Cardiovascular Disease in all Regions
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates by region ranged from 73.6 per 100,000 in High-income Asia Pacific to 432.3 per 100,000 in Eastern Europe in 2022. Global CVD mortality decreased by 34.9% from 1990 to 2022. Ischemic heart disease had the highest global age-standardized DALYs of all diseases at 2,275.9 per 100,000. Intracerebral hemorrhage and ischemic stroke were the next highest CVD causes for age-standardized DALYs. Age-standardized CVD prevalence ranged from 5,881.0 per 100,000 in South Asia to 11,342.6 per 100,000 in Central Asia. High systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 2,564.9 per 100,000 globally. Of all risks, household air pollution from solid fuels had the largest change in attributable age-standardized DALYs from 1990 to 2022 with a 65.1% decrease.
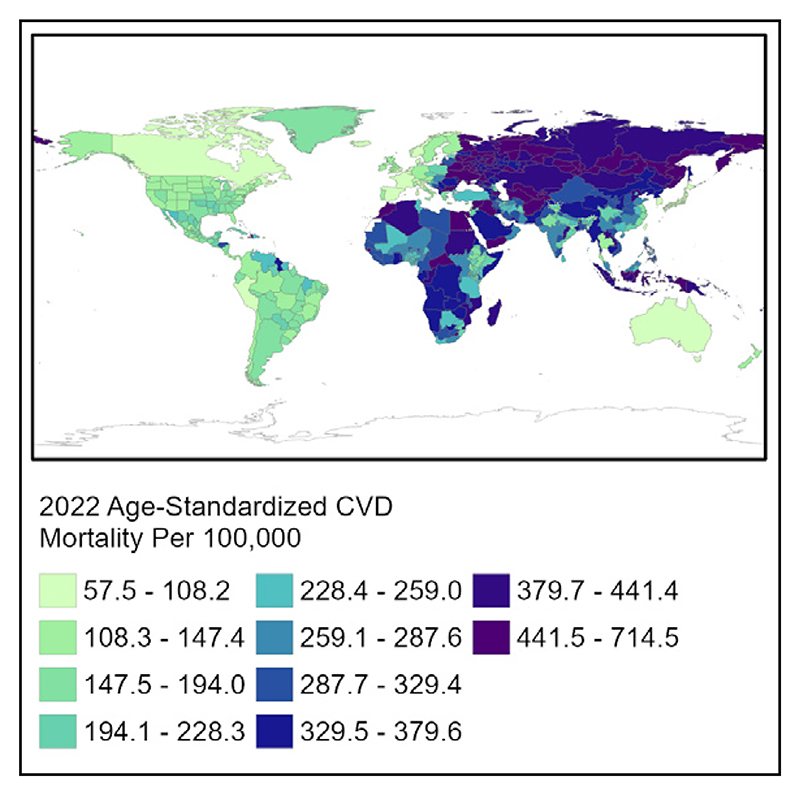
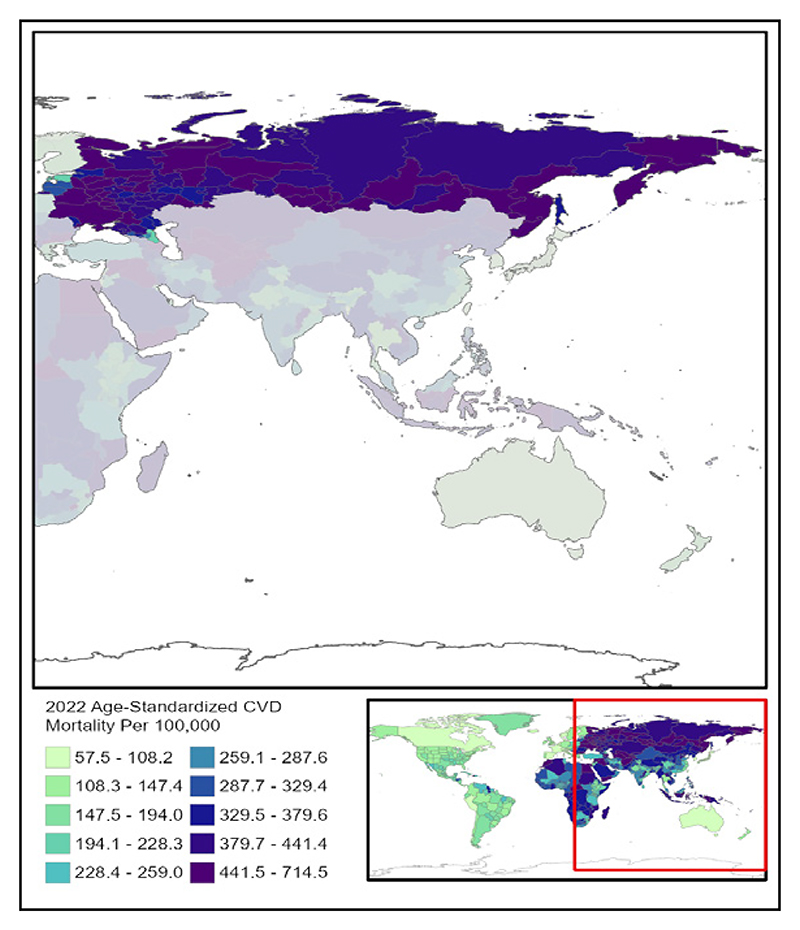
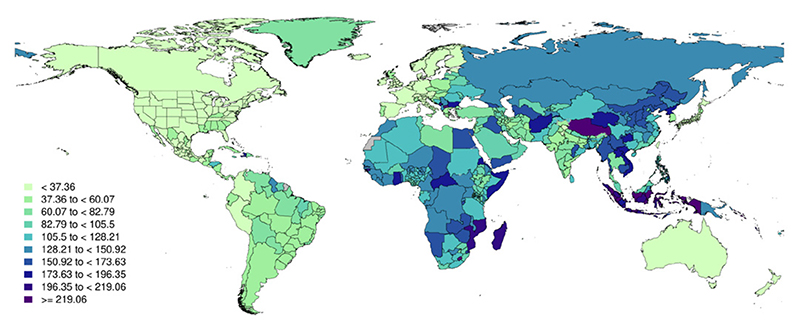
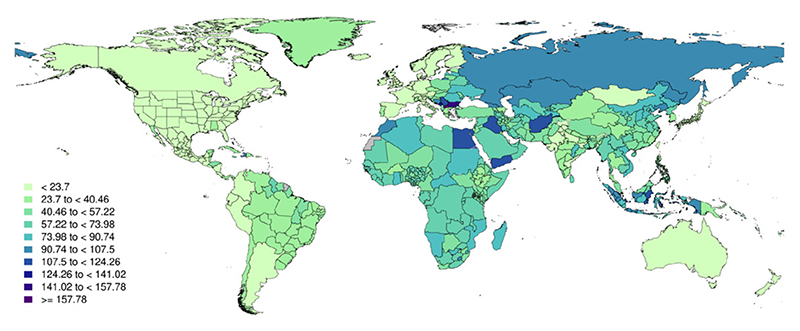
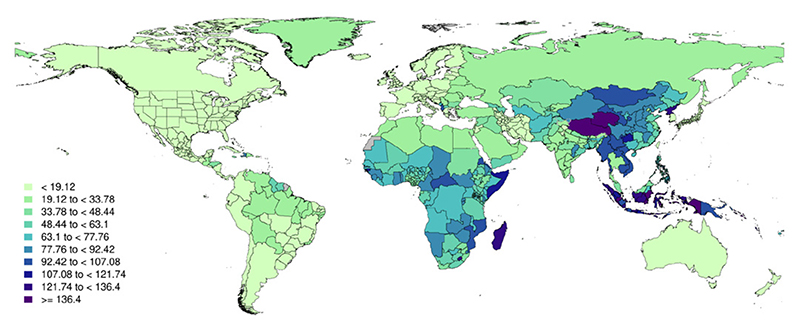
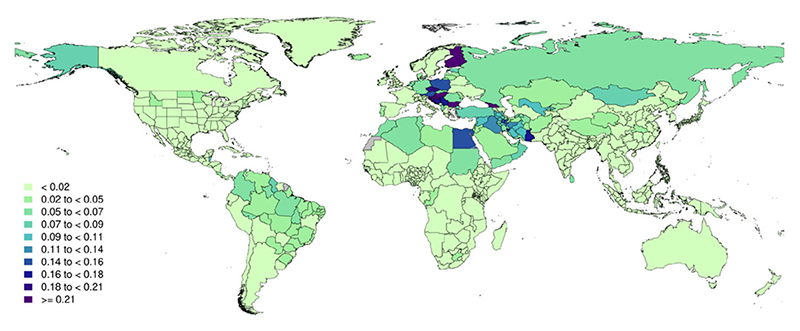
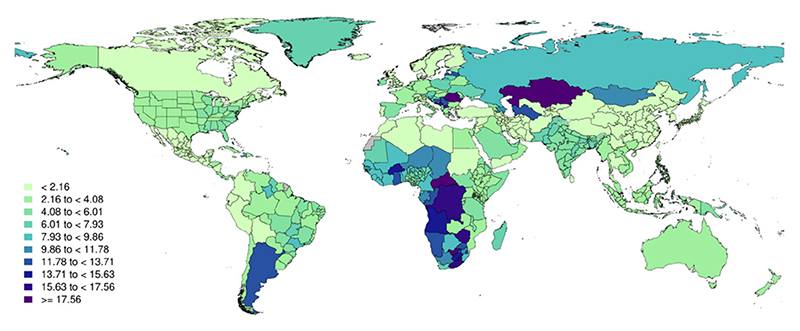
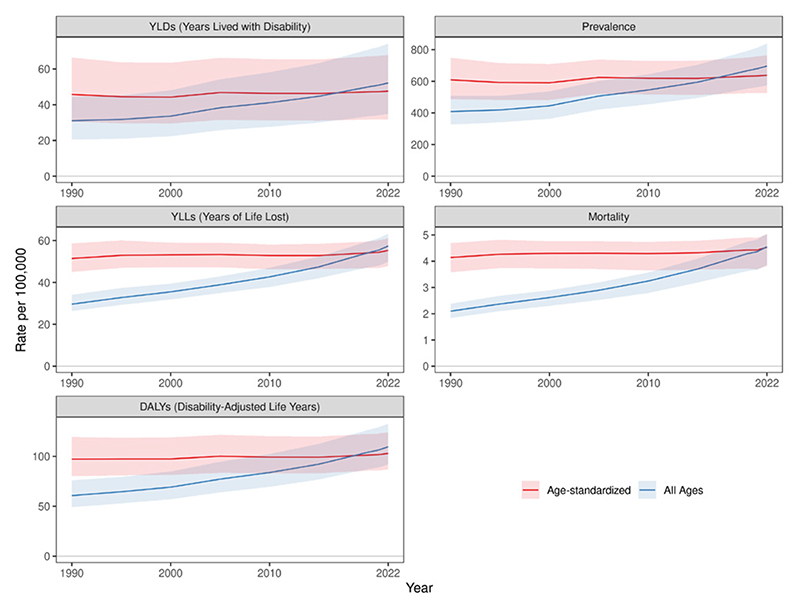
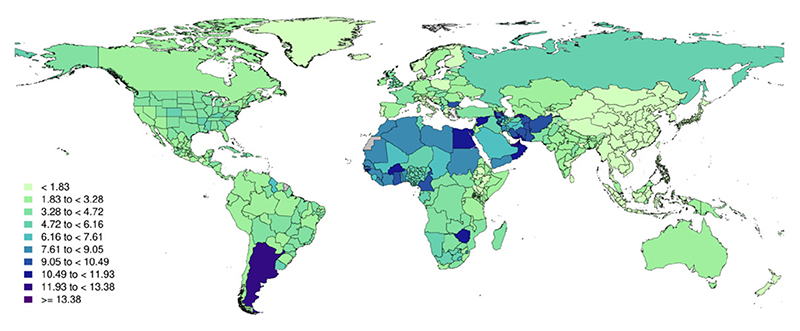
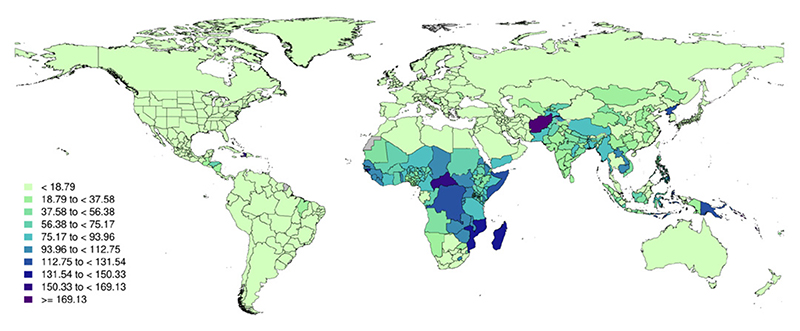
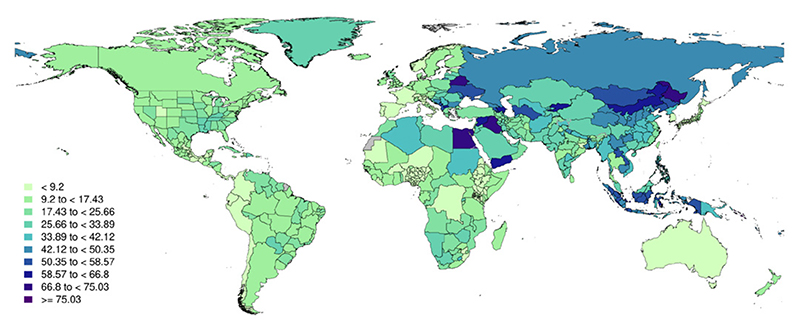
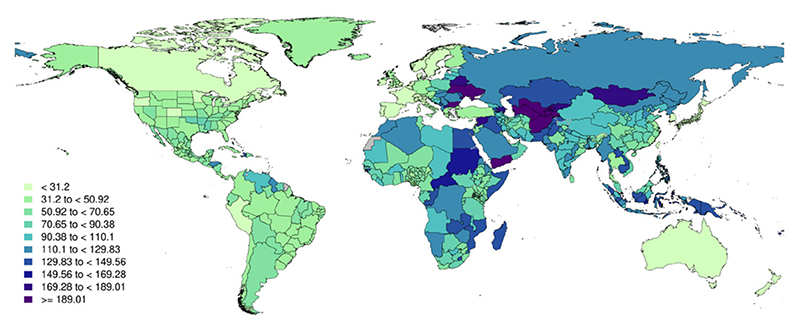
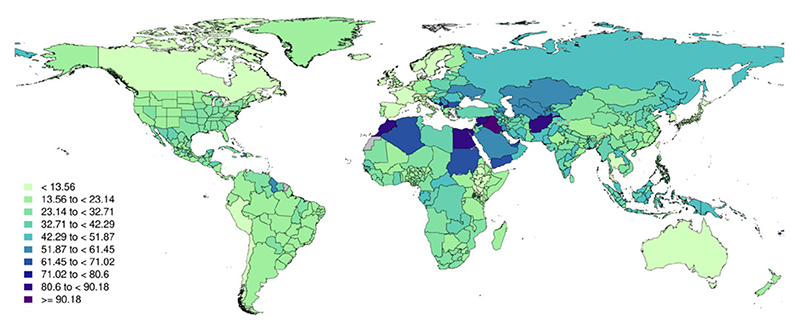
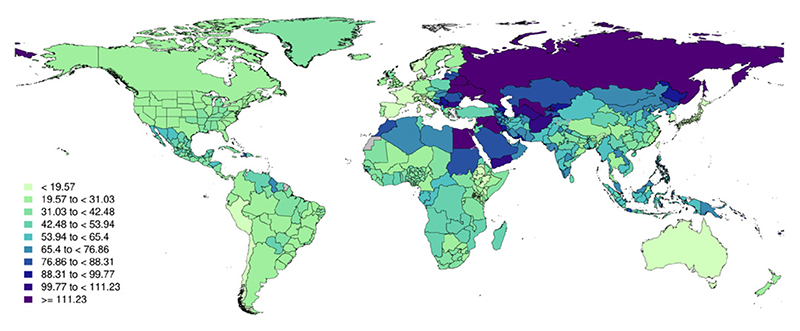
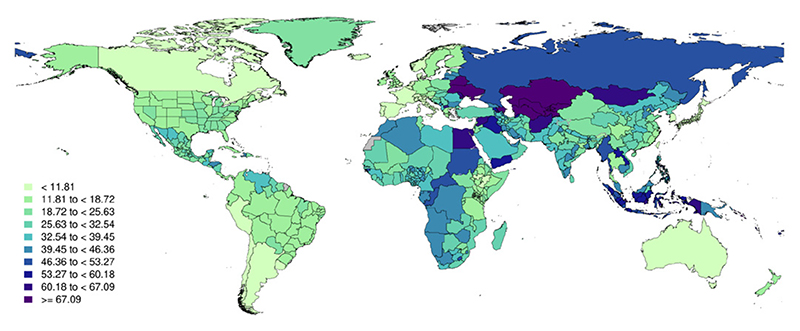
Figure 1.
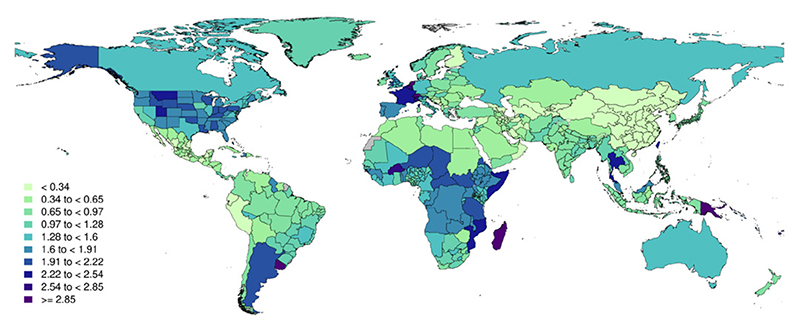
Global map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
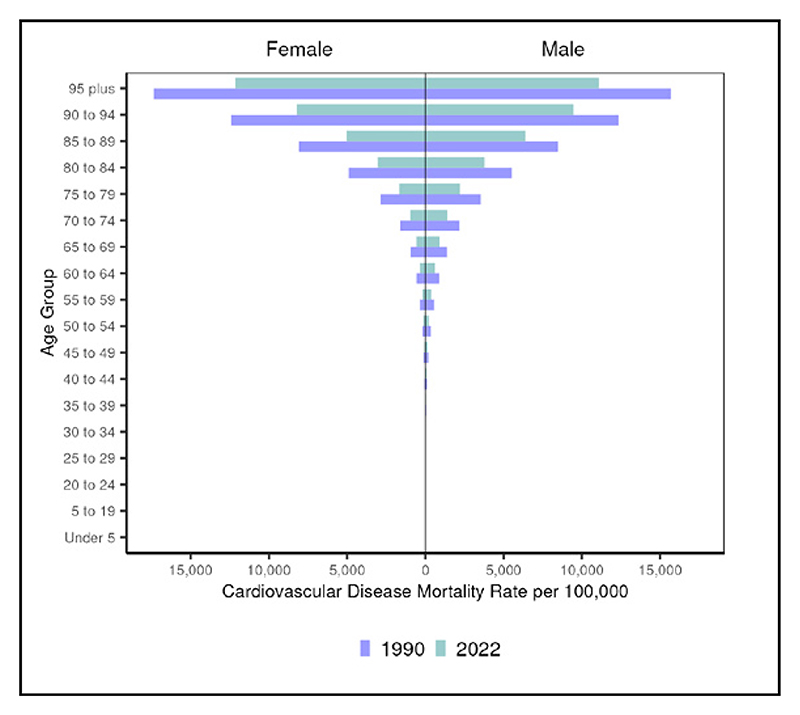
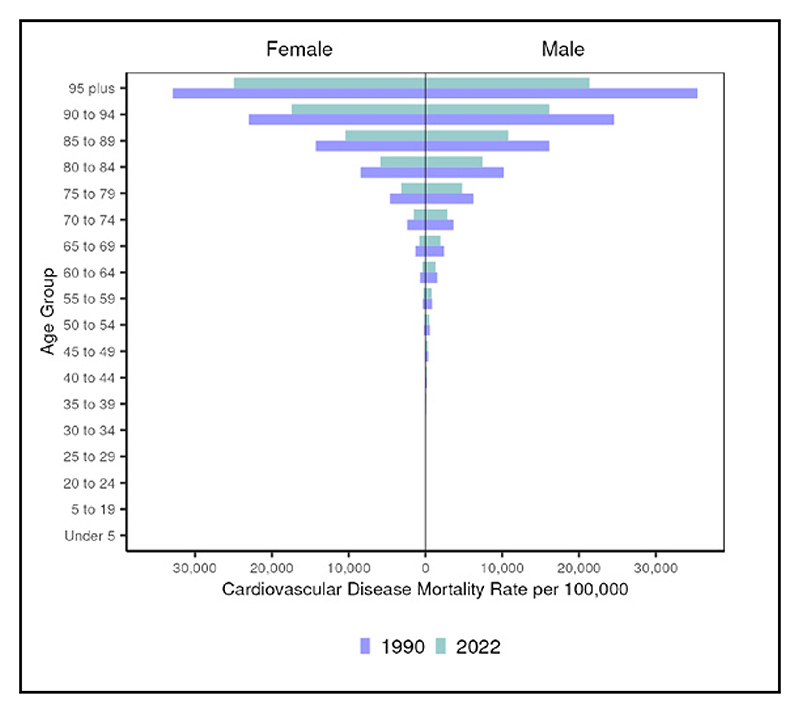
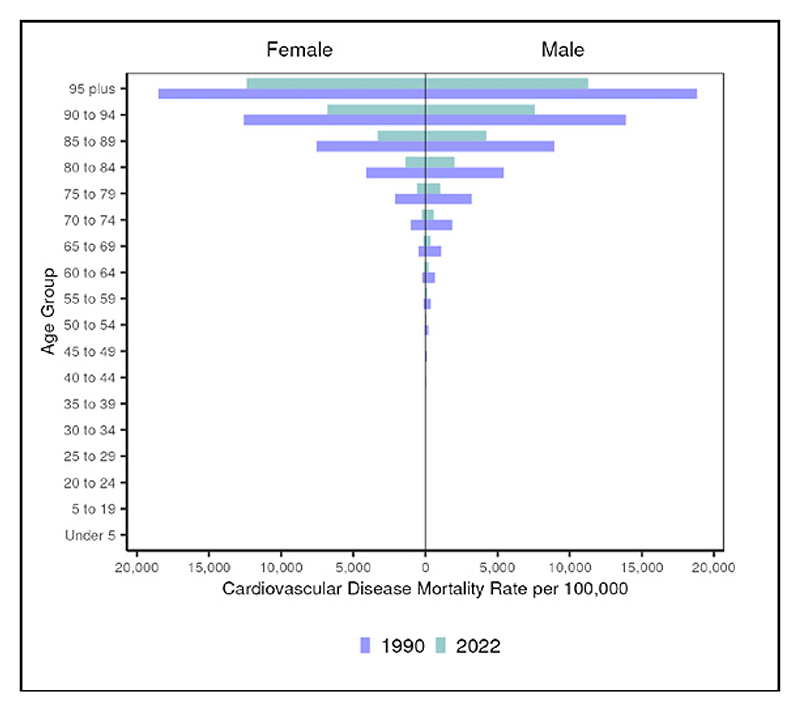
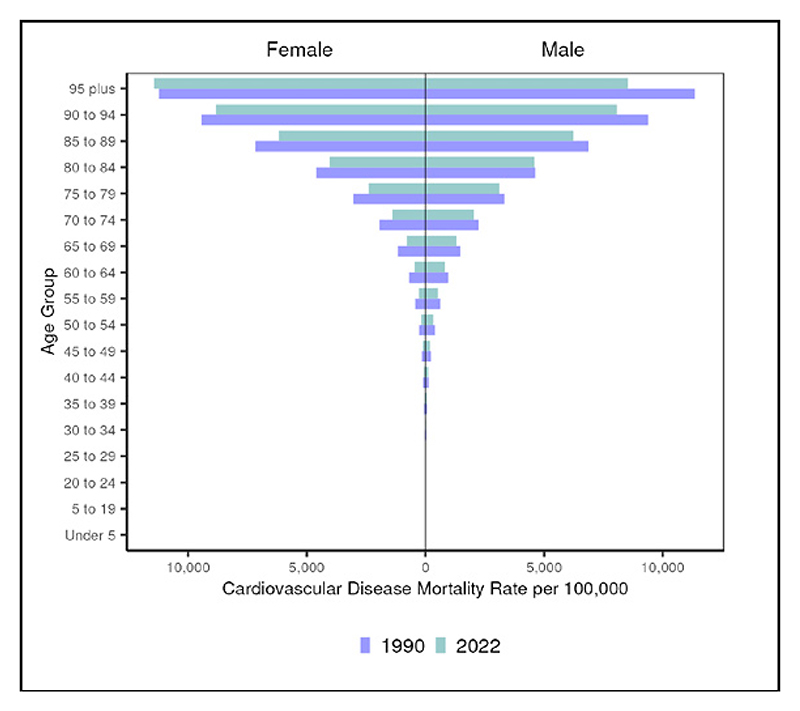
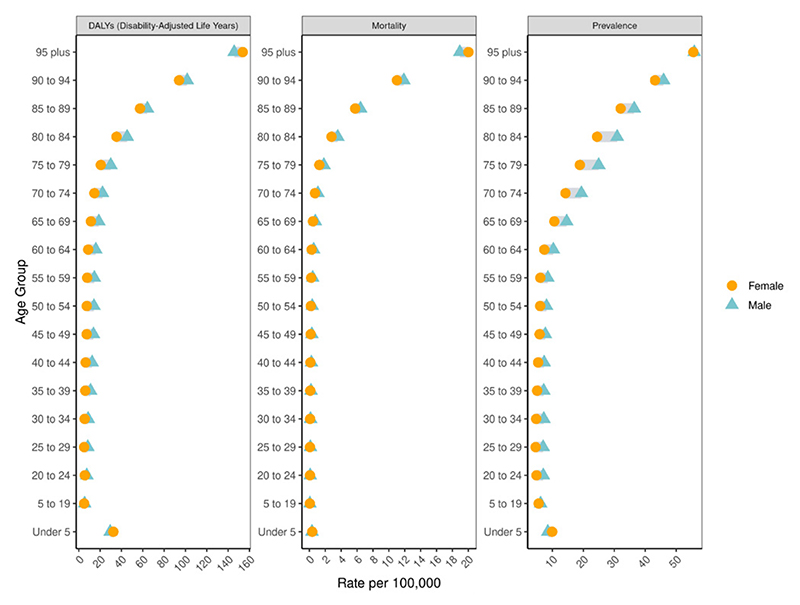
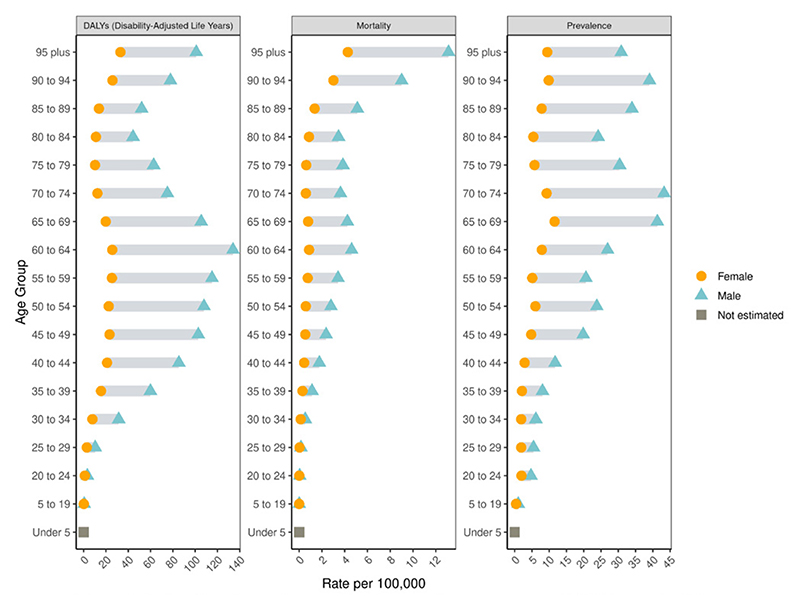
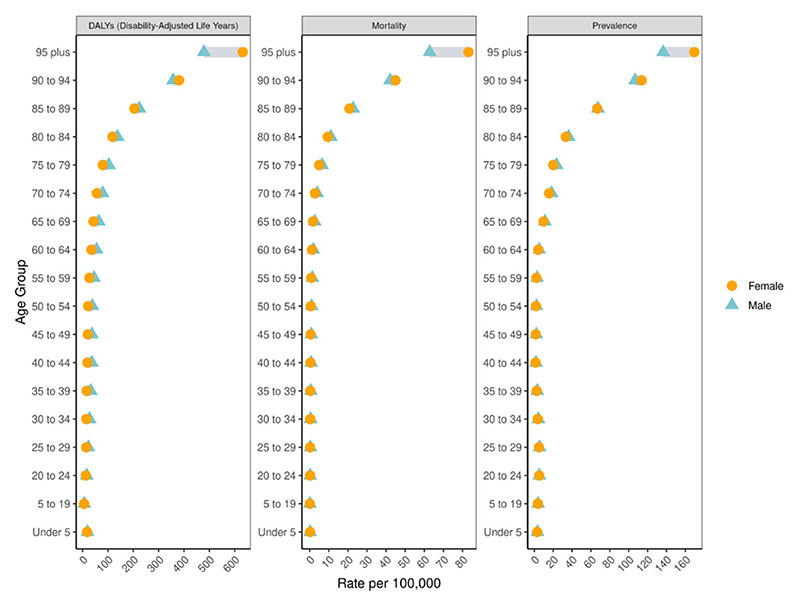
Figure 2.
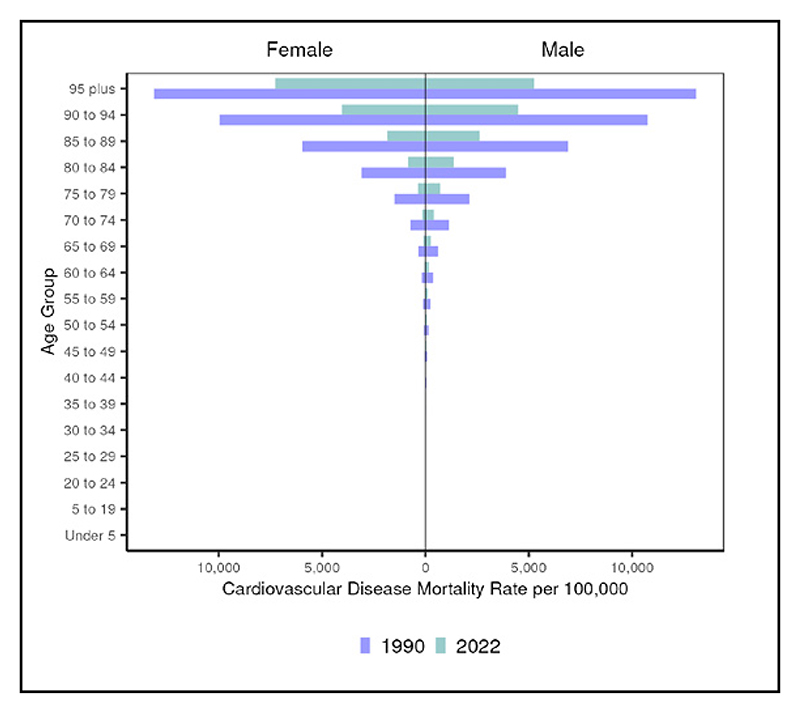
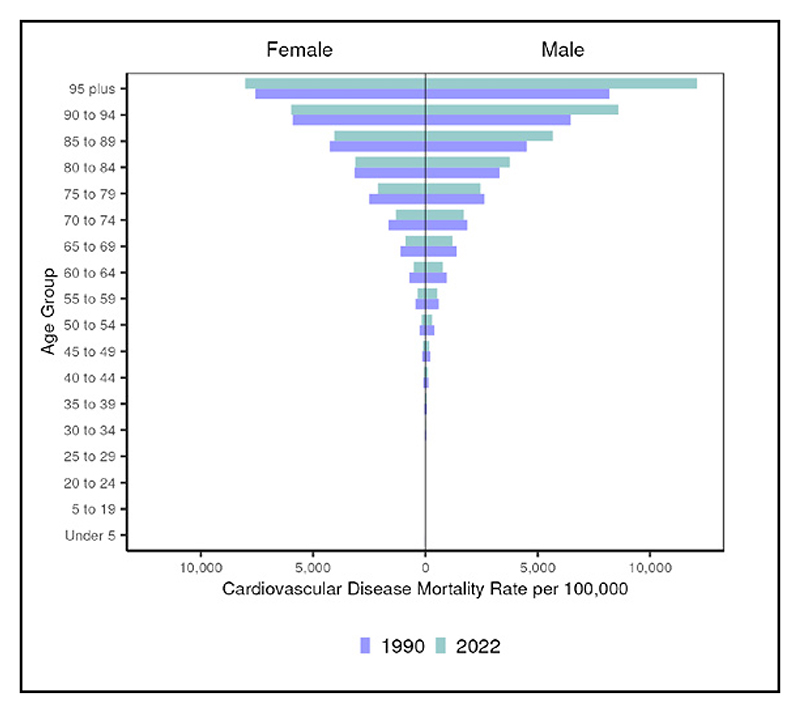
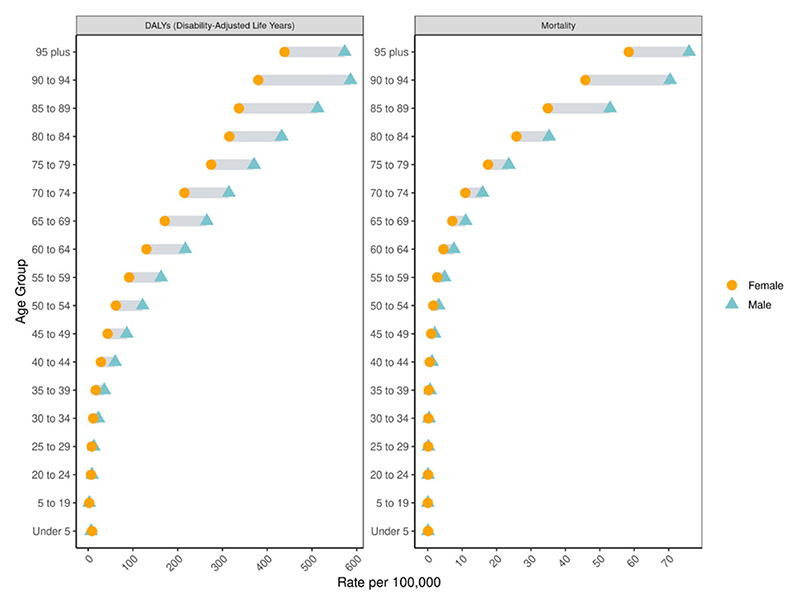
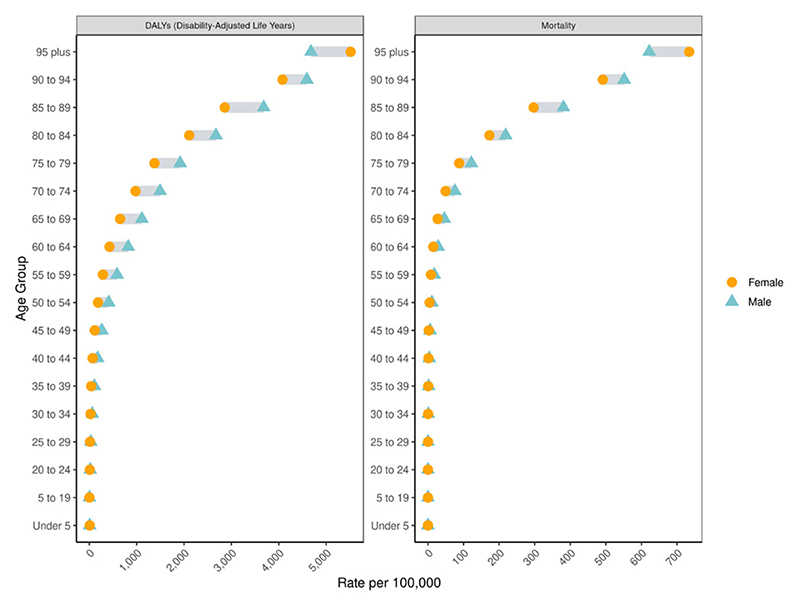
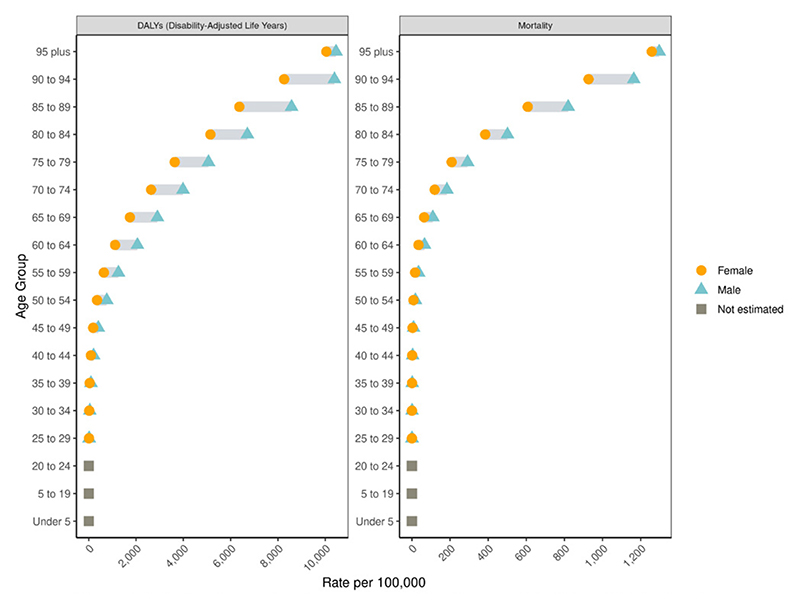
Global cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
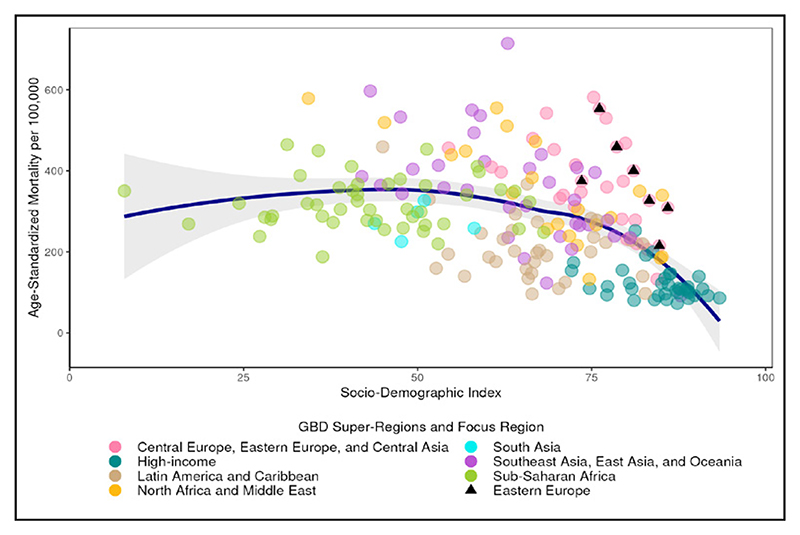
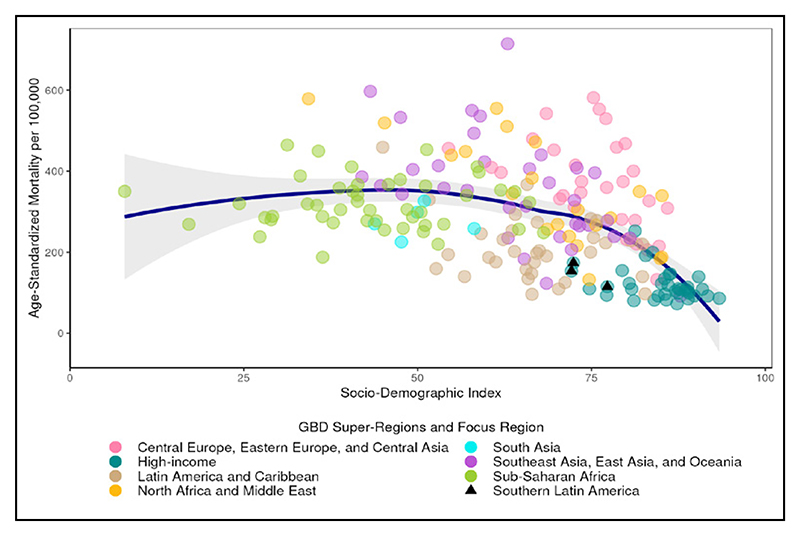
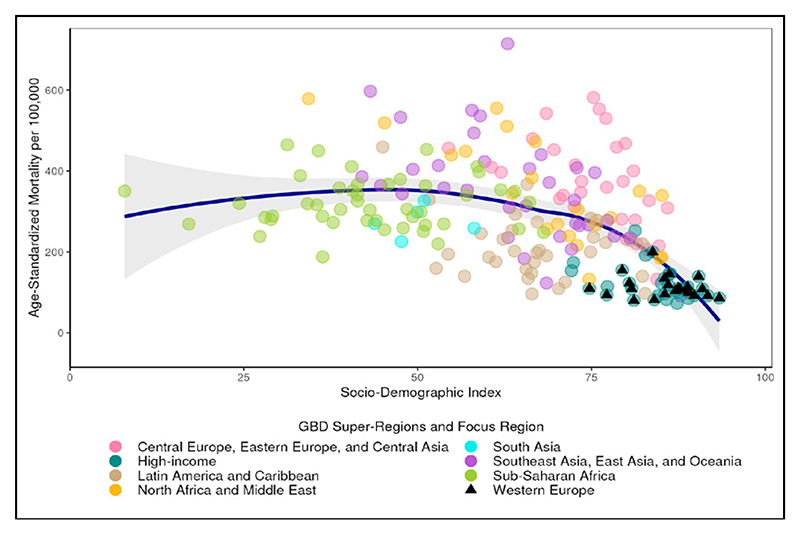
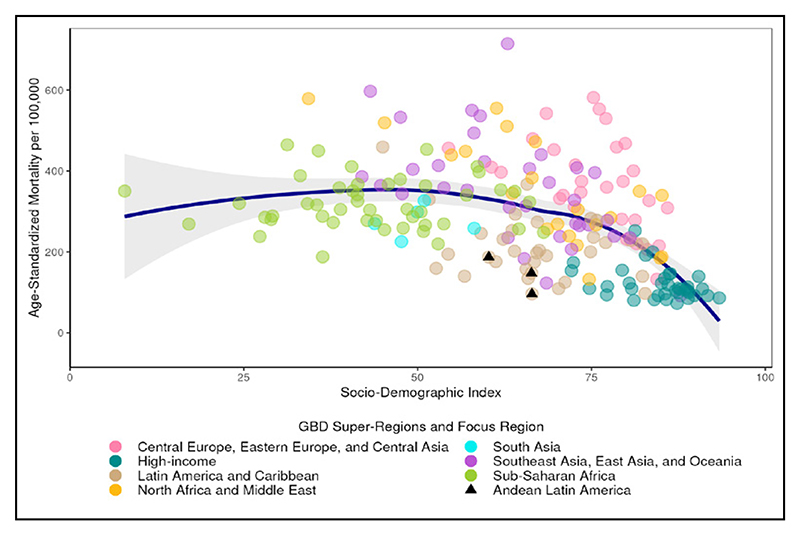
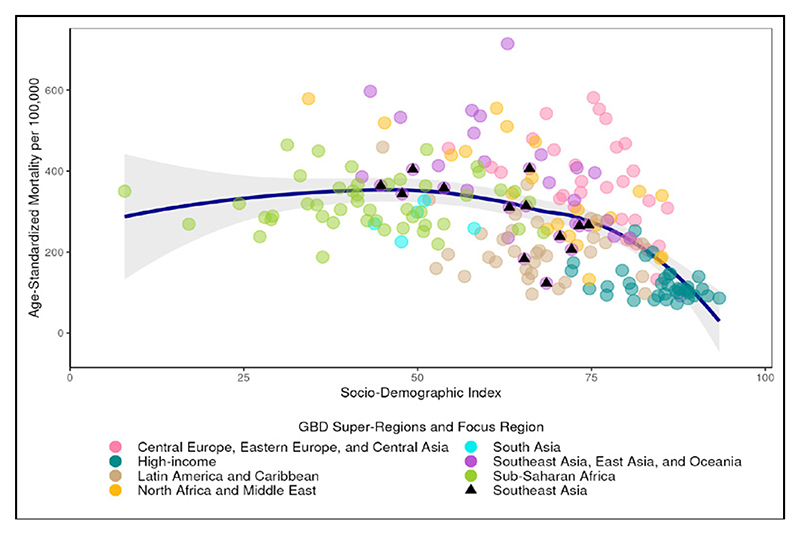
Figure 3.
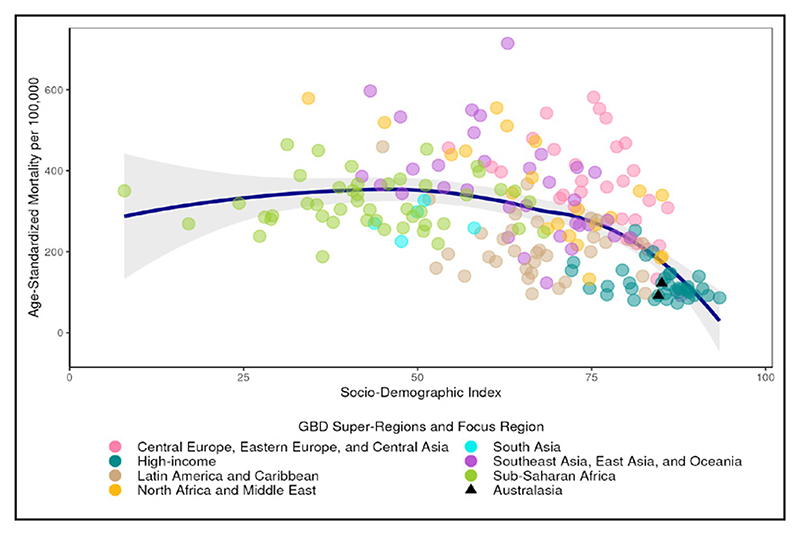
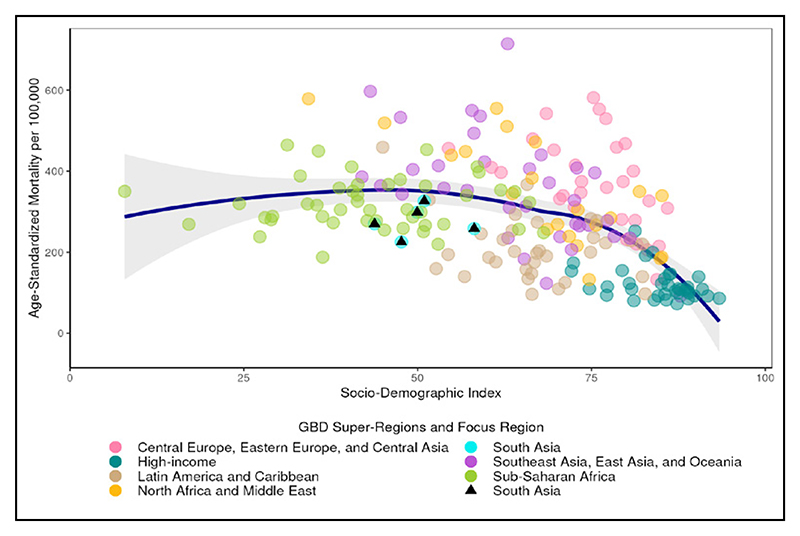
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Global estimate indicated by a triangle, loess line in blue with shaded 95% uncertainty interval.
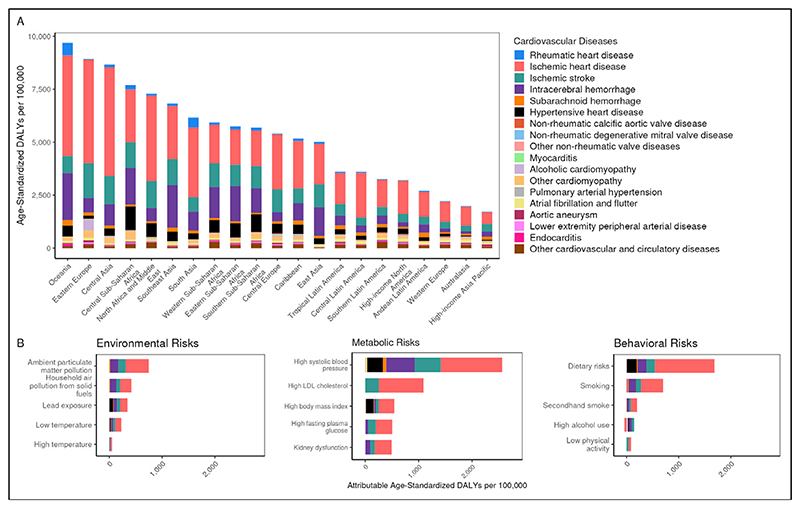
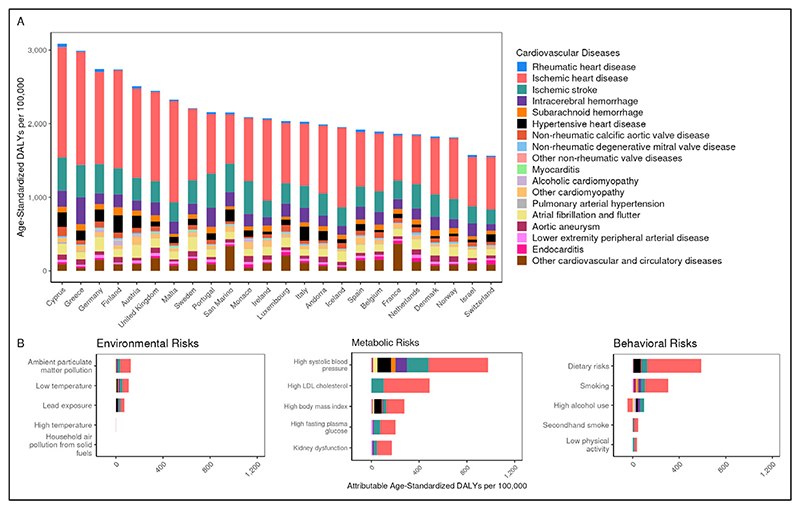
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by region and (B) burden attributable to selected risk factors, globally, compared to the theoretical minimum risk exposure level
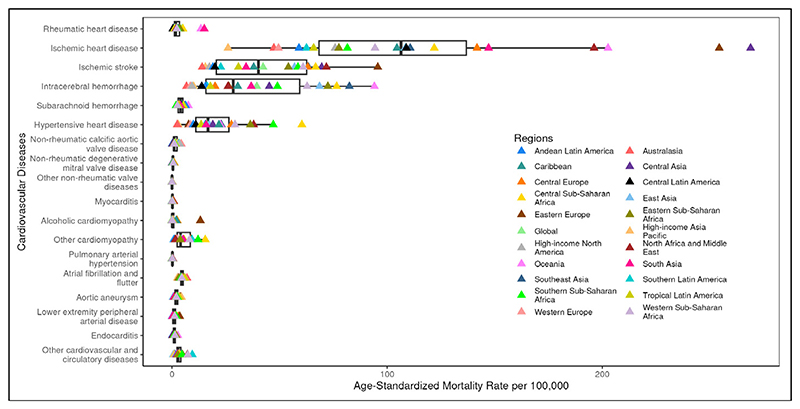
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and region. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Global cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 46,358,651 | 386,947 | 575.5 | 4.5 | 162.5 |
| Ischemic heart disease | 315,390,626 | 9,239,181 | 3,610.2 | 108.8 | 2,275.9 |
| Ischemic stroke | 86,661,746 | 3,542,299 | 994.5 | 42.3 | 819.5 |
| Intracerebral hemorrhage | 20,509,587 | 3,428,876 | 237.9 | 39.4 | 923.8 |
| Subarachnoid hemorrhage | 9,281,913 | 344,872 | 107.2 | 4.0 | 120.7 |
| Hypertensive heart disease | 13,052,641 | 1,353,074 | 150.9 | 16.1 | 292.7 |
| Non-rheumatic calcific aortic valve disease | 13,551,699 | 146,199 | 156.6 | 1.8 | 26.8 |
| Non-rheumatic degenerative mitral valve disease | 15,592,046 | 37,843 | 177.9 | 0.5 | 11.1 |
| Other non-rheumatic valve diseases | 12,130 | 2,033 | 0.1 | <0.1 | 0.6 |
| Myocarditis | 625,129 | 26,702 | 7.8 | 0.3 | 11.8 |
| Alcoholic cardiomyopathy | 554,214 | 62,661 | 6.3 | 0.7 | 24.6 |
| Other cardiomyopathy | 4,715,332 | 295,751 | 58.7 | 3.5 | 99.3 |
| Pulmonary arterial hypertension | 193,710 | 20,561 | 2.3 | 0.2 | 7.4 |
| Atrial fibrillation and flutter | 55,414,434 | 362,381 | 637.5 | 4.5 | 102.9 |
| Aortic aneurysm | Not estimated | 153,118 | Not estimated | 1.8 | 34.6 |
| Lower extremity peripheral arterial disease | 105,980,247 | 73,928 | 1,213.3 | 0.9 | 19.6 |
| Endocarditis | 438,374 | 82,402 | 5.4 | 1.0 | 25.8 |
| Other cardiovascular and circulatory diseases | 86,722,785 | 221,797 | 1,006.1 | 2.6 | 118.8 |
Cardiovascular Disease in Central Asia
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Central Asia ranged from 331.8 to 542.3 per 100,000 in 2022. CVD mortality decreased by 16.5% from 1990 to 2022. Of the 21 regions, Central Asia ranked 4th in 1990 and 2nd in 2022 for age-standardized CVD mortality, and 1st in CVD age-standardized prevalence in 2022. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 337.4 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 4,875.3 per 100,000.
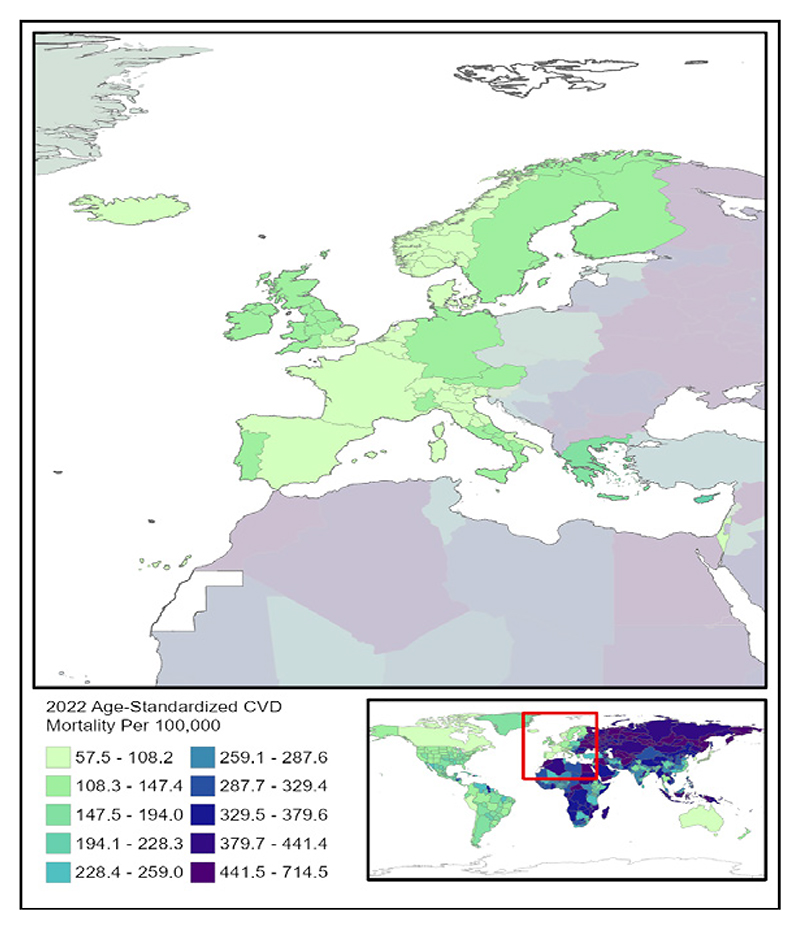
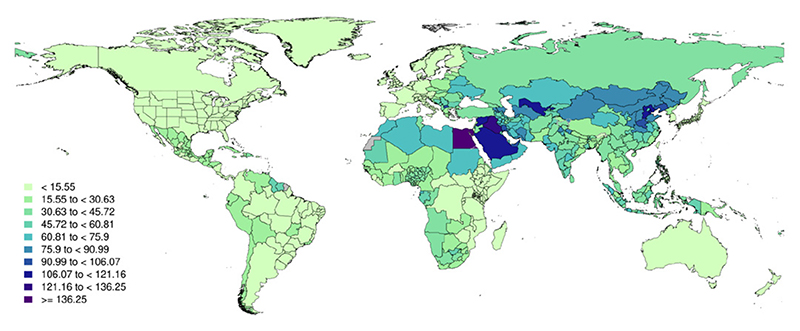
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
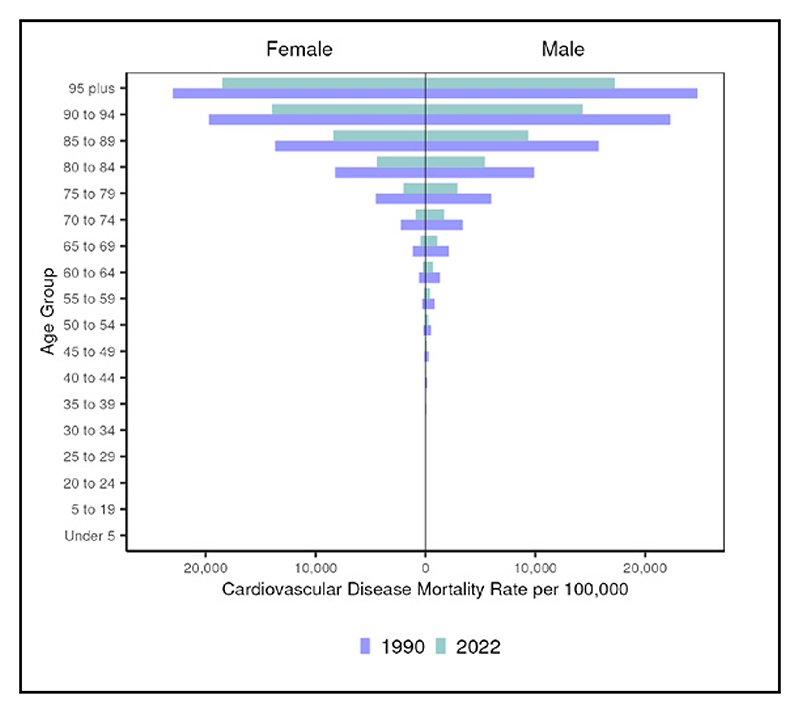
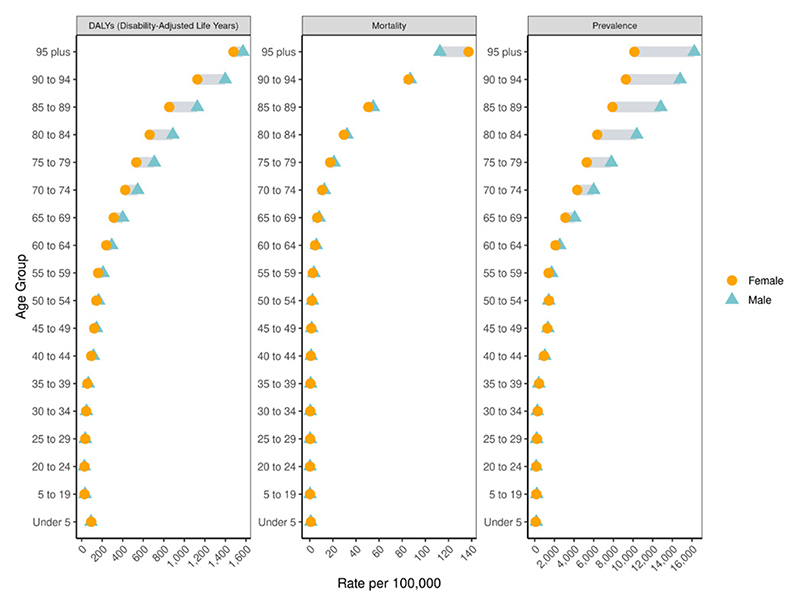
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
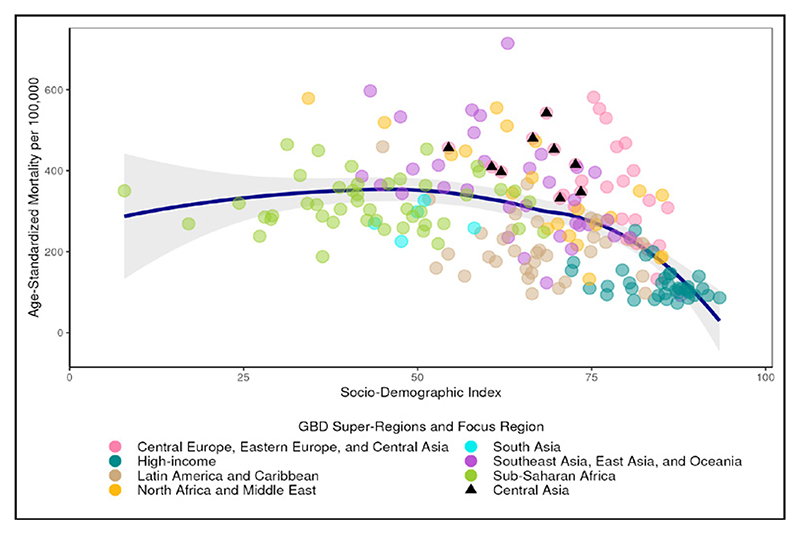
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
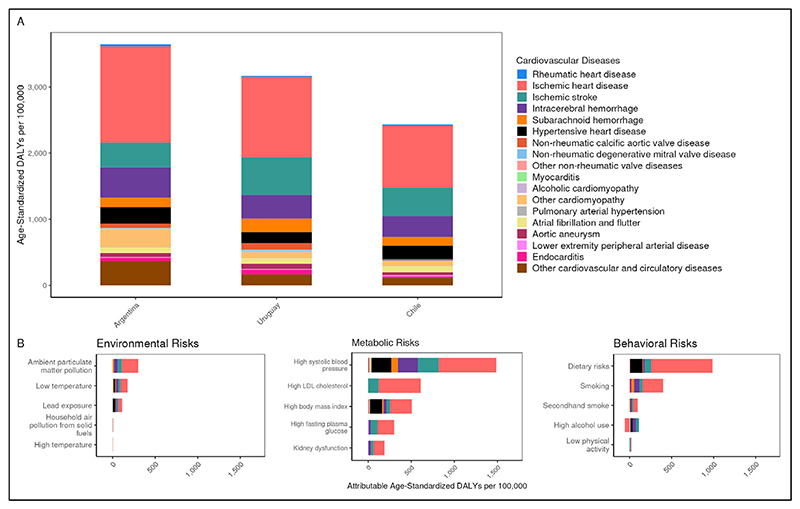
Figure 4.
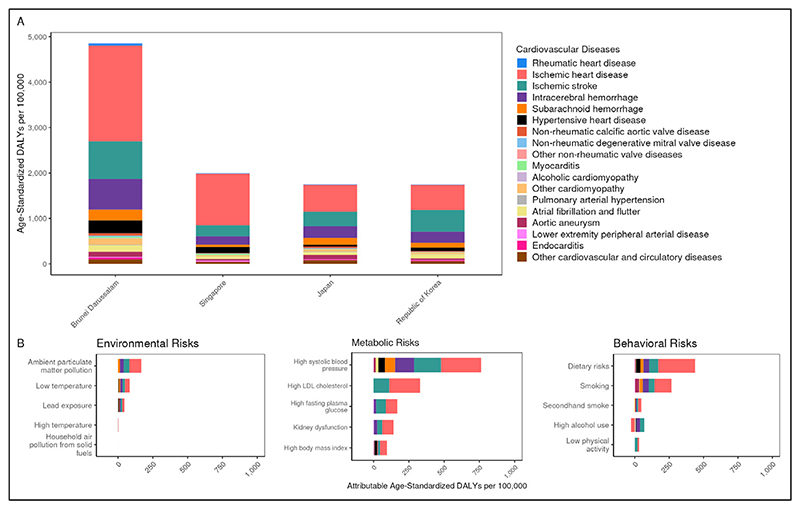
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
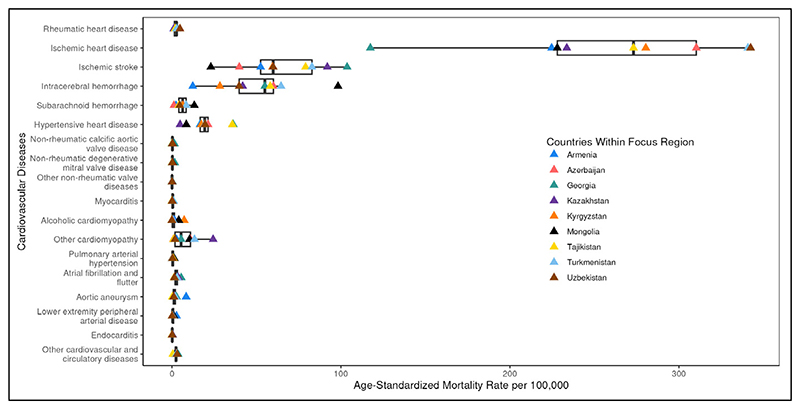
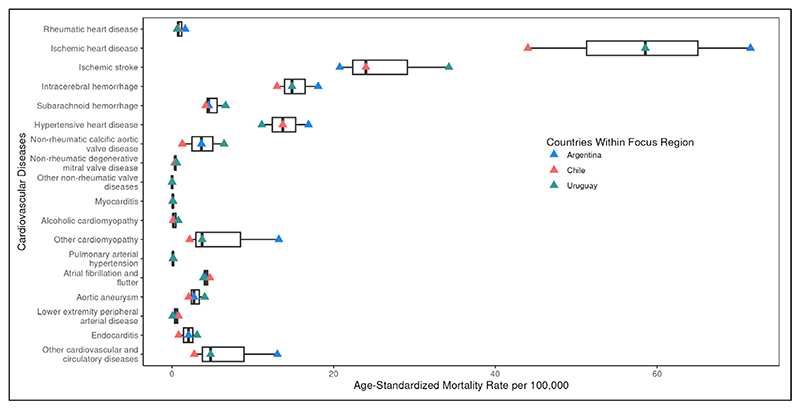
Figure 5.
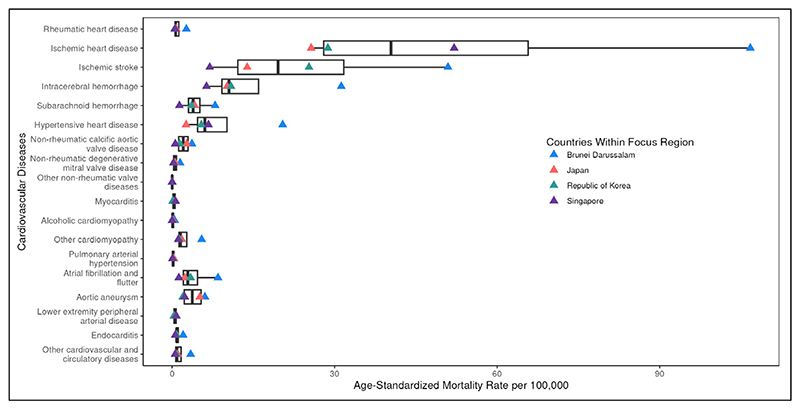
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 618,471 | 2,480 | 624.3 | 2.8 | 119.3 |
| Ischemic heart disease | 7,125,865 | 182,604 | 8,573.3 | 268.9 | 5,135.8 |
| Ischemic stroke | 951,108 | 45,226 | 1,091.5 | 69.6 | 1,330.9 |
| Intracerebral hemorrhage | 184,547 | 34,154 | 194.0 | 45.2 | 1,008.4 |
| Subarachnoid hemorrhage | 102,912 | 4,109 | 109.7 | 5.2 | 147.4 |
| Hypertensive heart disease | 71,919 | 12,724 | 96.4 | 19.0 | 337.4 |
| Non-rheumatic calcific aortic valve disease | 117,564 | 236 | 147.0 | 0.3 | 8.5 |
| Non-rheumatic degenerative mitral valve disease | 375,266 | 246 | 500.0 | 0.3 | 14.7 |
| Other non-rheumatic valve diseases | 220 | 54 | 0.3 | 0.1 | 1.8 |
| Myocarditis | 6,279 | 303 | 6.8 | 0.3 | 12.0 |
| Alcoholic cardiomyopathy | 5,279 | 861 | 5.5 | 0.9 | 32.5 |
| Other cardiomyopathy | 54,216 | 7,598 | 60.3 | 8.7 | 272.5 |
| Pulmonary arterial hypertension | 2,208 | 330 | 2.3 | 0.4 | 13.1 |
| Atrial fibrillation and flutter | 424,061 | 1,571 | 565.6 | 2.6 | 79.6 |
| Aortic aneurysm | Not estimated | 1,326 | Not estimated | 1.8 | 37.9 |
| Lower extremity peripheral arterial disease | 612,533 | 349 | 835.5 | 0.5 | 13.2 |
| Endocarditis | 854 | 177 | 0.9 | 0.2 | 7.5 |
| Other cardiovascular and circulatory diseases | 427,924 | 2,008 | 497.1 | 2.6 | 90.7 |
Cardiovascular Disease in Central Europe
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Central Europe ranged from 132.6 to 581.4 per 100,000 in 2022; a 4.4 fold difference. CVD mortality decreased by 47.0% from 1990 to 2022. Out of the 21 regions, Central Europe was ranked 2nd in 1990 and 7th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 444.3 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable agestandardized CVD DALYs at 2,963.3 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
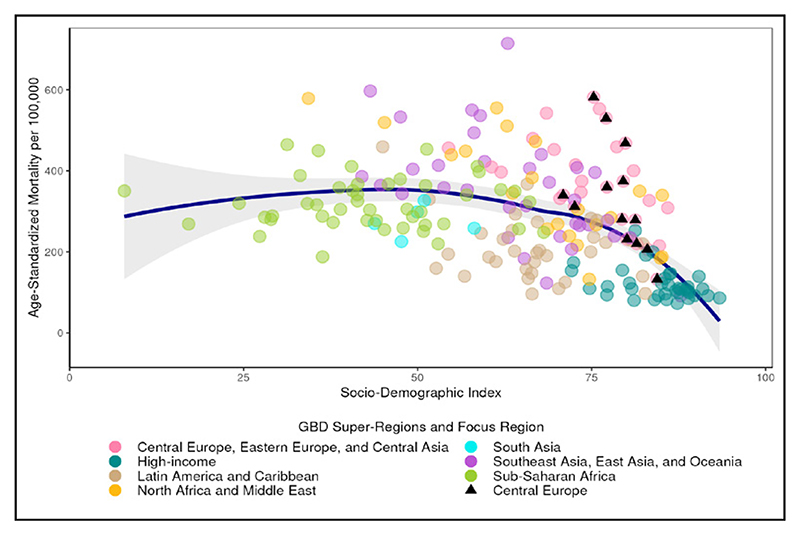
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 63,222 | 2,976 | 30.7 | 1.3 | 30.7 |
| Ischemic heart disease | 12,141,290 | 338,314 | 5,430.8 | 141.8 | 2,601.9 |
| Ischemic stroke | 1,841,834 | 155,795 | 853.9 | 63.1 | 1,063.1 |
| Intracerebral hemorrhage | 193,385 | 46,002 | 121.7 | 20.0 | 443.8 |
| Subarachnoid hemorrhage | 177,955 | 7,020 | 108.0 | 3.4 | 114.2 |
| Hypertensive heart disease | 356,261 | 66,782 | 151.7 | 27.6 | 444.3 |
| Non-rheumatic calcific aortic valve disease | 869,200 | 6,517 | 377.5 | 2.7 | 49.2 |
| Non-rheumatic degenerative mitral valve disease | 677,172 | 2,486 | 288.1 | 1.1 | 24.2 |
| Other non-rheumatic valve diseases | 1,303 | 347 | 0.8 | 0.2 | 3.1 |
| Myocarditis | 12,887 | 1,594 | 11.1 | 0.8 | 19.7 |
| Alcoholic cardiomyopathy | 42,646 | 4,804 | 25.2 | 2.4 | 71.9 |
| Other cardiomyopathy | 160,289 | 20,028 | 95.7 | 8.6 | 169.5 |
| Pulmonary arterial hypertension | 3,515 | 445 | 2.3 | 0.2 | 6.1 |
| Atrial fibrillation and flutter | 1,412,498 | 12,606 | 604.9 | 5.1 | 111.8 |
| Aortic aneurysm | Not estimated | 6,482 | Not estimated | 2.8 | 61.7 |
| Lower extremity peripheral arterial disease | 2,227,532 | 7,116 | 942.2 | 2.9 | 50.4 |
| Endocarditis | 6,884 | 1,351 | 5.9 | 0.7 | 20.5 |
| Other cardiovascular and circulatory diseases | 1,879,255 | 6,875 | 951.1 | 3.1 | 118.1 |
Cardiovascular Disease in Eastern Europe
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Eastern Europe ranged from 215.0 to 553.0 per 100,000 in 2022; a 2.6 fold difference. CVD mortality decreased by 24.3% from 1990 to 2022. Out of the 21 regions, Eastern Europe was ranked 1st in both 1990 and 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, alcoholic cardiomyopathy had the highest age-standardized DALYs in 2022 at 521.2 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 4,619.4 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 241,126 | 3,324 | 73.9 | 1.0 | 28.6 |
| Ischemic heart disease | 25,389,496 | 914,066 | 7,243.7 | 254.3 | 4,882.7 |
| Ischemic stroke | 3,074,246 | 348,195 | 924.7 | 95.7 | 1,642.8 |
| Intracerebral hemorrhage | 467,843 | 90,934 | 159.3 | 26.4 | 680.1 |
| Subarachnoid hemorrhage | 317,276 | 16,751 | 108.9 | 5.0 | 154.7 |
| Hypertensive heart disease | 171,771 | 27,760 | 46.8 | 7.7 | 138.5 |
| Non-rheumatic calcific aortic valve disease | 963,872 | 2,470 | 266.4 | 0.7 | 19.2 |
| Non-rheumatic degenerative mitral valve disease | 949,952 | 832 | 259.7 | 0.2 | 9.6 |
| Other non-rheumatic valve diseases | 395 | 131 | 0.2 | <0.1 | 1.3 |
| Myocarditis | 17,479 | 743 | 7.7 | 0.2 | 8.6 |
| Alcoholic cardiomyopathy | 177,153 | 38,801 | 63.6 | 13.2 | 521.2 |
| Other cardiomyopathy | 157,875 | 25,924 | 76.2 | 8.9 | 339.9 |
| Pulmonary arterial hypertension | 7,722 | 117 | 2.8 | <0.1 | 1.7 |
| Atrial fibrillation and flutter | 2,384,327 | 19,282 | 663.1 | 5.3 | 119.9 |
| Aortic aneurysm | Not estimated | 13,936 | Not estimated | 4.0 | 93.8 |
| Lower extremity peripheral arterial disease | 4,018,233 | 13,208 | 1,099.9 | 3.6 | 66.3 |
| Endocarditis | 9,142 | 3,058 | 4.8 | 1.1 | 48.1 |
| Other cardiovascular and circulatory diseases | 2,914,750 | 16,721 | 863.9 | 4.9 | 164.1 |
Cardiovascular Disease in Australasia
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Australasia ranged from 92.0 to 122.5 per 100,000 in 2022; a 1.3 fold difference. CVD mortality decreased by 65.5% from 1990 to 2022. Of the 21 regions, Australasia ranked 16th in 1990 and 20th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, other cardiovascular and circulatory diseases had the highest age-standardized DALYs in 2022 at 152.2 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 777.3 per 100,000.
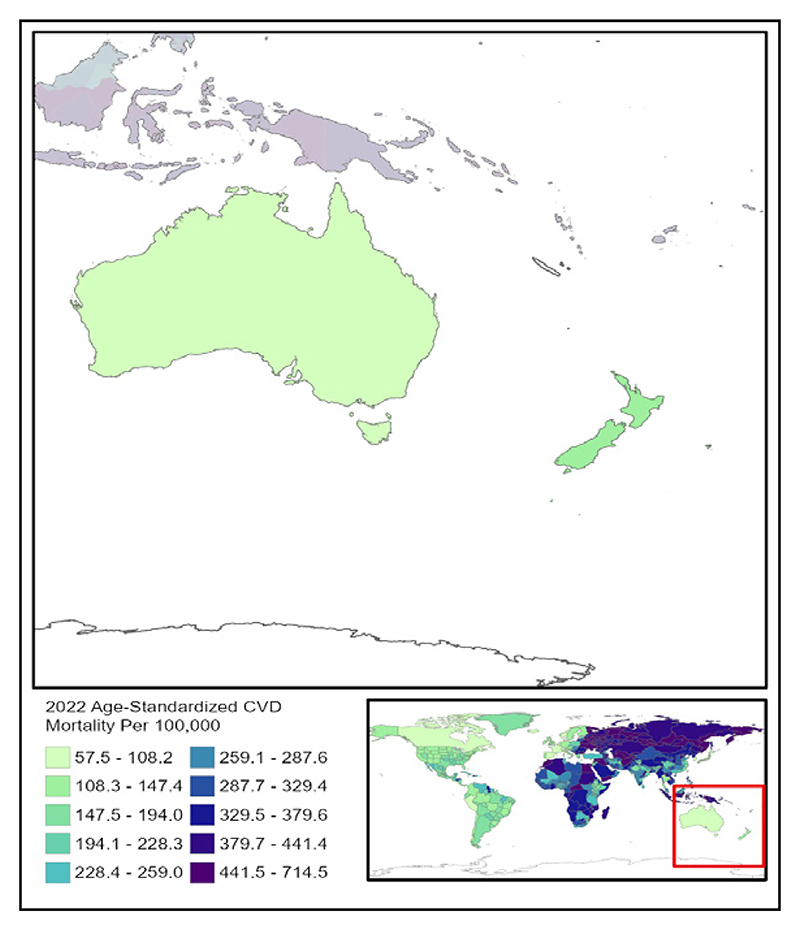
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 22,224 | 638 | 52.9 | 1.1 | 27.1 |
| Ischemic heart disease | 1,282,122 | 29,819 | 2,380.2 | 47.4 | 893.0 |
| Ischemic stroke | 322,348 | 9,651 | 625.8 | 14.0 | 250.4 |
| Intracerebral hemorrhage | 41,072 | 4,199 | 95.2 | 6.8 | 130.1 |
| Subarachnoid hemorrhage | 34,529 | 1,457 | 80.0 | 2.7 | 76.8 |
| Hypertensive heart disease | 33,550 | 1,606 | 56.5 | 2.4 | 39.8 |
| Non-rheumatic calcific aortic valve disease | 198,197 | 2,162 | 331.3 | 3.2 | 45.5 |
| Non-rheumatic degenerative mitral valve disease | 118,556 | 373 | 199.4 | 0.6 | 11.7 |
| Other non-rheumatic valve diseases | 55 | 7 | 0.1 | <0.1 | 0.2 |
| Myocarditis | 4,306 | 73 | 14.6 | 0.2 | 9.0 |
| Alcoholic cardiomyopathy | 12,654 | 470 | 27.6 | 0.9 | 29.8 |
| Other cardiomyopathy | 39,079 | 1,331 | 107.7 | 2.3 | 62.7 |
| Pulmonary arterial hypertension | 1,192 | 62 | 2.8 | 0.1 | 3.8 |
| Atrial fibrillation and flutter | 533,587 | 4,748 | 918.4 | 7.0 | 149.8 |
| Aortic aneurysm | Not estimated | 1,764 | Not estimated | 2.9 | 49.6 |
| Lower extremity peripheral arterial disease | 515,310 | 1,056 | 878.6 | 1.6 | 23.3 |
| Endocarditis | 4,542 | 755 | 9.7 | 1.3 | 26.1 |
| Other cardiovascular and circulatory diseases | 1,018,013 | 1,335 | 2,019.0 | 2.3 | 152.2 |
Cardiovascular Disease in High-Income Asia Pacific
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in High-income Asia Pacific ranged from 72.7 to 252.6 per 100,000 in 2022; a 3.5 fold difference. CVD mortality decreased by 64.2% from 1990 to 2022. Out of the 21 regions, High-income Asia Pacific was ranked 20th in 1990 and 21st in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, aortic aneurysm had the highest age-standardized DALYs in 2022 at 79.6 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 762.7 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 51,813 | 5,344 | 15.8 | 0.7 | 11.6 |
| Ischemic heart disease | 12,020,073 | 160,226 | 2,586.8 | 26.0 | 581.2 |
| Ischemic stroke | 3,765,022 | 115,125 | 900.3 | 15.5 | 347.4 |
| Intracerebral hemorrhage | 826,618 | 55,686 | 238.1 | 10.1 | 249.5 |
| Subarachnoid hemorrhage | 685,207 | 18,210 | 186.2 | 3.9 | 133.5 |
| Hypertensive heart disease | 310,906 | 22,366 | 58.4 | 3.0 | 46.7 |
| Non-rheumatic calcific aortic valve disease | 1,479,296 | 20,761 | 285.1 | 2.5 | 32.5 |
| Non-rheumatic degenerative mitral valve disease | 1,970,448 | 4,122 | 390.3 | 0.5 | 11.8 |
| Other non-rheumatic valve diseases | 326 | 31 | 0.1 | <0.1 | 0.2 |
| Myocarditis | 27,538 | 559 | 15.7 | 0.2 | 8.9 |
| Alcoholic cardiomyopathy | 13,218 | 479 | 5.0 | 0.1 | 4.4 |
| Other cardiomyopathy | 201,378 | 9,689 | 81.9 | 1.7 | 44.0 |
| Pulmonary arterial hypertension | 9,259 | 1,137 | 3.0 | 0.2 | 8.8 |
| Atrial fibrillation and flutter | 2,188,998 | 18,040 | 461.2 | 2.5 | 68.1 |
| Aortic aneurysm | Not estimated | 26,762 | Not estimated | 4.4 | 79.6 |
| Lower extremity peripheral arterial disease | 5,112,414 | 2,692 | 951.9 | 0.4 | 9.5 |
| Endocarditis | 24,892 | 5,825 | 6.8 | 0.8 | 14.9 |
| Other cardiovascular and circulatory diseases | 3,392,925 | 5,480 | 962.4 | 1.0 | 71.0 |
Cardiovascular Disease in High-Income North America
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in High-income North America ranged from 99.4 to 191.6 per 100,000 in 2022; a 1.9 fold difference. CVD mortality decreased by 45.9% from 1990 to 2022. High-income North America was ranked 17th in both 1990 and in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 245.2 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 762.7 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
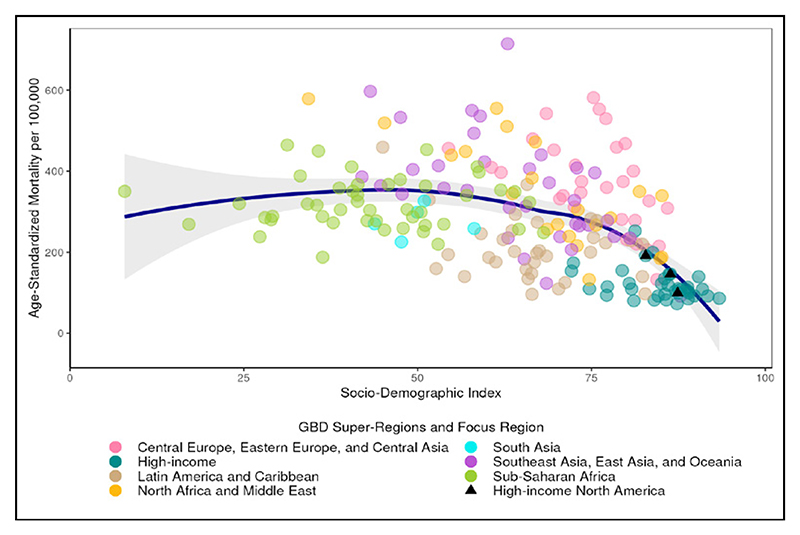
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
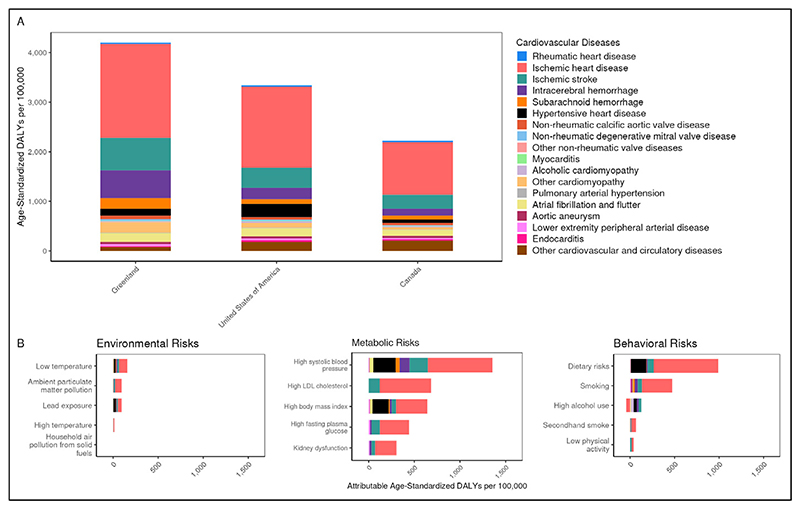
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
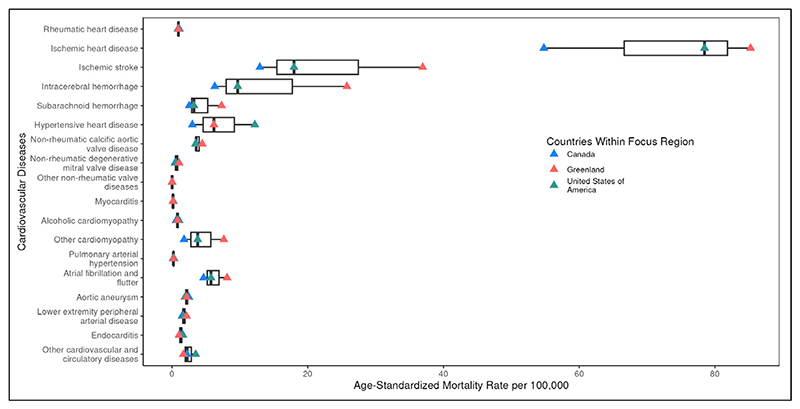
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 667,615 | 6,262 | 104.0 | 0.9 | 22.5 |
| Ischemic heart disease | 29,774,092 | 545,993 | 4,512.7 | 75.8 | 1,572.4 |
| Ischemic stroke | 7,310,116 | 133,791 | 1,243.8 | 17.4 | 392.9 |
| Intracerebral hemorrhage | 811,487 | 64,618 | 161.1 | 9.3 | 217.9 |
| Subarachnoid hemorrhage | 424,733 | 20,234 | 84.2 | 3.1 | 93.3 |
| Hypertensive heart disease | 1,030,771 | 77,701 | 159.5 | 11.2 | 245.2 |
| Non-rheumatic calcific aortic valve disease | 2,822,210 | 26,859 | 399.9 | 3.5 | 51.3 |
| Non-rheumatic degenerative mitral valve disease | 3,765,229 | 4,250 | 531.1 | 0.6 | 16.3 |
| Other non-rheumatic valve diseases | 712 | 78 | 0.2 | <0.1 | 0.4 |
| Myocarditis | 55,489 | 809 | 17.3 | 0.2 | 11.3 |
| Alcoholic cardiomyopathy | 94,817 | 5,917 | 18.1 | 1.0 | 31.7 |
| Other cardiomyopathy | 525,115 | 23,631 | 124.8 | 3.6 | 95.4 |
| Pulmonary arterial hypertension | 8,771 | 1,888 | 1.7 | 0.3 | 7.5 |
| Atrial fibrillation and flutter | 8,517,878 | 43,337 | 1,209.9 | 5.6 | 161.4 |
| Aortic aneurysm | Not estimated | 13,625 | Not estimated | 2.0 | 42.2 |
| Lower extremity peripheral arterial disease | 12,665,608 | 12,402 | 1,784.6 | 1.7 | 33.7 |
| Endocarditis | 51,368 | 10,617 | 10.2 | 1.6 | 36.4 |
| Other cardiovascular and circulatory diseases | 10,519,632 | 21,465 | 1,884.4 | 3.3 | 182.8 |
Cardiovascular Disease in Southern Latin America
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Southern Latin America ranged from 114.9 to 173.6 per 100,000 in 2022; a 1.5 fold difference. CVD mortality decreased by 51.2% from 1990 to 2022. Of the 21 regions, Southern Latin America ranked 13th in 1990 and 16th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, other cardiovascular and circulatory diseases had the highest age-standardized DALYs in 2022 at 281.0 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 1,486.4 per 100,000.
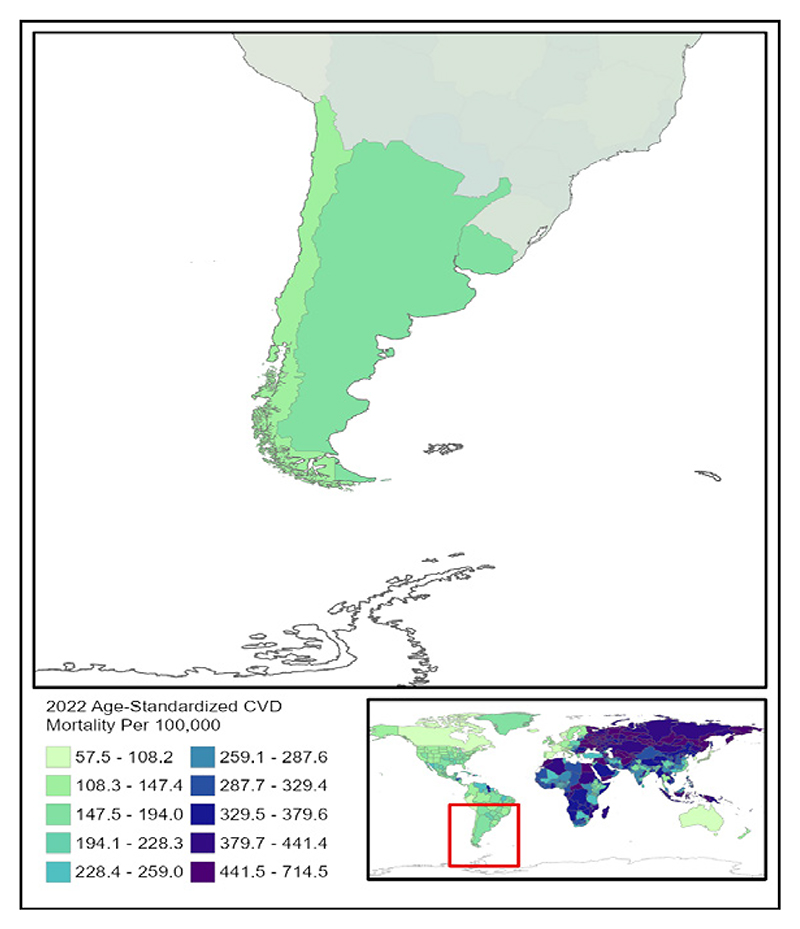
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 52,634 | 1,201 | 61.0 | 1.3 | 26.7 |
| Ischemic heart disease | 2,609,524 | 57,655 | 2,920.1 | 62.5 | 1,287.1 |
| Ischemic stroke | 528,575 | 21,539 | 615.0 | 22.7 | 401.3 |
| Intracerebral hemorrhage | 204,460 | 14,720 | 253.2 | 16.4 | 412.0 |
| Subarachnoid hemorrhage | 102,243 | 3,945 | 125.9 | 4.5 | 144.0 |
| Hypertensive heart disease | 98,942 | 14,678 | 107.9 | 15.5 | 230.0 |
| Non-rheumatic calcific aortic valve disease | 244,711 | 2,972 | 267.5 | 3.2 | 53.0 |
| Non-rheumatic degenerative mitral valve disease | 128,886 | 336 | 141.0 | 0.4 | 9.5 |
| Other non-rheumatic valve diseases | 23 | 7 | <0.1 | <0.1 | 0.2 |
| Myocarditis | 3,935 | 87 | 5.4 | 0.1 | 3.7 |
| Alcoholic cardiomyopathy | 2,095 | 172 | 2.6 | 0.2 | 5.9 |
| Other cardiomyopathy | 71,655 | 8,491 | 97.2 | 9.3 | 198.6 |
| Pulmonary arterial hypertension | 2,260 | 132 | 2.8 | 0.2 | 5.7 |
| Atrial fibrillation and flutter | 419,791 | 4,074 | 459.7 | 4.3 | 87.2 |
| Aortic aneurysm | Not estimated | 2,380 | Not estimated | 2.6 | 55.4 |
| Lower extremity peripheral arterial disease | 983,138 | 567 | 1,071.6 | 0.6 | 14.1 |
| Endocarditis | 4,242 | 1,566 | 5.6 | 1.7 | 41.4 |
| Other cardiovascular and circulatory diseases | 1,700,581 | 8,696 | 1,970.7 | 9.5 | 281.0 |
Cardiovascular Disease in Western Europe
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Western Europe ranged from 80.2 to 199.9 per 100,000 in 2022; a 2.5 fold difference. CVD mortality decreased by 60.2% from 1990 to 2022. Of the 21 regions, Western Europe ranked 15th in 1990 and 19th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, other cardiovascular and circulatory diseases had the highest age-standardized DALYs in 2022 at 166.7 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 977.2 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 115,044 | 18,447 | 14.9 | 1.6 | 26.5 |
| Ischemic heart disease | 27,188,008 | 576,481 | 2,928.5 | 49.5 | 957.8 |
| Ischemic stroke | 6,280,537 | 228,785 | 702.4 | 17.4 | 312.8 |
| Intracerebral hemorrhage | 795,635 | 95,176 | 112.6 | 8.5 | 170.5 |
| Subarachnoid hemorrhage | 570,991 | 22,622 | 84.6 | 2.3 | 68.3 |
| Hypertensive heart disease | 1,211,065 | 115,009 | 108.9 | 8.6 | 114.2 |
| Non-rheumatic calcific aortic valve disease | 4,297,106 | 55,830 | 419.1 | 4.3 | 61.9 |
| Non-rheumatic degenerative mitral valve disease | 3,167,713 | 9,420 | 308.5 | 0.8 | 15.4 |
| Other non-rheumatic valve diseases | 1,693 | 298 | 0.2 | <0.1 | 0.5 |
| Myocarditis | 45,972 | 1,523 | 9.6 | 0.2 | 5.2 |
| Alcoholic cardiomyopathy | 95,734 | 4,892 | 14.4 | 0.6 | 17.2 |
| Other cardiomyopathy | 530,824 | 31,479 | 86.2 | 2.7 | 58.5 |
| Pulmonary arterial hypertension | 23,892 | 1,756 | 3.6 | 0.2 | 4.8 |
| Atrial fibrillation and flutter | 7,681,289 | 81,522 | 749.7 | 6.1 | 128.1 |
| Aortic aneurysm | Not estimated | 29,615 | Not estimated | 2.7 | 51.0 |
| Lower extremity peripheral arterial disease | 20,564,688 | 17,682 | 2,099.2 | 1.4 | 30.4 |
| Endocarditis | 94,539 | 19,801 | 12.7 | 1.7 | 31.4 |
| Other cardiovascular and circulatory diseases | 17,808,574 | 32,595 | 2,140.9 | 3.0 | 166.7 |
Cardiovascular Disease in Andean Latin America
Findings from the Global Burden of Disease Study
Summary
Age-standardized CVD mortality rates among countries in Andean Latin America ranged from 96.1 to 187.2. per 100,000 in 2022; a 1.9 fold difference. CVD mortality decreased by 39.9% from 1990 to 2022. Out of the 21 regions, Andean Latin America was ranked 21st in 1990 and 18th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 169.3 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 1,230.6 per 100,000.
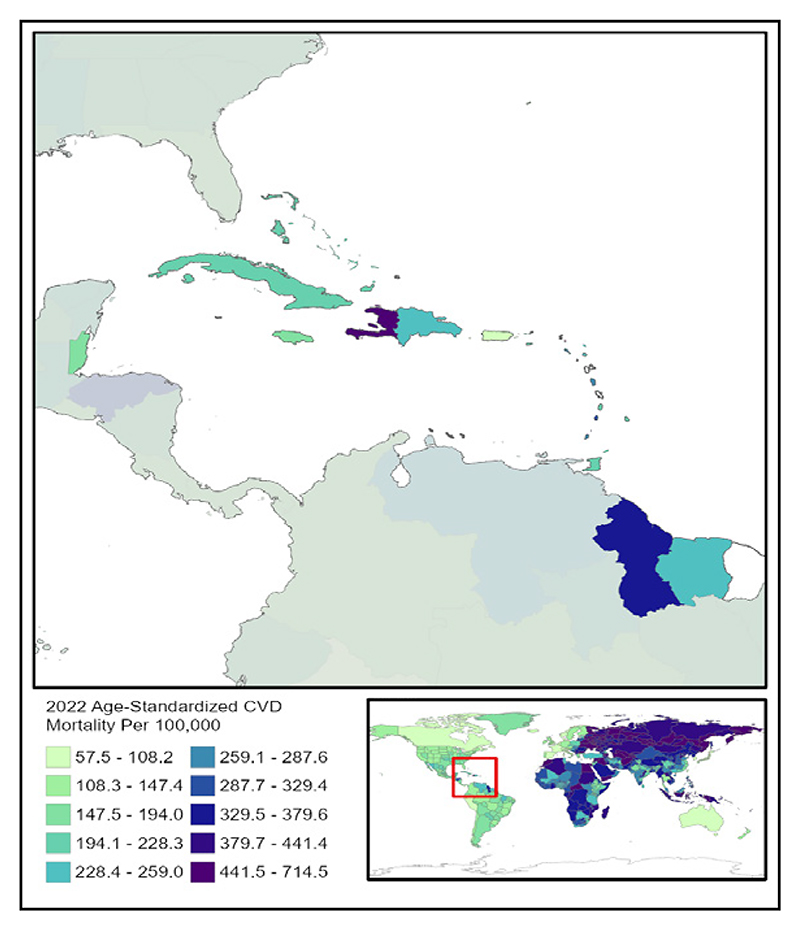
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
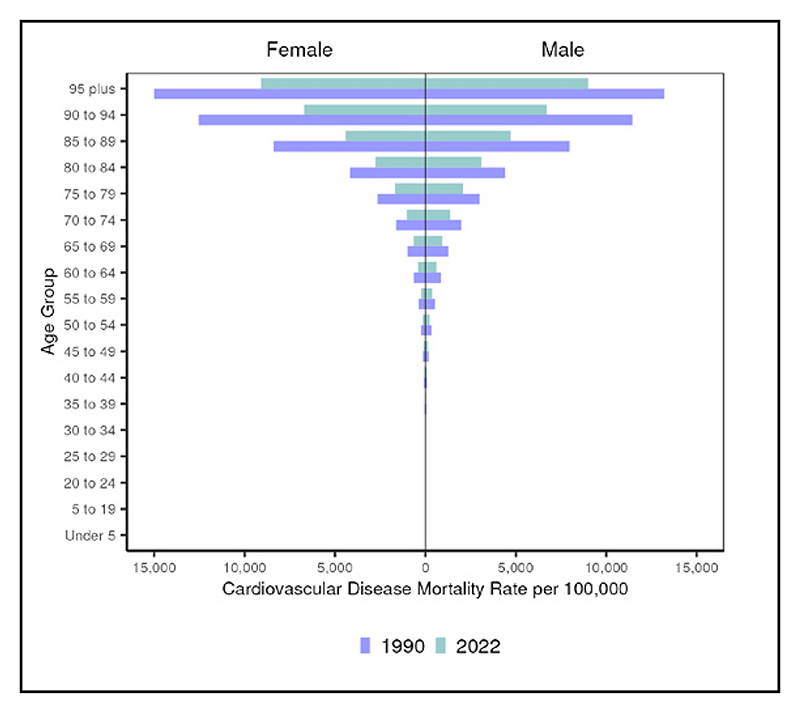
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
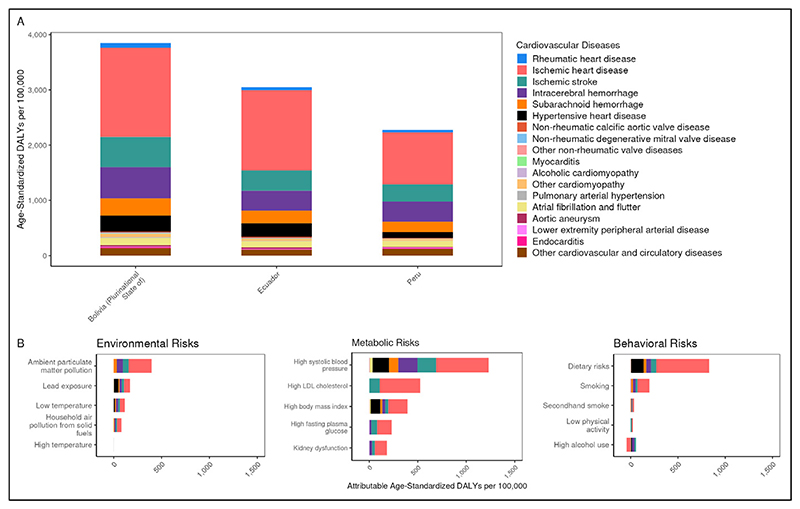
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
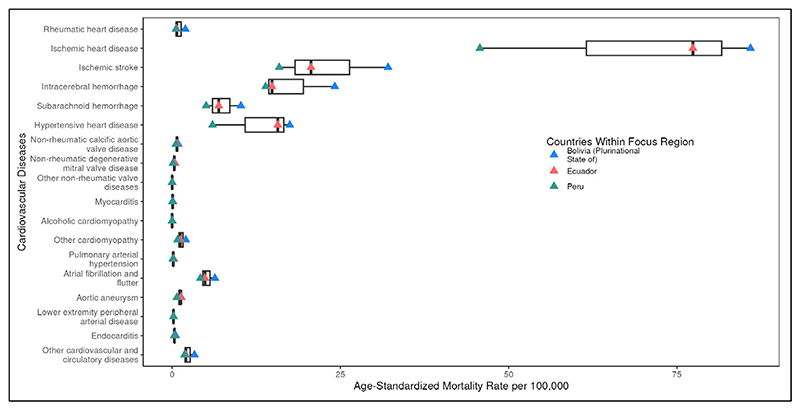
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 457,455 | 494 | 656.7 | 0.8 | 53.7 |
| Ischemic heart disease | 1,070,915 | 34,037 | 1,721.7 | 59.0 | 1,173.5 |
| Ischemic stroke | 469,672 | 10,679 | 756.7 | 19.0 | 356.2 |
| Intracerebral hemorrhage | 99,306 | 9,357 | 150.7 | 15.6 | 397.3 |
| Subarachnoid hemorrhage | 155,742 | 3,937 | 242.6 | 6.3 | 216.0 |
| Hypertensive heart disease | 85,773 | 5,595 | 145.0 | 9.9 | 169.3 |
| Non-rheumatic calcific aortic valve disease | 80,043 | 391 | 134.1 | 0.7 | 17.1 |
| Non-rheumatic degenerative mitral valve disease | 16,939 | 144 | 28.4 | 0.2 | 6.7 |
| Other non-rheumatic valve diseases | 24 | 4 | <0.1 | <0.1 | 0.1 |
| Myocarditis | 3,365 | 39 | 5.2 | 0.1 | 2.4 |
| Alcoholic cardiomyopathy | 27 | 3 | <0.1 | <0.1 | 0.1 |
| Other cardiomyopathy | 23,166 | 660 | 35.9 | 1.1 | 39.2 |
| Pulmonary arterial hypertension | 1,809 | 84 | 2.8 | 0.1 | 5.1 |
| Atrial fibrillation and flutter | 402,429 | 2,532 | 684.4 | 4.6 | 111.4 |
| Aortic aneurysm | Not estimated | 563 | Not estimated | 1.0 | 20.3 |
| Lower extremity peripheral arterial disease | 502,546 | 116 | 858.6 | 0.2 | 7.8 |
| Endocarditis | 2,992 | 221 | 4.6 | 0.4 | 13.6 |
| Other cardiovascular and circulatory diseases | 780,772 | 1,237 | 1,247.7 | 2.1 | 118.8 |
Cardiovascular Disease in the Caribbean
Findings from the Global Burden of Disease Study
Summary.
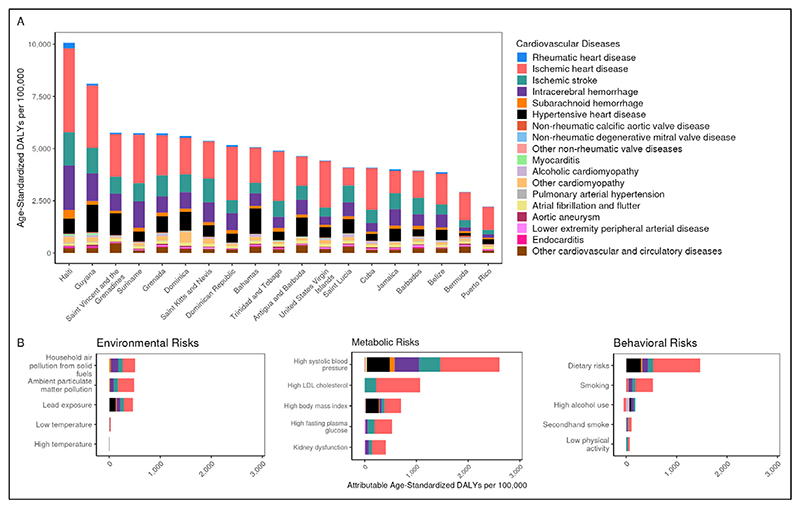
Age-standardized CVD mortality rates among countries in the Caribbean ranged from 97.3 to 459.2 per 100,000 in 2022; a 4.7 fold difference. CVD mortality decreased by 34.7% from 1990 to 2022. Out of the 21 regions, the Caribbean was ranked 11th in 1990 and 13th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 441.6 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 2,605.3 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 261,123 | 921 | 540.7 | 1.8 | 110.6 |
| Ischemic heart disease | 1,659,127 | 58,168 | 3,058.2 | 104.6 | 2,235.9 |
| Ischemic stroke | 490,869 | 21,153 | 913.3 | 38.0 | 701.9 |
| Intracerebral hemorrhage | 105,537 | 16,704 | 202.2 | 30.6 | 812.9 |
| Subarachnoid hemorrhage | 107,267 | 2,705 | 203.4 | 5.1 | 192.7 |
| Hypertensive heart disease | 101,513 | 12,193 | 185.4 | 21.8 | 441.6 |
| Non-rheumatic calcific aortic valve disease | 83,167 | 473 | 151.0 | 0.9 | 21.6 |
| Non-rheumatic degenerative mitral valve disease | 20,214 | 214 | 36.9 | 0.4 | 12.6 |
| Other non-rheumatic valve diseases | 34 | 10 | 0.1 | <0.1 | 0.5 |
| Myocarditis | 3,162 | 178 | 6.5 | 0.4 | 21.4 |
| Alcoholic cardiomyopathy | 9,102 | 1,096 | 17.2 | 2.0 | 62.3 |
| Other cardiomyopathy | 25,868 | 2,200 | 53.5 | 4.2 | 138.5 |
| Pulmonary arterial hypertension | 1,233 | 106 | 2.4 | 0.2 | 11.6 |
| Atrial fibrillation and flutter | 388,887 | 2,633 | 704.9 | 4.6 | 112.8 |
| Aortic aneurysm | Not estimated | 1,189 | Not estimated | 2.2 | 41.2 |
| Lower extremity peripheral arterial disease | 602,048 | 1,111 | 1,087.3 | 2.0 | 37.5 |
| Endocarditis | 2,215 | 444 | 4.6 | 0.9 | 33.3 |
| Other cardiovascular and circulatory diseases | 586,853 | 2,294 | 1,101.1 | 4.3 | 179.7 |
Cardiovascular Disease in Central Latin America
Findings from the Global Burden of Disease Study
Summary.
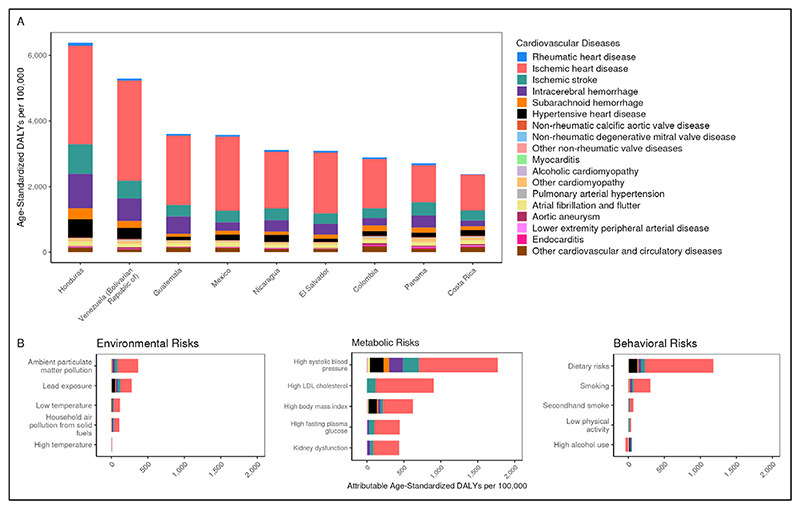
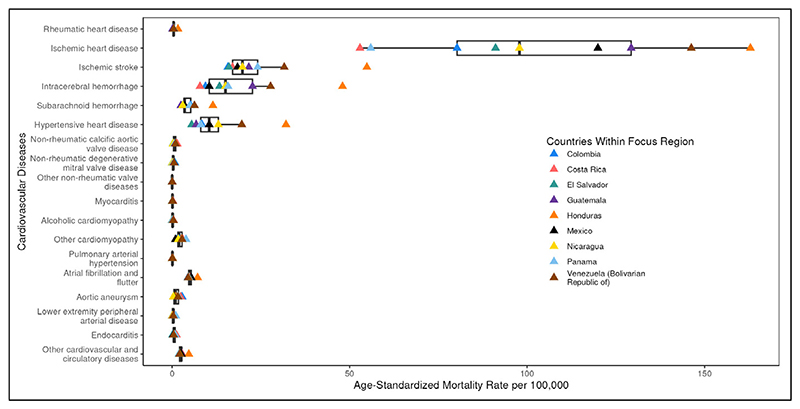
Age-standardized CVD mortality rates among countries in Central Latin America ranged from 109.5 to 329.4 per 100,000 in 2022; a 3.0 fold difference. CVD mortality decreased by 25.1% from 1990 to 2022. Out of the 21 regions, Central Latin America was ranked 19th in 1990 and 14th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 185.0 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized DALYs at 1,771.4 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 2,180,136 | 1,085 | 818.2 | 0.4 | 50.5 |
| Ischemic heart disease | 6,773,869 | 266,503 | 2,606.2 | 108.9 | 2,112.4 |
| Ischemic stroke | 2,013,978 | 47,303 | 782.1 | 19.9 | 369.8 |
| Intracerebral hemorrhage | 414,191 | 34,937 | 156.5 | 13.8 | 339.3 |
| Subarachnoid hemorrhage | 515,867 | 11,313 | 195.6 | 4.4 | 145.5 |
| Hypertensive heart disease | 293,297 | 26,580 | 119.2 | 11.1 | 185.0 |
| Non-rheumatic calcific aortic valve disease | 415,329 | 1,998 | 163.5 | 0.8 | 20.0 |
| Non-rheumatic degenerative mitral valve disease | 94,050 | 918 | 37.1 | 0.4 | 9.0 |
| Other non-rheumatic valve diseases | 416 | 53 | 0.2 | <0.1 | 0.5 |
| Myocarditis | 15,823 | 219 | 6.2 | 0.1 | 4.0 |
| Alcoholic cardiomyopathy | 7,615 | 473 | 2.8 | 0.2 | 6.3 |
| Other cardiomyopathy | 98,861 | 3,939 | 40.4 | 1.6 | 50.8 |
| Pulmonary arterial hypertension | 8,503 | 223 | 3.2 | 0.1 | 3.2 |
| Atrial fibrillation and flutter | 1,830,384 | 11,672 | 731.2 | 5.0 | 121.3 |
| Aortic aneurysm | Not estimated | 3,108 | Not estimated | 1.3 | 25.9 |
| Lower extremity peripheral arterial disease | 3,237,956 | 906 | 1,293.0 | 0.4 | 13.0 |
| Endocarditis | 11,943 | 1,309 | 4.8 | 0.5 | 17.6 |
| Other cardiovascular and circulatory diseases | 3,451,669 | 6,319 | 1,330.6 | 2.6 | 131.7 |
Cardiovascular Disease in Tropical Latin America
Findings from the Global Burden of Disease Study
Summary.
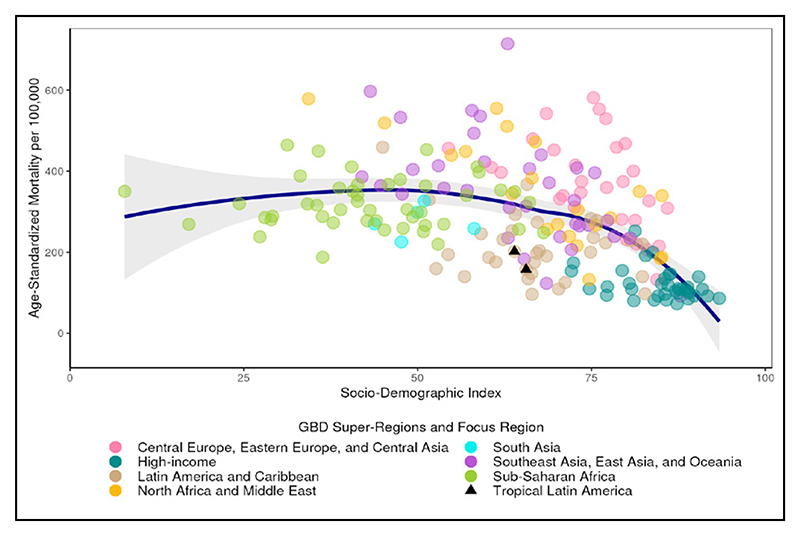
Age-standardized CVD mortality rates among countries in Tropical Latin America ranged from 157.7 to 201.8 per 100,000 in 2022; a 1.3 fold difference. CVD mortality decreased by 52.6% from 1990 to 2022. Out of the 21 regions, Tropical Latin America was ranked 12th in 1990 and 15th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 245.4 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized DALYs at 1,706.2 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
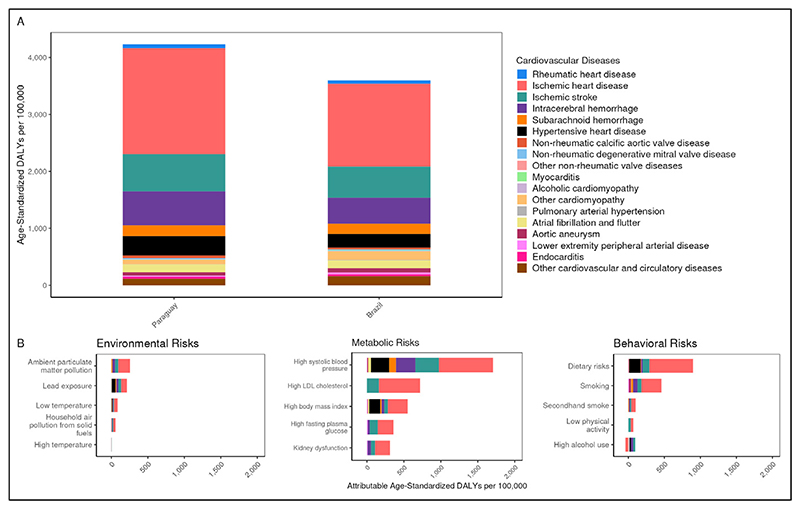
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
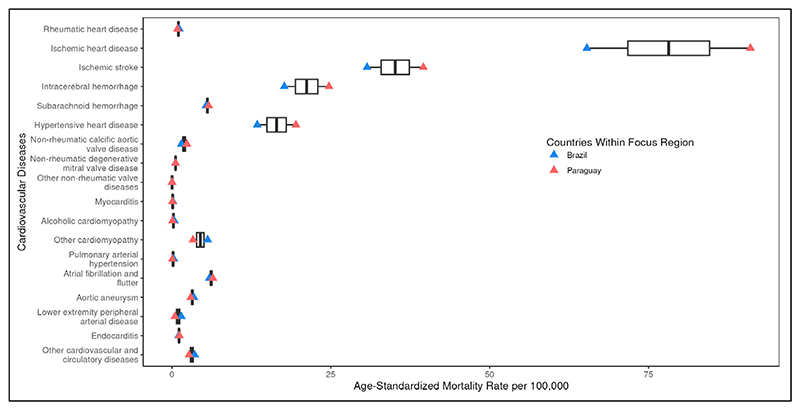
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
| Rheumatic heart disease | 1,178,179 | 3,017 | 492.9 | 1.2 | 59.1 |
| Ischemic heart disease | 3,706,448 | 170,497 | 1,397.5 | 65.8 | 1,467.1 |
| Ischemic stroke | 2,083,023 | 77,319 | 795.6 | 30.9 | 545.1 |
| Intracerebral hemorrhage | 450,678 | 46,943 | 173.2 | 17.8 | 462.2 |
| Subarachnoid hemorrhage | 394,619 | 14,180 | 150.2 | 5.4 | 175.8 |
| Hypertensive heart disease | 424,780 | 34,337 | 166.1 | 13.6 | 245.4 |
| Non-rheumatic calcific aortic valve disease | 377,483 | 3,857 | 143.7 | 1.5 | 31.1 |
| Non-rheumatic degenerative mitral valve disease | 113,713 | 1,459 | 43.2 | 0.6 | 14.2 |
| Other non-rheumatic valve diseases | 477 | 73 | 0.2 | <0.1 | 0.8 |
| Myocarditis | 16,568 | 379 | 7.1 | 0.2 | 6.3 |
| Alcoholic cardiomyopathy | 19,642 | 983 | 7.5 | 0.4 | 13.6 |
| Other cardiomyopathy | 276,933 | 14,154 | 118.0 | 5.6 | 147.0 |
| Pulmonary arterial hypertension | 6,328 | 709 | 2.5 | 0.3 | 9.3 |
| Atrial fibrillation and flutter | 2,055,246 | 14,553 | 787.2 | 5.9 | 136.0 |
| Aortic aneurysm | Not estimated | 8,909 | Not estimated | 3.4 | 74.5 |
| Lower extremity peripheral arterial disease | 2,903,792 | 3,707 | 1,118.7 | 1.5 | 30.9 |
| Endocarditis | 14,833 | 2,771 | 6.6 | 1.1 | 33.9 |
| Other cardiovascular and circulatory diseases | 3,621,645 | 9,064 | 1,403.2 | 3.6 | 158.2 |
Cardiovascular Disease in North Africa and Middle East
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in North Africa and Middle East ranged from 132.5 to 578.7 per 100,000 in 2022; a 4.4 fold difference. CVD mortality decreased by 31.6% from 1990 to 2022. Of the 21 regions, North Africa and Middle East ranked 3rd in 1990 and 5th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 654.8 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 3,914.0 per 100,000.
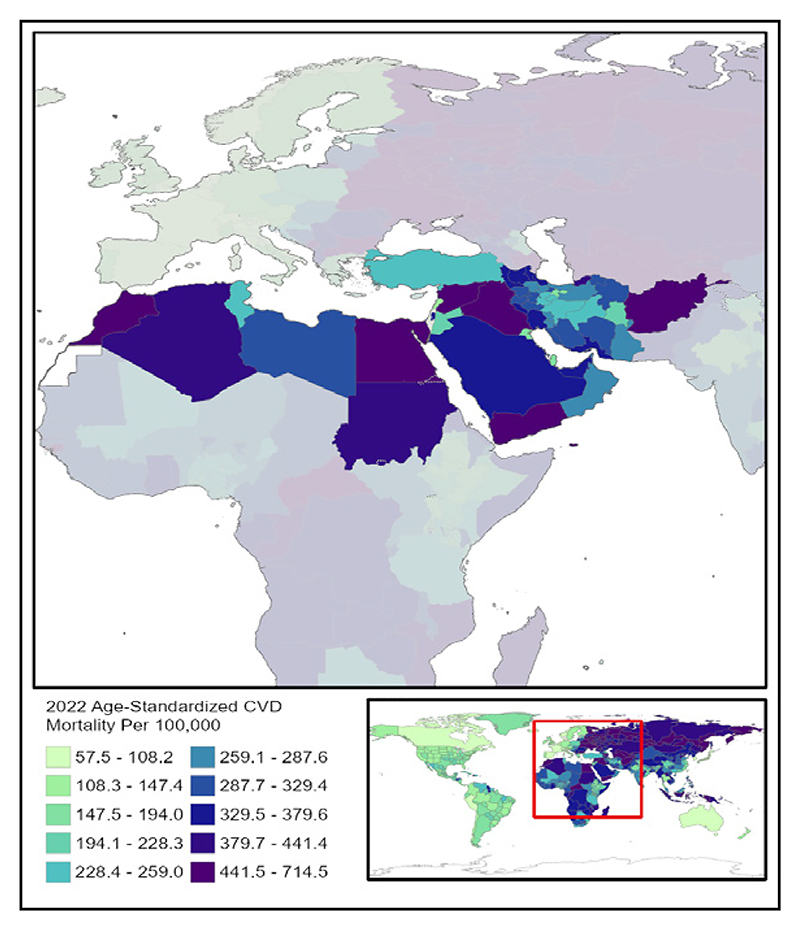
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
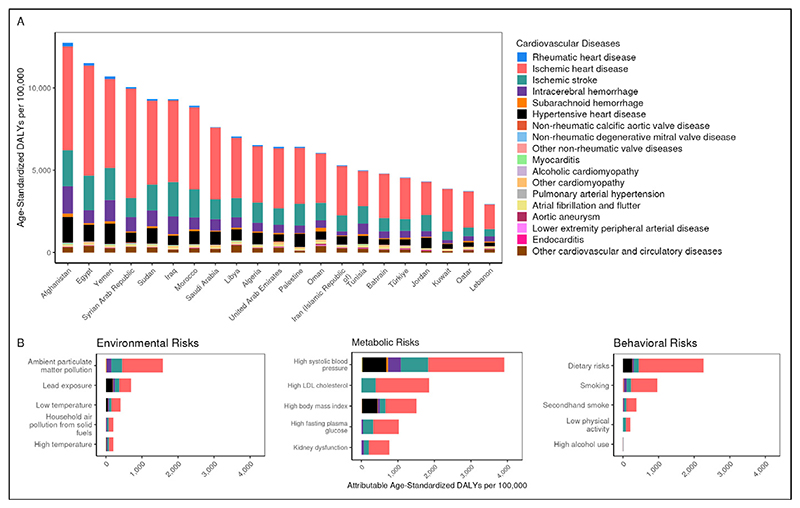
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
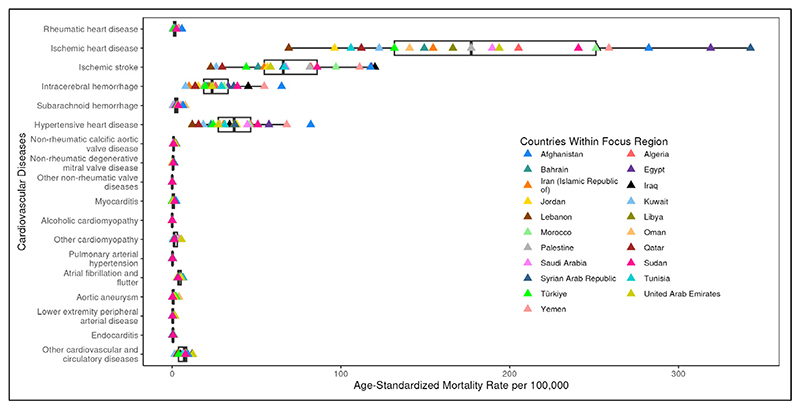
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 2,764,881 | 9,411 | 420.5 | 1.9 | 82.2 |
| Ischemic heart disease | 29,397,709 | 770,738 | 5,780.2 | 196.2 | 4,028.1 |
| Ischemic stroke | 4,390,907 | 254,063 | 803.4 | 71.8 | 1,267.9 |
| Intracerebral hemorrhage | 1,207,552 | 112,756 | 199.2 | 26.0 | 631.2 |
| Subarachnoid hemorrhage | 660,160 | 12,513 | 115.1 | 2.8 | 86.9 |
| Hypertensive heart disease | 1,043,500 | 136,843 | 240.0 | 38.0 | 654.8 |
| Non-rheumatic calcific aortic valve disease | 260,404 | 3,603 | 56.9 | 0.9 | 20.0 |
| Non-rheumatic degenerative mitral valve disease | 271,543 | 3,108 | 63.3 | 0.7 | 18.2 |
| Other non-rheumatic valve diseases | 3,516 | 338 | 0.6 | 0.1 | 2.0 |
| Myocarditis | 33,842 | 3,336 | 5.8 | 0.8 | 22.0 |
| Alcoholic cardiomyopathy | 3,065 | 124 | 0.5 | <0.1 | 0.8 |
| Other cardiomyopathy | 311,277 | 7,084 | 52.1 | 1.5 | 53.3 |
| Pulmonary arterial hypertension | 11,860 | 1,459 | 2.0 | 0.3 | 11.6 |
| Atrial fibrillation and flutter | 1,560,144 | 11,850 | 397.3 | 4.0 | 78.6 |
| Aortic aneurysm | Not estimated | 4,152 | Not estimated | 1.0 | 21.5 |
| Lower extremity peripheral arterial disease | 3,580,213 | 1,941 | 876.0 | 0.5 | 13.8 |
| Endocarditis | 17,388 | 2,628 | 3.0 | 0.6 | 17.4 |
| Other cardiovascular and circulatory diseases | 8,613,986 | 30,165 | 1,640.6 | 7.2 | 271.6 |
Cardiovascular Disease in South Asia
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in South Asia ranged from 225.4 to 326.5 per 100,000 in 2022. CVD mortality decreased by 11.3% from 1990 to 2022. Of the 21 regions, South Asia ranked 14th in 1990 and 10th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, rheumatic heart disease had the highest age-standardized DALYs in 2022 at 466.1 per 100,000. South Asia had the lowest CVD age-standardized prevalence in 2022. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 2,841.1 per 100,000.
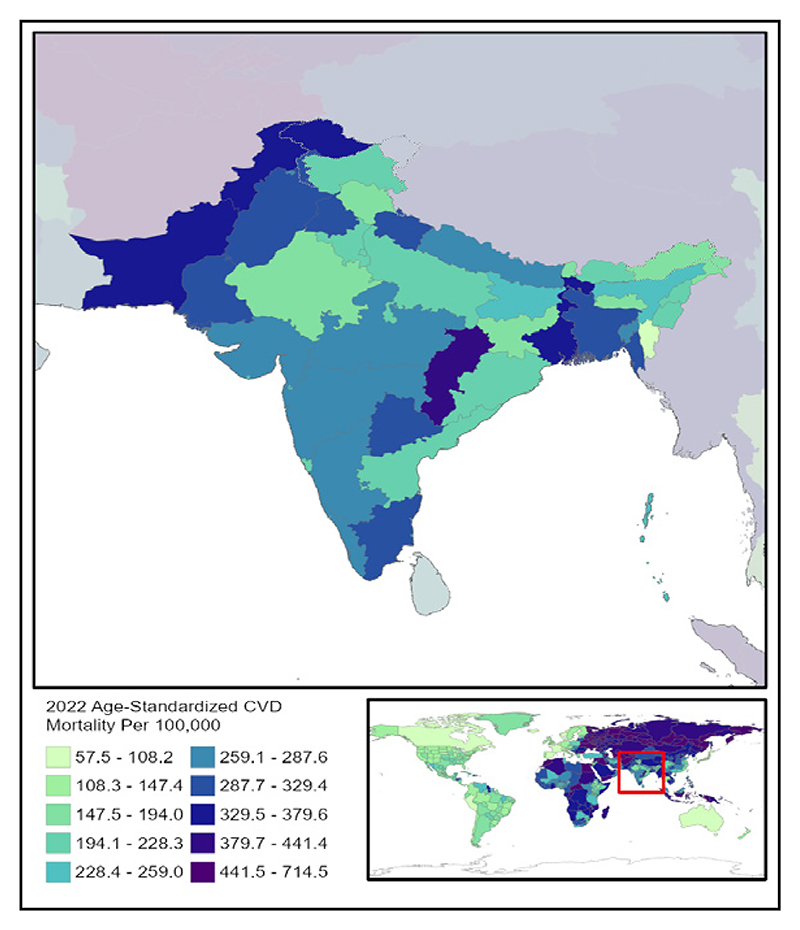
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 13,791,295 | 225,729 | 692.5 | 15.0 | 466.1 |
| Ischemic heart disease | 36,416,292 | 2,021,289 | 2,214.6 | 147.1 | 3,285.4 |
| Ischemic stroke | 13,333,231 | 417,001 | 838.0 | 34.4 | 678.0 |
| Intracerebral hemorrhage | 4,234,810 | 538,372 | 242.9 | 36.8 | 902.9 |
| Subarachnoid hemorrhage | 1,543,909 | 61,635 | 85.1 | 4.0 | 126.8 |
| Hypertensive heart disease | 1,478,240 | 194,286 | 111.8 | 15.9 | 285.1 |
| Non-rheumatic calcific aortic valve disease | 362,863 | 10,800 | 25.1 | 0.9 | 16.0 |
| Non-rheumatic degenerative mitral valve disease | 505,344 | 5,230 | 35.6 | 0.4 | 9.1 |
| Other non-rheumatic valve diseases | 717 | 225 | <0.1 | <0.1 | 0.4 |
| Myocarditis | 112,625 | 5,127 | 6.5 | 0.3 | 14.2 |
| Alcoholic cardiomyopathy | 12,545 | 1,550 | 0.7 | 0.1 | 3.0 |
| Other cardiomyopathy | 797,264 | 72,352 | 48.7 | 5.2 | 136.8 |
| Pulmonary arterial hypertension | 30,055 | 3,646 | 1.7 | 0.3 | 8.3 |
| Atrial fibrillation and flutter | 7,938,649 | 32,239 | 589.6 | 3.2 | 84.7 |
| Aortic aneurysm | Not estimated | 12,746 | Not estimated | 1.0 | 19.0 |
| Lower extremity peripheral arterial disease | 10,775,328 | 3,447 | 798.3 | 0.3 | 9.3 |
| Endocarditis | 48,426 | 11,991 | 2.8 | 0.8 | 23.5 |
| Other cardiovascular and circulatory diseases | 10,705,232 | 32,698 | 707.4 | 2.4 | 94.3 |
Cardiovascular Disease in East Asia
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in East Asia ranged from 91.8 to 352.9 per 100,000 in 2022; a 3.8 fold difference. CVD mortality decreased by 32.4% from 1990 to 2022. Out of the 21 regions, East Asia was ranked 7th in 1990 and 11th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 269.3 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 2,745.2 per 100,000.
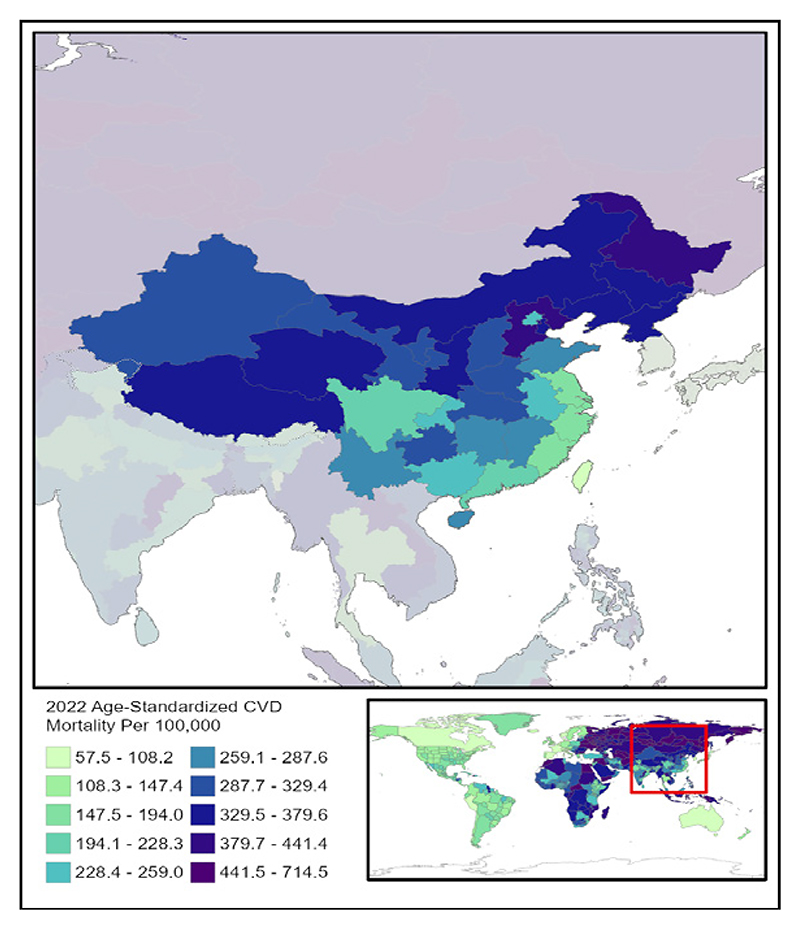
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
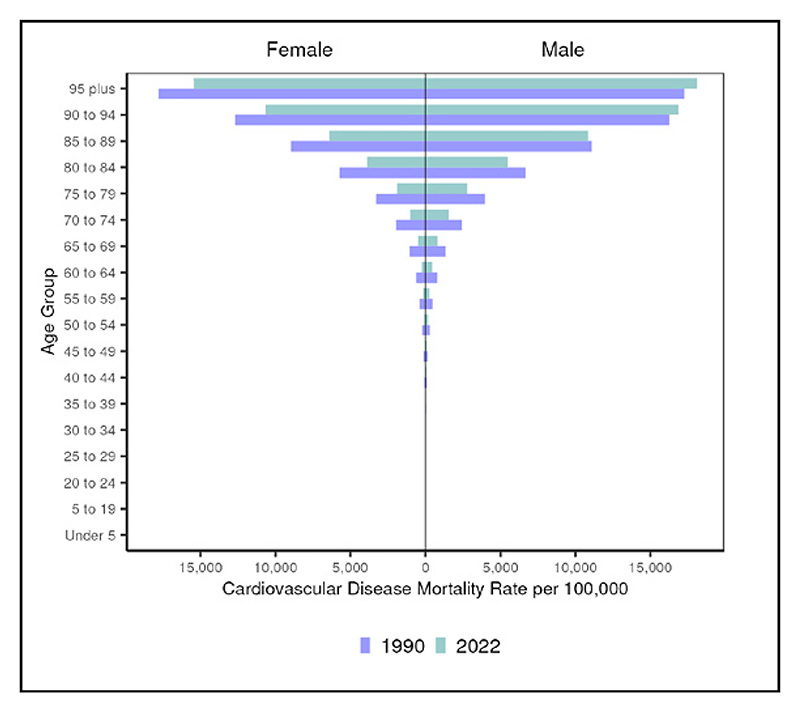
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
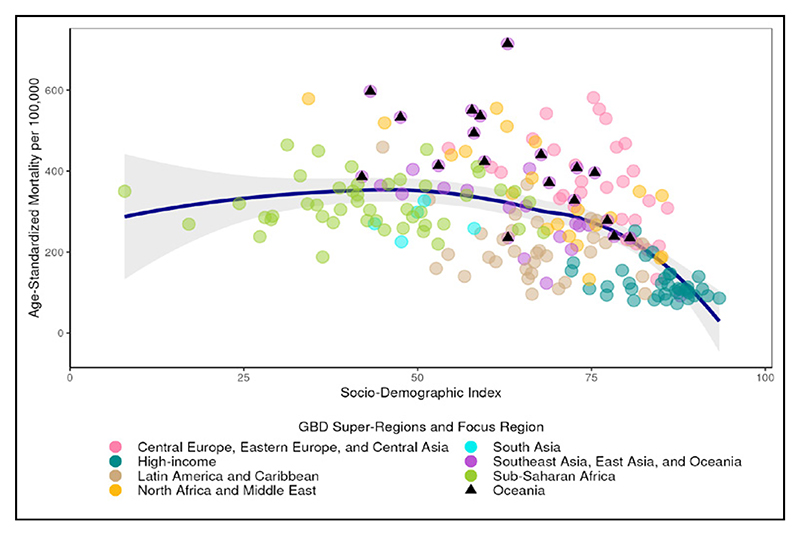
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
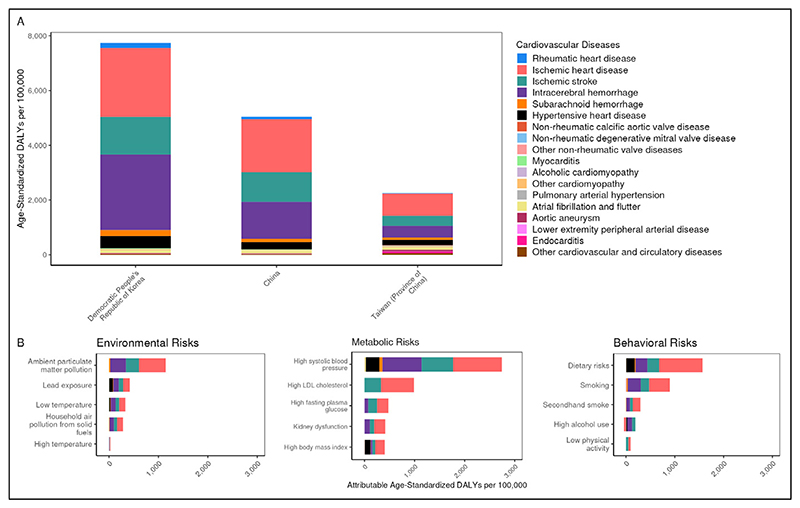
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 5,266,540 | 75,927 | 343.8 | 3.7 | 89.1 |
| Ischemic heart disease | 68,751,838 | 2,099,130 | 3,183.8 | 108.4 | 1,917.9 |
| Ischemic stroke | 23,266,169 | 1,139,094 | 1,064.1 | 57.0 | 1,072.0 |
| Intracerebral hemorrhage | 4,923,009 | 1,433,592 | 239.3 | 68.6 | 1,361.0 |
| Subarachnoid hemorrhage | 1,720,413 | 91,177 | 85.9 | 4.3 | 111.1 |
| Hypertensive heart disease | 4,114,002 | 331,523 | 189.0 | 17.4 | 269.3 |
| Non-rheumatic calcific aortic valve disease | 751,611 | 1,805 | 33.5 | 0.1 | 2.2 |
| Non-rheumatic degenerative mitral valve disease | 2,832,655 | 1,066 | 125.3 | 0.1 | 2.9 |
| Other non-rheumatic valve diseases | 1,382 | 247 | 0.1 | <0.1 | 0.3 |
| Myocarditis | 165,695 | 9,139 | 11.0 | 0.5 | 17.5 |
| Alcoholic cardiomyopathy | 32,864 | 1,551 | 1.8 | 0.1 | 2.8 |
| Other cardiomyopathy | 280,309 | 12,430 | 19.1 | 0.7 | 20.0 |
| Pulmonary arterial hypertension | 42,191 | 6,687 | 2.2 | 0.3 | 7.7 |
| Atrial fibrillation and flutter | 12,179,180 | 67,436 | 551.6 | 4.0 | 88.1 |
| Aortic aneurysm | Not estimated | 11,241 | Not estimated | 0.5 | 14.3 |
| Lower extremity peripheral arterial disease | 27,223,946 | 2,326 | 1,197.4 | 0.1 | 8.3 |
| Endocarditis | 37,262 | 3,171 | 2.2 | 0.2 | 4.8 |
| Other cardiovascular and circulatory diseases | 6,009,279 | 12,839 | 290.8 | 0.7 | 31.2 |
Cardiovascular Disease in Oceania
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Oceania ranged from 235.0 to 714.5 per 100,000 in 2022; a 3.0 fold difference. CVD mortality decreased by 16.4% from 1990 to 2022. Out of the 21 regions, Oceania was ranked 5th in 1990 and 3rd in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, rheumatic heart disease had the highest age-standardized DALYs in 2022 at 593.7 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 4,420.7 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
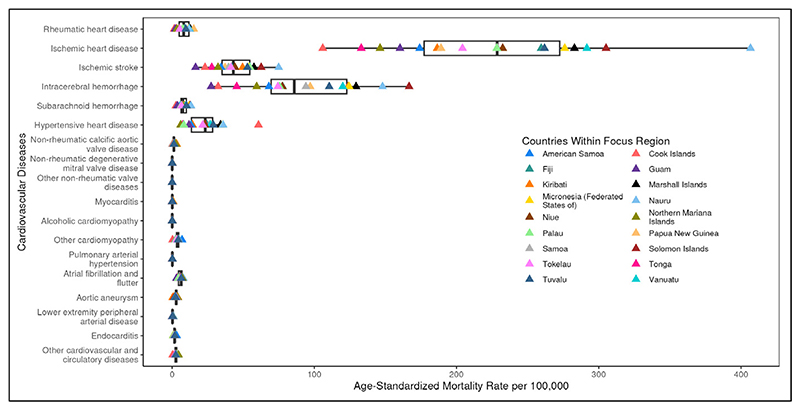
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 101,882 | 1,468 | 700.3 | 13.4 | 593.7 |
| Ischemic heart disease | 448,962 | 13,551 | 5,133.3 | 202.7 | 4,755.9 |
| Ischemic stroke | 84,641 | 1,802 | 985.3 | 37.9 | 790.5 |
| Intracerebral hemorrhage | 43,925 | 6,451 | 414.8 | 94.1 | 2,226.2 |
| Subarachnoid hemorrhage | 22,127 | 646 | 205.4 | 7.6 | 267.2 |
| Hypertensive heart disease | 6,669 | 1,487 | 102.9 | 22.6 | 505.5 |
| Non-rheumatic calcific aortic valve disease | 1,718 | 59 | 27.0 | 0.9 | 22.0 |
| Non-rheumatic degenerative mitral valve disease | 4,404 | 7 | 71.2 | 0.1 | 3.8 |
| Other non-rheumatic valve diseases | 5 | 2 | 0.1 | <0.1 | 0.6 |
| Myocarditis | 670 | 33 | 5.5 | 0.2 | 14.0 |
| Alcoholic cardiomyopathy | 20 | 6 | 0.2 | 0.1 | 2.0 |
| Other cardiomyopathy | 2,892 | 427 | 24.5 | 4.5 | 159.7 |
| Pulmonary arterial hypertension | 198 | 23 | 1.8 | 0.2 | 8.9 |
| Atrial fibrillation and flutter | 33,404 | 185 | 542.1 | 4.2 | 103.8 |
| Aortic aneurysm | Not estimated | 118 | Not estimated | 1.9 | 40.0 |
| Lower extremity peripheral arterial disease | 65,617 | 8 | 1,009.2 | 0.1 | 8.9 |
| Endocarditis | 450 | 252 | 4.2 | 2.7 | 93.4 |
| Other cardiovascular and circulatory diseases | 30,024 | 204 | 392.8 | 2.3 | 97.2 |
Cardiovascular Disease in Southeast Asia
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Southeast Asia ranged from 123.2 to 406.2 per 100,000 in 2022; a 3.3 fold difference. CVD mortality decreased by 16.9% from 1990 to 2022. Out of the 21 regions, Southeast Asia was ranked 8th in 1990 and 6th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 458.5 per 100,000. For all risks, high systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 3,925.7 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
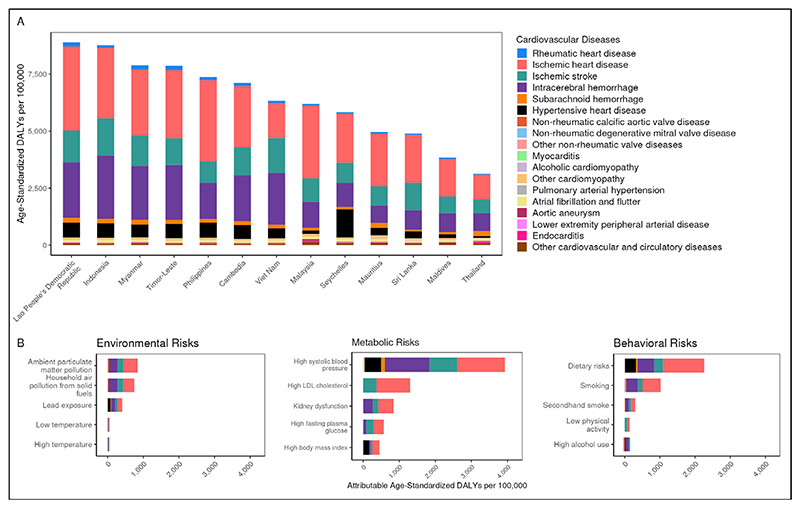
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 5,706,614 | 11,882 | 769.9 | 1.7 | 113.3 |
| Ischemic heart disease | 31,693,855 | 656,205 | 4,589.4 | 110.7 | 2,501.3 |
| Ischemic stroke | 9,373,197 | 325,362 | 1,358.5 | 63.4 | 1,239.7 |
| Intracerebral hemorrhage | 3,334,389 | 526,960 | 441.4 | 82.5 | 2,002.4 |
| Subarachnoid hemorrhage | 1,194,567 | 38,419 | 158.1 | 6.0 | 186.6 |
| Hypertensive heart disease | 1,017,714 | 132,805 | 168.1 | 22.9 | 458.5 |
| Non-rheumatic calcific aortic valve disease | 157,395 | 1,425 | 25.6 | 0.3 | 5.1 |
| Non-rheumatic degenerative mitral valve disease | 513,144 | 635 | 84.3 | 0.1 | 3.7 |
| Other non-rheumatic valve diseases | 271 | 62 | <0.1 | <0.1 | 0.2 |
| Myocarditis | 44,350 | 1,369 | 6.5 | 0.3 | 7.6 |
| Alcoholic cardiomyopathy | 3,649 | 333 | 0.5 | <0.1 | 1.7 |
| Other cardiomyopathy | 163,221 | 14,967 | 26.4 | 2.7 | 62.7 |
| Pulmonary arterial hypertension | 13,615 | 661 | 1.9 | 0.1 | 4.0 |
| Atrial fibrillation and flutter | 3,614,518 | 23,517 | 597.6 | 5.4 | 109.4 |
| Aortic aneurysm | Not estimated | 7,031 | Not estimated | 1.3 | 23.3 |
| Lower extremity peripheral arterial disease | 7,493,846 | 821 | 1,195.2 | 0.1 | 9.8 |
| Endocarditis | 37,970 | 7,559 | 6.1 | 1.2 | 35.5 |
| Other cardiovascular and circulatory diseases | 2,746,132 | 8,101 | 410.2 | 1.3 | 60.1 |
Cardiovascular Disease in Central Sub-Saharan Africa
Findings from the Global Burden of Disease Study
Summary.
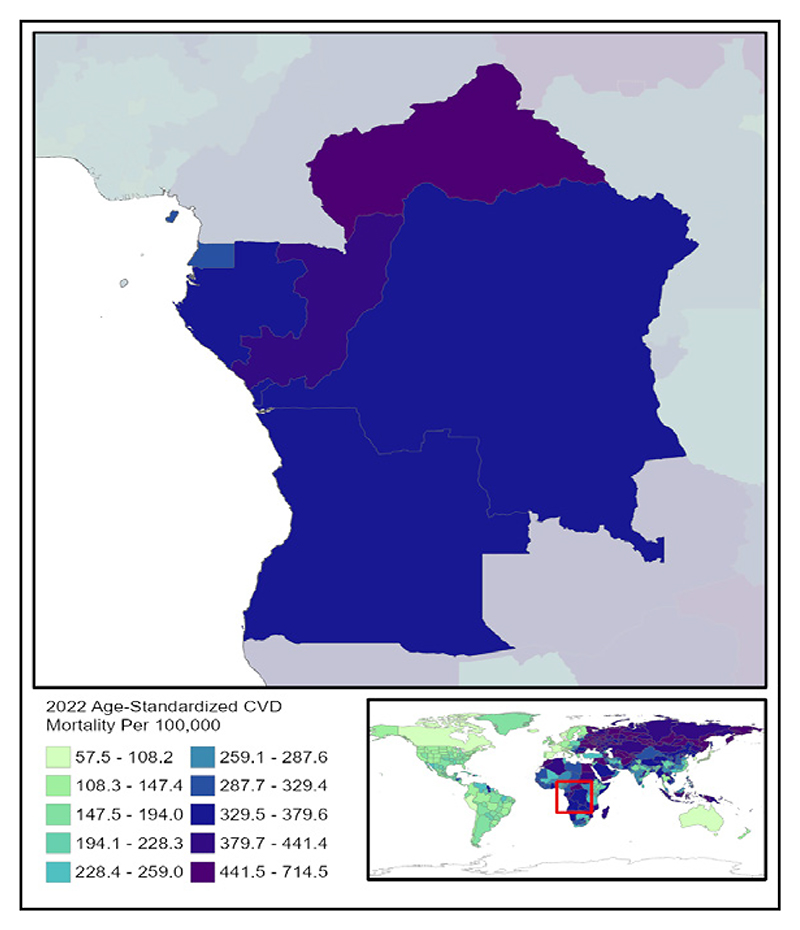
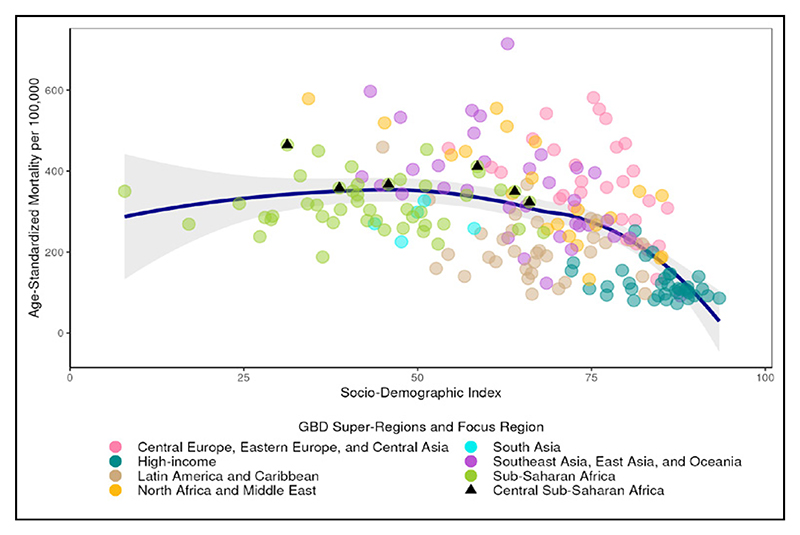
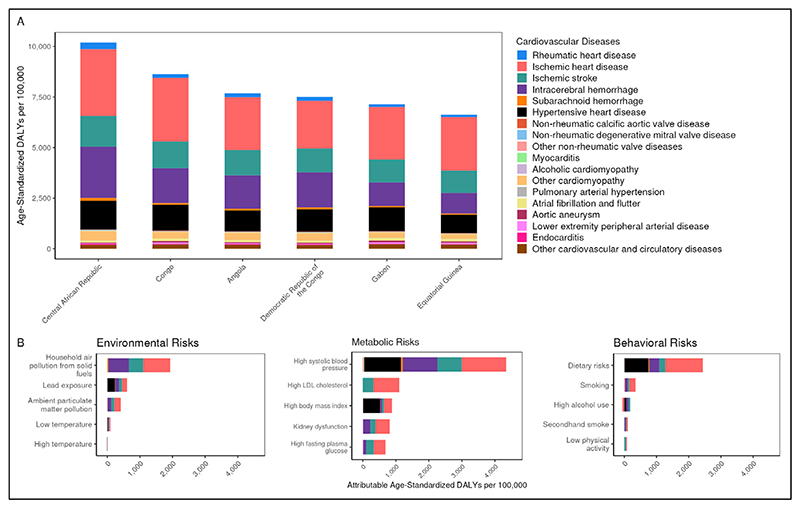
Age-standardized CVD mortality rates among countries in Central Sub-Saharan Africa ranged from 323.5 to 464.6 per 100,000 in 2022; a 1.4 fold difference. CVD mortality decreased by 12.3% from 1990 to 2022. Out of the 21 regions, Central Sub-Saharan Africa was ranked 6th in 1990 and 4th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 1,110.7 per 100,000. High systolic blood pressure accounted for the largest number of attributable age-standardized CVD DALYs at 4,339.8 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 1,906,645 | 3,030 | 1,380.7 | 5.1 | 201.0 |
| Ischemic heart disease | 2,207,929 | 51,104 | 3,464.7 | 121.9 | 2,491.6 |
| Ischemic stroke | 781,664 | 21,875 | 1,239.4 | 66.7 | 1,209.9 |
| Intracerebral hemorrhage | 225,657 | 37,452 | 259.0 | 76.5 | 1,730.8 |
| Subarachnoid hemorrhage | 66,885 | 1,827 | 77.0 | 3.0 | 92.2 |
| Hypertensive heart disease | 112,616 | 23,406 | 254.0 | 60.4 | 1,110.7 |
| Non-rheumatic calcific aortic valve disease | 7,840 | 578 | 14.4 | 1.5 | 27.2 |
| Non-rheumatic degenerative mitral valve disease | 7,619 | 423 | 13.8 | 0.9 | 19.5 |
| Other non-rheumatic valve diseases | 46 | 10 | <0.1 | <0.1 | 0.4 |
| Myocarditis | 5,594 | 256 | 5.1 | 0.3 | 11.5 |
| Alcoholic cardiomyopathy | 1,823 | 2 | 2.1 | <0.1 | 0.3 |
| Other cardiomyopathy | 116,974 | 8,352 | 112.0 | 15.5 | 387.0 |
| Pulmonary arterial hypertension | 1,727 | 134 | 1.8 | 0.2 | 6.1 |
| Atrial fibrillation and flutter | 198,070 | 1,357 | 443.8 | 4.8 | 98.8 |
| Aortic aneurysm | Not estimated | 999 | Not estimated | 2.2 | 45.6 |
| Lower extremity peripheral arterial disease | 306,848 | 612 | 726.1 | 1.8 | 33.3 |
| Endocarditis | 6,117 | 1,024 | 4.4 | 1.8 | 46.5 |
| Other cardiovascular and circulatory diseases | 1,122,426 | 1,897 | 1,885.0 | 3.5 | 178.8 |
Cardiovascular Disease in Eastern Sub-Saharan Africa
Findings from the Global Burden of Disease Study
Summary.
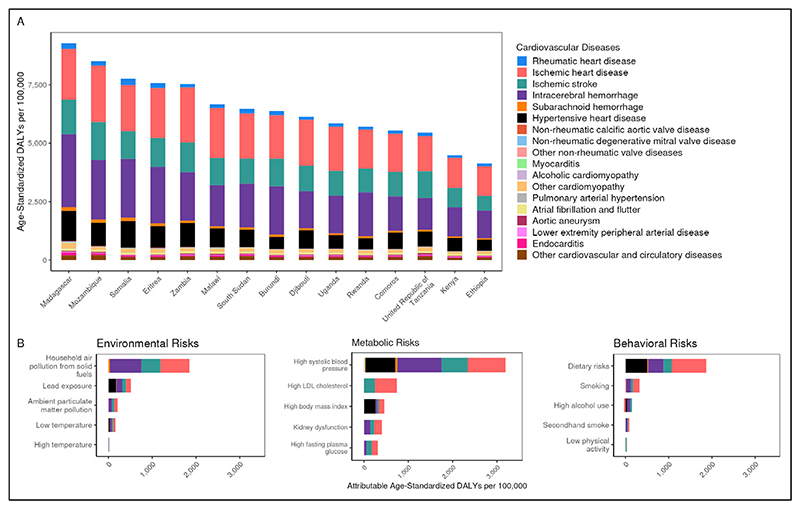
Age-standardized CVD mortality rates among countries in Eastern Sub-Saharan Africa ranged from 187.8 to 410.8 per 100,000 in 2022; a 2.2 fold difference. CVD mortality decreased by 23.6% from 1990 to 2022. Of the 21 regions, Eastern Sub-Saharan Africa ranked 10th in 1990 and 12th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 676.3 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 3,193.0 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
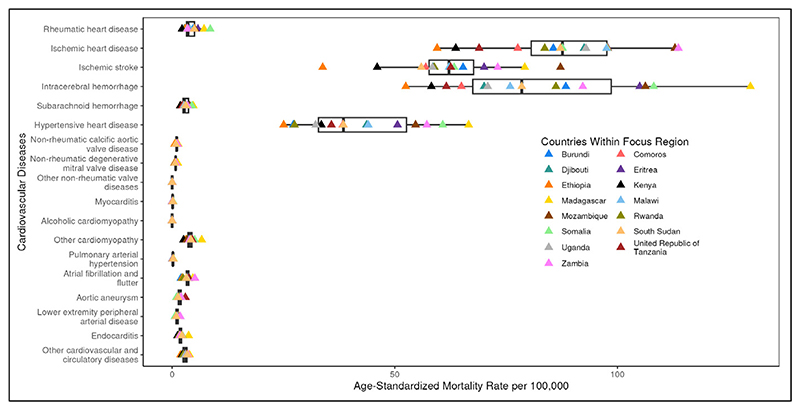
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 5,548,728 | 6,452 | 1,295.3 | 3.8 | 153.1 |
| Ischemic heart disease | 6,423,413 | 109,091 | 3,169.3 | 77.6 | 1,664.7 |
| Ischemic stroke | 2,297,408 | 61,695 | 1,147.3 | 54.1 | 997.6 |
| Intracerebral hemorrhage | 734,889 | 114,782 | 270.5 | 72.4 | 1,671.9 |
| Subarachnoid hemorrhage | 213,645 | 5,213 | 78.6 | 2.6 | 85.7 |
| Hypertensive heart disease | 512,396 | 46,238 | 349.8 | 36.4 | 676.3 |
| Non-rheumatic calcific aortic valve disease | 23,487 | 1,206 | 13.8 | 0.9 | 16.8 |
| Non-rheumatic degenerative mitral valve disease | 22,598 | 1,266 | 13.0 | 0.7 | 17.9 |
| Other non-rheumatic valve diseases | 273 | 23 | 0.1 | <0.1 | 0.3 |
| Myocarditis | 18,811 | 365 | 5.5 | 0.1 | 5.4 |
| Alcoholic cardiomyopathy | 9,559 | 3 | 3.1 | <0.1 | 0.3 |
| Other cardiomyopathy | 498,218 | 8,394 | 161.4 | 3.8 | 134.5 |
| Pulmonary arterial hypertension | 6,099 | 453 | 2.1 | 0.2 | 6.4 |
| Atrial fibrillation and flutter | 578,307 | 3,044 | 400.7 | 3.2 | 71.7 |
| Aortic aneurysm | Not estimated | 2,549 | Not estimated | 1.7 | 35.8 |
| Lower extremity peripheral arterial disease | 933,431 | 1,280 | 675.1 | 1.1 | 21.9 |
| Endocarditis | 33,390 | 4,027 | 7.0 | 1.9 | 57.3 |
| Other cardiovascular and circulatory diseases | 2,582,036 | 5,139 | 1,283.6 | 2.7 | 135.9 |
Cardiovascular Disease in Southern Sub-Saharan Africa
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Southern Sub-Saharan Africa ranged from 248.3 to 453.3 per 100,000 in 2022; a 1.8 fold difference. CVD mortality increased by 8.0% from 1990 to 2022. Of the 21 regions, Southern Sub-Saharan Africa ranked 18th in 1990 and 9th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 839.6 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 3,138.2 per 100,000.
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
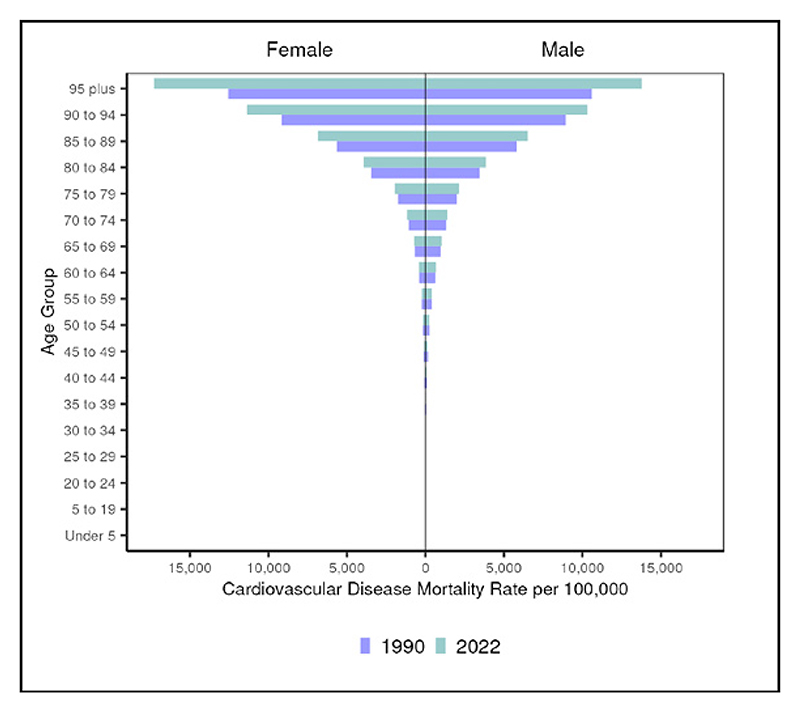
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
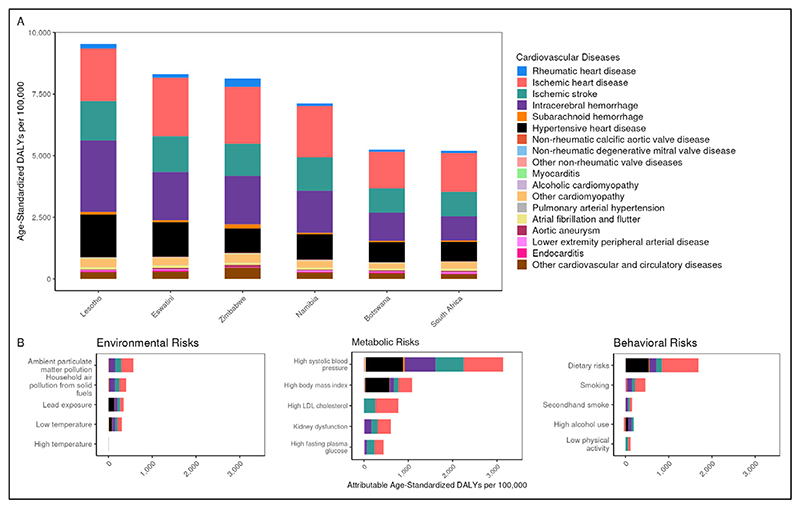
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
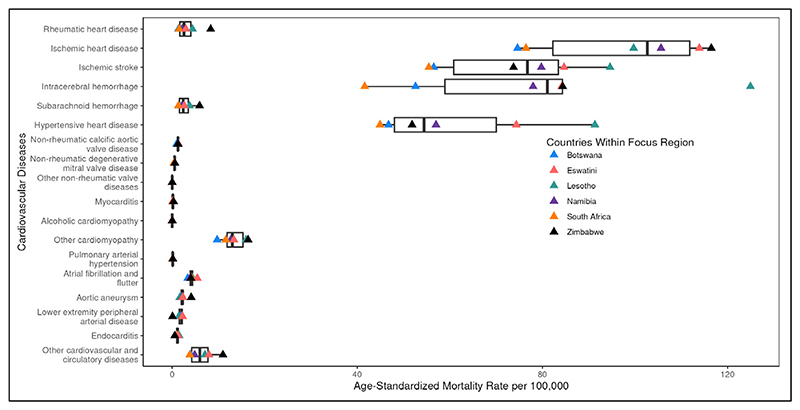
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 722,444 | 1,682 | 847.1 | 2.5 | 133.9 |
| Ischemic heart disease | 1,857,089 | 38,915 | 2,992.7 | 81.5 | 1,680.0 |
| Ischemic stroke | 800,106 | 23,969 | 1,339.5 | 58.6 | 1,038.3 |
| Intracerebral hemorrhage | 144,626 | 26,826 | 206.0 | 49.0 | 1,166.8 |
| Subarachnoid hemorrhage | 40,248 | 1,181 | 54.0 | 2.0 | 63.1 |
| Hypertensive heart disease | 80,643 | 21,221 | 153.2 | 47.1 | 839.6 |
| Non-rheumatic calcific aortic valve disease | 13,379 | 545 | 23.1 | 1.3 | 22.0 |
| Non-rheumatic degenerative mitral valve disease | 7,705 | 232 | 12.4 | 0.4 | 11.6 |
| Other non-rheumatic valve diseases | 22 | 8 | <0.1 | <0.1 | 0.4 |
| Myocarditis | 4,353 | 94 | 5.9 | 0.1 | 6.3 |
| Alcoholic cardiomyopathy | 374 | 4 | 0.5 | <0.1 | 0.2 |
| Other cardiomyopathy | 67,206 | 6,134 | 91.0 | 12.1 | 276.7 |
| Pulmonary arterial hypertension | 1,625 | 66 | 2.3 | 0.1 | 3.9 |
| Atrial fibrillation and flutter | 263,389 | 1,435 | 510.9 | 4.2 | 89.4 |
| Aortic aneurysm | Not estimated | 1,246 | Not estimated | 2.5 | 50.5 |
| Lower extremity peripheral arterial disease | 488,286 | 940 | 973.7 | 2.0 | 42.8 |
| Endocarditis | 3,338 | 614 | 4.1 | 0.9 | 33.3 |
| Other cardiovascular and circulatory diseases | 1,460,546 | 2,386 | 2,458.0 | 4.7 | 225.9 |
Cardiovascular Disease in Western Sub-Saharan Africa
Findings from the Global Burden of Disease Study
Summary.
Age-standardized CVD mortality rates among countries in Western Sub-Saharan Africa ranged from 238.1 to 449.7 per 100,000 in 2022; a 1.9 fold difference. CVD mortality decreased by 19.9% from 1990 to 2022. Of the 21 regions, Western Sub-Saharan Africa ranked 9th in 1990 and 8th in 2022 for age-standardized CVD mortality. After ischemic heart disease and all stroke subtypes, hypertensive heart disease had the highest age-standardized DALYs in 2022 at 593.8 per 100,000. High systolic blood pressure had the largest number of attributable age-standardized CVD DALYs at 3,330.4 per 100,000
Figure 1.
Regional map of 2022 age-standardized cardiovascular disease mortality rate per 100,000 with quantile classification
Figure 2.
Regional cardiovascular disease mortality rate per 100,000 by age and sex in 1990 vs. 2022
Figure 3.
Age-standardized cardiovascular disease mortality rate per 100,000 by country (circle) in 2022 by socio-demographic index (0-100), a composite indicator of fertility, income, and education. Focus region countries indicated by triangles, loess line in blue with shaded 95% uncertainty interval.
Figure 4.
Age-standardized disability-adjusted life years (DALYs) per 100,000 in 2022 for (A) cardiovascular diseases by country and (B) burden attributable to selected risk factors, for the region, compared to the theoretical minimum risk exposure level
Figure 5.
Age-standardized mortality rate per 100,000 for cardiovascular diseases in 2022 by cause of death and country. Boxplot shows first quartile, median, and third quartile of mortality range.
Table 1.
Regional cardiovascular disease in 2022: counts and age-standardized rates per 100,000. Results, uncertainty intervals, and methods available online.
| Cardiovascular Disease Type | Prevalent Cases (Count) | Deaths (Count) | Prevalence (Rate) | Deaths (Rate) | Disability-Adjusted Life Years (DALYs, Rate) |
|---|---|---|---|---|---|
| Rheumatic heart disease | 4,640,580 | 5,175 | 963.3 | 2.3 | 108.1 |
| Ischemic heart disease | 7,452,708 | 144,797 | 3,228.8 | 94.4 | 1,824.3 |
| Ischemic stroke | 3,203,095 | 82,875 | 1,240.4 | 60.9 | 1,114.1 |
| Intracerebral hemorrhage | 1,065,970 | 118,256 | 336.7 | 62.8 | 1,478.2 |
| Subarachnoid hemorrhage | 230,618 | 5,777 | 73.8 | 2.5 | 81.3 |
| Hypertensive heart disease | 496,314 | 47,933 | 289.7 | 29.3 | 593.8 |
| Non-rheumatic calcific aortic valve disease | 24,823 | 1,650 | 11.3 | 1.1 | 19.3 |
| Non-rheumatic degenerative mitral valve disease | 28,895 | 1,077 | 13.0 | 0.6 | 13.0 |
| Other non-rheumatic valve diseases | 220 | 27 | 0.1 | <0.1 | 0.3 |
| Myocarditis | 26,383 | 478 | 6.1 | 0.1 | 5.8 |
| Alcoholic cardiomyopathy | 10,332 | 139 | 3.1 | 0.1 | 2.1 |
| Other cardiomyopathy | 312,714 | 16,486 | 83.9 | 8.2 | 204.8 |
| Pulmonary arterial hypertension | 9,646 | 444 | 3.0 | 0.1 | 5.4 |
| Atrial fibrillation and flutter | 809,397 | 4,749 | 474.5 | 4.6 | 88.4 |
| Aortic aneurysm | Not estimated | 3,377 | Not estimated | 2.0 | 40.0 |
| Lower extremity peripheral arterial disease | 1,166,933 | 1,641 | 708.6 | 1.3 | 23.1 |
| Endocarditis | 25,587 | 3,241 | 5.3 | 1.4 | 39.6 |
| Other cardiovascular and circulatory diseases | 5,350,530 | 14,280 | 2,502.3 | 7.4 | 293.3 |
Aggregate Cause: Cardiovascular Disease
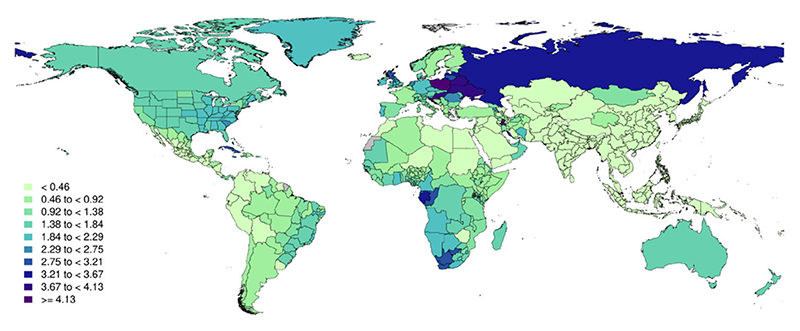
Figure 1.
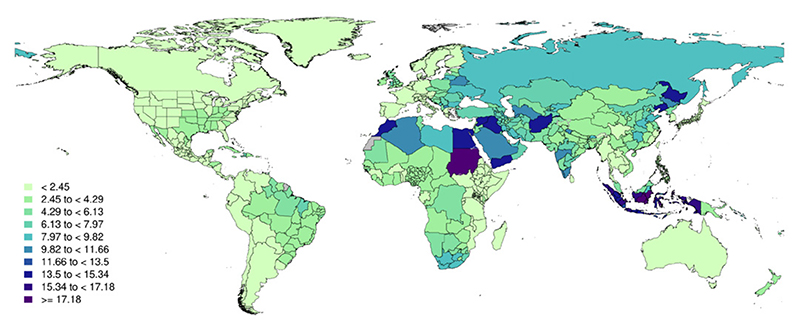
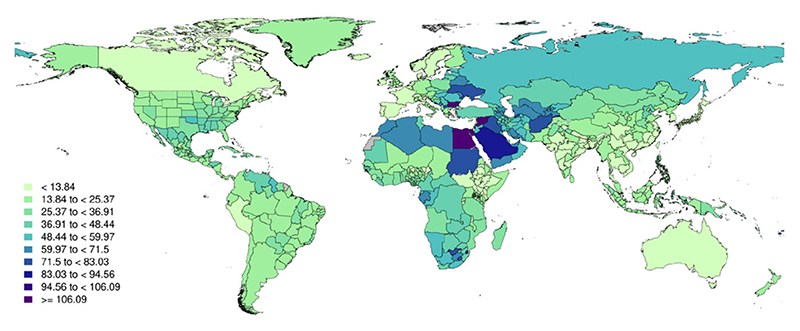
Global map of age–standardized cardiovascular disease mortality rate per 100,000 in 2022 with equal interval classification
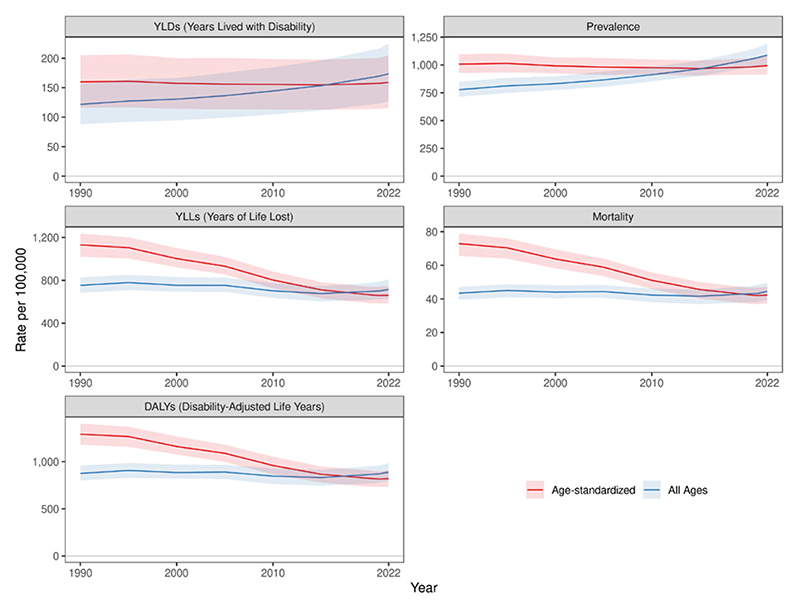
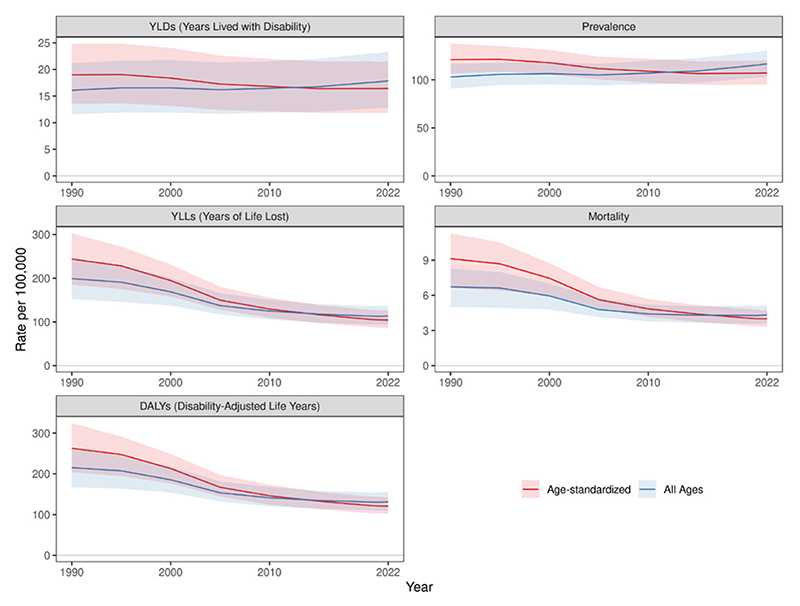
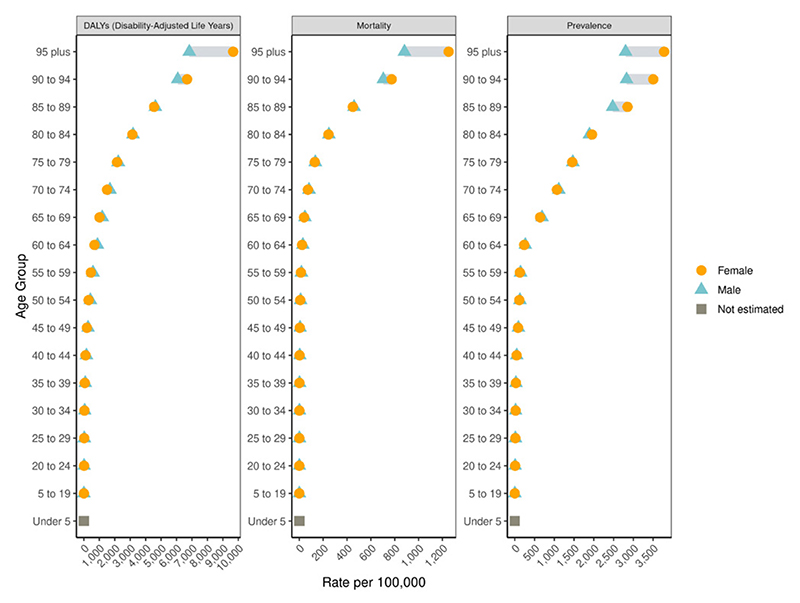
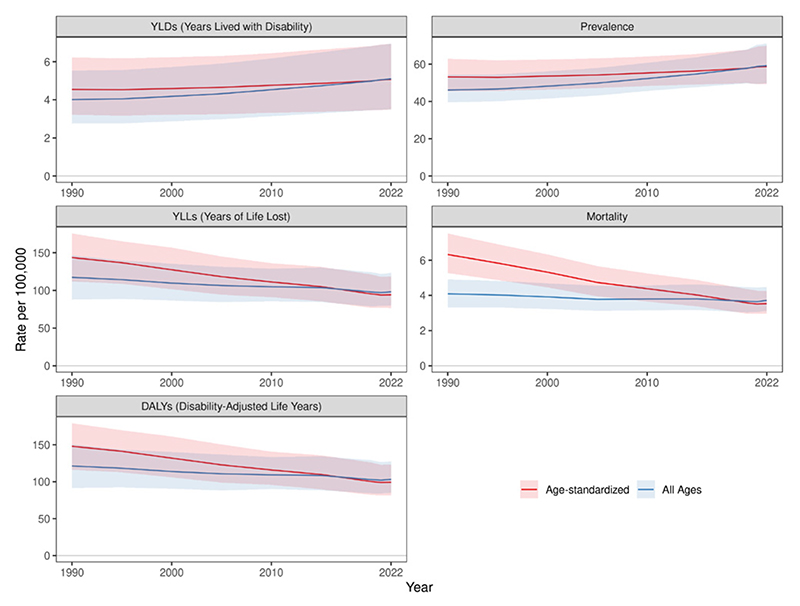
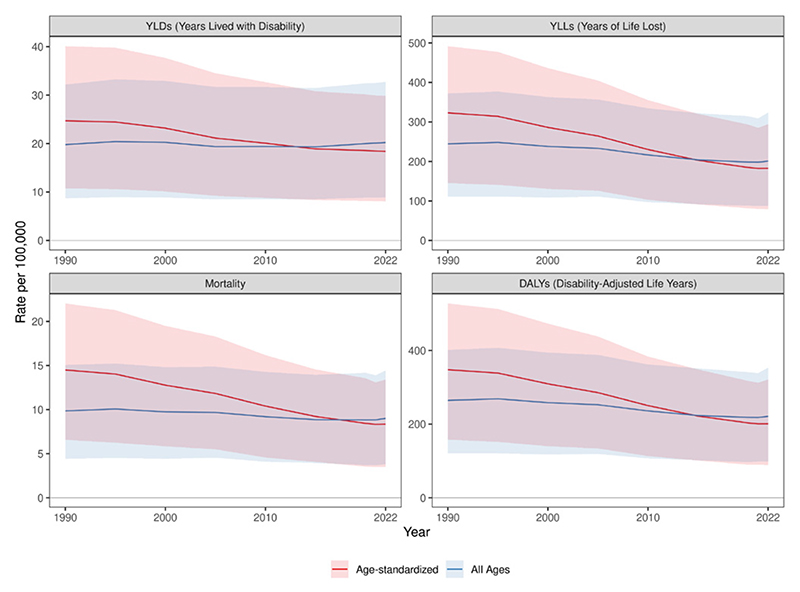
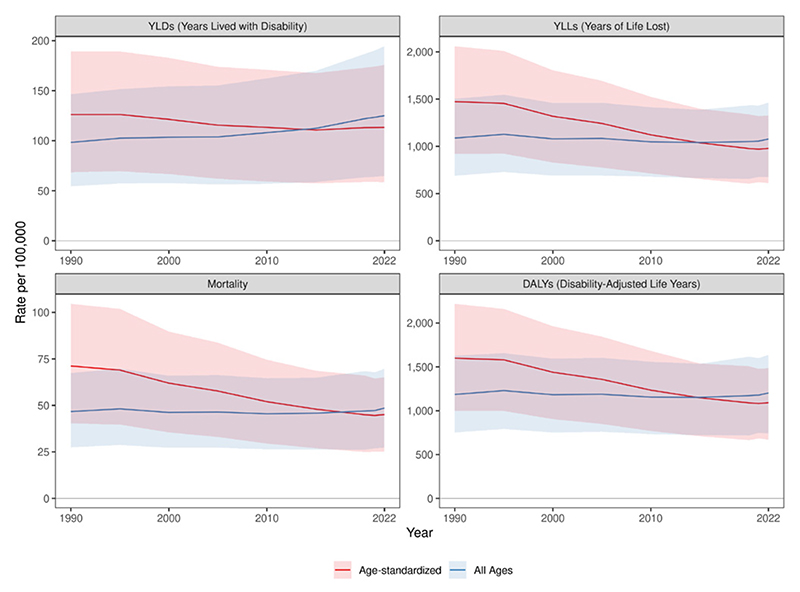
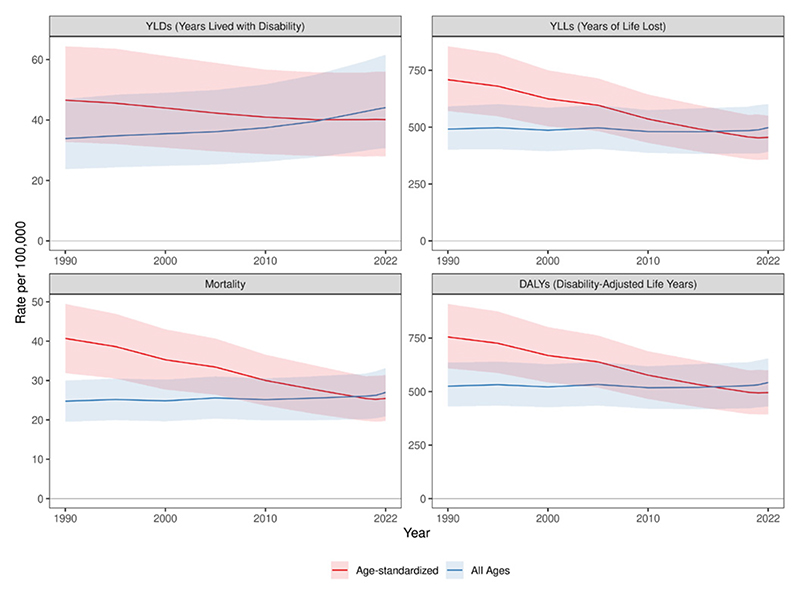
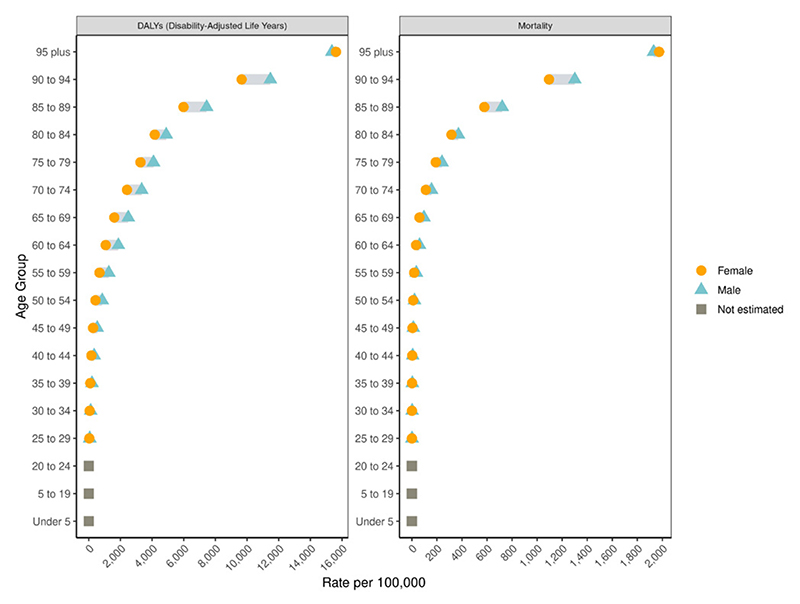
Figure 2.
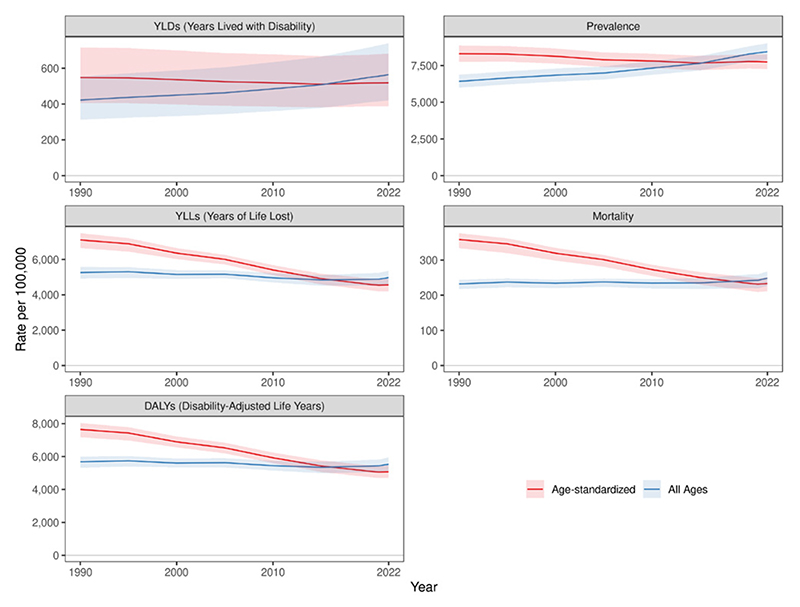
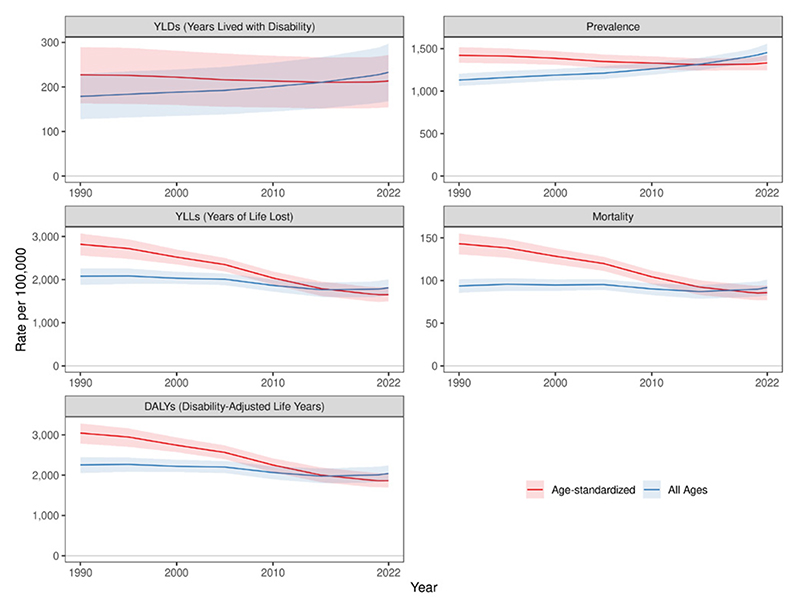
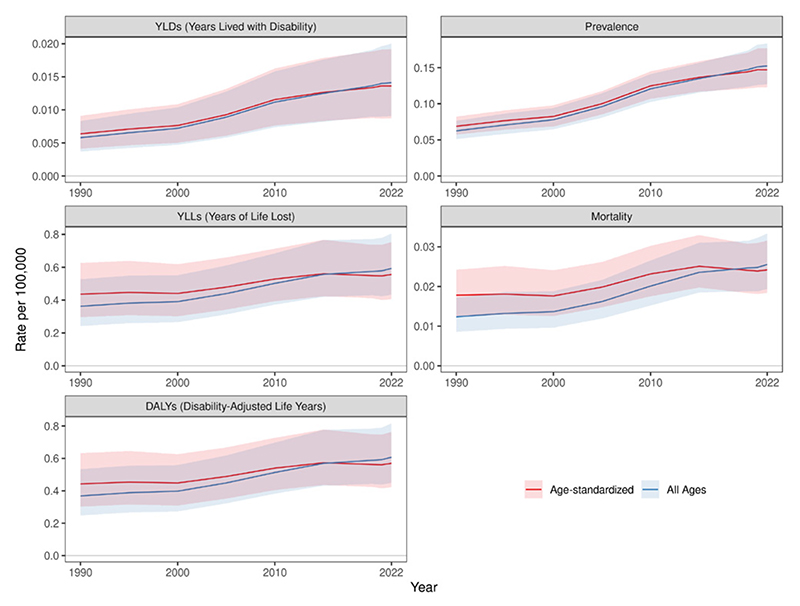
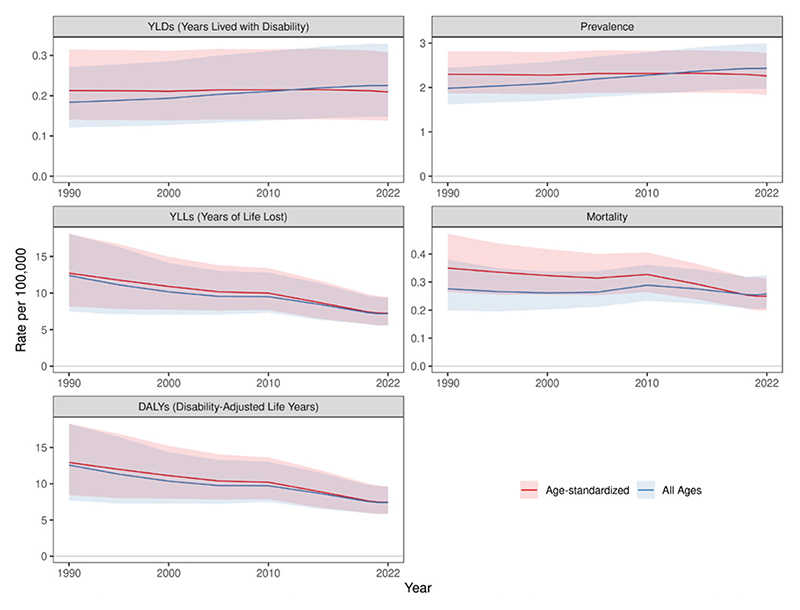
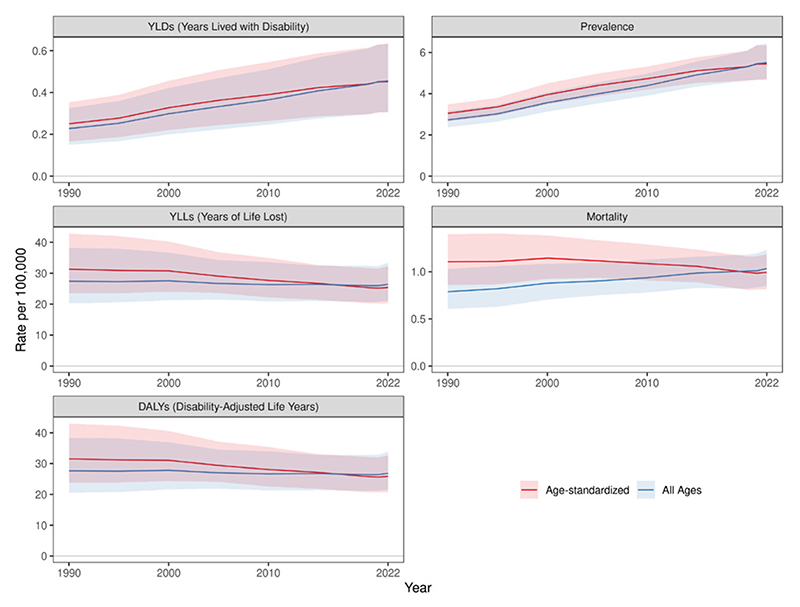
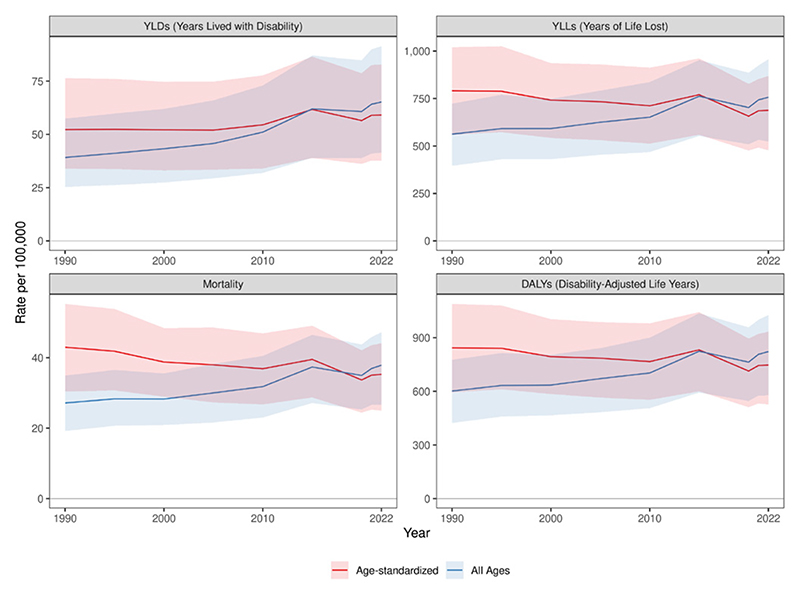
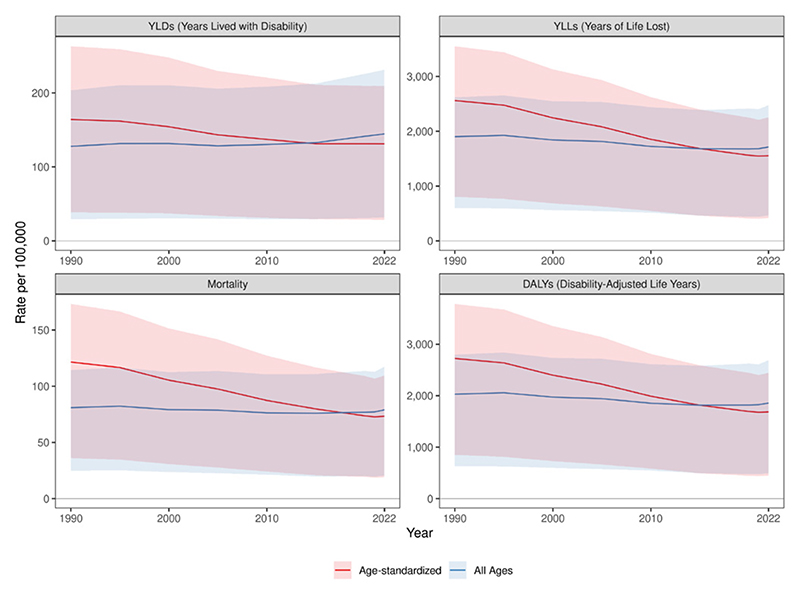
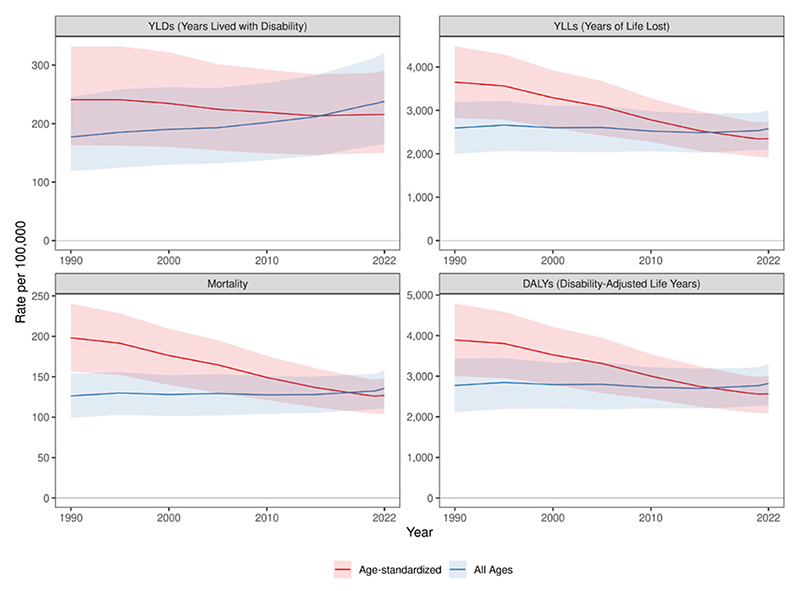
Global cardiovascular disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
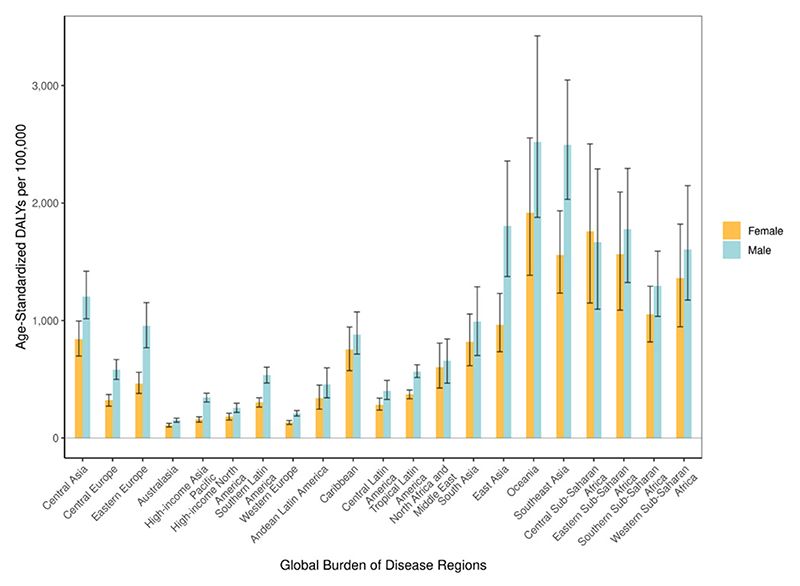
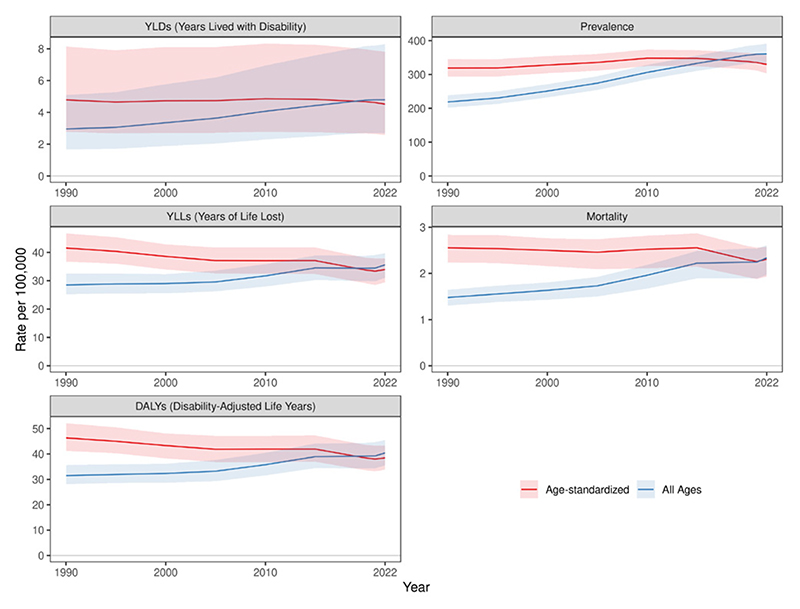
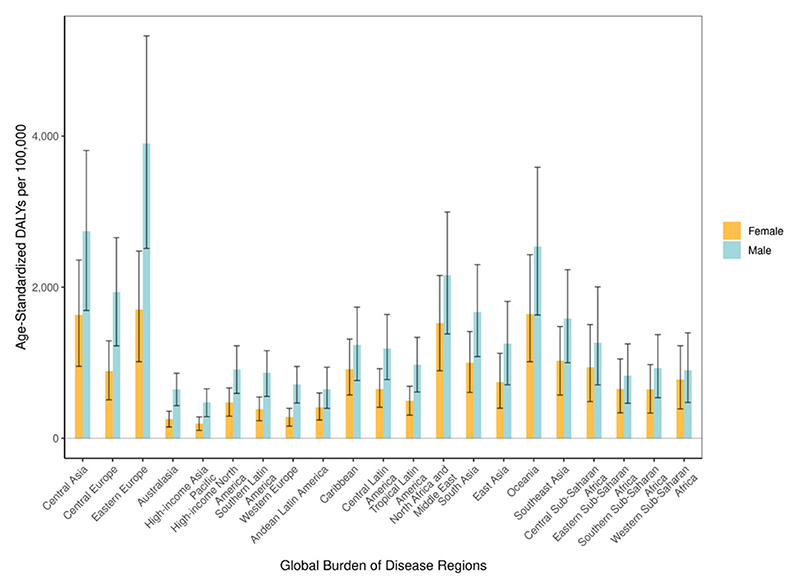
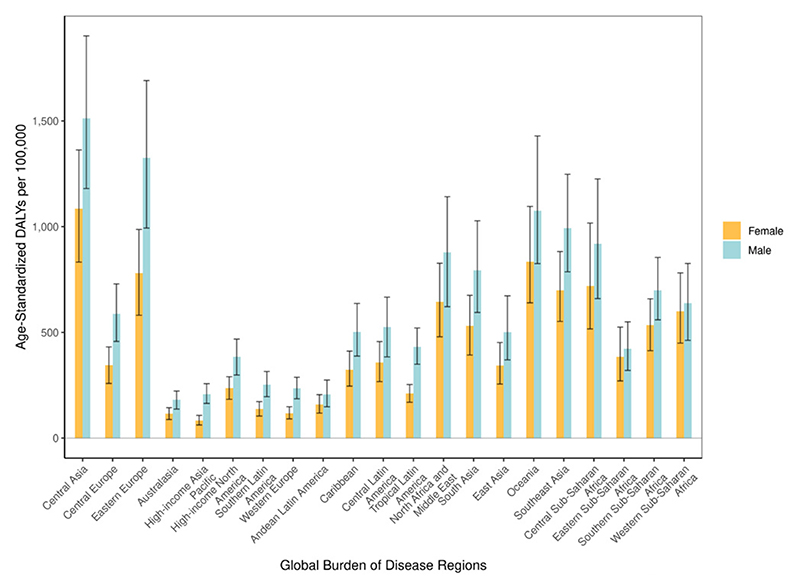
Figure 3.
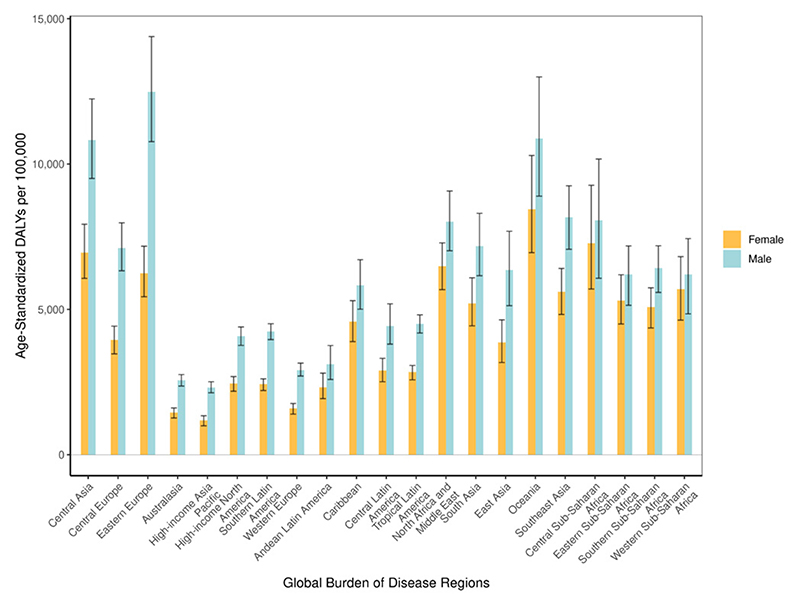
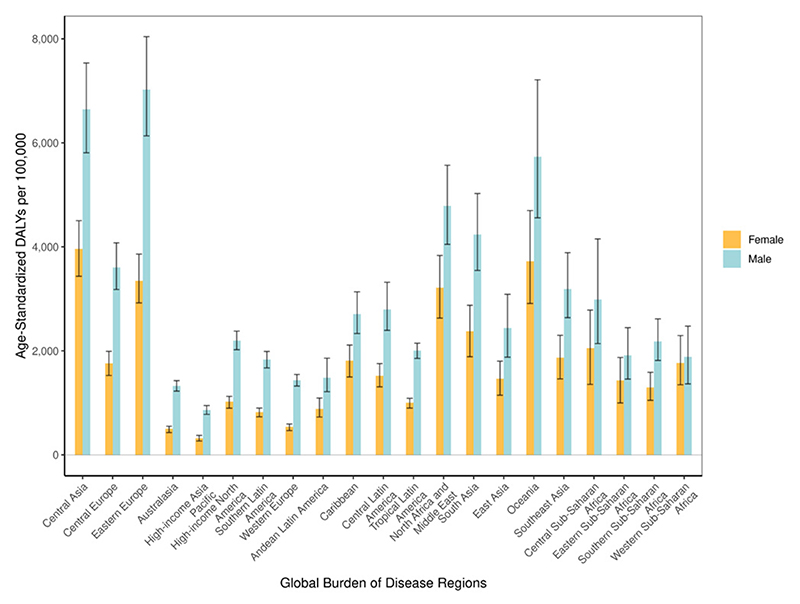
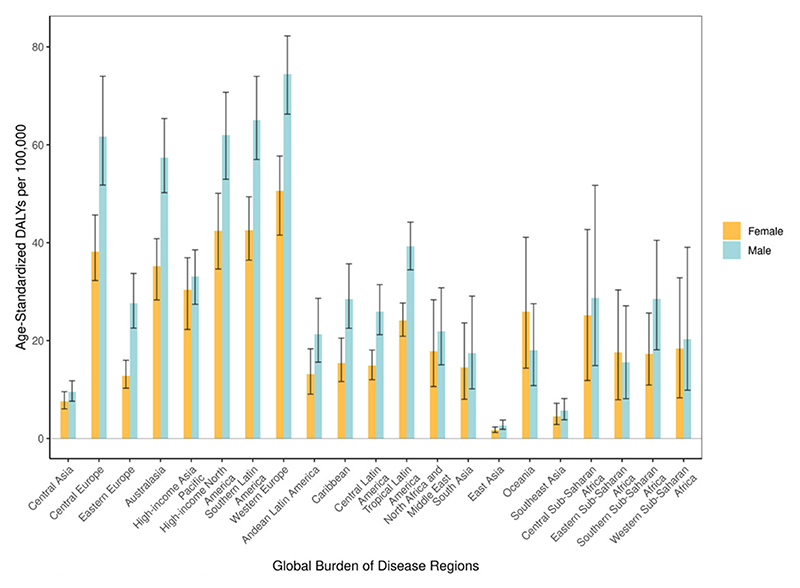
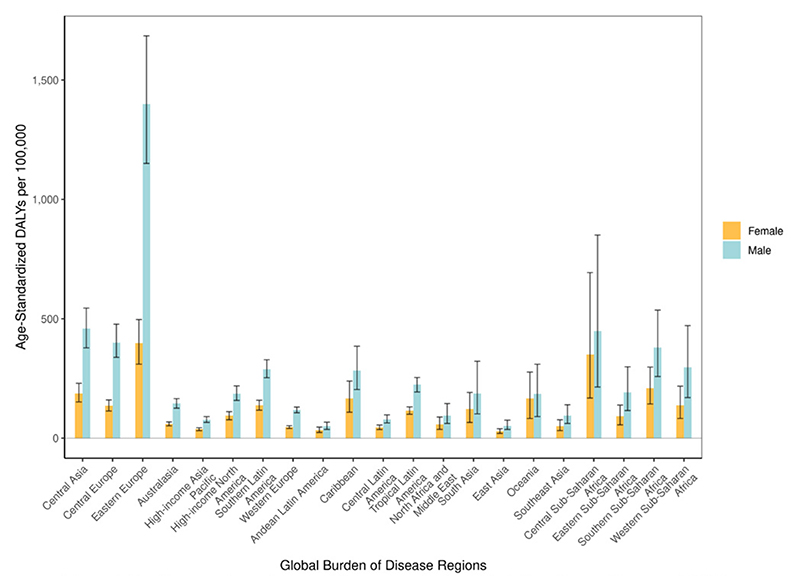
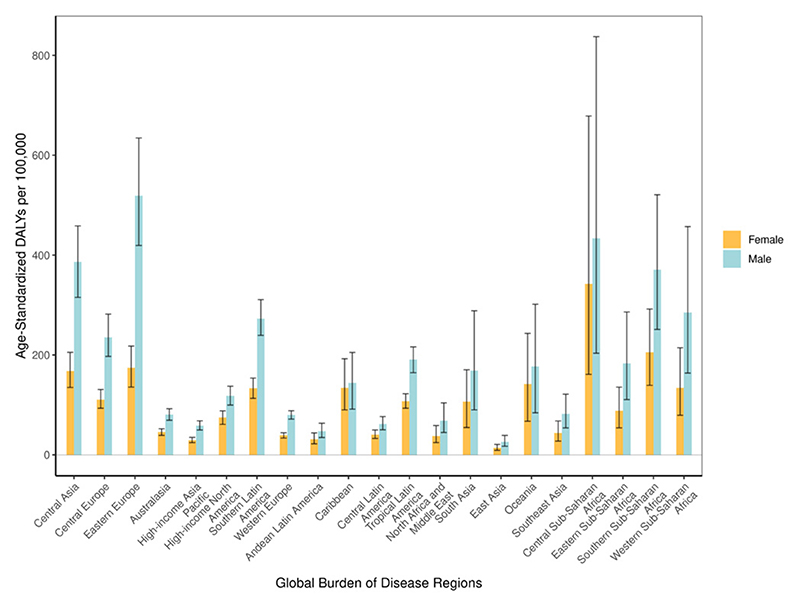
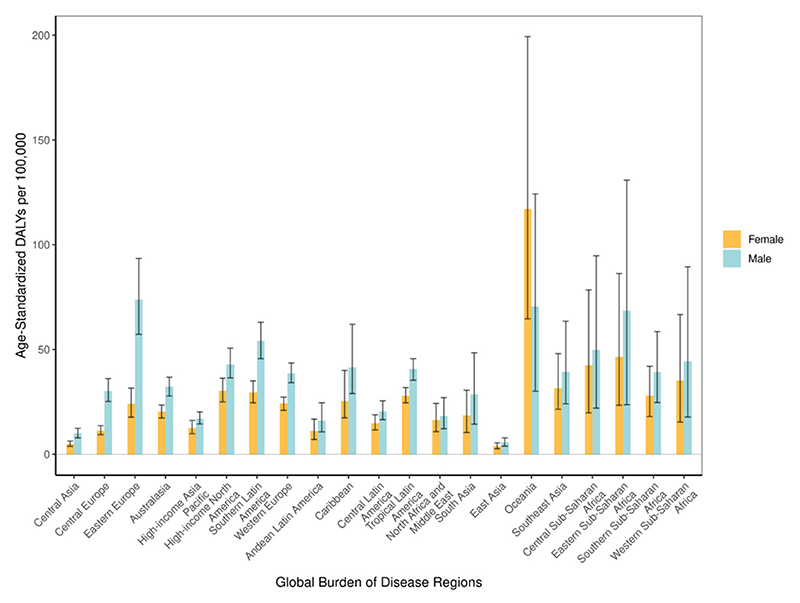
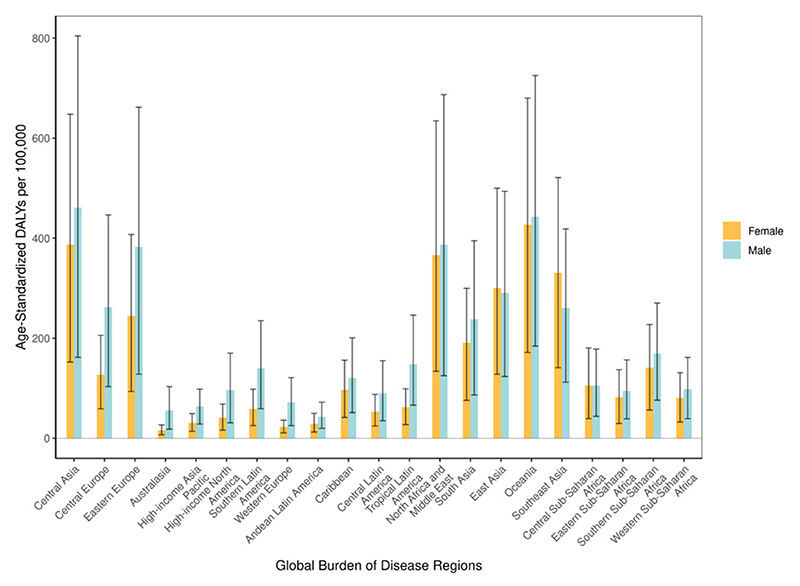
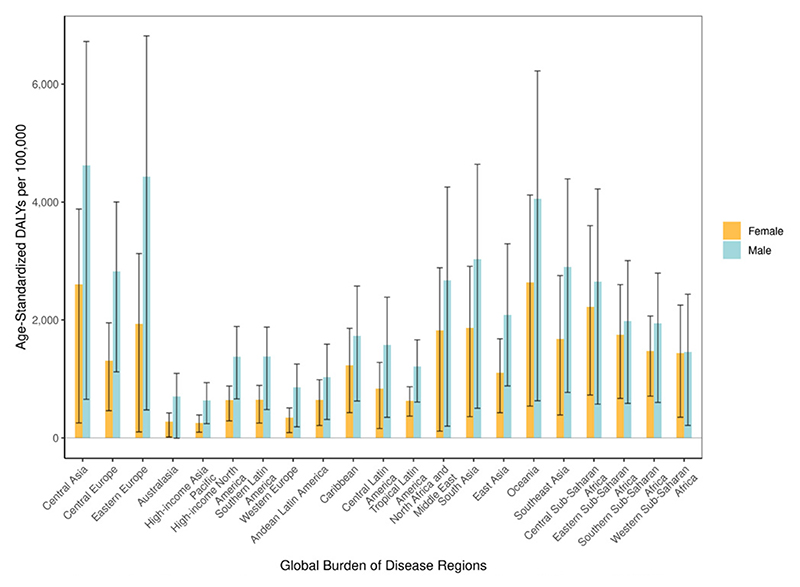
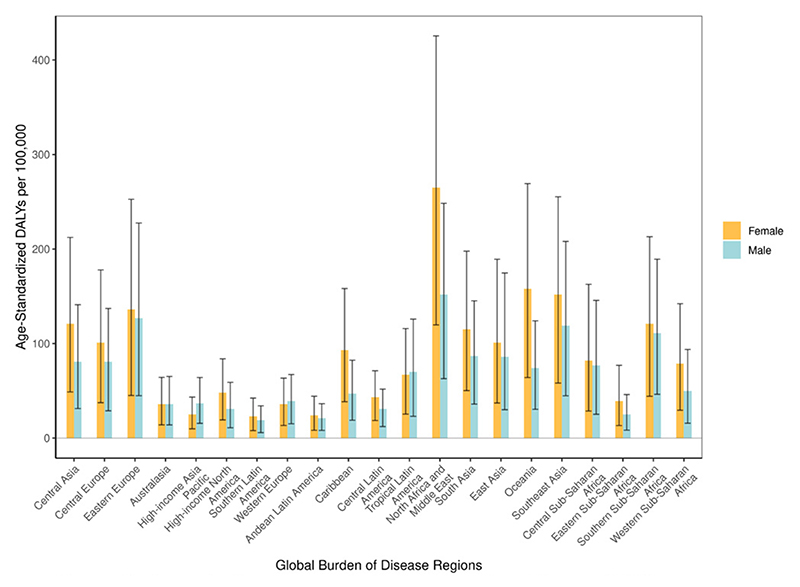
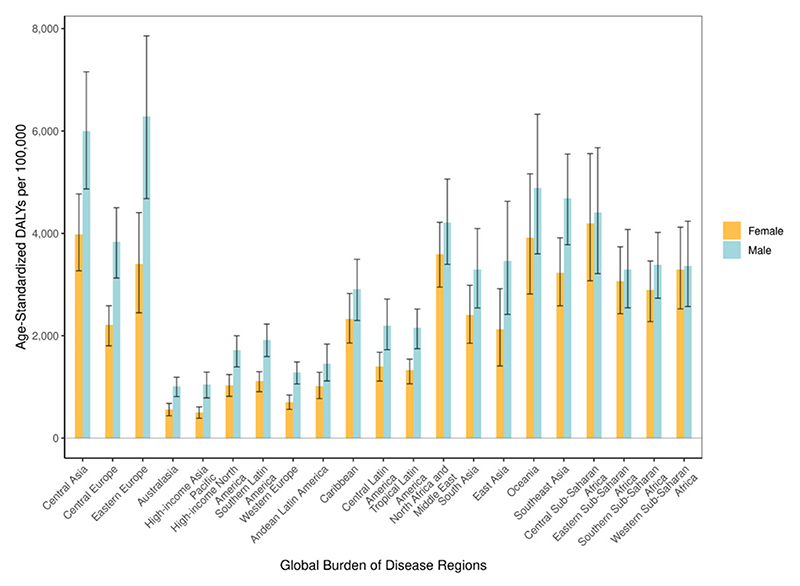
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
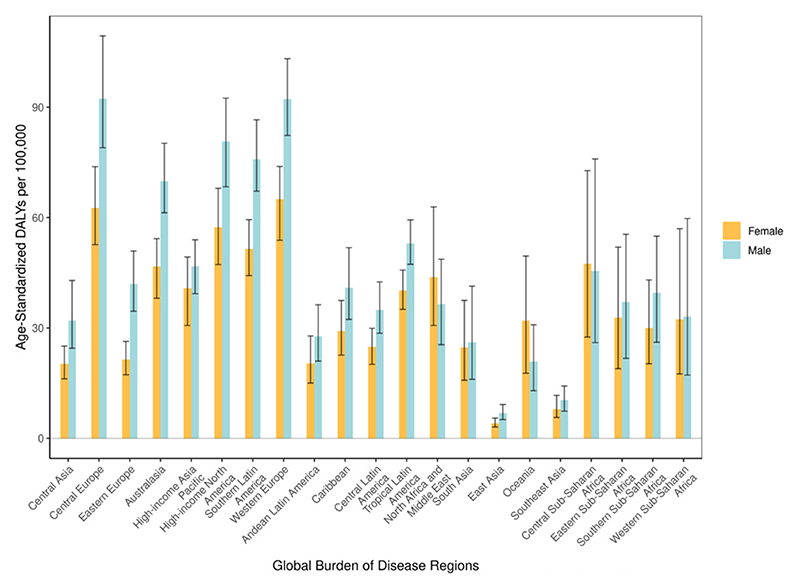
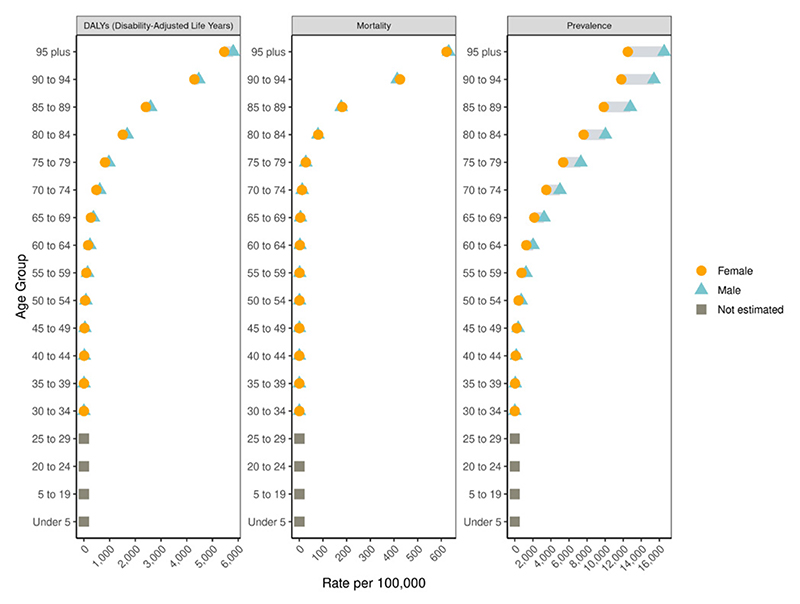
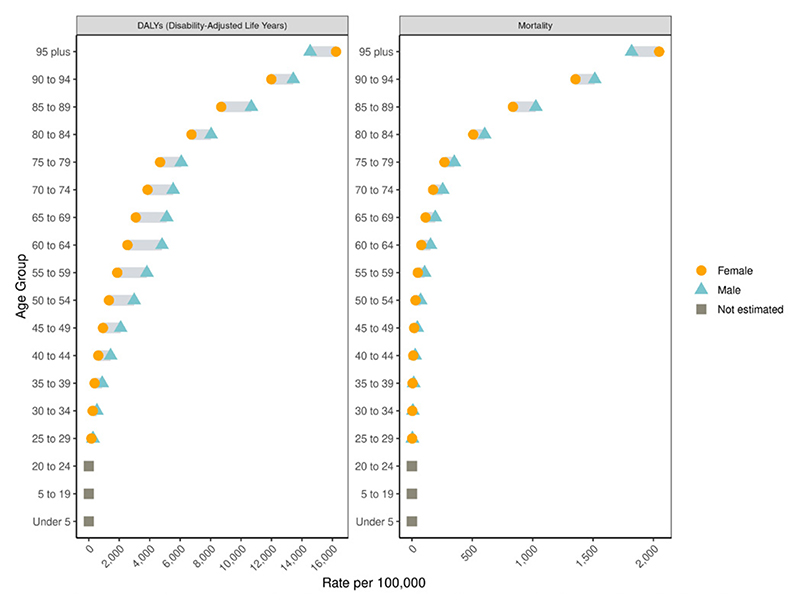
Figure 4.
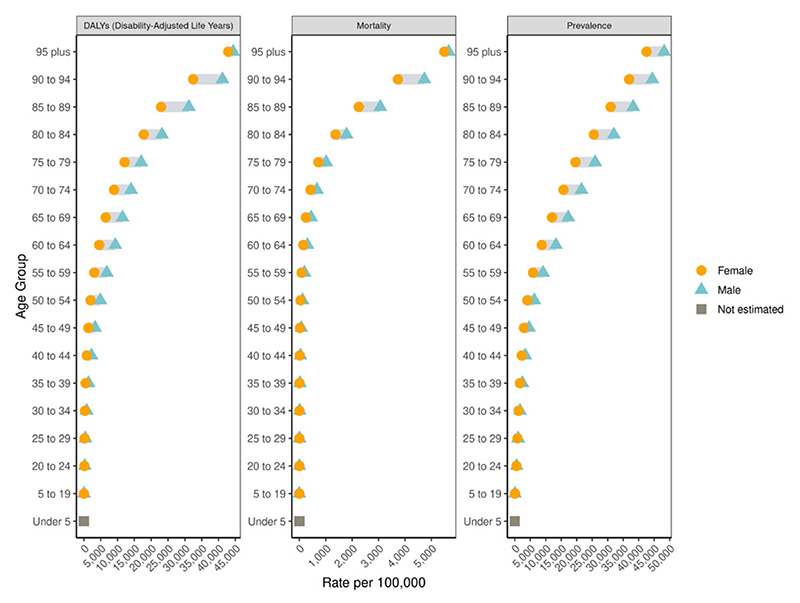
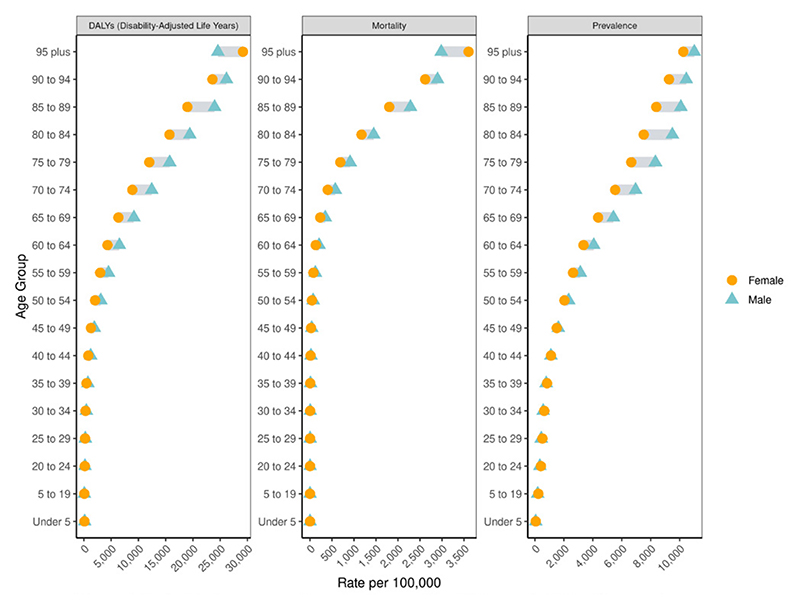
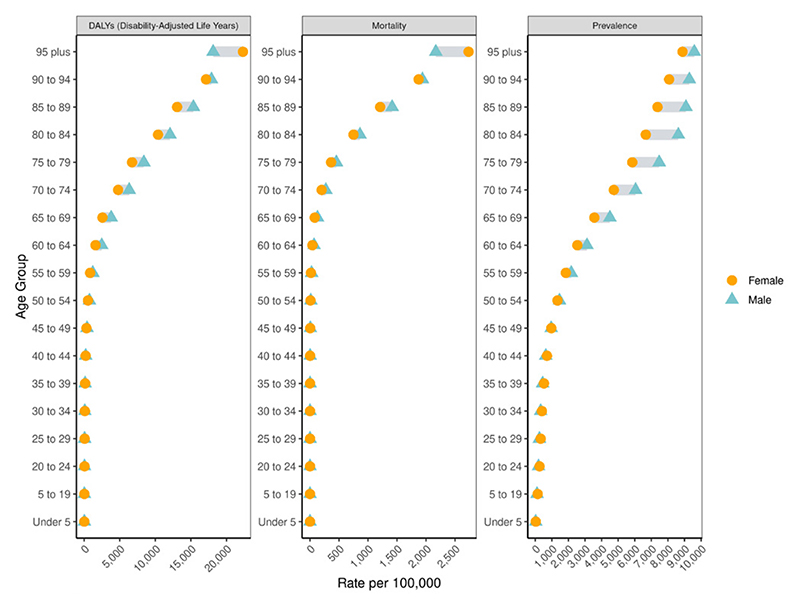
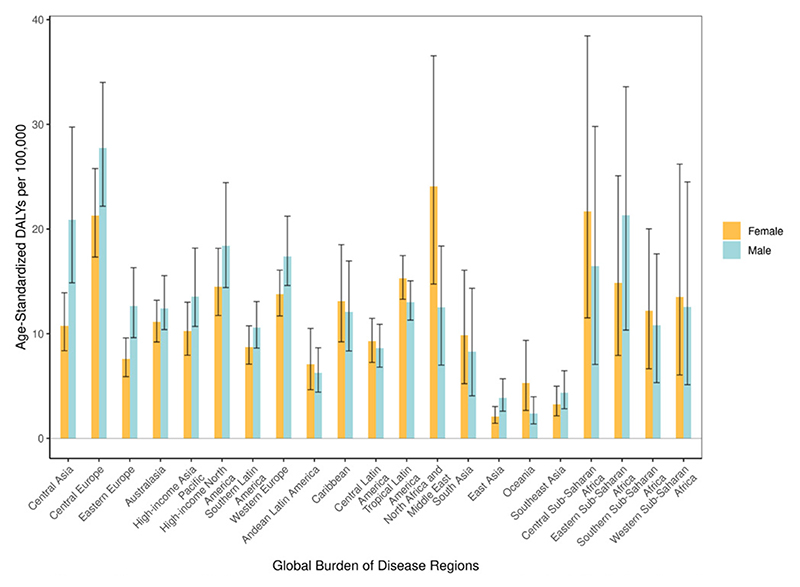
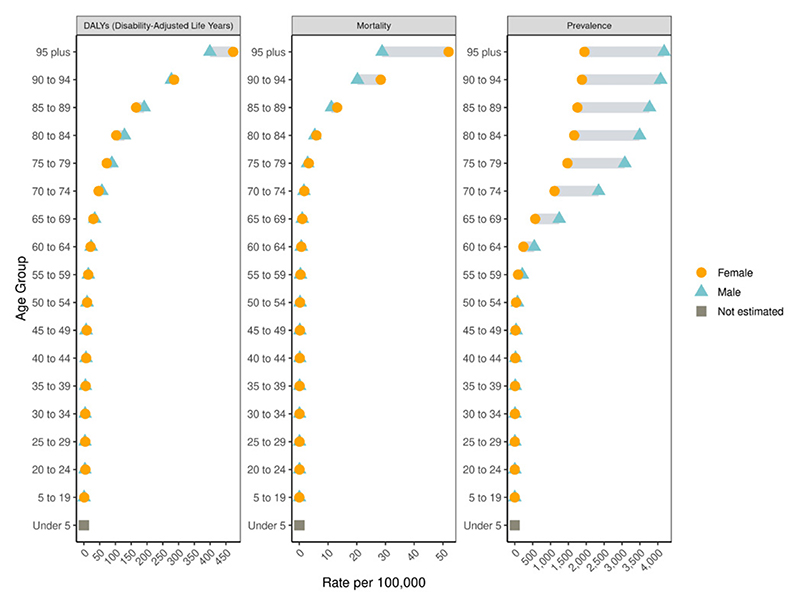
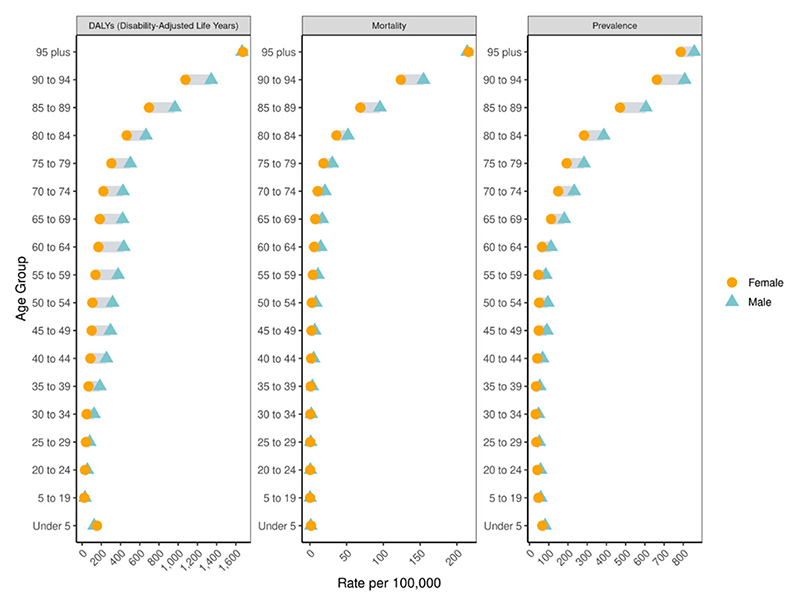
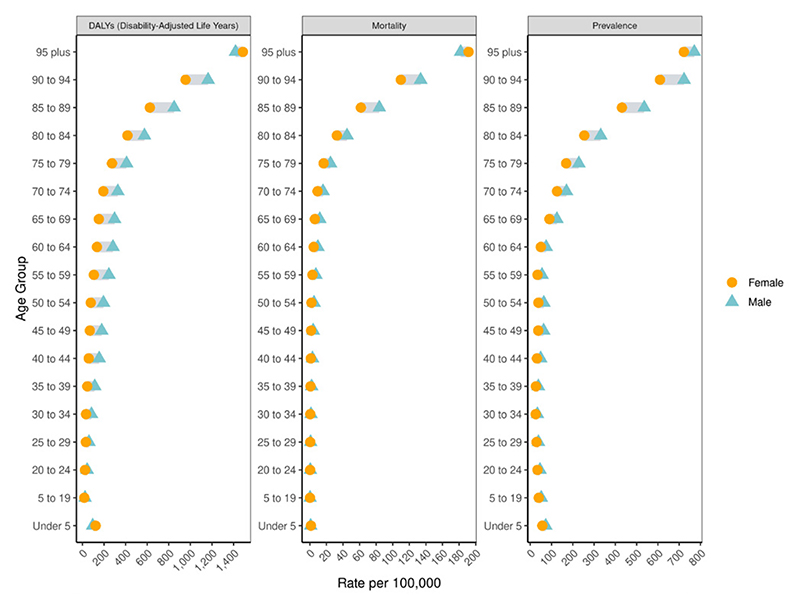
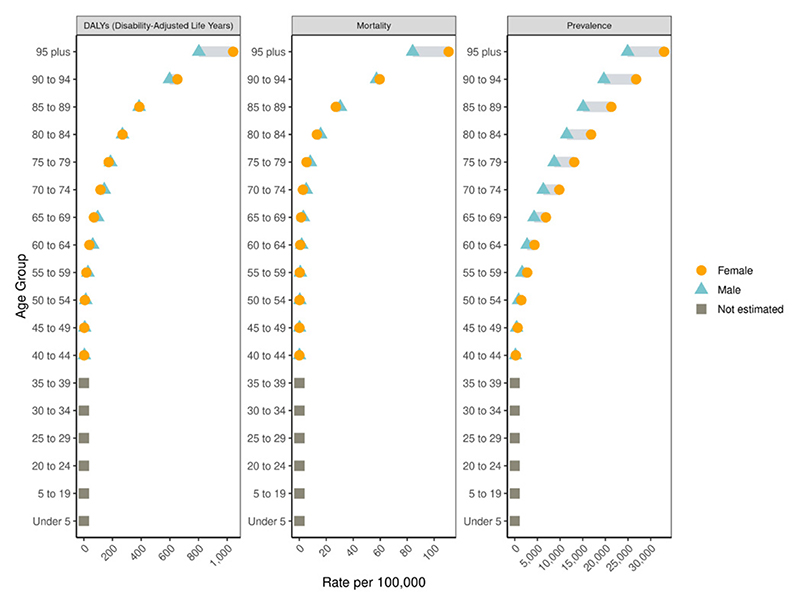
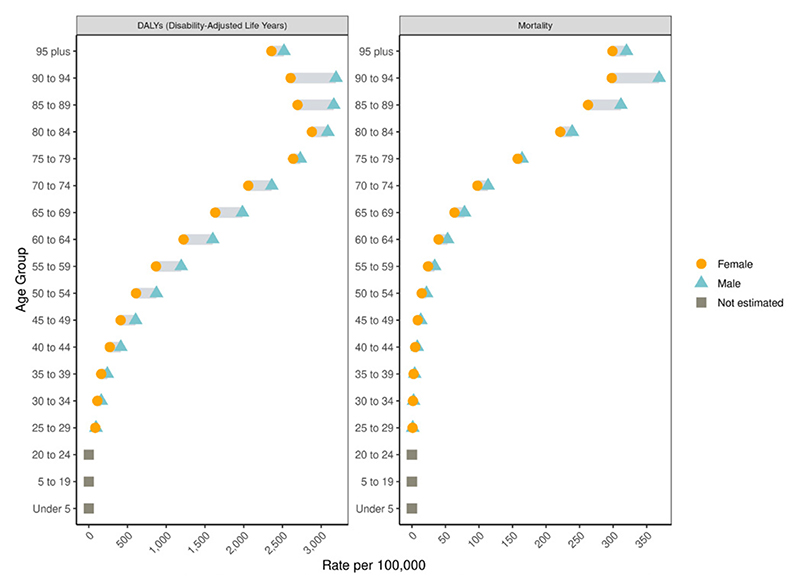
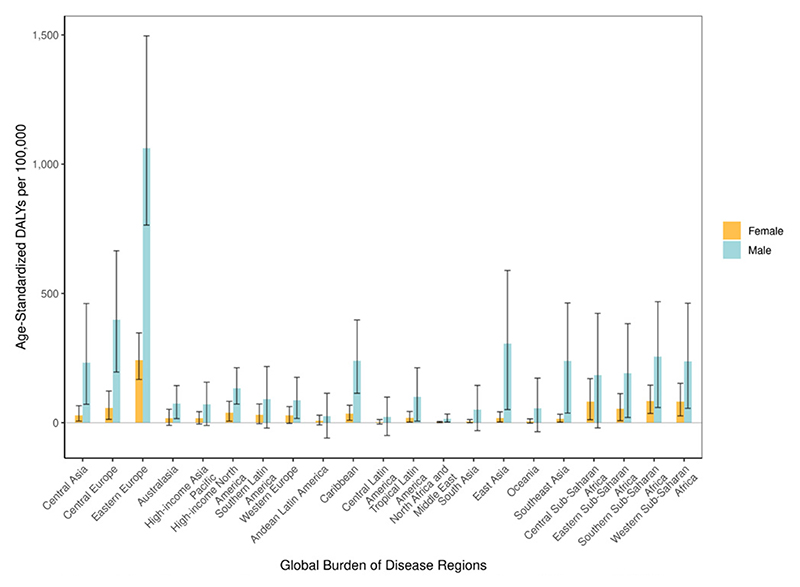
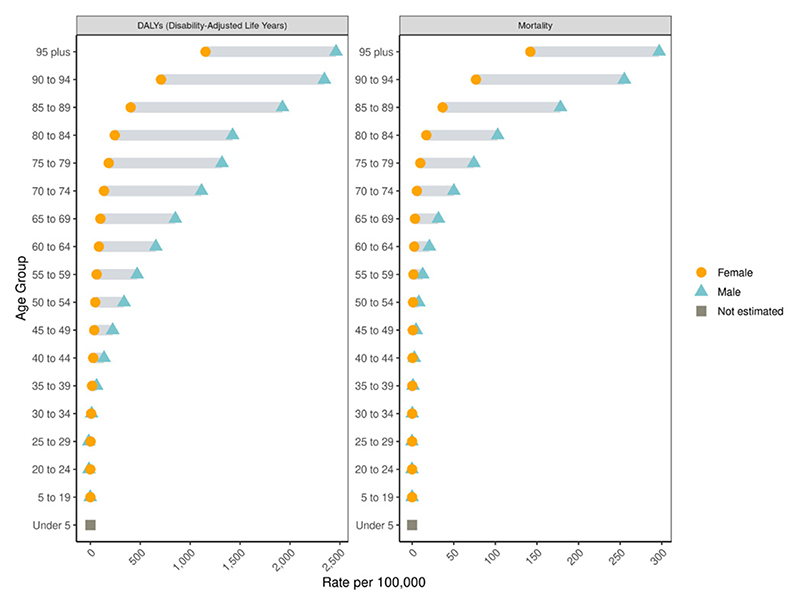
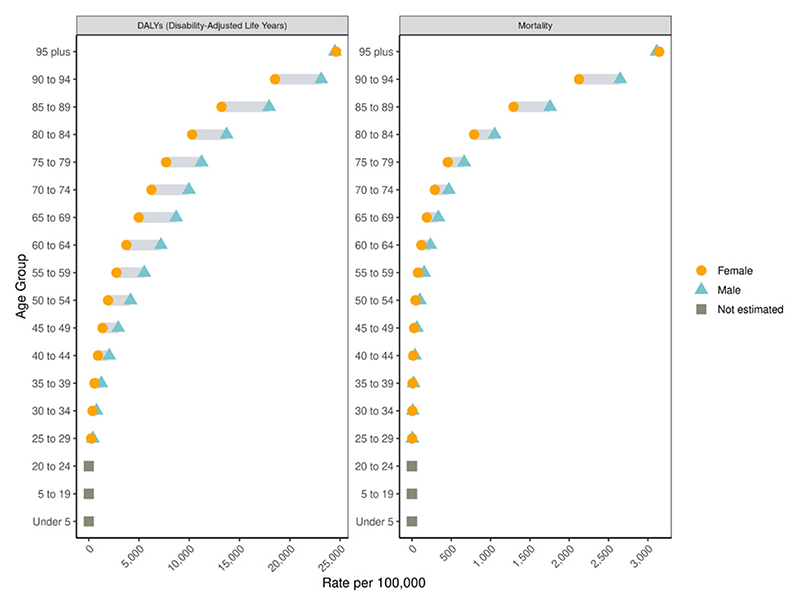
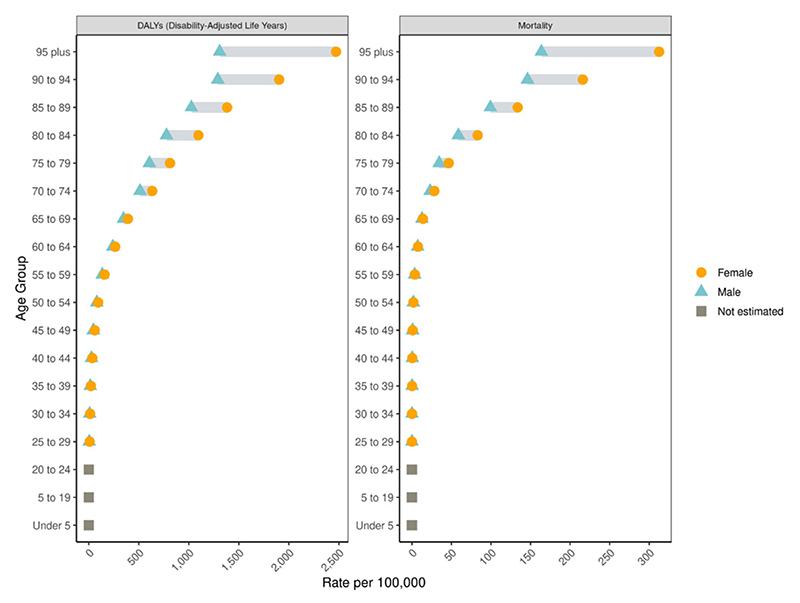
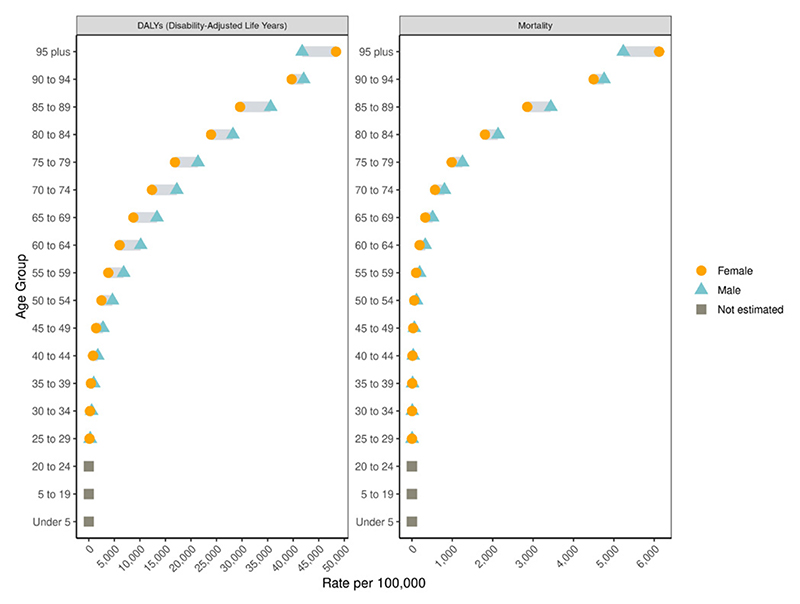
Global cardiovascular disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Rheumatic Heart Disease
Figure 1.
Global map of age-standardized rheumatic heart disease mortality rate per 100,000 in 2022 with equal interval classification
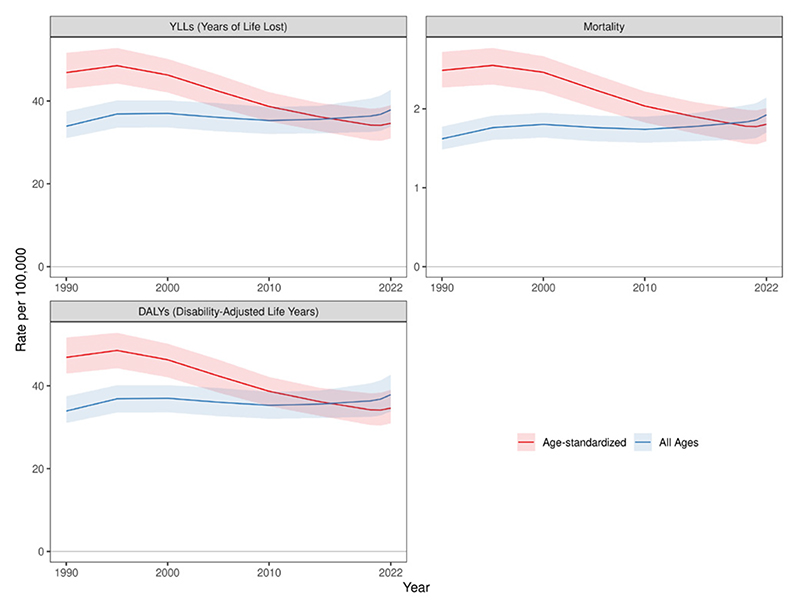
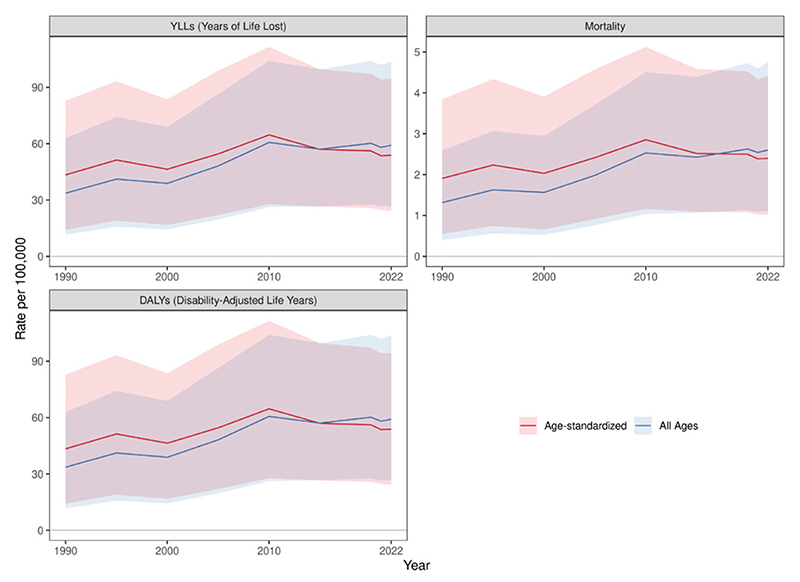
Figure 2.
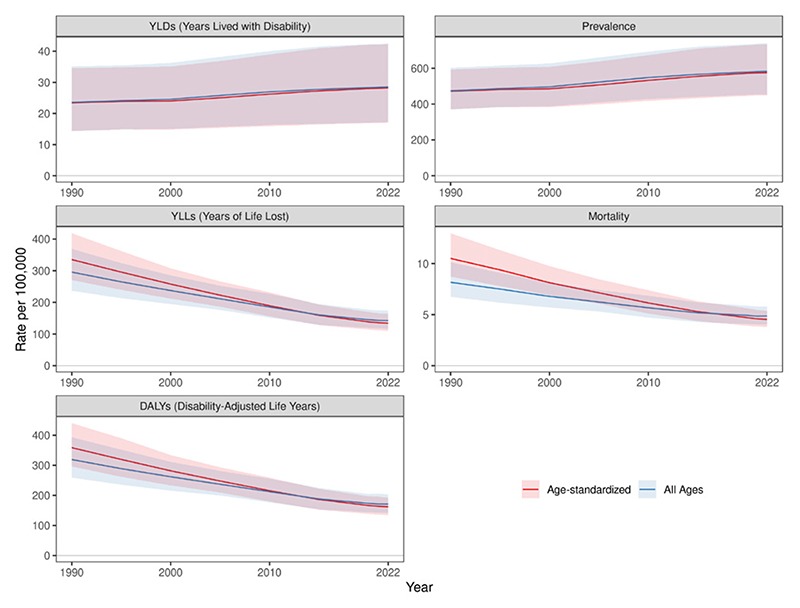
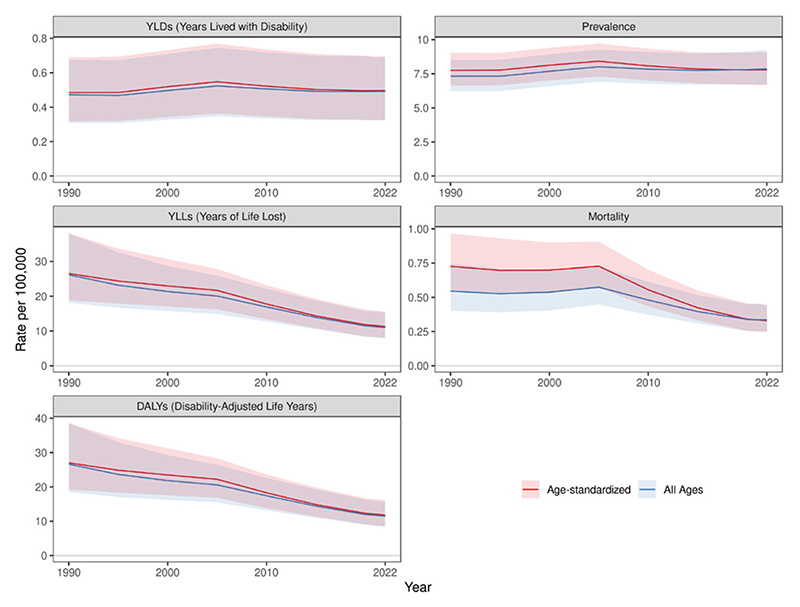
Global rheumatic heart disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
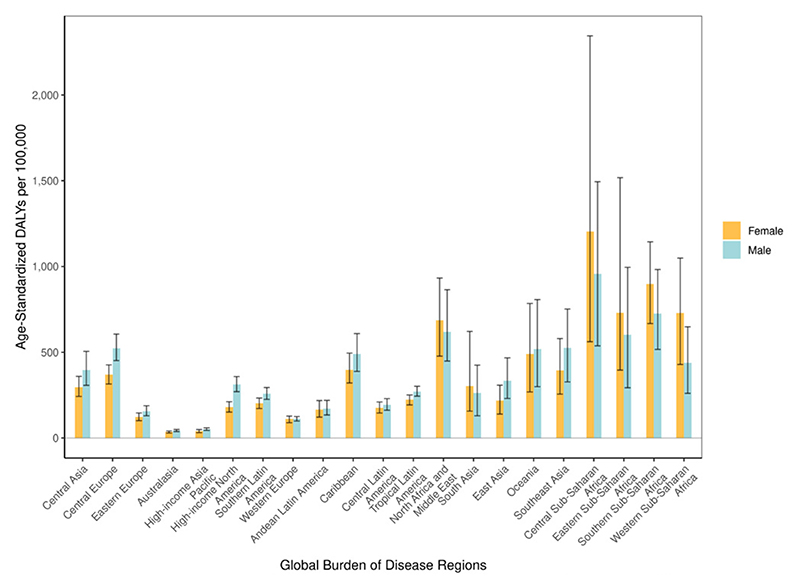
Figure 3.
Rheumatic heart disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
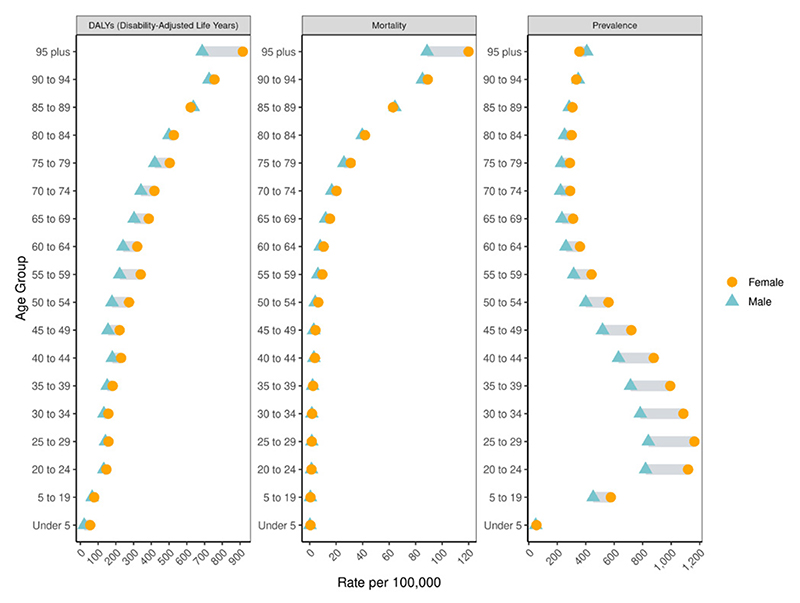
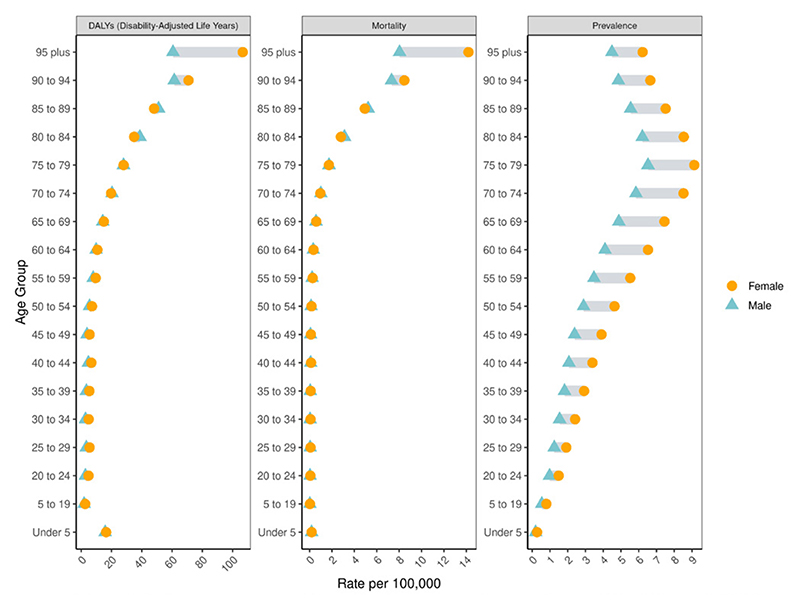
Global rheumatic heart disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
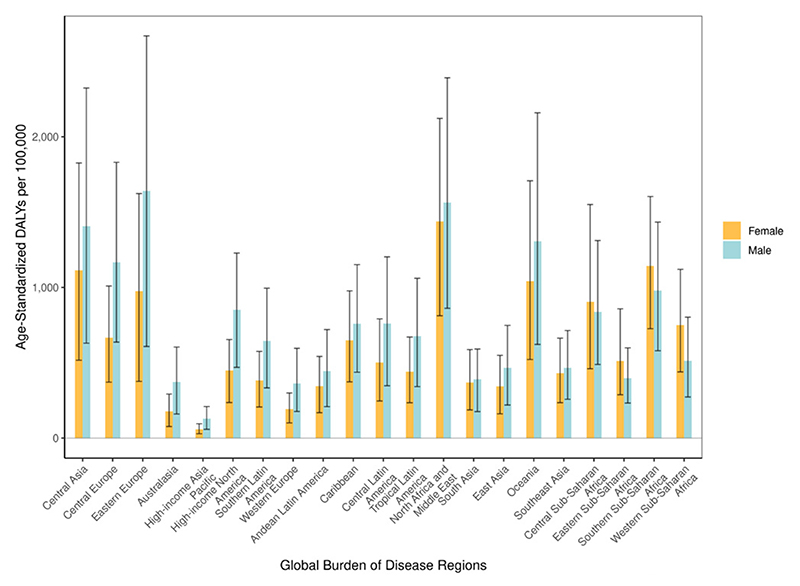
Ischemic Heart Disease
Figure 1.
Global map of age-standardized ischemic heart disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global ischemic heart disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Ischemic heart disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
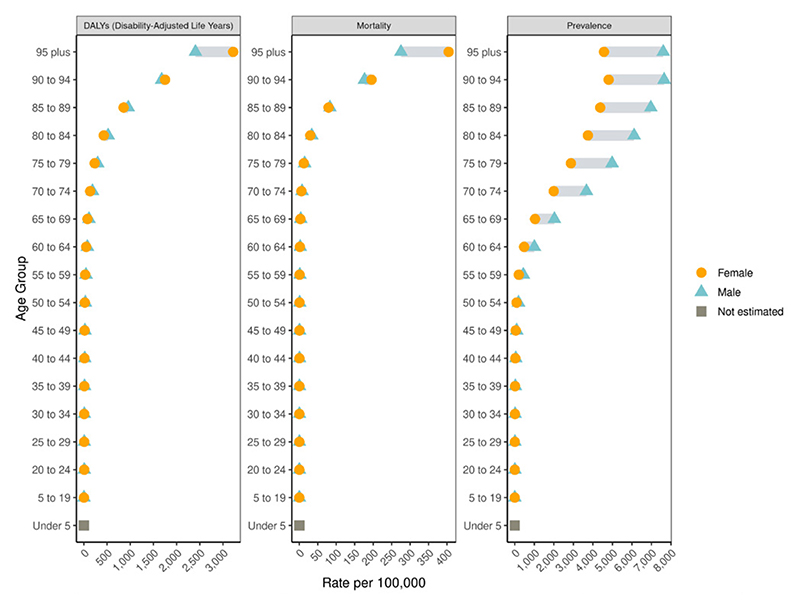
Figure 4.
Global ischemic heart disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Aggregate Cause: Stroke
Figure 1.
Global map of age-standardized stroke mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global stroke estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Stroke age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global stroke age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Ischemic Stroke
Figure 1.
Global map of age-standardized ischemic stroke mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global ischemic stroke estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Ischemic stroke age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global ischemic stroke age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Intracerebral Hemorrhage
Figure 1.
Global map of age-standardized intracerebral hemorrhage mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global intracerebral hemorrhage estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Intracerebral hemorrhage age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global intracerebral hemorrhage age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Subarachnoid Hemorrhage
Figure 1.
Global map of age-standardized subarachnoid hemorrhage mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global subarachnoid hemorrhage estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Subarachnoid hemorrhage age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global subarachnoid hemorrhage age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Hypertensive Heart Disease
Figure 1.
Global map of age-standardized hypertensive heart disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global hypertensive heart disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Hypertensive heart disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global hypertensive heart disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Aggregate Cause: Non-Rheumatic Valvular Heart Disease
Figure 1.
Global map of age-standardized non-rheumatic valvular heart disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global non-rheumatic valvular heart disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Non-rheumatic valvular heart disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global non-rheumatic valvular heart disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Non-Rheumatic Calcific Aortic Valve Disease
Figure 1.
Global map of age-standardized non-rheumatic calcific aortic valve disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global non-rheumatic calcific aortic valve disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Non-rheumatic calcific aortic valve disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global non-rheumatic calcific aortic valve disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Non-Rheumatic Degenerative Mitral Valve Disease
Figure 1.
Global map of age-standardized non-rheumatic degenerative mitral valve disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global non-rheumatic degenerative mitral valve disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Non-rheumatic degenerative mitral valve disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global non-rheumatic degenerative mitral valve disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Other Non-Rheumatic Valve Diseases
Figure 1.
Global map of age-standardized other non-rheumatic valve diseases mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global other non-rheumatic valve diseases estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Other non-rheumatic valve diseases age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global other non-rheumatic valve diseases age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Aggregate Cause: Cardiomyopathy and Myocarditis
Figure 1.
Global map of age-standardized cardiomyopathy and myocarditis mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiomyopathy and myocarditis estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiomyopathy and myocarditis age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiomyopathy and myocarditis age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Myocarditis
Figure 1.
Global map of age-standardized myocarditis mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global myocarditis estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Myocarditis age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global myocarditis age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Alcoholic Cardiomyopathy
Figure 1.
Global map of age-standardized alcoholic cardiomyopathy mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global alcoholic cardiomyopathy estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Alcoholic cardiomyopathy age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global alcoholic cardiomyopathy age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Other Cardiomyopathy
Figure 1.
Global map of age-standardized other cardiomyopathy mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global other cardiomyopathy estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Other cardiomyopathy age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global other cardiomyopathy age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Pulmonary Arterial Hypertension
Figure 1.
Global map of age-standardized pulmonary arterial hypertension mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global pulmonary arterial hypertension estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Pulmonary arterial hypertension age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global pulmonary arterial hypertension age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Atrial Fibrillation and Flutter
Figure 1.
Global map of age-standardized atrial fibrillation and flutter mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global atrial fibrillation and flutter estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Atrial fibrillation and flutter age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global atrial fibrillation and flutter age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Aortic Aneurysm
Figure 1.
Global map of age-standardized aortic aneurysm mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global aortic aneurysm estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Aortic aneurysm age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global aortic aneurysm age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Lower Extremity Peripheral Arterial Disease
Figure 1.
Global map of age-standardized lower extremity peripheral arterial disease mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global lower extremity peripheral arterial disease estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Lower extremity peripheral arterial disease age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global lower extremity peripheral arterial disease age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Endocarditis
Figure 1.
Global map of age-standardized endocarditis mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global endocarditis estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Endocarditis age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global endocarditis age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Other Cardiovascular and Circulatory Diseases
Figure 1.
Global map of age-standardized other cardiovascular and circulatory diseases mortality rate per 100,000 in 2022 with equal interval classification
Figure 2.
Global other cardiovascular and circulatory diseases estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Other cardiovascular and circulatory diseases age-standardized disability-adjusted life years (DALYs) per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global other cardiovascular and circulatory diseases age-specific estimates per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Ambient Particulate Matter Pollution
Figure 1.
Global map of cardiovascular disease mortality attributable to ambient particulate matter pollution per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to ambient particulate matter pollution estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to ambient particulate matter pollution per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to ambient particulate matter pollution per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Household Air Pollution from Solid Fuels
Figure 1.
Global map of cardiovascular disease mortality attributable to household air pollution from solid fuels per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to household air pollution from solid fuels estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to household air pollution from solid fuels per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to household air pollution from solid fuels per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Temperature
Figure 1.
Global map of cardiovascular disease mortality attributable to high temperature per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high temperature estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high temperature per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high temperature per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Low Temperature
Figure 1.
Global map of cardiovascular disease mortality attributable to low temperature per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to low temperature estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to low temperature per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to low temperature per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Lead Exposure
Figure 1.
Global map of cardiovascular disease mortality attributable to lead exposure per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to lead exposure estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to lead exposure per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to lead exposure per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Smoking
Figure 1.
Global map of cardiovascular disease mortality attributable to smoking per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to smoking estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to smoking per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to smoking per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Secondhand Smoke
Figure 1.
Global map of cardiovascular disease mortality attributable to secondhand smoke per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to secondhand smoke estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to secondhand smoke per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to secondhand smoke per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Alcohol Use
Figure 1.
Global map of cardiovascular disease mortality attributable to high alcohol use per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high alcohol use estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high alcohol use per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high alcohol use per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Dietary Risks
Figure 1.
Global map of cardiovascular disease mortality attributable to dietary risks per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to dietary risks estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to dietary risks per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to dietary risks per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Low Physical Activity
Figure 1.
Global map of cardiovascular disease mortality attributable to low physical activity per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to low physical activity estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to low physical activity per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to low physical activity per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Fasting Plasma Glucose
Figure 1.
Global map of cardiovascular disease mortality attributable to high fasting plasma glucose per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high fasting plasma glucose estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high fasting plasma glucose per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high fasting plasma glucose per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Ldl Cholesterol
Figure 1.
Global map of cardiovascular disease mortality attributable to high LDL cholesterol per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high LDL cholesterol estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high LDL cholesterol per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high LDL cholesterol per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Systolic Blood Pressure
Figure 1.
Global map of cardiovascular disease mortality attributable to high systolic blood pressure per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high systolic blood pressure estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high systolic blood pressure per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high systolic blood pressure per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
High Body Mass Index
Figure 1.
Global map of cardiovascular disease mortality attributable to high body mass index per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to high body mass index estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to high body mass index per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to high body mass index per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Kidney Dysfunction
Figure 1.
Global map of cardiovascular disease mortality attributable to kidney dysfunction per 100,000 in 2022 with equal interval classification
Figure 2.
Global cardiovascular disease attributable to kidney dysfunction estimates per 100,000 by measure with shaded 95% uncertainty interval, 1990-2022
Figure 3.
Cardiovascular disease age-standardized disability-adjusted life years (DALYs) attributable to kidney dysfunction per 100,000 by Global Burden of Disease region and sex in 2022, 95% uncertainty interval indicated by black bar
Figure 4.
Global cardiovascular disease age-specific estimates attributable to kidney dysfunction per 100,000 by sex in 2022, difference in sex estimates indicated by gray bar
Summary of Global Burden of Disease Study Methods
Background
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) is a multinational collaborative research study with >10,000 collaborators around the world. GBD generates a time series of summary measures of health, including prevalence, cause-specific mortality (CSMR), years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs) to provide a comprehensive view of health burden for a wide range of stakeholders including clinicians, public and private health systems, ministries of health, and other policymakers. These estimates are produced for 371 causes of death and 88 risk factors according to mutually exclusive, collectively exhaustive hierarchies of health conditions and risks. The study is led by a principal investigator and governed by a study protocol, with oversight from a Scientific Council, and an Independent Advisory Committee.1 GBD is performed in compliance with Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).2 GBD uses de-identified data, and the waiver of informed consent was reviewed and approved by the University of Washington Institutional Review Board (study number 9060).
This almanac presents results for 18 cardiovascular diseases (CVD) and the CVD burden attributed to 15 risk factors (including an aggregate grouping of dietary risks) by GBD region. A summary of methods follows. Additional information can be found online at https://ghdx.healthdata.org/record/ihme-data/cvd-1990-2022, including:
-
1)
detailed methods, including information on the GBD location hierarchy, the GBD cause hierarchy, mapping of International Classification of Disease (ICD) codes to the GBD cause list, and health states and associated disability weights used in the comorbidity simulation;
-
2)
mean values and 95% uncertainty intervals for all estimates presented in the almanac, by country, sex, age group, and year;
-
3)
cause-specific write-ups outlining methods for estimation of mortality with details of model parameters for each cause, including selection of location-specific covariates;
-
4)
cause-specific write-ups outlining methods for estimation of prevalence, with details of systematic reviews, input data, all data adjustments, modeling frameworks, and model parameter selection;
-
5)
risk factor write-ups containing details of systematic reviews, input data, all data adjustments, modeling frameworks, and model parameter selection;
-
6)
documentation of compliance with GATHER.
Methods
Demographic groupings
This study estimated CVD burden for 204 countries and territories grouped into 21 regions and 7 super-regions. GBD regions are made up of countries and territories that are geographically close and epidemiologically similar. GBD regions are grouped into super-regions based on observed cause of death patterns. Estimates presented in this almanac were produced at the sub-national level (eg, region, state, or province) for a subset of locations including Brazil, China, Ethiopia, India, Indonesia, Italy, Iran, Japan, Kenya, Mexico, Nigeria, Norway, Pakistan, the Philippines, Russia, South Africa, the UK, and the USA. Since GBD 2019, the GBD location hierarchy has included all WHO member states. Each epidemiological quantity of interest was estimated for 23 age groups from birth to 95 years and older; males, females, and both sexes combined from 1990 to 2022. Age standardization used the direct method with the GBD standard global population age structure. This standard population is determined by using the population structure of all national locations with a population >5 million people. First, the proportion of the location-specific population in each age group is calculated. Second, these age-specific proportions are averaged across all locations.3
Sociodemographic index
Results are also presented by socio-demographic index (SDI) value. SDI is a composite measure of overall development comprised of lag-distributed income per capita (LDI), average years of education, and fertility rates among females younger than 25 years (TFU25). LDI and education are positively correlated with improved health outcomes, while TFU25 is negatively correlated. SDI is thus calculated as the geometric mean of LDI, education, and the inverse of TFU25.3
Cardiovascular disease case definitions
A set of case definitions was used to consistently identify and harmonize data on cardiovascular diseases for all locations across the entire time period. CVD case definitions used by GBD are shown in Table 1. Of note, heart failure is classified as an impairment rather than an underlying cause of death in the GBD classification system. Heart failure is a structural or functional abnormality of the heart that impairs cardiac filling and output and, within the GBD, contributes burden to many underlying causes of death including all cardiovascular diseases as described with the exception of aortic aneurysm and lower extremity peripheral arterial disease. GBD relies on data in which heart failure has been diagnosed by clinicians using structured criteria, such as the Framingham, European Society of Cardiology, or Universal Definition and Classification of Heart Failure criteria. Prevalent heart failure is defined as structural heart disease with current or previous symptoms of heart failure (ACCF/AHA stages C or D).4 As part of the GBD estimation process, heart failure burden is included in the burden estimates for each etiologic underlying cause of death.
Table 1. Cardiovascular Case Definitions.
| GBD Cause | Definition |
|---|---|
| Rheumatic heart disease | Diagnosis by a physician with use of echocardiography. This case definition for echocardiographic confirmation of rheumatic heart disease follows the World Heart Federation criteria for echocardiographic diagnosis.12 |
| Ischemic heart disease |
|
| Ischemic stroke | Brain imaging showing blood flow to part of the brain being occluded and according to WHO criteria of rapidly developing clinical signs of disturbance of cerebral function lasting >24 h or leading to death.16,17 |
| Intracerebral hemorrhage | Brain imaging showing bleeding into the tissue of the brain and according to WHO criteria of rapidly developing clinical signs of disturbance of cerebral function lasting >24 h or leading to death. Only nontraumatic events were included.16,17 |
| Subarachnoid hemorrhage | Brain imaging or lumbar puncture indicating the rupture of a blood vessel resulting in bleeding into the subarachnoid space and according to WHO criteria of rapidly developing clinical signs of disturbance of cerebral function lasting >24 h or leading to death. Only nontraumatic events were included.16,17 |
| Hypertensive heart disease | Heart condition caused by long-term high blood pressure, resulting in left ventricular hypertrophy, diastolic dysfunction, and clinical heart failure with either preserved or reduced systolic function of the left ventricle. Clinical diagnosis of heart failure is based on structured criteria as described.4 |
| Non-rheumatic calcific aortic valve disease | Diagnosis by a physician based on echocardiographic findings of stenosis or regurgitation caused by progressive calcification of the valve, excluding congenital, rheumatic, or infectious causes but including stenosis of a bicuspid aortic valve.18 |
| Non-rheumatic degenerative mitral valve disease | Diagnosis by a physician based on echocardiographic findings of myxomatous degeneration or prolapse of the mitral valve leading to at least moderate mitral regurgitation, excluding disease due to annular dilation, congenital, rheumatic, or infectious causes.18 |
| Other non-rheumatic valve diseases | Residual category capturing diagnosis by a physician based on echocardiographic findings of stenosis or regurgitation of pulmonary and tricuspid valves. Valve dysfunction due to congenital, infectious, or rheumatic causes was estimated separately.18 |
| Myocarditis | Acute myocarditis is defined by symptoms, clinical examination, cardiac imaging such as cardiac MRI, or endomyocardial biopsy.19 Heart failure due to myocarditis is a clinical diagnosis of heart failure based on structured criteria as described with a history of myocarditis.4 |
| Alcoholic cardiomyopathy | Clinical diagnosis of heart failure based on structured criteria as described due to the toxic effects of ingested alcohol.4 |
| Other cardiomyopathy | Residual category capturing a clinical diagnosis of heart failure based on structured criteria as described without a history of other potential causes of heart failure.4 |
| Pulmonary arterial hypertension | Diagnosis by a physician based on findings of restricted blood flow and elevated pressure in the pulmonary arteries based on right heart catheterization or echocardiography.20 |
| Atrial fibrillation and flutter | ECG studies demonstrating irregularly irregular RR intervals; and no P waves.21,22 |
| Aortic aneurysm | Abdominal or thoracic aorta is abnormally enlarged and weakened due to atherosclerosis, high blood pressure, or inflammation, which can lead to tearing or rupture of the blood vessel.23 Prevalence and YLDs are not currently estimated for aortic aneurysm. |
| Lower-extremity peripheral artery disease | An ankle-brachial index ≤0.90.24 |
| Endocarditis | Acute infective endocarditis was diagnosed defined as a clinical diagnosis clinically via based on the Duke Criteria, which includes confirmation through clinical signs and blood tests.25 Heart failure due to endocarditis was based on a clinical diagnosis of heart failure based on structured criteria as described with a history of acute infective endocarditis.4 |
| Other cardiovascular and circulatory diseases | This aggregate cause incorporates less common cardiovascular diseases that are not modelled independently; for example, pericarditis. Diagnostic criteria vary based on the underlying condition. |
ECG = echocardiogram; MRI = magnetic resonance imaging; WHO = World Health Organization; YLDs = years lived with disability.
All-cause mortality and population estimates
GBD produces estimates of all-cause mortality and population; for cause-specific burden, these are integral inputs into the cause-specific estimation process. Detailed methods have been previously reported.3
Cause-specific mortality
Death records, including vital registration for all cardiovascular causes and verbal autopsy data for total cardiovascular disease, ischemic heart disease, and total stroke, were mapped to the GBD cause list. Records where the underlying cause was considered nonspecific, intermediate, or implausible were reassigned to a valid underlying cause of death via redistribution algorithms which utilized proportional information, cause-specific priors, or data sets with information on all contributing causes of death in addition to the underlying cause.5 A counterfactual approach, based on data from 2014 to 2019, was used to estimate excess cause-specific deaths in 2020 and 2021 and reclassify them as deaths due to COVID-19. A noise reduction algorithm was applied to mortality data and a Bayesian geospatial ensemble regression model (CODEm, the cause of death ensemble model, Institute for Health Metrics and Evaluation [IHME], Seattle, Washington) was used with location-specific covariates to produce smoothed time series for each location, including where data was sparse or missing.6 Individual models included in the ensemble are weighted according to performance on out-of-sample predictive validity testing.
CoDCorrect
As each cause-specific model is estimated separately, the sum of these models is not certain to equal the all-cause mortality estimates. The CoDCorrect process rescales each level of the GBD cause hierarchy such that the sum of the cause-specific estimates does not exceed the all-cause mortality estimates.6 Using the GBD cause hierarchy, this process begins by rescaling the Level 1 causes to match the all-cause mortality estimates. Level 2 causes are then rescaled to their corrected parent cause estimates. This process continues for Level 3 and Level 4 causes such that all levels of the hierarchy are rescaled.
Prevalence
Prevalence was estimated for each disease using the Disease Model—Bayesian metaregression (DisMod-MR 2.1 [IHME, Seattle, Washington]), an epidemiologic state-transition disease modeling tool. DisMod-MR evaluates all available high-quality, population-representative data for disease incidence, prevalence, remission, and mortality, while enforcing consistency among these various parameters.6 Possible input data sources included scientific literature identified via systematic reviews of published literature and expert review, population surveys, and administrative health facility data. Where applicable, network meta-analysis was performed using the meta-regression—Bayesian, regularized, trimmed software (MR-BRT, IHME, Seattle, Washington) to allow adjustment for study-level differences in case definition or measurement method.7 If necessary, correction factors were calculated to adjust tabulated inpatient-only health facility data to account for readmission, nonprimary diagnoses, and outpatient visits.
Risk factors
Definitions used for each risk factor can be found in Table 2.
Table 2. Risk Factor Exposure Definitions.
| Risk Factor | Definition |
|---|---|
| High systolic blood pressure | Brachial SBP >105-115 mm Hg in adults >25 years of age. |
| High LDL cholesterol | LDL-cholesterol >0.9-1.4 mmol/L in adults >25 years of age. |
| High body mass index | Body mass index >20-23 kg/m2 in adults >20 years of age. |
| High fasting plasma glucose | Serum fasting plasma glucose >4.9-5.3 mmol/L in adults >25 years of age. |
| Kidney dysfunction | Estimated glomerular filtration rate <60 mL/min/1.73 m2 and/or albumin-to-creatinine ratio ≤30 mg/g. |
| Ambient particulate matter pollution | Population-weighted annual average mass concentration of PM2.5 in a cubic meter of air >2.4-5.9 μg/m3. |
| Household air pollution from solid fuels | Proportion of individuals exposed to >2.4-5.9 μg/m3 of PM2.5 due to the use of solid fuels for cooking, including coal, charcoal, wood, agricultural residue, and animal dung. |
| High temperature | Exposure to temperatures warmer than the temperature associated with the lowest overall mortality attributable to the risk, in a given location and year. |
| Low temperature | Exposure to temperatures colder than the temperature associated with the lowest overall mortality attributable to the risk, in a given location and year. |
| Lead exposure | Micrograms of lead per gram of bone greater than the age-specific TMREL. |
| Dietary risks | Composite risk factor consisting of suboptimal exposure to dietary factors including fruits, vegetables, whole grains, nuts and seeds, fiber, omega-3 fatty acids, polyunsaturated fatty acids, calcium, milk, legumes, red meat, processed meat, sugar-sweetened beverages, trans fatty acids, and sodium. |
| Smoking | Current or former users of any smoked tobacco product on a daily or occasional basis. |
| Secondhand smoke | Current exposure of nonsmokers to secondhand tobacco smoke at home, at work, or in other public places. |
| High alcohol use | Grams per day of pure alcohol consumed among current drinkers greater than the age-, sex-, and region-specific TMREL |
| Low physical activity | Physical activity performed by adults >25 years of age, for at least 10 minutes at a time, across all domains of life (leisure/recreation, work/household, and transport) <3,000-4,500 metabolic equivalent-minutes per week. |
LDL = low-density lipoprotein; PM2.5 = particulate matter <2.5 µm in diameter; SBP = systolic blood pressure; TMREL = theoretical minimum risk exposure level.
Attributable burden estimation
The GBD estimates disease burden attributable to risk factors using a comparative risk assessment framework.8
Population-level exposure to each risk factor was estimated using statistical models. Most risk exposure was estimated using spatiotemporal Gaussian process regression (ST-GPR) or DisMod-MR, as described. ST-GPR is a geospatial Gaussian process regression model that borrows strength between locations and over time to generate estimates of mean risk factor exposures.8 Input data sources included scientific literature identified via systematic reviews of published literature and expert review, population health surveys, and, for ambient air pollution, satellite data. Person-level data from cohort studies were used to determine the standard deviation of the risk factor exposure and to estimate the shape of the exposure distribution.
Each risk was assigned outcomes from the GBD study list of diseases to form risk-outcome pairs based on the availability of convincing or probable evidence of a disease-risk association. For each risk factor, the level of exposure where disease risk is minimized, or theoretical minimum risk exposure level (TMREL), was determined.
Relative risks were estimated for each risk outcome pair following the burden of proof (BoP) method, previously reported.9 Briefly, following PRISMA guidelines, systematic reviews were performed for studies reporting relative risk or hazard ratios, and data were extracted using a standardized template.10 Using MR-BRT, the relative risk between risk and disease outcome was modeled, integrating over the exposure ranges reported. This approach allows us to identify publication or reporting bias and to account for between-study heterogeneity and within-study correlation. An example of this approach has been reported in detail for the relationship between systolic blood pressure and ischemic heart disease.11
Population-attributable fractions (PAF) were then calculated for each risk-outcome pair using the exposure levels, the estimated relative risk, and the TMREL to generate the amount of burden for each disease due to risk factor exposure. Attributable burden was then estimated as the PAF for that risk-outcome pair multiplied by the burden measure of interest.
Summary measures of disease burden
YLDs were estimated by multiplying disease prevalence by the relevant disability weight after accounting for comorbidity in a simulation process.6 Disability weights, which represent the magnitude of health loss associated with the outcome were constructed based on surveys of the general population, with a statistical adjustment made to account for comorbidity. YLLs due to premature mortality were computed by multiplying the number of estimated deaths by the standard life expectancy at age of death.6 The standard life expectancy was determined by using the lowest observed age-specific mortality rates by location and sex across all estimation years from locations with total populations >5 million in 2016 to establish a theoretical minimum risk reference life table. DALYs were calculated as the sum of YLLs and YLDs and represent the total health burden associated with each cause. All summary measures were estimated using 500 draws, and uncertainty intervals were determined as the 2.5th and 97.5th values of the posterior distribution of model draws.
Supplementary Material
For a complete list of the Global Burden of Cardiovascular Diseases and Risks Collaborators, please see pages 1 to 35 of the Supplemental Appendix, available in the online version of this paper. Please see pages 36 to 47 of the Supplemental Appendix for more detailed information about individual author contributions to the research, divided into the following categories: providing data or critical feedback on data sources; developing methods or computational machinery; providing critical feedback on methods or results; drafting the manuscript or revising it critically for important intellectual content; and managing the estimation or publications process. For author disclosures, please see pages 48 to 56 of the Supplemental Appendix.
Acknowledgments
Funding Support and Author Disclosures Funding was provided by the Bill and Melinda Gates Foundation, and the American College of Cardiology Foundation. The authors have reported that they have no relationships relevant to the contents of this paper to disclose. The contents and views expressed in this report are those of the authors and do not necessarily reflect the official views of the National Institutes of Health, the Department of Health and Human Services, the U.S. Government, or the affiliated institutions.
References
- 1.Murray CJL. Protocol for the Global Burden of Diseases, Injuries, And Risk Factors Study (GBD) [Accessed November 10, 2023]. https://www.healthdata.org/sites/default/files/files/Projects/GBD/March2020_GBD%20Protocol_v4.pdf .
- 2.Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. The Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Abbas KM, Abbasifard M, et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gibson G, Blumer V, Mentz RJ, Lala A. Universal Definition and Classification of Heart Failure: A Step in the Right Direction from Failure to Function. [Accessed November 8, 2023]. https://www.acc.org/Latest-in-Cardiology/Articles/2021/07/12/12/31/Universal-Definition-and-Classification-of-Heart-Failure .
- 5.Johnson SC, Cunningham M, Dippenaar IN, et al. Public health utility of cause of death data: applying empirical algorithms to improve data quality. [Accessed November 8, 2023]; doi: 10.1186/s12911-021-01501-1. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01501-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng P, Barber R, Sorensen RJD, Murray CJL, Aravkin AY. Trimmed constrained mixed effects models: formulations and algorithms. Journal of Computational and Graphical Statistics. 2021;30:544–556. [Google Scholar]
- 8.GBD 2019 Risk Factor Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. [Accessed November 8, 2023]. https://www.theLancet.com/journas/Lancet/artice/PIIS0140-6736(20)30752-2/fuext . [DOI] [PMC free article] [PubMed]
- 9.Zheng P, Afshin A, Biryukov S, et al. The burden of proof studies: assessing the evidence of risk. Nat Med. 2022;28:2038–2044. doi: 10.1038/s41591-022-01973-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Razo C, Welgan CA, Johnson CO, et al. Effects of elevated systolic blood pressure on ischemic heart disease: a burden of proof study. Nat Med. 2022;28:2056–2065. doi: 10.1038/s41591-022-01974-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rwebembera J, Marangou J, Mwita JC, et al. 2023 World Heart Federation guidelines for the echocardiographic diagnosis of rheumatic heart disease. Nat Rev Cardiol. doi: 10.1038/s41569-023-00940-9. Published online November 2, 2023. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Apert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction. [Accessed November 9, 2023];2018 doi: 10.1161/CIR.0000000000000617. [DOI] [Google Scholar]
- 14.Jones WB, Riley CP, Reeves TJ, Sheffield LT. Natural history of coronary artery disease. Bull N Y Acad Med. 1972;48:1109–1125. [PMC free article] [PubMed] [Google Scholar]
- 15.Raff GL, Abidov A, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr. 2009;3:122–136. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Donkor ES. Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018;2018:3238165. doi: 10.1155/2018/3238165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980;58:113–130. [PMC free article] [PubMed] [Google Scholar]
- 18.Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;77:e25–e197. doi: 10.1016/j.jacc.2020.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Ammirati E, Frigerio M, Adler ED, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy. Circ Heart Fail. 2020;13:e007405. doi: 10.1161/CIRCHEARTFAILURE.120.007405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galiè N, Humbert M, Vachiery J-L, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Heart J. 2016;37:67–119. doi: 10.1093/eurheartj/ehv317. [DOI] [PubMed] [Google Scholar]
- 21.Iwasaki Y, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124:2264–2274. doi: 10.1161/CIRCULATIONAHA.111.019893. [DOI] [PubMed] [Google Scholar]
- 22.Saleh K, Haldar S. Atrial fibrillation: a contemporary update. Clin Med (Lond) 2023;23:437–441. doi: 10.7861/clinmed.2023-23.5.Cardio2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isselbacher EM, Preventza O, Hamilton Black J, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;80:e223–e393. doi: 10.1016/j.jacc.2022.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Criqui MH, Matsushita K, Aboyans V, et al. Lower extremity peripheral artery disease: contemporary epidemiology, management gaps, and future directions: a scientific statement from the American Heart Association. Circulation. 2021;144:e171–e191. doi: 10.1161/CIR.0000000000001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fowler VG, Durack DT, Selton-Suty C, et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for infective endocarditis: updating the Modified Duke Criteria. Clin Infect Dis. 2023;77:518–526. doi: 10.1093/cid/ciad271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.