Abstract
Under physiological conditions, retinal pigment epithelium (RPE) is a cellular monolayer composed of mitotically quiescent cells. Tight junctions and adherens junctions maintain the polarity of RPE cells, and are required for cellular functions. In proliferative vitreoretinopathy (PVR), upon retinal tear, RPE cells lose cell-cell contact, undergo epithelial-mesenchymal transition (EMT), and ultimately transform into myofibroblasts, leading to the formation of fibrocellular membranes on both surfaces of the detached retina and on the posterior hyaloids, which causes tractional retinal detachment. In PVR, RPE cells are crucial contributors, and multiple signaling pathways, including the SMAD-dependent pathway, Rho pathway, MAPK pathways, Jagged/Notch pathway, and the Wnt/β-catenin pathway are activated. These pathways mediate the EMT of RPE cells, which play a key role in the pathogenesis of PVR. This review summarizes the current body of knowledge on the polarized phenotype of RPE, the role of cell-cell contact, and the molecular mechanisms underlying the RPE EMT in PVR, emphasizing key insights into potential approaches to prevent PVR.
Keywords: Proliferative vitreoretinopathy, Retinal pigment epithelium, Epithelial-mesenchymal transition, Tight junctions, Adherens junctions
Introduction
Proliferative vitreoretinopathy (PVR) is a complex blinding disease that occurs after rhegmatogenous retinal detachment (RRD), surgical interventions, or ocular trauma. As a prolonged and exaggerated scarring process, PVR is characterized by the formation of contractile fibrocellular membranes in the vitreous cavity and on the inner and outer surfaces of the retina (The Retina Society Terminology Committee, 1983; Mudhar, 2020; Tosi et al., 2014). At present, surgical interventions, including vitrectomy, membrane peeling, pneumatic retinopexy, and scleral buckle, remain the mainstay of treatment in PVR. Although work in recent decades has led to advancements in surgical techniques and management, PVR cannot be effectively treated and is still the most common cause of failure to reattach the retina (Coffee, Jiang & Rahman, 2014; Khan, Brady & Kaiser, 2015; Mitry et al., 2012; Wickham et al., 2011). In addition, in spite of successful anatomic reattachment, the visual function of such cases cannot be improved, due to the retinal damage resulting from the mechanical contraction of fibrous membranes. Therefore, in order to improve postoperative visual function and reduce the incidence of this serious complication, it is particularly important to explore new prophylactic and therapeutic approaches based on a deeper understanding of the pathogenesis of PVR.
A growing body of evidence indicates that the mechanisms of PVR are orchestrated by multiple elements (Idrees, Sridhar & Kuriyan, 2019; Jin et al., 2017; Pastor et al., 2016), such as growth factors (Charteris, 1998; Ni et al., 2020; Pennock et al., 2014; Wubben, Besirli & Zacks, 2016), cytokines (Bastiaans et al., 2018; Harada, Mitamura & Harada, 2006; Limb et al., 1991), extracellular matrix proteins (Feist et al, 2014; Miller et al., 2017) and various cells (Eastlake et al., 2016; Pennock et al., 2011; Shu & Lovicu, 2017). According to the histopathology of PVR, the fibrocellular membrane of PVR is composed of excessive extracellular matrix (ECM) and multiple types of cells, and retinal pigment epithelial (RPE) cells have been indicated as the most consistently present and the most abundant (Amarnani et al., 2017; Ding et al., 2017; Hiscott et al., 1989; Machemer & Laqua, 1975), proving that the RPE cell plays a crucial role in PVR. Under physiological condition, the polarized RPE cell is non-proliferative by cell–cell contact. However, when the eye suffers from a retinal break or trauma, RPE cells are exposed to various growth factors and cytokines that are produced by activated immune cells, leading to the disruption of junctional complexes in RPE cells. Subsequently, activated RPE cells detach from Bruch’s membrane, migrate through the defect of the retina, proliferate, and transform into myofibroblasts, forming fibrotic membranes (Chen, Shao & Li, 2015; Morescalchi et al., 2013; Palma-Nicolás & López-Colomé, 2013). In an analogous process to exaggerated wound healing response, these membranes can attach to the retina and contract, resulting in further retinal detachment and poor vision (Chiba, 2014; Garweg, Tappeiner & Halberstadt, 2013). It is noteworthy that due to the loss of cell–cell contact, RPE cells undergo epithelial-mesenchymal transition (EMT), which is pivotal in the development of PVR. During EMT, RPE cells transdifferentiate into mesenchymal cells that are characterized by increased motility, and enhanced ability to proliferate, resist apoptosis and produce extracellular matrix proteins, thus participating in PVR (Tamiya & Kaplan, 2016; Zhang et al., 2018c). These indicate that in-depth knowledge of EMT may provide insight into potential approaches to prevent PVR. Therefore, this review focuses on the polarized phenotype of RPE and molecular mechanisms of RPE cell EMT, discussing the role of RPE cells in PVR.
Survey Methodology
We used the PubMed database to search available literature based on keywords including “proliferative vitreoretinopathy(PVR)” and “retinal pigment epithelial cell”. To include more information on the polarity of RPE, we also searched articles about the structure and function of cell–cell junctions in RPE cells that explored the role of cell–cell contact in EMT.
The polarized retinal pigment epithelial cell
The human RPE cell achieves terminal differentiation at four to six weeks of gestation and subsequently remains mitotically quiescent (Lutty & McLeod, 2018; Stern & Temple, 2015). The RPE, which is situated between the photoreceptors and the choroid, plays many complex roles indispensable to the health of the neural retina and the choroid. These roles include recycling of components of the visual cycle, absorption of light to protect from photo-oxidative stress, production of essential growth factors, immunological regulation of the eye, phagocytosis of photoreceptor outer segments generated during daily photoreceptor renewal, and transportation across the blood retina barrier (BRB) (Ferrington, Sinha & Kaarniranta, 2016; Fields et al., 2019; Mateos et al., 2014; Naylor et al., 2019; Strauss, 2005; Vigneswara et al., 2015). In order to maintain these multiple functions, RPE cells display a highly specialized structural and functional polarity.
Similar to other epithelia, the RPE displays three characteristics of the epithelial phenotype: apical plasma membrane, junctional complexes, and basolateral domain. RPE cells display structural polarity, with apical microvilli and melanosomes, and basal microinfolds. The abundant melanin granules in RPE cells absorb stray light, a process that is essential for visual function (Strauss, 2005). In a polarized cell, the distributions of surface proteins on the apical and basal plasma membranes are different, contributing to the performance of cellular functions (Khristov et al., 2018). However, a highly polarized distribution of ion channels, transporters and receptors in RPE is different from that observed in conventional extraocular epithelia (Lehmann et al., 2014). For example, Na, K-ATPase (Sonoda et al., 2009) and monocarboxylate transporters (MCT) 1 (Deora et al., 2005) are localized to the apical aspect of RPE cells, while chloride transporter CFTR (Maminishkis et al., 2006) is basally located. On the apical plasma membrane, RPE cells phagocytize the photoreceptor outer segments, which are regulated by polarized receptors. Bulloj et al. (2018) found that binding of Semaphorin 4D (sema4D) to RPE apical receptor Plexin-B1 suppresses outer segment internalization, contributing to the maintenance of photoreceptor function and longevity. The RPE also transports fluid out of the subretinal space, and regulates bidirectional nutrient transport between the outer retina and the choroid, in a manner dependent on the polarized distribution of membrane channels and transporters (Strauss, 2005). The RPE basolaterally secretes extracellular matrix components and factors, which participate in ECM remodeling and maintain the outer BRB (oBRB) function (Caceres & Rodriguez-Boulan, 2020). Therefore, the polarized phenotype of the RPE is vital to both the oBRB and is the basis of the homeostasis of the outer retina (Caceres & Rodriguez-Boulan, 2020; Lehmann et al., 2014). The disruption of RPE polarity contributes to the development of several retinal diseases, such as PVR and age-related macular degeneration (AMD). A comprehensive understanding of the way in which this polarity is achieved may provide insights into the pathogenesis of PVR.
However, most available data on RPE polarity is contributed by studies performed on RPE-immortalized cell lines that show partial preservation of the RPE phenotype, and were extrapolated from data obtained from the prototype Madin-Darby Canine Kidney (MDCK) cell line (Lehmann et al., 2014). The detailed mechanisms that determine RPE polarization remain unclear. Some scholars believe that junctional complexes, including adherens junctions (AJs) and tight junctions (TJs), are essential for building epithelial cell polarity and maintaining the integrity of epithelial layers such as RPE (Niessen, 2007; Pei et al., 2019; Tamiya & Kaplan, 2016).
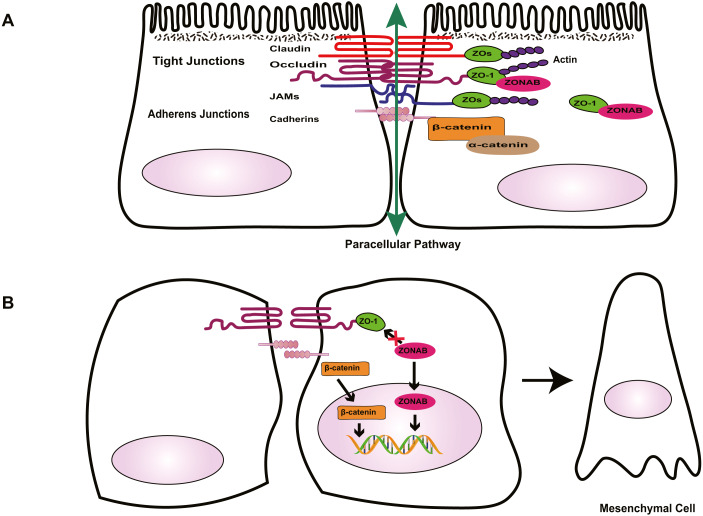
Tight junctions are complex cell–cell junctions formed by transmembrane proteins interactions with peripheral cytoplasmic proteins (Fig. 1). Transmembrane proteins include occludin, members of the claudin family, and junctional adhesion molecules (JAMs). Peripheral cytoplasmic proteins, such as zonula occludens (ZOs), form bridges between transmembrane proteins and the actin filament cytoskeleton and play a key role in the assembly and organization of TJs (Bazzoni & Dejana, 2004; Bazzoni et al., 2000; Naylor et al., 2019).
Figure 1. Role of cell-cell contact in health and PVR.
(A) Tight junctions and adherens junctions maintain cell-cell contact and cell polarity in RPE cells. Mature RPE cells with cell-cell contact remain dormant by sequestering EMT effectors to prevent nuclear localization. ZO-1 sequesters nucleic acid-binding protein (ZONAB) at tight junctions/cytoplasm, and adherens junctions sequester β-catenin by binding to epithelial cadherins. Tight junctions have a barrier function that control the passage of solutes. (B) Loss of cell-cell contact initiates EMT. Deconstruction of junctional complexes or reduction of epithelial cadherins/ZO-1 elicits nuclear localization of ZONAB/β-catenin and activation of their target genes, and disrupts the outer blood retinal barrier, facilitating the release of growth factors and cytokines, which further aggravate PVR.
The RPE tight junctions regulate the paracellular movement of solutes via size and charge selectivity (Benedicto et al., 2017; Caceres et al., 2017; Naylor et al., 2019).Occludin and claudins determine the permeability and semi-selectivity of the TJs, and as such play critical roles in the oBRB (Balda et al., 2000; Fields et al., 2019; Furuse et al., 1998; Günzel & Yu, 2013; Rosenthal et al., 2017). JAMs regulate TJ assembly and function by recruiting other proteins to the TJ and play an important role in the barrier property of TJs (Balda & Matter, 2016; Orlova et al., 2006; Shin, Fogg & Margolis, 2006). In patients with RRD, damage to TJs elicits the breakdown of oBRB and promotes the penetration of growth factors and cytokines, aggravating PVR. As well as having a barrier function, TJs define the physical separation between apical and basal domains of the plasma membrane, to maintain RPE cell polarity (Campbell, Maiers & DeMali, 2017; González-Mariscal et al., 2014; Sluysmans et al., 2017). The two extracellular loops of occludin mediate adhesion of adjacent cells and block the movement of plasma components. The C-terminal domain combines directly with ZOs, subsequently interacting with the actin cytoskeleton, which is essential to organizing and maintaining cell polarization (Balda & Matter, 2016; Furuse et al., 1994; Shin, Fogg & Margolis, 2006; Tarau et al., 2019). Feng et al. (2019) demonstrated that during EMT, the breakdown of TJs resulting from loss of claudin-1 causes ARPE-19 cells to lose their epithelial phenotype and transform into fibroblasts, promoting the development of PVR. TJs are involved in the regulation of signaling pathways that govern various cellular functions such as proliferation, migration, and differentiation (Bhat et al., 2018; Shi et al., 2018; Sluysmans et al., 2017). Vietor et al. (2001) found that decreased amounts of occludin can cause up-regulation and translocation of the adhesion junction protein β-catenin, which interacts with the transcription factor lymphoid enhancer-binding factor (LEF)/T cell factor (TCF) in the nucleus, leading to a loss of the polarized epithelial phenotype in EpH4 cells. ZOs, adaptor proteins within the TJ complex, exhibit dual localization at TJs and in the nucleus. Under injury or stress, the disruption of TJs increases ZO-2 nuclear accumulation, driving its interaction with transcription factors, and inducing MDCK epithelial cell proliferation (Islas et al., 2002; Shi et al., 2018; Traweger et al., 2003). In differentiated RPE cells, the interaction between ZO-1 with ZO-1-associated nucleic acid-binding protein (ZONAB) maintains cell–cell contact by sequestering ZONAB at the TJ or in the cytoplasm, maintaining cells dormancy. However, when damage to TJs decreases ZO-1 levels, ZONAB is translocated into the nucleus, leading to the up-regulation of cyclin D1 (CD1) and subsequent cell proliferation (Balda, Garrett & Matter, 2003; González-Mariscal et al., 2014). Therefore, TJs provide a structural foundation for the maintenance of cell–cell contact. Georgiadis et al. (2010) demonstrated that the overexpression of ZONAB or knockdown of ZO-1 could result in increased RPE proliferation and the development of EMT. Recent research has confirmed that during EMT, ZO-1 is decreased in ARPE-19 cells, and the knockdown of either ZO-1 or AJ protein E-cadherin leads to the downregulation of the other protein, indicating the existence of an interaction between the two junctional complexes (Bao et al., 2019). Due to the importance of TJs in the maintenance of integrity and functionality of epithelial cells, several researchers have focused on novel factors that stimulate the formation of TJs, such as nicotinamide (Hazim et al., 2019) and lysophosphatidic acid (Lidgerwood et al., 2018). Studies into these factors may produce well-differentiated RPE cell lines and a platform to enable the rapid expansion of our understanding of many RPE functions and retinal pathologies. This approach could be conducive to finding novel therapeutic interventions for PVR.
Besides the TJ complex described above, another type of junctional complex called AJs plays a key role in the maintenance of the integrity of epithelial cells and cell–cell contact (Fig. 1). Cadherins, the major proteins of AJs, belong to the glycoprotein superfamily, of which there are more than 20 members. The cytoplasmic domain of cadherins regulates interactions between cadherins and catenins, including β-catenin, α-catenin, and p120-catenin, and other scaffolding proteins such as ZO-1, to maintain cell shape and modulate cell proliferation (Aberle et al., 1994; Nelson & Nusse, 2004; Wheelock & Johnson, 2003). In quiescent adult RPE cells, epithelial cadherins (E- and/or P-cadherin) sequester β-catenin at the AJs to maintain cell–cell contact. Reduction of cadherin levels or dissociation of AJs allows β-catenin to translocate into the nucleus, where it interacts with the transcription factor LEF, and activates the transcription of various genes, including Snail and cyclin D1, which participate in RPE cell EMT via the canonical Wnt/β-catenin signaling pathway (Gonzalez & Medici, 2014; Lamouille, Xu & Derynck, 2014; Nelson & Nusse, 2004; Yang et al., 2018) . Tamiya, Liu & Kaplan (2010) suggested that the loss of P-cadherin causes the loss of cell–cell contact and initiates RPE cell migration and EMT. These events coincide with a switch in cadherin isoform expression from P- to N-cadherin. In addition, hepatocyte growth factor (HGF) and its receptor c-Met can destabilize cell–cell adhesion and elicit nuclear translocation of β-catenin, resulting in RPE cell migration (Lilien & Balsamo, 2005; Liou et al., 2002). Jin et al. found that HGF induces loss or redistribution of junctional proteins ZO-1, occludin, and β-catenin in RPE explants, potentially damaging barrier function and increasing the migration of RPE cells, resulting in retinal detachment(RD) and PVR (Jin et al., 2002; Jin et al., 2004). Given the importance of HGF in the interruption of RPE junction, HGF may be a potential target for the prevention and treatment of PVR. However, this possibility needs further study.
Under physiological conditions in the eye, TJs and AJs maintain the specialized structural and functional polarity of RPE cells and play a pivotal role in the maintenance of cell–cell contact; they sequester EMT signaling effectors ZONAB and β-catenin at the junction or cytoplasm to prevent cells from responding to mitotic factors, causing cells to leave the cell-cycle (Fig. 1). Thus, normally, RPE cells form a cobblestone-like monolayer of immotile, polarized, and mitotically quiescent cells. However, once junctional complexes break down, RPE cells undergo EMT, which is an important contributor to proliferative vitreoretinopathy. In this pathological process, RPE cells lose their structural and functional polarity and transdifferentiate into mesenchymal cells, which proliferate, resist apoptosis, possess migratory ability, and produce abundant ECM, leading to the formation of an aberrant scar-like fibrocellular membrane.
De-differentiated RPE and fibrocellular membrane
Proliferative vitreoretinopathy is characterized by the formation of fibrocellular membranes composed of proliferative and migratory cells and excessive, aberrant ECM. Histopathological analysis of PVR has demonstrated that PVR membranes have contractile activity and strain the retina, leading to tractional retinal detachment (TRD), which is responsible for blurring vision.
Several studies (Feist et al, 2014; Takahashi et al., 2010) have found that the cellular components of PVR membranes include RPE cells, myofibroblasts, fibroblasts, glial cells and macrophages, and that myofibroblasts are critical for the formation and contractile activity of fibrocellular membranes. Based on the indirect immunofluorescence evaluation of human PVR membranes, Feist et al (2014) showed that myofibroblasts originate principally from RPE cells through EMT. Myofibroblasts are characterized by increased expression of alpha-smooth muscle actin (α-SMA) and incorporation of α-SMA into newly formed actin stress fibers, which enhances their contractile properties. Myofibroblasts also secrete excessive matrix and pro-fibrogenic factors, promoting the contraction of PVR membranes that ultimately cause irreversible loss of vision (Gamulescu et al., 2006; Hinz et al., 2001; Shu & Lovicu, 2017; Tamiya & Kaplan, 2016; Tomasek et al., 2002).
In addition to myofibroblasts, abnormally increased ECM reinforces the continuous contractile tension of PVR membranes, and this mechanical tension, together with specialized ECM proteins, regulates myofibroblast differentiation and its function, contributing to PVR. In PVR membranes, the primary components of ECM are collagen and fibronectin. The majority of collagen fibrils are type I collagen, which is synthesized by RPE cells and Müller cells. Collagen fibrils provide tensile strength to the ECM, and activate Rho, resulting in the translocation of myocardin-related transcription factor (MRTF) into the nucleus and promoting RPE cell EMT (Guettler et al., 2008; Miralles et al., 2003). Fibronectin may also play a significant role in PVR. During pathological ECM remodeling, fibronectin is one of the earliest ECM components recruited, serving as a scaffold for other ECM proteins (Kadler, Hill & Canty-Laird, 2008; Miller et al., 2017; Miller et al., 2014). Extra domain (ED)-A fibronectin, a splice variant of fibronectin, is increased in transforming growth factor (TGF)-β2-induced RPE cells and induces myofibroblast differentiation, participating in PVR (Khankan et al., 2011).
Under normal conditions, ECM breakdown by proteases such as matrix-metalloproteases (MMPs) plays a crucial role in ECM remodeling and the release of growth factors, maintaining tissue homeostasis in cooperation with ECM synthesis, reassembly, and chemical modification (Bonnans, Chou & Werb, 2014; Craig et al., 2015; Lindsey et al., 2016). As mentioned above, the polarized RPE is able to basolaterally secrete the extracellular matrix components fibronectin and collagens, MMP and tissue inhibitors of MMPs (TIMPs), which participate in ECM remodeling. However, under pathological conditions such as inflammation and retinal injury, RPE cells lose their apical-basal polarity, undergo EMT and abnormally secrete MMPs, TIMPs and ECM proteins, leading to dysregulated ECM remodeling (Greene et al., 2017). Such ECM has aberrant composition and organization and mechanical properties, and enhances matrix stiffness and strain, which disrupts the normal structure and function of the retina, exacerbating the progression of PVR.
RPE and epithelial-mesenchymal transition
EMT of RPE cell
Epithelial-mesenchymal transition is an important biological process, in which epithelial cells transdifferentiate into mesenchymal cells. Although EMT can occur in normal embryonic development and wound healing, it also participates in pathological processes such as fibrosis, cancer progression, and PVR. There are three distinct subtypes of EMT: type 1 occurs during tissue and embryo development, type 2 is involved in wound healing and organ fibrosis, and type 3 is associated with cancer progression and metastasis (Dongre & Weinberg, 2019; Kalluri & Weinberg, 2009). This review focuses on type 2 EMT, which is crucial to PVR. During EMT, due to junctional complexes damage, RPE cells relinquish their apical-basal polarity, reorganize their cytoskeletal architecture, and convert into spindle-shaped cells (Fig. 1). These cells downregulate the expression of epithelial proteins such as E-cadherin and ZO-1, and increase expression of mesenchymal drivers including N-cadherin, vimentin, α-SMA and fibronectin (Li, Zhao & He, 2020). This mesenchymal transdifferentiation of RPE cells can increase the directional motility of individual cells, confer resistance to apoptosis, and facilitate cell proliferation and dysregulated ECM remodeling, eventually leading to the formation of PVR membranes.
Transcription factors of EMT
The details of the molecular mechanisms that drive RPE cell EMT and lead to PVR remain to be clarified. Emerging evidence suggests that diverse extracellular inductive signals, including soluble cytokines and growth factors, and ECM components, can modulate the expression and activity of EMT-associated transcription factors and act together to control the initiation and progression of EMT in responding epithelial cells (Yang et al., 2020). Among the various transcription factors involved in the induction of EMT, core transcription factors including Snail 1, Snail 2(also known as Slug), Twist 1 and zinc-finger E-box-binding (Zeb) 1 have been identified as important regulators of RPE cell EMT. These factors impact the expression of genes that control repression of the epithelial phenotype and activation of the mesenchymal phenotype (Boles et al., 2020; Feng et al., 2019; Li et al., 2019; Li et al., 2014; Liu et al., 2009; Palma-Nicolás & López-Colomé, 2013). For example, thrombin can repress the expression of E-cadherin by stimulating Snail 2 expression and promote the expression of N-cadherin by phosphoinositide 3-kinase (PI3K)/PKC-ζ/mTOR signaling in Rat RPE cells (Palma-Nicolás & López-Colomé, 2013). During RPE dedifferentiation in primary culture, Zeb1 is overexpressed and binds to the MITF A promoter to repress the cyclin dependent kinase inhibitor, p21CDKN1a, resulting in RPE cell proliferation and EMT (Liu et al., 2009). These EMT transcription factors often act in concert, functionally cooperating at target genes by the convergence of signaling pathways. However, the molecular details of how these transcription factors contribute to EMT are still elusive (Lamouille, Xu & Derynck, 2014; Stone et al., 2016).
Epigenetic factors of EMT
Due to the importance of epigenetic regulation of EMT, epigenetic modifiers have attracted increasing attention. Evidence has shown that epigenetic modifiers work in concert with transcription factors at different molecular layers to regulate the EMT process (Skrypek et al., 2017). Several epigenetic factors have been described including DNA methylation, histone modification and non-coding RNA. Because of the specific machinery utilized for EMT activation, these modifications are characterized by cell type specificity. In RPE cells, Methyl-CpG-binding protein 2 (MeCP2), a DNA methylation reader, plays a crucial role in the induction of EMT, and DNA methylation may participate in the pathogenesis of PVR (He et al., 2015; Li, Zhao & He, 2020). He et al. (2015) found high levels of expression of MeCP2 in all human PVR membranes, and concluded that MeCP2 mediates α-SMA expression through Ras GTPase activating protein (RASAL1). Furthermore, DNA methylation inhibitor 5-Aza-2′ deoxycytidine (5-AZA-dC) reportedly inhibits the expression of TGF-β-induced α-SMA and FN in human fetal RPE cells. It appears that 5-AZA-dC may have therapeutic value in the treatment of PVR. However, the mechanisms underlying the blockade of α-SMA and FN expression are complex, and further investigation is warranted.
Recently, the role of histone modifications associated with EMT has been assessed in RPE cells. However, there has been little research into the regulation of RPE cell EMT by histone modification. Boles et al. (2020) reported that TGF-β1 and TNF-α co-treatment (TNT) induces an EMT program in adult human RPE stem cell (RPESC)-RPE cells, involving an apparent reorganization of H3K27ac and H3K4me1 patterns at distal enhancers. The regions that gain H3K27ac tend to have a high H3K4me1/H3K4me3 ratio, indicating that they have enhancer activity and are associated with upregulated genes. Xiao et al. (2014) found that the expression of histone deacetylases (HDACs) in TGF-β-induced EMT of RPE cells was increased, and that Trichostatin A (TSA), a class I and II HDAC inhibitor, attenuated TGF-β2-induced EMT by inhibiting the canonical SMAD pathway and the non-canonical signaling pathways, including Akt, p38MAPK, ERK1/2 pathways and Notch pathway. Therefore, histone modifications may participate in the regulation of RPE cell EMT, and HDAC inhibitors may have potential as drugs for the prevention and treatment of PVR.
The study of EMT mechanisms at the RNA level has provided new perspectives on the treatment of PVR (Kaneko & Terasaki, 2017; Wang et al., 2016). MicroRNAs (miRNAs) are small noncoding RNAs that contribute to cellular processes by regulating gene expression. In differentiated RPE cells, microRNA-204 is highly expressed, and represses the expression of type II TGF-β receptors and Snail 2, maintaining epithelial structure and function. In contrast, low expression levels of miR-204 and anti-miR-204 promote RPE cells proliferation, participating in EMT (Wang et al., 2010). MicroRNA-194 overexpression can also suppress RPE cell EMT by attenuating the expression of Zeb1 (Cui et al., 2019). In addition to miRNAs, long non-coding RNAs (lncRNAs) contribute to the regulation of RPE EMT (Zhang et al., 2019). In RPE cells treated with PVR vitreous or TGF-β1, MALAT1 expression is increased, and knockdown of MALAT1 attenuates the phosphorylation of SMAD2/3 and the expression of Snail, Slug, and Zeb1, preventing cell migration and proliferation (Yang et al., 2016). In patients with PVR, MALAT1 is increased in the blood, and is reduced after surgery. Thus, MALAT1 may be a potential prognostic and diagnostic indicator for PVR (Zhou et al., 2015).
Signaling pathways of EMT
During RPE cell EMT, extracellular signals change the expression of genes encoding epithelial and mesenchymal proteins and mediate cellular behavior such as cell migration, proliferation, and apoptosis through a network of interacting signaling pathways that contribute to the development of PVR (Chen et al., 2014a; Chen et al., 2014b; Lee-Rivera et al., 2015). Among these, TGF-β and its intracellular cascades play a key role in the EMT of RPE cells.
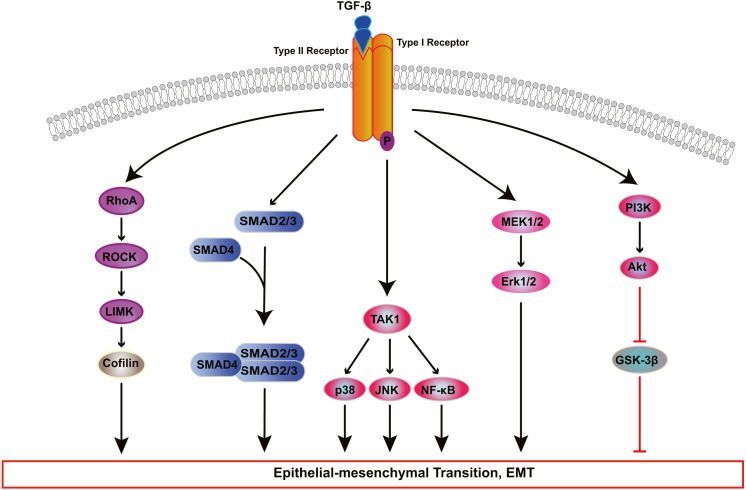
TGF-β induces EMT of RPE cells via two pathways: the classical SMAD-dependent pathway and the SMAD-independent pathway (Fig. 2) (Cai et al., 2018; He et al., 2017; Heffer et al., 2019; Ishikawa et al., 2015; Takahashi, Haga & Tanihara, 2015; Yao et al., 2019; Zhang et al., 2017; Zhang et al., 2018b; Zhou et al., 2017). In the SMAD dependent pathway, TGF-β binds to cell surface receptor complexes, and activates type I TGF-β receptors, which phosphorylate SMAD2 and SMAD3. The activated SMADs combine with SMAD4 to form a SMAD complex, which then enters the nucleus and combines with regulatory elements to regulate the expression of key genes associated with EMT. In addition to SMAD-dependent signaling, TGF β induces EMT through SMAD independent signaling pathways including Rho GTPase-dependent pathways (Lee, Ko & Joo, 2008), PI3K/Akt pathway (Huang et al., 2017; Yokoyama et al., 2012), mitogen-activated kinase (MAPK) pathways (Chen et al., 2017; Lee et al., 2020; Matoba et al., 2017; Schiff et al., 2019) and Jagged/Notch signaling pathway (Zhang et al., 2017). The MAPK signaling pathways include extracellular signal-regulated kinase(ERK) MAPK pathway, p38 MAPK pathway, and JUN N-terminal kinase (JNK) pathway (Parrales et al., 2013; Schiff et al., 2019; Xiao et al., 2014; Zhang et al., 2018a).
Figure 2. Signaling pathways of TGF-β-induced RPE cells EMT.
Transforming growth factor-β (TGF-β) activates various signaling pathways that cooperate to cause EMT. Besides canonical SMAD-dependent signaling, TGF-β can activate the Rho, PI3K/AKT, ERK MAPK, p38 MAPK, JUN N-terminal kinase (JNK) and nuclear factor-κB (NF-κB) pathways.
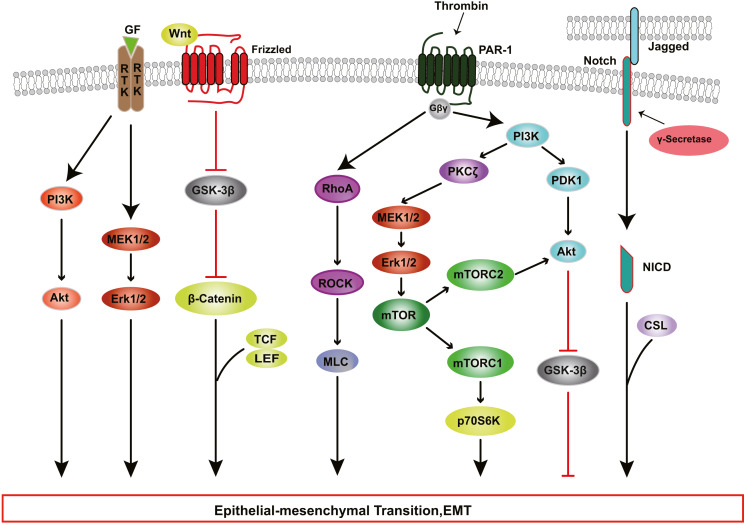
The Rho pathway has been reported to regulate the assembly and organization of the actin cytoskeleton and associated gene expression, and may be essential for the fibrotic response of RPE cells in PVR. In TGF-β1-treated ARPE-19 cells, activated RhoA or its downstream effector Rho kinase (ROCK) increase the kinase activity of LIM kinase (LIMK) which then phosphorylates cofilin. This phosphorylation attenuates the activity of cofilin, which promotes actin polymerization and reorganizes the actin cytoskeleton, leading to stress fiber formation (Lee, Ko & Joo, 2008). TGF-β-induced RhoA activation also facilitates cell migration and increases α-SMA expression in primary RPE cells (Tsapara et al., 2010). Itoh et al. (2007) demonstrated that ROCK inhibitor Y27632 and RhoA inhibitor, simvastatin, suppress TGF-β2-induced type I collagen expression in ARPE-19 cells, and confirmed the existence of crosstalk between the SMAD pathway and the Rho pathway. Some studies have suggested that activated SMAD3 induces NET1 gene expression to regulate RhoA activation in RPE cells (Lee et al., 2010). Moreover, thrombin can activate Rho and ROCK, leading to myosin light chain (MLC) phosphorylation and actin stress fiber formation in EMT of RPE cells (Fig. 3) (Ruiz-Loredo, López & López-Colomé, 2011). Therefore, ROCK inhibitor and RhoA inhibitor may be new potential therapeutic target drugs for PVR.
Figure 3. RTK, Wnt, Notch, and Thrombin signaling in RPE cells EMT.
Growth factors (GFs) stimulate receptor tyrosine kinases (RTKs) and induce EMT through PI3K-AKT and ERK MAPK signaling pathways. Thrombin activates PI3K and Rho signaling. PI3K promote EMT through Akt and mTOR pathways. WNT signaling promotes EMT by inhibiting glycogen synthase kinase-3β (GSK-3β) to result in nuclear localization of β-catenin, which interact with the transcription factors lymphoid enhancer factor (LEF) /T cell factor (TCF) and change genes expression. The intercellular interaction of Jagged ligands with Notch receptors induces EMT through the cleavage and release of the Notch ICD, which then activate target genes.
The PI3K/Akt pathway mediates a broad range of cellular functions, such as cell transformation, migration, proliferation, apoptosis, and gene expression (Aguilar-Solis et al., 2017; Liu et al., 2019). During PVR, binding of TGF-β to its receptor activates PI3K, resulting in the phosphorylation of Akt; activated Akt inhibits glycogen synthase kinase 3β (GSK-3β), promoting EMT in RPE cells (Shukal et al., 2020; Zhang et al., 2018a). Researchers have found that inhibition or knockdown of GSK-3β promotes cell migration and collagen contraction in ARPE-19 cells, while GSK-3β overexpression and PI3K/Akt inhibitor reverse these cellular responses (Huang et al., 2017). Some studies have shown that thrombin can activate PI3K, resulting in increased cyclin D1 expression and RPE cell proliferation, processes that are involved in the development of PVR through PDK1/Akt and PKCζ/mTORC signaling (Fig. 3) (Lee-Rivera et al., 2015; Palma-Nicolás & López-Colomé, 2013; Parrales et al., 2013).
In addition to the PI3K-AKT pathway, other kinase pathways contribute to EMT in cooperation with the SMAD-dependent signaling pathways. In human RPE cells, TGF-β activates TGF-β-activated kinase 1 (TAK1), which subsequently transduces signals to several downstream effectors, including p38 (Heffer et al., 2019), JNK (Kimura et al., 2015) and nuclear factor-κB (NF-κB) (Chen et al., 2016b), which participate in EMT. Dvashi et al. (2015) found that TAK1 inhibitor caused a reduction in both p38 and SMAD2/3 activity, attenuating cell migration, cell contractility and α-SMA expression in TGF-β1-induced RPE cells. Moreover, the ERK MAPK pathway plays a role in TGF-β-induced EMT and cooperates with other signaling pathways in the regulation of EMT in RPE cells. Recent studies (Chen et al., 2014b; Tan et al., 2017; Xiao et al., 2014) have shown that blocking the ERK1/2 pathway inhibits the phosphorylation of SMAD2 and the Jagged/Notch pathway. Inhibition of the Jagged/Notch signaling pathway can alleviate TGF-β2-induced EMT by regulating the expression of Snail, Slug and Zeb1 (Fig. 3); this also suppresses the ERK1/2 signaling (Chen et al., 2014b).
The contribution of growth factors other than TGF-β, such as HGF, fibroblast growth factor (FGF), epidermal growth factor (EGF) and platelet derived growth factor (PDGF) should also be factored in with regard to the induction of RPE EMT. These factors bind to and stimulate the autophosphorylation of transmembrane receptors on Tyr, subsequently participating in RPE cell EMT via PI3K/Akt pathway, ERK MAPK pathway, p38 MAPK pathway (Fig. 3) (Chen et al., 2016a; Ozal et al., 2020). Chen et al. (2012) explored the role of Wnt/β-catenin signaling in PVR, and found that when EGTA disrupted contact inhibition in RPE cells, EGF+FGF2 could activate Wnt signaling and increase nuclear levels of β-catenin, which interacts with TCF and/or LEF, leading to cell proliferation (Fig. 3); and EGF+FGF2 cooperated with TGF-β1 to induce EMT through SMAD/Zeb1/2 signaling. Acting together, various inductive signals received by RPE cells from their niche can trigger the activation of EMT programs by individual intracellular cascades or the crosstalk of multiple intracellular signaling pathways.
Interventions of RPE EMT
Therapeutic interventions against RPE EMT have largely been explored in mechanistic experiments using in vitro cell culture and in vivo animal models. To date, some promising drug candidates have been trialed in preclinical studies of PVR, including TGF-β receptor inhibitors, peroxisome proliferator-activated receptor (PPAR)-γ agonists, retinoic acid receptor-γ (RAR-γ) agonists and methotrexate (Shu, Butcher & Saint-Geniez, 2020; Zhou et al., 2020).Nassar et al. (2014) found that TGF-β receptor 1 inhibitor LY-364947 (LY) attenuates RPE cell transdifferentiation in vitro, and that intravitreal injection of LY completely prevents PVR and TRD in vivo. Evidence is emerging to show that the up-regulation of PPAR-γ expression may be beneficial for the treatment of fibrosis in several organs (Wang et al., 2019). Hatanaka et al. (2012) reported that PPAR-γ agonist pioglitazone could prevent TGF-β-induced morphological changes and the up-regulation of EMT-related markers in primary monkey RPE cells, through inhibition of the SMAD pathway. Some drugs, including dichloroacetate (DCA) (Shukal et al., 2020), salinomycin (SNC) (Heffer et al., 2019), resveratrol (Ishikawa et al., 2015), protein kinase A inhibitor H89 (Lyu et al., 2020) and heavy chain-hyaluronan/pentraxin3 (He et al., 2017), reportedly inhibit EMT in an in vitro EMT cell model and prevent PVR development by blocking the activation of theTGF-β pathway. Thus, inhibition of EMT by pharmacological agents may be an effective strategy to prevent PVR development.
Conclusion
Clinical and experimental studies have shown that RPE cells play an important role in PVR. Junctional complexes are crucial for the maintenance of RPE polarity. Under the influence of growth factors and cytokines, RPE cells lose cell–cell contact and apical-basal polarity, and undergo EMT via multiple signaling pathways, which promote cell proliferation, migration, and ECM production. RPE cells further transform into myofibroblasts and form fibrocellular membranes that have contractile activity and strain the retina, leading to tractional retinal detachment in PVR. As a complex refractory blinding disorder, PVR involves multiple signaling pathways and factors. In addition, the specialized polarity of RPE cells is fundamental for retinal homeostasis, and RPE EMT plays a key role in the development of PVR. Nevertheless, further research into the mechanisms underlying RPE polarity and EMT is needed to prevent this devastating complication. A deeper understanding of RPE polarization is fundamental for elucidating the mechanism of EMT initiation and progression, and is essential to exploring the potential pharmacologic prophylactic and therapeutic approaches to PVR. Various factors, such as microenvironmental signals, transcription factors, and epigenetic factors, participate in the regulation of EMT at different molecular levels. Further studies about the detailed molecular mechanisms of EMT are needed to facilitate the development of therapeutic strategies for PVR.
Funding Statement
This work was supported by the Medical and Health Personnel Special Project of Jilin Province (Grant No. 2019SCZT021) and the Health Service Capacity Improvement Project of Health and Family Planning Commission of Jilin Province (Grant No. 3D5172173429). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Hui Zou conceived and designed the experiments, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Chenli Shan and Linlin Ma performed the experiments, prepared figures and/or tables, and approved the final draft.
Jia Liu and Ning Yang analyzed the data, prepared figures and/or tables, and approved the final draft.
Jinsong Zhao conceived and designed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Data Availability
References
- Aberle et al. (1994).Aberle H, Butz S, Stappert J, Weissig H, Kemler R, Hoschuetzky H. Assembly of the cadherin-catenin complex in vitro with recombinant proteins. Journal of Cell Science. 1994;107(Pt 12):3655–3663. doi: 10.1242/jcs.107.12.3655. [DOI] [PubMed] [Google Scholar]
- Aguilar-Solis et al. (2017).Aguilar-Solis ED, Lee-Rivera I, Álvarez Arce A, López E, López-Colomé AM. FAK phosphorylation plays a central role in thrombin-induced RPE cell migration. Cellular Signalling. 2017;36:56–66. doi: 10.1016/j.cellsig.2017.04.016. [DOI] [PubMed] [Google Scholar]
- Amarnani et al. (2017).Amarnani D, Machuca-Parra AI, Wong LL, Marko CK, Stefater JA, Stryjewski TP, Eliott D, Arboleda-Velasquez JF, Kim LA. Effect of methotrexate on an in vitro patient-derived model of proliferative vitreoretinopathy. Investigative Ophthalmology and Visual Science. 2017;58:3940–3949. doi: 10.1167/iovs.16-20912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balda et al. (2000).Balda MS, Flores-Maldonado C, Cereijido M, Matter K. Multiple domains of occludin are involved in the regulation of paracellular permeability. Journal of Cellular Biochemistry. 2000;78:85–96. [PubMed] [Google Scholar]
- Balda, Garrett & Matter (2003).Balda MS, Garrett MD, Matter K. The ZO-1-associated Y-box factor ZONAB regulates epithelial cell proliferation and cell density. Journal of Cell Biology. 2003;160:423–432. doi: 10.1083/jcb.200210020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balda & Matter (2016).Balda MS, Matter K. Tight junctions as regulators of tissue remodelling. Current Opinion in Cell Biology. 2016;42:94–101. doi: 10.1016/j.ceb.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Bao et al. (2019).Bao H, Yang S, Li H, Yao H, Zhang Y, Zhang J, Xu G, Jin H, Wang F. The Interplay Between E-Cadherin, Connexin 43, and Zona Occludens 1 in Retinal Pigment Epithelial Cells. Investigative Ophthalmology and Visual Science. 2019;60:5104–5111. doi: 10.1167/iovs.19-27768. [DOI] [PubMed] [Google Scholar]
- Bastiaans et al. (2018).Bastiaans J, Mulder VC, Van Meurs JC, Smits-Te Nijenhuis M, Van Holten-Neelen C, Van Hagen PM, Dik WA. Dabigatran inhibits intravitreal thrombin activity. Acta Ophthalmologica. 2018;96:452–458. doi: 10.1111/aos.13630. [DOI] [PubMed] [Google Scholar]
- Bazzoni & Dejana (2004).Bazzoni G, Dejana E. Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiological Reviews. 2004;84:869–901. doi: 10.1152/physrev.00035.2003. [DOI] [PubMed] [Google Scholar]
- Bazzoni et al. (2000).Bazzoni G, Martinez-Estrada OM, Orsenigo F, Cordenonsi M, Citi S, Dejana E. Interaction of junctional adhesion molecule with the tight junction components ZO-1, cingulin, and occludin. Journal of Biological Chemistry. 2000;275:20520–20526. doi: 10.1074/jbc.M905251199. [DOI] [PubMed] [Google Scholar]
- Benedicto et al. (2017).Benedicto I, Lehmann GL, Ginsberg M, Nolan DJ, Bareja R, Elemento O, Salfati Z, Alam NM, Prusky GT, Llanos P, Rabbany SY, Maminishkis A, Miller SS, Rafii S, Rodriguez-Boulan E. Concerted regulation of retinal pigment epithelium basement membrane and barrier function by angiocrine factors. Nature Communications. 2017;8:15374. doi: 10.1038/ncomms15374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat et al. (2018).Bhat AA, Uppada S, Achkar IW, Hashem S, Yadav SK, Shanmugakonar M, Al-Naemi HA, Haris M, Uddin S. Tight junction proteins and signaling pathways in cancer and inflammation: a functional crosstalk. Frontiers in Physiology. 2018;9:1942. doi: 10.3389/fphys.2018.01942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boles et al. (2020).Boles NC, Fernandes M, Swigut T, Srinivasan R, Schiff L, Rada-Iglesias A, Wang Q, Saini JS, Kiehl T, Stern JH, Wysocka J, Blenkinsop TA, Temple S. Epigenomic and transcriptomic changes during human RPE EMT in a stem cell model of epiretinal membrane pathogenesis and prevention by nicotinamide. Stem Cell Reports. 2020;14:631–647. doi: 10.1016/j.stemcr.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnans, Chou & Werb (2014).Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nature Reviews Molecular Cell Biology. 2014;15:786–801. doi: 10.1038/nrm3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulloj et al. (2018).Bulloj A, Maminishkis A, Mizui M, Finnemann SC. Semaphorin4D-PlexinB1 signaling attenuates photoreceptor outer segment phagocytosis by reducing rac1 activity of RPE cells. Molecular Neurobiology. 2018;55:4320–4332. doi: 10.1007/s12035-017-0649-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caceres et al. (2017).Caceres PS, Benedicto I, Lehmann GL, Rodriguez-Boulan EJ. Directional fluid transport across organ-blood barriers: physiology and cell biology. Cold Spring Harbor Perspectives in Biology. 2017;9:a027847. doi: 10.1101/cshperspect.a027847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caceres & Rodriguez-Boulan (2020).Caceres PS, Rodriguez-Boulan E. Retinal pigment epithelium polarity in health and blinding diseases. Current Opinion in Cell Biology. 2020;62:37–45. doi: 10.1016/j.ceb.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai et al. (2018).Cai W, Yu D, Fan J, Liang X, Jin H, Liu C, Zhu M, Shen T, Zhang R, Hu W, Wei Q, Yu J. Quercetin inhibits transforming growth factor β1-induced epithelial-mesenchymal transition in human retinal pigment epithelial cells via the Smad pathway. Drug Design, Development and Therapy. 2018;12:4149–4161. doi: 10.2147/dddt.s185618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, Maiers & DeMali (2017).Campbell HK, Maiers JL, DeMali KA. Interplay between tight junctions & adherens junctions. Experimental Cell Research. 2017;358:39–44. doi: 10.1016/j.yexcr.2017.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charteris (1998).Charteris DG. Growth factors in proliferative vitreoretinopathy. British Journal of Ophthalmology. 1998;82:106. doi: 10.1136/bjo.82.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2012).Chen HC, Zhu YT, Chen SY, Tseng SC. Wnt signaling induces epithelial-mesenchymal transition with proliferation in ARPE-19 cells upon loss of contact inhibition. Laboratory Investigation. 2012;92:676–687. doi: 10.1038/labinvest.2011.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2016a).Chen X, Tzekov R, Su M, Hong H, Min W, Han A, Li W. Auranofin inhibits retinal pigment epithelium cell survival through reactive oxygen species-dependent epidermal growth factor receptor/ mitogen-activated protein kinase signaling pathway. PLOS ONE. 2016a;11:e0166386. doi: 10.1371/journal.pone.0166386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2014a).Chen X, Xiao W, Liu X, Zeng M, Luo L, Wu M, Ye S, Liu Y. Blockade of Jagged/Notch pathway abrogates transforming growth factor β2-induced epithelial-mesenchymal transition in human retinal pigment epithelium cells. Current Molecular Medicine. 2014a;14:523–534. doi: 10.2174/1566524014666140331230411. [DOI] [PubMed] [Google Scholar]
- Chen et al. (2014b).Chen X, Xiao W, Wang W, Luo L, Ye S, Liu Y. The complex interplay between ERK1/2, TGFβ/Smad, and Jagged/Notch signaling pathways in the regulation of epithelial-mesenchymal transition in retinal pigment epithelium cells. PLOS ONE. 2014b;9:e96365. doi: 10.1371/journal.pone.0096365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2016b).Chen Z, Mei Y, Lei H, Tian R, Ni N, Han F, Gan S, Sun S. LYTAK1, a TAK1 inhibitor, suppresses proliferation and epithelial-mesenchymal transition in retinal pigment epithelium cells. Molecular Medicine Reports. 2016b;14:145–150. doi: 10.3892/mmr.2016.5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2017).Chen Z, Ni N, Mei Y, Yang Z. LYTAK1 attenuates proliferation of retinal pigment epithelial cells through TGF-β-mediated epithelial-mesenchymal transition via the ERK/AKT signaling pathway. Experimental and Therapeutic Medicine. 2017;14:4951–4957. doi: 10.3892/etm.2017.5187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Shao & Li (2015).Chen Z, Shao Y, Li X. The roles of signaling pathways in epithelial-to-mesenchymal transition of PVR. Molecular Vision. 2015;21:706–710. [PMC free article] [PubMed] [Google Scholar]
- Chiba (2014).Chiba C. The retinal pigment epithelium: an important player of retinal disorders and regeneration. Experimental Eye Research. 2014;123:107–114. doi: 10.1016/j.exer.2013.07.009. [DOI] [PubMed] [Google Scholar]
- Coffee, Jiang & Rahman (2014).Coffee RE, Jiang L, Rahman SA. Proliferative vitreoretinopathy: advances in surgical management. International Ophthalmology Clinics. 2014;54:91–109. doi: 10.1097/iio.0000000000000023. [DOI] [PubMed] [Google Scholar]
- Craig et al. (2015).Craig VJ, Zhang L, Hagood JS, Owen CA. Matrix metalloproteinases as therapeutic targets for idiopathic pulmonary fibrosis. American Journal of Respiratory Cell and Molecular Biology. 2015;53:585–600. doi: 10.1165/rcmb.2015-0020TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui et al. (2019).Cui L, Lyu Y, Jin X, Wang Y, Li X, Wang J, Zhang J, Deng Z, Yang N, Zheng Z, Guo Y, Wang C, Mao R, Xu J, Gao F, Jin C, Zhang J, Tian H, Xu GT, Lu L. miR-194 suppresses epithelial-mesenchymal transition of retinal pigment epithelial cells by directly targeting ZEB1. Annals of Translational Medicine. 2019;7:751. doi: 10.21037/atm.2019.11.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deora et al. (2005).Deora AA, Philp N, Hu J, Bok D, Rodriguez-Boulan E. Mechanisms regulating tissue-specific polarity of monocarboxylate transporters and their chaperone CD147 in kidney and retinal epithelia. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:16245–16250. doi: 10.1073/pnas.0504419102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding et al. (2017).Ding X, Bai Y, Zhu X, Li T, Jin E, Huang L, Yu W, Zhao M. The effects of pleiotrophin in proliferative vitreoretinopathy. Graefes Archive for Clinical and Experimental Ophthalmology. 2017;255:873–884. doi: 10.1007/s00417-016-3582-9. [DOI] [PubMed] [Google Scholar]
- Dongre & Weinberg (2019).Dongre A, Weinberg RA. New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nature Reviews Molecular Cell Biology. 2019;20:69–84. doi: 10.1038/s41580-018-0080-4. [DOI] [PubMed] [Google Scholar]
- Dvashi et al. (2015).Dvashi Z, Goldberg M, Adir O, Shapira M, Pollack A. TGF-β1 induced transdifferentiation of rpe cells is mediated by TAK1. PLOS ONE. 2015;10:e0122229. doi: 10.1371/journal.pone.0122229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastlake et al. (2016).Eastlake K, Banerjee PJ, Angbohang A, Charteris DG, Khaw PT, Limb GA. Müller glia as an important source of cytokines and inflammatory factors present in the gliotic retina during proliferative vitreoretinopathy. Glia. 2016;64:495–506. doi: 10.1002/glia.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feist Jr et al (2014).Feist Jr RM, King CD, Morris JL, Witherspoon R, Guidry C. Myofibroblast and extracellular matrix origins in proliferative vitreoretinopathy. Graefes Archive for Clinical and Experimental Ophthalmology. 2014;252:347–357. doi: 10.1007/s00417-013-2531-0. [DOI] [PubMed] [Google Scholar]
- Feng et al. (2019).Feng H, Zhao X, Guo Q, Feng Y, Ma M, Guo W, Dong X, Deng C, Li C, Song X, Han S, Cao L. Autophagy resists EMT process to maintain retinal pigment epithelium homeostasis. International Journal of Biological Sciences. 2019;15:507–521. doi: 10.7150/ijbs.30575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrington, Sinha & Kaarniranta (2016).Ferrington DA, Sinha D, Kaarniranta K. Defects in retinal pigment epithelial cell proteolysis and the pathology associated with age-related macular degeneration. Progress in Retina and Eye Research. 2016;51:69–89. doi: 10.1016/j.preteyeres.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields et al. (2019).Fields MA, Priore LVDel, Adelman RA, Rizzolo LJ. Interactions of the choroid, Bruch’s membrane, retinal pigment epithelium, and neurosensory retina collaborate to form the outer blood-retinal-barrier. Progress in Retina and Eye Research. 2019;76:100803. doi: 10.1016/j.preteyeres.2019.100803. [DOI] [PubMed] [Google Scholar]
- Furuse et al. (1994).Furuse M, Itoh M, Hirase T, Nagafuchi A, Yonemura S, Tsukita S, Tsukita S. Direct association of occludin with ZO-1 and its possible involvement in the localization of occludin at tight junctions. Journal of Cell Biology. 1994;127:1617–1626. doi: 10.1083/jcb.127.6.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse et al. (1998).Furuse M, Sasaki H, Fujimoto K, Tsukita S. A single gene product, claudin-1 or -2, reconstitutes tight junction strands and recruits occludin in fibroblasts. The Journal of Cell Biology. 1998;143:391–401. doi: 10.1083/jcb.143.2.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamulescu et al. (2006).Gamulescu MA, Chen Y, He S, Spee C, Jin M, Ryan SJ, Hinton DR. Transforming growth factor beta2-induced myofibroblastic differentiation of human retinal pigment epithelial cells: regulation by extracellular matrix proteins and hepatocyte growth factor. Experimental Eye Research. 2006;83:212–222. doi: 10.1016/j.exer.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Garweg, Tappeiner & Halberstadt (2013).Garweg JG, Tappeiner C, Halberstadt M. Pathophysiology of proliferative vitreoretinopathy in retinal detachment. Survey of Ophthalmology. 2013;58:321–329. doi: 10.1016/j.survophthal.2012.12.004. [DOI] [PubMed] [Google Scholar]
- Georgiadis et al. (2010).Georgiadis A, Tschernutter M, Bainbridge JW, Balaggan KS, Mowat F, West EL, Munro PM, Thrasher AJ, Matter K, Balda MS, Ali RR. The tight junction associated signalling proteins ZO-1 and ZONAB regulate retinal pigment epithelium homeostasis in mice. PLOS ONE. 2010;5:e15730. doi: 10.1371/journal.pone.0015730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez & Medici (2014).Gonzalez DM, Medici D. Signaling mechanisms of the epithelial-mesenchymal transition. Science Signaling. 2014;7:re8. doi: 10.1126/scisignal.2005189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Mariscal et al. (2014).González-Mariscal L, Domínguez-Calderón A, Raya-Sandino A, Ortega-Olvera JM, Vargas-Sierra O, Martínez-Revollar G. Tight junctions and the regulation of gene expression. Seminars in Cell and Developmental Biology. 2014;36:213–223. doi: 10.1016/j.semcdb.2014.08.009. [DOI] [PubMed] [Google Scholar]
- Greene et al. (2017).Greene WA, Burke TA, Kaini RR, Por ED, Wang HC. Polarized secretion of matrix metalloproteinases and their inhibitors by retinal pigment epithelium derived from induced pluripotent stem cells during wound healing. Journal of Ocular Pharmacology and Therapeutics. 2017;33:132–140. doi: 10.1089/jop.2016.0070. [DOI] [PubMed] [Google Scholar]
- Guettler et al. (2008).Guettler S, Vartiainen MK, Miralles F, Larijani B, Treisman R. RPEL motifs link the serum response factor cofactor MAL but not myocardin to Rho signaling via actin binding. Molecular and Cellular Biology. 2008;28:732–742. doi: 10.1128/mcb.01623-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Günzel & Yu (2013).Günzel D, Yu AS. Claudins and the modulation of tight junction permeability. Physiological Reviews. 2013;93:525–569. doi: 10.1152/physrev.00019.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada, Mitamura & Harada (2006).Harada C, Mitamura Y, Harada T. The role of cytokines and trophic factors in epiretinal membranes: involvement of signal transduction in glial cells. Progress in Retina and Eye Research. 2006;25:149–164. doi: 10.1016/j.preteyeres.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Hatanaka et al. (2012).Hatanaka H, Koizumi N, Okumura N, Kay EP, Mizuhara E, Hamuro J, Kinoshita S. Epithelial-mesenchymal transition-like phenotypic changes of retinal pigment epithelium induced by TGF-β are prevented by PPAR-γ agonists. Investigative Ophthalmology and Visual Science. 2012;53:6955–6963. doi: 10.1167/iovs.12-10488. [DOI] [PubMed] [Google Scholar]
- Hazim et al. (2019).Hazim RA, Volland S, Yen A, Burgess BL, Williams DS. Rapid differentiation of the human RPE cell line, ARPE-19, induced by nicotinamide. Experimental Eye Research. 2019;179:18–24. doi: 10.1016/j.exer.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He et al. (2017).He H, Kuriyan AE, Su CW, Mahabole M, Zhang Y, Zhu YT, Flynn HW, Parel JM, Tseng SC. Inhibition of proliferation and epithelial mesenchymal transition in retinal pigment epithelial cells by heavy chain-hyaluronan/pentraxin 3. Scientific Reports. 2017;7:43736. doi: 10.1038/srep43736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He et al. (2015).He S, Barron E, Ishikawa K, Khanamiri HNazari, Spee C, Zhou P, Kase S, Wang Z, Dustin LD, Hinton DR. Inhibition of DNA methylation and methyl-CpG-binding protein 2 suppresses RPE transdifferentiation: relevance to proliferative vitreoretinopathy. Investigative Ophthalmology and Visual Science. 2015;56:5579–5589. doi: 10.1167/iovs.14-16258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffer et al. (2019).Heffer AM, Proaño J, Roztocil E, Phipps RP, Feldon SE, Huxlin KR, Sime PJ, Libby RT, Woeller CF, Kuriyan AE. The polyether ionophore salinomycin targets multiple cellular pathways to block proliferative vitreoretinopathy pathology. PLOS ONE. 2019;14:e022259. doi: 10.1371/journal.pone.0222596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinz et al. (2001).Hinz B, Celetta G, Tomasek JJ, Gabbiani G, Chaponnier C. Alpha-smooth muscle actin expression upregulates fibroblast contractile activity. Molecular Biology of the Cell. 2001;12:2730–2741. doi: 10.1091/mbc.12.9.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiscott et al. (1989).Hiscott P, Morino I, Alexander R, Grierson I, Gregor Z. Cellular components of subretinal membranes in proliferative vitreoretinopathy. Eye. 1989;3(Pt 5):606–610. doi: 10.1038/eye.1989.94. [DOI] [PubMed] [Google Scholar]
- Huang et al. (2017).Huang L, Zhang C, Su L, Song Z. GSK3β attenuates TGF-β1 induced epithelial-mesenchymal transition and metabolic alterations in ARPE-19 cells. Biochemical and Biophysical Research Communications. 2017;486:744–751. doi: 10.1016/j.bbrc.2017.03.113. [DOI] [PubMed] [Google Scholar]
- Idrees, Sridhar & Kuriyan (2019).Idrees S, Sridhar J, Kuriyan AE. Proliferative vitreoretinopathy: A review. International Ophthalmology Clinics. 2019;59:221–240. doi: 10.1097/iio.0000000000000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa et al. (2015).Ishikawa K, He S, Terasaki H, Nazari H, Zhang H, Spee C, Kannan R, Hinton DR. Resveratrol inhibits epithelial-mesenchymal transition of retinal pigment epithelium and development of proliferative vitreoretinopathy. Scientific Reports. 2015;5:16386. doi: 10.1038/srep16386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islas et al. (2002).Islas S, Vega J, Ponce L, González-Mariscal L. Nuclear localization of the tight junction protein ZO-2 in epithelial cells. Experimental Cell Research. 2002;274:138–148. doi: 10.1006/excr.2001.5457. [DOI] [PubMed] [Google Scholar]
- Itoh et al. (2007).Itoh Y, Kimoto K, Imaizumi M, Nakatsuka K. Inhibition of RhoA/Rho-kinase pathway suppresses the expression of type I collagen induced by TGF-beta2 in human retinal pigment epithelial cells. Experimental Eye Research. 2007;84:464–472. doi: 10.1016/j.exer.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Jin et al. (2002).Jin M, Barron E, He S, Ryan SJ, Hinton DR. Regulation of RPE intercellular junction integrity and function by hepatocyte growth factor. Investigative Ophthalmology and Visual Science. 2002;43:2782–2790. [PubMed] [Google Scholar]
- Jin et al. (2004).Jin M, Chen Y, He S, Ryan SJ, Hinton DR. Hepatocyte growth factor and its role in the pathogenesis of retinal detachment. Investigative Ophthalmology and Visual Science. 2004;45:323–329. doi: 10.1167/iovs.03-0355. [DOI] [PubMed] [Google Scholar]
- Jin et al. (2017).Jin Y, Chen H, Xu X, Hu Y, Wang C, Ma Z. TRAUMATIC PROLIFERATIVE VITREORETINOPATHY: clinical and histopathological observations. Retina. 2017;37:1236–1245. doi: 10.1097/iae.0000000000001350. [DOI] [PubMed] [Google Scholar]
- Kadler, Hill & Canty-Laird (2008).Kadler KE, Hill A, Canty-Laird EG. Collagen fibrillogenesis: fibronectin, integrins, and minor collagens as organizers and nucleators. Current Opinion in Cell Biology. 2008;20:495–501. doi: 10.1016/j.ceb.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri & Weinberg (2009).Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. Journal of Clinical Investigation. 2009;119:1420–1428. doi: 10.1172/jci39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaneko & Terasaki (2017).Kaneko H, Terasaki H. Biological involvement of micrornas in proliferative vitreoretinopathy. Translational Vision Science and Technology. 2017;6:5. doi: 10.1167/tvst.6.4.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, Brady & Kaiser (2015).Khan MA, Brady CJ, Kaiser RS. Clinical management of proliferative vitreoretinopathy: an update. Retina. 2015;35:165–175. doi: 10.1097/iae.0000000000000447. [DOI] [PubMed] [Google Scholar]
- Khankan et al. (2011).Khankan R, Oliver N, He S, Ryan SJ, Hinton DR. Regulation of fibronectin-EDA through CTGF domain-specific interactions with TGFβ2 and its receptor TGFβRII. Investigative Ophthalmology and Visual Science. 2011;52:5068–5078. doi: 10.1167/iovs.11-7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khristov et al. (2018).Khristov V, Wan Q, Sharma R, Lotfi M, Maminishkis A, Bharti K. Polarized Human Retinal Pigment Epithelium Exhibits Distinct Surface Proteome on Apical and Basal Plasma Membranes. Methods in Molecular Biology. 2018;1722:223–247. doi: 10.1007/978-1-4939-7553-2_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura et al. (2015).Kimura K, Orita T, Liu Y, Yang Y, Tokuda K, Kurakazu T, Noda T, Yanai R, Morishige N, Takeda A, Ishibashi T, Sonoda KH. Attenuation of EMT in RPE cells and subretinal fibrosis by an RAR-γ agonist. Journal of Molecular Medicine. 2015;93:749–758. doi: 10.1007/s00109-015-1289-8. [DOI] [PubMed] [Google Scholar]
- Lamouille, Xu & Derynck (2014).Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nature Reviews Molecular Cell Biology. 2014;15:178–196. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2020).Lee H, Hwang-Bo H, Ji SY, Kim MY, Kim SY, Park C, Hong SH, Kim GY, Song KS, Hyun JW, Choi YH. Diesel particulate matter2.5 promotes epithelial-mesenchymal transition of human retinal pigment epithelial cells via generation of reactive oxygen species. Environmental Pollution. 2020;262:114301. doi: 10.1016/j.envpol.2020.114301. [DOI] [PubMed] [Google Scholar]
- Lee, Ko & Joo (2008).Lee J, Ko M, Joo CK. Rho plays a key role in TGF-beta1-induced cytoskeletal rearrangement in human retinal pigment epithelium. Journal of Cellular Physiology. 2008;216:520–526. doi: 10.1002/jcp.21424. [DOI] [PubMed] [Google Scholar]
- Lee et al. (2010).Lee J, Moon HJ, Lee JM, Joo CK. Smad3 regulates Rho signaling via NET1 in the transforming growth factor-beta-induced epithelial-mesenchymal transition of human retinal pigment epithelial cells. Journal of Biological Chemistry. 2010;285:26618–26627. doi: 10.1074/jbc.M109.073155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee-Rivera et al. (2015).Lee-Rivera I, López E, Parrales A, Alvarez-Arce A, López-Colomé AM. Thrombin promotes the expression of Ccnd1 gene in RPE cells through the activation of converging signaling pathways. Experimental Eye Research. 2015;139:81–89. doi: 10.1016/j.exer.2015.08.001. [DOI] [PubMed] [Google Scholar]
- Lehmann et al. (2014).Lehmann GL, Benedicto I, Philp NJ, Rodriguez-Boulan E. Plasma membrane protein polarity and trafficking in RPE cells: past, present and future. Experimental Eye Research. 2014;126:5–15. doi: 10.1016/j.exer.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2014).Li H, Li M, Xu D, Zhao C, Liu G, Wang F. Overexpression of Snail in retinal pigment epithelial triggered epithelial-mesenchymal transition. Biochemical and Biophysical Research Communications. 2014;446:347–351. doi: 10.1016/j.bbrc.2014.02.119. [DOI] [PubMed] [Google Scholar]
- Li et al. (2019).Li D, Yuan D, Shen H, Mao X, Yuan S, Liu Q. Gremlin-1: an endogenous BMP antagonist induces epithelial-mesenchymal transition and interferes with redifferentiation in fetal RPE cells with repeated wounds. Molecular Vision. 2019;25:625–635. [PMC free article] [PubMed] [Google Scholar]
- Li, Zhao & He (2020).Li X, Zhao M, He S. RPE epithelial-mesenchymal transition plays a critical role in the pathogenesis of proliferative vitreoretinopathy. Annals of Translational Medicine. 2020;8:263. doi: 10.21037/atm.2020.03.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidgerwood et al. (2018).Lidgerwood GE, Morris AJ, Conquest A, Daniszewski M, Rooney LA, Lim SY, Hernández D, Liang HH, Allen P, Connell PP, Guymer RH, Hewitt AW, Pébay A. Role of lysophosphatidic acid in the retinal pigment epithelium and photoreceptors. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2018;1863:750–761. doi: 10.1016/j.bbalip.2018.04.007. [DOI] [PubMed] [Google Scholar]
- Lilien & Balsamo (2005).Lilien J, Balsamo J. The regulation of cadherin-mediated adhesion by tyrosine phosphorylation/dephosphorylation of beta-catenin. Current Opinion in Cell Biology. 2005;17:459–465. doi: 10.1016/j.ceb.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Limb et al. (1991).Limb GA, Little BC, Meager A, Ogilvie JA, Wolstencroft RA, Franks WA, Chignell AH, Dumonde DC. Cytokines in proliferative vitreoretinopathy. Eye. 1991;5(Pt 6):686–693. doi: 10.1038/eye.1991.126. [DOI] [PubMed] [Google Scholar]
- Lindsey et al. (2016).Lindsey ML, Iyer RP, Jung M, DeLeon-Pennell KY, Ma Y. Matrix metalloproteinases as input and output signals for post-myocardial infarction remodeling. Journal of Molecular and Cellular Cardiology. 2016;91:134–140. doi: 10.1016/j.yjmcc.2015.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou et al. (2002).Liou GI, Matragoon S, Samuel S, Behzadian MA, Tsai NT, Gu X, Roon P, Hunt DM, Hunt RC, Caldwell RB, Marcus DM. MAP kinase and beta-catenin signaling in HGF induced RPE migration. Molecular Vision. 2002;8:483–493. [PubMed] [Google Scholar]
- Liu et al. (2019).Liu L, Wu N, Wang Y, Zhang X, Xia B, Tang J, Cai J, Zhao Z, Liao Q, Wang J. TRPM7 promotes the epithelial-mesenchymal transition in ovarian cancer through the calcium-related PI3K /AKT oncogenic signaling. Journal of Experimental & Clinical Cancer Research. 2019;38:106. doi: 10.1186/s13046-019-1061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2009).Liu Y, Ye F, Li Q, Tamiya S, Darling DS, Kaplan HJ, Dean DC. Zeb1 represses Mitf and regulates pigment synthesis, cell proliferation, and epithelial morphology. Investigative Ophthalmology and Visual Science. 2009;50:5080–5088. doi: 10.1167/iovs.08-2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutty & McLeod (2018).Lutty GA, McLeod DS. Development of the hyaloid, choroidal and retinal vasculatures in the fetal human eye. Progress in Retinal and Eye Research. 2018;62:58–76. doi: 10.1016/j.preteyeres.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu et al. (2020).Lyu Y, Xu W, Zhang J, Li M, Xiang Q, Li Y, Tan T, Ou Q, Zhang J, Tian H, Xu JY, Jin C, Gao F, Wang J, Li W, Rong A, Lu L, Xu GT. Protein Kinase A Inhibitor H89 Attenuates Experimental Proliferative Vitreoretinopathy. Investigative Ophthalmology and Visual Science. 2020;61:1. doi: 10.1167/iovs.61.2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machemer & Laqua (1975).Machemer R, Laqua H. Pigment epithelium proliferation in retinal detachment (massive periretinal proliferation) American journal of Ophthalmology. 1975;80:1–23. doi: 10.1016/0002-9394(75)90862-4. [DOI] [PubMed] [Google Scholar]
- Maminishkis et al. (2006).Maminishkis A, Chen S, Jalickee S, Banzon T, Shi G, Wang FE, Ehalt T, Hammer JA, Miller SS. Confluent monolayers of cultured human fetal retinal pigment epithelium exhibit morphology and physiology of native tissue. Investigative Ophthalmology and Visual Science. 2006;47:3612–3624. doi: 10.1167/iovs.05-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateos et al. (2014).Mateos MV, Kamerbeek CB, Giusto NM, Salvador GA. The phospholipase D pathway mediates the inflammatory response of the retinal pigment epithelium. International Journal of Biochemistry and Cell Biology. 2014;55:119–128. doi: 10.1016/j.biocel.2014.08.016. [DOI] [PubMed] [Google Scholar]
- Matoba et al. (2017).Matoba R, Morizane Y, Shiode Y, Hirano M, Doi S, Toshima S, Araki R, Hosogi M, Yonezawa T, Shiraga F. Suppressive effect of AMP-activated protein kinase on the epithelial-mesenchymal transition in retinal pigment epithelial cells. PLOS ONE. 2017;12:e018148. doi: 10.1371/journal.pone.0181481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller et al. (2017).Miller CG, Budoff G, Prenner JL, Schwarzbauer JE. Minireview: fibronectin in retinal disease. Experimental Biology and Medicine. 2017;242:1–7. doi: 10.1177/1535370216675245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller et al. (2014).Miller CG, Pozzi A, Zent R, Schwarzbauer JE. Effects of high glucose on integrin activity and fibronectin matrix assembly by mesangial cells. Molecular Biology of the Cell. 2014;25:2342–2350. doi: 10.1091/mbc.E14-03-0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miralles et al. (2003).Miralles F, Posern G, Zaromytidou AI, Treisman R. Actin dynamics control SRF activity by regulation of its coactivator MAL. Cell. 2003;113(03):329–342. doi: 10.1016/s0092-8674(03)00278-2. [DOI] [PubMed] [Google Scholar]
- Mitry et al. (2012).Mitry D, Awan MA, Borooah S, Siddiqui MA, Brogan K, Fleck BW, Wright A, Campbell H, Singh J, Charteris DG, Yorston D. Surgical outcome and risk stratification for primary retinal detachment repair: results from the Scottish Retinal Detachment study. British Journal of Ophthalmology. 2012;96:730–734. doi: 10.1136/bjophthalmol-2011-300581. [DOI] [PubMed] [Google Scholar]
- Morescalchi et al. (2013).Morescalchi F, Duse S, Gambicorti E, Romano MR, Costagliola C, Semeraro F. Proliferative vitreoretinopathy after eye injuries: an overexpression of growth factors and cytokines leading to a retinal keloid. Mediators of Inflammation. 2013;2013:269787. doi: 10.1155/2013/269787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudhar (2020).Mudhar HS. A brief review of the histopathology of proliferative vitreoretinopathy (PVR) Eye. 2020;34:246–250. doi: 10.1038/s41433-019-0724-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassar et al. (2014).Nassar K, Grisanti S, Tura A, Lüke J, Lüke M, Soliman M, Grisanti S. A TGF-β receptor 1 inhibitor for prevention of proliferative vitreoretinopathy. Experimental Eye Research. 2014;123:72–86. doi: 10.1016/j.exer.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Naylor et al. (2019).Naylor A, Hopkins A, Hudson N, Campbell M. Tight junctions of the outer blood retina barrier. International Journal of Molecular Sciences. 2019;21(1):211. doi: 10.3390/ijms21010211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson & Nusse (2004).Nelson WJ, Nusse R. Convergence of Wnt, beta-catenin, and cadherin pathways. Science. 2004;303:1483–1487. doi: 10.1126/science.1094291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni et al. (2020).Ni Y, Qin Y, Huang Z, Liu F, Zhang S, Zhang Z. Distinct serum and vitreous inflammation-related factor profiles in patients with proliferative vitreoretinopathy. Advances in Therapy. 2020;37:2550–2559. doi: 10.1007/s12325-020-01325-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niessen (2007).Niessen CM. Tight junctions/adherens junctions: basic structure and function. Journal of Investigative Dermatology. 2007;127:2525–2532. doi: 10.1038/sj.jid.5700865. [DOI] [PubMed] [Google Scholar]
- Orlova et al. (2006).Orlova VV, Economopoulou M, Lupu F, Santoso S, Chavakis T. Junctional adhesion molecule-C regulates vascular endothelial permeability by modulating VE-cadherin-mediated cell–cell contacts. Journal of Experimental Medicine. 2006;203:2703–2714. doi: 10.1084/jem.20051730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozal et al. (2020).Ozal SA, Gurlu V, Turkekul K, Guclu H, Erdogan S. Neferine inhibits epidermal growth factor-induced proliferation and migration of retinal pigment epithelial cells through downregulating p38 MAPK and PI3K/AKT signalling. Cutaneous and Ocular Toxicology. 2020;39:97–105. doi: 10.1080/15569527.2020.1730882. [DOI] [PubMed] [Google Scholar]
- Palma-Nicolás & López-Colomé (2013).Palma-Nicolás JP, López-Colomé AM. Thrombin induces slug-mediated E-cadherin transcriptional repression and the parallel up-regulation of N-cadherin by a transcription-independent mechanism in RPE cells. Journal of Cellular Physiology. 2013;228:581–589. doi: 10.1002/jcp.24165. [DOI] [PubMed] [Google Scholar]
- Parrales et al. (2013).Parrales A, López E, Lee-Rivera I, López-Colomé AM. ERK1/2-dependent activation of mTOR/mTORC1/p70S6K regulates thrombin-induced RPE cell proliferation. Cellular Signalling. 2013;25:829–838. doi: 10.1016/j.cellsig.2012.12.023. [DOI] [PubMed] [Google Scholar]
- Pastor et al. (2016).Pastor JC, Rojas J, Pastor-Idoate S, Di Lauro S, Gonzalez-Buendia L, Delgado-Tirado S. Proliferative vitreoretinopathy: a new concept of disease pathogenesis and practical consequences. Progress in Retina and Eye Research. 2016;51:125–155. doi: 10.1016/j.preteyeres.2015.07.005. [DOI] [PubMed] [Google Scholar]
- Pei et al. (2019).Pei D, Shu X, Gassama-Diagne A, Thiery JP. Mesenchymal-epithelial transition in development and reprogramming. Nature Cell Biology. 2019;21:44–53. doi: 10.1038/s41556-018-0195-z. [DOI] [PubMed] [Google Scholar]
- Pennock et al. (2014).Pennock S, Haddock LJ, Eliott D, Mukai S, Kazlauskas A. Is neutralizing vitreal growth factors a viable strategy to prevent proliferative vitreoretinopathy? Progress in Retina and Eye Research. 2014;40:16–34. doi: 10.1016/j.preteyeres.2013.12.006. [DOI] [PubMed] [Google Scholar]
- Pennock et al. (2011).Pennock S, Rheaume MA, Mukai S, Kazlauskas A. A novel strategy to develop therapeutic approaches to prevent proliferative vitreoretinopathy. The American Journal of Pathology. 2011;179:2931–2940. doi: 10.1016/j.ajpath.2011.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal et al. (2017).Rosenthal R, Günzel D, Theune D, Czichos C, Schulzke JD, Fromm M. Water channels and barriers formed by claudins. Annals of the New York Academy of Sciences. 2017;1397:100–109. doi: 10.1111/nyas.13383. [DOI] [PubMed] [Google Scholar]
- Ruiz-Loredo, López & López-Colomé (2011).Ruiz-Loredo AY, López E, López-Colomé AM. Thrombin promotes actin stress fiber formation in RPE through Rho/ROCK-mediated MLC phosphorylation. Journal of Cellular Physiology. 2011;226:414–423. doi: 10.1002/jcp.22347. [DOI] [PubMed] [Google Scholar]
- Schiff et al. (2019).Schiff L, Boles NC, Fernandes M, Nachmani B, Gentile R, Blenkinsop TA. P38 inhibition reverses TGFβ1 and TNFα-induced contraction in a model of proliferative vitreoretinopathy. Commun Biol. 2019;2:162. doi: 10.1038/s42003-019-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi et al. (2018).Shi J, Barakat M, Chen D, Chen L. Bicellular tight junctions and wound healing. International Journal of Molecular Sciences. 2018;19(12):3862. doi: 10.3390/ijms19123862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin, Fogg & Margolis (2006).Shin K, Fogg VC, Margolis B. Tight junctions and cell polarity. Annual Review of Cell and Developmental Biology. 2006;22:207–235. doi: 10.1146/annurev.cellbio.22.010305.104219. [DOI] [PubMed] [Google Scholar]
- Shu, Butcher & Saint-Geniez (2020).Shu DY, Butcher E, Saint-Geniez M. EMT and EndMT: emerging roles in age-related macular degeneration. International Journal of Molecular Sciences. 2020;21(12):4271. doi: 10.3390/ijms21124271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu & Lovicu (2017).Shu DY, Lovicu FJ. Myofibroblast transdifferentiation: the dark force in ocular wound healing and fibrosis. Progress in Retina and Eye Research. 2017;60:44–65. doi: 10.1016/j.preteyeres.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shukal et al. (2020).Shukal D, Bhadresha K, Shastri B, Mehta D, Vasavada A, Johar K. Dichloroacetate prevents TGFβ-induced epithelial-mesenchymal transition of retinal pigment epithelial cells. Experimental Eye Research. 2020;197:108072. doi: 10.1016/j.exer.2020.108072. [DOI] [PubMed] [Google Scholar]
- Skrypek et al. (2017).Skrypek N, Goossens S, Smedt EDe, Vandamme N, Berx G. Epithelial-to-mesenchymal transition: epigenetic reprogramming driving cellular plasticity. Trends in Genetics. 2017;33:943–959. doi: 10.1016/j.tig.2017.08.004. [DOI] [PubMed] [Google Scholar]
- Sluysmans et al. (2017).Sluysmans S, Vasileva E, Spadaro D, Shah J, Rouaud F, Citi S. The role of apical cell–cell junctions and associated cytoskeleton in mechanotransduction. Biology of the Cell. 2017;109:139–161. doi: 10.1111/boc.201600075. [DOI] [PubMed] [Google Scholar]
- Sonoda et al. (2009).Sonoda S, Spee C, Barron E, Ryan SJ, Kannan R, Hinton DR. A protocol for the culture and differentiation of highly polarized human retinal pigment epithelial cells. Nature Protocols. 2009;4:662–673. doi: 10.1038/nprot.2009.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern & Temple (2015).Stern J, Temple S. Retinal pigment epithelial cell proliferation. Experimental Biology and Medicine. 2015;240:1079–1086. doi: 10.1177/1535370215587530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone et al. (2016).Stone RC, Pastar I, Ojeh N, Chen V, Liu S, Garzon KI, Tomic-Canic M. Epithelial-mesenchymal transition in tissue repair and fibrosis. Cell and Tissue Research. 2016;365:495–506. doi: 10.1007/s00441-016-2464-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss (2005).Strauss O. The retinal pigment epithelium in visual function. Physiological Reviews. 2005;85:845–881. doi: 10.1152/physrev.00021.2004. [DOI] [PubMed] [Google Scholar]
- Takahashi, Haga & Tanihara (2015).Takahashi E, Haga A, Tanihara H. Merlin regulates epithelial-to-mesenchymal transition of ARPE-19 cells via TAK1-p38MAPK-mediated activation. Investigative Ophthalmology and Visual Science. 2015;56:2449–2458. doi: 10.1167/iovs.14-16300. [DOI] [PubMed] [Google Scholar]
- Takahashi et al. (2010).Takahashi E, Nagano O, Ishimoto T, Yae T, Suzuki Y, Shinoda T, Nakamura S, Niwa S, Ikeda S, Koga H, Tanihara H, Saya H. Tumor necrosis factor-alpha regulates transforming growth factor-beta-dependent epithelial-mesenchymal transition by promoting hyaluronan-CD44-moesin interaction. Journal of Biological Chemistry. 2010;285:4060–4073. doi: 10.1074/jbc.M109.056523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiya & Kaplan (2016).Tamiya S, Kaplan HJ. Role of epithelial-mesenchymal transition in proliferative vitreoretinopathy. Experimental Eye Research. 2016;142:26–31. doi: 10.1016/j.exer.2015.02.008. [DOI] [PubMed] [Google Scholar]
- Tamiya, Liu & Kaplan (2010).Tamiya S, Liu L, Kaplan HJ. Epithelial-mesenchymal transition and proliferation of retinal pigment epithelial cells initiated upon loss of cell–cell contact. Investigative Ophthalmology and Visual Science. 2010;51:2755–2763. doi: 10.1167/iovs.09-4725. [DOI] [PubMed] [Google Scholar]
- Tan et al. (2017).Tan X, Chen C, Zhu Y, Deng J, Qiu X, Huang S, Shang F, Cheng B, Liu Y. Proteotoxic stress desensitizes TGF-beta signaling through receptor downregulation in retinal pigment epithelial cells. Current Molecular Medicine. 2017;17:189–199. doi: 10.2174/1566524017666170619113435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarau et al. (2019).Tarau IS, Berlin A, Curcio CA, Ach T. The cytoskeleton of the retinal pigment epithelium: from normal aging to age-related macular degeneration. International Journal of Molecular Sciences. 2019;20(4):3578. doi: 10.3390/ijms20143578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Retina Society Terminology Committee (1983).The Retina Society Terminology Committee The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90:121–125. doi: 10.1016/s0161-6420(83)34588-7. [DOI] [PubMed] [Google Scholar]
- Tomasek et al. (2002).Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nature Reviews Molecular Cell Biology. 2002;3:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- Tosi et al. (2014).Tosi GM, Marigliani D, Romeo N, Toti P. Disease pathways in proliferative vitreoretinopathy: an ongoing challenge. Journal of Cellular Physiology. 2014;229:1577–1583. doi: 10.1002/jcp.24606. [DOI] [PubMed] [Google Scholar]
- Traweger et al. (2003).Traweger A, Fuchs R, Krizbai IA, Weiger TM, Bauer HC, Bauer H. The tight junction protein ZO-2 localizes to the nucleus and interacts with the heterogeneous nuclear ribonucleoprotein scaffold attachment factor-B. Journal of Biological Chemistry. 2003;278:2692–2700. doi: 10.1074/jbc.M206821200. [DOI] [PubMed] [Google Scholar]
- Tsapara et al. (2010).Tsapara A, Luthert P, Greenwood J, Hill CS, Matter K, Balda MS. The RhoA activator GEF-H1/Lfc is a transforming growth factor-beta target gene and effector that regulates alpha-smooth muscle actin expression and cell migration. Molecular Biology of the Cell. 2010;21:860–870. doi: 10.1091/mbc.e09-07-0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vietor et al. (2001).Vietor I, Bader T, Paiha K, Huber LA. Perturbation of the tight junction permeability barrier by occludin loop peptides activates beta-catenin/TCF/LEF-mediated transcription. EMBO Reports. 2001;2:306–312. doi: 10.1093/embo-reports/kve066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigneswara et al. (2015).Vigneswara V, Esmaeili M, Deer L, Berry M, Logan A, Ahmed Z. Eye drop delivery of pigment epithelium-derived factor-34 promotes retinal ganglion cell neuroprotection and axon regeneration. Molecular and Cellular Neuroscience. 2015;68:212–221. doi: 10.1016/j.mcn.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2016).Wang L, Dong F, Reinach PS, He D, Zhao X, Chen X, Hu DN, Yan D. MicroRNA-182 suppresses HGF/SF-induced increases in retinal pigment epithelial cell proliferation and migration through targeting c-Met. PLOS ONE. 2016;11:e016768. doi: 10.1371/journal.pone.0167684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2019).Wang L, Lu W, Gao Y-H, Yan H-J, Pei F, Liu X-E, Zhuang H. Anluohuaxianwan alleviates carbon tetrachloride-induced hepatic fibrosis in rats through upregulation of peroxisome proliferator-activated receptor-Gamma and downregulation of nuclear factor-Kappa B/I & #954;B & #945; signaling pathway. World Journal of Traditional Chinese Medicine. 2019;5:95–103. doi: 10.4103/wjtcm.wjtcm_16_19. [DOI] [Google Scholar]
- Wang et al. (2010).Wang FE, Zhang C, Maminishkis A, Dong L, Zhi C, Li R, Zhao J, Majerciak V, Gaur AB, Chen S, Miller SS. MicroRNA-204/211 alters epithelial physiology. The FASEB Journal. 2010;24:1552–1571. doi: 10.1096/fj.08-125856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheelock & Johnson (2003).Wheelock MJ, Johnson KR. Cadulators of cellular phenotype. Annual Review of Cell and Developmental Biology. 2003;19:207–235. doi: 10.1146/annurev.cellbio.19.011102.111135. [DOI] [PubMed] [Google Scholar]
- Wickham et al. (2011).Wickham L, Ho-Yen GO, Bunce C, Wong D, Charteris DG. Surgical failure following primary retinal detachment surgery by vitrectomy: risk factors and functional outcomes. British Journal of Ophthalmology. 2011;95:1234–1238. doi: 10.1136/bjo.2010.190306. [DOI] [PubMed] [Google Scholar]
- Wubben, Besirli & Zacks (2016).Wubben TJ, Besirli CG, Zacks DN. Pharmacotherapies for retinal detachment. Ophthalmology. 2016;123:1553–1562. doi: 10.1016/j.ophtha.2016.02.040. [DOI] [PubMed] [Google Scholar]
- Xiao et al. (2014).Xiao W, Chen X, Liu X, Luo L, Ye S, Liu Y. Trichostatin A, a histone deacetylase inhibitor, suppresses proliferation and epithelial-mesenchymal transition in retinal pigment epithelium cells. Journal of Cellular and Molecular Medicine. 2014;18:646–655. doi: 10.1111/jcmm.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2020).Yang J, Antin P, Berx G, Blanpain C, Brabletz T, Bronner M, Campbell K, Cano A, Casanova J, Christofori G, Dedhar S, Derynck R, Ford HL, Fuxe J, Herreros AGarcíade, Goodall GJ, Hadjantonakis AK, Huang RJY, Kalcheim C, Kalluri R, Kang Y, Khew-Goodall Y, Levine H, Liu J, Longmore GD, Mani SA, Massagué J, Mayor R, McClay D, Mostov KE, Newgreen DF, Nieto MA, Puisieux A, Runyan R, Savagner P, Stanger B, Stemmler MP, Takahashi Y, Takeichi M, Theveneau E, Thiery JP, Thompson EW, Weinberg RA, Williams ED, Xing J, Zhou BP, Sheng G. Guidelines and definitions for research on epithelial-mesenchymal transition. Nature Reviews Molecular Cell Biology. 2020;21:341–352. doi: 10.1038/s41580-020-0237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2018).Yang X, Chung JY, Rai U, Esumi N. Cadherins in the retinal pigment epithelium (RPE) revisited: P-cadherin is the highly dominant cadherin expressed in human and mouse RPE in vivo. PLOS ONE. 2018;13:e0191279. doi: 10.1371/journal.pone.0191279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2016).Yang S, Yao H, Li M, Li H, Wang F. Long non-coding RNA MALAT1 mediates transforming growth factor beta1-induced epithelial-mesenchymal transition of retinal pigment epithelial cells. PLOS ONE. 2016;11:e0152687. doi: 10.1371/journal.pone.0152687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao et al. (2019).Yao H, Ge T, Zhang Y, Li M, Yang S, Li H, Wang F. BMP7 antagonizes proliferative vitreoretinopathy through retinal pigment epithelial fibrosis in vivo and in vitro. The FASEB Journal. 2019;33:3212–3224. doi: 10.1096/fj.201800858RR. [DOI] [PubMed] [Google Scholar]
- Yokoyama et al. (2012).Yokoyama K, Kimoto K, Itoh Y, Nakatsuka K, Matsuo N, Yoshioka H, Kubota T. The PI3K/Akt pathway mediates the expression of type I collagen induced by TGF-β2 in human retinal pigment epithelial cells. Graefes Archive for Clinical and Experimental Ophthalmology. 2012;250:15–23. doi: 10.1007/s00417-011-1766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2019).Zhang L, Dong Y, Wang Y, Gao J, Lv J, Sun J, Li M, Wang M, Zhao Z, Wang J, Xu W. Long non-coding RNAs in ocular diseases: new and potential therapeutic targets. Febs j. 2019;286:2261–2272. doi: 10.1111/febs.14827. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2018a).Zhang C, Su L, Huang L, Song ZY. GSK3β inhibits epithelial-mesenchymal transition via the Wnt/β-catenin and PI3K/Akt pathways. Int J Ophthalmol. 2018a;11:1120–1128. doi: 10.18240/ijo.2018.07.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2017).Zhang J, Yuan G, Dong M, Zhang T, Hua G, Zhou Q, Shi W. Notch signaling modulates proliferative vitreoretinopathy via regulating retinal pigment epithelial-to-mesenchymal transition. Histochemistry and Cell Biology. 2017;147:367–375. doi: 10.1007/s00418-016-1484-x. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2018b).Zhang P, Zhao G, Ji L, Yin J, Lu L, Li W, Zhou G, Chaum E, Yue J. Knockdown of survivin results in inhibition of epithelial to mesenchymal transition in retinal pigment epithelial cells by attenuating the TGFβ pathway. Biochemical and Biophysical Research Communications. 2018b;498:573–578. doi: 10.1016/j.bbrc.2018.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2018c).Zhang Y, Zhao D, Yang S, Yao H, Li M, Zhao C, Zhang J, Xu GT, Li H, Wang F. Protective effects of fucoidan on epithelial-mesenchymal transition of retinal pigment epithelial cells and progression of proliferative vitreoretinopathy. Cellular Physiology and Biochemistry. 2018c;46:1704–1715. doi: 10.1159/000489246. [DOI] [PubMed] [Google Scholar]
- Zhou et al. (2017).Zhou X, Kuang X, Long C, Liu W, Tang Y, Liu L, Liu H, He J, Huang Z, Fan Y, Zhang Q, Shen H. Curcumin inhibits proliferation and epithelial-mesenchymal transition of retinal pigment epithelial cells via multiple pathways. Current Molecular Medicine. 2017;17:312–319. doi: 10.2174/1566524017666171106115655. [DOI] [PubMed] [Google Scholar]
- Zhou et al. (2020).Zhou M, Geathers JS, Grillo SL, Weber SR, Wang W, Zhao Y, Sundstrom JM. Role of epithelial-mesenchymal transition in retinal pigment epithelium dysfunction. Frontiers in Cell and Developmental Biology. 2020;8:501. doi: 10.3389/fcell.2020.00501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou et al. (2015).Zhou RM, Wang XQ, Yao J, Shen Y, Chen SN, Yang H, Jiang Q, Yan B. Identification and characterization of proliferative retinopathy-related long noncoding RNAs. Biochemical and Biophysical Research Communications. 2015;465:324–330. doi: 10.1016/j.bbrc.2015.07.120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability: