Background:
Concerns regarding infection, extrusion, and pain have traditionally precluded the use of mesh to treat severe rectus diastasis during abdominoplasty in the United States. We describe a mesh abdominoplasty technique, and we hypothesize that the complication rate using mesh is greater than the complication rate of suture plication.
Methods:
Inclusion criteria for mesh abdominoplasty were patients who (1) had retrorectus planar mesh for repair of rectus diastasis, (2) did not have concurrent ventral hernia, and (3) underwent skin tailoring. Patients who underwent rectus plication with suture, and met criteria 2 and 3 above were included in a sample of consecutive standard abdominoplasty patients. The primary endpoint was surgical site occurrence at any time after surgery, as determined with review of their office and hospital medical records. Secondary endpoints included surgical site infection, revision rates, postoperative course, and aesthetics assessed with their last set of office photographs.
Results:
Surgical site occurrence rate was 0% of the 40 patients in the mesh group and 19% of the 37 patients in the standard group (P = 0.005); rates of soft-tissue revision were 23% in the mesh group and 27% in the standard group (P = 0.84). As to aesthetics, the mesh abdominoplasty patients had mean statistically lower preoperative scores in comparison with the standard plication group (65.8 ± 11.6 versus 70.3 ± 11.4, P = 0.0013). The mesh group had a statistical improvement to 75.9 ± 12.6 (P < 0.0001), whereas the standard plication group improved to 82.5 ± 11.4 (P < 0.0001).
Conclusions:
Retrorectus mesh placement in a cohort of patients with severe rectus diastasis had a complication rate lower than that seen in a cohort of patients with less severe rectus diastasis, therefore negating our original hypothesis. This was done without compromising aesthetic improvement.
INTRODUCTION
The majority of patients with rectus diastasis are treated with suture plication of the anterior rectus sheath, and this technique tightens the abdominal wall with low recurrence rates.1 However, for severe rectus diastasis with a lack of tone of the anterior abdominal wall, the risk of recurrence and suture pull-through is high due to the excessive forces placed by the sutures, onto an already weakened abdominal wall fascia. Inadequate plication of rectus diastasis and/or recurrent rectus diastasis are implicated as two of the leading indications for secondary abdominoplasty.2,3 Rates of rectus diastasis re-occurrence have been quoted between 40% and 100% in certain patient populations.4,5 Thus, there is a clinical need and a gap in our current knowledge in how best to achieve a reliable surgical procedure for severe rectus diastasis. Reported techniques include plication of the posterior rectus sheath, additional rows of sutures, and even advancement/reefing of the external oblique insertion onto the rectus muscles.6,7 These procedures still rely on the simple suture—an implant designed over 3000 years ago, to maintain tissues under tension in apposition. General surgeons regard the use of mesh as the standard of care for their abdominal wall hernia repairs, raising the question if the surgical principles of force distribution and elimination of suture pull-through with the aid of a mesh should be considered for the so-called floppy abdomen. The macroporous mesh produces a magnified foreign body response at the repair due to the fibrovascular ingrowth and microencapsulation of the polypropylene filaments, and thus minimizes tension and risk of suture pull-through in high-tension internal closures.
Although mesh support in ventral hernia repair is widely accepted as the standard of care over simple suture repair, concerns in the United States regarding mesh for a cosmetic procedure exist to the point that highly regarded abdominoplasty surgeons do not even mention the use of mesh in their writings.1 These concerns could include the surgical difficulty for implantation, infection, extrusion, pain, cost, and potential need for mesh removal. Despite the general hesitation to use mesh for any of the proceeding reasons, the use of prosthetic mesh in abdominoplasty to treat severe musculoaponeurotic laxity was described in 18 patients as early as 1995.8 More recently, plastic surgeons have reported mesh treatment of ventral hernias larger than 3 cm, mesh reinforcement of posterior rectus fascia plication in multiparous women with severe myoaponeurotic laxity without hernia, and posterior polypropylene mesh reinforcement—all at the time of abdominoplasty.9–12 The senior author has published a preliminary report describing the use of a narrow well-fixed prosthetic mesh, which achieved an acceptable 6% surgical site occurrence rate and no clinical recurrences in 32 patients, with 471 days of average follow-up treated for severe female- and male-pattern rectus diastasis and moderate-to-large ventral hernias at the time of abdominoplasty.13
To improve the understanding on the use of mesh for rectus diastasis, we performed a single surgeon retrospective cohort study. We hypothesize that prosthetic mesh support of severe rectus diastasis during abdominoplasty will have a higher complication rate (SSO) than suture-only plication due to the increased surgical dissection and opening of new tissue planes to achieve a retrorectus mesh implantation. In this study, we describe the senior author’s mesh abdominoplasty technique, which uses a combination of a narrow well-fixed mesh to narrow the distance between the semilunar lines, as well as mesh strips for the midline closure to correct severe rectus diastasis during abdominoplasty. We present two case examples that illustrate the benefits of this procedure. Second, we compare postoperative complications, follow-up events, and aesthetic outcomes between the series of patients undergoing mesh abdominoplasty and a sample of consecutive, standard abdominoplasty patients who were operated on by the senior author.
METHODS
A chart review of all female patients undergoing abdominal wall surgery with mesh between 2007 and 2018 performed by the senior author (GD) was conducted for this retrospective cohort study. Inclusion criteria for mesh abdominoplasty were female patients who (1) had retrorectus planar mesh placed for repair of rectus diastasis, (2) did not have a sizable ventral hernia requiring intraabdominal dissection, and (3) had skin tailoring as part of the procedure. A chart review of all patients undergoing standard abdominoplasty by the senior author between 2014 and the present was also conducted to identify a convenience sample of consecutive standard abdominoplasty patients who underwent rectus plication with suture. Patients all paid out of pocket for these procedures.
The identified patients’ charts were analyzed for patients’ demographics, clinical characteristics, and for postoperative outcomes. Extracted clinical characteristics were history of smoking or diabetes, body mass index (BMI), presence and amount of muscle resection, and width of rectus diastasis. The primary endpoint was surgical site occurrence (SSO) at any time after surgery. We defined SSO by the Ventral Hernia Working Group definition of an infection, a wound dehiscence, a seroma, or the development of an enterocutaneous fistula.14 Surgical site infection is a component of SSO, but it is also reported independently for clarity as a secondary endpoint. Additional secondary endpoints included follow-up time defined as number of weeks between surgery and until the last documented clinic visit, the number of follow-up visits in the first 6 months was extracted as a proxy for patient satisfaction and complications, the number of revisions performed in the office, and aesthetics. Aesthetic outcomes were measured using a professional aesthetic scale for the abdomen.15 This scale includes 11 questions in five domains—abdominal wall shape, skin, umbilicus, abdominal muscle lines, and scar. Scores range from 32 to 100, with a higher score indicating a better aesthetic outcome. Two attending-level plastic surgeons and two medical students independently rated pre and postoperative photographs of all included patients, with standardized photographs available in their clinical chart. The four reviewers were blinded to the surgery performed. For each rater, mean preoperative mesh abdominoplasty, mean preoperative standard abdominoplasty, mean postoperative mesh abdominoplasty, and mean postoperative standard abdominoplasty scores were calculated. Inter-rater reliability was calculated with the Pearson correlation coefficient. This study was approved by the Northwestern University Institutional Review Board.
PATIENT EVALUATION
A thorough history from the patient is obtained regarding the abdominal wall, including the number of prior pregnancies, the size of each baby, and any surgical procedures, including Cesarian sections and prior umbilical hernia repairs. Patients are evaluated for the tone of the abdominal wall clinically by simple palpable standing and lying down. Routine measurements of height and weight are recorded for calculation of BMI. The patient is requested to perform a “reversed sit-up” maneuver. The abdominal wall of the patients is palpated while she places her hands behind her head, and transitions from a sitting to a lying position. During the downward phase of this sit-up, a measurement of rectus diastasis can be made. An assessment is made if the abdominal wall tone is poor due to a focal widening between two strong rectus abdominis muscles, or if there is a generalized widening of the tissues between the semilunar lines.
Inclusion criteria for both operations included women who are good surgical candidates, are done having children, and who desire cosmetic improvement of their abdominal wall. Inclusion criteria also include the provision of informed consent for abdominoplasty as explained by the senior author based on his experience of hernia closures. Patients with significant abdominal wall laxity are also consented for the use of polypropylene mesh based on the senior author’s experience. All patients are told that they can have severe complications, including chronic pain, deep vein thrombosis, pulmonary emboli, and death. Exclusion criteria include BMI more than 40, poor cardiac or pulmonary status that would prevent walking up several flights of stairs, or the inability to lie flat, bleeding disorders, and smoking.
PREOPERATIVE DECISION-MAKING
The narrower the rectus diastasis (<4–5 cm gap clinically) and the better the firmness or quality of the rectus muscles to palpation, the more that sutures were used for abdominal wall tightening. Patients with either generalized laxity between the semilunar lines or severe widening of the linea alba >5 cm receive mesh as a component of their surgery. Another relative indication for the use of mesh is for high-demand women who need a solid reconstruction for their work or leisure activities. Several of the mesh abdominoplasty patients were thin physical therapists who were no longer able to use their core muscles for patient care due to a loss of abdominal wall tone.
Hospital costs are based on time in the operating room, and not on the technique chosen. The patients are not required to pay an additional charge for mesh, and so this did not factor into decision-making. However, the added 2-day hospital stay for pain control was an additional cost for the patient.
SURGICAL TECHNIQUE
Skin
The majority of women in this study had low transverse incisions for their abdominoplasties. Skin is elevated to expose the abdominal wall widely, including and past the semilunar lines. The medial border of the rectus muscles is incised to develop the retrorectus space for the length of the abdominal wall from xyphoid to pubis. The skin is elevated widely enough so that it redrapes flat at the end of the procedure, even after repair of the rectus diastasis. A minority of patients (6) had vertical skin incisions for their procedures. These patients were for redo procedures, surgeries involving the removal of old mesh, and the patients with the most lax abdominal walls. For vertical incisions, an umbilicus is created using “pumpkin-teeth” flaps, and a short suprapubic transverse incision is typically required to prevent a dog-ear.16
Abdominal Wall
Suture plication of rectus diastasis is performed with a double stranded 0-nylon suture. Bites of the anterior rectus fascia are taken every 5–8 mm, running from the xyphoid to the umbilicus, and from the umbilicus to the symphysis pubis. Care is taken not to overtighten the hypogastrium. The patient is sat up repeatedly during the tightening process to assess abdominal wall tension.
For mesh abdominoplasty, after skin elevation the anterior sheath is opened on its medial border to expose the rectus muscle. The muscle is freed from the underlying posterior rectus sheath with blunt dissection, until the lateral border of the rectus is identified. The width of the rectus diastasis can be measured at this point in the procedure. A midweight, macroporous polypropylene uncoated mesh (Soft Prolene, Ethicon, New Brunswick, N.J.) 10–11 cm in transverse dimension is placed in the retrorectus plane as an underlay and secured every 2–3 cm with interrupted trans-rectus 0-polypropylene sutures that pass through the anterior rectus fascia and muscle near the semilunar lines, grab a small element of the mesh as a “U” bite, and then return back through the muscle and anterior rectus fascia (Fig. 1). The prior skin elevation allows for placement of these sutures under direct vision. Polydiaxanone sutures can be used in thin patients to avoid knot palpability. The sutures are snapped long and are tied later to facilitate visualization and avoidance of the inferior epigastric artery and intercostal nerves.
Fig. 1.
Illustrations of coronal and anteroposterior views showing width of mesh, retrorectus placement, and approximate locations of interrupted trans-rectus sutures to secure mesh.
Mesh width, rectus muscle width, and suture placement is critical to narrow the rectus complex for a more aesthetic outcome. The goal is the creation of a 6-cm wide rectus muscle at the level of the umbilicus. The sutures angle a bit as per Figure 1, and so half of the mesh (about 5.5 cm) underlies the left rectus, and half (about 5.5 cm) underlies the right rectus muscle. The tension on the tied sutures narrows the rectus muscles and corrects the rectus diastasis at the same time. The mesh is cut and narrowed about 1–2 cm in the upper and lower abdomen to conform with the normal shape of the female rectus muscle, again as per Figure 1. For extremely wide rectus muscles, the medial several centimeters can be excised, but with experience over time, the senior author now routinely bunches as opposed to excises the medial muscle. Excess mesh is trimmed to avoid bunching and wrinkling. A hole is cut in the mesh for the umbilical stalk to emerge. Maintenance of the branches of the inferior epigastric artery to the umbilical stalk is possible with this technique to decrease the chance of umbilical necrosis. The posterior sheath and linea alba now remain posterior to the mesh and are not imbricated or otherwise manipulated. The anterior rectus sheath is closed over the mesh to create a direct supported repair with a running strip of polypropylene mesh 2-cm wide that is cut from the same piece of mesh used earlier. No mesh is exposed to the skin flap, and all of the mesh is covered by the abdominal wall muscles. Figure 2 displays an intraoperative photograph of the rectus muscles after placement and suturing of the retrorectus mesh.
Fig. 2.
Intraoperative photograph of mesh abdominoplasty patient. Photograph highlights author’s technique of tacking the anterior rectus sheath to the retrorectus mesh to accentuate the central midline depression.
Two drains are used for all patients, and removed when the drainage is less than 30 cm3 from each. Drains typically come out within 1 week. No quilting sutures are used, though the umbilicus recreation with local flaps serves to act as a strong quilting element. The majority of patients received postoperative prophylactic anticoagulation for 2 weeks.
SAMPLE SIZE DETERMINATION AND STATISTICS
A power analysis revealed that with 40 patients in each group, and with a baseline rate of complications of 15% for complications with suture plication,1 the mesh group would need to have a four-fold increased level of complications of 60% for an 80% power and with a statistical significance of 0.05 of showing inferiority. Welch T-test was used to compare inpatient hospital stay and follow-up visits in the first 6 months, between the mesh and standard groups. Chi-squared test of independence and Fischer exact test were used to compare SSI, SSO, muscle revision, and soft tissue revision, between mesh and standard groups. Statistical analysis was performed using R Studio and GraphPad software.
RESULTS
Case Examples
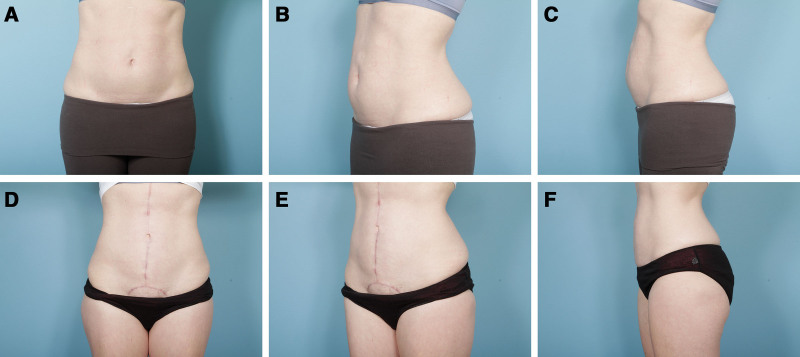
A 39-year-old woman with BMI 26 underwent mesh abdominoplasty with a retrorectus mesh. Three centimeters of muscle was resected from each side, and her rectus diastasis measured 6 cm intraoperatively. Thus, her operation corrected 12 cm of rectus complex pathology. She remained inpatient for 1 day and returned to the office three times in the first 6 months. Over 52 weeks of follow-up, she had no complications, and did not require any postoperative revision. Figure 3 displays her pre and postoperative photographs. Figure 4 demonstrates the pre and postoperative results of a female mesh abdominoplasty patient who had a vertical skin incision due to the requirement to remove a previously placed painful umbilical hernia mesh at the time of her abdominoplasty. The images are 10 months after her procedure.
Fig. 3.
Patient example: Preoperative (A–C) and 12-month postoperative (D–F) photographs of mesh abdominoplasty patient.
Fig. 4.
Patient example: Preoperative (A–C) and 10-month postoperative (D–F) photographs of a mesh abdominoplasty patient with a vertical skin incision. Vertical skin incision was indicated in this patient because she underwent removal of painful umbilical mesh at the time of her abdominoplasty procedures.
Outcomes
A total of 40 mesh abdominoplasty and 37 standard abdominoplasty female patients were identified. The baseline demographic and clinical characteristics of both groups are shown in Table 1. Six mesh abdominoplasty patients received a vertical skin incision, whereas the remaining mesh abdominoplasties and all of the standard abdominoplasties involved a low transverse incision. Of the 40 mesh abdominoplasty patients, the width of rectus diastasis was reported for 28 patients and averaged 7 cm (range 4–15 cm). In the standard abdominoplasty group, width was reported for seven of the 37 patients and averaged 4 cm (range 2–6 cm).
Table 1.
Demographic and Clinical Characteristics of Mesh Abdominoplasty and Standard Abdominoplasty Patients
| Demographic Characteristics | |||
|---|---|---|---|
| Mesh Abdominoplasty (n = 40) |
Standard Abdominoplasty (n = 37) |
||
| Age (mean, range) | 42 (29–70) | 43 (27–65) | |
| Clinical Characteristics | |||
| Mesh Abdominoplasty (n = 40) |
Standard Abdominoplasty (n = 37) |
||
| BMI (kg/m2) (mean, range, SD) | 26 (18–40) (5.3) | 25 (19–27) (4.7) | Welch t test, 2-sided: P = 0.38 |
| Smoking status | |||
| Current (n, %) | 0 (0%) | 0 (0%) | |
| Former (n, %) | 0 (1%) | 1 (3%) | |
| Never (n, %) | 40 (95%) | 36 (97%) | |
| Diabetes | |||
| Yes (n, %) | 0 (4%) | 1 (3%) | |
| No (n, %) | 40 (96%) | 36 (97%) | |
| Concomitant hernia (patients) (n) | 7 | ||
| Epigastric | 9 | 4 | |
| Umbilical | 13 | 3 | |
| Incisional | 1 | 0 | |
| Width of rectus diastasis (cm) (mean, range) | 7 (4–15) | 4 (2–6) | |
| Muscle resection | |||
| No. patients (n) | 16 | 0 | |
| Amount resected (average, range) | 3.8 (2–8) | NA | |
Table 2 reports a comparison of postoperative outcomes assessed with office and hospital electronic medical chart review. Mean follow-up time was 45 weeks for the mesh abdominoplasty (range 4–175) group and 51.8 weeks for the standard abdominoplasty group (range 4–520). Regarding outcomes, mean postoperative inpatient stay for the mesh abdominoplasty group was 2 days versus 0 days for the standard group (P = 1.797 × 10−14). SSI rate was 3% in the mesh group (one superficial stitch abscess) and 0% in the standard group (P = 1); SSO rate was 0% in the mesh group and 19% in the standard group (P = 0.005), including multiple seromas and two hematomas. One patient in the mesh abdominoplasty group had a return to the operating room for additional muscle tightening. The rates of soft-tissue revision as an office procedure were 23% in the mesh group and 27% in the standard group (P = 0.84). These were at the patient’s request, typically for dog-ears at the end of the incision or touch-up liposuction of the lower abdomen. No patient in either group required hospital re-admission. Mean number of follow-up visits in first 6 months were not significantly different between the two groups (P = 0.3619).
Table 2.
Follow-up and Postoperative Outcomes of Mesh Abdominoplasty and Standard Abdominoplasty Patients
| Mesh Abdominoplasty (n = 40) |
Standard Abdominoplasty (n = 37) |
Welch T-Test, 2-sided | |
|---|---|---|---|
| Follow-up visits in the first 6 months (mean, range) | 3 (1–7) | 2 (1–7) | P = 0.3619, CI −0.86 to −0.32 |
| Hospital stay (d) (mean, range) |
2 (0–6) | 0 (0–3) | P = 1.797 × 10−14, CI 1.32–2.03 |
| Fischer exact test/Chi-squared test | |||
| SSI (n, %) | 1 (3%) | 0 (0%) | 95% CI 0.02–Inf, P = 1 |
| SSO (n, %) | 0 (0%) | 7 (19%) | 95% CI 0–0.59, P = 0.005 |
| Other complications | Superficial suture abscess–1 | Hematoma–2 | NA |
| Hospital readmission (n, %) | 0 (0%) | 0 (0%) | NA |
| Muscle revision (n, %) | 1 (3%) | 0 (0%) | 95% CI 0.02–inf, P = 1 |
| Office soft tissue revision (n, %) | 9 (23%) | 10 (27%) | Xsq 0.04, P = 0.84 |
Standardized preoperative clinic photographs were available for 36 of the 40 mesh abdominoplasty patients and for 33 of the 37 standard abdominoplasty patients. Standardized postoperative clinic photographs were available for 30 of the 40 mesh and 22 of the 37 standard abdominoplasty patients. When rated by four independent raters blinded to the treatment (two attending plastic surgeons, two medical students), the mesh abdominoplasty patients had mean statistically lower preoperative scores in comparison with the standard plication group (65.8 ± 11.6 versus 70.3 ± 11.4, P = 0.0013). The mesh group had a statistical improvement to 75.9 ± 12.6 (P < 0.0001), whereas the standard plication group improved to 82.5 ± 11.4 (P < 0.0001).
DISCUSSION
The results for these patients not only negated the original hypothesis that mesh is associated with higher complications than sutures, but were actually in the opposite direction of the original hypothesis. Mesh abdominoplasty patients had a lower SSO than suture plication patients. We theorize that the retrorectus mesh acts as a sturdy platform upon which the soft tissues can heal. SSI, muscle revision, and soft-tissue revision rates were comparable to standard abdominoplasty patients in the senior author’s practice, despite the additional opening of tissue planes performed in the mesh patients.
Rectus muscles widened by pregnancy are handled in dramatically different ways in standard abdominoplasty and mesh abdominoplasty. For standard suture abdominoplasties, not only is the linea alba invaginated towards the peritoneal cavity, but for additional tightening the rectus muscle itself is plicated with additional rows of sutures, causing an internal folding and a turning of the orientation of the rectus muscles by 90 degrees. This deepens the position of the umbilicus, making it more difficult to exteriorize. In comparison, for a mesh abdominoplasty, the sutures and mesh provide a mechanism to narrow the rectus muscles. The repair distributes forces between numerous transfascial sutures that, along with the mesh, close down the rectus diastasis and narrow the rectus muscles to an aesthetic width.
There were comparable aesthetic outcomes between mesh and standard abdominoplasty patients, as demonstrated by mean scores on a professional aesthetic scale for the abdomen. Mesh abdominoplasty patients present with wider rectus diastasis at baseline, which may correlate with greater abdominal protuberance and poorer preoperative aesthetics. In our sample, preoperative aesthetic scale scores were lower in the mesh abdominoplasty group than in the standard abdominoplasty group. While postoperative aesthetic scores were higher in the standard than in the mesh abdominoplasty group, we believe that the lower preoperative aesthetic score in the mesh abdominoplasty group contributes to this numeric discrepancy. The vertical scars in six mesh abdominoplasty patients also brought down the overall scores for this group. Indeed, the delta between pre and postoperative was comparable in both groups, indicating that the mesh abdominoplasty procedure leads to a similar aesthetic improvement as a standard abdominoplasty.
Is mesh truly required for high-tension internal closures such as for these patients with marked widening between the medial borders of the rectus muscles, or for widened rectus muscles? It is clearly established that abdominal wall repairs with mesh are more durable than abdominal wall repairs with sutures17 The senior author uses a nearly identical abdominal wall closure technique with mesh for his incisional hernia repairs, and has reported a zero failure rate at a full two years of follow-up in 100 patients.18 Opponents of mesh point to cost, complications, and the concept that the altered compliance of the postpartum female abdominal wall negates the need for mesh.
Our results add to the existing body of published work on mesh treatment of myoaponeurotic laxity during abdominoplasty. Prado and colleagues’ case series of 20 patients included four patients treated with midline mesh for rectus diastasis and showed no seroma, infection, or flap necrosis over a mean 24 months of follow-up.4 Caldeira and colleagues previously described submuscular mesh in 14 (seven primary and seven revision) abdominoplasty patients to treat unsatisfactory bulging or to reinforce the rectus plication.8 They reported a complication profile of one umbilical fistula and two patients with chronic postoperative pain. Although we did not include a standardized measure of postoperative pain, no patients in our sample had chronic pain or nerve pain. Emanuelsson in an RCT concluded that mesh has no advantages over a double row of suture plication,19 but the degree or severity of rectus diastasis seemed less than in our study, where only the most severe cases of abdominal wall laxity were treated with mesh.
Limitations for the study include its retrospective nature, a nonblinded observer performing the follow-up and categorization of complications, no functional outcomes for core strength for the groups, and the lack of long-term follow-up using ultrasound or other radiologic tests for recurrence of rectus diastasis. The single surgeon design is both a strength and a weakness of this article. Many of these patients received strips of polypropylene mesh as sutures for their midline,20 and surgeons may not be familiar with this technique. However, single-surgeon studies remove many confounding issues as to surgeon ability, handling of tissues, and decision-making. The aesthetic outcomes determined for both groups are a unique contribution of this article.
We conclude that the use of mesh for cosmetic abdominoplasty can be performed with a complication rate the same or lower than suture plication, even for patients with severe rectus diastasis and abdominal wall laxity. Mesh does not “cause” surgical complications so long as a technique is chosen to implant the mesh safely and appropriately. This is despite the opening of additional tissue planes and increased foreign material. The improvement in assessed cosmetic outcomes for these patients with severe abdominal wall laxity is similar to that achieved in more localized widening of the linea alba. Future studies are planned to repeat this protocol prospectively and with ultrasound measurements of the widths of the linea alba and rectus muscles to better establish the algorithm of who should receive mesh, and for whom sutures alone will suffice.
Footnotes
Published online 4 August 2021.
Disclosure: Dr. Dumanian is a consultant for Checkpoint Surgical, and the founder of Advanced Suture, Inc and Mesh Suture, Inc. All the other authors have no financial interest in relation to the content of this article. No funding was received for this article.
REFERENCES
- 1.ElHawary H, Abdelhamid K, Meng F, et al. A comprehensive, evidence-based literature review of the surgical treatment of rectus diastasis. Plast Reconstr Surg. 2020;146:1151–1164. [DOI] [PubMed] [Google Scholar]
- 2.Matarasso A, Schneider LF, Barr J. The incidence and management of secondary abdominoplasty and secondary abdominal contour surgery. Plast Reconstr Surg. 2014;133:40–50. [DOI] [PubMed] [Google Scholar]
- 3.Cormenzana PS, Samprón NM, Escudero-Nafs FJ. Secondary abdominoplasty. Aesthetic Plast Surg. 2008;32:503–508. [DOI] [PubMed] [Google Scholar]
- 4.al-Qattan MM. Abdominoplasty in multiparous women with severe musculoaponeurotic laxity. Br J Plast Surg. 1997;50:450–455. [DOI] [PubMed] [Google Scholar]
- 5.van Uchelen JH, Kon M, Werker PM. The long-term durability of plication of the anterior rectus sheath assessed by ultrasonography. Plast Reconstr Surg. 2001;107:1578–1584. [DOI] [PubMed] [Google Scholar]
- 6.Mommers EHH, Ponten JEH, Al Omar AK, et al. The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017;31:4934–4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prado A, Andrades PR, Benitez S. Abdominoplasty: the use of polypropylene mesh to correct myoaponeurotic-layer deformity. Aesthetic Plast Surg. 2004;28:144–147. [DOI] [PubMed] [Google Scholar]
- 8.Marques A, Brenda E, Pereira MD, et al. Plicature of abdominoplasties with Marlex mesh. Ann Plast Surg. 1995;34:117–122. [DOI] [PubMed] [Google Scholar]
- 9.Sakr M, Habib M, Hamed H, Kholosy H. Outcome of combining ventral hernia repair with abdominoplasty or mesh-abdominoplasty in multiparous women. Glob J Surg. 2019;7:5–11. [Google Scholar]
- 10.Batchvarova Z, Leymarie N, Lepage C, et al. Use of a submuscular resorbable mesh for correction of severe postpregnancy musculoaponeurotic laxity: an 11-year retrospective study. Plast Reconstr Surg. 2008;121:1240–1248. [DOI] [PubMed] [Google Scholar]
- 11.Caldeira AML, Carrión K, Jaulis J. Repair of the severe muscle aponeurotic abdominal laxity with alloplastic mesh in aesthetic abdominoplasty. Aesthetic Plast Surg. 2018;42:1039–1049. [DOI] [PubMed] [Google Scholar]
- 12.Emanuelsson P, Gunnarsson U, Strigård K, et al. Early complications, pain, and quality of life after reconstructive surgery for abdominal rectus muscle diastasis: a 3-month follow-up. J Plast Reconstr Aesthet Surg. 2014;67:1082–1088. [DOI] [PubMed] [Google Scholar]
- 13.Cheesborough JE, Dumanian GA. Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg. 2015;135:268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breuing K, Butler CE, Ferzoco S, et al. Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery. 2010;148:544–558. [DOI] [PubMed] [Google Scholar]
- 15.Sood R, Muhammad LN, Sasson DC, et al. Development and initial validation of a novel professional aesthetic scale for the female abdomen. Plast Reconstr Surg (accepted). [DOI] [PubMed] [Google Scholar]
- 16.Purnell CA, Turin SY, Dumanian GA. Umbilicus reconstruction with bilateral square “Pumpkin-Teeth” advancement flaps. Plast Reconstr Surg. 2018;141:186–189. [DOI] [PubMed] [Google Scholar]
- 17.Luijendijk RW, Hop WC, van den Tol MP, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343:392–398. [DOI] [PubMed] [Google Scholar]
- 18.Lanier ST, Fligor JE, Miller KR, et al. Reliable complex abdominal wall hernia repairs with a narrow, well-fixed retrorectus polypropylene mesh: a review of over 100 consecutive cases. Surgery. 2016;160:1508–1516. [DOI] [PubMed] [Google Scholar]
- 19.Swedenhammar E, Strigård K, Emanuelsson P, et al. Long-term follow-up after surgical repair of abdominal rectus diastasis: a prospective randomized study [Epub ahead of print]. Scand J Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lanier ST, Dumanian GA, Jordan SW, et al. Mesh sutured repairs of abdominal wall defects. Plast Reconstr Surg Glob Open 2016;28:e1060. v [DOI] [PMC free article] [PubMed] [Google Scholar]