Abstract
Background and aims
Long COVID is the collective term to denote persistence of symptoms in those who have recovered from SARS-CoV-2 infection.
Methods
WE searched the pubmed and scopus databases for original articles and reviews. Based on the search result, in this review article we are analyzing various aspects of Long COVID.
Results
Fatigue, cough, chest tightness, breathlessness, palpitations, myalgia and difficulty to focus are symptoms reported in long COVID. It could be related to organ damage, post viral syndrome, post-critical care syndrome and others. Clinical evaluation should focus on identifying the pathophysiology, followed by appropriate remedial measures. In people with symptoms suggestive of long COVID but without known history of previous SARS-CoV-2 infection, serology may help confirm the diagnosis.
Conclusions
This review will helps the clinicians to manage various aspects of Long COVID.
Keywords: Long COVID”, “Long haulers”, “Post COVID syndrome”
1. Introduction
SARS-CoV-2 infection (COVID-19) is a major pandemic resulting in substantial mortality and morbidity worldwide. Of the individuals affected, about 80% had mild to moderate disease and among those with severe disease, 5% develop critical illness [1]. A few of those who recovered from COVID-19 develop persistent or new symptoms lasting weeks or months; this is called “long COVID”, “Long Haulers” or “Post COVID syndrome.”
1.1. Acute COVID
Those infected with SARS-CoV-2 virus commonly develop symptoms 4–5 days after exposure. Acute COVID symptoms include fever, throat pain, cough, muscle or body aches, loss of taste or smell and diarrhea. A study from England, Wales and Scotland identified three clusters of symptoms during acute illness [2]. They are.
-
•
respiratory symptom cluster: with cough, sputum, shortness of breath, and fever;
-
•
musculoskeletal symptom cluster: with myalgia, joint pain, headache, and fatigue
-
•
enteric symptom cluster: with abdominal pain, vomiting, and diarrhea
COVID Symptom Study group identified six clusters of symptoms [3]. They are:
-
•
“Flu-like” with no fever—headache, loss of smell, muscle pains, cough, sore throat, chest pain, no fever
-
•
“Flu-like” with fever—headache, loss of smell, cough, sore throat, hoarseness, fever, loss of appetite
-
•
Gastrointestinal—headache, loss of smell, loss of appetite, diarrhea, sore throat, chest pain, no cough
-
•
Severe level one, fatigue—headache, loss of smell, cough, fever, hoarseness, chest pain, fatigue
-
•
Severe level two, confusion—headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, muscle pain
-
•
Severe level three, abdominal and respiratory—headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, muscle pain, shortness of breath, diarrhea, abdominal pain
Recovery from mild SARS-CoV-2 infection commonly occurs within 7–10 days after the onset of symptoms in mild disease; it could take 3–6 weeks in severe/critical illness [4]. However, continued follow up of patients who recovered from COVID-19 showed that one or more symptoms persist in a substantial percentage of people, even weeks or months after COVID-19.
1.2. “Long COVID”
The term long COVID was first used by Perego in social media to denote persistence of symptoms weeks or months after initial SARS-CoV-2 infection and the term ‘long haulers’ was used by Watson and by Yong [[5], [6], [7]].
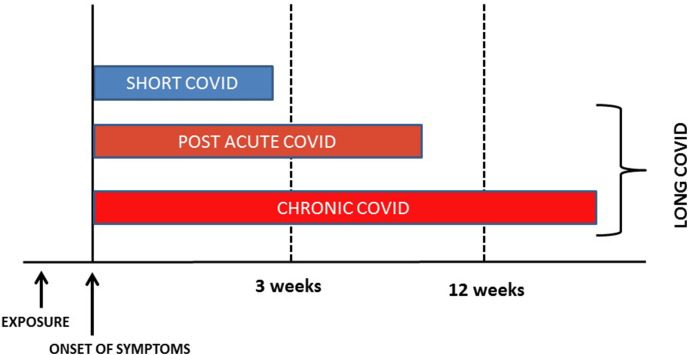
“Long COVID” is a term used to describe presence of various symptoms, even weeks or months after acquiring SARS-CoV-2 infection irrespective of the viral status [8]. It is also called “post-COVID syndrome”. It can be continuous or relapsing and remitting in nature [9]. There can be the persistence of one or more symptoms of acute COVID, or appearance of new symptoms. Majority of people with post-COVID syndrome are PCR negative, indicating microbiological recovery. In other words, post COVID syndrome is the time lag between the microbiological recovery and clinical recovery [10]. Majority of those with long COVID show biochemical and radiological recovery. Depending upon the duration of symptoms, post COVID or Long COVID can be divided into two stages-post acute COVID where symptoms extend beyond 3 weeks, but less than 12 weeks, and chronic COVID where symptoms extend beyond 12 weeks [11]. (Fig. 1 ).
Fig. 1.
Classification of long COVID.
Thus, among people infected with SARS-CoV-2 the presence of one or more symptoms (continuous or relapsing and remitting; new or same symptoms of acute COVID) even after the expected period of clinical recovery, irrespective of the underlying mechanism, is defined as post COVID syndrome or Long COVID.
There are several challenges in the diagnosis of long COVID. The time taken for the clinical recovery varies depending upon the severity of illness; while associated complications make it difficult to define the cut-off time for the diagnosis. A significant proportion of SARS-CoV-2 infected individuals are asymptomatic, and many individuals would not have undergone any test to confirm SARS-CoV-2 infection. If these individuals develop multiple symptoms subsequently, making a diagnosis of long COVID without a preceding evidence of SARS-CoV-2 infection is challenging. The testing policy varies in different countries and it is a common practice during a pandemic to diagnose clinically based on symptoms without any confirmatory tests. Therefore, persistence of symptoms in those who had never checked for COVID is a challenge [12]. Similarly, residual symptoms in those checked negative for COVID (false negative as testing may be done too early or too late in the disease course) may also add to diagnostic dilemma [13]. Antibody response to infection also varies and about 20% does not seroconvert. Antibody level may decrease over time challenging the retrospective diagnosis of recent SARS-CoV-2 infection [14,15].
1.3. “Long COVID”-real world scenario
A report from Italy found that 87% of people recovered and discharged from hospitals showed persistence of at least one symptom even at 60 days [16]. Of these 32% had one or two symptoms, where as 55% had three or more. Fever or features of acute illness was not seen in these patients. The commonly reported problems were fatigue (53.1%), worsened quality of life (44.1%), dyspnoea (43.4%), joint pain, (27.3%) and chest pain (21.7%). Cough, skin rashes, palpitations, headache, diarrhea, and ‘pins and needles’ sensation were the other symptoms reported. Patients also reported inability to do routine daily activities, in addition to mental health issues such as anxiety, depression and post-traumatic stress disorder.
Another study found that COVID-19 patients discharged from hospital experience breathlessness and excessive fatigue even at 3 months [17].
The prevalence of residual symptoms is about 35% in patients treated for COVID-19 on outpatient basis, but around 87% among cohorts of hospitalized patients [16,18].
The percentage of people, who failed to return to their job at 14–21 days after becoming COVID positive, was 35% according to one survey [18]. It is more common in older age groups (26% in 18–34 years, 32% in 35–49 years and 47% in 50 years and above), and among those with co morbidities (28% with nil or one co-morbidity, 46% with two and 57% with three or more co morbidities). Obesity (BMI>30) and presence of psychiatric conditions (anxiety disorder, depression, posttraumatic stress disorder, paranoia, obsessive-compulsive disorder and schizophrenia) are associated with greater than two-fold odds of not returning to job by 14–21 days after a positive result [18]. Fever and chills present in the acute stage of infection resolved in 97% and 96% of individuals respectively. But cough, fatigue and shortness of breath did not resolve in 43%, 35% and 29% of patients during interview. Loss of taste and loss of smell took longer duration for resolution (8 days). As per a recent meta analysis the 5 most common manifestations of Long COVID-19 were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), dyspnea (24%) [19].
Among patients admitted to critical care unit who were on ventilator for a prolonged time, residual symptoms are common. However, COVID patients who had mild disease also report not regaining their pre-COVID health status, effectively questioning the terminology of “mild” disease.
1.4. Risk factors for long COVID
Follow up of patients recovered from COVID identified a few factors which are commonly associated with development of long COVID. The risk of long COVID is twice common in women compared to men [9]. Increasing age is also a risk factor and it is found that patients with long COVID are around four years older than those without [9]. Presence of more than 5 symptoms in the acute stage of illness is associated with increased risk of developing long COVID [20]. Symptoms most commonly associated with long COVID include fatigue, headache, dyspnea, hoarse voice and myalgia [20]. Presence of co morbidities also increases the risk of developing post COVID syndrome. Even those with mild symptoms at initial presentation were noted to develop long COVID.
1.5. Pathophysiology of “Long COVID”
The exact mechanism behind the persistence of symptoms has to be identified. Reason for the persistence of symptoms can be the sequelae of organ damage, varying extent of injury (organ damage) and varying time required for the recovery of each organ system, persistence of chronic inflammation (convalescent phase) or immune response/auto antibody generation, rare persistence of virus in the body, nonspecific effect of hospitalization, sequelae of critical illness, post-intensive care syndrome, complications related to corona infection or complications related to co morbidities or adverse effects of medications used [21,22].(Fig. 2 ) Persistence of infection can be due to persistent viremia in people with altered immunity, re-infection or relapse [[23], [24], [25]]. Deconditioning, psychological issues like post-traumatic stress also contribute to symptoms [[26], [27], [28]]. The social and financial impact of COVID-19 also contributes to post COVID issues including psychological issues. Differentiating residual symptoms from re-infection is important in the public health perspective. Persistently elevated inflammatory markers point towards chronic persistence of inflammation. It is helpful to remember that in any patient, multiple mechanisms may contribute to long COVID symptoms.
Fig. 2.
Various pathophysiological mechanism of “Long COVID”.
1.6. Common symptoms in “Long COVID”
Common symptoms in people with “Long COVID” are profound fatigue, breathlessness, cough, chest pain, palpitations, headache, joint pain, myalgia and weakness, insomnia, pins and needles, diarrhea, rash or hair loss, impaired balance and gait, neurocognitive issues including memory and concentration problems and worsened quality of life. In people with “Long COVID” one or more symptoms may be present.
Researchers identified two main patterns of symptoms in people with long COVID: they are 1) fatigue, headache and upper respiratory complaints (shortness of breath, sore throat, persistent cough and loss of smell) and 2) multi-system complaints including ongoing fever and gastroenterological symptoms [20]. Survivor Corps report shows that 26.5% of people with Long COVID experienced painful symptoms [27-PP45] [29]. In patients with long COVID some of the symptoms are first reported 3–4 weeks after the onset of acute symptoms [20].
Profound fatigue is a common problem and one study showed that at 10 weeks of follow up after SARS-CoV-2 infection; more than 50% of people were suffering from fatigue. There was no association between development of fatigue, COVID-19 severity and level of inflammatory markers. Female sex and diagnosis of depression/anxiety is more common in those with fatigue [30]. Post viral fatigues are commonly reported in people with viral infections like EBV, Ebola, influenza, SARS and MERS. In the absence of any other reason, if fatigue persists for 6 months or longer it is called chronic fatigue syndrome. Up to 40% of patients who recovered from SARS of 2003 have chronic fatigue. The presence of chronic oxidative and nitrosative stress, low-grade inflammation and impaired heat shock protein production were among the proposed mechanisms for muscle fatigue. Profound fatigue is a challenge not only to the patient but also the healthcare provider, as there are no objective methods to diagnose it with certainty. Disruption of trust in the doctor-patient relationship can occur in such settings [31].
Infection with SARS-CoV-2 can leads to various pulmonary complications like chronic cough, fibrotic lung disease (post-COVID fibrosis or post-ARDS fibrosis), bronchiectasis, and pulmonary vascular disease [32]. Chronic shortness of breath could be the result of residual pulmonary involvement, which is known to clear slowly with time. Unfortunately, many asymptomatic patients with COVD-19 have significant lung involvement, as shown on CT scans. COVID-19 may lead to pulmonary fibrosis, which can result in persistence of dyspnea and need for supplementary oxygen.
Common cardiac issues in patients from COVID 19 include labile heart rate and blood pressure responses to activity, myocarditis and pericarditis, impaired myocardial flow reserve from micro vascular injury, myocardial infarction, cardiac failure, life-threatening arrhythmias and sudden cardiac death. Coronary artery aneurysm, aortic aneurysm, accelerated atherosclerosis, venous and arterial thromboembolic disease including life threatening pulmonary embolism can also occur [33]. Several of these may manifest as Long-COVID after recovery from acute illness.
Presence of SARS-CoV-2 in CSF shows its neuro-invasive features and there is possible disruption to micro-structural and functional brain integrity in patients recovered from COVID-19 [34,35]. Headache, tremor, problem with attention and concentration; cognitive blunting (“brain fog”), dysfunction in the peripheral nerves; and mental health problems like anxiety, depression and PTSD are common in people with long COVID. Neuropsychiatric manifestations of COVID-19 have been documented in a British study. Stroke and altered mental status were the commonest among this group. Multiple psychiatric symptoms stemming from encephalopathy or encephalitis and primary psychiatric diagnoses, were noted commonly in young patients [36]. Acquired focal or multifocal peripheral nerve injury (PNI) was noticed in those who received prone ventilation for COVID related ARDS [37]. Critical illness and prolonged mechanical ventilation due to any cause can results in ICU-acquired weakness, deconditioning, myopathies, neuropathies and delirium.
Post COVID inflammation can result in various symptoms. Inflammatory arthralgia has to be differentiated from other similar conditions like Rheumatoid arthritis and SLE [38]. Severe infection with SARS-CoV-2 can results in autoreactivity against a variety of self-antigens [39]. COVID-19 associated coagulopathy (CAC) can results in both arterial and venous thrombosis [40].
1.7. Approach to patients with long COVID
Detailed history and clinical examination help with the diagnosis in people with recent SARS-CoV-2 infection. In patients with symptoms suggestive of long COVID, without previous evidence of SARS-CoV-2 infection, demonstration of antibody positivity helps to confirm the diagnosis. However, antibody levels are known to drop with time; therefore a negative serology test does not rule out a past SARS-CoV-2 infection. In such scenario diagnosis of long COVID can be challenging. Raveendran’s criteria for the diagnosis of long COVID-19, helps to categorise as confirmed, probable, possible or doubtful long COVID-19 syndrome [12]. Majority of the people with long COVID does not require extensive evaluation. Investigations may be directed by symptoms.
Clinical evaluation of patients presenting with long COVID starts with documentation of the existing problem-its improvement or deterioration, and also documentation of new problems, if any (Fig. 3 ).
Fig. 3.
Approach to patients with Long COVID.
Long COVID can be divided into different categories depending upon the predominant residual symptoms as post COVID cardio-respiratory syndrome, post COVID fatigue syndrome and post COVID neuro-psychiatric syndrome [13,41,42]. (See Table 1 ). Categorization of symptoms according to the organ system involved will help to identify the etiology. For example, in people with breathlessness, evaluation mainly focuses on cardiac and respiratory system involvement. Severe fatigue necessitates ruling out common causes like anemia, hyperglycemia, electrolyte imbalance and hypothyroidism, depending upon the clinical scenario. Any new onset symptoms after recovery from COVID-19 should be properly addressed to rule out life threatening complications such as pneumothorax, pulmonary embolism, coronary artery disease and stroke (see Table 1).
Table 1.
Post COVID syndrome categories.
| Post COVID syndrome | Predominant clinical features | Remarks |
|---|---|---|
| Post COVID fatigue syndrome | Profound fatigue | Rule out causes like anaemia, hypothyroidism, electrolyte imbalance |
| Post COVID cardio-respiratory syndrome | Cough, low grade fever, shortness of breath, chest pain, | Sudden increase in dyspnoea can be due to tension pneumothorax, pulmonary embolism, coronary artery disease or heart failure in patients recovered from COVID-19 |
| Post COVID neuro-psychiatric syndrome | Headaches, anosmia, neurocognitive difficulties, insomnia, depression and other mental health conditions | In patients with acute onset neurological symptoms consider vasculitis, thrombosis or demyelination. Post COVID psychological issues have to be addressed properly. |
| Post COVID gastro-intestinal syndrome | Abdominal discomfort, diarrhea, constipation, vomiting, | GI symptoms can be a sequelae of the disease. Various drugs used during acute COVID, especially lopinavir/ritonavir produces GI symptoms |
| Post COVID hepato-biliary syndrome | Nausea, jaundice, deranged LFT | Drugs used in the treatment of COVID-19 like remdesivir, favipiravir, lopinavir/ritonavir and tocilizumab can cause hepatic impairment. |
| Post COVID musculo-skeletal syndrome | Muscle pains and weakness, arthralgia | May be due to disease, prolonged ICU care, neurological problems, myopathy or electrolyte imbalance. Usually subside during follow up. Inflammatory arthralgia has to be differentiated from other causes like RA, SLE |
| Post COVID thromboembolic syndrome | Depending upon the vascular territory of involvement breathlessness in PE, chest pain in CAD and limb weakness and neurological deficit in CVA | Early diagnosis and treatment is life saving. Follow the standard treatment protocol. |
| Post COVID multisystem inflammatory syndrome/post COVID autoimmune syndrome | Fever, gastrointestinal symptoms, rash, chest pain, palpitations | Elevated levels of markers of inflammation. |
| Post COVID genito-urinary symptoms | Proteinuria, haematuria, development of kidney injury | Endothelial dysfunction, coagulopathy, complement activation, direct effect of virus on kidney, sepsis and multi-organ dysfunction contribute to the development |
| Post COVID dermatological syndrome | Vesicular, maculopapular, urticarial, or chilblain-like lesions on the extremities (COVID toe) |
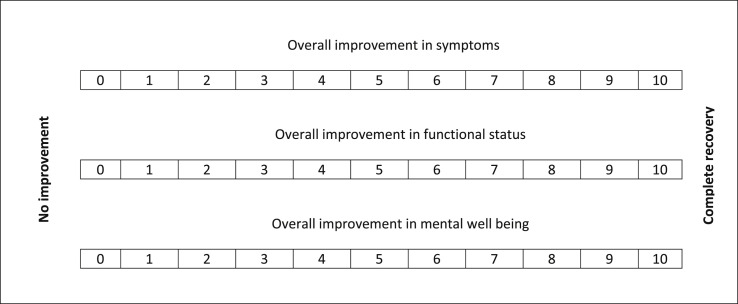
During each visit, the overall improvement in symptoms can be assessed by using score of 0–10, where 0 represents no improvement, and 10 represents complete recovery. In patients with multiple symptoms, each symptom can be documented using a similar score. Overall functional status improvement and overall improvement in mental wellbeing can also be represented by a score of 0–10 (see Table 2 ). Appearance of new symptoms can also be assessed by a score of 0–10, with a prefix of “N" to indicate new symptoms. Enquiring about the patient’s health and functional status before SARS-CoV-2 infection helps to understand the impact of long COVID.
Table 2.
Post COVID status assessment scale.
1.8. Management of patients with long COVID
Treatment of people with long COVID requires a multi-disciplinary approach including evaluation, symptomatic treatment, treatment of underlying problems, physiotherapy, occupational therapy and psychological support [11]. Minor symptoms like cough, pain, myalgia can be treated symptomatically with paracetamol, cough suppressants and oral antibiotics (if secondary bacterial infection is suspected). Etiology behind the symptoms, if any, like pulmonary embolism, cerebrovascular accident, coronary artery disease, has to be treated as per the standard protocol. Chest physiotherapy and neuro rehabilitation is important in patients with pulmonary and neuromuscular sequelae. Since it is a new disease, the knowledge regarding long term effects and treatment options is still evolving. Worsening of underlying co-morbidities like diabetes, hypertension and cardiovascular illness could occur in people after SARS-CoV-2 infection, requiring optimization of treatment.
The ideal frequency and duration of follow up is also not clearly defined. In people with COVID-19 interstitial pneumonia, in the first 12 months, 7 interactions with healthcare professionals (4 face-to-face) are recommended, alongside 4 HRCTs, 4 6MWT, 4 blood tests (including blood count and metabolic panel) and 2 SARS-CoV-2-IgG tests [43]. In our experience, majority of people with mild-moderate symptoms and those who show improvement in symptoms can be followed up with online or telephonic consultation, with fewer face-to-face interactions. Those with severe symptoms and progressive worsening need frequent in-person review. Those developing acute worsening of symptoms or acute onset of new symptoms should be advised to report the emergency department immediately. Frequency of follow up has to be individualized according to patient’s clinical profile.
Chronic persistence of symptoms in people with SARS-CoV-2 infection has significant social and economic impact. As the disease continues to spread, more people may need health care support in the near future, which could overburden the health care system. Clear guidelines regarding management of long COVID-19 will help clear the confusion among health care providers. Long term follow up of COVID recovered patients will throw more light into “long COVID” and its management [44].
2. Conclusion
Persistence of various symptoms in people who recovered from COVID-19 (collectively called Long COVID) is a major health issue worldwide. It could be due to various mechanisms such as post-intensive care syndrome, post-viral fatigue syndrome, permanent organ damage or others. Proper clinical evaluation will help identify the etiology, and to customize treatment. As the disease is new, it is too early to know the true long-term outlook.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA2020; 323: 1239-1242. [DOI] [PubMed]
- 2.Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudre C., Lee K., Lochlainn M., et al. Symptom clusters in covid 19: a potential clinical prediction tool from the COVID Symptom study app. Sci Adv. 2021 Mar 19;7(12) doi: 10.1126/sciadv.abd4177. PMID: 33741586; PMCID: PMC7978420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Who-China Joint Mission Members . World Health Organization; 2020. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) [Google Scholar]
- 5.Perego E. Twitter. 20 May. 2020 https://twitter.com/elisaperego78/status/1263172084055838721?s=20 [Google Scholar]
- 6.Edwards E. NBC News; 2020. COVID-19 “long-haulers” report nearly 100 symptoms for more than 100 days. [cited 2020 Jul 31] https://www.nbcnews.com/health/health-news/covid-19-long-haulers-report-nearly-100-symptoms-more-100-n1235217. [Google Scholar]
- 7.Yong E. COVID-19 can last for several months. 2020. https://www.theatlantic.com/health/archive/2020/06/covid-19-coronavirus-longterm-symptoms-months/612679/ The Atlantic, [cited 2020 Jul 31]
- 8.Geddes L. Why strange and debilitating coronavirus symptoms can last for months. New Sci. 2020 https://www.newscientist.com/article/mg24632881-400-why-strange-and-debilitatingcoronavirus-symptoms-can-last-for-months/ [Google Scholar]
- 9.NabaviNikki Long covid: how to define it and how to manage it. BMJ. 2020;370 doi: 10.1136/bmj.m3489. m3489. [DOI] [PubMed] [Google Scholar]
- 10.Garg P., Arora U., Kumar A., Wig N. The "post-COVID" syndrome: how deep is the damage? J Med Virol. 2020 Aug doi: 10.1002/jmv.26465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenhalgh Trisha, Knight Matthew, A’Court Christine, Buxton Maria, Husain Laiba. Management of post-acute covid-19 in primary care. BMJ. 2020;370 doi: 10.1136/bmj.m3026. m3026. [DOI] [PubMed] [Google Scholar]
- 12.Raveendran A.V. Long COVID-19: challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab Syndr. 2020;15(1):145–146. doi: 10.1016/j.dsx.2020.12.025. Epub ahead of print. PMID: 33341598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Assaf G., Davis H., McCorkell L., et al. Patient Led Research; 2020. An analysis of the prolonged COVID-19 symptoms survey by Patient-Led Research Team.https://patientresearchcovid19.com/ [Google Scholar]
- 14.Van Elslande J., Vermeersch P., Vandervoort K., Wawina-Bokalanga T., Vanmechelen B., Wollants E., et al. Symptomatic SARS-CoV-2 reinfection by a phylogenetically distinct strain. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Falahi S., Kenarkoohi A. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes and New Infections. 2020;38 doi: 10.1016/j.nmni.2020.100812. 100812, ISSN 2052-2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carfì A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. J Am Med Assoc. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold DT, Hamilton FW, Milne A, et al Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort thorax Published Online First: 03 December 2020. doi: 10.1136/thoraxjnl-2020-216086. [DOI] [PMC free article] [PubMed]
- 18.Tenforde M.W., Kim S.S., Lindsell C.J., et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:993–998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P.A., Cuapio A., Villapol S. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. medRxiv. 2021 Jan 30 doi: 10.1101/2021.01.27.21250617.PMID:33532785. [Preprint] 2021.01.27.21250617, PMCID: PMC7852236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudre C.H., Murray B., Varsavsky T., et al. medRxiv; 2020. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. [DOI] [Google Scholar]
- 21.Colafrancesco S., Alessandri C., Conti F., Priori R. COVID-19 gone bad: a new character in the spectrum of the hyperferritinemicsyndrome? Autoimmun Rev. 2020;19 doi: 10.1016/j.autrev.2020.102573.pmid:32387470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tay M.Z., Poh C.M., Rénia L., MacAry P.A., Ng L.F.P. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8.pmid:32346093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu F., Wang A., Liu M., et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. 2020. https://www.medrxiv.org/content/medrxiv/early/2020/04/06/2020.03.30.20047365.full.pdf
- 24.Lan L., Xu D., Ye G., etal Positive RT-PCR test results in patients recovered from COVID-19. J Am Med Assoc. 2020;323:1502–1503. doi: 10.1001/jama.2020.2783pmid:32105304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biehl Michelle, Sese Denise. Post-intensive care syndrome and COVID-19 — implications post pandemic. Cleve Clin J Med. Aug 2020 doi: 10.3949/ccjm.87a.ccc055. [DOI] [PubMed] [Google Scholar]
- 26.GemelliAgainst Covid-19 Post-Acute Care Study Group Post-COVID-19 global health strategies: the need for an interdisciplinary approach. Aging ClinExp Res. 2020 doi: 10.1007/s40520-020-01616-x. pmid: 32529595. [DOI] [Google Scholar]
- 27.Forte G., Favieri F., Tambelli R., Casagrande M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Environ Res Publ Health. 2020;17:4151. doi: 10.3390/ijerph17114151.pmid:32532077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang H-j, Nan J., Lv Z-y, etal Psychological impacts of the COVID-19 epidemic on Chinese people: exposure, post-traumatic stress symptom, and emotion regulation. Asian Pac J Trop Med. 2020;13:252. [Google Scholar]
- 29.Lambert N.J., Corps Survivor. Indiana University School of Medicine; 2020. COVID-19 “long Hauler”Symptoms survey report. [Google Scholar]
- 30.Townsend L., Dyer A.H., Jones K., Dunne J., Mooney A., Gaffney F., et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PloS One. 2020;15(11) doi: 10.1371/journal.pone.0240784. e0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gerwyn M., Maes M. Mechanisms explaining muscle fatigue and muscle pain in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a review of recent findings. Curr Rheumatol Rep. 2017 Jan;19(1):1. doi: 10.1007/s11926-017-0628-x.PMID:28116577. [DOI] [PubMed] [Google Scholar]
- 32.Fraser Emily. Long term respiratory complications of covid-19. BMJ. 2020;370:m300. doi: 10.1136/bmj.m3001. [DOI] [PubMed] [Google Scholar]
- 33.Becker R.C. Toward understanding the 2019 Coronavirus and its impact on the heart. J Thromb Thrombolysis. 2020 doi: 10.1007/s11239-020-02107-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moriguchi T., Harii N., Goto J., et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu, Yiping; Li, Xuanxuan; Geng, Daoying; Mei, Nan; Wu, Pu-Yeh; Huang, Chu-Chung; Jia, Tianye; Zhao, Yajing; Wang, Dongdong; Xiao, Anling; Yin, Bo.Cerebral micro-structural changes in COVID-19 patients - an MRI-based 3-month follow-up study.EClinicalMedicine: 100484, 2020 Aug 03. [DOI] [PMC free article] [PubMed]
- 36.Varatharaj A., Thomas N., Ellul M.A., Davies N.W.S., Pollak T.A., otros Tenorio EL y. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. The Lancet Psychiatry. 2020 oct 1;7(10) doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malik G.R., Wolfe A.R., Soriano R., Rydberg L., Wolfe L.F., Deshmukh S., et al. 2020 Jun 01. Injury-prone: peripheral nerve injuries associated with prone positioning for COVID-19-related acute respiratory distress syndrome. medRxiv 20144436 [Preprint], [cited 2020 Jul 06]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chandrashekara S., Jaladhar P., Paramshetti S., Ramachandran V., Nizar S.F., Kori D. Post COVID inflammation syndrome: different manifestations caused by the virus. J Assoc Phys India. 2020 Dec;68(12):33–34. PMID: 33247640. [PubMed] [Google Scholar]
- 39.Woodruff Matthew C., Ramonell Richard P., Eun-Hyung Lee F., Sanz Ignacio. Clinically identifiable autoreactivity is common in severe SARS-CoV-2 Infection. medRxiv. 2020;10 doi: 10.1101/2020.10.21.20216192. 21.20216192. [DOI] [Google Scholar]
- 40.Mucha Simon R., Dugar Siddharth, Keith McCrae, Douglas Joseph, John Bartholomew, Sacha Gretchen L., Militello Michael Coagulopathy in COVID-19: manifestations and management. Cleve Clin J Med. 2020;87(8):461–468. doi: 10.3949/ccjm.87a.ccc024. [DOI] [PubMed] [Google Scholar]
- 41.Dasgupta A., Kalhan A., Kalra S. Long term complications and rehabilitation of COVID-19 patients. J Pakistan Med Assoc. 2020;70:S131–S135. doi: 10.5455/JPMA.32.pmid:32515393. [DOI] [PubMed] [Google Scholar]
- 42.Galván Casas C., Català A., Carretero Hernández G., etal Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183:71–77. doi: 10.1111/bjd.19163.pmid:32348545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raghu G., Wilson K.C. COVID-19 interstitial pneumonia: monitoring the clinical course in survivors. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30349-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The post-hospitalisation COVID-19 study (PHOSP-COVID) https://www.phosp.org