major retroperitoneal vascular injuries (MRVI) Surg Endosc. 1995;9:1096–1100. doi: 10.1007/BF00188995. [DOI] [PubMed] [Google Scholar]
- 11.Leng J, Lang J, Huang R, Liu Z, Sun D. Complications in laparoscopic gynecologic surgery. Chin Med Sci J. 2000;15:222–226. [PubMed] [Google Scholar]
- 12.Miranda CS, Carvajal AR. Complications of operative gynecological laparoscopy. JSLS. 2003;7:53–58. [PMC free article] [PubMed] [Google Scholar]
- 13.Härkki-Sieren P, Sjöberg J, Kurki T. Major complications of laparoscopy: a follow-up Finish study. Obstet Gynecol. 1999;9:94–98. [PubMed] [Google Scholar]
- 14.Hanney RM, Carmalt HL, Merrett N, Tait N. Use of the Hasson cannula producing major vascular injury at laparoscopy. Surg Endosc. 1999;13:1238–1240. doi: 10.1007/pl00009630. [DOI] [PubMed] [Google Scholar]
- 15.Seidman DS, Nasserbakht F, Nezhat F, Nezhat C, Nezhat C. Delayed recognition of iliac artery injury during laparoscopic surgery. Surg Endosc. 1996;10:1099–1101. doi: 10.1007/s004649900250. [DOI] [PubMed] [Google Scholar]
- 16.Soderstrom RM. Injuries to major blood vessels during endoscopy. J Am Assoc Gynecol Laparosc. 1997;4:395–398. doi: 10.1016/s1074-3804(05)80234-8. [DOI] [PubMed] [Google Scholar]
- 17.Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461–465. [PubMed] [Google Scholar]
- 18.Fruhwirth J, Koch G, Werkgartner G, Tesch NP. Vascular complications in minimally invasive surgery. Surg Laparosc Endosc. 1997;7:251–254. [PubMed] [Google Scholar]
- 19.Lantz PE, Smith JD. Fatal carbon dioxide embolism complicating attempted laparoscopic cholecystectomy: case report and literature review. J Forensic Sci. 1994;39:1468–1480. [PubMed] [Google Scholar]
- 20.Hurd WW, Bude RO, DeLancey JO, Pearl ML. The relationship of the umbilicus to the aortic bifurcation: implications for laparoscopic technique. Obstet Gynecol. 1992;80:48–51. [PubMed] [Google Scholar]
- 21.Hurd WH, Bude RO, DeLancey JO, Gauvin JM, Aisen AM. Abdominal wall characterization with magnetic resonance imaging and computed tomography. The effect of obesity on the laparoscopic approach. J Reprod Med. 1991;36:473–476. [PubMed] [Google Scholar]
- 22.Nezhat FR, Silfen SL, Evans D, Nezhat C. Comparison of direct insertion of disposable and standard reusable laparoscopic trocars and previous pneumoperitoneum with Veress needle. Obstet Gynecol. 1991;78:148–150. [PubMed] [Google Scholar]
- 23.Vilos GA, Ternamian A, Dempster J, Laberge PY The Society of Obstetricians and Gynaecologists of Canada. Laparoscopic entry: a review of techniques, technologies, and complications. J Obstet Gynaecol Can. 2007;29:433–465. doi: 10.1016/S1701-2163(16)35496-2. [DOI] [PubMed] [Google Scholar]
- 24.Yim SF, Yuen PM. Randomized double-masked comparison of radially expanding access device and conventional cutting tip trocar in laparoscopy. Obstet Gynecol. 2001;97:435–438. doi: 10.1016/s0029-7844(00)01156-x. [DOI] [PubMed] [Google Scholar]
- 25.Feste JR, Bojahr B, Turner DJ. Randomized trial comparing a radially expandable needle system with cutting trocars. JSLS. 2000;4:11–15. [PMC free article] [PubMed] [Google Scholar]


