Abstract
Background
Epilepsy is one of the most common neurological conditions worldwide. As a chronic condition, epilepsy imposes a significant burden on people with epilepsy and society. We aimed to assess the burden and unmet need of individuals with epilepsy and their caregivers, focusing on focal seizures, the main type of seizure in adults and children.
Methods
A targeted evidence review of the burden of epilepsy, focusing on focal seizures, was conducted to identify articles reporting: epidemiology, mortality, morbidity, quality of life (QoL), and costs.
Results
Focal seizures affect up to ∼61% of people with epilepsy. They are associated with an increased risk of injury and premature death than the general population. People with epilepsy also have high comorbidity, particularly depression, anxiety, and cognitive impairments. Higher seizure frequency, adverse treatment events, and employment concerns reduce QoL. A reduction in caregivers' QoL is also often reported. Epilepsy requires long‐term treatment accounting for high individual costs. Hospitalizations and antiseizure medications (ASMs) are the leading cost drivers of inpatient management and indirect costs with high unemployment rates, particularly in drug‐resistant populations. Despite the advent of new treatments, a high unmet need remains unaddressed; approximately 40% of people with epilepsy are drug‐resistant, further increasing the risks associated with epilepsy.
Conclusions
Our findings highlight a substantial burden of illness and unmet needs in individuals with focal seizures, especially those with drug‐resistant epilepsy. Suboptimal treatment options negatively impact QoL and, consequently, a sizeable economic burden indicating the need for new treatments and prioritizing this condition
Keywords: antiseizure medication, caregivers, costs, drug‐resistant epilepsy, quality of life
Seizure freedom is the ultimate goal for the treatment of focal epilepsy. A 30‐year study found that the probability of achieving seizure freedom decreases substantially with each additional antiseizure medication regimen attempted. If the first ASM is ineffective, the second ASM results in an 11.6% chance of seizure freedom, decreasing to 4.4% if a third drug is required. After this, only 2.1% achieved seizure control on subsequent ASM regimens.

1. INTRODUCTION
Epilepsy is one of the most common neurological conditions; it affects people of all ages, races, social classes, and geographical locations. Focal seizures (formerly known as partial seizures) constitute the most common seizure type, representing up to 61% of the epilepsy population (Gupta et al., 2017).
Over the last 20 years, several new antiseizure medications (ASMs) became available. Clinical practice guidelines incorporating these newer ASMs into treatment recommendations have been released. It is recommended that, where possible, people should be treated with a single medication (monotherapy) (NICE, 2012). A large proportion of people with epilepsy, however, are on adjunctive treatment as a second option to control seizures when monotherapy fails to do so. Approximately 40% of people with epilepsy may be drug‐resistant (DRE 1 ), deriving no benefit from two ASMs (Chen et al., 2018; Kwan & Brodie, 2000).
Due to its chronic nature, epilepsy imposes a significant burden on individuals and society. The extent of the burden is influenced by several factors, including seizure type and response to ASMs (Strzelczyk et al., 2008). According to the Global Burden of Epilepsy study 2019 (GBD 2019), idiopathic epilepsy and epilepsy due to other causes, altogether, resulted in 18.3 million (95% UI 12.3−24.8) global years lost due to disability (YLDs) in 2019 and were responsible for 2.1% (1.6−2.7) of total global YLDs (IHME, 2020).
DRE further increases the disease burden (Kwan et al., 2010); it is associated with increased premature mortality, increased morbidity, and lower quality of life (QoL) than controlled epilepsy (Laxer et al., 2014; Strzelczyk et al., 2017).
People with epilepsy need a holistic approach to take into account the global disease burden. To better delineate this global burden, we conducted a literature review to assess the epidemiological, clinical, humanistic, and economic burden and unmet need in individuals with epilepsy and their caregivers, focusing on focal seizures as these constitute the predominant seizure type in adults and children.
2. METHODS
A targeted literature review of the burden of illness associated with epilepsy, focusing on focal seizures, was carried out in February 2019 (updated in March 2021) to identify publications reporting information on the following review topics: epidemiological burden, clinical burden, humanistic burden, economic burden, and unmet needs.
2.1. Search strategy
The searches were targeted and aimed to identify the most relevant and up‐to‐date material available for inclusion in a narrative summary of each review topic. Searches were performed using electronic medical databases (i.e., Embase [OvidSP] and MEDLINE [OvidSP]). We also manually searched the bibliographies of critical systematic literature reviews for studies of interest. The Institute for Health Metrics and Evaluation (IHME) data collected through the GBD study were also considered.
These searches applied specific keywords relevant to the burden and unmet need for epilepsy and focal seizures. Broadly, the search included the following terms, among others:
Terms related to the condition, for example, “focal seizures,” “partial seizures,” “epilepsy,” “drug‐resistant epilepsy”;
Terms related to the main review topic, for example, “unmet need” and “burden”;
Terms related to outcomes of interest, for example, “prevalence,” “incidence,” “mortality,” “comorbidity,” “quality of life,” “caregiver burden,” “cost”
2.2. Study selection
The scope of this review was limited to literature published within the last 20 years (1999 to March 2021) and in English. Literature reporting global data was considered for inclusion in the narrative summary of each review topic, focusing on data for European countries.
Titles and abstracts of identified publications were reviewed for inclusion against the predefined criteria by one researcher. To check for potential error or bias, selected publications were reviewed by a second researcher; any differences were then resolved by consensus. Full‐text articles were then obtained and reviewed using the same process. Data of interest were extracted from included studies by one reviewer and verified by a second researcher. Extracted data included mortality and morbidity (clinical burden), QoL and caregiver burden (humanistic burden), and direct and indirect costs (economic burden) in people with epilepsy/focal seizures.
3. RESULTS AND DISCUSSION
A total of 104 publications were included in this review, of which 32 publications reported data regarding the epidemiological burden, 41 the clinical burden, 20 the humanistic burden, 17 the economic burden, and seven the unmet need of epilepsy/focal seizures.
3.1. Epidemiological burden
3.1.1. Incidence
Studies published between 1985 and 2013 estimated the annual cumulative epilepsy incidence 2 as 67.77 per 100,000 persons (95% confidence interval [CI] 56.69−81.03) with an incidence rate 3 of 61.44 per 100,000 person‐years (95% CI 50.75−74.38) (Fiest et al., 2017).
Epilepsy has an unequal distribution (Ngugi et al., 2010), with ∼80% of the affected individuals residing in low‐ and middle‐income countries (LMICs) (Espinosa‐Jovel et al., 2018). A meta‐analysis in 2017 indicated that the incidence rates in high‐income countries (HICs) and LMICs (Fiest et al., 2017) are:
HICs: 48.86 per 100,000 person‐years (95% CI 39.05−61.13)
LMICs: 138.99 per 100,000 person‐years (95% CI 69.45−278.16)
Differences in incidence rate estimates between LMICs and HICs are attributable to differences in standards in health delivery systems, demography, hygiene, sanitation, infection risks, and brain injury rates (De Boer et al., 2008; Ngugi et al., 2011). Further to these, in poor regions, especially in rural areas, ∼75% of people with epilepsy in these geographic areas do not receive treatment (Espinosa‐Jovel et al., 2018). Genetic factors may also play an important role; several African studies have identified familial clustering of epilepsy (Goudsmit & Van Der Waals, 1983; Jilek‐Aall et al., 1979; Neuman et al., 1995; Versteeg et al., 2003). Further studies have suggested a correlation between ion channel polymorphisms and seizure development, although it is unclear whether there are differences in these polymorphisms between people in LMICs and HICs (Anderson et al., 2002; Berkovic & Scheffer, 2001; Chioza et al., 2002; Sander, 2000; Wallace et al., 2002). Differences can also be due to methodological issues, such as more stringent case verification and the exclusion of isolated and acute symptomatic seizures in some studies (Beghi, 2019).
Several studies have shown that socioeconomic status is inversely associated with epilepsy incidence due to treatment gap, lower‐income level, poorer housing, occupation conditions, and lower education levels among more disadvantaged socioeconomic groups (Birbeck et al., 2007; Hesdorffer et al., 2005; Li et al., 2008; Noronha et al., 2007; Tang et al., 2015).
Epilepsy incidence has a bimodal age distribution with the highest risk in infants (genetic, metabolic, and obstetrical causes) and older people (higher risk for stroke and neurodegenerative diseases) (Camfield & Camfield, 2015; Fiest et al., 2017; Thijs et al., 2019). Based on the age‐specific incidence rates in European studies, the estimated number of new cases per year among European adults aged 20−64 is 960,000 (incidence rate 30 per 100,000) and 85,000 in the ≥ 65 years population (incidence 100 per 100,000) (Forsgren et al., 2005).
Focal seizures are more common than generalized seizures. The median focal seizure incidence rate is 30.4 per 100,000 per year, compared to 19.6 per 100,000 per year for generalized seizures (Kotsopoulos et al., 2002). The most common type of focal seizures are focal impaired awareness seizures, accounting for approximately a third of all cases (Banerjee et al., 2009; WHO, 2019).
3.1.2. Prevalence
It is estimated that epilepsy affects around 52.5 million people of all ages worldwide (IHME, 2020). Its prevalence differs significantly among countries depending on the local distribution of risk and etiologic factors, the number of seizures at diagnosis, and if considering only active epilepsy (active prevalence) or including also cases in remission (lifetime prevalence) (Beghi, 2019). In selected populations, prevalence estimates also vary and tend to be higher in individuals of certain ethnicities (Kelvin et al., 2007), older individuals with lower socioeconomic status (Tang et al., 2015), and people in poor health or socially deprived (Kaiboriboon et al., 2013).
3.1.3. Active prevalence
Based on the International League Against Epilepsy (ILAE) definition, active epilepsy is defined as having one or more unprovoked seizures in the last 5 years or having been on ASMs in the previous 5 years (Fisher et al., 2014).
The systematic review and meta‐analysis of international studies discussed earlier found that the point prevalence 4 of active epilepsy was 6.38 per 1000 persons (95% CI 5.57−7.30). The lifetime prevalence was 7.60 per 1000 persons (95% CI 6.17−9.38) (Fiest et al., 2017). Lifetime prevalence was higher for LMICs (8.75 (95% CI 7.23−10.59) per 1000) compared to HICs (5.18 (95% CI 3.75−7.15) per 1000) (Fiest et al., 2017).
Table 1 shows the estimated active diagnosed prevalent cases of epilepsy in men and women of all ages combined between 2016 and 2026 in selected countries (GlobalData, 2017). France is expected to see the most significant annual increase in cases (4.28%), followed by Spain (0.92%), the US (0.84%), and the UK (0.62%). Changes in the active diagnosed prevalent cases of epilepsy in Germany, Italy, Spain, the US, the UK, and Japan are attributable to changing population demographics. Changes in France are attributable to changes in the prevalence rates of epilepsy and underlying population dynamics such as ageing and population growth (GlobalData, 2017).
TABLE 1.
Active diagnosed prevalent cases of epilepsy in France, Germany, Italy, Spain, UK, Japan, and the US, select years 2016−2026 (GlobalData, 2017)
| Country | 2016 | 2018 | 2020 | 2022 | 2024 | 2026 | Annual rise in cases (%) |
|---|---|---|---|---|---|---|---|
| France | 137,218 | 153,831 | 170,555 | 187,253 | 195,707 | 195,983 | 4.28 |
| Germany | 819,882 | 819,596 | 818,990 | 818,012 | 816,792 | 815,669 | −0.05 |
| Italy | 288,554 | 290,081 | 291,083 | 292,243 | 293,415 | 294,184 | 0.20 |
| Spain | 201,299 | 205,441 | 209,822 | 213,679 | 216,948 | 219,857 | 0.92 |
| UK | 628,654 | 636,444 | 644,267 | 652,270 | 660,132 | 667,488 | 0.62 |
| Japan | 319,772 | 315,229 | 310,875 | 306,118 | 300,707 | 295,270 | −0.77 |
| US | 3,265,796 | 3,327,885 | 3,385,404 | 3,436,165 | 3,486,103 | 3,539,355 | 0.84 |
There is limited data estimating the active prevalence of epilepsy by seizure type. Based on a GlobalData analysis, there were approximately 3.5 million prevalent cases with active focal seizures in 2016 in these countries—see Table 1 (GlobalData, 2017). The greatest percentage of focal seizures was 76.2%, 72.9%, and 72.9% in Italy, Germany, and Spain. The UK had the lowest proportion (52%). Across all countries, focal seizures were the most predominant among prevalent cases (GlobalData, 2017).
Seizure type distribution was obtained from various sources using different data collection methodologies. For France, specifically, seizure type and distribution for prevalent cases was obtained from a regional epilepsy study conducted in Beziers (Beghi & Giussani, 2018). The prevalence of focal epilepsy was 3.70 per 1000, accounting for 61% of epilepsy (Beghi & Giussani, 2018). According to GlobalData figures, the number of focal cases could be underestimated (Dantoine, 2016).
Overall, estimates in 2016 for France, Germany, Italy, Spain, and the UK show that two‐thirds of people with epilepsy had focal seizures, equating to over 1.3 million people (Beghi & Giussani, 2018). GlobalData estimates for 2021 suggest that two‐thirds will experience focal seizures, highlighting the need for improved treatment for focal seizures.
3.2. Clinical burden
3.2.1. Mortality
Adults with epilepsy have an increased risk of injury and premature death as compared to the general population (Bowman et al., 2010; Ding et al., 2013; Ficker, 2000; Ridsdale et al., 2011). The standardized mortality ratio in LMICs (19.8 [95% CI 9.7−45.1]) (Levira et al., 2017) is higher than that in HICs (1.6 to 3.0) (Thurman et al., 2017). The 2019 GBD study estimated 114,011 deaths (rate of 1.47 per 100,000) attributable to idiopathic epilepsy 5 globally, with the highest rates of mortality in Africa (rate of 1.95 per 100,000), as depicted in Table 2 (GHDx, 2019). The standardized mortality ratio is slightly higher in adult men than in women and in children and adolescents. It is also higher for people with etiologically confirmed epilepsy and in those reporting less adherence to treatment (Beghi, 2019).
TABLE 2.
Global Burden of Disease (GBD) study 2019 data on mortality due to idiopathic epilepsy according to WHO region (GHDx, 2019)
| Mortality, 2019 | ||
|---|---|---|
| WHO region | Counts | Rate (per 100,000) |
| Global | 114,011 | 1.47 (1.29−1.68) |
| African | 21,460 | 1.95 (1.61−2.50) |
| Eastern Mediterranean | 9311 | 1.28 (0.93−1.62) |
| European | 16,800 | 1.80 (1.54−1.93) |
| The Americas | 12,364 | 1.22 (1.13−1.35) |
| South‐East Asia | 38,242 | 1.90 (1.58−2.24) |
| Western Pacific | 15,594 | 0.81 (0.70−0.93) |
Uncontrolled focal seizures, in particular, are associated with premature mortality; people who continue to suffer seizures appear to have an almost 40 times higher risk of mortality than those in remission (Lhatoo & Sander, 2005). An Austrian study found that the standardized mortality ratio for those not seizure free was 3.3 (95% CI 2.6−4.4) compared to 1.4 (95% CI 0.8−2.3) for those seizure free 2 years after diagnosis (Trinka et al., 2013). Brain surgery can reduce the mortality rate in DRE when seizures are abolished and when it results in significant palliation of tonic‐clonic seizure frequency (Sperling et al., 2016).
Sudden unexpected death in epilepsy (SUDEP) (i.e., sudden and unexpected death of a person with epilepsy without an anatomical or toxicological cause of death after an autopsy and not linked to drowning or status epilepticus [Whitney & Donner, 2019]) is the most critical epilepsy‐related mode of death, particularly in those with chronic epilepsy (Tomson et al., 2008). SUDEP affects approximately 1 in 1000 people with epilepsy annually (Thurman et al., 2017). People with epilepsy are at a 27‐fold higher risk of sudden death than controls, but this falls to a 16‐fold risk when adjusted for sex, comorbidities, and the Charlson comorbidity score (Holst et al., 2013).
Studies also show that SUDEP incidence increases with the severity of epilepsy, with variation in incidence across different epilepsy populations (Figure 1) (Devinsky et al., 2016). Studies suggest that the incidence ranges from 0.09 per 1000 patient‐years in people with newly diagnosed epilepsy to 9 per 1000 patient‐years in candidates for epilepsy surgery (Tomson et al., 2008). Clinic‐based studies report an estimate of SUDEP in people with drug‐resistant focal epilepsy of up to 6.3 per 1000 people (Thurman et al., 2017).
FIGURE 1.
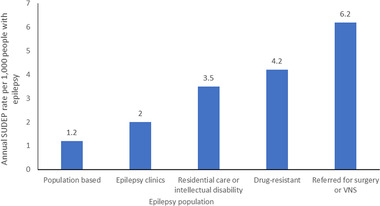
Estimated annual SUDEP incidence in different epilepsy populations (Devinsky et al., 2016)
In 2011, a combined analysis of four case–control studies to identify SUDEP risk factors was published. Factors associated with a statistically significant SUDEP risk were: a high number of generalized tonic‐clonic seizures (GTCS), epilepsy lasting more than 15 years, young age at onset, symptomatic epilepsy, and male gender. The primary risk factor for SUDEP is the presence and frequency of GTCS. The frequency of GTCS affects the risk significantly, with an odds ratio over three times higher in those with more than three yearly GTCS than those with one to two per year. People with three or more GTCS per year have a 15‐fold increased SUDEP risk (Table 3) (Harden et al., 2017; Whitney & Donner, 2019). Not being seizure‐free for 1 to 5 years carries a significant SUDEP risk. Seizure freedom, in turn, is associated with marked reductions in SUDEP risk, emphasizing the importance of seizure freedom (Harden et al., 2017).
TABLE 3.
SUDEP risk factors using evidence from a systematic review (Harden et al., 2017)
| Factor | Odds ratio of SUDEP (CI) | Confidence level |
|---|---|---|
| Convulsion vs. none | 10 (17−14) | Moderate |
| Frequency of GTCS | • OR 5.07 (2.94−8.76) for 1−2 GTCS per year | |
| • OR 15.46 (9.92−24.10) > 3 GTCS per year | High | |
| Not being seizure‐free for 1−5 years | 4.7 (1.4−16) | Moderate |
Abbreviations: CI, confidence interval; GTCS, generalized tonic‐clonic seizures; OR, odds ratio; SUDEP, sudden unexpected death in epilepsy.
Other important causes of mortality in epilepsy include unintentional injuries (Chen et al., 2013; Manjunath et al., 2012; Marson et al., 2007) and suicide (Bell et al., 2009). An observational study of people with epilepsy and convulsive seizures found that ∼60% of the population experienced at least one accidental injury associated with convulsions over 12 months; common injuries in this population included head injuries (35.5%), dental injuries (4.9%), and burns (4.9%) (Salas‐Puig et al., 2019). The risk of drowning is also higher in people with epilepsy, with an estimated relative risk ranging from 13‐ to 19‐fold (Bell et al., 2008; Day et al., 2005).
3.2.2. Comorbidities
Conditions comorbid in epilepsy are associated with a range of body organ systems (Seidenberg et al., 2009). Approximately 50% of adults with active epilepsy have one or more comorbid conditions, with several conditions, such as depression, anxiety, dementia, migraine, heart disease, peptic ulcers, and arthritis being eight times more common in people with epilepsy compared to the general population (Keezer et al., 2016).
Psychiatric comorbidities are the most prevalent comorbidities in epilepsy with a reported prevalence of 29−40%, which is 7‐ to 10‐fold higher than mental health conditions in the general population (GBD, 2017). Epilepsy is associated with an increased onset of psychiatric disorders before and after epilepsy diagnosis, and there is a two‐way relationship between epilepsy and suicidality (Hesdorffer et al., 2012).
The most prevalent psychiatric comorbidities are depression (23.1%) and anxiety (20.2%) (Fiest et al., 2013; Scott et al., 2017), as compared with 4.4% and 3.6% in the general population globally (WHO, 2020). People with epilepsy may also present with alcohol abuse (8.7%), drug abuse (7.8%), and interictal psychosis (5.2%) (Clancy et al., 2014; Patel et al., 2017; Verrotti et al., 2014). Attempted and completed suicides are estimated to occur in 5−14.3% of people with epilepsy (Pompili et al., 2006), and the suicide‐specific standardized mortality ratio among those with epilepsy is estimated to be 3.3 (95% CI: 2.8−3.7) (Bell et al., 2009). Additionally, some ASMs have been shown to induce depressive symptoms, while others are associated with mood stabilizing properties and, in such cases, discontinuation may lead to depression (Schmidt & Schachter, 2014).
Among people with intellectual disability, approximately one in five will also have epilepsy, with prevalence increasing with increasing severity of the intellectual disability (Robertson et al., 2015). Epilepsy in adults with intellectual disability has a worse prognosis than epilepsy in the general population, with lower seizure freedom rates and higher premature mortality, including SUDEP (Wagner et al., 2017). Aside from severe learning disabilities, epilepsy can impact learning through memory impairment. Seizures can reduce alertness and interfere with short‐term information storage. Frequent uncontrolled or night‐time seizures can impair new information learning, disrupt memory consolidation, and affect language function (De Boer et al., 2008).
Cognitive impairments, such as learning difficulties, behavior change, and memory impairment, can be induced or exacerbated by ASMs, particularly those with impaired cognition, depending on dose and individual susceptibility (De Boer et al., 2008; Witt & Helmstaedter, 2013).
In addition to these cognitive impairments, drug‐resistant focal seizures are associated with structural brain changes that resemble premature brain ageing. A study found that people with DRE presented a difference between predicted brain age and chronological age that was on average 4.5 years older than healthy controls (p = 4.6 × 10−5). Earlier onset was associated with an increased brain age difference in the drug‐resistant group (p = .034) (Pardoe et al., 2017). DRE is related to cognitive decline, and this phenomenon has been conceptualized as accelerated cognitive ageing (Breuer et al., 2016).
3.3. Humanistic burden
3.3.1. Quality of life
People with epilepsy have a lower QoL than the general population (Gholami et al., 2016). Some risk factors for reduced QoL have been identified, including frequent seizures, longer seizure duration, convulsions, and earlier age of onset (Baker et al., 1997; Jacoby & Baker, 2008; Kerr et al., 2011; Wheless, 2006). The presence of somatic comorbidity further negatively impacts QoL (Gaitatzis et al., 2012). Other factors affecting QoL include ASM side effects, depression or anxiety, lack of social support, stigma, and employment concerns (Aydemir et al., 2011; Baker et al., 2005; Hovinga et al., 2008; Taylor et al., 2011). Adults with epilepsy are likely to report more mentally and physically unhealthy days per month than those without epilepsy, with the highest rates in those with seizures in the past 3 months (Kobau et al., 2007; Kobau et al., 2008; Wiebe et al., 1999).
People seizure‐free for more than 1 year have a significantly higher preference‐based HRQoL than those in any other seizure frequency group. Further differentiation of QoL at higher response levels has been reported, with people achieving high response rates (particularly ≥90%) exhibiting higher QoL than people with ≤50% response rates (Elizebath et al., 2021). This suggests that for a significant QoL improvement, seizure freedom must be attained and maintained (Choi et al., 2014). A Thai study indicated that people with seizure freedom reported significantly higher utility scores than those with no seizure reduction (Figure 2). This is further supported by a study in people with a lower QoL, including EuroQol‐5 Dimension (EQ‐5D) and Quality of Life in Epilepsy Inventory‐31 (QOLIE‐31) mean scores, compared to those who are drug responsive (Figure 3) (Villanueva et al., 2013). Another study suggested that depression (assessed using the Montgomery‐Asberg Depression Rating Scale [MADRS] and the Beck Depression Inventory‐II [BDI‐II]), in people with drug‐resistant focal seizures further decreases QOLIE‐31 scores (Garcia et al., 2015).
FIGURE 2.
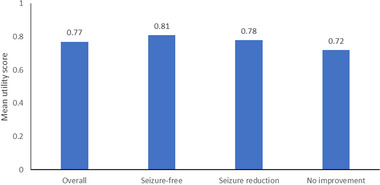
Mean utility scores of 224 individuals with focal seizures (Villanueva et al., 2013)
FIGURE 3.
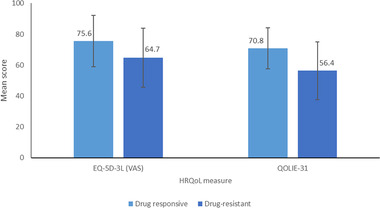
Mean EQ‐5D‐3L (VAS) and QOLIE‐31 scores in drug‐responsive versus drug‐resistant focal seizures (Villanueva et al., 2013)
3.3.2. Caregiver burden
Few studies investigating caregiver burden in epilepsy are available, with most studies focusing on the pediatric population. In a 2014 study in which 92% of people had focal seizures, a higher caregiver burden was associated with the individuals taking a higher number of ASMs, lower neuropsychological performance, lower QoL score, and lower caregiver education level. On average, 11.4 (±21.2) h were spent on care per week, with the majority (58.3%) of caregivers being a spouse/partner (Lai et al., 2019).
Another study found that unemployed adults with epilepsy who had early‐onset or had frequent seizures with mental comorbidities significantly impacted their burden. Inadequate family support and a negative attitude towards epilepsy affected the perceived burden. Caregivers of adults with epilepsy experience extreme psychological distress and poor QoL (Lai et al., 2019).
A recent study reported the online STEP survey (Seize the Truth of Epilepsy Perceptions) designed to examine how adults with epilepsy, caregivers, and healthcare professionals perceive epilepsy‐related fears (Stern et al., 2020). The results suggest that 72% of caregivers strongly agree that they fear another seizure, irrespective of when the last episode was. The highest percentage of caregivers reported being extremely afraid of their loved one having a seizure while driving, alone, or asleep. Lastly, about half of caregivers said that the worry of a loved one having a seizure, while they were not present is disruptive to their QoL. Knowledge of these fears and burden to QoL provides an opportunity to provide broader care and potentially reduce the impact of fear on treatment decisions (Stern et al., 2020).
3.4. Economic burden
Epilepsy is a chronic condition requiring long‐term treatment; thus, it is a significant economic burden to individuals and society (Allers et al., 2015; Kotsopoulos et al., 2001; Strzelczyk et al., 2008). It imposes high direct costs, including healthcare costs (medicines, diagnostic investigations, surgery, and hospitalization) and non‐medical services such as social support, health education, and transportation. It also creates indirect costs due to comorbidities, disabling side effects, and premature mortality. It prevents people from reaching their full potential in school, employment, or household activities. Costs vary according to the severity of the condition, treatment response, length of time since diagnosis and associated comorbidities (WHO, 2019).
3.4.1. Direct costs
The cost of epilepsy depends on seizure severity, frequency, and drug refractoriness (20% to 40% of people with drug‐refractory epilepsy account for 80% of the costs). The main cost drivers are hospitalizations and ASM costs (De Kinderen et al., 2014; Vrouchou et al., 2015).
DRE incurs significantly higher resource utilization and costs than controlled epilepsy (Cramer et al., 2014; Strzelczyk et al., 2017; Villanueva et al., 2013). A German study demonstrated that in people with severe DRE (i.e., prescribed at least four different ASMs in 18 months) epilepsy‐related admissions ranged between 1.7 and 1.9 per year, with an average duration for each epilepsy‐caused hospitalization of 10−11.1 days (Strzelczyk et al., 2017). In accordance, a US‐based study estimated the odds of epilepsy‐related hospitalization (OR: 2.2) and epilepsy‐related emergency department visits (OR: 1.9) to be more significant for people with uncontrolled epilepsy; epilepsy‐related costs were found to be ∼$6890/case/year higher for DRE (Cramer et al., 2014).
Little work has focused on the economic burden of focal seizures. The mean annual direct epilepsy‐related costs in 2010 were estimated in France to be €3850 per case per year (De Zelicourt et al., 2014) and €4505 (Villanueva et al., 2013) per case per year in Spain. ASMs are the main cost drivers accounting for 60% and 67% of total costs in France and Spain, followed by hospitalizations (26% and 21%). People with DRE incur significantly higher costs than controlled epilepsy in both countries (€4485 vs. €1926 per case per year in France [De Zelicourt et al., 2014] and €4964 vs. €2978 per case per year in Spain [Villanueva et al., 2013]). An Italian study found that the direct medical costs associated with DRE were average €4677 per individual, a mid‐part figure seen in previous studies in comparable populations (Luoni et al., 2015).
Despite the use of ASMs, uncontrolled seizures may harm health and well‐being. People may injure themselves during a seizure resulting in fractures, head injury, sprains, and open wounds (Chen et al., 2013; Manjunath et al., 2012). A German study of the costs associated with ictal falls, and “situationally inappropriate, complex behavior” such as automatisms, both regarded as a high risk for injuries, had interesting findings. These two factors were found to contribute to epilepsy‐related costs significantly. The mean cost of a fall was €1300 (±€1820) and of “complex behavior” was €1760 (±€2630) (Hamer et al., 2006). Another US study found that hospitalization and pharmacy costs in people with focal seizures were twice as high in the refractory cohort versus the nonrefractory cohort. This was mainly due to the higher prevalence of injuries, including fractures, sprains and strains, and wounds (Chen et al., 2013).
3.4.2. Indirect costs
Productivity loss and unemployment among people with epilepsy are the primary sources of the individual and societal burden (Allers et al., 2015). Among people with drug‐resistant focal seizures in Europe, high unemployment rates have been shown compared to a matched control population (46% vs. 19%) (Vrouchou et al., 2015). A recent review of epilepsy's economic impact found that very few studies provided reasonable estimates of indirect costs to make robust conclusions about their relative societal burden (Allers et al., 2015).
Another factor to consider in the indirect costs is the costs and productivity loss of the caregivers. A 2018 study found that caregivers of people on monotherapy had an average of 2.7 days of work lost annually due to sick leave and short‐term disability. In contrast, the caregivers to those on adjunctive therapy had an average of 5.1 days of work lost annually due to the same reasons (Brook et al., 2018). Sick leave in caregivers of those on monotherapy was associated with average costs of $582; whereas, in the adjunctive therapy caregivers group, this increased to $1123. A Spanish study also reported that the mean cost of paid caregivers per case and year increased by ∼€95 in those who were drug resistant rather than drug responsive (Villanueva et al., 2013).
4. UNMET NEED
Seizure freedom is the ultimate goal of treatment. The use of newer ASMs with reported similar or improved efficacy and better tolerability than older ASMs would be expected to benefit overall epilepsy treatment success and individual outcomes. There has been, however, no meaningful improvement in epilepsy treatment‐related outcomes and no significant reduction of DRE frequency in the past 20 years. Most people who achieve complete seizure control do so with the first or second ASM (Chen et al., 2018). A 30‐year study found that the probability of achieving seizure freedom decreases substantially with each additional ASM regimen attempted (Chen et al., 2018). If the first ASM is ineffective, the second ASM results in an 11.6% chance of seizure freedom, decreasing to 4.4% if a third drug is required. After this, only 2.1% achieved seizure control on subsequent ASM regimens (Chen et al., 2018) (Figure 4).
FIGURE 4.
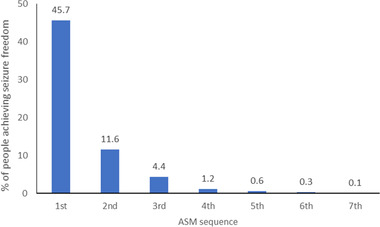
The percentage of people achieving seizure freedom with each ASM sequence attempted (Chen et al., 2018)
New therapies with fewer adverse events and interactions are critical for unmet medical needs (Younus & Reddy, 2018). Commonly occurring side effects of ASMs are memory problems, fatigue, tremors, gastrointestinal symptoms, osteoporosis, depression, drowsiness, dizziness, weight change, and nausea (Carpay et al., 2005). People exposed to multiple ASM regimens are at a higher risk of experiencing adverse events due to drug load (Beghi, 2016). In up to a quarter of people, tolerability issues may lead to treatment discontinuation, as well as harming adherence (Kwan & Brodie, 2000; Perucca et al., 2009). Adverse events increase the burden of the disease from a humanistic and an economic perspective (De Kinderen et al., 2014).
Treating people with epilepsy with ASMs characterized by improved tolerability and high efficacy, while improving QoL and reducing comorbidities, remain the ultimate unmet medical need to address the burden.
5. CONCLUSIONS
Current evidence on the burden of focal seizures on individuals, caregivers, and society is limited. Focal seizures are associated with premature death, high comorbidity, and seizure‐related injuries. Adults with drug‐resistant focal seizures incur higher direct (hospitalizations, outpatient visits, and pharmacy costs) and indirect (caregiver costs and unemployment rates) costs than those seizure‐free.
Reducing seizure frequency can improve QoL in people with epilepsy and minimize resource utilization and associated direct and indirect costs, thus reducing the burden of epilepsy. Existing treatments are often not sufficient to achieve treatment goals, with many people poorly responding to treatment or experiencing adverse events, if not both. People with epilepsy are frequently treated with polypharmacotherapy, which further increases the risk of drug to drug interactions and, thus, adverse events. High drug loads do not leave many options for further drug escalation when the condition worsens.
New therapies and prioritization are needed to address this pressing public health concern.
CONFLICT OF INTERESTS
SK Pharmaceuticals is the licensor of cenobamate. Persefoni Ioannou and Daniella L. Foster are full‐time employees at PHMR. PHMR received financial support from Arvelle Therapeutics for the work, including developing the review and drafting of the manuscript. Elena Alvarez‐Baron, Ewa Drogon O'Flaherty, and Jasmina Medjedovic are full‐time employees of Arvelle Therapeutics. Josemir W. Sander reports fees as speaker or consultant from Eisai, UCB, GW Pharma, Arvelle, and Zogenix. Other authors report no conflicts of interest concerning this work.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/brb3.2589.
ACKNOWLEDGMENT
This study was sponsored by Arvelle Therapeutics.
Ioannou, P. , Foster, D. L. , Sander, J. W. , Dupont, S. , Gil‐Nagel, A. , Drogon O'Flaherty, E. , Alvarez‐Baron, E. , & Medjedovic, J. (2022). The burden of epilepsy and unmet need in people with focal seizures. Brain and Behavior, 12, e2589. 10.1002/brb3.2589
NOTES
Drug‐resistant epilepsy (DRE) can be defined as failure of adequate trials of two tolerated, appropriately chosen and used ASM schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom.
Cumulative incidence is the number of new cases of epilepsy over the total number of people in the population at risk for developing epilepsy during a specified period of time.
The incidence rate of epilepsy is the number of new cases of epilepsy over the total amount of person‐time at risk for developing epilepsy during a specified period of time.
Point prevalence is the number of existing cases of epilepsy in a population, over the total population at one specific point in time (e.g., on June 30, 2013).
Includes idiopathic epilepsy and epilepsy secondary to known infectious and neonatal causes. Case definition in GBD study includes cases of active epilepsy with at least one seizure in the previous 5 years, regardless of treatment.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- Allers, K. , Essue, B. M. , Hackett, M. L. , Muhunthan, J. , Anderson, C. S. , Pickles, K. , Scheibe, F. , & Jan, S. (2015). The economic impact of epilepsy: A systematic review. BMC Neurology [Electronic Resource], 15, 245–245. 10.1186/s12883-015-0494-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, E. , Berkovic, S. , Dulac, O. , Gardiner, M. , Jain, S. , Friis, M. L. , Lindhout, D. , Noebels, J. , Ottman, R. , Scaramelli, A. , Serratosa, J. , Steinlein, O. , Avanzini, G. , Bailey‐Wilson, J. , Cardon, L. , Fischbach, R. , Gwinn‐Hardy, K. , Leppert, M. , Ott, J. , … Weiss, K. , & ILAE Genetics Commission . (2002). ILAE genetics commission conference report: Molecular analysis of complex genetic epilepsies. Epilepsia, 10, 1262–1267. [DOI] [PubMed] [Google Scholar]
- Aydemir, N. , Özkara, Ç. , Ünsal, P. , & Canbeyli, R. (2011). A comparative study of health related quality of life, psychological well‐being, impact of illness and stigma in epilepsy and migraine. Seizure: The Journal of the British Epilepsy Association, 20(9), 679–685. 10.1016/j.seizure.2011.06.017 [DOI] [PubMed] [Google Scholar]
- Baker, G. A. , Jacoby, A. , Buck, D. , Stalgis, C. , & Monnet, D. (1997). Quality of life of people with epilepsy: A European study. Epilepsia, 38(3), 353–362. 10.1111/j.1528-1157.1997.tb01128.x [DOI] [PubMed] [Google Scholar]
- Baker, G. A. , Jacoby, A. , Gorry, J. , Doughty, J. , & Ellina, V. (2005). Quality of life of people with epilepsy in Iran, the Gulf, and Near East. Epilepsia, 46(1), 132–140. 10.1111/j.0013-9580.2005.20704.x [DOI] [PubMed] [Google Scholar]
- Banerjee, P. N. , Filippi, D. , & Allen Hauser, W. (2009). The descriptive epidemiology of epilepsy—A review. Epilepsy Research, 85, 31–41. 10.1016/j.eplepsyres.2009.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beghi, E. (2016). Addressing the burden of epilepsy: Many unmet needs. Pharmacological Research, 107, 79–84. 10.1016/j.phrs.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Beghi, E. (2019). The epidemiology of epilepsy. Neuroepidemiology, 54, 185–191. 10.1159/000503831 [DOI] [PubMed] [Google Scholar]
- Beghi, E. , & Giussani, G. (2018). Aging and the epidemiology of epilepsy. Neuroepidemiology, 51(3–4), 216–223. 10.1159/000493484 [DOI] [PubMed] [Google Scholar]
- Bell, G. S. , Gaitatzis, A. , Bell, C. L. , Johnson, A. L. , & Sander, J. W. (2008). Drowning in people with epilepsy: How great is the risk? Neurology, 71(8), 578–582. 10.1212/01.wnl.0000323813.36193.4d [DOI] [PubMed] [Google Scholar]
- Bell, G. S. , Gaitatzis, A. , Bell, C. L. , Johnson, A. L. , & Sander, J. W. (2009). Suicide in people with epilepsy: How great is the risk? Epilepsia, 50(8), 1933–1942. 10.1111/j.1528-1167.2009.02106.x [DOI] [PubMed] [Google Scholar]
- Berkovic, S. F. , & Scheffer, I. E. (2001). Genetics of the epilepsies. Epilepsia, 42, (Suppl 5), 16–23. 10.1046/j.1528-1157.2001.0420s5016.x [DOI] [PubMed] [Google Scholar]
- Birbeck, G. , Chomba, E. , Atadzhanov, M. , Mbewe, E. , & Haworth, A. (2007). The social and economic impact of epilepsy in Zambia: A cross‐sectional study. Lancet Neurology, 6(1), 39–44. 10.1016/s1474-4422(06)70629-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowman, S. M. , Aitken, M. E. , & Sharp, G. B. (2010). Disparities in hospital outcomes for injured people with epilepsy/seizures. Epilepsia, 51(5), 862–867. 10.1111/j.1528-1167.2009.02492.x [DOI] [PubMed] [Google Scholar]
- Breuer, L. E. M. , Boon, P. , Bergmans, J. W. M. , Mess, W. H. , Besseling, R. M. H. , De Louw, A. , Tijhuis, A. G. , Zinger, S. , Bernas, A. , Klooster, D. C. W. , & Aldenkamp, A. P. (2016). Cognitive deterioration in adult epilepsy: Does accelerated cognitive ageing exist? Neuroscience and Biobehavioral Reviews, 64, 1–11. 10.1016/j.neubiorev.2016.02.004 [DOI] [PubMed] [Google Scholar]
- Brook, R. A. , Rajagopalan, K. , & Smeeding, J. E. (2018). Healthcare costs and absenteeism among caregivers of adults with partial‐onset seizures: Analysis of claims from an employer database. American Health & Drug Benefits, 11(8), 396–403. [PMC free article] [PubMed] [Google Scholar]
- Camfield, P. , & Camfield, C. (2015). Incidence, prevalence and aetiology of seizures and epilepsy in children. Epileptic Disorders, 17(2), 117–123. 10.1684/epd.2015.0736 [DOI] [PubMed] [Google Scholar]
- Carpay, J. A. , Aldenkamp, A. P. , & Van Donselaar, C. A. (2005). Complaints associated with the use of antiepileptic drugs: Results from a community‐based study. Seizure: The Journal of the British Epilepsy Association, 14(3), 198–206. 10.1016/j.seizure.2005.01.008 [DOI] [PubMed] [Google Scholar]
- Chen, S.‐Y. , Wu, N. , Boulanger, L. , & Sacco, P. (2013). Antiepileptic drug treatment patterns and economic burden of commercially‐insured patients with refractory epilepsy with partial onset seizures in the United States. Journal of Medical Economics, 16(2), 240–248. 10.3111/13696998.2012.751918 [DOI] [PubMed] [Google Scholar]
- Chen, Z. , Brodie, M. J. , Liew, D. , & Kwan, P. (2018). Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: A 30‐year longitudinal cohort study. JAMA Neurology, 75(3), 279–286. 10.1001/jamaneurol.2017.3949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chioza, B. , Osei‐Lah, A. , Nashef, L. , Suarez‐Merino, B. , Wilkie, H. , Sham, P. , Knight, J. , Asherson, P. , & Makoff, A. J. (2002). Haplotype and linkage disequilibrium analysis to characterise a region in the calcium channel gene CACNA1A associated with idiopathic generalised epilepsy. European Journal of Human Genetics, 10(12), 857–864. 10.1038/sj.ejhg.5200896 [DOI] [PubMed] [Google Scholar]
- Choi, H. , Hamberger, M. J. , Munger Clary, H. , Loeb, R. , Onchiri, F. M. , Baker, G. , Hauser, W. A. , & Wong, J. B. (2014). Seizure frequency and patient‐centered outcome assessment in epilepsy. Epilepsia, 55(8), 1205–1212. 10.1111/epi.12672 [DOI] [PubMed] [Google Scholar]
- Clancy, M. J. , Clarke, M. C. , Connor, D. J. , Cannon, M. , & Cotter, D. R. (2014). The prevalence of psychosis in epilepsy; a systematic review and meta‐analysis. Bmc Psychiatry [Electronic Resource], 14, 75. 10.1186/1471-244x-14-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer, J. A. , Wang, Z. J. , Chang, E. , Powers, A. , Copher, R. , Cherepanov, D. , & Broder, M. S. (2014). Healthcare utilisation and costs in adults with stable and uncontrolled epilepsy. Epilepsy & Behavior, 31, 356–362. 10.1016/j.yebeh.2013.09.046 [DOI] [PubMed] [Google Scholar]
- Dantoine, F. (2016). Care pathways for people with epilepsy through national health insurance data. Journal of Epidemiology and Public Health, 66(1), S39–S40. [Google Scholar]
- Day, S. M. , Wu, Y. W. , Strauss, D. J. , Shavelle, R. M. , & Reynolds, R. J. (2005). Causes of death in remote symptomatic epilepsy. Neurology, 65(2), 216. 10.1212/01.wnl.0000169018.44950.68 [DOI] [PubMed] [Google Scholar]
- De Boer, H. M. , Mula, M. , & Sander, J. W. (2008). The global burden and stigma of epilepsy. Epilepsy & Behavior, 12(4), 540–546. 10.1016/j.yebeh.2007.12.019 [DOI] [PubMed] [Google Scholar]
- De Kinderen, R. J. A. , Evers, S. , Rinkens, R. , Postulart, D. , Vader, C. I. , Majoie, M. , & Aldenkamp, A. P. (2014). Side‐effects of antiepileptic drugs: The economic burden. Seizure: The Journal of the British Epilepsy Association, 23(3), 184–190. 10.1016/j.seizure.2013.11.009 [DOI] [PubMed] [Google Scholar]
- Devinsky, O. , Hesdorffer, D. C. , Thurman, D. J. , Lhatoo, S. , & Richerson, G. (2016). Sudden unexpected death in epilepsy: Epidemiology, mechanisms, and prevention. Lancet Neurology, 15(10), 1075–1088. 10.1016/S1474-4422(16)30158-2 [DOI] [PubMed] [Google Scholar]
- De Zelicourt, M. , De Toffol, B. , Vespignani, H. , Laurendeau, C. , Lévy‐Bachelot, L. , Murat, C. , & Fagnani, F. (2014). Management of focal epilepsy in adults treated with polytherapy in France: The direct cost of drug resistance (ESPERA study). Seizure: The Journal of the British Epilepsy Association, 23(5), 349–356. 10.1016/j.seizure.2014.01.016 [DOI] [PubMed] [Google Scholar]
- Ding, D. , Wang, W. , Wu, J. , Yang, H. , Li, S. , Dai, X. , Yang, B. , Wang, T. , Yuan, C. , Ma, G. , Bell, G. S. , Kwan, P. , De Boer, H. M. , Hong, Z. , & Sander, J. W. (2013). Premature mortality risk in people with convulsive epilepsy: Long follow‐up of a cohort in rural China. Epilepsia, 54(3), 512–517. 10.1111/epi.12048 [DOI] [PubMed] [Google Scholar]
- Elizebath, R. , Zhang, E. , Coe, P. , Gutierrez, E. G. , Yang, J. , & Krauss, G. L. (2021). Cenobamate treatment of focal‐onset seizures: Quality of life and outcome during up to eight years of treatment. Epilepsy & Behavior, 116, 107796. 10.1016/j.yebeh.2021.107796 [DOI] [PubMed] [Google Scholar]
- Espinosa‐Jovel, C. , Toledano, R. , Aledo‐Serrano, Á. , García‐Morales, I. , & Gil‐Nagel, A. (2018). Epidemiological profile of epilepsy in low income populations. Seizure: The Journal of the British Epilepsy Association, 56, 67–72. 10.1016/j.seizure.2018.02.002 [DOI] [PubMed] [Google Scholar]
- Ficker, D. M. (2000). Sudden unexplained death and injury in epilepsy. Epilepsia, 41, (Suppl 2), S7–S12. 10.1111/j.1528-1157.2000.tb01519.x [DOI] [PubMed] [Google Scholar]
- Fiest, K. M. , Dykeman, J. , Patten, S. B. , Wiebe, S. , Kaplan, G. G. , Maxwell, C. J. , Bulloch, A. G. M. , & Jette, N. (2013). Depression in epilepsy: A systematic review and meta‐analysis. Neurology, 80(6), 590–599. 10.1212/WNL.0b013e31827b1ae0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiest, K. M. , Sauro, K. M. , Wiebe, S. , Patten, S. B. , Kwon, C.‐S. , Dykeman, J. , Pringsheim, T. , Lorenzetti, D. L. , & Jetté, N. (2017). Prevalence and incidence of epilepsy: A systematic review and meta‐analysis of international studies. Neurology, 88(3), 296–303. 10.1212/wnl.0000000000003509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, R. S. , Acevedo, C. , Arzimanoglou, A. , Bogacz, A. , Cross, J. H. , Elger, C. E. , Engel, J. , Forsgren, L. , French, J. A. , Glynn, M. , Hesdorffer, D. C. , Lee, B. I. , Mathern, G. W. , Moshé, S. L. , Perucca, E. , Scheffer, I. E. , Tomson, T. , Watanabe, M. , & Wiebe, S. (2014). ILAE official report: A practical clinical definition of epilepsy. Epilepsia, 55(4), 475–482. 10.1111/epi.12550 [DOI] [PubMed] [Google Scholar]
- Forsgren, L. , Beghi, E. , Oun, A. , & Sillanpaa, M. (2005). The epidemiology of epilepsy in Europe—A systematic review. European Journal of Neurology, 12(4), 245–253. 10.1111/j.1468-1331.2004.00992.x [DOI] [PubMed] [Google Scholar]
- Gaitatzis, A. , Sisodiya, S. M. , & Sander, J. W. (2012). The somatic comorbidity of epilepsy: A weighty but often unrecognised burden. Epilepsia, 53(8), 1282–1293. 10.1111/j.1528-1167.2012.03528.x [DOI] [PubMed] [Google Scholar]
- Garcia, M. E. , Garcia‐Morales, I. , & Gil‐Nagel, A. (2015). Prevalence of depressive symptoms and their impact on quality of life in patients with drug‐resistant focal epilepsy (IMDYVA study). Epilepsy Research, 110, 157–165. 10.1016/j.eplepsyres.2014.11.003 [DOI] [PubMed] [Google Scholar]
- GBD . (2017). Global burden of disease study 2016 (GBD 2016) results .
- GHDx . (2019). GBD results: Idiopathic epilepsy. https://ghdx.healthdata.org/gbd‐results‐tool?params=gbd‐api‐2019‐permalink/18c71f2e1f39764dd16f7a20a625aa93
- Gholami, A. , Salarilak, S. , Lotfabadi, P. , Kiani, F. , Rajabi, A. , Mansori, K. , & Jahromi, Z. M. (2016). Quality of life in epileptic patients compared with healthy people. Medical Journal of the Islamic Republic of Iran, 30, 388–388. [PMC free article] [PubMed] [Google Scholar]
- GlobalData . (2017). PharmaPoint: Epilepsy – Global drug forecast and market analysis to 2026 (Reference Code: GDHC154PIDR).
- Goudsmit, J. , & Van Der Waals, F. (1983). Endemic epilepsy in an isolated region of Liberia. Lancet, 8323, 528–529. 10.1016/S0140-6736(83)92215-8 [DOI] [PubMed] [Google Scholar]
- Gupta, S. , Ryvlin, P. , Faught, E. , Tsong, W. , & Kwan, P. (2017). Understanding the burden of focal epilepsy as a function of seizure frequency in the United States, Europe, and Brazil. Epilepsia Open, 2(2), 199–213. 10.1002/epi4.12050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer, H. M. , Spottke, A. , Aletsee, C. , Knake, S. , Reis, J. , Strzelczyk, A. , Oertel, W. H. , Rosenow, F. , & Dodel, R. (2006). Direct and indirect costs of refractory epilepsy in a tertiary epilepsy center in Germany. Epilepsia, 47(12), 2165–2172. 10.1111/j.1528-1167.2006.00889.x [DOI] [PubMed] [Google Scholar]
- Harden, C. , Tomson, T. , Gloss, D. , Buchhalter, J. , Cross, J. H. , Donner, E. , French, J. A. , Gil‐Nagel, A. , Hesdorffer, D. C. , Smithson, W. H. , Spitz, M. C. , Walczak, T. S. , Sander, J. W. , & Ryvlin, P. (2017). Practice guideline summary: sudden unexpected death in epilepsy incidence rates and risk factors: Report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsy Currents, 17(3), 180–187. 10.5698/1535-7511.17.3.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesdorffer, D. C. , Ishihara, L. , Mynepalli, L. , Webb, D. J. , Weil, J. , & Hauser, W. A. (2012). Epilepsy, suicidality, and psychiatric disorders: A bidirectional association. Annals of Neurology, 72(2), 184–191. 10.1002/ana.23601 [DOI] [PubMed] [Google Scholar]
- Hesdorffer, D. C. , Tian, H. , Anand, K. , Hauser, W. A. , Ludvigsson, P. , Olafsson, E. , & Kjartansson, O. (2005). Socioeconomic status is a risk factor for epilepsy in Icelandic adults but not in children. Epilepsia, 46(8), 1297–1303. 10.1111/j.1528-1167.2005.10705.x [DOI] [PubMed] [Google Scholar]
- Holst, A. G. , Winkel, B. O. G. , Risgaard, B. , Nielsen, J. B. , Rasmussen, P. V. , Haunsø, S. , Sabers, A. , Uldall, P. , & Tfelt‐Hansen, J. (2013). Epilepsy and risk of death and sudden unexpected death in the young: A nationwide study. Epilepsia, 54(9), 1613–1620. 10.1111/epi.12328 [DOI] [PubMed] [Google Scholar]
- Hovinga, C. A. , Asato, M. R. , Manjunath, R. , Wheless, J. W. , Phelps, S. J. , Sheth, R. D. , Pina‐Garza, J. E. , Zingaro, W. M. , & Haskins, L. S. (2008). Association of non‐adherence to antiepileptic drugs and seizures, quality of life, and productivity: Survey of patients with epilepsy and physicians. Epilepsy & Behavior, 13(2), 316–322. 10.1016/j.yebeh.2008.03.009 [DOI] [PubMed] [Google Scholar]
- IHME (2020). Epilepsy—Level 1 impairment. http://www.healthdata.org/results/gbd_summaries/2019/epilepsy‐level‐1‐impairment
- Jacoby, A. , & Baker, G. A. (2008). Quality‐of‐life trajectories in epilepsy: A review of the literature. Epilepsy & Behavior, 2(4), 557–571. 10.1016/j.yebeh.2007.11.013 [DOI] [PubMed] [Google Scholar]
- Jilek‐Aall, L. , Jilek, W. , & Miller, J. R. (1979). Clinical and genetic aspects of seizure disorders prevalent in an isolated African population. Epilepsia, 20(6), 613–622. 10.1111/j.1528-1157.1979.tb04845.x [DOI] [PubMed] [Google Scholar]
- Kaiboriboon, K. , Bakaki, P. M. , Lhatoo, S. D. , & Koroukian, S. (2013). Incidence and prevalence of treated epilepsy among poor health and low‐income Americans. Neurology, 80(21), 1942–1949. 10.1212/WNL.0b013e318293e1b4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakis, I. , Cole, A. J. , Montouris, G. D. , San Luciano, M. , Meador, K. J. , & Piperidou, C. (2014). Caregiver burden in epilepsy: Determinants and impact. Epilepsy Research and Treatment, 2014, 808421. 10.1155/2014/808421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keezer, M. R. , Sisodiya, S. M. , & Sander, J. W. (2016). Comorbidities of epilepsy: Current concepts and future perspectives. Lancet Neurology, 15(1), 106–115. 10.1016/s1474-4422(15)00225-2 [DOI] [PubMed] [Google Scholar]
- Kelvin, E. A. , Hesdorffer, D. C. , Bagiella, E. , Andrews, H. , Pedley, T. A. , Shih, T. T. , Leary, L. , Thurman, D. J. , & Hauser, W. A. (2007). Prevalence of self‐reported epilepsy in a multiracial and multiethnic community in New York City. Epilepsy Research, 77(2‐3), 141–150. 10.1016/j.eplepsyres.2007.09.012 [DOI] [PubMed] [Google Scholar]
- Kerr, C. , Nixon, A. , & Angalakuditi, M. (2011). The impact of epilepsy on children and adult patients' lives: Development of a conceptual model from qualitative literature. Seizure: The Journal of the British Epilepsy Association, 20(10), 764–774. 10.1016/j.seizure.2011.07.007 [DOI] [PubMed] [Google Scholar]
- Kobau, R. , Zahran, H. , Grant, D. , Thurman, D. J. , Price, P. H. , & Zack, M. M. (2007). Prevalence of active epilepsy and health‐related quality of life among adults with self‐reported epilepsy in California: California Health Interview Survey, 2003. Epilepsia, 48(10), 1904–1913. 10.1111/j.1528-1167.2007.01161.x [DOI] [PubMed] [Google Scholar]
- Kobau, R. , Zahran, H. , Thurman, D. J. , Zack, M. M. , Henry, T. R. , Schachter, S. C. , & Price, P. H. , & Centers for Disease Control and Prevention (CDC) . (2008). Epilepsy surveillance among adults—19 States, Behavioral Risk Factor Surveillance System, 2005. Morbidity and Mortality Weekly Report Surveillance Summaries, 57(6), 1–20. [PubMed] [Google Scholar]
- Kotsopoulos, I. A. W. , Evers, S. , Ament, A. , & De Krom, M. (2001). Estimating the costs of epilepsy: An international comparison of epilepsy cost studies. Epilepsia, 42(5), 634–640. 10.1046/j.1528-1157.2001.18200.x [DOI] [PubMed] [Google Scholar]
- Kotsopoulos, I. A. W. , Van Merode, T. , Kessels, F. G. H. , De Krom, M. , & Knottnerus, J. A. (2002). Systematic review and meta‐analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia, 43(11), 1402–1409. 10.1046/j.1528-1157.2002.t01-1-26901.x [DOI] [PubMed] [Google Scholar]
- Kwan, P. , Arzimanoglou, A. , Berg, A. T. , Brodie, M. J. , Allen Hauser, W. , Mathern, G. , Moshé, S. L. , Perucca, E. , Wiebe, S. , & French, J. (2010). Definition of drug resistant epilepsy: Consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia, 51(6), 1069–1707. 10.1111/j.1528-1167.2009.02397.x [DOI] [PubMed] [Google Scholar]
- Kwan, P. , & Brodie, M. J. (2000). Early identification of refractory epilepsy. New England Journal of Medicine, 342(5), 314–319. 10.1056/nejm200002033420503 [DOI] [PubMed] [Google Scholar]
- Lai, S.‐T. , Tan, W.‐Y. , Wo, M. C.‐M. , Lim, K.‐S. , Ahmad, S. B. , & Tan, C.‐T. (2019). Burden in caregivers of adults with epilepsy in Asian families. Seizure: The Journal of the British Epilepsy Association, 71, 132–139. 10.1016/j.seizure.2019.07.008 [DOI] [PubMed] [Google Scholar]
- Laxer, K. D. , Trinka, E. , Hirsch, L. J. , Cendes, F. , Langfitt, J. , Delanty, N. , Resnick, T. , & Benbadis, S. R. (2014). The consequences of refractory epilepsy and its treatment. Epilepsy & Behavior, 37, 59–70. 10.1016/j.yebeh.2014.05.031 [DOI] [PubMed] [Google Scholar]
- Levira, F. , Thurman, D. J. , Sander, J. W. , Hauser, W. A. , Hesdorffer, D. C. , Masanja, H. , Odermatt, P. , Logroscino, G. , & Newton, C. R. (2017). Premature mortality of epilepsy in low‐ and middle‐income countries: A systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia, 58(1), 6–16. 10.1111/epi.13603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lhatoo, S. D. , & Sander, J. (2005). Cause‐specific mortality in epilepsy. Epilepsia, 46, (Suppl 11), 36–39. 10.1111/j.1528-1167.2005.00406.x [DOI] [PubMed] [Google Scholar]
- Li, X. , Sundquist, J. , & Sundquist, K. (2008). Socioeconomic and occupational risk factors for epilepsy: A nationwide epidemiological study in Sweden. Seizure: The Journal of the British Epilepsy Association, 17(3), 254–260. 10.1016/j.seizure.2007.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoni, C. , Canevini, M. P. , Capovilla, G. , De Sarro, G. , Galimberti, C. A. , Gatti, G. , Guerrini, R. , La Neve, A. , Mazzucchelli, I. , Rosati, E. , Specchio, L. M. , Striano, S. , Tinuper, P. , & Perucca, E. (2015). A prospective study of direct medical costs in a large cohort of consecutively enrolled patients with refractory epilepsy in Italy. Epilepsia, 56(7), 1162–1173. 10.1111/epi.13030 [DOI] [PubMed] [Google Scholar]
- Manjunath, R. , Paradis, P. E. , Parise, H. , Lafeuille, M.‐H. , Bowers, B. , Duh, M. S. , Lefebvre, P. , & Faught, E. (2012). Burden of uncontrolled epilepsy in patients requiring an emergency room visit or hospitalisation. Neurology, 79(18), 1908–1916. 10.1212/WNL.0b013e318271f77e [DOI] [PubMed] [Google Scholar]
- Marson, A. , Appleton, R. , Baker, G. , Chadwick, D. , Doughty, J. , Eaton, B. , Gamble, C. , Jacoby, A. , Shackley, P. , Smith, D. , Tudur‐Smith, C. , Vanoli, A. , & Williamson, P. (2007). A randomised controlled trial examining the longer‐term outcomes of standard versus new antiepileptic drugs. The SANAD trial. Health Technology Assessment (Winchester, England), 11(37), iii–iv. ix‐x, 1–134. 10.3310/hta11370 [DOI] [PubMed] [Google Scholar]
- Neuman, R. J. , Kwon, J. M. , Jilek‐Aall, L. , Rwiza, H. T. , Rice, J. P. , & Goodfellow, P. J. (1995). Genetic analysis of kifafa, a complex familial seizure disorder. American Journal of Human Genetics, 57(4), 902–910. [PMC free article] [PubMed] [Google Scholar]
- Ngugi, A. K. , Bottomley, C. , Kleinschmidt, I. , Sander, J. W. , & Newton, C. R. (2010). Estimation of the burden of active and lifetime epilepsy: A meta‐analytic approach. Epilepsia, 51(5), 883–890. 10.1111/j.1528-1167.2009.02481.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngugi, A. K. , Kariuki, S. M. , Bottomley, C. , Kleinschmidt, I. , Sander, J. W. , & Newton, C. R. (2011). Incidence of epilepsy: A systematic review and meta‐analysis. Neurology, 77(10), 1005–1012. 10.1212/WNL.0b013e31822cfc90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE . (2012). Epilepsies: Diagnosis and management: Clinical guidance [CG137] .
- Noronha, A. L. A. , Borges, M. A. , Marques, L. H. N. , Zanetta, D. M. T. , Fernandes, P. T. , De Boer, H. , Espíndola, J. , Miranda, C. T. , Prilipko, L. , Bell, G. S. , Sander, J. W. , & Li, L. M. (2007). Prevalence and pattern of epilepsy treatment in different socioeconomic classes in Brazil. Epilepsia, 48(5), 880–885. 10.1111/j.1528-1167.2006.00974.x [DOI] [PubMed] [Google Scholar]
- Pardoe, H. R. , Cole, J. H. , Blackmon, K. , Thesen, T. , & Kuzniecky, R. (2017). Human Epilepsy Project I. Structural brain changes in medically refractory focal epilepsy resemble premature brain aging. Epilepsy Research, 133, 28–32. 10.1016/j.eplepsyres.2017.03.007 [DOI] [PubMed] [Google Scholar]
- Patel, R. S. , Elmaadawi, A. , Mansuri, Z. , Kaur, M. , Shah, K. , & Nasr, S. (2017). Psychiatric comorbidities and outcomes in epilepsy patients: An insight from a nationwide inpatient analysis in the United States. Cureus, 9(9), e1686. 10.7759/cureus.1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perucca, P. , Carter, J. , Vahle, V. , & Gilliam, F. G. (2009). Adverse antiepileptic drug effects: Toward a clinically and neurobiologically relevant taxonomy. Neurology, 72(14), 1223–12239. 10.1212/01.wnl.0000345667.45642.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili, M. , Girardi, P. , Tatarelli, G. , Angeletti, G. , & Tatarelli, R. (2006). Suicide after surgical treatment in patients with epilepsy: A meta‐analytic investigation. Psychological Reports, 98(2), 323–338. 10.2466/pr0.98.2.323-338 [DOI] [PubMed] [Google Scholar]
- Ridsdale, L. , Charlton, J. , Ashworth, M. , Richardson, M. P. , & Gulliford, M. C. (2011). Epilepsy mortality and risk factors for death in epilepsy: A population‐based study. British Journal of General Practice, 61(586), e271–e278. 10.3399/bjgp11X572463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson, J. , Hatton, C. , Emerson, E. , & Baines, S. (2015). Prevalence of epilepsy among people with intellectual disabilities: A systematic review. Seizure: The Journal of the British Epilepsy Association, 29, 46–62. 10.1016/j.seizure.2015.03.016 [DOI] [PubMed] [Google Scholar]
- Salas‐Puig, X. , Iniesta, M. , Abraira, L. , & Puig, J. , & Group Q‐Gs . (2019). Accidental injuries in patients with generalised tonic‐clonic seizures. A multicenter, observational, cross‐sectional study (QUIN‐GTC study). Epilepsy & Behavior, 92, 135–139. 10.1016/j.yebeh.2018.10.043 [DOI] [PubMed] [Google Scholar]
- Sander, T. (2000). Genome search for susceptibility loci of common idiopathic generalised epilepsies. Human Molecular Genetics, 9(10), 1465–1472. 10.1093/hmg/9.10.1465 [DOI] [PubMed] [Google Scholar]
- Schmidt, D. , & Schachter, S. C. (2014). Drug treatment of epilepsy in adults. BMJ, 348, g254. 10.1136/bmj.g254 [DOI] [PubMed] [Google Scholar]
- Scott, A. J. , Sharpe, L. , Hunt, C. , & Gandy, M. (2017). Anxiety and depressive disorders in people with epilepsy: A meta‐analysis. Epilepsia, 58(6), 973–982. 10.1111/epi.13769 [DOI] [PubMed] [Google Scholar]
- Seidenberg, M. , Pulsipher, D. T. , & Hermann, B. (2009). Association of epilepsy and comorbid conditions. Future Neurology, 4(5), 663–668. 10.2217/fnl.09.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling, M. R. , Barshow, S. , Nei, M. , & Asadi‐Pooya, A. A. (2016). A reappraisal of mortality after epilepsy surgery. Neurology, 86(21), 1938–1944. 10.1212/WNL.0000000000002700 [DOI] [PubMed] [Google Scholar]
- Stern, J. , Penovich, P. , Becker, D. , Long, L. , Santilli, N. , & Peck, E. (2020). Perspectives on epilepsy‐related fears among adult patients living with epilepsy, caregivers, and healthcare professionals. American Academy of Neurology 2020 Virtual Annual Meeting.
- Strzelczyk, A. , Griebel, C. , Lux, W. , Rosenow, F. , & Reese, J.‐P. (2017). The burden of severely drug‐refractory epilepsy: A comparative longitudinal evaluation of mortality, morbidity, resource use, and cost using German Health Insurance Data. Front Neurology, 8, 712. 10.3389/fneur.2017.00712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strzelczyk, A. , Reese, J. P. , Dodel, R. , & Hamer, H. M. (2008). Cost of epilepsy: A systematic review. Pharmacoeconomics, 26(6), 463–476. 10.2165/00019053-200826060-00002 [DOI] [PubMed] [Google Scholar]
- Tang, D. H. , Malone, D. C. , Warholak, T. L. , Chong, J. , Armstrong, E. P. , Slack, M. K. , Hsu, C.‐H. , & Labiner, D. M. (2015). Prevalence and incidence of epilepsy in an elderly and low‐income population in the United States. Journal of Clinical of Neurology, 11(3), 252–261. 10.3988/jcn.2015.11.3.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, R. S. , Sander, J. W. , Taylor, R. J. , & Baker, G. A. (2011). Predictors of health‐related quality of life and costs in adults with epilepsy: A systematic review. Epilepsia, 52(12), 2168–2180. 10.1111/j.1528-1167.2011.03213.x [DOI] [PubMed] [Google Scholar]
- Thijs, R. D. , Surges, R. , O'Brien, T. J. , & Sander, J. W. (2019). Epilepsy in adults. Lancet, 393(10172), 689–701. 10.1016/s0140-6736(18)32596-0 [DOI] [PubMed] [Google Scholar]
- Thurman, D. J. , Logroscino, G. , Beghi, E. , Hauser, W. A. , Hesdorffer, D. C. , Newton, C. R. , Scorza, F. A. , Sander, J. W. , & Tomson, T. (2017). The burden of premature mortality of epilepsy in high‐income countries: A systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia, 58(1), 17–26. 10.1111/epi.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomson, T. , Nashef, L. , & Ryvlin, P. (2008). Sudden unexpected death in epilepsy: Current knowledge and future directions. Lancet Neurology, 7(11), 1021–31. 10.1016/S1474-4422(08)70202-3 [DOI] [PubMed] [Google Scholar]
- Trinka, E. , Bauer, G. , Oberaigner, W. , Ndayisaba, J.‐P. , Seppi, K. , & Granbichler, C. A. (2013). Cause‐specific mortality among patients with epilepsy: Results from a 30‐year cohort study. Epilepsia, 54(3), 495–501. 10.1111/epi.12014 [DOI] [PubMed] [Google Scholar]
- Verrotti, A. , Carrozzino, D. , Milioni, M. , Minna, M. , & Fulcheri, M. (2014). Epilepsy and its main psychiatric comorbidities in adults and children. Journal of the Neurological Sciences, 343(1–2), 23–29. 10.1016/j.jns.2014.05.043 [DOI] [PubMed] [Google Scholar]
- Versteeg, A. C. , Carter, J. A. , Dzombo, J. , Neville, B. G. , & Newton, C. (2003). Seizure disorders among relatives of Kenyan children with severe falciparum malaria. Tropical Medicine & International Health: Tm & Ih, 8(1), 12–16. 10.1046/j.1365-3156.2003.00965.x [DOI] [PubMed] [Google Scholar]
- Villanueva, V. , Girón, J. M. , Martín, J. , Hernández‐Pastor, L. J. , Lahuerta, J. , Doz, M. , Cuesta, M. , & Lévy‐Bachelot, L. (2013). Quality of life and economic impact of refractory epilepsy in Spain: The ESPERA study. Neurologia, 28(4), 195–204. 10.1016/j.nrl.2012.04.012 [DOI] [PubMed] [Google Scholar]
- Vrouchou, P. , Risi, A. , Annoni, E. , Alvarez, G. , & Grovale, N. (2015). Humanistic and economic burden of focal drug‐refractory epilepsy in Europe. Value in Health, 18(7), A765. 10.1016/j.jval.2015.09.2510 [DOI] [Google Scholar]
- Wagner, A. P. , Croudace, T. J. , Bateman, N. , Pennington, M. W. , Prince, E. , Redley, M. , White, S. R. , & Ring, H. (2017). Clinical services for adults with an intellectual disability and epilepsy: A comparison of management alternatives. Plos One, 12(7), e0180266–e0180266. 10.1371/journal.pone.0180266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace, R. H. , Scheffer, I. E. , Parasivam, G. , Barnett, S. , Wallace, G. B. , Sutherland, G. R. , Berkovic, S. F. , & Mulley, J. C. (2002). Generalised epilepsy with febrile seizures plus: Mutation of the sodium channel subunit SCN1B. Neurology, 58(9), 1426–1429. 10.1212/wnl.58.9.1426 [DOI] [PubMed] [Google Scholar]
- Wheless, J. W. (2006). Intractable epilepsy: A survey of patients and caregivers. Epilepsy & Behavior, 8(4), 756–764. 10.1016/j.yebeh.2006.03.010 [DOI] [PubMed] [Google Scholar]
- Whitney, R. , & Donner, E. J. (2019). Risk Factors for Sudden Unexpected Death in Epilepsy (SUDEP) and Their Mitigation. Current Treatment Options in Neurology, 21(2), 7. 10.1007/s11940-019-0547-4 [DOI] [PubMed] [Google Scholar]
- WHO . (2019). Epilepsy: A public health imperative . https://www.who.int/mental_health/neurology/epilepsy/report_2019/en/
- WHO . (2020). Depression and other common mental disorders: Global health estimates. https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/
- Wiebe, S. , Eliasziw, M. , Bellhouse, D. R. , & Fallahay, C. (1999). Burden of epilepsy: The Ontario Health Survey. Canadian Journal of Neurological Sciences, 26(4), 263–270. 10.1017/s0317167100000354 [DOI] [PubMed] [Google Scholar]
- Witt, J.‐A. , & Helmstaedter, C. (2013). Monitoring the cognitive effects of antiepileptic pharmacotherapy—Approaching the individual patient. Epilepsy & Behavior, 26(3), 450–456. 10.1016/j.yebeh.2012.09.015 [DOI] [PubMed] [Google Scholar]
- Younus, I. , & Reddy, D. S. (2018). A resurging boom in new drugs for epilepsy and brain disorders. Expert Review of Clinical Pharmacology, 11(1), 27–45. 10.1080/17512433.2018.1386553 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.


