Abstract
Systemic lupus erythematosus (SLE) may be more prevalent among most ethnic groups in the low-and-middle income countries (LMICs), still these countries are under-represented in epidemiological data on SLE. The aim of this study was to review the prevalence and incidence of SLE in LMICs and use meta-analytic techniques. The MEDLINE, CINHAL, Web of Science, Scopus and Global Index Medicus databases were searched for relevant studies published up to July of 2022. Papers selected for full-text review were included in the systematic review if they provided the prevalence or incidence of SLE in LMICs and published in English language. The reference lists of included articles were also searched for additional studies. Two individuals independently performed abstract and full-text review, data extraction, and quality assessment of the papers. The prevalence and incidence of SLE were pooled through random effects model. Pooled estimates were expressed with 95% confidence. Out of 2340 papers, 23 studies were included in the review. The mean age at diagnosis ranged from 25.5 to 45.8 years. Three studies were conducted in Argentina and Brazil, two studies in China and one study in Cuba, Colombia, Democratic Republic Congo, Ecuador, Egypt, India, Kenya, Malaysia, Mexico, Nigeria, Pakistan, Turkey, Ukraine, Venezuela, and Zimbabwe. The SLE prevalence and incidence varied from 3.2 to 159 per 100,000 and 0.3–8.7 per 100,000 persons, respectively. In a random effects meta-analysis (n = 10), the pooled prevalence of SLE was 103 (95% confidence interval [CI] – 17 to 224) per 100,000. Meta‐analysis of data from 6 incidence studies revealed an incidence of 5 cases per year (95% CI 2–8) per 100,000. According to WHO regions, the pooled prevalence of American and Western Pacific regions was 300 (95% CI – 200 to 900) and 36 (95% CI 35–37) per 100,000, respectively. The pooled incidence of the American region was 10 (95%, 0–14) per 100,000 inhabitants. Systemic lupus erythematosus is a common disease with considerable variation in prevalence and incidence among the general population in LMICs. Accurate estimates of prevalence and incidence of SLE are required to put in place appropriate programmes to reduce its burden in LMICs. PROSPERO registration number: CRD: 42020197495, https://www.crd.york.ac.uk/prospero/.
Keywords: Systemic lupus erythematosus, Systematic review, Incidence, Prevalence, LMICs
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that causes inflammation of connective tissues [1]. In general, SLE has propensity to affect every organ and tissue of the body, and its pattern of clinical manifestations varies widely among patients [2]. The complex interactions among genetic disposition, environmental risk factors, and the hormonal status contribute to the clinical heterogeneity in clinical manifestation of SLE, thus making its often problematic or keenly dependent on clinical expertise, in addition to immunological findings [2–5].
The incidence and prevalence of SLE vary widely in population demographics, socioeconomic factors, and certain ethnic population, such as Hispanic population, black and Asian [1, 6–8]. Specifically, in Europe and North America, people of African descent [9, 10], American Indians and Alaska Natives [11, 12] have higher predilection and worse outcomes from SLE than Caucasians within the same contexts [13]. Therefore, there are numerous indications that SLE is less severe in patients of European ancestry than Asian, African, and certain “Hispanic” or various indigenous populations [6, 14]. In Australia, Canada and USA, SLE disease among aboriginal/indigenous individuals are twofold to fourfold more common compared to non-aboriginal individuals [15]. Furthermore, patients from Asia and African ancestry are also likely to have a greater number of clinical manifestations, active SLE onset and higher mortality than white populations [16].
The clinical technicalities and complexity with diagnosing SLE may have contributed to assertions that the disease is infrequent in Africa [9, 10]. However, emerging reports indicates that the prevalence of SLE in sub-Saharan African was 1.7% (0.8–2.9 which is lower than the Asian–Pacific countries [19]. The overall incidence and prevalence of SLE across Asian–Pacific countries ranged from 0.9 to 3.1 and 4.3–45.3 per 100,000, respectively [18]. Furthermore, the incidence of SLE in North America and Europe ranged from 3.7 to 49 and 1.5 and 7.4 per 100,000 person-years, respectively [20–22]. Evidence also suggests that there is a gradual increase of SLE prevalence in North America, Europe and Asia [17]. Though, study design reporting bias, case definitions and SLE classification criteria may also result to a variation of the proportion of the population that has SLE [17].
Despite the variation of SLE across all age groups, it is more common between the ages of 15 and 45 years [23]. Evidence showed that in 10–20% of patients with SLE disease starts in childhood, this is due to increased renal, neuropsychiatric and cardiopulmonary disease [24–26]. The gender disparity of SLE is also widely recognised with a 1: 9 ratio of male to female patients. The incidence and prevalence of SLE in females is usually highest at 15–44 and 45–64 years of age, respectively [11].
Due to environmental, genetic, and racial factors the prevalence and incidence of SLE varies across the various regions of the world. For instance, changes in environmental factors are associated with increased in SLE [27]. Furthermore, the severity and course of SLE may often be related to the difference education, health insurance status, income level, ethnicity, medication compliance and level of social support. The survival rate of SLE patients in LMICs is lower than high income countries, this is due to higher mortality, poor intervention, and co-morbidities of infection [28]. To date there is no systematic review that summarized the prevalence and incidence of SLE published in LMICs [11, 21, 29]. The aim of this review was to summarise the global and regional prevalence and incidence of SLE in LMICs.
Methods
This systematic review followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline [30]. The review was registered with PROSPERO—the International Prospective Register of Systematic Reviews CRD: 42020197495.
Data sources and search strategy
An electronic database search was carried out on titles and abstracts till 11th of July 2022. MEDLINE, CINHAL, Web of Science, Scopus and Global Index Medicus databases and were used to search the literature. Search terms used were: lupus, systemic lupus erythematosus, disseminated lupus erythematosus’, lupus erythematosus disseminates and libman-sacks disease, prevalence, incidence, epidemiology, and rheumatic disease (see Appendix for detailed search strategy). In addition to these databases, hand searches from the references of the included studies were also used. All references were downloaded to EndNote X8 and duplicates were removed.
Study selection
One reviewer (TG) conducted the search. Two independent researchers (TG & FF) screened titles and abstracts. The potential eligible papers were retrieved, and two reviewers (TG & FF) agreed the initial inclusion criteria. The inclusion criteria were population of all age groups with lupus, both retrospective and prospective study designs and prevalence and incidence estimates of lupus in LMICs and studies should be available in English and full text. LMIC classification was confirmed by cross-referencing with the World Bank list of Countries by Income Level. Conference proceedings, review articles, articles in press, abstracts or editorials were the exclusion criteria. Articles on SLE cases in the context of overlap syndrome were also excluded from the review. The classification for SLE was based on the 1982 American College of Rheumatology and/or revised 1997 American College of Rheumatology criteria [11, 31]. Any disagreement in study selection was resolved through discussion and consultation with a third reviewer (CM) where necessary.
Data extraction
Data were extracted from the full text articles by one (TG) of the authors using a predefined form. The data extracted included authors and date of the study, population and setting, ethnicity/race, case definition, incidence rate and prevalence. The extracted data were cross-checked by another reviewer (FF). If disagreement occurred, consensus was reached through discussion.
Appraisal of individual study quality
Two independent reviewers (TG & FF) appraised the quality of the included studies. The included studies were assessed using a risk of bias tool developed by Hoy et al. [32]. The assessment tool consists of 10 items addressing the external and internal validity. This tool consists of ten items, including six items addressing internal validity (i.e., measurement reliability) and four items addressing external validity (i.e., representativeness of sample). The questions can be responded as ‘yes’ or ‘no’. The overall risk of bias for each study was evaluated low, moderate, and low. Studies with scores of 9 or 10 ‘yes’-answers were considered to have low risk of bias; studies with scores of 7 or 8 were considered to have moderate risk of bias and studies with scores of 6 or less were considered to have high risk of bias. Any disagreement was resolved by discussion with the third author (CM).
Data synthesis and analysis
Studies were included in the meta-analysis if they reported the number of SLE cases and sample denominator, the estimate with 95% CI, or the information with which to calculate the estimated prevalence or incidence. All studies reporting period prevalence were converted to annual prevalence estimate. A statistical heterogeneity was assessed with I2, a statistic that estimates the percentage of total variation due to heterogeneity across studies, where 0–25% was low, 26–74% moderate and 75% and over high statistical heterogeneity [33]. All the pooled estimates and 95% confidence intervals were calculated using a random-effects model. The Comprehensive Meta-Analysis software version 3 (CMA.V3) (Biostat, Inc., Englewood, NJ, USA) were used to analyse the data [34, 35].
Results
Study selection and characteristics
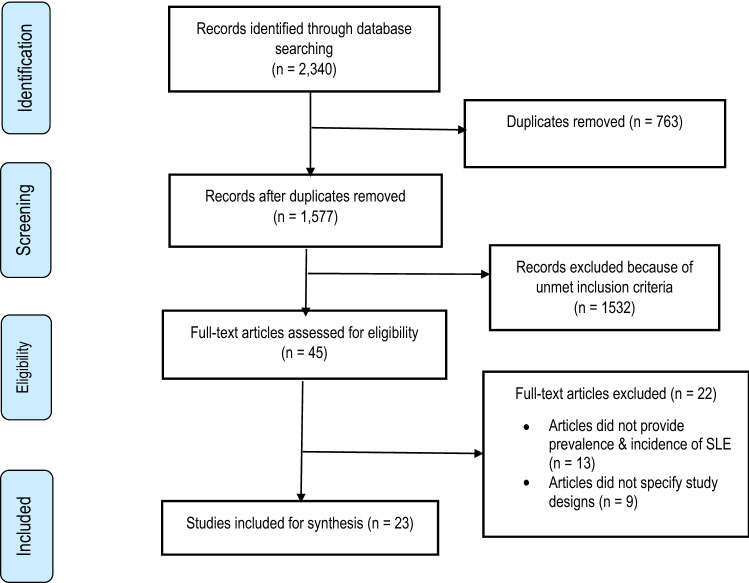
The systematic literature search results are presented in Fig. 1. Out of 2,340 titles, 23 studies that summarise the prevalence and incidence of SLE in LMICs were included in the review. Of the 23 included papers, 16 had low risk of bias and the remaining 7 had moderate risk of bias. The full risk-of-bias assessment is shown in Table 1.
Fig. 1.
Flow diagram of publications included and excluded in the review
Table 1.
Basic characteristics of the studies retained for the analyses
| Study, country | Study population (Mean age, years) | WHO regions | Sample size | Ethnicity/Race (%) | Case definition | Prevalence/ 100,000 |
Incidence/ 100,000 |
Risk of bias |
|---|---|---|---|---|---|---|---|---|
| Gonzalez et al. 2016 [36]; Argentina | Tucuma´n population; (30.5 ± 11.7) | AMRO |
904,188 W = 93.5% M = 6.5% |
83 Mestizos and 17 were African–Latin American | ACR | 24.3 (95% CI 22.6–28.8) |
1.8 (95% CI 1–2.9) 4.2 (95% CI 2.9–5.8) |
Low |
| Pamuk et al. 2016 [37], Turkey | Rural and urban population in Turkey; (38.5) | EURO |
620,477 W = 306,036 M = 314,411 |
N/A | ICD-10 code | 51.7 (95% CI 46–57.4) | 4.44 | Low |
| Fernández-Ávila et al. 2019 [38]; Colombia | Colombian population (Over 18) | AMRO |
47,663,162 W = 89% M = 11% |
N/A | Not explicitly addressed | 126.3 | N/A | Low |
| Zou et al. 2014 [39]; China | General residents in rural Anhui, China (All age groups) | WPRO |
1,358,725 M = 51.2% |
All Chinese | ACR | 36.03 (95% CI 35.54, 36.51) | N/A | Low |
| Ekwom 2013 [40]; Kenya | Patients attended at Kenyatta National Hospital (34) | AFRO |
394 W = 100% |
Black Africans | ACR | 3000 [95% 1800–5600] | N/A | Moderate |
| Gbané-Koné et al. 2015 [41]; Nigeria | Patients attended in rheumatology department’s; (35.76) | AFRO | 18,076 | Black Africans | ACR | 640 [95% 500–800] | N/A | Moderate |
| Wang et al. 1997 [42]; Malaysia | Patients attended in hospital (25.5 ± 10.1) | WPRO |
539 W = 93%; Men = 7% |
Chinese = 76 Malays = 17 Indians = 7 | ACR | 43 | N/A | Moderate |
| Farooqi and Gibson 1998 [43]; Pakistan | Population in Punjabis, Pakistan | EMRO | 700 | N/A | WHO–ILAR COPCORD study | 50 | N/A | Low |
| Taylor and Stein 1986 [44]; Zimbabwe | Patients attended Mpilo Hospital (28) | AFRO |
31 W = 30; M = 1 |
Mestizos = 83 | ACR revised criteria | N/A | 0.3 | Moderate |
| Nakashima et al. 2011 [45]; Brazil | Patients in Cascavel, state Paraná (41.5 ± 14.44) | AMRO |
291,747 W = 149,790 M = 141,957 |
N/A | ACR | N/A | 4.8 | Low |
| Vilar et al. [46]; Brazil | Patients living in Natal (31.8) | AMRO | 493 239 (W = 269 900; M = 223 339) |
White = 77 Non-White = 23 |
ACR | N/A |
8.7 (95% CI 6.3 – 11.7) W = 14.1(95% CI 10.0 – 19.3) M = 2.2 (95% CI 0.7 – 5.2) |
Low |
| Scolnik et al. 2014 [47]; Argentina | Patients attended in hospital, Buenos Aires | AMRO | 127,959 | All Caucasian | ACR | 58.6 (95% CI 46.1–73.5) | 6.3 (95% CI 4.9—7.7) | Low |
| Nasonov et al. 2014 [48]; Ukraine | Population in Ukraine (37) | EURO |
367,500 M = 163,538 W = 203,962 |
98.6 Caucasian; 1.14 Asian | ACR | 14.9 (95% CI 10.9–19.9) | 0.3 (95% CI 0.0–1.8) | Low |
| Senna et al. 2004 [49]; Brazil | Individuals from Montes Claros (37) | AMRO | 3038 |
White = 38 Non-White = 62 |
ACR | 98 | N/A | Moderate |
| Granados et al. 2015 [50]; Venezuela | Urban community in Venezuela (43.7) | AMRO |
3,973 M = 1,606 W = 2,367 |
All Las Cocuizas |
ACR | 70 (95% CI 10–200) | N/A | Moderate |
| Pelaez-Ballestas et al. 2011[51]; Mexico | Patients from México (42.8 (SD 17.9)) | AMRO | 4059 | N/A | ACR | 90 (95% 20–200) | N/A | Low |
| Li et al. 2012 [52]; China | Chinese population, (45.8) | WPRO | 14,642 | N/A | ACR | 30 (95% CI 0–60) | N/A | Low |
| Malaviya et al. 1993 [53]; India | Northern Indian population | SEARO | 91 888 | N/A | ANA | 3.2 (95% CI 0–6.86) | N/A | Low |
| Malemba and Mbuyi-Muamba 2008 [54]; DRC | Patients attending hospital (49.7 ± 13.1) | AFRO |
2370 W = 55.3% M = 44.7% |
Black Africans | ACR | 100 [95% 60–1500] | N/A | Moderate |
| Reyes-Llerena et al. 2009 [56]; Cuba | Patients with musculoskeletal complaints | AMRO |
3155 M = 1238; W = 1917 |
N/A | ACR | 60 (95% CI 10–250) | N/A | Low |
| Gheita et al. 2021[57]; Egypt | Patients of SLE across the nation (32.4 (SD 10.1)) | EMRO |
3661 (W = 3296; M = 365) |
N/A | N/A | 6.1 | N/A | Low |
| Guevara- Pacheco et al. 2016 [55]; Ecuador | Patients living Cuenca City, 42.8 (SD 18.8) | AMRO | 4877 (W = 59.7%) | N/A | COPCORD questionnaire | 60 (95% CI 10–100) | N/A | Low |
| Quintana et al. 2016 [58]; Argentina | Patients in Rosario City (35.3 (SD 13.9)) | AMRO | 1656 (W = 61.5%) | N/A | WHO ICD-10 | 60 (95% CI 1–300) | N/A | Low |
WPRO Western Pacific, AMRO American region, EMRO Eastern Mediterranean region, AFRO African region, ACR American College of Rheumatology criteria, N/A Not available, W Women, M Men, WHO-ILAR COPCORD World Health Organization and the International League of Associations for Rheumatology The Community Oriented Program for Control of Rheumatic Diseases, EURO European, ACR American College of Rheumatology criteria, ANA Anti-Nuclear Antibody test, DRC Democratic Republic of the Congo, COPCORD Community-Oriented Program for the Control of Rheumatic Diseases
The characteristics of the included studies are presented in Table 1. The included studies were from European regions (n = 2), Western Pacific regions (n = 3), the American region (n = 11), Eastern Mediterranean region (n = 2), the African region (n = 4) and Southeast Asia region (n = 1). The included studies were carried out in 17 countries. The studies were contributed from Argentina (n = 3), Brazil (n = 3), China (n = 2), Colombia, Ecuador, Egypt, Turkey, India, Malaysia, Pakistan, Ukraine, Venezuela, Zimbabwe, Mexico, Democratic Republic Congo, Cuba and Nigeria and Kenya. The mean age at diagnosis ranged from 25.5 to 49.7 years.
Prevalence and incidence
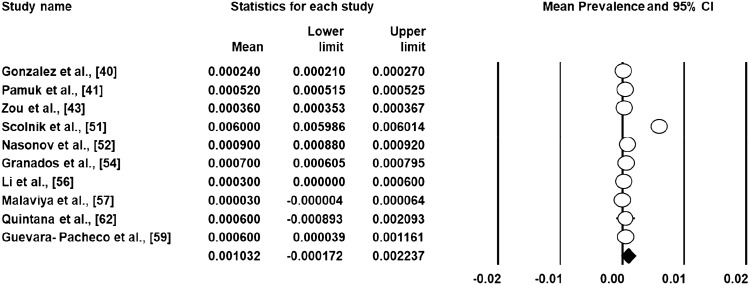
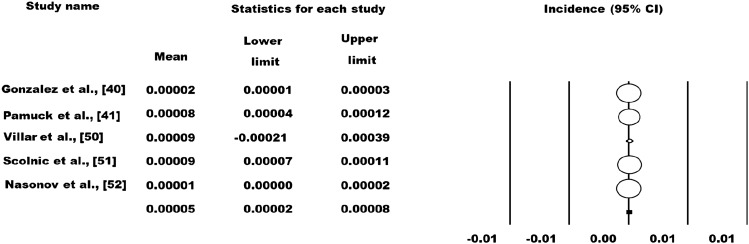
The prevalence and incidence rates of SLE varied from 3.2 to 3000 per 100,000 and 1.4–8.7 per 100,000 persons, respectively. The highest and lowest prevalence rate of SLE were reported in Colombia and Ukraine, respectively. In relation to the incidence rate the highest and lowest rate was recorded in Brazil and Ukraine. In the random effects meta-analysis (n = 10), the pooled prevalence of SLE was 103 (95% CI – 17 to 223) per 100,000 (Fig. 2). Meta‐analysis of data from five incidence studies revealed an incidence of 5 cases per year (95% CI: 2–8) per 100,000 (Fig. 3). According to WHO regions, the pooled prevalence of American region, Western Pacific regions and African region was 300 (95% CI – 200 to 900); 36 (95% CI 35–37) and 60 (95% CI – 40 to 1300) per 100,000, respectively. The pooled incidence of the American region was 10 (95% CI 0–14) per 100,000 persons.
Fig. 2.
Prevalence of SLE across LMICs settings
Fig. 3.
Incidence of SLE across LMICs settings. a Annual incidence of SLE, 2005–2012 in Tucuma´n, Argentina. b Incidence rates of SLE by 4-year periods (2003–2006, 2007–2010, 2011–2014) in Turkey. c Prevalence of SLE between 2012 and 2016 in Colombia
Sex related prevalence and incidence
Out of the total, twelve of the included studies reported the sex related prevalence or incidence of SLE (Table 2). The prevalence and incidence of men ranged from 0 to 90 and 0.5 to 2.6 per 100, 000 inhabitants, respectively. For the female population, the prevalence and incidence of SLE ranged from 23.8 to 204.3 and 4.72 to 14.1 per 100, 000 persons, respectively. Overall, the prevalence and incidence of SLE among women are higher than men.
Table 2.
Sex-related prevalence and incidence of SLE per 100,000
| Study | Number (prevalence) | Number (incidence) | ||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Pamuk et al. 2016 [36] | 314,411 (7 (95% CI 4.1–9.9)) | 306,036 (97.7 (95% CI 86.6–108.8)) | 314,411 (0.64 (95% CI 0–1.52)) | 306,036 (8.4 (95% CI 5.2–11.6)) |
| Fernández-Ávila et al. 2019 [38] | 42 million (20.3) | 5.2 million (204.3) | N/A | N/A |
| Zou et al. 2014 [39] | 642,036 (6.17) | 611,796 (67.78) | N/A | N/A |
| Nakashima et al. 2011 [45] | N/A | N/A | 141,957 (0) | 149,790 (9.3) |
| Vilar et al. 2011[46] | N/A | N/A | 223,339 (2.2 (95% CI 0.7–5.2)) | 269,900 (14.1 (95% CI 10.0–19.3)) |
| Gonzalez et al. 2016 [36] | N/A | 940,404 (34.9 (95% CI 32.8–41.1) | N/A | 940,404 (4.2 (95% CI 2.9–5.8)) |
| Scolnik et al. 2014 [47] | 12,795 (23 (CI 95% 11.9–40.1)) | 115,163 (83.2 (CI 95% 63.9–106.4)) | 12,795 (2.6 (CI 1.2–3.9)) | 115,163 (8.9 (CI 95% 6.6–11.2)) |
| Nasonov et al. 2014 [48] | 183,600 (3.7 (CI 1.2–8.7)) | 229,900 (23.8 (CI 17.0–32.4)) | N/A | N/A |
| Senna et al. 2004 [49] | 1109 (90 (CI 0.0–260)) | 1929 (110 (CI 0.0–240)) | N/A | N/A |
| Li et al. 2012 [52] | 5223 (0) | 5333 (60 (95% CI 10, 170)) | N/A | N/A |
| Quintana et al. 2016 [58] | 0 | 90 (95% CI 2–500) | N/A | N/A |
| Gheita et al. 2021 [57] | 365 (1.2) | 3296 (11.3) | N/A | N/A |
N/A Not available
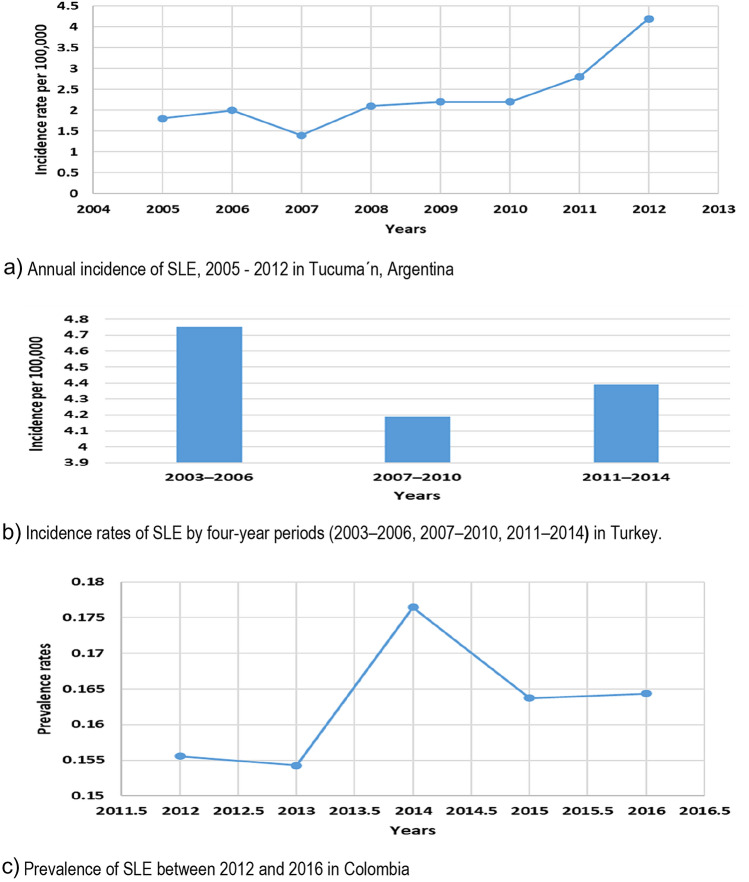
Three studies were identified that examined the prevalence and incidence of people with SLE over time, allowing us to examine its temporal trend in Argentina [47], Turkey [37] and Colombia [38] (Fig. 4). The incidence of SLE in Argentina showed a substantial increase over the period of 8 years, the annual incidence in 2005 was 1.8 cases/100.000 inhabitants (95% CI 1–2.9) and in 2012 of 4.2 cases/100.000 inhabitants (95% CI 2.9–5.8). In Turkey [37], the annual incidence between the period of 2003–2006 (4.75 per 100,000 persons) were higher than 2011–2014 (4.39 cases per 100,000 persons). Number of patients with SLE also showed increment in Colombia from 15,556 to 16,437 per 100,000 persons for 2012 and 2016, respectively.
Fig. 4.
Incidence and prevalence of SLE stratified by years
Discussion
To our knowledge, this is the first review to evaluate and synthesise the incidence and prevalence data for SLE across the WHO regions of LMICs. This review represents a published data of prevalence and incidence of SLE from Argentina, China, Cuba, Colombia, Democratic Republic Congo, India, Kenya, Malaysia, Mexico, Nigeria, Pakistan, Turkey, Ukraine, Venezuela, and Zimbabwe. The prevalence and incidence of SLE ranged from 3.2 to 3000 per 100,000 and 0.3 to 8.7 per 100,000 persons, respectively. The highest estimates of incidence and prevalence of SLE were in Brazil [8.7(95% CI 6.3–11.7)/100 000 persons and in Kenya 3000 [95% 1800–5600]/100 000 persons, respectively. The lowest incidences of SLE were reported in Ukraine (0.3 (95% CI 0.0–1.8)/100 000 people, and the lowest prevalence was in India 3.2 (95% CI 0–6.86)/100,000 persons. Compared to high income countries, a lower prevalence of SLE is reported in LMICs. A systematic review on the incidence and prevalence of SLE reported that people in the in the United States of America (USA) 241/100 000 have much lower prevalence than people in Kenya 3000/100,000 [31]. On the other hand, evidence suggested that the highest incidence of SLE is reported in the USA (23.2/100 000 person-years) compared to Africa [1].
However, the results of the current review indicated that SLE is common in LMICs and the variation is considerably high across these countries. This variation is attributable to a variety of factors including the definition of SLE applied, ethnic and geographic differences in the populations being studied, access to health care, environmental (infections and ultraviolet light) and the methods of case identification [6, 59]. The incidence of SLE in Ukraine and Zimbabwe was the lowest compared to other countries in LMICs, this may be due to methodological differences used to collect the data. For example, the data sources and the skills used to identify SLE cases in Zimbabwe were inadequate, this is due to the data collected were relied upon hospital admission of one study hospital, and the low life expectancy of patients. On the other hand, the high prevalence estimate of SLE was reported in the Kenya, Nigeria, Colombia and Mexico, this may be because of an unadjusted rate in the population at risk.
Although the ratio varies, the prevalence and incidence estimate of SLE is more common in women than men. This may be due to oestrogen, a stimulant of lymphocytes, where women continue to have the higher oestrogen activity [60]. Moreover, clear differences in women and men immunity may also contribute to variation in response to predisposition of SLE [61, 62]. Most of the included studies in the current review reported a substantial difference of the prevalence and incidence of men and women. One study reported a prevalence rate of females (204) and male (20.3) per 100,000 persons [38]. The Incidence rate comparison between sexes also indicated this phenomenon, with one study contributing to the considerable variations of people with SLE in females compared to males [46].
Some studies that analysed the difference of occurrence of SLE among various ethnic groups in our review reported that black people to have high prevalence and incidence of SLE than white people [36, 46, 49]. It is also important to point out that there are studies that reported low incidence of SLE in black African population [43, 44]. The variation in the epidemiology of SLE is associated not only with genetic but also with environmental, sociodemographic, and sociocultural factors [61].
There are some strengths and limitations to be considered when interpreting the findings of this review. When identifying the relevant studies on prevalence and incidence of SLE, a systematic and rigorous approach was adopted. The adoption of different methodologies such as case identification method and analytical issues within the included studies have made it difficult to assess the epidemiological trend over time. Although an extensive literature search was carried out, we did not search for papers published in languages other than English, this could have influenced the incidence and prevalence estimates of SLE in LMICs. Due to the lack of financial resources and an inadequate health professional workforce, rheumatology services are limited or non-existent in many parts of Southeast Asia and sub-Saharan Africa [62, 63]. These may have resulted patients to a less likely to be diagnosed with SLE. The clinical and policy implications of this review is related with the female population who are at risk of SLE, it may help in the allocation of healthcare resources as well as priority for research funding. Moreover, the lack of epidemiological studies of SLE in Africa requires attention from researchers, and clinical and policy makers to understand its burden with the hope of improving the health outcomes of people with SLE in LMICs.
Conclusions
Systemic lupus erythematosus is a common condition with considerable variation in prevalence and incidence among the general population in LMICs. The findings also suggested that the incidence and prevalence of SLE is higher in females compared with males. Furthermore, the trend of prevalence of SLE is increasing with time. The same to other public health problems, it is crucial for policy makers to intervene in the prevention and management of SLE. Furthermore, urgent need of research in terms of estimating its direct and indirect costs and impaired health related quality of life due to the condition is necessary in LMICs settings.
Author contributions
FF, TG and CM have contributed equally to this paper. All authors had conceived, designed, analysed the data, and interpreted the results of the work. All co-authors take full responsibility for the accuracy and integrity of all aspects of the work. All authors approved the final version of this manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Competing interests
The authors have no competing interests to declare.
Ethical approval
The study is a systematic review. For this study ethical approval was not required. Note: Abstract for this study has already been published previously https://www.sciencedirect.com/science/article/pii/S109830152101367X.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology. 2017;56(11):1945–1961. doi: 10.1093/rheumatology/kex260. [DOI] [PubMed] [Google Scholar]
- 2.Fava A, Petri M. Systemic lupus erythematosus: diagnosis and clinical management. J Autoimmun. 2019;96:1–13. doi: 10.1016/j.jaut.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blomberg J, Nived O, Pipkorn R, Bengtsson A, Erlinge D, Sturfelt G. Increased antiretroviral antibody reactivity in sera from a defined population of patients with systemic lupus erythematosus. Arthritis & Rheum: Off J Am Coll Rheumatol. 1994;37(1):57–66. doi: 10.1002/art.1780370109. [DOI] [PubMed] [Google Scholar]
- 4.Tsokos GC, Lo MS, Reis PC, Sullivan KE. New insights into the immunopathogenesis of systemic lupus erythematosus. Nat Rev Rheumatol. 2016;12(12):716–730. doi: 10.1038/nrrheum.2016.186. [DOI] [PubMed] [Google Scholar]
- 5.Generali E, Ceribelli A, Stazi MA, Selmi C. Lessons learned from twins in autoimmune and chronic inflammatory diseases. J Autoimmun. 2017;83:51–61. doi: 10.1016/j.jaut.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Carter EE, Barr SG, Clarke AE. The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol. 2016;12(10):605–620. doi: 10.1038/nrrheum.2016.137. [DOI] [PubMed] [Google Scholar]
- 7.Yen EY, Singh RR. Brief report: lupus—an unrecognized leading cause of death in young females: a population-based study using nationwide death certificates, 2000–2015. Arthritis Rheumatol. 2018;70(8):1251–1255. doi: 10.1002/art.40512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee YH, Choi SJ, Ji JD, Song GG. Overall and cause-specific mortality in systemic lupus erythematosus: an updated meta-analysis. Lupus. 2016;25(7):727–734. doi: 10.1177/0961203315627202. [DOI] [PubMed] [Google Scholar]
- 9.Symmons DPM. Occasional series: lupus around the world frequency of lupus in people of African origin. Lupus. 1995;4(3):176–178. doi: 10.1177/096120339500400303. [DOI] [PubMed] [Google Scholar]
- 10.Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39(4):257–268. doi: 10.1016/j.semarthrit.2008.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danchenko N, Satia JA, Anthony MS. Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus. 2006;15(5):308–318. doi: 10.1191/0961203306lu2305xx. [DOI] [PubMed] [Google Scholar]
- 12.Ferucci ED, Johnston JM, Gaddy JR, Sumner L, Posever JO, Choromanski TL, Helmick CG. Prevalence and incidence of systemic lupus erythematosus in a population-based registry of American Indian and Alaska Native people, 2007–2009. Arthritis Rheumatol. 2014;66(9):2494–2502. doi: 10.1002/art.38720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krishnan E, Hubert HB. Ethnicity and mortality from systemic lupus erythematosus in the US. Ann Rheum Dis. 2006;65(11):1500–1505. doi: 10.1136/ard.2005.040907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petri M, Robinson C. Oral contraceptives and systemic lupus erythematosus. Arthritis Rheum. 1997;40(5):797–803. doi: 10.1002/art.1780400504. [DOI] [PubMed] [Google Scholar]
- 15.González LA, Toloza SMA, McGwin G, Jr, Alarcón GS. Ethnicity in systemic lupus erythematosus (SLE): its influence on susceptibility and outcomes. Lupus. 2013;22(12):1214–1224. doi: 10.1177/0961203313502571. [DOI] [PubMed] [Google Scholar]
- 16.Lerang K, Gilboe I, Garen T, Thelle DS, Gran JT. High incidence and prevalence of systemic lupus erythematosus in Norway. Lupus. 2012;21(12):1362–1369. doi: 10.1177/0961203312458168. [DOI] [PubMed] [Google Scholar]
- 17.Barber MR, Drenkard C, Falasinnu T, Hoi A, Mak A, Kow NY, Ramsey-Goldman R. Publisher correction: global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol. 2021;17(10):642. doi: 10.1038/s41584-021-00690-3. [DOI] [PubMed] [Google Scholar]
- 18.Jakes RW, Bae SC, Louthrenoo W, Mok CC, Navarra SV, Kwon N. Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: prevalence, incidence, clinical features, and mortality. Arthritis Care Res. 2012;64(2):159–168. doi: 10.1002/acr.20683. [DOI] [PubMed] [Google Scholar]
- 19.Bertsias G, Karampli E, Sidiropoulos P, Gergianaki I, Drosos A, Sakkas L, Boumpas D. Clinical and financial burden of active lupus in Greece: a nationwide study. Lupus. 2016;25(12):1385–1394. doi: 10.1177/0961203316642310. [DOI] [PubMed] [Google Scholar]
- 20.Campbell R, Jr, Cooper GS, Gilkeson GS. Two aspects of the clinical and humanistic burden of systemic lupus erythematosus: mortality risk and quality of life early in the course of disease. Arthritis Care Res. 2008;59(4):458–464. doi: 10.1002/art.23539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Essouma M, Nkeck JR, Endomba FT, Bigna JJ, Ralandison S. Epidemiology of rheumatoid arthritis in sub-Saharan Africa: a systematic review and meta-analysis protocol. Syst Rev. 2020;9(1):1–4. doi: 10.1186/s13643-020-01342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li S, Gong T, Peng Y, Nieman KM, Gilbertson DT. Prevalence and incidence of systemic lupus erythematosus and associated outcomes in the 2009–2016 US Medicare population. Lupus. 2020;29(1):15–26. doi: 10.1177/0961203319888691. [DOI] [PubMed] [Google Scholar]
- 23.McMurray RW, May W. Sex hormones and systemic lupus erythematosus: review and meta-analysis. Arthritis Rheum: Off J Am Coll Rheumatol. 2003;48(8):2100–2110. doi: 10.1002/art.11105. [DOI] [PubMed] [Google Scholar]
- 24.Dave M, Rankin J, Pearce M, Foster HE. Global prevalence estimates of three chronic musculoskeletal conditions: club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol. 2020;18(1):1–7. doi: 10.1186/s12969-020-00443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewandowski LB, Schanberg LE, Thielman N, Phuti A, Kalla AA, Okpechi I, Scott C. Severe disease presentation and poor outcomes among pediatric systemic lupus erythematosus patients in South Africa. Lupus. 2017;26(2):186–194. doi: 10.1177/0961203316660625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aggarwal A, Phatak S, Srivastava P, Lawrence A, Agarwal V, Misra R. Outcomes in juvenile onset lupus: single center cohort from a developing country. Lupus. 2018;27(11):1867–1875. doi: 10.1177/0961203318791046. [DOI] [PubMed] [Google Scholar]
- 27.Fessel WJ. Systemic lupus erythematosus in the community: incidence, prevalence, outcome, and first symptoms; the high prevalence in black women. Arch Intern Med. 1974;134(6):1027–1035. [PubMed] [Google Scholar]
- 28.Tikly M, Navarra SV. Lupus in the developing world–is it any different? Best Pract Res Clin Rheumatol. 2008;22(4):643–655. doi: 10.1016/j.berh.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Mody GM. Rheumatology in Africa—challenges and opportunities. Arthritis Res Ther. 2019;219(1):1–3. doi: 10.1186/s13075-017-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Magro R, Borg AA. Characterisation of patients with systemic lupus erythematosus in Malta: a population based cohort cross-sectional study. BioMed Res Int. 2018;2018:1–7. doi: 10.1155/2018/2385386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 32.Tan EM, Cohen AS, Fries JF, Masi AT, Mcshane DJ, Rothfield NF, Winchester RJ. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum: Off J Am Coll Rheumatol. 1982;25(11):1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 33.Hochberg MC. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725–1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 34.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Borenstein M, Rothstein H, Cohen J (1999) Comprehensive meta-analysis: a computer program for research synthesis
- 36.Gonzalez Lucero L, Barbaglia AL, Bellomio VI, Bertolaccini MC, Machado Escobar MA, Sueldo HR, Lucero E. Prevalence and incidence of systemic lupus erythematosus in Tucumán. Argent Lupus. 2020;29(13):1815–1820. doi: 10.1177/0961203320957719. [DOI] [PubMed] [Google Scholar]
- 37.Pamuk ON, Balci MA, Donmez S, Tsokos GC. The incidence and prevalence of systemic lupus erythematosus in Thrace, 2003–2014: a 12-year epidemiological study. Lupus. 2016;25(1):102–109. doi: 10.1177/0961203315603141. [DOI] [PubMed] [Google Scholar]
- 38.Fernández-Ávila DG, Bernal-Macías S, Rincón-Riaño DN, Gutiérrez Dávila JM, Rosselli D. Prevalence of systemic lupus erythematosus in Colombia: data from the national health registry 2012–2016. Lupus. 2019;28(10):1273–1278. doi: 10.1177/0961203319864168. [DOI] [PubMed] [Google Scholar]
- 39.Zou YF, Feng CC, Zhu JM, Tao JH, Chen GM, Ye QL, Ye DQ. Prevalence of systemic lupus erythematosus and risk factors in rural areas of Anhui Province. Rheumatol Int. 2014;34(3):347–356. doi: 10.1007/s00296-013-2902-1. [DOI] [PubMed] [Google Scholar]
- 40.Ekwom PE. Systemic lupus erythematosus (SLE) at the Kenyatta national hospital. Clin Rheumatol. 2013;32(8):1215–1217. doi: 10.1007/s10067-013-2217-3. [DOI] [PubMed] [Google Scholar]
- 41.Gbané-Koné M, Ouattara B, Djaha KJM, Megne E, Ngandeu AN, Coulibaly AK, Kouakou MNZ. Autoantibodies in systemic lupus erythematosus, on Black African subject, in Abidjan. Open J Rheumatol Autoimmune Dis. 2015;5(02):28. [Google Scholar]
- 42.Wang F, Wang CL, Tan CT, Manivasagar M. Systemic lupus erythematosus in Malaysia: a study of 539 patients and comparison of prevalence and disease expression in different racial and gender groups. Lupus. 1997;6(3):248–253. doi: 10.1177/096120339700600306. [DOI] [PubMed] [Google Scholar]
- 43.Farooqi A, Gibson T. Prevalence of the major rheumatic disorders in the adult population of north Pakistan. Br J Rheumatol. 1998;37(5):491–495. doi: 10.1093/rheumatology/37.5.491. [DOI] [PubMed] [Google Scholar]
- 44.Taylor HG, Stein CM. Systemic lupus erythematosus in Zimbabwe. Ann Rheum Dis. 1986;45(8):645–648. doi: 10.1136/ard.45.8.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakashima CAK, Galhardo AP, Silva JFMD, Fiorenzano GR, Santos ABDSD, Leite MFS, Menolli RA. Incidence and clinical-laboratory aspects of systemic lupus erythematosus in a Southern Brazilian city. Rev Bras Reumatol. 2011;51:235–239. [PubMed] [Google Scholar]
- 46.Vilar MP, Sato EI. Estimating the incidence of systemic lupus erythematosus in a tropical region (Natal, Brazil) Lupus. 2002;11(8):528–532. doi: 10.1191/0961203302lu244xx. [DOI] [PubMed] [Google Scholar]
- 47.Scolnik M, Marin J, Valeiras SM, Marchese MF, Talani AS, Avellaneda NL, Soriano ER. Incidence and prevalence of lupus in Buenos Aires, Argentina: a 11-year health management organisation-based study. Lupus Sci Med. 2014;1(1):e000021. doi: 10.1136/lupus-2014-000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nasonov E, Soloviev S, Davidson JE, Lila A, Ivanova R, Togizbayev G, Pereira MHS. The prevalence and incidence of systemic lupus erythematosus (SLE) in selected cities from three commonwealth of independent states countries (the Russian Federation, Ukraine and Kazakhstan) Lupus. 2014;23(2):213–219. doi: 10.1177/0961203313512881. [DOI] [PubMed] [Google Scholar]
- 49.Senna ER, De Barros ALP, Silva EO, Costa IF, Pereira LVB, Ciconelli RM, Ferraz MB. Prevalence of rheumatic diseases in Brazil: a study using the COPCORD approach. J Rheumatol. 2004;31(3):594–597. [PubMed] [Google Scholar]
- 50.Granados Y, Cedeño L, Rosillo C, Berbin S, Azocar M, Molina ME, Peláez-Ballestas I. Prevalence of musculoskeletal disorders and rheumatic diseases in an urban community in Monagas State, Venezuela: a COPCORD study. Clin Rheumatol. 2015;34(5):871–877. doi: 10.1007/s10067-014-2689-9. [DOI] [PubMed] [Google Scholar]
- 51.Peláez-Ballestas I, Sanin LH, Moreno-Montoya J, Alvarez-Nemegyei J, Burgos-Vargas R, Garza-Elizondo M, Cardiel MH. Epidemiology of the rheumatic diseases in Mexico. a study of 5 regions based on the COPCORD methodology. J Rheumatol Suppl. 2011;86:3–8. doi: 10.3899/jrheum.100951. [DOI] [PubMed] [Google Scholar]
- 52.Li R, Sun J, Ren LM, Wang HY, Liu WH, Zhang XW, Li ZG. Epidemiology of eight common rheumatic diseases in China: a large-scale cross-sectional survey in Beijing. Rheumatology. 2012;51(4):721–729. doi: 10.1093/rheumatology/ker370. [DOI] [PubMed] [Google Scholar]
- 53.Malaviya AN, Singh RR, Singh YN, Kapoor SK, Kumar A. Prevalence of systemic lupus erythematosus in India. Lupus. 1993;2(2):115–118. doi: 10.1177/096120339300200209. [DOI] [PubMed] [Google Scholar]
- 54.Malemba JJ, Mbuyi-Muamba JM. Clinical and epidemiological features of rheumatic diseases in patients attending the university hospital in Kinshasa. Clin Rheumatol. 2008;27(1):47–54. doi: 10.1007/s10067-007-0650-x. [DOI] [PubMed] [Google Scholar]
- 55.Guevara-Pacheco S, Feicán-Alvarado A, Sanín LH, Vintimilla-Ugalde J, Vintimilla-Moscoso F, Delgado-Pauta J, Peláez-Ballestas I. Prevalence of musculoskeletal disorders and rheumatic diseases in Cuenca, Ecuador: a WHO-ILAR COPCORD study. Rheumatol Int. 2016;36(9):1195–1204. doi: 10.1007/s00296-016-3446-y. [DOI] [PubMed] [Google Scholar]
- 56.Reyes-Llerena GA, Guibert-Toledano M, Penedo-Coello A, Pérez-Rodríguez A, Baez-Dueñas RM, Charnicharo-Vidal R, Cardiel MH. Community-based study to estimate prevalence and burden of illness of rheumatic diseases in Cuba: a COPCORD study. JCR: J Clin Rheumatol. 2009;15(2):51–55. doi: 10.1097/RHU.0b013e31819b61cb. [DOI] [PubMed] [Google Scholar]
- 57.Gheita TA, Noor RA, Abualfadl E, Abousehly OS, El-Gazzar II, El Shereef RR, Raafat HA. Adult systemic lupus erythematosus in Egypt: the nation-wide spectrum of 3661 patients and world-wide standpoint. Lupus. 2021;30(9):1526–1535. doi: 10.1177/09612033211014253. [DOI] [PubMed] [Google Scholar]
- 58.Quintana R, Silvestre AM, Goñi M, García V, Mathern N, Jorfen M, Pons-Estel BA. Prevalence of musculoskeletal disorders and rheumatic diseases in the indigenous Qom population of Rosario. Argent Clin Rheumatol. 2016;35(1):5–14. doi: 10.1007/s10067-016-3192-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcón GS, Costenbader KH. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000–2004. Arthritis Rheum. 2013;65(3):753–763. doi: 10.1002/art.37795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tiffin N, Adeyemo A, Okpechi I. A diverse array of genetic factors contribute to the pathogenesis of systemic lupus erythematosus. Orphanet J Rare Dis. 2013;8(1):1–8. doi: 10.1186/1750-1172-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Borchers AT, Naguwa SM, Shoenfeld Y, Gershwin ME. The geoepidemiology of systemic lupus erythematosus. Autoimmun Rev. 2010;9(5):A277–A287. doi: 10.1016/j.autrev.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 62.Pineles D, Valente A, Warren B, Peterson MGE, Lehman TJA, Moorthy LN. Worldwide incidence and prevalence of pediatric onset systemic lupus erythematosus. Lupus. 2011;20(11):1187–1192. doi: 10.1177/0961203311412096. [DOI] [PubMed] [Google Scholar]
- 63.Webb K, Peckham H, Radziszewska A, Menon M, Oliveri P, Simpson F, Ioannou Y. Sex and pubertal differences in the type 1 interferon pathway associate with both X chromosome number and serum sex hormone concentration. Front Immunol. 2019;9:3167. doi: 10.3389/fimmu.2018.03167. [DOI] [PMC free article] [PubMed] [Google Scholar]