Introduction
Heart failure (HF) is growing to a modern epidemic and despite advances in therapy, it still carries an ominous prognosis and a significant socioeconomic burden.1 Many novel agents that emerged as promising HF drugs failed to improve residual morbidity and mortality.2,3 Since developing and testing new agents has become increasingly costly,4 the concept of repurposing existing drugs for new indications has gained considerable importance.
Conceptually, comorbidities such as type 2 diabetes mellitus (T2DM), obesity or chronic kidney disease, all highly prevalent in HF populations, have shifted from being innocent bystanders to drivers of HF. This applies especially to HF with preserved ejection fraction (HFpEF), a phenotype that accounts for more than 50% of HF patients and for which no effective therapy exists thus far.5,6 In particular, the prevalence of T2DM, thereby its combination with HF is rapidly increasing, mainly due to the obesity epidemic.
Cardiovascular (CV) outcomes are addressed by an increasing number of clinical studies in T2DM, mainly as safety endpoints for anti-diabetic agents. Some of those drugs have beneficial CV effects independent of their glucose-lowering action. Consequently, anti-diabetic agents have gained interest for their potential repurposing in HF treatment. In this context, the Translational Research Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) organized a workshop on HF and T2DM, focusing on the pathophysiological and therapeutic aspects of this relationship. Here, we summarize the main points raised during this workshop, providing an overview of current evidence and open issues.
Clinical background
Epidemiology
Patients with HF have a four-fold higher prevalence of T2DM (20%) than patients without HF (4–6%),4,7 and this rises to 40% in T2DM patients hospitalized for HF.8,9 T2DM worsens prognosis for patients with HF with reduced ejection fraction (HFrEF), but even more with HFpEF, by increasing the risk of death and hospitalization.10 Patients with T2DM have a 75% higher risk of CV death or HF hospitalization compared with those without T2DM.11 Furthermore, the risk to develop HF is 2.5-fold increased for patients with T2DM12 and 1.7-fold for patients with impaired glucose tolerance (IGT) or insulin resistance13 compared with normal (non-diabetic) individuals, respectively. In T2DM patients who are older than 65 years, the coexistence of HF portends a 10-fold higher mortality risk.7 Thus, epidemiological evidence implies a bidirectional association between HF and T2DM (Figure 1), with one increasing the incidence and worsening the prognosis of the respective other.14
Figure 1.
Systemic interdependence of heart failure and type 2 diabetes mellitus. In heart failure, neuroendocrine activation alters haemodynamics and metabolism, predisposing to the development of diabetes through insulin resistance. In diabetes, hyperglycaemia induces macro- and microvascular dysfunction, and myocardial ischaemia and/or infarction bias towards systolic dysfunction (heart failure with reduced ejection fraction), while in the absence of ischaemia, diastolic dysfunction (heart failure with preserved ejection fraction) prevails through a combination of sarcomere stiffness and fibrosis. Inflammation is a key systemic factor that contributes to several of these processes. The specific points of intervention by glucose-lowering drugs are indicated (all have in common that they lowed hyperglycaemia). AGEs, advanced glycation end products; AMP, adenosine monophosphate; AMPK, AMP-kinase; DPP4/GLP1, DPP4-inhibitors/GLP-1 analogons; SGLT2, SGLT2-inhibitors.
Diabetic cardiomyopathy
Type 2 diabetes mellitus affects the heart through several mechanisms. Diabetic macroangiopathy causes coronary artery disease (CAD) and myocardial ischaemia. In addition, a distinct, ischaemia- and hypertension-independent cardiomyopathy was defined as diabetic cardiomyopathy, describing the direct effects of diabetes-associated metabolic alterations on myocardial function. Its diagnosis requires a history of long-standing and/or poorly controlled T2DM along with exclusion of significant coronary, hypertensive, valvular and/or congenital heart disease as well as of familial, viral, toxic, or infiltrative cardiomyopathy. As reviewed in more detail elsewhere,15 diabetic cardiomyopathy was initially described as a dilated, HFrEF-like phenotype occurring in diabetic patients with microvascular complications such as nephropathy and retinopathy. More recently, diabetic cardiomyopathy shifted towards a rather restrictive, HFpEF-like phenotype, occurring more commonly in obese women with poor glycaemic control.15 However, since it is difficult to study the cardiac phenotype of patients with diabetes without the confounding influence of any other risk factors, the epidemiological evidence for such diabetic cardiomyopathy requires more epidemiological, but also basic research.
Pathophysiology
Mechanisms related to diabetic cardiomyopathy
In HF, the coexistence of T2DM mainly aggravates left ventricular (LV) diastolic dysfunction by increasing LV stiffness and mass, without impairing global pump function.16,17 In diabetic patients, LV diastolic dysfunction correlates with fasting blood glucose, HbA1c levels and body mass index (BMI), all markers of insulin resistance.18 However, it is currently unresolved which factors drive the development of one or the other diabetic cardiomyopathy phenotype. The restrictive phenotype is more prevalent in patients with T2DM and obesity, while the dilated phenotype is more common in type 1 diabetes.15 Accordingly, hyperglycaemia, hyperinsulinaemia, and lipotoxicity may predispose more to the restrictive phenotype, while autoimmune processes rather favour the dilated phenotype.15 At the same time, the diverse pathogenetic origins of myocardial dysfunction and remodelling in HFpEF and HFrEF may also determine the development of diabetic cardiomyopathy into either the restrictive or the dilated phenotype, respectively (Figure 1).5,15 In HFpEF, endothelial dysfunction of the coronary microvasculature predominates, triggered by comorbidity-related inflammation, while in HFrEF, cardiomyocyte loss caused by ischaemia or toxic agents prevails.19 In addition, interstitial and perivascular myocardial fibrosis and increased production of advanced glycation end products (AGEs) increase collagen stiffness through cross-linking, enhancing diastolic dysfunction in diabetic cardiomyopathy (Figure 1).20 Fibrosis, although relevant to both phenotypes, appears more important in the dilated form.16
Changes in intracellular Ca2+ homeostasis are another hallmark of cardiac dysfunction in diabetes (Figure 1). Overall, the mechanisms of dysfunctional Ca2+ handling observed in diabetic mouse models resemble those in HFrEF, including decreased sarcoplasmic reticulum Ca2+ load and decreased amplitudes of cytosolic Ca2+ transients, but also elevated intracellular sodium (Na+).21,22 In HFrEF, severe alterations in cytosolic Na+ and Ca2+ handling have a negative impact on mitochondrial Ca2+ uptake, thereby the matching of ATP supply and demand and the regeneration of the anti-oxidative capacity, resulting in energetic deficit and oxidative stress.23 Whether dysregulated cytosolic and mitochondrial Na+ and Ca2+ handling contribute to the development of diabetic cardiomyopathy remains unclear in vivo, despite recent in vitro data pointing towards such mechanisms.21,22,24
A number of relevant mechanisms including derangement of myocardial energy substrates, insulin resistance and endothelial dysfunction, resulting from a series of underlying conditions and risk factors such as obesity, link T2DM, and myocardial dysfunction through inflammation, nutrient imbalance, and neurohormonal activation.25
Myocardial energy substrate
The normal heart mainly consumes free fatty acids (FFA; ∼70%) and glucose (∼30%) (Figure 2).26 It is, however, an ‘omnivore’ and can adapt its choice of fuels according to their availability. This metabolic flexibility is predominantly regulated by the ‘Randle cycle’, by which high circulating levels of glucose decrease rates of FFA oxidation and vice versa.27
Figure 2.
Cardiac metabolic alterations in heart failure. In heart failure, increased uptake of free fatty acids and glucose into the cytosol is uncoupled from mitochondrial uptake and oxidation of free fatty acid and pyruvate, respectively. This provokes accumulation of metabolic intermediates in the cytosol which can trigger lipo- and glucotoxicity. Instead, utilization of ketone bodies is increased in heart failure. Impaired overall substrate oxidation reduces Krebs cycle (TCA) activity, oxidizing electron donors NADH and FADH2 for the electron transport chain (ETC). This reduces metabolic flux through creatine kinase (CK), thereby the phosphocreatine (PCr) to ATP ratio. β-Ox., β-oxidation; CPT-1/2, carnitine palmitoyltransferase type 1/2; FA-CoA, fatty acyl-coenzyme A; FACS, fatty acyl-coenzyme A synthetase; FAT/CD36, fatty acid translocase; GLUT 1/4, glucose transporters 1/4; G6P, glucose-6-phosphate; PDH, pyruvate dehydrogenase complex; PPP, pentose phosphate pathway; Polyol P., Polyol pathway; TAG, triacylglycerol; UDPGlcNac, UDP-glycnacylation. Red arrows (↓↑) indicate the changes in heart failure.
In HF, uptake of glucose and FFA into cardiac myocytes is increased, while their further uptake and oxidation in mitochondria is decreased (Figure 2). This leads to accumulation of metabolic intermediates in the cytosol, inducing maladaptive signalling.26
In T2DM, increased FFA levels activate peroxisome proliferator-activated receptor (PPAR)-α, a nuclear receptor increasing transcripts of FFA metabolism, shifting substrate utilization towards FFA (Figure 3). Together with increasing insulin resistance, this minimizes glucose utilization and makes the heart metabolically less flexible.26,28
Figure 3.
Cardiac metabolic alterations in diabetes. In diabetes, strongly increased free fatty acid activate peroxisome proliferator-activated receptor α (PPARα), which up-regulates expression of genes involved in fatty acid (FA) oxidation. Increased FA oxidation shuts down glucose uptake and oxidation (insulin resistance), thereby blunts metabolic flexibility. Excessive FA are stored as triacylglycerol (TAG), which can mediate lipotoxicity. FA and reactive oxygen species (ROS) activate uncoupling protein 3 (UCP3), which makes ATP production less efficient. Abbreviations see legend of Figure 2.
The dominance of FFA utilization in diabetic hearts contributes to energetic inefficiency. First, FFA oxidation requires 11% more O2 per carbon unit than glucose oxidation. Second, FFA induce expression of mitochondrial uncoupling protein (UCP) 3 through PPAR-α,29 dissipating the mitochondrial proton gradient. This deteriorates ATP production efficiency, as more O2 is required for ATP synthesis, a process termed ‘mitochondrial uncoupling’ (Figure 3).30 A similar concept emerged for UCP2 and UCP3 in HF.31
In T2DM, nutritional supply accounts for elevated FFA and glucose plasma levels. Conversely, in HF, sympathetic activation promotes lipolysis and release of FFA from adipose tissue into the plasma (Figure 1). Elevated FFA plasma levels are associated with LV diastolic dysfunction, while their lowering improves diastolic function.32–34 Drugs that interfere with FFA utilization, thereby shift substrate utilization towards glucose, such as trimetazidine and perhexilline, (Figure 4), improve cardiac function in patients with ischaemic heart disease and/or HF, respectively.35,36
Figure 4.
Metabolic interventions in diabetes and heart failure. For details see text. DPP4/GLP1, DPP4-inhibitors/GLP-1 analogons; SGLT2, SGLT2-inhibitors.
Ketone bodies (mainly, D-beta-hydroxybutyrate) increase as a response to energy depletion or starvation, providing an alternative substrate for oxidative phosphorylation.37 Ketone bodies are not readily available from food, but produced in the liver by incomplete oxidation of FFA released from adipose tissue in response to fasting.38 The enzymes regulating ketone body metabolism are up-regulated in mice and humans with end-stage HF, while those regulating glucose and FFA metabolism are down-regulated (Figure 2).39–41 Accordingly, the failing heart oxidizes ketone bodies when metabolism of other energy substrates is impaired.42 However, whether enhanced ketone body metabolism is a cause, a consequence, a bystander or a compensating mechanism in HF is presently unknown.42 Furthermore, ketone bodies induce FFA uptake into adipocytes, therefore decreasing FFA in the circulation and in turn, increasing glucose uptake into myocytes, thus improving substrate provision and possibly energy production in the heart. A dietary increase in ketone bodies is difficult to accomplish and requires strict adherence to a high-fat and low-carbohydrate diet, the so called ‘ketogenic diet’. A synthetic ketone ester drink (ΔG®) that achieved 10-fold higher circulating D-β-hydroxybutyrate levels than any dietary approach43 improved physical performance and cognitive function in rats and humans.37,43,44 Furthermore, ΔG® reduced fasting lipid, HbA1c, fasting and postprandial glucose levels in T2DM patients as well as liver fat in obese subjects (Kieran Clarke, unpublished data); however, controlled trails are yet missing.
Insulin resistance in heart failure
Insulin resistance, the impaired ability of cells to take up glucose from the bloodstream in response to insulin, is associated with increased lipolysis, hepatic lipogenesis, and hepatic gluconeogenesis (Figure 1), thus increasing substrate supply to the heart.45 However, myocardial substrate overload decreases substrate oxidation, leading to metabolic maladaptation and myocardial dysfunction through lipo- and glucotoxicity (Figure 3).46 In this context, myocardial insulin resistance may even be an adaptive mechanism to ameliorate substrate overload,46,47 possibly explaining (at least to some extent) the adverse CV effects of tight glycaemic control with insulin and of some insulin-sensitizing agents such as the group of thiazolidinediones (TZD).46,48–51
Endothelial function
Diabetes is associated with endothelial dysfunction (Figure 1), disturbing endothelial-cardiomyocyte communication and vascular function.5,52 Intensified glucose control reduced diabetic microvascular complications but has less impact on macrovascular complications and HF in T2DM patients, indicating direct HF protective effects of anti-diabetic drugs on endothelial function independent of their glycaemic effects.53 A common mechanism of several anti-diabetic drugs is activation of phosphatidyl-inositol 3-kinase (PI3K), which controls the activity of endothelial nitric oxide synthase (eNOS) (Figure 4).
The drugs: anti-diabetic agents and the heart—mechanisms and evidence
Metformin
Metformin is the first-line drug for the treatment of T2DM, although its mechanisms of action have not yet been fully elucidated.54 Metformin inhibits respiratory chain enzymes (complex I) in mitochondria, hence decreasing ATP production with a parallel increase in AMP (Figure 4).55 This inhibits glucose synthesis from pyruvate, thereby reducing hepatocytes gluconeogenesis (Figure 1). Furthermore, increased AMP stimulates AMP-activated protein kinase (AMPK), which inhibits acetyl-CoA carboxylase, malonyl-CoA, lipid and cholesterol synthesis (Figure 1).54
In addition to its metabolic actions, metformin protects against myocardial ischaemia/reperfusion injury in animal models, limiting infarct size and attenuating post-ischaemic myocardial remodelling, irrespective of the presence of diabetes.56 These effects are mediated by AMPK and eNOS (Figure 4), adenosine release and prevention of mitochondrial permeability transition pore opening during reperfusion.57 Metformin also prevented HF progression in dogs through AMPK activation (Figure 4).58 Furthermore, metformin improves endothelial function in vivo by reducing superoxide production and increasing NO bioavailability (Figure 4). It also exerts anti-inflammatory effects in mammals independent of AMPK,59 while attenuating myocardial fibrosis.60 Interestingly, the anti-inflammatory action of metformin in humans was independent of the presence of T2DM.
In one randomized controlled trial (RCT), metformin reduced mortality and CV morbidity in T2DM patients,61 and positive outcomes confirmed by cohort studies and meta-analyses.62,63 While no prospective RCT with metformin in patients with T2DM and prevalent HF is available, a series of case–control- or cohort studies, systematic reviews and one meta-analysis showed that metformin (mono- or add-on-therapy) resulted in lower all-cause mortality, HF readmission and lower rates of lactic acidosis in diabetic patients with HF.64–69 Accordingly, metformin is recommended as first line therapy for the management of diabetes mellitus (DM) in patients with HF by the current ESC Guidelines (class IIa, level of evidence C).70
Reducing infarct size and preventing post-ischaemic myocardial dysfunction and remodelling could be a potential beneficial mechanism of metformin in diabetic patients that provides some ground for drug repurposing in non-diabetic individuals. However, with the exception of one retrospective analysis,71 coexistent metformin therapy was not associated with reduced infarct size or improved LV systolic or diastolic function in T2DM patients with ST-elevation myocardial infarction (STEMI).72–74 Although a prospective trial in diabetic and non-diabetic patients with STEMI is missing, short-term metformin pre-treatment did not limit myocardial injury in non-diabetic patients undergoing coronary artery bypass grafting.75 Lastly, the anti-inflammatory properties of metformin in non-diabetic HF could provide additional grounds for investigating the drug’s repurposing in non-diabetic individuals, given the recent CANTOS trial establishing proof-of-concept of inflammation as a target in CV disease.76
Main findings for metformin in T2DM and HF
Metformin is a first-line therapy for glycaemic control in T2DM patients, particularly those with HF.
Retrospective and cohort studies suggest reduced mortality and CV morbidity in DM patients with or without HF.
Clinical data do not support protection against ischaemia–reperfusion injury despite positive preclinical studies.
Open questions for metformin in T2DM and HF
What are the mechanisms supporting a beneficial effect in T2DM with HF?
How does metformin compare with newer anti-diabetic agents in T2DM with HF?
Does metformin during coronary reperfusion prevent HF in STEMI patients?
Glitazones (Thiazolidinediones)
Glitazones, or TZD, are insulin-sensitizing agents that activate the nuclear receptor PPAR-γ, a transcription factor that regulates multiple genes implicated in several metabolic pathways related to insulin sensitivity. These drugs improve glucose metabolism by increasing insulin sensitivity (Figures 1and4), thereby reducing hyperglycaemia and hyperinsulinaemia. The main effect of TZD is to shift FFA towards adipose tissue and away from other tissues, hence inducing a ‘lipid-steal’ effect that, in turn, improves glucose utilization. In addition, PPAR-γ agonists restore other metabolic derangements in insulin resistance and obesity by attenuating macrophage pro-inflammatory cytokine expression, adipocyte differentiation, and adipokine expression in adipocytes.77,78 Furthermore, PPAR-γ activation abrogates vasoconstriction and atherogenic effects of angiotensin II and improves eNOS-dependent vasodilation (Figures 1and4).79 Its activation may also exert anti-remodelling effects by inhibiting glucose-induced induction of TGFβ1 and TGFβ1-mediated fibronectin expression.80,81 PPARy activation with pioglitazone may improve diastolic function,82 and a recent meta-analysis suggests that TZD may protect against atrial fibrillation.83 Furthermore, TZD exert beneficial effects on endothelial function, as rosiglitazone AMPK-dependently stimulates NO synthesis (Figure 4), and glitazones improve endothelial function in non-diabetic individuals with CAD.84 However, PPAR-γ agonism also confers some adverse effects, as it causes Na+ and fluid retention and oedema, body weight increase and bone fractures (Figure 1).
Meta-analyses of TZD studies suggested that rosiglitazone conferred an increased risk of myocardial infarction and HF, with or without an increased risk of CV death.50,51,85–87 The latter was not replicated by the RECORD trial in T2DM patients without a history of HF,88 but HF occurrence did increase with rosiglitazone, leading the European Medicines Agency to recommend suspension of the drug’s license in 2010. In the PROactive trial in patients with T2DM and CAD, ischaemic stroke or peripheral arterial disease but not HF, pioglitazone actually reduced the composite endpoint of all-cause death, non-fatal myocardial infarction and non-fatal stroke.84 Here, the drug increased the risk of episodes of HF worsening, but the decrease in the composite endpoint was maintained in severe HF patients.84,89 The differential clinical outcome of rosiglitazone and pioglitazone may reflect their aforementioned differential effects on lipid metabolism. In a meta-analysis, pioglitazone even increased the risk of HF, without, however, an increase in the composite endpoint of death, myocardial infarction or stroke.49,87 These findings lead to the concept that HF worsening was a class effect of TZD.90 In this context, the ESC Guidelines for HF state that TZD are contraindicated for the treatment of T2DM in patients with HF (class III, level of evidence A).70
Fluid retention by TZD is central in the pathophysiology of drug-induced hospitalizations for HF worsening, as the prevalence of oedema with TZD increases. Combined action of PPAR-γ activation in kidneys and the vasculature, including increased Na+ and water retention in distal tubules, arterial vasodilatation, and increased vascular volume capacity and capillary permeability may underlie these clinical observations.79 In this context, the observed effect of the drug might have been simple fluid retention and not true HF in the PROactive trial.84,91 On the other hand, since insulin resistance may actually be an adaptive mechanism of the failing heart to resist substrate overload, insulin sensitization by TZD may be detrimental by increasing fuel supply.46
The clinical side effects of full PPARy agonism sparked interest in partial PPARy agonists. INT131 is the most advanced member of this novel class of selective PPARy modulators (SPPARM), which may provide similar glucose-lowering potential but less fluid retention. INT131 is currently evaluated in phase I and II clinical studies in diabetes.
Main findings for glitazones in T2DM and HF
PPARy activation confers benefits in metabolic signalling, vascular function, inflammation, fibrosis, and diastolic function in the diabetic heart.
PPARy activation by glitazones may cause fluid retention and worsening in HF.
Glitazones are not recommended in patients with pre-existing HF.
Pioglitazone reduces all-cause death, non-fatal myocardial infarction and non-fatal stroke, a benefit maintained in patients who experienced HF worsening.
Open questions for glitazones in T2DM and HF
What is the exact pathophysiology of glitazone-induced HF worsening (fluid retention, insulin sensitization with cardiac substrate overload)?
What is the value of partial PPARy activation, including the novel SPPARMs causing less fluid retention in diabetic HF?
Incretin-based therapies: Glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors
Glucagon-like peptide-1 receptor agonists
Incretins, i.e. glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) are intestinal hormones released in response to food intake and inflammatory stimuli.92,93 Activation of the GLP-1 receptor impacts the pancreas, stomach, and brain to accommodate food ingestion, including decreased gastric motility and appetite. Dipeptidyl peptidase-4 (DPP-4) breaks GLP-1 down to the inactive GLP-1 metabolite (9-36 amide).
Glucagon-like peptide-1 receptor agonists lower blood glucose by increasing insulin and decreasing glucagon release (Figure 1), while further decreasing body weight in T2DM patients.94–96 In animal models, GLP-1 receptor agonists reduced infarct size and improved cardiac function after ischaemia/reperfusion through pro-survival pathways such as PI3K, Akt, and ERK1/2 (Figure 4)97,98 and attenuated post-ischaemic LV remodelling by activating AMPK/eNOS/cGMP/PKG pathways.98,99 They also improved LV function in non-ischaemic HF models, such as anthracycline-induced cardiotoxicity, potentially by increasing myocardial glucose uptake.99,100 In another preclinical model, GLP-1 lowered blood pressure by atrial natriuretic peptide release, which was, however, not recapitulated in humans.101 GLP-1 and GLP-1 receptor agonists may also improve endothelial function by PI3K-induced eNOS activation (Figures 1and4).102
Some trials on GLP-1 receptor agonists yielded beneficial CV outcomes. The long-lasting and structurally related GLP-1-agonists liraglutide or semaglutide reduced CV death, non-fatal myocardial infarction or non-fatal stroke in high-risk T2DM patients, as shown by the LEADER and SUSTAIN-6 trials, respectively.95,96 In contrast, the short-acting lixisenatide (ELIXA) and the long-acting exenatide (EXSCEL) GLP-1 receptor agonists had neutral CV effects.103,104
The mechanisms for this differential response remain elusive.95,96,104,105 The beneficial CV outcomes provided by liraglutide and semaglutide occurred in high-risk T2DM patients with a history of CAD, ischaemic stroke, peripheral arterial disease, HF or kidney disease and therefore concern mostly secondary prevention.95,96 None of the GLP-1 receptor agonists improved HF outcomes in these populations, but rather increased heart rate by approximately 3 b.p.m.95,96,103,104 In addition, in the FIGHT and LIVE studies in patients with HFrEF with or without T2DM, liraglutide increased adverse CV events compared with placebo.106,107 Safety concerns were also raised for vildagliptin, but no increase in adverse CV events was confirmed by subsequent retrospective studies or meta-analyses.108,109 Ongoing RCTs with long-acting GLP-1 receptor agonists dulaglutide (REWIND, NCT01394952) and albiglutide (HARMONY outcomes, NCT0246551; both expected to report 2019) will provide further insights into their potential effect on CV outcome in high-risk patients with DM.
Interestingly, the first-in-class angiotensin receptor neprilysin inhibitor (ARNI) sacubitril/valsartan also lowered HbA1c in patients with HFrEF and T2DM.110 This effect may be mediated by GLP-1 enhancement through decreased metabolization by neutral endopeptidase, the target of sacubitril.110–112 However, the change in HbA1c and the composite primary outcome did not correlate in the seminal PARADIGM-HF trial.110
Dipeptidyl peptidase-4 inhibitors
Dipeptidyl peptidase-4 inhibitors lower blood glucose by increasing insulin and decreasing glucagon release (Figure 1) without decreasing body weight in T2DM patients.94–96 In diabetic mice, DPP-4 inhibition improved cardiac contractility after myocardial infarction and improved LV diastolic function,113,114 although another study failed to confirm those beneficial effects.115
In contrast to GLP-1 receptor agonists and despite the beneficial vascular effects of DPP-4 inhibitors in pre-clinical116 and clinical studies,117 RCTs with DPP-4 inhibitors were neutral regarding major adverse CV events at glucose equipoise.105,118,119 In the SAVOR-TIMI 53 trial, saxagliptin even increased the risk for HF hospitalization by 27% in patients with a history of CAD, ischaemic stroke, peripheral artery disease or CV risk factors.119 This was, however, neither the case for alogliptin in T2DM patients with a recent acute coronary syndrome (EXAMINE) nor with sitaglipitin in T2DM patients with a history of CAD, ischaemic stroke or peripheral artery disease (TECOS).105,120 A meta-analysis of RCTs revealed a non-significant 14% increased HF risk with DPP-4 inhibition, but with large heterogeneity between different substances.121 Nevertheless, the FDA added a HF warning for this class of drugs. Ongoing RCTs with linagliptin (CARMELINA and CAROLINA expected to report 2018 and 2019) will provide more evidences on safety of DPP-4 inhibitors in HF.
Main findings for Incretin-based therapies in T2DM and HF
Incretin-based therapies do not increase the risk of major adverse CV events (MACE).
In LEADER and SUSTAIN-6, GLP-1 receptor agonists reduced MACE.
Open questions for incretin-based therapies in T2DM and HF
Do incretin-based therapies prevent macrovascular events?
Are incretin-based therapies efficient in T2DM with HF?
What are the mechanisms of CV mortality reduction by long-acting GLP-1 receptor agonist liraglutide, and how can this affect patient selection?
Sodium glucose co-transporter 2 inhibitors
The sodium glucose co-transporter 2 (SGLT2) is located in the proximal renal tubule and accounts for 90% of glucose reabsorption.122 The remaining urinary glucose is reabsorbed by SGLT1, which is also expressed in the intestine and the heart. Inhibition of SGLT2 by empagliflozin, dapagliflozin, ertugliflozin, or canagliflozin (with the latter also featuring some SGLT1-inhibitory capacity) increases urinary glucose excretion, thereby urine volume.123 The concept of SGLT2-inhibition is different from other glucose-lowering strategies since glucose is removed from the ‘system’, thereby reducing total body and cellular glucose toxicity independent of insulin. The mode of action of SGLT2-inhibitors has metabolic and haemodynamic consequences.
Metabolic consequences
Besides reducing fasting and postprandial blood glucose levels, SGLT2-inhibitors decrease uric acid but increase glucagon, FFA, and ketone body (beta-hydroxybutyrate) levels (Figure 1). In addition, SGLT2 inhibition increases endogenous glucose production, which partly compensates glucose excretion, preventing hypoglycaemia.124,125 Through early diuretic and longer-term metabolic effects, SGLT2-inhibitors reduce body weight.123,126 In addition, SGLT2 inhibitors affect cardiac metabolism by changing myocardial substrate supply and by altering myocardial energy demand.125
Substrate supply: SGLT2 inhibitors decrease glucose and increase FFA and ketone bodies (Figure 4), thereby shifting myocardial substrate supply.125,127 In DM patients, SGLT2 inhibitors up-regulate ketone body levels and oxidation; ketone bodies may represent a more efficient metabolic substrate than lipids (but not glucose) as they liberate more energy per carbon unit (the ‘thrifty substrate hypothesis’; Figure 4).128 Furthermore, empagliflozin increases BCAA catabolism in T2DM,129 which is diminished in HF. Whether these actions are translated into clinically meaningful effects on the myocardium is presently unclear.130
Mitochondrial function: While the natriuretic effect of empagliflozin occurs only transiently at the onset of therapy,131 empagliflozin reduced [Na+]i in cardiac myocytes, presumably by inhibiting the Na+/H+ exchanger (NHE).132 This may increase mitochondrial Ca2+ by slowing mitochondrial Na+/Ca2+ exchange.132 In mitochondria, Ca2+ is required to match ATP supply to demand and regenerate the antioxidative capacity through Krebs cycle activation.23 In DM and HF, [Na+]i is elevated and causes energetic mismatch and oxidative stress.21,23 Therefore, empagliflozin may exert beneficial effects by preventing energetic mismatch and oxidative stress in cardiac myocytes by lowering [Na+]i (the ‘Na+ hypothesis’),24 which may also have consequences for preventing arrhythmias.133
Haemodynamic consequences
In the kidney, empagliflozin lowers intra-glomerular pressure through the ‘tubulo-glomerular feedback’ mechanism: due to increased Na+ concentrations at the macula densa, afferent arteriole vasoconstriction lowers glomerular pressure, thereby reducing albuminuria and conferring renal protection.134,135 The diuretic effect lowers blood pressure and the heart rate-blood pressure product as determinants of myocardial O2 consumption,136,137 thereby unloading the heart. Furthermore, this ameliorates arterial stiffness, decreases the aortic and carotid augmentation index as well as LV mass.138 Finally, anti-inflammatory and anti-oxidative properties were observed.139
In the EMPA-REG OUTCOME trial, empagliflozin reduced the composite primary endpoint of CV death, nonfatal myocardial infarction, and nonfatal stroke in type 2 DM patients with CV disease.126 This effect was driven by a 38% reduction in CV death, while empagliflozin also reduced all-cause death and HF hospitalizations. In particular, the risk of HF hospitalization was lowered by 35%, and this reduction reached 40% in patients with estimated glomerular filtration rate (eGFR) between 30 and 60 mL/min/1.73 m2 at baseline. The early separation of the curves in favour of empagliflozin and the unexpected action on HF hospitalizations suggest that the favourable effects of empagliflozin are mainly due to a reduction in HF-associated events. Although only 10% of patients in EMPA-REG had a history of HF at baseline, the beneficial effects on HF hospitalizations and CV death were consistent in patients with or without HF.140 Since mortality and hospitalization rates in the placebo group of the EMPA-REG OUTCOME trial were comparable to the rates in trials on patients with HFpEF,141 it may be speculated that a higher fraction of patients than the 10% had undiagnosed HF, and in particular, HFpEF. However, it seems plausible that by its mode of action, empagliflozin may also provide benefit in HFrEF patients, although this view was recently challenged.142 Empagliflozin slowed the progression of kidney disease and related events, including incident albuminuria, and incident or worsening nephropathy.143
Canagliflozin also reduced the primary endpoint of CV death, nonfatal myocardial infarction and nonfatal stroke in patients with T2DM at high CV risk vs. placebo in the CANVAS trial program, and—comparable to empagliflozin—also HF hospitalization.144 However, it did not reduce all-cause mortality, but increased the risk for amputation and bone fracture. The EMPA-REG OUTCOME trial, however, did not confirm such findings.145
Ongoing large studies evaluate the CV efficacy of dapagliflozin (DECLARE; expected to report 2018) and ertugliflozin (VERTIS CV; expected to report 2020) in patients with diabetes in a primary and secondary prevention setting. The effects on HF outcomes may be considered a class effect of SGLT2-inhibitors. Several new studies are underway, including two new trials with empagliflozin in HFrEF and HFpEF (EMPEROR-Reduced/Preserved) and one trial with dapagliflozin in HFrEF (DAPA-HF).146 Those trials will provide evidence on whether SGLT2-inhibitors may improve outcome in HF patients with or without DM.
Main findings for SGLT2-inhibitors in T2DM and HF
In EMPA-REG OUTCOME, empagliflozin reduced CV death and HF hospitalizations.
The favourable effect of empagliflozin occurred in patients with and without HF history.
Patients with renal impairment benefited from empagliflozin.
In CANVAS, canagliflozin also reduced HF hospitalization, suggesting a class-effect.
Open questions for SGLT2-inhibitors in T2DM and HF
What are the underlying mechanisms explaining the beneficial effect of SGLT2 inhibitors on HF hospitalization and CV mortality?
Is the protective effect of SGLT2 inhibitors on HF restricted to patients with T2DM or does it also apply to non-diabetic HF patients?
Which subgroup of T2DM patients has the greatest benefit from SGLT2-inhibitors?
Is the benefit maintained in T2DM patients without CV comorbidities or high CV risk?
Open issues and perspectives for future research
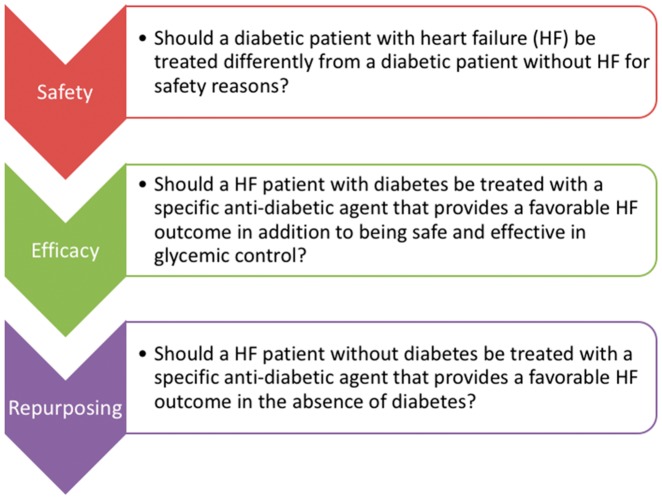
Knowledge on the CV safety of anti-diabetic drugs and in particular, their potential benefits for patients with HF is increasing (Table 1). The treatment of patients with HF and T2DM still remains challenging as many issues regarding the properties of anti-diabetic drugs in HF remain unresolved (Table 2). However, the recent benefits with GLP-1 receptor agonists and SGLT2-inhibitors re-spurred enthusiasm. Defining whether the favourable effects of specific anti-diabetic agents are preserved in patients with HF in the absence of T2DM is the next logical step towards the concept of drug repurposing (Figure 5). In this context, SGLT2-inhibitor trials designed to prove their efficiency rather than safety in patients with HF with or without T2DM are currently underway.
Table 1.
Effects of anti-diabetic agents on combined cardiovascular and heart failure endpoints according to key randomized trials (hazards ratio and 95% confidence intervals or percent of events in active treatment vs. placebo and P values)
| Drug class | Agent (trial) | Composite CV endpoints | Heart failure endpoints |
|---|---|---|---|
| Biguanides | Metformin | CV death, MI, HF, stroke | Not reported |
| (Meta-analysis; 35 trials)90 | 0.94 (0.82–1.07) | ||
| Glitazones (thiazolidinediones) | Pioglitazone | Death, MI, stroke | Any HF event |
| (PROactive; n = 5238)119 | 0.84 (0.72–0.98) | 11% vs. 8% (P < 0.0001) | |
| Rosiglitazone | CV death or hospital | HF death or hospital | |
| (RECORD; n = 4447)118 | 0.99 (0.85–1.16) | 2.10 (1.35–3.27) | |
| GLP-1 receptor agonists | Lixisenatide | CV death, MI, UA, stroke | HF hospital |
| (ELIXA; n = 6068)136 | 1.02 (0.89–1.17) | 0.96 (0.75–1.23) | |
| Liraglutide | CV death, MI, stroke | HF hospital | |
| (LEADER; n = 9340)127 | 0.87 (0.78–0.97) | 0.87 (0.73–1.05) | |
| Semaglutide | CV death, MI, stroke | HF hospital | |
| (SUSTAIN-6; n = 3297)126 | 0.74 (0.58–0.95) | 1.11 (0.77–1.61) | |
| Exenatide | CV death, MI, stroke | HF hospital | |
| (EXSCEL; n = 14752)137 | 0.91 (0.83–1.00) | 0.94 (0.78–1.13) | |
| DDP-4 inhibitors | Alogliptin | CV death, MI, stroke | Not reported |
| (EXAMINE; n = 5380)120 | 0.96 (≤1.16) | ||
| Saxagliptin | CV death, MI, stroke | HF hospital | |
| (SAVOR-TIMI 53; n = 16492)119 | 1.00 (0.89–1.12) | 1.27 (1.07–1.51) | |
| Sitagliptin | CV death, MI, UA, stroke | HF hospital | |
| (TECOS; n = 14671)105 | 0.98 (0.88–1.09) | 1.00 (0.83–1.20) | |
| SGLT2 inhibitors | Empagliflozin | CV death, MI, stroke | HF hospital |
| (EMPA-REG; n = 7020)126 | 0.86 (0.74–0.99) | 0.65 (0.50–0.85) | |
| Canagliflozin | CV death, MI, stroke | HF hospital | |
| (CANVAS; n = 10142)144 | 0.86 (0.75–0.97) | 0.67 (0.52–0.87) |
CV, cardiovascular; DDP-4, dipeptidyl peptidase-4; GLP-1, glucagon-like peptide-1; HF, heart failure; MI, myocardial infarction; SGLT2, sodium glucose co-transporter 2; UA, unstable angina.
Table 2.
Open issues and gaps of evidence regarding the co-treatment of diabetes mellitus and heart failure
| Open issue | Gaps in evidence |
|---|---|
| Insulin resistance and the failing heart | Role of insulin resistance as an adaptive mechanism in heart failure |
| Beneficial metabolic effects of ketone bodies | Myocardial glucose uptake and energy production in the presence of increased circulating ketone levels |
| Role of ketone metabolism in heart failure | |
| Clinical trials of the synthetic ketone ester Delta-G® in diabetic and non-diabetic patients with heart failure | |
| Pleiotropic effects of metformin | Prospective evidence on ischaemia/reperfusion injury in non-diabetic patients |
| Clinical effects of anti-inflammatory action | |
| Detrimental effects of glitazones | Pathophysiology of glitazone-induced heart failure |
| Differentiation between glitazone-induced heart failure and fluid retention | |
| Potential detrimental effects of insulin sensitization in the failing heart | |
| Evaluation of selective PPAR-gamma modulators to improve clinical efficacy and decrease side effects | |
| Cardiovascular effects of incretin-based therapies | Effect of insulin increase in the failing heart |
| Relevance of the GLP-1 receptor agonism in cardioprotection; signalling pathways of GLP-1 metabolite (9–36 amide) | |
| Cardiovascular outcomes of liraglutide and semaglutide in primary prevention setting (diabetic patients without cardiovascular disease) | |
| Cardiovascular outcomes of liraglutide and semaglutide in non-diabetic patients | |
| Effects of GLP-1 receptor agonists left ventricular diastolic function | |
| Effects of GLP-1 receptor agonists on vascular endpoints (central pressures, arterial stiffness, endothelial function) and ventriculo-arterial coupling | |
| Cardioprotective effect of SGLT2 inhibitors | Effects of SGLT2 on myocardial substrate utilization, energy production and energy demand |
| Cardiovascular outcomes of gliflozins in primary prevention setting (T2DM patients without cardiovascular disease) | |
| Cardiovascular outcomes of gliflozins in non-diabetic patients | |
| Heart failure phenotype | Effects of antidiabetic agents specifically on HFrEF and HFpEF |
GLP-1, glucagon-like peptide-1; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; PPAR, peroxisome proliferator-activated receptors; SGLT2, sodium glucose co-transporter 2.
Figure 5.
Basic concepts concerning the use of anti-diabetic drugs in patients with heart failure.
Understanding the pathophysiology of CV alterations in HF and T2DM is important. Key open questions include the relevance of insulin resistance in the failing heart (adaptive vs. maladaptive),47 the impact of substrate switch in response to SGLT2-inhibition, the role of SGLT2-inhibitors on cardiac Na+ metabolism and many others. Selection of proper preclinical models that reflect a specific HF phenotype is crucial as experimental results obtained by different models may not be comparable.
The CV effects of several anti-diabetic agents are not fully resolved. As patient populations recruited in large clinical trials are quite heterogeneous, this may prevent the detection of potential benefits. Identifying subpopulations of responding patients may be useful in guiding the design of future clinical trials.147
An important and yet under-investigated issue is the differential efficacy of anti-diabetic drugs in men and women. In two meta-analyses, diabetes was associated with a less favourable CV risk profile and a higher risk of death from CAD in females compared with males,148,149 while women also display a reduced response to low-dose aspirin.150,151 Emerging evidence suggests that treatment with glitazones may lower bone density, increasing the risk of fractures in diabetic women.
Therapy of T2DM often involves combination of anti-diabetic agents, but the additive or synergistic effects of combined drugs in HF remains to be investigated. For instance, metformin alone or in combination with sulfonylurea reduced CV morbidity and mortality compared with sulfonylurea monotherapy in T2DM with HF in a retrospective study,152 but this was not confirmed in a systemic review of observational studies.67
Finally, the selection of endpoints remains a crucial issue that was lately debated. ‘Hard’ endpoints, required for regulatory reasons, are suitable for large safety trials of anti-diabetic agents in broad CV populations, but impose large sample sizes and huge expenditures. Clinically relevant ‘soft’ or surrogate (patient-oriented) endpoints require smaller samples and considerably less costs and may be used in focused efficacy trials in selected subpopulations.
Acknowledgements
The authors would like to thank Dr Richard Carr and Dr Hans-Juergen Woerle for their contribution to this manuscript.
Funding
C.M. is supported by the Deutsche Forschungsgemeinschaft (DFG; SFB 894, TRR-219, and Ma 2528/7-1), the German Federal Ministry of Education and Science (BMBF; 01EO1504) and the Corona foundation. J.B. is supported by the DFG (SFB 1118) and the DZHK (German Centre for Cardiovascular Research) and by the BMBF. M.L. is supported by the DFG (SFB TRR 219M-03). R.B. is supported by the Netherlands Heart Foundation (CVON DOSIS 2014-40, CVON SHE-PREDICTS-HF 2017-21, and CVON RED-CVD 2017-11); and the Innovational Research Incentives Scheme program of the Netherlands Organization for Scientific Research (NWO VIDI, grant 917.13.350). N.M. is supported by the DFG (SFB TRR 219M-03, M-05). H.T. is supported by grants from the National Institutes of Health of the US Public Health Service (HL-RO1 061483 and HL-RO1 073162). A.B.G. was supported by grants from the Ministerio de Educación y Ciencia (SAF2014-59892; SAF2017-84324), Fundació La MARATÓ de TV3 (201502, 201516), CIBER Cardiovascular (CB16/11/00403), and AdvanceCat 2014-2020. H.B. is supported by the DFG (Bu2126/3-1). A.D.C. was supported by ‘FIL’ funds for research from University of Parma. A.G. was supported by grants from the European Union Commission’s FP7 programme (HOMAGE and FIBROTARGETS) and ERA-CVD Joint Transnational Call 2016 LYMIT-DIS. G.R. acknowledges recent funding from The Cunningham Trust, MRC (MR/K012924/1) and the Diabetes UK RW and JM Collins studentship. S.H. received funding from the European Union Commission’s Seventh Framework programme (2007-2013) under grant agreement N° 305507 (HOMAGE), N° 602904 (FIBROTARGETS) and N° 602156 (HECATOS). S.H. acknowledges the support from the Netherlands Cardiovascular Research Initiative: an initiative with support of the Dutch Heart Foundation, CVON-ARENA-PRIME, CVON-EARLY HFPEF, and SHE-PREDICTS. This research is co-financed as a PPP-allowance Research and Innovation by the Ministry of Economic Affairs within Top Sector Life sciences & Health.
Conflict of interest: C.M. serves as an advisor to Servier and received speaker honoraria from Servier, Boehringer Ingelheim, Bayer, Bristol Myers Squibb, Pfizer, Daiichi Sankyo, Novartis and Berlin Chemie. M.L. serves as an advisor to MSD, Boehringer Ingelheim, Novo Nordisk, Amgen and received speaker honoraria from MSD, Boehringer Ingelheim, Novo Nordisk, Amgen, Sanofi, Bayer, Lilly, Astra Zeneca. J.B. serves as an advisor to and received speaker honoraria from Bayer, Servier, Novartis, Boehringer Ingelheim, Bristol Myers Squibb, Pfizer, Daiichi Sankyo; he also received research support from Bayer. N.M. has served as a speaker for Amgen, Bayer, Boehringer Ingelheim, Sanofi-Aventis, MSD, BMS, AstraZeneca, Lilly, NovoNordisk; Bayer; as an advisor to Amgen, Bayer, Boehringer Ingelheim, Sanofi-Aventis, MSD, BMS, AstraZeneca, NovoNordisk, but declines all personal compensation from pharma or device companies. P.R. reports personal fees (consulting) from Novartis, Relypsa, AstraZeneca, Grünenthal, Stealth Peptides, Fresenius, Vifor Fresenius Medical Care Renal Pharma, Vifor and CTMA; lecture fees from Bayer and CVRx; cofounder of CardioRenal. K.C. is a director of TΔS Ltd, a company spun out of the University of Oxford to develop and commercialize products based on the science of ketone bodies in human nutrition. ADC received speaker honoraria from Boehringer Ingelheim, Eli Lilly, Novo Nordisk, DOC generic, MSD, AstraZeneca, Sanofi. A.R.L. serves as an advisor to Novartis, Servier, Stealth Peptides and Bristol Myers Squibb and received speaker honoraria from Novartis, Servier, Boehringer Ingelheim, AMGEN and Pfizer. MH has received speaker honoraria, advisory board fees and/or travel grants from Novartis, Roche Diagnostics, Pfizer, Vifor Pharma, Merck, Servier and BRAHMS. C.W. received honoraria of steering committee meetings and lecturing from Boehringer-Ingelheim and Genzyme-Sanofi. D.F. has received speaker honoraria, advisory board fees and/or travel grants from Novartis, Servier, Boehringer Ingelheim, Pfizer, Daiichi-Sankyo and Menarini. RB: the UMCG, which employs RB has received research grants and/or fees from AstraZeneca, Bristol-Myers Squibb, Novartis, Roche, Trevena and ThermoFisher GmbH; RB is a minority shareholder of scPharmaceuticals, Inc. and received personal fees from Novartis and Servier. All other authors declared no conflict of interest.
References
- 1. Farmakis D, Stafylas P, Giamouzis G, Maniadakis N, Parissis J.. The medical and socioeconomic burden of heart failure: a comparative delineation with cancer. Int J Cardiol 2016;203:279–281. [DOI] [PubMed] [Google Scholar]
- 2. Becher PM, Fluschnik N, Blankenberg S, Westermann D.. Challenging aspects of treatment strategies in heart failure with preserved ejection fraction: “Why did recent clinical trials fail?”. World J Cardiol 2015;7:544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Voors AA, van Veldhuisen DJ.. Why do drugs for acute heart failure fail? Eur J Heart Fail 2012;14:955–956. [DOI] [PubMed] [Google Scholar]
- 4. Lombardi C, Spigoni V, Gorga E, Dei Cas A.. Novel insight into the dangerous connection between diabetes and heart failure. Herz 2016;41:201–207. [DOI] [PubMed] [Google Scholar]
- 5. Paulus WJ, Tschope C.. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 2013;62:263–271. [DOI] [PubMed] [Google Scholar]
- 6. Mentz RJ, Kelly JP, von Lueder TG, Voors AA, Lam CS, Cowie MR, Kjeldsen K, Jankowska EA, Atar D, Butler J, Fiuzat M, Zannad F, Pitt B, O'Connor CM.. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 2014;64:2281–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bertoni AG, Hundley WG, Massing MW, Bonds DE, Burke GL, Goff DC Jr.. Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes Care 2004;27:699–703. [DOI] [PubMed] [Google Scholar]
- 8. Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CS, Sato N, Shah AN, Gheorghiade M.. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014;63:1123–1133. [DOI] [PubMed] [Google Scholar]
- 9. Greenberg BH, Abraham WT, Albert NM, Chiswell K, Clare R, Stough WG, Gheorghiade M, O'Connor CM, Sun JL, Yancy CW, Young JB, Fonarow GC.. Influence of diabetes on characteristics and outcomes in patients hospitalized with heart failure: a report from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). Am Heart J 2007;154:277 e1–278. [DOI] [PubMed] [Google Scholar]
- 10. Sarma S, Mentz RJ, Kwasny MJ, Fought AJ, Huffman M, Subacius H, Nodari S, Konstam M, Swedberg K, Maggioni AP, Zannad F, Bonow RO, Gheorghiade M; EVEREST investigators. Association between diabetes mellitus and post-discharge outcomes in patients hospitalized with heart failure: findings from the EVEREST trial. Eur J Heart Fail 2013;15:194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kristensen SL, Mogensen UM, Jhund PS, Petrie MC, Preiss D, Win S, Kober L, McKelvie RS, Zile MR, Anand IS, Komajda M, Gottdiener JS, Carson PE, McMurray JJ.. Clinical and echocardiographic characteristics and cardiovascular outcomes according to diabetes status in patients with heart failure and preserved ejection fraction: a report from the I-Preserve Trial (Irbesartan in Heart Failure With Preserved Ejection Fraction). Circulation 2017;135:724–735. [DOI] [PubMed] [Google Scholar]
- 12. Nichols GA, Gullion CM, Koro CE, Ephross SA, Brown JB.. The incidence of congestive heart failure in type 2 diabetes: an update. Diabetes Care 2004;27:1879–1884. [DOI] [PubMed] [Google Scholar]
- 13. Thrainsdottir IS, Aspelund T, Thorgeirsson G, Gudnason V, Hardarson T, Malmberg K, Sigurdsson G, Ryden L.. The association between glucose abnormalities and heart failure in the population-based Reykjavik study. Diabetes Care 2005;28:612–616. [DOI] [PubMed] [Google Scholar]
- 14. Dei Cas A, Fonarow GC, Gheorghiade M, Butler J.. Concomitant diabetes mellitus and heart failure. Curr Probl Cardiol 2015;40:7–43. [DOI] [PubMed] [Google Scholar]
- 15. Seferovic PM, Paulus WJ.. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Eur Heart J 2015;36:1718–1727, 1718–1727c. [DOI] [PubMed] [Google Scholar]
- 16. van Heerebeek L, Hamdani N, Handoko ML, Falcao-Pires I, Musters RJ, Kupreishvili K, Ijsselmuiden AJ, Schalkwijk CG, Bronzwaer JG, Diamant M, Borbely A, van der Velden J, Stienen GJ, Laarman GJ, Niessen HW, Paulus WJ.. Diastolic stiffness of the failing diabetic heart: importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation 2008;117:43–51. [DOI] [PubMed] [Google Scholar]
- 17. Falcao-Pires I, Hamdani N, Borbely A, Gavina C, Schalkwijk CG, van der Velden J, van Heerebeek L, Stienen GJ, Niessen HW, Leite-Moreira AF, Paulus WJ.. Diabetes mellitus worsens diastolic left ventricular dysfunction in aortic stenosis through altered myocardial structure and cardiomyocyte stiffness. Circulation 2011;124:1151–1159. [DOI] [PubMed] [Google Scholar]
- 18. Holzmann M, Olsson A, Johansson J, Jensen-Urstad M.. Left ventricular diastolic function is related to glucose in a middle-aged population. J Intern Med 2002;251:415–420. [DOI] [PubMed] [Google Scholar]
- 19. De Keulenaer GW, Brutsaert DL.. Systolic and diastolic heart failure are overlapping phenotypes within the heart failure spectrum. Circulation 2011;123:1996–2004; discussion 2005. [DOI] [PubMed] [Google Scholar]
- 20. Russo I, Frangogiannis NG.. Diabetes-associated cardiac fibrosis: cellular effectors, molecular mechanisms and therapeutic opportunities. J Mol Cell Cardiol 2016;90:84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lambert R, Srodulski S, Peng X, Margulies KB, Despa F, Despa S.. Intracellular Na+ concentration ([Na+]i) is elevated in diabetic hearts due to enhanced Na+-glucose cotransport. J Am Heart Assoc 2015;4:e002183.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pereira L, Ruiz-Hurtado G, Rueda A, Mercadier J-J, Benitah J-P, Gómez AM.. Calcium signaling in diabetic cardiomyocytes. Cell Calcium 2014;56:372–380. [DOI] [PubMed] [Google Scholar]
- 23. Bertero E, Maack C.. Calcium signaling and reactive oxygen species in mitochondria. Circ Res 2018;122:1460–1478. [DOI] [PubMed] [Google Scholar]
- 24. Bertero E, Roma L, Ameri P, Maack C.. Cardiac effects of SGLT2 inhibitors: the sodium hypothesis. Cardiovasc Res 2018;114:12–18. [DOI] [PubMed] [Google Scholar]
- 25. Gadde KM, Martin CK, Berthoud HR, Heymsfield SB.. Obesity: pathophysiology and management. J Am Coll Cardiol 2018;71:69–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bertero E, Maack C.. Metabolic remodeling in heart failure. Nat Rev Cardiol 2018; doi:10.1038/s41569-018-0044-6. [DOI] [PubMed] [Google Scholar]
- 27. Randle PJ, Garland PB, Hales CN, Newsholme EA.. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1963;1:785–789. [DOI] [PubMed] [Google Scholar]
- 28. Bugger H, Abel ED.. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia 2014;57:660–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Young ME, Patil S, Ying J, Depre C, Ahuja HS, Shipley GL, Stepkowski SM, Davies PJ, Taegtmeyer H.. Uncoupling protein 3 transcription is regulated by peroxisome proliferator-activated receptor (alpha) in the adult rodent heart. FASEB J 2001;15:833–845. [DOI] [PubMed] [Google Scholar]
- 30. Cadenas S. Mitochondrial uncoupling, ROS generation and cardioprotection. Biochim Biophys Acta 2018;1859:940–950. [DOI] [PubMed] [Google Scholar]
- 31. Murray AJ, Anderson RE, Watson GC, Radda GK, Clarke K.. Uncoupling proteins in human heart. Lancet 2004;364:1786–1788. [DOI] [PubMed] [Google Scholar]
- 32. Hammer S, van der Meer RW, Lamb HJ, Schar M, de Roos A, Smit JW, Romijn JA.. Progressive caloric restriction induces dose-dependent changes in myocardial triglyceride content and diastolic function in healthy men. J Clin Endocrinol Metab 2008;93:497–503. [DOI] [PubMed] [Google Scholar]
- 33. Leichman JG, Aguilar D, King TM, Vlada A, Reyes M, Taegtmeyer H.. Association of plasma free fatty acids and left ventricular diastolic function in patients with clinically severe obesity. Am J Clin Nutr 2006;84:336–341. [DOI] [PubMed] [Google Scholar]
- 34. Hammer S, Snel M, Lamb HJ, Jazet IM, van der Meer RW, Pijl H, Meinders EA, Romijn JA, de Roos A, Smit JW.. Prolonged caloric restriction in obese patients with type 2 diabetes mellitus decreases myocardial triglyceride content and improves myocardial function. J Am Coll Cardiol 2008;52:1006–1012. [DOI] [PubMed] [Google Scholar]
- 35. Lee L, Campbell R, Scheuermann-Freestone M, Taylor R, Gunaruwan P, Williams L, Ashrafian H, Horowitz J, Fraser AG, Clarke K, Frenneaux M.. Metabolic modulation with perhexiline in chronic heart failure: a randomized, controlled trial of short-term use of a novel treatment. Circulation 2005;112:3280–3288. [DOI] [PubMed] [Google Scholar]
- 36. Zhang L, Lu Y, Jiang H, Zhang L, Sun A, Zou Y, Ge J.. Additional use of trimetazidine in patients with chronic heart failure: a meta-analysis. J Am Coll Cardiol 2012;59:913–922. [DOI] [PubMed] [Google Scholar]
- 37. Cox PJ, Kirk T, Ashmore T, Willerton K, Evans R, Smith A, Murray AJ, Stubbs B, West J, McLure SW, King MT, Dodd MS, Holloway C, Neubauer S, Drawer S, Veech RL, Griffin JL, Clarke K.. Nutritional ketosis alters fuel preference and thereby endurance performance in athletes. Cell Metab 2016;24:256–268. [DOI] [PubMed] [Google Scholar]
- 38. Owen O. Ketone bodies as a fuel for the brain during starvation. Biochem Mol Biol Educ 2005;33:246–251. [Google Scholar]
- 39. Aubert G, Martin OJ, Horton JL, Lai L, Vega RB, Leone TC, Koves T, Gardell SJ, Kruger M, Hoppel CL, Lewandowski ED, Crawford PA, Muoio DM, Kelly DP.. The failing heart relies on ketone bodies as a fuel. Circulation 2016;133:698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bedi KC Jr, Snyder NW, Brandimarto J, Aziz M, Mesaros C, Worth AJ, Wang LL, Javaheri A, Blair IA, Margulies KB, Rame JE.. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation 2016;133:706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Razeghi P, Young ME, Alcorn JL, Moravec CS, Frazier OH, Taegtmeyer H.. Metabolic gene expression in fetal and failing human heart. Circulation 2001;104:2923–2931. [DOI] [PubMed] [Google Scholar]
- 42. Taegtmeyer H. Failing heart and starving brain: ketone bodies to the rescue. Circulation 2016;134:265–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Clarke K, Tchabanenko K, Pawlosky R, Carter E, Todd King M, Musa-Veloso K, Ho M, Roberts A, Robertson J, Vanitallie TB, Veech RL.. Kinetics, safety and tolerability of (R)-3-hydroxybutyl (R)-3-hydroxybutyrate in healthy adult subjects. Regul Toxicol Pharmacol 2012;63:401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Murray AJ, Knight NS, Cole MA, Cochlin LE, Carter E, Tchabanenko K, Pichulik T, Gulston MK, Atherton HJ, Schroeder MA, Deacon RM, Kashiwaya Y, King MT, Pawlosky R, Rawlins JN, Tyler DJ, Griffin JL, Robertson J, Veech RL, Clarke K.. Novel ketone diet enhances physical and cognitive performance. FASEB J 2016;30:4021–4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Taegtmeyer H, McNulty P, Young ME.. Adaptation and maladaptation of the heart in diabetes: part I: general concepts. Circulation 2002;105:1727–1733. [DOI] [PubMed] [Google Scholar]
- 46. Khalaf KI, Taegtmeyer H.. After avandia: the use of antidiabetic drugs in patients with heart failure. Tex Heart Inst J 2012;39:174–178. [PMC free article] [PubMed] [Google Scholar]
- 47. Taegtmeyer H, Beauloye C, Harmancey R, Hue L.. Insulin resistance protects the heart from fuel overload in dysregulated metabolic states. Am J Physiol Heart Circ Physiol 2013;305:H1693–H1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Aguilar D, Bozkurt B, Ramasubbu K, Deswal A.. Relationship of hemoglobin A1C and mortality in heart failure patients with diabetes. J Am Coll Cardiol 2009;54:422–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lincoff AM, Wolski K, Nicholls SJ, Nissen SE.. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA 2007;298:1180–1188. [DOI] [PubMed] [Google Scholar]
- 50. Nissen SE, Wolski K.. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 2007;356:2457–2471. [DOI] [PubMed] [Google Scholar]
- 51. Nissen SE, Wolski K.. Rosiglitazone revisited: an updated meta-analysis of risk for myocardial infarction and cardiovascular mortality. Arch Intern Med 2010;170:1191–1201. [DOI] [PubMed] [Google Scholar]
- 52. Lim SL, Lam CS, Segers VF, Brutsaert DL, De Keulenaer GW.. Cardiac endothelium-myocyte interaction: clinical opportunities for new heart failure therapies regardless of ejection fraction. Eur Heart J 2015;36:2050–2060. [DOI] [PubMed] [Google Scholar]
- 53. Eriksson L, Nystrom T.. Antidiabetic agents and endothelial dysfunction—beyond glucose control. Basic Clin Pharmacol Toxicol 2015;117:15–25. [DOI] [PubMed] [Google Scholar]
- 54. Rena G, Pearson ER, Sakamoto K.. Molecular mechanism of action of metformin: old or new insights? Diabetologia 2013;56:1898–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Owen MR, Doran E, Halestrap AP.. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem J 2000;348: 607–614. [PMC free article] [PubMed] [Google Scholar]
- 56. El Messaoudi S, Rongen GA, de Boer RA, Riksen NP.. The cardioprotective effects of metformin. Curr Opin Lipidol 2011;22:445–453. [DOI] [PubMed] [Google Scholar]
- 57. Calvert JW, Gundewar S, Jha S, Greer JJ, Bestermann WH, Tian R, Lefer DJ.. Acute metformin therapy confers cardioprotection against myocardial infarction via AMPK-eNOS-mediated signaling. Diabetes 2008;57:696–705. [DOI] [PubMed] [Google Scholar]
- 58. Sasaki H, Asanuma H, Fujita M, Takahama H, Wakeno M, Ito S, Ogai A, Asakura M, Kim J, Minamino T, Takashima S, Sanada S, Sugimachi M, Komamura K, Mochizuki N, Kitakaze M.. Metformin prevents progression of heart failure in dogs: role of AMP-activated protein kinase. Circulation 2009;119:2568–2577. [DOI] [PubMed] [Google Scholar]
- 59. Cameron AR, Morrison VL, Levin D, Mohan M, Forteath C, Beall C, McNeilly AD, Balfour DJ, Savinko T, Wong AK, Viollet B, Sakamoto K, Fagerholm SC, Foretz M, Lang CC, Rena G.. Anti-inflammatory effects of metformin irrespective of diabetes status. Circ Res 2016;119:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yin M, van der Horst ICC, van Melle JP, Qian C, van Gilst WH, Silljé HHW, de Boer RA.. Metformin improves cardiac function in a nondiabetic rat model of post-MI heart failure. Am J Physiol Heart Circ Physiol 2011;301:H459–H468. [DOI] [PubMed] [Google Scholar]
- 61. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865. [PubMed] [Google Scholar]
- 62. Evans JM, Ogston SA, Emslie-Smith A, Morris AD.. Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 2006;49:930–936. [DOI] [PubMed] [Google Scholar]
- 63. Lamanna C, Monami M, Marchionni N, Mannucci E.. Effect of metformin on cardiovascular events and mortality: a meta-analysis of randomized clinical trials. Diabetes Obes Metab 2011;13:221–228. [DOI] [PubMed] [Google Scholar]
- 64. Aguilar D, Chan W, Bozkurt B, Ramasubbu K, Deswal A.. Metformin use and mortality in ambulatory patients with diabetes and heart failure. Circ Heart Fail 2011;4:53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Crowley MJ, Diamantidis CJ, McDuffie JR, Cameron CB, Stanifer JW, Mock CK, Wang X, Tang S, Nagi A, Kosinski AS, Williams JW Jr.. Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart failure, or chronic liver disease: a systematic review. Ann Intern Med 2017;166:191–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Eurich DT, McAlister FA, Blackburn DF, Majumdar SR, Tsuyuki RT, Varney J, Johnson JA.. Benefits and harms of antidiabetic agents in patients with diabetes and heart failure: systematic review. BMJ 2007;335:497.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Eurich DT, Weir DL, Majumdar SR, Tsuyuki RT, Johnson JA, Tjosvold L, Vanderloo SE, McAlister FA.. Comparative safety and effectiveness of metformin in patients with diabetes mellitus and heart failure: systematic review of observational studies involving 34,000 patients. Circ Heart Fail 2013;6:395–402. [DOI] [PubMed] [Google Scholar]
- 68. MacDonald MR, Eurich DT, Majumdar SR, Lewsey JD, Bhagra S, Jhund PS, Petrie MC, McMurray JJ, Petrie JR, McAlister FA.. Treatment of type 2 diabetes and outcomes in patients with heart failure: a nested case-control study from the UK. General Practice Research Database. Diabetes Care 2010;33:1213–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Shah DD, Fonarow GC, Horwich TB.. Metformin therapy and outcomes in patients with advanced systolic heart failure and diabetes. J Card Fail 2010;16:200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891–975. [DOI] [PubMed] [Google Scholar]
- 71. Lexis CP, Wieringa WG, Hiemstra B, van Deursen VM, Lipsic E, van der Harst P, van Veldhuisen DJ, van der Horst IC.. Chronic metformin treatment is associated with reduced myocardial infarct size in diabetic patients with ST-segment elevation myocardial infarction. Cardiovasc Drugs Ther 2014;28:163–171. [DOI] [PubMed] [Google Scholar]
- 72. Al Ali L, Hartman MT, Lexis CP, Hummel YM, Lipsic E, van Melle JP, van Veldhuisen DJ, Voors AA, van der Horst IC, van der Harst P.. The effect of metformin on diastolic function in patients presenting with ST-elevation myocardial infarction. PLoS One 2016;11:e0168340.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Basnet S, Kozikowski A, Makaryus AN, Pekmezaris R, Zeltser R, Akerman M, Lesser M, Wolf-Klein G.. Metformin and myocardial injury in patients with diabetes and ST-segment elevation myocardial infarction: a propensity score matched analysis. J Am Heart Assoc 2015;4:e002314.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lexis CP, van der Horst IC, Lipsic E, Wieringa WG, de Boer RA, van den Heuvel AF, van der Werf HW, Schurer RA, Pundziute G, Tan ES, Nieuwland W, Willemsen HM, Dorhout B, Molmans BH, van der Horst-Schrivers AN, Wolffenbuttel BH, ter Horst GJ, van Rossum AC, Tijssen JG, Hillege HL, de Smet BJ, van der Harst P, van Veldhuisen DJ; Investigators G-I. Effect of metformin on left ventricular function after acute myocardial infarction in patients without diabetes: the GIPS-III randomized clinical trial. JAMA 2014;311:1526–1535. [DOI] [PubMed] [Google Scholar]
- 75. El Messaoudi S, Nederlof R, Zuurbier CJ, van Swieten HA, Pickkers P, Noyez L, Dieker HJ, Coenen MJ, Donders AR, Vos A, Rongen GA, Riksen NP.. Effect of metformin pretreatment on myocardial injury during coronary artery bypass surgery in patients without diabetes (MetCAB): a double-blind, randomised controlled trial. Lancet Diabetes Endocrinol 2015;3:615–623. [DOI] [PubMed] [Google Scholar]
- 76. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, Group CT.. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119–1131. [DOI] [PubMed] [Google Scholar]
- 77. Odegaard JI, Ricardo-Gonzalez RR, Goforth MH, Morel CR, Subramanian V, Mukundan L, Red Eagle A, Vats D, Brombacher F, Ferrante AW, Chawla A.. Macrophage-specific PPARgamma controls alternative activation and improves insulin resistance. Nature 2007;447:1116–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Sharma AM, Staels B.. Review: peroxisome proliferator-activated receptor gamma and adipose tissue–understanding obesity-related changes in regulation of lipid and glucose metabolism. J Clin Endocrinol Metab 2007;92:386–395. [DOI] [PubMed] [Google Scholar]
- 79. Goltsman I, Khoury EE, Winaver J, Abassi Z.. Does Thiazolidinedione therapy exacerbate fluid retention in congestive heart failure? Pharmacol Ther 2016;168:75–97. [DOI] [PubMed] [Google Scholar]
- 80. Derosa G, Cicero AF, Gaddi A, Ragonesi PD, Piccinni MN, Fogari E, Salvadeo S, Ciccarelli L, Fogari R.. A comparison of the effects of pioglitazone and rosiglitazone combined with glimepiride on prothrombotic state in type 2 diabetic patients with the metabolic syndrome. Diabetes Res Clin Pract 2005;69:5–13. [DOI] [PubMed] [Google Scholar]
- 81. Panchapakesan U, Sumual S, Pollock CA, Chen X.. PPARgamma agonists exert antifibrotic effects in renal tubular cells exposed to high glucose. Am J Physiol Renal Physiol 2005;289:F1153–F1158. [DOI] [PubMed] [Google Scholar]
- 82. van der Meer RW, Rijzewijk LJ, de Jong HW, Lamb HJ, Lubberink M, Romijn JA, Bax JJ, de Roos A, Kamp O, Paulus WJ, Heine RJ, Lammertsma AA, Smit JW, Diamant M.. Pioglitazone improves cardiac function and alters myocardial substrate metabolism without affecting cardiac triglyceride accumulation and high-energy phosphate metabolism in patients with well-controlled type 2 diabetes mellitus. Circulation 2009;119:2069–2077. [DOI] [PubMed] [Google Scholar]
- 83. Zhang Z, Zhang X, Korantzopoulos P, Letsas KP, Tse G, Gong M, Meng L, Li G, Liu T.. Thiazolidinedione use and atrial fibrillation in diabetic patients: a meta-analysis. BMC Cardiovasc Disord 2017;17:96.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefebvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Koranyi L, Laakso M, Mokan M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J; PROactive Investigators. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279–1289. [DOI] [PubMed] [Google Scholar]
- 85. Singh S, Loke YK, Furberg CD.. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA 2007;298:1189–1195. [DOI] [PubMed] [Google Scholar]
- 86. Komajda M, McMurray JJ, Beck-Nielsen H, Gomis R, Hanefeld M, Pocock SJ, Curtis PS, Jones NP, Home PD.. Heart failure events with rosiglitazone in type 2 diabetes: data from the RECORD clinical trial. Eur Heart J 2010;31:824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hernandez AV, Usmani A, Rajamanickam A, Moheet A.. Thiazolidinediones and risk of heart failure in patients with or at high risk of type 2 diabetes mellitus: a meta-analysis and meta-regression analysis of placebo-controlled randomized clinical trials. Am J Cardiovasc Drugs 2011;11:115–128. [DOI] [PubMed] [Google Scholar]
- 88. Home PD, Pocock SJ, Beck-Nielsen H, Curtis PS, Gomis R, Hanefeld M, Jones NP, Komajda M, McMurray JJ, Team RS.. Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet 2009;373:2125–2135. [DOI] [PubMed] [Google Scholar]
- 89. Erdmann E, Charbonnel B, Wilcox RG, Skene AM, Massi-Benedetti M, Yates J, Tan M, Spanheimer R, Standl E, Dormandy JA; PROactive Investigators. Pioglitazone use and heart failure in patients with type 2 diabetes and preexisting cardiovascular disease: data from the PROactive study (PROactive 08). Diabetes Care 2007;30:2773–2778. [DOI] [PubMed] [Google Scholar]
- 90. Benbow A, Stewart M, Yeoman G.. Thiazolidinediones for type 2 diabetes. All glitazones may exacerbate heart failure. BMJ 2001;322:236.. [PubMed] [Google Scholar]
- 91. Tang WH, Francis GS, Hoogwerf BJ, Young JB.. Fluid retention after initiation of thiazolidinedione therapy in diabetic patients with established chronic heart failure. J Am Coll Cardiol 2003;41:1394–1398. [DOI] [PubMed] [Google Scholar]
- 92. Kahles F, Meyer C, Mollmann J, Diebold S, Findeisen HM, Lebherz C, Trautwein C, Koch A, Tacke F, Marx N, Lehrke M.. GLP-1 secretion is increased by inflammatory stimuli in an IL-6-dependent manner, leading to hyperinsulinemia and blood glucose lowering. Diabetes 2014;63:3221–3229. [DOI] [PubMed] [Google Scholar]
- 93. Cummings DE, Overduin J.. Gastrointestinal regulation of food intake. J Clin Invest 2007;117:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Gallwitz B, Rosenstock J, Rauch T, Bhattacharya S, Patel S, von Eynatten M, Dugi KA, Woerle HJ.. 2-Year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet 2012;380:475–483. [DOI] [PubMed] [Google Scholar]
- 95. Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, Lingvay I, Rosenstock J, Seufert J, Warren ML, Woo V, Hansen O, Holst AG, Pettersson J, Vilsboll T; SUSTAIN-6 Investigators. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834–1844. [DOI] [PubMed] [Google Scholar]
- 96. Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, Steinberg WM, Stockner M, Zinman B, Bergenstal RM, Buse JB, Committee LS; Investigators LT. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Timmers L, Henriques JP, de Kleijn DP, Devries JH, Kemperman H, Steendijk P, Verlaan CW, Kerver M, Piek JJ, Doevendans PA, Pasterkamp G, Hoefer IE.. Exenatide reduces infarct size and improves cardiac function in a porcine model of ischemia and reperfusion injury. J Am Coll Cardiol 2009;53:501–510. [DOI] [PubMed] [Google Scholar]
- 98. Bose AK, Mocanu MM, Carr RD, Brand CL, Yellon DM.. Glucagon-like peptide 1 can directly protect the heart against ischemia/reperfusion injury. Diabetes 2005;54:146–151. [DOI] [PubMed] [Google Scholar]
- 99. Ussher JR, Baggio LL, Campbell JE, Mulvihill EE, Kim M, Kabir MG, Cao X, Baranek BM, Stoffers DA, Seeley RJ, Drucker DJ.. Inactivation of the cardiomyocyte glucagon-like peptide-1 receptor (GLP-1R) unmasks cardiomyocyte-independent GLP-1R-mediated cardioprotection. Mol Metab 2014;3:507–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Lehrke M, Marx N.. Cardiovascular effects of incretin-based therapies. Rev Diabet Stud 2011;8:382–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Kim M, Platt MJ, Shibasaki T, Quaggin SE, Backx PH, Seino S, Simpson JA, Drucker DJ.. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure. Nat Med 2013;19:567–575. [DOI] [PubMed] [Google Scholar]
- 102. Erdogdu O, Nathanson D, Sjoholm A, Nystrom T, Zhang Q.. Exendin-4 stimulates proliferation of human coronary artery endothelial cells through eNOS-, PKA- and PI3K/Akt-dependent pathways and requires GLP-1 receptor. Mol Cell Endocrinol 2010;325:26–35. [DOI] [PubMed] [Google Scholar]
- 103. Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, Chan JC, Choi J, Gustavson SM, Iqbal N, Maggioni AP, Marso SP, Ohman P, Pagidipati NJ, Poulter N, Ramachandran A, Zinman B, Hernandez AF, Group ES.. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med 2017;377:1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, Lawson FC, Ping L, Wei X, Lewis EF, Maggioni AP, McMurray JJ, Probstfield JL, Riddle MC, Solomon SD, Tardif JC; ELIXA Investigators. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 2015;373:2247–2257. [DOI] [PubMed] [Google Scholar]
- 105. Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, Josse R, Kaufman KD, Koglin J, Korn S, Lachin JM, McGuire DK, Pencina MJ, Standl E, Stein PP, Suryawanshi S, Van de Werf F, Peterson ED, Holman RR, Group TS.. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;373:232–242. [DOI] [PubMed] [Google Scholar]
- 106. Jorsal A, Kistorp C, Holmager P, Tougaard RS, Nielsen R, Hanselmann A, Nilsson B, Moller JE, Hjort J, Rasmussen J, Boesgaard TW, Schou M, Videbaek L, Gustafsson I, Flyvbjerg A, Wiggers H, Tarnow L.. Effect of liraglutide, a glucagon-like peptide-1 analogue, on left ventricular function in stable chronic heart failure patients with and without diabetes (LIVE)-a multicentre, double-blind, randomised, placebo-controlled trial. Eur J Heart Fail 2017;19:69–77. [DOI] [PubMed] [Google Scholar]
- 107. Margulies KB, Hernandez AF, Redfield MM, Givertz MM, Oliveira GH, Cole R, Mann DL, Whellan DJ, Kiernan MS, Felker GM, McNulty SE, Anstrom KJ, Shah MR, Braunwald E, Cappola TP, Network NHFCR.. Effects of liraglutide on clinical stability among patients with advanced heart failure and reduced ejection fraction: a randomized clinical trial. JAMA 2016;316:500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. McInnes G, Evans M, Del Prato S, Stumvoll M, Schweizer A, Lukashevich V, Shao Q, Kothny W.. Cardiovascular and heart failure safety profile of vildagliptin: a meta-analysis of 17 000 patients. Diabetes Obes Metab 2015;17:1085–1092. [DOI] [PubMed] [Google Scholar]
- 109. Williams R, de Vries F, Kothny W, Serban C, Lopez-Leon S, Chu C, Schlienger R.. Cardiovascular safety of vildagliptin in patients with type 2 diabetes: a European multi-database, non-interventional post-authorization safety study. Diabetes Obes Metab 2017;19:1473–1478. [DOI] [PubMed] [Google Scholar]
- 110. Seferovic JP, Claggett B, Seidelmann SB, Seely EW, Packer M, Zile MR, Rouleau JL, Swedberg K, Lefkowitz M, Shi VC, Desai AS, McMurray JJV, Solomon SD.. Effect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: a post-hoc analysis from the PARADIGM-HF trial. Lancet Diabetes Endocrinol 2017;5:333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Packer M. Augmentation of glucagon-like peptide-1 receptor signalling by neprilysin inhibition: potential implications for patients with heart failure. Eur J Heart Fail 2018;20:973–977. [DOI] [PubMed] [Google Scholar]
- 112. Willard JR, Barrow BM, Zraika S.. Improved glycaemia in high-fat-fed neprilysin-deficient mice is associated with reduced DPP-4 activity and increased active GLP-1 levels. Diabetologia 2017;60:701–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Chen J, Wang D, Wang F, Shi S, Chen Y, Yang B, Tang Y, Huang C.. Exendin-4 inhibits structural remodeling and improves Ca2+ homeostasis in rats with heart failure via the GLP-1 receptor through the eNOS/cGMP/PKG pathway. Peptides 2017;90:69–77. [DOI] [PubMed] [Google Scholar]
- 114. Hamdani N, Hervent AS, Vandekerckhove L, Matheeussen V, Demolder M, Baerts L, De Meester I, Linke WA, Paulus WJ, De Keulenaer GW.. Left ventricular diastolic dysfunction and myocardial stiffness in diabetic mice is attenuated by inhibition of dipeptidyl peptidase 4. Cardiovasc Res 2014;104:423–431. [DOI] [PubMed] [Google Scholar]
- 115. Yin M, Sillje HH, Meissner M, van Gilst WH, de Boer RA.. Early and late effects of the DPP-4 inhibitor vildagliptin in a rat model of post-myocardial infarction heart failure. Cardiovasc Diabetol 2011;10:85.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Fiordaliso F, Maggioni S, Balconi G, Schiarea S, Corbelli A, De Luigi A, Figliuzzi M, Antoniou X, Chiabrando C, Masson S, Cervo L, Latini R.. Effects of dipeptidyl peptidase-4 (DPP-4) inhibition on angiogenesis and hypoxic injury in type 2 diabetes. Life Sci 2016;154:87–95. [DOI] [PubMed] [Google Scholar]
- 117. Monami M, Ahren B, Dicembrini I, Mannucci E.. Dipeptidyl peptidase-4 inhibitors and cardiovascular risk: a meta-analysis of randomized clinical trials. Diabetes Obes Metab 2013;15:112–120. [DOI] [PubMed] [Google Scholar]
- 118. White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Cushman WC, Zannad F; EXAMINE Investigators. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 2013;369:1327–1335. [DOI] [PubMed] [Google Scholar]
- 119. Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I; SAVOR-TIMI 53 Steering Committee and Investigators. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 2013;369:1317–1326. [DOI] [PubMed] [Google Scholar]
- 120. Zannad F, Cannon CP, Cushman WC, Bakris GL, Menon V, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Lam H, White WB; EXAMINE Investigators. Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet 2015;385:2067–2076. [DOI] [PubMed] [Google Scholar]
- 121. Kongwatcharapong J, Dilokthornsakul P, Nathisuwan S, Phrommintikul A, Chaiyakunapruk N.. Effect of dipeptidyl peptidase-4 inhibitors on heart failure: a meta-analysis of randomized clinical trials. Int J Cardiol 2016;211:88–95. [DOI] [PubMed] [Google Scholar]
- 122. Rubera I, Poujeol C, Bertin G, Hasseine L, Counillon L, Poujeol P, Tauc M.. Specific Cre/Lox recombination in the mouse proximal tubule. J Am Soc Nephrol 2004;15:2050–2056. [DOI] [PubMed] [Google Scholar]
- 123. Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ.. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation 2016;134:752–772. [DOI] [PubMed] [Google Scholar]
- 124. Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, Broedl UC, Woerle HJ.. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest 2014;124:499–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Ferrannini E, Baldi S, Frascerra S, Astiarraga B, Barsotti E, Clerico A, Muscelli E, Renal handling of ketones in response to sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care 2017;40:771–776. [DOI] [PubMed] [Google Scholar]
- 126. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME Investigators. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–2128. [DOI] [PubMed] [Google Scholar]
- 127. Joubert M, Jagu B, Montaigne D, Marechal X, Tesse A, Ayer A, Dollet L, Le May C, Toumaniantz G, Manrique A, Charpentier F, Staels B, Magre J, Cariou B, Prieur X.. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes 2017;66:1030–1040. [DOI] [PubMed] [Google Scholar]
- 128. Mudaliar S, Alloju S, Henry RR.. Can a shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG OUTCOME study? A unifying hypothesis. Diabetes Care 2016;39:1115–1122. [DOI] [PubMed] [Google Scholar]
- 129. Kappel BA, Lehrke M, Schutt K, Artati A, Adamski J, Lebherz C, Marx N.. Effect of empagliflozin on the metabolic signature of patients with type 2 diabetes mellitus and cardiovascular disease. Circulation 2017;136:969–972. [DOI] [PubMed] [Google Scholar]
- 130. Lopaschuk GD, Verma S.. Empagliflozin's fuel hypothesis: not so soon. Cell Metab 2016;24:200–202. [DOI] [PubMed] [Google Scholar]
- 131. Heise T, Jordan J, Wanner C, Heer M, Macha S, Mattheus M, Lund SS, Woerle HJ, Broedl UC.. Pharmacodynamic effects of single and multiple doses of empagliflozin in patients with type 2 diabetes. Clin Ther 2016;38:2265–2276. [DOI] [PubMed] [Google Scholar]
- 132. Baartscheer A, Schumacher CA, Wust RC, Fiolet JW, Stienen GJ, Coronel R, Zuurbier CJ.. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 2017;60:568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Clancy CE, Chen-Izu Y, Bers DM, Belardinelli L, Boyden PA, Csernoch L, Despa S, Fermini B, Hool LC, Izu L, Kass RS, Lederer WJ, Louch WE, Maack C, Matiazzi A, Qu Z, Rajamani S, Rippinger CM, Sejersted OM, O'Rourke B, Weiss JN, Varró A, Zaza A.. Deranged sodium to sudden death. J Physiol 2015;593:1331–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Skrtic M, Yang GK, Perkins BA, Soleymanlou N, Lytvyn Y, von Eynatten M, Woerle HJ, Johansen OE, Broedl UC, Hach T, Silverman M, Cherney DZ.. Characterisation of glomerular haemodynamic responses to SGLT2 inhibition in patients with type 1 diabetes and renal hyperfiltration. Diabetologia 2014;57:2599–2602. [DOI] [PubMed] [Google Scholar]
- 135. Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, Fagan NM, Woerle HJ, Johansen OE, Broedl UC, von Eynatten M.. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 2014;129:587–597. [DOI] [PubMed] [Google Scholar]
- 136. Chilton R, Tikkanen I, Cannon CP, Crowe S, Woerle HJ, Broedl UC, Johansen OE.. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab 2015;17:1180–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y.. The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 1978;57:549–556. [DOI] [PubMed] [Google Scholar]
- 138. Verma S, Garg A, Yan AT, Gupta AK, Al-Omran M, Sabongui A, Teoh H, Mazer CD, Connelly KA.. Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPA-REG OUTCOME trial? Diabetes Care 2016;39:e212–e213. [DOI] [PubMed] [Google Scholar]
- 139. Cherney DZ, Perkins BA, Soleymanlou N, Har R, Fagan N, Johansen OE, Woerle HJ, von Eynatten M, Broedl UC.. The effect of empagliflozin on arterial stiffness and heart rate variability in subjects with uncomplicated type 1 diabetes mellitus. Cardiovasc Diabetol 2014;13:28.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME® trial investigators. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME(R) trial. Eur Heart J 2016;37:1526–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Butler J, Hamo CE, Filippatos G, Pocock SJ, Bernstein RA, Brueckmann M, Cheung AK, George JT, Green JB, Januzzi JL, Kaul S, Lam CSP, Lip GYH, Marx N, McCullough PA, Mehta CR, Ponikowski P, Rosenstock J, Sattar N, Salsali A, Scirica BM, Shah SJ, Tsutsui H, Verma S, Wanner C, Woerle HJ, Zannad F, Anker SD; EMPEROR Trials Program. The potential role and rationale for treatment of heart failure with sodium-glucose co-transporter 2 inhibitors. Eur J Heart Fail 2017;19:1390–1400. [DOI] [PubMed] [Google Scholar]
- 142. Packer M. Are the effects of drugs to prevent and to treat heart failure always concordant? The statin paradox and its implications for understanding the actions of antidiabetic medications. Eur J Heart Fail 2018;20:1100–1105. [DOI] [PubMed] [Google Scholar]
- 143. Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B; Investigators E-RO. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 2016;375:323–334. [DOI] [PubMed] [Google Scholar]
- 144. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR, Group CPC.. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644–657. [DOI] [PubMed] [Google Scholar]
- 145. Verma S, Mazer CD, Al-Omran M, Inzucchi SE, Fitchett D, Hehnke U, George JT, Zinman B.. Cardiovascular outcomes and safety of empagliflozin in patients with type 2 diabetes mellitus and peripheral artery disease: a subanalysis of EMPA-REG OUTCOME. Circulation 2018;137:405–407. [DOI] [PubMed] [Google Scholar]
- 146. Singh JS, Fathi A, Vickneson K, Mordi I, Mohan M, Houston JG, Pearson ER, Struthers AD, Lang CC.. Research into the effect Of SGLT2 inhibition on left ventricular remodelling in patients with heart failure and diabetes mellitus (REFORM) trial rationale and design. Cardiovasc Diabetol 2016;15:97.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Pollesello P, Papp Z, Nieminen MS.. Lessons from Lisbon on AHF drug treatment: is it really true that all-old-failed-all-new-will-succeed? Int J Cardiol 2013;168:4798–4799. [DOI] [PubMed] [Google Scholar]
- 148. Huxley R, Barzi F, Woodward M.. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 2006;332:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Lee WL, Cheung AM, Cape D, Zinman B.. Impact of diabetes on coronary artery disease in women and men: a meta-analysis of prospective studies. Diabetes Care 2000;23:962–968. [DOI] [PubMed] [Google Scholar]
- 150. Lee PY, Chen WH, Ng W, Cheng X, Kwok JY, Tse HF, Lau CP.. Low-dose aspirin increases aspirin resistance in patients with coronary artery disease. Am J Med 2005;118:723–727. [DOI] [PubMed] [Google Scholar]
- 151. Shen H, Herzog W, Drolet M, Pakyz R, Newcomer S, Sack P, Karon H, Ryan KA, Zhao Y, Shi X, Mitchell BD, Shuldiner AR.. Aspirin Resistance in healthy drug-naive men versus women (from the Heredity and Phenotype Intervention Heart Study). Am J Cardiol 2009;104:606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Eurich DT, Majumdar SR, McAlister FA, Tsuyuki RT, Johnson JA.. Improved clinical outcomes associated with metformin in patients with diabetes and heart failure. Diabetes Care 2005;28:2345–2351. [DOI] [PubMed] [Google Scholar]