Abstract
Background and Objectives
The goal of this work was to determine whether the prevalence of multiple sclerosis (MS) varies by race and ethnicity.
Methods
We conducted a retrospective cohort study of >2.6 million adults from the multiethnic, community-dwelling members of Kaiser Permanente Southern California. The complete electronic health records of individuals with at least 1 ICD-9 code for MS between January 1, 2008 and December 31, 2010 were reviewed. MS prevalence and 95% CIs stratified by age, sex, and race and ethnicity among 2010 members were estimated with binomial regression. Age- and sex-standardized prevalence was estimated according to the 2010 US Census population.
Results
We identified 3,863 patients with MS. The average age of patients with prevalent MS was 51.7 years (SD 13.1 years), and 76.8% were women. The female preponderance was more pronounced among Black (81.2%) and Asian (83.6%) than White (76.3%) or Hispanic (74.5%) individuals with MS. Age- and sex-standardized MS prevalence per 100,000 was similarly high among Black (225.8, 95% CI 207.1–244.5) and White (237.7, 95% CI 228.2–247.2) and significantly lower among Hispanic (69.9, 95% CI 64.4–75.5) and Asian (22.6, 95% CI 17.1–28.1) persons. MS prevalence was highest between the ages of 35 and 64 years and declined after 65 years of age across all racial and ethnic groups. Among adults 18 to 24 years of age, the crude MS prevalence was low but was highest among Black and Hispanic young adults, lower in White people, and lowest in Asian/Pacific Islander individuals (48.5, 25.0, 18.0, and 7.1 per 100,000, respectively).
Discussion
MS prevalence varies by race and ethnicity, being similarly high in White and Black and significantly lower in Hispanic and Asian persons in Southern California. Taken together with previous studies, these findings indicate that the burden of MS in the US Black community has long been underrecognized. More studies are needed to determine whether MS is an emerging disease among US Hispanic adults and whether MS susceptibility and prevalence vary among Hispanic or Asian individuals from different cultures or ancestral backgrounds.
Long believed to be a disease primarily of White people, we recently showed that multiple sclerosis (MS) incidence is highest in Black followed by White women and significantly lower in Hispanic and Asian individuals residing in Southern California.1 Understanding whether similar differences exist in MS prevalence in the United States has important policy and resource allocation implications as an increasing proportion of inhabitants identify as non-White.2
The dearth of MS prevalence estimates in the United States is a result of the fragmented US health care system and the difficulties of carrying out studies in sufficiently large, well-defined populations with sampling frames. Most previous studies of MS prevalence in well-defined community-based populations in the United States have reported that women have significantly higher prevalence than men, with female:male ratios ranging from 2.15 to 4.133 and age-specific prevalence that peaks in the fifth decade.4 These studies, however, are of largely White populations, necessitating new studies in diverse populations that can provide robust race-specific prevalence estimates.
Previous race-specific MS prevalence studies in the United States have yielded conflicting results. A study in Texas in 1998 to 2000 reported a relatively low crude prevalence in White persons (56 per 100,000),5 even compared to contemporary cohorts (177 per 100,000),4 followed by much lower prevalence in Black and Hispanic persons (22 and 11 per 100,000, respectively).5 More recent studies that used electronic health record data from an insured population in Northern California reported that the age-standardized MS prevalence was highest in Black individuals, followed by White and Hispanic individuals, and lowest in Asian Americans (521.4, 384.6, 183.7, and 63.8 per 100,000, respectively).6 A pooled US administrative claims database that did not distinguish between Hispanic and non-Hispanic individuals reported a slightly higher age- and sex-standardized prevalence among White than Black Americans (283.7 and 226.1 per 100,000.respectively),7 whereas a large national US telephone survey reported a very high crude self-reported MS prevalence in White, Black, and Hispanic respondents (824, 741, and 349 per 100,000, respectively).8 These studies have significant methodologic limitations, including patient finding methods that are unvalidated and expected to inflate the number of patients with MS,6-8 particularly in the elderly/high health care users,7,8 unvalidated and unspecified methods for identifying race and ethnicity,7 and a small, nonrepresentative sample.6
The purpose of our study was to determine whether MS prevalence varies by race and ethnicity using rigorous patient and race and ethnicity identification methods and, if so, whether there are additional differences in prevalence by age or sex within groups in a large, well-enumerated, diverse population representative of Southern California.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
The institutional review board at Kaiser Permanente Southern California (KPSC) approved this study. Informed consent was waived because this was a database and chart review study without direct patient contact.
Identification of Patients With MS
KPSC is a large prepaid health maintenance organization with >3.5 million members in 2010. At that time, it provided comprehensive health care coverage to ≈20% of the population in the geographic area it serves. The costs of specialist consultations, hospitalizations, MRI scans, other diagnostic tests, and medications are fully covered. The KPSC membership is representative of the general population in Southern California for ethnicity, age, sex, and socioeconomic status, except for an underrepresentation of the lowest and highest ends of the socioeconomic spectrum.9 In 2010, the number of adults (≥18 years of age) with at least 6 months of membership was 2,655,194.
To identify patients with prevalent MS, we searched electronic databases with any mention of ICD-9 diagnostic code for MS (340) from January 1, 2008 to December 31, 2010, including all inpatient and outpatient encounters among individuals with at least 6 months of membership in 2008, 2009, or 2010 (N = 4,892). Diagnoses were confirmed according to the revised McDonald criteria10 through full medical records abstraction including all inpatient and outpatient records, MRI scans, and diagnostic test results by trained medical chart abstractors (E.G.G., J.B.S.) and, when uncertain, an MS specialist (A.M.L.-G.). There was sufficient documentation to apply MS diagnostic criteria in 97.1% of members with at least 1 ICD-9 code for MS, of whom 83.9% met criteria and 13.2% clearly did not (e.g., misuse of code or misdiagnosis). In the remaining patients, the documentation was insufficient to meet diagnostic criteria, most of whom were elderly adults.
To avoid underestimating MS prevalence in older adults due to insufficient documentation, we further classified these patients as likely having MS on the basis of available documentation (insuff-yes) or unlikely MS (insuff-no). Those classified as insuff-yes (1.5%) were typically elderly patients who appeared to have either advanced or benign MS but lacked clear documentation of ≥2 clinical relapses or progressive disability over ≥1 year and did not have brain MRI scans. Those classified as insuff-no (1.3%) were typically elderly people with MS entered into their problem list by a primary care provider with no or only a brief comment (e.g., “diagnosed in 20s”).
Race and ethnicity information was obtained from medical records review (patients only), health plan administrative records, and birth certificates.11 We categorized race and ethnicity as non-Hispanic White (White), Hispanic White (Hispanic), Black (regardless of ethnicity), Asian or Pacific Islander (Asian/Pacific Islander), other or multiple races and ethnicities (e.g., Black and Asian, Asian and Hispanic), and unknown because of missing information. For unknown race and ethnicity information (0% patients with MS, 9% of cohort members), we assigned the probability on each member using the Bayesian Improved Surname Geocoding method.12,13 The racial and ethnic distribution of the cohort population remained essentially unaltered after race imputation.
Statistical Analyses
MS 1-year period prevalence in 2010 by race and ethnicity, age group (18–24, 25–34, 35–44, 45–54, 55–64, 65–74, ≥75 years), or sex (male, female) was estimated by dividing the number of adult (≥18 years) patients with MS by the number of adult members of that same group. Binomial distribution was used to calculate 95% CIs. Age- and sex-standardized prevalence ratios were calculated from direct standardization14 with the 2010 US Census population as the reference population. Crude and risk ratios (RRs) adjusted for age and sex comparing prevalence between groups were calculated with Poisson regression between racial and ethnic groups with White non-Hispanic as the reference category. For the primary analyses, MS was defined as those who met diagnostic criteria or were classified as insuff-yes.
The means and SDs of normally distributed variables were compared by 2-sample t tests; medians were compared with the Kruskal-Wallis test; and for binary or categorical variables, χ2 with Fisher exact test was used. Only 22 patients (0.6%) of other/mixed races were identified, so reliable estimates for this racial and ethnic category could not be calculated. They are included, however, in analyses of the total population. All analyses were conducted with SAS software version 9.4 (SAS Institute Inc, Cary, NC).
Data Availability
Due to the KPSC institutional review board, deidentified data would be available on reasonable request.
Results
Demographic and KPSC coverage characteristics in 2010 of the 3,863 adults with MS are presented in Table 1. The average age of patients with prevalent MS was 51.7 years, and 76.8% were women. The female preponderance was more pronounced among Black (81.2%) and Asian/Pacific Islander (83.6%) than White (76.3%) or Hispanic (74.5%) individuals with MS. Hispanic and Asian/Pacific Islander persons were younger on average compared to White or Black individuals. More patients with MS were White (65.7%) or Black (15.1%), and fewer were Hispanic (16.9%) or Asian/Pacific Islander (1.7%) than would be expected from the underlying distribution of KPSC members (40.7% White, 9.4% Black, 37.1% Hispanic, 10.7% Asian/Pacific Islander, and 2.0% other/mixed). Black and Hispanic individuals with MS were more likely to receive KPSC coverage through Medicaid or other public assistance programs than White or Asian/Pacific Islander patients, although the majority of patients with MS were covered through employer- or self-pay options across all racial and ethnic groups (Table 1).
Table 1.
Demographic and Kaiser Permanente Coverage Characteristics of Patients With Prevalent MS by Race and Ethnicity
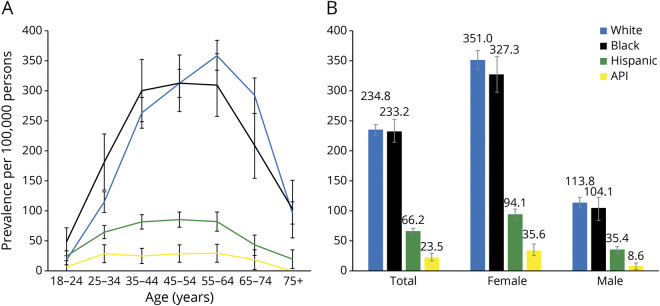
Age- and sex-standardized MS prevalence was highest in White (237.7 per 100,000) and Black (225.8) persons, significantly lower in Hispanic persons (69.9, adjusted RR 0.29, 95% CI 0.27–0.32), and even lower in Asian/Pacific Islander individuals (22.6, adjusted RR 0.09, 95% CI 0.07–0.12) compared to White persons (Table 2). There was no significant difference in MS prevalence between Black and White individuals (adjusted RR 0.93, 95% CI 0.85–1.02, p = 0.13). This similarly high prevalence among White and Black and lower prevalence among Hispanic and Asian/Pacific Islander persons were consistent in both crude and age- and sex-stratified analyses (Figure 1, A and B, respectively).
Table 2.
Standardized Prevalence and Estimated Number of Adults With MS in the United States in 2010 by Race and Ethnicity
Figure 1. MS Prevalence by Race and Ethnicity in Southern California.
Prevalence (indicated by the number above each bar in B) and 95% CIs of multiple sclerosis (MS) in White (blue), Black (black), Hispanic (green), and Asian/Pacific Islander (API) (orange) individuals residing in Southern California by age groups by years (A) and sex (B). MS prevalence is highest in White and Black persons, lower in Hispanic individuals, and lowest in the heterogeneous group of Asian/Pacific Islander persons residing in Southern California across all age groups except 18- to 24-year-olds, for whom the prevalence in Hispanic persons is similar to that in White and highest in Black persons. MS prevalence continues to increase with age in White persons through 55 to 64 years of age, whereas in Black persons, MS prevalence rises until 35 to 44 years of age and then remains stable through 55 to 64 years of age. MS prevalence declines in the ≥65-year-old age groups across all racial and ethnic groups. MS prevalence is similar in Black and White persons in both women (crude risk ratio [RR] 0.93, 95% CI 0.84–1.03, p = 0.17, Poisson regression with White persons as the reference group) and men (crude RR 0.91, 95% CI 0.75–1.02, p = 0.39, Poisson regression with White persons as the reference group). MS prevalence is lower in Hispanic and Asian/Pacific Islander compared to White persons, regardless of sex. MS prevalence is higher in women compared to men across all racial and ethnic groups (White individuals: crude RR 3.09, 95% CI 2.82–3.39, p < 0.0001; Black individuals: crude RR 3.15, 95% CI 2.56–3.88, p < 0.0001; Hispanic individuals: crude RR 2.66, 95% CI 2.23–3.17, p < 0.0001; Asian/Pacific Islander individuals: crude RR 4.12, 95% CI 2.16–7.87, p < 0.0001).
MS prevalence varied by age and sex across all racial and ethnic groups (Figure 1). In Black and White individuals, regardless of sex, prevalence continued to increase with age, peaking at 313 and 360 per 100,000 among 45- to 64-year-olds, respectively. While MS prevalence increased in these age groups among Hispanic and Asian individuals as well, the magnitude of increase was significantly smaller, peaking at only 85.4 and 29.2 per 100,000 respectively. Prevalence declined among those ≥65 years of age across all racial and ethnic groups (Figure 1A).
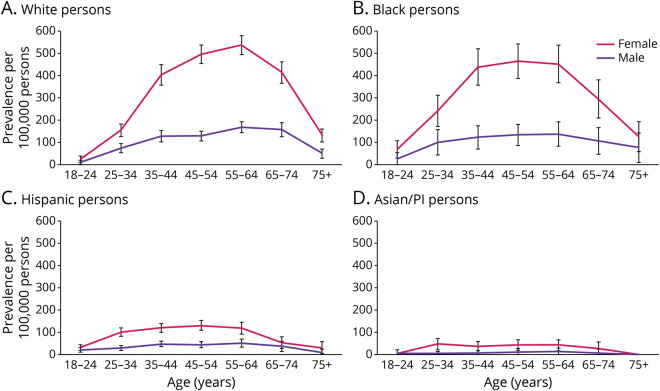
MS prevalence was significantly higher in women compared to men across all racial and ethnic groups (Figure 2), and there was no significant difference between Black and White women (p = 0.16) or Black and White men (p = 0.48) (Figure 1B). The female:male ratios across age strata were also similar among White and Black persons and were highest (3.1–3.8) during the peak prevalence ages of 35 to 64 years (Table 3 and Figure 2, A and B). In contrast, the female:male ratio was highest at ages 25 to 34 years among Hispanic and Asian/Pacific Islander individuals.
Figure 2. MS Sex- and Age-Specific Prevalence by Race and Ethnicity in Southern California.
Crude sex- and age-specific prevalence of multiple sclerosis (MS) and 95% CIs among White persons (A), Black persons (B), Hispanic persons (C), and the heterogeneous group of Asian/Pacific Islander persons (A/PI; D) residing in Southern California. The female predominance and peak prevalence between 35 and 64 years of age are remarkably similar between White and Black persons. While this pattern is similar in Hispanic persons, the magnitude of increase among Hispanic women and men is significantly lower than for Black or White persons. Among Asian women, prevalence increased from ages 18 to 24 years to 25 to 34 years but no longer after that. MS prevalence was very low among Asian men in all age groups.
Table 3.
Age-Specific and Age-Adjusted MS Prevalence per 100,000 by Sex and Race and Ethnicity, KPSC, 2010
Among young adults 18 to 24 years of age, MS prevalence was relatively low (compared to middle and older ages), but the racial and ethnic pattern was somewhat different. In this age group, prevalence was highest among Black (48.5 per 100,000, 95% CI 24.7–72.2) and Hispanic (25.0, 95% CI 16.9–33.0) persons, lower in White people (18.0, 95% CI 10.1–25.9), and lowest in Asian/Pacific Islander individuals (Figure 1A). The difference in MS prevalence between young Hispanic and White adults was driven by a higher prevalence among men but not women, whereas both Black men and women had a higher prevalence than young White men and women (Table 3 and Figure 2).
Discussion
The findings from this study, together with 2 US MS incidence studies1,15 and a US death certificate study,16 contradict the widely held belief that MS is rare in Black Americans. Moreover, the findings from this study and the death certificate study16 indicate that MS has affected US Black and White adults at similar rates for decades.
The belief that MS is rare in Black individuals was based on problematic evidence, including ecologic studies and a 1950s prevalence study of veterans that found that White men were twice as likely as Black men to be service-connected for MS.17 However, becoming service-connected is a complicated benefit process that was likely difficult for Black men to navigate, particularly in the 1950s. When a similar military personnel study of Gulf War era veterans (1990–2007) found that MS incidence was 1.27-fold higher in Black15 than White persons and we reported that Black individuals had a 47% increased incidence of MS compared to White people1 in the same study population included herein, some concluded that MS was an emerging disease in US Black adults.15
If MS were truly an emerging disease in Black persons, then we would expect to see significantly lower MS prevalence and MS-related mortality in older age groups compared to White persons. Because prevalence is a combination of incidence and longevity and US Black persons have a shorter life expectancy than White individuals, the fact that we found similar MS prevalence in older Black and White persons is rather remarkable. A large US insurance claims study also found that the age- and sex-standardized prevalence was similar among Black and White adults (226.1 and 283.7 per 100,000, respectively).7 In addition, a study of US death certificates from 1999 to 2015 found that MS was just as likely to be listed as a cause of death in Black adults <65 years of age and only slightly less likely to be listed in those ≥65 years of age compared to White adults.16 These findings strongly suggest that MS is not a new disease among US Black individuals; rather, the burden of disease in Black persons was not measured until recently6-8 and was incorrectly assumed to be low.
On the other hand, whether MS is an emerging disease among Hispanic individuals is unclear yet appears plausible. This concern has been raised by multiple investigators and is supported by increasing MS incidence and prevalence in selected Latin American countries,18 particularly Argentina19 and Puerto Rico.20
Our findings that MS prevalence is higher among young Hispanic adults than among young White adults yet significantly lower among older Hispanic adults compared to White adults residing in Southern California are consistent with emerging disease hypotheses. The magnitude of difference in prevalence between Hispanic persons compared to White and Black persons in all age groups ≥35 years of age appears too large to be explained by underlying population differences in all-cause mortality. In addition, greater longevity may influence higher later-life prevalence among White adults but would not explain higher prevalence in older Black adults compared to US Hispanic adults because Black Americans have a shorter life expectancy than US Hispanic persons. MS-related mortality among Hispanic individuals also appears to be significantly less common after 35 years of age compared to US White and Black adults.16 Alternatively, our findings could be explained by a younger age at onset yet lower incidence of MS among Hispanic individuals, as we previously reported.1,21 Even if MS incidence is not increasing in Hispanic persons, the burden of disease in the Hispanic community is likely to increase because this is a rapidly growing racial and ethnic group and is projected to account for 28% of the US population by 2060.22
The broad group of individuals referred to as Asian, in contrast, has a consistently low incidence and prevalence of MS regardless of ethnicity or setting. MS prevalence is quite low in Asia, even in resource-rich countries like Japan23; among South Asian individuals living in London24; in our study population; and among indigenous Asiatic Russian persons compared to European Russian persons who migrated to Siberia.25 In addition, MS incidence among Asian individuals was 80% lower than in White persons in our study population (1.39 and 6.94 per 100,000 person-years, respectively)1 and ≈9- to 10-fold lower in Asian adults residing in Canada compared to non-Asian adults.26 An intriguing finding in the latter study was a doubling in the incidence of MS among Asian women from 0.71 per 100,000 in 2005 to 2.08 per 100,000 in 2006 to 2010 but no change in men.26 This finding is consistent with the high female:male ratio (4.0) among Asian/Pacific Islander persons reported herein and is deserving of further study.
The main limitation of this study, like other studies of racial and ethnic disparities, is that the terms Hispanic, Asian, Black, and White are socially constructed labels that influence social standing and opportunities for advancement in the United States, not uniform biological or even cultural differences. Therefore, these groups, particularly Hispanic and Asian/Pacific Islander persons in the United States, represent a broad group of cultures and ancestral backgrounds, which may have different effects on MS risk. The majority of Hispanic persons residing in Southern California are from Mexico (77%) or other Central American countries (12%) and are less diverse than Hispanic persons residing on the East Coast.27 Mexicans are predominantly Mestizos (mixed Spanish and Amerindian/Indigenous descent, 62%), while another 21% identify as predominantly Amerindian, 7% as Amerindian, and only 10% as other/mostly European.28 Puerto Ricans, on the other hand, are predominantly of White European descent (65.9%), followed by African descent (11.7%) and only 0.2% of Indigenous descent.29 Thus, it may not come as a surprise that MS incidence in Puerto Rico was 2-fold higher than in our Hispanic population (6.1 in 201320 and 3.0 per 100,000 in 2008–2010,1 respectively).
Similarly, the term Asian/Pacific Islander encompasses Chinese, Korean, Indian, Filipino, Japanese, and Vietnamese people, among others. In Southern California, most Asian/Pacific Islander individuals are of Chinese, Filipino, or Korean origin,30 whereas the largest Asian group in the majority of midwestern and southern states is of Indian origin.31 Whether MS prevalence varies among Asian individuals of Chinese, Filipino, or Indian descent in the United States has not been studied but is certainly plausible. The age-standardized MS prevalence in South Asian individuals residing in East London (29 per 100,000)24 was higher than the age- and sex-standardized estimates reported herein (22.6 per 100,000), even though the prevalence among White individuals was significantly lower (18024 and 237.7 per 100,000, respectively). Last, whether there are differences in MS susceptibility among different US Black populations (e.g., descents of slaves, recent African or Caribbean immigrants) has not been studied.
For all these reasons, it is uncertain whether extrapolating incidence or prevalence rates from Southern California Hispanic, Asian, Black, and White persons to the rest of the US population is valid. Further calling this into question is a recent study indicating that a true south-to-north increasing MS prevalence in the United States remains.32 Thus, our national estimate should be viewed cautiously and is likely an underestimation of the true prevalence. We have provided these estimates to help others approximate how changing demographics may affect MS prevalence in specific communities, but future studies should aim to provide estimates in other subgroups. Future studies should also establish whether the latitude gradient applies to all racial and ethnic groups of individuals and MS incidence or whether state-by-state differences in MS prevalence33 are best explained by differences in racial and ethnic subgroup composition, migration, or insurance status rather than latitude. Of note, our standardized US prevalence estimate of 465,322 persons with MS in 2010 is strikingly similar to the uninflated standardized 2010 estimate derived from a recent national MS prevalence study based on multiple administrative health claims datasets (470,053).33 Taken together, these findings reaffirm that applying an inflation factor to arrive at the final 2010 estimate was warranted.33
Other study limitations include the possibility of undercounting patients with true MS in the very old in whom we were unable to apply MS diagnostic criteria due to lack of documentation, imprecise estimates due to small samples particularly in Asian men, and inability to estimate MS prevalence in the uninsured. However, undercounting MS among the uninsured is more likely to underestimate the true prevalence of MS in Black and Hispanic persons who were far more likely to be uninsured than White persons during the study period (43.5%, 27.1%, and 15.7%, respectively, in 2010).
Strengths of this study are the rigorous patient finding methods; application of the 2017 diagnostic criteria; and a large, diverse well-characterized study population that is representative of the underlying geographic community. An important strength was our ability to carefully exclude misdiagnosed patients, a feature that is not possible without the availability of electronic health records. Misdiagnosed MS appears to be increasing as the diagnostic criteria become more complex34 and may represent up to 19% of clinically diagnosed patients.35 This is a significant advantage over the use of administrative claims datasets or reliance on ICD codes6,7 for which the misdiagnoses would likely be classified as true because MS misdiagnoses are perpetuated for ≥3 years in >50% of patients and use of MS disease-modifying treatments in misdiagnosed patients is common.34
It is becoming increasingly clear that the burden of MS in the US Black community has long been understudied and therefore underrecognized. While the prevalence of MS is relatively low among Hispanic persons, this segment of the US population is growing rapidly. Simultaneously, the financial toxicity of MS treatments continues to rise at alarming rates,36 and Black and Hispanic individuals remain far more likely to be uninsured than White Americans. This raises concerns that preventable MS-related disability will or may already disproportionately affect non-White adults residing in the United States from a combination of underrecognition of the magnitude of the problem, delays in diagnosis, and inconsistent access to treatments in a timely manner. Future studies are urgently needed to address these issues and to provide refined incidence and prevalence rates among racial and ethnic groups across the United States.
Glossary
- ICD-9
International Classification of Diseases, 9th revision
- insuff-no
insufficient documentation but not likely MS
- insuff-yes
insufficient documentation but likely MS
- KPSC
Kaiser Permanente Southern California
- MS
multiple sclerosis
- RR
risk ratio
Appendix. Authors

Footnotes
Editorial, page 739
Study Funding
Funding provided by the National Multiple Sclerosis Society (RES-2005-36596).
Disclosure
A. Langer-Gould receives grant support and awards from the Patient Centered Outcomes Research Institute and the National MS Society. She currently serves as a voting member on the California Technology Assessment Forum, a core program of the Institute for Clinical and Economic Review (ICER). She has received sponsored and reimbursed travel from ICER and the NIH. E.G. Gonzales, J.B. Smith, and B.H. Li report no conflicts of interest. L.M. Nelson receives grants support from the Centers for Disease Control and Prevention, NIH, and National MS Society and compensation for serving as a consultant to Acumen, Inc. Go to Neurology.org/N for full disclosures.
References
- 1.Langer-Gould A, Brara SM, Beaber BE, Zhang JL. Incidence of multiple sclerosis in multiple racial and ethnic groups. Neurology. 2013;80(19):1734-1739. [DOI] [PubMed] [Google Scholar]
- 2.US Census Bureau. The chance that two people chosen at random are of different race or ethnicity groups has increased since 2010. Accessed August 19, 2021. census.gov/library/stories/2021/08/2020-united-states-population-more-racially-ethnically-diverse-than-2010.html [Google Scholar]
- 3.Evans C, Beland SG, Kulaga S, et al. Incidence and prevalence of multiple sclerosis in the Americas: a systematic review. Neuroepidemiology. 2013;40(3):195-210. [DOI] [PubMed] [Google Scholar]
- 4.Mayr WT, Pittock SJ, McClelland RL, Jorgensen NW, Noseworthy JH, Rodriguez M. Incidence and prevalence of multiple sclerosis in Olmsted County, Minnesota, 1985-2000. Neurology. 2003;61(10):1373-1377. [DOI] [PubMed] [Google Scholar]
- 5.Williamson DM, Henry JP, Schiffer R, Wagner L. Prevalence of multiple sclerosis in 19 Texas counties, 1998-2000. J Environ Health. 2007;69(10):41-45. [PubMed] [Google Scholar]
- 6.Romanelli RJ, Huang Q, Lacy J, Hashemi L, Wong A, Smith A. Multiple sclerosis in a multi-ethnic population from Northern California: a retrospective analysis, 2010-2016. BMC Neurol. 2020;20(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briggs FB, Hill E. Estimating the prevalence of multiple sclerosis using 56.6 million electronic health records from the United States. Mult Scler. 2020;26(14):1948-1952. [DOI] [PubMed] [Google Scholar]
- 8.Buka SL, Wallin MT, Culpepper WJ, et al. Feasibility of using a nationally representative telephone survey to monitor multiple sclerosis prevalence in the United States. Neuroepidemiology. 2020;54(2):123-130. [DOI] [PubMed] [Google Scholar]
- 9.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162-173. [DOI] [PubMed] [Google Scholar]
- 11.US Census Bureau. Census 2000 surname list. US Census Bureau; 2009. [Google Scholar]
- 12.Elliott MN, Morrison PA, Fremont A, McCaffrey DF, Pantoja P, Lurie N. Using the Census Bureau's surname list to improve estimates of race/ethnicity and associated disparities. Health Serv Outcomes Res Methodol. 2009;9:69-83. [Google Scholar]
- 13.Derose SF, Contreras R, Coleman KJ, Koebnick C, Jacobsen SJ. Race and ethnicity data quality and imputation using U.S. Census data in an integrated health system: the Kaiser Permanente Southern California experience. Med Care Res Rev. 2013;70(3):330-345. [DOI] [PubMed] [Google Scholar]
- 14.Breslow NE, Day NE. Statistical Methods in Cancer Research, Volume II: The Design and Analysis of Cohort Studies. IARC Scientific Publications; 1987:1-406. [PubMed] [Google Scholar]
- 15.Wallin MT, Culpepper WJ, Coffman P, et al. The Gulf War era multiple sclerosis cohort: age and incidence rates by race, sex and service. Brain. 2012;135(pt 6):1778-1785. [DOI] [PubMed] [Google Scholar]
- 16.Amezcua L, Rivas E, Joseph S, Zhang J, Liu L. Multiple sclerosis mortality by race/ethnicity, age, sex, and time period in the United States, 1999-2015. Neuroepidemiology. 2018;50(1-2):35-40. [DOI] [PubMed] [Google Scholar]
- 17.Kurtzke JF, Beebe GW, Norman JE Jr. Epidemiology of multiple sclerosis in U.S. veterans, 1: race, sex, and geographic distribution. Neurology. 1979;29(9 pt 1):1228-1235. [DOI] [PubMed] [Google Scholar]
- 18.Cristiano E, Rojas JI. Multiple sclerosis epidemiology in Latin America: an updated survey. Mult Scler J Exp Transl Clin. 2017;3(2):2055217317715050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cristiano E, Patrucco L, Miguez J, Giunta D, Peroni J, Rojas JI. Increasing incidence of multiple sclerosis among women in Buenos Aires: a 22 year health maintenance organization based study. Neurol Sci. 2016;37(10):1621-1626. [DOI] [PubMed] [Google Scholar]
- 20.Chinea A, Ríos-Bedoya CF, Vicente I, et al. Increasing incidence and prevalence of multiple sclerosis in Puerto Rico (2013-2016). Neuroepidemiology. 2017;49(3-4):106-112. [DOI] [PubMed] [Google Scholar]
- 21.Langer-Gould A, Qian L, Tartof SY, et al. Vaccines and the risk of multiple sclerosis and other central nervous system demyelinating diseases. JAMA Neurol. 2014;71(12):1506-1513. [DOI] [PubMed] [Google Scholar]
- 22.Vespa J, Medina L, Armstrong D. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. In: Current Population Reports. US Census Bureau; 2020:P25-1144. Accessed August 19, 2021. census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf [Google Scholar]
- 23.GBD 2016 Multiple Sclerosis Collaborators. Global, regional, and national burden of multiple sclerosis 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(3):269-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albor C, du Sautoy T, Kali Vanan N, Turner BP, Boomla K, Schmierer K. Ethnicity and prevalence of multiple sclerosis in east London. Mult Scler. 2017;23(1):36-42. [DOI] [PubMed] [Google Scholar]
- 25.Rosati G. The prevalence of multiple sclerosis in the world: an update. Neurol Sci. 2001;22(2):117-139. [DOI] [PubMed] [Google Scholar]
- 26.Lee JD, Guimond C, Yee IM, et al. Incidence of multiple sclerosis and related disorders in Asian populations of British Columbia. Can J Neurol Sci. 2015;42(4):235-241. [DOI] [PubMed] [Google Scholar]
- 27.Pew Research Center. Latino populations in U.S. metro areas are more diverse along the East Coast. Accessed December 15, 2021. pewresearch.org/fact-tank/2019/09/16/key-facts-about-u-s-hispanics/ft_19-09-09_latinoorigin_latino-populations-metro-areas/.
- 28.WorldAtlas. Largest ethnic groups in Mexico. 2019. Accessed August 19, 2021. worldatlas.com/articles/largest-ethnic-groups-in-mexico.html. [Google Scholar]
- 29.US Census Bureau. QuickFacts Puerto Rico. 2019. Accessed August 19, 2021. census.gov/quickfacts/PR. [Google Scholar]
- 30.Los Angeles Almanac. Asian ethnic origin Los Angeles County: 2010 Census & 2019 Census estimates.Accessed August 19, 2021. laalmanac.com/population/po16.php [Google Scholar]
- 31.Pew Research Center. Largest Asian origin groups by state. Accessed August 19, 2021. pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-origin-groups-in-the-u-s/ft_2021-04-29_asianorigins_02/.
- 32.Hittle M, Topol B, Cutter GR, et al. Geographic variation of MS in the United States. Presented at the Consortium of Multiple Sclerosis Centers, October 25-28, 2021, Orlando, FL. cmscscholar.org/2021-annual-meeting/. [Google Scholar]
- 33.Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029–e1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Solomon AJ, Naismith RT, Cross AH. Misdiagnosis of multiple sclerosis: impact of the 2017 McDonald criteria on clinical practice. Neurology. 2019;92(1):26-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaisey M, Solomon AJ, Luu M, Giesser BS, Sicotte NL. Incidence of multiple sclerosis misdiagnosis in referrals to two academic centers. Mult Scler Relat Disord. 2019;30:51-56. [DOI] [PubMed] [Google Scholar]
- 36.San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the KPSC institutional review board, deidentified data would be available on reasonable request.