Abstract
Chicago Classification v4.0 (CCv4.0) is the updated classification scheme for esophageal motility disorders using metrics from high-resolution manometry (HRM). Fifty-two diverse international experts separated into seven working sub-groups utilized formal validated methodologies over two-years to develop CCv4.0. Key updates in CCv.4.0 revolve around a more rigorous and expansive protocol that incorporates different positions and provocative testing, a refined definition of esophago-gastric junction (EGJ) outflow obstruction (EGJOO), an increased threshold for the diagnosis of ineffective esophageal motility and inclusion of a description of baseline EGJ metrics. Further, the CCv4.0 sought to define motility disorder diagnoses as conclusive and inconclusive based on associated symptoms, the use of provocative testing and corroborating supportive testing with barium esophagram with tablet and/or functional lumen imaging probe. These changes attempt to minimize ambiguity in prior iterations of Chicago Classification and provide more standardized and rigorous criteria for patterns of disorders of peristalsis and obstruction at the EGJ.
INTRODUCTION
The Chicago Classification categorizes esophageal motility disorders via an algorithmic scheme using metrics from esophageal high-resolution manometry (HRM). The first full version of the Chicago Classification was published in 2009, with two updates, most recently version 3.0 published in 2015.1–3 Over the past 5 years, both clinical applications and research investigations involving HRM have expanded, with introduction of novel HRM metrics. Therefore, an International HRM Working Group of 52 members worked for two years to develop the Chicago Classification version 4.0 (CCv4.0). This overview document will summarize the CCv4.0 initiative and present the updated modern-day Chicago Classification of esophageal motility disorders. Although the Chicago Classification provides a framework for classification of esophageal motility disorders based on HRM, the final clinical diagnosis may require supportive testing to inform clinical decisions, particularly in borderline cases or instances where discordant findings are noted in different positions or during provocative testing.
METHODS
The CCv4.0 Working Group is comprised of 52 members selected by six international motility societies, representative of 20 countries. Characteristics of the working group are detailed in Supplemental Table 1. The CCv4.0 initiative was a two-year process (November 2018 to October 2020) which included three international meetings (May 2019, San Diego, CA; October 2019, Barcelona, Spain; August 2020, web-conference), multiple sub-group meetings, and seven surveys.
An initial survey conducted in January 2019 identified priority areas for update and modification from the previous 3.0 version (Supplemental Table 1). Accordingly, members were assigned to seven sub-groups: Standard HRM protocol, Achalasia, Esophagogastric junction (EGJ) outflow obstruction (EGJOO), Distal esophageal spasm (DES), Hypercontractile esophagus, Ineffective esophageal motility (IEM), and EGJ metrics. Each sub-group was led by two co-chairs and included a non-voting member who independently reviewed supportive literature and assessed level of evidence. Co-chairs and sub-group members were tasked with developing statements to define a conclusive diagnosis of the motility disorder assigned to their sub-group, as well as to describe inconclusive scenarios for motility disorders and the value of supportive testing. These statements were based on literature review and expert consensus.
In addition to expert consensus, a priority for CCv4.0 was to utilize formally validated methodologies to determine both appropriateness of statements, and level of supportive evidence for each statement. The RAND Appropriateness Method (RAM) was utilized, with two rounds of independent electronic voting to determine appropriateness of each statement per RAM using University of California San Diego Research Electronic Database Capture (REDCap). Statements were considered appropriate when meeting ≥80% agreement, and are included in the final CCv4.0.4, 5 Statements with ≥85% agreement were considered strong recommendations, while those with 80 to 85% agreement were considered conditional recommendations. Statements nearly meeting criteria and/or those generating controversy were discussed at working group meetings. Additionally, statements that met criteria for inclusion in the final CCv4.0 underwent further independent evaluation to assess the level of supportive evidence, using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process, when possible.6 Two experts external to the working sub-groups, one a formally trained GRADE methodologist, independently evaluated the supportive literature provided by the sub-groups. Some statements were not amenable to the GRADE process, either because of the structure of the statement or lack of available evidence.
This document summarizes the final recommendations of the CCv4.0 working group. Separate technical reviews specific to each working group will summarize the statement development process, survey results, and supporting literature. These will be published separately in future issues of Neurogastroenterology and Motility over the coming months.
STANDARD HRM PROTOCOL & THRESHOLDS
Standard HRM Protocol
An important priority of the Chicago Classification was a standardized manometry protocol for motility laboratories around the world, to facilitate procedural consistency, improve diagnostic reliability, and promote collaborative research. The final standard esophageal HRM protocol is summarized below, in Figure 1, and depicted in Figure 2. Details regarding positions, maneuvers and bolus consistency are described in the subsequent technical review on HRM protocol.
Figure 1.
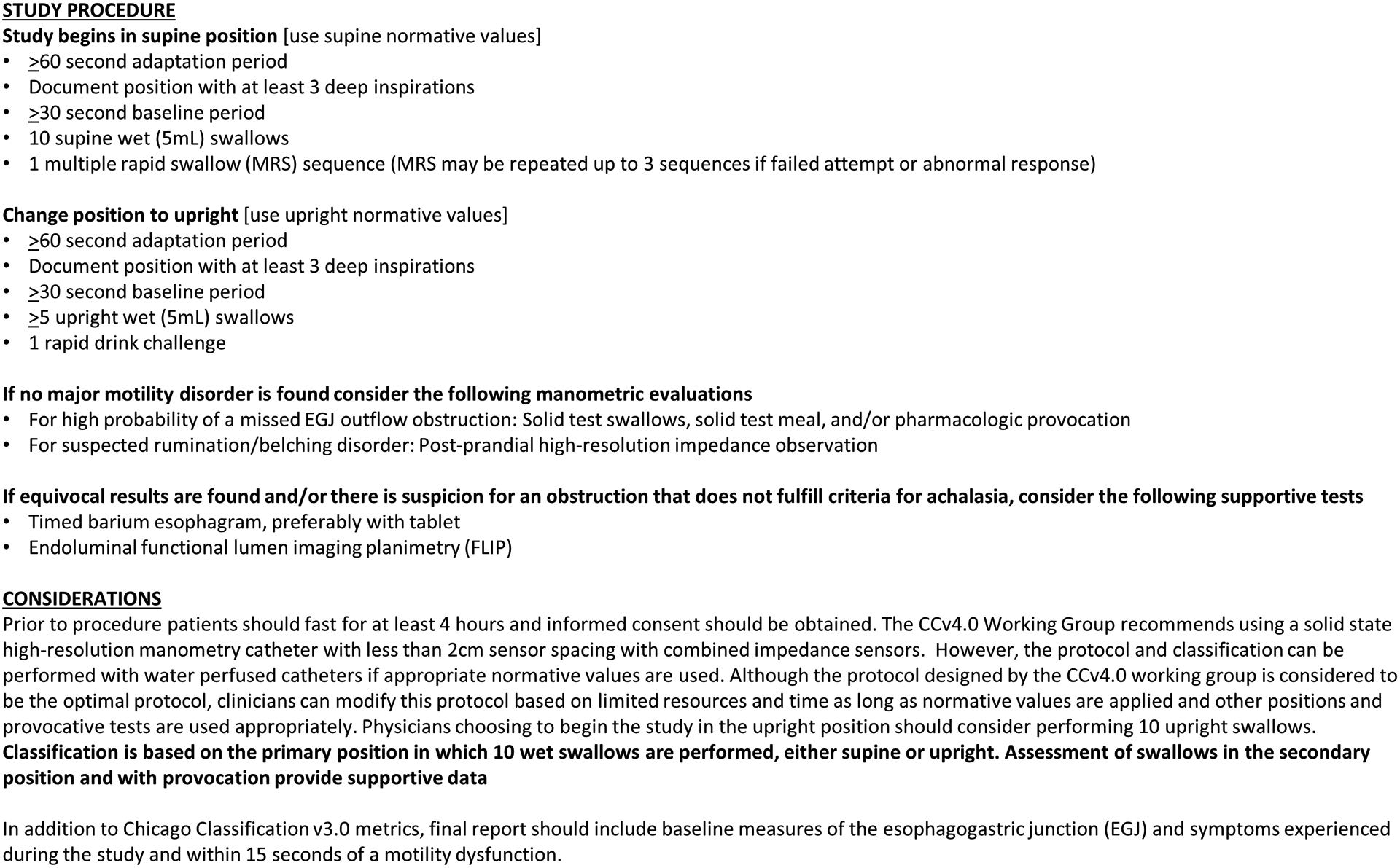
Standard high-resolution esophageal manometry protocol per CCv4.0
Figure 2.

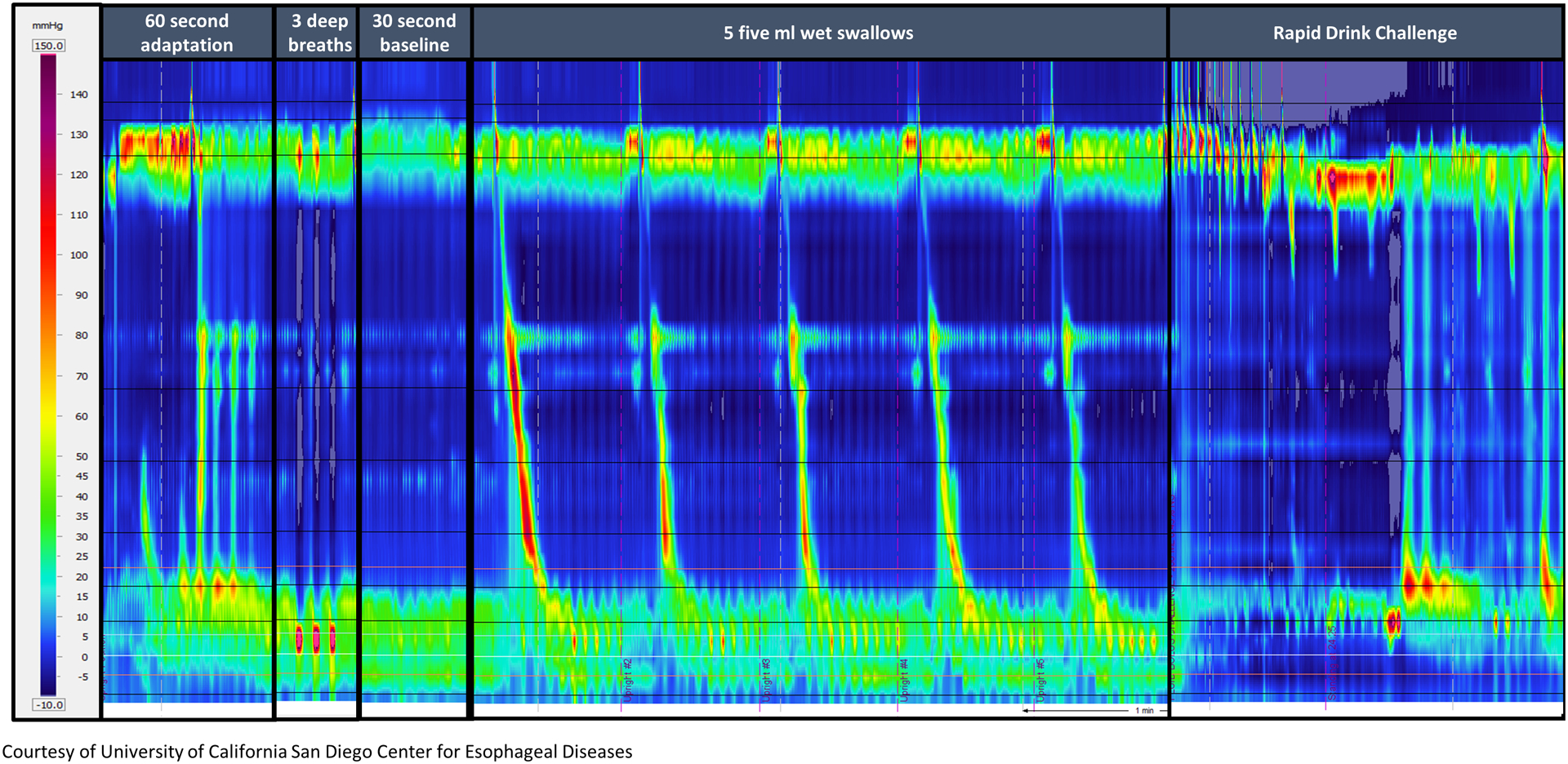
High-resolution manometry images depicted the standard protocol. 2A) The supine position includes a 60 second adaptation period, 3 deep breaths, 30 second baseline period, 10 five ml wet swallows and at least one multiple rapid swallow. 2B) Position is changed to the upright position followed by a 60 second adaptation, 3 deep breaths, 30 second baseline period, 5 five ml wet swallows and a rapid drink challenge.
Prior to the procedure, patients should fast for at least 4 hours (small amounts of clear fluid allowed) and informed consent should be obtained.
The study begins in the supine position (Figure 2A). Following catheter placement, a minimum of 60 seconds of quiet rest allows for an adaptation period, following which catheter position is confirmed using a minimum of three deep inspirations. Next, a baseline period of at least 30 seconds is captured to enable identification of anatomic landmarks including the upper esophageal sphincter (UES), lower esophageal sphincter (LES), respiratory inversion point (RIP), and basal EGJ pressure. Following this, ten 5 ml wet swallows of ambient temperature water or saline (when using high resolution impedance manometry) are performed. There should be at least 30 seconds between wet swallows to avoid effects of deglutitive inhibition. Finally, one multiple rapid swallow (MRS) sequence is performed (five 2 mL wet swallows administered using a 10 mL syringe 2–3 seconds apart), which can be repeated up to three times if there is a failed attempt or an abnormal contractile response.7, 8
Patient position is then changed to the upright position (sitting at 80 degrees or higher with legs hanging off side of bed, but not hunched or leaning over) (Figure 2B). Following the position change, a minimum of 60 seconds to allow for adaptation, a minimum of three deep inspirations to assess catheter position, and a baseline period of at least 30 seconds to enable identification of anatomic landmarks are once again performed. Next, at least five 5 ml wet swallows are performed. There should be at least 30 seconds between wet swallows to avoid effects of deglutitive inhibition. Finally, one rapid drink challenge (RDC) with 200 ml water, ingested as fast as possible through a straw, is performed.9
If no conclusive evidence of a major motility disorder is identified, if results from the standard esophageal HRM protocol are not fully consistent with clinical presentation and/or if findings do not explain patient symptoms, additional HRM supportive measures can be considered including solid test swallows and solid test meal to assess for EGJ obstruction, and/or post-prandial observation for rumination and/or belching disorder.10 Pharmacologic provocation can also be performed during the initial protocol to help support a diagnosis of a true disorder of EGJ obstruction. (Supplemental Figures 1–3)11
Additionally, if equivocal results are identified and/or there is a suspicion for an EGJ outflow obstruction that does not fulfill the criteria for achalasia, a timed barium esophagram (TBE), preferably with tablet, and/or endoluminal functional lumen imaging probe (FLIP) should be obtained as an independent supportive test to assess for EGJ obstruction.12, 13
The CCv4.0 Working Group recommends using a solid-state HRM catheter with less than 2cm sensor spacing. However, the protocol and classification can be performed with water perfused catheters if appropriate normative values are used (with the limitation of only supine swallows and maneuvers possible with water perfused manometry). Using high-resolution impedance manometry is recommended, though not required, to optimally assess intrabolus pressure, bolus clearance and bolus flow through the EGJ. The protocol should be performed as efficiently as possible to minimize potential of pressure drift, reduce patient discomfort and improve patient tolerance.
Diagnostic Thresholds and Definitions (Table 1)
Table 1.
HRM Metrics and Thresholds
| Assessment | Pressure Topography Metrics | Definition | Diagnostic Threshold | Additional Considerations |
|---|---|---|---|---|
| Relaxation pressure across the esophago-gastric junction in response to deglutition | Integrated relaxation pressure (IRP) | Mean of the 4s of maximal deglutitive relaxation in the 10-s window beginning at UES relaxation, contiguous or non-contiguous, referenced to gastric pressure | Abnormal deglutitive IRP relaxation:
|
IRP > 12mmHg (Medtronic) on rapid drink challenge (RDC) or IRP > 25mmHg (Medtronic) on solid test meal supports outflow obstruction |
| Esophageal peristalsis | Distal Contractile Integral (DCI) – Contractile Vigor | Amplitude × duration × length (mmHg·s·cm) of the distal esophageal contraction exceeding 20 mmHg from the transition zone to the proximal margin of the LES |
|
Intact contractile response on multiple rapid swallow (MRS): DCI < 100 mmHg·s·cm during MRS and DCI greater than single swallow mean DCI following MRS |
| Contractile Wavefront Integrity | Contiguity of peristalsis in an isobaric contour of 20 mmHg |
|
||
| Latency of deglutitive inhibition | Distal latency (DL) | Interval between UES relaxation and CDP |
|
|
| Pressurization | Isobaric Contour |
|
Panesophageal pressurization >20mmHg on RDC or solid test meal supports outflow obstruction |
Upper esophageal sphincter (UES); lower esophageal sphincter (LES)
The key HRM metrics utilized in the CCv4.0 remain assessment of deglutitive relaxation across the LES/EGJ using integrated relaxation pressure (IRP), vigor of esophageal body contraction using distal contractile integral (DCI), contractile wavefront integrity at 20mmHg isobaric contour setting, and latency of deglutitive inhibition using distal latency (DL). The thresholds for median IRP are higher in the supine position compared to the upright position. The thresholds for DCI and DL are the same for both supine and upright positions.
Integrated Relaxation Pressure:
Threshold for median IRP in the supine position remains 15mmHg for Medtronic systems and 22mmHg for Laborie/Diversatek systems (Moderate GRADE, Strong Recommendation).14–17
Threshold for median IRP in the upright position is 12mmHg for Medtronic systems and 15mmHg for Laborie/Diversatek systems (Low GRADE, Strong Recommendation).16–18
Contractility in the Esophageal Body:
Measured by contractile vigor and contractile pattern.16, 17
Normal Contraction: DCI of 450 mmHg•s•cm to 8,000 mmHg•s•cm
- Ineffective Swallow includes any of the following:
- Weak Contraction: DCI between 100 mmHg•s•cm and less than 450 mmHg•s•cm
- Failed Peristalsis: DCI less than 100 mmHg•s•cm
- Fragmented Swallow: Transition zone defect of peristalsis greater than 5cm under an isobaric contour of 20mmHg in the setting of a DCI of 450 mmHg•s•cm or greater
- Hypercontractile Swallow: DCI greater than 8,000 mmHg•s•cm.
- Available literature on normal values suggests that the threshold of 8,000 mmHg•s•cm is suitable across HRM systems.
Latency of Deglutitive Inhibition:
DL is measured as the interval from the start of relaxation of the UES to the contractile deceleration point (CDP). The CDP is the inflection point between the proximal rapid and the distal slow phase of the esophageal contraction, located within 3 cm of the proximal aspect of the pre-swallow EGJ high-pressure zone. Physiologically this likely represents conversion from smooth muscle esophageal body contraction to the LES after-contraction.
Premature contraction: A distal latency shorter than 4.5 seconds, in the setting of a DCI of 450 mmHg•s•cm or greater16
If the CDP is difficult to determine, a horizontal line can be drawn 2–3 cm above the proximal aspect of the pre-swallow EGJ high-pressure zone and the DL can be determined by the duration of time from the start of the UES relaxation to the intersection at the contractile wave-front. It is important that this horizontal line is extended to the contraction and not to the pressurization front that can be compartmentalized ahead of the peristaltic contractile wave-front.
Esophageal contractile activity must be distinguished from other causes of pressure rise in the distal esophagus such as intrabolus pressure and/or artifact. (Very Low GRADE, Strong Recommendation)19, 20
Pressurization
Panesophageal pressurization: The cut-off for panesophageal pressurization is set at 30 mmHg using the isobaric contour tool (Very Low GRADE, Strong Recommendation).21
Intrabolus pressurization: The intrabolus pressure threshold for supine wet swallows using the Medtronic system is 20mmHg using the isobaric contour tool (Moderate GRADE, Strong Recommendation).14, 22, 23
Response to Provocation (Table 2)
Table 2.
Supportive Manometric Measures which may Increase Confidence for a Disorder
| Supportive Measure | Protocol | Normal Response |
|---|---|---|
| Multiple Rapid Swallow (MRS) | Five swallows of 2‐mL liquid at 2‐3 second intervals | Absence of esophageal body contractility (DCI < 100 mmHg•s•cm) with complete deglutitive inhibition of the LES during MRS and presence of post-MRS contraction augmentation (DCI post MRS greater than single swallow mean DCI). |
| Rapid Drink Challenge (RDC) | Rapid drink of 200ml of liquid | Absence of esophageal body contractility (DCI < 100 mmHg•s•cm) with complete deglutitive inhibition of the LES during RDC and no evidence of major motility disorder post-RDC. |
| Solid Test Swallow | Ten swallows of ~1-cm3 soft solid (e.g. bread, soft boiled rice, marshmallow) | Presence of >20% pharyngeal swallows being followed by an effective esophageal contraction defined by DCI > 1000 mmHg•s•cm and without a large break (>5 cm) in the contractile front. |
| Solid Test Meal (STM) | 200g of soft solid meal (e.g. soft boiled rice, bread) ingested at normal rate for patient. Study stopped if STM not completed in 8-min. | Presence of >20% pharyngeal swallows being followed by an effective esophageal contraction defined by DCI > 1000 mmHg-s-cm and without a large break (>5 cm) in the contractile front. No symptoms during STM (any symptoms should be recorded in electronic record to assess association with abnormal motility or function). Slow eating with <200g ingested during 8-minutes also considered abnormal. |
| Post-Prandial Meal (High-resolution impedance manometry) | Administration of a STM or a self-identified symptom inducing meal followed by extended monitoring (minimum of 10 minutes and occurrence of abnormal activity) | Absence of symptoms and abnormal motility or function during postprandial period. Maximum 4 transient LES relaxations (TLESRs) with belching during initial 10-minutes post-prandial, no volume regurgitation, no rumination or supra-gastric belching episodes. |
| Pharmacologic Provocation | Amyl Nitrite inhalator (4–5 sniffs) in recumbent position | Profound distal esophageal and LES smooth muscle inhibition with reduction in deglutitive IRP. In healthy controls amyl nitrite-induced EGJ IRP is similar to deglutitive IRP. In patients with a disorder of EGJ obstruction, such as achalasia and true functional EGJOO, amyl nitrite-induced EGJ pressure drop is markedly lower (≥10mmHg) than compromised deglutitive IRP (i.e., relaxation gain). In contrast, amyl nitrite in patients with EGJOO secondary to other factors than LES smooth muscle dysfunction will display little amyl nitrite-induced EGJ pressure change (< 10mmHg). |
| Cholecystokinin (CCK) 40ng/kg IV in recumbent position | CCK generally triggers a biphasic esophageal motor response. Phase 1 is always present and starts shortly after injection. In healthy controls, CCK induces a mild esophageal shortening (2cm or less) associated with incomplete EGJ relaxation (inspiratory crural diaphragm contraction preserved). In contrast, CCK in patients with inhibitory dysfunction such as achalasia induces a paradoxical EGJ contraction of more than 50 mmHg. |
Distal Contractile Integral (DCI); lower esophageal sphincter (LES); integrated relaxation pressure (IRP); esophago-gastric junction (EGJ); EGJ outflow obstruction (EGJOO)
Classification is based on the primary position in which 10 wet swallows are performed, either supine or upright. Assessment of swallows in the secondary position and with provocation serve as supportive data (with the exception of EGJOO and absent contractility).
Multiple Rapid Swallow: An intact response to MRS is defined as absence of esophageal body contractility (DCI < 100 mmHg•s•cm) with complete deglutitive inhibition of the LES during the repetitive swallows, and presence of post-MRS contraction augmentation (DCI post-MRS greater than single swallow mean DCI).7, 24–26 The post-MRS contraction needs to be true peristaltic contractility and not artifact or pressurization.
Rapid Drink Challenge: An intact response to RDC is defined as absence of esophageal body contractility (DCI < 100 mmHg•s•cm) with complete deglutitive inhibition of the LES during the RDC. When assessing response to RDC, IRP >12mmHg (using Medtronic software) over the first 30 seconds of the RDC challenge and panesophageal pressurization >20mmHg are criteria for outflow obstruction (Low GRADE, Conditional Recommendation).9, 26–29 The presence of a normal contraction sequence following the RDC is a specific marker of normal contractility; however, this is not present in all healthy controls.9, 27, 28
Solid Test Swallows: An intact esophageal body contractile response to solid swallows requires presence of >20% pharyngeal swallows, followed by an effective esophageal contraction defined by DCI > 1000mmHg•s•cm and without a large break (>5 cm) in the contractile front. The upper limit of normal IRP (using Medtronic software) with solid swallows is 25mmHg.30 Temporal association of ineffective contractions with patient symptoms (e.g. dysphagia) supports diagnosis of clinically relevant, abnormal peristaltic function.10, 29
Pharmacologic Provocation: If available at the motility lab, pharmacologic provocation using either an amyl nitrite and/or cholecystokinin protocol can be useful to evaluate physiology at the EGJ. The protocol and physiologic responses to pharmacologic provocation are detailed in Table 2.31, 32
Key Considerations for Protocol in Context of the Chicago Classification
It is expected that the majority of labs will continue with the convention of starting the manometry protocol in the supine position. Although the standard HRM protocol described is considered to be optimal and inclusive, clinicians can modify this protocol to adapt to available resources and time, as long as established normative values are applied and other positions and supportive measures are used appropriately. Clinicians choosing to begin the study in the upright position should perform 10 upright swallows at the outset.
CHICAGO CLASSIFICATION v4.0 OF ESOPHAGEAL MOTILITY DISORDERS
The hierarchical classification scheme of the Chicago Classification is maintained in CCv4.0, whereby motility disorders are classified as disorders of EGJ outflow and/or disorders of peristalsis (Table 3, Figure 3). The classification scheme applies to patients with normal foregut anatomy, without prior surgical or invasive foregut intervention and without large hiatal hernias and/or paraesophageal hernias, as these anatomical changes can alter measurement of the CC metrics and are associated with contact artifacts due to bending of the catheter that may persist after position change. Additionally, a careful index endoscopy is crucial prior to manometry testing, as endoscopic or radiographic evidence of mechanical obstruction precludes the use of CCv4.0. An additional update in CCv4.0 is the emphasis that specific motility disorders should be considered clinically relevant only in the context of compatible symptoms and/or supportive testing, as detailed in this document and indicated by an asterisk in the figures.
Table 3.
Classification and Definition of Manometric Disorders
| Classification | Disorder | Definition |
|---|---|---|
| Disorders of EGJ Outflow | Type I Achalasia | Abnormal median IRP & 100% failed peristalsis |
| Type II Achalasia | Abnormal median IRP, 100% failed peristalsis, & ≥20% swallows with panesophageal pressurization | |
| Type III Achalasia∞ | Abnormal median IRP & ≥20% swallows with premature/spastic contraction and no evidence of peristalsis | |
| EGJ Outflow Obstruction*† | Abnormal median IRP (supine and upright), ≥20% elevated intrabolus pressure (supine), and not meeting criteria for achalasia | |
| Disorders of Peristalsis | Absent Contractility | Normal median IRP (supine and upright) & 100% failed peristalsis |
| Distal Esophageal Spasm* | Normal median IRP & ≥20% swallows with premature/spastic contraction | |
| Hypercontractile Esophagus* | Normal median IRP & ≥20% hypercontractile swallows | |
| Ineffective Esophageal Motility | Normal median IRP, with >70% ineffective swallows or ≥50% failed peristalsis |
CCv4.0 recognizes that the distinction between type III achalasia and conclusive EGJOO can be difficult and was vague in CCv3.0. In CCv4.0 achalasia is defined by 100% absent peristalsis which is inclusive of swallows that are either failed or premature and Type III achalasia should not have evidence of normal peristalsis [normal or ineffective swallows].
Patients with EGJ obstruction and evidence of peristalsis would fulfill strict criteria for EGJOO and may have features suggestive of achalasia or other patterns of peristalsis defined by criteria used for disorders of peristalsis: EGJOO with spastic features [presence of ≥ 20% premature swallows], EGJOO with hypercontractile features, EGJOO with ineffective motility, or EGJOO with no evidence of disordered peristalsis.
Denote manometric patterns of unclear clinical relevance. A clinically relevant conclusive diagnosis requires additional information which may include clinically relevant symptoms and/or supportive testing (as detailed in the document).
Distal Contractile Integral (DCI); integrated relaxation pressure (IRP); esophagogastric junction (EGJ)
Figure 3.

Chicago Classification 4.0 Hierarchical Classification Scheme. This flow diagram represents a conceptual model of a state of the art algorithm that defines the flow process of how the CCv4.0 diagnosis is generated within the constructs of the various phases of the protocol. In this conceptual model, the current protocol allows for some flexibility if the diagnosis is conclusive with 10 swallows in either the primary supine or upright position and allows for a sequenced progression of the protocol to help confirm or rule out the diagnosis. This flow diagram represents the optimal flow process, however exceptions will exist based on the fact that some cutoffs are arbitrary and that the model assumes that a motility expert or a highly qualified motility technician or nurse is performing the protocol and analysis. *Denote manometric patterns of unclear clinical relevance. A clinically relevant conclusive diagnosis requires additional information which may include clinically relevant symptoms and/or supportive testing (as detailed in the document). †Patients with EGJ obstruction and presence of peristaltic swallows would fulfill strict criteria for EGJOO and may have features suggestive of achalasia or other patterns of peristalsis defined by criteria for disorders of peristalsis: EGJOO with spastic features, EGJOO with hypercontractile esophagus, EGJOO with ineffective motility, or EGJOO with no evidence of disordered peristalsis. ‡ RDC, solid test swallows, and/or pharmacologic provocation with amyl nitrite or cholecystokinin (if available) can be instituted here to assess for obstruction. ◊Patients previously defined absent contractility based on 10 swallows in the primary position may have achalasia if the IRP is elevated in the alternate position, with the RDC, and/or with MRS. These cases should be considered inconclusive for type I or II achalasia as appropriate and evaluated further with TBE/FLIP. ¥ If no evidence of a disorder of peristalsis or EGJ outflow in a patient with high probability of a missed EGJOO, a solid test meal can be added to rule out an obstructive pattern; if abnormal then possibility of a mechanical obstruction should be readdressed. In a patient with regurgitation or belching post-prandial high-resolution impedance monitoring to assess for rumination/belching disorder.
Integrated relaxation pressure (IRP); Multiple rapid swallow (MRS); Rapid drink challenge (RDC); Lower esophageal sphincter (LES); Intrabolus pressurization (IBP); Panesophageal pressurization (PEP); Esophagogastric junction (EGJ): EGJ outflow obstruction (EGJOO); Timed barium esophagram (TBE); Functional lumen imaging probe (FLIP)
DISORDERS OF EGJ OUTFLOW (Supplemental Table 2)
Consistent with prior iterations of Chicago Classification, disorders of EGJ outflow include achalasia (types I, II, and III) and EGJ outflow obstruction. All disorders of EGJ outflow require an abnormal median IRP in the primary position. Given the high pre-test probability of achalasia with the requirement of 100% absent peristalsis, an abnormal IRP in the primary position is considered conclusive for achalasia. On the other hand, the presence of appreciable peristalsis in EGJOO lowers the pre-test probability of true LES dysfunction, and thus a conclusive manometric diagnosis of EGJOO requires an abnormal median IRP in both primary and secondary positions, as well as complimentary testing to confirm the diagnosis.
ACHALASIA
CCv4.0 maintains three subtypes of achalasia: type I akin to classic achalasia, type II seen with panesophageal pressurization, and type III, or spastic, achalasia (Figure 4). As mentioned, a CCv4.0 update for achalasia is that an abnormal median IRP can be observed in either a primary supine position or a primary upright position (if performed with 10 wet swallows), and does not require an abnormal median IRP in both supine and upright positions. Further, in CCv4.0 a definition of achalasia requires 100% absent peristalsis, defined as all swallows with either failed peristalsis or premature contraction.
Figure 4.

Achalasia Subtypes. Type I Achalasia: integrated relaxation pressure (IRP) is elevated with failed peristalsis (distal contractile integral (DCI) < 100 mmHg-s-cm), and without panesophageal pressurization. Type II Achalasia: IRP is elevated with failed peristalsis and panesophageal pressurization. Type III Achalasia: IRP is elevated with a normal DCI, and a reduced distal latency. Not applicable (NA)
TYPE I ACHALASIA:
A conclusive diagnosis of type I achalasia is defined as an abnormal median IRP and absent contractility (100% failed peristalsis) (Very Low GRADE, Strong Recommendation).21, 33–36
TYPE II ACHALASIA:
A conclusive diagnosis of type II achalasia is defined as an abnormal median IRP and absent contractility (100% failed peristalsis) with panesophageal pressurization in 20% or more swallows (Very Low GRADE, Strong Recommendation).21, 33–36
TYPE III ACHALASIA:
A conclusive diagnosis of type III achalasia is defined as an abnormal IRP and evidence of spasm (20% or more swallows with premature contraction) with no evidence of peristalsis (Very Low GRADE, Strong Recommendation).21, 33–36
Inconclusive Diagnosis of Achalasia (Figure 5)
Figure 5.

Inconclusive Diagnosis for Achalasia or Absent Contractility Requires Supportive Testing. Findings are inconclusive for type I achalasia or absent contractility as there is 100% failed peristalsis but the median integrated relaxation pressure (IRP) is at the upper limit of normal with 5ml wet swallows. With the rapid drink challenge there is absence of deglutitive inhibition across the lower esophageal sphincter (LES). Supportive testing is required in the setting of inconclusive findings with timed barium esophagram and/or functional lumen imaging probe (FLIP). Here the timed barium esophagram demonstrates a dilated distal esophagus with barium retention. On FLIP the esophago-gastric junction (EGJ) distensibility index (EGJ-DI) is reduced, maximal EGJ diameter is reduced and there is absent contractile response to distension.
An inconclusive diagnosis of type I or II achalasia includes absent contractility with no appreciable peristalsis in the setting of IRP values at the upper limit of normal in both positions, with or without panesophageal pressurization in 20% or more swallows (Strong Recommendation).
Evidence of appreciable peristalsis with changing position in the setting of a type I or II achalasia pattern in the primary position can shift the diagnosis towards an inconclusive diagnosis requiring supportive testing (Accepted Clinical Observation).
An inconclusive diagnosis of type III achalasia includes an abnormal IRP with evidence of spasm and evidence of peristalsis. If these cases fulfill strict criteria for EGJOO (as detailed in the EGJOO section) these patients should be classified as EGJOO with spastic features, which may represent an achalasia variant.
Additional Considerations
The cutoff of spasm in 20% of swallows is arbitrary, and confidence in a diagnosis of a type III achalasia variant may be increased with a higher number of premature/spastic swallows.
Supportive testing with a TBE, preferably with tablet, and/or FLIP should be performed in patients with an inconclusive diagnosis of achalasia in the setting of dysphagia as a presenting symptom (Very Low GRADE, Strong Recommendation).12, 13, 37–43
Opioids are associated with type III achalasia and patients should be studied off opioid medication if possible (Low GRADE, Conditional Recommendation).44, 45 Timing of opioid discontinuation should be based on medication half-life.
The following achalasia statements did not meet criteria for agreement, but are recommended considerations for HRM studies suggestive of achalasia as detailed further in the technical reviews. The pressure cut-off value for panesophageal pressurization is meant to be a guide rather than a hard threshold. The distinction between type I and II achalasia is somewhat arbitrary, and does not have important clinical implications beyond the very low levels (typically <15mmHg) seen with moderate to severe esophageal dilatation and an inability to generate emptying pressurization. Patients with panesophageal pressurization values above 70 mmHg may have embedded spasm, which may impact clinical outcome.
EGJ OUTFLOW OBSTRUCTION
A critical update in CCv4.0 is clarification and rigorous definition of EGJOO (Figure 6). Following introduction of EGJOO as a motility disorder, nearly 10% of patients undergoing HRM were identified to have an EGJOO motility pattern.18, 46 While a proportion of EGJOO may evolve towards achalasia or represent a variant of achalasia, more than one-third of cases may be clinically irrelevant, and related to benign etiologies including mechanical effects, opioid use, and artifact as detailed in the subsequent EGJOO technical review. To avoid unnecessary treatments and to optimize outcomes, there is a critical need to clarify which patients with manometric EGJOO have obstructive physiology causing symptoms and requiring intervention.13, 18, 22, 23, 39, 46–52 Therefore, CCv4.0 recommends the following to distinguish between clinically relevant EGJOO that may represent an underlying pathologic motor disorder responsive to treatment versus a clinically irrelevant manometric observation.
Figure 6.

EGJOO sub-types: EGJOO with hypercontractile features: IRP is elevated with intrabolus pressurization and hypercontractile swallow. EGJOO with no evidence of disordered peristalsis peristalsis. IRP is elevated with normal contractile vigor. Manometric EGJOO related to artifactual rise in IRP: IRP is elevated in the absence of intrabolus pressurization, and is likely associated with artifact.
Esophago-gastric junction (EGJ); EGJ outflow obstruction (EGJOO); integrated relaxation pressure (IRP); distal contractile integral (DCI)
Clinically Relevant Conclusive Diagnosis of EGJOO
A manometric diagnosis of EGJOO is always considered clinically inconclusive (Strong Recommendation).
A manometric diagnosis of EGJOO is defined as an elevated median IRP in the primary and secondary position and ≥20% swallows with elevated intrabolus pressure in the supine position, with evidence of peristalsis (Low GRADE, Conditional Recommendation).11, 18, 46, 50, 51, 53–55
A clinically relevant conclusive diagnosis of EGJOO requires a manometric diagnosis of EGJOO and clinically relevant symptoms with at least one of the following supportive investigations supporting obstruction (TBE, preferably with tablet, and/or FLIP) (Moderate GRADE, Conditional Recommendation).11–13, 18, 37
Clinically relevant symptoms of EGJOO include dysphagia and/or non-cardiac chest pain (Low GRADE, Conditional Recommendation).23, 39, 47, 49–51, 56, 57
Inconclusive Diagnosis of EGJOO
Isolated elevated abnormal findings are inconclusive for a manometric diagnosis of EGJOO. These include isolated elevated supine IRP, isolated elevated upright IRP, or isolated elevated supine intrabolus pressure (Low GRADE, Strong Recommendation).46, 58, 59
Additional Considerations:
The following are not required in the definition of EGJOO however provide supportive evidence for a diagnosis of EGJOO
Supportive evidence for a manometric diagnosis of EGJOO includes outflow obstruction and esophageal pressurization during the RDC (Very Low GRADE, Conditional Recommendation)9, 10, 27–30, 46
Supportive evidence for a manometric diagnosis of EGJOO includes outflow obstruction during the solid test meal, especially if temporally associated with patient symptoms (Conditional Recommendation)10, 30 (Supplemental Figure 1)
Supportive evidence for a manometric diagnosis of EGJOO includes abnormal EGJ function following pharmacologic provocation11(Conditional Recommendation) (Supplemental Figure 2)
EGJOO should be described in the context of the pattern of peristalsis: EGJOO with spastic features (features of type III achalasia), EGJOO with hypercontractile features, EGJOO with ineffective motility, or EGJOO with no evidence of disordered peristalsis. (Accepted Clinical Observation)
DISORDERS OF PERISTALSIS (Supplemental Table 3)
Consistent with prior iterations of Chicago Classification, absent contractility, DES, hypercontractile esophagus and IEM are considered disorders of peristalsis. Fragmented peristalsis is now removed as a disorder and incorporated into the overall diagnosis of IEM (Very Low GRADE, Strong Recommendation).60, 61 Disorders of peristalsis are considered when a disorder of EGJ outflow has been ruled out. There is potential for overlapping features of abnormal peristalsis to exist. In these scenarios, a hierarchical approach to diagnostic classification should be used in the order of DES first, hypercontractile esophagus next, and last IEM, with a comment acknowledging presence of overlapping features.
It is again highlighted that diagnostic determination should be based on the primary position in which 10 wet swallows are performed, either supine or upright. Assessment of swallows in the secondary position and with provocation provide supportive evidence. Concordance of peristaltic classification with changing positions strengthens the confidence in the classification and eventual clinical diagnosis, whereas discordance should prompt reconsideration of the classification and eventual diagnosis with consideration of further supportive testing.
An important update in CCv4.0 is the recognition that DES and hypercontractile esophagus are manometric patterns that do not always equate to a clinical disease, similar to concepts underlying EGJOO. Per CCv4.0 these disorders of peristalsis are clinically relevant only in the appropriate clinical context and when they are supported by further testing, as detailed in this section.
ABSENT CONTRACTILITY
Criteria for a diagnosis of absent contractility was not revised in CCv4.0.
A conclusive diagnosis for absent contractility is defined as normal median IRP in the supine and upright position and 100% failed peristalsis (DCI < 100 mmHg•s•cm) (Accepted Clinical Observation) (Figure 7).
Figure 7.

Disorders of Peristalsis with Reduced Contractile Vigor or Contiguity of Peristalsis. These include absent contractility or ineffective esophageal motility (either related to reduced contractile vigor or fragmented peristalsis). In this example of Absent Contractility there is failed peristalsis with a normal IRP. In the first example of IEM the DCI is reduced with a normal IRP. In the second example of IEM the DCI is normal with a fragmentation in peristalsis of > 5cm in the setting of a normal IRP. During the multiple rapid swallows (MRS) there is absence of contractile activity and there is deglutitive inhibition of lower esophageal sphincter followed by DCI which is greater than the single swallow DCI, signifying an intact contractile augmentation.
In the context of absent contractility, borderline median IRP values, particularly supine median IRP of 10mmHg to 15mmHg using the Medtronic system, should prompt consideration of type I achalasia. As discussed in the Achalasia section, supportive testing with TBE, preferably with tablet, and FLIP should be considered in these cases if dysphagia is the dominant symptom (Figure 5).
DISTAL ESOPHAGEAL SPASM
DES describes a specific abnormal esophageal motor pattern characterized by spastic or premature contractions in the distal esophagus (Figure 8). As aforementioned a spastic or premature contraction is defined as an esophageal contraction with a distal latency shorter than 4.5 seconds, in the setting of a DCI greater than 450 mmHg•s•cm. Manometric DES may have varying clinical significance, and thus, an update in CCv4.0 is the distinction between clinically relevant DES and clinically irrelevant manometric observations.
Figure 8.

Disorders of Peristalsis with Esophageal Spasticity or Hypercontractility. These include distal esophageal spasm or hypercontractile esophagus. In this example of Distal Esophageal Spasm the DCI is normal with a reduced distal latency and normal IRP. Hypercontractile esophagus includes sub-groups: Single peak hypercontractile swallow, hypercontractile with jackhammer esophagus, and hypercontractile with LES after-contraction.
integrated relaxation pressure (IRP); distal contractile integral (DCI); lower esophageal sphincter (LES)
Clinically Relevant Diagnosis of Distal Esophageal Spasm
A clinically relevant diagnosis of DES requires both clinically relevant symptoms and a conclusive manometric diagnosis of DES (Low GRADE, Conditional Recommendation).19
A conclusive manometric diagnosis of DES is defined as presence of at least 20% of premature contractions (Low GRADE, Strong Recommendation).19
Clinically relevant symptoms for DES include dysphagia and non-cardiac chest pain (Accepted Clinical Observation).
Inconclusive Diagnosis of Distal Esophageal Spasm
The presence of at least 20% contractions with a reduced distal latency (DL < 4.5 seconds) but with a DCI < 450 mmHg•s•cm is inconclusive for a manometric diagnosis of DES (Low GRADE, Conditional Recommendation).19
The CCv4.0 Working Group recognizes that the CDP might be difficult to identify. In this setting alternative methodologies need to be considered to diagnose DES (Strong Recommendation). This is further detailed in the section above on metrics and will be further addressed in the subsequent DES technical review.
HYPERCONTRACTILE ESOPHAGUS
Hypercontractile esophagus describes a distinct manometric abnormality defined by excessive peristaltic vigor, which may include excessive LES after-contraction, not associated with a mechanical obstruction (Figure 8) (Very Low GRADE, Conditional Recommendation)62–64. Obstruction at the EGJ or the distal esophagus can induce a hypercontractile response and it is crucial that obstruction is ruled out before a diagnosis of hypercontractile esophagus is considered. Heterogeneous motor patterns can meet manometric criteria for hypercontractile esophagus and have varying clinical significance. Therefore, similar to DES, an important update in CCv4.0 is to distinguish between clinically relevant hypercontractile esophagus versus clinically irrelevant manometric observations.
Clinically Relevant Conclusive Diagnosis of Hypercontractile Esophagus
A clinically relevant diagnosis of hypercontractile esophagus requires both clinically relevant symptoms and a conclusive manometric diagnosis of hypercontractile esophagus (Very Low GRADE, Strong Recommendation).56, 62, 64, 65
A conclusive manometric diagnosis of hypercontractile esophagus is defined as 20% or more hypercontractile supine swallows (Very Low GRADE, Conditional Recommendation).62–64
Clinically relevant symptoms of hypercontractile esophagus include dysphagia and non-cardiac chest pain (Very Low GRADE, Strong Recommendation).56, 62, 64, 65
Additional Considerations:
A diagnosis of hypercontractile esophagus can only be made when criteria for achalasia or distal esophageal spasm are not met and a mechanical obstruction has been carefully ruled out (Very Low GRADE, Strong Recommendation).62–64
Given the heterogeneity of hypercontractile patterns, the group advocated for a cautious approach in terms of treating contractile vigor as an endpoint and advocated for conservative medical therapy before endoscopic or surgical interventions are considered. The hypercontractile esophagus working group also proposed statements which did not meet criteria for agreement, further detailed in the subsequent technical review. There are three general sub-groups of hypercontractile esophagus: single-peaked hypercontractile swallows, jackhammer with repetitive prolonged contractions (especially in the post-peak phase), and hypercontractile swallows with a vigorous LES after-contraction. The jackhammer subgroup of hypercontractile esophagus is typically associated with higher DCI values and worse symptom severity.66–68 Overall the CCv4.0 working group recognizes the critical need for further research to better characterize physiologic phenotypes and clinical outcomes in hypercontractile esophagus.
INEFFECTIVE ESOPHAGEAL MOTILITY
Prior iterations of Chicago Classification categorized IEM and fragmented peristalsis as minor motility disorders. In CCv4.0 fragmented peristalsis as detailed in previous iterations of the Chicago Classification is now included under the definition of IEM. Further, the diagnostic criteria for IEM have been made more stringent, commensurate with emerging data. As a result of these changes to IEM and fragmented peristalsis, CCv4.0 does not distinguish between major or minor disorders (Figure 7).
Conclusive Diagnosis of Ineffective Esophageal Motility
A conclusive diagnosis of IEM requires more than 70% ineffective swallows or at least 50% failed peristalsis (Very Low GRADE, Strong Recommendation).60, 69–71
As detailed in Diagnostic Thresholds and in Table 1, an ineffective swallow includes a weak contraction (DCI ≥ 100 mmHg•s•cm and < 450 mmHg•s•cm), failed peristalsis (DCI < 100 mmHg•s•cm), or a fragmented swallow.
Inconclusive Diagnosis of Ineffective Esophageal Motility
The presence of 50 to 70% of ineffective swallows is inconclusive for a diagnosis of IEM. Supportive testing will strengthen confidence in IEM diagnosis in these cases (Very Low GRADE, Conditional Recommendation).61, 72
Additional Considerations:
The following are not required for the definition of IEM however provide supportive evidence:
ESOPHAGO-GASTRIC JUNCTION METRICS
An advantage of modern day high-resolution esophageal pressure topography over conventional line tracing is the ability to precisely assess the EGJ barrier function at rest including the relationship between the LES, crural diaphragm (CD), and respiratory inversion point (RIP), as well as the EGJ contractile integral (EGJ-CI), a measure of EGJ contractility in relation to respiration. Thus, a priority of CCv4.0 was to provide guidance to enable better characterization of the EGJ complex during a baseline recording in the primary position.
The EGJ complex should be measured during quiet respiration in the baseline recording in a segment relatively devoid of swallowing and/or recording artifacts. This also refers to measurement of intragastric pressure, which should be measured below the CD over three complete respiratory cycles, preferably in the same segment as used to measure the EGJ-CI (Strong Recommendation).
The RIP is the axial location at which the inspiratory change in pressure transitions from an inspiratory increase, characteristic of intra-abdominal recordings, to an inspiratory decrease, characteristic of intrathoracic recordings. (Strong Recommendation)
The EGJ-CI should be referenced to intragastric pressure and expressed in units of mmHg•cm. (Strong Recommendation). While not met with agreement, it was suggested that an EGJ-CI (or LES-contractile integral) value of <25 mmHg•cm be considered a hypotensive EGJ.77–85
LES-CD separation should be scored as the distance between the center of the CD and LES signal during inspiration, unless obscured in which case the LES position should be scored at expiration (Strong Recommendation).
The EGJ complex should be defined based on LES-CD separation and location of the RIP. (Low GRADE, Conditional Recommendation)86–92
As for EGJ morphology, it was acknowledged that there were three subtypes: 1) normal with the CD superimposed on the LES and the RIP localizing proximal to the complex; 2) LES-CD separation with the RIP localized proximal to the CD; and 3) LES-CD separation with the RIP localized proximal to the LES. However, there was no consensus regarding the subtype classification scheme (I, II, III vs A, C, B) and both versions were deemed acceptable (Supplemental Figure 4).86, 91 More research is clearly needed applying standardized, pre-specified methodology. The EGJ Metrics technical review details further recommendations regarding measurement of the EGJ complex in setting of hiatal hernia and temporal variability, as well as intragastric pressure and the role of end-expiratory LES pressure.
CONCLUSION
CCv4.0 is the state-of-the-art classification scheme of esophageal motility disorders derived from a two-year international initiative involving 52 esophageal motility experts representing professional societies from five continents. The Chicago Classification has always been a dynamic process, subject to revision and refinement with every new iteration. True to this concept, CCv4.0 has updates that improve precision of previously characterized motility diagnoses, and deletions of infrequently encountered diagnoses or clinically irrelevant criteria. A key update in CCv4.0 is the recognition that, similar to other medical investigations, HRM patterns alone may not equate to a conclusive diagnosis that explains patient symptoms and guides effective management (actionable pathology). Thus, CCv4.0 separates patterns that do provide a conclusive diagnosis (e.g. achalasia) from other patterns that are suggestive but inconclusive for a diagnosis, where additional clinical information and supportive testing may either confirm or refute the diagnosis in question. In particular, EGJOO, hypercontractile esophagus and DES are manometric patterns that require presence of dysphagia and/or non-cardiac chest pain to be considered clinically relevant. Further, a conclusive diagnosis of EGJOO requires corroboration with at least one supportive test (e.g. TBE, FLIP).
The methodologic rigor that has been applied to the CCv4.0 process consists of the use of formal consensus methods and formal level of evidence review when applicable. Further, CCv4.0 recommends a standardized HRM protocol to improve technical consistency and diagnostic accuracy, so that future iterations of the Chicago Classification can rely on further research from a comprehensive, uniformly collected data. Finally, CCv4.0 represents motility perspectives from a diverse working group in terms of geography, age, gender, practice type, years in practice, and research contributions to the field.
CCv4.0 also highlights areas ripe for future investigation and clarity, as further summarized in the specific technical reviews. Future iterations of Chicago Classification will need to delineate the role of impedance topography for intrabolus pressure and bolus flow. Additional outcomes studies are needed to better understand the reliability of solid test swallows and meals in identifying clinically relevant abnormal EGJ and peristaltic function. With refinement of the diagnostic criteria for EGJOO in CCv4.0, it will be important to understand the natural history and treatment outcome of EGJOO, with and without supportive testing. Understanding mechanisms of spastic esophageal disorders remains of great interest, as well as exploring overlaps with opioid induced esophageal dysfunction.45 Understanding the spectrum of hypercontractile disorders will require further work to explore whether jackhammer esophagus represents a unique subtype with clinical significance. Future iterations of Chicago Classification may propose manometric criteria for therapy selection, such as role of per-oral endoscopic myotomy for spastic disorders, and risk stratification and tailoring of fundoplication to prevent post-fundoplication dysphagia.
Supplementary Material
Supplemental Figure 1. Supplemental Figure 1. Supportive Role of Solid Test Swallows and Solid Test Meal. In 5ml wet swallow the distal contractile integral (DCI) and integrated relaxation pressure (IRP) are normal. With solid test swallows the IRP is elevated and symptoms of dysphagia are elicited, unmasking an obstruction and supporting a diagnosis of esophago-gastric junction (EGJ) outflow obstruction in an otherwise normal study.
Supplemental Figure 2. Supportive Role of Pharmacologic Provocation. Representative esophageal pressure topography plot during wet swallow, amyl nitrite (AN) inhalation and subsequent recovery phase in a patient with AN-responsive EGJOO (early achalasia). Note that after sniffing AN there is a significant drop in EGJ pressure and distal esophageal smooth muscle contractility is inhibited. The dramatic exaggerated rebound EGJ contraction response during recovery phase may indicate chronic esophageal nitric oxide deprivation.
Supplemental Figure 3. Supportive Role of Post-Prandial Monitoring. In Post-prandial monitoring there is a transient lower esophageal sphincter (LES) relaxation (TLESR) with reflux with symptoms of reflux/belching, followed by a rumination episode with symptom of regurgitation. Upper esophageal sphincter (UES); High resolution manometry (HRM)
Supplemental Figure 4. EGJ Morphology. Three subtypes of EGJ morphology include A) normal with the CD superimposed on the LES and the RIP localizing proximal to the complex (Akimoto A or Type I EGJ morphology), B) LES-CD separation with the RIP localized proximal to the CD (Type II EGJ morphology or Akimoto C), C) LES-CD separation with the RIP localized proximal to the LES (Type III EGJ morphology or Akimoto B)
Supplemental Table 1 Working Group Baseline Characteristics and Responses to Initial Survey
Supplemental Table 2. Disorders of EGJ Outflow. Definitions of a conclusive diagnosis, inconclusive diagnosis and supportive testing.
Supplemental Table 3. Disorders of Esophageal Peristalsis. Definitions of a conclusive diagnosis, inconclusive diagnosis and supportive testing.
Supplemental Table 4. Recommendations of the Chicago Classification v4.0
Classification using CCv.4.0 is based on the primary position in which 10 wet swallows are performed, either supine or upright. Assessment of swallows in the secondary position and with provocation provide supportive data (with the exception of EGJOO and absent contractility as detailed later in this document). CCv4.0 recognizes the potential for variation in findings with changing positions. Concordant findings in the secondary position and with provocation increase strength of confidence of the classification and eventual diagnosis. On the other hand, discordant findings in the secondary position and/or with provocation should prompt reconsideration of the classification and eventual diagnosis with consideration of further supportive testing.
Conflicts of Interest:
Rena Yadlapati: Institutional Consulting Agreement: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals; Advisory Board: Phatom Pharmaceuticals
Peter J. Kahrilas: Consultant: Ironwood Pharmaceuticals; Advisory Board: Ironwood Pharmaceuticals; Research Grant: Ironwood Pharmaceuticals; Royalties: Medtronic; Licensing Agreement: Medtronic
Mark R. Fox: Speaker: Medtronic, Diversatek, Laborie; Research Grant: Medtronic, Diversatek, Laborie
Albert J. Bredenoord: Consulting: Medtronic, Laborie, AstraZeneca, Gossamer, Arena, EsoCap, Calypso, Regeneron, Dr Falk; Speaker: Medtronic, Laborie, Dr Falk; Advisory Board: Medtronic, Laborie, AstraZeneca, Gossamer, Arena, EsoCap, Calypso, Regeneron, Dr Falk; Research Grants: Medtronic, Laborie, Nutricia, SST; Stock Options: SST
C. Prakash Gyawali: Consulting: Medtronic, Diversatek, Ironwood Pharmaceuticals, Isothrive, Quintiles
Sabine Roman: Consulting: Medtronic: research Grants: Medtronic, Diversatek Healthcare
Nathalie Rommel: Patent on Automated Impedance Manometry technology
Edoardo Savarino: Consulting: Unifarco; Speaker: Medtronic, Reckitt Benckiser, Takeda, Abbvie, Novartis, Sandoz, Sofar, Malesci, Janssen, Grifols, Aurora Pharma, Innovamedica, Johnson&Johnson, SILA, Alfasigma, Shire, EG Stada Group; Advisory Board: Merck & Co, Bristol-Myers Squibb, Amgen, Fresenius Kabi; Research Grant: Sofar
Michael F. Vaezi: Consulting: Diversatek; Phathom; Ironwood; Speaker: Diversateak; Advisory Board: Diversatek; Phathom; Ironwood; Research Grants: Diversatek; Phathom; Ironwood; Patent: Mucosal Integrity Testing
Frank Zerbib: Consulting: Reckitt Benckiser
Junichi Akiyama: Speaker: StarMedical, Takeda, AstraZeneca, Otsuka, Daiichi Sankyo
Serhat Bor: Speaker: Laborie
Dustin A. Carlson: Consulting: Medtronic, Speaker: Medtronic
Daniel Cisternas: Speaker: Medtronic
Enrique Coss-Adame: Consulting: Asofarma de México, Ferrer de México, Siegfried Rhein, Takeda de México, Medtronic de Mexico; Speaker: Asofarma de México, Ferrer de México, Siegfried Rhein, Takeda de México, Medtronic de Mexico, Grunenthal de Mexico.; Advisory Board: Asofarma de México, Ferrer de México, Siegfried Rhein, Takeda de México, Medtronic de Mexico
Ronnie Fass: Consulting: Ironwood, Takeda, Daewoong, Medtronic, Phathom; Speaker: Astrazeneca, Takeda, Diversatek, Eisai; Advisory Board: Phathom; Research Grants: Ironwood, Salix; Royalties: UpToDate
Philip Katz: Consulting: Medtronic; Research Grants: Diversatek
David A. Katzka: Consulting: Shire
Abraham Khan: Consulting: Medtronic; Speaker: Medtronic
Daniel Pohl: Consulting: Medtronic, Sanofi; Speaker: Permamed, Alfa Sigma, Schwabe Pharma, Takeda, Advisory Board: Sanofi, Schwabe Pharma
Jordi Serra: Consulting: Reckit Benckiser; Speaker: Norgine, Allergan, Cassen Recordati, AB biotics; Advisory Board: Almirall; Research Grants: Bayer, Salvat Biotech, Zespri
Rami Sweis: Speaker: Medtronic, Covidian, Given, Falk Pharma, Ethicon; Advisory Board: Falk Pharma, Ethicon
Jan Tack: Research Grant: Sofar Pharmaceuticals
Radu Tutuian: Consulting: Laborie MMS; Speaker: Laborie MMS; Royalties: UpToDate
Marcelo F. Vela: Consulting: Medtronic
Reuben Wong: Consulting: MMS Laborie, Speaker: MMS Laborie
John E. Pandolfino: Consultant: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals, Takeda; Advisory Board: Medtronic, Diversatek; Stock Options: Crospon Inc
None to report: Arash Babaei, Ravinder K. Mittal, Daniel Sifrim, Andre Smout, Shobna Bhatia, Joan Chen, Charles Cock, Nicola de Bortoli, Claudia Defilippi, Uday C. Ghoshal, Sutep Gonlachanvit, Albis Hani, Geoffrey S. Hebbard, Kee Wook Jung, Geoffrey P. Kohn, Adriana Lazarescu, Johannes Lenglinger, Sumeet K. Mittal, Taher Omari, Moo In Park, Roberto Penagini, Joel E. Richter, Roger P. Tatum, Justin Wu, Yinglian Xiao
Research Funding Support:
P01 DK092217 (John E. Pandolfino) from the US Public Health Service
Abbreviations:
- HRM
High resolution manometry
- CCv4.0
Chicago Classification version 4.0
- EGJ
Esophagogastric junction
- EGJOO
EGJ outflow obstruction
- IEM
Ineffective esophageal motility
- RAM
RAND Appropriateness Method
- REDCap
Research Electronic Database Capture
- GRADE
Grading of Recommendations Assessment Development and Evaluation
- UES
Upper esophageal sphincter
- LES
Lower esophageal sphincter
- RIP
Respiratory inversion point
- MRS
Multiple repetitive swallow
- RDC
Rapid drink challenge
- TBE
Timed barium esophagram
- FLIP
Functional lumen imaging probe
- IRP
Integrated relaxation pressure
- DCI
Distal contractile integral
- DL
Distal latency
- CDP
Contractile deceleration point
- CD
Crural diaphragm
- EGJ-CI
EGJ contractile integral
REFERENCES
- 1.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil 2009;21:796–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24 Suppl 1:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yadlapati R, Gawron AJ, Keswani RN, et al. Identification of Quality Measures for Performance of and Interpretation of Data From Esophageal Manometry. Clin Gastroenterol Hepatol 2016;14:526–534 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yadlapati R, Vaezi MF, Vela MF, et al. Management options for patients with GERD and persistent symptoms on proton pump inhibitors: recommendations from an expert panel. Am J Gastroenterol 2018;113:980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. [DOI] [PubMed] [Google Scholar]
- 7.Shaker A, Stoikes N, Drapekin J, et al. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol 2013;108:1706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mauro A, Savarino E, De Bortoli N, et al. Optimal number of multiple rapid swallows needed during high-resolution esophageal manometry for accurate prediction of contraction reserve. Neurogastroenterol Motil 2018;30:e13253. [DOI] [PubMed] [Google Scholar]
- 9.Woodland P, Gabieta-Sonmez S, Arguero J, et al. 200 mL Rapid Drink Challenge During High-resolution Manometry Best Predicts Objective Esophagogastric Junction Obstruction and Correlates With Symptom Severity. J Neurogastroenterol Motil 2018;24:410–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ang D, Misselwitz B, Hollenstein M, et al. Diagnostic yield of high-resolution manometry with a solid test meal for clinically relevant, symptomatic oesophageal motility disorders: serial diagnostic study. Lancet Gastroenterol Hepatol 2017;2:654–661. [DOI] [PubMed] [Google Scholar]
- 11.Babaei A, Shad S, Szabo A, et al. Pharmacologic interrogation of patients with esophagogastric junction outflow obstruction using amyl nitrite. Neurogastroenterol Motil 2019;31:e13668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Triggs JR, Carlson DA, Beveridge C, et al. Functional Luminal Imaging Probe Panometry Identifies Achalasia-Type Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol 2020;18:2209–2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clayton SB, Patel R, Richter JE. Functional and Anatomic Esophagogastic Junction Outflow Obstruction: Manometry, Timed Barium Esophagram Findings, and Treatment Outcomes. Clin Gastroenterol Hepatol 2016;14:907–911. [DOI] [PubMed] [Google Scholar]
- 14.Herregods TV, Roman S, Kahrilas PJ, et al. Normative values in esophageal high-resolution manometry. Neurogastroenterol Motil 2015;27:175–87. [DOI] [PubMed] [Google Scholar]
- 15.Kuribayashi S, Iwakiri K, Kawada A, et al. Variant parameter values-as defined by the Chicago Criteria-produced by ManoScan and a new system with Unisensor catheter. Neurogastroenterol Motil 2015;27:188–94. [DOI] [PubMed] [Google Scholar]
- 16.Sifrim D, Roman S, Savarino E, et al. Normal values and regional differences in oesophageal impedance-pH metrics: a consensus analysis of impedance-pH studies from around the world. Gut 2020. [DOI] [PubMed] [Google Scholar]
- 17.A R, BD R, Z W, et al. High-resolution manometry thresholds and motor patterns among asymptomatic individuals. Clin Gastroenterol Hepatol 2020. [DOI] [PubMed] [Google Scholar]
- 18.Triggs JR, Carlson DA, Beveridge C, et al. Upright Integrated Relaxation Pressure Facilitates Characterization of Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol 2019;17:2218–2226 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pandolfino JE, Roman S, Carlson D, et al. Distal esophageal spasm in high-resolution esophageal pressure topography: defining clinical phenotypes. Gastroenterology 2011;141:469–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roman S, Kahrilas PJ, Kia L, et al. Effects of large hiatal hernias on esophageal peristalsis. Arch Surg 2012;147:352–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008;135:1526–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biasutto D, Mion F, Garros A, et al. Rapid drink challenge test during esophageal high resolution manometry in patients with esophago-gastric junction outflow obstruction. Neurogastroenterol Motil 2018;30:e13293. [DOI] [PubMed] [Google Scholar]
- 23.Song BG, Min YW, Lee H, et al. Clinicomanometric factors associated with clinically relevant esophagogastric junction outflow obstruction from the Sandhill high-resolution manometry system. Neurogastroenterol Motil 2018;30. [DOI] [PubMed] [Google Scholar]
- 24.Elvevi A, Mauro A, Pugliese D, et al. Usefulness of low- and high-volume multiple rapid swallowing during high-resolution manometry. Dig Liver Dis 2015;47:103–7. [DOI] [PubMed] [Google Scholar]
- 25.Martinucci I, Savarino EV, Pandolfino JE, et al. Vigor of peristalsis during multiple rapid swallows is inversely correlated with acid exposure time in patients with NERD. Neurogastroenterol Motil 2016;28:243–50. [DOI] [PubMed] [Google Scholar]
- 26.Krause AJ, Su H, Triggs JR, et al. Multiple rapid swallows and rapid drink challenge in patients with esophagogastric junction outflow obstruction on high-resolution manometry. Neurogastroenterol Motil 2020:e14000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ang D, Hollenstein M, Misselwitz B, et al. Rapid Drink Challenge in high-resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil 2017;29. [DOI] [PubMed] [Google Scholar]
- 28.Marin I, Serra J. Patterns of esophageal pressure responses to a rapid drink challenge test in patients with esophageal motility disorders. Neurogastroenterol Motil 2016;28:543–53. [DOI] [PubMed] [Google Scholar]
- 29.Sanagapalli S, McGuire J, Leong R, et al. The clinical relevance of manometric esophagogastric junction outflow obstruction can be determined using rapid drink challenge and solid swallows. Am J Gastroenterol 2020. [DOI] [PubMed] [Google Scholar]
- 30.Hollenstein M, Thwaites DT, Buetikofer S, et al. Pharyngeal swallowing and oesophageal motility during a solid meal test: a prospective study in healthy volunteers and patients with major motility disorders. The Lancet Gastroenterology & Hepatology 2017;2:644–653. [DOI] [PubMed] [Google Scholar]
- 31.Babaei A, Shad S, Massey BT. Diagnostic differences in the pharmacologic response to cholecystokinin and amyl nitrite in patients with absent contractility vs type I Achalasia. Neurogastroenterol Motil 2020;32:e13857. [DOI] [PubMed] [Google Scholar]
- 32.Babaei A, Shad S, Massey BT. Motility Patterns Following Esophageal Pharmacologic Provocation With Amyl Nitrite or Cholecystokinin During High-Resolution Manometry Distinguish Idiopathic vs Opioid-Induced Type 3 Achalasia. Clin Gastroenterol Hepatol 2020;18:813–821 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andolfi C, Fisichella PM. Meta-analysis of clinical outcome after treatment for achalasia based on manometric subtypes. Br J Surg 2019;106:332–341. [DOI] [PubMed] [Google Scholar]
- 34.Lee JY, Kim N, Kim SE, et al. Clinical characteristics and treatment outcomes of 3 subtypes of achalasia according to the chicago classification in a tertiary institute in Korea. J Neurogastroenterol Motil 2013;19:485–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Min M, Peng LH, Yang YS, et al. Characteristics of achalasia subtypes in untreated Chinese patients: a high-resolution manometry study. J Dig Dis 2012;13:504–9. [DOI] [PubMed] [Google Scholar]
- 36.Rohof WO, Salvador R, Annese V, et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 2013;144:718–25; quiz e13–4. [DOI] [PubMed] [Google Scholar]
- 37.Blonski W, Kumar A, Feldman J, et al. Timed Barium Swallow: Diagnostic Role and Predictive Value in Untreated Achalasia, Esophagogastric Junction Outflow Obstruction, and Non-Achalasia Dysphagia. Am J Gastroenterol 2018;113:196–203. [DOI] [PubMed] [Google Scholar]
- 38.Clayton SB, Shin CM, Ewing A, et al. Pneumatic dilation improves esophageal emptying and symptoms in patients with idiopathic esophago-gastric junction outflow obstruction. Neurogastroenterol Motil 2019;31:e13522. [DOI] [PubMed] [Google Scholar]
- 39.Okeke FC, Raja S, Lynch KL, et al. What is the clinical significance of esophagogastric junction outflow obstruction? evaluation of 60 patients at a tertiary referral center. Neurogastroenterol Motil 2017;29. [DOI] [PubMed] [Google Scholar]
- 40.Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol 2016;111:1726–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim E, Yoo IK, Yon DK, et al. Characteristics of a Subset of Achalasia With Normal Integrated Relaxation Pressure. J Neurogastroenterol Motil 2020;26:274–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ponds FA, Bredenoord AJ, Kessing BF, et al. Esophagogastric junction distensibility identifies achalasia subgroup with manometrically normal esophagogastric junction relaxation. Neurogastroenterol Motil 2017;29. [DOI] [PubMed] [Google Scholar]
- 43.Sanagapalli S, Roman S, Hastier A, et al. Achalasia diagnosed despite normal integrated relaxation pressure responds favorably to therapy. Neurogastroenterol Motil 2019;31:e13586. [DOI] [PubMed] [Google Scholar]
- 44.Babaei A, Szabo A, Shad S, et al. Chronic daily opioid exposure is associated with dysphagia, esophageal outflow obstruction, and disordered peristalsis. Neurogastroenterol Motil 2019;31:e13601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ratuapli SK, Crowell MD, DiBaise JK, et al. Opioid-Induced Esophageal Dysfunction (OIED) in Patients on Chronic Opioids. Am J Gastroenterol 2015;110:979–84. [DOI] [PubMed] [Google Scholar]
- 46.Misselwitz B, Hollenstein M, Butikofer S, et al. Prospective serial diagnostic study: the effects of position and provocative tests on the diagnosis of oesophageal motility disorders by high-resolution manometry. Aliment Pharmacol Ther 2020;51:706–718. [DOI] [PubMed] [Google Scholar]
- 47.Beveridge CA, Falk GW, Ahuja NK, et al. Low Yield of Cross-Sectional Imaging in Patients With Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol 2020;18:1643–1644. [DOI] [PubMed] [Google Scholar]
- 48.DeLay K, Austin GL, Menard-Katcher P. Anatomic abnormalities are common potential explanations of manometric esophagogastric junction outflow obstruction. Neurogastroenterol Motil 2016;28:1166–71. [DOI] [PubMed] [Google Scholar]
- 49.Liu A, Woo M, Nasser Y, et al. Esophagogastric junction outflow obstruction on manometry: Outcomes and lack of benefit from CT and EUS. Neurogastroenterol Motil 2019;31:e13712. [DOI] [PubMed] [Google Scholar]
- 50.Perez-Fernandez MT, Santander C, Marinero A, et al. Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol Motil 2016;28:116–26. [DOI] [PubMed] [Google Scholar]
- 51.van Hoeij FB, Smout AJ, Bredenoord AJ. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol Motil 2015;27:1310–6. [DOI] [PubMed] [Google Scholar]
- 52.Wang YT, Tai LF, Yazaki E, et al. Investigation of Dysphagia After Antireflux Surgery by High-resolution Manometry: Impact of Multiple Water Swallows and a Solid Test Meal on Diagnosis, Management, and Clinical Outcome. Clin Gastroenterol Hepatol 2015;13:1575–83. [DOI] [PubMed] [Google Scholar]
- 53.Hoscheit M, Gabbard S. Elevated Intrabolus Pressure Predicts Abnormal Timed Barium Esophagram in Esophagogastric Junction Outflow Obstruction. J Neurogastroenterol Motil 2019;25:521–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quader F, Reddy C, Patel A, et al. Elevated intrabolus pressure identifies obstructive processes when integrated relaxation pressure is normal on esophageal high-resolution manometry. Am J Physiol Gastrointest Liver Physiol 2017;313:G73–G79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Singendonk MJ, Lin Z, Scheerens C, et al. High-resolution impedance manometry parameters in the evaluation of esophageal function of non-obstructive dysphagia patients. Neurogastroenterol Motil 2019;31:e13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schupack D, Katzka DA, Geno DM, et al. The clinical significance of esophagogastric junction outflow obstruction and hypercontractile esophagus in high resolution esophageal manometry. Neurogastroenterol Motil 2017;29:1–9. [DOI] [PubMed] [Google Scholar]
- 57.Song BG, Min YW, Lee H, et al. Combined Multichannel Intraluminal Impedance and High-resolution Manometry Improves Detection of Clinically Relevant Esophagogastric Junction Outflow Obstruction. J Neurogastroenterol Motil 2019;25:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Babaei A, Lin EC, Szabo A, et al. Determinants of pressure drift in Manoscan() esophageal high-resolution manometry system. Neurogastroenterol Motil 2015;27:277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Babaei A, Szabo A, Yorio SD, et al. Pressure exposure and catheter impingement affect the recorded pressure in the Manoscan 360 system. Neurogastroenterol Motil 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zerbib F, Marin I, Cisternas D, et al. Ineffective esophageal motility and bolus clearance. A study with combined high-resolution manometry and impedance in asymptomatic controls and patients. Neurogastroenterol Motil 2020;32:e13876. [DOI] [PubMed] [Google Scholar]
- 61.Rogers BD, Rengarajan A, Mauro A, et al. Fragmented and failed swallows on esophageal high-resolution manometry associate with abnormal reflux burden better than weak swallows. Neurogastroenterol Motil 2020;32:e13736. [DOI] [PubMed] [Google Scholar]
- 62.Herregods TV, Smout AJ, Ooi JL, et al. Jackhammer esophagus: Observations on a European cohort. Neurogastroenterol Motil 2017;29. [DOI] [PubMed] [Google Scholar]
- 63.Kahn A, Al-Qaisi MT, Obeid RA, et al. Clinical features and long-term outcomes of lower esophageal sphincter-dependent and lower esophageal sphincter-independent jackhammer esophagus. Neurogastroenterol Motil 2019;31:e13507. [DOI] [PubMed] [Google Scholar]
- 64.Roman S, Pandolfino JE, Chen J, et al. Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Am J Gastroenterol 2012;107:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Al-Qaisi MT, Siddiki HA, Crowell MD, et al. The clinical significance of hypercontractile peristalsis: comparison of high-resolution manometric features, demographics, symptom presentation, and response to therapy in patients with Jackhammer esophagus versus Nutcracker esophagus. Dis Esophagus 2017;30:1–7. [DOI] [PubMed] [Google Scholar]
- 66.Philonenko S, Roman S, Zerbib F, et al. Jackhammer esophagus: Clinical presentation, manometric diagnosis, and therapeutic results-Results from a multicenter French cohort. Neurogastroenterol Motil 2020:e13918. [DOI] [PubMed] [Google Scholar]
- 67.Xiao Y, Carlson DA, Lin Z, et al. Jackhammer esophagus: Assessing the balance between prepeak and postpeak contractile integral. Neurogastroenterol Motil 2018;30:e13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xiao Y, Carlson DA, Lin Z, et al. Chaotic peak propagation in patients with Jackhammer esophagus. Neurogastroenterol Motil 2020;32:e13725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bulsiewicz WJ, Kahrilas PJ, Kwiatek MA, et al. Esophageal pressure topography criteria indicative of incomplete bolus clearance: a study using high-resolution impedance manometry. Am J Gastroenterol 2009;104:2721–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jain A, Baker JR, Chen JW. In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil 2018;30:e13297. [DOI] [PubMed] [Google Scholar]
- 71.Roman S, Lin Z, Kwiatek MA, et al. Weak peristalsis in esophageal pressure topography: classification and association with Dysphagia. Am J Gastroenterol 2011;106:349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rengarajan A, Bolkhir A, Gor P, et al. Esophagogastric junction and esophageal body contraction metrics on high-resolution manometry predict esophageal acid burden. Neurogastroenterol Motil 2018;30:e13267. [DOI] [PubMed] [Google Scholar]
- 73.Chugh P, Collazo T, Dworkin B, et al. Ineffective Esophageal Motility Is Associated with Impaired Bolus Clearance but Does Not Correlate with Severity of Dysphagia. Dig Dis Sci 2019;64:811–814. [DOI] [PubMed] [Google Scholar]
- 74.Lin Z, Nicodeme F, Lin CY, et al. Parameters for quantifying bolus retention with high-resolution impedance manometry. Neurogastroenterol Motil 2014;26:929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wu JF, Tsai IJ, Tong TW, et al. Pressure-impedance analysis: Assist the diagnosis and classification of ineffective esophageal motility disorder. J Gastroenterol Hepatol 2020;35:1317–1324. [DOI] [PubMed] [Google Scholar]
- 76.Quader F, Rogers B, Sievers T, et al. Contraction Reserve With Ineffective Esophageal Motility on Esophageal High-Resolution Manometry is Associated With Lower Acid Exposure Times Compared With Absent Contraction Reserve. Am J Gastroenterol 2020. [DOI] [PubMed] [Google Scholar]
- 77.Gor P, Li Y, Munigala S, et al. Interrogation of esophagogastric junction barrier function using the esophagogastric junction contractile integral: an observational cohort study. Dis Esophagus 2016;29:820–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ham H, Cho YK, Lee HH, et al. Esophagogastric junction contractile integral and morphology: Two high-resolution manometry metrics of the anti-reflux barrier. J Gastroenterol Hepatol 2017;32:1443–1449. [DOI] [PubMed] [Google Scholar]
- 79.Jasper D, Freitas-Queiroz N, Hollenstein M, et al. Prolonged measurement improves the assessment of the barrier function of the esophago-gastric junction by high-resolution manometry. Neurogastroenterol Motil 2017;29. [DOI] [PubMed] [Google Scholar]
- 80.Nicodeme F, Pipa-Muniz M, Khanna K, et al. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil 2014;26:353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rengarajan A, Gyawali CP. High-resolution Manometry can Characterize Esophagogastric Junction Morphology and Predict Esophageal Reflux Burden. J Clin Gastroenterol 2020;54:22–27. [DOI] [PubMed] [Google Scholar]
- 82.Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil 2015;27:1423–31. [DOI] [PubMed] [Google Scholar]
- 83.Wang D, Patel A, Mello M, et al. Esophagogastric junction contractile integral (EGJ-CI) quantifies changes in EGJ barrier function with surgical intervention. Neurogastroenterol Motil 2016;28:639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xie C, Wang J, Li Y, et al. Esophagogastric Junction Contractility Integral Reflect the Anti-reflux Barrier Dysfunction in Patients with Gastroesophageal Reflux Disease. J Neurogastroenterol Motil 2017;23:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rogers BD, Rengarajan A, Abrahao L, et al. Esophagogastric junction morphology and contractile integral on high-resolution manometry in asymptomatic healthy volunteers: An international multicenter study. Neurogastroenterol Motil 2020:e14009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Akimoto S, Singhal S, Masuda T, et al. Classification for esophagogastric junction (EGJ) complex based on physiology. Dis Esophagus 2017;30:1–6. [DOI] [PubMed] [Google Scholar]
- 87.Akimoto S, Singhal S, Masuda T, et al. Esophagogastric Junction Morphology and Distal Esophageal Acid Exposure. Dig Dis Sci 2016;61:3537–3544. [DOI] [PubMed] [Google Scholar]
- 88.Mittal RK, Zifan A, Kumar D, et al. Functional morphology of the lower esophageal sphincter and crural diaphragm determined by three-dimensional high-resolution esophago-gastric junction pressure profile and CT imaging. Am J Physiol Gastrointest Liver Physiol 2017;313:G212–G219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nicodeme F, Lin Z, Pandolfino JE, et al. Esophagogastric Junction pressure morphology: comparison between a station pull-through and real-time 3D-HRM representation. Neurogastroenterol Motil 2013;25:e591–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Niebisch S, Wilshire CL, Peters JH. Systematic analysis of esophageal pressure topography in high-resolution manometry of 68 normal volunteers. Dis Esophagus 2013;26:651–60. [DOI] [PubMed] [Google Scholar]
- 91.Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102:1056–63. [DOI] [PubMed] [Google Scholar]
- 92.Tolone S, de Cassan C, de Bortoli N, et al. Esophagogastric junction morphology is associated with a positive impedance-pH monitoring in patients with GERD. Neurogastroenterol Motil 2015;27:1175–82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Supplemental Figure 1. Supportive Role of Solid Test Swallows and Solid Test Meal. In 5ml wet swallow the distal contractile integral (DCI) and integrated relaxation pressure (IRP) are normal. With solid test swallows the IRP is elevated and symptoms of dysphagia are elicited, unmasking an obstruction and supporting a diagnosis of esophago-gastric junction (EGJ) outflow obstruction in an otherwise normal study.
Supplemental Figure 2. Supportive Role of Pharmacologic Provocation. Representative esophageal pressure topography plot during wet swallow, amyl nitrite (AN) inhalation and subsequent recovery phase in a patient with AN-responsive EGJOO (early achalasia). Note that after sniffing AN there is a significant drop in EGJ pressure and distal esophageal smooth muscle contractility is inhibited. The dramatic exaggerated rebound EGJ contraction response during recovery phase may indicate chronic esophageal nitric oxide deprivation.
Supplemental Figure 3. Supportive Role of Post-Prandial Monitoring. In Post-prandial monitoring there is a transient lower esophageal sphincter (LES) relaxation (TLESR) with reflux with symptoms of reflux/belching, followed by a rumination episode with symptom of regurgitation. Upper esophageal sphincter (UES); High resolution manometry (HRM)
Supplemental Figure 4. EGJ Morphology. Three subtypes of EGJ morphology include A) normal with the CD superimposed on the LES and the RIP localizing proximal to the complex (Akimoto A or Type I EGJ morphology), B) LES-CD separation with the RIP localized proximal to the CD (Type II EGJ morphology or Akimoto C), C) LES-CD separation with the RIP localized proximal to the LES (Type III EGJ morphology or Akimoto B)
Supplemental Table 1 Working Group Baseline Characteristics and Responses to Initial Survey
Supplemental Table 2. Disorders of EGJ Outflow. Definitions of a conclusive diagnosis, inconclusive diagnosis and supportive testing.
Supplemental Table 3. Disorders of Esophageal Peristalsis. Definitions of a conclusive diagnosis, inconclusive diagnosis and supportive testing.
Supplemental Table 4. Recommendations of the Chicago Classification v4.0


