Abstract
Medial knee injuries are prevalent, especially in young athletes. A detailed history and physical examination are needed to accurately diagnose injuries to the superficial medial collateral ligament (sMCL), deep medial collateral ligament (dMCL), and posterior oblique ligament (POL). The mechanism of medial knee injury often involves a coupled valgus and external rotation force with pain and tenderness across the medial joint line. Valgus stress radiographs assist with the diagnosis of medial knee injuries based on the quantitative extent of medial joint gapping. Specifically, 3.2 mm of increased medial gapping is observed with an isolated grade-III sMCL injury and greater than 9.8 mm of gapping indicates a complete medial knee injury. Nonoperative treatment is recommended for grade-I and II medial knee injuries. Patients with chronic medial knee instability, or a complete tear of the medial knee structures, may require operative treatment. Anatomic surgical techniques have proven to be highly effective in restoring functional knee stability.
Key Words: Anterior cruciate, Medial collateral ligament, Posterior cruciate
Introduction
Injury to the medial collateral ligament (MCL) and additional structures that comprise the posteromedial corner of the knee (PMC) are prevalent and usually involve a valgus force combined with external rotation of the tibia. The main static stabilizers of the PMC are the superficial medial collateral ligament (sMCL), deep medial collateral ligament (dMCL), and the posterior oblique ligament (POL). Historically, the sMCL was considered the primary stabilizer of the medial knee. However, recent studies have elucidated the critical roles of the dMCL and the POL in stabilizing the medial knee. These principles have paved the way for anatomically oriented reconstruction techniques which have resulted in improved measures of knee stability and functionality following PMC reconstruction. The objective of this article is to discuss the most recent concepts related to the surgically pertinent treatment of injuries to the PMC.
Surgically Relevant Anatomy
Superficial Medial Collateral Ligament
The sMCL has two tibial attachments and a single femoral attachment. The femoral attachment is rotund and located in an osseous depression 3.2 mm proximal to the medial epicondyle and 4.8 mm posterior. 1,2 The sMCL connects directly to soft tissues on the anterior arm of the semimembranosus tendon, 1.2 distal to the proximal joint line. 1,3 This attachment site is wide and is positioned distal to the meniscotibial ligament and anterior to the tibia’s posteromedial crest. The distal tibial attachment of the sMCL is encompassed by the floor of the pes anserine bursa, which itself has a direct osseous attachment to the tibia. 1,2 On average, the center of this attachment point is 6 cm distal to the medial joint line. 1,2,4
Deep Medial Collateral Ligament
The dMCL originates on the femur, approximately 1.3 cm distal to the femoral sMCL attachment.2,5 The dMCL runs deep to the sMCL and extends distal to the tibial articular margin, firmly attaching to the medial meniscus to form individual meniscofemoral and meniscotibial aspects [Figure 1].6 On average, the meniscotibial component attaches to the tibia 3.2 mm distal to the tibial joint line.2 This aspect is shorter and thicker compared to the meniscofemoral aspect, which attaches to the femur 15.7 mm proximal to the femoral joint line.1,2 The meniscofemoral aspect of the dMCL attaches to the tibia 12.6 mm distal to the proximal sMCL attachment. The meniscotibial portion attaches 9.0 mm proximal to the proximal sMCL attachment.4
Figure 1.
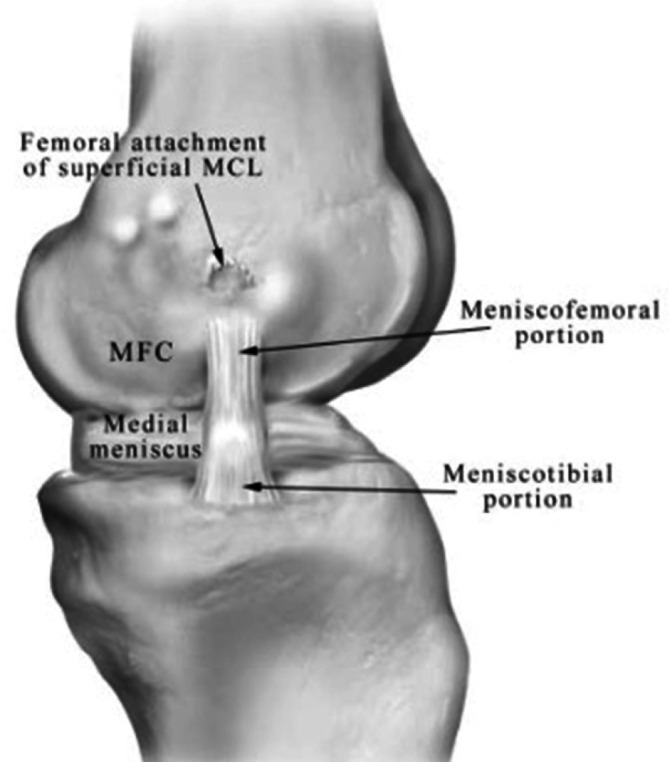
Medial view illustrates the meniscofemoral and meniscotibial components of the dMCL (left knee). The dMCL attaches to the medial meniscus slightly distal to the tibial articular margin. dMCL, deep medial collateral ligament; MFC, medial femoral condyle, MCL, medial collateral ligament.14
Posterior Oblique Ligament
Originating from the distal end of the semimembranosus tendon, the posterior oblique ligament (POL) reinforces the posteromedial component of the joint capsule. The POL is comprised of three distinct fascial arms: a superficial, central (tibial), and capsular arm. The superficial arm of the POL runs medial to the semimembranosus tendon’s anterior arm and alongside the posterior aspect of the sMCL.4 The central arm is the thickest portion of the POL and originates from the primary semimembranosus tendon, spreading out in a posterolateral fashion. This characteristic may be used to differentiate the POL from the sMCL. As it courses towards the tibia, the central arm merges with the posteromedial aspect of the medial meniscus and firmly adheres to the tibia at the posterior articular surface. 7 The central arm merges with the superficial arm to form a shared femoral attachment, 7.7 mm distal to the adductor tubercle and 6.4 mm posterior. This common femoral attachment is also 1.4 mm distal to the gastrocnemius tubercle and 2.9 mm anterior. 1 LaPrade et al. proposed that anatomic-based POL reconstruction should reproduce the native orientation and attachments of the central arm. 8
Biomechanics
Superficial MCL
The sMCL represents the main restraint to valgus knee laxity. 9 Recent studies have revealed that the sMCL is functionally comprised of proximal and distal components, each with distinct properties essential for knee kinematics and stability. 10,11 Surgical sMCL treatment must anatomically restore the discrete functions of the proximal and distal components.
The proximal component of the sMCL is the principal static stabilizer of valgus movement for all angles of knee flexion. 2 The distal component of the sMCL is the principal restraint against external rotation at 30° of knee flexion and the main static stabilizer to resist internal rotation at all degrees of knee flexion. 2,10 When severe injury to the sMCL components occurs, the main objective should be to reconstruct the native anatomy such that the distinct biomechanical functions of the sMCL proximal and distal components is restored.12
The sMCL provides knee stability in conjunction with the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). Chronic valgus instability due to sMCL injury disrupts the load-sharing equilibrium of the knee and aberrantly intensifies the loads on the ACL and PCL.13
The sMCL and POL function in concert to resist internal rotation of the knee. When a sMCL injury occurs, the load response on the POL is abnormally increased, suggesting a codependent relationship with the sMCL. The POL should be anatomically reconstructed concurrently with the sMCL in cases of severe sMCL injury. 8,14
Posterior Oblique Ligament
The POL primarily functions to protect the knee against abnormal internal rotation for all degrees of knee flexion, a function complementary to the sMCL.2 The POL also serves as a secondary stabilizer for valgus and external rotation.5,10,15
Deep Medial Collateral Ligament
The dMCL has the lowest values for stiffness and load-at-failure of the medial knee structures and primarily functions to restrain the knee against abnormal valgus movement. 12 The meniscofemoral component of the dMCL provides this function for all degrees of knee flexion, whereas the meniscotibial component primarily resists valgus motion at 60° of knee flexion [Figure 3]. 9,14 A study by LaPrade et al. found that ligament tears of the dMCL meniscofemoral and meniscotibial components occur more frequently than injures of the dMCL intrasubstance. 16
Figure 3.
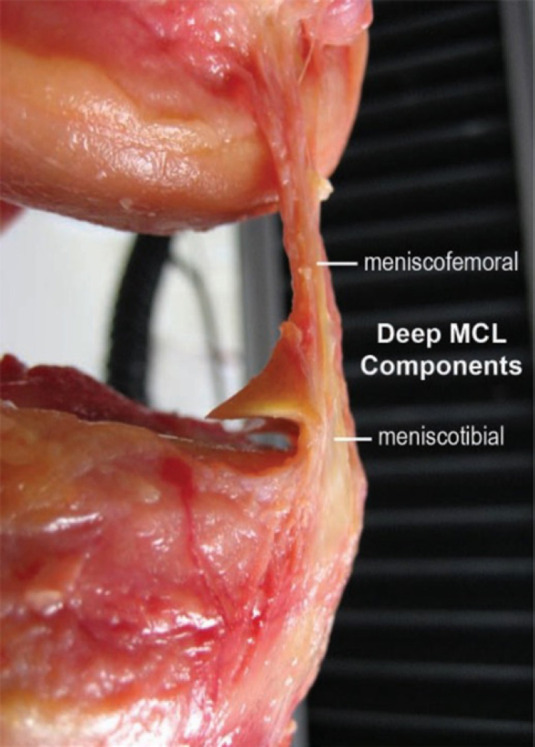
Photograph of a right knee illustrating the meniscofemoral and meniscotibial components of the deep medial collateral ligament (dMCL)
Clinical Evaluation
Clinical evaluation of the knee is an essential step in identifying the specific location and extent of a knee injury. However, factors such as pain, swelling, and polytrauma may limit the effectiveness of the clinical assessment. Due to the variability of presentation, radiographic evaluation is widely regarded as a useful, objective supplement to the clinical assessment of MCL injuries. 2,9,17
To assess the degree of medial knee injury, the valgus stress test is performed at both full extension and with the knee flexed at 30°. It is essential to assess for the presence of a firm valgus endpoint. If an endpoint is not detected with an applied valgus load, it is likely that the PMC structures are completely ruptured, requiring the ACL to secondarily function as a valgus restraint. 9,17 As a result, the Lachman and pivot shift tests should be used to assess ACL integrity in the setting of medial knee injury. 9
The valgus stress test is first performed at 30° of flexion. Subjective gapping of 3-5 mm of the medial compartment indicates an isolated sMCL injury and 5-7 mm of gapping indicates additional ligamentous injury to the dMCL and POL [Figure 4]. Greater than 7 mm of medial compartment laxity signals the involvement of an ACL injury. 18
Figure 4.

Valgus stress examination in a left knee performed at 30° of knee flexion by cradling the leg to assess for subjective medial joint gapping
Next, the valgus stress test is performed with the knee in full extension, allowing the clinician to determine the presence of a concomitant knee injury. 17 For an isolated MCL injury, little-to-no laxity is typically present when a valgus stress is applied to a knee at full extension. A grade-III MCL injury corresponds to 1-2 mm of increased medial compartment gapping at full extension compared to the uninjured knee. 17 However, in the case of a complete MCL complex injury or a combined MCL and ACL injury, greater than 2 mm of medial compartment gapping is observed when valgus stress is placed on the knee in full extension. 18
It is important to assess the degree of an sMCL injury and determine the involvement of additional PMC structures. Increased valgus gapping at 30° of flexion, but not in full knee extension, indicates an intact POL. 9 The anteromedial drawer test is performed if injury to the POL is suspected, assessing for the extent of anteromedial tibial rotation compared to the uninjured knee.9,17,18
Previous studies have reported that the dial test can identify the presence of a complete injury to the medial structures. 9,10 Performed at 30° and 90° of knee flexion, a positive dial test is observed with excessive external rotation of the tibia.
Radiographic Evaluation
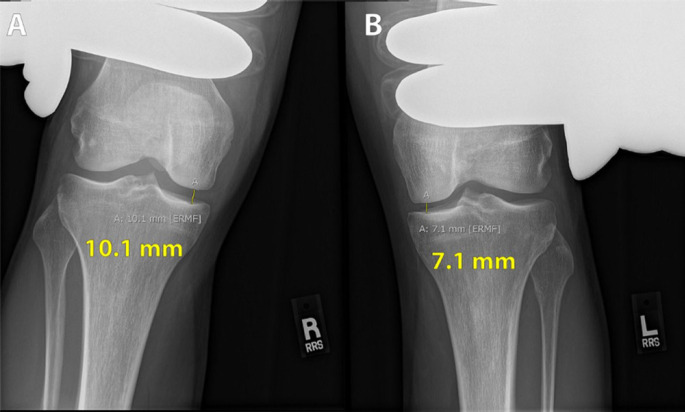
Stress radiography is an invaluable asset for the management of medial knee injuries [Figure 5]. Valgus stress radiographs are a reliable, accessible, and quantifiable method for evaluating medial compartment gapping, especially when complemented with a history of injury and detailed clinical assessment. 16,17 However, pain, immobility, and the degree of muscular relaxation may decrease the practicality of stress radiography.16,19,20
Figure 5.
Valgus stress radiographs depict a 3.0 mm difference in medial compartment gapping between the right knee (A) and the left knee (B). LaPrade et al. reported that greater than 3.2 mm of side-to-side medial compartment gapping is required to diagnose a grade-III MCL tear.16 MCL, medial collateral ligament
The utility of radiographs has increased over the past few years due to the adoption of anatomic-based PMC reconstructions. 21 In a cadaveric model, Wijdicks et al. concluded that standard radiographs were consistently and accurately able to assess the attachment points of medial knee structures to well-established osseous landmarks. 3
Valgus stress radiographs are used to quantitatively grade the extent of a medial knee injury. Isolated grade-III sMCL injury results in enhanced medial compartment gapping of 1.7 mm and 3.2 mm, respectively, at 0° and 20° of knee flexion. 16 Furthermore, complete medial knee tears were associated with 6.5 mm and 9.8 mm of medial compartment gapping at 0° and 20° of knee flexion, respectively. 16,17
Magnetic resonance imaging (MRI) is another useful modality for the evaluation of PMC injury [Figure 6]. In a study of sixty-three patients, Yao et al. reported that MRI had a diagnostic accuracy of 87%.9,22 The MRI coronal plane is optimal for precise evaluation of the medial structures of the knee and it has been suggested that T-2 weighted imaging provides superior visualization of focal injury. 18,22 The extent of subcutaneous edema, striation, hyperintensity, and discontinuity are all relevant to grading MCL injury. 18,22 The MRI is most useful in acute cases to precisely identify injury to the individual ligamentous structures of the PMC.
Figure 6.

T2 Weighted Fat Saturation MRI illustrates a coronal view of a proximal avulsion tear of the sMCL in a multiligament injured knee. MRI, magnetic resonance imaging; sMCL, superficial medial collateral ligament (left knee)
Subjective and Objective Classification of PMC Injuries
The American Medical Association (AMA) provides a standardized guide to classify medial knee injuries as grade-I, grade-II, or grade-III, based on the amount of localized tenderness and subjective medial compartment laxity compared to the uninjured knee. 23 Accurate grading of medial knee injuries highly depends on the detection of a firm endpoint on physical exam and the pain tolerance of the patient. 5,9
Unlike higher-grade injuries, grade-I tears typically present without knee instability. A grade-I tear is consistent with 0 to 5 mm increased medial compartment gapping compared to the contralateral knee. 9 Grade-II tears present with 6 to 10 mm of increased medial compartment gapping due to partially torn MCL and POL fibers. Isolated grade-III MCL injuries involve a complete tear of the medial knee ligaments and present with a minimum of 10 mm of medial compartment gapping. 9 It is important to recognize that subjective laxity correlated with the AMA classification overestimates the true extent of objective medial knee gapping that is observed on stress radiographs. The grade of the knee injury predicts both the healing capability and the necessity of surgical management.
Treatment
Nonoperative treatment
The MCL has significant potential to heal, unlike other ligamentous structures of the knee. In addition, surgical treatment is not always required for isolated complete medial knee tears. 2,9,12 The profuse vascular supply to the MCL facilitates healing through a standard mechanism of inflammation, repair, and remodeling. 9,24
The capacity of the MCL to heal is not uniform. It is well reported that meniscotibial (distal sMCL) tears have a worse healing rate than meniscofemoral tears. 16 Cinque et al. proposed that the sMCL tibial fixation on the interposed pes anserine, rather than directly on the osseous surface, results in poor vascularity and decreased healing potential. 5
Nonoperative treatment is generally recommended for grade-I and II MCL injuries. 18,25 Lundberg and Messner observed that 92% of patients with partial MCL injury experienced a return to normal knee function. However, in the injured knee, preliminary osteoarthritic changes were observed in some imaging studies ten years after the injury. 18,26 Partial MCL injury treatment should emphasize early and controlled postoperative range of motion exercises starting on day one, along with protective weight-bearing to lower the risk of joint stiffness and arthrofibrosis. 27
The optimal treatment of grade-III MCL injuries has attracted significant controversy in the literature. Several studies have reported positive outcomes associated with nonsurgical management of grade III MCL injuries.28-31 Hence, nonoperative management is typically the first line treatment for most isolated and acute grade-III MCL injuries, after careful exclusion of concomitant injuries that may require operative management. 18 For acute grade-III MCL injuries, current management favors an early range of motion through a functional rehabilitation program. The knee should be effectively stabilized to minimize the degree of external rotation and valgus stress. Although there is no current consensus in the literature about the effectiveness of a hinged brace following grade III MCL complex injury, the present researchers recommend a hinged knee brace to protect the healing MCL fibers so that it does not heal in an attenuated position. 5
Grade-III MCL nonoperative treatment may result in residual knee instability that jeopardizes other knee ligaments. A study that compared grade-II and grade-III MCL complex injuries found that a significant majority of patients with grade-III injuries experienced residual laxity and had evidence of osteoarthritic changes. 32 Successful nonoperative treatment of complete grade-III MCL injuries highly depends on an intact ACL. 17 For a combined grade-III MCL injury and ACL tear, to prevent ACL graft failure, it is essential that the MCL heals completely for 5–7 weeks before ACL reconstruction is completed. 17,33
Operative Treatment
Operative treatment is often performed on patients with multiligament knee injury involving high-grade tears to the PMC or patients with subacute or chronic valgus instability who have failed to improve through nonoperative management. 17,34 Combined PCL and MCL tears almost always require surgical treatment to correct the significant medial knee laxity commonly observed. 17 In addition, reconstruction for combined ACL/PCL/MCL injury is recommended because delaying treatment (greater than three weeks) may result in persistent medial knee laxity that is resistant to surgical correction. 18,35 Other injuries can require surgical restoration of the normal anatomy to facilitate healing. For example, the sMCL may be situated externally to the pes anserine tendons or may become entrapped in the medial knee joint, preventing reattachment to the tibia. 18
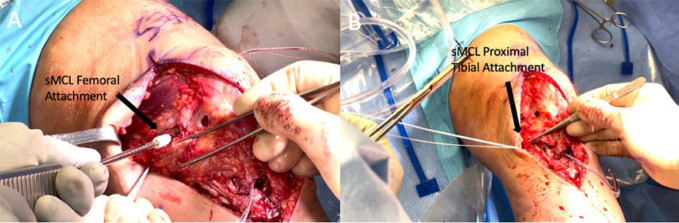
Complete PMC reconstruction is typically indicated in patients who are limited in their day-to-day activities by chronic valgus and rotary knee instability [Figure 7]. 5,17 The knee alignment of the weight-bearing frontal plane should be evaluated prior to reconstruction. Valgus misalignment may lead to soft tissue stretching of the graft and is linked with a greater likelihood of failure for chronic PMC injuries. 17 Valgus malalignment in cases of chronic PMC injury should be initially corrected with first-stage distal femoral osteotomy or concurrently with a PMC reconstruction [Table 1].5,17
Figure 7.
Intraoperative images of sMCL reconstruction. (A) illustrating the placement of a bioscrew to fix the proximal sMCL graft within the femoral tunnel. (B) illustrating the placement of a suture anchor to fix the distal end of the sMCL graft to the tibia. sMCL, superficial medial collateral ligament (left knee)
Table 1.
Pearls and Pitfalls of PMC Reconstruction
| Pearls | Pitfalls |
|---|---|
| A thorough physical exam, supplemented with stress radiographs and MRI, is essential for an accurate and complete diagnosis of a medial-sided knee injury. | MCL reconstruction may be compromised by nonanatomic tunnel placement. Verify that the guide pins are in the correct anatomic placement prior to drilling. |
| Medial sided femoral tunnels should be drilled by aiming anteriorly and proximally. | The sMCL tunnel should be aimed transversely across the tibia and 30° distally to reduce the risk of sMCL and POL tunnel convergence. |
| Posterior placement of the sMCL graft tibial insertion more closely reproduces native anatomy and decreases the risk of graft failure. | If chronic limb malalignment is not addressed before or concurrently with the reconstruction, there is increased risk of graft stretching or failure. |
| Passing sutures should be left in place after each tunnel is drilled to assist with later graft passage. | Failure to properly remove all soft tissue from tunnels may impede graft passage. |
Anatomic Augmentation Repair of the Superficial Medial Collateral Ligament (sMCL)
Anatomic augmentation repair is typically performed if poor tissue quality prevents primary sMCL repair. 4 We advocate for an anatomic augmented repair technique reported on by Serra Cruz et al.36 Anatomic augmentation of the sMCL is initiated with an incision starting directly between the medial portion of the patella and the adductor tubercle (AT) and distally extending 7 cm past the joint line. The surgeon must carefully bypass the saphenous nerve located 5 cm posterior to the AT. 37
Blunt dissection is then completed until the sartorial fascia is visualized, allowing for the identification and isolation of the pes anserinus tendons. A hamstring tendon stripper detaches the proximal end of the gracilis and semitendinosus tendons, leaving the distal insertions intact. 36 The surgeon should identify a remnant of the sMCL at the point of tibial attachment on the posterior aspect of the medial tibia, 6 or 7 cm distal to the joint line. To securely attach the hamstring grafts to the tibia, two double-loaded suture anchors are fixed at the sMCL distal tibial insertion, which is 6 cm distal to the joint line indicated by the sMCL remnant. 36 The first anchor is posteriorly inserted on the tibia, and the second is inserted marginally proximal and anterior to the first. Both grafts and any present sMCL remnants are then sutured to the tibia to reconstruct the distal tibial sMCL attachment.36,38
Attention is next given to the proximal attachment site of the sMCL, positioned 12 mm distal to the adductor tubercle and 8 mm anterior. This structure can be identified by following the adductor magnus tendon to its femoral insertion. 38 Sharp dissection of bone is necessary to clear the surrounding soft tissues and visualize the proximal sMCL attachment. An eyelet pin is drilled through the sMCL femoral attachment with an aiming guide and a 7-mm acorn reamer is used to over-ream a 35-mm-deep tunnel. The tendon grafts must be placed deep into the sartorial fascia, reproducing the native orientation of the sMCL.36 The gracilis and semitendinosus grafts should be measured from their distal insertion to 30 mm past the reconstruction tunnel and excess graft removed. This measurement allows 30 mm of the graft to be whipstitched and, using the passing suture, brought into the tunnel [Figure 8]. With the knee flexed to 20° and neutrally rotated, the graft is fastened in the tunnel using a 7 x 20 mm bioabsorbable screw to stabilize the graft while applying a slight varus force reduction. A final double-loaded suture is placed to recreate the sMCL attachment to the proximal tibia.5,36,39
Figure 8.
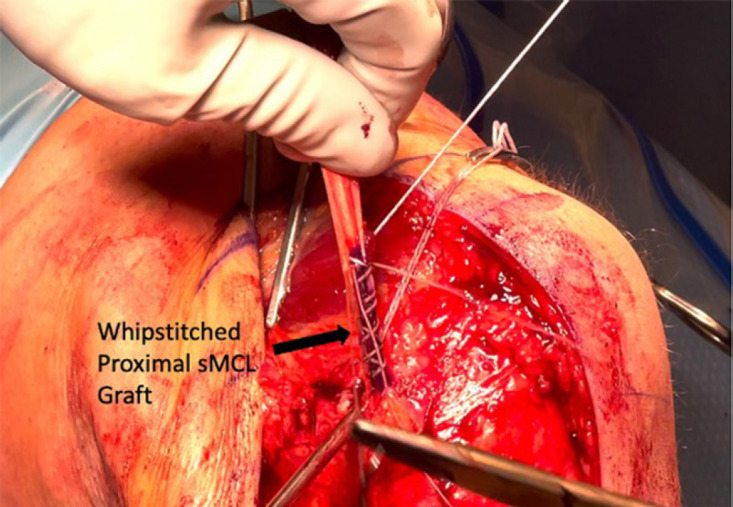
Intraoperative image illustrating proper marking and whipstitching of the proximal end of the sMCL graft. This is done to mark the correct graft length before removing excess graft tissue. This allows for enough graft length for fixation within the femur and proper tensioning of the graft. (left knee)
Anatomic Complete Posteromedial Corner (PMC) Reconstruction
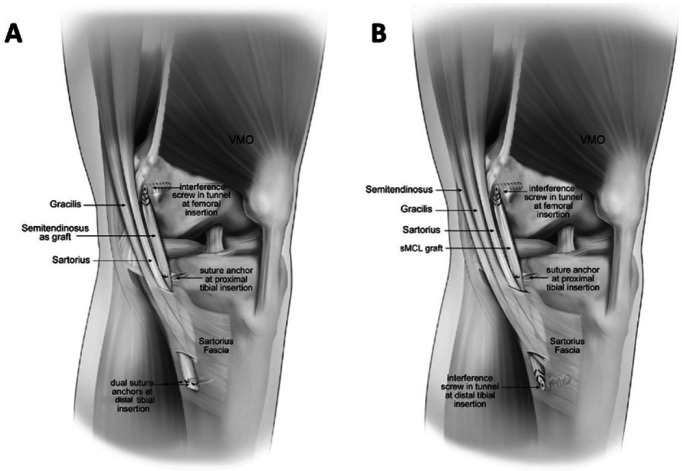
We recommend an anatomic-based technique developed by LaPrade et al. which reconstructs the proximal and distal components of the sMCL and POL with two separate grafts [Figure 9]. To expose the attachment sites, an anteromedial longitudinal incision is made 4 cm medial to the patella and extended along the medial knee until the incision is distal to the joint line by 7 cm. Next, 6 cm distal to the joint line, the sMCL distal tibial attachment site is identified deep to the fascial expansion of the sartorius muscle and pes anserine bursa. Once exposed, an eyelet passing pin is transversely drilled into the distal sMCL attachment. A 7-mm reamer is then used to ream the tunnel to a depth of 25 mm.5,8 To avoid tunnel convergence in the tibia during combined PMC and PCL reconstruction, the sMCL tunnel is aimed transversely across the fibula, at a 30° angle distally.40 A 25-mm deep closed-socket tunnel is then drilled with a 7-mm reamer at the POL tibial attachment site, slightly anterior to the semimembranosus tendon’s direct arm. When a PCL tunnel is also present, the POL tibial tunnel guide pin is aimed approximately 15 mm medial to Gerdy’s tubercle and drilled across the tibia.
Figure 9.
Illustration of sMCL surgical techniques in a left knee: (A) anatomic sMCL repair and (B) anatomic sMCL reconstruction. sMCL, superficial medial collateral ligament; VMO, vastus medialis oblique. Reproduced with permission from LaPrade et al.43
Anatomic femoral tunnel placement of the sMCL and POL requires the quantitative identification of osseous landmarks and results in near-native force distribution across the reconstructed grafts. The adductor magnus tendon should be isolated and traced back to the AT, also referred to as the “lighthouse of the medial knee.” The medial epicondyle is identified 8.3 mm anterior and 12.6 mm distal to the AT. The sMCL proximal attachment is 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. 1 The POL femoral attachment site is 7.7 mm distal to the gastrocnemius tubercle and 2.9 mm anterior. Once the sMCL and POL attachment sites are identified, an eyelet passing pin is first reamed at the POL site and then the sMCL site, maintaining a sufficient bone bridge between sites. Twenty-five mm deep tunnels are reamed with a 7-mm reamer at the sMCL and POL femoral attachment sites.
It is critical to avoid tunnel convergence during medial knee reconstructions. Moatshe et al. proposed guidelines to avoid sMCL and POL tunnel collision. In combined PMC and PCL reconstruction, the femoral tunnels should be aimed anteriorly 20° to 40° and proximally by 40°. The same study found that POL tunnel orientation was optimized at 20° proximally and 20° anteriorly. 41
Reconstruction graft lengths for the sMCL and POL should measure approximately 16 cm and 12 cm in length, respectively. After the grafts are fixated using a cannulated bioabsorbable screw, the POL graft must be fastened at full extension. This orientation maximizes tension on the POL fibers. 17 Once the POL is fastened, the sMCL is secured at 20° of knee flexion with the application of a slight varus reduction force and with the tibia neutrally rotated. The varus reduction force is necessary to prevent medial compartment instability. Lastly, the proximal tibial attachment of the sMCL is secured with a suture anchor placed 12.2 mm distal to the joint line, slightly medial to the anterior arm of the semimembranosus tibial attachment.1,5,8
Postoperative Rehabilitation
Patients remain non-weight bearing with crutches for six weeks after surgery and utilize a knee immobilizer to support the joint. 5 They may transition into a hinged knee brace once swelling reduces enough for proper brace fit. The immobilizer or brace is removed for bathing and four times daily for therapeutic exercise sessions. Frequent sessions of vasopneumatic cryotherapy and routine use of lower extremity compression stockings are recommended for managing postoperative knee and limb swelling. 42
Arthrofibrosis represents the most frequent complication following operative treatment of a PMC-related injury. 38 An effective rehabilitation program should aim to decrease the incidence of arthrofibrosis through early passive motion starting on day one postoperatively. Anatomic-based reconstructions coupled with early motion rehabilitation decrease the risk of arthrofibrosis with no additional risk of the graft(s) stretching.4 Therefore, we advocate for early, supervised rehabilitation which begins the first day after surgery. 4,5,38
Surgical Outcomes
There is debate regarding the optimal surgical treatment for a grade-III PMC injury. Wijdicks et al. investigated cadaveric knee kinematics after sMCL augmentation (sMCLA) and anatomic sMCL reconstruction (sMCLR). The researchers reported that both the sMCLA and sMCLR significantly decreased medial compartment gapping in addition to decreasing the extent of valgus and external rotation when compared to a sectioned sMCL.38 The sMCLA and sMCLR techniques did not demonstrate significantly different outcomes. Each technique allowed for fewer than 2 mm of medial joint gapping, performed at 0° and 20° of knee flexion. Neither the sMCLA nor the sMCLR was able to recreate the stability of a native MCL.38
A recent study by LaPrade et al.43 investigated the clinical outcomes of sMCL augmentation repair versus sMCL autograft reconstruction. The researchers reported no significant differences in objective clinical outcomes at one year follow up for the sMCL augmentation repair and sMCL autograft reconstruction groups. All patients completed a rehabilitation program with early knee motion, and there was no evidence of graft attenuation or arthrofibrosis at one year postoperatively.43
LaPrade and Wijdicks reported significantly improved outcomes following an anatomic medial knee reconstruction. 8 Postoperative International Knee Documentation Committee (IKDC) scores after surgery averaged 76.2, versus preoperative average IKDC score of 43.5. All patients in the cohort reported elimination of side-to-side instability, confirmed by side-to-side stress radiographs. The researchers concluded that anatomic medial knee reconstruction effectively restored valgus and rotational stability. 8
Figure 2.
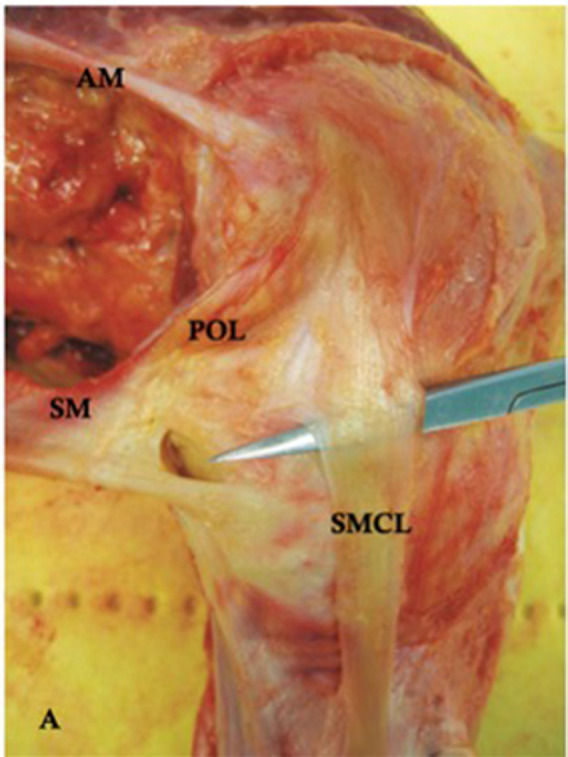
A medial view of a cadaveric dissection demonstrates the relationship of the sMCL to the POL (left knee). The attachment sites of the semimembranosus (SM) tendon and adductor magnus (AM) tendon are also noted. 18 sMCL, superficial medial collateral ligament; POL, posterior oblique ligament
References
- 1.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. Sep. 2007;89(9):2000–10. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 2.LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc Rev. Jun. 2015;23(2):63–70. doi: 10.1097/JSA.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 3.Wijdicks CA, Griffith CJ, LaPrade RF, et al. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. Mar. 2009;91(3):521–9. doi: 10.2106/JBJS.H.00909. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade RF, Engebretsen L, Marx RG. Repair and Reconstruction of Medial- and Lateral-sided Knee Injuries. Instr Course Lect. 2015;64:531–42. [PubMed] [Google Scholar]
- 5.Cinque ME, Chahla J, Kruckeberg BM, DePhillipo NN, Moatshe G, LaPrade RF. Posteromedial Corner Knee Injuries: Diagnosis, Management, and Outcomes: A Critical Analysis Review. JBJS Rev. Nov. 2017;5(11) doi: 10.2106/JBJS.RVW.17.00004. [DOI] [PubMed] [Google Scholar]
- 6.Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 7.Dold AP, Swensen S, Strauss E, Alaia M. The Posteromedial Corner of the Knee: Anatomy, Pathology, and Management Strategies. J Am Acad Orthop Surg. Nov. 2017;25(11):752–761. doi: 10.5435/JAAOS-D-16-00020. [DOI] [PubMed] [Google Scholar]
- 8.Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. Mar. 2012;470(3):806–14. doi: 10.1007/s11999-011-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. May. 2010;92(5):1266–80. doi: 10.2106/JBJS.I.01229. [DOI] [PubMed] [Google Scholar]
- 10.Griffith CJ, LaPrade RF, Johansen S, Armitage B, Wijdicks C, Engebretsen L. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am J Sports Med. Sep. 2009;37(9):1762–70. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 11.Griffith CJ, Wijdicks CA, LaPrade RF, Armitage BM, Johansen S, Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. Jan. 2009;37(1):140–8. doi: 10.1177/0363546508322890. [DOI] [PubMed] [Google Scholar]
- 12.Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, Laprade RF. Structural properties of the primary medial knee ligaments. Am J Sports Med. Aug. 2010;38(8):1638–46. doi: 10.1177/0363546510363465. [DOI] [PubMed] [Google Scholar]
- 13.Fanelli GC, Harris JD. Surgical treatment of acute medial collateral ligament and posteromedial corner injuries of the knee. Sports Med Arthrosc Rev. Jun. 2006;14(2):78–83. doi: 10.1097/01.jsa.0000212301.80496.dc. [DOI] [PubMed] [Google Scholar]
- 14.Wijdicks CA, Griffith CJ, LaPrade RF, et al. Medial knee injury: Part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med. Sep. 2009;37(9):1771–6. doi: 10.1177/0363546509335191. [DOI] [PubMed] [Google Scholar]
- 15.Robinson JR, Bull AM, Thomas RR, Amis AA. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med. Nov. 2006;34(11):1815–23. doi: 10.1177/0363546506289433. [DOI] [PubMed] [Google Scholar]
- 16.Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. Feb. 2010;38(2):330–8. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 17.Laprade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. Mar. 2012;42(3):221–33. doi: 10.2519/jospt.2012.3624. [DOI] [PubMed] [Google Scholar]
- 18.Marchant MH Jr, Tibor LM, Sekiya JK, Hardaker WT Jr, Garrett WE Jr, Taylor DC. Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med. May. 2011;39(5):1102–13. doi: 10.1177/0363546510385999. [DOI] [PubMed] [Google Scholar]
- 19.Jackman T, LaPrade RF, Pontinen T, Lender PA. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med. Aug. 2008;36(8):1571–6. doi: 10.1177/0363546508315897. [DOI] [PubMed] [Google Scholar]
- 20.James EW, Williams BT, LaPrade RF. Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res. Sep. 2014;472(9):2644–57. doi: 10.1007/s11999-014-3470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.LaPrade RF, Moulton SG, Nitri M, Mueller W, Engebretsen L. Clinically relevant anatomy and what anatomic reconstruction means. Knee Surg Sports Traumatol Arthrosc. Oct. 2015;23(10):2950–9. doi: 10.1007/s00167-015-3629-1. [DOI] [PubMed] [Google Scholar]
- 22.Yao L, Dungan D, Seeger LL. MR imaging of tibial collateral ligament injury: comparison with clinical examination. Skeletal Radiol. Oct. 1994;23(7):521–4. doi: 10.1007/BF00223082. [DOI] [PubMed] [Google Scholar]
- 23.American Medical A. Committee on the Medical Aspects of S, Subcommittee on Classification of Sports I. Standard nomenclature of athletic injuries. 1966. [Google Scholar]
- 24.Quarles JD, Hosey RG. Medial and lateral collateral injuries: prognosis and treatment. Prim Care. Dec. 2004;31(4):957–75, ix. doi: 10.1016/j.pop.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Kim C, Chasse PM, Taylor DC. Return to Play After Medial Collateral Ligament Injury. Clin Sports Med. Oct. 2016;35(4):679–96. doi: 10.1016/j.csm.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med. Mar-Apr. 1996;24(2):160–3. doi: 10.1177/036354659602400207. [DOI] [PubMed] [Google Scholar]
- 27.Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5 Suppl):S51–7. doi: 10.1177/28.suppl_5.s-51. [DOI] [PubMed] [Google Scholar]
- 28.Hastings DE. The non-operative management of collateral ligament injuries of the knee joint. Clin Orthop Relat Res. Mar-Apr. 1980;(147):22–8. [PubMed] [Google Scholar]
- 29.Reider B, Sathy MR, Talkington J, Blyznak N, Kollias S. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation A five-year follow-up study. Am J Sports Med. Jul-Aug. 1994;22(4):470–7. doi: 10.1177/036354659402200406. [DOI] [PubMed] [Google Scholar]
- 30.Ballmer PM, Jakob RP. The non operative treatment of isolated complete tears of the medial collateral ligament of the knee A prospective study. Arch Orthop Trauma Surg. 1988;107(5):273–6. doi: 10.1007/BF00451505. [DOI] [PubMed] [Google Scholar]
- 31.Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Relat Res. Dec. 1986;(213):137–40. [PubMed] [Google Scholar]
- 32.Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. Jan. 1988;(226):103–12. [PubMed] [Google Scholar]
- 33.Razi M, Soufali AP, Ziabari EZ, Dadgostar H, Askari A, Arasteh P. Treatment of Concomitant ACL and MCL Injuries: Spontaneous Healing of Complete ACL and MCL Tears. J Knee Surg. Apr. 2020 doi: 10.1055/s-0040-1708858. [DOI] [PubMed] [Google Scholar]
- 34.Varelas AN, Erickson BJ, Cvetanovich GL, Bach BR Jr. Medial Collateral Ligament Reconstruction in Patients With Medial Knee Instability: A Systematic Review. Orthop J Sports Med. 2017;5(5): 2325967117703920. doi: 10.1177/2325967117703920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tibor LM, Marchant MH Jr, Taylor DC, Hardaker WT Jr, Garrett WE Jr, Sekiya JK. Management of medial-sided knee injuries, part 2: posteromedial corner. Am J Sports Med. Jun. 2011;39(6):1332–40. doi: 10.1177/0363546510387765. [DOI] [PubMed] [Google Scholar]
- 36.Serra Cruz R, Olivetto J, Dean CS, Chahla J, LaPrade RF. Superficial Medial Collateral Ligament of the Knee: Anatomic Augmentation With Semitendinosus and Gracilis Tendon Autografts. Arthrosc Tech. Apr. 2016;5(2):e347–52. doi: 10.1016/j.eats.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wijdicks CA, Westerhaus BD, Brand EJ, Johansen S, Engebretsen L, LaPrade RF. Sartorial branch of the saphenous nerve in relation to a medial knee ligament repair or reconstruction. Knee Surg Sports Traumatol Arthrosc. Aug. 2010;18(8):1105–9. doi: 10.1007/s00167-009-0934-6. [DOI] [PubMed] [Google Scholar]
- 38.Wijdicks CA, Michalski MP, Rasmussen MT, et al. Superficial medial collateral ligament anatomic augmented repair versus anatomic reconstruction: an in vitro biomechanical analysis. Am J Sports Med. Dec. 2013;41(12):2858–66. doi: 10.1177/0363546513503289. [DOI] [PubMed] [Google Scholar]
- 39.Serra Cruz R, Mitchell JJ, Dean CS, Chahla J, Moatshe G, LaPrade RF. Anatomic Posterolateral Corner Reconstruction. Arthrosc Tech. Jun. 2016;5(3):e563–72. doi: 10.1016/j.eats.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moatshe G, Slette EL, Engebretsen L, LaPrade RF. Intertunnel Relationships in the Tibia During Reconstruction of Multiple Knee Liga-ments: How to Avoid Tunnel Convergence. Am J Sports Med. Nov. 2016;44(11):2864–2869. doi: 10.1177/0363546516656371. [DOI] [PubMed] [Google Scholar]
- 41.Moatshe G, Brady AW, Slette EL, et al. Multiple Ligament Reconstruction Femoral Tunnels: Intertunnel Relationships and Guidelines to Avoid Convergence. Am J Sports Med. Mar. 2017;45(3):563–569. doi: 10.1177/0363546516673616. [DOI] [PubMed] [Google Scholar]
- 42.Tischer TS, Oye S, Lenz R, et al. Impact of compression stockings on leg swelling after arthroscopy - a prospective randomised pilot study. BMC Musculoskelet Disord. Apr. 2019;20(1):161. doi: 10.1186/s12891-019-2540-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.LaPrade RF, DePhillipo NN, Dornan GJ, et al. Comparative Outcomes Occur After Superficial Medial Collateral Ligament Augmented Repair vs Reconstruction: A Prospective Multicenter Randomized Controlled Equivalence Trial. Am J Sports Med. 2022:3635465211069373. doi: 10.1177/03635465211069373. [DOI] [PubMed] [Google Scholar]