Abstract
Molar-Incisor Hypomineralization (MIH) is a qualitative defect of enamel of unknown etiology, affecting one or more permanent molars and may include incisors. This condition is a clinical challenge and its prevalence is still uncertain given the recent increase in research. Thus, we aimed to comprehensively estimate the overall prevalence of MIH and associated characteristics. This systematic review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). We searched articles using PubMed, MEDLINE, CENTRAL, Web of Science, SciELO, LILACS and TRIP databases, until July 2021. Heterogeneity and publication bias were computed via I2 test statistics and Egger’s significance test, respectively. Random-effects meta-analysis of prevalence were processed. We used the Strength of Recommendation Taxonomy [SORT] to grading the strength of evidence. Overall, 116 observational studies were included, with one study with moderate methodological quality and the remaining of high methodological quality. Subgroup analysis confirmed an influence of not using the 2003 MIH case definition (p = 0.0066). The pooled prevalence of MIH was 13.5% (95% CI 12.0–15.1, I2 = 98.0%). Affected incisors were seen in 36.6% (95% CI 30.0–43.7, I2 = 92.5%) of the cases. Lastly, the prevalence of hypomineralization of the second primary molars was observed in 3.6% of the MIH cases (95% CI 1.9–6.8, I2 = 96.3%). America was the continent with highest prevalence (15.3, 95% CI 12.8–18.3, p < 0.001, I2 = 96.3%) and Asia had the lowest prevalence (10.7, 95% CI 8.5–13.5, p < 0.001, I2 = 98.7%), however no continental differences were found. Sample size and year of publication were slight contributing factors to the heterogeneity in the analysis. Overall, these results were classified with a SORT A recommendation.
Subject terms: Oral diseases, Diseases, Health care, Medical research, Oral manifestations
Introduction
Molar-Incisor Hypomineralization (MIH) is designated as a qualitative defect of unknown etiology in the enamel development1,2. Since 2003, the European Academy of Pediatric Dentistry (EAPD) has proposed its first nomenclature to define a pathology of unknown etiology that affects one or more permanent molars and may include permanent incisors1.
As a potential oral public health concern, the prevalence of MIH became imperative to determine as a measure of interest in oral health programs. The prevalence of MIH was reported to range 2.8 to 40.2%, yet this inconsistency leads to a challenging interpretation and is mainly caused by the lack of standardization among clinicians/researchers3. As a result, the EAPD introduced a diagnostic and classification system for MIH, with the purpose of improving epidemiological assessments3,4.
Two systematic reviews have estimated the prevalence of MIH between 13.1% and 14.2, with significant variances amid regions5,6. Moreover, Schwendicke et al.5 estimated MIH prevalence on country scale via the Global Burden of Disease database, which may explain the variances between those regions. Additionally, both searches were conducted until mid 2017, and ever since, a number of new epidemiological studies have been published. However, other relevant information remains to be elucidated, namely the prevalence of moderate/severe cases, prevalence of molars and incisors affected and the prevalence of hypomineralization of the second primary molars (HSPM). For these reasons, conducting a new systematic review on the topic would be convenient and relevant globally.
In this sense, and given the increase research on the prevalence of MIH, we aimed to comprehensively investigate the global prevalence of MIH, as well as its associated characteristics.
Methods
Protocol and registration
The protocol for this systematic review was defined by all authors and registered at the National Institute for Health Research PROSPERO, International Prospective Register of Systematic Review (http://www.crd.york.ac.uk/PROSPERO, ID Number: CRD42021229435). We based our review design following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline7.
Focused question and eligibility criteria
We aimed to answer the following PECO question: “What is the global prevalence of MIH?”. The respective statements were as follows: Clinical/Epidemiologic studies in humans (P, Population); Diagnosis of MIH (E, Exposure); No MIH (C, Comparison); Prevalence of MIH (O, Outcome).
The primary aim was the prevalence of MIH. The secondary aims were the prevalence of moderate/severe MIH cases, prevalence of molars and incisors affected and the prevalence of HSPM.
Studies were eligible for inclusion based on the following criteria: (1) Observational studies reporting the prevalence of MIH; (2) Studies with clear reporting of MIH definition; (3) Subjects with no systemic disorders; (4) Studies including both genders.
In contrast, studies based on specific population, for example, children born preterm, studies which only reported on primary molars, and studies which focused on non-representative samples (e.g., institutionalized populations, particular professions, those with specific dental outcomes like high caries experience, among others) were excluded.
Search strategy
Identification of studies for this systematic review was performed through detailed search strategies developed for each database (Pubmed, MEDLINE, CENTRAL [The Cochrane Central Register of Controlled Trials], Web of Science, SciELO [Scientific Electronic Library Online], EMBASE [The Excerpta Medica Database], LILACS [Latin-American scientific literature in health sciences], and TRIP [Turning Research Into Practise]) up to July 2021. Our search strategy was based on the following algorithm: "(hypomineralization OR hypomineralisation OR hypomineralized OR hypomineralized OR hypoplasia OR demarcated OR opacities OR MIH OR cheese molars) AND (survey OR questionnaire OR cross-sectional OR prevalence OR frequency OR population OR sample OR sampling) AND (molar OR molars OR incisors)".
Study selection
Study selection was assessed independently by two investigators (LBL and JB), who performed the assessment of titles and/or abstracts of retrieved studies. For measurement reproducibility purposes, inter-examiner reliability following full-text assessment was calculated via kappa statistics. Any disagreements were resolved by discussion with a third author (VM).
Data extraction process and data items
Data extraction was performed by two reviewers independently and in duplicate (LBL and JB). The agreement between the reviewers was assessed by Kappa statistics. Any paper classified as potentially eligible by either reviewer was ordered as a full text and independently screened by the reviewers. All disagreements were resolved through discussion with a third reviewer (VM). The following information was gathered in general description, research characteristics, methodology, and outcome measurements. The following standard information was extracted from each eligible study: first author’s name, year of publication, year of study conduct, country and place (region, city) of sampling, setting of sampling, sampling strategy, case definition, setting, observation setting, sample size, age of participants, total sample size, prevalence estimation, sex-specific sample size and prevalence (if available), the diagnostic criteria of MIH, mean number of affected teeth, and funding. Also, severity of MIH was registered whenever studies reported it. We considered studies that have defined or used classifications that considered severe cases of MIH as having demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and strong aesthetic concerns.
We applied no publication year nor language restrictions. Grey literature was searched via http://www.opengrey.eu/. If not reported, corresponding authors were contacted to obtain baseline data.
Risk of bias (RoB) assessment
The Newcastle–Ottawa (NOS) Scale for case–control studies was used by two calibrated reviewers (LBL and JB). For calibration purposes, a random sample of 10 studies was assessed and reassessed 2 days later (to calculate Cohen's kappa). We have categorized studies as of low RoB (with 7–9 stars), moderate RoB (studies with 5–6 stars), and high RoB (with less than 5 stars) (as previously performed8,9). If any doubt occurred, they were resolved by discussion with a third author (VM).
Summary measures and synthesis of results
We began by conducting a prior sensitivity analysis to understand if studies reporting MIH with the 2003 case definition would differ from other alternative case definitions. Predefined tables were prepared to collect continuous data, mean values and standard deviations (SD). Random-effects meta-analysis and forest plots of prevalence were calculated in R version 3.4.1 (R Studio Team 2018) using ‘meta’ package10, through DerSimonian-Laird random-effects meta-analysis. Subgroup meta-analysis was conducted for two reasons: (a) comparing the EAPD case definition with other alternative methods; (b) comparing continental prevalence of MIH. Also, a meta-analysis of binary outcome data comparing females and males prevalence was performed. Heterogeneity and publication bias were computed via I2 test statistics (p < 0.1) and Egger’s significance test, respectively11. Substantial heterogeneity was considered when I2 statistics exceeded 50%11. In meta-analysis with 10 or more studies included, we analyzed publication bias11. Meta-regressions were conducted using continuous variables to appraise potential sources of heterogeneity, such as sample size, female/male ratio (FMR), geographic location (latitude and longitude) and year of publication. The regression approach also allowed to quantify the percentage of heterogeneity that could be explained by that variable. All tests were two-tailed with alpha set at 0.05 except for the homogeneity test whose significance level cutoff was 0.10 due to the low power of the χ2 test with a limited number of studies. Estimates were described with 95% confidence interval (CI).
Additional analyses
We employed the Strength of Recommendation Taxonomy (SORT) to appraise the strength and quality of the evidence12.
Results
Study selection
The online search retrieved strategy 2290 possibly relevant publications. After duplicates removal, 357 papers were judged against the eligibility criteria, and 1576 were excluded after titles and/or abstracts review. Among 138 articles assessed for full paper review eligibility, 22 articles were excluded with the respective reasons for exclusion detailed in the Supplementary S2. As a result, a final number of 116 observational studies were included for qualitative synthesis (Fig. 1). Inter-examiner reliability at the full-text screening was considered very substantial (kappa score = 0.915, 95% CI 0.895–0.925).
Figure 1.
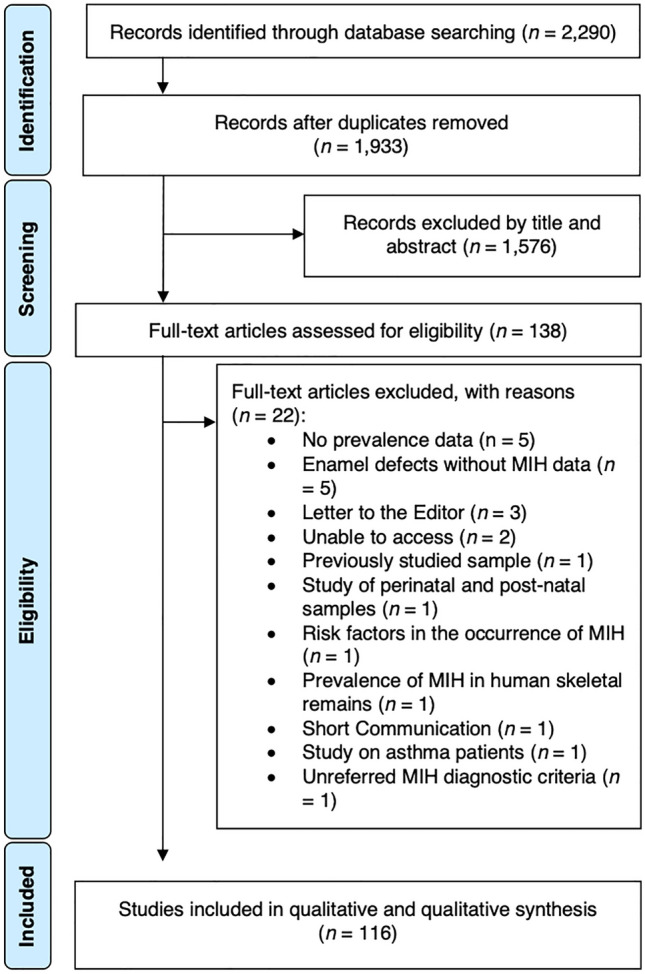
PRISMA flowchart.
Studies characteristics
The characteristics of the included studies are presented in Table 1. We identified 116 different cohorts13–128 from fifty different countries, across five continents. The year of publication of the included studies ranged between 2003 and 2021. Overall, a total of 135,181 participants were included in this review, being 52,876 girls and 52,872 boys, even though 18 manuscripts did not report on sex distribution. Thirty-four papers did not report the prevalence of MIH according to sex. Seven studies reported data on HSPM. Most studies recorded the MIH-related hypomineralization according to the diagnostic criteria of the EAPD case definition1, and others indices were also used such as the modified Developmental Defects of Enamel (mDDE) index129, the Kemoli88, Mathu-Muju and Wright130 criteria, and the diagnostic criteria of Cho et al.17,92.
Table 1.
Characteristics of the included studies.
| Authors (year) (country) | Funding | Age range (years) | MIH classification | Total (MIH/No MIH) (n) | Females (n) | Males (n) | Molars affected (%) | Incisors affected (%) | Incisors and molars affected (%) | HSPM cases (n) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIH | Total | MIH | Total | ||||||||||||
| 1 | 2 | 3 | 4 | ||||||||||||
| Abdalla et al. (2021) (Sudan) | None | 8–11 | EAPD1 | 568 (114/470) | 55 | 284 | 59 | 284 | 33.3 | 29.8 | 23.7 | 13.2 | 7.6 | 12.5 | NR |
| Ahmad et al. (2019) (United Arab Emirates) | NI | 6–10 | EAPD1 | 779 (59/720) | 39 | 515 | 20 | 264 | 11.9 | 47.5 | 25.4 | 15.3 | 25.4 | 25.4 | NR |
| Ahmadi et al. (2012) (Iran) | NI | 7–9 | EAPD1 | 433 (55/378) | 25 | 218 | 30 | 215 | NR | NR | NR | NR | NR | NR | NR |
| Alhowaish et al. (2021) (Saudi Arabia) | NR | 8–10 | EAPD1 | 893 (362/531) | 194 | 461 | 168 | 432 | NR | NR | NR | NR | NR | NR | NR |
| Allazzam et al. (2014) (Saudi Arabia) | NI | 8–12 | EAPD1 | 267 (23/244) | 10 | 133 | 13 | 134 | 21.7 | 34.8 | 8.7 | 34.8 | 65.2 | 67.5 | NR |
| Amend et al. (2020) (Germany) | Self-funded | 6–12 | EAPD1 | 2103 (283/1820) | NR | 1005 | NR | 1098 | 30.4 | 24.7 | 19.4 | 25.4 | 48.7 | 65.2 | 64 |
| Arheiam et al. (2021) (Saudi Arabia) | NI | 8–10 | EAPD1 | 1047 (162/885) | 78 | 550 | 84 | 497 | NR | NR | NR | NR | 49.4 | NR | NR |
| Arslanagic-Muratbegovic et al. (2020) (Bosnia and Herzegovina) | NI | 6–9 | EAPD1 | 444 (51/393) | 28 | NR | 23 | NR | 11.8 | 35.3 | 23.5 | 35.3 | 64.7 | 64.7 | NR |
| Balmer et al. (2011)/(2015) (England) | NI | 12 | mDDE129 | 3233 (514/2719) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bhaskar et al. (2014) (India) | NI | 8–13 | EAPD1 | 1173 (111/1062) | 47 | 536 | 64 | 637 | 6.3 | 27.0 | 17.1 | 49.6 | 29.0 | NR | NR |
| Biondi et al. (2011) (Argentina) | NI | NR | Mathu-Muju and Wright130 | 1098 (175/923) | NR | 577 | NR | 521 | NR | NR | NR | NR | 18.9 | NR | NR |
| Biondi et al. (2012) (Argentina and Uruguay) | NI | 7–17 | Mathu-Muju and Wright130 | 512 (32/480) | 29 | 519 | 36 | 456 | NR | NR | NR | NR | 24.6 | NR | NR |
| 463 (33/430) | 29 | 519 | 36 | 456 | NR | NR | NR | NR | 26.1 | NR | NR | ||||
| Buchgraber et al. (2017) (Austria) | Medical University Graz | 6–12 | EAPD1 | 1111 (78/1033) | 40 | 564 | 38 | 547 | 24.4 | 16.7 | 23.1 | 35.7 | NR | NR | NR |
| Calderara et al. (2005) (Italy) | European Union, Regione Lombardia and Academy of Finland | 7.3–8.3 | EAPD1 | 227 (39/188) | NR | 113 | NR | 114 | NR | NR | NR | NR | NR | NR | NR |
| Cho et al. (2008) (Hong Kong) | NR | 11–14 | Cho et al. criteria92 | 2635 (73/2562) | NR | NR | NR | NR | 49.3 | 24.7 | 15.1 | 11.0 | 33.0 | 45.0 | NR |
| Da Costa-Silva et al. (2010) (Brazil) | NR | 6–12 | EAPD1 | 918 (182/736) | 92 | 508 | 90 | 410 | 71 | NR | NR | 24 | NR | 55.2 | NR |
| Dantas-Neta et al. (2016) (Brazil) | Piauí Research Foundation | 11–14 | EAPD1 | 594 (109/485) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Dantas-Neta et al. (2018) (Brazil) | Piauí Research Foundation | 8–10 | EAPD1 | 744 (186/558) | 103 | 412 | 83 | 332 | NR | NR | NR | NR | NR | NR | NR |
| Davenport et al. (2019) (USA) | Marquette University | 7–12 | EAPD1 | 375 (36/339) | 25 | 226 | 11 | 142 | 52,8 | 33,3 | 5.6 | 8.3 | 52.8 | 52.8 | NR |
| De Lima et al. (2015) (Brazil) | State of Piauí Research Foundation | 11–14 | EAPD1 | 594 (109/485) | 69 | 375 | 40 | 219 | NR | NR | NR | NR | NR | NR | NR |
| Dietrich et al. (2003) (Germany) | NI | 10–17 | mDDE129 | 2408 (135/2273) | NR | NR | NR | NR | 34.1 | 28.1 | 9.7 | 28.1 | 23.0 | 23.0 | NR |
| Dourado et al. (2020) (Brazil) | NR | 8–14 | EAPD1 | 251 (117/134) | 55 | 116 | 62 | 135 | NR | NR | NR | NR | NR | NR | NR |
| Elfrink et al. (2012) (The Netherlands) | Erasmus MC, the Netherlands Organization for Health Research and Development and GABA | 6–10 | EAPD1 | 2530 (203/2327) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Elzein et al. (2019) (Lebanon) | NR | 7–9 | EAPD1 | 659 (176/483) | 96 | NR | 80 | NR | 12.8 | 19.5 | 26.8 | 40.9 | 45.1 | 45.1 | NR |
| Emmaty et al. (2020) (India) | None | 8–15 | EAPD1 | 5318 (216/5102) | 96 | 2613 | 120 | 2705 | NR | NR | NR | NR | NR | NR | NR |
| Farias et al. (2020) (Brazil) | Paraíba State Research Support Foundation | 8–10 | EAPD1 | 471 (46/425) | 26 | 265 | 20 | 206 | NR | NR | NR | NR | NR | NR | NR |
| Fatturi et al. (2020) (Brazil) | São Paulo Research Foundation | 8 | EAPD1 | 731 (88/643) | 39 | 357 | 49 | 374 | NR | NR | NR | NR | NR | NR | NR |
| Fernandes et al. (2021) (Brazil) | NI | 6–12 | EAPD1 | 610 (60/550) | 26 | 281 | 34 | 329 | NR | NR | NR | NR | NR | NR | NR |
| Freitas Fernandes et al. (2021) (Brazil) | CAPES, National Council for Scientific and Technological Development (CNPq), Research Productivity Scholarship (302850/2016-3), and the State of Paraíba Research Support Foundation (FAPESQ/PB) | 11–14 | EAPD1 | 463 (50/413) | NR | 293 | NR | 170 | NR | NR | NR | NR | NR | NR | NR |
| Fteita et al. (2006) (Libya) | Academy of Finland | 7–8,9 | mDDE129 | 378 (11/367) | 6 | 188 | 5 | 190 | 63.6 | 27.3 | NR | 9.1 | NR | NR | NR |
| Gambetta-Tessini et al. (2018) (Australia) | NI | 6–12 | EAPD1 | 327 (48/279) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 26 |
| Gambetta-Tessini et al. (2019) (Chile) | Melbourne Dental School and Fund. Becas Chile | 6–12 | EAPD1 | 577 (91/486) | 52 | 292 | 39 | 285 | NR | NR | NR | NR | NR | NR | 29 |
| Garcia-Margarit et al. (2013) (Spain) | University of Valencia | 8 | EAPD1 | 840 (183/657) | NR | 412 | NR | 428 | NR | NR | NR | NR | 32.5 | NR | NR |
| Ghanim et al. (2011) (Iraq) | NI | 7–9 | EAPD1 | 823 (197/626) | NR | 352 | NR | 471 | NR | NR | NR | NR | NR | 28.8 | NR |
| Ghanim et al. (2013) (Iran) | Shiraz University of Medical Sciences | 9–11 | EAPD1 | 810 (164/646) | 96 | 450 | 68 | 360 | NR | NR | NR | NR | NR | NR | NR |
| Glodkowska et al. (2019) (Poland) | NI | 6–12 | EAPD1 | 1437 (51/1386) | 27 | 726 | 24 | 711 | 3.9 | 17.0 | 21.0 | 58.0 | NR | 3.2 | NR |
| Goswami et al. (2019) (India) | None | 6–12 | EAPD1 | 1026 (12/1014) | 1 | 492 | 11 | 534 | 0 | 16.7 | 0 | 83.3 | 42.9 | 41.7 | NR |
| Groselj et al. (2013) (Slovenia) | Slovenian Ministry of Science and Education | 6.0–11.5 | EAPD1 | 478 (102/376) | NR | 212 | NR | 266 | NR | NR | NR | NR | NR | NR | NR |
| Gurrusquieta et al. (2017) (Mexico) | NI | 6–12 | EAPD1 | 1156 (183/973) | NR | 582 | NR | 574 | NR | NR | NR | NR | NR | NR | NR |
| Hanan et al. (2015) (Brazil) | NI | 6–10 | EAPD1 | 2062 (188/1874) | 90 | 941 | 98 | 933 | NR | NR | NR | NR | NR | NR | NR |
| Hartsock et al. (2020) (USA) | University of Pittsburgh | 7–32 | EAPD1 | 104 (10/94) | 8 | 64 | 2 | 40 | NR | NR | NR | NR | NR | NR | NR |
| Heitmuller et al. (2013) (Germany) | Federal Ministry of Environment and the GABA GmBH | 10 | Koch et al.140 | 693 (253/2327) | NR | 359 | N R | 334 | NR | NR | NR | NR | NR | NR | NR |
| Hernández et al. (2018) (Spain) | NI | 6–14 | EAPD1 | 705 (56/649) | 34 | 361 | 22 | 344 | 23.2 | 35.7 | 21.4 | 19.6 | 92.8 | NR | NR |
| Hussain et al. (2018) (United Arab Emirates) | NI | 6–12 | EAPD1 | 342 (93/249) | 70 | 215 | 23 | 127 | NR | NR | NR | NR | NR | NR | NR |
| Hussein et al. (2015) (Malaysian) | Research Management Institute of Universiti Teknologi MARA | 7–12 | EAPD1 | 154 (26/128) | NR | 87 | NR | 67 | NR | NR | NR | NR | NR | 50.0 | NR |
| Hysi et al. (2016) (Albania) | NR | 8–10 | EAPD1 | 1575 (227/1348) | 114 | 744 | 113 | 831 | NR | NR | NR | NR | NR | NR | NR |
| Irigoyen-camacho et al. (2019) (Mexico) | NI | 6–8 | EAPD1 | 232 (47/185) | 19 | 115 | 28 | 117 | NR | NR | NR | NR | NR | NR | NR |
| 317 (101/216) | 52 | 171 | 49 | 146 | NR | NR | NR | NR | NR | NR | NR | ||||
| Jancovik et al. (2014) (Bosnia and Herzegovina) | NI | 8 | EAPD1 | 141 (26/115) | NR | 70 | NR | 71 | NR | NR | NR | NR | NR | NR | NR |
| Jasulaityte et al. (2007) (Lithuania) | NI | 6–9 | EAPD1 | 1227 (190/1087) | 102 | 629 | 88 | 560 | NR | NR | NR | NR | NR | 44.4 | NR |
| Jasulaityte et al. (2008) (Netherlands) | NI | 9 | EAPD1 | 442 (63/379) | NR | 220 | NR | 222 | 11.1 | 30.2 | 22.2 | 36.5 | 2.6 | NR | NR |
| Jeremias et al. (2013) (Brazil) | Federal funding from São Paulo State | 6–12 | EAPD1 | 1157 (142/1015) | 88 | 622 | 54 | 535 | 23.9 | NR | NR | NR | 51.4 | 51.4 | NR |
| Jurlina et al. (2020) (Croatia) | None | 8 | EAPD1 | 729 (88/641) | 49 | 356 | 39 | 373 | NR | NR | NR | NR | NR | 6.6 | NR |
| Kemoli et al. (2009) (Kenya) | NI | NR | Kemoli88 | 3591 (493/3098) | 375 | 1593 | 118 | 1998 | NR | NR | NR | NR | NR | NR | NR |
| Kevrekidou et al. (2015) (Greece) | NI | 8–14 | EAPD1 | 2335 (498/1837) | 253 | 1196 | 245 | 1139 | 48.0 | 28.0 | 13.0 | 11.0 | NR | 54.0 | NR |
| Kilinç et al. (2019) (Turkey) | NI | 9–10 | EAPD1 | 1237 (142/1095) | 69 | NR | 73 | NR | NR | NR | NR | 23.4 | NR | NR | NR |
| Kirthiga et al. (2015) (India) | NI | 11–16 | Cho et al.92 | 2000 (179/1821) | 92 | 827 | 87 | 1173 | NR | NR | NR | NR | NR | NR | NR |
| Kohlboeck et al. (2013) (Germany) | Federal Ministry of Environment and the GABA GmBH | 10 | EAPD1 | 1126 (381/745) | NR | 549 | NR | 577 | NR | NR | NR | NR | NR | NR | NR |
| Koruyucu et al. (2018) (Turkey) | Istanbul University | 8 and 11 | EAPD1 | 1511 (215/1296) | 113 | 751 | 102 | 760 | NR | NR | NR | NR | NR | NR | NR |
| Krishnan et al. (2015) (India) | NI | 8–13 | EAPD1 | 4989 (384/4605) | 253 | 2831 | 131 | 2158 | NR | NR | NR | NR | NR | NR | NR |
| Kühnisch et al. (2018) (Germany) | Federal Ministry for Education | 15 | EAPD1 | 1302 (224/1078) | NR | 651 | NR | 651 | 38.2 | NR | NR | 17.1 | NR | 9.8 | NR |
| Kuscu et al. (2009) (Turkey) | NI | NR | EAPD1 | 153 (14/139) | 6 | 72 | 8 | 67 | NR | 21.4 | NR | NR | NR | 50.0 | NR |
| López Jordi et al. (2014) (Argentina & Uruguay) | NI | 7–17 | Mathu-Muju and Wright130 | 1090 (176/914) | NR | 572 | NR | 518 | NR | NR | NR | NR | NR | NR | NR |
| 626 (77/549) | NR | 328 | NR | 298 | NR | NR | NR | NR | NR | NR | NR | ||||
| Lygidakis et al. (2008) (Greece) | NI | 5.5–12 | EAPD1 | 3518 (360/3158) | 211 | NR | 149 | NR | NR | NR | NR | NR | NR | 62.5 | NR |
| Mahoney et al. (2009) (New Zealand) | NR | 7–10 | mDDE129 | 234 (44/190) | NR | 117 | 25 | 117 | NR | NR | NR | NR | NR | NR | NR |
| Mahoney et al. (2011) (New Zealand) | NR | 7–10 | mDDE129 | 522 (78/444) | NR | 282 | NR | 240 | NR | NR | NR | NR | NR | NR | NR |
| Martínez Gomez et al. (2012) (Spain) | NI | 6–14 | EAPD1 | 505 (90/415) | 45 | 246 | 45 | 259 | 10.0 | 11.1 | 11.1 | 8.8 | NR | 58.8 | NR |
| Martinovic et al. (2017) (Kosovo) | NR | 8 and 10 | EAPD1 | 712 (87/625) | 49 | 383 | 38 | 329 | NR | NR | NR | NR | NR | 100.0 | NR |
| Mejia et al. (2019) (Colombia) | NI | 6–15 | EAPD1 | 1075 (120/955) | 46 | 443 | 74 | 632 | NR | NR | NR | NR | NR | NR | NR |
| Mishra et al. (2016) (India) | None | 8–12 | EAPD1 | 1369 (191/1178) | 99 | NR | 92 | NR | NR | NR | NR | NR | NR | 27.7 | NR |
| Mittal et al. (2013) (India) | NI | 6–9 | EAPD1 | 1792 (113/1679) | 50 | NR | 63 | NR | NR | NR | NR | NR | NR | NR | NR |
| Mulic et al. (2017) (Bosnia and Herzegovina) | University of Oslo | 8–9 | EAPD1 | 103 (12/91) | NR | 41 | NR | 62 | 25 | 50 | 25 | NR | NR | NR | NR |
| Muratbegovic et al. (2007) (Bosnia and Herzegovina) | NI | 12 | EAPD1 | 560 (69/491) | 36 | NR | 33 | NR | NR | NR | NR | NR | NR | 92.5 | NR |
| Negre-Barber et al. (2016) (Spain) | Spanish national R&D&I Plan and European Regional Development Fund | 8–9 | EAPD1 | 414 (100/314) | 46 | 202 | 54 | 212 | 17.0 | 22.0 | 26.0 | 35.0 | 60.0 | NR | 60 |
| Ng et al. (2014) (Singapore) | NI | NR | EAPD1 | 1083 (135/948) | 68 | 608 | 67 | 475 | 46.7 | 22.2 | 8.1 | 4.4 | 25.2 | 3.2 | 23 |
| Ordonez-Romero et al. (2021) (Ecuador) | None | 7–12 | EAPD1 | 249 (23/226) | 17 | 144 | 6 | 105 | NR | NR | NR | NR | 25.6 | NR | NR |
| Oyedele et al. (2015) (Nigeria) | NI | 8–10 | EAPD1 | 469 (83/386) | 32 | 214 | 51 | 255 | NR | NR | NR | NR | NR | NR | NR |
| Padavala et al. (2018) (India) | None | 7–12 | EAPD1 | 170 (22/148) | 7 | 85 | 15 | 85 | NR | NR | NR | NR | 10.8 | 40.9 | NR |
| Parikh et al. (2012) (India) | NI | 8–12 | EAPD1 | 1366 (126/1240) | 58 | NR | 68 | NR | NR | NR | NR | NR | NR | 82.5 | NR |
|
Petrou et al. (2014)/(2015) (Germany) |
NI | 7–10 | EAPD1 | 2395 (242/2153) | 114 | 1200 | 128 | 1195 | 39.2 | NR | NR | NR | 42.2 | NR | NR |
| Pitiphat et al. (2014) (Thailand) | Thailand Research Fund | 6–7 | EAPD1 | 484 (95/389) | 51 | 246 | 44 | 238 | 86.0 | NR | NR | NR | NR | NR | NR |
| Portella et al. (2019) (Brazil) | CAPES Grant/Award Number: 001 | 8 | EAPD1 | 728 (88/640) | NR | 356 | NR | 372 | NR | NR | NR | NR | 54.5 | NR | NR |
| Preusser et al. (2007) (Germany) | NR | 6–12 | Koch et al.140 | 1002 (59/943) | NR | 496 | NR | 506 | NR | NR | NR | NR | NR | NR | NR |
| Rai et al. (2018) (India) | NI | 7–9 | mDDE129 | 992 (212/780) | 80 | 460 | 132 | 532 | NR | NR | NR | NR | NR | NR | NR |
| Rai et al. (2019) (India) | Indian Council of Medical Research | 9–12 | EAPD1 | 1600 (210/1390) | 104 | 814 | 106 | 786 | NR | NR | NR | NR | 12.1 | 70.2 | NR |
| Ray et al. (2020) (India) | None | 8–12 | EAPD1 | 1525 (87/1438) | 37 | 725 | 50 | 800 | NR | NR | NR | NR | 56.3 | 18.4 | NR |
| Reyes et al. (2019) (Brazil) | NI | 8 | EAPD1 | 731 (88/643) | 39 | 357 | 49 | 374 | NR | NR | NR | N R | 6.6 | NR | NR |
| Rodrigues et al. (2015) (Brazil) | NI | 7–14 | mDDE129 | 1179 (30/1149) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Saber et al. (2018) (Egypt) | NI | 8–12 | EAPD1 | 1001 (23/978) | 14 | 502 | 9 | 499 | NR | NR | NR | NR | NR | NR | NR |
| Saitoh et al. (2018) (Japan) | Japanese Dental Science Federation | 7–9 | EAPD1 | 4496 (892/3604) | 464 | 2280 | 428 | 2216 | NR | NR | NR | NR | NR | NR | NR |
| Sakly et al. (2020) (Tunisia) | None | 7–12 | EAPD1 | 510 (181/329) | 82 | 257 | 99 | 253 | NR | NR | NR | NR | NR | NR | NR |
| Schmalfuss et al. (2015) (Norway) | NI | 16 | EAPD1 | 794 (110/684) | NR | 380 | NR | 414 | 48.2 | 30.0 | 12.7 | 9.1 | 41.8 | NR | NR |
| Shrestha et al. (2015) (Nepal) | NI | 7–12 | EAPD1 | 747 (102/645) | 48 | 357 | 54 | 288 | 4.9 | 9.8 | 10.8 | 74.5 | 84.3 | 85.3 | NR |
| Sidhu et al. (2019) (Canada) | Hospital for Sick Children | NR | EAPD1 | 429 (29/400) | NR | 181 | NR | 248 | NR | NR | NR | NR | NR | NR | 19 |
| Silva et al. (2020) (Brazil) | Coordenação de Aperfeiçonamento de Pessoal de Nivel Superior Brasil—(CAPES) | 7–14 | EAPD1 | 407 (59/348) | 26 | 182 | 33 | 225 | NR | NR | NR | NR | NR | NR | NR |
| Silva Júnior et al. (2015) (Brazil) | Federal University of Pará | 5–17 | EAPD1 | 260 (23/237) | 11 | 112 | 12 | 148 | NR | NR | NR | NR | 39.1 | 34.8 | NR |
| Singh et al. (2020) (India) | None | 7–10 | EAPD1 | 649 (97/552) | NR | NR | NR | NR | 5.7 | 39.3 | 7.4 | 47.5 | 93.8 | 8.8 | NR |
| Sonmez et al. (2013) (Turkey) | NI | 7–12 | EAPD1 | 4018 (308/3710) | 156 | 2029 | 152 | 2020 | NR | NR | NR | NR | NR | NR | NR |
| Sosa-Soto et al. (2021) (Mexico) | Programa de Fortalecimiento de la Calidad Educativa | 8 | EAPD1 | 613 (76/537) | NR | 295 | NR | 318 | 38.2 | NR | NR | 17.1 | NR | NR | NR |
| Souza et al. (2013) (Brazil) | Federal Funding from São Paulo State | 7–12 | EAPD1 | 1151 (142/1009) | 88 | 624 | 54 | 527 | NR | NR | NR | NR | NR | NR | NR |
| Soviero et al. (2009) (Brazil) | State University of Rio de Janeiro | 7–13 | EAPD1 | 249 (100/149) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Subramaniam et al. (2016) (India) | None | 7–9 | EAPD1 | 2500 (12/2488) | 7 | 1104 | 5 | 1396 | 42.3 | 40.4 | 5.8 | 11.5 | 23.1 | 23.1 | NR |
| Tagelsir Ahmed et al. (2020) (USA) | NI | 6–15 | EAPD1 | 337 (43/294) | 24 | 169 | 19 | 168 | NR | NR | NR | NR | NR | NR | 6 |
| Temilola et al. (2015) (Nigeria) | NI | NR | Kemoli88 | 236 (23/213) | 14 | 120 | 9 | 116 | NR | NR | NR | NR | NR | NR | 8 |
| Thakur et al. (2020) (India) | NR | 8–16 | EAPD1 | 2000 (58/1942) | NR | 967 | NR | 1033 | 8.5 | 32.3 | 13.6 | 44.2 | 41.2 | 41.2 | 13 |
| Tourino et al. (2016) (Brazil) | None | 8–9 | EAPD1 | 1181 (241/940) | 125 | 599 | 116 | 582 | NR | NR | NR | NR | NR | NR | NR |
| Villanueva-Gutierrez et al. (2019) (Mexico) | Metropolitan Autonomous University-Xochimilco | 7–12 | EAPD1 | 686 (243/443) | 120 | 365 | 123 | 321 | 6.6 | 21.7 | 28.3 | 43.4 | NR | NR | NR |
| Wogelius et al. (2008) (Danmark) | “Augustinus Foundation’’, the Danish Cancer Society, and Boernecancerfonden | 6–8 | EAPD1 | 647 (241/426) | 116 | 321 | 125 | 326 | 32.0 | 27.4 | 13.7 | 27.0 | NR | NR | NR |
| Wuollet et al. (2014) (Finland) | Academy of Finland | 7–13 | EAPD1 | 818 (140/678) | 66 | 401 | 74 | 417 | NR | NR | NR | NR | NR | NR | NR |
| Wuollet et al. (2016) (Finland) | Academy of Finland | NR | EAPD1 | 287 (33/254) | 17 | 128 | 16 | 159 | NR | NR | NR | NR | NR | NR | NR |
| Wuollet et al. (2018) (Finland) | Academy of Finland | 8–13 | EAPD1 | 636 (115/521) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Yannam et. (2016) (India) | NI | 8–12 | EAPD1 | 2864 (277/2587) | NR | 1365 | NR | 1499 | NR | NR | NR | NR | NR | NR | NR |
| Yi et al. (2020) (China) | Scientific Research Fund of National Health Commission of China | 12–15 | EAPD1 | 6523 (655/5868) | 340 | 3295 | 315 | 3228 | NR | NR | NR | NR | 28.4 | 28.4 | NR |
| Zawaideh et al. (2011) (Jordania) | NI | 7–9 | EAPD1 | 3241 (570/2671) | 302 | 1539 | 268 | 1702 | 41.0 | 28.0 | 20.0 | 11.0 | 32.0 | 32.0 | NR |
NR Not reported, NI No information, EAPD European Academy of Pediatric Dentistry (Weerheijm et al.1), mDDE modified Developmental Defects of Enamel index.
Three cohorts had their data reported in more than one article (Petrou et al.78 and Petrou et al.109; Balmer et al.13 and Balmer et al.14; Negre-Barber et al.110 and Negre-Barber et al.111); thus, these papers were grouped under a single name study as follows: Petrou et al.78,109; Balmer et al.13,14; and, Negre-Barber et al.110,111. Also, three studies reported in the same study two cohorts: Biondi et al.16 reported data for Buenos Aires (Argentina) and Montevideo (Uruguay); López Jordi et al.108 reported data for Buenos Aires (Argentina) and Montevideo (Uruguay); and Irigoyen-Camacho et al.62 reported data for both 2008 and 2017 cohorts.
Assessment of RoB within studies
Inter-examiner reliability at RoB analysis was considered very substantial (kappa score = 0.885, 95% CI 0.865–0.905). The RoB for observational studies, with the NOS, ranged from 6 to 9 stars (Supplementary S3). After the assessment, forty-eight had the maximum score (9/9). Additionally, fifty-three and six articles scored 8/9 and 7/9, respectively. Only one paper was of moderate RoB (score = 6/9). The main sources of inconsistencies arose from the representativeness of the cases. While all articles succeed to apply an adequate MIH case definition, selection of control, ascertainment of exposure, equal method of assessment of cases and controls and non-response rate (100.0%, n = 113), studies failed to provide adequate representativeness of the cases (48.7%, n = 55), two studies failed the definition of controls (1.8%) and 8.8% only provided information regarding MIH and not any other variables (n = 10).
Prevalence of MIH
A first subgroup meta-analysis confirmed that estimates from studies using the EAPD 2003 classification were significantly different from studies with alternative classifications (categorized as ‘others’) (p = 0.0061) (Supplementary S4). This initial analysis comprised 133,734 participants. Thus, we proceeded with the analyses using only studies reporting prevalence through the 2003 MIH case definition.
Global prevalence (primary outcome)
The overall prevalence of MIH for a total of 113,089 participants was estimated at 13.5% (95% CI 12.1–15.1, p < 0.001) (Table 2), with high heterogeneity (I2 = 98.0%) (Supplementary S5). Cumulative meta-analysis confirmed the overall estimate was not influenced by a particular study or group of studies (Supplementary S6A). We further confirmed the non-existence of influential studies through leave-one-out meta-analysis (Supplementary S6B).
Table 2.
Meta-analysis on the prevalence of MIH cases, severity of cases, number of affected molars, cases with affected incisors and HSPM.
| Condition | N | Estimate (%) | 95% CI (%) | p-value | I2 (%) | Egger test t (p-value) |
|---|---|---|---|---|---|---|
| MIH | 98 | 13.5 | 12.0–15.1 | < 0.001 | 98.0 | − 2.366 (0.179) |
| Moderate-to-severe cases | 33 | 36.3 | 29.9–43.2 | < 0.001 | 95.2 | 0.233 (0.052) |
| Number of affected molars | ||||||
| 1 | 31 | 24.3 | 18.9–30.7 | < 0.001 | 94.2 | − 3.392 (0.002) |
| 2 | 27 | 26.7 | 23.9–29.7 | < 0.001 | 65.0 | − 0.141 (0.889) |
| 3 | 26 | 18.1 | 13.8–23.3 | < 0.001 | 90.9 | − 1.207 (0.239) |
| 4 | 27 | 27.4 | 21.1–34.7 | < 0.001 | 94.0 | − 0.020 (0.984) |
| Cases with affected incisors | 31 | 38.7 | 32.1–45.8 | < 0.001 | 93.2 | − 0.747 (0.461) |
| Cases with both molars and incisors affected | 36 | 42.1 | 34.9–50.0 | < 0.001 | 95.5 | − 0.153 (0.774) |
| HSPM | 7 | 3.6 | 1.9–6.8 | < 0.001 | 95.9 | – |
MIH Molar-Incisor Hypomineralization, HSPM Hypomineralization of the Second Primary Molars, 95% CI 95% Confidence Interval.
The prevalence of moderate to severe cases of MIH was estimated at 36.3% (95% CI 29.9–43.2, I2 = 95.2%) (Table 2, Supplementary S7). Detailed information on the definition of severity in each study was collectively presented in Table 3. Regarding the number of affected molars, estimates point to 24.3% of cases with one molar (95% CI 18.9–30.7, I2 = 94.2%), 26.7% of cases with two molars (95% CI 23.9–29.7, I2 = 65.0%), 18.1% of cases with three molars (95% CI 13.8–23.3, I2 = 90.0%) and 26.8% of cases with four molars (95% CI 21.1–34.7, I2 = 94.0%) (Supplementary S8-S11). The cases with affected incisors were estimated at 38.7% (95% CI 32.1–45.8, I2 = 93.2%) (Supplementary S12), while cases with both molars and incisors were estimated at 42.1% (95% CI 34.9–50.0, I2 = 95.5%) (Supplementary S13). Lastly, the prevalence of HSPM cases was estimated at 3.6% (95% CI 1.9–6.8, I2 = 96.3%) (Supplementary S14). All the latter results had high heterogeneity.
Table 3.
Detailed case definition of MIH severity for each study with the respective reported prevalence.
| Authors (year) (country) | Severity Index/definition | Definition | Moderate/severe cases (%) |
|---|---|---|---|
| Amend et al. (2020) (Germany) | Wetzel and Reckel scale34 | Degree 1 (isolated hypomineralization of white cream to yellow–brown color, solely located in the uppermost part of the tooth crown (chewing surface), no post-eruptive enamel breakdown); degree 2 (enamel hypomineralization of yellow–brown color affecting almost all humps in the coronal part of the tooth crown combined with a small amount of post-eruptive enamel breakdown), and degree 3 (extensive enamel hypomineralization of yellow–brown color along with extensive post-eruptive enamel breakdown causing changes of the tooth crown morphology) | 78.4 |
| Arslanagic-Muratbegovic et al. (2020) (Bosnia & Herzegovina) | – | ≥ 1 tooth with post-eruptive enamel breakdown, atypical fillings or tooth extracted due to MIH | 82.0 |
| Da Costa-Silva et al. (2010) (Brazil) | Leppäniemi et al.135 | Mild (demarcated opacities without fracture), moderate (hard and fractured enamel and need for treatment), and severe (loss of tooth structure affecting the enamel and dentine, replacement of hard tissues with atypical restorations, and tooth extraction due to hypomineralization) | 54.0 |
| Dantas-Neta et al. (2016) (Brazil) | Leppäniemi et al.135 | Mild (demarcated opacities without fracture), moderate (hard and fractured enamel and need for treatment), and severe (loss of tooth structure affecting the enamel and dentine, replacement of hard tissues with atypical restorations, and tooth extraction due to hypomineralization) | 50.5 |
| Dantas-Neta et al. (2018) (Brazil) | Leppäniemi et al.135 | Mild (demarcated opacities without fracture), moderate (hard and fractured enamel and need for treatment), and severe (loss of tooth structure affecting the enamel and dentine, replacement of hard tissues with atypical restorations, and tooth extraction due to hypomineralization) | 5.4 |
| Davenport et al. (2019) (USA) | – | Mild (demarcated opacities without enamel breakdown, occasional sensitivity to external stimuli) and severe (demarcated enamel with breakdown, caries, and persistent/ spontaneous hypersensitivity) | 30.6 |
| Ghanim et al. (2013) (Iran) | – | Mild (color changes only [i.e. creamy white or yellow/brown]), moderate (loss of enamel substance), and severe (loss of enamel associated with affected dentine and/or atypical restoration) | 34.3 |
| Glodkowska et al. (2019) (Poland) | Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 26.6 |
| Gurrusquieta et al. (2017) (Mexico) | Mathu-Muju and Wright130 | Mild (Opacities delimited in areas free of occlusal forces, isolated opacities, no enamel loss in opaque areas, no history of dental hypersensitivity, no activities related to caries of affected enamel, alterations of incisors), moderate (atypical and intact restorations may be present, opacities delimited in the occlusal/incisal third of the tooth, without loss of the structure after eruption, loss of post-eruptive enamel and carious lesions that are limited to 1 or 2 areas, without participation of cusps, tooth sensitivity and often, aesthetic complaints) and severe (post-eruptive losses, history of tooth sensitivity, extensive carious lesions associated with the affected enamel, coronary destruction with pulp involvement, presence of defects in atypical restorations, aesthetic complaints) | 43.7 |
| Hartsock et al. (2020) (USA) | Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 30.0 |
| Hussain et al. (2018) (United Arab Emirates) | Chawla et al.138 | Hypomineralisation Severity Index | 47.0 |
| Irigoyen-camacho et al. (2019) (Mexico) | – | Mild (demarcated opacities affected less than one-third of the tooth surface, without post-eruptive enamel breakdown), moderate (demarcated opacities that affected at least one-third but less than two-thirds of the surface, without post-eruptive enamel breakdown; atypical caries lesions could affect less than two-thirds of the surface), and severe (demarcated opacities that affected more than two-thirds of the tooth surface, or the presence of post-eruptive enamel breakdown, atypical caries lesions larger than two-thirds of the surface, or large restorations with unusual shape, extended to smooth surfaces, or extraction of the tooth because of MIH) | 21.2 |
| 30.7 | |||
| Janković et al. (2014) (Bosnia and Herzegovina) | – | Mild (tooth enamel color changes [white, yellow or brown]), moderate (discoloration and minimal loss of tooth substances without the need for restoration), and severe (damaged enamel and dentin loss that require restoration) | 13.4 |
| Jasulaityte et al. (2008) (The Netherlands) | – | Mild (opacities) and severe (enamel breakdown and atypical restorations both include lesions with disintegrated enamel, in one case restored) | 45.2 |
| Jeremias et al. (2013) (Brazil) | Jasulaityte et al.63 | Severe (post-eruptive enamel breakdown, atypical restorations and extraction due to MIH) | 9.3 |
| Kevrekidou et al. (2015) (Greece) | Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 25.0 |
| Kühnisch et al. (2018) (Germany) | Kühnisch et al.69 | Severe (hypomineralization on first permanent molars and incisors) | 56.7 |
|
Martínez Gomez et al. (2012) (Spain) |
Mathu-Muju and Wright130 | Mild (Opacities delimited in areas free of occlusal forces, isolated opacities, no enamel loss in opaque areas, no history of dental hypersensitivity, no activities related to caries of affected enamel, alterations of incisors), moderate (atypical and intact restorations may be present, opacities delimited in the occlusal/incisal third of the tooth, without loss of the structure after eruption, loss of post-eruptive enamel and carious lesions that are limited to 1 or 2 areas, without participation of cusps, tooth sensitivity and often, aesthetic complaints) and severe (post-eruptive losses, history of tooth sensitivity, extensive carious lesions associated with the affected enamel, coronary destruction with pulp involvement, presence of defects in atypical restorations, aesthetic complaints) | 50.0 |
| Martinovic et al. (2017) (Kosovo) | – | Mild (stained changes in the tooth enamel), moderate (changes in color [white/opaque, yellow or brown] and minimal loss of tooth substance with no need for restoration, or minimally invasive treatment is sufficient to repair defects), and severe (loss of damaged enamel and dentin which require restoration) | 40.3 |
| Mejia et al. (2019) (Colombia) | Leppäniemi et al.135 | Mild (demarcated opacities without fracture), and severe (opacity with loss of structure compromising enamel and/or dentin, with atypical restorations, and/or exodontia due to hypomineralization) | 15.0 |
| Parikh et al. (2012) (India) | Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 22.3 |
|
Petrou et al. (2014)/(2015) (Germany) |
Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 52.1 |
| Portella et al. (2019) (Brazil) | Leppäniemi et al.135 | Mild (demarcated opacities without fracture), moderate (hard and fractured enamel and need for treatment), and severe (loss of tooth structure affecting the enamel and dentine, replacement of hard tissues with atypical restorations, and tooth extraction due to hypomineralization) | 28.4 |
| Silva et al. (2020) (Brazil) | Lygidakis et al.134 | Mild (demarcated enamel opacities without enamel breakdown, occasional sensitivity to external stimuli but not brushing and only mild aesthetic concerns on discoloration of the incisors), and severe (demarcated enamel opacities with breakdowns, caries, persistent/spontaneous hypersensitivity affecting function and finally strong aesthetic concerns that may have socio-psychological impact) | 22.6 |
|
Silva Júnior et al. (2015) (Brazil) |
Mathu-Muju and WrightWetzel and Reckel scale130 | Mild (Opacities delimited in areas free of occlusal forces, isolated opacities, no enamel loss in opaque areas, no history of dental hypersensitivity, no activities related to caries of affected enamel, alterations of incisors), moderate (atypical and intact restorations may be present, opacities delimited in the occlusal/incisal third of the tooth, without loss of the structure after eruption, loss of post-eruptive enamel and carious lesions that are limited to 1 or 2 areas, without participation of cusps, tooth sensitivity and often, aesthetic complaints) and severe (post-eruptive losses, history of tooth sensitivity, extensive carious lesions associated with the affected enamel, coronary destruction with pulp involvement, presence of defects in atypical restorations, aesthetic complaints) | 21.5 |
| Thakur et al. (2020) (India) | Wetzel and Reckel scale34 | Degree 1 (isolated hypomineralization of white cream to yellow–brown color, solely located in the uppermost part of the tooth crown (chewing surface), no post-eruptive enamel breakdown); degree 2 (enamel hypomineralization of yellow–brown color affecting almost all humps in the coronal part of the tooth crown combined with a small amount of post-eruptive enamel breakdown), and degree 3 (extensive enamel hypomineralization of yellow–brown color along with extensive post-eruptive enamel breakdown causing changes of the tooth crown morphology) | 29.2 |
| Yi et al. (2020) (China) | Jalevik et al.139 | Mild (demarcated enamel opacities without enamel breakdown), and severe (demarcated enamel opacities with post-eruptive enamel breakdown, atypical caries, atypical restoration, and missing due to MIH) | 39.1 |
| Zawaideh et al. (2011) (Jordania) | Wetzel and Reckel scale34 | Degree 1 (isolated hypomineralization of white cream to yellow–brown color, solely located in the uppermost part of the tooth crown (chewing surface), no post-eruptive enamel breakdown); degree 2 (enamel hypomineralization of yellow–brown color affecting almost all humps in the coronal part of the tooth crown combined with a small amount of post-eruptive enamel breakdown), and degree 3 (extensive enamel hypomineralization of yellow–brown color along with extensive post-eruptive enamel breakdown causing changes of the tooth crown morphology) | 56.0 |
| Villanueva-Gutierrez et al. (2019) (Mexico) | – | Mild (demarcated opacities affected less than one-third of the tooth surface, without post-eruptive enamel breakdown), moderate (demarcated opacities that affected at least one-third but less than two-thirds of the surface, without post-eruptive enamel breakdown; atypical caries lesions could affect less than two-thirds of the surface), and severe (demarcated opacities that affected more than two-thirds of the tooth surface, or the presence of post-eruptive enamel breakdown, atypical caries lesions larger than two-thirds of the surface, or large restaurations with unusual shape, extended to smooth surfaces, or extraction of the tooth because of MIH) | 81.5 |
| Negre-Barber et al. (2016) (Spain) | – | Mild (white, creamy/yellow or dark brown opacities were counted as mild MIH/HSPM), and severe (post-eruptive enamel breakdown, extensive caries with surrounding opacities and atypical restorations, crowns or extractions due to MIH were counted as severe MIH/HSPM) | 28.0 |
| Fernandes et al. (2021) (Brazil) | Ghanim et al.3 | Mild (only color changes—cream, white, yellow, orange, or brown), and severe (fracture and/or atypical restoration/atypical caries/loss due to MIH) | 41.7 |
NR Not reported, NI No information, EAPD European Academy of Pediatric Dentistry1, mDDE modified Developmental Defects of Enamel index.
Sex and geographic location (secondary outcomes)
We further analyzed whether the prevalence results were influenced by study sample size, female/male ratio, geographic location (latitude and longitude) and year of publication (Table 4).
Table 4.
Meta-regression analyses on the effect of female/male ratio (FMR), latitude, longitude and year. Values are provided as estimate (Standard Error) [Variance explained (%)].
| Condition | Sample Size | p-value | FMR | p-value | Latitude | p-value | Longitude | p-value | Year | p-value |
|---|---|---|---|---|---|---|---|---|---|---|
| MIH | − 0.00 (0.00) [12.5] | < 0.001* | − 0.46 (0.37) [0.0] | 0.225 | − 0.00 (0.00) [0.0] | 0.794 | − 0.00 (0.00) [0.0] | 0.211 | − 0.03 (0.01) [0.0] | 0.066 |
| Number of affected molars (%) | ||||||||||
| 1 | 0.00 (0.00) [0.0] | 0.284 | − 0.93 (0.99) [0.0] | 0.344 | − 0.02 (0.01) [0.0] | 0.068 | − 0.00 (0.00) [0.0] | 0.332 | − 0.09 (0.04) [11.6] | 0.023* |
| 2 | − 0.00 (0.00) [0.0] | 0.863 | − 0.13 (0.48) [0.0] | 0.790 | − 0.00 (0.01) [0.0] | 0.890 | − 0.00 (0.00) [0.0] | 0.920 | 0.02 (0.02) [0.0] | 0.301 |
| 3 | − 0.00 (0.00) [0.0] | 0.963 | 0.56 (0.57) [0.0] | 0.327 | 0.00 (0.01) [0.0] | 0.897 | − 0.00 (0.00) [0.0] | 0.629 | 0.03 (0.02) [0.0] | 0.209 |
| 4 | − 0.00 (0.00) [0.0] | 0.227 | 1.31 (1.28) [0.0] | 0.308 | 0.01 (0.01) [0.0] | 0.302 | 0.00 (0.00) [0.0] | 0.139 | 0.06 (0.04) [0.0] | 0.120 |
| Cases with affected incisors | − 0.00 (0.00) [0.0] | 0.433 | − 1.03 (1.05) [0.0] | 0.325 | 0.01 (0.01) [0.0] | 0.584 | 0.00 (0.00) [0.0] | 0.633 | 0.02 (0.06) [0.0] | 0.694 |
| Cases with both molars and incisors affected | − 0.00 (0.00) [0.0] | 0.478 | − 0.85 (0.96) [0.0] | 0.376 | − 0.00 (0.00) [0.0] | 0.074 | 0.00 (0.00) [0.0] | 0.915 | 0.10 (0.03) [0.0] | 0.052 |
| HSPM | − 0.00 (0.00) [0.0] | 0.116 | 0.10(2.51) [0.0] | 0.966 | − 0.00 (0.02) [0.0] | 0.932 | − 0.01 (0.01) [0.0] | 0.338 | − 0.16 (0.18) [0.0] | 0.394 |
MIH Molar-Incisor Hypomineralization, HSPM Hypomineralization of the Second Primary Molars, 95%CI 95% Confidence Interval, FMR Female/Male Ratio. *Significant p-value < 0.05.
Overall, MIH was influenced by the study sample size explaining 7.7% of the accounted heterogeneity, respectively. The year of publication (estimate = − 0.09, p = 0.023) demonstrated a slight influence on the prevalence of MIH cases with one molar affected (explained 11.6% of heterogeneity).
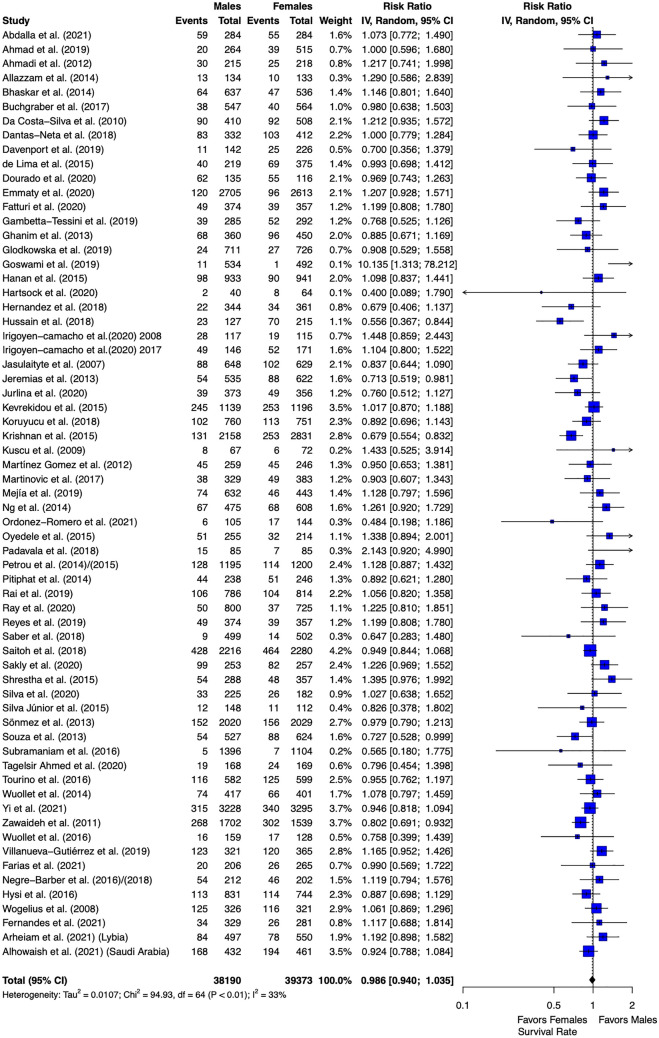
We then explored whether the prevalence between males and females would differ regarding MIH. Meta-analysis confirmed the latter result from meta-regression that MIH is not sex-related and females and males present a non-significant difference on the prevalence of MIH (0.986, 95% CI 0.940–1.035, I2 = 32.6%, p = 0.564) (Fig. 2).
Figure 2.
Forest plot of meta-analysis comparing MIH prevalence of female versus male participants.
We further explored the prevalence of MIH per continent (Table 5). Among the five continents analyzed, America was the continent with highest prevalence (15.3, 95% CI 12.8–18.3, p < 0.001, I2 = 96.3%) and Asia had the lowest prevalence (10.7, 95% CI 78.5–13.5, p < 0.001, I2 = 98.7%). The differences between continents (test for subgroup differences) were not significant (p = 0.1643).
Table 5.
Meta-analysis on the prevalence of MIH per continent.
| Continent | N | Estimate | 95% CI | p-value | I2 (%) |
|---|---|---|---|---|---|
| Africa | 5 | 14.5 | 7.7–25.6 | < 0.001 | 98.1 |
| Asia | 29 | 10.7 | 8.5–13.5 | < 0.001 | 98.7 |
| America | 30 | 15.3 | 12.8–18.3 | < 0.001 | 96.3 |
| Europe | 34 | 14.4 | 12.1–17.1 | < 0.001 | 97.8 |
| Oceania | 1 | 14.7 | 11.2–18.9 | – | – |
| Test for subgroup differences (random effects model) | p-value = 0.1643 | ||||
MIH Molar-Incisor Hypomineralization, HSPM Hypomineralization of the Second Primary Molars, 95%CI 95% Confidence Interval, FMR female/male ratio.
Additional analyses
No publication bias was detected in the overall analysis (Table 2), except for the prevalence of cases with one molar affected (p = 0.004).
Using the SORT recommendation, we concluded the estimates obtained are classified as SORT A, that means, the results provide high level of confidence.
Discussion
Summary of main findings
The results of the present systematic review estimated a pooled prevalence of MIH at 13.5%. The moderate to severe cases of MIH were estimated at 36.3% of all cases. Having three molars affected with MIH is the least probable situation and affected incisors were seen in 36.6% of the cases. The prevalence of HSPM in MIH cases was estimated at 3.6%. The sample size was a significant source of heterogeneity for the overall MIH prevalence and the year of publication for the prevalence of one molar affected. Sex, year of publication and geographic location were not deemed influential factors in almost all the results. Continents showed no different prevalence on MIH, with the American continent displaying the highest prevalence and the Asian continent the lowest.
Quality of the evidence and potential biases in the review process
Overall, these results were categorized with a SORT A recommendation, which means that all studies found coherent conclusions regarding the prevalence of MIH and that these results are consistent and good-quality patient-oriented evidence. Furthermore, this is the first systematic review providing pooled estimates on molars and incisors affected with MIH and HSPM cases.
As previously presented, two previous systematic reviews have focused on the prevalence of MIH. Overall, our results provided similar prevalence to the one reported by Schwendicke et al.5 (13.1%) and slightly above from Zhao et al.6 (14.2%). However, comparing with the latter, the present systematic review expanded the number of countries (49), confirmed the downgrading of alternative case definition of MIH to the overall pooled estimate (while the previous reviews combined classifications), and present new prevalence estimates concerning clinical characteristics of MIH (molas and incisors affected, severity and HSPM).
Regarding the comparison between sexes, our result fully align with those by Schwendicke et al.5 (OR 0.92; 0.81–1.04) and Zhao et al.6 (regression estimate = 0.005, p-value = 0.938), which means that both girls and boys present similar distribution of MIH lesions.
When analyzing the prevalence among continents, the comparison with literature is not reasonable as we only accounted for the EAPD classification, and this explains why Oceania had no studies available (despite two publication by Mahoney et al.118,119). Also, in Zhao et al.6, Africa was the continent with lowest prevalence, yet in our review Asia had the lowest prevalence. The American continent includes for the first time studies from the United States of America and Mexico which may explain a decrease in MIH prevalence from the two previous studies, however remains as the continent (super-region) with highest prevalence.
Regarding the methodological aspects, by comparing the EAPD with alternative diagnostic methods as a subgroup analysis we confirmed the downgrading potential of alternative methods to the overall estimates. Thus, this step methodological assortment into the analyses despite the substantial heterogeneity from the meta-analytical estimations. Also, our analyses on the severity, teeth affected and HSPM were severely reduced because this sort of data is still scarce. Future studies shall provide extensive information on these characteristics to confirm these results. Also, we were unable to explore hypothetical MIH-related factors (both medical, sociodemographic and environmental) once again because of the lack of relevant information, and this should be taken into account in future epidemiological studies.
All in all, readers must bear in mind that although the overall prevalence seems to be constant over the time, new prevalence data has been pooled that contribute to understand the clinical characteristics of this enamel defect entity.
Strengths and potential limitations
This systematic review was conducted following PRISMA a strict guideline for data reporting, a comprehensive literature search and a meticulous predefined protocol. Furthermore, prior to any analysis, we compared the EAPD case definition with other classifications than the EAPD, and we confirmed substantial differences with a downgrading in prevalence when alternative methods were applied. We have attempted to explore ways to mitigate heterogeneity, and all studies used to compute estimates (and that employed the EAPD case definition) were of high methodological quality. Another advantage of this study is that we have expanded the search for potential sources of heterogeneity with the addition of geographic measures and the further assessment into the new prevalence estimates. Also, the number of included participants has increase, which is logical given the increase in studies included, yet this is a point to keep in mind.
Nevertheless, there are a number of limitations important discussing. Almost half of the studies had not fulfilled the criterion of representativeness and this is a point where future studies shall be careful. These results should be prudently analyzed because of the elevated heterogeneity observed in some of the reported estimates, though from our analyses the heterogeneity mostly derives from the variability between regions already discussed in a previous study assessing meta-analysis of prevalence131, rather than the sources of heterogeneity considered as proven through meta-regression.
Also, a number of studies have not employed the EAPD case definition for MIH and after the subgroup analysis aforementioned they were not accounted for the analyses. It is essential that there is a standardization of the classification used, which is a topic already widely discussed in the literature132. Ergo, and given the results of the present systematic review, several challenges may emerge. First, a global partnership between all geographic representative associations shall be attained, to ultimately ensure a standardization of MIH reporting and, certainly, will encourage new and updated epidemiological and clinical data. Second, this suggested consensus will clarify the terminologies and guidelines towards a global alliance that will benefit all people affected by MIH. All in all, these may contribute to overcoming the lack of epidemiological data and a still methodologically unsettled reporting approach.
Only a percentage of the overall included studies reported data on the teeth affected with MIH, the severity of cases or HSPM cases. Several classifications for the severity of MIH have been proposed133,134, and some date before the EAPD 2003, such as Leppäniemi135 or the Wetzel & Reckel scale117,136. Moreover, the MIH Treatment Need Index (MIH-TNI) was recently presented, which is137 part of the Wuerzburg MIH concept. Nevertheless, the lack of a homogeneous definition may have contributed to the heterogeneity of results, making it urgent to establish a consensual severity classification.
Hence, future studies should focus on data on these prevalence characteristics to deepen our knowledge regarding the specifics of MIH. These information are of the utmost relevance for clinicians and may aid the development and implementation of future oral health programs.
Conclusion
The estimated prevalence of MIH was estimated at 13.5%. Moderate to severe cases of MIH were estimated at 36.3%. Affected incisors were seen in 36.6% of the cases. The prevalence of hypomineralization of the second primary molars in MIH cases was estimated at 3.6%. Overall, these results were categorized with a SORT A recommendation.
Supplementary Information
Author contributions
Conceptualization: L.B.L., V.M., J.B. Data curation: L.B.L., P.M., J.B. Formal Analysis: P.M., V.M., J.B. Investigation: L.B.L., V.M., J.B. Methodology: J.B. Project administration: L.B.L., J.B. Resources: J.B. Visualization: J.B. Writing—original draft: L.B.L., V.M., P.M., J.J.M., J.B. Writing—review & editing: L.B.L., V.M., P.M., J.J.M., J.B.
Funding
This work is financed by national funds through the FCT—Foundation for Science and Technology, I.P., under the Project UIDB/04585/2020.
Data availability
Data is provided in the materials of the paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-01541-7.
References
- 1.Weerheijm KL, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens, 2003. Eur. J. Paediatr. Dent. 2003;4:110–113. [PubMed] [Google Scholar]
- 2.Elhennawy K, et al. Structural, mechanical and chemical evaluation of molar-incisor hypomineralization-affected enamel: A systematic review. Arch. Oral. Biol. 2017;83:272–281. doi: 10.1016/j.archoralbio.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Ghanim A, et al. Molar incisor hypomineralisation (MIH) training manual for clinical field surveys and practice. Eur. Arch. Paediatr. Dent. 2017;18:225–242. doi: 10.1007/s40368-017-0293-9. [DOI] [PubMed] [Google Scholar]
- 4.Almuallem Z, Busuttil-Naudi A. Molar incisor hypomineralisation (MIH): An overview. Br. Dent. J. 2018 doi: 10.1038/sj.bdj.2018.814. [DOI] [PubMed] [Google Scholar]
- 5.Schwendicke F, et al. Global burden of molar incisor hypomineralization. J. Dent. 2018;68:10–18. doi: 10.1016/j.jdent.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of molar incisor hypomineralization: Evidence from 70 studies. Int. J. Paediatr. Dent. 2018;28:170–179. doi: 10.1111/ipd.12323. [DOI] [PubMed] [Google Scholar]
- 7.Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Botelho J, et al. Periodontitis and circulating blood cell profiles: A systematic review and meta-analysis. Exp. Hematol. 2021;93:1–13. doi: 10.1016/j.exphem.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Machado V, Escalda C, Proença L, Mendes JJ, Botelho J. Is there a bidirectional association between polycystic ovarian syndrome and periodontitis? A systematic review and meta-analysis. J. Clin. Med. 2020;9:E1961. doi: 10.3390/jcm9061961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins JPT, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928–d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JP, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2. Wiley; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman MG, Weyant R, Hujoel P. JEBDP improves grading system and adopts strength of recommendation taxonomy grading (SORT) for guidelines and systematic reviews. J. Evid. Based Dent. Pract. 2007;7:147–150. doi: 10.1016/j.jebdp.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Balmer R, Toumba J, Godson J, Duggal M. The prevalence of molar incisor hypomineralisation in Northern England and its relationship to socioeconomic status and water fluoridation. Int. J. Paediatr. Dent. 2012;22:250–257. doi: 10.1111/j.1365-263X.2011.01189.x. [DOI] [PubMed] [Google Scholar]
- 14.Balmer R, Toumba KJ, Munyombwe T, Godson J, Duggal MS. The prevalence of incisor hypomineralisation and its relationship with the prevalence of molar incisor hypomineralisation. Eur. Arch. Paediatr. Dent. 2015;16:265–269. doi: 10.1007/s40368-014-0171-7. [DOI] [PubMed] [Google Scholar]
- 15.Biondi AM, et al. Prevalence of molar incisor hypomineralization in the city of Buenos Aires. Acta Odontol. Latinoam. 2011;24:81–85. [PubMed] [Google Scholar]
- 16.Biondi AM, et al. Prevalence of molar-incisor hypomineralization (MIH) in children seeking dental care at the Schools of Dentistry of the University of Buenos Aires (Argentina) and University of la Republica (Uruguay) Acta Odontol. Latinoam. 2012;25:224–230. [PubMed] [Google Scholar]
- 17.Kirthiga M, et al. Prevalence and severity of molar incisor hypomineralization in children aged 11–16 years of a city in Karnataka, Davangere. J. Indian Soc. Pedod. Prev. Dent. 2015;33:213–217. doi: 10.4103/0970-4388.160366. [DOI] [PubMed] [Google Scholar]
- 18.Tagelsir Ahmed A, Soto-Rojas AE, Dean JA, Eckert GJ, Martinez-Mier EA. Prevalence of molar-incisor hypomineralization and other enamel defects and associated sociodemographic determinants in Indiana. J. Am. Dent. Assoc. 2020;151:491–501. doi: 10.1016/j.adaj.2020.02.027. [DOI] [PubMed] [Google Scholar]
- 19.Allazzam SM, Alaki SM, El Meligy OAS. Molar incisor hypomineralization, prevalence, and etiology. Int. J. Dent. 2014;2014:234508. doi: 10.1155/2014/234508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amend S, et al. Prevalence of molar-incisor-hypomineralisation (MIH) among 6–12-year-old children in Central Hesse (Germany) Clin. Oral Investig. 2021;25:2093–2100. doi: 10.1007/s00784-020-03519-7. [DOI] [PubMed] [Google Scholar]
- 21.Bhaskar SA, Hegde S. Molar-incisor hypomineralization: Prevalence, severity and clinical characteristics in 8- to 13-year-old children of Udaipur, India. J. Indian Soc. Pedod. Prev. Dent. 2014;32:322–329. doi: 10.4103/0970-4388.140960. [DOI] [PubMed] [Google Scholar]
- 22.Ghanim A, Morgan M, Mariño R, Bailey D, Manton D. Molar-incisor hypomineralisation: Prevalence and defect characteristics in Iraqi children. Int. J. Paediatr. Dent. 2011;21:413–421. doi: 10.1111/j.1365-263X.2011.01143.x. [DOI] [PubMed] [Google Scholar]
- 23.Martínez Gómez TP, Guinot Jimeno F, Bellet Dalmau LJ, Giner Tarrida L. Prevalence of molar-incisor hypomineralisation observed using transillumination in a group of children from Barcelona (Spain): MIH prevalence using transillumination. Int. J. Paediatr. Dent. 2012;22:100–109. doi: 10.1111/j.1365-263X.2011.01172.x. [DOI] [PubMed] [Google Scholar]
- 24.Hartsock LA, Burnheimer J, Modesto A, Vieira AR. A snapshot of the prevalence of molar incisor hypomineralization and fluorosis in Pittsburgh, Pennsylvania, USA. Pediatr. Dent. 2020;42:36–40. [PubMed] [Google Scholar]
- 25.Hussein AS, Faisal M, Haron M, Ghanim AM, Abu-Hassan MI. Distribution of molar incisor hypomineralization in Malaysian children attending university dental clinic. J. Clin. Pediatr. Dent. 2015;39:219–223. doi: 10.17796/1053-4628-39.3.219. [DOI] [PubMed] [Google Scholar]
- 26.Janković S, Ivanović M, Davidović B, Lecić J. Distribution and characteristics of molar-incisor hypomineralization. Vojnosanit. Pregl. 2014;71:730–734. doi: 10.2298/vsp1408730j. [DOI] [PubMed] [Google Scholar]
- 27.Silva Júnior I, et al. Prevalence and severity of molar incisor hypomineralization in students of Belém Brazil. Pesqui. Bras. Odontopediatr. Clín. Integr. 2015;15:377–385. [Google Scholar]
- 28.Kılınç G, Çetin M, Köse B, Ellidokuz H. Prevalence, aetiology, and treatment of molar incisor hypomineralization in children living in Izmir City (Turkey) Int. J. Paediatr. Dent. 2019;29:775–782. doi: 10.1111/ipd.12508. [DOI] [PubMed] [Google Scholar]
- 29.Kuscu OO, et al. The prevalence of molar incisor hypomineralization (MIH) in a group of children in a highly polluted urban region and a windfarm-green energy island. Int. J. Paediatr. Dent. 2009;19:176–185. doi: 10.1111/j.1365-263X.2008.00945.x. [DOI] [PubMed] [Google Scholar]
- 30.de Lima MDM, et al. Epidemiologic study of molar-incisor hypomineralization in schoolchildren in North-eastern Brazil. Pediatr. Dent. 2015;37:513–519. [PubMed] [Google Scholar]
- 31.Lygidakis NA, Dimou G, Briseniou E. Molar-incisor-hypomineralisation (MIH). Retrospective clinical study in Greek children. I. Prevalence and defect characteristics. Eur. Arch. Paediatr. Dent. 2008;9:200–206. doi: 10.1007/BF03262636. [DOI] [PubMed] [Google Scholar]
- 32.Mejía J, et al. Molar incisor hypomineralization in colombia: Prevalence, severity and associated risk factors. J. Clin. Pediatr. Dent. 2019;43:185–189. doi: 10.17796/1053-4625-43.3.7. [DOI] [PubMed] [Google Scholar]
- 33.Mittal NP, Goyal A, Gauba K, Kapur A. Molar incisor hypomineralisation: Prevalence and clinical presentation in school children of the northern region of India. Eur. Arch. Paediatr. Dent. 2014;15:11–18. doi: 10.1007/s40368-013-0045-4. [DOI] [PubMed] [Google Scholar]
- 34.Portella PD, et al. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: A hierarchical approach. Int. J. Paediatr. Dent. 2019;29:496–506. doi: 10.1111/ipd.12482. [DOI] [PubMed] [Google Scholar]
- 35.Ray P, Mohanty UK, Sethi D, Mahakur M, Sharma G. Prevalence and treatment need of molar incisor hypomineralisation in 8–12 year old school going children of Cuttack, Odisha. JCDR. 2020 doi: 10.7860/JCDR/2020/41782.13558. [DOI] [Google Scholar]
- 36.Reyes MRT, et al. Demarcated opacity in primary teeth increases the prevalence of molar incisor hypomineralization. Braz. Oral Res. 2019;33:e048. doi: 10.1590/1807-3107bor-2019.vol33.0048. [DOI] [PubMed] [Google Scholar]
- 37.Saitoh M, et al. Prevalence of molar incisor hypomineralization and regional differences throughout Japan. Environ. Health Prev. Med. 2018;23:55. doi: 10.1186/s12199-018-0748-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sakly EH, Amor WB, Zokkar N, Charavet C, Amor FB. Prevalence of molar incisor hypomineralisation among school children aged 7–12 years in Tunis, Tunisia. Pesqui. Bras. Odontopediatr. Clín. Integr. 2020;20:160. [Google Scholar]
- 39.Shrestha R, Upadhaya S, Bajracharya M. Prevalence of molar incisor hypomineralisation among school children in Kavre. Kathmandu Univ. Med. J. 2014;12:38–42. doi: 10.3126/kumj.v12i1.13631. [DOI] [PubMed] [Google Scholar]
- 40.Tourino LFPG, et al. Association between molar incisor hypomineralization in schoolchildren and both prenatal and postnatal factors: A population-based study. PLoS ONE. 2016;11:e0156332. doi: 10.1371/journal.pone.0156332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yi X, et al. Prevalence of MIH in children aged 12 to 15 years in Beijing, China. Clin. Oral. Investig. 2021;25:355–361. doi: 10.1007/s00784-020-03546-4. [DOI] [PubMed] [Google Scholar]
- 42.Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH. Molar incisor hypomineralisation: Prevalence in Jordanian children and clinical characteristics. Eur. Arch. Paediatr. Dent. 2011;12:31–36. doi: 10.1007/BF03262776. [DOI] [PubMed] [Google Scholar]
- 43.da Costa-Silva CM, et al. Molar incisor hypomineralization: Prevalence, severity and clinical consequences in Brazilian children. Int. J. Paediatr. Dent. 2010;20:426–434. doi: 10.1111/j.1365-263X.2010.01097.x. [DOI] [PubMed] [Google Scholar]
- 44.Dantas-Neta NB, et al. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz. Oral Res. 2016;30:e117. doi: 10.1590/1807-3107BOR-2016.vol30.0117. [DOI] [PubMed] [Google Scholar]
- 45.Davenport M, et al. Prevalence of molar-incisor hypomineralization in Milwaukee, Wisconsin, USA: A pilot study. Clin. Cosmet. Investig. Dent. 2019;11:109–117. doi: 10.2147/CCIDE.S172736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dourado DG, et al. Molar-incisor hypomineralization in quilombola children and adolescents: A study of prevalence and associated factors. J. Public Health. Dent. 2020 doi: 10.1111/jphd.12429. [DOI] [PubMed] [Google Scholar]
- 47.Elzein R, Chouery E, Abdel-Sater F, Bacho R, Ayoub F. Molar incisor hypomineralisation in Lebanon: Prevalence and clinical characteristics. Eur. Arch. Paediatr. Dent. 2020;21:609–616. doi: 10.1007/s40368-019-00505-w. [DOI] [PubMed] [Google Scholar]
- 48.Fatturi AL, et al. The relationship between molar incisor hypomineralization, dental caries, socioeconomic factors, and polymorphisms in the vitamin D receptor gene: A population-based study. Clin. Oral Investig. 2020;24:3971–3980. doi: 10.1007/s00784-020-03263-y. [DOI] [PubMed] [Google Scholar]
- 49.Rai PM, et al. Prevalence of molar incisor hypomineralization among school children aged 9 to 12 years in Virajpet, Karnataka, India. Open Access Maced. J. Med. Sci. 2019;7:1042–1046. doi: 10.3889/oamjms.2019.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abdalla HE, Abuaffan AH, Kemoli AM. Molar incisor hypomineralization, prevalence, pattern and distribution in Sudanese children. BMC Oral Health. 2021;21:9. doi: 10.1186/s12903-020-01383-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahmad SH, Petrou MA, Alhumrani A, Hashim R, Splieth C. Prevalence of molar-incisor hypomineralisation in an emerging community, and a possible correlation with caries, fluorosis and socioeconomic status. Oral Health Prev. Dent. 2019;17:323–327. doi: 10.3290/j.ohpd.a42725. [DOI] [PubMed] [Google Scholar]
- 52.Ahmadi R, Ramazani N, Nourinasab R. Molar incisor hypomineralization: A study of prevalence and etiology in a group of Iranian children. Iran J. Pediatr. 2012;22:245–251. [PMC free article] [PubMed] [Google Scholar]
- 53.Arslanagic-Muratbegovic A, Markovic N, Zukanovic A, Tiro A, Dzemidzic V. Molar incisor hypomineralization: Prevalence and severity in six to nine-year-old Sarajevo children. Eur. J. Paediatr. Dent. 2020;21:243–247. doi: 10.23804/ejpd.2020.21.03.16. [DOI] [PubMed] [Google Scholar]
- 54.Gambetta-Tessini K, Mariño R, Ghanim A, Calache H, Manton DJ. The impact of MIH/HSPM on the carious lesion severity of schoolchildren from Talca, Chile. Eur. Arch. Paediatr. Dent. 2019;20:417–423. doi: 10.1007/s40368-019-00416-w. [DOI] [PubMed] [Google Scholar]
- 55.Garcia-Margarit M, Catalá-Pizarro M, Montiel-Company JM, Almerich-Silla JM. Epidemiologic study of molar-incisor hypomineralization in 8-year-old Spanish children. Int. J. Paediatr. Dent. 2014;24:14–22. doi: 10.1111/ipd.12020. [DOI] [PubMed] [Google Scholar]
- 56.Ghanim A, Manton D, Bailey D, Mariño R, Morgan M. Risk factors in the occurrence of molar-incisor hypomineralization amongst a group of Iraqi children. Int. J. Paediatr. Dent. 2013;23:197–206. doi: 10.1111/j.1365-263X.2012.01244.x. [DOI] [PubMed] [Google Scholar]
- 57.Glodkowska N, Emerich K. Molar incisor hypomineralization: Prevalence and severity among children from Nothern Poland. Eur. J. Paediatr. Dent. 2019;20:59–66. doi: 10.23804/ejpd.2019.20.01.12. [DOI] [PubMed] [Google Scholar]
- 58.Gurrusquieta BJ, Núñez VMM, López MLAJ. Prevalence of molar incisor hypomineralization in Mexican children. J. Clin. Pediatr. Dent. 2017;41:18–21. doi: 10.17796/1053-4628-41.1.18. [DOI] [PubMed] [Google Scholar]
- 59.Hanan S, et al. Molar-incisor hypomineralization in schoolchildren of Manaus, Brazil. Pesqui. Bras. Odontopediatr. Clín. Integr. 2015;15:309–317. [Google Scholar]
- 60.Hernández M, Boj J-R, Espasa E, Peretz B. First permanent molars and permanent incisors teeth by tooth prevalence of molar–incisor–hypomineralisation in a group of Spanish schoolchildren. Acta Stomatol. Croat. 2018;52:4–11. doi: 10.15644/asc52/1/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hussain G, Al-Halabi M, Kowash M, Hassan A. The Prevalence and severity of molar incisor hypomineralization and molar hypomineralization in Dubai, UAE. J. Dent. Child. 2018;85:102–107. [PubMed] [Google Scholar]
- 62.Irigoyen-Camacho ME, et al. Evaluating the changes in molar incisor hypomineralization prevalence: A comparison of two cross-sectional studies in two elementary schools in Mexico City between 2008 and 2017. Clin. Exp. Dent. Res. 2020;6:82–89. doi: 10.1002/cre2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jasulaityte L, Weerheijm KL, Veerkamp JS. Prevalence of molar-incisor-hypomineralisation among children participating in the Dutch National Epidemiological Survey (2003) Eur. Arch. Paediatr. Dent. 2008;9:218–223. doi: 10.1007/BF03262638. [DOI] [PubMed] [Google Scholar]
- 64.Jeremias F, et al. Dental caries experience and molar-incisor hypomineralization. Acta Odontol. Scand. 2013;71:870–876. doi: 10.3109/00016357.2012.734412. [DOI] [PubMed] [Google Scholar]
- 65.Jurlina D, Uzarevic Z, Ivanisevic Z, Matijevic N, Matijevic M. Prevalence of molar-incisor hypomineralization and caries in eight-year-old children in Croatia. Int. J. Environ. Res. Public Health. 2020;17:E6358. doi: 10.3390/ijerph17176358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kevrekidou A, Kosma I, Arapostathis K, Kotsanos N. Molar incisor hypomineralization of eight- and 14-year-old children: Prevalence, severity, and defect characteristics. Pediatr. Dent. 2015;37:455–461. [PubMed] [Google Scholar]
- 67.Koruyucu M, Özel S, Tuna EB. Prevalence and etiology of molar-incisor hypomineralization (MIH) in the city of Istanbul. J. Dent. Sci. 2018;13:318–328. doi: 10.1016/j.jds.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Krishnan R, Ramesh M, Chalakkal P. Prevalence and characteristics of MIH in school children residing in an endemic fluorosis area of India: An epidemiological study. Eur. Arch. Paediatr. Dent. 2015;16:455–460. doi: 10.1007/s40368-015-0194-8. [DOI] [PubMed] [Google Scholar]
- 69.Kühnisch J, et al. Relationship between caries experience and demarcated hypomineralised lesions (including MIH) in the permanent dentition of 15-year-olds. Clin. Oral. Investig. 2018;22:2013–2019. doi: 10.1007/s00784-017-2299-4. [DOI] [PubMed] [Google Scholar]
- 70.Mishra A, Pandey RK. Molar incisor hypomineralization: An epidemiological study with prevalence and etiological factors in Indian pediatric population. Int. J. Clin. Pediatr. Dent. 2016;9:167–171. doi: 10.5005/jp-journals-10005-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mulic A, Cehajic E, Cehajic E, Tveit AB, Stenhagen KR. How serious is molar incisor hypomineralisation (MIH) among 8- and 9-year-old children in Bosnia-Herzegovina? A clinical study. Eur. J. Paediatr. Dent. 2017;18:153–157. doi: 10.23804/ejpd.2017.18.02.12. [DOI] [PubMed] [Google Scholar]
- 72.Muratbegovic A, Markovic N, Ganibegovic Selimovic M. Molar incisor hypomineralisation in bosnia and herzegovina: Prevalence, aetiology and clinical consequences in medium caries activity population. Eur. Arch. Paediatr. Dent. 2007;8:189–194. doi: 10.1007/BF03262595. [DOI] [PubMed] [Google Scholar]
- 73.Ng JJ, Eu OC, Nair R, Hong CHL. Prevalence of molar incisor hypomineralization (MIH) in Singaporean children. Int. J. Paediatr. Dent. 2015;25:73–78. doi: 10.1111/ipd.12100. [DOI] [PubMed] [Google Scholar]
- 74.Ordonez-Romero I, Jijon-Granja Y, Ubilla-Mazzini W, Porro-Porro L, Alvarez-Giler G. Distribution of molar incisor hypomineralization in Ecuadorian children. Dent. Hypotheses. 2019;10:65. [Google Scholar]
- 75.Oyedele TA, Folayan MO, Adekoya-Sofowora CA, Oziegbe EO, Esan TA. Prevalence, pattern and severity of molar incisor hypomineralisation in 8- to 10-year-old school children in Ile-Ife, Nigeria. Eur. Arch. Paediatr. Dent. 2015;16:277–282. doi: 10.1007/s40368-015-0175-y. [DOI] [PubMed] [Google Scholar]
- 76.Padavala S, Sukumaran G. Molar incisor hypomineralization and its prevalence. Contemp. Clin. Dent. 2018;9:246. doi: 10.4103/ccd.ccd_161_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Parikh DR, Ganesh M, Bhaskar V. Prevalence and characteristics of molar incisor hypomineralisation (MIH) in the child population residing in Gandhinagar, Gujarat, India. Eur. Arch. Paediatr. Dent. 2012;13:21–26. doi: 10.1007/BF03262836. [DOI] [PubMed] [Google Scholar]
- 78.Petrou MA, et al. Prevalence of molar-incisor-hypomineralisation among school children in four German cities. Int. J. Paediatr. Dent. 2014;24:434–440. doi: 10.1111/ipd.12089. [DOI] [PubMed] [Google Scholar]
- 79.Pitiphat W, Savisit R, Chansamak N, Subarnbhesaj A. Molar incisor hypomineralization and dental caries in six- to seven-year-old Thai children. Pediatr. Dent. 2014;36:478–482. [PubMed] [Google Scholar]
- 80.Saber F, Waly N, Moheb D. Prevalence of molar incisor hypomineralisation in a group of Egyptian children using the short form: A cross-sectional study. Eur. Arch. Paediatr. Dent. 2018;19:337–345. doi: 10.1007/s40368-018-0364-6. [DOI] [PubMed] [Google Scholar]
- 81.Schmalfuss A, Stenhagen KR, Tveit AB, Crossner C-G, Espelid I. Canines are affected in 16-year-olds with molar-incisor hypomineralisation (MIH): An epidemiological study based on the Tromsø study: ‘Fit Futures’. Eur. Arch. Paediatr. Dent. 2016;17:107–113. doi: 10.1007/s40368-015-0216-6. [DOI] [PubMed] [Google Scholar]
- 82.Sidhu N, Wang Y, Barrett E, Casas M. Prevalence and presentation patterns of enamel hypomineralisation (MIH and HSPM) among paediatric hospital dental patients in Toronto, Canada: A cross-sectional study. Eur. Arch. Paediatr. Dent. 2020;21:263–270. doi: 10.1007/s40368-019-00477-x. [DOI] [PubMed] [Google Scholar]
- 83.da Silva FMF, et al. Defining the prevalence of molar incisor hypomineralization in Brazil. Pesqui. Bras. Odontopediatr. Clín. Integr. 2020;20:e5146. [Google Scholar]
- 84.Singh R, Srivastava B, Gupta N. Prevalence and pattern of molar incisor hypomineralization in Delhi region. J. Anat. Soc. India. 2020;69:150. [Google Scholar]
- 85.Souza JF, et al. Aetiology of molar-incisor hypomineralisation (MIH) in Brazilian children. Eur. Arch. Paediatr. Dent. 2013 doi: 10.1007/s40368-013-0054-3. [DOI] [PubMed] [Google Scholar]
- 86.Subramaniam P, Gupta T, Sharma A. Prevalence of molar incisor hypomineralization in 7-9-year-old children of Bengaluru City, India. Contemp. Clin. Dent. 2016;7:11–15. doi: 10.4103/0976-237X.177091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Temilola OD, Folayan MO, Oyedele T. The prevalence and pattern of deciduous molar hypomineralization and molar-incisor hypomineralization in children from a suburban population in Nigeria. BMC Oral Health. 2015;15:73. doi: 10.1186/s12903-015-0059-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kemoli AM. Prevalence of molar incisor hypomineralisation in six to eight year-olds in two rural divisions in Kenya. East Afr. Med. J. 2008;85:514–519. doi: 10.4314/eamj.v85i10.9668. [DOI] [PubMed] [Google Scholar]
- 89.Wuollet E, Laisi S, Salmela E, Ess A, Alaluusua S. Background factors of molar-incisor hypomineralization in a group of Finnish children. Acta Odontol. Scand. 2014;72:963–969. doi: 10.3109/00016357.2014.931459. [DOI] [PubMed] [Google Scholar]
- 90.Wuollet E, Laisi S, Alaluusua S, Waltimo-Sirén J. The association between molar-incisor hypomineralization and dental caries with socioeconomic status as an explanatory variable in a group of Finnish children. Int. J. Environ. Res. Public Health. 2018;15:E1324. doi: 10.3390/ijerph15071324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Buchgraber B, Kqiku L, Ebeleseder KA. Molar incisor hypomineralization: Proportion and severity in primary public school children in Graz, Austria. Clin. Oral Investig. 2018;22:757–762. doi: 10.1007/s00784-017-2150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cho S-Y, Ki Y, Chu V. Molar incisor hypomineralization in Hong Kong Chinese children. Int. J. Paediatr. Dent. 2008;18:348–352. doi: 10.1111/j.1365-263X.2008.00927.x. [DOI] [PubMed] [Google Scholar]
- 93.Dantas-Neta NB, et al. Factors associated with molar-incisor hypomineralisation in schoolchildren aged 8–10 years: A case-control study. Int. J. Paediatr. Dent. 2018;28:570–577. doi: 10.1111/ipd.12412. [DOI] [PubMed] [Google Scholar]
- 94.Thakur H, Kaur A, Singh N, Singh R, Kumar S. Prevalence and clinical characteristics of molar-incisor hypomineralization in 8–16-year-old children in industrial town of Solan District of Himachal Pradesh. Int. J. Clin. Pediatr. Dent. 2020;13:230–234. doi: 10.5005/jp-journals-10005-1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sosa-Soto J, et al. Molar incisor hypomineralization (MIH): Prevalence and degree of severity in a Mexican pediatric population living in an endemic fluorosis area. J. Public Health Dent. 2021 doi: 10.1111/jphd.12446. [DOI] [PubMed] [Google Scholar]
- 96.Martinović B, et al. Prevalence, characteristics and severity of hypomineralization of the first permanent molars and incisors in children from the northern part of Kosovo and Metohija. Srp. Arh. Celok. Lek. 2017;145:364–369. [Google Scholar]
- 97.Fteita D, Ali A, Alaluusua S. Molar-incisor hypomineralization (MIH) in a group of school-aged children in Benghazi, Libya. Eur. Arch. Paediatr. Dent. 2006;7:92–95. doi: 10.1007/BF03320821. [DOI] [PubMed] [Google Scholar]
- 98.Goswami M, Bhushan U, Pandiyan R, Sharma S. Molar incisor hypomineralization-an emerging burden: A short study on prevalence and clinical characteristics in Central Delhi, India. Int. J. Clin. Pediatr. Dent. 2019;12:211–214. doi: 10.5005/jp-journals-10005-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Emmatty TB, et al. The prevalence of molar incisor hypomineralization of school children in and around Muvattupuzha, Kerala. J. Indian Soc. Pedod. Prev. Dent. 2020;38:14–19. doi: 10.4103/JISPPD.JISPPD_152_18. [DOI] [PubMed] [Google Scholar]
- 100.Dietrich G, Sperling S, Hetzer G. Molar incisor hypomineralisation in a group of children and adolescents living in Dresden (Germany) Eur. J. Paediatr. Dent. 2003;4:133–137. [PubMed] [Google Scholar]
- 101.Villanueva-Gutiérrez T, et al. Prevalence and severity of molar-incisor hypomineralization, maternal education, and dental caries: A cross-sectional study of Mexican Schoolchildren with low socioeconomic status. J. Int. Soc. Prev. Community Dent. 2019;9:513–521. doi: 10.4103/jispcd.JISPCD_130_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wuollet E, Laisi S, Salmela E, Ess A, Alaluusua S. Molar-incisor hypomineralization and the association with childhood illnesses and antibiotics in a group of Finnish children. Acta Odontol. Scand. 2016;74:416–422. doi: 10.3109/00016357.2016.1172342. [DOI] [PubMed] [Google Scholar]
- 103.Farias L, et al. Presence of molar-incisor hypomineralization is associated with dental caries in Brazilian schoolchildren. Braz. Oral Res. 2021;35:e13. doi: 10.1590/1807-3107bor-2021.vol35.0013. [DOI] [PubMed] [Google Scholar]
- 104.Yannam S, Amarlal D, Rekha C. Prevalence of molar incisor hypomineralization in school children aged 8–12 years in Chennai. J. Indian Soc. Pedod. Prev. Dent. 2016;34:134. doi: 10.4103/0970-4388.180438. [DOI] [PubMed] [Google Scholar]
- 105.Rodrigues F, et al. Molar-incisor hypomineralization in school children of São Luis, Brazil Maranhão: Prevalence and associated factors. Pesqui. Bras. Odontopediatr. Clín. Integr. 2015;15:271–278. [Google Scholar]
- 106.Sönmez H, Yıldırım G, Bezgin T. Putative factors associated with molar incisor hypomineralisation: An epidemiological study. Eur. Arch. Paediatr. Dent. 2013;14:375–380. doi: 10.1007/s40368-013-0012-0. [DOI] [PubMed] [Google Scholar]
- 107.Calderara PC, et al. The prevalence of molar incisor hypomineralisation (MIH) in a group of Italian school children. Eur. J. Paediatr. Dent. 2005;6:79–83. [PubMed] [Google Scholar]
- 108.LópezJordi MDC, et al. Comparison of the prevalence of molar incisor hypomineralization among children with different health care coverage in the cities of Buenos Aires (Argentina) and Montevideo (Uruguay) Salud. Colect. 2014;10:243–251. doi: 10.18294/sc.2014.225. [DOI] [PubMed] [Google Scholar]
- 109.Petrou MA, et al. Severity of MIH findings at tooth surface level among German school children. Eur. Arch. Paediatr. Dent. 2015;16:271–276. doi: 10.1007/s40368-015-0176-x. [DOI] [PubMed] [Google Scholar]
- 110.Negre-Barber A, Montiel-Company JM, Boronat-Catalá M, Catalá-Pizarro M, Almerich-Silla JM. Hypomineralized second primary molars as predictor of molar incisor hypomineralization. Sci. Rep. 2016;6:31929. doi: 10.1038/srep31929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Negre-Barber A, Montiel-Company JM, Catalá-Pizarro M, Almerich-Silla JM. Degree of severity of molar incisor hypomineralization and its relation to dental caries. Sci. Rep. 2018;8:1248. doi: 10.1038/s41598-018-19821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Soviero V, Haubek D, Trindade C, Da Matta T, Poulsen S. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol. Scand. 2009;67:170–175. doi: 10.1080/00016350902758607. [DOI] [PubMed] [Google Scholar]
- 113.Kohlboeck G, et al. Is there a relationship between hyperactivity/inattention symptoms and poor oral health? Results from the GINIplus and LISAplus study. Clin. Oral. Invest. 2013;17:1329–1338. doi: 10.1007/s00784-012-0829-7. [DOI] [PubMed] [Google Scholar]
- 114.Hysi D, et al. Prevalence and aetiology of Molar-Incisor Hypomineralisation among children aged 8–10 years in Tirana, Albania. Eur. J. Paediatr. Dent. 2016;17:75–79. [PubMed] [Google Scholar]
- 115.Elfrink MEC, et al. Deciduous molar hypomineralization and molar incisor hypomineralization. J. Dent. Res. 2012;91:551–555. doi: 10.1177/0022034512440450. [DOI] [PubMed] [Google Scholar]
- 116.Heitmüller D, et al. Is there a positive relationship between molar incisor hypomineralisations and the presence of dental caries? Caries in children with MIH. Int. J. Pediatr. Dent. 2013;23:116–124. doi: 10.1111/j.1365-263X.2012.01233.x. [DOI] [PubMed] [Google Scholar]
- 117.Preusser SE, Ferring V, Wleklinski C, Wetzel W-E. Prevalence and severity of molar incisor hypomineralization in a region of Germany ? A brief communication. J. Public Health Dent. 2007;67:148–150. doi: 10.1111/j.1752-7325.2007.00040.x. [DOI] [PubMed] [Google Scholar]
- 118.Mahoney EK, Morrison DG. The prevalence of molar-incisor hypomineralisation (MIH) in Wainuiomata children. N. Z. Dent. J. 2009;105:121–127. [PubMed] [Google Scholar]
- 119.Mahoney EK, Morrison DG. Further examination of the prevalence of MIH in the Wellington region. N. Z. Dent. J. 2011;107:79–84. [PubMed] [Google Scholar]
- 120.Wogelius P, Haubek D, Poulsen S. Prevalence and distribution of demarcated opacities in permanent 1st molars and incisors in 6 to 8-year-old Danish children. Acta Odontol. Scand. 2008;66:58–64. doi: 10.1080/00016350801926941. [DOI] [PubMed] [Google Scholar]
- 121.Grošelj M, Jan J. Molar incisor hypomineralisation and dental caries among children in Slovenia. Eur. J. Paediatr. Dent. 2013;14:241–245. [PubMed] [Google Scholar]
- 122.Fernandes IC, Forte FDS, Sampaio FC. Molar-incisor hypomineralization (MIH), dental fluorosis, and caries in rural areas with different fluoride levels in the drinking water. Int. J. Paediatr. Dent. 2021;31:475–482. doi: 10.1111/ipd.12728. [DOI] [PubMed] [Google Scholar]
- 123.Freitas Fernandes LH, et al. Incisor molar hypomineralization and quality of life: A population-based study with Brazilian schoolchildren. Int. J. Dent. 2021;2021:6655771. doi: 10.1155/2021/6655771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Arheiam A, et al. Prevalence, distribution, characteristics and associated factors of molar-incisor hypo-mineralisation among Libyan schoolchildren: A cross-sectional survey. Eur. Arch. Paediatr. Dent. 2021 doi: 10.1007/s40368-020-00594-y. [DOI] [PubMed] [Google Scholar]
- 125.Alhowaish L, Baidas L, Aldhubaiban M, Bello LL, Al-Hammad N. Etiology of molar-incisor hypomineralization (MIH): A cross-sectional study of Saudi children. Children. 2021;8:466. doi: 10.3390/children8060466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jasulaityte L, Veerkamp JS, Weerheijm KL. Molar incisor hypomineralization: Review and prevalence data from the study of primary school children in Kaunas/Lithuania. Eur. Arch. Paediatr. Dent. 2007;8:87–94. doi: 10.1007/BF03262575. [DOI] [PubMed] [Google Scholar]
- 127.Gambetta-Tessini K, Mariño R, Ghanim A, Calache H, Manton D. Carious lesion severity and demarcated hypomineralized lesions of tooth enamel in schoolchildren from Melbourne, Australia. Aust. Dent. J. 2018;63:365–373. doi: 10.1111/adj.12626. [DOI] [PubMed] [Google Scholar]
- 128.Rai A. et al. Molar Incisor Hypomineralization: Prevalence and Risk Factors Among 7-9 Years Old School Children in Muradnagar, Ghaziabad. Open Dent J.12, 714–722. 10.2174/1745017901814010714 (2018). [DOI] [PMC free article] [PubMed]
- 129.Clarkson J. Review of terminology, classifications, and indices of developmental defects of enamel. Advances in dental research, 3(2), 104–109. 10.1177/08959374890030020601 (1989). [DOI] [PubMed]
- 130.Mathu-Muju K, Wright JT. Diagnosis and treatment of molar incisor hypomineralization. Compend. Contin. Educ. Dent. 2006;27:604–610. [PubMed] [Google Scholar]
- 131.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 132.Bandeira Lopes L, Machado V, Botelho J, Haubek D. Molar-incisor hypomineralization: An umbrella review. Acta Odontol. Scand. 2021;79:359–369. doi: 10.1080/00016357.2020.1863461. [DOI] [PubMed] [Google Scholar]
- 133.Ghanim A, Elfrink M, Weerheijm K, Mariño R, Manton D. A practical method for use in epidemiological studies on enamel hypomineralisation. Eur. Arch. Paediatr. Dent. 2015;16:235–246. doi: 10.1007/s40368-015-0178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lygidakis NA, et al. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An EAPD policy document. Eur. Arch. Paediatr. Dent. 2010;11:75–81. doi: 10.1007/BF03262716. [DOI] [PubMed] [Google Scholar]
- 135.Leppäniemi A, Lukinmaa PL, Alaluusua S. Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res. 2001;35:36–40. doi: 10.1159/000047428. [DOI] [PubMed] [Google Scholar]
- 136.Wetzel WE, Reckel U. Defective 6-year molars increasing: An inquiry. Zahnarztl. Mitt. 1991;81:650–652. [PubMed] [Google Scholar]
- 137.Steffen R, Krämer N, Bekes K. The Würzburg MIH concept: the MIH treatment need index (MIH TNI): A new index to assess and plan treatment in patients with molar incisior hypomineralisation (MIH) Eur. Arch. Paediatr. Dent. 2017;18:355–361. doi: 10.1007/s40368-017-0301-0. [DOI] [PubMed] [Google Scholar]
- 138.Chawla, N., Messer, L. B., & Silva, M. Clinical studies on molar-incisor-hypomineralisation part 2: development of a severity index. European archives of paediatric dentistry : official journal of the European Academy of Paediatric Dentistry, 9(4), 191–199. 10.1007/BF03262635 (2008). [DOI] [PubMed]
- 139.Jälevik, B. Prevalence and Diagnosis of Molar-Incisor-Hypomineralisation (MIH): A systematic review. European archives of paediatric dentistry : official journal of the European Academy of Paediatric Dentistry, 11(2), 59–64. 10.1007/BF03262714 (2010). [DOI] [PubMed]
- 140.Koch, G. et al. Epidemiologic study of idiopathic enamel hypomineralization in permanent teeth of Swedish children. Community Dent Oral Epidemiol.15, 279–85 (1987). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is provided in the materials of the paper.