Abstract
Purpose
To describe a case of Waldenström's macroglobulinemia/lymphoplasmacytic lymphoma with infiltration of both lacrimal glands.
Observations
A 63-year-old male with Waldenström's macroglobulinemia was referred to the ophthalmological clinic due to intermittent bilateral painless swollen eyelids. The patient had slight bilateral chemosis along with swelling of both eyelids. A mechanical ptosis was present on both sides. Funduscopic examination and tonometry were normal. Computed tomography and positron emission tomography showed an enlargement of both lacrimal glands with positive PET signal, and hence a biopsy was performed for histological and cytogenetic examination. Histopathological examination revealed an infiltrate of lymphoplasmacytic cells and small lymphocytes within the lacrimal gland. The tumor cells stained positive for IgM and CD20, CD79, BCL-2, and kappa light chain. A cytogenetic examination revealed a mutation in MYD88 confirming Morbus Waldenström/lymphoplasmacytic lymphoma.
Conclusions and importance
Intermittent swollen lacrimal glands are a rather common symptom, and Morbus Waldenström/lymphoplasmacytic lymphoma should be considered as a differential diagnosis. This symptom should be carefully evaluated in Waldenström patients, as it can be a sign of disease progression in case of lacrimal gland involvement.
Keywords: Lymphoplasmacytic lymphoma, Lymphoma, Waldenström macroglobulinaemia, Bilateral, Lacrimal gland
1. Introduction
Bilateral swelling of the lacrimal glands is a rather common symptom, usually associated with inflammatory diseases, such as dacryoadenitis, idiopathic orbital inflammation (IOI), and sarcoidosis, or due to structural changes of the lacrimal gland. Bilateral lacrimal gland lymphoma is extremely rare and only few patients present with bilateral swelling as the initial symptom.1 Waldenström's macroglobulinemia (WM) is defined as systemic lymphoplasmacytic lymphoma (LPL) with elevated serum IgM-levels (>3 g/dL).1 WM/LPL is a rare non-Hodgkin lymphoma of the B-cell lineage that constitutes 1.5% of all nodal lymphomas.2,3 The median age at the time of WM/LPL diagnosis is 63 years, and a slight male predominance is observed (53%).2,3 Bone marrow, lymph nodes, and the spleen are the most commonly affected anatomic locations, while peripheral blood and extra-nodal infiltrates may also be seen.2 Histologically, WM/LPL presents a diffuse pattern consisting of small lymphocytes, plasmacytoid cells, and plasma cells.2 In most cases, a genetic alteration in the MYD88 gene is found.2,4 The median survival is 5 years and about 20% of patients survive >10 years.2
Lymphomas located in the lacrimal gland are rare and represent up to 26% of ocular adnexal lymphomas.1 However, 37% of malignant tumors in the lacrimal gland are lymphomas.5,6
Lacrimal gland WM/LPL is exceedingly rare and the first case was described in 1969 by Little et al.7 Since then, an additional four cases have been reported.8, 9, 10, 11, 12
We present an unusual case of WM infiltration of both lacrimal glands following a clinical history of fluctuating swollen eyelids for almost 4 years. This case demonstrates that WM/LPL should be considered in case of bilateral swelling of the lacrimal glands, where no obvious other cause is found. Waldenström macroglubolinemia patients often attend routine ophthalmological examinations, and this case highlights that intermittent swelling of the eyelids should be evaluated further in these patients, as this can be a sign of disease progression.
2. Case report
2.1. Clinical course
A 63-year-old man was referred to the oculoplastic unit after complaining of discomfort from swollen eyelids on both sides. The patient was known with clinical stable WM following treatment with chemotherapy with dexamethasone, rituximab, and cyclophosphamide (DRC). At the time of WM diagnosis, IgM serum level was 29.4 g/L (normal: 0.5–3 g/L). At this time, an ophthalmological examination was performed routinely to evaluate the fundus for hyperviscosity retinopathy. Slit-lamp examination was normal and ophthalmoscopy indicated no signs of vessel abnormality or bleeding. A bilateral periorbital swelling was noted, but neither scanning nor biopsy of the lacrimal glands were performed at this time. The patient later reported that this swelling may have decreased following the chemotherapy.
Three years and ten months after the initial diagnosis, the patient complained of discomfort from the swollen eyelids. The patient reported intermittent change in the size of his eyelids over the last approximately four years, as well as vague neuropathy in both hands and feet. At this time, serum IgM level was 12.1 g/L.
An ophthalmological examination revealed the right lacrimal gland measuring 2 × 2.5 cm and the left measuring 1.5 × 1 cm by digital palpation (Fig. 1). Additionally, mechanical ptosis and slight chemosis was observed. Visual acuity (VA) was 0.6 in the right eye and 0.9 in the left eye, which was habitual. Slit-lamp examination including ophthalmoscopy was normal. Tonometry showed that the intraocular pressure was within normal range in both eyes.
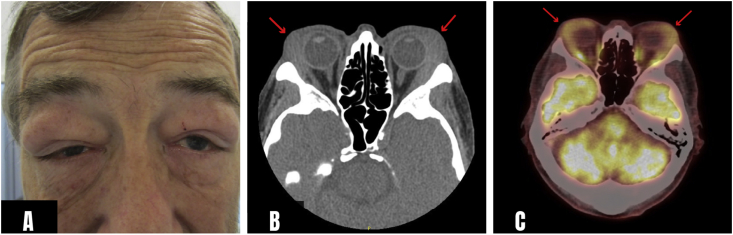
Fig. 1.
(a) A 63-year-old male known with Waldenström's macroglobulinemia presented with temporal mechanical ptosis of both upper eyelids. The symptoms had been fluctuating the last 46 months before the patient consulted his ophthalmologist. (b) Computerized tomography demonstrated bilateral enlarged lacrimal glands measuring 2 × 2.5 cm on the right side and 1 × 1.5 cm on the left side (green arrows). (c) Positron emission tomography showing positive signal in both lacrimal gland tumors.
Computed tomography (CT) and positron emission tomography (PET) was performed and showed enlarged bilateral lacrimal glands with positive PET signal (Fig. 1). A biopsy of the right lacrimal gland was performed for histological examination.
The patient was treated with local radiotherapy applying 24 Gy in 12 fractions, which completely resolved the lacrimal gland masses. Thirty months after radiotherapy, the patient was still alive with stable disease and no ocular symptoms.
2.2. Histopathology and immunohistochemistry
Histochemical and immunohistochemical stainings were performed as previously described.13 The following antibodies were used: CD5, CD20, CD79a, CD30, CD138, MUM-1, BCL-2, IgM, IgA, IgG, kappa light chain, lambda light chain, and Ki-67.
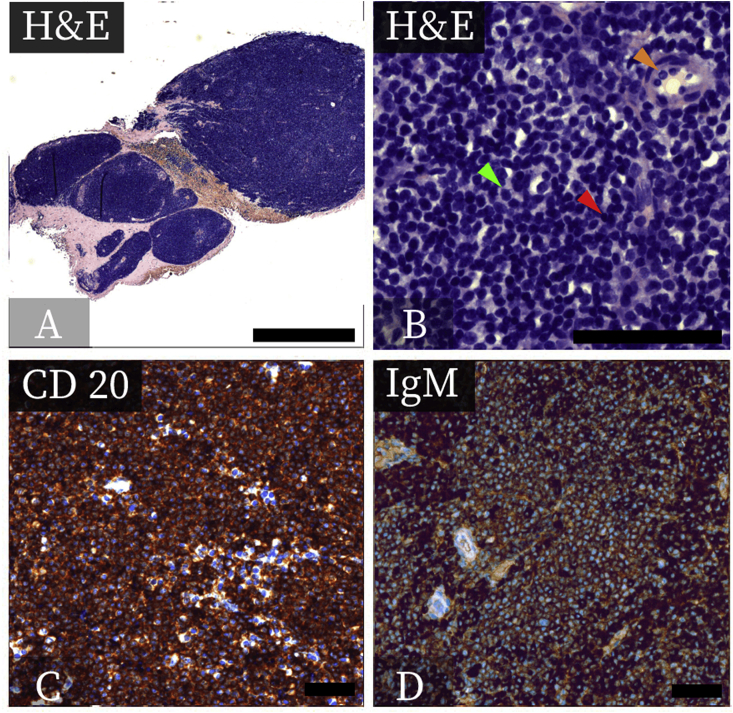
Light microscopy of the lacrimal gland biopsy revealed a diffuse dense pattern dominated by lymphoplasmacytic- and small lymphocytic tumor cells. The lymphoplasmacytic cells contained a dense basophilic nucleus with abundant cytoplasm. The small lymphocytic tumor cells presented with a dense nucleus with little cytoplasm. Some of the neoplastic cells had a blast morphology (Fig. 2). Minor areas of connective tissue as well as islands of normal ductal structures were present (Fig. 2). Neither pseudofollicles, neoplastic follicles, marginal zone, nor monocytoid B cells were present.
Fig. 2.
Histopathological features of a lymphoplasmacytic lymphoma of the lacrimal gland. A: A microscopic overview of the infiltrated lacrimal gland demonstrating many lymphocytic tumor cells (H&E, bar = 1 mm). B: A dense infiltration by lymphocytes is seen with some normal tubular structures still remaining (orange arrowhead). Characteristic small lymphocytic tumor cells (red arrowhead), lymphoplasmacytic B cells (green arrowhead) were seen in the specimen (H&E, bar = 70μm). C: Staining for the B-cell marker CD20 was positive (bar = 70μm). D: Positive immunoreaction was seen when staining for IgM, suggestive for an IgM secreting lymphoplasmacytic lymphoma (bar = 70μm).
The tumor presented a strong surface and cytoplasmic immunoreaction when staining for IgM. Furthermore, the tumor cells stained positive for CD20, CD79a, CD30, and BCL-2. Additionally, the specimen stained positive for kappa light chain and negative for lambda light chain (Fig. 2). Stainings for IgG, IgA, CD5, CD138, and MUM-1 were negative. The Ki-67 proliferative index was 15%. Based on these findings, LPL of the lacrimal gland was suggested as the final diagnosis.
2.3. Quantitative polymerase chain reaction (qPCR)
DNA was extracted from formalin-fixed and paraffin-embedded tissue using an in-house raw extraction method (Proteinase K and Tris EDTA). qPCR and high-resolution melting analysis of the MYD88 gene was performed on a Cobas 4800 system (Roche Diagnostics A/S, Hvidovre, Denmark) according to manufacturer's instructions.
Polymerase chain reaction of the MYD88 gene showed a mutation in MYD88 (c. 794T > C, p.L265P) highly suggestive for the diagnosis of LPL.
3. Discussion
This study presents a case of a 63-year-old male with systemic Waldenström's macroglubolinemia (WM) and bilateral lacrimal gland lymphoplasmacytic lymphoma with intermittent symptoms lasting for almost 4 years.
Morbus Waldenström (also known as Waldenström's macroglobulinemia) is a rare indolent hematological neoplasia constituting 1–2% of all hematological neoplasias.3 WM is defined by the World Health Organization (WHO) as a lymphoplasmacytic lymphoma (LPL) with systemic involvement, including bone marrow affection and with elevated serum IgM levels.2 The tumor cells are secreting IgM, and consequently, the symptoms are anemia and hyperviscosity. Initial signs are often found in the retinal vessels, with microvascular sludging and circulatory impairment due to the hyperviscosity with the risk of retinopathy.10 Extranodal infiltrates are frequently found; however, lacrimal gland infiltrates have only been reported in 5 cases (Table 1).
Table 1.
Cases of lymphoplasmacytic lymphoma in the lacrimal gland.
| Authors (year) | Age (years) | Gender | Symptoms | Duration | Location | Bilateral | Treatment | Recurrence |
|---|---|---|---|---|---|---|---|---|
| Little et al. (1967)7 | 65 | M | Swelling | N/A | Lacrimal gland | Yes | Radiotherapy | No |
| Schechterman et al. (1970)8 | 33 | F | Swelling | <6 months | Lacrimal gland | Yes | Chemotherapy | No |
| Krishnan et al. (1995)9 | 57 | M | Swelling | <12 months | Lacrimal gland + orbit | Yes | Radiotherapy | No |
| Leone et al. (1996)10 | 74 | F | Swelling | <12 months | Lacrimal gland | Yes | Chemotherapy | No |
| Hafezi et al. (2013)11 | 62 | F | Swelling | 6 months | Lacrimal gland | Yes | Chemotherapy | No |
| Present case | 63 | M | Swelling | 46 months | Lacrimal gland | Yes | Radiotherapy | No |
The diagnosis of WM/LPL can be difficult and often calls for a detailed morphologic and immunohistochemical investigation, as LPL may morphologically mimic several other lymphoma subtypes, including extranodal marginal zone B-cell lymphoma. In the present case, the patient was known with IgM secreting WM, and the histopathology along with immunohistochemistry pointed towards the diagnosis of LPL in the lacrimal gland specimen (Fig. 2). We performed a mutational analysis of the MYD88 gene and found the somatic mutation MYD88-L265P4. This particular somatic mutation is found in 90% of WM cases and thus supported the final diagnosis in our case.4,13 The MYD88 L265P mutation is known to trigger IRAK-mediated NFκB signaling, which is known to be involved in the lymphomagenesis of many lymphoma subtypes, including extranodal marginal zone B-cell lymphoma (EMZL).14,15
In the previous reported cases, the median age at presentation was 62 years and no sex predilection was observed. All previously reported cases of lacrimal gland WM/LPL presented with a gradually developing painless periorbital swelling. The present case presented with intermittent swelling of both eyelids over a 4-year period until the swelling was functionally disturbing the patient. This fluctuating clinical course has not previously been reported. In every other case, the swelling was reported to be progressive and thus became disturbing within a year from first presenting periocular swelling. Most previous cases were treated with chemotherapy, whereas the present case was effectively treated with local radiotherapy, which completely resolved the lacrimal gland masses. Both treatment options may be used with success, and the treatment of choice should be made on a patient-by-patient basis taking comorbidities and the risk of side effects into account.16 If the patient presents with previously unknown WM/LPL, a systemic treatment is recommended.16
In the present case along with all the other previously reported cases, both lacrimal glands were affected. An interesting question in this matter is how/why systemic WM suddenly infiltrates both lacrimal glands after several years of clinical stable disease. It is possible that expression of specific types of adhesion molecules on the neoplastic cells along with specific integrins may determine the homing properties and sites of infiltration in this disease.9
4. Conclusions
This case highlights that bilateral lacrimal gland WM/LPL may be causing intermittent periocular swelling and that lacrimal gland WM/LPL patients may benefit from local radiotherapy. Intermittent bilateral swelling of the eyelids should be carefully examined further in WM patients attending routine ophthalmological examination, as this can be a sign of lacrimal gland involvement and progression of the hematological disease.
Patient consent
This study adheres to the declaration of Helsinki, and the patient has given his written informed consent to the publication of all the included clinical information along with photographs.
Funding
None.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
No funding received. None of the authors have conflicts of interest with this submission.None of the authors have any conflicts of interest or disclosures relevant to this article.
Acknowledgements
LHM was funded by Candys Foundation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100597.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Rasmussen P., Ralfkiaer E., Prause J.U., Sjo L.D., Siersma V.D., Heegaard S. Malignant lymphoma of the lacrimal gland: a nation-based study. Arch Ophthalmol. 2011;129(10):1275–1280. doi: 10.1001/archophthalmol.2011.270. [DOI] [PubMed] [Google Scholar]
- 2.Swerdlow S.H.C.E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J. fourth ed. IARC; Lyon: 2017. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised. [Google Scholar]
- 3.Fonseca R., Hayman S. Waldenstrom macroglobulinaemia. Br J Haematol. 2007;138(6):700–720. doi: 10.1111/j.1365-2141.2007.06724.x. [DOI] [PubMed] [Google Scholar]
- 4.Treon S.P., Xu L., Yang G. MYD88 L265P somatic mutation in Waldenstrom's macroglobulinemia. N Engl J Med. 2012;367(9):826–833. doi: 10.1056/NEJMoa1200710. [DOI] [PubMed] [Google Scholar]
- 5.von Holstein S.L., Therkildsen M.H., JU Prause, Stenman G., Siersma V.D., Heegaard S. Lacrimal gland lesions in Denmark between 1974 and 2007. Acta Ophthalmol. 2013;91(4):349–354. doi: 10.1111/j.1755-3768.2012.02403.x. [DOI] [PubMed] [Google Scholar]
- 6.Andreasen S., Esmaeli B., Holstein S.L., Mikkelsen L.H., Rasmussen P.K., Heegaard S. An update on tumors of the lacrimal gland. Asia-Pacific journal of ophthalmology (Philadelphia, Pa) 2017;6(2):159–172. doi: 10.22608/APO.201707. [DOI] [PubMed] [Google Scholar]
- 7.Little J.M. Waldenstrom's macroglobulinemia in the lacrimal gland. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1967;71(6):875–879. [PubMed] [Google Scholar]
- 8.Schechterman L., Tyler S.J. Waldenstrom's macroglobulinemia. Localization in ileum and lacrimal glands. N Y State J Med. 1970;70(15):2025–2029. [PubMed] [Google Scholar]
- 9.Krishnan K., Adams P.T. Bilateral orbital tumors and lacrimal gland involvement in Waldenstrom's macroglobulinemia. Eur J Haematol. 1995;55(3):205–206. doi: 10.1111/j.1600-0609.1995.tb00253.x. [DOI] [PubMed] [Google Scholar]
- 10.Leone G., Parisi V., Rebecchi A., Guinetti C., Neuschuler R. Multiple ocular impairment in a patient affected by Waldenstrom's macroglobulinaemia. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 1996;234(8):533–535. doi: 10.1007/BF00184864. [DOI] [PubMed] [Google Scholar]
- 11.Hafezi F., Moesen I., Carels G., Mooy C., Paridaens D. [Waldenstrom's macroglobulinaemia of the lacrimal gland in a patient with sarcoidosis] Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2010;107(1):60–63. doi: 10.1007/s00347-009-2010-5. [DOI] [PubMed] [Google Scholar]
- 12.Verdijk R.M. An update of ocular adnexal lymphomas. Diagn Histopathol. 2015;21(1):26–33. [Google Scholar]
- 13.Mikkelsen L.H., Andreasen S., Melchior L.C. Genomic and immunohistochemical characterisation of a lacrimal gland oncocytoma and review of literature. Oncology Letters. 2017;14:4176–4182. doi: 10.3892/ol.2017.6713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu X., Li W., Deng Q. MYD88 L265P mutation in lymphoid malignancies. Cancer Res. 2018;78(10):2457–2462. doi: 10.1158/0008-5472.CAN-18-0215. [DOI] [PubMed] [Google Scholar]
- 15.Cabeçadas J., Martinez D., Andreasen S. Lymphomas of the head and neck region: an update. Virchows Arch. 2019;474(6):649–665. doi: 10.1007/s00428-019-02543-7. [DOI] [PubMed] [Google Scholar]
- 16.Mikkelsen L.H., Würtz N.S., Heegaard S. Recent advances in treating extra-ocular lymphomas. Expert Rev Ophthalmol. 2018;13(4):205–217. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.