Abstract
Background
The unanticipated difficult airway is a potentially life‐threatening event during anaesthesia or acute conditions. An unsuccessfully managed upper airway is associated with serious morbidity and mortality. Several bedside screening tests are used in clinical practice to identify those at high risk of difficult airway. Their accuracy and benefit however, remains unclear.
Objectives
The objective of this review was to characterize and compare the diagnostic accuracy of the Mallampati classification and other commonly used airway examination tests for assessing the physical status of the airway in adult patients with no apparent anatomical airway abnormalities. We performed this individually for each of the four descriptors of the difficult airway: difficult face mask ventilation, difficult laryngoscopy, difficult tracheal intubation, and failed intubation.
Search methods
We searched major electronic databases including CENTRAL, MEDLINE, Embase, ISI Web of Science, CINAHL, as well as regional, subject specific, and dissertation and theses databases from inception to 16 December 2016, without language restrictions. In addition, we searched the Science Citation Index and checked the references of all the relevant studies. We also handsearched selected journals, conference proceedings, and relevant guidelines. We updated this search in March 2018, but we have not yet incorporated these results.
Selection criteria
We considered full‐text diagnostic test accuracy studies of any individual index test, or a combination of tests, against a reference standard. Participants were adults without obvious airway abnormalities, who were having laryngoscopy performed with a standard laryngoscope and the trachea intubated with a standard tracheal tube. Index tests included the Mallampati test, modified Mallampati test, Wilson risk score, thyromental distance, sternomental distance, mouth opening test, upper lip bite test, or any combination of these. The target condition was difficult airway, with one of the following reference standards: difficult face mask ventilation, difficult laryngoscopy, difficult tracheal intubation, and failed intubation.
Data collection and analysis
We performed screening and selection of the studies, data extraction and assessment of methodological quality (using QUADAS‐2) independently and in duplicate. We designed a Microsoft Access database for data collection and used Review Manager 5 and R for data analysis. For each index test and each reference standard, we assessed sensitivity and specificity. We produced forest plots and summary receiver operating characteristic (ROC) plots to summarize the data. Where possible, we performed meta‐analyses to calculate pooled estimates and compare test accuracy indirectly using bivariate models. We investigated heterogeneity and performed sensitivity analyses.
Main results
We included 133 (127 cohort type and 6 case‐control) studies involving 844,206 participants. We evaluated a total of seven different prespecified index tests in the 133 studies, as well as 69 non‐prespecified, and 32 combinations. For the prespecified index tests, we found six studies for the Mallampati test, 105 for the modified Mallampati test, six for the Wilson risk score, 52 for thyromental distance, 18 for sternomental distance, 34 for the mouth opening test, and 30 for the upper lip bite test. Difficult face mask ventilation was the reference standard in seven studies, difficult laryngoscopy in 92 studies, difficult tracheal intubation in 50 studies, and failed intubation in two studies. Across all studies, we judged the risk of bias to be variable for the different domains; we mostly observed low risk of bias for patient selection, flow and timing, and unclear risk of bias for reference standard and index test. Applicability concerns were generally low for all domains. For difficult laryngoscopy, the summary sensitivity ranged from 0.22 (95% confidence interval (CI) 0.13 to 0.33; mouth opening test) to 0.67 (95% CI 0.45 to 0.83; upper lip bite test) and the summary specificity ranged from 0.80 (95% CI 0.74 to 0.85; modified Mallampati test) to 0.95 (95% CI 0.88 to 0.98; Wilson risk score). The upper lip bite test for diagnosing difficult laryngoscopy provided the highest sensitivity compared to the other tests (P < 0.001). For difficult tracheal intubation, summary sensitivity ranged from 0.24 (95% CI 0.12 to 0.43; thyromental distance) to 0.51 (95% CI 0.40 to 0.61; modified Mallampati test) and the summary specificity ranged from 0.87 (95% CI 0.82 to 0.91; modified Mallampati test) to 0.93 (0.87 to 0.96; mouth opening test). The modified Mallampati test had the highest sensitivity for diagnosing difficult tracheal intubation compared to the other tests (P < 0.001). For difficult face mask ventilation, we could only estimate summary sensitivity (0.17, 95% CI 0.06 to 0.39) and specificity (0.90, 95% CI 0.81 to 0.95) for the modified Mallampati test.
Authors' conclusions
Bedside airway examination tests, for assessing the physical status of the airway in adults with no apparent anatomical airway abnormalities, are designed as screening tests. Screening tests are expected to have high sensitivities. We found that all investigated index tests had relatively low sensitivities with high variability. In contrast, specificities were consistently and markedly higher than sensitivities across all tests. The standard bedside airway examination tests should be interpreted with caution, as they do not appear to be good screening tests. Among the tests we examined, the upper lip bite test showed the most favourable diagnostic test accuracy properties. Given the paucity of available data, future research is needed to develop tests with high sensitivities to make them useful, and to consider their use for screening difficult face mask ventilation and failed intubation. The 27 studies in 'Studies awaiting classification' may alter the conclusions of the review, once we have assessed them.
Plain language summary
Bedside examination tests to detect beforehand adults who are likely to be difficult to intubate
Review question
We looked for the most suitable and accurate rapid screening test in adults with no obvious airway abnormalities, to identify those who are likely to be difficult to intubate (i.e. insertion of a tube into the windpipe).
Background
Intubation ensures a patient’s airway is clear while they are heavily sedated, unconscious or anaesthetized, so their breathing can be controlled by machine (ventilation), and appropriate levels of oxygen can be given during surgery, following major trauma, during critical illness, or following cardiac arrest. Having an airway that is difficult to intubate is a potentially life‐threatening situation.
Tube insertion is preceded by laryngoscopy (insertion of mini‐camera to view route of tube insertion), requires advanced skills, and is generally uneventful. Intubation is difficult in approximately 10% of patients, who require special equipment and precautions. Several physical features are associated with difficult airways and failed intubation, so warning of potentially difficult airways would be helpful. Several quick bedside tests are in routine clinical use to identify those at high risk for difficult airways, but how accurate these are remains unclear.
Population
We included studies of adults aged 16 years or older without obvious airway abnormalities who were to receive standard intubation.
Test under investigation
We assessed the seven most common bedside tests, routinely used to detect difficult airways. These take only a few seconds to complete and require no special equipment.
The index tests (diagnostic tests of interest) included:
‐ the Mallampati test (original or modified; asking a sitting patient to open his mouth and to protrude the tongue as much as possible so that visibility can be determined);
‐ Wilson risk score (including patient's weight, head and neck movement, jaw movement, receding chin, buck teeth);
‐ thyromental distance (length between the chin and the upper edge of Adam's apple);
‐ sternomental distance (length between the chin and the notch between the collar bones);
‐ mouth opening test;
‐ upper lip bite test;
‐ or any combination of these tests.
Search date
The evidence is current to 16 December 2016. (We searched for new studies in March 2018, but we have not yet included them in the review.)
Study characteristics
We included 133 studies (844,206 participants) which investigated the accuracy of the seven tests above, plus 69 other common tests and 32 test combinations, in detection of difficult airways.
Key results
For difficult laryngoscopy, the average sensitivity (percentage of correctly identified difficult airways) ranged from 22% (mouth opening test) to 63% (upper lip bite test). The average specificity (percentage of correctly classified patients without difficult airways) ranged from 80% (modified Mallampati test) to 95% (Wilson risk score). The upper lip bite test had the highest sensitivity of all tests considered.
For difficult tube insertion, the average sensitivity ranged from 24% (thyromental distance) to 51% (modified Mallampati test) and the average specificity ranged from 87% (modified Mallampati test) to 93% (mouth opening test). The modified Mallampati test had the highest sensitivity of all tests considered.
For difficult face mask ventilation (another indication of a difficult airway), there were only enough data to calculate average sensitivity of 17% and specificity 90% for the modified Mallampati test.
Quality of the evidence
Overall, the evidence from the studies was of moderate to high quality. The likelihood of the studies providing reliable results was generally high, although in half of them, the intubating physician knew the result of the preceding test, which may have influenced results, but this is the normal situation in routine clinical care. The characteristics of patients, tests, and conditions were comparable to those seen in a wide range of everyday clinical settings. The results of this review should apply to standard preoperative airway assessments in apparently normal hospital patients worldwide.
Conclusion
The bedside screening tests examined in this review are not well suited for the purpose of detecting unanticipated difficult airways because they missed a large number of people who had a difficult airway.
Summary of findings
Summary of findings'. 'Airway physical examination tests for detection of difficult airway management in apparently normal patients.
| Patients or population: adults with no apparent anatomical airway abnormalities | ||||||
| Settings: operating theatres, intensive care units and emergency departments | ||||||
| Studies: total of 133 studies, mostly cohort type studies; six case‐control studies. Each study can be present in more than one analysis | ||||||
| Test | Number of participants (studies) | Summary sensitivity (95% confidence interval) | Summary specificity (95% confidence interval) | Prevalence median (IQR) | Implications | Quality and comments |
| Difficult laryngoscopy | ||||||
| Mallampati test | 2165 (6) | 0.40 (0.16 to 0.71) | 0.89 (0.75 to 0.96) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 6 will be missed by the Mallampati test (60% of 10). Of the 90 patients without difficult laryngoscopy 10 will be unnecessarily classified as having difficult airway. | Limited number of studies. Risk of bias mostly low in all domains. Applicability concerns low. |
| Modified Mallampati test | 232,939 (80) | 0.53 (0.47 to 0.59) | 0.80 (0.74 to 0.85) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 5 will be missed by the modified Mallampati test (47% of 10). Of the 90 patients without difficult laryngoscopy 18 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly unclear in all domains. Applicability concerns mostly low. |
| Wilson risk score | 5862 (5) | 0.51 (0.40 to 0.61) | 0.95 (0.88 to 0.98) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 5 will be missed by the Wilson risk score (49% of 10). Of the 90 patients without difficult laryngoscopy 5 will be unnecessarily classified as having a difficult airway. | Limited number of studies. Risk of bias unclear. Applicability concerns mostly low in all domains. |
| Thyromental distance | 33,189 (42) | 0.37 (0.28 to 0.47) | 0.89 (0.84 to 0.93) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 6 will be missed by thyromental distance (63% of 10). Of the 90 patients without difficult laryngoscopy 10 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Sternomental distance | 12,211 (16) | 0.33 (0.16 to 0.56) | 0.92 (0.86 to 0.96) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 7 will be missed by sternomental distance (67% of 10). Of the 90 patients without difficult laryngoscopy 7 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Mouth opening test | 22,179 (24) | 0.22 (0.13 to 0.33) | 0.94 (0.90 to 0.97) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 8 will be missed by the mouth opening test (78% of 10). Of the 90 patients without difficult laryngoscopy 5 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Upper lip bite test | 19,609 (27) | 0.67 (0.45 to 0.83) | 0.92 (0.86 to 0.95) | 10% (5% to 16%) | With a prevalence of 10%, 10 out of 100 patients will have difficult laryngoscopy. Of these, 3 will be missed by the upper lip bite test (33% of 10). Of the 90 patients without difficult laryngoscopy 7 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Difficult tracheal intubation | ||||||
| Modified Mallampati test | 191,849 (24) | 0.51 (0.40 to 0.61) | 0.87 (0.82 to 0.91) | 11% (5% to 13%) | With a prevalence of 11%, 11 out of 100 patients will have difficult tracheal intubation. Of these, 5 will be missed by the modified Mallampati test (49% of 11). Of the 89 patients without difficult tracheal intubation 12 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly unclear in all domains. Applicability concerns mostly low in all domains. |
| Thyromental distance | 5089 (10) | 0.24 (0.12 to 0.43) | 0.90 (0.80 to 0.96) | 11% (5% to 13%) | With a prevalence of 11%, 11 out of 100 patients will have difficult tracheal intubation. Of these, 8 will be missed by thyromental distance (76% of 11). Of the 89 patients without difficult tracheal intubation 9 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Mouth opening test | 6091 (9) | 0.27 (0.16 to 0.41) | 0.93 (0.87 to 0.96) | 11% (5% to 13%) | With a prevalence of 11%, 11 out of 100 patients will have difficult tracheal intubation. Of these, 8 will be missed by the mouth opening test (73% of 11). Of the 89 patients without difficult tracheal intubation 6 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly low in all domains. Applicability concerns low. |
| Difficult face mask ventilation | ||||||
| Modified Mallampati test | 56,323 (6) | 0.17 (0.06 to 0.39) | 0.90 (0.81 to 0.95) | 11% (6% to 28%) | With a prevalence of 11%, 11 out of 100 patients will have difficult face mask ventilation. Of these, 9 will be missed by the modified Mallampati test (83% of 11). Of the 89 patients without difficult face mask ventilation 9 will be unnecessarily classified as having a difficult airway. | Risk of bias mostly unclear in all domains. Applicability concerns mostly low. |
| CAUTION: the results on this table should not be interpreted in isolation from the results of the individual included studies contributing to each summary test accuracy measure. We have reported these in the main body of the text of the review. We calculated prevalences from the included studies by reference standard. IQR: interquartile range. | ||||||
Background
Target condition being diagnosed
The difficult airway is a potentially life‐threatening event during anaesthesia, following major trauma, with the onset of critical illness, and for resuscitation following cardiac arrest. While any part of the respiratory tract (through which air passes during breathing) is considered to be part of the airway, the difficult airway is focused on the upper airway, that is, the portion of the respiratory tract that extends from the nares or mouth to, and including, the larynx. Thus subglottic stenosis, a type of airway obstruction, and other subglottic problems are not part of this definition of the difficult airway. The upper airway must be patent (open and unblocked) to allow spontaneous lung ventilation by the patient and for physician‐, nurse‐ or therapist‐managed assisted ventilation. Additionally, during severe illness or states of altered consciousness the airway must be secured to prevent soiling of the lower airway (trachea, bronchi, etc.) and lung parenchyma by gastric contents, oral secretions, infectious material and blood. Without a patent airway, asphyxia develops within seconds to minutes; without resolution of the loss of a patent airway, death occurs quickly (ASA 2003).
Most commonly, there is an orderly sequence of events in the process of upper airway management by practitioners that terminates with endotracheal intubation. The initial step is the application of a tight fitting face mask with the patient continuing to breath spontaneously. Typically, sedating and paralysing drugs are administered to facilitate airway access. This is followed by the application of positive airway pressure, generated manually with a breathing bag, to provide assisted ventilation. Next, a laryngoscope is inserted into the mouth and pharynx to allow visualization of the glottis and, finally, a tracheal tube is advanced through the glottis into the trachea (ASA 2003).
The difficult airway is not a disease; neither is it just one particular anatomical characteristic of patient physiognomy. Strictly speaking, the difficult airway (or difficult airway event) describes difficulty in or failure to complete one or more of the sequential steps in upper airway management. It is a complex interaction of patient anatomy, clinical circumstances and clinician skill. Nevertheless, the usual focus of the difficult airway is anatomical anomalies in contrast to functional airway obstruction that can accompany inadequate anaesthesia (the struggling patient, coughing, laryngospasm, opioid induced skeletal muscle and laryngeal rigidity, bronchospasm etc.). Thus, the difficult airway does not have a reference standard other than the result of the actual attempted airway management for a patient. While there are no standardized definitions of a difficult airway event, the 2003 practice guidelines from the American Society of Anesthesiologists (ASA), suggested using at least four descriptors of difficult airway events (ASA 2003). In a simplified form, these are as follows.
Difficult face mask ventilation: it is not possible to provide adequate face mask ventilation.
Difficult laryngoscopy: even with multiple attempts it is not possible to visualize any portion of the vocal cords during conventional laryngoscopy.
Difficult tracheal intubation: tracheal intubation requires multiple attempts.
Failed intubation: placement of the tracheal tube fails after multiple intubation attempts.
Current guidelines added difficult placement or functioning of supraglottic devices as a dimension for the difficult airway (ASA 2013). Difficult face mask ventilation is generally due to an inadequate mask fit or excessive resistance to gas ingress or egress; face mask ventilation is usually facilitated by the insertion of an oral airway or by the administration of muscle relaxants (El‐Orbany 2009). Beside the signs of absent or inadequate chest wall movement and breath sounds, difficult ventilation is also recognized by falling oxygen saturation or increasing partial pressure of carbon dioxide in the arterial blood (PaCO2), or both. Kheterpal and colleagues reported the risk of this difficult airway event during anaesthesia in over 50,000 patients (Kheterpal 2009). Using the descriptions "difficult ventilation (inadequate, unstable, or requiring two providers) with or without muscle relaxant" and "unable to mask ventilate with or without muscle relaxant" the prevalence was 2.2% (1141/53,401) for the former and 0.15% (77/53,041) for the latter.
The standard rigid laryngoscope typically consists of a handle containing batteries and an interchangeable blade with a light source. There are many types of laryngoscope blades. The two main types are the curved Macintosh blade and the straight Miller blade. The tip of the Macintosh blade is advanced into the vallecula, where it sits anterior to the epiglottis and raises the epiglottis out of the visual pathway; the Miller blade is advanced further into the airway with the tip sitting posterior to the epiglottis, trapping and elevating the epiglottis while exposing the glottis and vocal folds. However, both a curved and a straight blade can be used in either fashion with the tip of the blade in the vallecula or behind the epiglottis. Each blade comes in several lengths and widths to accommodate patient size (ASA 2003).
Cormack and Lehane (Cormack 1984), proposed a four‐grade scoring system to describe the view at direct laryngoscopy. using these standard laryngoscopes. The assigned grades are:
full view of the glottis;
partial view of the glottis or arytenoids;
only epiglottis visible;
neither glottis nor epiglottis visible.
This scoring system was extended by Yentis and Lee (Yentis 1998), by subdividing grade 2 into 2a) partial view of the glottis; and 2b) arytenoids or posterior part of the vocal cords only just visible. Other modifications of the Cormack and Lehane grades were proposed in the Cook 2000 study. Difficult laryngoscopy is usually defined as a laryngeal exposure with a score of grade 3 or grade 4. A systematic review (9 studies with 14,438 participants) found that the prevalence of difficult laryngoscopy ranged from 6% to 27% (Lee 2006); in these nine studies the original Cormack and Lehane grades were almost uniformly used to classify difficult laryngoscopy.
Difficult tracheal intubation has been variously defined as a procedure requiring excessive time, multiple attempted passages of the tracheal tube, or having to resort to specialized equipment. A quantitative intubation difficulty scale has been proposed (Adnet 1997). Lundstrom and colleagues defined a non‐difficult tracheal intubation as "intubated by direct laryngoscope by the first anaesthetist and in two attempts maximally"; difficult tracheal intubation was any event with more than two anaesthetists, more than two attempts, use of specialized equipment or failed passage (Lundstrom 2009). In a cohort of over 90,000 patients having anaesthesia, the prevalence of difficult tracheal intubation was 5.2% (4704/91,297) (Lundstrom 2009).
Failed intubation is the least common of the difficult airway events. Lundstrom and colleagues reported a frequency of 0.15% in 91,297 participants (Lundstrom 2009). Failed intubation may be defined as "a maximum of three attempts at intubation; a fourth attempt by a more experienced colleague is permissible. If unsuccessful, a failed intubation should be declared and Plan B implemented" (DA Society 2015).
Because the definitions of the difficult airway are not standardized, the prevalence depends on the definition. For example, the Rose 1996 study used three definitions for difficulties during intubation. These are: poor view at laryngoscopy (Cormack and Lehane grade 3 to 4); three or more direct laryngoscopy attempts before insertion of the endotracheal tube; and failure to insert the endotracheal tube with direct laryngoscopy. The prevalence was 10.1%, 1.9%, and 0.1% respectively. The prevalence also depends on the circumstances of medical management, being more difficult in a prehospital setting (Adnet 1997). The Combes 2006 study found the prevalence of difficult tracheal intubation in a prehospital setting to be 7.4%.
Index test(s)
The difficult airway may be the result of obvious upper airway pathology or anatomical anomaly. When such upper airway distortion is obvious, the prudent practitioner will choose alternate plans for airway management. It is the unanticipated difficult airway in a patient without obvious airway pathology or anatomical anomaly that has fostered the search for diagnostic screening tests. These have most commonly been extensions of the physical examination of the patient, with a grading or scoring system for one or more particular attributes of the head, neck and mouth. Some of these particular attributes that are thought to be relevant for detection of the unanticipated difficult airway include the following (ASA 2013).
Distance between upper and lower incisors.
Length of the upper incisors.
Neck length.
Neck diameter.
Range of neck flexion and extension.
Shape of the palate.
Thyromental distance.
Tissue compliance of the submandibular space.
Relationship of maxillary and mandibular incisors during normal jaw closure.
Relationship of maxillary and mandibular incisors during voluntary protrusion of mandible.
Visibility of the uvula.
The most popular of these screening tests by airway physical examination include the following.
Mallampati test.
Modified Mallampati test.
Wilson risk score.
Thyromental distance.
Sternomental distance.
Mouth opening test.
Upper lip bite test.
See Table 2 for more details.
1. Index screening tests for the difficult airway.
| Test | Reference | Technique | Definition of positive response | Standard cut‐off in this review |
| Mallampati test | Mallampati 1985 | Quote: "Visibility of pharyngeal structures (faucial pillars, soft palate, and base of uvula) is noted by instructing the patient to open his/her mouth and protrude the tongue maximally while in the sitting position." | Class 1. Faucial pillars, soft palate, and uvula could be visualized Class 2. Faucial pillars and soft palate could be visualized, but uvula was masked by the base of the tongue Class 3. Only soft palate could be visualized This ordinal scale is dichotomized with assignment to Class 3 being the predictor of a DA. |
Class 1 and 2 versus Class 3 |
| Modified Mallampati test | Ezri 2001;Samsoon 1987 | Quote: "All the airway assessments were done by the same anaesthesiologist, in the sitting position, with the patient’s head in neutral position, mouth fully open, tongue fully extended, and without phonation." | Class 0. Ability to see any part of the epiglottis on mouth opening and tongue protrusion Class 1. Soft palate, fauces, uvula, pillars seen Class 2. Soft palate, fauces, uvula seen Class 3. Soft palate, base of uvula seen Class 4. Soft palate not seen at all This ordinal scale is dichotomized with assignment to Class 3 and 4 being the predictor of a DA. |
Class 0 to 2 versus Class 3 and 4 |
| Wilson risk score | Wilson 1988 | Risk factor criteria score Weight: < 90 kg (score 0), 90kg to 110 kg (score 1), > 110 kg (score 2) Head and neck movement: > 90 º (score 0), about 90 º (i.e. ± 10 º) (score 1), < 90 º (score 2) Jaw movement: I G ≥ 5 cm or SLux > 0 (score 0), IG < 5 cm and SLux = 0 (score 1), I G < 5 cm and SLux < 0 (score 2) Receding mandible: normal (score 0), moderate (score 1), severe (score 2) Buck teeth: normal (score 0), moderate (score 1), severe (score 2) |
The maximum possible score is 10. Higher scores are considered to be predictive of a DA. The chosen cut‐off points have been > 2 or > 4. | > 2 |
| Thyromental distance | Lewis 1994 | The distance between the mentum and the hyoid bone (alternatively thyroid cartilage) is measured in cm or finger widths. There is considerable variation in performance of this examination. Patient position (sitting versus supine), neck position (extension versus neutral), and proximal endpoint (inside mentum versus outside mentum) are not standardized. | Shorter distances are considered to be predictive of a DA. The chosen cut‐off points have been < 4 cm, 6 cm, 6.5 cm, 7 cm or < 3 finger widths. | 6.5 cm |
| Sternomental distance | Ramadhani 1996 | Quote: "...sternomental distance was measured as the straight distance between the upper border of the manubrium sterni and the bony point of the mentum with the head in full extension and the mouth closed. A ruler was used and the distance measured was approximated to the nearest 0.5 cm." | Shorter distances are considered to be predictive of a DA. The chosen cut‐off points have been < 12.5 cm or 13.5 cm. | 12.5 cm |
| Mouth opening | Calder 2003 | The interdental distance between the upper and lower incisors is measured in mm. Neck position is a factor affecting maximum mouth opening. Neck position is not standardized. | Shorter distances are considered to be predictive of a DA. The chosen cut‐off points have been < 3.5 cm or < 2 finger widths. | 3.5 cm |
| Upper lip bite test | Khan 2003 | The patient is instructed to protrude their mandible forward and bite their upper lip. | Class I. Lower incisors bite the upper lip above the vermilion border, mucosa not being visible Class II. Lower incisors bite the upper lip below the vermilion border, mucosa partially visible Class III. Lower incisors fail to bite the upper lip This ordinal scale is dichotomized with assignment to Class III being a predictor of a DA. |
Class I and II versus III |
DA difficult airway; IG interincisor gap; SLux subluxation (maximal forward protrusion of the lower incisors beyond the upper incisors.
Clinical pathway
Before patients undergo surgery with general anaesthesia, it is common practice to screen for a difficult airway. This screening includes taking a medical history and identifying overt flags for the difficult airway, such as malformations or deformations. For these individuals, alternative methods of airway management are planned in advance. For the remaining apparently normal patients, there is still a risk of unanticipated difficult airway.
To further reduce the number of individuals with an unanticipated difficult airway, clinicians perform bedside airway physical examination tests. The results of these bedside tests help healthcare providers to plan different levels of alternative airway management. A difficult airway occurs in the early phases of general anaesthesia when airway management takes place.
With the exception of the Wilson risk score, each of these tests can be completed in five to 15 seconds; the Wilson risk score also requires information about the patient's weight. Two tests, Mallampati and thyromental distance, have been combined in some reports of screening tests. The performance of these tests by different examiners can have large interobserver variability. The Karkouti 1996 study had two observers independently perform an airway physical examination with 10 characteristics in 59 patients, including some of the specific tests in Table 2. The poorest test performance was with the Mallampati, with classification of patients having only a fair agreement between the observers (Kappa coefficient 0.31). The difficulty in achieving repeatability of airway classification may explain some of the skepticism about using the index tests before surgery.
Rationale
The serious morbidity and mortality associated with unsuccessfully managed upper airway was recognized decades ago. This prompted the standard use of pulse oximetry and capnography during anaesthesia and emergency care. In addition, learned societies, in particular the ASA and the Difficult Airway Society, have promulgated guidelines for management of the difficult airway (ASA 2013; DA Society 2015). There is indirect evidence from the ASA's closed claims analysis that claims for death and brain damage during the induction of anaesthesia have decreased between the years 1985 to 1992 and 1993 to 1999 (Peterson 2005). Also, the Berkow 2009 study reported a reduction in the need for an emergent surgical airway via tracheostomy through the introduction of a comprehensive difficult airway programme. These improvements in outcomes have been ascribed to standardized airway examination, improved monitoring, new airway devices and technology, and practice guidelines. Specifically, significant advances in the availability of robust video laryngoscopy equipment and other airway devices, such as laryngeal mask airways, have dramatically increased the techniques available for patients with a difficult airway (Luba 2010; Pott 2008).
The role of screening tests and their benefits are still uncertain. Four systematic reviews of airway examination tests have been published (ASA 2003; Lee 2006; Lundstrom 2011; Shiga 2005). The ASA Taskforce concluded that "There is insufficient published evidence to evaluate the predictive value of multiple features of the airway physical examination versus single features in predicting the presence of a difficult airway" and "An airway physical examination should be conducted, whenever feasible, before the initiation of anaesthetic care and airway management in all patients" (ASA 2013); this report did not present a meta‐analysis. The Lee 2006 systematic review and meta‐analysis reported that "the Mallampati tests have limited accuracy for predicting the difficult airway and thus are not useful screening tests". The Lundstrom 2011 systematic review and meta‐analysis was limited to the modified Mallampati score only. Their conclusion was "that the modified Mallampati score is inadequate as a stand‐alone test of a difficult laryngoscopy or tracheal intubation". The Shiga 2005 systematic review and meta‐analysis of six airway screening tests found that "the clinical value of bedside screening tests for predicting difficult intubation remains limited". Nevertheless, an airway physical examination is still recommended (ASA 2003; ASA 2013). For example, airway examination may be useful in order to select the patients for which newer devices are most likely to be useful.
Since the previous systematic reviews, new statistical methods for the meta‐analysis of diagnostic tests with correct handling of the dependency structure of such data are available. For example, the variability of the predictive performance of a diagnostic test in future patients can now be more correctly estimated. Additionally, more studies of large sample size have been published. This review will incorporate an up‐to‐date literature search and new statistical methods to establish the diagnostic properties of airway physical examination screening tests.
Objectives
The objective of this review was to characterize and compare the diagnostic accuracy of the Mallampati classification and other commonly used airway examination tests for assessing the physical status of the airway in adult patients with no apparent anatomical airway abnormalities. We performed this individually for each of the four descriptors of the difficult airway: difficult face mask ventilation, difficult laryngoscopy, difficult tracheal intubation, and failed intubation.
Methods
Criteria for considering studies for this review
Types of studies
We considered diagnostic test accuracy studies (case‐control or consecutive series) of any individual index test or a combination of the tests listed in Table 2 against a reference standard. We required studies to provide data for true positives, false positives, false negatives and true negatives. We excluded studies that were reported only in abstract form, were uncontrolled reports (case series, case reports), randomized controlled trials of test‐treatment design that are more appropriately analysed as intervention than as diagnostic test accuracy studies, and studies that examined an index test other than bedside tests (for example, those involving radiological imaging).
Participants
We included adults of either sex, aged 16 years or greater, without obvious airway abnormalities who were having laryngoscopy performed with a standard laryngoscope (usually size 3 Macintosh blade) and the trachea intubated with a styletted or non‐styletted tracheal tube. We excluded studies performed in populations with a high prevalence of abnormal airways (maxillofacial trauma, cervical spine trauma, or otorhinolaryngology tumours) or those performed using specialized laryngoscopes or techniques (for example, awake fibreoptic intubation).
Index tests
We included bedside tests used singly or in combination for detection of a difficult airway. These include any version of the Mallampati test (Ezri 2001; Mallampati 1985; Samsoon 1987), Wilson risk score (Wilson 1988), thyromental distance (Lewis 1994), sternomental distance (Ramadhani 1996), mouth opening test (Calder 2003), and upper lip bite test (Khan 2003), but were not limited to these tests. We collected information on the inter‐ or intraobserver correlation of the tests, or both, if reported or referenced in the study.
Target conditions
The target condition was difficult airway. Although the difficult airway does not have a reference standard other than the result of the actual attempted airway management for a patient, the 2003 practice guidelines of the American Society of Anesthesiologists (ASA), suggested using at least four descriptions of difficult airway events (ASA 2003), as follows.
Difficult face mask ventilation.
Difficult laryngoscopy.
Difficult tracheal intubation.
Failed intubation.
Reference standards
As outline above in Target condition being diagnosed, the reference standards were: difficult face mask ventilation, difficult laryngoscopy, difficult tracheal intubation, and failed intubation. As there were no standard definitions for the reference standards, we accepted the authors' definition used for each study.
Search methods for identification of studies
We performed electronic searches and searched other resources.
Electronic searches
The search is current to 16 December 2016. For identifying any eligible studies, we searched the following electronic databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 11), in the Cochrane Library (see Appendix 1).
Cochrane Register of Diagnostic Test Accuracy Studies
MEDLINE Ovid SP (1946 to 16 December 2016; see Appendix 2).
Embase Ovid SP (1874 to 16 December 2016; see Appendix 3).
ISI Web of Science (1950 to 16 December 2016; see Appendix 4).
CINAHL EBSCO host (1982 to 16 December 2016; see Appendix 5).
When searching the databases, we used both subject headings and free text terms. We adapted our MEDLINE search strategy for searching all other databases.
We also searched the following regional electronic bibliographic databases, subject‐specific databases, and dissertation and theses databases.
IndMED
KoreaMED
LILACS
Panteleimon
PASCAL
Google Scholar
Turning Research into Practice (TRIP) database
DissOnline
OpenSIGLE
We did not apply any language restrictions.
We performed a further search in March 2018. We have added those results to 'Studies awaiting classification' and we will incorporate them into the review at the next update.
Searching other resources
For identifying any additional published, unpublished and ongoing studies, we searched the Science Citation Index and checked the references of all the relevant studies. We also handsearched the following journals and proceedings of the following conferences.
Acta Anaesthesiologica Scandinavica (from 1995 to 29 December 2016).
British Journal of Anaesthesia (from 1995 to 29 December 2016).
Canadian Journal of Anesthesia (from 1995 to 29 December 2016).
Critical Care Medicine (from 1995 to 29 December 2016).
Intensive Care Medicine (from 1995 to 29 December 2016).
American Journal of Respiratory and Critical Care Medicine (from 1995 to 29 December 2016).
Abstracts from congresses of the European Society of Anaesthesiology (from 2004 to 29 December 2016).
Abstracts from the International Anesthesia Research Society (from 2000 to 29 December 2016).
ATS international conference proceedings (from 2008 to 29 December 2016).
International Symposium on Intensive Care and Emergency Medicine proceedings (from 1997 to 29 December 2016).
American Society of Anesthesiologists Annual Meeting proceedings (from 2000 to 29 December 2016).
We also searched guidelines by the French, Italian, Spanish and German Societies of Anaesthesiology and Intensive Care.
Data collection and analysis
Selection of studies
NLP, DR and HH independently, and in duplicate, performed selection of studies. We resolved disagreements by discussion or by involving AL as arbiter. We initially screened studies by the title and abstract and then retrieved full reports for potentially relevant studies. For these studies, we used a predefined electronic spreadsheet to assess and document studies for inclusion and exclusion according to the above selection criteria. We documented study selection in a flow chart (Liberati 2009; Figure 1).
1.

Study flow diagram.
Data extraction and management
We independently, and in duplicate, performed data extraction using a predefined electronic spreadsheet within the database, MS Access. We resolved disagreements by discussion or by involving AL or HH as arbiter. We then transferred data to Review Manager 5 (Review Manager 2014), Stata 14 (Stata 2015) and to R (R 2017), for further calculations.
Assessment of methodological quality
We independently, and in duplicate, performed assessment of methodological quality using a predefined electronic spreadsheet. We resolved disagreements by discussion or by involving AL or HH as arbiter. We used all four domains (Table 3), from the QUADAS‐2 tool (Whiting 2011), a revision of the original QUADAS tool (Whiting 2003), to assess the methodological quality of the included studies that is implemented in Review Manager 2014. This included the risk of bias with signalling questions and applicability judgement. We presented both a description and the judgement (coded 'yes', 'no', or 'unclear') for each signalling question. Additionally, we coded risk of bias and applicability as 'high', 'low', or 'unclear'.
2. Four domains for quality assessment.
| 1 |
Patient selection A. Risk of Bias Patient sampling description Signalling question 1: was a consecutive or random sample of patients enrolled? Signalling question 2: was a case‐control design avoided? Signalling question 3: did the study avoid inappropriate exclusions? (Criteria met if the study did not exclude patients due to methods unusual in clinical practice, i.e. performed examination tests before study inclusion) Signaling questions reported as yes, no, unclear Could the selection of patients have introduced bias? Risk of bias judged as low, high, or unclear B. Concerns regarding applicability Are there concerns that the included patients and setting do not match the review question? (Criteria met if the study sample did not correspond to the patient population encountered in daily clinical practice of airway management in apparently normal patients) Concerns about applicability reported as high, low, or unclear |
| 2 |
Index test A. Risk of bias Description of index test and how it was conducted and interpreted Signalling question 1: were the index test results interpreted without knowledge of the results of the reference standard? (Criteria met if index test and reference standard were conducted by different persons) Signalling question 2: if a threshold was used, was it prespecified? Signalling questions reported as yes, no, unclear Could the conduct or interpretation of the index test have introduced bias? Risk of bias judged as low, high, or unclear B. Concerns regarding applicability Are there concerns that the index test, its conduct, or interpretation differed from the review question? (Applied to "non‐bedside" tests, i.e. tests which require imaging techniques, etc.) Concerns about applicability reported as high, low, or unclear |
| 3 |
Reference standard A. Risk of bias Describe condition and reference standard(s) Signalling question 1: are the reference standards likely to correctly classify the target condition? (Criteria met if the study used reference standards as defined in the review) Signalling question 2: were the reference standards interpreted without knowledge of the results of the index test? (Criteria met if index test and reference standard were conducted by different persons) Signalling questions reported as yes, no, unclear Could the reference standard, its conduct, or its interpretation have introduced bias? Risk of bias judged as low, high, or unclear B. Concerns regarding applicability Are there concerns that the target condition as defined by the reference standard does not match the review question? Concerns about applicability reported as high, low, or unclear |
| 4 |
Flow and timing A. Risk of bias Describe any patients who did not receive index tests or reference standard or was excluded from 2 x 2 table Describe the interval and interventions between the index test and the reference standard Signalling question 1: was there an appropriate interval between index tests and reference standard? (Usually not a problem in this review. Considered appropriate if index tests and reference standards were conducted within a usual time‐span in clinical practice, e.g. during pre‐anaesthesia visit or within same hospital stay) Signalling question 2: did all patients receive the same reference standard? Signalling question 3: were all patients included in the analysis? Signalling questions reported as yes, no, unclear Could the patient flow have introduced bias? Risk of bias judged as low, high, or unclear |
We piloted the quality checklist independently on a sample of five papers and refined the checklist before proceeding further. When necessary, we contacted authors of original studies for information on unclear quality items.
We have presented the items on methodological quality assessments in methodological quality summary figuress 12 to 15 in the Results section. In addition, we have presented methodological quality graphs showing the relative distribution of methodological quality assessments for each included study in Appendix 6.
Statistical analysis and data synthesis
For each included study, we treated the index test results as separate binary classifiers; we recorded the cutpoint for dichotomization. The included studies reported one or more difficult airway events.
We separately tallied each type of reported difficult airway event. We collected details on definitions of positive and negative reference standard responses. We constructed 2×2 tables of test and reference standard results to show the cross‐classification of difficult airway status and test outcome. In studies where multiple index tests were performed, we also constructed a series of 2×2 tables where the results of investigations were combined, provided that they were derived from the total study population, and that the definition of a positive result for combined tests was reported.
We used sensitivity and specificity of each test or test combination as the underlying parameter in our calculations. As healthcare providers want to avoid false negatives, we considered sensitivity as the most important property when comparing diagnostic accuracy between tests: overlooking a person at high risk for a difficult airway event may be potentially life‐threatening during anaesthesia. False positives on the other hand, have less severe implications in this scenario. To describe and visualize the data, we produced forest plots showing pairs of sensitivity and specificity together with 95% confidence intervals (CIs) from each study in Review Manager 2014. We presented data for all eligible studies on forest plots, but included only cohort type studies in the meta‐analyses to minimise the risk of bias. We meta‐analysed pairs of sensitivity and specificity using a generalized linear mixed model approach to perform a bivariate meta‐analysis of sensitivity and specificity (Chu 2006).
We primarily performed meta‐analyses for pooling estimates using the 'lme4' package in R (R 2017). From this package we used the bivariate binomial method using the glmer function. We presented results as sensitivity and specificity, as from the bivariate estimates (logit transformed) with 95% CIs.
We produced a specificity versus sensitivity plot showing the study estimates of individual studies, the summary receiver operating characteristic (ROC) point (summary values for sensitivity and specificity) and the 95% confidence region around the summary ROC point.
We indirectly compared index tests and index test combinations by including a covariate for test type in bivariate models (i.e. meta‐regression) using methods suggested by Partlett and Takwoingi (Partlett 2016). For pairwise, between‐index‐test difference comparisons, we used a bivariate mixed effects regression model to test the joint null hypothesis of no difference in sensitivity and specificity between two index tests as calculated in the models described above. We formally compared models using a likelihood ratio test. If we rejected the joint null hypothesis, we individually compared sensitivity and specificity. We present differences only for test comparison pairs where sufficient data were available and where models converged.
Investigations of heterogeneity
To explore heterogeneity, we considered patient demographics (e.g. age, sex, weight); the indication for airway management (e.g. elective surgery, emergent surgery, critical illness, trauma, resuscitation); and different standards for declaring a difficult airway as potential covariates in a bivariate model (Whiting 2011).
Sensitivity analyses
We assessed the impact of study design on our findings by excluding case‐control studies. We assessed the impact of the risk of bias due to lack of blinding by excluding studies where the results of the index tests were not blinded.
Assessment of reporting bias
Testing for reporting bias and small study effects may not be especially useful in the context of studies of diagnostic tests (Begg 2005), therefore, we did not present analyses on reporting bias.
Results
Results of the search
We searched up to 16 December 2016. Our search yielded a total of 12,277 papers after combining search results from all sources and after removing duplications. Based on independent title and abstract evaluations, we excluded 11,779 references and retrieved the full text for 498 references. After careful evaluation, we excluded another 365 studies (Figure 1). The studies we excluded because of insufficient data are reported in the 'Characteristics of excluded studies' tables. After detailed assessments, we included 133 studies involving 844,206 participants (Figure 1).
From an updated search in March 2018, we have added 27 study reports to 'Characteristics of studies awaiting classification' tables.
The 133 studies evaluated a total of seven different prespecified test strategies, as well as 69 non‐prespecified, and 32 combinations (Table 4). For the prespecified index tests, we found six studies for the Mallampati test, 105 for the modified Mallampati test, six for the Wilson risk score, 52 for thyromental distance, 18 for sternomental distance, 34 for the mouth opening test and 30 for the upper lip bite test. A total of 42 studies evaluated one individual test, 36 studies evaluated two tests, 21 studies evaluated three tests, and 36 studies evaluated four to 12 tests. Eberhart 2005 reported interobserver correlation (IOC) for the upper lip bite test (IOC = 0.79), and for the modified Mallampati test (IOC = 0.59). None of the studies reported intraobserver correlations.
3. Non‐prespecified tests and combinations of screening tests for the difficult airway.
| Test | References | Main characteristics |
| Combination of ULBT and MMT | Allahyary 2008 | ULBT and MMT, if any single test positive combination considered positive |
| Combination of MMT, TM distance, anatomical abnormalities, head movement | Ambesh 2013 | MMT, TM distance, anatomical abnormalities, head movement MMT 1 to 4 points, all others 0 or 1 point > 3 points: considered positive |
| Telemedicine ASA checklist | Applegate 2013 | ASA 11‐point checklist; 2 or more points: considered positive |
| ASA checklist | Applegate 2013 | ASA 11‐point checklist; 2 or more points: considered positive |
| Prayer's sign | Baig 2014 | Patients not able to do praying gesture considered positive |
| Combination of mouth opening test, TM distance, SM distance, MMT, atlanto‐occipital extension | Basaranoglu 2010 | Mouth opening, TM distance, SM distance, atlanto‐occipital extension, MMT combination cut‐off not defined |
| Calder test | Basunia 2013 | Protrusion of lower jaw not possible: considered positive |
| Delilkan test | Basunia 2013 | "While performing Delilkan's test the patient was asked to look straight ahead. The head was held in the neutral position. The index finger of the left hand of the observer was placed under the tip of the jaw, whereas the index finger of the right hand was placed on the patient's occipital tuberosity. The patient was now asked to look at the ceiling. If the left index finger became higher than the right, extension of the atlanto‐occipital joint was considered normal." |
| Combination of MMT and ULBT | Bhat 2007 | MMT and ULBT, if any single test positive combination considered positive |
| Neck mobility | Cattano 2004 | Grading I to IV, III and IV: considered positive |
| Cervical mobility | Chaves 2009 | < 90°: considered positive |
| El‐Ganzouri index test | Cortellazzi 2007 | Index assigning points to mouth opening, TM distance, MMT, neck movement, ability to prognatha, body weight, history of difficult tracheal intubation > 2: considered positive |
| Head mobility | Descoins 1994 | < 90°: considered positive |
| Cormack‐Lehane | Dohrn 2015 | III and IV: considered positive |
| Lower jaw protrusion | Domi 2009 | Not possible: considered positive |
| Irregular teeth | Domi 2009 | Presence of irregular teeth: considered positive |
| BMI | Domi 2009 | > 30: considered positive |
| Lower jaw length | Domi 2009 | < 9 cm: considered positive |
| Delilkan test | Domi 2009 | Same definition used as Basunia 2013 |
| Body weight | El‐Ganzouri 1996 | > 110 kg: considered positive |
| Neck movement | El‐Ganzouri 1996 | < 80°: considered positive |
| Neck movement | Ezri 2003a | < 90°: considered positive |
| Abnormal upper teeth | Ezri 2003b | Presence of irregular teeth: considered positive |
| Neck movement | Ezri 2003b | < 90°: considered positive |
| Combination of MMT and TM distance | Frerk 1991 | MMT and TM distance, any positive considered positiveif any single test positive combination considered positive |
| Cormack‐Lehane | Freund 2012 | III and IV: considered positive |
| Receding mandible | Fritscherova 2011 | Presence: considered positive |
| LEMON | Hagiwara 2015 | At least one positive: considered positiveif any single item positive test considered positive |
| Head movement | Hashim 2014 | < 35°: considered positive |
| Palm print sign | Hashim 2014 | "Deficiency in the inter‐phalangeal areas of second to fifth digit" |
| Prayer sign | Hashim 2014 | A gap observed between the palms |
| Combination of ULBT and MMT | Healy 2016 | ULBT and MMT, if any single test positive combination considered positive |
| Combination of MMT and TM distance | Healy 2016 | MMT and TM distance, if any single test positive combination considered positive |
| Combination of ULBT and MMT | Honarmand 2008 | ULBT and MMT, if any single test positive combination considered positive |
| Combination of MMT and TM distance | Ittichaikulthol 2010 | MMT and TM distance, if any single test positive combination considered positive |
| Neck movement | Juvin 2003 | < 80°: considered positive |
| Mandibular recession | Juvin 2003 | Presence: considered positive |
| Abnormal teeth | Juvin 2003 | Buck/missing tooth: considered positive |
| Hyomental distance | Kalezic 2016 | < 5.3 cm: considered positive |
| Own score | Kalezic 2016 | Including gender, age, BMI, MMT, hyomental distance |
| Acromioaxillosuprasternal notch index | Kamranmanesh 2013 | < 0.5 considered positive |
| Combination of mouth opening and ULBT | Khan 2009a | Mouth opening and ULBT, if any single test positive combination considered positive |
| Combination of SM distance and ULBT | Khan 2009a | SM distance and ULBT, if any single test positive combination considered positive |
| Combination of mouth opening and SM distance | Khan 2009a | Mouth opening and SM distance, if any single test positive combination considered positive |
| Mandible length | Khan 2011 | < 9 cm: considered positive |
| TM distance | Khan 2011 | < 6.5 cm: considered positive |
| Combination of mandible length and TM distance | Khan 2011 | Mandible length and TM distance, if any single test positive combination considered positive |
| Combination of mouth opening and ULBT | Khan 2014 | Mouth opening and ULBT, if any single test positive combination considered positive |
| Cormack‐Lehane | Kim 2011 | III and IV: considered positive |
| Combination of Cormack‐Lehane and history | Kim 2011 | Cormack‐Lehane and history of difficult tracheal intubation, if any single test positive combination considered positive |
| Cormack‐Lehane | Knudsen 2014 | III and IV: considered positive |
| Modified Cormack‐Lehane | Koh 2002 | IIb, III, IV: considered positive |
| Mandible length | Kolarkar 2015 | < 9 cm: considered positive |
| Combination of mandible length and hyomental distance | Kolarkar 2015 | Mandible length and hyomental distance, if any single test positive combination considered positive |
| Combination of mandible length and TM distance | Kolarkar 2015 | Mandible length and TM distance, if any single test positive combination considered positive |
| Subjective anticipation | Langeron 2000 | Subjective anticipation of difficult tracheal intubation by anaesthesiologist |
| Beard | Langeron 2000 | Presence: considered positive |
| Lack of teeth | Langeron 2000 | Lack of teeth: considered positive |
| Receding mandible | Langeron 2000 | Presence: considered positive |
| Macroglossia | Langeron 2000 | Presence: considered positive |
| Cormack‐Lehane | Langeron 2000 | III and IV: considered positive |
| Combination of ULBT and MMT | Mashour 2008 | ULBT and MMT, if any single test positive combination considered positive |
| Mandible length | Merah 2004 | < 9 cm: considered positive |
| Bellhouse | Montemayor‐Cruz 2015 | III, IV: considered positive |
| Patil Aldreti | Montemayor‐Cruz 2015 | III: considered positive |
| Short neck | Prakash 2013 | Not defined |
| Mandibular protrusion | Prakash 2013 | Limited protrusion: considered positive |
| Neck movement | Prakash 2013 | < 80°: considered positive |
| Snoring | Prakash 2013 | History of snoring: considered positive |
| Beard | Prakash 2013 | Presence: considered positive |
| Receding mandible | Prakash 2013 | Presence: considered positive |
| Own score | Reghunathan 2016 | > 1.4: considered positive |
| Ratio of height to TM distance | Safavi 2014 | > 29: considered positive |
| Jaw excursion | Sahin 2011 | < 5°: considered positive |
| Mandibular protrusion | Savva 1994 | Lack: considered positive |
| Neck extension | Schmitt 2000 | < 80°: considered positive |
| Head and neck movement | Seo 2012 | < 90°: considered positive |
| Buck teeth | Seo 2012 | Presence: considered positive |
| Head movement | Shah 2013 | < 80°: considered positive |
| Mandibular length | Singh 2009 | < 9 cm: considered positive |
| Cormack‐Lehane | Soyuncu 2009 | III, IV: considered positive |
| Combination of hyomental distance and MMT | Tantri 2016 | Hyomental distance and MMT, if any single test positive combination considered positive |
| Combination of MMT and retrognathia | Tuzuner‐Oncul 2008 | MMT and retrognathia, if any single test positive combination considered positive |
| Combination of MMT and mouth opening | Tuzuner‐Oncul 2008 | MMT and mouth opening, if any single test positive combination considered positive |
| Combination of MMT, TM distance, SM distance, and mouth opening | Tuzuner‐Oncul 2008 | MMT and TM distance and SM distance and mouth opening, if any single test positive combination considered positive |
| Combination of MMT and history | Tuzuner‐Oncul 2008 | MMT and history of snoring, if any single test positive combination considered positive |
| Cormack‐Lehane | Tuzuner‐Oncul 2008 | III, IV: considered positive |
| Combination of MMT and TM distance | Tse 1995 | MMT and TM distance, if any single test positive combination considered positive |
| Lower jaw protrusion | Ul Haq 2013 | Grades A, B, C B and C: considered positive |
| Neck extension | K Nasa 2014 | < 80°: considered positive |
| Combination of MMT and TM distance | Wong 1999 | MMT and TM distance, if any single test positive combination considered positive |
| Mandibular luxation score | Wong 2009 | Grades A, B, C B and C: considered positive |
| Beard | Yildiz 2005 | Presence: considered positive |
| Mandibular protrusion | Yildiz 2007 | Grades A, B, C B and C: considered positive |
| Combination of MMT and mandibular protrusion | Yildiz 2007 | MMT and mandibular protrusion, if any single test positive combination considered positive |
| Combination of TM distance and mandibular protrusion | Yildiz 2007 | TM distance and mandibular protrusion, if any single test positive combination considered positive |
| Combination of MMT and SM distance | Yildiz 2007 | MMT and SM distance, if any single test positive combination considered positive |
| Combination of MMT and TM distance | Yildiz 2007 | MMT and TM distance, if any single test positive combination considered positive |
| Combination of MMT and mouth opening | Yildiz 2007 | MMT and mouth opening, if any single test positive combination considered positive |
| Combination of SM distance and mandibular protrusion | Yildiz 2007 | SM distance and mandibular protrusion, if any single test positive combination considered positive |
| Combination of mouth opening and hyomental distance | Yildiz 2007 | Mouth opening and hyomental distance, if any single test positive combination considered positive |
ASA: American Society of Anesthesiologists; BMI: body mass index; MMT: modified Mallampati test; SM: sternomental; TM: thyromental; ULBT: upper lip bite test; aPrognath: the ability to bring the jaw in a forward position so that the mandibular incisors are before the upper incisors.
Table 2 defines the cut‐off thresholds for index tests. Details on reported cut‐offs are presented in the 'Characteristics of included studies' tables. Overall, we did not consider variations of cut‐offs to be clinically important.
Eighteen comparisons (7 studies) defined the target condition as: difficult face mask ventilation; 218 comparisons (92 studies) as difficult laryngoscopy; 72 comparisons (50 studies) as difficult tracheal intubation; and two comparisons (two studies) as failed intubation.
The median number of participants per study was 380, with an interquartile range (IQR) from 200 to 662. The median (IQR) percentage of females included in the studies was 53% (44% to 64%). The median (IQR) age of the participants was 45 years (39 to 52). The median (IQR) body mass index (BMI) was 27.3 kg/m2(24.8 to 30.0). All studies, apart from two (Freund 2012; Soyuncu 2009), performed airway management in the operating theatre; the Freund 2012 study involved airway management in ambulance cars and the Soyuncu 2009 study in an emergency department. We did not subgrouped studies according to where the study took place. The characteristics of the individual studies are described in the 'Characteristics of included studies' tables.
Methodological quality of included studies
We report the details for individual study quality in the 'Characteristics of included studies' tables. Due to the complex structure of the review (multiple combinations of index tests and reference standards reported within individual studies), we were not able to use Review Manager 5 in‐built features to report all the risk of bias domains and applicability concerns for each study in the 'Characteristics of included studies' tables (Review Manager 2014).
We judged the risk of bias to be variable, across all studies, for the different domains; with mostly low risk of bias observed with patient selection, flow and timing, and mostly unclear risk of bias with reference standard and index test. We judged applicability concerns to be low for all domains. Most of the included studies were cohort type studies, only six of the included studies were case‐control type studies (Connor 2011; Frerk 1996; Fritscherova 2011; Naguib 1999; Naguib 2006; Nath 1997). Given the nature of the setting, and the test, we did not observe partial or differential verification in any of the studies.
For difficult laryngoscopy, the reference standard was performed blinded in 42, non‐blinded in six, and blinding was unclear in 43 studies. For difficult tracheal intubation, the reference standard was performed blinded in 11, non‐blinded in eight, and blinding was unclear in 29 studies. For difficult face mask ventilation, the reference standard was performed blinded in one, non‐blinded in one and blinding was unclear in five studies. For failed intubation, the reference standard was performed blinded in none, non‐blinded in none and blinding was unclear in three studies. The index test was blinded in all studies investigating prespecified index tests as expected. Among alternative tests or test combinations, eight studies had non‐blinded index tests (Fritscherova 2011; Gonzalez 2008; Hagiwara 2015; Kim 2011; Langeron 2000; Nath 1997; Wilson 1988; Wong 1999). All studies evaluated the index test before the reference standard, except for the Fritscherova 2011 study, which performed the index test the day after intubation. Ninety‐five studies included all participants in the analysis. We found incomplete or unclear reporting in 40 studies.
For a graphical summary of the risk of bias and applicability, see the graphs in Appendix 6. For a summary for each difficult airway component, refer to Figure 2 for difficult laryngoscopy; Figure 3 for difficult tracheal intubation; Figure 4 for failed intubation; and Figure 5 for difficult face mask ventilation.
2.

Risk of bias and applicability concerns graph for difficult laryngoscopy: review authors' judgements about each domain presented as percentages across included studies.
3.

Risk of bias and applicability concerns graph for difficult tracheal intubation: review authors' judgements about each domain presented as percentages across included studies.
4.

Risk of bias and applicability concerns graph for failed intubation: review authors' judgements about each domain presented as percentages across included studies.
5.

Risk of bias and applicability concerns graph for difficult face mask ventilation: review authors' judgements about each domain presented as percentages across included studies.
Findings
The median (IQR) prevalence for difficult laryngoscopy, difficult tracheal intubation, difficult face mask ventilation, and failed intubation was 11% (6% to 19%), 13% (5% to 16%), 6% (5% to 25%) and 0.6% (0.3% to 0.9%), respectively.
We were able to perform meta‐analyses for 11 comparisons (all 7 prespecified index tests for difficult laryngoscopy; modified Mallampati test, thyromental distance and mouth opening test for difficult tracheal intubation; modified Mallampati test for difficult face mask ventilation). We did not perform meta‐analyses of studies with the Mallampati test, Wilson risk score, sternomental distance or upper lip bite test for difficult tracheal intubation; studies with thyromental distance, upper lip bite test or mouth opening test for difficult face mask ventilation; or studies with the modified Mallampati test for failed intubation because only one or two studies were available. For the remaining comparisons, we did not find any studies. All studies that we included in the meta‐analyses used one clinically identical cut‐off value per test. See Table 1 for key findings.
Difficult laryngoscopy
For the Mallampati test, there were six studies involving 2165 participants with 153 cases of difficult laryngoscopy (Data table 1). Sensitivity varied from 0.05 to 0.85, and specificity from 0.65 to 0.98. We estimated a summary sensitivity of 0.40 (95% confidence interval (CI) 0.16 to 0.71) and a summary specificity of 0.89 (95% CI 0.75 to 0.96).
1. Test.
Mallampati test: difficult laryngoscopy.
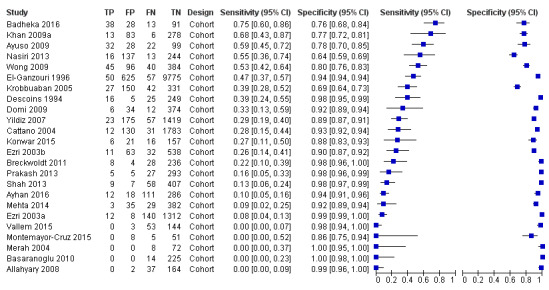
For the modified Mallampati test, there were 80 studies involving 232,939 participants with 10,545 cases of difficult laryngoscopy (Data table 3). Both sensitivity and specificity varied from 0.00 to 1.00. We estimated a summary sensitivity of 0.53 (95% CI 0.47 to 0.59) and a summary specificity of 0.80 (95% CI 0.74 to 0.85). See Figure 6.
3. Test.
Modified Mallampati test: difficult laryngoscopy.
6.

Forest plot of modified Mallampati test for difficult laryngoscopy, sorted by descending sensitivity. Summary sensitivity 0.53 (95% confidence interval (CI) 0.47 to 0.59); summary specificity 0.80 (95% CI 0.74 to 0.85).
For the Wilson risk score, there were five studies involving 5862 participants with 145 cases of difficult laryngoscopy (Data table 7). Sensitivity varied from 0.00 to 0.75, and specificity from 0.86 to 0.99. We estimated a summary sensitivity of 0.51 (95% CI 0.40 to 0.61) and a summary specificity of 0.95 (95% CI 0.88 to 0.98).
7. Test.
Wilson risk score: difficult laryngoscopy.
For thyromental distance, there were 42 studies involving 33,189 participants with 2364 cases of difficult laryngoscopy (Data table 9). Sensitivity varied from 0.03 to 1.00, and specificity from 0.08 to 0.99. We estimated a summary sensitivity of 0.37 (95% CI 0.28 to 0.47) and a summary specificity of 0.89 (95% CI 0.84 to 0.93). See Figure 7.
9. Test.
Thyromental distance: difficult laryngoscopy.
7.

Forest plot of thyromental distance for difficult laryngoscopy, sorted by descending sensitivity. Summary sensitivity 0.37 (95% CI 0.28 to 0.47); summary specificity 0.89 (95% CI 0.84 to 0.93).
For sternomental distance, there were 16 studies involving 12,211 participants with 762 cases of difficult laryngoscopy (Data table 12). Sensitivity varied from 0.00 to 0.84, and specificity from 0.71 to 1.00. We estimated a sensitivity of 0.33 (95% CI 0.16 to 0.56) and a specificity of 0.92 (95% CI 0.86 to 0.96).
12. Test.
Sternomental distance: difficult laryngoscopy.
For the mouth opening test, there were 24 studies involving 22,179 participants with 1220 cases of difficult laryngoscopy (Data table 14). Sensitivity varied from 0.00 to 0.75, and specificity from 0.64 to 1.00. We estimated a summary sensitivity of 0.22 (95% CI 0.13 to 0.33) and a summary specificity of 0.94 (95% CI 0.90 to 0.97). See Figure 8.
14. Test.
Mouth opening: difficult laryngoscopy.
8.
Forest plot of mouth opening for difficult laryngoscopy, sorted by descending sensitivity. Summary sensitivity 0.22 (95% CI 0.13 to 0.33); summary specificity 0.94 (95% CI 0.90 to 0.97).
For the upper lip bite test, there were 27 studies involving 19,609 participants with 1998 cases of difficult laryngoscopy (Data table 17). Sensitivity varied from 0.02 to 1.00, and specificity from 0.00 to 1.00. We estimated a summary sensitivity of 0.67 (95% CI 0.45 to 0.83) and a summary specificity of 0.92 (95% CI 0.86 to 0.95). See Figure 9.
17. Test.
Upper lip bite test: difficult laryngoscopy.
9.

Forest plot of upper lip bite test for difficult laryngoscopy, sorted by descending sensitivity. Summary sensitivity 0.67 (95% CI 0.45 to 0.83); summary specificity 0.92 (95% CI 0.86 to 0.95).
Forty‐two studies reported non‐prespecified index tests or index test combinations involving 230,680 participants with 7197 cases of difficult laryngoscopy (Data table 20). Both sensitivity and specificity varied from 0.00 to 1.00. We did not perform a meta‐analysis on these combinations, as outlined above.
20. Test.
Combination of tests: difficult laryngoscopy.
We were able to formally compare four index tests for difficult laryngoscopy. The upper lip bite test had the highest sensitivity, which was significantly different from mouth opening (P < 0.001). The modified Mallampati test showed a significantly higher sensitivity compared to thyromental distance (P = 0.012) and mouth opening (P < 0.001).
Mouth opening had the highest specificity, which was significantly different from the modified Mallampati test (P < 0.001). The modified Mallampati test had significantly lower specificity than the upper lip bite test (P = 0.007), and thyromental distance (P = 0.037). See Figure 10 for a graphical display. We were unable to calculate test comparisons for other test combinations given the lack of data.
10.

Summary receiver operating characteristic (ROC) plot of modified Mallampati test, thyromental distance, mouth opening, and upper lip bite test for difficult laryngoscopy. For each index test, the summary point with the 95% confidence region is displayed.
Difficult tracheal intubation
For the Mallampati test, there was only one study (500 participants) with 40 cases of difficult tracheal intubation (Data table 2). Sensitivity in this study was 0.42 (95% CI 0.27 to 0.59), and specificity was 0.93 (95% CI 0.90 to 0.95).
2. Test.
Mallampati test: difficult tracheal intubation.
For the modified Mallampati test, there were 24 studies involving 191,849 participants with 6615 cases of difficult tracheal intubation (Data table 5). Sensitivity varied from 0.19 to 0.91, and specificity from 0.62 to 0.98. We estimated a summary sensitivity of 0.51 (95% CI 0.40 to 0.61) and a summary specificity of 0.87 (95% CI 0.82 to 0.91). See Figure 11.
5. Test.
Modified Mallampati test: difficult tracheal intubation.
11.

Forest plot of modified Mallampati test for difficult tracheal intubation, sorted by descending sensitivity. Summary sensitivity 0.51 (95% CI 0.40 to 0.61); summary specificity 0.87 (95% CI 0.82 to 0.91).
For the Wilson risk score, there was only one study (123 participants) with 17 cases of difficult tracheal intubation (Data table 8). Sensitivity in this study was 0.47 (95% CI 0.23 to 0.72), and specificity was 0.92 (95% CI 0.84 to 0.96).
8. Test.
Wilson risk score: difficult tracheal intubation.
For sternomental distance, there were two studies (864 participants) with 115 cases of difficult tracheal intubation (Data table 13). Sensitivity varied from 0.31 to 0.60, and specificity from 0.63 to 0.90. We did not perform a meta‐analysis on these combinations, as outlined above.
13. Test.
Sternomental distance: difficult tracheal intubation.
For thyromental distance, there were 10 studies involving 5089 participants with 437 cases of difficult tracheal intubation (Data table 11). Sensitivity varied from 0.06 to 0.78, and specificity from 0.63 to 0.98. We estimated a summary sensitivity of 0.24 (95% CI 0.12 to 0.43) and a summary specificity of 0.90 (95% CI 0.80 to 0.96). See Figure 12.
11. Test.
Thyromental distance: difficult tracheal intubation.
12.

Forest plot of thyromental distance for difficult tracheal intubation, sorted by descending sensitivity. Summary sensitivity 0.24 (95% CI0.12 to 0.43); summary specificity 0.90 (95% CI 0.80 to 0.96).
For the upper lip bite test, there were two studies (598 participants) with 121 cases of difficult tracheal intubation (Data table 19). Sensitivity varied from 0.34 to 0.91, and specificity from 0.93 to 0.96. We did not perform a meta‐analysis on these combinations, as outlined above.
19. Test.
Upper lip bite test: difficult tracheal intubation.
For mouth opening, there were 9 studies involving 6091 participants with 607 cases of difficult tracheal intubation (Data table 16). Sensitivity varied from 0.00 to 0.51, and specificity from 0.76 to 0.99. We estimated a summary sensitivity of 0.27 (95% CI 0.16 to 0.41) and a summary specificity of 0.93 (95% CI 0.87 to 0.96). See Figure 13.
16. Test.
Mouth opening: difficult tracheal intubation.
13.

Forest plot of mouth opening for difficult tracheal intubation, sorted by descending sensitivity. Summary sensitivity 0.27 (95% CI 0.16 to 0.41); summary specificity 0.93 (95% Cl 0.87 to 0.96).
Fifteen studies reported non‐prespecified index tests or index test combinations involving 11,089 participants with 1030 cases of difficult tracheal intubation (Data table 22). Sensitivity varied from 0.00 to 0.92, and specificity from 0.48 to 1.00. We did not perform a meta‐analysis on these combinations, as outlined above.
22. Test.
Combination of tests: difficult tracheal intubation.
We were able to formally compare three index tests for difficult tracheal intubation. The modified Mallampati test had the highest sensitivity. It was significantly higher than the mouth opening test (P < 0.001) and thyromental distance (P < 0.001). Sensitivity was not significantly different between mouth opening and thyromental distance (P = 0.07).
The mouth opening test showed the highest specificity, which was higher than the thyromental distance and the modified Mallampati test. Specificity was significantly different for all test comparisons ( P < 0.001). See Figure 14 for a graphical display. We were unable to calculate test comparisons for other test combinations, given the lack of data.
14.

Summary receiver operating characteristic (ROC) plot of modified Mallampati test, thyromental distance, and mouth opening test for difficult tracheal intubation. For each index test the summary point with the 95% confidence region is displayed.
Difficult face mask ventilation
For the modified Mallampati test, there were six studies involving 56,323 participants with 493 cases of difficult face mask ventilation (Data table 4). Sensitivity varied from 0.00 to 0.36, and specificity from 0.80 to 0.99. We estimated a summary sensitivity of 0.17 (95% CI 0.06 to 0.39) and a summary specificity of 0.90 (95% CI 0.81 to 0.95). See Figure 15.
4. Test.
Modified Mallampati test: difficult face mask ventilation.
15.

Forest plot of modified Mallampati test for difficult face mask ventilation, sorted by descending sensitivity. Summary sensitivity 0.17 (95% CI 0.06 to 0.39); summary specificity 0.90 (95% CI 0.81 to 0.95).
For thyromental distance, there was only one study (53,041 participants) with 77 cases of difficult face mask ventilation (Data table 10). Sensitivity in this study was 0.13 (95% CI 0.06 to 0.23), and specificity was 0.94 (95% CI 0.94 to 0.95).
10. Test.
Thyromental distance: difficult face mask ventilation.
For the upper lip bite test, there was only one study (200 participants) with 56 cases of difficult face mask ventilation (Data table 18). Sensitivity in this study was 0.75 (95% CI 0.62 to 0.86), and specificity was 0.60 (95% CI 0.51 to 0.68).
18. Test.
Upper lip bite test: difficult face mask ventilation.
For mouth opening, there were two studies (53,469 participants) with 370 cases of difficult face mask ventilation (Data table 15). Sensitivity was 0.06 in both studies, and specificity ranged from 0.91 to 0.96. We did not perform a meta‐analysis on these combinations, as outlined above.
15. Test.
Mouth opening: difficult face mask ventilation.
Four studies reported non‐prespecified index tests or index test combinations (10,819 participants) with 655 cases of difficult face mask ventilation (Data table 21). Sensitivity varied from 0.04 to 0.81, and specificity from 0.27 to 0.97. We did not perform a meta‐analysis on these combinations, as outlined above.
21. Test.
Combination of tests: difficult face mask ventilation.
Failed intubation
For the modified Mallampati test, there were two studies (485 participants) with three cases of failed intubation (Data table 6). Sensitivity was 0.00 in one study and not estimable due to a lack of cases (reference standard positives) in the other study. Specificity varied from 0.80 to 0.94. We did not perform a meta‐analysis on these combinations, as outlined above.
6. Test.
Modified Mallampati test: failed intubation.
Sensitivity analyses
We performed sensitivity analyses for study design and lack of blinding of index test results; we found no effect on our findings.
Heterogeneity
For non‐prespecified index tests or index test combinations we did not perform a meta‐analysis because of the large clinical heterogeneity in terms of differences in test properties. For all index tests where pooling was possible, we found high variability in the estimates.
Discussion
Summary of main results
There was limited to moderate accuracy in commonly used airway examination tests for assessing the physical status of the airway in adult patients with no apparent anatomical airway abnormality. There was a consistent pattern of wide variability in the ranges around the 50% sensitivity point. On the other hand, specificity was high with less variability across most of the tests. This applied likewise for all reference standards. Standard airway examination tests do not appear to work well as screening tests. The potential high rate of false negatives could lead to disastrous situations during induction of anaesthesia.
Overall, the quality of the estimates was moderate to high. The methodological quality was high for applicability and moderate to high for the risk of bias in the individual studies.
Among the tests under investigation (Table 1), the upper lip bite test had the highest sensitivity to foresee difficult laryngoscopy and was significantly better than the modified Mallampati test and the mouth opening test. For difficult tracheal intubation, there was insufficient information for the upper lip bite test. Here the modified Mallampati test had the highest sensitivity. For difficult tracheal intubation, there was no evidence of a difference in sensitivity between the mouth opening and thyromental distance tests. For face mask ventilation and failed intubation, there was insufficient information for test comparisons.
Strengths and weaknesses of the review
This review systematically summarized current evidence about standard bedside airway examination tests using up‐to‐date methodology from a total of 133 studies involving 844,206 patients. It updates the evidence described in a published systematic review (Lee 2006), and expands the scope of index tests beyond the Mallampati test. We attempted to conduct a comprehensive search for studies, but the fact that 27 studies have not yet been incorporated may be a source of potential bias. We designed our review to cover the most common bedside tests used in clinical routine practice globally. However, this resulted in a large number of comparisons, with varying numbers of studies with sufficient data. We therefore, can provide good quality evidence for a selected set of tests. Moreover, we found a large number of studies on test combinations which contained considerable heterogeneity, and prevented pooling in some cases. We also found some heterogeneity in the definition of index tests and target conditions, which might potentially result in a loss in precision in the estimates. In addition, we were not able to formally analyse the heterogeneity by demographics and the clinical setting such as anaesthesia, critically ill patient, major trauma, or cardiac arrest, where clinicians face very different conditions, sometimes with serious limitations to perform bedside tests.
The risk of bias in the studies, one aspect of quality of the evidence, was generally low. However, as expected, we noted an issue with blinding of the index test results when assessing the target condition in approximately half of the included studies, as in the clinical setting. Despite standardized outcome assessment instruments, this could explain the relatively high specificity compared to sensitivity if outcome assessors tended to classify the airway more frequently difficult when they knew that the bedside test predicted a difficult airway. However, this potential bias may also act in the opposite direction, i.e. better preparation due to knowledge of a potential difficult airway, leading to less problems in actual airway management. We therefore do not expect that this provides sufficient explanation for our results.
Applicability of findings to the review question
The included studies were generally performed in a broad range of standard clinical settings and are expected to apply to standard preoperative airway assessments done in apparently normal hospital patients internationally. This review covers a broad range of standard and routinely applied bedside tests. The outcomes comply with routine target conditions, such as difficult laryngoscopy and difficult tracheal intubation, which all healthcare professionals in the field are familiar with (ASA 2003). For some relevant target conditions, such as difficult face mask ventilation and failed intubation, data were too scarce to draw robust conclusions, and therefore the applicability is limited. As prespecified, this review includes only studies with clinical reference standards, such as difficult tracheal intubation or difficult face mask ventilation. We did not include studies deriving prediction tools solely from radiological imaging and other non‐clinical reference standards.
Authors' conclusions
Implications for practice.
Bedside airway examination tests for assessing the physical status of the airway in adult patients with no apparent anatomical airway abnormality are designed as screening tests. Screening tests are expected to have high sensitivities and depend less on specificity. We found that all the investigated examination tests had relatively low sensitivities with high variability. In contrast, specificities were consistently and markedly better than sensitivities across all tests. Standard airway examination tests do not appear to work well as screening tests. Although false negatives can result from bedside examination tests, it is important to put the risk of an unanticipated difficult airway into context. Whereas failure to predict both difficult face mask ventilation and difficult tracheal intubation could lead to disastrous clinical situations ("cannot intubate ‐ cannot ventilate"), unexpected isolated difficult laryngoscopy might be handled by face mask ventilation. Among the investigated tests, the upper lip bite test showed the most favourable diagnostic test accuracy properties.
The 27 studies in ‘Studies awaiting classification’ may alter the conclusions of the review once we have assessed them.
Implications for research.
Current bedside tests have limited accuracy. Therefore, research to develop tests with high sensitivities are needed to make them useful screening tests. Scarce information is available for difficult face mask ventilation and failed intubation, which are suitable target conditions to examine in future studies.
What's new
| Date | Event | Description |
|---|---|---|
| 7 March 2019 | Amended | Co‐publication Roth 2019 |
History
Protocol first published: Issue 12, 2010 Review first published: Issue 5, 2018
| Date | Event | Description |
|---|---|---|
| 4 October 2018 | Amended | Acknowledgement section amended to include Co‐ordinating Editor |
Acknowledgements
We would like to thank Jane Cracknell, Cochrane Anaesthesia Critical and Emergency Care Group (ACE) Managing Editor; Andrew Smith, ACE Content Editor; Peer Reviewers (Pierre Diemunsch, Haldun Akoglu, Subrahmanyan Radhakrishna); Janet Wale, Consumer Editor; Janne Vendt, Information Specialist who re‐ran the search in December 2016 and March 2018; the Diagnostic Test Accuracy (DTA) Editorial team and Peer Reviewers; and Marialena Trivella, ACE Statistical Editor. We would also like to thank the Co‐ordinating Editor Andrew Smith.
We would like to thank Alexander Hartmann who helped with data extraction for several papers. We thank Pablo Emilio Verde, Senior Researcher, University of Duesseldorf, Germany, for consultation about Bayesian methods. We would also like to thank Yemisi Takwoingi, School of Health and Population Sciences, University of Birmingham, for her help with the GLMM models in R. We would like to thank Zahid Hussain Khan, Professor of Anaesthesiology and Intensive Care at Tehran University of Medical Sciences, Iran, for providing additional information on study patients.
We would also like to thank Mathew Zacharias, ACE Content Editor; Mariska Leeflang, DTA Contact Editor; Pierre Diemunsch and Markus Weiss, ACE Peer Reviewers; and the DTA Peer Reviewers for their help and editorial advice during the preparation of the protocol for the review (Lee 2010).
This review was selected for the third Cochrane Review Support Programme.
Appendices
Appendix 1. Search strategy for CENTRAL, the Cochrane Library
#1 ((airway* near (test* or physical status or assess* or examinat*)) or ((distance or gap* or test* or length) near (interdental or sternomental or thyromental or interincisor* or incisor*)) or Wilson risk score or upper lip bite test or physical examin* test* or (length near upper incisor*) or (relat* and (maxillary or mandibular) and incisor*) or (visibility near uvula) or (shape near palate) or ((submandibular or mandibular) near space) or (neck near (length or thickness or diameter)) or (range and (motion or movement or flexion or extension) and (head or neck))) or mouth opening #2 MeSH descriptor Laryngoscopy explode all trees #3 MeSH descriptor Intubation, Intratracheal explode all trees #4 MeSH descriptor Bronchoscopy explode all trees #5 MeSH descriptor Laryngeal Masks explode all trees #6 MeSH descriptor Anesthesia, this term only #7 MeSH descriptor Laryngoscopes explode all trees #8 (difficult* near (airway or face mask or ventilation or laryngoscopy or intubation or tracheal)) or (intubat* near (fiberoptic or stylet* or retrograde or failed)) or (laryngeal mask* or airway access):ti,ab or ((styletted or unstyletted) near tube*):ti,ab or ((laryngoscope* or Macintosh) near blade*):ti,ab or airway management:ti,ab #9 (#2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8) #10 (#9 AND #1) #11 mallampati* or (difficult near intubation):ti,ab #12 (#10 OR #11)
Appendix 2. Search strategy for MEDLINE (Ovid SP)
1. ((airway* adj3 (test* or physical status or assess* or examinat*)) or ((distance or gap* or test* or length) adj5 (interdental or sternomental or thyromental or interincisor* or incisor*)) or Wilson risk score or upper lip bite test or physical examin* test* or (length adj3 upper incisor*) or (relat* and (maxillary or mandibular) and incisor*) or (visibility adj3 uvula) or (shape adj3 palate) or ((submandibular or mandibular) adj3 space) or (neck adj3 (length or thickness or diameter)) or (range and (motion or movement or flexion or extension) and (head or neck))).mp. or mouth opening.af. 2. exp Laryngoscopy/ or exp Intubation, Intratracheal/ or exp Bronchoscopy/ or exp Laryngeal Masks/ or Anesthesia/ or Laryngoscopes/ or (difficult* adj5 (airway or face mask or ventilation or laryngoscopy or intubation or tracheal)).mp. or (intubat* adj5 (fiberoptic or stylet* or retrograde or failed)).mp. or (laryngeal mask* or airway access).ti,ab. or ((styletted or unstyletted) adj3 tube*).ti,ab. or ((laryngoscope* or Macintosh) adj3 blade*).ti,ab. or airway management.ti,ab. 3. 1 and 2 4. mallampati*.af. or (difficult adj3 intubation).ti. 5. 3 or 4
Appendix 3. Search strategy for Embase (Ovid SP)
1. ((airway* adj3 (test* or physical status or assess* or examinat*)) or ((distance or gap* or test* or length) adj5 (interdental or sternomental or thyromental or interincisor* or incisor*)) or Wilson risk score or upper lip bite test or physical examin* test* or (length adj3 upper incisor*) or (relat* and (maxillary or mandibular) and incisor*) or (visibility adj3 uvula) or (shape adj3 palate) or ((submandibular or mandibular) adj3 space) or (neck adj3 (length or thickness or diameter)) or (range and (motion or movement or flexion or extension) and (head or neck)) or mouth opening).mp. 2. exp laryngoscopy/ or exp endotracheal intubation/ or exp bronchoscopy/ or exp laryngeal mask/ or anesthesia/ or laryngoscope/ or (difficult* adj5 (airway or face mask or ventilation or laryngoscopy or intubation or tracheal)).mp. or (intubat* adj5 (fiberoptic or stylet* or retrograde or failed)).mp. or (laryngeal mask* or airway access).ti,ab. or ((styletted or unstyletted) adj3 tube*).ti,ab. or ((laryngoscope* or Macintosh) adj3 blade*).ti,ab. or airway management.ti,ab. 3. 1 and 2 4. mallampati*.af. or (difficult adj3 intubation).ti. 5. 3 or 4
Appendix 4. Search strategy for ISI Web of Science
#1 TS=( mallampati* or Wilson risk score or Upper Lip Bite test or Mouth Opening or physical examin* test*) or TS=(airway* SAME (test* or physical status or assess* or examinat*)) or TS=((distance or gap* or test* or length) SAME (sternomental or thyromental or interincisor* or incisor*)) or TS=(relat* and (maxillary or mandibular) and incisor*) or TS=(Visibility SAME uvula) or TS=(Shape SAME palate) or TS=((submandibular or mandibular) SAME space) or TS=(neck SAME (length or thickness or diameter)) or TS=(range and (motion or movement or flexion or extension) and (head or neck)) #2 TS=(endotracheal intubation or bronchoscopy or laryngeal mask) or TS=(difficult* SAME (airway or face mask or ventilation or laryngoscopy or intubation or tracheal)) or TS=(Intubat* SAME (fiberoptic or stylet* or retrograde or failed)) or TS=(laryngeal mask* or airway access) or TS=((styletted or unstyletted) SAME tube*) or TS=((laryngoscope* or Macintosh) SAME blade*) or TI=anesthesia
#3 #2 AND #1
Appendix 5. Search strategy for CINAHL (EBSCO host)
S1 (MM "Physical Examination") S2 TX mallampati* or TX Wilson risk score or TX Upper Lip Bite test or TX Mouth Opening or TX physical examin* test* S3 airway* N3 (test* or physical status or assess* or examinat*) S4 ((distance or gap* or test* or length) N4 (sternomental or thyromental or interincisor* or incisor*)) S5 Length N3 upper incisor* S6 relat* and (maxillary or mandibular) and incisor* S7 Visibility N3 uvula S8 Shape N3 palate S9 ((submandibular or mandibular) N3 space) S10 (neck N3 (length or thickness or diameter)) S11 (range and (motion or movement or flexion or extension) and (head or neck)) S12 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 S13 (MM "Laryngoscopy") OR (MM "Intubation, Intratracheal") OR (MM "Bronchoscopy") OR (MM "Laryngeal Masks") OR (MH "Anesthesia+") S14 difficult* N4 (airway or face mask or ventilation or laryngoscopy or intubation or tracheal) S15 Intubat* N4 (fiberoptic or stylet* or retrograde or failed) S16 AB laryngeal mask* or AB airway access S17 ((styletted or unstyletted) N3 tube*) S18 ((laryngoscope* or Macintosh) N3 blade*) S19 S13 or S14 or S15 or S16 or S17 or S18 S20 S19 and S12
Appendix 6. Risk of bias and applicability concerns summary figures
Mallampati test Figure 38
16.

Risk of bias and applicability concerns summary for Mallampati test: review authors' judgements about each domain for each included study.
Modified Mallampati test (part 1) Figure 39
17.

Risk of bias and applicability concerns summary for modified Mallampati test (part 1): review authors' judgements about each domain for each included study.
Modified Mallampati test (part 2) Figure 40
18.

Risk of bias and applicability concerns summary for modified Mallampati test (part 2): review authors' judgements about each domain for each included study.
Mouth opening test Figure 41
19.

Risk of bias and applicability concerns summary for mouth opening: review authors' judgements about each domain for each included study.
Sternomental distance Figure 42
20.

Risk of bias and applicability concerns summary for sternomental distance: review authors' judgements about each domain for each included study.
Thyromental distance Figure 43
21.

Risk of bias and applicability concerns summary for thyromental distance: review authors' judgements about each domain for each included study.
Upper lip bite test Figure 44
22.

Risk of bias and applicability concerns summary for upper lip bite test: review authors' judgements about each domain for each included study.
Wilson risk score Figure 45
23.

Risk of bias and applicability concerns summary for Wilson risk score: review authors' judgements about each domain for each included study.
Combinations of tests (part 1) Figure 46
24.

Risk of bias and applicability concerns summary for combination of tests (part 1): review authors' judgements about each domain for each included study.
Combinations of tests (part 2) Figure 47
25.

Risk of bias and applicability concerns summary for combination of tests (part 2): review authors' judgements about each domain for each included study.
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adamus 2010.
| Study characteristics | |||
| Patient sampling | All adult patients selected for endotracheal intubation for non‐emergency surgical procedures | ||
| Patient characteristics and setting | Sample size: 1518 763 females |
||
| Index tests | Modified Mallampati | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: following induction of general anaesthesia and muscle relaxation, direct laryngoscopy was performed. The laryngoscopic view under optimal conditions (“morning air sniffing position”) was described | ||
| Flow and timing | Index test: on arrival at operating theatre Reference standard: following induction of general anaesthesia | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Adnet 2001.
| Study characteristics | |||
| Patient sampling | All consecutive surgical patients scheduled for anaesthesia requiring tracheal intubation were studied | ||
| Patient characteristics and setting | University hospital, surgical patients (abdominal, cardiac, thoracic, orthopaedic, ENT surgery) Sample size: 1171 505 females Mean age: 49 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy, IDS > 5 | ||
| Flow and timing | Preoperative visit to surgery | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Aktas 2015.
| Study characteristics | |||
| Patient sampling | "Selected at random" excluding emergency operations, patients needing awake intubation and patients with congenital anomalies | ||
| Patient characteristics and setting | Sample size: 120 67 females Mean age: 47.5 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Al Ramadhani 1996.
| Study characteristics | |||
| Patient sampling | Patients planned for caesarian section were evaluated. If patients were selected for general anaesthesia, they were included | ||
| Patient characteristics and setting | Sample size: 523 523 females Mean age: 30.4 years |
||
| Index tests | SMD (13.5 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test during pre‐anaesthesia assesment Target condition after RSI | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ali 2009.
| Study characteristics | |||
| Patient sampling | Over 5 years, 66 consecutive patients with acromegaly who presented for pituitary surgery | ||
| Patient characteristics and setting | Consecutive patients with acromegaly who presented for pituitary surgery Sample size: 66 32 females Mean age: 43.4 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | The time interval was not described. Modified Mallampati grade was assessed preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ali 2012.
| Study characteristics | |||
| Patient sampling | Adult patients (> 18 years of age) undergoing elective surgeries requiring general anaesthesia with endotracheal intubations were enrolled | ||
| Patient characteristics and setting | Edentulous patients, those unable to open the mouth or with limited cervical movement or requiring rapid sequence induction were excluded Sample size: 324 199 females Mean age: 43 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: laryngoscopy was done with Macintosh laryngoscope blade size 3 or 4, and laryngoscopic view of the first attempt at intubation was graded and recorded according to Cormack and Lehane classification with the patient in the sniffing position but without applying external laryngeal pressure | ||
| Flow and timing | Preoperatively; no further information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Allahyary 2008.
| Study characteristics | |||
| Patient sampling | Consecutive women were prospectively included Exclusion criteria were gross anatomical abnormality or recent surgery of the head and neck, preeclampsia, severe cardiorespiratory disorders, inability to sit and edentulous patients | ||
| Patient characteristics and setting | Consecutive obstetric parturients with ASA I/II undergoing general anaesthesia for caesarean delivery Sample size: 203 203 females |
||
| Index tests | MMT, TMD, SMD (13.5cm), mouth opening, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No time interval defined, but the tests were performed preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ambesh 2013.
| Study characteristics | |||
| Patient sampling | Consecutive adult patients ASA I and II undergoing scheduled general anaesthesia | ||
| Patient characteristics and setting | Obvious difficult airway excluded Sample size: 500 208 females Mean age: 46 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult larnygoscopy: Cormack and Lehane, Macintosh blade after general anesthesia and muscle relaxation | ||
| Flow and timing | Preoperatively; no further information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Applegate 2013.
| Study characteristics | |||
| Patient sampling | Adult patients scheduled for head and neck surgery with the ability to read, write, and speak English were considered for inclusion | ||
| Patient characteristics and setting | Sample size: 160 70 females Mean age: 55 years |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, Macintosh blade after general anesthesia and muscle relaxation | ||
| Flow and timing | Preoperatively; no further information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Arne 1998.
| Study characteristics | |||
| Patient sampling | During an 18‐month period, any patient older than 15 years of age undergoing ENT or general surgery with tracheal intubation was considered as potentially eligible | ||
| Patient characteristics and setting | Sample size: 1200 Mean age: 47 years |
||
| Index tests | MMT, TMD, mouth opening (< 5 cm) | ||
| Target condition and reference standard(s) | DIfficult tracheal intubation: patient placed in optimal (sniffing) position on OR table Anaesthesia induced followed by neuromuscular blockade Macintosh blade at first attempt | ||
| Flow and timing | Index tests during preoperative consultation | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ayhan 2016.
| Study characteristics | |||
| Patient sampling | Adult patients surgically treated for endometrial cancer from January 2011 to December 2014 | ||
| Patient characteristics and setting | Patients operated for endometrial cancer were reviewed and only those patients with BMI ≥ 25 (N = 427) were included in the study Sample size: 427 427 females Mean age: 58 years |
||
| Index tests | MMT, mouth opening | ||
| Target condition and reference standard(s) | DIfficult laryngoscopy: Cormack and Lehane; difficult face mask ventilation | ||
| Flow and timing | During preoperative visit and during induction of anaesthesia | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ayuso 2009.
| Study characteristics | |||
| Patient sampling | Consecutive adult patients with laryngeal disease to undergo laryngeal microsurgry under general anaesthesia | ||
| Patient characteristics and setting | No prior testing Sample size: 181 47 females Mean age: 53.5 years |
||
| Index tests | MMT, TMD, mouth opening (< 4 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Badheka 2016.
| Study characteristics | |||
| Patient sampling | Patients of both gender between 20 and 70 years of age with ASA I–III scheduled to undergo elective surgery under general anaesthesia with endotracheal intubation | ||
| Patient characteristics and setting | Patients with airway malformation, oral surgery, neck burns contracture, midline neck swelling, emergency surgery, caesarean section, edentulous patients, limitation of temporomandibular/atlantoaxial joint mobility, and history of neck surgery were excluded from the study Sample size: 170 73 females |
||
| Index tests | MMT, TMD (< 6 cm), SMD, mouth opening, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: laryngoscopy was done by a qualified and experienced anaesthesiologist, who was blinded to the results of preoperative airway assessment and glottic visualization were assessed and noted according to modified Cormack and Lehane grade | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Baig 2014.
| Study characteristics | |||
| Patient sampling | Patients having ASA II status, age above 18 years and known cases of diabetes mellitus planned for elective surgeries requiring general anaesthesia | ||
| Patient characteristics and setting | Those who already had airway deformity due to surgical or medical problem or those undergoing rapid sequence induction were excluded Sample size: 357 145 females Mean age: 53.7 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Basaranoglu 2010.
| Study characteristics | |||
| Patient sampling | Consecutive patients for emergency caesarean delivery | ||
| Patient characteristics and setting | No prior testing, routine evaluation Sample size: 239 239 females Mean age: 28 years |
||
| Index tests | MMT, TMD (< 6 cm), SMD, mouth opening (< 3 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Within Minutes | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Basunia 2013.
| Study characteristics | |||
| Patient sampling | Patients (16 to 60 years), ASA I and II, scheduled for elective surgical procedures requiring ETI were included | ||
| Patient characteristics and setting | Patients with inoral growth, unable to open mouth, chin on chest challenged person, pregnancy, previous history of difficult intubation, acquired disorders of head and neck were excluded Sample size: 300 |
||
| Index tests | MMT, SMD, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Bergler 1997.
| Study characteristics | |||
| Patient sampling | Patients with planned laser surgery (ENT) Patients with reduced mobility were excluded | ||
| Patient characteristics and setting | Sample size: 91 22 females Mean age: 54 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No details given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Bhat 2007.
| Study characteristics | |||
| Patient sampling | ASA 1/2 patients, admitted for elective surgical procedure were prospectively included | ||
| Patient characteristics and setting | Excluded: edentulous patients, restricted mouth opening, restricted cervical movement
Presence of oropharyngeal, laryngeal pathology Sample size: 500 286 females |
||
| Index tests | MMT, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not described | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Bilgin 1998.
| Study characteristics | |||
| Patient sampling | ASA I‐II for GA requiring endotracheal intubation. Excluded known abnormalities of upper airway or head and neck trauma | ||
| Patient characteristics and setting | Sample size: 500 253 females Mean age: 45.6 years |
||
| Index tests | MT, TMD (< 6 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: using Macintosh blade size 3, with head in "sniffing" position on a pillow. Cormack and Lehane III/IV defined as difficult. Difficult tracheal intubation | ||
| Flow and timing | Exact timing not specified | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Bindra 2010.
| Study characteristics | |||
| Patient sampling | Not stated | ||
| Patient characteristics and setting | No prior test; standard assessment; routine preoperative care Sample size: 123 52 females Mean age: 38 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not stated, but apparently just prior to being taken to operating theatre | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Bouaggad 2004.
| Study characteristics | |||
| Patient sampling | All patients aged 18 years and older scheduled to undergo thyroid surgery under general anaesthesia were prospectively included in the study. Patients with obvious malformations of the airway were excluded from the study | ||
| Patient characteristics and setting | Patients undergoing elective thyroid surgery Sample size: 320 281 females |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: the laryngeal view was assessed with rigid laryngoscopy by a certified anaesthesiologist or certified nurse anaesthetist using a Macintosh laryngoscope, Blade 3 or 4. Difficult tracheal intubation: evaluated by IDS | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Breckwoldt 2011.
| Study characteristics | |||
| Patient sampling | All ETIs performed by the emergency physicians of the mobile intensive care unit and the helicopter emergency medical system were included. | ||
| Patient characteristics and setting | Sample size: 276 105 females Mean age: 65 years |
||
| Index tests | Mouth opening | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Directly before intubation | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Brodsky 2002.
| Study characteristics | |||
| Patient sampling | Consecutive | ||
| Patient characteristics and setting | Morbidly obese patients (BMI > 40) undergoing elective surgery Sample size: 100 78 females Mean age: 44 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Butler 1992.
| Study characteristics | |||
| Patient sampling | Mixed surgical patients | ||
| Patient characteristics and setting | Patients with known abnormalities of the airway or with head or neck trauma were excluded Sample size: 250 153 females |
||
| Index tests | MMT, TMD (< 6 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Cattano 2004.
| Study characteristics | |||
| Patient sampling | Consecutive | ||
| Patient characteristics and setting | Adult patients scheduled to receive general anaesthesia requiring endotracheal intubation for elective abdominal, vascular, urologic, and endocrinologic surgery Sample size: 1956 |
||
| Index tests | MMT, TMD, SMD (< 1.2 cm), mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult face mask ventilation | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Cattano 2014.
| Study characteristics | |||
| Patient sampling | A retrospective investigation was performed. 1399 anaesthetics were identified where both mask ventilation was attempted and a preprocedure airway evaluation was documented. Of these, 557 obese patients were identified and included for analysis | ||
| Patient characteristics and setting | Obese patients Sample size: 557 307 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult face mask ventilation | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Chaves 2009.
| Study characteristics | |||
| Patient sampling | Chart review | ||
| Patient characteristics and setting | Patients having elective thyroid surgery between January 2005 and June 2007; routine anaesthesia care
About 10% of patients had clinical signs of tracheal compression or radiographic signs of intrathoracic goiter or tracheal compression in cervical radiogram Sample size: 512 448 females Mean age: 55 years |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening (< 5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: more than three attempts necessary or a change in materials used | ||
| Flow and timing | Not given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Choi 2013.
| Study characteristics | |||
| Patient sampling | Consecutive patients of ASA I or II, aged 18 to 70 years old, and who were scheduled to undergo elective surgery under general anaesthesia were considered for enrolment | ||
| Patient characteristics and setting | Patients with loose upper incisors, airway pathology, gross anatomical abnormalities, BMI more than 35 kg/m2, or any history of difficult intubation were excluded Sample size: 269 132 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Connor 2011.
| Study characteristics | |||
| Patient sampling | "Patients meeting our entry criteria were identified by examination of their anesthesia records in the postanesthesia care unit" | ||
| Patient characteristics and setting | Only one sex, one ethnicity Sample size: 80 0 female |
||
| Index tests | MMT, TMD | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Standard preoperative examination | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Cortellazzi 2007.
| Study characteristics | |||
| Patient sampling | "Data of consecutive patients intubated in two 5‐month periods in 2004 and 2006 were anonymously entered in a computerized database for the purpose of the present study" | ||
| Patient characteristics and setting | Sample size: 1837 885 females |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test was performed 1 day before surgery | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
De Jong 2015.
| Study characteristics | |||
| Patient sampling | All consecutive intubation procedures in obese (BMI >= 30) patients using two multicentre databases, one containing data from 60 French medical, surgical ICUs, and the other containing data from four anaesthesia departments | ||
| Patient characteristics and setting | Obese (BMI >= 30) patients
Exclusion criteria were pregnancy or being under 18 years of age
setting both ICU and OR Sample size: 2385 1238 females Mean age: 55 years |
||
| Index tests | MMT, TMD (< 5 cm), mouth opening | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: three or more laryngoscopic attempts or > 10 minutes | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Descoins 1994.
| Study characteristics | |||
| Patient sampling | ENT patients | ||
| Patient characteristics and setting | Sample size: 295 | ||
| Index tests | MMT, TMD, mouth opening (< 5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Dohrn 2015.
| Study characteristics | |||
| Patient sampling | Consecutive patients scheduled for laparoscopic gastric bypass surgery | ||
| Patient characteristics and setting | Sample size: 539 437 females |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: more than two attempts | ||
| Flow and timing | No further information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Domi 2009.
| Study characteristics | |||
| Patient sampling | "The patients were selected and evaluated by a senior anesthesiologist" | ||
| Patient characteristics and setting | "All the patients with previous anesthesia records sugesting difficult intubation as well as patients with congenital and acquired illnesses of neck and head were excluded from the study" Sample size: 426 |
||
| Index tests | MMT, Wilson risk score, TMD, SMD, mouth opening (< 4 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Domi 2010.
| Study characteristics | |||
| Patient sampling | Convenience sample | ||
| Patient characteristics and setting | Exclusion: < 14 years; history of difficult to intubate Sample size: 426 209 females |
||
| Index tests | MMT, TMD, SMD | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Eberhart 2005.
| Study characteristics | |||
| Patient sampling | Consecutive | ||
| Patient characteristics and setting | Sample size: 1269 449 females Mean age: 61 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
El‐Ganzouri 1996.
| Study characteristics | |||
| Patient sampling | All patients who underwent general surgery | ||
| Patient characteristics and setting | Sample size: 10,507 | ||
| Index tests | MMT, TMD (< 6 cm), mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not specified | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ezri 2001.
| Study characteristics | |||
| Patient sampling | All patients > 18 years in preoperative holding area between 08:00 h to 16:00 h enrolled | ||
| Patient characteristics and setting | Excluded patients given regional anaesthesia and patients receiving GA without endotracheal intubation. Excluded also patients with upper airway pathology, cervical spine fractures and increased risk for aspiration of gastric contents Sample size: 764 367 females Mean age: 44.4 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Exact time interval between airway bedside test and laryngoscopy not described | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ezri 2003a.
| Study characteristics | |||
| Patient sampling | All consecutive patients older than 18 years of age, who arrived in the preoperative holding area for elective surgery | ||
| Patient characteristics and setting | Patients with upper airway pathology, history of difficult laryngoscopy/intubation and full stomach were excluded Sample size: 50 29 females Mean age: 35 years |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ezri 2003b.
| Study characteristics | |||
| Patient sampling | Consecutive patients undergoing coronary artery bypass surgery and general surgery (laparoscopies and open laparotomies) | ||
| Patient characteristics and setting | All aged > 40 years, patients with BMI > 35, upper airway pathology, history of difficult aryngoscopy/intubation and full stomach were excluded Sample size: 1472 735 females Mean age: 44.2 years |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening (< 4 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ezri 2003c.
| Study characteristics | |||
| Patient sampling | Morbidly obese (BMI > 35) scheduled for weight reduction surgery | ||
| Patient characteristics and setting | See above | ||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Night before surgery | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Frerk 1991.
| Study characteristics | |||
| Patient sampling | Adults requiring tracheal intubation as part of anaesthesia assessed before operation | ||
| Patient characteristics and setting | Sample size: 244 101 females Mean age: 44.3 years |
||
| Index tests | MMT, TMD (< 7 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, Macintosh blade for laryngoscopy | ||
| Flow and timing | Tests done at preoperative visit | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Frerk 1996.
| Study characteristics | |||
| Patient sampling | Case‐control | ||
| Patient characteristics and setting | Ten patients with a history of difficult tracheal intubation (Cormack and Lehane grade III or IV) and 10 control patients in whom the trachea was easy to intubate (Cormack and Lehane grade I or II) were examined Sample size: 20 |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Freund 2012.
| Study characteristics | |||
| Patient sampling | Unknown | ||
| Patient characteristics and setting | Patients intubated in physician‐staffed EMS; patients with alternative airway management at first or second attempt excluded Sample size: 694 264 females Mean age: 60.5 years |
||
| Index tests | TMD, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Fritscherova 2011.
| Study characteristics | |||
| Patient sampling | Patients over 18 years of age undergoing surgery under general anaesthesia with their airway secured by tracheal intubation | ||
| Patient characteristics and setting | Patients in whom difficult intubation could be anticipated were excluded from the study Sample size: 158 78 females Mean age: 59.6 years |
||
| Index tests | MMT, TMD, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation: failed or > 10 mins | ||
| Flow and timing | Reference standard in the operation Index test the following day for difficult intubation group, no details for easy intubation group | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Gonzalez 2008.
| Study characteristics | |||
| Patient sampling | All obese patients scheduled for surgery under general anaesthesia with endotracheal intubation were enrolled in this prospective study at University Hospital of Toulouse Obesity was defined as a BMI > 30 kg/m2. Concomitantly, all the lean (BMI < 30 kg/m2) adult patients who were scheduled for surgery during the same period and who were intubated by the same anaesthesiologists were included in the control group |
||
| Patient characteristics and setting | Sample size: 131 115 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: IDS | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hagberg 2009.
| Study characteristics | |||
| Patient sampling | Retrospective analysis | ||
| Patient characteristics and setting | Obese (BMI > 35) patients undergoing elective surgery during a period of 9 years within one hospital Sample size: 283 216 females Mean age: 44.6 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Failed intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hagiwara 2015.
| Study characteristics | |||
| Patient sampling | Patients requiring emergency intubation at the ED Those where alternative airway techniques at first attempt were excluded | ||
| Patient characteristics and setting | Sample size: 3313 1236 females Mean age: 71 years |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: more than two attempts | ||
| Flow and timing | Unclear; form filled out after intubation | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hashim 2014.
| Study characteristics | |||
| Patient sampling | Patients who were diabetic for at least a year in the age group between 30 and 80 years and underwent elective surgery under general anaesthesia with endotracheal intubation | ||
| Patient characteristics and setting | Patients with obvious anatomical variation of their face, neck, palate or hands and history of difficult intubation in the past were excluded from the study. Patients with coexisting diseases such as rheumatoid arthritis, oral malignancies and large neck masses were also excluded Sample size: 60 37 females Mean age: 56 years |
||
| Index tests | MMT, TMD (< 6 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane using Macintosh blade | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Healy 2016.
| Study characteristics | |||
| Patient sampling | Patients undergoing general anaesthesia with a documented preoperative airway examination in combination with a documented glottic view obtained at direct laryngoscopy | ||
| Patient characteristics and setting | Excluded all patients without a documented intraoperative view or presence of an existing airway and patients in which intubation was performed by alternative means Sample size: 80,709 43,015 females |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, using either Macintosh or Miller blade Difficult tracheal intubation: IDS | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Heinrich 2013.
| Study characteristics | |||
| Patient sampling | Database | ||
| Patient characteristics and setting | Patients undergoing anaesthesia
Patients with videolaryngoscopic assistance without documentation of a direct laryngeal view were excluded Sample size: 102,305 50,608 females Mean age: 57 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, standard cold light MacIntosh blade sized appropriately | ||
| Flow and timing | Preoperative maximum 12 hours | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hekiert 2007.
| Study characteristics | |||
| Patient sampling | Retrospetive analysis of consecutive obese patients | ||
| Patient characteristics and setting | Obese patients only (BMI > 30) Sample size: 14 9 females Mean age: 52.2 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Reference standard: otolaryngology office index test: OP | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hirmanpour 2014.
| Study characteristics | |||
| Patient sampling | Unclear | ||
| Patient characteristics and setting | Patients with a history of trauma to the airway or cranial, cervical and facial regions, or were edentulous or requiring awake intubation, patients with restricted motility of the neck and mandible (e.g. cervical disc disorders or rheumatoid arthritis) and inability to sit were not included in the study Sample size: 657 657 females Mean age: 27 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, size three Macintosh laryngoscope blade | ||
| Flow and timing | Preoperative | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Honarmand 2008.
| Study characteristics | |||
| Patient sampling | Consecutive patients selected for elective caesarean delivery | ||
| Patient characteristics and setting | Exclusion: < 18, obvious malformations of the airway, inability to sit, head/neck surgery Sample size: 400 400 females Mean age: 24 years |
||
| Index tests | MMT, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane. A anesthesiologist with 7 years experience in anaesthesia, who was not informed of the results of the index tests, carried out laryngoscopy and assessed difficulty of laryngoscopy at intubation, which was performed with the patient adequately anaesthetized and fully relaxed on the operating room table. Laryngoscopy was performed using a Macintosh #4 | ||
| Flow and timing | Test was carried out prior to transfer to operating room | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Honarmand 2014.
| Study characteristics | |||
| Patient sampling | ASA I‐III adult patients programmed to be given general anaesthesia necessitate endotracheal intubation for elective surgery | ||
| Patient characteristics and setting | Patients with a history of previous surgery, burns or trauma to the airways or to the cranial, cervical and facial regions, patients with tumours or a mass in the above‐mentioned regions, patients with restricted motility of the neck and mandible (e.g. rheumatoid arthritis or cervical disk disorders), inability to sit, edentulous or need awake intubation were excluded from the study Sample size: 525 184 females Mean age: 46 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, laryngoscopy was done with using a Macintosh #4 blade to visualize the larynx | ||
| Flow and timing | Preoperative | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Honarmand 2015.
| Study characteristics | |||
| Patient sampling | Adult patients, who were scheduled to undergo elective operations under general anaesthesia with endotracheal intubation | ||
| Patient characteristics and setting | Sample size: 600 319 females Mean age: 44 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane. Laryngoscopy was done by a Macintosh number 4 laryngoscope blade | ||
| Flow and timing | Preoperative | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Huh 2009.
| Study characteristics | |||
| Patient sampling | Consecutive adult patients scheduled to undergo general anesthesia requiring tracheal intubation for elective surgery | ||
| Patient characteristics and setting | Exclusion criteria included a gross anatomical abnormality, recent surgery of the
head and neck, upper airway disease (e.g. maxillofacial fracture or tumours), loose teeth, or those requiring a rapid sequence or awake intubation Sample size: 213 104 females |
||
| Index tests | MMT, TMD (< 6.2 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Reference standard immediately after index tests | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Hui 2009.
| Study characteristics | |||
| Patient sampling | Patients presenting for elective, non‐cardiac surgery requiring intubation | ||
| Patient characteristics and setting | Sample size: 27 | ||
| Index tests | MT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Istvan 2010.
| Study characteristics | |||
| Patient sampling | Retrospective chart review of patients undergoing appendectomy within 1 year | ||
| Patient characteristics and setting | Inclusion criteria were patients from all ages and sexes who were admitted to hospital from
the emergency department and whose preoperative and postoperative diagnosis was acute appendicitis. Exclusion criteria were patients already in hospital whose postoperative
diagnosis was not acute appendicitis or who underwent other surgical procedures in the same setting Sample size: 254 100 females Mean age: 29.5 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Failed intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ittichaikulthol 2010.
| Study characteristics | |||
| Patient sampling | Consecutive ASA I‐IV adult patients | ||
| Patient characteristics and setting | Patients scheduled to receive general anaesthesia requiring endotracheal intubation for all surgery Sample size: 1888 1239 females |
||
| Index tests | MMT (I versus II‐IV), TMD (< 6 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Juvin 2003.
| Study characteristics | |||
| Patient sampling | All obese (BMI > 35), adult (> 18 years) patients scheduled for laparoscopic gastroplasty and all lean (BMI < 30) adult patients who were scheduled for inguinal hernia repair or laparoscopic cholecystectomy during the same period and who were intubated by the same anaesthesiologists were included | ||
| Patient characteristics and setting | Excluded: ASA III or IV, BMI 30 to 35 Sample size: 263 189 females Mean age: 41 years |
||
| Index tests | MMT, mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: IDS | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
K Nasa 2014.
| Study characteristics | |||
| Patient sampling | Patients above the age of 12 years who were fit for general endotracheal anaesthesia irrespective of their ASA physical status were included in the study | ||
| Patient characteristics and setting | Patients with obvious airway malformations, patient with inter incisor distance < 3 cm, patients allergic to drugs used in study were excluded from the study Sample size: 400 190 females |
||
| Index tests | MMT, TMD (< 6 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: IDS | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kalezic 2016.
| Study characteristics | |||
| Patient sampling | Consecutive adult patients scheduled for thyroid surgery | ||
| Patient characteristics and setting | Sample size: 2000 1705 females |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kamalipour 2005.
| Study characteristics | |||
| Patient sampling | Adult patients who were scheduled for elective surgery under general anaesthesia were randomly selected (using the branched block randomization method) and considered for enrolment | ||
| Patient characteristics and setting | Patients with obvious malformations of the airway, edentulous patients, patients who required cricoid pressure for rapid sequence intubation and pregnant women were excluded from the study. Edentulous patients were also excluded. Sample size: 100 36 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kamranmanesh 2013.
| Study characteristics | |||
| Patient sampling | Consecutive adult asian patients aged 20 to 65 years with ASA I and II, scheduled to undergo elective surgery requiring endotracheal intubation, were enrolled in this prospective observational study | ||
| Patient characteristics and setting | Exclusion criteria were as follows: obvious anatomical abnormality, upper airway abnormality (e.g. tong tumour, maxillofacial tumour, or fracture), recent head and neck
surgery, ASA class III and IV, and disability to open the mouth Sample size: 603 173 females Mean age: 42.4 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2003.
| Study characteristics | |||
| Patient sampling | Consecutive male and female patients, aged >= 16 years, scheduled to undergo surgery under general anaesthesia between January 2001 and November 2001, were considered for enrolment | ||
| Patient characteristics and setting | Edentulous patients, those unable to open the mouth, with laryngeal masses, or with limitation of cervical movements were excluded from the study Sample size: 300 |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2009a.
| Study characteristics | |||
| Patient sampling | ASA I patients older than 16 years scheduled for elective surgical procedures requiring endotracheal intubation were enrolled | ||
| Patient characteristics and setting | Patients with any airway abnormality or obvious neck pathology were excluded Sample size: 380 171 females Mean age: 34 years |
||
| Index tests | TMD (< 13.5 cm), SMD, mouth opening, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2009b.
| Study characteristics | |||
| Patient sampling | Patients undergoing surgery and requiring endotracheal intubation were enrolled in this study | ||
| Patient characteristics and setting | Exclusion criteria included compromised critical airway, emergent cases, noncompliable patients and those with anatomical anomalies in the airway, pregnant, edentulous, those having beard and patients less than 14 years and those in whom a good mask fit was not possible Sample size: 200 118 females |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult face mask ventilation: mask ventilation was performed by means of an appropriate sized face mask applied to the face and a reservoir bag receiving a continuous flow of oxygen from the anaesthesia machine | ||
| Flow and timing | Shortly one after another | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2011.
| Study characteristics | |||
| Patient sampling | Consecutive patients of ASA physical status I and II, aged 20‐60 scheduled for elective surgical procedures requiring tracheal intubation between July 2008 and June 2009 | ||
| Patient characteristics and setting | Edentulous patients, those unable to open the mouth, patients with pharyngolaryngeal pathology, with a history of thyroid neck surgery, pregnancy, or with limitation of temporomandibular and atlanto‐axial joints were excluded from the study Sample size: 300 175 females Mean age: 38.4 years |
||
| Index tests | ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2013.
| Study characteristics | |||
| Patient sampling | Consecutive patients, ASA I to III who required general anaesthesia and endotracheal intubation were studied prospectively over a 3‑year period from January 2007 until December 2010 | ||
| Patient characteristics and setting | Exclusion criteria included inability to sit, gross anatomical abnormality or recent surgery of the head and neck and patients with pregnancy or severe cardiorespiratory disorders Sample size: 4500 1505 females Mean age: 55.7 years |
||
| Index tests | TMD, SMD, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2014.
| Study characteristics | |||
| Patient sampling | Consecutive male or female edentulous patients ≥ 60 years old scheduled to undergo elective surgery under GA between March 2008 and June 2011 were considered for enrolment | ||
| Patient characteristics and setting | Uncooperative patients, those unable to open the mouth or with pharyngolaryngeal pathology were excluded from the study. Patients with fixed prosthetic dentures were also excluded and mobile dentures, if present, were removed to adhere to the true definition of an edentulous case Sample size: 588 253 females Mean age: 64 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Khan 2015.
| Study characteristics | |||
| Patient sampling | "In this cross‐sectional study, 661 patients aged 16‐60 years were recruited during the years 2011 to 2012" | ||
| Patient characteristics and setting | Exclusion criteria included ASA class higher than II, urgency of the situation, facial, mouth, throat and airway anomalies, pregnancy and awake intubation Sample size: 661 366 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kheterpal 2009.
| Study characteristics | |||
| Patient sampling | All adult patients (age 18 years or older) undergoing a general anaesthetic at a tertiary care university hospital were included over a 4‐year period from 2004 to 2008 | ||
| Patient characteristics and setting | All cases without an attempt at mask ventilation were excluded from the data collection and analysis, including planned awake fiberoptic intubations Sample size: 53,041 28,657 females Mean age: 51 years |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening (< 3 cm) | ||
| Target condition and reference standard(s) | Difficult face mask ventilation: inability to establish face mask ventilation despite multiple airway adjuvants and two‐hand mask ventilation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kim 2011.
| Study characteristics | |||
| Patient sampling | Patients undergoing surgery under general anaesthesia with tracheal intubation | ||
| Patient characteristics and setting | Patients were divided into obese (BMI >= 27.5) and non‐obese groups. Sufficient measures of DTA presented for obese patients only. Same number of obese and non‐obese patients (130 each), so consecutive sample is unlikely Sample size: 123 77 females Mean age: 48.6 years |
||
| Index tests | MMT, Wilson risk score, combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: IDS | ||
| Flow and timing | No details given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Knudsen 2014.
| Study characteristics | |||
| Patient sampling | Patients scheduled for elective day surgery, inclusion criteria were patients with ASA scores of I or II who were older than 17 years and were scheduled for general anaesthesia requiring endotracheal intubation | ||
| Patient characteristics and setting | Exclusion criteria were anaesthesia with rapid sequence induction, pregnancy, and BMI higher than 35 kg/ma Sample size: 87 68 females Mean age: 42 years |
||
| Index tests | MMT, TMD (< 10 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: "according to ASA recommendations" | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Koh 2002.
| Study characteristics | |||
| Patient sampling | Succesive adult (> 16 years) patients scheduled for elective surgery under general anaesthesia Exclusion: RSI | ||
| Patient characteristics and setting | Sample size: 605 339 females Mean age: 44.5 years |
||
| Index tests | MMT, TMD (< 6 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane, Macintosh size 3, best view, BURP if needed; difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Kolarkar 2015.
| Study characteristics | |||
| Patient sampling | 300 patients of either sex, undergoing elective surgery under general anaesthesia with endotracheal intubation. Inclusion criteria being patients of ASA grade I/II, age: 21‐60 years of either sex, elective surgery under GA | ||
| Patient characteristics and setting | Exclusion criteria were edentulous patient, unable to open the mouth, with pharyngolaryngeal pathology, history of thyroid/neck surgery, limitations of temporomandibular or atlanto‐axial joint. Congenital facial deformity Sample size: 300 160 females Mean age: 40.6 years |
||
| Index tests | ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Komatsu 2007.
| Study characteristics | |||
| Patient sampling | Morbidly obese patients (BMI > 35) scheduled for elective surgery under GA with tracheal intubation. Patients with removable upper dentures, upper airway pathology, cervical spine fractures, full stomach, significant gastro‐oesophageal reflux or a history of difficult laryngoscopy were excluded. Pregnant women were also excluded | ||
| Patient characteristics and setting | Sample size: 64 64 females |
||
| Index tests | MMT (I versus II‐IV) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Konwar 2015.
| Study characteristics | |||
| Patient sampling | 200 patients were randomly selected and enrolled in this study. The study population consisted of patients of ASA class I and II, belonging to either sex of age group 18‐40 years admitted for operation under GA with endotracheal intubation | ||
| Patient characteristics and setting | Patients with concurrent pregnancy; intraoral, laryngeal or pharyngeal mass; altered head and neck anatomy; and restricted movement of the neck were excluded Sample size: 200 83 females Mean age: 28 years |
||
| Index tests | TMD, mouth opening, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Krobbuaban 2005.
| Study characteristics | |||
| Patient sampling | Consecutive ASA I–II adult patients scheduled to receive GA requiring endotracheal intubation for elective orthopaedic, urologic, abdominal, and gynaecologic surgery | ||
| Patient characteristics and setting | Patients younger than 18 years of age, with obvious malformations of the airway, edentulous, or requiring a RSI or awake intubation were excluded from the study Sample size: 550 289 females Mean age: 45 years |
||
| Index tests | MMT, TMD, mouth opening | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Langeron 2000.
| Study characteristics | |||
| Patient sampling | All adult patients scheduled for orthopaedic, urologic, abdominal, gynaecologic and neurosurgery with GA were prospectively included in the study over a 6‐month period | ||
| Patient characteristics and setting | Those with contraindication of mask ventilation (i.e. emergency cases requiring a RSI, planned awake intubation) were excluded Sample size: 1502 831 females Mean age: 50.5 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult face mask ventilation: the inability of an unassisted anaesthesiologist to maintain the measured oxygen saturation as measured by pulse oximetry > 92% or to prevent or reverse signs of inadequate ventilation during positive‐pressure mask ventilation under GA | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Lee 2015.
| Study characteristics | |||
| Patient sampling | The 2011 year operating schedule was reviewed to identify study patients | ||
| Patient characteristics and setting | Exclusion criteria were: children, nasotracheal intubation, emergency intubation, fiberoptic‐assisted intubation, existing tracheostomies or laryngectomies, laryngeal mask airway
cases, regional anaesthesia without intubation, and incomplete charts. Inclusion criteria were adult (18 years) male and female patients undergoing direct laryngoscopy for the purpose of general endotracheal anaesthesia Sample size: 344 |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not stated in study | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Liaskou 2014.
| Study characteristics | |||
| Patient sampling | 387 consecutive adult patients (age > 18 years) ASA I–II, without known airway pathology, scheduled for surgical procedures under GA with tracheal intubation were assessed for eligibility | ||
| Patient characteristics and setting | Teaching hospital, patients scheduled for surgery Sample size: 341 178 females Mean age: 50 years |
||
| Index tests | SMD (< 15 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not described | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Lundstrom 2009.
| Study characteristics | |||
| Patient sampling | Nationwide prospective registry | ||
| Patient characteristics and setting | For this retrospective analysis patients with regional anaesthesia, sedation alone, no planned endotracheal intubation, intubation previous to OP, fibre optic intubation were excluded Sample size: 103,728 59,287 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: more than two attempts or more than one anaesthesist | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Mallat 2010.
| Study characteristics | |||
| Patient sampling | Patients were selected when at least one of the following criteria was found at preoperative evaluation: inability to palpate the cricoid cartilage, endothoracic goitre (every goitre that extends below the manubrium on the chest x‐ray), tracheal deviation of more than 1 cm or tracheal stenosis on the chest x‐ray | ||
| Patient characteristics and setting | Patients with goitre only (see above) Sample size: 80 Mean age: 56 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: IDS | ||
| Flow and timing | No details given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Mashour 2008.
| Study characteristics | |||
| Patient sampling | All patients receiving anaesthesia with BMI >= 40 | ||
| Patient characteristics and setting | Only patients with BMI >= 40 Sample size: 346 231 females Mean age: 50 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Mehta 2014.
| Study characteristics | |||
| Patient sampling | Patients posted for elective surgery under GA Patients with obvious head and neck pathology, edentulous patients, mass in the mouth, BMI > 40, protruding upper incisors (total of 34) were excluded from the study |
||
| Patient characteristics and setting | Sample size: 484 130 females Mean age: 44 years |
||
| Index tests | MMT, TMD (< 6 cm), SMD (< 1.5 cm), mouth opening, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Merah 2004.
| Study characteristics | |||
| Patient sampling | ASA I‐III patients selected for GA for caesarean section | ||
| Patient characteristics and setting | Exclusion: inability to sit, gross anatomical abnormity of head and neck, recent surgery of this areas, severe cardiorespiratory disorders Sample size: 80 80 females Mean age: 30.9 years |
||
| Index tests | MMT, TMD, SMD (< 13.5 cm), mouth opening (< 2.5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Mishra 2009.
| Study characteristics | |||
| Patient sampling | No details given | ||
| Patient characteristics and setting | 100 pregnant patients posted for caesarean section under GA (both emergency and elective) Patients with a history of burns, trauma, tumours or a mass and previous surgery involving the craniofaciocervical region or the airway, patients with restricted mobility of the neck andmandible (e.g. rheumatoid arthritis or cervical disk disorders), and severe pregnancy induced hypertension were excluded from the study Sample size: 100 100 females Mean age: 25 years |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Montemayor‐Cruz 2015.
| Study characteristics | |||
| Patient sampling | A non‐probabilistic sample was performed by selecting consecutive cases over the month of January 2014 | ||
| Patient characteristics and setting | Inclusion criteria: male and female patients of 15 to 75 years of age;elective surgical procedure; GA requiring orotracheal intubation Exclusion criteria: patients who refused to participate in the study (in the case of minors, patients whose legal guardians refused their participation in the study); patients who, due to their clinical status, were unable to co‐operate with airway assessment (low Glasgow Coma Scale score, mental retardation, dementia, etc.); anatomical abnormalities altering the airway (deformity, tumours, etc.) and that precluded airway exploration regardless of the diagnosis the surgical procedure was to be performed for; patients already intubated. Sample size: 70 35 females Mean age: 48 years |
||
| Index tests | MMT, mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Myneni 2010.
| Study characteristics | |||
| Patient sampling | "All adult patients 18 years of age and older, presenting in all surgical specialties, were included in the study except for obstetric anesthesia or plastic surgery for burns" | ||
| Patient characteristics and setting | Sample size: 6882 | ||
| Index tests | ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Nadal 1998.
| Study characteristics | |||
| Patient sampling | All diabetic patients for elective surgery under GA included from May 1994 to May 1995 | ||
| Patient characteristics and setting | Excluded: obvious anatomical variations of face, neck, palate or hands, or had a history of difficult tracheal intubation Sample size: 83 53 females Mean age: 53 years |
||
| Index tests | MT, TMD (< 6 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test done one day before surgery | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Naguib 1999.
| Study characteristics | |||
| Patient sampling | Case‐control | ||
| Patient characteristics and setting | Patients in whom an unanticipated difficult intubation was identified and were scheduled to undergo endotracheal anaesthesia for any type of non‐emergency surgical procedures except traumatic facial abnormalities or obstetric and cardiac surgery. Also
random control group whom laryngoscopy and intubation was found to be easy and anaesthetized by the same anaesthesiologists Sample size: 57 15 females Mean age: 36.9 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Naguib 2006.
| Study characteristics | |||
| Patient sampling | Case‐control | ||
| Patient characteristics and setting | Adult patients presenting for GA for any type of non‐emergency surgical procedures except traumatic facial abnormalities, obstetric surgery, or cardiac surgery with unanticipated difficult intubation. Also second patient from same day as control Sample size: 194 84 females Mean age: 53.7 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation: two or more attempts at placing the endotracheal tube or the use of an alternative device | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Nasir 2011.
| Study characteristics | |||
| Patient sampling | 122 patients were selected from the operative schedule by convenient non‐probability sampling | ||
| Patient characteristics and setting | Adult patients belonging to ASA‐I , II and III ranging from 18‐65 years of either gender undergoing elective procedures from all surgical specialties requiring endotracheal intubation were included in the study. Emergency surgical procedures, patients with age < 18 years, pregnant patients, patients with unstable cervical spine and patients with tumour of the larynx were excluded Sample size: 122 79 females Mean age: 32.8 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unknown | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Nasiri 2013.
| Study characteristics | |||
| Patient sampling | "Our study population included all patients who were referred for elective surgery, adult patients aged 18 to 75 years. Patients with burns, neck, tumors, head and neck injury were excluded" | ||
| Patient characteristics and setting | Sample size: 410 204 females |
||
| Index tests | Mouth opening, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not reported | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Nath 1997.
| Study characteristics | |||
| Patient sampling | Case‐control | ||
| Patient characteristics and setting | Adults requiring GA and intubation (including easy and difficult intubations). Also 16 patients reported to be difficult to intubate Sample size: 300 127 females Mean age: 39.7 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test postoperative. Reference standard was re‐checked according to documentation for those who were included retrospectively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Noorizad 2006.
| Study characteristics | |||
| Patient sampling | No details given | ||
| Patient characteristics and setting | Sample size: 379 200 females |
||
| Index tests | MMT, TMD (< 6 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test at preoperative visit. Reference standard at OP | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Oates 1990.
| Study characteristics | |||
| Patient sampling | Subgroup of patients scheduled for elective surgery from an unpublished prospective study | ||
| Patient characteristics and setting | Sample size: 334 | ||
| Index tests | MT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Oates 1991.
| Study characteristics | |||
| Patient sampling | Patients requiring tracheal intubation for operation. No further details | ||
| Patient characteristics and setting | Sample size: 751 448 females |
||
| Index tests | MT, Wilson risk score | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Pottecher 1991.
| Study characteristics | |||
| Patient sampling | Gynaecologic‐obstetric patients requiring intubation for OP | ||
| Patient characteristics and setting | Sample size: 663 663 females Mean age: 37.9 years |
||
| Index tests | MMT (I versus II‐IV), TMD (< 8 cm), SMD, mouth opening (< 4.1 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Prakash 2013.
| Study characteristics | |||
| Patient sampling | "Patients under general anaesthesia requiring tracheal intubation were included in this prospective study" | ||
| Patient characteristics and setting | Adult ASA I and II adult patients scheduled for elective surgery. Patients with obvious abnormality of the airway where intubation under GA would be contraindicated, those at increased risk of aspiration, inter‐incisor distance < 2.5 cm and unstable cervical spine were excluded from the study Sample size: 330 222 females Mean age: 37.8 years |
||
| Index tests | MMT, mouth opening, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not provided | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Qudaisat 2011.
| Study characteristics | |||
| Patient sampling | Unclear. "variety of elective procedures under general anaesthesia" Exclusion: facial asymmetry, upper incisor protrusion, edentulousness, limited mouth opening | ||
| Patient characteristics and setting | Sample size: 235 98 females |
||
| Index tests | TMD | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Reghunathan 2016.
| Study characteristics | |||
| Patient sampling | Patients of both sexes, between 15 and 55 years, and belonging to ASA grade I or II were selected. Patients with obesity, malposition of teeth, microstomia, macroglossia, edentulous or with artificial dentures, cervical spondylosis, short neck, contractures of neck, neck swellings, postradiation fibrosis, developmental anomalies which may affect airway assessment, and in whom difficult intubation was expected were excluded from the study | ||
| Patient characteristics and setting | Sample size: 200 Mean age: 35 years |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Rocke 1992.
| Study characteristics | |||
| Patient sampling | All patients undergoing elective or emergency caesarean section under GA; no further information | ||
| Patient characteristics and setting | Sample size: 1500 1500 females Mean age: 26.4 years |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation | ||
| Flow and timing | No information | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Safavi 2014.
| Study characteristics | |||
| Patient sampling | Consecutive ASA I‐III adult patients | ||
| Patient characteristics and setting | "These patients were scheduled for elective surgery under general anesthesia requiring endotracheal intubation" Sample size: 476 150 females Mean age: 36.6 years |
||
| Index tests | MMT, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not described | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Sahin 2011.
| Study characteristics | |||
| Patient sampling | ASA I–III patients scheduled for elective surgery and requiring endotracheal intubation were enrolled in the study prospectively over a 1‐year period | ||
| Patient characteristics and setting | The exclusion criteria included patients aged less than 18 years, obstetric patients, patients with anatomic abnormality or recent surgery of the head/neck, burns or trauma to the airways or to the cranial, cervical, and facial regions, patients with tumours or a mass in the aforementioned regions, patients with restricted mobility of the neck and mandible, and patients who do not have incisor teeth. Sample size: 762 367 females |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Index tests: during the preoperative visit Reference standard: after induction of GA | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Salimi 2008.
| Study characteristics | |||
| Patient sampling | All patients aged above 16 who required GA with endotracheal intubation for elective surgery within 1 year were included | ||
| Patient characteristics and setting | Patients with a history of previous surgery, burns or trauma to the airways or to the cranial, cervical and facial regions, patients with tumours or a mass in the above‐mentioned regions, patients with restricted motility of the neck and mandible (e.g. rheumatoid arthritis or cervical disk disorders), patients without teeth, and patients with incomplete information forms were excluded from the study Sample size: 350 114 females Mean age: 32 years |
||
| Index tests | TMD (< 4 cm), ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Samra 1995.
| Study characteristics | |||
| Patient sampling | Random selection, no further details given | ||
| Patient characteristics and setting | Patients with clinically obvious mandibular abnormalities (i.e. receding mandible, poor mobility of temporomandibular joint either due to arthritis, pain, trauma, or trismus) and those patients with history of arthritis and/or limitation of movement of cervical spine were excluded Sample size: 564 |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Savva 1994.
| Study characteristics | |||
| Patient sampling | Consecutive patients (322 of them obstetric) requiring tracheal intubation as part of their anaesthesia | ||
| Patient characteristics and setting | Sample size: 350 185 females Mean age: 39 years |
||
| Index tests | MMT, TMD, SMD, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Schmitt 2000.
| Study characteristics | |||
| Patient sampling | "Between March 1994 and December 1998, all acromegalic patients (American Society of Anesthesiologists class I‐III,68 women, 60 men) scheduled for elective transsphenoidal resection of a growth hormone secreting pituitary adenoma were investigated. The diagnosis of acromegaly was contirmed by clinical and endocrine reassessment (failure to suppress growth hormone to < 2 pg/l after an oral glucose load) as well as by magnetic resonance imaging showing the size and the extent of a pituitary adenoma just before surgery" | ||
| Patient characteristics and setting | "All patients showed typical acromegalic features such as macro‐glossia, prognathism, or soft tissue swelling in various degrees. Preoperatively, Mallampati classification, thyromental distance, and head and neck movement were determined in each patient. After induction of anesthesia and muscle paralysis, laryngoscopic grade was assessed during direct laryngoscopy" Sample size: 128 68 females Mean age: 46 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Seo 2012.
| Study characteristics | |||
| Patient sampling | The study was performed at the hospital on 305 ASA I and II patients between ages 19 and 70 years, who were scheduled for surgery under GA | ||
| Patient characteristics and setting | Patients were excluded from the study if their teeth were incomplete, if the patient had limited head and neck movement, had impairment of the temporomandibular joint, or had oral or laryngeal tumour Sample size: 305 157 females |
||
| Index tests | MMT, TMD (< 6 cm), mouth opening, ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult tracheal intubation: IDS | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Shah 2013.
| Study characteristics | |||
| Patient sampling | Adult patients of more than 18 years age, of either sex, of ASA grade I and II, undergoing elective surgeries under GA | ||
| Patient characteristics and setting | Patients unable to sit or stand erect, pregnant females, those having obvious malformation of the airway or those requiring awake intubation were excluded from the study Sample size: 480 241 females |
||
| Index tests | MMT, TMD, mouth opening (< 4 cm), ULBT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not provided | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Shah 2014.
| Study characteristics | |||
| Patient sampling | Patients aged ≥16 years, scheduled to undergo surgery under GA were included in the study using nonprobability consecutive sampling | ||
| Patient characteristics and setting | Edentulous patients, those unable to open the mouth, those with laryngeal masses, those having large goiters or with limitation of cervical movements were excluded from the study Sample size: 450 254 females Mean ag: 38.8 years |
||
| Index tests | ULBT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Preoperatively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Sharma 2010.
| Study characteristics | |||
| Patient sampling | Case‐control | ||
| Patient characteristics and setting | Over a period of 5 years, 64 consecutive acromegalic patients presenting for surgery for excision of pituitary tumor were enrolled. For each acromegaly patient enrolled, the subsequent nonacromegalic patient scheduled for excision of pituitary tumour during the same 5‐year period was also enrolled to serve as a control Sample size: 125 |
||
| Index tests | MMT, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Singh 2009.
| Study characteristics | |||
| Patient sampling | No information of selection process | ||
| Patient characteristics and setting | ASA I and II patients undergoing elective lower segment caesarean section under GA. Women with full stomach and apparent abnormalities of the neck and face were excluded Sample size: 300 |
||
| Index tests | MMT (I versus II‐IV), Wilson risk score, TMD (< 5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Soyuncu 2009.
| Study characteristics | |||
| Patient sampling | All patients who required intubation in the ED were included in the study | ||
| Patient characteristics and setting | ED patients Sample size: 366 115 females Mean age: 46.8 years |
||
| Index tests | Mouth opening (< 3 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Tantri 2016.
| Study characteristics | |||
| Patient sampling | "Patients who underwent elective surgery with general anesthesia were included in this study" | ||
| Patient characteristics and setting | The inclusion criteria were patients aged 18 to 65 years old; an ASA score of 1 or 2; Indonesians of Malay race; and willingness to participate in this study, as indicated by signing the informed consent form. Patients with oral opening restricted to less than 3 cm, acute burns on the face and neck, tumours on the airway, limitations on neck movement, airway trauma, protruding upper teeth, a high risk of bleeding, acute respiratory infection (croup, epiglottitis, Ludwig’s angina), or anatomical disturbances (macroglossia, short neck, micrognathia, prognathism) were excluded from this study Sample size: 277 160 females Mean age: 40.38 years |
||
| Index tests | MMT, TMD, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Not described | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Thompson 2009.
| Study characteristics | |||
| Patient sampling | Database of obstetric patients who underwent tracheal intubation and who had MMT and Cormack and Lehane grade recorded | ||
| Patient characteristics and setting | Sample size: 1602 | ||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | No information given | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Tse 1995.
| Study characteristics | |||
| Patient sampling | Consecutive male and female patients aged 18 years and older undergoing elective surgery | ||
| Patient characteristics and setting | Excluded patients with obvious malformations of airway, edentulous patiens, and patients who required cricoid pressure for RSI Sample size: 471 251 females |
||
| Index tests | MT, TMD (< 7 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperative measurements recorded on a form not seen by attending anaesthetist. Exact time interval not specified | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Tuzuner‐Oncul 2008.
| Study characteristics | |||
| Patient sampling | No details on selection | ||
| Patient characteristics and setting | Adult maxillofacial surgery patients Sample size: 208 108 females Mean age: 29 years |
||
| Index tests | MMT, TMD (< 6 cm), SMD, mouth opening test (< 2.5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Ul Haq 2013.
| Study characteristics | |||
| Patient sampling | Patients from the preoperative clinic, preoperative waiting area, and operating rooms were enrolled. ASA I‐III patients aged above 18 years of either sex who were scheduled for elective surgeries under GA requiring tracheal intubation were included in the study | ||
| Patient characteristics and setting | Sample size: 760 422 females Mean age: 43.44 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Preoperative, operative, no time interval reported | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Uribe 2015.
| Study characteristics | |||
| Patient sampling | "A computerized search was initiated through the electronic medical records, which revealed 20,985 patients who underwent abdominal surgery requiring general anesthesia at The Ohio State University Wexner Medical Center during a period of 12 months, from January 1, 2007 to December 31, 2007. Using Microsoft Excel, every third patient from an alphabetized list was selected to generate a random sample of 6964 patients for this study. We performed a retrospective chart review of patients who underwent abdominal surgeries with ASA stratification I–V under general anesthesia requiring endotracheal intubation" | ||
| Patient characteristics and setting | Sample size: 1970 2333 females |
||
| Index tests | MMT | ||
| Target condition and reference standard(s) | Difficult tracheal intubation | ||
| Flow and timing | Not reported | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Vallem 2015.
| Study characteristics | |||
| Patient sampling | 200 ASA grade I and II (18 to 60 years of age) adult patients scheduled to receive GA with endotracheal intubation | ||
| Patient characteristics and setting | Patients with airway malformations, edentulous patients, pregnancy and lactating mothers and patients with craniofacial anamolies were excluded from the study. Preoperative airway examination was performed using multiple screening tests to predict difficult airway Sample size: 200 35 females Mean age: 39.5 years |
||
| Index tests | MMT, TMD (< 6 cm), SMD (< 11 cm), mouth opening, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Vani 2000.
| Study characteristics | |||
| Patient sampling | Patients with diabetes undergoing elective surgery | ||
| Patient characteristics and setting | Excluded: diabetes < 1 year, obvious anatomical malformation, history of difficult intubation Sample size: 50 28 females Mean age: 57.1 years |
||
| Index tests | MMT, TMD (< 6 cm) | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Wajekar 2015.
| Study characteristics | |||
| Patient sampling | ASA I and II patients above 18 years undergoing elective surgical procedures requiring endotracheal intubation were included in the study | ||
| Patient characteristics and setting | Patients with a history of previous surgery, burns or trauma, tumours/mass in the airways or the cranial, cervical and facial regions, patients with restricted mobility of the neck and mandible (rheumatoid arthritis, cervical disc disorders, or temporomandibular joint disorders), edentulous patients, pregnant patients, and BMI > 26 kg/m2 were excluded from the study Sample size: 402 294 females Mean age: 41.9 years |
||
| Index tests | MMT, TMD, ULBT | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Wilson 1988.
| Study characteristics | |||
| Patient sampling | Patients > 16 years undergoing non‐emergent surgery who underwent anaesthesia by four doctors | ||
| Patient characteristics and setting | Sample size: 778 | ||
| Index tests | Wilson risk score | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test was calculated retrospectively | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Wong 1999.
| Study characteristics | |||
| Patient sampling | All women scheduled for elective caesarean section under GA. Also all women scheduled for elective gynaecological OPs under GA | ||
| Patient characteristics and setting | Sample size: 411 411 females Mean age: 27.9 years |
||
| Index tests | MMT, TMD, combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index test by primary invastigator. Reference standard by attending anaesthesiologist | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Wong 2009.
| Study characteristics | |||
| Patient sampling | A prospective survey on consecutive adult patients scheduled for elective and emergency head and neck surgery requiring GA was performed. Data were collected over a 12‐month period | ||
| Patient characteristics and setting | Sample size: 644 241 females Mean age: 52 years |
||
| Index tests | MMT, TMD, mouth opening (< 2.5 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index tests during preoperative visit. Reference standard in the OR | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Yamamoto 1997.
| Study characteristics | |||
| Patient sampling | Consecutive patients | ||
| Patient characteristics and setting | Routine patient care Sample size: 7270 3635 females Mean age: 52 years |
||
| Index tests | MMT, Wilson risk score | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane | ||
| Flow and timing | Index tests performed 2 days before general surgery | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Yildiz 2005.
| Study characteristics | |||
| Patient sampling | Unknown | ||
| Patient characteristics and setting | Patients presenting to a Turkish hospital. No other details Sample size: 576 346 females Mean age: 45 years |
||
| Index tests | MMT, combination of tests | ||
| Target condition and reference standard(s) | Difficult face mask ventilation | ||
| Flow and timing | Unclear | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Yildiz 2007.
| Study characteristics | |||
| Patient sampling | ASA I–III patients scheduled for elective surgery and requiring endotracheal intubation from seven sites. Patients aged > 18 years, those requiring RSI or an awake intubation, obstetrical patients, surgical procedures involving the upper airway, or patients with a history of difficult intubation or tracheotomy were excluded from the study. No informaiton on selection | ||
| Patient characteristics and setting | Sample size: 1700 994 females Mean age: 43.5 years |
||
| Index tests | MMT, TMD (< 4.8 cm), SMD (< 10.5 cm), mouth opening (< 4 cm), combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack and Lehane; difficult face mask ventilation | ||
| Flow and timing | Index tests: preoperative visit Reference standard: after induction of GA | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
Yu 2015.
| Study characteristics | |||
| Patient sampling | "This prospective, observational study was conducted among patients who had been admitted to our 20‐bed operation center in a university hospital During the observation, 1200 patients scheduled to undergo general anesthesia with endotracheal intubation for elective surgery were screened." | ||
| Patient characteristics and setting | All Chinese patients Sample Size: 732 358 females Mean age 50.8 years |
||
| Index tests | Combination of tests | ||
| Target condition and reference standard(s) | Difficult laryngoscopy: Cormack & Lehane; Difficult tracheal intubation | ||
| Flow and timing | |||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | |||
| Was a case‐control design avoided? | |||
| Did the study avoid inappropriate exclusions? | |||
| DOMAIN 2: Index Test All Tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | |||
| If a threshold was used, was it pre‐specified? | |||
| Did the assessors of the index test have appropriate training? | |||
| Was interobserver variability reported for some or all patients? | |||
| Was interobserver agreement acceptable? | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | |||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | |||
| Did all patients receive the same reference standard? | |||
| Were all patients included in the analysis? | |||
ASA: American Society of Anesthesiologists Physical Status; BMI: body mass index; BURP: backward, upward and rightward pressure; DTA: diagnostic test accuracy; ED: emergency department; EMS: emergency medical services; ENT: ear, nose and throat; ETI: endotracheal intubation; GA: general anaesthesia; ICU: intensive care unit; IDS: intubation difficulty scale; MT: Mallampati test; MMT: modified Mallampati test; OP: operation; OR: operating room; RSI: rapid sequence induction; SMD: sternomental distance; TMD: thyromental distance; ULBT: upper lip bite test
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Acer 2011 | Insufficient data to calculate measures of diagnostic test accuracy |
| Acikgoz 2015 | Insufficient data to calculate measures of diagnostic test accuracy |
| Beyus 2010 | Insufficient data to calculate measures of diagnostic test accuracy |
| Hiremath 1998 | Insufficient data to calculate measures of diagnostic test accuracy |
| Lewis 1994 | Insufficient data to calculate measures of diagnostic test accuracy |
| Meininger 2010 | Insufficient data to calculate measures of diagnostic test accuracy |
| Moon 2013 | Insufficient data to calculate measures of diagnostic test accuracy |
| Oriol‐López 2009 | Insufficient data to calculate measures of diagnostic test accuracy |
| Orozco‐Díaz 2010 | Insufficient data to calculate measures of diagnostic test accuracy |
| Reed 2005 | Insufficient data to calculate measures of diagnostic test accuracy |
| Safavi 2011 | Insufficient data to calculate measures of diagnostic test accuracy |
| Siyam 2002 | Insufficient data to calculate measures of diagnostic test accuracy |
| Tripathi 2006 | Insufficient data to calculate measures of diagnostic test accuracy |
Characteristics of studies awaiting classification [ordered by study ID]
Akhlaghi 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Andrade 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Awan 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Banik 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Belda 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Card 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Carlson 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Dar 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Eiamcharoenwit 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Han 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Hanouz 2018.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Jain 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Khatiwada 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Lee 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Mahmoodpoor 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Norskov 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Prakash 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Rao 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Riad 2018.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Selvi 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Shankar 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Siljeblad 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update. | ||
Srivilaithon 2018.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Torres 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Wang 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Workeneh 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Yildirim 2017.
| Study characteristics | |||
| Patient sampling | |||
| Patient characteristics and setting | |||
| Index tests | |||
| Target condition and reference standard(s) | |||
| Flow and timing | |||
| Comparative | |||
| Notes | Result from top‐up search; will be incorporated into the review at the next update | ||
Differences between protocol and review
We removed the secondary objective of this review: to determine which test or combination of tests has the highest accuracy in studies with direct comparisons for assessing the physical status of the airway in patients with no apparent anatomical airway abnormalities.
Contributions of authors
Conceiving the review: Nathan L Pace (NLP)
Designing the review: Anna Lee (AL), NLP, Harald Herkner (HH), Karen Hovhannisyan (KH)
Co‐ordinating the review: HH, NLP
Undertaking manual searches: KH, HH, Dominik Roth (DR)
Screening search results: DR, NLP, HH, AL
Organizing retrieval of papers: AL, KH, DR, HH
Screening retrieved papers against inclusion criteria: NLP, HH, DR, AL
Appraising quality of papers: NLP, HH, Alexandra Warenits (AW), Jasmin Arrich (JA), DR, AL
Abstracting data from papers: NLP, HH, AW, JA, DR, AL
Writing to authors of papers for additional information: DR, KH, JA
Providing additional data about papers: AL, KH, JA
Obtaining and screening data on unpublished studies: DR, KH
Data management for the review: NLP, HH, DR
Entering data into Review Manager (Review Manager 2014): NLP, HH, DR
Checking data entry in Review Manager (Review Manager 2014): AL, DR
Review Manager statistical data (Review Manager 2014): AL, NLP, HH, DR
Other statistical analysis, not using Review Manager (Review Manager 2014): NLP
Interpretation of data: AL, NLP, HH, DR
Statistical inferences: AL, NLP, HH, DR
Writing the review: AL, NLP, HH , KH, DR, AW, JA
Providing guidance on the review: AL, NLP, HH, KH, DR
Securing funding for the review: not applicable
Performing previous work that was the foundation of the present study: AL
Guarantor for the review (one author): HH
Person responsible for reading and checking review before submission: AL, NLP, HH, KH, AW, JA, DR
Sources of support
Internal sources
The Chinese University of Hong Kong, Shatin, NT, Hong Kong.
Medical University of Vienna, Vienna, Austria.
The Cochrane Anaesthesia Review Group, Rigshospitalet, Copenhagen, Denmark.
University of Utah, Salt Lake City, UT, USA.
Third Cochrane Review Support Programme, Other.
External sources
No sources of support supplied
Declarations of interest
Dominik Roth: none known
Nathan L Pace: none known
Anna Lee: is the first author of a previously published diagnostic test accuracy review of the Mallampati score (Lee 2006).
Karen Hovhannisyan: none known
Alexandra‐Maria Warenits: none known
Jasmin Arrich: none known
Harald Herkner: none known
This review was selected for the third Cochrane Review Support Programme.
Edited (no change to conclusions)
References
References to studies included in this review
Adamus 2010 {published data only}
- Adamus M, Fritscherova S, Hrabalek L, Gabrhelik T, Zapletalova J, Janout V. Mallampati test as a predictor of laryngoscopic view. Biomedical papers of the Medical Faculty of the University Palacký, Olomouc, Czechoslovakia 2010;154(4):339‐43. [PUBMED: 21293546] [DOI] [PubMed] [Google Scholar]
Adnet 2001 {published data only}
- Adnet F, Racine SX, Borron SW, Clemessy JL, Fournier JL, Lapostolle F, et al. A survey of tracheal intubation difficulty in the operating room: a prospective observational study. Acta Anaesthesiologica Scandinavica 2001;45(3):327‐32. [PUBMED: 11207469 ] [DOI] [PubMed] [Google Scholar]
Aktas 2015 {published data only}
- Aktas S, Atalay YO, Tugrul M. Predictive value of bedside tests for difficult intubations. European Review for Medical and Pharmacological Sciences 2015;19(9):1595‐9. [PUBMED: 26004598 ] [PubMed] [Google Scholar]
Ali 2009 {published data only}
- Ali Z, Bithal PK, Prabhakar H, Rath GP, Dash HH. An assessment of the predictors of difficult intubation in patients with acromegaly. Journal of Clinical Neuroscience 2009;16(8):1043‐5. [PUBMED: 19457671 ] [DOI] [PubMed] [Google Scholar]
Ali 2012 {published data only}
- Ali MA, Qamar‐ul‐Hoda M, Samad K. Comparison of upper lip bite test with Mallampati test in the prediction of difficult intubation at a tertiary care hospital of Pakistan. Journal of the Pakistan Medical Association 2012;62(10):1012‐5. [PUBMED: 23866436 ] [PubMed] [Google Scholar]
Allahyary 2008 {published data only}
- Allahyary E, Ghaemei SR, Azemati S. Comparison of six methods for predicting difficult intubation in obstetric patients. Iranian Red Crescent Medical Journal 2008;10(3):197‐204. [Google Scholar]
Al Ramadhani 1996 {published data only}
- Al Ramadhani S, Mohamed LA, Rocke DA, Gouws E. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. British Journal of Anaesthesia 1996;77(3):312‐6. [PUBMED: 8949801 ] [DOI] [PubMed] [Google Scholar]
Ambesh 2013 {published data only}
- Ambesh SP, Singh N, Rao PB, Gupta D, Singh PK, Singh U. A combination of the modified Mallampati score, thyromental distance, anatomical abnormality, and cervical mobility (M‐TAC) predicts difficult laryngoscopy better than Mallampati classification. Acta Anaesthesiologica Taiwanica 2013;51(2):58‐62. [PUBMED: 23968655 ] [DOI] [PubMed] [Google Scholar]
Applegate 2013 {published data only}
- Applegate RL 2nd, Gildea B, Patchin R, Rook JL, Wolford B, Nyirady J, et al. Telemedicine pre‐anesthesia evaluation: a randomized pilot trial. Telemedicine Journal and e‐health 2013;19(3):211‐6. [PUBMED: 23384334 ] [DOI] [PubMed] [Google Scholar]
Arne 1998 {published data only}
- Arné J, Descoins P, Fusciardi J, Ingrand P, Ferrier B, Boudigues D, et al. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. British Journal of Anaesthesia 1998;80(2):140. [PUBMED: 9602574] [DOI] [PubMed] [Google Scholar]
Ayhan 2016 {published data only}
- Ayhan A, Kaplan S, Kayhan Z, Arslan G. Evaluation and management of difficult airway in obesity a single center retrospective study. Acta Clinica Croatica 2016;55(Suppl 1):27‐32. [PUBMED: 27276769 ] [PubMed] [Google Scholar]
Ayuso 2009 {published data only}
- Ayuso MA, Sala X, Luis M, Carbó JM. Predicting difficult orotracheal intubation in pharyngo‐laryngeal disease: preliminary results of a composite index. Canadian Journal of Anesthesia 2003;50(1):81‐5. [PUBMED: 12514157 ] [DOI] [PubMed] [Google Scholar]
Badheka 2016 {published data only}
- Badheka JP, Doshi PM, Vyas AM, Kacha NJ, Parmar VS. Comparison of upper lip bite test and ratio of height to thyromental distance with other airway assessment tests for predicting difficult endotracheal intubation. Indian Journal of Critical Care Medicine 2016;20(1):3‐8. [PUBMED: 26955210 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baig 2014 {published data only}
- Baig MM, Khan FH. To compare the accuracy of prayer's sign and Mallampatti test in predicting difficult intubation in diabetic patients. The Journal of the Pakistan Medical Association 2014;64(8):879‐83. [PUBMED: 25252511 ] [PubMed] [Google Scholar]
Basaranoglu 2010 {published data only}
- Basaranoglu G, Columb M, Lyons G. Failure to predict difficult tracheal intubation for emergency caesarean section. European Journal of Anaesthesiology 2010;27(11):947‐9. [PUBMED: 20864892] [DOI] [PubMed] [Google Scholar]
Basunia 2013 {published data only}
- Basunia SR, Ghosh S, Bhattacharya S, Saha I, Biswas A, Prasad A. Comparison between different tests and their combination for prediction of difficult intubation: An analytical study. Anesthesia, Essays and Researches 2013;7(1):105‐9. [PUBMED: 25885730 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergler 1997 {published data only}
- Bergler W, Maleck W, Baker‐Schreyer A, Petroianu G, Hörmann K. Difficult intubation in otorhinolaryngologic laser surgery. Is there a predictive parameter? [Schwierige Intubation in der HNO‐Laserchirurgie Gibt es einen prädikativen Parameter?]. Hals‐ Nasen‐ und Ohrenärzte 1997;45(11):923‐6. [PUBMED: 9476105 ] [DOI] [PubMed] [Google Scholar]
- Bergler W, Maleck W, Baker‐Schreyer A, Ungemach J, Petroianu G, Hörmann K. The Mallampati Score. Prediction of difficult intubation in otolaryngologic laser surgery by Mallampati Score [Der Mallampati‐Score Vorhersage der schwierigen Intubation in der HNO‐Laserchirurgie mittels Mallampati‐Score]. Anaesthesist 1997;46(5):437‐40. [PUBMED: 9245215 ] [DOI] [PubMed] [Google Scholar]
Bhat 2007 {published data only}
- Bhat RR, Mishra Sk, Badhe AS. Comparison of upper lip bite test and modified Mallampati classification in predicting difficult intubation. The Internet Journal of Anesthesiology 2007;13(1):1‐4. [https://print.ispub.com/api/0/ispub‐article/7795] [Google Scholar]
Bilgin 1998 {published data only}
- Bilgin H, Ozyurt G. Screening tests for predicting difficult intubation. A clinical assessment in Turkish patients. Anaesthesia and Intensive Care 1998;26(4):382‐6. [PUBMED: 9743852 ] [DOI] [PubMed] [Google Scholar]
Bindra 2010 {published data only}
- Adamus M. Comment on the article by Bindra A et al.: Is the modified Mallampati test performed in supine position a reliable predictor of difficult tracheal intubation?. Journal of Anesthesia 2011;25(1):135. [PUBMED: 21052736] [DOI] [PubMed] [Google Scholar]
- Bindra A, Prabhakar H, Singh GP, Ali Z, Singhal V. Is the modified Mallampati test performed in supine position a reliable predictor of difficult tracheal intubation?. Journal of Anesthesia 2010;24(3):482‐5. [PUBMED: 20217151] [DOI] [PubMed] [Google Scholar]
Bouaggad 2004 {published and unpublished data}
- Bouaggad A, Nejmi SE, Bouderka MA, Abbassi O. Prediction of difficult tracheal intubation in thyroid surgery. Anesthesia and Analgesia 2004;99(2):603‐6. [PUBMED: 15271749] [DOI] [PubMed] [Google Scholar]
Breckwoldt 2011 {published data only}
- Breckwoldt J, Klemstein S, Brunne B, Schnitzer L, Mochmann HC, Arntz HR. Difficult prehospital endotracheal intubation ‐ predisposing factors in a physician based EMS. Resuscitation 2011;82(12):1519‐24. [PUBMED: 21749908 ] [DOI] [PubMed] [Google Scholar]
Brodsky 2002 {published and unpublished data}
- Brodsky JB, Lemmens HJ, Brock‐Utne JG, Vierra M, Saidman LJ. Morbid obesity and tracheal intubation. Anesthesia and Analgesia 2002;94(3):732‐6. [PUBMED: 11867407] [DOI] [PubMed] [Google Scholar]
Butler 1992 {published data only}
- Butler PJ, Dhara SS. Prediction of difficult laryngoscopy: an assessment of the thyromental distance and Mallampati predictive tests. Anaesthesia and Intensive Care 1992;20(2):139‐42. [PUBMED: 1595845 ] [DOI] [PubMed] [Google Scholar]
Cattano 2004 {published data only}
- Cattano D, Panicucci E, Paolicchi A, Forfori F, Giunta F, Hagberg C. Risk factors assessment of the difficult airway: an Italian survey of 1956 patients. Anesthesia and Analgesia 2004;99(6):1774‐9. [PUBMED: 15562070 ] [DOI] [PubMed] [Google Scholar]
Cattano 2014 {published data only}
- Cattano D, Katsiampoura A, Corso RM, Killoran PV, Cai C, Hagberg CA. Predictive factors for difficult mask ventilation in the obese surgical population. F1000Research 2014;9(3):239. [PUBMED: 25485099 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaves 2009 {published data only}
- Chaves A, Carvalho S, Botelho M. Difficult endotracheal intubation In thyroid surgery: A retrospective study. The Internet Journal of Anesthesiology 2009;22(1):1‐4. [Google Scholar]
Choi 2013 {published data only}
- Choi JW, Kim JA, Kim HK, Oh MS, Kim DK. Chest anteroposterior diameter affects difficulty of laryngoscopy for non‐morbidly obese patients. Journal of Anesthesia 2013;27(4):563‐8. [PUBMED: 23455773 ] [DOI] [PubMed] [Google Scholar]
Connor 2011 {published data only}
- Connor CW, Segal S. Accurate classification of difficult intubation by computerized facial analysis. Anesthesia and Analgesia 2011;112(1):84‐93. [PUBMED: 21081769] [DOI] [PubMed] [Google Scholar]
Cortellazzi 2007 {published data only}
- Cortellazzi P, Minati L, Falcone C, Lamperti M, Caldiroli D. Predictive value of the El‐Ganzouri multivariate risk index for difficult tracheal intubation: a comparison of Glidescope videolaryngoscopy and conventional Macintosh laryngoscopy. British Journal of Anaesthesia 2007;99(6):906‐11. [PUBMED: 17962241 ] [DOI] [PubMed] [Google Scholar]
De Jong 2015 {published data only}
- Jong A, Molinari N, Pouzeratte Y, Verzilli D, Chanques G, Jung B, et al. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. British Journal of Anaesthesia 2015;114(2):297‐306. [PUBMED: 25431308 ] [DOI] [PubMed] [Google Scholar]
Descoins 1994 {published data only}
- Descoins P, Arné J, Bresard D, Ariès J, Fusciardi J. Proposal for a new multifactor screening score of difficult intubation in ORL and stomatognathic surgery: preliminary study. Annales Françaises d'anesthèsie et de Rèanimation 1994;13(2):195‐200. [PUBMED: 7818203 ] [DOI] [PubMed] [Google Scholar]
Dohrn 2015 {published data only}
- Dohrn N, Sommer T, Bisgaard J, Rønholm E, Larsen JF. Difficult tracheal intubation in obese gastric bypass patients. Obesity Surgery 2016;26(11):2640‐7. [PUBMED: 26989060 ] [DOI] [PubMed] [Google Scholar]
Domi 2009 {published data only}
- Domi R. A comparison of Wilson Sum Score and Combination Mallampati, Tiromental and Sternomental Distances for predicting difficult intubation. Macedonian Journal of Medical Sciences 2009;2(2):141‐4. [DOI: 10.3889/MJMS.1857-5773.2009.0045] [DOI] [Google Scholar]
Domi 2010 {published data only}
- Domi R. The best prediction test of difficult intubation. Journal of Anaesthesiology Clinical Pharmacololgy 2010;26(2):193‐6. [Google Scholar]
Eberhart 2005 {published data only}
- Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: an external prospective evaluation. Anesthesia and Analgesia 2005;101(1):284‐9. [PUBMED: 15976247] [DOI] [PubMed] [Google Scholar]
El‐Ganzouri 1996 {published data only}
- el‐Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: predictive value of a multivariate risk index. Anesthesia and Analgesia 1996;82(6):1197‐204. [PUBMED: 8638791 ] [DOI] [PubMed] [Google Scholar]
Ezri 2001 {published data only}
- Ezri T, Warters RD, Szmuk P, Saad‐Eddin H, Geva D, Katz J, et al. The incidence of class "zero" airway and the impact of Mallampati score, age, sex, and body mass index on prediction of laryngoscopy grade. Anesthesia and Analgesia 2001;93(4):1073‐5. [PUBMED: 11574386 ] [DOI] [PubMed] [Google Scholar]
Ezri 2003a {published data only}
- Ezri T, Medalion B, Weisenberg M, Szmuk P, Warters RD, Charuzi I. Increased body mass index per se is not a predictor of difficult laryngoscopy. Canadian Journal of Anaesthesia = Journal Canadien d'anesthésie 2003;50(2):179‐83. [PUBMED: 12560311 ] [DOI] [PubMed] [Google Scholar]
Ezri 2003b {published data only}
- Ezri T, Weisenberg M, Khazin V, Zabeeda D, Sasson L, Shachner A, et al. Difficult laryngoscopy: incidence and predictors in patients undergoing coronary artery bypass surgery versus general surgery patients. Journal of Cardiothoracic Anesthesia 2003;17(3):321‐4. [PUBMED: 12827579 ] [DOI] [PubMed] [Google Scholar]
Ezri 2003c {published data only}
- Ezri T, Gewürtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia 2003;58(11):1111‐4. [PUBMED: 14616599] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frerk 1991 {published data only}
- Frerk CM. Predicting difficult intubation. Anaesthesia 1991;46(12):1005‐8. [PUBMED: 1781521 ] [DOI] [PubMed] [Google Scholar]
Frerk 1996 {published data only}
- Frerk CM, Till CB, Bradley AJ. Difficult intubation: thyromental distance and the atlanto‐occipital gap. Anaesthesia 1996;51(8):738‐40. [PUBMED: 8795315 ] [DOI] [PubMed] [Google Scholar]
Freund 2012 {published data only}
- Freund Y, Duchateau FX, Devaud ML, Ricard‐Hibon A, Juvin P, Mantz J. Factors associated with difficult intubation in prehospital emergency medicine. European Journal of Emergency Medicine 2012;19(5):304‐8. [PUBMED: 22008586 ] [DOI] [PubMed] [Google Scholar]
Fritscherova 2011 {published data only}
- Fritscherova S, Adamus M, Dostalova K, Koutna J, Hrabalek L, Zapletalova J, et al. Can difficult intubation be easily and rapidly predicted?. Biomedical Papers of the Medical Faculty of the University Palacký, Olomouc, Czechoslovakia 2011;155(2):165‐71. [PUBMED: 21804626] [DOI] [PubMed] [Google Scholar]
Gonzalez 2008 {published data only}
- Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesthesia and Analgesia 2008;106(4):1132‐6. [PUBMED: 18349184] [DOI] [PubMed] [Google Scholar]
Hagberg 2009 {published data only}
- Hagberg CA, Vogt‐Harenkamp C, Kamal J. A retrospective analysis of airway management in obese patients at a teaching institution. Journal of Clinical Anesthesia 2009;21(5):348‐51. [PUBMED: 19700274] [DOI] [PubMed] [Google Scholar]
Hagiwara 2015 {published data only}
- Hagiwara Y, Watase H, Okamoto H, Goto T, Hasegawa K, Japanese Emergency Medicine Network Investigators. Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. The American Journal of Emergency Medicine 2015;33(10):1492‐6. [PUBMED: 26166379 ] [DOI] [PubMed] [Google Scholar]
Hashim 2014 {published data only}
- Hashim K, Thomas M. Sensitivity of palm print sign in prediction of difficult laryngoscopy in diabetes: A comparison with other airway indices. Indian Journal of Anaesthesia 2014;58(3):298‐302. [PUBMED: 25024473 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Healy 2016 {published data only}
- Healy DW, LaHart EJ, Peoples EE, Jewell ES, Bettendorf RJ Jr, Ramachandran SK. A comparison of the Mallampati evaluation in neutral or extended cervical spine positions: a retrospective observational study of > 80,000 patients. British Journal of Anaesthesia 2016;116(5):690‐8. [PUBMED: 27106973 ] [DOI] [PubMed] [Google Scholar]
Heinrich 2013 {published data only}
- Heinrich S, Birkholz T, Irouschek A, Ackermann A, Schmidt J. Incidences and predictors of difficult laryngoscopy in adult patients undergoing general anesthesia: a single‐center analysis of 102,305 cases. Journal of Anesthesia 2013;27(6):815‐21. [PUBMED: 23748552 ] [DOI] [PubMed] [Google Scholar]
Hekiert 2007 {published data only}
- Hekiert AM, Mandel J, Mirza N. Laryngoscopies in the obese: predicting problems and optimizing visualization. Annals of Otology, Rhinology and Laryngology 2007;116(4):312‐6. [PUBMED: 17491533 ] [DOI] [PubMed] [Google Scholar]
Hirmanpour 2014 {published data only}
- Hirmanpour A, Safavi M, Honarmand A, Jabalameli M, Banisadr G. The predictive value of the ratio of neck circumference to thyromental distance in comparison with four predictive tests for difficult laryngoscopy in obstetric patients scheduled for caesarean delivery. Advanced Biomedical Research 2014;3:200. [PUBMED: 25337530 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Honarmand 2008 {published data only}
- Honarmand A, Safavi MR. Prediction of difficult laryngoscopy in obstetric patients scheduled for Caesarean delivery. European Journal of Anaesthesiology 2008;25(9):714‐20. [PUBMED: 18471331] [DOI] [PubMed] [Google Scholar]
Honarmand 2014 {published data only}
- Honarmand A, Safavi M, Ansari N. A comparison of between hyomental distance ratios, ratio of height to thyromental, modified Mallamapati classification test and upper lip bite test in predicting difficult laryngoscopy of patients undergoing general anesthesia. Advanced Biomedical Research 2014;3:166. [PUBMED: 25221769 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Honarmand 2015 {published data only}
- Honarmand A, Safavi M, Yaraghi A, Attari M, Khazaei M, Zamani M. Comparison of five methods in predicting difficult laryngoscopy: Neck circumference, neck circumference to thyromental distance ratio, the ratio of height to thyromental distance, upper lip bite test and Mallampati test. Advanced Biomedical Research 2015;4:122. [PUBMED: 26261824 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huh 2009 {published data only}
- Huh J, Shin HY, Kim SH, Yoon TK, Kim DK. Diagnostic predictor of difficult laryngoscopy: the hyomental distance ratio. Anesthesia and Analgesia 2009;108(2):544‐8. [PUBMED: 19151285] [DOI] [PubMed] [Google Scholar]
Hui 2009 {published data only}
- Hui C, Tsui BC. Sublingual ultrasound examination of the airway: a pilot study. Canadian Journal of Anaesthesia = Journal Canadien d'anesthésie 2009;56:S1‐150. [DOI] [PubMed] [Google Scholar]
Istvan 2010 {published data only}
- Istvan J, Belliveau M, Donati F. Rapid sequence induction for appendectomies: a retrospective case‐review analysis. Canadian Journal of Anaesthesia = Journal Canadien d'anesthésie 2010;57(4):330‐6. [PUBMED: 20049576 ] [DOI] [PubMed] [Google Scholar]
Ittichaikulthol 2010 {published data only}
- Ittichaikulthol W, Chanpradub S, Amnoundetchakorn S, Arayajarernwong N, Wongkum W. Modified Mallampati test and thyromental distance as a predictor of difficult laryngoscopy in Thai patients. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet 2010;93(1):84‐9. [PUBMED: 20196416] [PubMed] [Google Scholar]
Juvin 2003 {published data only}
- Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesthesia and Analgesia 2003;97(2):595‐600. [PUBMED: 12873960 ] [DOI] [PubMed] [Google Scholar]
Kalezic 2016 {published data only}
- Kalezić N, Lakićević M, Miličić B, Stojanović M, Sabljak V, Marković D. Hyomental distance in the different head positions and hyomental distance ratio in predicting difficult intubation. Bosnian Journal of Basic Medical Sciences / Udruženje Basičnih Mediciniskih Znanost 2016;16(3):232‐6. [PUBMED: 27299374 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamalipour 2005 {published data only}
- Kamalipour H, Bagheri M, Kamali K, Taleie A, Yarmohammadi H. Lateral neck radiography for prediction of difficult orotracheal intubation. European Journal of Anaesthesiology 2005;22(9):689‐93. [PUBMED: 16163916] [DOI] [PubMed] [Google Scholar]
Kamranmanesh 2013 {published data only}
- Kamranmanesh MR, Jafari AR, Gharaei B, Aghamohammadi H, Poor Zamany NKM, Kashi AH. Comparison of acromioaxillosuprasternal notch index (a new test) with modified Mallampati test in predicting difficult visualization of larynx. Acta Anaesthesiologica Taiwanica 2013;51(4):141‐4. [PUBMED: 24529668 ] [DOI] [PubMed] [Google Scholar]
Khan 2003 {published data only}
- Khan ZH, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a simple new technique) with modified Mallampati classification in predicting difficulty in endotracheal intubation: a prospective blinded study. Anesthesia and Analgesia 2003;96(2):595‐9. [PUBMED: 12538218] [DOI] [PubMed] [Google Scholar]
Khan 2009a {published data only}
- Khan ZH, Mohammadi M, Rasouli MR, Farrokhnia F, Khan RH. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesthesia and Analgesia 2009;109(3):822‐4. [PUBMED: 19690252] [DOI] [PubMed] [Google Scholar]
Khan 2009b {published data only}
- Khan ZH, Mofrad MK, Arbabi S, Javid MJ, Makarem J. Upper lip bite test as a predictor of difficult mask ventilation: a prospective study. Middle East Journal of Anaesthesiology 2009;20(3):377‐82. [PUBMED: 19950730] [PubMed] [Google Scholar]
Khan 2011 {published data only}
- Khan ZH, Maleki A, Makarem J, Mohammadi M, Khan RH, Zandieh A. A comparison of the upper lip bite test with hyomental/thyrosternal distances and mandible length in predicting difficulty in intubation: A prospective study. Indian Journal of Anaesthesia 2011;55(1):43‐6. [PUBMED: 21431052 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2013 {published data only}
- Khan ZH, Arbabi S. Diagnostic value of the upper lip bite test in predicting difficulty in intubation with head and neck landmarks obtained from lateral neck X‐ray. Indian Journal of Anaesthesia 2013;57(4):381‐6. [PUBMED: 24163453 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2014 {published data only}
- Khan ZH, Arbabi S, Yekaninejad MS, Khan RH. Application of the upper lip catch test for airway evaluation in edentulous patients: An observational study. Saudi Journal of Anaesthesia 2014;8(1):73‐7. [PUBMED: 24665244 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2015 {published data only}
- Khan ZH, Eskandari S, Yekaninejad MS. A comparison of the Mallampati test in supine and upright positions with and without phonation in predicting difficult laryngoscopy and intubation: A prospective study. Journal of Anaesthesiology, Clinical Pharmacology 2015;31(2):207‐11. [PUBMED: 25948902 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kheterpal 2009 {published data only}
- Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology 2009;110(4):891‐7. [PUBMED: 19293691 ] [DOI] [PubMed] [Google Scholar]
Kim 2011 {published data only}
- Kim WH, Ahn HJ, Lee CJ, Shin BS, Ko JS, Choi SJ, et al. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. British Journal of Anaesthesia 2011;106(5):743‐8. [PUBMED: 21354999 ] [DOI] [PubMed] [Google Scholar]
K Nasa 2014 {published data only}
- K Nasa V, S Kamath S. Risk factors assessment of the difficult intubation using intubation difficulty scale (IDS). Journal of Clinical and Diagnostic Research: JCDR 2014;8(7):GC01‐3. [PUBMED: 25177576 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Knudsen 2014 {published data only}
- Knudsen K, Högman M, Larsson A, Nilsson U. The best method to predict easy intubation: a quasi‐experimental pilot study. Journal of Perianesthesia Nursing 2014;29(4):292‐7. [PUBMED: 25062573 ] [DOI] [PubMed] [Google Scholar]
Koh 2002 {published data only}
- Koh LK, Kong CE, Ip‐Yam PC. The modified Cormack‐Lehane score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesthesia and Intensive Care 2002;30(1):48‐51. [PUBMED: 11939440 ] [DOI] [PubMed] [Google Scholar]
Kolarkar 2015 {published data only}
- Kolarkar P, Badwaik G, Watve A, Abhishek K, Bhangale N, Bhalerao A, et al. Upper lip bite test: A novel test of predicting difficulty in intubation. Journal of Evolution of Medical and Dental Sciences 2015;4(24):4149‐56. [Google Scholar]
Komatsu 2007 {published data only}
- Komatsu R, Sengupta P, Wadhwa A, Akça O, Sessler DI, Ezri T, et al. Ultrasound quantification of anterior soft tissue thickness fails to predict difficult laryngoscopy in obese patients. Anaesthesia and Intensive Care 2007;35(1):32‐7. [PUBMED: 17323663 ] [DOI] [PubMed] [Google Scholar]
Konwar 2015 {published data only}
- Konwar C, Baruah ND, Saikia P, Chakrabartty A. A prospective study of the usefulness of upper lip bite test in combination with sternomental distance, thyromental distance and inter‐incisor distance as predictor of ease of laryngoscopy. Journal of Evolution of Medical and Dental Sciences 2015;4(97):16286‐89. [Google Scholar]
Krobbuaban 2005 {published data only}
- Krobbuaban B, Diregpoke S, Kumkeaw S. An assessment of the ratio of height to thyromental distance compared to thyromental distance as a predictive test for prediction of difficult tracheal intubation in Thai patients. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet 2006;89(5):638‐42. [PUBMED: 16756049] [PubMed] [Google Scholar]
- Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: four predictive tests for difficult laryngoscopy. Anesthesia and Analgesia 2005;101(5):1542‐5. [PUBMED: 16244029 ] [DOI] [PubMed] [Google Scholar]
Langeron 2000 {published data only}
- Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology 2000;92(5):1229‐36. [PUBMED: 10781266 ] [DOI] [PubMed] [Google Scholar]
Lee 2015 {published data only}
- Lee SL, Hosford C, Lee QT, Parnes SM, Shapshay SM. Mallampati class, obesity, and a novel airway trajectory measurement to predict difficult laryngoscopy. Laryngoscope 2015;125(1):161‐6. [PUBMED: 25042696 ] [DOI] [PubMed] [Google Scholar]
Liaskou 2014 {published data only}
- Liaskou C, Vouzounerakis E, Moirasgenti M, Trikoupi A, Staikou C. Anatomic features of the neck as predictive markers of difficult direct laryngoscopy in men and women: A prospective study. Indian Journal of Anaesthesia 2014;58(2):176‐82. [PUBMED: 24963183 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lundstrom 2009 {published data only}
- Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Gätke MR, Wetterslev J, et al. A documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia 2009;64(10):1081‐8. [PUBMED: 19735399 ] [DOI] [PubMed] [Google Scholar]
- Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Gätke MR, Wetterslev J, et al. Avoidance of neuromuscular blocking agents may increase the risk of difficult tracheal intubation: a cohort study of 103,812 consecutive adult patients recorded in the Danish Anaesthesia Database. British Journal of Anaesthesia 2009;103(2):283‐90. [PUBMED: 19457894] [DOI] [PubMed] [Google Scholar]
- Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology 2009;110(2):266‐74. [PUBMED: 19194154] [DOI] [PubMed] [Google Scholar]
Mallat 2010 {published data only}
- Mallat J, Robin E, Pironkov A, Lebuffe G, Tavernier B. Goitre and difficulty of tracheal intubation. Annales Françaises d'anesthèsie et de Rèanimation 2010;296(6):436‐9. [PUBMED: 20547033] [DOI] [PubMed] [Google Scholar]
Mashour 2008 {published data only}
- Mashour GA, Kheterpal S, Vanaharam V, Shanks A, Wang LY, Sandberg WS, et al. The extended Mallampati score and a diagnosis of diabetes mellitus are predictors of difficult laryngoscopy in the morbidly obese. Anesthesia and Analgesia 2008;107(6):1919‐23. [PUBMED: 19020139 ] [DOI] [PubMed] [Google Scholar]
Mehta 2014 {published data only}
- Mehta T, Jayaprakash J, Shah V. Diagnostic value of different screening tests in isolation or combination for predicting difficult intubation: A prospective study. Indian Journal of Anaesthesia 2014;58(6):754‐7. [PUBMED: 25624545 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Merah 2004 {published data only}
- Merah NA, Foulkes‐Crabbe DJ, Kushimo OT, Ajayi PA. Prediction of difficult laryngoscopy in a population of Nigerian obstetric patients. West African Journal of Medicine 2004;23(1):38‐41. [PUBMED: 15171524 ] [DOI] [PubMed] [Google Scholar]
- Merah NA, Wong DT, Ffoulkes‐Crabbe DJ, Kushimo OT, Bode CO. Modified Mallampati test, thyromental distance and inter‐incisor gap are the best predictors of difficult laryngoscopy in West Africans. Canadian Journal of Anesthesia 2005;52(3):291‐6. [PUBMED: 15753502 ] [DOI] [PubMed] [Google Scholar]
Mishra 2009 {published data only}
- Mishra SK, Bhat RR, Sudeep K, Nagappa M, Badhe AS. Comparison of upper lip bite test with modified Mallampati classification for prediction of difficult obstetric intubation. The Internet Journal of Anesthesiology 2010;19(1):1‐3. [Google Scholar]
Montemayor‐Cruz 2015 {published data only}
- Montemayor‐Cruz JM, Guerrero‐Ledezma RM. Diagnostic utility of the hyomental distance ratio as predictor of difficult intubation at UMAE 25. Gaceta Médica de México 2015;151(5):599‐607. [PUBMED: 26526473 ] [PubMed] [Google Scholar]
Myneni 2010 {published data only}
- Myneni N, O'Leary AM, Sandison M, Roberts K. Evaluation of the upper lip bite test in predicting difficult laryngoscopy. Journal of Clinical Anesthesia 2010;22(3):174‐8. [PUBMED: 20400002] [DOI] [PubMed] [Google Scholar]
Nadal 1998 {published data only}
- Nadal JL, Fernandez BG, Escobar IC, Black M, Rosenblatt WH. The palm print as a sensitive predictor of difficult laryngoscopy in diabetics. Acta Anaesthesiologica Scandinavica 1998;42(2):199‐203. [PUBMED: 9509203 ] [DOI] [PubMed] [Google Scholar]
- Rae R, Kinsella J, Daniel M, Booth M. The palm print as predictor of difficult intubation. Acta Anaesthesiologica Scandinavica 2001;45(8):1053. [PUBMED: 11576065 ] [DOI] [PubMed] [Google Scholar]
Naguib 1999 {published data only}
- Naguib M, Malabarey T, AlSatli RA, Al Damegh S, Samarkandi AH. Predictive models for difficult laryngoscopy and intubation. A clinical, radiologic and three‐dimensional computer imaging study. Canadian Journal of Anaesthesia = Journal Canadien d'anesthésie 1999;46(8):748‐59. [PUBMED: 10451134 ] [DOI] [PubMed] [Google Scholar]
Naguib 2006 {published data only}
- Naguib M, Scamman FL, O'Sullivan C, Aker J, Ross AF, Kosmach S, et al. Predictive performance of three multivariate difficult tracheal intubation models: a double‐blind, case‐controlled study. Anesthesia and Analgesia 2006;102(3):818‐24. [PUBMED: 16492835 ] [DOI] [PubMed] [Google Scholar]
Nasir 2011 {published data only}
- Nasir KK, Shahani AS, Maqbool MS. Correlative value of airway assessment by Mallampati classification and Cormack and Lehane grading. Rawal Medical Journal 2011;36:2‐4. [Google Scholar]
Nasiri 2013 {published data only}
- Nasiri E, Akbari H, Farrokhi H, Ebrahimi F, Nasiri R. A comparison of the Upper Lip Bite Test with Inter Incisor Distance in predicting difficult laryngoscopy and tracheal intubation. Journal of Mazandaran University of Medical Sciences 2013;23(105):71‐9. [Google Scholar]
Nath 1997 {published data only}
- Nath G, Sekar M. Predicting difficult intubation ‐ a comprehensive scoring system. Anaesthesia and Intensive Care 1997;25(5):482‐6. [PUBMED: 9352759 ] [DOI] [PubMed] [Google Scholar]
Noorizad 2006 {published data only}
- Noorizad S, Mahdian M. Mallampati and thyromental distance to predict difficult intubation. Journal of Medical Sciences 2006;6(2):169‐72. [Google Scholar]
Oates 1990 {published data only}
- Oates JD, Oates PD, Pearsall FJ, McLeod AD, Howie JC. Phonation affects Mallampati class. Anaesthesia 1990;45(11):984. [PUBMED: 2082969 ] [DOI] [PubMed] [Google Scholar]
Oates 1991 {published data only}
- Oates JD, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. British Journal of Anaesthesia 1991;66(3):305‐9. [PUBMED: 2015145 ] [DOI] [PubMed] [Google Scholar]
Pottecher 1991 {published data only}
- Pottecher T, Velten M, Galani M, Forrler M. Comparative value of clinical signs of difficult tracheal intubation in women. Annales Françaises d'anesthèsie et de Rèanimation 1991;10(5):430‐5. [PUBMED: 1755552 ] [DOI] [PubMed] [Google Scholar]
Prakash 2013 {published data only}
- Prakash S, Kumar A, Bhandari S, Mullick P, Singh R, Gogia AR. Difficult laryngoscopy and intubation in the Indian population: An assessment of anatomical and clinical risk factors. Indian Journal of Anaesthesia 2013;57(6):569‐75. [PUBMED: 24403616 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Qudaisat 2011 {published data only}
- Qudaisat IY, Al‐Ghanem SM. Short thyromental distance is a surrogate for inadequate head extension, rather than small submandibular space, when indicating possible difficult direct laryngoscopy. European Journal of Anaesthesiology 2011;28(8):600‐6. [PUBMED: 21610502] [DOI] [PubMed] [Google Scholar]
Reghunathan 2016 {published data only}
- Reghunathan U, Raghavan RK, Veetil BM. Airway assessment for anticipation of difficult intubation: a double blind comparative study. Journal of Evolution Medical and Dental Sciences 2016;5(40):2466‐9. [Google Scholar]
Rocke 1992 {published data only}
- Rocke DA, Murray WB, Rout CC, Gouws E. Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiology 1992;77(1):67‐73. [PUBMED: 1610011 ] [DOI] [PubMed] [Google Scholar]
Safavi 2014 {published data only}
- Safavi M, Honarmand A, Amoushahi M. Prediction of difficult laryngoscopy: Extended mallampati score versus the MMT, ULBT and RHTMD. Advances in Biomedical Engineering Research 2014;3:133. [PUBMED: 24949304 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sahin 2011 {published data only}
- Sahin SH, Yilmaz A, Gunday I, Kargi M, Sut N, Taskinalp O, et al. Using temporomandibular joint mobility to predict difficult tracheal intubation. Journal of Anesthesia 2011;25(3):457‐61. [PUBMED: 21451975 ] [DOI] [PubMed] [Google Scholar]
Salimi 2008 {published data only}
- Salimi A, Farzanegan B, Rastegarpour A, Kolahi AA. Comparison of the upper lip bite test with measurement of thyromental distance for prediction of difficult intubations. Acta Anaesthesiologica Taiwanica 2008;46(2):61‐5. [PUBMED: 18593650 ] [DOI] [PubMed] [Google Scholar]
Samra 1995 {published data only}
- Samra SK, Schork MA, Guinto FC Jr. A study of radiologic imaging techniques and airway grading to predict a difficult endotracheal intubation. Journal of Clinical Anesthesia 1995;7(5):373‐9. [PUBMED: 7576671] [DOI] [PubMed] [Google Scholar]
Savva 1994 {published data only}
- Savva D. Prediction of difficult tracheal intubation. British Journal of Anaesthesia 1994;73(2):149‐53. [PUBMED: 7917726 ] [DOI] [PubMed] [Google Scholar]
Schmitt 2000 {published data only}
- Schmitt H, Buchfelder M, Radespiel‐Tröger M, Fahlbusch R. Difficult intubation in acromegalic patients: incidence and predictability. Anesthesiology 2000;93(1):110‐4. [PUBMED: 10861153 ] [DOI] [PubMed] [Google Scholar]
Seo 2012 {published data only}
- Seo SH, Lee JG, Yu SB, Kim DS, Ryu SJ, Kim KH. Predictors of difficult intubation defined by the intubation difficulty scale (IDS): predictive value of 7 airway assessment factors. Korean Journal of Anesthesiology 2012;63(6):491‐7. [PUBMED: 23277808 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2013 {published data only}
- Shah PJ, Dubey KP, Yadav JP. Predictive value of upper lip bite test and ratio of height to thyromental distance compared to other multivariate airway assessment tests for difficult laryngoscopy in apparently normal patients. Journal of Anaesthesiology, Clinical Pharmacology 2013;29(2):191‐5. [PUBMED: 23878440 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2014 {published data only}
- Shah AA, Rafique K, Islam M. Can difficult intubation be accurately predicted using upper lip bite test?. Journal of Postgraduate Medical Institute 2014;28(3):282‐7. [Google Scholar]
Sharma 2010 {published data only}
- Sharma D, Prabhakar H, Bithal PK, Ali Z, Singh GP, Rath GP, et al. Predicting difficult laryngoscopy in acromegaly: a comparison of upper lip bite test with modified Mallampati classification. Journal of Neurosurgical Anesthesiology 2010;22(2):138‐43. [PUBMED: 20118795 ] [DOI] [PubMed] [Google Scholar]
Singh 2009 {published data only}
- Singh R, Jain A, Swatantra M, Kohli P. Clinical evaluation of predicting difficult laryngoscopy in obstetric patients. Journal of Anaesthesiology, Clinical Pharmacology 2009;25(1):38‐42. [Google Scholar]
Soyuncu 2009 {published data only}
- Soyuncu S, Eken C, Cete Y, Bektas F, Akcimen M. Determination of difficult intubation in the ED. The American Journal of Emergency Medicine 2009;27(8):905‐10. [PUBMED: 19857405 ] [DOI] [PubMed] [Google Scholar]
Tantri 2016 {published data only}
- Tantri AR, Firdaus R, Salomo ST. Predictors of difficult intubation among Malay patients in Indonesia. Anesthesiology and Pain Medicine 2016;6(2):e34848. [PUBMED: 27252905 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 2009 {published data only}
- Thompson J, O'Neill SS, Hutchings L, Jones R. Retrospective study of 1602 obstetric intubations: predicting difficult and failed intubation using the Mallampati test. International Journal of Obstetric Anesthesia 2009;18:S1‐63. [DOI: ] [Google Scholar]
Tse 1995 {published data only}
- Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: a prospective blind study. Anesthesia and Analgesia 1995;81(2):254‐8. [PUBMED: 7618711 ] [DOI] [PubMed] [Google Scholar]
Tuzuner‐Oncul 2008 {published data only}
- Tuzuner‐Oncul AM, Kucukyavuz Z. Prevalence and prediction of difficult intubation in maxillofacial surgery patients. Journal of Oral and Maxillofacial Surgery 2008;66(8):1652‐8. [PUBMED: 18634954 ] [DOI] [PubMed] [Google Scholar]
Ul Haq 2013 {published data only}
- Ul Haq MI, Ullah H. Comparison of Mallampati test with lower jaw protrusion maneuver in predicting difficult laryngoscopy and intubation. Journal of Anaesthesiology, Clinical Pharmacology 2013;29(3):313‐7. [PUBMED: 24106353 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uribe 2015 {published data only}
- Uribe AA, Zvara DA, Puente EG, Otey AJ, Zhang J, Bergese SD. BMI as a predictor for potential difficult tracheal intubation in males. Frontiers in Medicine (Lausanne) 2015;2(38):e. [PUBMED: 26137460 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vallem 2015 {published data only}
- Vallem B, Thalisetty J, Challapalli SR, Israel N, Gudise S, Murthigari S. Comparison of upper lip bite test with other four predictors for predicting difficulty in intubation. Journal of Evolution of Medical and Dental Sciences 2015;4(39):6811‐7. [DOI: 10.14260/jemds/2015/988] [DOI] [Google Scholar]
Vani 2000 {published data only}
- Vani V, Kamath SK, Naik LD. The palm print as a sensitive predictor of difficult laryngoscopy in diabetics: a comparison with other airway evaluation indices. Journal of Postgraduate Medicine 2000;46(2):75‐9. [PUBMED: 11013469 ] [PubMed] [Google Scholar]
Wajekar 2015 {published data only}
- Wajekar AS, Chellam S, Toal PV. Prediction of ease of laryngoscopy and intubation‐role of upper lip bite test, modified mallampati classification, and thyromental distance in various combination. Journal of Family Medicine and Primary Care 2015;4(1):101‐5. [PUBMED: 25810998 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 1988 {published data only}
- Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. British Journal of Anaesthesia 1988;61(2):211‐6. [PUBMED: 3415893 ] [DOI] [PubMed] [Google Scholar]
Wong 1999 {published data only}
- Wong SH, Hung CT. Prevalence and prediction of difficult intubation in Chinese women. Anaesthesia and Intensive Care 1999;27(1):49‐52. [PUBMED: 10050224 ] [DOI] [PubMed] [Google Scholar]
Wong 2009 {published data only}
- Wong P, Parrington S. Difficult intubation in ENT and maxillofacial surgical patients: a prospective survey. The Internet Journal of Anesthesiology 2009;21(1):1‐3. [Google Scholar]
Yamamoto 1997 {published data only}
- Yamamoto K, Tsubokawa T, Shibata K, Ohmura S, Nitta S, Kobayashi T. Predicting difficult intubation with indirect laryngoscopy. Anesthesiology 1997;86(2):316‐21. [PUBMED: 9054250 ] [DOI] [PubMed] [Google Scholar]
Yildiz 2005 {published data only}
- Yildiz TS, Solak M, Toker K. The incidence and risk factors of difficult mask ventilation. Journal of Anesthesia 2005;19(1):7‐11. [PUBMED: 15674508 ] [DOI] [PubMed] [Google Scholar]
Yildiz 2007 {published data only}
- Yildiz TS, Korkmaz F, Solak M, Toker K, Erciyes N, Bayrak F, et al. Prediction of difficult tracheal intubation in Turkish patients: a multi‐center methodological study. European Journal of Anaesthesiology 2007;24(12):1034‐40. [PUBMED: 17555609 ] [DOI] [PubMed] [Google Scholar]
Yu 2015 {published data only}
- Yu T, Wang B, Jin XJ, Wu RR, Wu H, He JJ, et al. Predicting difficult airways: 3‐3‐2 rule or 3‐3 rule?. Irish Journal of Medical Science 2015;184(3):677‐83. [PUBMED: 25740093 ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Acer 2011 {published data only}
- Acer N, Akkaya A, Tugay BU, Öztürk A. A comparison of Cormack‐Lehane and Mallampati tests with mandibular and neck measurements for predicting difficult intubation [Zor Entübasyonu Tahmin Etmek İçin Cormeck‐Lehane ve Mallampati Testleri İle Mandibula ve Boyun Ölçümlerinin Karşılaştırılması]. Balkan Medical Journal 2011;28:157‐63. [DOI: 10.5174/tutfd.2010.03475.1] [DOI] [Google Scholar]
Acikgoz 2015 {published data only}
- Acikgoz AO, Karagoz H, Yilbas AA, Akca B, Uzumcugil F, Pamuk G. Difficult airway and risk factors in bariatric surgery patients. Bariatric Surgical Practice and Patient Care 2015;10(4):145‐9. [DOI: 10.1089/bari.2015.0026] [DOI] [Google Scholar]
Beyus 2010 {published data only}
- Beyus C, Mort T. Challenges of airway management in obesity. Thirty‐Ninth Critical Care Congress of the Society of Critical Care Medicine; 2010 Jan 9‐13; Miami Beach (FL). Miami Beach, FL: Society of Critical Care Medicine, 2010.
Hiremath 1998 {published data only}
- Hiremath AS, Hillman DR, James AL, Noffsinger WJ, Platt PR, Singer SL. Relationship between difficult tracheal intubation and obstructive sleep apnoea. British Journal of Anaesthesia 1998;80:606‐11. [DOI] [PubMed] [Google Scholar]
Lewis 1994 {published data only}
- Lewis M, Keramati S, Benumof JL, Berry CC. What is the best way to determine oropharyngeal classification and mandibular space length to predict difficult laryngoscopy?. Anaesthesiology 1994;81:69‐75. [DOI] [PubMed] [Google Scholar]
Meininger 2010 {published data only}
- Meininger D, Strouhal U, Weber CF, Fogl D, Holzer L, Zacharowski K, et al. Direct laryngoscopy or C‐MAC video laryngoscopy? Routine tracheal intubation in patients undergoing ENT surgery [Direkte laryngoskopie oder C‐MAC‐ Vvdeolaryngoskopie? Routineintubation von patienten in der HNO‐heilkunde]. Anaesthesist 2010;59:806‐11. [DOI] [PubMed] [Google Scholar]
Moon 2013 {published data only}
- Moon HY, Baek CW, Kim JS, Koo GH, Kim JY, Woo YC, et al. The causes of difficult tracheal intubation and preoperative assessments in different age groups. Korean Journal of Anesthesiology 2013;64(4):308‐14. [PUBMED: 23646239 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oriol‐López 2009 {published data only}
- Oriol‐Lopez SA, Hernandez‐Bernal CE. Assessment, prediction and presence of difficult intubation [Valoración, predicción y presencia de intubación difícil]. Revista Mexicana de Anestesiologica 2009;32(1):41‐9. [Google Scholar]
Orozco‐Díaz 2010 {published data only}
- Orozco‐Díaz E, Alvarez‐Ríos JJ, Arceo‐Díaz JL, Ornelas‐Aguirre JM. Predictive factors of difficult airway with known assessment scales. Cirugia y Cirujanos 2010;78(5):393‐9. [PUBMED: 21219809] [PubMed] [Google Scholar]
Reed 2005 {published data only}
- Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department?. Emergency Medicine Journal 2005;22(2):99‐102. [PUBMED: 15662057 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Safavi 2011 {published data only}
- Safavi M, Honarmand A, Zare N. A comparison of the ratio of patient's height to thyromental distance with the modified Mallampati and the upper lip bite test in predicting difficult laryngoscopy. Saudi Journal of Anaesthesia 2011;5(3):258‐63. [PUBMED: 21957403 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siyam 2002 {published data only}
- Siyam MA, Benhamou D. Difficult endotracheal intubation in patients with sleep apnea syndrome. Anesthesia and Analgesia 2002;95(4):1098‐102. [PUBMED: 12351303 ] [DOI] [PubMed] [Google Scholar]
Tripathi 2006 {published data only}
- Tripathi M, Pandey M. Short thyromental distance: a predictor of difficult intubation or an indicator for small blade selection?. Anesthesiology 2006;104(6):1131‐6. [PUBMED: 16732082 ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Akhlaghi 2017 {published data only}
- Akhlaghi M, Abedinzadeh M, Ahmadi A, Heidari Z. Predicting difficult laryngoscopy and intubation with laryngoscopic exam test: a new method. Acta Medica Iranica 2017;55:453‐8. [PubMed] [Google Scholar]
Andrade 2017 {published data only}
- Andrade R, Lima BL, Lopes DK, Couceiro Filho RO, Lima LC, Couceiro TC. Difficult laryngoscopy and tracheal intubation: observational study. Revista Brasileira de Anestesiologia 2017;20:20. [Google Scholar]
Awan 2017 {published data only}
- Awan A, Rehman A. Comparison of neck circumference to thyromental distance ratio with modified Mallampati score for prediction of difficult intubation in obese patients. Acta Anaesthesiologica Scandinavica 2017;61:997. [Google Scholar]
Banik 2017 {published data only}
- Banik D, Ray L, Akhtaruzzaman AK, Bhowmick DK, Hossain MS, Islam MS, et al. Assessment of difficulties associated with endotracheal intubation using modified mallampati and upper lip bite test. Mymensingh Medical Journal: MMJ 2017;26:395‐405. [PubMed] [Google Scholar]
Belda 2017 {published data only}
- Belda I, Ayuso MA, Sala‐Blanch X, Luis M, Berge R. A predictive test for difficult intubation in laryngeal microsurgery. Validation study. Revista Espanola de Anestesiologia y Reanimacion 2017;64:71‐8. [DOI] [PubMed] [Google Scholar]
Card 2017 {published data only}
- Card ME, Rucci J, Honiden S, Heavner J. Identifying factors associated with difficult airway during endotracheal intubation in the medical ICU. Chest 2017;152(4 Suppl 1):A218. [Google Scholar]
Carlson 2017 {published data only}
- Carlson JN, Hostler D, Guyette FX, Pinchalk M, Martin‐Gill C. Derivation and validation of the prehospital difficult airway identification tool (PreDAIT): a predictive model for difficult intubation. The Western Journal of Emergency Medicine 2017;18:662‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dar 2017 {published data only}
- Dar S, Khan MS, Iqbal F, Nazeer T, Hussain R. Comparison of upper lip bite test (ULBT) with mallampati classification, regarding assessment of difficult intubation. Pakistan Journal of Medical and Health Sciences 2017;11:767‐9. [Google Scholar]
Eiamcharoenwit 2017 {published data only}
- Eiamcharoenwit J, Itthisompaiboon N, Limpawattana P, Suwanpratheep A, Siriussawakul A. The performance of neck circumference and other airway assessment tests for the prediction of difficult intubation in obese parturients undergoing cesarean delivery. International Journal of Obstetric Anesthesia 2017;31:45‐50. [DOI] [PubMed] [Google Scholar]
Han 2017 {published data only}
- Han YZ, Tian Y, Xu M, Ni C, Li M, Wang J, et al. Neck circumference to inter‐incisor gap ratio: A new predictor of difficult laryngoscopy in cervical spondylosis patients. BMC Anesthesiology 2017;17(1):1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanouz 2018 {published data only}
- Hanouz JL, Bonnet V, Buleon C, Simonet T, Radenac D, Zamparini G, et al. Comparison of the mallampati classification in sitting and supine position to predict difficult tracheal intubation: a prospective observational cohort study. Anesthesia and Analgesia 2018;126:161‐9. [DOI] [PubMed] [Google Scholar]
Jain 2017 {published data only}
- Jain N, Das S, Kanchi M. Thyromental height test for prediction of difficult laryngoscopy in patients undergoing coronary artery bypass graft surgical procedure. Annals of Cardiac Anaesthesia 2017;20:207‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khatiwada 2017 {published data only}
- Khatiwada S, Bhattarai B, Pokharel K, Acharya R. Prediction of difficult airway among patients requiring endotracheal intubation in a tertiary care hospital in eastern Nepal. JNMA; Journal of the Nepal Medical Association 2017;56(207):314‐8. [PubMed] [Google Scholar]
Lee 2017 {published data only}
- Lee SY, Chien DK, Huang MY, Huang CH, Shih SC, Wu KM, et al. Patient‐specific factors associated with difficult mask ventilation in the emergency department. International Journal of Gerontology 2017;11:263‐6. [Google Scholar]
Mahmoodpoor 2017 {published data only}
- Mahmoodpoor A, Soleimanpour H, Golzari SE, Nejabatian A, Pourlak T, Amani M, et al. Determination of the diagnostic value of the modified mallampati score, upper lip bite test and facial angle in predicting difficult intubation: a prospective descriptive study. Journal of Clinical Anesthesia 2017;37:99‐102. [DOI] [PubMed] [Google Scholar]
Norskov 2017 {published data only}
- Norskov AK, Wetterslev J, Rosenstock CV, Afshari A, Astrup G, Jakobsen JC, et al. Prediction of difficult mask ventilation using a systematic assessment of risk factors vs. existing practice ‐ a cluster randomised clinical trial in 94,006 patients. Anaesthesia 2017; Vol. 72, issue 3:296‐308. [DOI] [PubMed]
Prakash 2017 {published data only}
- Prakash S, Mullick P, Bhandari S, Kumar A, Gogia AR, Singh R. Sternomental distance and sternomental displacement as predictors of difficult laryngoscopy and intubation in adult patients. Saudi Journal of Anaesthesia 2017;11:273‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rao 2017 {published data only}
- Rao CS, Ranganath T, Rao SP, Sujani K. Comparison of upper lip bite test with modified mallampati test and thyromental distance for predicting difficulty in endotracheal intubation ‐ a prospective study. Journal of Evolution of Medical and Dental Sciences 2017;6:1413‐6. [Google Scholar]
Riad 2018 {published data only}
- Riad W, Ansari T, Shetty N. Does neck circumference help to predict difficult intubation in obstetric patients? A prospective observational study. Saudi Journal of Anaesthesia 2018;12:77‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Selvi 2017 {published data only}
Shankar 2017 {published data only}
- Shankar D, Suresh YV. Comparison of various airway assessment factors with ratio of height to thyromental distance (rhtmd) in predicting difficult airway in apparently normal patients. Journal of Evolution of Medical and Dental Sciences 2017;6:902‐7. [Google Scholar]
Siljeblad 2017 {published data only}
- Siljeblad M, Lofgren B, Snygg J, Nellgard P. A comparison of predictive factors for identifying difficult airway (laryngoscopy & intubation) patients. Acta Anaesthesiologica Scandinavica 2017;61(8):1036‐7. [Google Scholar]
Srivilaithon 2018 {published data only}
- Srivilaithon W, Muengtaweepongsa S, Sittichanbuncha Y, Patumanond J. Predicting difficult intubation in emergency department by intubation assessment score. Journal of Clinical Medicine Research 2018;10:247‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Torres 2017 {published data only}
- Torres K, Blonski M, Pietrzyk L, Piasecka‐Twarog M, Maciejewski R, Torres A. Usefulness and diagnostic value of the NEMA parameter combined with other selected bedside tests for prediction of difficult intubation. Journal of Clinical Anesthesia 2017;37:132‐5. [DOI] [PubMed] [Google Scholar]
Wang 2017 {published data only}
- Wang B, Yao W D, Peng H, Guo L, Jin X J. Interincisor distance predicting difficulty airway in men and women. Anesthesia and Analgesia 2017;124:23‐4. [Google Scholar]
Workeneh 2017 {published data only}
- Workeneh SA, Gebregzi AH, Denu ZA. Magnitude and predisposing factors of difficult airway during induction of general anaesthesia. Anesthesiology Research and Practice 2017;2017:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildirim 2017 {published data only}
- Yildirim I, Inal MT, Memis D, Turan FN. Determining the efficiency of different preoperative difficult intubation tests on patients undergoing caesarean section. Balkan Medical Journal 2017;34:436‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Adnet 1997
- Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997;87(6):1290‐7. [PUBMED: 9416711] [DOI] [PubMed] [Google Scholar]
ASA 2003
- American Society of Anesthesiologists. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2003;98(5):1269‐77. [PUBMED: 12717151] [DOI] [PubMed] [Google Scholar]
ASA 2013
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013;118(2):251‐70. [PUBMED: 23364566] [DOI] [PubMed] [Google Scholar]
Begg 2005
- Begg CB. Systematic reviews of diagnostic accuracy studies require study by study examination: first for heterogeneity, and then for sources of heterogeneity. Journal of Clinical Epidemiology 2005;58(9):865‐6. [PUBMED: 16085189] [DOI] [PubMed] [Google Scholar]
Berkow 2009
- Berkow LC, Greenberg RS, Kan KH, Colantuoni E, Mark LJ, Flint PW, et al. Need for emergency surgical airway reduced by a comprehensive difficult airway program. Anesthesia and Analgesia 2009;109(6):1860‐9. [PUBMED: 19713264] [DOI] [PubMed] [Google Scholar]
Calder 2003
- Calder I, Picard J, Chapman M, O'Sullivan C, Crockard HA. Mouth opening: a new angle. Anesthesiology 2003;99(4):799‐801. [PUBMED: 14508309] [DOI] [PubMed] [Google Scholar]
Chu 2006
- Chu H, Cole SR. Bivariate meta‐analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. Journal of Clinical Epidemiology 2006;59(2):1331‐2. [DOI] [PubMed] [Google Scholar]
Combes 2006
- Combes X, Jabre P, Jbeili C, Leroux B, Bastuji‐Garin S, Margenet A, et al. Prehospital standardization of medical airway management: incidence and risk factors of difficult airway. Academic Emergency Medicine 2006;13(8):828‐34. [PUBMED: 16807397] [DOI] [PubMed] [Google Scholar]
Cook 2000
- Cook TM. A new practical classification of laryngeal view. Anaesthesia 2000;55(3):274‐9. [PUBMED: 10671848] [DOI] [PubMed] [Google Scholar]
Cormack 1984
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39(11):1105‐11. [PUBMED: 6507827] [PubMed] [Google Scholar]
DA Society 2015
- Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. British Journal of Anaesthesia 2015;115(6):827‐48. [PUBMED: 26556848] [DOI] [PMC free article] [PubMed] [Google Scholar]
El‐Orbany 2009
- El‐Orbany M, Woehlck HJ. Difficult mask ventilation. Anesthesia and Analgesia 2009;109(6):1870‐80. [PUBMED: 19923516] [DOI] [PubMed] [Google Scholar]
Karkouti 1996
- Karkouti K, Rose DK, Ferris LE, Wigglesworth DF, Meisami‐Fard T, Lee H. Inter‐observer reliability of ten tests used for predicting difficult tracheal intubation. Canadian Journal of Anaesthesia 1996;43(6):554‐9. [PUBMED: 8773859] [DOI] [PubMed] [Google Scholar]
Lee 2006
- Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta‐analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesthesia and Analgesia 2006;102(6):1867‐78. [PUBMED: 16717341] [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6(6):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luba 2010
- Luba K, Cutter TW. Supraglottic airway devices in the ambulatory setting. Anesthesiology Clinics 2010;28:295‐314. [PUBMED: 20488396 ] [DOI] [PubMed] [Google Scholar]
Lundstrom 2011
- Lundstrøm LH, Vester‐Andersen M, Møller AM, Charuluxananan S, L'hermite J, Wetterslev J, et al. Poor prognostic value of the modified Mallampati score: a meta‐analysis involving 177 088 patients. British Journal of Anaesthesia 2011;107(5):659‐67. [PUBMED: 21948956] [DOI] [PubMed] [Google Scholar]
Mallampati 1985
- Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Canadian Anaesthetists' Society Journal 1985;32(4):429‐34. [PUBMED: 4027773] [DOI] [PubMed] [Google Scholar]
Partlett 2016
- Partlett C, Takwoingi Y. Meta‐analysis of test accuracy studies in R: a summary of user‐written programs and step‐by‐step guide to using glmer. Version 1.0. www.methods.cochrane.org/sdt/ (accessed 2 August 2016).
Peterson 2005
- Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology 2005;103(1):33‐9. [PUBMED: 15983454] [DOI] [PubMed] [Google Scholar]
Pott 2008
- Pott LM, Murray WB. Review of video laryngoscopy and rigid fiberoptic laryngoscopy. Current Opinion in Anaesthesiology 2008;21(6):750‐8. [PUBMED: 18997526] [DOI] [PubMed] [Google Scholar]
R 2017 [Computer program]
- R Foundation for Statistical Computing. R: A language and environment for statistical computing. Version 3.4.2. Vienna, Austria: R Foundation for Statistical Computing, 2017.
Ramadhani 1996
- Ramadhani SAL, Mohamed LA, Rocke DA, Gouws E. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. British Journal of Anaesthesia 1996;77(3):312‐6. [PUBMED: 8949801] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rose 1996
- Rose DK, Cohen MM. The incidence of airway problems depends on the definition used. Canadian Journal of Anaesthesia 1996;43(1):30‐4. [PUBMED: 8665631] [DOI] [PubMed] [Google Scholar]
Samsoon 1987
- Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia 1987;42(5):487‐90. [PUBMED: 3592174] [DOI] [PubMed] [Google Scholar]
Shiga 2005
- Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta‐analysis of bedside screening test performance. Anesthesiology 2005;103(2):429‐37. [PUBMED: 16052126] [DOI] [PubMed] [Google Scholar]
Stata 2015 [Computer program]
- StataCorp. Stata. Version 14. College Station, TX, USA: StataCorp, 2015.
Whiting 2003
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Medical Research Methodology 2003;3:25. [PUBMED: 14606960] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS‐2 Group. QUADAS‐2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529‐36. [PUBMED: 22007046] [DOI] [PubMed] [Google Scholar]
Yentis 1998
- Yentis SM, Lee DJ. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia 1998;53(11):1041‐4. [PUBMED: 10023271] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Lee 2010
- Lee A, Herkner H, Hovhannisyan K, Pace NL. Airway physical examination tests for detection of difficult airway management in apparently normal patients. Cochrane Database of Systematic Reviews 2010, Issue 12. [DOI: 10.1002/14651858.CD008874] [DOI] [PMC free article] [PubMed] [Google Scholar]
Roth 2019
- Roth D, Pace NL, Lee A, Hovhannisyan K, Warenits AM, Arrich J, et al. Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia 2019;epub. [DOI: 10.1111/anae.14608] [DOI] [PubMed] [Google Scholar]


