Abstract
Respiratory syncytial virus (RSV) is one of the leading causes of lower respiratory tract infections in young children. Globally, there is huge disease burden, high treatment cost, and health impact beyond acute episodes due to RSV which necessitate development and implementation of preventive strategies for the control of RSV infection. The disease burden due to RSV in pediatric population across India is still not clearly understood so this literature review was therefore conducted to gather data on disease burden due to RSV in Indian pediatric population. Systematic literature search was performed using PubMed and Google search with different medical subject headings from 2007 to 2020. Studies performed in Indian pediatric population were selected for review. Literature review revealed that in India, epidemiology of RSV infection is well documented in young children (0-5 years) as compared to children from other age groups. The rates of RSV detection in various studies conducted in younger children (0-5 years) vary from 2.1% to 62.4% in India which is higher as compared to children from other age groups. In India, RSV mainly peaks around rainy to early winter season, that is, during months of June through October while smaller peak was noted during December, January, and February. In 2020, higher RSV-associated disease burden was reported among children (<5 years) in low-income and lower-middle-income countries. Considering significant disease burden due to RSV in young Indian children, availability of RSV vaccine would be crucial to prevent RSV infections in children and its spread in the community.
Keywords: Epidemiology, India, respiratory syncytial virus
Introduction
Respiratory syncytial virus (RSV) is a common respiratory virus that infects the linings of the airways which causes cold-like symptoms (such as sneezing, coughing, and nasal discharge) in patients and is found in both cold and warm climates worldwide. The virus infects both adults and children, but children often have a more severe infection than adults. RSV infection is contagious and spreads easily either by direct contact (kissing, touching, or shaking hands) with infected person or through contact with secretions or droplets as it is carried on secretions or droplets and can live for hours on non-living objects. Upper respiratory infection with rhinorrhea and nasal congestion are major clinical characteristics of RSV infection.1,2 In developing countries, RSV reinfection rates vary between 6% and 83% every year. 2 Reinfections generally are observed to be milder. 3 Globally, acute lower respiratory infection (ALRI) is one of the leading causes of morbidity and mortality in children younger than 5 years. Human respiratory syncytial virus (hRSV) is the most common viral pathogen identified in children with ALRI. 4 In 2005, approximately, 33.8 million new episodes of RSV-associated ALRI occurred worldwide in younger children aged >5 years (22% of ALRI episodes) with at least 3.4 million episodes representing severe RSV-associated ALRI, necessitating hospital admission. Approximately, 66 000 to 199 000 younger children (>5 years) died due to RSV-associated ALRI in 2005, and 99% of these deaths occurred in developing countries. 5
RSV is a single-stranded, enveloped, ssRNA virus belonging to the Paramyxoviridae family, and genus Pneumovirus. The virus has 10 genes that result in the production of 2 separate proteins. First, RSV attachment (G) protein (envelope protein) which mediates attachment to the host cell via cell surface glycosaminoglycans and antigenic variability; second, fusion (F) protein which mediates virus entry by directing the fusion of virion envelope and the plasma membrane of the host cell. The F protein has demonstrated activation of Toll-like receptor (TLR)4, and human studies exhibit a correlation between the TLR4 receptor and susceptibility to severe RSV-induced respiratory disease.3,6 HRSV (Human Respiratory Syncytial Virus) has been divided into 2 subgroups (HRSV-A and HRSV-B) by reactivity with monoclonal antibody. Currently, HRSV-A has 10 genotypes (GA1–GA7, SAA1, NA1, NA2) whereas HRSV-B has 9 genotypes (SAB1–SAB4, GB1–GB4, BA) with BA having 11 branches (BA1-11). 7
In high-risk infants such as those with a history of prematurity, incomplete development-damage- hyperactivity of airway, males with cord blood vitamin D deficiency, bronchopulmonary dysplasia (BPD), congenital heart disease (CHD), neuromuscular impairment, immunodeficiency, and Down’s syndrome, RSV was considered as a leading cause of lower respiratory tract infection. Risk factors that have been mostly identified to be associated with severe RSV related lower respiratory tract infection include young age (below 6 months at the beginning of RSV season), low socioeconomic status and parental education, crowded living conditions, malnutrition/small for gestational age, family history of atopy or recurrent wheezing, lack of breast feeding, smoking in household, daycare attendance, longer stay in hospital. Other risk factors include viral load and isolates, escape from neutralization, reduction in fracktalkine action, low antibody titer, genetic polymorphism etc. 8 10 Clinical complications associated with progression of RSV infection include asthma, bronchiolitis, influenza, croup, bronchitis, pneumonia, neurological complications which include seizures, encephalopathy, and abnormal neurological examination.11,12
In 2020, the RSV-associated disease burden among children in 72 Gavi-eligible countries (mostly low-income and lower-middle-income) was estimated at an average of 20.8 million cases, 1.8 million hospital admissions, 40 000 deaths, 1.2 million discounted disability-adjusted life years (DALYs), and US$611 million discounted direct costs. 13 Despite huge disease burden due to RSV, high treatment cost and complications so far, the development of a RSV vaccine has lagged behind. Currently, though there are 2 therapies are approved by United States Food and Drug Administration (USFDA) which includes palivizumab for prevention and ribavirin for treatment of RSV infection; ribavirin is practically not used and at the moment there is no treatment other than supportive. 14 There is currently no drug approved for prevention and treatment of RSV infection in children in India. However, American Association of Pediatrics (AAP) and Standard treatment Guidelines by Ministry of Health & Family Welfare for Management of common Respiratory Infections in Children in India 15 recommends the use of inhaled bronchodilators (albuterol, salbutamol, nebulized epinephrine), corticosteroids, antibacterial medications (only in patients who reported comorbid bacterial infections), oral or intravenous fluids (as a supportive care to maintain proper hydration), chest therapy, and oxygen for the treatment of RSV infections. 16 The health impact of RSV infection is significant and goes beyond the acute episode phase so, there is a need for therapy that aimed at reducing the impact of RSV infection by targeting health education, information, and prophylaxis in high-risk populations. 17
However, in recent years, with the advances in understanding of RSV immunopathology and innovation in immunogen design, few RSV vaccines and monoclonal antibodies are still under development and none of the studied preparations have yet been approved. 18 According to review conducted in 2017 by University of Alberta, Canada, RSV will most likely undergo vaccine escape mutation amid any active RSV vaccination program. 4 Hence, it is important to understand the epidemiology and burden of RSV infection which will help in future for implementation of prevention strategies in India. While the data reported in previous literature review on disease burden due to RSV in Indian pediatric population are unclear. There has been a surge in studies on RSV epidemiology all over the world, including India. 2 So this narrative review presents the summary of information available on epidemiology and disease burden of RSV infection in Indian pediatric population.
Methodology
Initially the literature search was performed to establish a systematic literature review, but as sufficient data was not available on disease burden or epidemiology of RSV infection in Indian pediatric population to perform meta-analysis, this narrative review was attempted. The systematic literature search was performed using PubMed (Table 1) and Google search (Table 2)with following medical subject headings.
Table 1.
Search strategy for literature using PubMed.
| Keywords | Number of hits (PubMed) | Total no. of relevant article after analysis of individual article including duplicates |
|---|---|---|
| (((Respiratory Syncytial Virus)) OR (RSV)) AND (etiology)) AND (India) | 15 | 13 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Risk Factor)) AND (India) | 4 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Epidemiology)) AND (India) | 11 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Prevalence)) AND (India) | 11 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Incidence)) AND (India) | 11 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Disease Burden)) AND (India) | 6 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Statistics)) AND (India) | 5 | 0 |
| ((((Respiratory Syncytial Virus) OR (RSV)) AND (Morbidity)) AND (Mortality)) AND (India) | 7 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Challenges)) AND (India) | 2 | 1 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Treatment)) AND (India) | 25 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Serotypes)) AND (India) | 0 | 0 |
| ((((Respiratory Syncytial Virus)) OR (RSV)) AND (Genotypes)) AND (India) | 2 | 0 |
| (((Respiratory Syncytial Virus) OR (RSV)) AND (Diagnosis)) AND (India) | 14 | 1 |
| (((Respiratory Syncytial Virus) OR (RSV)) AND (Management)) AND (India) | 3 | 0 |
| (((Respiratory Syncytial Virus) OR (RSV)) AND (Prevention)) AND (India) | 9 | 0 |
| Total | 125 | 15 |
Table 2.
Search strategy for literature using Google (hand search).
| S no. | Keywords search | Total number of results found via hand search |
|---|---|---|
| 1 | Pneumococcal infections/diagnostic imaging; pneumococcal infections/diagnosis | 00 |
| 2 | Pneumococcal infections/classification; pneumococcal infections/epidemiology; pneumococcal infections/mortality; pneumococcal infections/etiology; fatality | 01 |
| 3 | Pneumococcal infections/physiopathology; pneumococcal infections/complications | 00 |
| 4 | Pneumococcal infections/prevention and control; pneumococcal infections/economics; pneumococcal infections/therapy; safety; immunogenicity; recommendation; guideline | 04 |
| 5 | Community acquired pneumonia; manifestation | 01 |
| 6 | community acquired pneumonia; challenges | 01 |
| Total | 07 | |
((Respiratory Syncytial Virus) OR (RSV)) AND (etiology)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Risk Factor)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Epidemiology)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Prevalence)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Incidence)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Disease Burden)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Statistics)) AND (India)
((((Respiratory Syncytial Virus) OR (RSV)) AND (Morbidity)) AND (Mortality)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Challenges)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Treatment)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Serotypes)) AND (India)
((((Respiratory Syncytial Virus)) OR (RSV)) AND (Genotypes)) AND (India)
(((Respiratory Syncytial Virus) OR (RSV)) AND (Diagnosis)) AND (India)
(((Respiratory Syncytial Virus) OR (RSV)) AND (Treatment)) AND (India)
(((Respiratory Syncytial Virus) OR (RSV)) AND (Management)) AND (India)
(((Respiratory Syncytial Virus) OR (RSV)) AND (Prevention)) AND (India)
Subject headings mentioned above provided 125 citations, out of which only 15 were qualified for the inclusion, rest of the studies were included based on manual search explained below.
A manual search for additional data was performed using references cited in the original articles as required. Other research/review papers were identified by reviewing the bibliographies of published works and by conducting general web search about the disease. The research conducted to identify the relevant research/review papers are based on the articles/studies published in last 10 to 15 years in Indian pediatric population. The review was limited to data in Indian subcontinent. Only articles published in English language were included in the review.
Search Strategy
PubMed search
Manual search
Included in this review were original prospective, randomized controlled, observational studies involving infants (<6 months), young children (<5 years) and children of less than 18 years of age reporting RSV infection incidence. Studies in adult population (⩾18 years) were excluded. Studies where investigated RSV infection was hospital acquired pneumonia and case reports, meta-analysis and commentaries were also excluded.
The distribution of studies in Indian population has been described in the Tables 3–5 based on the age wise prevalence, hospital or community, diagnostic procedures, and region (east, west, north, south, and central).
Table 3.
Age wise distribution of respiratory syncytial virus detection in India (2007-2020).
| Study | Region (East, West, North, and South, Central India) | Hospital/community based | Total sample tested | Year | Age | ||
|---|---|---|---|---|---|---|---|
| <23 months old (%) | 2-5 years old (%) | 6-18 years old (%) | |||||
| Prevalence | |||||||
| Panda et al 19 | Eastern India | Hospital | 332 | 2017 | 7 (2.1) | 8 (2.4) | - |
| Saxena et al 20 | North India | Hospital | 375 | 2019 | 103 (27.46) | - | |
| Yadav et al 21 | North India | Hospital | 130 | 2016 | 14 (10.8) | - | |
| Sahu et al 22 | Central India | Hospital | 75 | 2015 | 33 (44) | - | |
| Kini et al 23 | South India | Hospital | 383 | 2019 | 94 (24.5) | - | |
| Mishra et al 24 | Eastern India | Hospital | 300 | 2016 | 61 (20.33) | - | |
| Agrawal et al 25 | Eastern India | Hospital | 1720 | 2009 | 177 (10.29) | - | |
| Incidence | |||||||
| Samad et al 26 | India | Hospital | 68 | 2019 | 2 (2.94) | ||
| Broor et al 27 | North India | Community | 1279 | 2007 | 502/1000 child per year | 94/1000 child per year | - |
| Epidemiology | |||||||
| Yeolekar 28 | Western India | Hospital | 385 | 2008 | 100 (26) | - | |
| Bharaj et al 29 | North India | Hospital | 301 | 2009 | 61 (20.2) | - | |
| Hemalatha et al 30 | South India | Hospital | 126 | 2010 | 56 (46.66) | - | - |
| Gupta et al 31 | South India | Hospital | 77 | 2011 | 17 (22.1) | - | - |
| Choudhary et al 32 | Western India | Hospital | 843 | 2013 | 159 (18.86) | - | |
| Biswas et al 33 | Northeast India | Community | 493 | 2013 | 39 (7.9) | - | |
| Singh et al 34 | North India | Hospital | 188 | 2014 | 39 (25.16) | 1 (3) | |
| Mathew et al 35 | North India | Community | 428 | 2015 | 9 (12.9) | ||
| Saha et al 36 | North India | Hospital | 505 | 2015 | 73 (14.45) | 9 (1.78) | - |
| Saxena et al 37 | North India | Hospital | 1653 | 2017 | 199 (12) | ||
| Swamy et al 38 | Northwestern India | Hospital | 689 | 2017 | 175 (25.40) | - | |
| Broor et al 27 | North India | Community | 1279 | 2007 | 103 (8) | - | |
| Kumar et al 39 | North India | Community | 85 | 2018 | 53 (62.4) | - | - |
| Disease burden | |||||||
| Mazumdar et al 40 | East India | Hospital | 880 | 2013 | 88 (10) | ||
Table 4.
Prevalence of hRSV-A, hRSV-B, and hRSV-AB among RSV positive cases.
| Study | HRSV-A (%) | HRSV-B (%) | HRSV-AB (%) |
|---|---|---|---|
| Panda et al 19 | 0.93 | 13 | - |
| Sahu et al 22 | 76 | 24 | - |
| Mishra et al 24 | 49.18 | 50.81 | - |
| Samad et al 26 | 0 | 100 | - |
| Choudhary et al 32 | 3.44 | 15.42 | - |
| Biswas et al 33 | 100 | 0 | - |
| Singh et al 34 | 20.1 | 1.1 | - |
| Swamy et al 38 | 78.85 | 11.42 | 9.71 |
| Parveen et al 41 | 77 | 23 | - |
| Patil et al 42 | 65.30 | 34.69 | - |
| Agrawal et al 25 | 5 | 95 | - |
| Chadha et al 43 | 0 | 98-100 | - |
Table 5.
Diagnostic procedure and methods used in various studies in India.
| Study | Region (East, West, North, and South, Central India) | Total sample tested | Year | Diagnostic method | Sensitivity for RSV (%) | Specificity for RSV (%) |
|---|---|---|---|---|---|---|
| Abinaya et al 8 | South India | 33 | 2020 | Multiplex PCR | - | - |
| Panda et al 19 | Eastern India | 332 | 2017 | Multiplex PCR | - | - |
| Saxena et al 20 | North India | 375 | 2019 | rt-PCR | 90.5 50 | 99.7 50 |
| Yadav et al 21 | North India | 130 | 2016 | RT-PCR | 73% 51 | 99% 51 |
| Sahu et al 22 | Central India | 75 | 2015 | qRT-PCR | ⩾98 44 | - |
| Kini et al 23 | South India | 383 | 2019 | DFA | - | - |
| Mishra et al 24 | Eastern India | 300 | 2016 | Mono/multiplex rt-PCR | - | - |
| Agrawal et al 44 | Eastern India | 1720 | 2009 | Conventional RT-PCR | ⩾95 | - |
| Broor et al 27 | North India | 1279 | 2007 | DFA | 77.8 52 | 99.6 52 |
| Yeolekar 28 | Western India | 385 | 2008 | IFT | 90.1 53 | 98.8 53 |
| Bharaj et al 29 | North India | 301 | 2009 | Multiplex PCR | 100% | 88.9% |
| Gupta et al 31 | South India | 77 | 2011 | DFA | - | - |
| Choudhary et al 32 | Western India | 843 | 2013 | Multiplex RT-PCR | 100% | 100% |
| Biswas et al 33 | Northeast India | 493 | 2013 | RT-PCR | - | - |
| Singh et al 34 | North India | 188 | 2014 | RT-PCR | - | - |
| Mathew et al 35 | North India | 428 | 2015 | Multiplex RT-PCR | - | - |
| Saha et al 36 | North India | 505 | 2015 | rt-RT-PCR | 99.3 54 | 95.7 54 |
| Saxena et al 37 | North India | 1653 | 2017 | rt-RT-PCR | - | - |
| Swamy et al 38 | Northwestern India | 689 | 2017 | rt-RT-PCR | - | - |
| Broor et al 27 | North India | 1279 | 2007 | Virus culture | 49.5 44 | 100 44 |
| Kumar et al 39 | North India | 85 | 2018 | Immunochromatographic assay | 90 55 | 98.18 55 |
| Mazumdar et al 40 | East India | 880 | 2013 | rt-RT-PCR | - | - |
Abbreviations: DFA, direct fluorescent antibody; rt-RT-PCR, real time reverse transcriptase polymerase chain reaction; RT-PCR, reverse transcriptase polymerase chain reaction; rt-PCR, real time polymerase chain reaction; IFT, immunofluorescence test.
Results
A total of 23 hospital and community-based studies which reported RSV detection rate in India were identified through literature search from 2007 to 2020. Out of these, 13 reported epidemiology, 7 reported prevalence, 2 reported incidence rate of RSV while only 1 reported disease burden due to RSV in Indian pediatric population. None of the studies reported mortality due to RSV. Majority of the studies were conducted in north region of India (45.45%), followed by east (18.18%) and south (13.63%) while only 2 studies were from west region and 1 each from central, northwest, and northeast regions. Most studies (more than 90%) reported RSV detection rate in young Indian children (aged 0 to 5 years). The rates of RSV detection in various hospital and community-based studies vary from 2.1% to 62.4% in children aged 0 to 5 years (based on data from 23 studies) compared to 3% in children aged 6 years and above (based on only 1 study). A study conducted by Broor et al 27 reported an incidence rate of 502/1000 child per year for children aged 0 to 23 months and 94/1000 child per year for children aged 24 to 60 months. Table 3 represents age wise distribution of RSV detection in Indian children from 2007 to 2020. Overall, RSV infection is prevalent in young Indian children (⩽5 years) which indicates positive association between the young age and RSV infection. No significant gender specific differences were observed in RSV positive cases.
A prospective study conducted in children from rural India identified 22 RSV reinfections, accounting for 21% (22/103) of all RSV infections identified. The repeat infections occurred 1 to 27 months after the previous infection which indicates need of RSV vaccination as well as their management.27,37 Most of the RSV positive cases were from lower-income groups (suggestive of malnutrition) and from areas with poor sanitation, facilitating the spread of respiratory infections in the community. 44 Of the 23 studies. 12 studies reported that both hRSV-A and hRSV-B are significantly prevalent in Indian children, while only 1 study detected mixed form of RSV (hRSV-AB). Distribution of hRSV-A, hRSV-B and hRSV-AB among RSV positive cases is presented in Table 4.
The regional distribution of Indian studies reveal that 12 studies are from north region (including 1 from northeast) followed by 4 from east, 3 from south, 2 from west and 1 from central region.
Phylogenetic analysis revealed that all the 3 HRSV A strains were ON1 and all the HRSV B strains were BA9 genotype. In recent years, ON1 and different lineages of BA genotypes have been consistently reported from India and other parts of the world. It was also reported that HRSV A had more number of variable sites than HRSV B suggesting that these amino acids have a high potential for substitution resulting in genetic diversity. 5
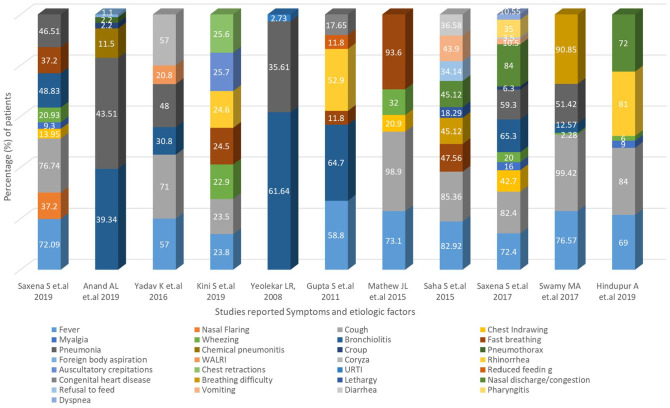
Studies conducted in Indian children reported that Reverse Transcriptase Polymerase Chain Reaction (RT-PCR), real-time Reverse Transcriptase Polymerase Chain Reaction (rt-RT-PCR), Multiplex real-time polymerase chain reaction (rt-PCR) were most frequently used in clinical setting for the detection of RSV followed by Direct Fluorescent Antibody (DFA), immunofluorescent test (IFT), immune-chromatographic assay, and virus culture. Fever, cough/coryza are the most common symptoms and bronchiolitis, pneumonia are major etiologic factors reported in children who tested positive for RSV infection followed by fast breathing/breathing difficulty, wheezing, chest-indrawing, nasal discharge/congestion, rhinorrhea, vomiting, diarrhea, and pharyngitis. Diagnostic procedures and methods used in various studies for the detection of RSV in children along with sensitivity and specificity for RSV are presented in Table 5 while symptoms/etiologic factors reported in RSV positive cases in Figure 1.
Figure 1.
Symptoms and etiologic factors reported in RSV positive cases.
WALRI, wheezing associated lower respiratory tract infection; URTI, upper respiratory tract infection; sore throat.
Two anti-RSV antibodies reported in studies conducted in Indian children were IgG and IgM. Overall, 72% to 90% of children (aged <5 years) tested positive for IgG while 36% to 44% for IgM. In a study conducted by Arankalle et al, 96% to 98% of adult population (aged 16-85 years) tested positive for IgG anti-RSV antibody. Anti-RSV antibodies were more in adult population because of prior exposure to RSV.45,46 Percentage of population reported positive for anti-RSV antibodies is presented in Table 6.
Table 6.
Percentage of patients (aged <5 years) with positive anti-RSV antibodies (serotype).
The RSV strains were classified into genotypes by phylogenetic analysis. Different genotypes of Group A (GA2, GA5, NA1 and ON1) and Group B (GB2, SAB4 and BA) have been reported in studies conducted in Indian pediatric population. BA genotype of Group B has 60 base pair (bp) duplication and ON1 genotype of Group A has 72 bp duplication in the G gene. These data may be useful for development of vaccine in India. Different genotype reported in studies conducted in Indian children are presented in Table 7.
Table 7.
Molecular epidemiological studies of respiratory syncytial virus from India.
| Study | Genotype |
|---|---|
| Parveen et al 41 | RSV-A: GA2, GA5 |
| RSV-B: BA | |
| Patil et al 42 | RSV-B: BA |
| Agrawal et al 25 | BA (BA 7, BA 9, BA 10, BA 12) |
| Raghuram et al 56 | RSV-A: NA1, ON1 |
| RSV-B: BA (BA9, BA10) | |
| Haider et al 57 | RSV-A: NA1, ON1 |
| RSV-B: GB2, BA (BA9, BA12) | |
| Haider et al 58 | RSV-A: NA1, ON1 |
| Choudhary et al 59 | RSV-B: SAB4, BA (BA9) |
| Biswas et al 33 | RSV-A: GA5, NA1 |
| Hindupur et al 47 | RSV-A: ON1 |
| RSV-B: BA9 |
Seasonality of RSV in India
In India, RSV activity begins in the rainy season (June–September) and continues to the beginning of winter (October–January) (RSV season duration 2017 = 13 weeks; 2018 = 12 weeks). 43 Most Indian studies reported a peak of RSV positive (both hRSV A and hRSVB) cases after the rainy and winter season during the months of July through November in India. A smaller peak was also noted during December, January, and February.23,24,27,47,48
Few Indian studies conducted in North India reported that RSV mainly peaks in winter (November to February) and observed some correlation with low temperature.44,49 While few studies reported negative co-relation between RSV cases with temperature and rainfall however a, positive correlation (25%-40%) was observed with cool, dry months (December–February). A mild epidemic of RSV was reported in West Bengal in October–November which did not correlate with a decrease in temperature but correlated with a drop in relative humidity and rainfall. 44
Study conducted by Hindupur et al 47 revealed that RSV positive cases correlates with mean monthly maximum temperature, mean monthly minimum temperature and average relative humidity. A study conducted by Mazumdar et al 40 in eastern region of India reported peak of RSV infection in the month of June and second peak in the month of September from 2010 to 2011. In light of these findings, a study conducted by Swamy et al 38 therefore suggested that palivizumab prophylaxis can be planned to be given to infants from post-monsoon to end of winter. 38 Data on month wise distribution of RSV infection cases in India reported in published studies is presented in Table 8.
Table 8.
Month wise distribution of RSV infection cases in India.
RSV as a Co-Infection
Six (6) studies reported RSV as co-infection along with other respiratory infections which was highly reported in children aged 0 to 5 years. Studies conducted in Indian children from various regions indicated strongest association between RSV and acute lower respiratory infections (ALRI), acute respiratory infection (ARI), upper respiratory infection (URI), lower respiratory tract infection (LRTI) and influenza.8,19,23,24,39,40,45,48,49 A study from north India reported 90% and 86% of the RSV–associated hospitalization rates in children with ARI aged <2 years and <5 years, respectively. 36 Outcome of the study conducted by Saxena et al 37 reported simultaneous diagnosis of RSV with influenza in pediatric population which shows that patients with influenza can be considered as high-risk group for RSV infection.
A prospective study conducted in children from rural India reported RSV in 8% of URIs, 7% of ALRIs, and 21% of severe ALRIs. The RSV associated ARI incident rate was highest in the first year of life while RSV associated ALRI incident rate was actually higher in the 12 to 23 months group as compared to other ages, whereas for RSV associated severe ALRI, the incident rate was slightly higher in the 0 to 11 month as compared to the 12 to 23 month group. 27 Overall, above data indicates that RSV is an important cause of ALRI, ARI, URI, LRTI, and influenza in Indian children. Studies that reported RSV as a co-infection are provided in Table 9.
Table 9.
Studies reporting RSV as a co-infection.
| Study | Region (East, West, North and South India) | Total sample tested | Year | Age | ||
|---|---|---|---|---|---|---|
| <23 months old (%) | 2-5 years old (%) | 6-18 years old (%) | ||||
| Abinaya et al 8 | South India | 33 | 2020 | 30 | 37.50 | 22.22 |
| Panda et al 19 | Eastern India | 332 | 2017 | 28.57 | ||
| Anand et al 45 | South India | 72 | 2019 | 77.78 | ||
| Kini et al 23 | South India | 383 | 2019 | 5.5 | ||
| Mishra et al 24 | Eastern India | 300 | 2016 | 31.14 | ||
| Mazumdar et al 40 | East India | 880 | 2013 | 5.90 | ||
Discussion
This article provides a review of current knowledge on disease burden due to RSV in Indian pediatric population based on published data since 2007 to 2020. We identified and included relevant studies published since 2007, from all regions of India and including different high-risk groups to provide a comprehensive picture of the RSV burden.
RSV is the most common pathogen identified in young children with acute lower respiratory infections (ALRI), primarily pneumonia and bronchiolitis. 4 In our review, the RSV (both hRSV-A and hRSV-B) detection rate was found to be significantly higher in young Indian children (aged 0-5 years old) as compared to older children (aged 6-18 years), which indicates that younger age population are more likely to have RSV infection while no significant gender specific differences were reported in RSV positive cases. RSV infection may decrease with increase in age however older age population can also be susceptible for RSV infection so they should not be neglected as a target population for the prevention of RSV infection which will help in reducing transmission in communities. The calculated incidence of RSV infection in hospitalized Indian adult patients after hematopoietic stem cell transplantation is 4% per year. 26 Similar data was reported in literature review conducted by Broor et al 49 in Indian population. Majority of RSV positive cases were reported after the rainy and winter season during the months of July through November in India while smaller peak was reported in December, January and February which was slightly similar to the data from countries in the Northern Hemisphere. 60 While minor changes were reported between different seasons from year to year globally and this variability can affect vaccination campaigns or development of vaccines. Availability of local seasonality data will help in optimization of the prevention, diagnosis, and treatment of RSV infections.
Data from this literature review reported strongest association between RSV and ALRI, ARI, URI, LRTI, and influenza which may help in identifying high risk patients who can have active immunization with a vaccine at an early stage of infection. Morbidity and mortality are greatly increased in children with bacterial co-infections or superinfections. Therefore, early detection of the virus is a critical step in the initiation of proper care, and the prevention of further spread of the virus in community. 52 It is also essential to fasten community surveillance for the identification of high-risk patient and initiate effective infection control measures, which help to reduce the length of hospital stay. RSV has emerged as a major cause of a variety of respiratory infections; there is therefore a need to have rapid, more sensitive, and highly specific diagnostic tests/methods for the detection of RSV. This literature review identified Multiplex PCR (100% sensitivity and specificity 32 and real time RT-PCR (99.3% sensitivity and 95.7% specificity 54 as the most commonly used diagnostic tests with high sensitivity and specificity for the detection of RSV infection.
Globally, higher disease burden due to RSV has kept vaccine development on high priority but development of safe and effective vaccines is still facing scientific challenges. 49 Considering significant prevalence of RSV in Indian children there is a need to provide effective interventions for the prevention of RSV which require understanding of current dynamics of maternal anti-RSV antibodies, so that necessary preventive measures can be planned and executed. Serological data in the study conducted by Arankalle et al 46 revealed that, approximately 30% of infants by the age of 3 months and almost the entire infant population by the age of 6 months is devoid of anti-RSV antibodies which indicates that children (0-6 months) need early protection with the vaccine-induced immune response. Furthermore, it is suggested that below mentioned 3 target populations would be the appropriate age groups for vaccination.
The epidemiology and burden of RSV infection suggest that there are at least 3 distinct target populations for RSV vaccines 49 :
Pregnant women to protect newborns both by transplacental transfer of antibodies and by blocking transmission
Infants (<6 months of age) who have the highest risk of severe disease
Children >6 months of age to prevent disease in them and reduce potential transmission to younger children
Neutralizing antibody titers of greater than or equal to 1:64 and greater than or equal to 1:256 for hRSV-A and hRSV-B respectively, were shown to be protective in relation to RSV-associated hospitalizations. 46 Currently, monoclonal antibodies and antiviral medications are available for the prevention and treatment of RSV infections which were reported to be expensive and thus, reserved for high risk infants, mainly in high income countries.
It has been estimated that the cost of prophylaxis with monoclonal antibodies and treatment with antivirals would be more than 10 times the actual cost of longer hospitalization in untreated patients and this magnitude is likely to be much more in India. In addition, the high-risk infants would still be at risk of succumbing to other more common viral and bacterial infections. Due to high cost of monoclonal antibodies and their transient effect, active vaccination would be most cost-effective approach for the prevention of RSV infections and their transmission to high-risk individuals which can cover a large population.61,62
RSV infections impose a significant burden among children under the age of 5 years and are among major causes of pneumonia mortality in India. 4 This necessitates the need of a RSV vaccine in India to prevent RSV infections in children and its spread in the community.
Conclusion
Data reported in various studies conducted in different regions of India revealed higher incidence rate (62.5%) and disease burden of RSV infection in younger children (aged 0-5 years) as compared to children of other age groups (6 years and older). RSV mainly peaks around rainy season to early winter season, that is, during the months of June through October. Considering a significant burden of RSV infections in young Indian children (aged 0-5 years), availability of a RSV vaccine would be crucial to prevent RSV infections in children and its spread in the community.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This literature review was funded by Pfizer Limited.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors are employees of Pfizer India.
Author Contributions: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Resources, Software, Supervision, Validation, Writing– Original Draft Preparation, Writing–Review and Editing: Canna Ghia and Gautam Rambhad.
ORCID iD: Canna Ghia  https://orcid.org/0000-0001-9839-3209
https://orcid.org/0000-0001-9839-3209
References
- 1. McIntosh NA. Pediatric Pulmonary Medicine-Respiratory Syncytial Virus (RSV). University of Michigan Health System; 2004. Last revised August, 2013. http://www.med.umich.edu/1libr/PedPulmonary/RSV.pdf [Google Scholar]
- 2. Sricharoenchai S, Palla E, Pasini FL, Sanicas M. Epidemiology of respiratory syncytial virus lower respiratory tract infection (RSV-LRTI) in children in developing countries. J Trop Dis Public Health. 2016;3:212. [Google Scholar]
- 3. Light MJ. Variability of respiratory syncytial virus seasonality and mortality. Respir Dis. 2012;2012:195-216. [Google Scholar]
- 4. Shi T, McAllister DA, O’Brien KL, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390:946-958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375:1545-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McNamara PS, Smyth RL. The pathogenesis of respiratory syncytial virus disease in childhood. Br Med Bull. 2002;61:13-28. [DOI] [PubMed] [Google Scholar]
- 7. Ohno A, Suzuki A, Lupisan S, et al. Genetic characterization of human respiratory syncytial virus detected in hospitalized children in the Philippines from 2008 to 2012. J Clin Virol. 2013;57:59-65. [DOI] [PubMed] [Google Scholar]
- 8. Abinaya S, Gaspar B, Benjamin A. A study on aetiology and outcomes of viral lower respiratory tract infections in hospitalized children from South India. Sri Lanka J Child Health. 2020;49:218-222. [Google Scholar]
- 9. Sommer C, Resch B, Simões EA. Suppl 2: risk factors for severe respiratory syncytial virus lower respiratory tract infection. Open Microbiol J. 2011;5:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watkiss ER. Pathogenesis of respiratory syncytial virus. Curr Opin Virol. 2012;2:300-305. [DOI] [PubMed] [Google Scholar]
- 11. Schweitzer JW, Justice NA. Respiratory syncytial virus infection. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 January. https://www.ncbi.nlm.nih.gov/books/NBK459215/ [PubMed]
- 12. Millichap JJ, Wainwright MS. Neurological complications of respiratory syncytial virus infection: case series and review of literature. J Child Neurol. 2009;24:1499-1503. [DOI] [PubMed] [Google Scholar]
- 13. Li X, Willem L, Antillon M, Bilcke J, Jit M, Beutels P. Health and economic burden of respiratory syncytial virus (RSV) disease and the cost-effectiveness of potential interventions against RSV among children under 5 years in 72 Gavi-eligible countries. BMC Med. 2020;18:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Verma N, Lodha R, Kabra SK. Recent advances in management of bronchiolitis. Indian Pediatr. 2013;50:939-949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Standard Treatment Guidelines. Management of Common Respiratory Infections in Children in India. Ministry of Health & Family Welfare, Government of India; 2016:31-32. [Google Scholar]
- 16. Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134:e1474-e1502. [DOI] [PubMed] [Google Scholar]
- 17. Díez-Domingo J, Pérez-Yarza EG, Melero JA, et al. Social, economic, and health impact of the respiratory syncytial virus: a systematic search. BMC Infect Dis. 2014;14:544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Griffiths C, Drews SJ, Marchant DJ. Respiratory syncytial virus: infection, detection, and new options for prevention and treatment. Clin Microbiol Rev. 2017;30:277-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Panda S, Mohakud NK, Suar M, Kumar S. Etiology, seasonality, and clinical characteristics of respiratory viruses in children with respiratory tract infections in Eastern India (Bhubaneswar, Odisha). J Med Virol. 2017;89:553-558. [DOI] [PubMed] [Google Scholar]
- 20. Saxena S, Tripathi R, Kushwaha RAS, Kumari R, Bhattacharya P, Dhole TN. Comparison of conventional and real-time PCR for monitoring of respiratory syncytial virus among pediatric patients in Northern India 2011-2014. IJPSR. 2019;10:2294-2300. [Google Scholar]
- 21. Yadav K, Ramachandran VG, Das S, Shah D. Respiratory syncytial virus–detection, prevalence and usefulness in clinical management: a hospital based study. Int J Curr Microbiol App Sci. 2016;5:86-91. [Google Scholar]
- 22. Sahu M, Kori BK, Sahare L, Barde PV. Respiratory syncytial virus in children with influenza-like illness. Indian Pediatr. 2015;52:339-340. [DOI] [PubMed] [Google Scholar]
- 23. Kini S, Kalal BS, Chandy S, Shamsundar R, Shet A. Prevalence of respiratory syncytial virus infection among children hospitalized with acute lower respiratory tract infections in Southern India. World J Clin Pediatr. 2019;8:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mishra P, Nayak L, Das RR, Dwibedi B, Singh A. Viral agents causing acute respiratory infections in children under five: a study from Eastern India. Int J Pediatr. 2016;2016:7235482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Agrawal AS, Sarkar M, Ghosh S, et al. Prevalence of respiratory syncytial virus group B genotype BA-IV strains among children with acute respiratory tract infection in Kolkata, Eastern India. J Clin Virol. 2009;45:358-361. [DOI] [PubMed] [Google Scholar]
- 26. Abdul Samad S, Dar L, Kumar L, et al. 1767. Incidence of respiratory syncytial virus infection among adults undergoing hematopoietic stem cell transplantation: a prospective study from India. InOpen Forum Infect Dis. 2019;6:S651-S651. [Google Scholar]
- 27. Broor S, Parveen S, Bharaj P, et al. A prospective three-year cohort study of the epidemiology and virology of acute respiratory infections of children in rural India. PLoS One. 2007;2:e491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yeolekar LR, Damle RG, Kamat AN, Khude MR, Simha V, Pandit AN. Respiratory viruses in acute respiratory tract infections in Western India. Indian J Pediatr. 2008;75:341. [DOI] [PubMed] [Google Scholar]
- 29. Bharaj P, Sullender WM, Kabra SK, et al. Respiratory viral infections detected by multiplex PCR among pediatric patients with lower respiratory tract infections seen at an urban hospital in Delhi from 2005 to 2007. Virol J. 2009;6:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hemalatha R, Swetha GK, Seshacharyulu M, Radhakrishna KV. Respiratory syncitial virus in children with acute respiratory infections. Indian J Pediatr. 2010;77:755-758. [DOI] [PubMed] [Google Scholar]
- 31. Gupta S, Shamsundar R, Shet A, Chawan R, Srinivasa H. Prevalence of respiratory syncytial virus infection among hospitalized children presenting with acute lower respiratory tract infections. Indian J Pediatr. 2011;78:1495-1497. [DOI] [PubMed] [Google Scholar]
- 32. Choudhary ML, Anand SP, Heydari M, et al. Development of a multiplex one step RT-PCR that detects eighteen respiratory viruses in clinical specimens and comparison with real time RT-PCR. J Virol Methods. 2013;189:15-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Biswas D, Yadav K, Borkakoty B, Mahanta J. Molecular characterization of human respiratory syncytial virus NA1 and GA5 genotypes detected in Assam in northeast India, 2009–2012. J Med Virol. 2013;85:1639-1644. [DOI] [PubMed] [Google Scholar]
- 34. Singh AK, Jain A, Jain B, et al. Viral aetiology of acute lower respiratory tract illness in hospitalised paediatric patients of a tertiary hospital: one year prospective study. Indian J Med Microbiol. 2014;32:13. [DOI] [PubMed] [Google Scholar]
- 35. Mathew JL, Singhi S, Ray P, et al. Etiology of community acquired pneumonia among children in India: prospective, cohort study. J Glob Health. 2015;5:050418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Saha S, Pandey BG, Choudekar A, et al. Evaluation of case definitions for estimation of respiratory syncytial virus associated hospitalizations among children in a rural community of Northern India. J Glob Health. 2015;5:010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Saxena S, Singh D, Zia A, et al. Clinical characterization of influenza A and human respiratory syncytial virus among patients with influenza like illness. J Med Virol. 2017;89:49-54. [DOI] [PubMed] [Google Scholar]
- 38. Swamy MA, Malhotra B, Reddy PJ, Tiwari JK, Kumar N, Gupta ML. Trends of respiratory syncytial virus sub-types in children hospitalised at a tertiary care centre in Jaipur during 2012–2014. Indian J Med Microbiol. 2017;35:134-136. [DOI] [PubMed] [Google Scholar]
- 39. Kumar S, Mehra B, Sethi GR, Saigal SR. Rapid detection of respiratory syncytial virus in community-acquired lower respiratory tract infections in children by chromatographic assay. Indian J Pathol Microbiol. 2018;61:236. [DOI] [PubMed] [Google Scholar]
- 40. Mazumdar J, Chawla-Sarkar M, Rajendran K, et al. Burden of respiratory tract infections among paediatric in and out-patient units during 2010-11. Eur Rev Med Pharmacol Sci. 2013;17:802. [PubMed] [Google Scholar]
- 41. Parveen S, Sullender WM, Fowler K, Lefkowitz EJ, Kapoor SK, Broor S. Genetic variability in the G protein gene of group A and B respiratory syncytial viruses from India. J Clin Microbiol. 2006;44:3055-3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Patil SL, Balakrishnan A. Genetic characterization respiratory syncytial virus in Kerala, the southern part of India. J Med Virol. 2017;89:2092-2097. [DOI] [PubMed] [Google Scholar]
- 43. Chadha M, Hirve S, Bancej C, et al. Human respiratory syncytial virus and influenza seasonality patterns—early findings from the WHO global respiratory syncytial virus surveillance. Influenza Other Respir Viruses. 2020;14:638-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Agrawal AS, Sarkar M, Chakrabarti S, et al. Comparative evaluation of real-time PCR and conventional RT-PCR during a 2 year surveillance for influenza and respiratory syncytial virus among children with acute respiratory infections in Kolkata, India, reveals a distinct seasonality of infection. J Med Microbiol. 2009;58:1616-1622. [DOI] [PubMed] [Google Scholar]
- 45. Anand AL, Vijayaraghavan S. Etiological factors and clinical profile of acute respiratory distress in children age group 2 months to 2 years and prevalence of respiratory syncytial virus in the study population. Int J Contemp Pediatr. 2019;6:1496-1500. [Google Scholar]
- 46. Arankalle VA, Kulkarni R, Malshe N, Palkar S, Lalwani S, Mishra AC. Seroepidemiology of respiratory syncytial virus in western India with special reference to appropriate age for infant vaccination. J Med Virol. 2019;91:1566-1570. [DOI] [PubMed] [Google Scholar]
- 47. Hindupur A, Menon T, Dhandapani P. Epidemiology of respiratory syncytial virus infections in Chennai, South India. Clin Epidemiol Glob Health. 2019;7:288-292. [Google Scholar]
- 48. Krishnan A, Kumar R, Broor S, et al. Epidemiology of viral acute lower respiratory infections in a community-based cohort of rural north Indian children. J Glob Health. 2019;9:010433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Broor S, Parveen S, Maheshwari M. Respiratory syncytial virus infections in India: epidemiology and need for vaccine. Indian J Med Microbiol. 2019;36:458-464. [DOI] [PubMed] [Google Scholar]
- 50. Zou X, Chang K, Wang Y, et al. Comparison of the Cepheid Xpert Xpress Flu/RSV assay and commercial real-time PCR for the detection of influenza A and influenza B in a prospective cohort from China. Int J Infect Dis. 2019;80:92-97. [DOI] [PubMed] [Google Scholar]
- 51. Falsey AR, Formica MA, Walsh EE. Diagnosis of respiratory syncytial virus infection: comparison of reverse transcription-PCR to viral culture and serology in adults with respiratory illness. J Clin Microbiol. 2002;40:817-820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shafik CF, Mohareb EW, Youssef FG. Comparison of direct fluorescence assay and real-time rt-PCR as diagnostics for respiratory syncytial virus in young children. J Trop Med. 2011;2011:781919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. da Silva Mesquita F, de Oliveira DB, Crema D, et al. Rapid antigen detection test for respiratory syncytial virus diagnosis as a diagnostic tool. J Pediatria (Versão em Português). 2017;93:246-252. [DOI] [PubMed] [Google Scholar]
- 54. Kuypers J, Wright N, Morrow R. Evaluation of quantitative and type-specific real-time RT-PCR assays for detection of respiratory syncytial virus in respiratory specimens from children. J Clin Virol. 2004;31:123-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Thuy Tien TT, Park H, Tuong HT, Yu ST, Choi DY, Yeo SJ. Development of a rapid fluorescent immunochromatographic test to detect respiratory syncytial virus. Int J Mol Sci. 2018;19:3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Raghuram SV, Khan WH, Deeba F, et al. Retrospective phylogenetic analysis of circulating BA genotype of human respiratory syncytial virus with 60 bp duplication from New Delhi, India during 2007-2010. Virus Dis. 2015;26:276-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Haider MS, Khan WH, Deeba F, et al. BA9 lineage of respiratory syncytial virus from across the globe and its evolutionary dynamics. PLoS One. 2018;13:e0193525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Haider MS, Deeba F, Khan WH, et al. Global distribution of NA1 genotype of respiratory syncytial virus and its evolutionary dynamics assessed from the past 11 years. Infect Genet Evol. 2018;60:140-150. [DOI] [PubMed] [Google Scholar]
- 59. Choudhary ML, Wadhwa BS, Jadhav SM, Chadha MS. Complete genome sequences of two human respiratory syncytial virus genotype A strains from India, RSV-A/NIV1114046/11 and RSV-A/NIV1114073/11. Genome Announc. 2013;1:pii, e00165-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Obando-Pacheco P, Justicia-Grande AJ, Rivero-Calle I, et al. Respiratory syncytial virus seasonality: a global overview. J Infect Dis. 2018;217:1356-1364. [DOI] [PubMed] [Google Scholar]
- 61. Gupta D, Gupta P. Palivizumab. Indian Pediatr. 2001;38:1265-1269. [PubMed] [Google Scholar]
- 62. Mammas IN, Drysdale SB, Rath B, et al. Update on current views and advances on RSV infection. Int J Mol Med. 2020;46:509-520. [DOI] [PMC free article] [PubMed] [Google Scholar]