Increasing energy/power costs as well as the worldwide discussion of cutting CO2 emissions seem to make necessary savings in power consumption in the private realm and especially in the hospital sector inevitable. Hospitals are characterized by high energy consumption. Tippköter et al showed that hospitals have a power requirement of 119 kWh per square meter of floor area per year (1), or, to put it differently, a hospital bed requires as much power as three to four one-family houses (2). The surgical units as well as intensive care units account for particularly high volumes—owing to air conditioning technology or steam production for the sterilizing unit/autoclave. One third of the energy volume consumed in hospital is due to electricity consumption, but this accounts for about half of the payable energy costs.
Our study aimed to identify potential energy savings of medical devices, based on ventilators, to calculate such savings, and to explain the possibility of a reduction in energy consumption.
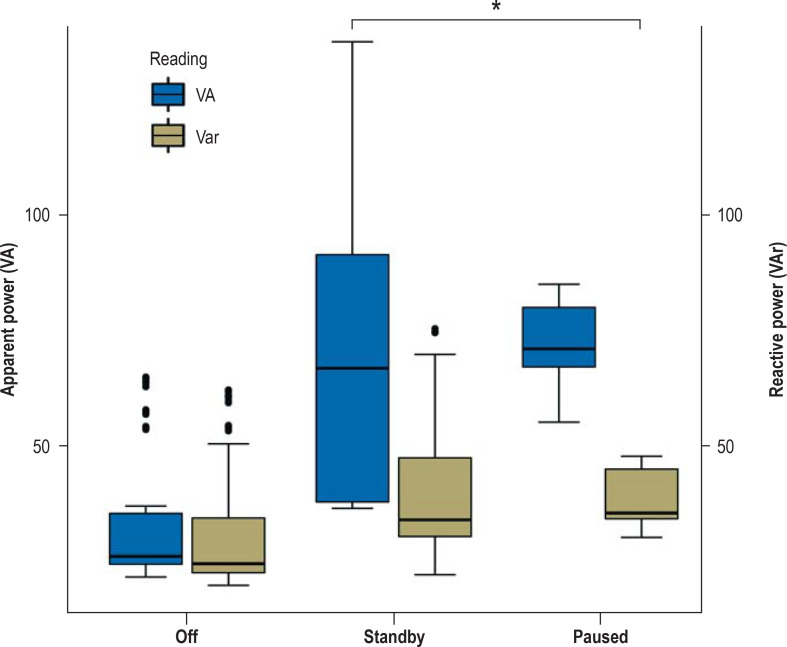
Figure 2.
Apparent power (VA) and reactive power (VAr) of anesthesia machines in different modes. A part of the power transmitted to the machines is reactive power. In contrast to the active power, the reactive power is fed back into the network. Simple gauges mostly measure apparent power—that is, active power including reactive power—and may therefore result in higher consumption values, with apparent, active, and reactive power have a more complex relation can cannot simply be added or subtracted. Box plots represent the 25th–75th percentiles with medians (horizontal line), n = 285, *p < 0.01 versus off.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Method
We investigated the power consumption (using gauge CLM1000 Professional[+] Christ-Elektronik GmbH, Germany) of the anesthesia machines in our central operating room (models from Dräger: Atlan [software version 1.02], Fabius Tiro [software version 3.37a], Primus [software version 4.53], Perseus A500 [software version 2.0] (n = 24) in the modes (where available)
Off
Paused
Standby
We took five individual readings at intervals of 30 seconds in each mode (0–120 s, n-285). Furthermore, we determined the timespan between switching the machine on and it being operational. To measure the power consumption of operating the machine, the current power consumption was recorded every 15 seconds while the machine was booting up. The data analysis was done in SPSS (21.0 IBM, USA) while testing for variance homogeneity, Kruskal–Wallis test, or Mann–Whitney U-test with Bonferroni correction (significance level p<0.05).
Result
An anesthesia machine in standby mode consumed on average 56.7±31.9 w (mean ± standard deviation), a switched-off device consumed 10.6 ± 4.1 w, and the consumption in paused mode was 61.4 ± 7.7 w (figure 1). In this context it is interesting that the machines in standby mode and paused mode consumed up to 127w. These peak values were not measured in switched-off mode. The average timespan for a switched-off anesthesia machine to become operational was only 35.5 ± 11.3 s with an energy expenditure of 35 ± 16 w. If extrapolated this would mean that the anesthesia machines in standby mode in our surgical units consume 4723.3 W. If we switched off 90% of the machines after the end of regular working hours (including late rooms and service workloads) we could save 51 kWh of power/day on weekdays and 166 kWh/day on weekends. Projected over a year, switching off the anesthesia machines alone could save 24 687 kWh in the surgical units. In view of Germany’s average mix for power production (3), this simple action could help save approximately 10.15 t CO2 at Freiburg University Medical Center alone.
Figure 1.
Power consumption in watt of anesthesia machines in different modes. Box plots represent the 25th–75th percentiles with medians (horizontal line), n = 285, *p < 0.01 versus off
Conclusion
The extensive requirements and standards as well as the complexity of a hospital building mean that power consumption in hospitals can be expected to always be above average compared with other buildings. In Germany, the 1900 existing hospitals contribute substantially to CO2 emissions as a result of their high power consumption. Our readings were taken at several time points over a short time period, employing several readings of power consumption rather than one-second readings. Still, preliminary data of the measurement series show the same trend, implying that switching off anesthesia machines that are not being used would yield a calculated power energy saving of 24 687 kWh per year and therefore a reduction of 10.15 t CO2. In these calculations the booting/loading cycle and power consumption of the machines for the charging process of the internal batteries in the standby and switched-off mode remain unknown. Compared with the consumption of large energy users—for example, air conditioning units (4)—saving energy by switching off anesthesia machines looks like a small contribution, but by contrast to energy savings in aircon technology, which require comprehensive reconstruction measures, it can be done easily and immediately. Changes to the lifespan of and replacement parts for the machines are not even included in the calculation of the CO2 balance. This is, however, the subject of controversial discussion, since according to the construction or as a result of switching the machine on and off, a greater wear of components can occur, for example, as a result of the active discharge of condensers in switching power supplies.
For safety relevant machines, change management is required as for example automated self-checks happen during the night, and switching these devices temporarily on and off is—on its own—unlikely to be sufficient. Since it only takes 35.5 seconds for the machines to become operational and do the obligatory quick check, the argument of prolonged duration and/or problematic activation after switching off can be discounted (5). However, we recommend not to switch off machines in critical infrastructures, such as the trauma resuscitation area or obsterics theater, so as to enable seamless emergency care.
It is possible with the simplest measures in routine clinical practice to reduce power consumption and thus CO2 emissions. Furthermore, we need new standards and routines. For example, all manufacturers should be required to produce more energy efficient machines and adjustable energy saving modes for our working days and nights in hospitals. But ultimately it is not technology that will be crucial for successful ecological transformation in hospitals but the factor “user”.
References
- 1.Tippkötter R, Wallschlag B. Leitfaden Energieeffizienz für Krankenhäuser EnergieAgentur.NRW (ed.) https://broschuerenservice.nrw.de/files/7/3/732584c16d3781 8338c9b7b6d8323b87.pdf (last accessed on 2 September 2022) 2009 [Google Scholar]
- 2.Loh M. Einsparpotenziale in Krankenhäusern: Effizienz, die sich rechnet. Dtsch Arztebl. 2014;111 A-277. [Google Scholar]
- 3.Icha P, Lauf T, Kuhs G. Entwicklung der spezifischen Treibhausgas-Emissionen des deutschen Strommix in den Jahren 1990-2021. Umweltbundesamt, Reihe: Climate Change15/ 2022:1–34. [Google Scholar]
- 4.Bolkenius D, Heller AR. Klimaschutz: Nachhaltigkeit in der Anästhesie. Dtsch Arztebl. 2021;118 A-2439. [Google Scholar]
- 5.Prien T, Bürkle H, Czaplik M, et al. Funktionsprüfung des Narkosegerätes zur Gewährleistung der Patientensicherheit - Empfehlung der Kommission für Normung und technische Sicherheit der DGAI. Anästh Intensivmed. 2019;60:75–83. [Google Scholar]