Short abstract
Background
Emergency Department imaging volume has increased significantly in North America and Asia.
Purpose
To assess Emergency Department imaging trends in a European center.
Material and Methods
The institutional radiological information system was queried for all computed tomography (CT), ultrasound (US), and magnetic resonance (MR) studies performed for the Emergency Department during 2002–2017. Descriptive statistics and linear regression analyses were used to assess overall study rates and temporal trends in overall and after-hours imaging after adjusting for patient visitations.
Results
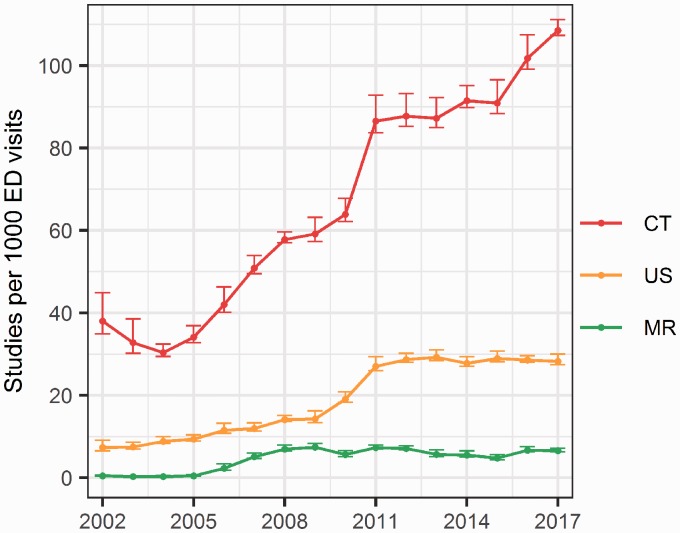
CT use increased significantly from 38/1000 visits to 108/1000 at the end of the observation by 5.5 new exams per 1000 visits/year (P < 0.0001). US use increased gradually at a rate of 1.2/1000 per year during 2002–2008 with an accelerated annual increase of 6.4/1000 in 2009–2011 (P < 0.0001) raising US rates from 7/1000 to 28/1000 visits per year with stable rates from 2012 onwards. After on-site MR became available in 2004, its use increased from 0.3/1000 to 7/1000 at a rate of 1.9/1000 visits per year in 2005–2009 (P < 0.0001) and remained stable from 2010. While there was a significant increase in after-hours imaging, growth remained proportional to the overall trend in the use of CT, MR, and night-time CT with the exception of a slight decrease in after-hour US in favor of standard working hours (P < 0.0001).
Conclusion
All modalities increased significantly in volume adjusted usage. US and MR rates have been stable since 2012 and 2010, respectively, after periods of increase while CT use continues to increase. Demand for after-hours imaging was mostly proportional to the overall trend.
Keywords: Emergency medicine, emergency radiology, imaging utilization, imaging volume, health resources
Introduction
Diagnostic imaging has an integral role in the evaluation of patients in the Emergency Department (ED) and its utilization has increased significantly in the last two decades. This trend of increased imaging is seen in North America and Asia, across adult and pediatric patient populations, on the institutional level as well as in larger national samples (1–9). The majority of the current literature originates from the United States while the European experience remains largely unknown. Only a couple of reports on CT usage among pediatric and young adult populations have been published from Europe and none on multi-modality diagnostic trends among the general ED population (1,10).
The purpose of the study was to explore imaging trends for an emergency department in an academic medical center over an extensive period by assessing changes in volume of cross-sectional radiological examinations: computed tomography (CT); magnetic resonance imaging (MRI); and ultrasound (US). We hypothesized that CT examinations had progressively increased from the early 2000s with a proportionally smaller role for US and furthermore speculated that demand for on-call imaging had increased beyond that of daytime imaging.
Material and Methods
The study was performed in a 669-bed university affiliated medical center with 70,000 ED patient visits per year. The ED was at the end of the study period served by two CT scanners, two MRI scanners, and an US lab. CT and US were available throughout the study while on-site MRI became available in December 2004. The number of CT and MR scanners increased from one to two in 2016 and 2017, respectively.
In this retrospective observational study, the institutional radiology information system (RIS) was used to retrieve information on all CT, US, and MR studies from the ED from 1 January 2002 to 31 December 2017, constituting 16 complete calendar years. Image-guided interventions were included under their respective modality due to the relatively few numbers. Cancelled studies and non-radiologist-performed US studies, such as cardiologist-performed echocardiography, were not included. Only unique accession numbers (study identifier) were considered. Compound studies such as non-contrast CT of the head and CT of the cervical spine performed in the same instance were considered as a single study when pertaining to a single accession number. Basic demographic information was extracted from the RIS as well as time and date of study acquisition.
Studies performed between 16:00 and 08:00 on weekdays and all studies on public holidays and weekends until 08:00 on the following Monday were considered after-hours studies. This included a subcategory of night-time studies which included all studies between 00:00 and 08:00. Ratios of after-hour imaging were compared to overall imaging of the respective modality to assess for changes in proportionality of workloads.
Information on the number of ED visits and admissions was obtained from publicly available hospital statistics. The numbers of admissions, available since 2006, were used to calculate admission rates as a departmental metric and a surrogate marker of patient severity. Total numbers of imaging studies were assessed for each modality as well as volume adjusted rates per 1000 patient visits to the ED per year/month. CT studies were stratified by patient age at acquisition into categories: 0–12, 13–17, 18–29, 30–44, 45–59 with an open ended 60+ category. Linear regression analysis was used to assess for temporal trends in the number of ED visits and imaging studies. Information on general population numbers was obtained from the state Statistics Iceland. The institutional radiologist workforce was assessed by calculating annual averages of quarterly data for full-time equivalent radiologists, available from 2007. The study was exempt from Institutional Review Board approval as it did not involve an intervention, patient contact or personally identifiable information. All statistical analysis was performed in R (CRAN) (11).
Results
During 1,003,263 patient visits to the ED in the 16-year observation, a total of 69,975 CT, 20,092 US, and 4782 MR examinations were performed. Patient visits to the ED increased from 49,111 to 72,665 per year, increasing on average by 1788 visits annually over the study period (P < 0.0001). ED visits increased over the study period by 48% while the general population increased by 18%. By age group, the increase in the general population was 14% in patients aged 18–29 years, 9% in patients aged 30–44 years, 28% in patients aged 45–59 years, and 53% in patients aged 60+ years (Suppl. Fig. 1). Table 1 shows total annual numbers and volume-adjusted rates of examinations for each modality as well as admission rates and the number of employed full-time equivalent radiologists.
Table 1.
Overview of total and volume adjusted examinations for each modality and patient visits to the ED.
| Year | Total CT | CT/1000 visits | Total US | US/1000 visits | Total MR | MR/1000 visits | Visits | Admissions | Admission rate (%) | Full-time equivalent radiologists |
|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 7879 | 108 | 2045 | 28 | 475 | 7 | 72,665 | 8522 | 11.7 | 19.7 |
| 2016 | 7343 | 102 | 2060 | 28 | 483 | 7 | 72,300 | 8041 | 11.1 | 18.9 |
| 2015 | 6522 | 91 | 2072 | 29 | 339 | 5 | 71,695 | 8300 | 11.6 | 17.7 |
| 2014 | 6420 | 91 | 1941 | 28 | 384 | 5 | 70,230 | 8441 | 12 | 15.2 |
| 2013 | 6094 | 87 | 2042 | 29 | 393 | 6 | 69,815 | 8143 | 11.7 | 15.3 |
| 2012 | 6366 | 88 | 2079 | 29 | 513 | 7 | 72,704 | 8436 | 11.6 | 15.6 |
| 2011 | 6221 | 87 | 1944 | 27 | 522 | 7 | 71,504 | 8332 | 11.7 | 16.4 |
| 2010 | 4155 | 64 | 1252 | 19 | 362 | 6 | 65,166 | 5937 | 9.1 | 17.2 |
| 2009 | 3436 | 59 | 825 | 14 | 430 | 7 | 58,282 | 5821 | 10.0 | 17.9 |
| 2008 | 3511 | 58 | 855 | 14 | 421 | 7 | 60,721 | 5205 | 8.6 | 18.8 |
| 2007 | 3056 | 51 | 717 | 12 | 304 | 5 | 60,139 | 5504 | 9.2 | 18.6 |
| 2006 | 2250 | 38 | 618 | 10 | 123 | 2 | 59,328 | 6294 | 10.6 | |
| 2005 | 1758 | 34 | 482 | 9 | 13 | 0.3 | 51,740 | |||
| 2004 | 1495 | 30 | 436 | 9 | 5 | 0.1 | 49,150 | |||
| 2003 | 1587 | 33 | 361 | 7 | 6 | 0.1 | 48,713 | |||
| 2002 | 1882 | 38 | 363 | 7 | 9 | 0.2 | 49,111 |
On-site MRI became available in late 2004. Admission data are available from 2006 onward. Data on radiologist workforce are available from 2007.
The annual overall increase in CT was 5.5 new examinations per 1000 visitations (P < 0.0001) which brought CT rates from 38/1000 visits to 108/1000 by the end of the study period (Figure 1). US examinations increased from 7/1000 visits to 28/1000 at an annual overall increase of 1.8 new exams per 1000 visits (P < 0.0001). The increase in US was found to be unevenly paced with a relatively gradual increase during 2002–2008 at a rate of 1.2 exams per 1000 visits (β = 0.10, P < 0.0001), followed by an accelerated increase during 2009–2011 at an annual rate of 6.4 exams per 1000 visits (β = 0.53, P < 0.0001) and finally stable rates in 2012–2017 (β = –0.0048, P = 0.735). On-site MR became available in late 2004 and showed a relatively rapid increase in 2005–2009 at the rate of 1.9 new examinations per year per 1000 visits (β = 0.16, P < 0.0001) which brought MR rates to 7/1000 from where they remained stable in 2010–2017 (β = –0.0045, P = 0.432). MR examinations had an annual overall increase of 0.46 examinations per 1000 visits (P < 0.0001) when assessed for the entire study period. Whereas both US and MR showed later stability, CT continued to increase when assessed similarly for the latter period of the observation (β = 0.35, P < 0.0001 for 2012–2017).
Volume-adjusted rates of CT examinations by age group were disproportionate among the adult patients with a greater increase for each successive age group (Fig. 2). Similar differences in increase among adults age groups were observed for US and MR but with less distinction (Suppl. Figs. 2 and 3).
Fig. 2.
Volume-adjusted CT imaging utilization by patient age groups. Annual averages of monthly data are depicted with 95% confidence intervals.
Fig. 1.
Volume-adjusted imaging utilization by modality. Annual averages of monthly data are depicted with 95% confidence intervals.
After-hour imaging increased significantly for all imaging modalities but did not exceed daytime demand. The ratio of after-hours CT compared to overall CT imaging had a range of 0.66–0.72 (median = 0.69) and did not change significantly throughout study period (β = –0.0003, P = 0.780). The proportion of the subset night-time CT had a range of 0.08–0.11 (median = 0.09) and remained stable as well (β = 0.0006, P = 0.231). The same was true for after-hours MR which had a range of 0.0–0.4 (median = 0.30) and did not change significantly (β = 0.002, P = 0.720). After-hours US examinations, however, decreased in proportion to total examinations from 0.6 to 0.5 (range = 0.49–0.61, median = 0.51) (β = –0.006, P < 0.001).
Discussion
The ED is a major consumer of medical imaging which makes awareness of its trends in medical imaging important. In this study, we show a large and continuous increase in CT scans performed for the ED. Similar trends have been seen from the United States and Asia but have not been previously reported in Europe. We are only aware of two European studies limited to CT in pediatric and young adult population, one of which is from the early multislice CT era (1,10). The majority of the current literature on this topic originates from North America from Medicare or survey data as well as single-institution studies and the general trend is of large increases in ED CT imaging across indications and patient populations (3,6,8,12,13). Interestingly, Raja et al. observed, in a single-center setting, a steady increase in CT examinations up to 2007 with a subsequent decrease toward the end of their study period in 2012, an effect the authors suggest may be caused by increase in cost and ionizing radiation awareness as well as institutional quality initiatives (9). While observing stability in US and MR examinations from 2012 and 2010, respectively, we continue to see an increase in CT rates at our institution.
The reason for the dramatic increase in CT is likely manifold. One is undoubtedly changing indications with an expanded role for CT, for instance replacing intravenous pyelography for renal colic as demonstrated by Rosenkrantz et al. with an ED cohort (4). Nuclear medicine has likewise, in a large part, been replaced by CT pulmonary angiography for the evaluation of suspected pulmonary embolism, shown by early national US data by Stein et al. (14). CT angiography for systemic vascular imaging has also been validated for various clinical uses and has seen an expanded role leading to dramatic decreases in the use of conventional diagnostic catheter angiography (15–18).
CT is an important diagnostic tool for the ED owing to speed, availability, and accuracy. CT results in the ED have been shown to change lead diagnosis in a significant number of cases as well as increase diagnostic confidence and alleviate diagnostic uncertainty for an array of indications (19). The effect of the observed increase in diagnostic imaging on eventual patient outcomes is, however, largely unknown. One study showed a significant decrease in negative appendectomy rates and decrease in appendiceal surgical rates after a practice shift towards preoperative CT, importantly at the expense of a large increase in abdominal scans (20). Increases in imaging have also evoked serious concerns for increases in cost and ionizing radiation exposure as well as increases in incidental imaging findings leading to still more imaging (21).
Of the modalities studied, the largest volume and the largest increase was in CT examinations, deserving special attention. A stratified increase for each successive age group was observed in CT examinations in keeping with previous studies with the largest volume and largest increase being in older patients, defined as those aged > 60 years (2,6,8). This increase in scans coincided with demographic changes during the study period where the population of the 60+ age group increased by 53% whereas the younger age groups grew by much lower percentages (Suppl. Fig. 1). This demographic shift, known as population aging, is seen throughout the developed world and is particularly advanced in Europe. We believe this may have been a significant factor in the observed increase in CT examinations and its contribution to increases in diagnostic imaging is an interesting area for further research.
The stable numbers of US examinations from 2012 onwards after periods of increase may be somewhat expected considering the increase in CT as well as ED-physician US examinations, which are thought to have increased in our institution. Although a subjective observation not verified by this study, ED-physician US examinations have been shown to have increased substantially in the United States Medicare population (22). Radiologist-performed US studies in the ED have also shown to have increased in the United States as well (9,22). MRI study rates showed similar trends as US with an early increase and subsequent plateauing. This might be somewhat skewed by the fact that on-site MR was not available for our ED until late 2004 but was previously available at a nearby campus. MRI was by far the least-ordered examination in keeping with previous studies and showed a similar trend of later stability as demonstrated in a couple of single-center studies but in contrast with US Medicare data which show a progressive increase (2,3,9). This may reflect a more limited access to MR compared to CT and US; the general diagnostic task of MR may also be less suited for the ED patient population.
There is a general perception of increasing demand for diagnostic imaging in quantity as well as of increased complexity outside standard working hours. This has led some institutions to enter teleradiology agreements with offshore radiology groups, often residing in a favorable time-belt to the respective institution (23). Others have implemented 24-h attending coverage (24). Despite this, there is limited published data on increases specific to after-hours imaging. One such study showed significant increases in absolute and volume-adjusted numbers of radiological studies across modalities and specialties consistently throughout three Canadian academic centers (25). We also show increases in after-hours CT studies, as well as in the subset night-time CT, but these have remained in proportion to the overall increase in CT. The same observation was seen with after-hours MR. A slight decrease, however, was noted in the proportion of after-hours US with a gradually decreasing proportion of US studies being performed on-call. In many centers, including our own, the on-call duties are very much dominated by ED studies and a large proportion of the total examinations are performed after hours. In our experience, the majority of ED CT studies are performed on-call (70%) and have been consistent throughout. This may be due to the nature and workflow of the ED, leading to considerable after-hours imaging volumes and makes for an interesting metric for workloads.
Our study is limited by the single-center setting making it vulnerable to unique institutional practices. This contrasts with larger national studies from the US which are, however, importantly, based on aggregated Medicare claims data, which cover only a fraction of the population, or sample survey data, which include only certain centers. The strengths of our study include a complete dataset over an extensive study period and importantly having accurate volume information for adjusting study rates according to changes in ED visitations as they have changed substantially in our practice. Our ED is the largest in the country, serving two-thirds of the national population with no competing ED and furthermore serves as an entryway to the only tertiary-care medical center for the remaining population. We believe this limits bias associated with healthcare restructuring. Another important limitation is that by considering studies by unique accession numbers, we were unable to account for study bundling, e.g. non-contrast CT head and CT cervical spine performed in the same instance, as well as equating all examinations and thus not being able to observe changes in study complexity or extent over time. This method, on the other hand, removed biases associated with changes in coding practices. Approaching the subject on the modality level, we were further unable to observe trends relating to specific examinations, clinical indications, or assess for study appropriateness.
In conclusion, we report large increases in ED diagnostic imaging over a 16-year period. The largest volume and greatest increase were in CT imaging, which shows increasing disparities among patient age groups. We note demographic shifts in our general population which may have contributed to increasing imaging utilization. We show that increasing workloads have increased in the daytime and for on-call duties at an equal rate for all modalities except for US, contrary to our initial hypothesis. Moreover, we confirm our suspicion that demand for radiologist-performed US has plateaued while cross-sectional imaging demand continues to increase. The observed changes in imaging practices are mostly in line with previous reports from North America and Asia.
Supplemental Material
Supplemental material, Supplemental Material1 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open
Supplemental Material
Supplemental material, Supplemental Material2 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open
Supplemental Material
Supplemental material, Supplemental Material3 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open
Acknowledgement
The authors thank Jon Trausti Bragason for his help with data acquisition.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
References
- 1.Bosch de Basea M, Salotti JA, Pearce MS, et al. Trends and patterns in the use of computed tomography in children and young adults in Catalonia - results from the EPI-CT study. Pediatr Radiol 2016; 46:119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahn S, Kim WY, Lim KS, et al. Advanced radiology utilization in a tertiary care emergency department from 2001 to 2010. PLoS One 2014; 9:e112650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levin DC, Rao VM, Parker L, et al. Continued growth in emergency department imaging is bucking the overall trends. J Am Coll Radiol 2014; 11:1044–1047. [DOI] [PubMed] [Google Scholar]
- 4.Rosenkrantz AB, Hanna TN, Babb JS, et al. Changes in emergency department imaging: perspectives from national patient surveys over two decades. J Am Coll Radiol 2017; 14:1282–1290. [DOI] [PubMed] [Google Scholar]
- 5.Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department, 2000–2006. Emerg Radiol 2007; 14:227–232. [DOI] [PubMed] [Google Scholar]
- 6.Larson DB, Johnson LW, Schnell BM, et al. National trends in CT use in the emergency department: 1995–2007. Radiology 2011; 258:164–173. [DOI] [PubMed] [Google Scholar]
- 7.Broder J, Warshauer DM. Increasing utilization of computed tomography in the adult emergency department, 2000–2005. Emerg Radiol 2006; 13:25–30. [DOI] [PubMed] [Google Scholar]
- 8.Kocher KE, Meurer WJ, Fazel R, et al. National trends in use of computed tomography in the emergency department. Ann Emerg Med 2011; 58:452–462. [DOI] [PubMed] [Google Scholar]
- 9.Raja AS, Ip IK, Sodickson AD, et al. Radiology utilization in the emergency department: trends of the past 2 decades. AJR Am J Roentgenol 2014; 203:355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearce MS, Salotti JA, Howe NL, et al. CT scans in young people in Great Britain: temporal and descriptive patterns, 1993–2002. Radiol Res Pract 2012; 2012:594278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing, 2018. [Google Scholar]
- 12.Berdahl CT, Vermeulen MJ, Larson DB, et al. Emergency department computed tomography utilization in the United States and Canada. Ann Emerg Med 2013; 62:486–494. [DOI] [PubMed] [Google Scholar]
- 13.Hryhorczuk AL, Mannix RC, Taylor GA. Pediatric abdominal pain: use of imaging in the emergency department in the United States from 1999 to 2007. Radiology 2012; 263:778–785. [DOI] [PubMed] [Google Scholar]
- 14.Stein PD, Kayali F, Olson RE. Trends in the use of diagnostic imaging in patients hospitalized with acute pulmonary embolism. Am J Cardiol 2004; 93:1316–1317. [DOI] [PubMed] [Google Scholar]
- 15.Heijenbrok-Kal MH, Kock MCJM, Hunink MGM. Lower extremity arterial disease: multidetector CT angiography meta-analysis. Radiology 2007; 245:433–439. [DOI] [PubMed] [Google Scholar]
- 16.Romano M, Mainenti PP, Imbriaco M, et al. Multidetector row CT angiography of the abdominal aorta and lower extremities in patients with peripheral arterial occlusive disease: diagnostic accuracy and interobserver agreement. Eur J Radiol 2004; 50:303–308. [DOI] [PubMed] [Google Scholar]
- 17.Bartlett ES, Walters TD, Symons SP, et al. Quantification of carotid stenosis on CT angiography. AJNR Am J Neuroradiol 2006; 27:13–19. [PMC free article] [PubMed] [Google Scholar]
- 18.Cowell GW, Reid AW, Roditi GH. Changing trends in a decade of vascular radiology-the impact of technical developments of non-invasive techniques on vascular imaging. Insights Imaging 2012; 3:495–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pandharipande PV, Reisner AT, Binder WD, et al. CT in the Emergency Department: a real-time study of changes in physician decision making. Radiology 2016; 278:812–821. [DOI] [PubMed] [Google Scholar]
- 20.Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology 2010; 256:460–465. [DOI] [PubMed] [Google Scholar]
- 21.Hendee WR, Becker GJ, Borgstede JP, et al. Addressing overutilization in medical imaging. Radiology 2010; 257:240–245. [DOI] [PubMed] [Google Scholar]
- 22.Rosenkrantz AB, Bilal NH, Hughes DR, et al. National specialty trends in billable diagnostic ultrasound in the ED: analysis of Medicare claims data. Am J Emerg Med 2014; 32:1470–1475. [DOI] [PubMed] [Google Scholar]
- 23.Steinbrook R. The age of teleradiology. N Engl J Med 2007; 357:5–7. [DOI] [PubMed] [Google Scholar]
- 24.Coleman S, Holalkere NS, O’Malley J, et al. Radiology 24/7 in-house attending coverage: do benefits outweigh cost? Curr Probl Diagn Radiol 2016; 45:241–246. [DOI] [PubMed] [Google Scholar]
- 25.Chaudhry S, Dhalla I, Lebovic G, et al. Increase in utilization of afterhours medical imaging: a study of three Canadian academic centers. Can Assoc Radiol J 2015; 66:302–309. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental Material1 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open
Supplemental material, Supplemental Material2 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open
Supplemental material, Supplemental Material3 for Diagnostic imaging trends in the emergency department: an extensive single-center experience by Gunnar Juliusson, Birna Thorvaldsdottir, Jon Magnus Kristjansson and Petur Hannesson in Acta Radiologica Open