Abstract
COVID-19-associated coagulopathy (CAC) is a life-threatening complication of SARS-CoV-2 infection. However, the underlying cellular and molecular mechanisms driving this condition are unclear. Evidence supports the concept that CAC involves complex interactions between the innate immune response, the coagulation and fibrinolytic pathways, and the vascular endothelium, resulting in a procoagulant condition. Understanding of the pathogenesis of this condition at the genomic, molecular and cellular levels is needed in order to mitigate thrombosis formation in at-risk patients. In this Perspective, we categorize our current understanding of CAC into three main pathological mechanisms: first, vascular endothelial cell dysfunction; second, a hyper-inflammatory immune response; and last, hypercoagulability. Furthermore, we pose key questions and identify research gaps that need to be addressed to better understand CAC, facilitate improved diagnostics and aid in therapeutic development. Finally, we consider the suitability of different animal models to study CAC.
Subject terms: Immunology, SARS-CoV-2, Platelets
Here, the authors consider our emerging understanding of COVID-19-associated coagulopathy. They focus on the complex interactions between innate immune, coagulation and fibrinolytic pathways that can lead to potentially life-threatening thrombosis following SARS-CoV-2 infection.
Introduction
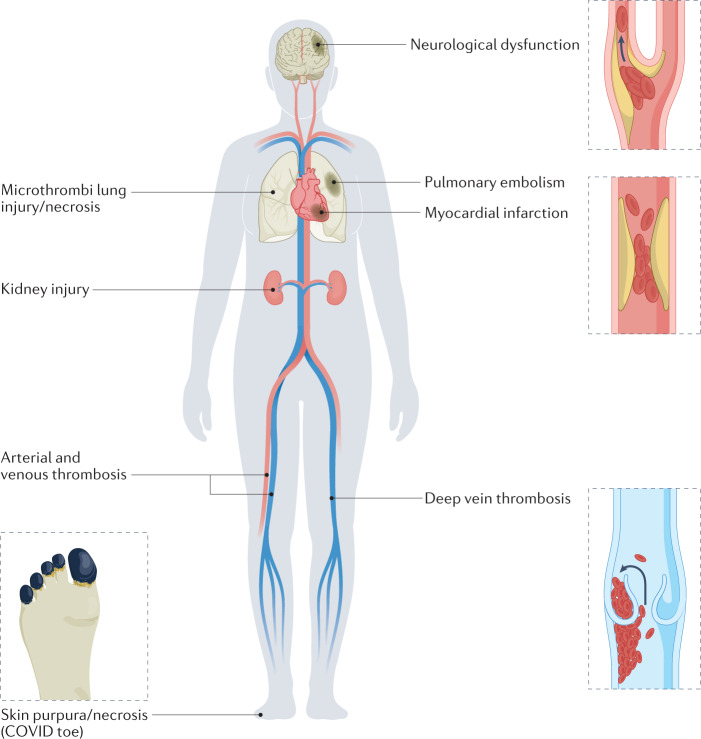
In the early days of the SARS-CoV-2 pandemic, reports from clinical investigators in Wuhan, China indicated a markedly increased risk of thrombosis among patients with COVID-19 (ref.1). This finding was confirmed by subsequent reports and is consistent with the idea that COVID-19-associated coagulopathy (CAC) contributes to the morbidity and mortality of patients infected with SARS-CoV-2 (refs.1–11). CAC can manifest as microthrombi and macrothrombi, resulting in damage to multiple organs, including the lungs, heart, brain and kidneys (Fig. 1). Recognizing the critical risk of CAC to public health, the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health (NIH) organized a 2-day workshop on CAC in May 2021. The goal was to explore the current understanding of the molecular and cellular mechanisms that trigger CAC, identify the scientific gaps and recommend high-priority research topics.
Fig. 1. Potential clinical consequences of COVID-19-associated coagulopathy.
COVID-19-associated coagulopathy (CAC) is characterized by coagulation disorders that affect multiple tissue and organ sites, and vary from skin purpura (also known as ‘COVID toe’) to myocardial infarction and neurological dysfunction. Circulating microthrombi and/or macrothrombi can lead to multi-organ injury or failure.
Compared with diseases caused by other common respiratory viral infections, patients with COVID-19 have a higher frequency and severity of clotting events, which in most cases are associated with elevated plasma levels of D-dimer, C-reactive protein, P-selectin and fibrinogen (see Box 1 for a glossary of terms)12–14. D-dimer is generated by plasmin cleavage of cross-linked fibrin and is therefore a marker of both coagulation events and fibrinolysis. It is notable that elevated D-dimer levels in patients with COVID-19 are accompanied by only occasional prolongation of the prothrombin time and activated partial thromboplastin time15, together with moderate changes in platelet counts. A recent report from the ACTIV-4B clinical trial suggests that D-dimer levels are elevated in approximately 10% of all patients with COVID-19, indicating a high frequency of coagulopathy16. The haematological findings are not consistent with classical disseminated intravascular coagulation17 but, instead, suggest a different aetiology for CAC that could include perturbations in fibrinolysis18.
Several lines of evidence indicate that CAC involves complex dysregulated interactions between the inflammatory, immune, coagulation, fibrinolytic, complement and kallikrein–kinin systems18–22. This association of the innate immune response with coagulation — particularly in the microvasculature where endothelial cell dysfunction promotes clot formation and inflammation — has been termed ‘immunothrombosis’19,23–25. It is an evolving concept, suggesting complex relationships between circulating immune cells, vascular endothelium and a host of soluble and membrane-bound factors that regulate coagulation and innate and adaptive immunity. This paradigm is increasingly being incorporated into our understanding of thrombosis in multiple settings, including in cancer, sepsis and acute respiratory distress syndrome26. However, in the context of COVID-19, a detailed understanding of the underlying molecular and cellular interactions of each of these systems is still lacking. In this Perspective, we discuss three pathways that are emerging as key pathological mechanisms in CAC: first, vascular endothelial cell dysfunction; second, a hyper-inflammatory immune response; and last, hypercoagulability. Although limited in scope, our aims are to summarize the key ideas raised during the NHLBI workshop, to highlight major gaps in our current knowledge and to provide a road map for future research on CAC.
Box 1 Glossary of terms.
D-dimer: the soluble degradation product of cross-linked fibrin; elevated levels indicate ongoing activation of the clotting system
Prothrombin time: a plasma clotting test that reports the integrity of the tissue factor and final common pathways of blood clotting
Activated partial thromboplastin time: a plasma clotting test that reports the integrity of the contact and final common pathways of blood clotting
Disseminated intravascular coagulation: the systemic activation of blood coagulation, commonly resulting in fibrin deposition, microvascular thrombi and consumption of clotting proteins and platelets; can cause multiple organ failure
Tissue factor (TF): the major trigger for coagulation
Tissue factor pathway inhibitor (TFPI): a major negative regulator of coagulation
Endothelial protein C receptor (EPCR): a cofactor for activation of protein C
von Willebrand factor (vWF): a large multimeric, pro-haemostatic factor released by activated endothelial cells and platelets
a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13): a zinc-containing metalloproteinase that cleaves ultra-large vWF multimers
SARS-CoV-2 and vascular dysfunction
Disruption of the vascular endothelium and antithrombotic function
Under normal conditions, the vascular endothelium provides an antithrombotic surface by expressing molecules that prevent both platelet activation (for example, nitric oxide, prostacyclin and ectonucleotidases) and coagulation (for example, tissue factor pathway inhibitor (TFPI), thrombomodulin and endothelial cell protein C receptor (EPCR)). The vascular endothelium is also lined by a carbohydrate-rich glycocalyx that includes anticoagulant molecules such as heparan sulfate, and serves to protect against pathogen invasion27. These finely regulated antithrombotic systems may be disrupted in the setting of bacterial and viral infections, with functional loss of anticoagulant molecules such as TFPI, thrombomodulin and EPCR from the endothelial surface, heightened expression of procoagulants (most notably tissue factor (TF)) and damage to the glycocalyx. With SARS-CoV-2 infection, dysfunction of the vascular endothelium is thought to be a major contributor to the pathogenesis of COVID-19 vasculopathy28–30. In the earliest stages of disease, this occurs primarily in the lungs, where SARS-CoV-2, via angiotensin-converting enzyme 2 (ACE2), infects type II pneumocytes, cells that are in direct apposition to the alveolar vascular network. Resultant damage to the alveoli and the microvascular endothelium features heightened inflammation, infiltration of activated neutrophils, release of neutrophil extracellular traps (NETs), activation of complement and diffuse microvascular thrombosis, all of which contribute to the diminished respiratory function and worsened prognosis19,31. It is not yet known whether the endothelial damage is initially caused by direct infection of the endothelium by SARS-CoV-2 (refs.20,32) and/or indirectly as a result of the so-called ‘cytokine storm’33–35, or by other innate, adaptive or autoimmune phenomena. However, as the disease progresses, it is likely that multiple factors contribute to the severity of the endothelial damage, and the extent of thrombosis and organ damage. Delineating the specific triggers and determinants of disease severity are under investigation.
Dysregulation of the kallikrein–kinin system and endothelial cell injury
Although vascular endothelial dysfunction can occur in any severe infection, SARS-CoV-2 has unique interactions with its host cell surface receptor, ACE2, that might induce endothelial cell dysfunction at an early stage of the infection. SARS-CoV-2 binds to ACE2 present on lung epithelial cells36, triggering endocytosis of the SARS-CoV-2–ACE2 complex by a similar mechanism to that seen with SARS-CoV-1 (refs.37,38). Consequently, ACE2 expression levels on the cell surface fall at the site of the infection, resulting in local ACE2 deficiency.
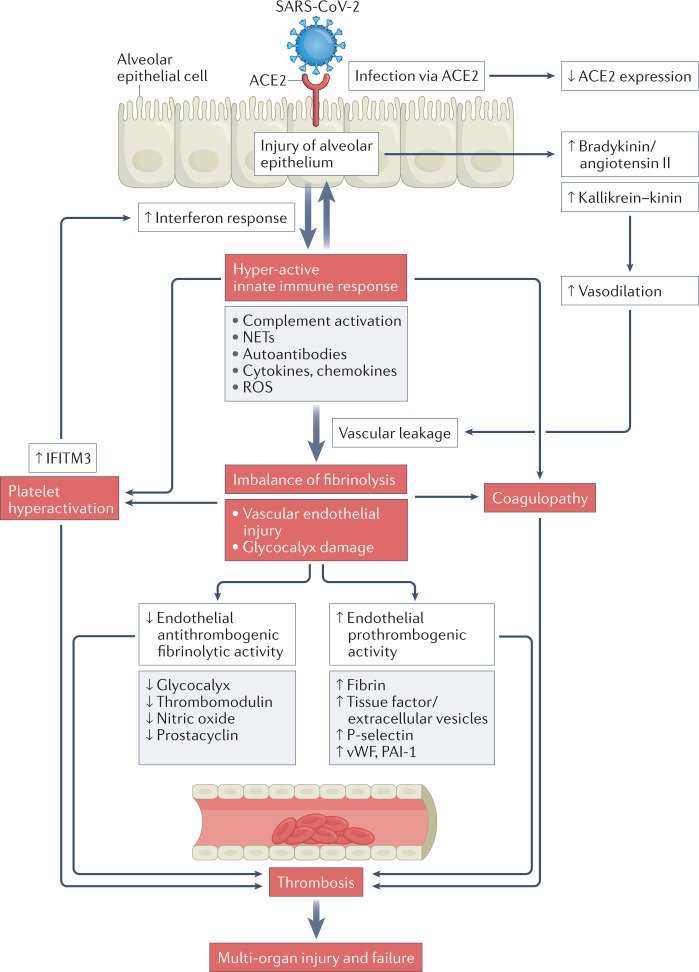
ACE2 has dual functions, as it regulates both the renin–angiotensin–aldosterone system and the kallikrein–kinin system39,40. Kinins are vasoactive peptides that cause relaxation of vascular smooth muscle cells and increased vascular permeability41,42. Dysregulated kinin degradation, owing to direct effects of the virus on ACE2, could increase kinin activity leading to angioedema43. The kallikrein–kinin system may thus be activated systemically during COVID-19, resulting in a ‘kinin storm’44 leading to increased vascular permeability, inflammation, fluid accumulation and organ damage (Fig. 2).
Fig. 2. Pathway contributing to COVID-19-associated coagulopathy.
COVID-19-associated coagulopathy (CAC) likely involves the dysregulation of numerous pathways that, in ways that are not currently well understood, culminate in endothelial damage, thrombosis and multi-organ failure. ACE2, angiotensin-converting enzyme 2; autoantibodies, anti-phospholipid-targeting autoantibodies; IFITM3, interferon-induced transmembrane protein 3; NET, neutrophil extracellular trap; PAI-1, plasminogen activator inhibitor 1; ROS, reactive oxygen species; vWF, von Willebrand factor. Adapted with permission from ref.35, Elsevier.
The markedly elevated D-dimer levels seen in severe COVID-19 (ref.3) implicate fibrin deposition and subsequent degradation as playing roles in the pathophysiology of COVID-19. However, the relative contributions of intravascular versus extravascular fibrin formation and lysis to D-dimer are not clear. Plasmin breakdown of this extravascular fibrin and leakage of D-dimer into the bloodstream may contribute to the observed elevated levels of D-dimer in patients with COVID-19. Indeed, during SARS-CoV-2 infection, prothrombotic TF and extracellular vesicles are released from multiple cell types. The predominant source of TF-positive (TF+) extracellular vesicles found in broncho-alveolar lavage fluid (BALF) from patients with COVID-19 is likely activated lung epithelial cells. Although the cellular origin of TF+ extracellular vesicles in the blood is not definitively known, they are probably mainly derived from activated monocytes, with endothelial cells, neutrophils and epithelial cells also contributing45. Whatever the source, elevated circulating levels of TF+ extracellular vesicles are associated with increased disease severity, including an increased incidence of venous thromboembolism in patients with COVID-19 (refs.46,47), strongly implicating their involvement in CAC.
SARS-CoV-2 and the blood–brain barrier
In addition to the lungs, clinically important targets of SARS-CoV-2 include the kidneys, liver, heart, skin and central nervous system (CNS), particularly the brain48–50 (Fig. 1). In serial histological analyses of 100 COVID-19-positive autopsies, 58 brains revealed widespread microthrombi and microinfarcts in the neocortex, and the presence of microthrombi was often associated with small and patchy infarctions. Moreover, immunohistochemical staining revealed robust expression of the ACE2 receptor in the intraparenchymal blood vessels51. Drawing from these observations, it is not surprising that patients infected with SARS-CoV-2 often encompass a wide spectrum of neurological symptoms, including headache, sleep disorders, alterations in sense of smell and taste, ischaemic stroke, major cognitive defects, delirium and diminished levels of consciousness52–54. These neurological manifestations of SARS-CoV-2 infections, which are associated with an increased risk of in-hospital mortality55, are believed to be primarily immunothrombosis-dependent51, resulting in so-called dysregulated ‘neurocoagulation’ with excess thrombin generation, alterations in blood–brain barrier endothelial cell function and neuroinflammation48,56,57 (Fig. 2).
Although somewhat controversial, SARS-CoV-2 may potentially infect brain tissue directly, thereby triggering cellular damage58. However, it seems likely that it also affects the brain via indirect mechanisms. In some post-mortem studies of patients with COVID-19, multifocal microvascular endothelial brain injury was detected without any evidence of SARS-CoV-2 in the brain, implicating an indirect effect via host defence mechanisms50. By contrast, in another post-mortem series, SARS-CoV-2 RNA was detected in some patients in one or more brain regions, suggesting that the virus might elicit direct neurocytopathic effects59. In vitro studies support the latter hypothesis, in that SARS-CoV-2 can directly infect murine and human neurons with accompanying metabolic effects on infected and neighbouring neurons60. It remains unclear, however, which brain regions or cell types are most susceptible to either direct or indirect SARS-CoV-2-mediated damage, and how the virus most effectively accesses the brain tissues via the blood–brain barrier.
When expressed by different cells in the CNS, including blood–brain barrier endothelial cells, SARS-CoV-2-derived molecules may trigger neuroinflammatory or behavioural responses via pattern-recognition receptors (PRRs), such as Toll-like receptor 2 (TLR2) and TLR4. For example, the S1 subunit of the SARS-CoV-2 spike protein, when dissociated from the virion, can cross the blood–brain barrier in mice61. Even in the absence of viral RNA, the S-protein can be found localized to microvascular endothelial cells, where its S1 subunit can trigger pro-inflammatory cytokine expression and complement activation that could provoke a thrombotic outcome62. In vivo, the S1 subunit can induce abnormal behavioural responses and neuroinflammation, putatively by triggering TLR2-dependent and TLR4-dependent cellular responses63. The S-protein is also highly glycosylated, providing a means of modulating the immune response locally and systemically. The main SARS-CoV-2 protease, Mpro, has also been proposed to contribute to CNS pathology, partly by cleaving endothelial cell-expressed NF-κB essential modulator (NEMO), thereby resulting in cellular damage and setting the stage for a hypercoagulable state64. Recognizing the heterogeneity of the neurovasculature, and the endothelial cells that form the blood–brain barrier, further investigation is needed to determine which specific regulatory factors are critical in modulating the passage of SARS-CoV-2 and its component proteins into the CNS and their ultimate role in triggering CNS pathology65.
In summary, there is now substantial evidence that SARS-CoV-2 infection can cause vascular endothelial cell dysfunction and that this underlies the pathology seen in many patients with severe COVID-19. Box 2 lists some of the major scientific questions that still need to be addressed in this area. In the following section we discuss how hyper-inflammation can contribute to CAC.
Box 2 SARS-CoV-2 and vascular dysfunction: major scientific gaps and questions.
What are the mechanisms underlying SARS-CoV-2-induced endothelial dysfunction, activation and vasculopathy?
How does SARS-CoV-2 differentially affect the vasculature at different sites in different organs?
What are the implications of endothelial glycocalyx disruption in different vascular beds? What are the mechanisms underlying glycocalyx disruption, how can it be monitored and what mitigating treatment modalities can be designed?
What roles do circulating tissue factor and extracellular vesicles play in COVID-19-associated coagulopathy (CAC), what are the mechanisms for their release, can they be targeted and are they useful predictive biomarkers for CAC?
What are the mechanisms for direct and indirect SARS-CoV-2 infection of the central nervous system and what is the pathogenesis of neuronal damage?
What features of the blood–brain barrier endothelium regulate the entry of SARS-CoV-2, viral proteins and inflammatory mediators into the brain?
Hyper-inflammation and coagulopathy
Neutrophils, NETs and complement
Neutrophils represent a major cellular component of the innate immune system and are recruited early after viral infection in response to chemotactic factors produced at sites of virus-mediated injury (Fig. 2). In addition to being phagocytic, neutrophils release various proteolytic enzymes, chemokines, cytokines and reactive oxygen species (ROS). They also contribute significantly during early immune responses to viral infections through the formation of NETs66. NETs are formed when neutrophils undergo programmed cell death, referred to as NETosis. Elevated in the blood of patients with COVID-19, and often in conjunction with neutrophilia67, NETs are web-like structures comprising DNA, histones, microbicidal proteins, oxidant enzymes, coagulants and complement factors66. During early activation of innate immunity, NETs can promote clotting, in part via expression of functional TF and by capturing platelets. This has been documented in COVID-19, where increased plasma levels of NETs and TF+ extracellular vesicles correlate with thrombin generation, severity of respiratory status and risk of death24,67. Moreover, sera from severely ill patients with COVID-19 can stimulate NET formation in neutrophils from uninfected controls, and can trigger heightened complement activation25,68. Indeed, excess complement activation and NETosis are well established in COVID-19 (ref.69). Potential relevance to CAC is underscored by reports showing that ex vivo inhibition of complement component C3 disrupts TF expression in neutrophils from patients with COVID-19 (ref.70). Also, pilot studies in patients with COVID-19 have reported that anti-C3 and anti-C5 agents dampen neutrophilia, attenuate NET release and reduce inflammation70.
Post-mortem analyses of tissues from patients with COVID-19 consistently revealed deposition of complement activation fragments in the vasculature of multiple organs together with microvascular and macrovascular endotheliopathy and thrombosis71. Clinically, microvascular thrombosis can manifest itself as skin purpura or the condition known as ‘COVID toe’ (Fig. 1). Serial studies of serum from patients with COVID-19 revealed early and persistent hyperactivation of complement, with increased circulating levels of proteolytic fragments72–75 that are predictive of poor outcomes. These findings suggest SARS-CoV-2 can trigger complement activation via all three major pathways: first, the classical pathway through formation of complement-fixing IgG and IgM antibody immune complexes73; second, the alternative pathway by competing with the negative regulator factor H76; and last, the lectin pathway through direct interaction of the viral spike protein with mannose-binding lectin (MBL), ficolin 2 and collectin 11, and by viral nucleocapsid protein-mediated enhancement of MASP2 cleavage of complement component C4 (refs.77,78). SARS-CoV-2 can also induce synthesis and release of complement factors from infected respiratory epithelial and endothelial cells via Janus kinase 1 (JAK1)-dependent and/or JAK2-dependent pathways, interestingly in parallel to the release of procoagulant factors79.
In addition to complement-triggered release of TF-carrying NETs, there are multiple other mechanisms by which SARS-CoV-2-induced complement hyperactivation may initiate coagulation80,81. For example, cleavage of complement component C5 leads to release of prothrombotic factors from platelets. Also, C5 cleavage can result in TF activation and increased P-selectin expression on endothelial cells, both of which recruit inflammatory leukocytes. COVID-19 complications in seriously ill patients are proposed to involve secondary tissue damage due to a cycle of dysregulated and/or hyperactive coagulation and inflammatory pathways, fuelled by positive feedback loops between complement, neutrophils, NETs and coagulation (Fig. 2). Several clinical trials involving treating patients with COVID-19 with anti-complement drugs have been performed (reviewed in refs.19,81). These have yielded promising results but were confounded by the small numbers of patients recruited and, also, the challenges of treating a dynamically changing disease.
Platelet dysfunction contributing to immunothrombosis
Although thrombocytopenia is common in many viral illnesses, it is not frequently observed in COVID-19 (refs.2,82–85). Nonetheless, heightened platelet activation is often detectable in COVID-19, triggered by multiple factors including soluble coagulation and complement factors (for example, thrombin, C3a and C5a), inflammatory cytokines, anti-SARS-CoV-2 immunoglobulins, changes in shear stress and exposure to activated endothelial cells and neutrophils86,87. Through the release of their intracellular granule constituents and externalization of the prothrombotic membranous phosphatidylserine surface, platelets help trigger and sustain an immunothrombotic amplification loop that contributes to CAC86. Platelets from patients with COVID-19 exhibit enhanced aggregation, accompanied by increased cell surface P-selectin expression88–90 (Fig. 2), but with reduced activation of αIIbβ3 integrin89,91,92. Patients with COVID-19 also have increased circulating levels of soluble platelet activation markers (for example, CC-chemokine ligand 5 (CCL5; also known as RANTES) and platelet factor 4)24,88,92,93, as well as increased platelet–neutrophil and platelet–monocyte aggregates24,89,94. With increased vascular endothelial activation, these aggregates may readily adhere to the vessel wall. Adherence of platelet–neutrophil aggregates is likely to result in the release of pro-thrombotic and pro-inflammatory NETs67,86,95, whereas platelet–monocyte aggregates can promote hypercoagulability via increased monocyte TF expression94. Overall, strong evidence points to activated platelets, neutrophils and NETs playing significant and complementary roles in thrombus formation, and as predictors of more severe disease8,96.
Mechanisms underlying the augmented platelet reactivity in COVID-19 appear to involve increased MAPK signalling and thromboxane A2 production88,89,97, responses that are likely due to reported SARS-CoV-2-induced changes in the platelet transcriptome98–100. RNA-sequencing analyses comparing platelets from patients with COVID-19 with those from healthy controls revealed more than 3,000 differentially expressed genes89. By contrast, only a subset of these genes was differentially expressed in the platelets of non-intensive care unit versus intensive care unit-admitted patients with COVID-19 (ref.89), indicating that these changes in platelet gene expression are most likely an early response to SARS-CoV-2 infection and not necessarily associated with disease severity.
It is not known whether SARS-CoV-2-induced changes to the platelet transcriptome occur as a result of direct viral infection of platelets, or indirectly secondary to hyper-inflammatory responses to the virus. Initial studies suggested that SARS-CoV-2 mRNA could be detected in platelets from some patients with COVID-19 (refs.88,89). However, it remains unclear whether platelets express ACE2, or whether there are other viral uptake pathways, such as via extracellular vesicles101,102. Comparative analyses of platelet transcriptomes from patients with COVID-19 with platelet transcriptomes from patients with other viral infections suggest that there are likely alternative mechanisms for viral entry into host cells. For instance, dengue virus, influenza virus and SARS-CoV-2 infections are all marked by increased levels of interferon-induced transmembrane 3 (IFITM3), an antiviral protein critical for regulating endocytosis, viral entry and replication89,101,103 (Fig. 2). Furthermore, SARS-CoV-2 alters the megakaryocyte transcriptome through an ACE2-independent but CD147-dependent mechanism, which could explain reports of SARS-CoV-2 uptake in platelets and megakaryocytes101.
Although platelet hyperactivity is common in COVID-19, platelet inhibitors have not convincingly provided benefit in preventing organ failure or CAC104,105. For example, in a randomized trial of more than 500 hospitalized non-critically ill patients with COVID-19, addition of P2Y12 inhibitors to therapeutic doses of heparin did not increase the odds of being free of acute respiratory distress syndrome, reduce the need for organ support, improve survival at 21 days or decrease thrombotic events105. Also, in a randomized, controlled trial of approximately 15,000 patients with COVID-19, it was similarly concluded that aspirin (which limits platelet function by inhibiting cyclooxygenase 1) had little effect on the incidence of mechanical ventilation or mortality104. However, the group receiving aspirin did experience a slight reduction in the number of thrombotic events and a small increase in the rate of being discharged within 28 days. Box 3 summarizes key questions that remain to be addressed in terms of understanding the contribution of hyper-inflammation and platelet dysfunction to CAC. In the following section we address the role of hypercoagulation in CAC.
Box 3 Hyper-inflammation and coagulopathy in COVID-19: major scientific gaps and questions.
What role do neutrophil extracellular traps (NETs) play in COVID-19-associated coagulopathy (CAC)? Are circulating NETs a marker of disease severity? Can NETs be safely targeted to improve clinical outcomes?
What are key complement activation products and pathways that promote CAC? Are these the same in all vascular beds?
Which complement pathways and components are the most efficacious and safest therapeutic targets?
Assuming SARS-CoV-2 can infect platelets and megakaryocytes, what are the mechanisms of viral entry into the cells? Are there specific viral receptors, aside from angiotensin-converting enzyme 2 (ACE2)? Could modified glycans participate in viral entry?
Can platelet transcriptomics be used as a tool to predict risk of thrombosis?
What ‘new’ molecular pathways regulating platelet activation might be targeted to reduce thrombosis in COVID-19, either alone or in combination with other interventions?
When in the course of COVD-19 is it safe and most efficacious to therapeutically target the innate immune response, while still ensuring an adequate host response to the infection?
Hypercoagulability in CAC
Changes in plasma procoagulant and fibrinolytic activity
Multiple studies have documented elevated procoagulant activity and suppressed fibrinolytic activity in patients with COVID-19, which together could drive CAC17,106,107. A study that compared the extent of these abnormalities in hospitalized patients with COVID-19 with patients with sepsis detected elevated plasma levels of soluble thrombomodulin in both groups, consistent with heightened endothelial cell activation17 (Fig. 2). Both patient groups also exhibited delayed but enhanced fibrin formation and increased fibrin resistance to fibrinolysis. However, plasma from patients with COVID-19 and from patients with sepsis showed different perturbations in the kinetics of thrombin generation and fibrinolytic activity. Whereas plasma from patients with sepsis had normal thrombin generation potential, plasma from patients with COVID-19 had enhanced rates of thrombin generation17,108,109. Plasma from patients with sepsis also showed delayed plasmin generation, whereas those with COVID-19 had normal plasmin-generating potential. Finally, plasma from patients with COVID-19 showed delayed times to thrombin, plasmin and fibrin formation with an increased sequential organ failure assessment (SOFA) score (a marker of disease severity).
Transcriptional profiling of BALF from patients with COVID-19 versus individuals without COVID-19 demonstrated differential regulation of genes encoding coagulation and fibrinolytic proteins110. Elevated TF transcripts were detected in BALF cell samples from patients with COVID-19, and TF expression may be higher in severely ill patients versus moderately ill patients or healthy controls111. SARS-CoV-2 was also associated with upregulation of genes encoding procoagulant proteins (for example, factor XI, factor VII and von Willebrand factor (vWF)) together with the downregulation of genes encoding anticoagulants (thrombomodulin and protein S) and profibrinolytic proteins (urokinase and urokinase plasminogen activator receptor).
Changes in urokinase pathway gene expression were previously implicated in a mouse model of SARS-CoV, including increased expression of genes encoding plasminogen activator inhibitor 1 (PAI-1), tissue plasminogen activator (tPA) and urokinase plasminogen activator receptor112. Notably, changes in gene expression were not completely congruous in these studies, which may reflect differences in the host (human versus mouse), the virus (SARS-CoV-2 versus mouse-adapted SARS-CoV), the disease stage (moderate versus severe disease), the sample (BALF versus lung) and/or other determinants of coronavirus infection or severity. Moreover, it is difficult to anticipate the functional implications of these changes, particularly given observations that fibrinolytic pathway genes with opposing function (for example, PAI-1 and tPA) are coordinately regulated in certain settings113.
Dysregulation of the protein C system contributing to CAC
Activated protein C is a naturally occurring plasma serine protease that has both anticoagulant activity and direct cell signalling activities that require, primarily, EPCR and the protease activated receptors (PARs) PAR1 and PAR3 (refs.114,115). There is growing evidence that the integrity of the protein C system, required for generation of activated protein C, is impaired in CAC. Low levels of protein C in hospitalized patients with COVID-19 were associated with worse disease progression and increased mortality116. This mirrors observations in patients with sepsis and disseminated intravascular coagulation where low protein C levels were a useful biomarker to identify patients at risk for developing severe illness117,118. Low protein C levels, which confer a heightened risk of ischaemic stroke119 and dementia120, may also increase the risk of stroke in patients with COVID-19 (ref.116) or ‘brain fog’, one of the features of long COVID (also known as post-acute sequelae of SARS-CoV-2 infection). Increased levels of soluble thrombomodulin — which correlate directly with lung endothelial cell damage and disease severity — may indicate that the generation of activated protein C is impaired17,110,121,122. Also consistent with reduced generation of activated protein C, as well as endothelial cell damage and activation, are reports of elevated levels of soluble EPCR in patients with COVID-19 (refs.110,123). EPCR shedding from inflamed endothelium may not only reduce the ability to generate activated protein C but also reduce the ability of activated protein C to induce cytoprotective signalling. Thus, shedding of endothelial thrombomodulin and EPCR may induce a protein C pathway dysfunction that, in turn, induces cellular resistance to activated protein C and limits its ability to rebalance dysregulated inflammatory and coagulant pathways.
From the preceding narrative, it is evident that the protein C system represents a potential target for mechanistic and therapeutic studies of CAC. The cytoprotective effects of activated protein C and/or its variants may be uniquely effective in blunting immunothrombosis in COVID-19, particularly as EPCR-dependent PAR1 and PAR3 signalling also elicits anti-inflammatory effects.
Anti-phospholipid antibodies
An unusual feature of CAC, among thrombotic disorders in general, is that it involves thrombosis in arteries, veins and the microcirculation — a spectrum reminiscent of patients with severe anti-phospholipid syndromes124. Indeed, there have been multiple case reports of patients with COVID-19 developing severe thrombotic disorders accompanied by anti-phospholipid antibodies and lupus anticoagulant124–126. However, transient development of anti-phospholipid antibodies can accompany other viral infections, so it remains to be established whether an anti-phospholipid syndrome is truly induced in patients with COVID-19 and what role this may have in driving thrombosis and organ damage in these patients124,126. Interestingly, some mechanistic studies have reported that isolated IgG from the serum of patients with COVID-19 who have high titres of anti-phospholipid antibodies is strongly prothrombotic when injected into mice127,128, and is capable of activating cultured human endothelial cells129. Clearly, more research is required to determine whether anti-phospholipid antibodies in patients with COVID-19 are driving CAC, and if so, whether such antibodies persist in these patients124,126. Box 4 lists key questions that need to be addressed to better understand the hypercoagulability that occurs in COVID-19. In the final section of this article, we consider the suitability of the available animal models of COVID-19 for studying the mechanisms of CAC.
Box 4 Hypercoagulability in COVID-19: major scientific gaps and questions.
Why is disseminated intravascular coagulation not a major feature of COVID-19?
Can combination therapies be considered to ‘rebalance’ alterations in coagulation and fibrinolysis in COVID-19, thereby minimizing the risk of COVID-19-associated coagulopathy (CAC)?
What is the relative contribution of respiratory epithelial cells in the release of coagulation, fibrinolytic and complement proteins that impact on local and systemic thrombosis and CAC? Can these cells be targeted to reduce thrombotic risk?
Which components of the protein C system and its downstream effectors are the best candidates as therapeutic targets to prevent and/or treat CAC? Can combination therapies be considered?
What are the mechanisms by which anti-phospholipid antibodies might contribute to CAC?
Animal models of COVID-19
Preclinical animal models of SARS-CoV-2 infection are important tools for improving our understanding of host–virus interactions and COVID-19. They are essential for rapid testing of novel therapies and can allow for controlled and detailed examination of the host response to infection. Two years into the pandemic, various small and large animal models have been developed, all with distinct advantages and disadvantages130.
Mice are the most commonly used small animal model due to their short gestation period and time to sexual maturity, minimal space requirements, ease of manipulating the mouse genome and relatively low cost. Additionally, mice models are useful tools to investigate mechanisms of underlying comorbidities, such as diabetes, hypertension, obesity and the impact of other factors such as age130. An initial limitation to using mice to study COVID-19 was that the original isolates of SARS-CoV-2 did not infect wild-type mice, as the virus did not bind to the murine ACE2 (mACE2) entry receptor131. Consequently, several laboratories adapted the SARS-CoV-2 spike protein to bind to mACE2. This approach combined with a serial passage in mice resulted in mouse-adapted SARS-CoV-2 strains that caused moderate to lethal lung disease132–134. Thus, mouse-adapted SARS-CoV-2 (MA10) could infect wild-type mice and drive acute lung injury and acute respiratory distress syndrome in a dose-dependent manner133. Infection also caused a decrease in lung surfactant production and significant respiratory dysfunction in mice. Similarly to SARS-CoV-2, MA10 also induced a pronounced hyper-immune, pro-inflammatory cytokine and chemokine response, leading to recruitment of inflammatory cells to the lung. Immunohistochemical analyses of the lungs from MA10-infected mice revealed increased TF expression that is accompanied by extravascular fibrin staining135. These initial studies suggest that the MA10 mouse model recapitulates some of the coagulopathic features observed in humans infected with SARS-CoV-2, and thus might prove a useful tool in deciphering mechanisms and identifying novel therapies.
To circumvent the challenge of having to manipulate the infecting virus, mice have also been engineered or transduced to express human ACE2. K18-hACE2 transgenic mice express hACE2 (ref.136), albeit restricted primarily to the respiratory epithelium and brain. Notably, they are highly susceptible to SARS-CoV-2 infection following intranasal exposure, and as such might serve as a good model for gaining novel insights into infection via this route. High levels of SARS-CoV-2 were detected in the lungs of SARS-CoV-2-infected K18-hACE2 mice, with lower levels of the virus found in other tissues. Over a period of 2–7 days, in concert with increased D-dimer levels and a prolonged prothrombin time, there was evidence of a progressive inflammatory process, again affecting predominantly the lungs137. Indeed, the pathology seen in this mouse model was similar to that observed in patients with severe COVID-19, with histological evidence of diffuse broncho-alveolar damage with oedema, fibrin deposits, leukocyte infiltration and pneumocyte hyperplasia137. This model is also proving to be an excellent tool to study SARS-CoV-2 neuroinvasion and the subsequent clinicopathologic manifestations, featuring meningoencephalitis, thrombosis, haemorrhage and vasculitis138.
Hamsters have emerged as a useful model for SARS-CoV-2 infection owing to their susceptibility to disease following infection and the ability to transmit the virus between animals via aerosolization139,140. They are a promising model, although some drawbacks are the lack of readily available genetic and biochemical reagents, their relatively high cost and their high space requirements. Underlining the value of this model, and particularly interesting in view of the heightened risk of COVID-19 in individuals with diabetes and obesity, hamsters on a high-fat and high-sugar diet developed worse lung disease following SARS-CoV-2 infection than mice fed a regular diet, with lung histological evidence of vasculitis, haemorrhage, oedema and notable fibrin deposition141. In spite of their limitations, hamsters are likely to be an essential tool for SARS-CoV-2 research and may yield important insights into COVID-19 pathogenesis and CAC. Indeed, these animal models are already holding promise to be instructive, as infection of K18-hACE2 mice and hamsters with the B.1.1.529 Omicron variant causes significantly milder disease, with less lung inflammation, findings that are in line with the apparent reduced pathogenicity of Omicron variants in humans142,143.
Studies of non-human primate infections of SARS-CoV-2 are limited by space and facility requirements and by the high cost of experiments. However, as the closest related species to humans, non-human primates remain an important consideration for preclinical vaccine and drug development, while also offering important insights into human pathophysiology and the immunothrombotic response to SARS-CoV-2 infections. Rhesus and cynomolgus macaques, as well as African green monkeys, experience mild (in the case of the macaque) to moderate (in African green monkeys) lung disease after SARS-CoV-2 infection144,145. Aged rhesus macaques develop more severe symptoms, reflecting what is seen in humans with COVID-19. Notably, researchers found that African green monkeys infected with SARS-CoV-2 also developed a coagulopathy141. Although not extensively evaluated, in the days following infection with SARS-CoV-2, circulating levels of fibrinogen and pro-inflammatory cytokines rapidly rose, and post-mortem analyses of the lungs revealed broncho-alveolar epithelial damage, with neutrophilic inflammation, alveolar oedema and haemorrhage, fibrin deposition and microthrombi within alveolar capillaries146. Involvement of other organs and tissues for evidence of small and large vessel thrombosis has also not been fully studied.
Animal models remain a cornerstone for gaining insights into mechanisms underlying the immunothrombosis associated with COVID-19 and for strategic development of novel and effective therapies. Moreover, they afford the opportunity to evaluate how CAC can be modified by known determinants of disease severity, including age, sex and epigenetic and genetic factors, and by underlying comorbidities, such as diabetes and obesity. A notable shortcoming of all current models is the apparent lack of phenotypes that fully recapitulate the CAC that occurs in humans, particularly in terms of modelling microvascular and macrovascular thrombosis. Recognition of the strengths and weaknesses of any animal model is therefore vital before extrapolating the results to humans.
Conclusion
The NHLBI’s workshop on CAC was convened in May 2021, soon after the first SARS-CoV-2 variants of concern began to emerge. Highlighting the urgency of assembling such a conference, it was already widely known that thrombosis in the microvasculature and macrovasculature was a life-threatening complication of COVID-19, particularly for those with severe disease7–11,147. Equally disconcerting was the increasing recognition that a high percentage of patients with COVID-19 suffer from long-term sequelae (long COVID)48,49. Whether excessive coagulation, impaired fibrinolytic capacity and/or a prominent endotheliopathy might contribute to the pathogenesis of long COVID by extending an acute CAC to a chronic condition remains to be determined148,149.
Although much has been learned in the past 2 years about the pathophysiology of COVID-19, insights into the triggering events of CAC remain elusive, as do effective preventative and therapeutic strategies (see Table 1). This is evident from the uncertainties and controversy surrounding the use of several therapeutic agents in different clinical scenarios150,151. This is not surprising, given that CAC is a highly complex and dynamic process, involving the interplay between multiple biochemical, proteolytic and cellular pathways. This makes it difficult to differentiate which processes are causal, consequential or merely coincidental. It is thus a challenge to discern which pathway to therapeutically target, and when to do so in the course of the disease, without disrupting natural protective mechanisms. Indeed, it is likely that one or more CAC mechanisms predominate at distinct stages of the disease and at different organ sites and vascular beds. In that regard, we have a better handle on the early stages of COVID-19 following infection, where the virus damages the alveoli and adjacent microvasculature, with an initial local hypoxic and immunothrombotic response19,31. With subsequent dissemination of the disease, identifying key triggers within the complex immunothrombotic web becomes more of a challenge.
Table 1.
Selected current treatments for non-pregnant adult patients hospitalized for COVID-19 (adapted from ref.153, Springer Nature Limited)
| Immunothrombosis therapy | Drug/target | Treatments and responses | Limits/recommendations | Refs. |
|---|---|---|---|---|
| Corticosteroids | Dexamethasone | Hospitalized patients; increases organ support-free days and reduces 28-day mortality | Recommended | 154–156 |
| Janus kinase (JAK) inhibitors | Baricitinib (with IL-6 inhibitor and dexamethasone) | Patients with moderate–severe illness; rapid declines of C-reactive protein, ferritin and D-dimer with gradual improvement in haemoglobin, platelet counts and clinical status | At least 2 large RCTs; high likelihood of benefit | 157 |
| IL-6 inhibitors | Toclizumab | Hospitalized patients; reduces inflammatory markers, D-dimer and fibrinogen; reduced 21 or 28-day mortality and organ support-free days | For critically and severely ill patients; widely used | 158 |
| Anticoagulants | Low molecular weight heparin (LMWH) — prophylactic intensity | Critically ill patients (hospitalized, intensive care unit) for venous thromboemboli prophylaxis and to increase the number of organ support-free days; no effect on survival to hospital discharge | Certainty of evidence from multiple trials is low; but widely used | 154–156,159 |
| LMWH — therapeutic dose | Patients with moderate-severity illness (hospitalized, low-flow oxygen use, elevated D-dimer) for venous/arterial thromboemboli prophylaxis and to reduce organ support-free survival; uncertain if an effect on survival; consider bleeding risk | Certainty of evidence from multiple trials is low; but widely used | 154–156,159 | |
| Rivaroxaban (or other direct oral anticoagulants) | Patients with moderate-severity illness; no effect on survival or need for supplemental oxygen | Not recommended | 154,160 | |
| Anti-platelets | Aspirin, P2Y12 inhibitors | Early use of ASA may lower odds of 28-day in-hospital mortality; no benefit from P2Y12 inhibitors | Not recommended | 104,161,162 |
| Thrombolytics | Alteplase (tPA) | For respiratory failure with heparin; evidence of moderate improved oxygenation | Early phase | 163 |
| Anti-spike protein monoclonal antibodies | Casirivumab and imdevimab | Hospitalized patients; may reduce 28-day mortality | Uncertain which patient groups will benefit most | 164 |
| Anti-complement | Inhibitor of C5 activation: ravulizumab | Critically ill patients, phase III study; stopped due to lack of clinical benefit | No clinical benefit | 81 |
| Inhibitor of C5 activation: zilucoplan | Patients with moderate-severity illness; improved oxygenation at day 15, reduced cytokine levels and reduced 28-day mortality | Underpowered | 165 | |
| C5a blockade: (e.g., violbelimab, BDB-001); C5a-receptor blockage (avdoralimab) | Hospitalized patients; evidence of improvements in oxygenation | Early phase or underpowered studies | 81 | |
| C3 inhibitors (e.g., AMY-101, APL9), C1-esterase inhibitor, MASP2 antibody (narsoplimab) | Hospitalized patients; evidence of improvements in oxygenation | Early phase or underpowered studies | 70,160 | |
| Bradykinin-targeted | Icatibant (bradykinin 2 receptor antagonist), ecallantide (kallikrein inhibitor) | Icatibant ± C1-esterase inhibitor; evidence of improvements in oxygenation | Underpowered | 164 |
Detailed, updated therapy guidelines for patients with COVID-19 and associated coagulopathy are available from several organizations. tPA, tissue plasminogen activator.
It is important to recognize that all of the preceding discussion refers to information gathered from patients infected with the Alpha or Delta variants. With few solid data143,152, the impression is that the more recent Omicron variants are less immunothrombotic and cause less severe disease. Animal studies support these observations142,143. In spite of the apparent reduced pathogenicity of these more recent variants, scientists in the field must nonetheless continue to be vigilant and persist in delineating the underlying mechanisms so that we can be ahead of the curve with effective diagnostics and therapeutics.
Adding to the complexity, we have few insights into the factors — acquired, environmental and/or epigenetic — that render some populations (for example, older people, individuals with obesity, individuals with diabetes) at increased risk of severe disease and CAC. The workshop provided a unique and important forum to gather wide expertise in diverse disciplines, with the common aim of integrating our knowledge to gain new insights into CAC, to identify gaps and opportunities in the science and to explore practical lines of study that might yield clinical benefit. With the continued uncertainty of the emergence of new SARS-CoV-2 variants, such focused research continues to be crucial for the development of effective anti-immunothrombotic preventative and therapeutic strategies for patients infected with SARS-CoV-2.
Acknowledgements
The authors acknowledge the support of the National Heart, Lung, and Blood Institute (NHLBI) for the ‘COVID-19 Associated Coagulopathy’ workshop. They thank all speakers and panellists who participated in the COVID-19-associated coagulopathy (CAC) workshop. They thank E. Middleton (Department of Internal Medicine, University of Utah, Salt Lake City, UT, USA) for providing the original resource for ‘COVID toe’ in Fig. 1. E.M.C. was supported, in part, by grants from CanVECTOR (COVID-19 Rapid Response Funding Competition), the Canada Research Chairs programme, the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Supported in part by National Institutes of Health (NIH) grants R01 HL142975 (J.H.G., L.O.M.), R01 HL104165 (L.O.M.), R35 HL135823 (J.H.M.) and OT2 HL156812 (J.H.M., D.N.).
Author contributions
D.N. and J.H.M. were the co-chairs of the COVID-19-associated coagulopathy (CAC) workshop. K.M., E.M.C., R.Q.W., A.S.W., L.O.M., L.E.G., R.A.C., M.T.R., F.L.vdV., K.M.H., J.H.G., N.M., D.N. and J.H.M. wrote and edited portions of the manuscript. K.M. designed Figs. 1 and 2.
Peer review
Peer review information
Nature Reviews Immunology thanks M. Levi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Disclaimer
The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the National Institutes of Health (NIH). No official endorsement by the National Heart, Lung, and Blood Institute (NHLBI)/NIH is intended or should be inferred.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
NIH Funding Opportunities for COVID-19 Research: https://covid19.nih.gov/funding/open-funding-opportunities
Notices of Special Interest (NOSI) on Enhancing Research on Deciphering Mechanisms of CAC: https://grants.nih.gov/grants/guide/notice-files/NOT-HL-23-003.html
Contributor Information
Kyung Moon, Email: kyung.moon@nih.gov.
James H. Morrissey, Email: jhmorris@umich.edu
References
- 1.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nahum J, et al. Venous thrombosis among critically ill patients with coronavirus disease 2019 (COVID-19) JAMA Netw. Open. 2020;3:e2010478. doi: 10.1001/jamanetworkopen.2020.10478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goshua G, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iba T, Warkentin TE, Thachil J, Levi M, Levy JH. Proposal of the definition for COVID-19-associated coagulopathy. J. Clin. Med. 2021 doi: 10.3390/jcm10020191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trimaille A, Bonnet G. [COVID-19 and venous thromboembolism] [French] Ann. Cardiol. Angeiol. 2020;69:370–375. doi: 10.1016/j.ancard.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolai L, et al. Immunothrombotic dysregulation in COVID-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation. 2020;142:1176–1189. doi: 10.1161/CIRCULATIONAHA.120.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang C, et al. Incidence of venous thromboembolism in hospitalized coronavirus disease 2019 patients: a systematic review and meta-analysis. Front. Cardiovasc. Med. 2020;7:151. doi: 10.3389/fcvm.2020.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang L, et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020;142:114–128. doi: 10.1161/CIRCULATIONAHA.120.046702. [DOI] [PubMed] [Google Scholar]
- 11.Wichmann D, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann. Intern. Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J. Med. Virol. 2020;92:2409–2411. doi: 10.1002/jmv.26097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agrati C, et al. Elevated P-selectin in severe COVID-19: considerations for therapeutic options. Mediterr. J. Hematol. Infect. Dis. 2021;13:e2021016. doi: 10.4084/mjhid.2021.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connors JM, et al. Effect of antithrombotic therapy on clinical outcomes in outpatients with clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial. JAMA. 2021;326:1703–1712. doi: 10.1001/jama.2021.17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouck EG, et al. COVID-19 and sepsis are associated with different abnormalities in plasma procoagulant and fibrinolytic activity. Arterioscler. Thromb. Vasc. Biol. 2021;41:401–414. doi: 10.1161/ATVBAHA.120.315338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell RA, et al. Comparison of the coagulopathies associated with COVID-19 and sepsis. Res. Pract. Thromb. Haemost. 2021;5:e12525. doi: 10.1002/rth2.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonaventura A, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat. Rev. Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ackermann M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J. Thromb. Haemost. 2020;18:1559–1561. doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat. Rev. Immunol. 2013;13:34–45. doi: 10.1038/nri3345. [DOI] [PubMed] [Google Scholar]
- 24.Middleton EA, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skendros P, et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Invest. 2020 doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mandel J, Casari M, Stepanyan M, Martyanov A, Deppermann C. Beyond hemostasis: platelet innate immune interactions and thromboinflammation. Int. J. Mol. Sci. 2022 doi: 10.3390/ijms23073868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Purcell SC, Godula K. Synthetic glycoscapes: addressing the structural and functional complexity of the glycocalyx. Interface Focus. 2019;9:20180080. doi: 10.1098/rsfs.2018.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat. Rev. Immunol. 2020;20:389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans PC, et al. Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc. Res. 2020;116:2177–2184. doi: 10.1093/cvr/cvaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagashima S, et al. Endothelial dysfunction and thrombosis in patients with COVID-19-brief report. Arterioscler. Thromb. Vasc. Biol. 2020;40:2404–2407. doi: 10.1161/ATVBAHA.120.314860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Renzi S, Landoni G, Zangrillo A, Ciceri F. MicroCLOTS pathophysiology in COVID 19. Korean J. Intern. Med. 2020 doi: 10.3904/kjim.2020.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varga Z, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCracken IR, et al. Lack of evidence of angiotensin-converting enzyme 2 expression and replicative infection by SARS-CoV-2 in human endothelial cells. Circulation. 2021;143:865–868. doi: 10.1161/CIRCULATIONAHA.120.052824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldsmith CS, Miller SE, Martines RB, Bullock HA, Zaki SR. Electron microscopy of SARS-CoV-2: a challenging task. Lancet. 2020;395:e99. doi: 10.1016/S0140-6736(20)31188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nicosia RF, Ligresti G, Caporarello N, Akilesh S, Ribatti D. COVID-19 vasculopathy: mounting evidence for an indirect mechanism of endothelial injury. Am. J. Pathol. 2021;191:1374–1384. doi: 10.1016/j.ajpath.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glowacka I, et al. Differential downregulation of ACE2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J. Virol. 2010;84:1198–1205. doi: 10.1128/JVI.01248-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang H, et al. SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Res. 2008;18:290–301. doi: 10.1038/cr.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Imai Y, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sodhi CP, et al. Attenuation of pulmonary ACE2 activity impairs inactivation of des-Arg9 bradykinin/BKB1R axis and facilitates LPS-induced neutrophil infiltration. Am. J. Physiol. Lung Cell Mol. Physiol. 2018;314:L17–L31. doi: 10.1152/ajplung.00498.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhoola KD, Figueroa CD, Worthy K. Bioregulation of kinins: kallikreins, kininogens, and kininases. Pharmacol. Rev. 1992;44:1–80. [PubMed] [Google Scholar]
- 42.Marceau F, et al. Bifunctional ligands of the bradykinin B2 and B1 receptors: an exercise in peptide hormone plasticity. Peptides. 2018;105:37–50. doi: 10.1016/j.peptides.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 43.van de Veerdonk FL, et al. Kallikrein–kinin blockade in patients with COVID-19 to prevent acute respiratory distress syndrome. eLife. 2020 doi: 10.7554/eLife.57555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meini S, et al. Understanding the pathophysiology of COVID-19: could the contact system be the key? Front. Immunol. 2020;11:2014. doi: 10.3389/fimmu.2020.02014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mackman N, Grover SP, Antoniak S. Tissue factor expression, extracellular vesicles, and thrombosis after infection with the respiratory viruses influenza A virus and coronavirus. J. Thromb. Haemost. 2021;19:2652–2658. doi: 10.1111/jth.15509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosell A, et al. Patients with COVID-19 have elevated levels of circulating extracellular vesicle tissue factor activity that is associated with severity and mortality-brief report. Arterioscler. Thromb. Vasc. Biol. 2021;41:878–882. doi: 10.1161/ATVBAHA.120.315547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guervilly C, et al. Dissemination of extreme levels of extracellular vesicles: tissue factor activity in patients with severe COVID-19. Blood Adv. 2021;5:628–634. doi: 10.1182/bloodadvances.2020003308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spudich S, Nath A. Nervous system consequences of COVID-19. Science. 2022;375:267–269. doi: 10.1126/science.abm2052. [DOI] [PubMed] [Google Scholar]
- 49.Nalbandian A, et al. Post-acute COVID-19 syndrome. Nat. Med. 2021;27:601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee MH, et al. Microvascular injury in the brains of patients with COVID-19. N. Engl. J. Med. 2021;384:481–483. doi: 10.1056/NEJMc2033369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bryce C, et al. Pathophysiology of SARS-CoV-2: the Mount Sinai COVID-19 autopsy experience. Mod. Pathol. 2021;34:1456–1467. doi: 10.1038/s41379-021-00793-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yaghi S, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51:2002–2011. doi: 10.1161/STROKEAHA.120.030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Katsoularis I, Fonseca-Rodriguez O, Farrington P, Lindmark K, Fors Connolly AM. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet. 2021;398:599–607. doi: 10.1016/S0140-6736(21)00896-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: a systematic review and meta-analysis. Int. J. Stroke. 2021;16:137–149. doi: 10.1177/1747493020972922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frontera JA, et al. A prospective study of neurologic disorders in hospitalized patients with COVID-19 in New York City. Neurology. 2021;96:e575–e586. doi: 10.1212/WNL.0000000000010979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shavit-Stein E, et al. Neurocoagulation from a mechanistic point of view in the central nervous system. Semin. Thromb. Hemost. 2022 doi: 10.1055/s-0041-1741569. [DOI] [PubMed] [Google Scholar]
- 57.McAlpine LS, et al. Ischemic stroke, inflammation, and endotheliopathy in COVID-19 patients. Stroke. 2021;52:e233–e238. doi: 10.1161/STROKEAHA.120.031971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Erickson MA, Rhea EM, Knopp RC, Banks WA. Interactions of SARS-CoV-2 with the blood–brain barrier. Int. J. Mol. Sci. 2021 doi: 10.3390/ijms22052681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Serrano GE, et al. Mapping of SARS-CoV-2 brain invasion and histopathology in COVID-19 disease. medRxiv. 2021 doi: 10.1101/2021.02.15.21251511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Song E, et al. Neuroinvasion of SARS-CoV-2 in human and mouse brain. J. Exp. Med. 2021 doi: 10.1084/jem.20202135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rhea EM, et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 2021;24:368–378. doi: 10.1038/s41593-020-00771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nuovo GJ, et al. Endothelial cell damage is the central part of COVID-19 and a mouse model induced by injection of the S1 subunit of the spike protein. Ann. Diagn. Pathol. 2021;51:151682. doi: 10.1016/j.anndiagpath.2020.151682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Frank MG, et al. SARS-CoV-2 spike S1 subunit induces neuroinflammatory, microglial and behavioral sickness responses: evidence of PAMP-like properties. Brain Behav. Immun. 2022;100:267–277. doi: 10.1016/j.bbi.2021.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wenzel J, et al. The SARS-CoV-2 main protease Mpro causes microvascular brain pathology by cleaving NEMO in brain endothelial cells. Nat. Neurosci. 2021;24:1522–1533. doi: 10.1038/s41593-021-00926-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ross JM, et al. The expanding cell diversity of the brain vasculature. Front. Physiol. 2020;11:600767. doi: 10.3389/fphys.2020.600767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Porto BN, Stein RT. Neutrophil extracellular traps in pulmonary diseases: too much of a good thing. Front. Immunol. 2016;7:311. doi: 10.3389/fimmu.2016.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zuo Y, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020 doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang Y, et al. Carboxypeptidase B blocks ex vivo activation of the anaphylatoxin–neutrophil extracellular trap axis in neutrophils from COVID-19 patients. Crit. Care. 2021;25:51. doi: 10.1186/s13054-021-03482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Marik PE, Iglesias J, Varon J, Kory P. A scoping review of the pathophysiology of COVID-19. Int. J. Immunopathol. Pharmacol. 2021;35:20587384211048026. doi: 10.1177/20587384211048026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mastellos DC, et al. Complement C3 vs C5 inhibition in severe COVID-19: early clinical findings reveal differential biological efficacy. Clin. Immunol. 2020;220:108598. doi: 10.1016/j.clim.2020.108598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Magro C, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Leatherdale A, et al. Persistently elevated complement alternative pathway biomarkers in COVID-19 correlate with hypoxemia and predict in-hospital mortality. Med. Microbiol. Immunol. 2022 doi: 10.1007/s00430-021-00725-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Holter JC, et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc. Natl Acad. Sci. USA. 2020;117:25018–25025. doi: 10.1073/pnas.2010540117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Nooijer AH, et al. Complement activation in the disease course of COVID-19 and its effects on clinical outcomes. J. Infect. Dis. 2021;223:2214–2224. doi: 10.1093/infdis/jiaa646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sinkovits G, et al. Complement overactivation and consumption predicts in-hospital mortality in SARS-CoV-2 infection. Front. Immunol. 2021;12:663187. doi: 10.3389/fimmu.2021.663187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yu J, et al. Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition. Blood. 2020;136:2080–2089. doi: 10.1182/blood.2020008248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ali YM, et al. Lectin pathway mediates complement activation by SARS-CoV-2 proteins. Front. Immunol. 2021;12:714511. doi: 10.3389/fimmu.2021.714511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Conway EM, Pryzdial EL. Is the COVID-19 thrombotic catastrophe complement-connected? J. Thromb. Haemost. 2020;18:2812–2822. doi: 10.1111/jth.15050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yan B, et al. SARS-CoV2 drives JAK1/2-dependent local and systemic complement hyper-activation. Res. Sq. 2020 doi: 10.21203/rs.3.rs-33390/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Conway EM. Reincarnation of ancient links between coagulation and complement. J. Thromb. Haemost. 2015;13:S121–S132. doi: 10.1111/jth.12950. [DOI] [PubMed] [Google Scholar]
- 81.Afzali B, Noris M, Lambrecht BN, Kemper C. The state of complement in COVID-19. Nat. Rev. Immunol. 2022;2:77–84. doi: 10.1038/s41577-021-00665-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schexneider KI, Reedy EA. Thrombocytopenia in dengue fever. Curr. Hematol. Rep. 2005;4:145–148. [PubMed] [Google Scholar]
- 83.Rondina MT, et al. In vivo platelet activation in critically ill patients with primary 2009 influenza A(H1N1) Chest. 2012;141:1490–1495. doi: 10.1378/chest.11-2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jansen AJG, et al. Influenza-induced thrombocytopenia is dependent on the subtype and sialoglycan receptor and increases with virus pathogenicity. Blood Adv. 2020;4:2967–2978. doi: 10.1182/bloodadvances.2020001640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang Y, et al. Mechanisms involved in the development of thrombocytopenia in patients with COVID-19. Thromb. Res. 2020;193:110–115. doi: 10.1016/j.thromres.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Caillon A, et al. Role of neutrophils, platelets, and extracellular vesicles and their interactions in COVID-19-associated thrombopathy. J. Thromb. Haemost. 2022;20:17–31. doi: 10.1111/jth.15566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Althaus K, et al. Antibody-induced procoagulant platelets in severe COVID-19 infection. Blood. 2021;137:1061–1071. doi: 10.1182/blood.2020008762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zaid Y, et al. Platelets can associate with SARS-Cov-2 RNA and are hyperactivated in COVID-19. Circ. Res. 2020 doi: 10.1161/CIRCRESAHA.120.317703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Manne BK, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136:1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Barrett TJ, et al. Platelets amplify endotheliopathy in COVID-19. Sci. Adv. 2021;7:eabh2434. doi: 10.1126/sciadv.abh2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Taus F, et al. Platelets promote thromboinflammation in SARS-CoV-2 pneumonia. Arterioscler. Thromb. Vasc. Biol. 2020;40:2975–2989. doi: 10.1161/ATVBAHA.120.315175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Leopold V, et al. Platelets are hyperactivated but show reduced glycoprotein VI reactivity in COVID-19 patients. Thromb. Haemost. 2021;121:1258–1262. doi: 10.1055/a-1347-5555. [DOI] [PubMed] [Google Scholar]
- 93.Yatim N, et al. Platelet activation in critically ill COVID-19 patients. Ann. Intensive Care. 2021;11:113. doi: 10.1186/s13613-021-00899-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hottz ED, et al. Platelet activation and platelet–monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136:1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Veras FP, et al. SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J. Exp. Med. 2020 doi: 10.1084/jem.20201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhao X, Zhou L, Kou Y, Kou J. Activated neutrophils in the initiation and progression of COVID-19: hyperinflammation and immunothrombosis in COVID-19. Am. J. Transl. Res. 2022;14:1454–1468. [PMC free article] [PubMed] [Google Scholar]
- 97.Barrett TJ, et al. Platelet and vascular biomarkers associate with thrombosis and death in coronavirus disease. Circ. Res. 2020;127:945–947. doi: 10.1161/CIRCRESAHA.120.317803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Davizon-Castillo P, et al. TNF-α-driven inflammation and mitochondrial dysfunction define the platelet hyperreactivity of aging. Blood. 2019;134:727–740. doi: 10.1182/blood.2019000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ezzaty Mirhashemi M, et al. The dynamic platelet transcriptome in obesity and weight loss. Arterioscler. Thromb. Vasc. Biol. 2021;41:854–864. doi: 10.1161/ATVBAHA.120.315186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Eicher JD, et al. Characterization of the platelet transcriptome by RNA sequencing in patients with acute myocardial infarction. Platelets. 2016;27:230–239. doi: 10.3109/09537104.2015.1083543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Barrett TJ, et al. Platelets contribute to disease severity in COVID-19. J. Thromb. Haemost. 2021;19:3139–3153. doi: 10.1111/jth.15534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koupenova M, et al. SARS-CoV-2 initiates programmed cell death in platelets. Circ. Res. 2021;129:631–646. doi: 10.1161/CIRCRESAHA.121.319117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Campbell RA, et al. Human megakaryocytes possess intrinsic antiviral immunity through regulated induction of IFITM3. Blood. 2019;133:2013–2026. doi: 10.1182/blood-2018-09-873984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Group RC. Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2022;399:143–151. doi: 10.1016/S0140-6736(21)01825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Berger JS, et al. Effect of P2Y12 inhibitors on survival free of organ support among non-critically ill hospitalized patients with COVID-19: a randomized clinical trial. JAMA. 2022;327:227–236. doi: 10.1001/jama.2021.23605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nougier C, et al. Hypofibrinolytic state and high thrombin generation may play a major role in SARS-COV2 associated thrombosis. J. Thromb. Haemost. 2020;18:2215–2219. doi: 10.1111/jth.15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Blasi A, et al. In vitro hypercoagulability and ongoing in vivo activation of coagulation and fibrinolysis in COVID-19 patients on anticoagulation. J. Thromb. Haemost. 2020;18:2646–2653. doi: 10.1111/jth.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ranucci M, et al. COVID-19-associated coagulopathy: biomarkers of thrombin generation and fibrinolysis leading the outcome. J. Clin. Med. 2020 doi: 10.3390/jcm9113487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.de la Morena-Barrio ME, et al. Prognostic value of thrombin generation parameters in hospitalized COVID-19 patients. Sci. Rep. 2021;11:7792. doi: 10.1038/s41598-021-85906-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mast AE, et al. SARS-CoV-2 suppresses anticoagulant and fibrinolytic gene expression in the lung. eLife. 2021 doi: 10.7554/eLife.64330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.FitzGerald ES, Chen Y, Fitzgerald KA, Jamieson AM. Lung epithelial cell transcriptional regulation as a factor in COVID-19-associated coagulopathies. Am. J. Respir. Cell Mol. Biol. 2021;64:687–697. doi: 10.1165/rcmb.2020-0453OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gralinski LE, et al. Mechanisms of severe acute respiratory syndrome coronavirus-induced acute lung injury. mBio. 2013 doi: 10.1128/mBio.00271-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zheng Z, et al. Interacting hepatic PAI-1/tPA gene regulatory pathways influence impaired fibrinolysis severity in obesity. J. Clin. Invest. 2020;130:4348–4359. doi: 10.1172/JCI135919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Griffin JH, Lyden P. COVID-19 hypothesis: activated protein C for therapy of virus-induced pathologic thromboinflammation. Res. Pract. Thromb. Haemost. 2020;4:506–509. doi: 10.1002/rth2.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Griffin JH, Zlokovic BV, Mosnier LO. Activated protein C, protease activated receptor 1, and neuroprotection. Blood. 2018;132:159–169. doi: 10.1182/blood-2018-02-769026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Stanne TM, Pedersen A, Gisslen M, Jern C. Low admission protein C levels are a risk factor for disease worsening and mortality in hospitalized patients with COVID-19. Thromb. Res. 2021;204:13–15. doi: 10.1016/j.thromres.2021.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jackson Chornenki NL, et al. Identification of hemostatic markers that define the pre-DIC state: a multi-center observational study. J. Thromb. Haemost. 2020;18:2524–2531. doi: 10.1111/jth.14973. [DOI] [PubMed] [Google Scholar]
- 118.Yan SB, Helterbrand JD, Hartman DL, Wright TJ, Bernard GR. Low levels of protein C are associated with poor outcome in severe sepsis. Chest. 2001;120:915–922. doi: 10.1378/chest.120.3.915. [DOI] [PubMed] [Google Scholar]
- 119.Folsom AR, Ohira T, Yamagishi K, Cushman M. Low protein C and incidence of ischemic stroke and coronary heart disease: the atherosclerosis risk in communities (ARIC) study. J. Thromb. Haemost. 2009;7:1774–1778. doi: 10.1111/j.1538-7836.2009.03577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tin A, et al. Association between circulating protein C levels and incident dementia: the atherosclerosis risk in communities study. Neuroepidemiology. 2021;55:306–315. doi: 10.1159/000516287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Juneja GK, et al. Biomarkers of coagulation, endothelial function, and fibrinolysis in critically ill patients with COVID-19: a single-center prospective longitudinal study. J. Thromb. Haemost. 2021;19:1546–1557. doi: 10.1111/jth.15327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Francischetti IMB, et al. Upregulation of pulmonary tissue factor, loss of thrombomodulin and immunothrombosis in SARS-CoV-2 infection. EClinicalMedicine. 2021;39:101069. doi: 10.1016/j.eclinm.2021.101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bayrakci N, et al. Relationship between serum soluble endothelial protein C receptor level and COVID-19 findings. Blood Coagul. Fibrinolysis. 2021;32:550–555. doi: 10.1097/MBC.0000000000001070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Knight JS, Kanthi Y. Mechanisms of immunothrombosis and vasculopathy in antiphospholipid syndrome. Semin. Immunopathol. 2022;44:347–362. doi: 10.1007/s00281-022-00916-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Stelzer M, Henes J, Saur S. The role of antiphospholipid antibodies in COVID-19. Curr. Rheumatol. Rep. 2021;23:72. doi: 10.1007/s11926-021-01041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Damoiseaux J, et al. Autoantibodies and SARS-CoV2 infection: the spectrum from association to clinical implication: report of the 15th Dresden Symposium on Autoantibodies. Autoimmun. Rev. 2022;21:103012. doi: 10.1016/j.autrev.2021.103012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zuo Y, et al. Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci. Transl. Med. 2020 doi: 10.1126/scitranslmed.abd3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hollerbach A, et al. Pathogenic lipid-binding antiphospholipid antibodies are associated with severity of COVID-19. J. Thromb. Haemost. 2021;19:2335–2347. doi: 10.1111/jth.15455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shi H, et al. Endothelial cell-activating antibodies in COVID-19. Arthritis Rheumatol. 2022 doi: 10.1002/art.42094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Munoz-Fontela C, et al. Animal models for COVID-19. Nature. 2020;586:509–515. doi: 10.1038/s41586-020-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dinnon KH, III, et al. A mouse-adapted model of SARS-CoV-2 to test COVID-19 countermeasures. Nature. 2020;586:560–566. doi: 10.1038/s41586-020-2708-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Muruato A, et al. Mouse-adapted SARS-CoV-2 protects animals from lethal SARS-CoV challenge. PLoS Biol. 2021;19:e3001284. doi: 10.1371/journal.pbio.3001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Leist SR, et al. A mouse-adapted SARS-CoV-2 induces acute lung injury and mortality in standard laboratory mice. Cell. 2020;183:1070–1085.e12. doi: 10.1016/j.cell.2020.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Huang K, et al. Q493K and Q498H substitutions in Spike promote adaptation of SARS-CoV-2 in mice. EBioMedicine. 2021;67:103381. doi: 10.1016/j.ebiom.2021.103381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Dinnon KH, et al. A model of persistent post SARS-CoV-2 induced lung disease for target identification and testing of therapeutic strategies. bioRxiv. 2022 doi: 10.1101/2022.02.15.480515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.McCray PB, Jr, et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J. Virol. 2007;81:813–821. doi: 10.1128/JVI.02012-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Winkler ES, et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat. Immunol. 2020;21:1327–1335. doi: 10.1038/s41590-020-0778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Vidal E, et al. Chronological brain lesions after SARS-CoV-2 infection in hACE2-transgenic mice. Vet. Pathol. 2021 doi: 10.1177/03009858211066841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sia SF, et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature. 2020;583:834–838. doi: 10.1038/s41586-020-2342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Imai M, et al. Syrian hamsters as a small animal model for SARS-CoV-2 infection and countermeasure development. Proc. Natl Acad. Sci. USA. 2020;117:16587–16595. doi: 10.1073/pnas.2009799117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Port JR, et al. High-fat high-sugar diet-induced changes in the lipid metabolism are associated with mildly increased COVID-19 severity and delayed recovery in the Syrian hamster. Viruses. 2021 doi: 10.3390/v13122506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Halfmann PJ, et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters. Nature. 2022;603:687–692. doi: 10.1038/s41586-022-04441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fan Y, et al. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal. Transduct. Target. Ther. 2022;7:141. doi: 10.1038/s41392-022-00997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cross RW, et al. Intranasal exposure of African green monkeys to SARS-CoV-2 results in acute phase pneumonia with shedding and lung injury still present in the early convalescence phase. Virol. J. 2020;17:125. doi: 10.1186/s12985-020-01396-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Clancy CS, et al. Histologic pulmonary lesions of SARS-CoV-2 in 4 nonhuman primate species: an institutional comparative review. Vet. Pathol. 2021 doi: 10.1177/03009858211067468. [DOI] [PubMed] [Google Scholar]
- 146.Woolsey C, et al. Establishment of an African green monkey model for COVID-19 and protection against re-infection. Nat. Immunol. 2021;22:86–98. doi: 10.1038/s41590-020-00835-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gomez CA, et al. Mortality and risk factors associated with pulmonary embolism in coronavirus disease 2019 patients: a systematic review and meta-analysis. Sci. Rep. 2021;11:16025. doi: 10.1038/s41598-021-95512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fogarty H, et al. Persistent endotheliopathy in the pathogenesis of long COVID syndrome. J. Thromb. Haemost. 2021;19:2546–2553. doi: 10.1111/jth.15490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pretorius E, et al. Persistent clotting protein pathology in long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021;20:172. doi: 10.1186/s12933-021-01359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rizk JG, et al. To anticoagulate or not to anticoagulate in COVID-19: lessons after 2 years. Semin. Thromb. Hemost. 2022 doi: 10.1055/s-0042-1744302. [DOI] [PubMed] [Google Scholar]
- 151.Alnima T, Mulder MMG, van Bussel BCT, Ten Cate H. COVID-19 coagulopathy: from pathogenesis to treatment. Acta Haematol. 2022 doi: 10.1159/000522498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Katsoularis I, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after COVID-19: nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377:e069590. doi: 10.1136/bmj-2021-069590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.van de Veerdonk FL, et al. A guide to immunotherapy for COVID-19. Nat. Med. 2022;28:39–50. doi: 10.1038/s41591-021-01643-9. [DOI] [PubMed] [Google Scholar]
- 154.American Society of Hematology. ASH guidelines on use of anticoagulation in patients with COVID-19. American Society of Hematologyhttps://www.hematology.org/education/clinicians/guidelines-and-quality-care/clinical-practice-guidelines/venous-thromboembolism-guidelines/ash-guidelines-on-use-of-anticoagulation-in-patients-with-covid-19 (2022).
- 155.COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Healthhttps://www.covid19treatmentguidelines.nih.gov/ (2022). [PubMed]
- 156.BC Centre for Disease Control. Antimicrobial and immunomodulatory therapy in adult patients with COVID-19. BC Centre for Disease Controlhttp://www.bccdc.ca/health-professionals/clinical-resources/covid-19-care/treatments (2022).
- 157.Thoms BL, Gosselin J, Libman B, Littenberg B, Budd RC. Efficacy of combination therapy with the JAK inhibitor baricitinib in the treatment of COVID-19. SN Compr. Clin. Med. 2022;4:42. doi: 10.1007/s42399-022-01121-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hafez W, et al. Treatment outcomes of tocilizumab in critically-ill COVID-19 patients, single-centre retrospective study. Antibiotics. 2022 doi: 10.3390/antibiotics11020241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Flumignan RL, et al. Anticoagulants for people hospitalised with COVID-19. Cochrane Database Syst. Rev. 2022;3:CD013739. doi: 10.1002/14651858.CD013739.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Vincent JL, Levi M, Hunt BJ. Prevention and management of thrombosis in hospitalised patients with COVID-19 pneumonia. Lancet Respir. Med. 2022;10:214–220. doi: 10.1016/S2213-2600(21)00455-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chow JH, et al. Association of early aspirin use with in-hospital mortality in patients with moderate COVID-19. JAMA Netw. Open. 2022;5:e223890. doi: 10.1001/jamanetworkopen.2022.3890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.REMAP-CAP Writing Committee for the REMAP-CAP Investigators. et al. Effect of antiplatelet therapy on survival and organ support-free days in critically ill patients with COVID-19: a randomized clinical trial. JAMA. 2022 doi: 10.1001/jama.2022.2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Barrett CD, et al. Study of alteplase for respiratory failure in SARS-CoV-2 COVID-19: a vanguard multicenter, rapidly adaptive, pragmatic, randomized controlled trial. Chest. 2022;161:710–727. doi: 10.1016/j.chest.2021.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.da Silva MF, et al. Bradykinin-target therapies in SARS-CoV-2 infection: current evidence and perspectives. Naunyn Schmiedebergs Arch. Pharmacol. 2022;395:275–283. doi: 10.1007/s00210-022-02206-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Declercq J, et al. Zilucoplan in patients with acute hypoxic respiratory failure due to COVID-19 (ZILU-COV): a structured summary of a study protocol for a randomised controlled trial. Trials. 2020;21:934. doi: 10.1186/s13063-020-04884-0. [DOI] [PMC free article] [PubMed] [Google Scholar]