Abstract
Background
Renal artery stenosis is one of the secondary causes of pediatric hypertension. Cases with critical unilateral renal artery stenosis manifesting with the hyponatremic hypertensive syndrome are rare and a comprehensive description of this disorder in the pediatric population is lacking in the literature.
Case presentation
We describe a 4-year-old boy who presented with severe hypertension, profound hyponatremia, hypokalemia, nephrotic range proteinuria, and polyuria. Distinctly, the diagnosis of hyponatremic hypertensive syndrome secondary to unilateral renal artery stenosis was confirmed in light of laboratory and radiographic findings of severe natriuresis, elevated renin, and unilateral small kidney. Two weeks following nephrectomy, there was resolution of hyponatremia, hypokalemia, nephrotic range proteinuria and hypertension.
Conclusions
Findings of hyponatremia, hypokalemia, hypertension, polyuria, and unilateral renal hypoplasia can be attributed to a unifying pathology of unilateral renal artery stenosis.
Electronic supplementary material
The online version of this article (10.1186/s12882-019-1246-9) contains supplementary material, which is available to authorized users.
Keywords: Hyponatremic-hypertensive syndrome, Renal artery stenosis
Background
Hypertension in children necessitates prompt work-up and diagnosis in order to uncover and appropriately treat secondary causes, such as coarctation of the aorta, renal parenchymal diseases, renal artery stenosis, and endocrine disorders. Concurrent hyponatremia in hypertension is most commonly caused by renin-secreting tumors, renal ischemia, and renal artery stenosis after exclusion of medication-induced hypertension [1]. The central pathomechanism that underlies hyponatremic hypertension syndrome (HHS) is the stimulation and activation of the renin-angiotensin-aldosterone (RAA) axis which consequently trigger hypertension through vasoconstriction as well as fluid and salt retention. In cases of unilateral renal artery stenosis, angiotensin II induces pressure natriuresis of the non-stenotic kidney and hence produces the unique finding of hyponatremia in conjunction with hypertension.
Hyponatremic hypertensive syndrome, a disorder of severe hypertension and hyponatremia, could result from any causes of high renin conditions. The most common etiology in children is unilateral renal artery stenosis. It could present with of conscious disturbance or seizure, polydipsia and polyuria, with the characteristics of extreme hypertension, hyponatremia, hypokalemia, and proteinuria. Due to its insidious course and potential fatality, it warrants careful investigation by an astute physician [2]. Without appropriate treatment, hypertensive encephalopathy, retinopathy, cardiomyopathy, and nephropathy can develop.
Herein, we present a 4-year-old boy with HHS, caused by unilateral renal artery stenosis, featured by hypertension, hyponatremia, polyuria, and polydipsia. After nephrectomy, he achieved full clinical recovery without sequelae.
Case presentation
A 4-year-old boy, who had no systemic or inherited disease, presented with a 3-week history of intermittent vomiting without diarrhea or abdominal pain. In the past year, he experienced polydipsia and polyuria. Physical examination revealed body weight 17.5 kg (50th percentile), body height 100 cm (15~50th percentile), blood pressure 230/120 mmHg, heart rate 138 /min, and decreased skin turgor. There was no focal neurological deficit, blood pressure discrepancy between upper and lower extremities, palpable mass, nor any appreciation of an abdominal thrill. Laboratory studies revealed serum Na+ 124 mmol/L, K+ 2.4 mmol/L, Cl− 87 mmol/L, Ca2+ 8.5 mg/dL, HCO3− 34.5 mEq/L, creatinine 0.41 mg/dL, albumin 3.4 g/dL, IgG 247 mg/dL, and osmolality 290 mOsm/KgH2O. Urine analysis was significant for creatinine 11.2 mg/dL, Na+ 24 mEq/L, K+ 18 mEq/L, Cl− 24 mEq/L, osmolality 232 mOsm/KgH2O, RBC 168/μL, FENa 6%, and nephrotic-range proteinuria (55 mg/m2/hour). Survey for possible glomerulonephritis demonstrated the absence of anti-streptolysin O, p-ANCA, c-ANCA, ANA, and normal immunoglobulin A, C3, and C4 levels. In addition, work-up for secondary hypertension included: free T4 1.51 (normal range 0.8–2.0 ng/dL), TSH 5.7 (normal range 0.25–5.00 μIU/mL), cortisol 40.18 (normal range 4.3–25 μg/dL), ACTH 9.32 (normal range < 46 pg/mL), renin 1745 (normal range 2–15 ng/L), aldosterone 92.6 (normal range 4–25 ng/dL), and urine vanillylmandelic acid 3.8 (normal range 1.9–9.9 g/day). Renal ultrasonography revealed hyperechoic right kidney (7.6 cm in length) and small left kidney (5.3 cm in length). Due to the presence of hyperreninemic hypertension, natriuretic-hyponatremia, hypokalemia, and nephrotic range proteinuria, HHS was highly suspected. Computed tomography angiography confirmed high-grade renal artery stenosis with hypoplasia of the left kidney (Fig. 1).
Fig. 1.
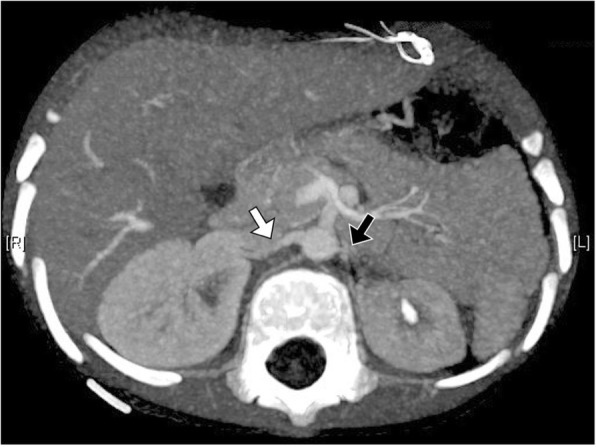
Computed tomographic angiography with maximum intensity projection. The axial view demonstrated the small caliber of the left renal artery (black arrow) with the compensatory change of the contralateral renal artery (white arrow)
In terms of management for this case, we began with volume repletion by normal saline administration. Subsequently, his blood pressure declined from 210/120 mmHg to 180/90 mmHg. Intravenous calcium channel blocker was used to treat his hypertensive emergency, while oral captopril was prescribed for RAA axis blockage after diagnosis of unilateral renal artery stenosis. The systolic blood pressure gradually declined to 150~160 mmHg on the 3rd day. Potassium supplement was infused for his profound hypokalemia and generalized muscle weakness. Due to the severity of left renal artery stenosis, he was not a candidate for angiographic intervention, and decision was made to proceed with left nephrectomy. Overall, electrolyte abnormalities such as hyponatremia and hypokalemia were corrected within 1 week after admission, and resolution of polyuria, polydipsia, proteinuria, and hypertension were achieved 2 weeks after nephrectomy (Additional file 1: Table S1).
Discussion and conclusions
This 4-year-old boy presented with severe hypertension and volume depletion. Comprehensive examinations excluded the possibility of coarctation of great vessels and renal parenchymal diseases and pointed towards an overactive renin-angiotensin-aldosterone axis. The presentation of natriuretic-hyponatremia, hypokalemia, polyuria, nephrotic range proteinuria, and hyperreninemic-hypertension was highly suggestive of HHS. Aside from HHS, primary neurologic diseases such as intracranial hemorrhage or malignancy may also cause hypertension and hyponatremia, secondary to the increase in intracranial pressure and inappropriate secretion of antidiuretic hormone. However, these diseases usually present with focal neurologic deficits and decreased urine output, which could be distinguished from the polyuria and volume depletion of HHS caused by the renal artery stenosis.
The main pathogenesis of HHS is renal ischemia, as shown in Fig. 2. Hypertension is induced by stimulation of unremitted renin secretion and subsequent angiotensin II-induced vasoconstriction and secondary hyperaldosteronism. Elevated circulating angiotensin II can cause glomerular hyperfiltration and subsequential pressure natriuresis of the non-stenotic kidney, which results in the clinical presentation of hyponatremia [3]. In addition, volume depletion contributes to the development of hyponatremia by stimulating the secretion of the anti-diuretic hormone. Sodium wasting and volume depletion further stimulates the renin excretion [4]. Hyperaldosteronism, secondary to hyperreninemia and volume depletion, lead to hypokalemia which is one of the leading complications of HHS. Glomerular hyperfiltration of contralateral healthy kidney, deriving from hyperreninemia-induced hypertension, could eventually result in tubulointerstitial injury from the effects of hypercalciuria and hyperuricosuria [5]. Proteinuria in cases of HHS, sometimes in nephrotic range, can result from the glomerular hyperfiltration, proteinuric effect of angiotensin II, and/or consequence of tubulointerstitial injury caused by prolonging hypercalciuria and hyperuricosuria [6].
Fig. 2.
Possible mechanism of hyponatremic-hypertensive syndrome
We conducted a careful search of literature and found a total of 15 reported pediatric cases, as shown in Table 1. The mean age at onset was 4.03 ± 3.38 years with male predominance (11/15). The combination of hypertension, polydipsia, and polyuria are the most common presentations (14/15), followed by hyponatremic seizure (7/15). The mean serum sodium, potassium, and bicarbonate levels were 123.4 ± 5.5 mEq/l, 2.9 ± 0.5 mEq/l, and 28.9 ± 3.5, respectively. Eight of the patients had proteinuria. Excluding the three patients whose renin and aldosterone data was unavailable, almost all patients had hyperreninemia (10/11) and hyperaldosteronism (12/12). The most common extra-renal involvements were neurological (8/15), cardiac (7/15), and retinal (5/15).
Table 1.
Summary of Clinical Characteristics of Reported Pediatric Cases
| Patient [Ref] |
Gender/ age | Presentations | BP (mmHg) | Renin (range) | Aldosterone | SNa (mEq/L) | SK (mEq/L) | SHCO3- (mEq/L) | Proteinuria | Organs involvement | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 [2] | F/ 2y9m | Polydipsia, polyuria Presyncope |
215/156 | Low | Elevated | 129 | 3 | 27 | 700 mg/day | CNSa Kidney |
IV β blocker, oral β blocker, CCBb, ACEIc dPTA |
Recovery |
| 2 [2] | M/ 2y3m | Polydipsia | 142/92 | NA | Elevated | 122 | 3.9 | 25.9 | 3200 mg/day | Heart Kidney |
IV β blocker, oral β blocker, CCB, ACEI PTA |
Recovery |
| 3 [2] | M/ 2y | Polydipsia, polyuria Restlessness |
220/150 | Elevated | Elevated | 125 | 3.2 | 27.2 | 5300 mg/day | Heart Kidney |
IV β blocker, oral β blocker, CCB, ACEI PTA |
Recovery |
| 5 [9] | M/ 1y6m | Seizure, hemorrhagic and ischemic stroke | 210/160 | 172 ng/ml/min (3~11) | 91 ng/dl (4~16) | 120 | 2.1 | NAe | NA | CNS Heart Kidney |
Nitroprusside, IV β blocker, oral CCB Aorto-renal bypass |
Hypertension |
| 4 [14] | F/ 1y3m | Polyuria, polydipsia | 190/120 | 24 ng/ml/hr. (1~4.5) | 8 nmol/l (0.1~0.8) | 122 | 2.4 | 29.5 | 1800 mg/day | Heart Kidney |
ACEI, β blocker, CCB, spironolactone PTA |
Recovery |
| 6 [15] | M/ 7y | Polydipsia, polyuria | 210/120 | NA | NA | 114 | 2.4 | NA | NA | Retina Kidney |
CCB, α1 blocker Nephrectomy | Recovery |
| 7 [16] | M/ 2y9m | Polydipsia, polyuria Seizure | 160/120 | 80.44 ng/ml/hr. (0.2~2.8) | 6861 pg/ml (10~160) | 118 | 1.9 | NA | NA | CNS Kidney |
CCB, desmopressin ACEI Nephrectomy |
Recovery |
| 8 [16] | F/ 1y4m | Polyuria, polydipsia | 140/90 | NA | NA | 131 | 2.6 | NA | NA | Kidney | CCB ACEI Nephrectomy |
Hypertension |
| 9 [17] | M/ 9y | Polyuria, polydipsia Seizure | 156/120 | NA | NA | 124 | 3.2 | 34 | NA | CNS Retina Kidney |
Nitroprusside ACEI, CCB PTA with stenting |
Hypertension |
| 10 [18] | M/ 1y7m | Polyuria Polydipsia Seizure | 248/150 | 137 ng/ml/min (3~11) | 743 ng/dl (7~93) | 128 | 3.2 | 24 | NA | CNS Heart Kidney |
Nitroprusside, ACEI PTA with stent |
Hypertension |
| 11 [19] | M/ 5y | Seizure | 236/132 | 21.06 ng/ml/hr. (1.3~3.9) | 1172 ng/dl (1~16) | 112 | 3.2 | 33.4 | fUP/UCr 6.84 | CNS Kidney |
β blocker, CCB, hydralazine | Proteinuria Hypertension |
| 12 [19] | M/ 8y | Polydipsia, polyuria Seizure | 184/110 | 32.8 ng/ml/hr. (1.3~3.9) | 1436 ng/dl (1~16) | 127 | 3.1 | 27.2 | UP/UCr 3.91 | CNS Retina Kidney |
β blocker, CCB, hydralazine PTA |
Recovery |
| 13 [19] | M/ 12y | Polydipsia, polyuria Seizure | 244/166 | 25.04 ng/ml/hr. (1.3~3.9) | 1358 ng/dl (1~16) | 126 | 3.2 | 32.2 | UP/UCr 4.36 | CNS Retina Kidney |
β blocker, CCB, hydralazine PTA with stenting |
Hypertension |
| 14 [20] | M/ 2y | Polydipsia, polyuria | NA | 2537 ng/dl | 31.6 ng/dl | 124 | 2.8 | NA | 1230 mg/day | Heart Kidney |
Hydralazine Angioplasty with patch |
Recovery |
| 15 [20] | F/ 2y | Polydipsia, polyuria | NA | 76.5 ng/dl | 48.1 ng/dl | 128 | 2.7 | NA | 2400 mg/day | Heart Retina Kidney |
CCB, β blockers, hydralazine Angioplasty with patch |
Recovery |
| Our case | M/ 4y | Polyuria, polydipsia | 230/120 | 174.5 ng/dl | 9.26 ng/dl | 124 | 2.4 | 34.5 | 55 mg/m2/hr | Kidney | IV CCB, Oral ACEI Nephrectomy |
Recovery |
aCNS, central nervous system; bCCB, calcium channel blocker; cACEI, angiotensin-converting enzyme inhibitor; dPTA, percutaneous transluminal angioplasty; eNA, not available; furine protein-to-creatinine ratio (mg/dl/ mg/dl)
The mainstay of treatment for renal artery stenosis-associated HHS lies in the restoration of intravascular volume, prevention of acute insult of hypertensive crisis and correction of underlying renal arterial stenosis. Volume depletion needs to be corrected first to improve systemic blood flow and prevent further injury resulting from renal ischemia [7]. After volume repletion, the prompt decline of blood pressure could be achieved by intravenous calcium channel blocker, which has been suggested to be the first line drug for severe hypertension with acute kidney injury [8]. For cases with HHS, angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker should be introduced to mitigate the over-activation of the RAA system [9]. However, the use of diuretics is not recommended due to the potential deleterious effects of fluid and sodium wasting which could further activate the RAA system [10]. Lastly, correction of renal artery stenosis can be achieved surgically by percutaneous renal angioplasty, renal artery reconstruction, or nephrectomy. As shown in Table 1, all patients received anti-hypertensive agents as the first line therapy. Eleven and three cases underwent angioplasty and unilateral nephrectomy, respectively. It is important to note that HHS caused by renal artery stenosis does not always result in a favorable outcome, as five patients had residual hypertension despite aggressive treatment. Several causes of residual hypertension in cases with HHS have been proposed. A longitudinal pediatric study stated that over 40% of renal artery angioplasty would develop restenosis [11]. Also, chronic kidney disease caused by prolonging tissue hypoxia and consequence of proteinuria could lead to hypertension despite restoration of renal blood flow [12]. Finally, uncontrolled hypertension itself could cause irreversible remodeling of vascular endothelium, resulting in permanent hypertension [13].
In conclusion, HHS caused by unilateral renal artery stenosis is a potentially curable and reversible disease when promptly diagnosed and appropriate treatment is implemented. Hyperreninemic hypertension, natriuretic hyponatremia, nephrotic range proteinuria, and unilateral renal hypoplasia are clinical clues that aid in uncovering the diagnosis.
Additional file
Table S1. Clinical and laboratory characteristics before and after treatment. (DOC 32 kb)
Acknowledgments
Not applicable.
Funding
None.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviation
- HHS
Hyponatremic hypertension syndrome
Authors’ contributions
JD, JL, HC, and MT acquired the data necessary for analysis. JD wrote the initial draft of the paper. JH, TW, SL, and MT contributed in data analysis and interpretation. TW, JL, and SL were involved in drafting and revising the manuscript. All authors approved the final version of the manuscript prior to submission. All authors agreed to be accountable for all aspects of the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the parents/guardians of the children.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jhao-Jhuang Ding, Email: jamesdin1124@gmail.com.
Shih-Hua Lin, Email: l521116@gmail.com.
Jin-Yao Lai, Email: jylai@cgmh.org.tw.
Tai-Wei Wu, Email: wutcz8@gmail.com.
Jing-Long Huang, Email: long@adm.cgmh.org.tw.
Hung-Tao Chung, Email: chd2162@gmail.com.
Min-Hua Tseng, Phone: 886-3-3281200, Email: doc31089@gmail.com.
References
- 1.Agarwal M, Lynn KL, Richards AM, Nicholls MG. Hyponatremic-hypertensive syndrome with renal ischemia: an underrecognized disorder. Hypertens (Dallas, Tex 1979) 1999;33:1020–1024. doi: 10.1161/01.HYP.33.4.1020. [DOI] [PubMed] [Google Scholar]
- 2.Kovalski Y, Cleper R, Krause I, Dekel B, Belenky A, Davidovits M. Hyponatremic hypertensive syndrome in pediatric patients: is it really so rare? Pediatr Nephrol. 2012;27:1037–1040. doi: 10.1007/s00467-012-2123-y. [DOI] [PubMed] [Google Scholar]
- 3.Ivy JR, Bailey MA. Pressure natriuresis and the renal control of arterial blood pressure. J Physiol. 2014;592:3955–3967. doi: 10.1113/jphysiol.2014.271676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zieg J. Pathophysiology of Hyponatremia in Children. Front Pediatr. 2017. 10.3389/fped.2017.00213. [DOI] [PMC free article] [PubMed]
- 5.Sendromlu H-H, Çocuk AE, Yılmaz D, Kelimeler A. Hyponatremic-hypertensive syndrome Hyponatremic-hypertensive syndrome in an 18-month-old male child. J Clin Anal Med. 2015;6(suppl 6):883–885. [Google Scholar]
- 6.Ogata H, Ishiyama N, Hamabe K, Tabata T, Mitsuhasi K, Miki T, et al. Renovascular Hypertension with Massive Proteinuria. Intern Med. 1996;35:569–73. [DOI] [PubMed]
- 7.van Tellingen V, Lilien MR, Bruinenberg JFM, de Vries WB. The Hyponatremic Hypertensive Syndrome in a Preterm Infant: A Case of Severe Hyponatremia with Neurological Sequels. Int J Nephrol. 2011;2011:1–4. doi: 10.4061/2011/406515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aronow WS. Treatment of hypertensive emergencies. Ann Transl Med. 2017;5:S5. doi: 10.21037/atm.2017.03.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dixit MP, Hughes JD, Theodorou A, Dixit NM. Hyponatremic hypertensive syndrome (HHS) in an 18-month old-child presenting as malignant hypertension: a case report. BMC Nephrol. 2004;5:5. doi: 10.1186/1471-2369-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh D, Akingbola O, Yosypiv I, El-Dahr S. Emergency Management of Hypertension in Children. Int J Nephrol. 2012. 10.1155/2012/420247. [DOI] [PMC free article] [PubMed]
- 11.Zhu G, He F, Gu Y, Yu H, Chen B, Hu Z, et al. Angioplasty for pediatric renovascular hypertension: a 13-year experience. Diagnostic Interv Radiol. 2014;20:285–292. doi: 10.5152/dir.2014.13208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Textor SC. “Renovascular hypertension: is there still a role for stent revascularization? ” Current opinion in nephrology and hypertension. Curr Opin Nephrol Hypertens. 2013;22:1. doi: 10.1097/MNH.0b013e328363ffe0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bleakley C, Hamilton PK, Pumb R, Harbinson M, Mcveigh GE. Endothelial function in hypertension: victim or culprit? J Clin Hypertens. 2015;17:651–654. doi: 10.1111/jch.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seracini D, Pela I, Favilli S, Bini RM. Hyponatraemic-hypertensive syndrome in a 15-month-old child with renal artery stenosis. Pediatr Nephrol. 2006;21:1027–1030. doi: 10.1007/s00467-006-0121-7. [DOI] [PubMed] [Google Scholar]
- 15.Neeli S. Renal artery stenosis with hyponatremic hypertensive syndrome in a 7-year-old child. J Pediatr Urol. 2008;4:407–408. doi: 10.1016/j.jpurol.2008.01.204. [DOI] [PubMed] [Google Scholar]
- 16.D’Angelo P, Catania S, Zirilli G, Collini P, Tropia S, Perotti D, et al. Severe polyuria and polydipsia in hyponatremic-hypertensive syndrome associated with Wilms tumor. Pediatr Blood Cancer. 2010;55:566–569. doi: 10.1002/pbc.22610. [DOI] [PubMed] [Google Scholar]
- 17.Pandey M, Sharma R, Kanwal SK, Chhapola V, Awasthy N, Mathur A, et al. Hyponatremic-hypertensive syndrome: think of unilateral renal artery stenosis. Indian J Pediatr. 2013;80:872–874. doi: 10.1007/s12098-012-0908-4. [DOI] [PubMed] [Google Scholar]
- 18.Parikh P, Duhame D, Monahan L, Woroniecki R. Renal artery stenosis precipitates hyponatremic hypertensive syndrome and posterior reversible leukoencephalopathy. Front Pediatr. 2015. 10.3389/fped.2015.00040. [DOI] [PMC free article] [PubMed]
- 19.Mukherjee D, Sinha R, Akhtar MS, Saha AS. Hyponatremic hypertensive syndrome - a retrospective cohort study. World J Nephrol. 2017;6:41. doi: 10.5527/wjn.v6.i1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trivelli A, Ghiggeri GM, Canepa A, Oddone M, Bava G, Perfumo F. Hyponatremic-hypertensive syndrome with extensive and reversible renal defects. Pediatr Nephrol. 2005;20:102–104. doi: 10.1007/s00467-004-1648-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Clinical and laboratory characteristics before and after treatment. (DOC 32 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this published article.



