Learning objectives.
By reading this article you should be able to:
-
•
Describe current UK guidance for emergency front of neck access (eFONA) in airway management.
-
•
Develop skills for identification of the cricothyroid membrane.
-
•
Review techniques to improve making the transition to eFONA for airway management.
-
•
Appraise your current departmental standards of care for eFONA equipment and training.
Key points.
-
•
Emergency front of neck access (eFONA) is a lifesaving intervention in airway management.
-
•
UK guidance recommends the ‘scalpel-bougie-tube’ technique when performing eFONA.
-
•
Delay in performing eFONA may result in brain injury and death.
-
•
The cricothyroid membrane should be identified in all patients before airway management.
-
•
All clinicians involved in airway management should undertake regular multidisciplinary training in eFONA.
The primary goal of airway management is the maintenance of alveolar oxygenation. Airway management using face mask ventilation, a supraglottic airway device (SAD), or tracheal intubation is a fundamental skill for all clinicians involved in airway management. Failure to achieve alveolar oxygenation using these methods may result in permanent harm and the risk of death. The Fourth National Audit Project (NAP4) of the Royal College of Anaesthetists (RCoA) and the Difficult Airway Society (DAS) showed that serious airway events occur in at least 1 in 22,000 general anaesthesia cases. They estimated the incidence of death or brain damage as at least 1 in 180,000 cases.1
Emergency front of neck access (eFONA) can be defined as the securing of a patent airway via the anterior neck to facilitate emergency alveolar oxygenation. eFONA is the final lifesaving step in airway management to reverse hypoxia and prevent resulting brain injury, cardiac arrest, and death.
Serious airway events requiring eFONA are rare. NAP4 identified the incidence of eFONA as 1 in 12,500–50,000 general anaesthesia cases in the UK, with an increased incidence associated with head and neck surgery.1 NAP4 revealed that 80 eFONA attempts were made during 184 serious airway events, 58 in operative anaesthesia, 12 in the ICU and 10 in the emergency department. The report highlighted knowledge gaps and numerous issues with eFONA including decision-making, system, equipment, and technical failures.1
Indications for eFONA
The ‘can’t intubate, can't oxygenate’ situation
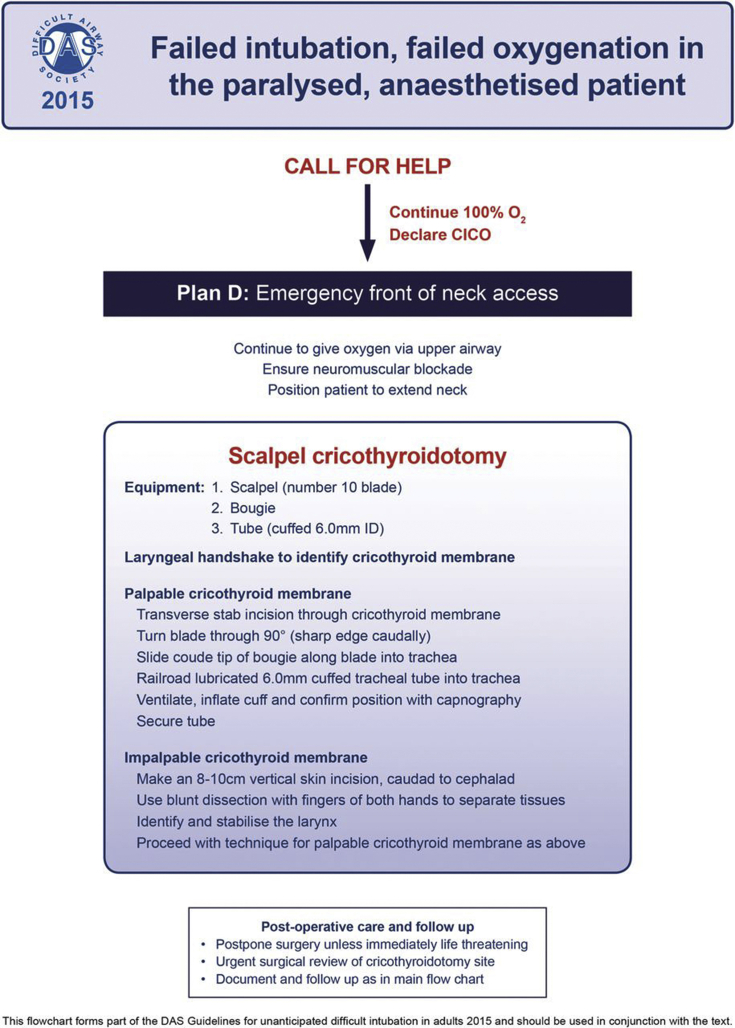
The ‘can’t intubate, can't oxygenate’ (CICO) situation occurs after attempts to manage the airway by a facemask, a supraglottic airway device, and a tracheal tube have failed. During a CICO situation, profound hypoxia will result in cardiac arrest and death unless oxygenation can be rapidly restored. In the ICU, cardiac arrest and death secondary to hypoxia from failed oxygenation during airway management typically occurs within 45–60 min of the first airway intervention.2 Depending on the duration and severity of the hypoxic event, there is a significant risk of brain injury in survivors and CICO situations account for more than 25% of all anaesthesia-related deaths.1 eFONA is the final, time-critical step in the management of a CICO situation (i.e. ‘Plan D’ in the DAS Difficult intubation guidelines) (Fig. 1). The clinician's reluctance to perform eFONA has been shown to be a major contributor to the morbidity and mortality in CICO situations.3
Figure 1.
DAS Difficult intubation guidelines—overview. Difficult Airway Society 2015. With permission from the Difficult Airway Society
Current UK guidance from DAS on the management of the CICO situation addresses the findings of NAP4 and presents a simplified approach to eFONA using standardised techniques with readily available equipment.2, 4 Figures of the DAS guidelines for the management of tracheal intubation in critically ill adults can be accessed in the online supplementary material (Supplementary Figs S1 and S2).
The ‘surgically inevitable’ airway
Achieving alveolar oxygenation in some circumstances using standard airway and intubating techniques will appear to have a very high likelihood of failure from the outset and therefore deemed too high risk. These can include patients with upper airway obstruction from advanced head and neck tumours, traumatic injuries to the face and neck, and severe airway oedema secondary to burn injuries, anaphylaxis, or infection. Alternative techniques such as awake fibreoptic intubation may not be feasible. Airway management may therefore necessitate a cricothyroidotomy or tracheostomy under local anaesthetic as the primary procedure to secure the airway.
In addition, other techniques have been recommended such as consideration to performing a ‘prophylactic’ cannula cricothyroidotomy before induction of anaesthesia in patients at high risk of a CICO, to facilitate rapid conversion to eFONA.1
Performing eFONA
Applied anatomy of the anterior neck
The cricothyroid membrane (CTM) is a dense fibroelastic ligament in the anterior neck, connecting the thyroid cartilage (superiorly) to the cricoid cartilage (inferiorly). Vascular structures crossing the CTM include the cricothyroid artery and vein. The pyramidal lobe of the thyroid gland and lymph nodes may overlie the CTM. In the majority of non-obese patients, the CTM lies superficially in the anterior neck, but in obesity the depth of the CTM from the skin may increase.
The cricotracheal membrane connects the cricoid cartilage (superiorly) to the first tracheal ring (inferiorly). Caudal to the cricotracheal membrane lies the first tracheal ring. The tracheal ring interspaces, typically the second or third, are common sites of airway access for both elective and emergency tracheostomy, and lie deeper in the neck. The thyroid isthmus overlies the superior tracheal rings and interspaces. Major vessels, most commonly the brachiocephalic artery, traverse the anterior tracheal wall in up to 53% patients at the suprasternal notch.5 The potential for overlying major vascular structures and narrower, deeper interspaces to access the airway makes the cricotracheal membrane and tracheal interspaces a less desirable location for eFONA.
Identification of the CTM
The CTM should be identified in all patients before induction of anaesthesia, before undertaking awake intubation techniques or before extubation in the ICU. Accurate identification of the CTM is crucial to success in eFONA in order to prevent complications such as device misplacement, damage to local structures, and airway injury.
Clinical examination
Visualisation of anterior neck skin creases in order to identify the CTM is effective in 50% of patients and should not be used as the sole method for CTM identification.6 The success of clinical palpation techniques to identify the CTM is dependent on sex, patient position, and body habitus. Misidentification of the CTM is more common in females than in males.7 Identification of the CTM by conventional palpation is successful in 70% of non-obese patients, decreasing to approximately 40% in obesity.8 The ‘laryngeal handshake’ technique uses a three-step technique to identify the CTM and is recommended by DAS (Supplementary Fig. S3).2, 4 It is more accurate at identifying the CTM in women compared with conventional palpation techniques, but takes longer to perform.9 Details on performing the laryngeal handshake can be found in the online supplementary material.
Ultrasound identification
Ultrasound identification should be undertaken in patients where clinical examination is insufficient to confirm the position of the CTM. Ultrasound has been shown to be superior to palpation for identifying the CTM in morbidly obese patients.10 Two ultrasound techniques for identifying the CTM have been advocated; the transverse method (Fig. 2) and the longitudinal method (Supplementary Fig. S4).11 Videos demonstrating these techniques can be accessed using the following weblinks: http://airwaymanagement.dk/taca and http://airwaymanagement.dk/pearls.12, 13
Figure 2.
Transverse thyroid cartilage-airline-cricoid cartilage-airline (‘TACA’) method for ultrasound identification of the CTM. Step 1— ‘T’: A linear high frequency array probe is placed transverse on the anterior neck at the estimated level of the thyroid cartilage. The transducer is moved until the thyroid cartilage is identified as a triangular structure. Step 2— ‘A’: The probe is moved caudally until the CTM is identified as a hyperechoic white line resulting from the air-tissue border of the mucosal lining, the airline. Reverberation artefacts will often be visible below as parallel white lines. Step 3— ‘C’: The probe is moved caudally again until the cricoid cartilage is identified as a ‘black lying C’ with a white lining. Step 4— ‘A’: The probe is repositioned cephalad until the centre of the CTM can be identified again as the airline. Step 5—The midpoint of the CTM can then be marked with a pen by placing a dot at the midpoint of the transducer on all four sides and subsequently connecting the dots. With permission from Michael S. Kristensen, The Scandinavian Airway management course, www.airwaymanagement.dk, illustration from Br J Anaesth.11.
The transverse technique is faster and more useful in patients with a short neck.14 The longitudinal method can identify both major blood vessels and potential additional sites to access the airway, such as the cricotracheal membrane or tracheal interspaces. This is particularly relevant if eFONA is required in smaller children or in patients with tumours overlying the CTM.
The role for ultrasound in a CICO situation is reserved for scenarios where there is both the immediate availability of an ultrasound machine and the presence of a skilled operator.
Techniques for eFONA
There are three principle techniques for accessing the airway in an emergency CICO scenario:
-
(i)
Scalpel cricothyroidotomy
-
(ii)
Cannula cricothyroidotomy
-
(iii)
Surgical tracheostomy
Scalpel cricothyroidotomy
Scalpel cricothyroidotomy, using a ‘scalpel-bougie-tube’ technique is recommended by the DAS guidelines as the first line technique for eFONA.2, 4 It is the fastest and most reliable method of securing the airway in an emergency setting.15 The cuffed tracheal tube provides the ability to ventilate using standard low-pressure airway equipment, confirm correct placement using capnography, protects against airway aspiration, and facilitates exhalation.2 Numerous variations in the technique for scalpel cricothyroidotomy exist with either low or very low-quality evidence, mainly from prehospital case series and simulation studies. These have failed to demonstrate superiority of one technique over the other.16
The DAS guidelines simplify both the equipment and the procedure to promote a standardised approach to eFONA with readily available equipment, allowing consistency in training and skill retention (Fig. 3). A number 10 blade scalpel, a size 6.0 mm cuffed tracheal tube and a bougie are recommended to perform eFONA. Before attempting eFONA, 100% oxygen should be applied to the upper airway, the patient's neck should be maximally extended, and full neuromuscular block should be established. Manual in-line stabilisation should be removed if in place to facilitate maximal extension of the neck. A ‘scalpel-bougie-tube’ technique with a horizontal stab incision is recommended if the CTM is palpable (Supplementary Fig. S5). If this fails, or the CTM is impalpable, then an 8–10 cm vertical incision followed by a ‘scalpel-finger-bougie-tube’ technique is recommended.2, 4 A DAS training video demonstrating both techniques can be accessed using the following weblink: https://das.uk.com/content/video/fona.17
Figure 3.
DAS 2015 guidelines for failed intubation, failed oxygenation in the paralysed, anaesthetised patient. Technique for scalpel cricothyroidotomy. With permission from the Difficult Airway Society.
Cannula cricothyroidotomy
Cannula cricothyroidotomy involves puncture of the CTM to allow passage of either a narrow bore (internal diameter ≤2 mm) or wide bore (internal diameter ≥4 mm) cannula to facilitate oxygenation.
Narrow bore cricothyroidotomy requires a specialised high-pressure ventilation source such as the Sanders injector or Manujet III (VBM, Sulz am Neckar, Germany) to facilitate low frequency, transtracheal jet ventilation (TTJV). Data from NAP4 showed that 63% of the narrow bore cannula cricothyroidotomies performed failed, with issues such as device misplacement, kinking, and detachment of the cannula from the ventilation source occurring.1 In addition, a systematic review of TTJV in a CICO situation highlighted a high incidence of failure (42%), complications (51%) and barotrauma (32%) with TTJV for narrow bore techniques.18 A kink-resistant cannula should be used for narrow bore cricothyroidotomy. Narrow bore cricothyroidotomy does not provide a tracheal cuff and will thus require conversion to a more definitive airway to protect against aspiration and allow application of PEEP.
Wide bore cannula cricothyroidotomy uses either a ‘cannula over guidewire’ or a ‘cannula over trocar’ technique. The principle advantage of a wide bore over a narrow bore cricothyroidotomy is the ability to use conventional ventilation techniques rather than TTJV. As with narrow bore cannula techniques, NAP4 demonstrated a high failure rate of wide bore techniques with 43% of insertion attempts failing to rescue the airway.1
Wide bore ‘cannula over trocar’ devices include the Quicktrach device (VBM) and the Portex Cricothyroidotomy Kit (Smith Medical, Ashford, UK). Both require a trocar to facilitate insertion. Wide bore ‘cannula over guidewire’ devices, such as the Melker emergency cricothyroidotomy set (Cook Medical, Bloomington, USA) allow the insertion of a wide bore cannula over guidewire. Although appealing to clinicians familiar with the Seldinger technique, disadvantages of wide bore cannula over guidewire techniques include the high incidence of guidewire kinking and device misplacement, slower insertion times in the hands of inexperienced operators, and the requirement for fine motor skills in a highly stressful situation.
Emergency tracheostomy
Emergency tracheostomy in a CICO scenario takes longer than a surgical cricothyroidotomy and in most situations should not be undertaken as a first-line attempt at eFONA. It requires specialist equipment, the tracheal interspaces are deeper in the neck, and there is the potential presence of major vascular structures and the thyroid gland. An emergency tracheostomy should therefore only be performed by experienced operators or when cricothyroidotomy has failed.
Debate on optimal eFONA technique
Evidence on the optimal technique for performing eFONA is limited to case series (mainly from prehospital or military medicine), simulation training using cadavers, mannequins, and wet lab training. To date there is no high quality patient-centred randomised control trial comparing cannula with scalpel techniques and therefore the optimal technique for eFONA in a CICO situation is still debated.19, 20 Advocates for the scalpel cricothyroidotomy approach cite NAP4, which showed high success rates of surgical techniques and a high failure rate of cannula techniques.1 Supporters of the cannula techniques highlight the low success rate by anaesthetists overall in NAP4 regardless of technique compared with surgeons who performed the majority of successful scalpel eFONAs.1 They also reference the work of Heard and colleagues, who have demonstrated a high success rate of cannula techniques for eFONA during wet lab simulation.21
Current international guidelines are based on expert consensus opinion (Table 1). The decision on which technique is optimal for rescuing the airway in a CICO situation ultimately lies with the operator, depending on their experience and judgement of the clinical situation.
Table 1.
International recommendations on eFONA techniques.
| Country | Professional body | Recommendation |
|---|---|---|
| UK Ireland |
DAS, RCoA, Association of Anaesthetists, Faculty of Intensive Care Medicine, Intensive Care Society, British Association of Otorhinolaryngologists | ‘Scalpel-bougie-tube’ technique recommended.2, 4, 22 |
| Australia New Zealand |
ANZCA | ‘Scalpel-first’ or a ‘needle-first’ approach’ recommended depending on specialist preference.23 |
| Canada | The Canadian Difficult Airway Focus Group | Percutaneous needle-guided wide-bore cannula or open surgical approach recommended. Narrow bore cannula techniques only recommended if the clinician very experienced with jet ventilation. Recommend commencing cricothyroidotomy with a 3cm vertical incision over presumed location of the CTM.24 |
| USA | ASA | Surgical or percutaneous techniques recommended.25 |
Complications of eFONA techniques
Immediate complications may include device misplacement leading to failure, bleeding from adjacent vascular structures, and damage to the laryngotracheal structures, particularly the posterior tracheal wall. Emergency TTJV required for narrow bore cannula cricothyroidotomy is associated with the risk of pneumothorax, pneumomediastinum, and subcutaneous emphysema.18 Late complications of eFONA may include subglottic stenosis, scarring, and voice changes.
Management of the patient after eFONA
Tracheal access should be confirmed with capnography; and a chest radiograph performed to assess for pneumothorax or pneumomediastinum and to confirm the position of the eFONA device. There should be an immediate surgical assessment of the eFONA site and a plan made for conversion to a definitive airway if required. Because of the risk of pharyngeal or oesophageal injury, the patient should be monitored for mediastinal infection and investigated appropriately. An airway alert should be completed. Debriefing of the event should take place with all members of the multidisciplinary team.
Human factors in eFONA
Human factors have been shown to contribute to adverse outcome in serious airway events.1 Task fixation, team communication and cognitive overload are particularly relevant to eFONA.
Task fixation
The clinician's reluctance to diagnose a CICO situation can result in delayed transition to eFONA and cause avoidable harm to the patient.3 The risk of delaying eFONA is greater than the risk of the procedure itself. Current airway algorithms are designed to promote timeliness in airway management and avoid task fixation.2, 4 ‘Priming for FONA’ has been incorporated into the UK guidelines for the management of tracheal intubation in critically ill adults and refers to a three-step process to formalise and speed up the transition to eFONA using defined triggers before and at the declaration of CICO (Supplementary Fig. S1).2
-
(i)
Step 1: ‘Getting the FONA set’ to the bedside (or ensuring it is there) after one failed intubation attempt.
-
(ii)
Step 2: ‘Opening the FONA set’ after one failed attempt at rescue oxygenation (SAD insertion or facemask ventilation).
-
(iii)
Step 3: Immediately using the FONA set at CICO declaration.
Team communication
Poor communication was highlighted as a frequent contributor to adverse airway events in NAP4.1 The use of critical language is fundamental to team communication in an airway crisis. Clear declarations of failure of each airway plan, alongside a declaration of a CICO situation and the necessity to perform eFONA, must be made explicitly to the team. Clinicians called to assist with airway rescue, such as surgeons, require clear instructions as to what is required of them. Knowledge and adoption of standardised terminology such as ‘emergency front of neck airway’ and ‘can’t intubate, can't oxygenate situation’ by all members of the multidisciplinary team facilitates this.
Cognitive overload
Emergency airway management can lead to cognitive overload, causing errors in airway management and impaired decision making. This can lead to a delay in performing eFONA.
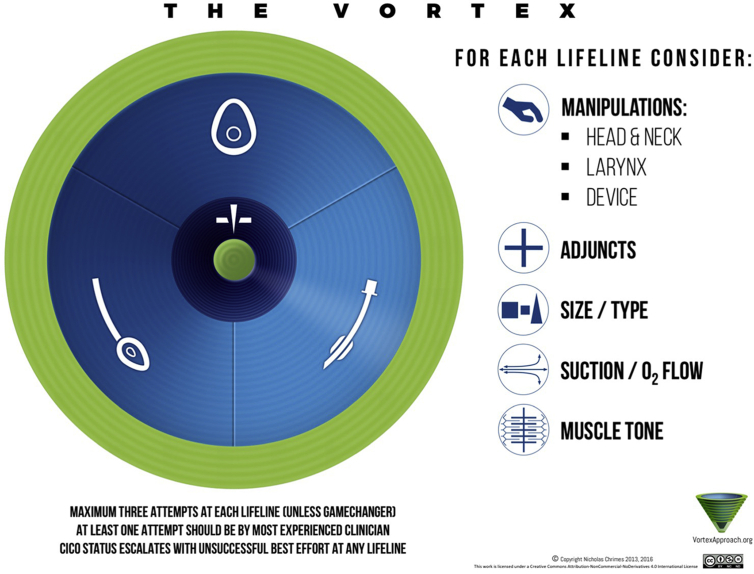
The Vortex approach to airway management is a ‘high acuity implementation tool’ designed to support team function and decision making in airway crisis management.26 It has been incorporated into the UK guidelines for tracheal intubation in critically ill adults.2 The tool is designed to be complimentary to text-based airway management algorithms, utilising a visual cognitive aid.26 It is based on the principle that there are three upper airway non-surgical methods for achieving alveolar oxygenation; tracheal intubation, SAD, and facemask ventilation, described as ‘lifelines’, each of which can be chosen for emergency airway management depending on the clinical situation. These are arranged in a circular fashion around a central zone representing CICO rescue (Fig. 4).
Figure 4.
The Vortex implementation tool. Copyright Nicholas Chrimes. Used with permission.
A failed attempt to achieve alveolar oxygenation using each ‘lifeline’ moves the situation towards the central CICO zone. Success in achieving alveolar oxygenation moves the situation back to the ‘green zone’; a place of relative patient safety giving time to restore oxygenation, assemble resources, and make a plan. The funnel concept used in the Vortex illustrates to the team that with each failure in a lifeline to restore oxygenation, there is diminishing time and options available before critical hypoxaemia will occur. If a best effort at any lifeline is unsuccessful, then ‘CICO status’ is initiated (Supplementary Fig. S6). This three-tiered implementation tool primes for eFONA using a ‘Ready, Set, Go’ prompt and is designed to facilitate early transition to eFONA by preparing the team and equipment. Once there is failure to achieve oxygenation after a best effort in all three ‘lifelines’, the team must perform eFONA, ‘Go’.
Training for eFONA
Regular training in eFONA is necessary in order to maintain technical and non-technical skills and promote skill retention. NAP4 identified poor training and education as being one of the commonest contributory causes to serious airway events requiring eFONA.1 This report recommends that all anaesthetists are trained in emergency cricothyroidotomy, maintain their skills, and learn cannula techniques alongside surgical techniques.1 Despite these recommendations, formal training on eFONA in the UK for all clinicians involved in airway management remains ad hoc, and there is currently no established guidance on frequency or methods for this training. The Australian and New Zealand College of Anaesthetists (ANZCA) mandates regular simulated management of eFONA for a CICO situation as part of their continuing professional development requirements.27
National, regional and local airway workshops on the management of CICO and eFONA using mannequin, cadaveric, or wet lab simulation, allow clinicians to acquire or refresh technical and non-technical skills. Training should be undertaken by all clinicians at regular intervals. Simulation training every 6 months promotes skill retention. DAS recommend eFONA training using initial technical skill development with low fidelity simulators, followed by high fidelity simulation to advance non-technical and psychological skills.28 RCoA Airway Leads should coordinate local multidisciplinary training, involving all members of the team who may be involved in eFONA, including surgeons, at regular intervals and using locally available equipment. Regular training improves team performance and should be undertaken in all areas of the hospital involved in airway management.
Departmental standards of care for eFONA equipment and training
The authors advocate the following standards of care with respect to eFONA equipment and training:
-
(i)
All clinicians involved in airway management, including surgeons who may be called to assist with eFONA, should be trained in emergency scalpel cricothyroidotomy using the ‘scalpel-bougie-tube’ technique.
-
(ii)
Additional techniques for eFONA should continue to be taught alongside the scalpel-bougie-tube technique.
-
(iii)
All clinicians involved in airway management should have regular simulated training on management of a CICO situation and eFONA, preferably every 6 months to encourage skill retention. A record of this training should be kept by the departmental airway lead. Anaesthetists and critical care doctors in training should record eFONA training as part of their annual review of competence progression.
-
(iv)
All areas of the hospital providing airway management should have a standardised eFONA kit in each airway trolley to allow consistency in equipment across the hospital. A size 6.0 cuffed tracheal tube, a number 10 blade scalpel, and a bougie should be included as a minimum.
-
(v)
Equipment for cannula cricothyroidotomy techniques should be present on the difficult airway trolley and the contents agreed at a local level.
-
(vi)
Regular multidisciplinary simulation training in CICO scenarios should be undertaken by all clinicians involved in airway management, including surgical teams. This training should take place in all areas of the hospital where airway management occurs, using locally available equipment.
-
(vii)
All clinicians involved in airway management must be familiar with current national guidance for the management of a CICO situation and eFONA.
-
(viii)
All areas of the hospital involved in airway management should have immediate access to an ultrasound machine to facilitate identification of the CTM when required. Training in ultrasound identification of the CTM should be offered locally or regionally.
Acknowledgments
The authors wish to thank Dr Michael Kristensen for his advice on the ultrasound section of the article and for allowing the reproduction of the ultrasound images and videos, and Dr Nicholas Chrimes for permission to use the Vortex tool and CICO status images.
Biographies
Thomas Price FRCA FFICM is an airway fellow and specialty registrar in anaesthesia and intensive care medicine at the Royal Victoria Hospital, Belfast.
Eamon McCoy MD FFARCSI is a consultant anaesthetist at the Royal Victoria Hospital whose interests are in major trauma, head and neck surgery, and difficult airway management. As an expert in difficult airway management he teaches locally, nationally, and internationally. Dr McCoy has worked in major trauma in various areas of conflict with the medical charity IDEALS. He has several publications in the area of airway management and invented the McCoy laryngoscope, of which more than 100,000 are used in more than 100 countries worldwide.
Matrix codes: 1I03, 2A01, 3C00
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bjae.2019.04.002.
Declaration of interest
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Supplementary data
The following are the Supplementary data to this article:
Supplementary figure 1.
Difficult Airway Society algorithm for tracheal intubation in critically ill adults. With permission of the Difficult Airway Society.
Supplementary figure 2.
Difficult Airway Society guidelines for the management of tracheal intubation in critically ill adults - “Can’t intubate, Can’t oxygenate” algorithm. With permission of the Difficult Airway Society.
Supplementary figure 3.
Laryngeal handshake. Step 1: Using the thumb and index finger of the non-dominant hand, palpate the top of the larynx and roll from side to side. Step 2: Slide the finger and thumb down over the thyroid laminae. Step 3: Palpate the cricoid cartilage with the middle finger and thumb. Now use the index finger to palpate the cricothyroid membrane.
Supplementary figure 4The longitudinal ‘string of pearls’ method for ultrasound identification of the cricothyroid membrane. With permission from Michael S. Kristensen, The Scandinavian Airway management course, www.airwaymanagement.dk, illustration from British Journal of Anaesthesia 2016; 117(S1): i39-i48.
Supplementary figure 5.
‘Scalpel-bougie-tube’ cricothyroidotomy technique.
Supplementary figure 6.
The CICO status implementation tool. Copyright Nicholas Chrimes. Used with permission.
References
- 1.Cook T.M., Woodall N., Frerk C. Fourth National Audit Project of the Royal College of Anaesthetists and Difficult Airway Society. In: Cook T.M., Woodall N., Frerk C., editors. Major complications of airway management in the United Kingdom. Report and findings. Royal College of Anaesthetists; London: London: 2011. [DOI] [PubMed] [Google Scholar]
- 2.Higgs A., McGrath B.A., Goddard C. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–352. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Peterson G.N., Domino K.B., Caplan R.A., Posner K.L., Lee L.A., Cheney F.W. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103:33–39. doi: 10.1097/00000542-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Frerk C., Mitchell V.S., McNarry A.F. Difficult Airway Society 2015 guidelines for the management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–848. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weightman W., Gibbs N.M. Prevalence of major vessels anterior to the trachea at sites of potential front-of-neck emergency airway access in adults. Br J Anaesth. 2018;121:1166–1172. doi: 10.1016/j.bja.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 6.Bair A.E., Chima R. The inaccuracy of using landmark techniques for cricothyroid membrane identification: a comparison of three techniques. Acad Emerg Med. 2015;22:908–914. doi: 10.1111/acem.12732. [DOI] [PubMed] [Google Scholar]
- 7.Campbell M., Shanahan H., Ash S., Royds J., Husarova V., McCaul C. The accuracy of locating the cricothyroid membrane by palpation—an intergender study. BMC Anaesthesiol. 2014;14:108. doi: 10.1186/1471-2253-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.You-Ten K.E., Desai D., Postnogova T., Siddiqui N. Accuracy of conventional digital palpation and ultrasound of the cricothyroid membrane in obese women in labour. Anaesthesia. 2015;70:1230–1234. doi: 10.1111/anae.13167. [DOI] [PubMed] [Google Scholar]
- 9.Drew T., McCaul C.L. Laryngeal handshake technique in localising the cricothyroid membrane: a non-randomised comparative study. Br J Anaesth. 2018;121:1173–1178. doi: 10.1016/j.bja.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 10.Kristensen M.S., Teoh W.H., Rudolph S.S. Structured approach to ultrasound-guided identification of the cricothyroid membrane: a randomized comparison with the palpation method in the morbidly obese. Br J Anaesth. 2015;114:1003–1004. doi: 10.1093/bja/aev123. [DOI] [PubMed] [Google Scholar]
- 11.Kristensen M.S., Teoh W.H., Rudolph S.S. Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact. Br J Anaesth. 2016;117(S1):i39–i48. doi: 10.1093/bja/aew176. [DOI] [PubMed] [Google Scholar]
- 12.Airway management for anaesthesiologists. TACA; 2016. http://airwaymanagement.dk/taca Available from: [Google Scholar]
- 13.Airway management for anaesthesiologists. pearls; 2016. http://airwaymanagement.dk/pearls Available from: [Google Scholar]
- 14.Kristensen M.S., Teoh W.H., Rudolph S.S., Hesselfeldt R., Børglum J., Tyede M.F. A randomised cross-over comparison of the transverse and longitudinal techniques for ultrasound-guided identification of the cricothyroid membrane in morbidly obese subjects. Anaesthesia. 2016;71:675–683. doi: 10.1111/anae.13465. [DOI] [PubMed] [Google Scholar]
- 15.Lockey D., Crewdson K., Weaver A., Davis G. Observational study on the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations in trauma patients by pre-hospital physicians. Br J Anaesth. 2014;113:220–225. doi: 10.1093/bja/aeu227. [DOI] [PubMed] [Google Scholar]
- 16.Langvad S., Hyldmo P.K., Nakstad A.R., Vist G.E., Sandberg M. Emergency cricothyrotomy—a systematic review. Scand J Trauma Resusc Emerg Med. 2013;21:43. doi: 10.1186/1757-7241-21-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DAS front of neck access training video. Available from: https://das.uk.com/content/video/fona (accessed 21 December 2018).
- 18.Duggan L.V., Ballantyne Scott B., Law J.A., Morris I.R., Murphy M.F., Griesdale D.E. Transtracheal jet ventilation in the ‘can’t intubate can’t oxygenate’ emergency: a systematic review. Br J Anaesth. 2016;117(S1):i28–i38. doi: 10.1093/bja/aew192. [DOI] [PubMed] [Google Scholar]
- 19.Greenland K.B., Bradley W.P.L., Chapman G.A., Goulding G. Emergency front-of-neck access: scalpel or cannula—and the parable of buridan’s ass. Br J Anaesth. 2017;118:811–814. doi: 10.1093/bja/aex101. [DOI] [PubMed] [Google Scholar]
- 20.Cook T.M. Response to: emergency front-of-neck access: scalpel or cannula—and the parable of buridan’s ass. Br J Anaesth. 2017;119:840–841. doi: 10.1093/bja/aex314. [DOI] [PubMed] [Google Scholar]
- 21.Heard A.M.B., Green R.J., Eakins P. The formulation and introduction of the “can't intubate, can't ventilate” algorithm into clinical practice. Anaesthesia. 2009;64:601–608. doi: 10.1111/j.1365-2044.2009.05888.x. [DOI] [PubMed] [Google Scholar]
- 22.Pracy J.P., Brennan L., Cook T.M. Surgical intervention during a can’t intubate can’t oxygenate (CICO) event: emergency front-of-neck airway (FONA)? Br J Anaesth. 2016;117:426–428. doi: 10.1093/bja/aew221. [DOI] [PubMed] [Google Scholar]
- 23.Australian and New Zealand College of Anaesthetists CICO and front of neck access. http://www.anzca.edu.au/front-page-news/cico-and-front-of-neck-access Available from:
- 24.Law J.A., Broemling N., Cooper R.M. The difficult airway with recommendations for management—part 1—difficult tracheal intubation encountered in an unconscious/induced patient. Can J Anaesth. 2013;60:1089–1118. doi: 10.1007/s12630-013-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Apfelbaum J.L., Hagberg C.A., Caplan R.A. Practice guidelines for management of the difficult airway: an updated report by the American society of anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013;118:251–270. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 26.Chrimes N. The vortex: a universal ‘high acuity implementation tool’ for emergency airway management. Br J Anaesth. 2016;117(S1):i20–i27. doi: 10.1093/bja/aew175. [DOI] [PubMed] [Google Scholar]
- 27.Australian and New Zealand College of Anaesthetists Management of “can't intubate, can't oxygenate” (CICO) http://www.anzca.edu.au/fellows/continuing-professional-development/breakdown-of-cpd-activities/management-of-can-t-intubate,-can-t-oxygenate Available from:
- 28.Difficult Airway Society Cricothyroidotomy trainer review. https://das.uk.com/cricothyroidotomy_trainer_review Available from: