Abstract
Monitoring and managing potential infected patients of COVID-19 is still a great challenge for the latest technologies. In this work, IoT based wearable monitoring device is designed to measure various vital signs related to COVID-19. Moreover, the system automatically alerts the concerned medical authorities about any violations of quarantine for potentially infected patients by monitoring their real time GPS data. The wearable sensor placed on the body is connected to edge node in IoT cloud where the data is processed and analyzed to define the state of health condition. The proposed system is implemented with three layered functionalities as wearable IoT sensor layer, cloud layer with Application Peripheral Interface (API) and Android web layer for mobile phones. Each layer has individual functionality, first the data is measured from IoT sensor layer to define the health symptoms. The next layer is used to store the information in the cloud database for preventive measures, alerts, and immediate actions. The Android mobile application layer is responsible for providing notifications and alerts for the potentially infected patient family respondents. The integrated system has both API and mobile application synchronized with each other for predicting and alarming the situation. The design serves as an essential platform that defines the measured readings of COVID-19 symptoms for monitoring, management, and analysis. Furthermore, the work disseminates how digital remote platform as wearable device can be used as a monitoring device to track the health and recovery of a COVID-19 patient.
Keywords: COVID-19, IoT, Wearable, Potential infected patient, Healthcare, GPS
1. Introduction
COVID-19 pandemic spread has impacted the world in a critical way in the present situation. To reduce its effect, the only viable solution is to mitigate steps in the spread and curb the disease. To restrict and control the disease, the best way is to monitor the Potential Infected Patient (PIP) in quarantine by enforcing the predestined location during the period. It is only possible by the help of the Internet of things (IoT) technologies as collecting, monitoring, managing, and analyzing the disease symptoms in a remote manner [1]. As vaccines are slow to emerge and underway in the market it is seen that wearable technology can monitor and predict the incidence of COVID-19 using sensor devices such as heart rate, temperature, oxygen saturation and other respiratory systems [24]. In healthcare industries wearable technology plays a prominent role in diagnosis of recent covid-19 pandemic. Deep learning technique can sort huge amount of data to process from sensor data. By the combination of IoT and Deep learning technology the approach of health care has totally changed [34]. Due to these technologies the critical issues in medical care have been effectively solved in a reliable manner [19].
In this context sensors, cloud and IoT architecture serves in real time applications for effective solution to aim as shown in Fig. 1 . As other form of viruses COVID-19 also goes through different stages of infection such as the incubation period as a first stage without symptoms which is referred as asymptomatic. Second stage includes high-level symptoms involving fever, cold and cough. In the third stage period, where the virus is released to spread across, and last stage is recovery with no virus and immunity developed [20]. It is envisaged that the basic symptoms of covid-19 can be used to observe a patient and isolate himself in restricted areas can minimize the spread of the virus [25]. Hence the health indicators such as body temperature, SpO2 and pulse rate are the potential to determine the symptoms of novel coronavirus.
Fig. 1.
Architecture unit of smart health care System.
As per the recent research by 2020-22 it is expected that IoT wearable sensors reach to 162 million devices [18]. Internet of Medical things (IoMT) use medical sensors to collect the data and process them to reveal the critical conditions by using Deep learning approach. Various cloud-based architectures dramatically have improved to support emergency situations in health care. Fog and edge computing paradigm are used to process health sensor data directly from the sensors as edge nodes to provide location, low latency, and high availability [[2], [3], [4]].
1.1. Early detection and remote monitoring
Wearable devices are used to measure the health symptoms of potential infected people and detect physiological changes time to time during the quarantine and alert users about the possibility of infection [28]. This Early detection process helps to self-isolate the patients in the predefined location by the authorities in each country [5]. This can help the organization and governments to mitigate the steps to avoid the spread of infection and disease progression. Wearable sensors with remote patient monitoring acts as a tool to monitor the health check and trace the location with GPS data [17]. This could help the authorities to restrict the patient in isolated places and track the status in a timely manner.
Smart health systems are designed to monitor physiological parameters of body in the form of skin and motion for early solutions as different set of devices and sensors [23]. Wearable body sensor networks serve as the best solution for remote monitoring in health care systems [6]. The accelerometer sensor, ECG data, temperature sensor, and other sensors act as a network to monitor the patient's health status condition through a local server as a node to collect the data and advise the clinician [22]. Here the E-sensor platform is used as a wearable sensor to monitor the patient health as static monitoring and dynamic monitoring. In simple, it is addressed as a patient monitor using edge, fog, and cloud level. Hence this wearable technology is quite useful to monitor the infected COVID-19 patient [21].
1.2. Monitoring physiological metrics by wearable sensors for COVID-19
Wearable sensors act as potential indicators for COVID-19 virus [16]. There are various sensors that are used as metrics to measure heart rate, respiration rate, motion activity, body temperature, oxygen saturation level, cough symptoms and stress. In Table 1 , metrics which are in wearable device, that can help to detect and monitor COVID-19 virus, is presented. Sensors send the physiological measurements to cloud where further processing and analysis predicts the situation of COVID-19 virus among individuals [15].
Table 1.
Various sensors used as diagnostic equipment to monitor and detect covid-19 symptoms.
| HR | RR | SpO2 | Motion Activity | Skin | location | RHR (Resting Heart Rate) | |
|---|---|---|---|---|---|---|---|
| Accelerometer | X | X | X | ||||
| Temperature | X | ||||||
| GPS | X | ||||||
| ECG | X | X | X | ||||
| Oxygen rate | X | ||||||
| PPG | X | X | X | X | X |
Through Aforementioned studies, it is confirmed that IoT and Deep learning technique together can effectively help in monitoring and alerting the health status of human [14]. The edge, fog, and cloud computing of IoT collects the data and processes it based on the threshold conditions. The deep learning approach is effectively used in decision making, treatment support and risk monitoring in reliable manner. The multimodal recognition, monitoring and disease treatment can together help in meeting the real time requirements. In this paper, a lightweight wearable monitoring device is designed to monitor the covid-19 potentially infected people (PIP) [2]. This wearable system is designed to monitor the patient remotely in convenient and effective manner to alert and notify the concerned people in case of emergency and based on violation of self-quarantine regulations [32]. The wearable device can measure and record the health symptoms of temperature, heart rate, oxygen saturation and cough count for doctor's assisted diagnosis. Also, it is devised to store the information on cloud-based API system to send notifications and access the violation data of the patient to the authorities [33]. This handheld system is easy to carry and provide the exact GPS location of the patient and allow the authorities to respond to any emergencies required [6]. The pervasive environment is feasible to address the need of choice to quarantine the potentially infected people [13,31].
1.3. Digital health platform
One of the best with digital health platform is it detects the disease in early stage and suggests a new way to monitor disease diagnosis and progression. During this pandemic, it is found that this platform has a leverage to monitor patient remotely and assist in disease detection. Additionally, the proposed work also measures a timely escalation of health data to track and avoid the spread of pandemic in the population [12]. Digital health technologies have a precise approach to test, trace and quarantine the patient the adoption of wearable technology [29]. This adoption has aimed to alert health authorities for reducing mortality and highlight the use of clinical applications in pandemic. To describe further let us understand the technical contributions of the manuscript as follows.
-
·
IoT based wearable device to measure, record the vital signs of health symptoms for remote patients during quarantines.
-
·
Design and implementation of the 3D model system interfaced with all sensors, microcontrollers as a prototype to wear, remove and carry effectively.
-
·
An Application peripheral interface (API) as web front end to access the patient record and alert the notified respondents during emergency.
-
·
Real time GPS data of the patient in the quarantine location and alert the authorities the severity of covid-19 pandemic.
-
·
Extraction of patient health data from the API and plan accordingly for utilization of hospital facilities and critical conditions.
The organization of the paper and its contribution is as follows: Section 2 discusses a review on the related works in smart health care systems based on IoT technologies for COVID-19 pandemic, Section 3 is implementation of the proposed system and conceptualization, Section 4 defines the system design and analysis for selected parameters of COVID-19 pandemic. Finally, the section 5 outlines the conclusion and recommendations for future studies.
2. Related works
In Table 2 , several papers related to wearable design and application which are aimed to sense physiological parameters from the human body. Wireless Body Sensor Networks (WBSN) provide the best solution to monitor the infection of covid-19 and helps in stopping spreading the virus. Each sensor is connected to edge node in IoT cloud where the data is processed and analyzed to define the state of health condition [35]. The wearable IoT sensor platform is capable to track and monitor the status of COVID-19 patient in the isolated place [42]. The IoT design framework is surveyed with existing technologies to know the status of smart health care systems for COVID-19.
Table 2.
Literature survey performed for similar articles related.
| Authors Publisher & year |
Objectives | Design methods | Limitations and strengths | Outlook measures |
|---|---|---|---|---|
| Seshadri Dhruv R. et al., Frontiers in digital Health, 2020 [1], | 1. Commercial devices used to measure physiological metrics to monitor health status. 2. Digital Health platforms to manage the COVID-19 pandemic |
Mitigating clinical trials in false positive diagnosis Commercial devices used in decision making. |
Clinical pathway and role of wearable sensor technology available as commercial device for monitoring covid-19 | Issue of Data privacy, Data sharing Design and develop an algorithm to accurately monitor |
| Nooruddin et al., Elsevier, 2019 [2]. | 1. IoT based invariant fall detection system in real time. 2. Alert system to rescue individuals and provide medical assistance |
Raspberry pi, Arduino, Node MCU, smartphones, Accelerometer, GPS, Buzzer, GSM. Custom Embedded system to use as client devices |
Workflow model used in development and deployment stages as data collection, preprocessing, model creation, training and testing and deploying model in the server | Performance evaluation as precision, sensitivity, FI score and accuracy. In future threshold-based algorithm in case of network connectivity failure |
| Nora El-Rashidy et al., MDPI- Electronics, 2020 [3]. | 1. Bridging the gap between the current context of technologies and health systems 2. Patient x-ray scan information using CNN based deep learning model to predict state of art |
Framework with three layers as patient, cloud, and hospital. Deep learning classification model architecture with Dataset to pretrain and predict, evaluate new classifier |
Power consumption of wireless sensors, vital signs aggregate automatic transmission | Early detection and isolation of infected patient, effectiveness in cloud monitoring, x-ray dataset and transfer learning |
| Leonardo Acho et al., actuators, MDPI, 2020 [4]. | 1. Patient pulmonary condition for monitor and detect healthy or unhealthy situation. 2. Illustration of Potential benefits using mechanical ventilator |
Intensive care units (ICU) use respiratory frequency, patient air volume and respiration cycle to define inhale and exhale. Pressure sensor data, Arduino, Raspberry pi, interface, servomotor, monitor, Resuscitator bag |
1. Fault is in equipment operation to classify. 2.Misinterpretation of signals collected from healthy and unhealthy patients |
Numerical method to classify and clegg- integrator philosophy for lung monitoring system |
| Aras R. Dagazany et al., Hindawi, 2019 [5]. | 1. Analyze and collect wearable big data. 2. Decision making process with recognition of spatial patterns |
Deep learning for CNS and brain, spinal cord for IoT and data transfer, peripheral nervous system to sense the skin to cloud servers | Unlabeled big data, complexity, data reliability and computational bottlenecks | Massive data, heterogenous, frequency, supporting elderly population, Decision making |
| Qureshi, Fayez et al. Sensors. (2020) [6]. | 1. Use of Internet of medical things to design wearable devices. 2. Front end API for Biomedical wearable |
Wearable PPG, Accelerometer, EMG sensors, Edge computing using Raspberry pi, Dashboard as physician | Sample of Biomedical signals, design factors as economic cost, human precautions | Arduino, Microphone and cloud space, sensors cost, comparative studies |
| AKM Jahangir Alam Majumder, Hindawi, 2019 [7]. | 1. Body Area sensor IoT system to collect data in providing early warning of cardiac Arrest. 2.Low power communication module to collect temperature and heart rates on smart phone |
System architecture with Arduino Uno, Bluetooth chip, pulse sensor, temperature sensor. The model data collection, data transmission, Data analysis and Emergency contact information. Prediction window algorithm with 50% threshold | Power consumption rate for whole working cycle. Durability and long-term feasibility | Healthy and unhealthy test performance with ECG signal analysis. Galvanic skin response and accelerometer |
| Petrovic et al. (2020). IcETRAN [8] | IoT based solution to provide indoor safety through social distancing, mask detection and temperature sensing contact less | Arduino uno, thermal camera, Raspberry pi, Open CV, MQTT, Mask detection algorithm, mobile Application | Limitations in performance due to number of processed frames per second but opensource software reliable | Accuracy and frame rate for mask detection, social distance, and temperature sense |
| Anto Arockia Rosaline R. (2020). Emerald insight [9] | Purpose Geo fencing and tracking of Covid zones to monitor the people and alerting on mobile | Virtual perimeter monitoring system with wireless infrastructure. Bluetooth, wi-fi, GPS, Mobile application | Bluetooth option to ensure data security but short distance and privacy are the concerns | Proximity range accuracy at different range levels. Central monitoring system through Application |
| Hiba Asri et al. (2019). Journal of big data, springer open [10] | To predict patterns with wearable health sensors and interact with mobile phones | Heart rate sensor, Temperature sensor, Activity sensor, IoT systems, Arduino, Raspberry pi, K means clustering algorithm. Clustering by means of Elbow and silhouette method, Apache spark data bricks | Data collection from sensors Arduino uno and Raspberry pi, Android studio for coding and big data to analyze data mining, server for interaction with mobile phone | Processing time, effectiveness and K-means algorithm for clustering data, Reliability of predictive results |
Monitoring and control of infection diseases, including Covid-19, have attracted the researchers, to adopt many solutions to control different types of infections such as using health monitoring mobile applications. In Ref. [26], a mobile based android system for infectious diseases, the system is limited but do not cover the cough system detection and temperature, although the device is not wearable. In Ref. [27], a PCB Board has been used to enable portable, reconfigurable, multichannel amperometry data acquisition to measure the current-input signals from biosensor. The electronic read-out circuit can provide constant biasing voltages to the amperometry sensor [36]. However, there is no scope for data analysis or data storing. The work in Ref. [29] has focused on finding, analysing the geographic location of the patients without providing health information system. The paper in Ref. [30] is good proposal to send infection index information for analysis, but again, no hardware part application. Mobile phone enabled social community extraction for controlling of disease propagation in healthcare is designed and tested to follow the disease, in other hand, the project is mainly focus on following the propagation pattern only through mobiles and without giving any health data analysis [35]. Modelling and evaluation of disease propagation factors has been studied theoretically on [36,37], but still there is no real time implementation. In addition to the previous discussion, countries have been implemented drones, Mobile phones, and thermal cameras to follow infections, however, this can be used only for on sport checking [11]. That are represent a temporary solution as they had no physical contact. Recently a wearable IOT design framework has been suggested on which can be considered as a good technical background for the proposed system implementations if it its implemented on its modified version [29].
3. Proposed system design
Internet of things (IoT) technologies has made remote health monitoring system simple, convenient, and accessible for measuring and recording the parameters of patients in conducive environment. The components involved in IoT such as sensors, Actuators, microcontrollers, and cloud enabled systems serves to assist the patients from home instead of visiting the hospitals frequently. The proposed IoT based health monitoring system can measure physiological parameters and health symptoms of COVID-19 affected patient and able transmit their health data to an Application peripheral interface (API) which acts as a database for perusal and monitor the level of infection. Furthermore, the work also provides the geographical data of possible infected patient in quarantine or self-isolated place. The stored database system is used for alerting the medical authorities about the patient health symptoms and designated location. Basically, the proposed system consists of three layers as wearable IoT layer, cloud layer, Mobile or web frontend layer. These layers have individual functioning and connected to each other for wireless monitoring of covid-19 infected patients. One of the significant facts of the proposed work is it can create great impact in alerting medical authorities from the geographical data of potential infected people to predict and analyze the situation. A database is created to store all the healthcare data of potential infected patient and extract the information to analyze the situation.
3.1. Three layered architecture
IoT based light weight monitoring device worn as bracelet to covid-19 potential infected people monitors the health symptoms in real time [6]. This device provides the geographical information of potential infected people and alerts the concerned people in case of emergency, violation of self-quarantine regulations. The implemented architecture system consists of 3 layers as shown in Fig. 2 is to address the desired features.
Fig. 2.
IoT Design Framework for the proposed system design.
3.2. Wearable IoT layer
This layer is responsible to collect two types of data where one type of data is location-based GPS sensor data and other is health care data for covid-19 symptoms such as temperature, heart rate, oxygen saturation (SpO2) and cough count symptoms. This layer consists of microcontroller that reads the data from connected sensor modules driven by IoT core based on application design. The IoT designed application collects all the geographical data of different patients by GPS sensor, and detect the location of patient in timely manner and stores the information on the cloud. The function of this layer is that it can sense the abnormal symptoms of the patient and collect the GPS data to help to predestine the patient in one location and monitor him timely.
3.3. Cloud layer
This layer is responsible to receive the data from Microcontroller and stores the patient record in the API interface designed uses cloud flare to deploy the webpage for real time performance and security. This Cloudflare is designed to support anything which is connected to internet in terms of infrastructure, applications, and teams. One of the significant capabilities of this resource is it protects all the data by built in firewall application and gives a freedom to the user in building a secure and globally reliable system for the application. Furthermore, all the details of patient symptoms, emergency contact, location data are stored in Cloudflare's global network. API endpoints are used to exchange data with authorized systems and users and sends Email/SMS alerts to authorities and patient relatives in case of emergency to take proper actions.
3.4. Web frontend layer
This layer main function is to receive real time data from the cloud-based system and interface to a domain which maintains the ownership, credibility for the data obtained. It can also be used to analyze the information and alert the authorities time to time and call-in emergency to the patient's respondents. The proposed system design is illustrated in Fig. 2 which shows the human patient worn with wearable device to the ankle as bracelet having sensors such as heart rate, temperature, SpO2 oxygen saturation, cough count (respiratory rate) and GPS sensor with antenna to locate the latitude and longitude of the patient location. This information sensed by sensing unit is received by microcontroller for processing and analysing the design application features and then sent to cloud layer for archiving and retrieval as per the requirement. The GPS data sensed is quite useful to analyze the patterns of predetermined geofence of potential infected patients. It can also be used to perform preventive care of potential infected people by observing them in timely manner and respond to any immediate measures in protecting the health of patient in emergency and geofencing them to limit the spread of the disease.
The work also helps in exploratory study of economic impact on any country by building a database of health history of all the potential infected patients and performs regular checks to the patients by regular monitoring from the sensor data. This can reduce the spread of the disease also restrict potential infected patients to home by self-quarantine and limit their movement. The pandemics alert can be predicted from the database and mitigate the steps to control the spread of the disease.
Even though there are major achievements in the work but still there are quite challenges to address with people, physiological systems, battery support and demographics for large data endeavours. The work shows the feasibility in providing the real time GPS data and physiological symptoms through the wearable device for distributed population. The results demonstrate in section 5 gives the insightful details of efficiency and effectiveness. Nevertheless, the findings have potential impact in social research and personal data trust. The hardware and software co-design and the components involved are discussed in the next section as a curated research project.
4. System analysis for COVID-19 symptoms
Wearable system design is a smart and intelligent assisted technology that is worn on the left or right ankle of the hand as bracelet for transmitting, assessing, monitoring, and evaluating the vital signs of covid-19 infection. There are different types of data received from sensors relating the physiological symptoms from the human body. As a broad category, the COVID-19 symptoms are defined in to two categories: basically, physical health indicator systems, and other as respiratory systems. The basic health indicators in first category are temperature, heart rate, oxygen saturation in the blood (SpO2). Respiratory support systems are cough count detection which is used to measure rate of cough and detect the shortness of breathing. Therefore, all these symptoms need to be considered through wearable device design, where it can play a vital role in detecting the symptoms of covid-19 as physical testing and monitoring the large number of people in parallel is not possible due to rapid diagnose community acquired phenomena. Let us understand each wearable sensor to identify and detect the signs of COVID-19 infected patients.
4.1. Basic physiological sensors
There are three vital signs considered in this category which are body temperature, oxygen saturation in the blood (SpO2) and pulse rate as they are considered as primary symptoms in corona virus infection [38]. The vital signs have a threshold indicating the possible virus infection such as body temperature greater than or equal to 38 °C, pulse rate as 100 bpm, oxygen saturation in the blood as 92–96%. These vital physiological signs of human body threshold predict the virus infection.
4.2. Body temperature
The first and foremost essential measurement of COVID-19 infection is body temperature as this is basic assessment carried to check the fever spread in human body. The skin temperature monitoring is an efficient solution to determine the COVID-19 virus infection. Studies have been reported in percentage that the main clinical presentation of covid-19 is having fever (90% or above) while cough may appear on 75% of possible infected persons [39]. The above-mentioned symptoms are considered as primary clinical feature. Hence, it is essential to monitor the temperature and cough for suspected person in non-medial entombment such as homes. Nowadays, temperature is measured mainly through imaging techniques such IR scanner which is affected by ambient and other external factors. In this work, direct temperature sensor is used to closely monitor the skin temperature. The Dallas Temperature Sensor (DS18B20) is a user programmable one wire temperature sensor introduced by maxim integrated to measure a range of −55C to +125 C consists of 3 pins, named as follows: VDD, GND and DQ. One of the significant features of this sensor is it can directly power the data line without the need of external power supply. It is quite flexible to use with programmable resolution from 9 to 12 bits. The pin configuration between Dallas temperature sensor and Arduino MKR GSM is shown below in Table 3 . The Data pin is connected to Pin 8 of the Arduino MKR GSM 1400.
Table 3.
PIN configuration of Temperature sensor to Arduino MKR.
| Dallas Temperature Sensor (DS18B20) | Arduino MKR GSM 1400 Pins |
|---|---|
| GND | GND |
| VDD | 5V |
| Data | Pin 8 |
The wearable design prototype uses Dallas 18B20 sensor as a standard temperature sensor, able to measure the temperature from −55 °C to 150 °C Range with 0.5 accuracy. It has an operating voltage from 4 to 30 V, the power to the sensor is given by the microcontroller to measure the skin temperature in real time for every 60 s. The sensor has three pins GND, Output and VDD. These pins are interfaced to the microcontroller with a standard one wire. The sensor is very small in size and fixed in the wearable device causing no discomfort to the human body and it is usually a health companion to measure and collect the skin temperature from time to time, furthermore it is used to evaluate the physical status and condition and update the same through the API platform for close investigation of patient ailments. The skin temperature collected also alerts the clinical staff for immediate action during sharp changes of high fever through web front end.
4.3. Oxygen saturation in the blood (SpO2) and heartbeat monitoring
The use of the sensor is to measure the amount of haemoglobin saturated with oxygen as it is an indicative measure of overall health person. The virus infection reduces the level of oxygen flow in the blood and decreases the percentage respiratory distress. It can be termed that the healthy person has 96–100% level and it decreases as the spread of infection increases. To further understand the pulse oximetry usually, a patient's body lung is filled of liquids and inflamed material. This restricts the lungs ability to pass the Oxygen to the blood stream. SpO2 Level range from 95% to 100% is considered as healthy scale, while 94% indicate a possible covid-19 infection where the patient must be admitted to ICU for very close monitoring. SpO2 device is a need to regularly monitor the oxygen level of possibly infected person and notify if there are any abnormal recordings [40]. This factor defines the acuteness and progression of the disease to severe stage. The proposed wearable device uses a Spark Fun pulse oximeter as it consumes less power and very compact in the design. The design chip for Spark Fun pulse oximeter is based on Maxim Integrated as MAX30101 pulse oximetry used to perform filtering and detection. The MAX30101 senses the LED to know the light absorbed from the arteries and photo detect the sensor confidence from the finger detection data as the dimensions of the chip are small enough as 25.4 mm × 12.7 mm. If required, the chip can be placed in head or chest area to know oximetry level with an error rate of 3%. The real time monitoring of SpO2 greatly helps to monitor the potentially infected patients as telemedicine to experience the health conditions during sleep apnea as well.
This monitoring significantly required to check the heart functioning continuously in convenient and effective manner. COVID-19 increases the physiological stress in the body due to which myocardial injury can happen in our cardiovascular system. Hence it is very important to monitor the heart rate per minute, the main reason behind the observation is to indicate possible infections of fever or cough. Standard heart rate is from 40 to 100 BPM, but it increases due to spread of infection and it strongly advice to have medical support for high heartbeat rate. Therefore, our wearable device is built with heart rate sensor of Spark Fun utilized to measure both oxygen saturation and heartrate. There are two maxim integrated chips used for measuring the pulse oximetry and heartbeat as one chip is useful for sensing and other for calculation, processing, filtering, and detection. The sensed data of oxygen saturation is passed to MAX32664 which applies its algorithms to determine heart rate and blood oxygen saturation (SpO2). This sensor system allows real time monitoring and detection to track the health conditions.
The Spark fun Pulse Oximeter and Heart rate Sensor consists of 4 pins which are connected to the Arduino MKR GSM 1400 via the QWIIC cable. These pins are as follows: Ground (GND), Voltage (VCC), Serial Data (SDA) and Serial Clock (SCL). The Spark fun Pulse Oximeter and Heart rate Sensor consists of 6 additional pins, out of 2 are connected to the Arduino MKR GSM 1400 via regular jumper wires. The 2 pins are as follows: MFIO and Reset (RST). Make sure that the supply voltage to the Spark fun Pulse Oximeter and Heart rate Sensor does not exceed 3.3V. Keeping this in mind the VCC pin was connected to the 3.3V pin of Arduino BLE sense. To interface the oximeter and heartrate sensor to Arduino MKR GSM 1400 the following pins defined in the Table 4 are used. SparkFun sensor system uses Inter Integrated circuit bus with sensors, actuators and cables which makes this sensor system to work faster and efficient. In short, this has pulse oximeter sensor which can provide LED reflective solution for low power operation with robust motion and high performance. This sensor can process both raw and mixed data available using finger-based algorithms which can measure pulse and heart rate simultaneously in real time. Table 5 indicates the pin connections between the Arduino Nano and ARDUINO MKR 1400.
Table 4.
Pin configuration of Spark fun Pulse Oximeter and Heart rate to Arduino MKR.
| Spark fun Pulse Oximeter and Heart rate | Arduino MKR GSM 1400 |
|---|---|
| GND | GND |
| VCC | 3.3V (Arduino BLE Sense) |
| SDA | Pin 11 |
| SCL | Pin 12 |
| MIFO | Pin 5 |
| RST | Pin 4 |
Table 5.
Pin configuration to Arduino nano to Arduino MKR.
| Arduino Nano 33 BLE Sense Pins |
Arduino MKR GSM 1400 Pins |
|---|---|
| GND | GND |
| VCC | 5V |
| Pin 12 | A0 |
4.4. Respiratory system
There are many respiratory systems available to assist and support during COVID-19 but in our proposed work dry cough is detected from the shortness of breath and cough count. Dry cough is one of the major symptoms of COVID-19 in the second stage of infections where the virus affects the lungs and create difficulty in breathing. In general, there are two sensors which detect the difficult in breathless: One is mechanical sensor and other is audio sensor. Both are efficient enough but due to compatibility and compact design the sensor chosen is audio sensor which is sensitive microphone. A cough detection system is implemented using edge impulse studio which provides a free platform to build machine learning (ML) system using artificial intelligence system. This platform provides interfacing capability with Arduino boards through wireless connectivity for data acquisition, feature extraction, training, testing, and downloading the program required for standalone operation of the Arduino boards. Arduino Nano BLE sense was used as target board in this implementation due to the availability of different types of sensor like microphone and accelerometer. Before making the prototype of cough detection, a machine learning system must be built to identify cough and other noise signals. In this section design steps of machine learning system are given in detail. The cough detection system can be considered as having major blocks described in Fig. 3 .
Fig. 3.
Cough Detection algorithm based on AI.
4.5. Signal acquisition
Edge impulse project was able to receive cough samples from built in microphone of Arduino nano BLE sense as sensor for data collection. Cough sounds and noise sounds are captured with the sensor at a sampling frequency of 16000 Hz for a duration of 2 s. Duration of sound was fixed at 2 s after experimental verification of cough sounds. If duration is kept more, then the system tends to get trained with noise as well since cough is not lasting for long in practice and cough is not a continuous process. 1200 samples per second are collected for cough signal, as the label for training the machine learning system files are saved in the project that the file name starts with ‘cough.’ followed by unique name for each signal. Cough signal of various type like long cough, short cough, dry cough was captured at this stage to ensure identification of different cough types. To differentiate between the targeted sample and the noise, 1200 noise samples per second is recorded in each time. Various types of sample noise signals, with respect to cough, like music, conversation, air condition noise, sound of pets and animals are also included in noise signal to train the model to a diverse classis of noises. Number of cough signals and noise signals are made almost equal to make the training dataset balanced, this ensured no over fitting or under fitting for a given class during the training phase of ML network.
4.6. Feature extraction
Mel-Frequency Cepstral Coefficients (MFCCs) are used to extract features from the recorded audio signals. MFCC provide a cepstral representation of audio signals. These MFCC coefficients are fed as features for the ML network. In Edge impulse project following parameters are selected to calculate the MFCCs. The design specifications are Number of cepstral coefficients = 24, frame length in seconds = 0.02, Step between successive frames in seconds = 0.02, Number of filters in the filter bank = 32, number of FFT points = 256, size of sliding window = 101, lowest band edge for MEL filters = 300 Hz, Highest band edge of MEL filters = sampling frequency/2 = 8000Hz, pre-emphasizing coefficient = 0.98, shift = 1. MFCC coefficients are calculated for all cough and noise signals recorded for training.
Convolution Neural Network Implementation is carried out with MFCC coefficients generated are passed through a sequential CNN network architecture consisting an input layer, followed by three layers of 1-Dimensional convolutional layers and Maxpooling. The layer uses Adam's optimizer. The network is trained for two target classes ‘Cough’ and ‘Noise’.
4.7. Cough model training
The model was tested by generating new test signals; cough and noise for 10 s and predicting the cough from the newly recorded test signal. Fig. 4 shows a sample test signal recorded for 10 s with a sampling frequency of 16 KHz. The model gives an output for every 2 s frame. The result shown in Fig. 4 shows that the model detects only one cough signal correctly (happening at around sample number 15000) and detect all other sounds as noise [41]. CNN provides an accuracy of 97.5% with very low training loss of 0.17. Model shows excellent performance, and the confusion matrix shows 96.9% score for True positive and 98% score for true negative cases showing that the model has trained very well absence of under or over training. Further the efficiency of model is confirmed by a near ideal F1 score of 0.97 and 0.98 for positive and negative cases.
Fig. 4.
Sample test signal with one cough happening with Sampling rate of 12000/second.
After verification of simulation results, the model is deployed to Arduino Nano BLE Sense board connect to the computer through a serial port. The libraries and codes are downloaded to the BLE sense board to make a standalone system. The board is then disconnected from the computer and was powered by a power supply and integrated with other systems in the prototype. The model can be developed further by having a greater number of real samples of cough which are recorded by an infected person as well.
4.8. Performance testing results of AI model
The model was tested by generating new test signal by recording signals (both cough and noise for 10 s) and predicting the cough from the newly recorded test signal. The model gives an output for every 2 s frame.
CNN provided an accuracy of 97.5% with very low training loss of 0.17. Model shows excellent performance, and the confusion matrix shows 96.9% score for True positive and 98% score for true negative cases showing that the model has trained very well absence of under or over training. Further the efficiency of model is confirmed by a near ideal F1 score of 0.97 and 0.98 for positive and negative cases. Here, it worth to mention that the sample tests have been performed based on available and licensed signal on public platform, however, the test can be tuned to detect the Covid-19 dry cough which hugely impact the sound in the future.
4.9. Microcontroller
MKR 1400 Arduino board is used as a central microcontroller to receive all sensors data. Nano BLE Arduino boards is used to deploy the AI models. GPS shield and other sensors are used to interface sensors based on IoT and process and analyze them as per the application design.
4.10. Bluetooth low energy Arduino BLE 33 SENSE
The Nano BLE is connected on the Arduino Board as shown in Fig. 5 , which is having various sensors such as 9 Axis inertial sensors, humidity, temperature, barometric sensors, sensitive microphone, gesture, proximity, light color, and other sensors. It is powered with 3.3 V and it suitable for Artificial Intelligence applications that is having very small dimension of 45 × 18mm. In this project, the sensor will be used for recording and analyzing the cough sound in each 2 s and give and send the update to the designed project website.
Fig. 5.
Circuit diagram with 2 BLE NANO Sense interfaced with ARDUINO MKR.
The Arduino Nano 33 BLE Sense is a microcontroller which is powered by the main Arduino MKR GSM 1400. The Vin and GND pins of the Arduino BLE sense 1 are connected to the 5v and GND pins of the main Arduino MKR GSM 1400. The output of the Arduino BLE sense is taken from pin 12 of the BLE sense and is connected to Analog pin A0 of the Arduino MKR GSM 1400.
Summary of Pin connections for Arduino Nano 33 BLE Sense and Arduino MKR GSM 1400 is indicated on Table 3.
4.11. ARDUINO MKR 1400
The chips are form Arduino family powered with the 3.3 V. It provides a secure connection to the internet and then to the cloud platform. In the designed work there are three functions.
-
•
It connects the SpO2 sensor and Heartbeat sensor to the Cloud.
-
•
It holds the GPS sensor through connecting shield. And send the GPS data to the receiver side.
-
•
The BLE Sensor output port directly to the MKR digital input port, and hence, the later acts as bridge to communicate the BLE sensor with the cloud. The Board is powered with the 3.3 V and it has built-in sim card low power chipset operating in the different bands of the cellular range (GSM 850 MHz, E-GSM 1900 MHz, DCS 1800 MHz, PCS 1900 MHz).
The overall circuit diagram is shown in Fig. 5 with single BLE nano sense connected to Arduino to know the human activity recognition by using different axial sensors also to track and locate the potential infected patient in real time conditions. The sensors connected to the microcontroller are used to collect, measure, and analyze the real time data.
5. Results and discussions
The proposed system is designed to use both web-based application as peripheral interface for medical authorities and Android based mobile application for patient family respondents. In actual both the interfaces are synchronized together to collect and notify the health-related data. To get insightful details further and complete design architecture of IoT based wearable device which is represented in three parties: At the user side potential infected patient (PIP) has wearable sensor device worn on any hand ankle as bracelet which is used to sense the physiological health symptoms of the patient along with the location of the potential infected patient to the API cloud processing system. At the receiver end there are two parties involved where one party is the registered user family member who is primarily responsible to receive the alerts and notifications of critical health symptoms of the patient in the quarantine. The other party on the receiver side is the Application peripheral interface (API) hosted on web domain with cloud flare for storage and retrieval. This API is under control of medical authorities to monitor and manage the critical situation in providing medications and Consultations. The API interface is synchronized with android application designed on mobile for frequent alert of the patient health symptoms in quarantine.
5.1. Device testing results
Device is connected to the human body and tested under different scenarios, all the testings have been conducted by wearing the device and measuring the data related to temperature, location, SpO2, heartbeats in addition to the cough detection. For temperature scenarios, an external source of heat has been used to test the operation of heat measurement. This is done due to expose limitation for Covid-19 Patient. The following sections describe the tested scenario. The device operating duration is lasting duration is done completely in 1 h successfully with synchronization duration of 10 Minutes.
5.1.1. Monitoring of person having normal signs
The sensor reading, including temperature, SpO2 and heartbeat will be measured and send to the cloud immediately to be presented in the case manager website. Moreover, automatically the device send the location data including latitude and longitude periodically to the website. Cough sound is recorded and analyzed by the Arduino BLE sense 33 on each to 2 s and send the count to the website to store and process. The location of the person will be indicated immediately a green symbol on the dashboard (which will be discussed in the next section) on the map to indicate a summary of a person's name, ID and health status (Green), further to mention here that the system has been tested in room temperature condition as well. Fig. 5 indicates a sequence of reading from a person having normal signs which indicate clearly that the person has no potential signs of Covid-19, where the temperature is on the normal range (T < 37), Oxygen saturation level is within normal range (SpO2 > 94), heartbeat rate is on the normal level < 120, and the patient does not suffer from any cough waves, Patient ID and device ID are assigned in the registration stage. This gives the unique patient ID and serial number of the device that will be assigned for the patient. The location is indicated through longitude and latitude value which will not be given unless the device is allocated and start sending data to the website (Case manager website). All the sensor information is sent to the cloud-based system that compares the reading and decides the final status, indicates as active safe in our example through comparing the instantaneous values with in the standard range.
5.1.2. Monitoring of person having possible infected signs
As per the WHO [36], the major COVID-19 sign is the temperature, any person having temperature more than 37.5 can have a possible infection. Fig. 6, Fig. 7 , indicate a report generated by the system which is suffering from high temperature. Additional signs can also be monitored such as cough and SpO2, Heartbeat. It is very important to mention that the cough count is based on the accumulated value of cough waves which helps the case manager to determine the severity of the symptoms and to avoid any false detecting. The system will declare (active potential infection, not tested) if the following values are recognized by the system (Temperature > 38; SpO2 < 94; Cough count is more than 10). More importantly the system indicates red color on the map to alert the case manager that the tested person may start suffering from Possible Covid-19 infection. The person with the location will be in system dashboard that counts the number of possibly infected people (see Fig. 9).
Fig. 6.
Report that is generated from the system indicating normal signs (No covid-19 signs).
Fig. 7.
System report indicating possible infection.
Fig. 9.
Patient registration details.
5.1.3. Alerting in case of self quarantine violation
The wearable device is supported by GPS Shield, which sends an update about patient location longitude and latitude at regular time interval. The initial shall be provided by the patient and shall be uploaded to the device so the initial location be fixed. Once the location is uploaded, then the PIP appears on the map with his/her location. A virtual moving area, in our case, it is 5 Km is used to test device functionality. Once the PIP start crosses the area, the device is started alerting indicating that the patient is out of the quarantine area in Table 6 . The advantage of such design is.
-
1
To make a gentle reminder and indicator that the person is out of the quarantine area.
-
2
To alert the surrounding people that such a case is close to them.
-
3
To help the case manager to allocate and support the PIP by indicating the location periodically.
Table 6.
Indicates the device response vs distance with geofencing alarm.
| Testing number | Distance from the quarantine area (in M) | Testing Result |
|---|---|---|
| 1 | 5000 | Alerting Successfully |
| 2 | 3000 | Alerting Successfully |
| 3 | 1000 | Alerting Successfully |
| 4 | 500 | Alerting Successfully |
| 5 | 100 | Alerting Successfully |
| 6 | 50 | Alerting Successfully |
| 7 | 30 | Alerting Successfully |
5.2. Patient case manager
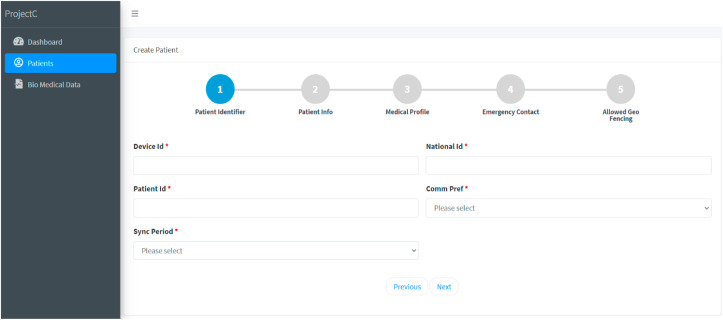
On this web page the first step is to register the possible infected person (PIP) by clicking on new patients. This registration involves 5 sequential steps to list out all the requirements of patient in quarantine (see Fig. 8).
Fig. 8.
New patient Registration on web page.
In first step patient registration is carried out where the necessary information such as name, age, National ID is included. The next step involves medical profile, details of the potential infected patient. Further steps are simple enough to fill such as emergency contact and initial geographical location or predestined location of the quarantine to track the status of the patient. The patient information can be edited by a case manager at any time and indicate the health status through a label. By using this page, the health status of the patient is indicated and identified with a Patient ID and Device ID. All the relevant details are stored, archived for monitoring, analysis, and documentation purpose. After registration, the patient details are downloaded in different text formats from the stored database.
5.3. Biomedical data web page
On the web page the wearable sensor information is collected and updated from hardware peripherals and adjusted with synch time. The biomedical data received from the patient wearable device are body temperature, SpO2 oxygen saturation, heartbeat, and cough detection per minute. This dashboard is also responsible to collect the quarantine location of the patient through GPS sensor. The latitude and longitude location of the patient is also updated and shown in the Fig. 10 .
Fig. 10.
Biomedical data of registered patients.
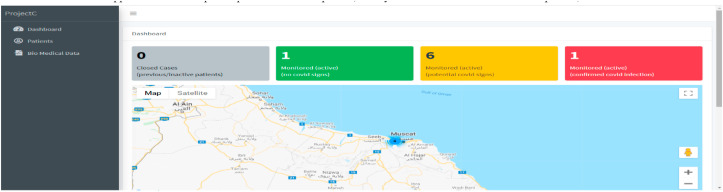
5.4. System dashboard
The dashboard continuously updates the information from the connected devices for every minute and represents the graphical representation of the situation as monitoring with no COVID-19 signs, potential COVID-19 signs, and confirmed COVID-19 signs. Each situation is shown in different colors for normal vital sign it is indicated with green colour and if the health symptoms are abnormal, then it is indicated as orange colour, confirmed cases as red and closed cases as black. The system is coloured counter gives the total overview of the patient count status, two major status is possible infected and confirmed infected cases. The dashboard has a major advantage of tracking the person location, this data synchronized with database of biomedical data which is given in the database sheet. Moreover, the dashboard generalized the total number of confirmed cases, closed cases as well. The violation of the patient and its relevant categories of Geofencing which is shown in below Fig. 11 .
Fig. 11.
Dashboard System with Indicative colors for COVID-19 status. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
5.5. Android application on mobile
The android application further updates potential infected patient, family about the health situation of the patient, which acts as a home control to discuss with doctor on behalf of the patient. The Android based application designed is very simple which has three sections home, dashboard, and notifications. The first step is to register patient's family respondent mobile number with respect to patient ID and after registration is complete then respondent can receive the alerts of a patient based on his physiological vitals in notifications section. The basic functions of the android based application are defined below.
-
•
Successful Registration of mobile number with patient ID
-
•
Receive health symptoms of the patient in quarantine.
-
•
Maintain the medical data record of the patient in consecutive time history.
-
•
Communicate with health authorities in emergencies.
Fig. 12 (a) shows the registered page of the patient with respect to his patient ID and Fig. 12 (b) shows the notification dashboard use to update the health symptoms of the patient in real time.
Fig. 12.
Android Application Requesting Registration page and Dashboard notifying patient health symptoms to family Respondents.
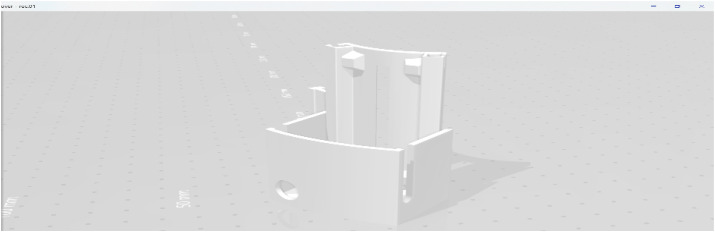
5.6. 3D wearable sensor device
Wearable sensor device prototype is a 3D design, including the hardware components such as Heart rate sensors, temperature sensor, spark fun pulse oximeter, Audio sensor, Arduino MKR 1400 board GSM, Arduino Nano 33 BLE sense, External Lithium Battery. All the components are built as 3D wearable devices, in a waterproof version to provide secure connection to API hosted in web domain. The 3D design involves a movable shape with three sections, one with microcontroller, sensors, GPS, and battery supply. The Fig. 13 shows the details of the .STL file used in 3D printing, design with proper structure and dimensions. The 3D model was designed using SketchUp software. The STL version before printing the model. The Fig. 13 shows further shape, dimensions, size of the 3D model.
Fig. 13.
3D design from SketchUp software.
The below Fig. 14 shows the layers encapsulated for automatic capturing of health data and avoiding discomfort to the patient. The 3D design is lightweight, encapsulated in a rigid manner, comfortable to ease and use, low cost, durable design.
Fig. 14.
(a) and (b) shows the 3d prototype design for a wearable device with use of all sensors.
The Fig. 14 shows the layers of the body sensors that are used to reduce the stress on the human body and the results are reflected in the system.
The final design, prototype showing the Fig. 14 defines the wearable body device for monitoring, managing and control the COVID-19 disease. The design prototype has been real time tested and demonstrated as an Application peripheral interface for various test case conditions with potential infected and normal patients in hospitals.
6. Conclusion
A wearable device prototype is designed to monitor the Covid-19 health symptoms of potentially infected patients (PIP) during the quarantine period from remote locations. The 3D prototype design involves three-layer wearable body sensor, web API layer and mobile front-end layer for an automated health care system to reduce stress and provide a means of communication between doctors, medical authorities, and family respondents. Each layer has its own functionality where wearable sensor layer is used to measure temperature, heartbeat, SpO2, and cough count. Also provides the GPS location data of the patient to the medical authorities in real time and notify the respondents of the family to reduce the alleviated stress. The Application peripheral interface layer is responsible to store, collect and analyze the data to monitor and control the social life and manage during the pandemic era. The 3D wearable design prototype is quite simple, ease of use for the potential infected patient to carry and ensure the quality of life by reducing the spread of COVID-19. The Android mobile application is very useful to provide the status of the patient to the family respondents and helps in reducing the transmission rate. The wearable device is fully developed to receive the health symptoms of the patient during and after infection. This system has been tested and verified in real time scenario in hospital to manage, monitor, and control the COVID-19 potential infected patients in the spread of the disease. It has been suggested to use the wearable device as a prototype for the passengers of the airport to quarantine during their entry and exit. There has been extensive study of this work to provide the best performance of the device by comparing the existing domains. The new features of this design accomplish different objectives to measure the health symptoms, track and monitor the patient during quarantine, maintain the data to predict the situation and alert the authorities on timely basis for efficient monitoring and use android platform to keep updated about the health status of the patient for family respondents.
Acknowledgements
The research leading to these results has received funding from the Ministry of Higher Education, Research and Innovation (MOHERI) of the Sultanate of Oman under COVID-19 Program Block Funding Agreement No. TRC/CRP/ MEC /COVID-19/20/09. Authors would like to thank Middle East college center of Research Consultancy for providing timely support and required facilities.
References
- 1.Seshadri D.R., Davies E.V., Harlow E.R., Hsu J.J., Knighton S.C., Walker T.A., Voos J.E., Drummond C.K. Wearable sensors for COVID-19: a call to action to harness our digital infrastructure for remote patient monitoring and virtual assessments. Front. Digit. Health. 2020;2(8) doi: 10.3389/fdgth.2020.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nooruddin Sheikh, Islam Md, Sharna Falguni. 2019. An IoT based device-type invariant fall detection system. 9. 100130. [DOI] [Google Scholar]
- 3.El-Rashidy Nora, El-Cappagh Shaker, Riazul Islam S.M., Hazem M., El-Bakry, Abdelrazek Samir. End to End deep learning framework for coronavirus. COVID-19) detection and monitoring. 2020;9(1):1–25. [Google Scholar]
- 4.Acho Leonardo, Vargas Alessandro N., Pujol Vazquez Gisela. Low cost, open-source Mechanical Ventilator with pulmonary monitoring for COVID-19 patients, Actuator. MDPI. 2020;9(3) [Google Scholar]
- 5.Dagazany Aras R., Stegagno Paolo, Mankodiya Kunal. Hindawi, Mobile Information systems; 2019. WearableDL: wearable internet-of-things and deep learning for big data analytics—concept, literature, and future; pp. 1–20. [Google Scholar]
- 6.Qureshi Fayez, Krishnan Sridhar. Wearable hardware design for the internet of medical things (IoMT) Sensors. 2018;18:3812. doi: 10.3390/s18113812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akm Jahangir Alam Majumder, Yosuf Amr ELsaadany, Roger Young Jr, Donald R. Ucci. Energy efficient wearable smart IoT system to predict cardiac Arrest, Hindawi. Advances in Human-computer Interaction. 2019;1507465:1–21. [Google Scholar]
- 8.Petrovic Nenad, Kocić Đorđe. IcETRAN; 2020. IoT-based system for COVID-19 indoor safety monitoring. [Google Scholar]
- 9.R., A.A.R., R., L., G., H., N., L. Tracking the Covid zones through geo-fencing technique. Int J Pervasive Comput Commun. 2020;16(5):409–417. doi: 10.1108/IJPCC-06-2020-0057. [DOI] [Google Scholar]
- 10.Asri Hiba, Mousannif Hajar, Hassan Al, Moatassime Reality mining and predictive analytics for building smart applications. J.big data, springer open. 2019;6(66):1–25. [Google Scholar]
- 11.Papadimitriou K.I., Evans D., Morgan H., Prodromakis T. 2016 IEEE biomedical circuits and systems conference (BioCAS), Shanghai. 2016. A PCB-based electronic ELISA system for rapid, portable infectious disease diagnosis; pp. 252–255. [Google Scholar]
- 12.Amador A.O., Jha N.K. Smart health care: an edge-side computing perspective. IEEE Consum. Electron. Mag. 2017;7(1):29–37. [Google Scholar]
- 13.Mei Z., Zirong Y. 2015 14th international symposium on distributed computing and applications for business engineering and science (DCABES), Guiyang. 2015. Design of epidemic monitoring platform based on ArcGIS; pp. 380–383. [Google Scholar]
- 14.Azimi I., Takalo-Mattila J., Anzanpour A., Rahmani A.M., Soininen J.P., Liljeberg P. IEEE/ACM international conference on connected health: applications, systems and engineering technologies (CHASE) IEEE; 2018. Empowering healthcare IoT systems with hierarchical edge-based deep learning; pp. 63–68. 2018. [Google Scholar]
- 15.Johansson B, Jain S, Montoya-Torres J, Hugan J, Yücesan E, Dibble C. Effective real-time allocation OF pandemic interventions.
- 16.Alwan O.S., Rao K.P. Dedicated real-time monitoring system for health care using ZigBee. Healthc. Technol. Lett. 2017;4(4):142–144. doi: 10.1049/htl.2017.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jang B., Lee M., hwi Kim M., jung Kim H., Yoo H., Kim J.W. 2019 IEEE international conference on consumer electronics (ICCE) IEEE; 2019. January. Infectious disease infection index information system; pp. 1–4. [Google Scholar]
- 18.Azmi I., Anzanpour A., Rahmani A.M., Pahikkala T., Levorato M., Liljeberg P., Dutt N. HiCH: hierarchical fog-assisted computing architecture for healthcare IoT. ACM Trans Embed Comput Syst (TECS) 2017;16(5s):174. [Google Scholar]
- 19.Ren Y., Yang J., Chuah M.C., Chen Y. 2011 IEEE eighth international conference on mobile ad-Hoc and sensor systems, Valencia. 2011. Mobile phone enabled social community extraction for controlling of disease propagation in healthcare; pp. 646–651. [Google Scholar]
- 20.Abdullatif A.A., Mohamed A., Chiasserini C.F., Tlili M., Erbad A. Edge computing for smart health: context-aware approaches, opportunities, and challenges. IEEE Netw. 2019;33(3):196–203. [Google Scholar]
- 21.Guizani, Ghafoor A. 2014 international wireless communications and mobile computing conference (IWCMC), Nicosia. 2014. Modeling and evaluation of disease spread behaviors; pp. 996–1003. [Google Scholar]
- 22.Ren Y., Yang J., Chuah M.C., Chen Y. 2011 IEEE eighth international conference on mobile ad-Hoc and sensor systems, Valencia. 2011. Mobile phone enabled social community extraction for controlling of disease propagation in healthcare; pp. 646–651. [Google Scholar]
- 23.Pilavaki E., Parolo C., McKendry R., Demosthenous A. IEEE SENSORS; Orlando, FL: 2016. Wireless paper-based biosensor reader for the detection of infectious diseases at the point of care; pp. 1–3. 2016. [Google Scholar]
- 24.Au A., Moser N., Rodriguez-Manzano J., Georgiou P. 2018 IEEE international symposium on circuits and systems (ISCAS), Florence. 2018. Live demonstration: a mobile diagnostic system for rapid detection and tracking of infectious diseases; p. 1. 1. [Google Scholar]
- 25.Papadimitriou K.I., Evans D., Morgan H., Prodromakis T. 2016 IEEE biomedical circuits and systems conference (BioCAS), Shanghai. 2016. A PCB-based electronic ELISA system for rapid, portable infectious disease diagnosis; pp. 252–255. [Google Scholar]
- 26.Mei Z., Zirong Y. 2015 14th international symposium on distributed computing and applications for business engineering and science (DCABES), Guiyang. 2015. Design of epidemic monitoring platform based on ArcGIS; pp. 380–383. [Google Scholar]
- 27.Johansson B, Jain S, Montoya-Torres J, Hugan J, Yücesan E, Dibble C. Effective real-time allocation OF pandemic interventions.
- 28.Jang B., Lee M., hwi Kim M., jung Kim H., Yoo H., Kim J.W. 2019 IEEE international conference on consumer electronics (ICCE) IEEE; 2019. January. Infectious disease infection index information system; pp. 1–4. [Google Scholar]
- 29.Ren Y., Yang J., Chuah M.C., Chen Y. 2011 IEEE eighth international conference on mobile ad-Hoc and sensor systems, Valencia. 2011. Mobile phone enabled social community extraction for controlling of disease propagation in healthcare; pp. 646–651. [Google Scholar]
- 30.Guizani, Ghafoor A. 2014 international wireless communications and mobile computing conference (IWCMC), Nicosia. 2014. Modeling and evaluation of disease spread behaviors; pp. 996–1003. [Google Scholar]
- 31.Ren Y., Yang J., Chuah M.C., Chen Y. 2011 IEEE eighth international conference on mobile ad-Hoc and sensor systems, Valencia. 2011. Mobile phone enabled social community extraction for controlling of disease propagation in healthcare; pp. 646–651. [Google Scholar]
- 32.Pilavaki E., Parolo C., McKendry R., Demosthenous A. IEEE SENSORS; Orlando, FL: 2016. Wireless paper-based biosensor reader for the detection of infectious diseases at the point of care; pp. 1–3. 2016. [Google Scholar]
- 33.Amer Zayegh A., Al Bassam N. Digital systems. IntechOpen; 2018. Neural network principles and applications. [Google Scholar]
- 34.Jerew O., Al Bassam N. Delay tolerance and energy saving in wireless sensor networks with a mobile base station. Hindawi Wireless Commun Mobile Comput. 2019;2019;2019:1–12. doi: 10.1155/2019/3929876. https://downloads.hindawi.com/journals/wcmc/2019/3929876.pdf 3929876, 2019, In this issue. [DOI] [Google Scholar]
- 35.Shaik Asif Hussain, Raza Hasan, Salman Mahmood, Shaik Javeed Hussain. Design of wireless robotic system for rescue operation in hazardous environments. Int. J.Mech. Eng. Robot Res. 2020;9(2):299–304. 10.18178/ijmerr.9.2.299-304 [Google Scholar]
- 36.Hussain S.J., Khan S., Hasan R., Hussain S.A., Mallick P., Balas V., Bhoi A., Chae G.S. Cognitive Informatics and soft computing. Advances in intelligent systems and computing. Springer; 2020. Design and implementation of animal activity monitoring system using TI sensor tag. Singapore. [DOI] [Google Scholar]
- 37.Hasan R., Asif Hussain S., Azeemuddin Nizamuddin S., Mahmood S. 2018 9th IEEE control and system graduate research colloquium (ICSGRC) Shah Alam; 2018. An autonomous robot for intelligent security systems; pp. 201–206. Malaysia. [DOI] [Google Scholar]
- 38.Chernbumroong S., Atkins A.S., Yu H. 2011 5th international conference on software, knowledge information, industrial management and applications (SKIMA) proceedings. 2011. Activity classification using a single wrist-worn accelerometer; pp. 1–6. [DOI] [Google Scholar]
- 39.Li M., Rozgica V., Thatte G., Lee S., Emken A., Annavaram M., Mitra U., Spruijt-Metz D., Narayanan S. Multimodal physical activity recognition by fusing temporal and cepstral information. IEEE Trans Neural Syst Rehabil Eng. 2010 Aug;18(4):369–380. doi: 10.1109/TNSRE.2010.2053217. PMID: 20699202; PMCID: PMC4326092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cornacchia M., Ozcan K., Zheng Y., Velipasalar S. A survey on activity detection and classification using wearable sensors. IEEE Sensor J. 2017;17(2):386–403. doi: 10.1109/JSEN.2016.2628346. 15 Jan.15. [DOI] [Google Scholar]
- 41.Ding X. Wearable sensing and telehealth technology with potential applications in the coronavirus pandemic. IEEE .Rev. Biomed. Eng. 2021;14:48–70. doi: 10.1109/RBME.2020.2992838. [DOI] [PubMed] [Google Scholar]
- 42.Stojanović R., Škraba A., Lutovac B. 2020 9th mediterranean conference on embedded computing (MECO) 2020. A headset like wearable device to track COVID-19 symptoms; pp. 1–4. [DOI] [Google Scholar]