Summary
Four factors have driven China's response to the HIV/AIDS pandemic: (1) existing government structures and networks of relationships; (2) increasing scientific information; (3) external influences that underscored the potential consequences of an HIV/AIDS pandemic and thus accelerated strategic planning; and (4) increasing political commitment at the highest levels. China's response culminated in legislation to control HIV/AIDS—the AIDS Prevention and Control Regulations. Three major initiatives are being scaled up concurrently. First, the government has prioritised interventions to control the epidemic in injection drug users, sex workers, men who have sex with men, and plasma donors. Second, routine HIV testing is being implemented in populations at high risk of infection. Third, the government is providing treatment for infected individuals. These bold programmes have emerged from a process of gradual and prolonged dialogue and collaboration between officials at every level of government, researchers, service providers, policymakers, and politicians, and have led to decisive action.
Introduction
In March, 2006, the State Council of the People's Republic of China officially announced the first legislation directly aimed at controlling HIV/AIDS: the AIDS Prevention and Control Regulations.1 These regulations, together with the Five-Year Action Plan to Control HIV/AIDS (2006–2010),2 are an important step in the development of government policy related to the care and prevention of HIV/AIDS. Although bold, these regulations were passed more than 20 years after the first case of HIV infection was identified. The development of a coherent policy was the result of a long and unsystematic process that involved initial mis-steps, considerable domestic and international education, debate, iterative trial-and-error learning, and scientific studies. The new legislation resulted from communication and coordination among many agencies, including administrators, service providers, politicians, the scientific community, and policymakers. We describe the influence of scientific studies and other factors on the development of HIV/AIDS policy in China and provide a timeline of important milestones in the development of the current policy (figure 1 ). This review is intended as a general overview of progress in China and does not attempt to provide a detailed account of province-to-province variation in the evolution and implementation of HIV prevention and control strategies.
Figure 1.
Important events in China's HIV/AIDS policy development, 1985–2006
ART=antiretroviral therapy. MMT=methadone maintenance treatment. NEP=needle exchange programme. PMTCT=prevention of mother-to-child transmission.
Overview of the epidemic
China's first AIDS case was identified in 1985 in a dying tourist.3 In 1989, the first indigenous cases were reported as an outbreak in 146 infected heroin users in Yunnan province, near China's southwest border.4 Between 1989 and the mid-1990s, HIV spread steadily from Yunnan into neighbouring areas and along the major drug trafficking routes, then from injecting drug users (IDUs) to their sexual partners and children. In the mid-1990s, the occurrence of a second major outbreak in commercial plasma donors in the east-central provinces became apparent.5 Plasma donors were paid to donate blood, the plasma removed, then the red blood cells reinfused to prevent anaemia. Reuse of tubing and mixing during collection and reinfusion led to thousands of new infections.6, 7 At the same time, HIV was also spreading through sexual transmission. By 1998, HIV had reached all 31 provinces and was in a phase of exponential growth (figure 2 ),8 which, by 2005, had culminated in an estimated 650 000 infections.9
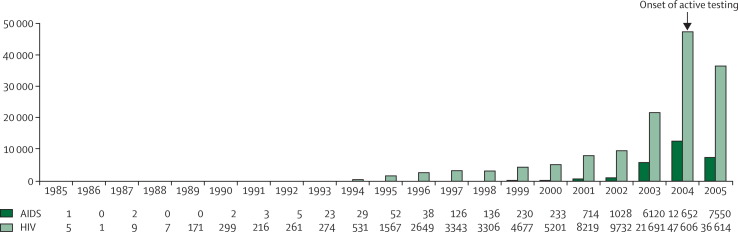
Figure 2.
Reported HIV/AIDS cases by year, 1985–2005
Early control strategies
Initially, the Chinese government focused its preventive strategies on stopping HIV from entering the country. Regulations were introduced that required foreigners who intended to stay 1 year or more and Chinese residents returning from overseas to have an HIV test.10, 11, 12 All imported blood products were banned.13, 14 There were attempts to stop transmission within the country as well—eg, laws against drug use15 and prostitution16 were strengthened and authorities were allowed to isolate HIV-positive individuals.12 In much the same way as other countries, traditional public-health methods of containment and isolation of infectious disease cases proved ineffective.17 Containment policies occurred in the context of rapid social and economic change, in which there were increases in drug use and changing sexual mixing patterns. These early policies did little to stop transmission of HIV; in fact, they probably promoted concealment of risk activities and made identification of HIV reservoirs more difficult.18, 19, 20
Information and communication networks
The attitudes of government officials shifted substantially over time, a result of increasing scientific evidence that Chinese people were becoming infected, the dramatic devastation caused by HIV/AIDS in other countries, and research in China that showed that HIV transmission could be reduced with targeted interventions.
As early as the mid-1990s, Chinese officials began to organise study tours to learn from the successes and failures of other countries in combating HIV/AIDS and to bring back information about strategies for HIV/AIDS control that could be adapted for China. Tour groups including officials from the Ministries of Health, Public Security, Justice, Education and Finance, Commissions of Development and Reform, and Population and Family Planning, as well as law and policymakers from the State Council, visited many places, including Australia, the USA, Brazil, Thailand, Europe, and Africa. These tours provided an opportunity for officials to learn from their counterparts in other countries, as well as promoting relationships between the different Chinese government sectors that participated in the study tours.
Workshops that involved key government agencies were also held within China to further foster cross-sector communications. The organisation of Chinese government services is traditionally hierarchical and departmentalised, not directly cultivating cooperation and collaboration across sectors. This tradition made the organisation of multifaceted responses appropriate for HIV/AIDS control difficult. The WHO Global Programme on AIDS, and subsequently UNAIDS, together with other UN agencies in Asia and the Pacific, such as the UN Drugs Control Programme (now the UN Office of Drugs and Crime), had important roles in working with the government of China to organise and facilitate cross-sector discussions.
One workshop in particular was pivotal in pushing policies to support interventions that targeted high-risk groups in China. Held in 1997 and organised by the Chinese Academy of Preventive Medicine (renamed the Chinese Centre for Disease Control and Prevention [CDC] in 2002) and the University of California at Los Angeles, the workshop drew together scholars from sociology, ethics, public health, and education, as well as government officials and representatives of international agencies such as WHO, UN, and the World Bank. This workshop was the first open discussion of evidence-based but controversial intervention strategies that targeted those at high risk of HIV infection who were also highly stigmatised—eg, sex workers, IDUs, and men who have sex with men. Although controversial—pitting scientific, evidence-based prevention approaches against conservative, moralistic attitudes—the consensus acknowledged the possible benefit of the implementation of new prevention strategies.
Members of these various workshops and study tours have been responsible for the identification of effective strategies that have increasingly been at the forefront of HIV control policy in China. They have also contributed to the development of strategic documents, including the Medium- and Long-Term Strategic Plan for HIV/AIDS (1998–2010),21 the Action Plan on HIV/AIDS Prevention and Containment (2001–2005),22 and the AIDS Regulations.1 Other key documents warned of the potential epidemic in China and might have influenced the attitudes of policymakers. China's Titanic Peril,23 published by the UN in 2002, made the unsubstantiated prediction that China could have 10 million HIV-infected individuals by 2010, a figure that has been repeatedly misused in discussions of China's HIV future. A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China (2004),8 developed jointly by UNAIDS and the State Council of China, estimated that China had 840 000 people living with HIV/AIDS. This figure has been revised down to 650 000 in 2005 in light of more representative data collection and more appropriate estimation methods.9 Although this figure represented a prevalence of about 0·05%, it was substantially higher than previous government estimates (300 000 in 199821) and provided the impetus for immediate scale-up of prevention and control strategies.
Scientific evidence for innovative policies
Concurrent with educational activities and network building for government officials, Chinese researchers identified the key risk groups, documented and predicted the course of the epidemic, observed successful programmes in other countries, and tested the effectiveness of behavioural interventions. HIV-related research projects were done by universities, hospitals, and community agencies, both independently and as collaborative projects with other domestic and international institutions. Most research and surveillance commissioned by the Chinese government is done by the National Centre for AIDS/STD Control and Prevention (NCAIDS) at the Chinese CDC. At the local level, almost all HIV research and intervention—whether done by the Chinese CDC or other research organisations—is done in collaboration with provincial and county CDCs, township hospitals, and village health workers. Research initiated by the Chinese CDC administrators, especially that commissioned by the Ministry of Health, is diffused and implemented faster than research done outside the existing government structure.
Reduction of transmission via injecting drug use
Intravenous drug use represents the largest single cause of HIV transmission in China, accounting for 44·3% of infections at the end of 2005.9 Ministry of Public Security data suggests that the number of registered drug users has risen steadily at a rate of about 122% per year, from 70 000 in 1990 to 1·16 million in 2005. The total number, including unregistered drug users, is thought to be much higher, with one estimate placing the figure at 3·5 million;24 the UNODC World Drug Report estimated that in 2003, 0·2% of 16–64-year-olds (ie, 1·7 million people) were opiate abusers.25 The most commonly used drug is heroin, which accounts for 85% of total reported drug use, although amphetamines are becoming more common, especially in urban areas.26 Many drug users begin heroin use by smoking, but later find it more cost effective to inject because of the stronger effect gained from injecting a smaller amount. Sharing injection equipment is common.27
National policymakers have recently shifted their position and publicly acknowledged the extent and pattern of increasing drug use, which has led to a rapid increase in treatment options for drug users. According to the regulations on the prohibition of narcotics,15 drug users identified by authorities for the first time are fined or sent to a voluntary detoxification centre run by the health system, which might include short-term use of methadone, buprenorphine, or traditional Chinese medicine. Detoxification costs 2000–5000 yuan (about US$250–625) for one phase of treatment.28, 29 If, as often happens, the treatment is not successful, relapsing patients identified by authorities are sent to a compulsory rehabilitation centre, administered by the Ministry for Public Security, for 3–6 months. Those with multiple relapses are detained in a re-education-through-labour centre, managed by the Ministry of Justice, for 1–3 years. In reality, internment procedures and durations vary enormously between administrative units. In general, centres focus on detoxification. Although some health education or treatment is provided, the relapse rate is extremely high.30, 31, 32
Cooperative actions by politicians, policymakers, government officials, and scientific researchers have resulted in the introduction of new strategies for drug control over the past 6 years. For example, the government is working with neighbouring countries to prevent drug smuggling, and is increasing anti-drug education for the general population and in schools.29 The government has also commissioned research on harm reduction strategies, such as methadone maintenance treatment and needle exchange programmes.
Needle exchange programmes
Needle exchange programmes are not a strategy officially sanctioned by the Ministry for Public Security since such strategies give the appearance of condoning drug use. Thus, when this strategy was first introduced, it was called needle social marketing—increasing the commercial availability and accessibility of needles in combination with health education about safe injecting practices and, in some cases, provision of free needles.27 Since 2001, the State Council has officially advocated needle social marketing as an HIV prevention measure.22 Evidence from research and study tours to countries such as Australia,33 which runs successful needle exchange programmes, prompted the Ministry of Health to support the first such programme in Yunnan province and Guangxi Zhuang Autonomous Region in 1999. In 2000–02, a larger intervention trial of needle exchange programmes was done in four counties of Guangdong province and Guangxi, funded by the World AIDS Foundation.34, 35 Cross-sectional data gathered at follow-up indicated that participants in intervention communities were almost three times less likely to have shared needles in the past month than those in control communities (odds ratio 0·36, 95% CI 0·25–0·52). Furthermore, rates of infection with hepatitis C virus were significantly lower in the intervention arm than in the control arm (51·1% vs 83·6%, p=0·001) and HIV rates were lower in the intervention arm; however, this was significant only in Guangdong (p=0·011) and not in Guangxi (p=0·2) nor overall (18·1% vs 23·6%, p=0·391).
The results of the trial were used to develop national policy guidelines in 2002, and needle exchange programmes have been included in the second 5-year action plan.2 The programme was substantially scaled-up in 2006, from 93 sites to 729 by the year's end. Scale-up has been focused in rural areas, and in many places additional services are offered to IDUs, including condom distribution, voluntary counselling and testing, antiretroviral therapy, and educational information about drug use and HIV.36
Methadone maintenance treatment programmes
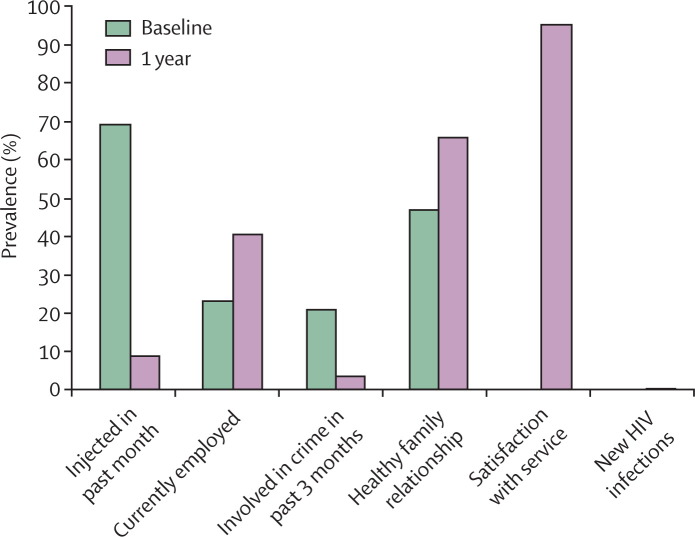
A large body of international research has shown the efficacy of methadone maintenance treatment programmes for the treatment of drug addiction and subsequent reduction in HIV risk behaviours.37, 38, 39, 40 In acknowledgment of this evidence, in 2004 the Chinese government called for the use of such practices to mitigate HIV transmission.41 Immediately, under the governance of the Ministries of Health and Public Security and the State Food and Drug Administration, a pilot study of eight clinics in five provinces was done.42, 43 Inclusion in the programme required: (1) several failed attempts to quit the use of heroin, (2) at least two terms in a detoxification centre, (3) age at least 20 years, (4) being a registered local resident of the area in which the clinic is located, and (5) being of good civil character. Those testing HIV positive need only fulfil criteria 4 and 5. To monitor the progress of the clinics, a database was established to gather data on demographics, medical issues, drug use, and other information about the patients. These data were assessed at 3, 6, and 12 months, and indicated reductions in heroin use, drug-related crime, and unemployment in those who received methadone maintenance treatment (figure 3 ).
Figure 3.
Prevalence of participant characteristics in the methadone maintenance treatment pilot project
On the basis of the successes of the pilot, the programme began scale-up in 2004 and plans are in place to open an additional 1500 methadone maintenance treatment clinics for about 300 000 heroin users by 2008. A National Training Centre for methadone maintenance treatment has been established in Yunnan to provide clinical and technical support. The services offered at such clinics have been broadened and provide access to other services, including HIV and hepatitis testing, antiretroviral therapy for eligible AIDS patients, group activities, and skills training for employment. The use of methadone maintenance therapy has been incorporated into the AIDS Regulations as a treatment for heroin addiction. Additionally, the requirements for entrance into methadone maintenance treatment programmes have been relaxed to encourage greater access. For example, patients are no longer required to have local residency or a previous history of internment in a detoxification centre. The programme is not without problems, however, and retaining drug users in the programme remains a critical challenge.
Sexual transmission
Although most HIV-infected individuals in China are drug users, patients infected through sexual transmission are the fastest growing group, accounting for close to 50% of new infections in 2005.9 Overall, they represent 43·6% of total HIV/AIDS cases, including commercial sex workers or their clients (19·6%), partners of HIV-infected individuals (16·7%), and men who have sex with men (7·3%).9 As with drug use, sexuality is not openly discussed in Chinese society and is therefore neither easily targeted by health promotion campaigns, nor has it traditionally been taught in schools. Even among university students, levels of AIDS knowledge and risk perception are alarmingly low.44, 45 On the other hand, attitudes towards sex are becoming increasingly more liberal and, as a result, premarital and extramarital sex are more commonly practised.46, 47 Although they are widely available, condoms are rarely used.48
Commercial sex work
Commercial sex work is illegal in China; hence, brothels are illegal and commercial sex workers operate out of places of entertainment (eg, karaoke bars), hotels, hair-dressing salons, or on the street.49 The traditional strategy for controlling HIV transmission through commercial sex workers has been the development of stricter laws to prevent risky behaviours,16 accompanied by raids on suspected sex establishments by public security officials.20, 49 Those apprehended are subject to compulsory education on law and morality, testing and treatment for sexually transmitted diseases,49 and forced participation in productive labour.20 Under the Frontier Health and Quarantine Law,12 those knowingly infected with HIV who continue to practise prostitution are subject to more severe penalties and criminal liability for creating a risk of spreading a quarantinable disease.12, 49 Detention ranges from 6 months to 2 years. Until recently, health education in this system was uncommon.
In 1996–97, following the success of prevention interventions in neighbouring Thailand,50 the Chinese CDC launched the first intervention projects to promote safer sex behaviours to prevent HIV and other sexually transmitted diseases in commercial sex workers working at entertainment establishments in Yunnan.51, 52 These projects showed the feasibility of such programmes, which included condom use to control the spread of HIV and other sexually transmitted diseases in commercial sex workers, and have been officially promoted since 1998.21 Between 1999 and 2001, the World AIDS Foundation supported a five-site trial of a behavioural intervention in commercial sex workers who worked in entertainment establishments.54, 55 The intervention included condom promotion, establishment of clinics for sexually transmitted diseases to provide check-ups, and outreach for health education and counselling. HIV-related knowledge improved substantially, and the rate of bacterial sexually transmitted diseases fell. The rate of condom use at last intercourse increased from around 55% to 68%, and fewer commercial sex workers agreed to sex without a condom when requested by a client who offered more money. The prevalence of gonorrhoea fell from about 26% at baseline to 4% after intervention, and the prevalence of chlamydia fell from about 41% to 26%.
The findings from this trial were used to draft national guidelines for interventions among sex workers in China. The provision of condoms at entertainment establishments is now an official requirement under the AIDS Regulations. Condom vending machines are being installed in venues such as university campuses and hotels, and condom promotion and HIV education campaigns that target youth and migrant workers are gradually being scaled up.55, 56
Influential forces
Changes in government
In 2003, a new administration led by President Hu Jintao, Premier Wen Jiabao, and Vice Premier and Health Minister Wu Yi substantially accelerated the commitment to and implementation of evidence-based HIV policies. Under this administration, a number of initiatives have been introduced: the China Comprehensive AIDS Response (China CARES), which assists 127 high-prevalence counties in providing care and support to people living with HIV/AIDS; the “Four Free and One Care” policy (panel ); and the formation of a State Council AIDS Working Committee responsible for the development of a comprehensive policy framework (eg, the Notice on Strengthening HIV/AIDS Prevention and Control).8 New policies, supported by expanded budgets, have been introduced (figure 4 ), which has permitted a substantial acceleration in programme development, testing, and scale-up.
Panel. Chinese government “Four Free and One Care” policy for AIDS control.
-
•
Free antiretroviral drugs to AIDS patients who are rural residents or people without insurance living in urban areas.
-
•
Free voluntary counselling and testing.
-
•
Free drugs to HIV-infected pregnant women to prevent mother-to-child transmission, and HIV testing of newborn babies.
-
•
Free schooling for AIDS orphans.
-
•
Care and economic assistance to the households of people living with HIV/AIDS.
Figure 4.
Chinese central government spending on HIV/AIDS by year, 1985–2005
Media
The media have exerted substantial influence over the timing and course of HIV control in China by bringing news of HIV to the attention of the public, administrators, and policymakers. In 1996, the Southern Weekend newspaper ran a front-page story and devoted another two pages to AIDS in China. This coverage was the first time any comprehensive exposure of the HIV/AIDS epidemic in China had been published by the Chinese press. From 1999, the international and subsequently the national media reported on the thousands of infected plasma donors in Henan and neighbouring provinces who did not have access to services. Although the government had acted quickly when the tragedy became apparent in 1995 by shutting down collection stations and, later, introducing new laws and regulations on the collection and management of blood and blood products,6, 57, 58 provision of HIV testing, prevention, and care for donors in the local areas was slower. Progress was stimulated by the media's attention to the plight of the infected plasma donors. Since these initial reports, the HIV/AIDS situation in China has received much attention from the local and international media.
Severe acute respiratory syndrome
The challenge of managing the severe acute respiratory syndrome (SARS) epidemic in 2003 is often credited with further motivating the government to take aggressive policy action on HIV-related issues. SARS showed not only how infectious diseases could threaten economic and social stability but also the effect of China's policies on international health problems.19 Policymakers announced a change of focus from purely economic goals to increasing the focus on health and social wellbeing and, as a result, increased support for public-health agencies. In controlling SARS, contact between the government and international agencies such as WHO, UN, and the US Centers for Disease Control and Prevention was essential and further stimulated stronger international collaboration for HIV/AIDS prevention and treatment. Intervention strategies necessary for SARS control have been translated into HIV/AIDS prevention—eg, real-time electronic case reporting.
Programme scale-up
Case finding
The first step in understanding the extent of an epidemic is to be able to identify cases. National sentinel surveillance has been implemented since 1995, but was initially restricted to high-risk areas and to attendees at sexually transmitted disease clinics, female sex workers, drug users, and long-distance truck drivers. Surveillance has gradually been expanded to 845 national sites and now also includes pregnant women and men who have sex with men.
Around the same time, voluntary testing and counselling was made available in some communities, but, even where available, was rarely used. Reluctance to seek HIV testing was probably due to a number of causes—eg, cost, inaccessibility of services, absence of any treatment, scant publicity or advocacy for testing, low or no perceived risk, and stigma associated with the use of testing services.59, 60, 61, 62 In the past 3 years, the government has addressed the environmental barriers. The high cost was addressed in 2003 by making free HIV testing available for the poor,63 and later, under the Four Free and One Care policy, antiretroviral treatment was made freely available for all through the Chinese health system. The number of screening laboratories has been expanded to 5500, and there are now 99 laboratories able to do confirmatory HIV tests. Free HIV testing has been made available, and expanded from 365 counties in 15 provinces in 2002 to over 2300 counties, with 3037 sites, in all provinces in 2006. The AIDS Regulations have introduced penalties for health units that do not provide free testing on request.
The rapid expansion of testing infrastructure has been largely prompted by the introduction of provider-initiated routine testing campaigns to identify infected individuals and put them in contact with treatment services. Client-initiated testing was failing to identify most infected individuals, so campaigns to screen high-risk groups, including drug users, commercial sex workers, prisoners, and former plasma donors, were commissioned to link patients to treatment services.64 The campaigns have resulted in a substantial increase in the number of individuals who know their HIV status, with an additional 60 000 people living with HIV/AIDS identified. This increased identification explains, at least in part, the rapid rise in reported HIV cases in the early 21st century (figure 2). However, even with this effort, only about 22% of the estimated 650 000 HIV-infected individuals living in China at the end of 2005 have been identified.9 Routine testing in high-risk groups continues.
Educating the public
Testing campaigns were accompanied by community-level social marketing to raise awareness of HIV and to reduce HIV-related stigma. The AIDS Regulations have outlined requirements for local governments at the county level and above, as well as for educational establishments, businesses, health providers, customs and border control, and the media to promote HIV/AIDS education and social marketing. A number of schools now include sex, drug, and HIV education for their pupils, especially in high-risk areas such as Yunnan, Guangxi, and Guangdong.
An important part of HIV education is targeting behaviour to reduce stigma towards people with HIV/AIDS. Stigma is well recognised as a major barrier to HIV control, because it prevents people from seeking services for testing and treatment, and discourages people from practising safer behaviours.59, 65, 66 To address this issue, senior political figures have been involved in anti-discrimination campaigns, and have publicly shown that HIV cannot be transmitted through casual contact. For example, on World AIDS Day, Dec 1, 2003, Premier Wen Jiabao publicly shook hands with AIDS patients in Beijing Ditan Hospital.67 The day before the 2004 World AIDS Day, President Hu Jintao and other senior government leaders visited patients living with HIV/AIDS and called for the elimination of bias against this group.68 During the Chinese New Year celebrations in 2005, Premier Wen Jiabao visited the homes of HIV-infected villagers in Henan province. These actions had a tremendous effect on the general community, and have now been backed up by policy changes. The AIDS Regulations have made it illegal to discriminate against people living with HIV/AIDS and their families in terms of their rights to schooling, employment, health services, and participation in community activities. Furthermore, the AIDS Regulations and the 2004 revision of the Law on the Prevention and Treatment of Infectious Disease69 include language to protect the identity and disease status of those with an infectious disease, with disciplinary action recommended for those individuals or institutions that violate these laws. Although there had been language in previous regulations to protect the rights of people living with HIV/AIDS, these new laws give such individuals and their families a stronger basis from which to defend their rights.
Antiretroviral treatment for people with HIV/AIDS
In 2001 and 2002, the number of patients living with HIV/AIDS being identified through treatment services began to increase. As many as 69 000 of these people were the rural poor who had been infected when they sold their blood and plasma in the mid-1990s and who were unable to access or afford much-needed antiretroviral treatment.9 On the basis of the successes of programmes in other nations, such as Brazil,70 a free antiretroviral therapy programme was piloted in late 2002 in Shangcai county, Henan province, one of the most severely affected areas.71 Patients were provided with a combination of zidovudine or didanosine plus lamivudine and nevirapine. On the basis of the improved health status and survival of the initial cohort, the programme was scaled up in early 2003, mainly through the China CARES programme.71
The provision of free antiretroviral therapy to rural residents and the urban poor became policy in 2003 under the Four Free and One Care policy (figure 4).67 The National HIV/AIDS Clinical Taskforce took the lead in establishing the programme, and set up a database to monitor it.71 As of the end of 2006, more than 30 640 patients have been treated in 800 counties in all 31 provinces. Research to inform further expansion and improvement of the programme is ongoing. Initial reports indicate that the current treatment regimen has a high drop-out rate (at least 8%), mainly due to side-effects, drug resistance, difficulty with adherence, and progression of disease.71 Therefore, the government is exploring options within the pharmaceutical industry to make additional regimens available,41 which will address both the issues of compliance, by making regimens with fewer side-effects available, and resistance, by making available additional lines of treatment.
Prevention of mother-to-child transmission
After reports of successful intervention in other developing countries,72 a feasibility trial of the prevention of mother-to-child transmission was piloted in late 2002 concurrent with the antiretroviral therapy pilot, with financial and technical support from UNICEF. Mothers who tested HIV positive were offered counselling, the option of abortion or antiretroviral therapy and, where available, caesarean delivery, to reduce the likelihood of mother-to-child transmission. Free formula milk for 12 months was provided for infants.73
On the basis of this pilot programme, national guidelines were developed to guide the prevention of mother-to-child transmission in the country. The provision of such services has been ratified by the AIDS Regulations. Services are being scaled up to cover at least 85% of infected pregnant women by 2007, and to reach at least 90% by 2010.2 Scale-up is being prioritised to the most heavily affected areas first. As of the end of 2005, more than 500 000 pregnant women in high-risk groups or in high-prevalence areas had been tested for HIV in 271 counties in 28 provinces. The overall participation rate in HIV testing in these pregnant women was 92%, and the HIV infection rate ranged from 0·3% to 0·7%. Among those who tested positive, 80% received antiretroviral therapy, and more than 90% accepted formula milk for the prevention of mother-to-child transmission.74
Planned programmes
Unlike prostitution and drug use, homosexuality has never been banned in China, but it was listed as a psychiatric disorder until 2001, and public acts of homosexual sex are punishable as hooliganism.75 Although increasingly tolerated in the cities, in general, homosexuality is highly stigmatised and men who have sex with men are under considerable pressure to conceal their sexual orientation.76 As a result, most homosexuals are married, or will be in the future, and form a bridge between the high-risk men who have sex with men group to their low-risk wives and other partners.75, 77, 78 The government has initiated few interventions for men who have sex with men, leaving such programmes to advocacy groups, non-governmental organisations (NGOs), and researchers.79 However, the government recently estimated that there were 5–10 million men who have sex with men living in China, of whom 1·35% are thought to be HIV positive.80 This information, in addition to studies indicating low levels of HIV knowledge, perceived risk, and testing, and high rates of sexually transmitted diseases,61, 81, 82 has prompted the Ministry of Health to now include men who have sex with men in the high-risk groups and to call for the development of novel interventions to target them.83
Challenges ahead
China has made impressive progress in the development and implementation of effective intervention strategies, especially in the past 3 years. The country is currently in a transition stage in its HIV policy development. It is increasingly adopting approaches that are based on scientific evidence and has encouraged the pilot testing of controversial methods of risk reduction (eg, methadone maintenance treatment, needle exchange programmes, and the targeting of men who have sex with men and sex workers).
Failures in scaling-up HIV prevention programmes have not been caused by an absence of policy, but rather, as with other countries, by there being no policy enforcement and timely scale-up. Although China has a strong central government, provincial and lower levels of government enjoy a great deal of autonomy, which has resulted in a mixed response and inconsistent enforcement of HIV/AIDS policy. For example, Yunnan province has shown strong support for implementation and advocacy of harm-reduction strategies that reduce HIV transmission in its many drug users, whereas Henan province had been slower to respond to the needs of former plasma donors in the early stages of the epidemic.84 Moreover, the distribution of HIV in China is not even, and is concentrated in areas with high drug use (eg, Yunnan, Guangxi, Xinjiang, and Sichuan) and in areas where people were infected through unsafe blood or plasma donation (eg, Henan, Anhui, Hebei, Shanxi, and Hubei). The number of cases ranges dramatically between provinces (figure 5 ), with, for example, just 20 cases reported from Tibet but well over 40 000 in neighbouring Yunnan. In provinces with an extremely low prevalence, it can be difficult for officials to see the need for HIV prevention and control.
Figure 5.
Reported HIV cases by province, 1985–2005
Conflicts of interest between departments, such as those responsible for health and public security, have also made coordination of services to reach high-risk groups that engage in illegal behaviour difficult.85 The central government has called for greater cooperation between relevant departments—including Public Security, Justice, Edu- cation, Civil Affairs, and Health—but implementation of this policy at the local level varies.
The problem is further exacerbated by inadequate resources and trained personnel. Many rural areas—where most of China's HIV-positive population resides—do not have the capacity to monitor patients' CD4+ cell counts and viral load. In some cases, the physical infrastructure exists, but staff do not have the skills or reagents to use it. Human resource capacity is a major constraint on China's ability to deliver HIV prevention and care. Many health workers and educators have poor knowledge of HIV and hold their own biases and stigmas towards those at risk or infected with HIV.86, 87, 88 A substantial proportion of the funds allocated to HIV prevention and control is being spent on establishing training centres and in building the capacity of health workers so that they can deliver better services. But many of those willing to work in rural areas do not have formal medical qualifications to begin with, which limits their abilities to understand the complexities of treating HIV patients.89 Furthermore, health services rely heavily on user fees, which often encourages health workers to do additional, chargeable services that many people living with HIV/AIDS cannot afford.90
With an estimated 650 000 people living with HIV/AIDS and an ever greater number of people at risk of infection, the government has embarked upon a formidable task. The provision of accessible testing and treatment services not only requires financial resources, but also, in many cases, reorganisation and supplementary funding of existing local health services infrastructure, especially in rural areas where most of Chinese HIV-positive individuals reside.91 In particular, rural areas do not have adequately trained staff capable of providing effective treatment and prevention services, as well as the laboratory and clinical infrastructure necessary to monitor treatment.71 The problem of inadequate human resources is not restricted to health departments—in rural areas, there are few adequately trained technical and management personnel at all levels and across all sectors. The combination of insufficiently trained staff, inadequate technical resources, and a largely remote, poorly educated, rural population represents a challenge to the implementation of effective programmes.
A major step has been the government's promotion of NGOs,92 which are a new concept in China.93 Many of the larger domestic groups are actually government funded, and those not affiliated with the government are required to go through a complicated registration procedure to be officially endorsed, although there might be a relaxation of these policies in the future.94 The presence of international NGOs is also increasing. The ability of NGOs to work with high-risk groups, especially those that engage in behaviours deemed to be illegal or immoral, and to provide care and outreach where overstretched health services cannot, is recognised.95 The private sector is also being encouraged to undertake prevention and education activities.96
Conclusion
What has allowed the mobilisation of multiple sectors within China? First, over a 15-year period there was a long series of educational workshops, conferences, collaborative projects, and networking between members at a number of levels of the government and administrative structural hierarchies. At local, national, and international forums, officials from many sectors were able to meet one another, share a common knowledge base, and debate the appropriateness of different interventions. Personal relationships were formed that facilitated the consideration and examination of previously unrecognised policy options for detection, prevention, and care. In a non-linear process, a consensus slowly evolved, identifying policy options.
Second, political officials, policymakers, administrators, and service providers were increasingly willing to recognise the relevance of a substantial body of scientific research that suggested effective intervention strategies that could change the course of the epidemic. Third, major policy recommendations with regard to behavioural interventions were preceded by small pilot projects that showed feasibility or efficacy in those populations at highest risk. Fourth, once the evidence base was documented, both the policymakers and politicians publicly showed their support for HIV prevention and care, as well as passing legislation to enforce and broadly disseminate health practices (eg, routine HIV testing and access to care).
These processes occurred in a context of ongoing influences from the media and international donor agencies, with some contribution from advocacy groups within China. The SARS epidemic showed the potentially disastrous effect of a fast-moving infectious disease and, simultaneously, allowed the HIV community to acquire new methods to fight the epidemic (eg, real-time data collection of new cases). However, mobilisation of resources, scientific evidence, and administrative drive did not occur until there was enthusiastic political commitment. The pace of implementation of innovative strategies for HIV detection, prevention, and care, accelerated with the commitments made by the government of Hu Jintao, starting in 2003.
After a slow start and reluctance to recognise the existence of risk activities in its population and of the HIV epidemic, China has responded to international influences, media coverage, and scientific evidence to take bold steps to control the epidemic, using scientifically validated strategies. The country now faces the challenge of scaling up these programmes and of convincing all levels of government to implement these innovative strategies and policies. This vigorous response, incorporating research findings into policy formulation, can be informative to other countries that face similar challenges in responding to the HIV/AIDS epidemic.
Acknowledgments
Acknowledgments
We thank Wendy Aft for editing the many drafts of this manuscript, and Professor Zuo-Feng Zhang for helpful suggestions. This work was supported by National Institutes of Health grants U19AI51915, D43TW000013, and U2RTW006918.
Conflict of interest statement
Z Wu is the Director of the National Centre for AIDS/STD Control and Prevention in the Chinese CDC. Y Wang is the Director of the Chinese CDC. Both have been directly involved in HIV/AIDS research and policy development in China.
References
- 1.State Council of the People's Republic of China. Regulations on AIDS prevention and treatment. Decree of the State Council of the People's Republic of China number 457. Beijing, 2006 (in Chinese).
- 2.State Council of People's Republic of China. China's action plan for reducing and preventing the spread of HIV/AIDS (2006–2010). State Council Document (2006) number 13. Beijing, 2006 (in Chinese).
- 3.Settle E. AIDS in China: an annotated chronology: 1985–2003. China AIDS Survey; Montreal: 2003. [Google Scholar]
- 4.Ma Y, Li ZZ, Zhang KX. Identification of HIV infection among drug users in China. Zhonghua Liu Xing Bing Xue Za Zhi. 1990;11:184–185. (in Chinese). [Google Scholar]
- 5.Wu Z, Liu Z, Detels R. HIV-1 infection in commercial plasma donors in China. Lancet. 1995;346:61–62. doi: 10.1016/s0140-6736(95)92698-4. [DOI] [PubMed] [Google Scholar]
- 6.Wu Z, Rou K, Detels R. Prevalence of HIV infection among former commercial plasma donors in rural eastern China. Health Policy Plan. 2001;16:41–46. doi: 10.1093/heapol/16.1.41. [DOI] [PubMed] [Google Scholar]
- 7.Zhuang K, Gui X, Su B, Tien P, Chen Z, Zhang L. High prevalence of HIV infection among women and their children in Henan Province, China. J Acquir Immune Defic Syndr. 2003;33:649–650. doi: 10.1097/00126334-200308150-00015. [DOI] [PubMed] [Google Scholar]
- 8.State Council AIDS Working Committee Office. UN Theme Group on HIV/AIDS in China . A joint assessment of HIV/AIDS prevention, treatment and care in China. China Ministry of Health; Beijing: 2004. [Google Scholar]
- 9.Ministry of Health of China. UNAIDS. WHO . 2005 update on the HIV/AIDS epidemic and response in China. Ministry of Health; Beijing: 2006. [Google Scholar]
- 10.Standing Committee of the National People's Congress. Law on the control of the entry and exit of aliens. Order number 31 of the President of the People's Republic of China. Beijing, 1985 (in Chinese).
- 11.Standing Committee of the National People's Congress. Law on the control of the exit and entry of Chinese citizens. Order number 32 of the President of the People's Republic of China. Beijing, 1985 (in Chinese).
- 12.Standing Committee of the National People's Congress. Frontier health and quarantine law. Order number 46 of the President of the People's Republic of China. Beijing, 1987 (in Chinese).
- 13.Ministry of Health of the People's Republic of China. Notice on banning import of blood products such as factor VIII. State Council Document (1985) number 49. Beijing, 1986 (in Chinese).
- 14.Ministry of Health of the People's Republic of China. Notice on strengthening management of imported blood products. State Council Document (1986) number 2. Beijing, 1987 (in Chinese).
- 15.Standing Committee of the National People's Congress. Decision on the prohibition of narcotic drugs. Beijing, 1990 (in Chinese).
- 16.Standing Committee of the National People's Congress. Decision on the strict prohibition against prostitution and whoring. Beijing, 1991 (in Chinese).
- 17.Wu Z, Rou K, Cui H. The HIV/AIDS epidemic in China: history, current strategies and future challenges. AIDS Educ Prev. 2004;16(3 suppl A):7–17. doi: 10.1521/aeap.16.3.5.7.35521. [DOI] [PubMed] [Google Scholar]
- 18.Li D, Xia G, Qiu R, Hamblin J, Yue T. Law, policies and regulations concerning HIV/AIDS prevention and containment: an assessment and recommendations. United Nations Development Programme; Beijing: 2003. [Google Scholar]
- 19.Xue B. HIV/AIDS policy and policy evolution in China. Int J STD AIDS. 2005;16:459–464. doi: 10.1258/0956462054308477. [DOI] [PubMed] [Google Scholar]
- 20.Husain L. Policing AIDS in China: official discourses, change, continuity, and unofficial voices. In: Christiansen F, Dosch J, Caroline R, Hamelman S, editors. Leeds East Asia Papers. Department of East Asia Studies, University of Leeds; Leeds: 2004. [Google Scholar]
- 21.Ministry of Health, State Development Planning Commission, Ministry of Science and Technology, Ministry of Finance. Chinese national medium-and long-term strategic plan for HIV/AIDS (1998–2010). State Council Document (1998) number 38. Beijing, 1998 (in Chinese).
- 22.State Council of the People's Republic of China. China's action plan on HIV/AIDS prevention and containment (2001–2005). State Council Document (2001) number 40. Beijing, 2001 (in Chinese).
- 23.The UN Theme Group on HIV/AIDS in China . China's titanic peril: 2001 update of the AIDS situation and needs assessment report. UNAIDS; Beijing: 2002. [Google Scholar]
- 24.Kulsudjarit K. Drug problem in southeast and southwest Asia. Ann N Y Acad Sci. 2004;1025:446–457. doi: 10.1196/annals.1316.055. [DOI] [PubMed] [Google Scholar]
- 25.UNODC . 2006 World drug report. United Nations Office on Drugs and Crime; Geneva: 2006. [Google Scholar]
- 26.National Drug Abuse Surveillance Center . Annual report on drug surveillance 2001. NDSAC in National Institute on Drug Dependence, China; Beijing: 2001. [Google Scholar]
- 27.Yap L, Wu Z, Liu W, Ming ZQ, Liang S. A rapid assessment and its implications for a needle social marketing intervention among injecting drug users in China. Int J Drug Policy. 2002;13:57–68. [Google Scholar]
- 28.Zhao C, Liu Z, Zhao D. Drug abuse in China. Ann N Y Acad Sci. 2004;1025:439–445. doi: 10.1196/annals.1316.054. [DOI] [PubMed] [Google Scholar]
- 29.Qian HZ, Schumacher JE, Chen HT, Ruan YH. Injection drug use and HIV/AIDS in China: review of current situation, prevention and policy implications. Harm Reduct J. 2006;3:4. doi: 10.1186/1477-7517-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Humeniuk R, Ali R. The first methadone clinic in Beijing. Drug Alcohol Rev. 2005;24:285–287. doi: 10.1080/09595230500167528. [DOI] [PubMed] [Google Scholar]
- 31.Liu H, Grusky O, Li X, Ma E. Drug users: a potentially important bridge population in the transmission of sexually transmitted diseases, including AIDS, in China. Sex Transm Dis. 2006;33:111–117. doi: 10.1097/01.olq.0000199762.28231.ee. [DOI] [PubMed] [Google Scholar]
- 32.Zou K. The “Re-education Through Labour” system in China's legal reform. Criminal Law Forum. 2002;12:459–485. [Google Scholar]
- 33.Bowtell W. Australia. In: Yamamoto T, Itoh S, editors. Fighting a rising tide: the response to AIDS in East Asia. 1st edn. Japan Center for International Exchange; Tokyo: 2006. pp. 19–52. [Google Scholar]
- 34.Wu Z, Lin P, Liu W, Ming ZQ, Pang L. Randomized community trial to reduce HIV risk behaviors among injecting drug users using needle social marketing strategies in China. 15th International AIDS Conference; Bangkok, Thailand; July 11–16, 2004.
- 35.Wu Z. Evaluation of a needle social marketing strategy for control of the HIV epidemic among injecting drug users in China. Final Report to the Word AIDS Foundation. Beijing: Chinese Academy of Preventive Medicine, 2002.
- 36.Liu B. Needle exchange programmes in China: effectiveness and factors associated with operation in two provinces. MSc thesis, Chinese Center for Disease Control and Prevention, 2006 (in Chinese).
- 37.Sullivan LE, Metzger DS, Fudala PJ, Fiellin DA. Decreasing international HIV transmission: the role of expanding access to opioid agonist therapies for injection drug users. Addiction. 2005;100:150–158. doi: 10.1111/j.1360-0443.2004.00963.x. [DOI] [PubMed] [Google Scholar]
- 38.Gossop M, Marsden J, Stewart D, Treacy S. Reduced injection risk and sexual risk behaviours after drug misuse treatment: results from the National Treatment Outcome Research Study. AIDS Care. 2002;14:77–93. doi: 10.1080/09540120220097955. [DOI] [PubMed] [Google Scholar]
- 39.Gibson DR, Flynn NM, McCarthy JJ. Effectiveness of methadone treatment in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 1999;13:1807–1818. doi: 10.1097/00002030-199910010-00002. [DOI] [PubMed] [Google Scholar]
- 40.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction. 1998;93:515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 41.Gill B, Morrison JS, Thompson D, editors. Defusing China's time bomb: sustaining the momentum of China's HIV/AIDS response. Center for Strategic and International Studies; Washington: 2004. [Google Scholar]
- 42.Wu Z. Landmark government methadone maintenance program in mainland China. 15th International AIDS Conference; Bangkok, Thailand; July 11–16, 2004.
- 43.Wu Z. Methadone maintenance program in mainland China: from pilot to scale-up. International Conference on the Reduction of Drug Related Harm; Belfast, UK; March 20–24, 2005.
- 44.Zhang H, Stanton B, Li X. Perceptions and attitudes regarding sex and condom use among Chinese college students: a qualitative study. AIDS Behav. 2004;8(2):105–117. doi: 10.1023/B:AIBE.0000030242.46843.71. [DOI] [PubMed] [Google Scholar]
- 45.Li X, Lin C, Gao Z. HIV/AIDS knowledge and the implications for health promotion programs among Chinese college students: geographic, gender and age differences. Health Promot Int. 2004;19:345–356. doi: 10.1093/heapro/dah308. [DOI] [PubMed] [Google Scholar]
- 46.Zhang K, Li D, Li H, Beck EJ. Changing sexual attitudes and behaviour in China: implications for the spread of HIV and other sexually transmitted diseases. AIDS Care. 1999;11:581–589. doi: 10.1080/09540129947730. [DOI] [PubMed] [Google Scholar]
- 47.Chen XS, Gong XD, Liang GJ, Zhang GC. Epidemiologic trends of sexually transmitted diseases in China. Sex Transm Dis. 2000;27:138–142. doi: 10.1097/00007435-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Yang H, Li X, Stanton B. Heterosexual transmission of HIV in China: a systematic review of behavioral studies in the past two decades. Sex Transm Dis. 2005;32:270–280. doi: 10.1097/01.olq.0000162360.11910.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gil VE, Wang MS, Anderson AF, Lin GM, Wu ZO. Prostitutes, prostitution and STD/HIV transmission in mainland China. Soc Sci Med. 1996;42:141–152. doi: 10.1016/0277-9536(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 50.Anon Thailand condom campaign reduced AIDS infections by fifty percent. AIDS Wkly Plus. 1996:19. Aug 12, [PubMed] [Google Scholar]
- 51.Wu Z. Final Report for Intervention on Female Prostitutes in Yunnan. Final Report to the World Bank. Chinese Academy of Preventive Medicine; Beijing, China: 1997. [Google Scholar]
- 52.Wu Z. Promoting condom use among female prostitutes in natural settings in Yunnan, China. 12th International AIDS Conference; Geneva, Switzerland; June 28–July 3, 1998.
- 54.Wu Z, Rou K, Li F, et al. Sustainability of effective STD/HIV prevention intervention targeting female sex workers and their clients at fice different settings in China. 14th International AIDS Conference; Barcelona, Spain: July 7–12, 2002.
- 55.Xinhua News Agency China to improve AIDS awareness among migrant workers. Xinhua News Agency. May 16, 2006. http://news.xinhuanet.com/english/2006-05/16/content_4554965.htm (accessed Oct 30, 2006).
- 56.Xinhua News Agency Tianjin makes AIDS prevention education compulsory. Xinhua News Agency. Feb 26, 2006. http://news.xinhuanet.com/english/2006-02/26/content_4229253.htm (accessed Oct 30, 2006).
- 57.Standing Committee of the National People's Congress. Blood donation law. Order number 93 of the President of the People's Republic of China. Beijing 1998 (in Chinese).
- 58.State Council of People's Republic of China. Regulations for the management of blood products. State Council Document number 208. Beijing, 1996 (in Chinese).
- 59.UNAIDS Stigma and discrimination fact sheet. http://siteresources.worldbank.org/INTEAPREGTOPHIVAIDS/Resources/fs_stigma_discrimination_en_pdf.pdf (accessed Oct 4, 2006).
- 60.Herek GM. AIDS and stigma. Am Behav Sci. 1999;42:1102–1112. [Google Scholar]
- 61.Choi KH, Lui H, Guo Y, Han L, Mandel JS. Lack of HIV testing and awareness of HIV infection among men who have sex with men, Beijing, China. AIDS Educ Prev. 2006;18:33–43. doi: 10.1521/aeap.2006.18.1.33. [DOI] [PubMed] [Google Scholar]
- 62.Wu Z, Rou K, Xu C, Lou W, Detels R. Acceptability of HIV/AIDS counseling and testing among premarital couples in China. AIDS Educ Prev. 2005;17:12–21. doi: 10.1521/aeap.17.1.12.58686. [DOI] [PubMed] [Google Scholar]
- 63.Koralage N. China to offer free HIV testing and treatment. BMJ. 2004;328:975. doi: 10.1136/bmj.328.7446.975-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu Z, Sun X, Sullivan SG, Detels R. Public health. HIV testing in China. Science. 2006;312:1475–1476. doi: 10.1126/science.1120682. [DOI] [PubMed] [Google Scholar]
- 65.Malcolm A, Aggleton P, Bronfman M, Galvao J, Mane P, Verrall J. HIV-related stigmatization and discrimination: its forms and contexts. Crit Pub Health. 1998;8:347–370. [Google Scholar]
- 66.Yang H, Li X, Stanton B. Willingness to participate in HIV/STD prevention activities among Chinese rural-to-urban migrants. AIDS Educ Prev. 2004;16:557–570. doi: 10.1521/aeap.16.6.557.53792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Watts J. China faces up to HIV/AIDS epidemic. Lancet. 2003;362:1983. doi: 10.1016/S0140-6736(03)15085-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.China Daily Hu visits AIDS patients in Beijing. China Daily. Nov 30, 2004. http://www.chinadaily.com.cn/english/doc/2004-11/30/content_396074.htm (accessed Nov 23, 2006).
- 69.Standing Committee of the National People's Congress. Infectious disease control act and HIV/AIDS act. Beijing, 2004 (amended) (in Chinese).
- 70.Teixeira PR, Vitoria MA, Barcarolo J. Antiretroviral treatment in resource-poor settings: the Brazilian experience. AIDS. 2004;18(suppl 3):S5–S7. doi: 10.1097/00002030-200406003-00002. [DOI] [PubMed] [Google Scholar]
- 71.Zhang FJ, Pan J, Yu L, Wen Y, Zhao Y. Current progress of China's free ART program. Cell Res. 2005;15:877–882. doi: 10.1038/sj.cr.7290362. [DOI] [PubMed] [Google Scholar]
- 72.WHO Technical Consultation . UNFPA/UNICEF/WHO/UNAIDS Inter-Agency Task Team on Mother-to-Child Transmission of HIV. New data on the prevention of mother-to-child transmission of HIV and their policy implications. World Health Organization; Geneva: 2000. [Google Scholar]
- 73.Wu Z, Sullivan SG. China. In: Yamamoto T, Itoh S, editors. Fighting a rising tide: the response to AIDS in east Asia. 1st edn. Japan Center for International Exchange; Tokyo: 2006. pp. 76–95. [Google Scholar]
- 74.Wang LH, Qiu X. Prevention mother to child transmission of HIV. In: Wang LD, editor. Epidemics of and responses to HIV/AIDS in China. Beijing Press; Beijing: 2006. (in Chinese). [Google Scholar]
- 75.Liu H, Yang H, Li X. Men who have sex with men and human immunodeficiency virus/sexually transmitted disease control in China. Sex Transm Dis. 2006;33:68–76. doi: 10.1097/01.olq.0000187266.29927.11. [DOI] [PubMed] [Google Scholar]
- 76.Choi KH, Liu H, Guo Y, Han L, Mandel JS, Rutherford GW. Emerging HIV-1 epidemic in China in men who have sex with men. Lancet. 2003;361:2125–2126. doi: 10.1016/S0140-6736(03)13690-2. [DOI] [PubMed] [Google Scholar]
- 77.Qian HZ, Vermund SH, Wang N. Risk of HIV/AIDS in China: subpopulations of special importance. Sex Transm Infect. 2005;81:442–447. doi: 10.1136/sti.2004.014258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Choi KH, Gibson DR, Han L, Guo Y. High levels of unprotected sex with men and women among men who have sex with men: a potential bridge of HIV transmission in Beijing, China. AIDS Educ Prev. 2004;16:19–30. doi: 10.1521/aeap.16.1.19.27721. [DOI] [PubMed] [Google Scholar]
- 79.Zhang BC, Chu QS. MSM and HIV/AIDS in China. Cell Res. 2005;15:858–864. doi: 10.1038/sj.cr.7290359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.China Daily Chinese gay population announced for the first time. China Daily. April 5, 2006. http://www.chinadaily.com.cn/hqylss/2006-04/05/content_560655.htm (accessed Nov 23, 2006).
- 81.Jiang J, Cao N, Zhang J. High prevalence of sexually transmitted diseases among men who have sex with men in Jiangsu Province, China. Sex Transm Dis. 2006;33:118–123. doi: 10.1097/01.olq.0000199763.14766.2b. [DOI] [PubMed] [Google Scholar]
- 82.Wong WC, Zhang J, Wu SC, Kong TS, Ling DC. The HIV related risks among men having sex with men in rural Yunnan, China: a qualitative study. Sex Transm Infect. 2006;82:127–130. doi: 10.1136/sti.2005.016790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu Z. Overview of behavioural interventions in China. In: Wang LD, editor. Epidemics of and responses to HIV/AIDS in China. Beijing Press; Beijing: 2006. (in Chinese). [Google Scholar]
- 84.Watts J. AIDS in China: new legislation, old doubts. Lancet. 2006;367:803–804. doi: 10.1016/S0140-6736(06)68318-9. [DOI] [PubMed] [Google Scholar]
- 85.Davis S. Restrictions of AIDS activists in China. Human Rights Watch. 2004;17:1–57. [Google Scholar]
- 86.Wu Z, Qi G, Zeng Y, Detels R. Knowledge of HIV/AIDS among health care workers in China. AIDS Educ Prev. 1999;11:353–363. [PubMed] [Google Scholar]
- 87.Hesketh T, Duo L, Li H, Tomkins AM. Attitudes to HIV and HIV testing in high prevalence areas of China: informing the introduction of voluntary counselling and testing programmes. Sex Transm Infect. 2005;81:108–112. doi: 10.1136/sti.2004.009704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li L, Lin C, Wu Z. Stigmatization and shame: consequences of caring for HIV/AIDS patients in China. AIDS Care. 2006;10:463–471. doi: 10.1080/09540120600828473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yip R. Opportunity for effective prevention of AIDS in China. In: Kaufman J, Kleinman A, Saich T, editors. AIDS and social policy in China. Harvard University Asia Center; Cambridge, MA, USA: 2006. pp. 177–189. [Google Scholar]
- 90.Zhang F, Hsu M, Yu L, Wen Y, Pan J. Initiation of the national free antiretroviral therapy program in rural China. In: Kaufman J, Kleinman A, Saich T, editors. AIDS and social policy in China. Harvard University Asia Center; Cambridge, MA, USA: 2006. pp. 96–124. [Google Scholar]
- 91.Ministry of Health of China . China's healthcare system and reform. Chinese Ministry of Health; Beijing: 2005. (in Chinese). [Google Scholar]
- 92.Xinhua News Agency China encourages NGO's participation in fight against AIDS. Xinhua News Agency. Mar 23, 2006. http://china.org.cn/english/2006/Mar/162981.htm (accessed Nov 29, 2006).
- 93.China Daily NGOs act as bridge between government and people. China Daily. Feb 23, 2006 [Google Scholar]
- 94.He Z. Helping NGOs develop strength. China Daily. May 28, 2005 [Google Scholar]
- 95.Chen HT, Liao Q. A pilot study of the NGO-based relational intervention model for HIV prevention among drug users in China. AIDS Educ Prev. 2005;17:503–514. doi: 10.1521/aeap.2005.17.6.503. [DOI] [PubMed] [Google Scholar]
- 96.People's Daily Chinese government invites private sector to join HIV/AIDS campaign. People's Daily Online. Mar 19, 2005. http://english.people.com.cn/200503/19/eng20050319_177468.html (accessed Oct 30, 2006).
Uncited reference
- 53.Wu Z. Sustainability of effective STD/HIV prevention intervention targeting female prostitutes and their clients at five different setting in China. Final Report to the World AIDS Foundation. Chinese Academy of Preventive Medicine; Beijing, China: 2002. [Google Scholar]