Abstract
Introduction
The locking attachment plate (LAP) can be added to a locking compression plate (LCP) to allow the fixation of locking screws bicortically around a femoral implant. We aimed to examine surgical and fracture characteristics associated with healing for periprosthetic femur fractures (PPFFx) treated with constructs employing LAP fixation. We hypothesize that the addition of an LAP provides stable peri-implant fixation.
Materials &Methods
We retrospectively reviewed a consecutive series of 28 PPFFx surgically treated with LCP-LAP constructs by 4 surgeons from 2015-2020. Fractures were classified and grouped using the Vancouver Classification System and included 12 B1, 2 B2, 11 C fractures, and 3 fractures around other stemmed implants. Primary outcome measures included hardware failure such as screw pullout, broken screws, and plate fracture. Clinical complications including infection, non-union, malunion, and reoperation were recorded.
Results
No LAP failures, screw pullout, or broken screws were observed. Two fractured plates (7.1%) occurred in patients with Vancouver C fracture types. Overall complication rate was 17.9% and included 3 non-unions, 1 deep infection, and 1 implant loosening with painful hardware, each requiring reoperation. Differences were observed between unions and nonunions for total number of screws (12.4 vs 14.7, P = .005) and number of locking screws used (8.04 vs 11.3, P = .03).
Conclusion
The LAP provides adequate fixation and low failure rates where fixation is required around a well-fixed stem. When failures occur, it is from plate breakage and not due to failure of fixation at the area of plate-stem overlap.
Keywords: periprosthetic fracture, plate, femur fracture, locking plate attachment, fixation
Introduction
The surgical treatment of periprosthetic femur fractures (PPFFx) around prior total hip or knee components or an intramedullary implant is guided by fracture location and the stability of the stem prosthesis. Fractures with an unstable stem are typically treated with revision surgery, while fractures around or distal to a well-fixed stem are treated with open reduction internal fixation (ORIF) using plate fixation. 1 Fixation options to host bone may be limited by the stem of the prosthesis. As PPFFx are increasing in number, more fractures are likely to occur around well-fixed prostheses, especially revision prosthesis or other devices such as intramedullary nails. Often cortices of bone are thin in osteoporotic individuals making fixation even more challenging. 2 Historically, fixation options included the use of unicortical locking screws, angled screws around the prosthesis, cerclage cables and the use of multiple plates or allograft struts. The primary failure mode of fixation has been screw pullout or cable breakage due to inadequate fixation and construct stability. 3
The locking attachment plate (LAP, Depuy-Synthes, Warsaw, IN) is a fixed-angled construct that provides the ability to avoid the intramedullary stem by aiming screws around the implant (Figure 1 and Figure 2). The LAP can be installed on a locking compression plate (LCP) or a variable angle LCP (VA-LCP) and is designed with 4 diagonally fixed arms that allow locking screws to be placed anteriorly or posteriorly around the implant. In a study using artificial femurs, the LAP-LCP construct provided superior mechanical stability and strength compared to a cerclage cable-LCP construct. 4 The LAP has also been successfully used in a case series of patients with periprosthetic fractures of the humerus, femur, and tibia. 5 There is a paucity of clinical literature available regarding the specific application and success of the LAP. We aimed to examine surgical and fracture characteristics associated with healing for a consecutive series of PPFFx treated with constructs utilizing a LAP. We hypothesize that the addition of LAP provides a stable peri-implant fixation while preventing hardware failure at the site of LAP and around an existing femoral prosthesis.
Figure 1.
Intraoperative image of LAP-LCP construct.
Figure 2.
Postoperative lateral radiograph demonstrating placement of LAP-LCP construct.
Methods
Following Institutional Review Board approval, a retrospective review of medical records was conducted to identify all patients with PPFFx treated surgically with LAP-LCP construct at a single academic level-1 trauma center. Periprosthetic fractures were treated with revision surgery if the stem was radiographically loose. If the treating surgeon deemed the stem stable, ORIF was performed in a lateral position on a radiolucent table. In most cases, the surgical approach included elevating the vastus to expose the femur while leaving the origin of the vastus from the greater trochanter intact. In a few cases a minimally invasive approach could be used for placement of the distal condylar portion of the plate when feasible. Often a full, open approach was required for fracture reduction and plate and LAP placement. The stem was checked for stability under direct visualization. The fracture was then reduced using clamps, and 1.0 mm cables (Depuy-Synthes, Westchester, PA) were used to hold the reduction. Fluoroscopy was used to assess reduction. In 19 cases,a condylar plate (4.5 mm VA-LCP Curved Condylar plate, Depuy Synthes Trauma, Westchester, PA) was selected to span the entire bone. The plate usually required contouring with a table-top bender to fit the profile of the greater trochanter. In 9 cases a 4.5 mm Curved Locking Compression Plate (Depuy Synthes Trauma, Westchester, PA) was utilized. The plate was placed to avoid strippage of the vastus insertion into the trochanter. The plate was applied and brought to the bone with cortical screws. Locking screws were only placed in the condylar portion of the bone in the distal femur. Our approach was first to try to angle cortical screws around the stem of the prosthesis. If 4 screws could be placed with solid fixation, a LAP was not used and those cases were excluded from this study. If the surgeon was not satisfied with the proximal fixation using cortical screws around the intramedullary femoral stem, then 1 or 2 LAP devices were applied for supplemental fixation. The four-hole or eight-hole LAP devices were available for use in each case. Unicortical 3.5 mm locking screws were placed in as many of these holes as possible for additional fixation (Figure 1). Attempts were made to try to get fixation on both the anterior and posterior sides of the existing stem (Figure 3 and Figure 4). Postoperatively, all patients were mobilized and weight bearing restrictions varied between treating surgeons, particularly in cases where the fixation was felt to be particularly tenuous.
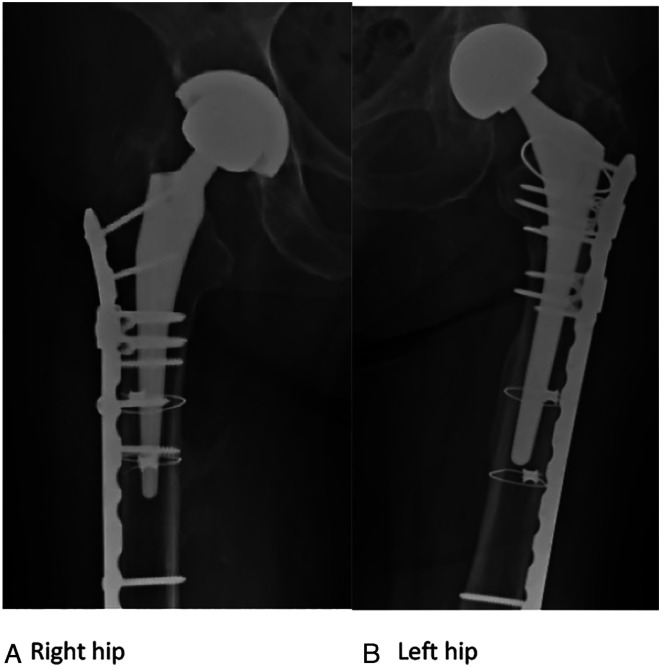
Figure 3.
(A) and (B): Injury radiographs of single individual sustaining bilateral Vancouver B1 fractures.
Figure 4.
(A) and (B): 12 month post-op, bilateral Vancouver (B) 1 fractures treated with LAP-LCP.
Individual charts were reviewed to record demographic factors including age, gender, body mass index (BMI), smoking history, and comorbidities such as diabetes, peripheral vascular disease, chronic kidney disease, and osteoporosis. Injury radiographs were reviewed to identify fracture location and classified using the Vancouver Classification System. 6 Operative notes were reviewed to determine final operative treatment (open reduction internal fixation (ORIF) vs Revision arthroplasty plus ORIF). Implant characteristics recorded included plate type, number of total screws, number of locking screws, number of cortical screws, number of LAP used, position of LAP in relation to fracture, number of screws used in LAP, and position of screws in LAP in relation to implant (anterior vs posterior). The working length (WL), defined as the distance measured between the nearest proximal and distal screws to the fracture site, was recorded. 7 To correct for x-ray magnification, the diameter of a known 4.5 mm screw was measured, and that ratio was applied to the measured working length to determine the corrected WL. Primary outcome measures included hardware failures such as screw pull out, broken screws, and plate fracture. Other outcomes recorded were number and types of clinical complications, including infection, nonunion, malunion, reoperation. Review of medical records were used to evaluate length of follow-up and weight-bearing status postoperatively and at 3- and 6-months post operation.
A total of 28 PPFFx were treated surgically by 4 surgeons with a LCP-LAP construct from July 2015- May 2020. Of the 28 fractures, 12 were Vancouver B1, 2 Vancouver B2, and 11 Vancouver C. Three fractures were around a distal femoral replacement, femoral nail, and total knee arthroplasty and classified as “other.” Sixteen fractures involved a primary implant and 12 involved revision implants. Twenty-five were treated with plate alone and 3 were treated with revision in addition to plate fixation. These fractures occurred in 20 female and 8 male patients. The average age at operation was 73.3 years and average BMI was 28.4 (Table 1). Basic implant characteristics, including construct WL, are recorded in Table 2. One patient, with a Vancouver B1 fracture, was excluded from WL calculation due to unobtainable post-op radiographs. No significant differences were observed between fracture types for age (P = .263), BMI (P = .320), total screws used (P = .121), total locking screws used (P = .331), total cortical screws used (P = .270), working length (P = .403), and average follow-up length (P = .828).
Table 1.
Patient Demographics.
| Total | Vancouver B1 | Vancouver B2 | Vancouver C | Other | |
|---|---|---|---|---|---|
| Number of patients | 28 | 12 | 2 | 11 | 3 |
| Gender | 20 female | 9 female | 2 female | 6 female | 3 female |
| 8 male | 3 male | — | 5 male | — | |
| Mean age at surgery (years) | 73.3 | 77.9 | 74.5 | 66 | 81 |
| BMI | 28.4 | 26.8 | 33.1 | 30.3 | 24.4 |
| Stem type | 25 uncemented | 12 uncemented | 2 uncemented | 10 uncemented | 1 uncemented |
| 3 cemented | 1 cemented | 2 cemented | |||
| Implant | 16 primary | 8 primary | 2 primary | 5 primary | 1 primary |
| 12 revision | 4 revision | 6 revision | 2 revision | ||
| ORIF vs Revision+ORIF | 25 ORIF | 11 ORIF | 2 Rev+ORIF | 11 ORIF | 3 ORIF |
| 3 Rev+ORIF | 1 Rev+ORIF | ||||
| Average length of follow-up (months) | 9.8 | 12.4 | 6.5 | 13.5 | 6.7 |
Table 2.
Plate and screw characteristics by fracture classification.
| Total | Vancouver B1 | Vancouver B2 | Vancouver C | Other | |
|---|---|---|---|---|---|
| # of LAP used | 16 1 LAP | 5 1 LAP | 2 1 LAP | 7 1 LAP | 2 1 LAP |
| 12 2 LAP | 7 2 LAP | 4 2 LAP | 1 2 LAP | ||
| Average number of screws (total) | 12.6 | 12.7 | 9.5 | 13.8 | 10 |
| Average number of locking screws | 8.4 | 7.7 | 7.5 | 10 | 6 |
| Average number of cortical screws | 4.1 | 5 | 2 | 3.5 | 3.7 |
| Average working length (mm) | 123.99 | 140.7 | 146.5 | 108.1 | 105.99 |
The average follow-up length was 9.8 months, range 2-51 months. Three patients died during this interval and 2 more patients never returned for follow-up appointments. Weight bearing restrictions varied between surgeons and the perceived amount of fixation and bone quality. Seven patients were non-weight bearing, 4 touch-down weight bearing, 10 partial weight bearing, and 7 weight bearing as tolerated immediately after surgery.
Data in our study were summarized with univariate statistics. We used a t-test to draw comparisons between groups and a single factor ANOVA was used to determine differences in demographics, hardware specifics, and working length. A P-value of <.05 was set as the threshold for statistical significance.
Results
All 28 PPFFx were treated surgically using an LCP with either 1 or 2 LAP. In total, 16 cases utilized 1 LAP and 12 cases utilized 2 LAP (Table 2). On average, 3.3 screws were used in each LAP device (range 2-4 with 0-2 screws anterior and 0-2 screws posterior). We did not observe any LAP failures, LAP screw pull-out, or broken LAP screws at most recent follow-up.
Overall complication rates for the cohort was 17.9% (5/28), including 3 non-unions (2 with broken plates), 1 deep infection, and 1 loosening of a revision femoral stem, all of which required reoperations. Two LCPs fractured with fracture nonunion. These both occurred in patients with Vancouver C fractures, around revision femoral stems at 8 months and 5 months post-op. The first, occurring at 8 months post-op, was a high energy fracture with a large bone defect that was electively bone grafted prior to plate breakage (Figure 5). The second, occurring at 5 months post-op, was sustained intraoperation while reducing the hip after revision surgery. The patient was noted having severe metallosis with significant soft tissue damage and little remaining bone proximal around the stem, as well as underlying diagnosis of recalcitrant osteoporosis that was not diagnosed and treated until a post-op referral to endocrinology (Figure 6). The third nonunion, without hardware failure, occurred in a patient with aVancouver B1 fracture around a revision stem. The patient was referred to endocrinology postoperatively and started on Vitamin D supplementation. At 10 months post-op the patient developed pain around the previous fracture site and nonunion was diagnosed on CT scan. Among the 3 nonunion cases, there was a difference observed compared to 25 unions in total number of screws (union average 12.4 vs nonunion average 14.7, P = .005) and number of locking screws used (union 8.0 vs nonunion 11.3, P = .03). While the 3 non-union cases were around this revision stems, this association failed to reach significance (P = .06). There was also no association observed in non-union cases when 1 vs 2 LAP were utilized (P = .56). There was no difference observed between working length (118.7 mm vs 166.2 mm, P = .42) and total number of cortical screws used (4.2 vs 3.3, P = .47) between instances of union and nonunion.
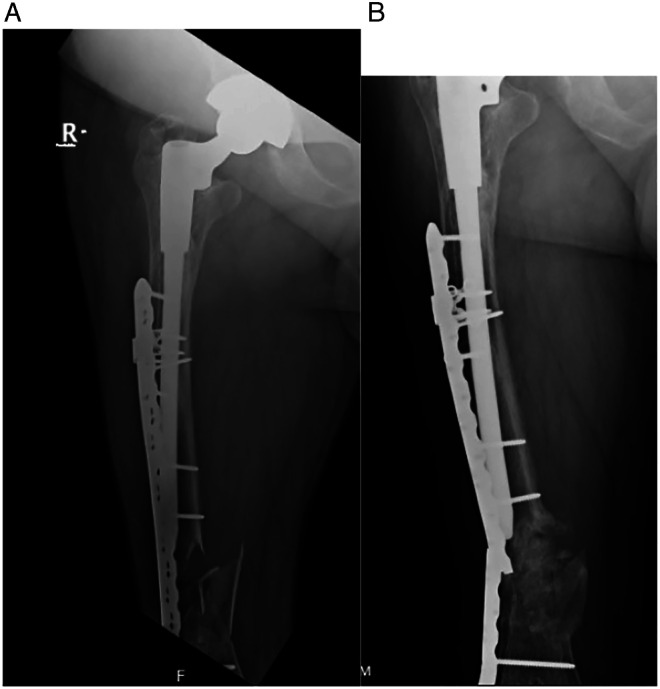
Figure 5.
(A) and (B): (A) A. Post-op AP femur, Vancouver C fracture with bone defect, (B) AP femur, 8 months post-op Vancouver C fracture non-union with plate fracture.
Figure 6.
(A) and (B): (A) Post-op AP femur, Vancouver C fracture. (B) AP femur, 5 months post-op Vancouver C fracture non-union with plate fracture.
The average working length among all cases in our series was 124.0 mm. There was no difference in working length between fracture types (P = .403). In addition, we found no difference in working length when 1 vs 2 LAP were used (1 LAP 117.7 mm vs two LAP 133.1 mm, P = .477). There was no difference in working length in patients with complications vs those with clinical and radiographic healing (healed 116.9 mm vs complications 165.0 mm, P = .227).
Discussion
In our series of 28 complex PPFFx treated surgically using a LCP-LAP construct, we observed no cases of LAP or screw failure. Despite limited opportunity for bicortical screw placement, the addition of the LAP gave sufficient fixation even in these difficult cases. Failure did not occur at the LAP device or from failure of fixation. Our largest complication was nonunion with plate breakage. Three out of twenty-eight subjects (10.7%) developed nonunion and in 2 cases, plate breakage. There were no associations between fixation failure, nonunion and WL of the plate.
The current literature on the clinical application of LAP is limited. Dumpies et al treated 7 Vancouver B1 and 3 Vancouver C PPFFx utilizing LCP-LAP constructs with no reported failures of LAP or screws. 5 All of their fractures were around primary hip implants presenting after minor trauma (ie same-level fall). In each case, ORIF was performed and 2 LAPs, 1 4-hole and 1 8-hole, were selected. The only complication recorded was a case of chronic infection in a patient with a Vancouver C fracture.5Our study has a larger sample size with more variety and complexity of presenting fractures including 12 fractures around revision implants and some high-energy injuries. In most of our patients, only 1 LAP was required (16 of 28). We did not find that the use of either 1 or 2 LAPs resulted in failures at the LAP site.
While 3 non-unions occurred in our series, the overall rate (10.7%) is comparable to that in the literature (6.7-13%).8-10 Recent literature evaluating the incidence of reoperation after the surgical treatment of PPFFx reports a 29% overall reoperation rate among cases with a stable femoral component, with nonunion or refracture being the most common indication for a return to surgery (21.4%). 8 Higher failure rates have recently been reported in transverse Vancouver B1 fractures around the stem tip. In a study of 63 PPFFx associated with well-fixed stems, overall fracture healing was achieved in 89% of cases, while 3/7 transverse Vancouver B1 fractures resulted in non-union with plate fracture. 9 While we also observed 2 non-unions with plate fracture, they occurred in patients with Vancouver C fractures around revision stems.
In addition to LCP-LAP constructs used in our series, other techniques include but are not limited to the use of allograft struts, cerclage cables, polyaxial plates, and double plating. Moore et al reviewed 37 manuscripts including 611 Vancouver B1 and 71 Vancouver C type fractures treated with varying combinations of plates, allograft struts, and cerclage cables. They primarily reported on rate of union and time to union and found that while rate of union was similar across groups, Vancouver B1 fractures treated with an allograft strut had a significantly increased time to union compared to those treated without an allograft strut (6.6 vs 4.4 months). 10 They concluded that while allograft struts can offer increased structural support, extensive soft tissue stripping required for application results in delayed bone healing and cautioned their use in treating Vancouver B1 fracture types. 10
Plates with polyaxial screws are another solution to obtain fixation around intramedullary implants, allowing the combination of conventional plating with angular stability. The Zimmer NCB (non-contact bridging) polyaxial locking plate (ZimmerBiomet, Warsaw, IN) consists of a diagonal three-hole pattern with 2 offset screw holes with 30-degree cone at which bicortical screw placement can be achieved around a stable prosthesis. Hoffman et al utilized the NCB plate in the treatment of 27 interprosthetic femur fractures around stable implants and reported successful healing in 24/27 (88.9%) cases with 1 construct leading to hardware failure. 11 The 3 nonunions were identified as AO/OTA type B fractures and were treated with longer plates and similar working lengths compared to AO/OTA Type A fractures treated in the same study. 11 More recently, Molinari et al reported successful consolidation of 42 PPFFx with adequate radiologic follow-up with no mechanical failures using the NCB plate. 12 A unique failure mode recently reported in a case study using Zimmer NCB plate was of a standard screw remaining in bone and then fretting through the annular seating of the plate. 13 Authors hypothesized that the use of standard screws made the construct too stiff and recommended using locking screws adjacent to the fracture site.13The Iron Lady ® Conical Coupling Locking Plate (Intrauma, Rivoli, Italy) is a new plate with a semitubular shape and triplanar locking screw placement that allows polyaxial screws to be placed around the femoral stem. It was recently used in the treatment of Vancouver B1 PPFFx, reporting fracture healing in 29/32 (91%) patients by 6 months follow-up, which they claimed was consistent with recent literature using other polyaxial plates.10,14,15
Double plating is another surgical solution to provide increased stability in areas with high bending forces. 16 Biomechanical testing comparing single and double plating showed that double plating with a lateral and anterior plate significantly reduces the stress concentration in the lateral plate at the fracture site under full weight bearing. This is a frequent location of implant failure and/or nonunion after the treatment of Vancouver B1 fractures and therefore authors concluded double plating a potential solution for such fractures. 17 An additional biomechanical study comparing the use of a LCP/LAP construct to double plating with lateral and anterior plates demonstrated significantly superior values in axial stiffness and cycles to failure for the double plate construct. 18 A review article of double-plating outcomes reported from 5 studies of PPFFx reported that healing was achieved in 85/96 (88.5%) cases with an overall complication rate of 21.9%. 19 Authors highlighted a study by Bologna et al that compared single and double plating in the treatment of complex distal femoral and periprosthetic fractures. While double plating resulted in union in 8/8 (100%) patients, single plating resulted in 6/13 (46.2%) non-unions and 4/13 (30.8) delayed unions. 20 It is difficult to make comparisons between the use of a single plate with LAP to double plating. The single plate approach allows for less soft tissue stripping at the fracture site. Specifically, in our series, 3 cases involved fractures distal to a THA and around TKA with stemmed femoral components. In each case, LAP was utilized distally to achieve fixation around the distal stem and no failures were observed in these cases.
Of the complications recorded in our series, 3 cases of nonunion were found with 2 having plate breakage at the nonunion site. We found no clear associations with nonunion development. One of these patients had a high energy injury and the other 2 patients had poor bone quality requiring post-op referral to endocrinology. We found no obvious association with plate working length. Although an ideal working lengthhas yet to be established, 7 very short working lengths can lead to excessive stiffness and lead to nonunion and/or implant failure. 21 It is generally recommended to leave 3-4 screw holes empty at the level of the fracture to allow a larger area of stress distribution on the plate. 21
Limitations of this consecutive case series are inherent to the retrospective nature, small sample size (28 patients), and short-term average follow-up (9.8 months), and lack of a control group directly comparing another surgical technique in the same PPFFx types. Despite these limitations, our sample size is greater than the only other clinical case series evaluating LAP use in the surgical treatment of PPFFx. In addition, our series consisted of 4 different treating surgeons with varying decision making. Additionally, the number and location of LAP applied to either LCP or VA-LCP curved condylar plates varied between individual treating surgeons. Our series consisted of 4 different treating surgeons with varying decision making and therefore treatment was not uniform between cases.
In conclusion, we found that the addition of LAP to LCP or VA-LCP constructs provided adequate fixation with a low overall failure rate. No screw pullout or failure of fixation around the implant was found and the most common failure was nonunion and plate breakage. Failure did not occur at the LAP device.
.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Simon C Mears https://orcid.org/0000-0002-0068-0283
References
- 1.Marsland D, Mears SC. A Review of Periprosthetic Femoral Fractures Associated with Total Hip Arthroplasty. Geriatric Orthopaedic Surgery & Rehabilitation. 2012;3(3):107-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottle A, Griffiths R, White S, et al. Periprosthetic fractures: The next fragility fracture epidemic? A national observational study. BMJ Open. 2020;10(12):e042371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmotzer H, Tchejeyan GH, Dall DM. Surgical management of intra- and postoperative fractures of the femur about the tip of the stem in total hip arthroplasty. J Arthroplasty. 1996;11(6):709-717. [DOI] [PubMed] [Google Scholar]
- 4.Lenz M, Windolf M, Mückley T, et al. The locking attachment plate for proximal fixation of periprosthetic femur fractures-a biomechanical comparison of two techniques. Int Orthop. 2012;36(9):1915-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumpies CW, Conrad T, Marintschev I, Hofmann GO. [Locking attachment plate - first experience]. Zeitschrift fur Orthopadie und Unfallchirurgie. 2012;150(3):302-308. [DOI] [PubMed] [Google Scholar]
- 6.Masri BA, Meek RMD, Duncan CP. Periprosthetic Fractures Evaluation and Treatment. Clin Orthop Relat Res. 2004;420:80-95. [DOI] [PubMed] [Google Scholar]
- 7.Pletka JD, Marsland D, Belkoff SM, Mears SC, Kates SL. Biomechanical comparison of 2 different locking plate fixation methods in vancouver b1 periprosthetic femur fractures. Geriatric Orthopaedic Surgery & Rehabilitation. 2011;2(2):51-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gausden EB, Tibbo ME, Perry KI, et al. Outcomes of vancouver c periprosthetic femur fractures. J Arthroplasty. 2021;36(21):360100208-360136074. [DOI] [PubMed] [Google Scholar]
- 9.Min B-W, Lee K-J, Cho C-H, Lee I-G, Kim B-S. High Failure Rates of Locking Compression Plate Osteosynthesis with Transverse Fracture around a Well-Fixed Stem Tip for Periprosthetic Femoral Fracture. J Clin Med. 2020;9(11):3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore RE, Baldwin K, Austin MS, Mehta S. A systematic review of open reduction and internal fixation of periprosthetic femur fractures with or without allograft strut, cerclage, and locked plates. J Arthroplasty. 2014;29(5):872-876. [DOI] [PubMed] [Google Scholar]
- 11.Hoffmann MF, Lotzien S, Schildhauer TA. Clinical outcome of interprosthetic femoral fractures treated with polyaxial locking plates. Injury. 2016;47(4):934-938. [DOI] [PubMed] [Google Scholar]
- 12.Molinari GP, Giaffreda G, Clementi D, Cabbanè G, Galmarini V, Capelli RM. Surgical treatment of peri-prosthetic femur fractures with dedicated NCB plates: our experience. Acta Biomed : Atenei Parmensis. 2020;91(2):297-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stockwell E, Mormino MA, Siebler JC. A unique mode of failure in the noncontact bridging periprosthetic plating system. J Am AcadOrthop Surg Glob Res Rev. 2021;5(2):e2000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Del Chiaro A, Piolanti N, Bonicoli E, Pd P, Marchetti S, Scaglione M. Treatment of Vancouver B1 periprosthetic femoral fractures using Intrauma Iron Lady® locking plate: A retrospective study on 32 patients. Injury. 2021;1383(21):S002000192-S002000193. [DOI] [PubMed] [Google Scholar]
- 15.Hoffmann MF, Lotzien S, Schildhauer TA. Outcome of periprosthetic femoral fractures following total hip replacement treated with polyaxial locking plate. Eur J Orthop Surg Traumatol. 2017;27(1):107-112. [DOI] [PubMed] [Google Scholar]
- 16.Katthagen JC, Schliemann B, Michel PA, Heilmann LF, Dyrna F, Raschke MJ. Clinical Application and Outcomes of Upper Extremity Double Plating. Zeitschrift fur Orthopadie und Unfallchirurgie. 2020;158(2):227-237. [DOI] [PubMed] [Google Scholar]
- 17.Takahashi D, Noyama Y, Asano T, et al. Finite element analysis of double‐plate fixation using reversed locking compression‐distal femoral plates for Vancouver B1 periprosthetic femoral fractures. BMC Muscoskel Disord. 2021;22(1):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wähnert D, Grüneweller N, Gehweiler D, Brunn B, Raschke MJ, Stange R. Double plating in Vancouver type B1 periprosthetic proximal femur fractures: A biomechanical study. J Orthop Res. 2016;35(2):234-239. [DOI] [PubMed] [Google Scholar]
- 19.Lodde MF, Raschke MJ, Stolberg-Stolberg J, Everding J, Rosslenbroich S, Katthagen JC. Union rates and functional outcome of double plating of the femur: Systematic review of the literature [published ahead of print Januray 23, 2021]. Arch Orthop Trauma Surg. doi: 10.1007/s00402-021-03767-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bologna MG, Claudio MG, Shields KJ, Katz C, Salopek T, Westrick ER. Dual plate fixation results in improved union rates in comminuted distal femur fractures compared to single plate fixation. J Orthop. 2019;18:76-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking Plates. J Bone Joint Surg. 2007;89(10):2298-2307. [DOI] [PubMed] [Google Scholar]