Abstract
Simple Summary
Novel antibody-drug conjugates (ADCs) show efficacy in advanced breast cancer with low HER2 levels. Little is known about the discordance of low HER2 levels between the primary tumor and distant metastases. The clinical relevance of discordance between the primary tumor and metastases prompted us to investigate the differences in HER2 expression between primary tumors and distant metastases, particularly in the HER2-negative (HER2-low and HER2-zero) primary breast cancer cohort. Our results show a relevant discordance of HER2-low status between primary tumors and their corresponding distant metastases.
Abstract
We examined differences in HER2 expression between primary tumors and distant metastases, particularly within the HER2-negative primary breast cancer cohort (HER2-low and HER2-zero). The retrospective study included 191 consecutive paired samples of primary breast cancer and distant metastases diagnosed between 1995 and 2019. HER2-negative samples were divided into HER2-zero (immunohistochemistry [IHC] score 0) and HER2-low (IHC score 1+ or 2+/in situ hybridization [ISH]-negative). The main objective was to analyze the discordance rate between matched primary and metastatic samples, focusing on the site of distant metastasis, molecular subtype, and de novo metastatic breast cancer. The relationship was determined by cross-tabulation and calculation of Cohen′s Kappa coefficient. The final study cohort included 148 paired samples. The largest proportion in the HER2-negative cohort was HER2-low [primary tumor 61.4% (n = 78), metastatic samples 73.5% (n = 86)]. The discordance rate between the HER2 status of primary tumors and corresponding distant metastases was 49.6% (n = 63) (Kappa −0.003, 95%CI −0.15–0.15). Development of a HER2-low phenotype occurred most frequently (n = 52, 40.9%), mostly with a switch from HER2-zero to HER2-low (n = 34, 26.8%). Relevant HER2 discordance rates were observed between different metastatic sites and molecular subtypes. Primary metastatic breast cancer had a significantly lower HER2 discordance rate than secondary metastatic breast cancer [30.2% (Kappa 0.48, 95%CI 0.27–0.69) versus 50.5% (Kappa 0.14, 95% CI −0.03–0.32)]. This highlights the importance of evaluating potentially therapy-relevant discordance rates between a primary tumor and corresponding distant metastases.
Keywords: HER2-low, HER2-zero, HER2 overexpression, HER2 dynamics, de-novo metastasis, antibody-drug conjugate
1. Introduction
Overexpression or amplification of human epidermal growth factor receptor 2 (HER2) characterizes a molecular subtype of breast cancer that progresses rapidly and has a poor prognosis [1,2]. However, with the advent of targeted therapies against HER2 such as the monoclonal antibody trastuzumab, the original prognostic disadvantage of HER2 positivity has been transformed into a clinically relevant predictive advantage [3]. In advanced HER2-positive breast carcinoma, survival was further prolonged by pertuzumab [4]. In the event of progression, tyrosine kinase inhibitors such as lapatinib or tucatinib showed efficacy in HER2-positive breast carcinoma [5,6]. In addition, antibody-drug conjugates (ADC) provided a further improvement not only in progression-free survival (PFS) but also in overall survival (OS) in advanced HER2-positive breast carcinoma [7,8].
Therefore, it was obvious to use anti-HER2 therapies also in early breast carcinoma. Indeed, the use of trastuzumab resulted in a statistically significant prolongation of overall survival [9]. Surprisingly, some of the patients who participated in the original trastuzumab trials and were ultimately HER2-negative at central HER2 reassessment benefited from trastuzumab [10,11]. Based on these findings, a large phase III trial was conducted in 3270 women, but it clearly showed that trastuzumab was not beneficial for patients without IHC 3+ or ISH-enhanced breast cancer [12]. In HER2-positive early breast cancer, the addition of pertuzumab led to a relevant increase in pathologic complete response rates (pCR) and an improvement in disease-free survival (DFS) [13,14]. The prolongation of DFS was further increased using the tyrosine kinase inhibitor neratinib after the completion of trastuzumab-based therapy in HER2-positive patients [15]. Furthermore, the ADC T-DM1 improved DFS in early HER2-positive breast cancer with residual disease after neoadjuvant trastuzumab-based treatment [16]. Overall, these HER2-targeted therapies represent tremendous progress for the 15–20% HER2-positive patients. Meanwhile, several retrospective studies have taken a closer look at the large group of HER2-negative breast cancer. Breast cancer showing HER2 protein expression without HER2 gene amplification could be divided into two separate groups (HER2-low [IHC 1+ or 2+ and ISH-negative] and HER2-zero [IHC 0]) with different prognosis or pCR after neoadjuvant chemotherapy [17,18,19,20,21,22]. However, these results could not be confirmed in several other studies [23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Nevertheless, interest in HER2-low tumors has increased greatly due to the results of the DESTINY-Breast04 trial, which demonstrated the superiority of trastuzumab-deruxtecan (T-DXd) over physician′s choice chemotherapy in patients with advanced HER2-low breast cancer [37]. The prolongation of PFS (10.1 months vs. 5.4 months; hazard ratio [HR] 0.51; p < 0.001) and OS (23.9 months vs. 17.5 months; HR 0.64; p = 0.003) was both statistically significant and clinically relevant. These compelling results led to a rapid update of the American Society of Clinical Oncology (ASCO) guideline and a positive opinion of the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommending the use of T-DXd in patients with HER2-low metastatic BC [38,39].
Until now, the only question regarding HER2 status was whether the tumor was HER2-positive or HER2-negative. However, the impressive data from T-DXd in HER2-low breast cancer highlights the importance of dividing the large group of HER2-negative patients. In principle, the well-known ASCO/College of American Pathologists (CAP) clinical practice guideline allows such a distinction [40]. However, potential difficulties such as tumor heterogeneity (clustered or mosaic type) or unusual staining patterns (moderate to intense but incomplete staining or carcinomas with limited strong HER2 overexpression) must be considered [41]. To address difficulties in distinguishing between HER2-low and HER2-zero, pathologists have already pointed out possible solutions for the assessment of immunohistochemical staining such as (1) application of the “magnification rule”, (2) staining pattern-circularity of membrane staining, and (3) percentage of tumor cells with HER2 expression [42].
In addition to these briefly outlined challenges for pathologists in distinguishing between HER2-low and HER2-zero, another fundamental problem is discordance between the primary tumor and corresponding metastases, since whenever possible, a recent metastatic biopsy is encouraged to guide therapy in advanced breast cancer. The problem of discordance between primary tumors and distant metastases arises when treating patients with metastatic disease with targeted therapies. The discordance of traditional HER2 dichotomy (positive or negative) between primary breast cancer and distant metastases is well established. Among others, Grassini et al. reviewed the phenomenon of HER2 conversion between primary breast tumors and relapsed/distant metastatic [41]. While early studies described a wide variability in HER2 discordance rates (0–44%), several meta-analyses showed discordance rates ranging from 7.8% to 13.7% [43,44,45]. Most commonly, conversion from HER2-positive to HER2-negative was observed, which is clinically important in both advanced and early breast cancer. In neoadjuvant studies, a loss of HER2 expression from a therapy-naïve primary tumor and the post-neoadjuvant residual tumor was described with a prognostic disadvantage [46,47,48,49,50,51].
However, less is known about the discordance of HER2-low between primary tumors and distant metastases. Thus, Tarantino and coworkers demonstrated a relevant discordance in HER2 expression between PTs and their associated metastases: 44% of HER2-zero PTs had an elevated HER2 score on biopsy, and 22% of HER2-low PTs became HER2-zero tumors [32]. Miglietta et al. reported an overall rate of HER2 discordance of 38.0%, with most transitioning from HER2-zero to HER2-low (15%) and from HER2-low to HER2-zero (14%) [52]. This discordance rate is clinically relevant to the use of ADCs and prompted us to investigate the discordance rate in 148 paired samples (primary breast tumor and distant metastasis), focusing on (i) molecular subtype, (ii) distant metastasis site, and (iii) differences between primary metastatic breast cancer (PMBC) and secondary metastatic breast cancer (SMBC).
2. Materials and Methods
2.1. Study Cohort
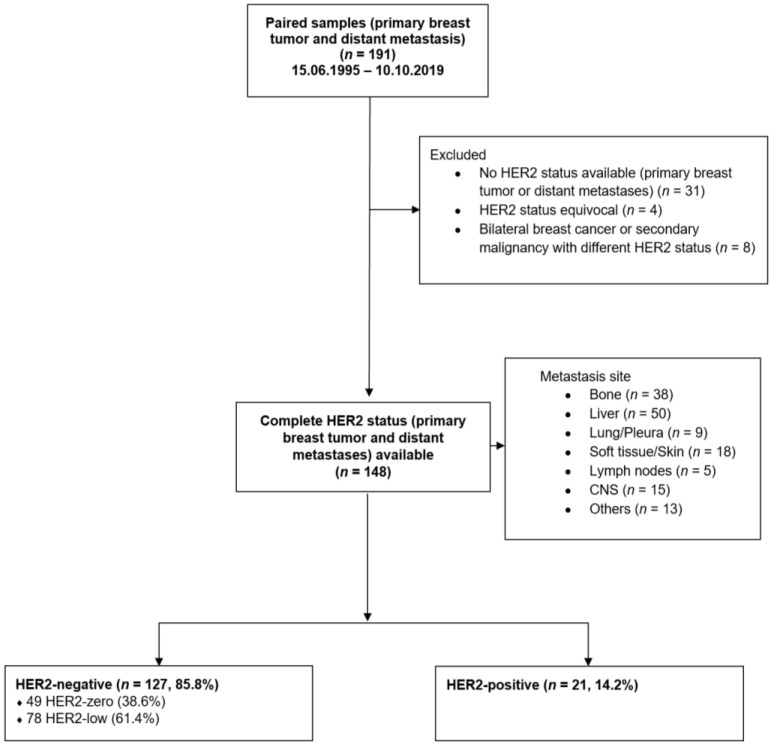
The certified breast cancer center of the University Medical Center Mainz has been prospectively documenting clinic-pathological characteristics as well as therapies of all treated breast cancer patients. This database was searched for patients with metastatic breast cancer between 15.06.1995 and 10.10.2019. We studied 191 consecutive paired samples of primary breast tumor and distant metastasis. Only solid distant metastases were considered. Paired samples without complete HER2 status (n = 31), with HER2 status equivocal (n = 4), or bilateral BC or secondary malignancy with different HER2 status (n = 8) were not eligible for this study (Figure 1).
Figure 1.
Patient enrolment.
PMBC was defined as the presence of metastasis at the time of diagnosis of the PT [53,54]. The median age at the time of initial breast cancer diagnosis was 53 years (range, 31–86 years). Table 1 provides an overview of the established clinico-pathologic prognostic factors in the final study cohort (n = 148).
Table 1.
Clinico-pathological parameters at diagnosis (n = 148).
| Total Number of Patients (n = 148) |
HER2-Negative (n = 127) |
HER2-Positive (n = 21) |
p-Value | |||
|---|---|---|---|---|---|---|
| HER2-Zero (n = 49) |
HER2-Low (n = 78) |
|||||
| Age at primary breast surgery | 0.087 | |||||
| Median [years] | 53 | 48 | 54 | 52 | ||
| <50 years | 66 (44.6%) | 28 (57.1%) | 29 (37.2%) | 9 (42.9%) |
||
| >50 years | 82 (55.4%) | 21 (42.9%) | 49 (62.8%) | 12 (57.1%) | ||
| Histological subtype | 0.221 | |||||
| Invasive carcinoma of no special type (NST) | 115 (77.7%) | 33 (67.3%) | 63 (80.8%) | 19 (90.5%) | ||
| Invasive lobular carcinoma | 24 (16.2%) | 12 (24.5%) | 11 (14.1%) | 1 (4.8%) |
||
| other | 9 (6.1%) | 4 (8.2%) | 4 (5.1%) | 1 (4.8%) |
||
| Tumor size | 0.032 | |||||
| pT1 | 32 (22.2%) | 11 (22.9%) | 18 (24.0%) | 3 (14.3%) |
||
| pT2 | 67 (46.5%) | 30 (62.5%) | 30 (40.0%) | 7 (33.3%) |
||
| pT3/4 | 45 (31.3%) | 7 (14.6%) | 27 (36.0%) | 11 (52.3%) | ||
| missing | 4 (2.7%) | |||||
| Nodal status | 0.710 | |||||
| Negative | 44 (29.7%) | 13 (26.5%) | 25 (33.3%) | 6 (28.6%) |
||
| positive | 101 (68.2%) | 36 (73.5%) | 50 (66.7%) | 15 (71.4%) | ||
| missing | 3 (2.0%) | |||||
| Histological grade | 0.049 | |||||
| G1 | 11 (7.4%) |
6 (12.2%) | 5 (6.7%) | 0 | ||
| G2 | 72 (48.6%) | 19 (38.8%) | 45 (60.0%) | 8 (40.0%) |
||
| G3 | 61 (41.2%) | 24 (49.0%) | 25 (33.3%) | 12 (60.0%) | ||
| missing | 4 (2.7%) | |||||
|
Hormone receptor
status |
0.252 | |||||
| negative | 23 (15.5%) | 11 (22.4%) | 9 (11.5%) | 3 (14.3%) |
||
| positive | 125 (84.5%) | 38 (77.6%) | 69 (88.5%) | 18 (85.7%) | ||
| HER2 status | ||||||
| Negative | 127 (85.8%) | 49 (100.0%) | 78 (100.0%) |
|||
| Positive | 21 (14.2%) | 21 (14.2%) | ||||
| 0 | 49 (33.1%) | 49 (100.0%) | ||||
| 1+ | 59 (39.9%) | 59 (75.6%) | ||||
| 2+ | 22 (14.9%) | 19 (24.4%) | 3 (14.3%) | |||
| 2+/ISH negative | 19 (12.8%) | |||||
| 2+/ISH positive | 3 (2.0%) | |||||
| 3+ | 18 (12.2%) | 18 (85.7%) | ||||
| Ki-67 | 0.022 | |||||
| <20% | 19 (12.8%) | 10 (35.7%) | 9 (17.3%) | 0 | ||
| >20% | 74 (50.0%) | 18 (64.3%) | 43 (82.7%) | 13 (100.0%) | ||
| Missing | 55 (37.2%) | |||||
| Molecular subtype | <0.001 | |||||
| Luminal-like | 107 (72.3%) | 38 (77.6%) | 69 (88.5%) | 0 | ||
| Luminal-A-like | 18 (12.2%) | 9 | 9 | 0 | ||
| Lumina-B-like | 46 (31.1%) | 10 | 36 | 0 | ||
| Missing Ki-67 | 43 (29.1%) | |||||
| HER2 positive | 21 (14.2%) | 21 (100.0%) | ||||
| Triple-negative | 20 (13.5%) | 11 (22.4%) | 9 (11.5%) | 0 | ||
| Metastatic site | 0.349 | |||||
| Liver | 50 (33.8%) | 16 (32.7%) | 28 (35.9%) | 6 (28.6%) | ||
| Bone | 38 (25.7%) | 13 (26.5%) | 23 (29.5%) | 2 (9.5%) |
||
| Skin/Soft tissue | 18 (12.2%) | 6 (12.2%) | 10 (12.8%) | 2 (9.5%) |
||
| Central nervous system | 15 (10.1%) | 6 (12.2%) | 4 (5.1%) | 5 (23.8%) | ||
| others | 13 (8.8%) | 5 (10.2%) | 6 (7.7%) | 2 (9.5%) |
||
| Lung/Pleura | 9 (6.1%) |
1 (2.0%) |
5 (6.4%) | 3 (14.3%) | ||
| Lymph node | 5 (3.4%) |
2 (4.1%) |
2 (2.6%) | 1 (4.8%) |
||
| Additional metastatic biopsy | ||||||
| Yes | 19 (12.8%) | 5 (10.2%) | 11 (14.1%) | 3 (14.3%) | 0.797 | |
| HER2 concordance with previous biopsy | 8 (42.1%) | 1 (20.0%) | 6 (54.5%) | 1 (33.3%) | ||
| HER2 discordance with previous biopsy | 11 (57.9%) | 4 (80.0%) | 5 (45.4%) | 2 (66.7%) | ||
| No | 129 (87.2%) | 44 (89.8%) | 67 (85.9%) | 18 (85.7%) | ||
| Treatment for early breast cancer | ||||||
| Neo-/Adjuvant chemotherapy | 72 (48.6%) | 35 (71.4%) | 30 (38.5%) | 7 (33.3%) | <0.001 | |
| Neo-/Adjuvant Anti-HER2-therapy | 9 (6.1%) | 0 | 0 | 9 (42.9%) | <0.001 | |
| Adjuvant endocrine therapy | 79 (53.4%) | 31 (63.3%) | 42 (56.0%) | 6 (28.6%) | 0.083 | |
| Treatment for metastatic breast cancer | ||||||
| chemotherapy | 45 (30.4%) | 8 (16.3%) | 26 (34.2%) | 11 (52.4%) | 0.007 | |
| Anti-HER2-therapy | 13 (8.8%) | 2 (4.1) | 0 | 11 (52.4%) | <0.001 | |
| Endocrine therapy | 52 (35.1%) | 18 (36.7%) | 29 (38.2%) | 5 (23.8%) | 0.468 | |
| Tumor progression | ||||||
| Time to metastasis, Median [month] |
25 (0–150) |
44 (0–150) |
14 (0–121) |
0 (0–111) |
||
| Time to metastasis biopsy, Median [month] | 39 (0–165) |
51 (0–150) |
36 (0–165) |
17 (0–37) |
||
| Time from metastasis diagnosis to metastasis biopsy, Median [month] | 1 (0–131) |
0 (0–55) |
1 (0–131) |
0 (0–94) |
||
| Primary metastatic breast cancer (PMBC) | Yes | 53 (35.8%) |
8 (16.3%) |
31 (39.7%) |
14 (66.7%) |
|
| No | 95 (64.9%) |
41 (83.7%) |
47 (60.3%) |
7 (33.3%) |
||
2.2. Immunohistochemistry (IHC) and In Situ Hybridization (ISH)
Immunohistochemical analyses and in situ hybridization were performed on 3 µm thick sections of paraffin-embedded formalin-fixed tissues according to standard procedures. HER2 was scored from 0 to 3+ [40]. HER2 2+ cases (n = 22) were further classified as amplified or non-amplified by either fluorescence in situ hybridization (FISH) (Her2 FISH pharmDX kit, Dako) or chromogenic in situ hybridization (CISH) (Ventana Her2 dual ISH assay, Roche). HER2 2+ tumors with amplification of HER2 and 3+ tumors were classified as HER2-positive. The HER2-negative cohort was defined as 0, 1+, and 2+ without amplification of HER2. HER2-low tumors included all 1+ and 2+ tumors without amplification of HER2. Tumors with a HER2 score 0 were classified as HER2-zero [41,42]. Hormone receptor status was positive if tumor cells showed nuclear expression of either the estrogen receptor (ER) and/or the progesterone receptor (PR), the cut-off being defined as 1% of tumor cells [55].
The study was approved by the Ethics Committee of the Rhineland-Palatinate Medical Association, Germany (2021-15657). Written informed consent was obtained from all patients, and all clinical investigations were performed according to ethical and legal standards and in compliance with the Declaration of Helsinki. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline [56].
2.3. Statistical Analysis
The main objective was to evaluate HER2 expression differences between primary tumor and distant metastasis, particularly in the HER2-negative (HER2-low and HER2-zero) primary breast cancer collective. Secondary objectives of our analysis were (i) that discordance rates differ according to the molecular subtype of the primary tumor, (ii) that discordance rates differ according to the site of distant metastasis, and (iii) the discordance rate in PMBC is lower than in SMBC. The relationship between the different categorical variables was determined by cross-tabulation. Comparisons between different HER2 status (primary tumor and metastasis) were calculated by Cohen’s Kappa coefficient. Relationships between HER2 status for primary tumor and clinico-pathological parameters were assessed by cross-tabulation and using Pearson’s chi-squared test (χ2 test). Statistical analyses were performed using the SPSS statistical software program, version 27.0 (SPSS Inc., Chicago, IL, USA), and the statistical language R, version 4.1.2 [57]. Patients’ characteristics were given in absolute and relative numbers. All p-values are two-sided. Because no correction was made for multiple testing due to the exploratory nature of the study, these are descriptive measures that should be interpreted with caution.
3. Results
3.1. Patient Population
The final study cohort included 148 paired samples. Primary tumors were divided into 127 (85.8%) HER2-negative samples [49 HER2-zero (38.6%) and 78 HER2-low (61.4%)] and 21 (14.2%) HER2-positive samples (Figure 1). One-hundred and seven (72.3%) primary tumors showed a luminal-like phenotype, 21 (14.2%) were HER2-positive, and 20 (13.5%) had a triple-negative phenotype. PMBC occurred in 35.8% (n = 53), and more frequently in the HER2-low (58.5%, n = 31) than in the HER2-zero cohort (15.1%, n = 8). The median time to first metastasis was 25 months (range 0–150). The median time between diagnosis of metastatic disease and biopsy was one month (range 0–131). Metastases were located in the liver (n = 50, 33.8%), bone (n = 38, 25.7%), skin/soft tissue (n = 18, 12.2%), central nervous system (CNS) (n = 15, 10.1%), other sites (n = 13, 8.8%), lung/pleura (n = 9, 6.1%), and lymph nodes (n = 5, 3.4%). Seventy-nine (53.4%) patients received adjuvant endocrine therapy and 72 (48.6%) neo-/adjuvant chemotherapy. A small proportion of patients were treated with adjuvant anti-HER2 therapy (n = 9, 6.1%). At the time of metastatic biopsy, 35.1% (n = 52) of patients were receiving endocrine therapy, 30.4% (n = 45) chemotherapy, and/or 8.8% (n = 13) anti-HER2 therapy for metastatic disease. Compared with HER2-zero and HER2-positive phenotype, HER2-low was significantly less frequently diagnosed in larger tumors (>T2) (HER2-low 66.0% vs. HER2-zero 77.1% and HER2-positive 85.6%, p = 0.032) and poorly differentiated tumors (G3) (HER2-low 33.3% vs. HER2-zero 49.0% and HER2-positive 60.0%, p = 0.049). HER2-low status was more common in tumors with higher Ki-67 (>20%) compared with HER2-zero (82.7% vs. 64.3%). However, higher Ki-67 levels were most frequently found in the HER2-positive cohort (100%) (p = 0.022). Low HER2 was significantly more common in luminal-like tumors than in triple-negative tumors (88.5% vs. 11.5%), while conversely, HER2-zero was more common in triple-negative tumors (22.4% vs. 11.5%) (p < 0.001). Additional tumor and patient characteristics are listed in Table 1.
3.2. Change of HER2 Status between Primary Breast Cancer and Metastasis
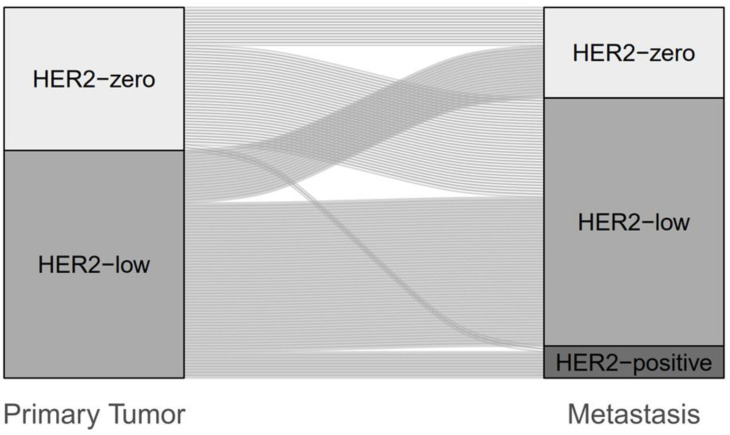
In the HER2-negative cohort, the HER2-low phenotype represented the largest group [primary tumor 61.4% (n = 78), metastatic samples 73.5% (n = 86)]. Discordance in HER2 status between the primary tumor and the matched metastatic biopsy was 49.6% (n = 63) (Kappa −0.003, 95%CI −0.15–0.15). Development of the HER2-low phenotype (HER2-zero to HER2-low or HER2-low to HER2-zero) was most common (n = 52, 40.9%), especially with enrichment to HER2-low (n = 34, 26.8%) (Figure 2 and Table S1).
Figure 2.
Change of HER2 status between primary tumor and metastasis in the HER2-negative cohort (n = 127).
In the entire cohort (n = 148), HER2 discordance was 43.2% (n = 64) (Kappa 0.270, 95%CI 0.14–0.41). Most frequently, an evolution from HER2-zero to HER2-low phenotype was observed (n = 34, 23.0%). Within the HER2-zero cohort, this represented a switch of 69.4% from HER2-zero to HER2-low. A change from HER2-low to HER2-zero occurred in 12.2% (n = 18). Considered for the HER2-low cohort alone, a switch from HER2-low to HER2-zero resulted in 23.1%. The HER2-positive cohort showed the greatest stability, with a discordance of 4.8% (n = 1 of 21) (Table S2 and Figure S1). When additional metastatic biopsies were performed, a discordance rate of 57.9% was observed compared with the previous biopsy (Table 1). Again, the most common finding was a change from HER2-zero to HER2-low (15.8%; within the HER2-zero cohort: 60.0%).
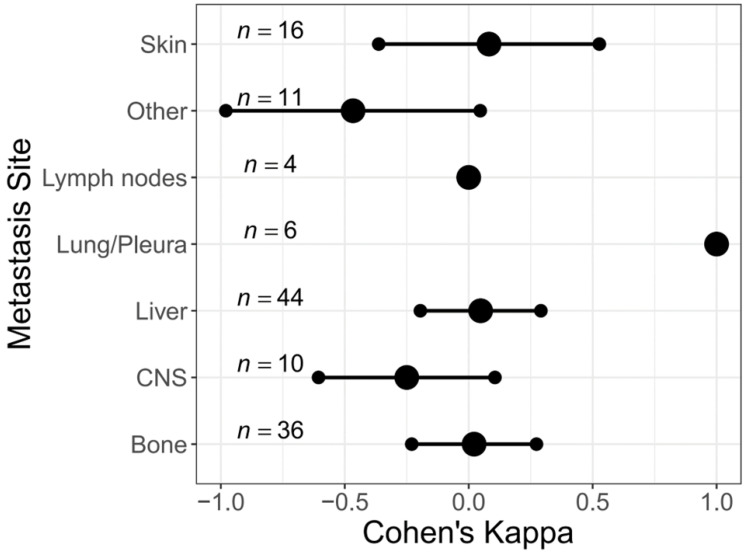
3.3. Change of HER2 Status in Different Metastatic Sites
The proportion of HER2-low did not differ significantly between the different metastatic sites (p = 0.349) (Table 1). In the HER2-negative population, a relevant HER2 discordance rate was observed between the different metastatic sites (bone: Kappa 0.022, -0.230–0.273; liver: Kappa 0.048, −0.195–0.291; skin/soft tissue: Kappa 0.082, −0.363–0.527, lymph node: Kappa 0.000; CNS: Kappa −0.250, −0.606–0.106; others: Kappa −0.467, −0.980–0.047). Only pulmonary/pleural metastases showed absolute concordance with the primary breast tumor (Kappa 1.0, 95%CI 1.0–1.0). An increase from HER2-zero to HER2-low at metastatic biopsy was most frequently detected, excluding bone metastases. A switch to HER2 positive has been observed especially in CNS metastases (n = 2, 20.0%) (Table S3 and Figure 3).
Figure 3.
Change of HER2 status in different metastatic sites in the HER2-negative cohort (n = 127).
Similarly, there was a relevant change in HER2 expression in the entire cohort (Table S4 and Figure S2).
3.4. Change of HER2 Status in Different Molecular Subtypes
HER2 discordance was observed according to the molecular subtype, in the Luminal A/B cohort (Kappa −0.044, −0.202–0.114) and in triple-negative breast cancer (Kappa 0.107, −0.247–0.461). In both subcohorts, a switch from HER2-zero to HER2-low was most frequently detected (Luminal A/B n = 28, 26.2%; Triple-negative n = 6, 30.0%) (Table S5 and Figure S3).
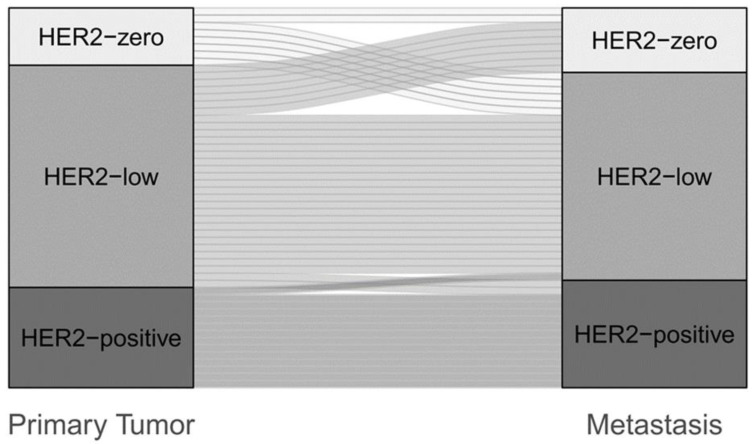
3.5. Change of HER2 Status in Primary vs. Secondary Metastatic Breast Cancer
PMBC was evidenced in 35.8% (n = 53). HER2-low represented the largest proportion in both the primary tumor (58.5%, n = 31) and matched de-novo metastases (54.7%, n = 29). The de-novo cohort showed a higher prevalence of HER2-low expression in PT (58.5%, n = 31) than in the relapsed collective (49.5%, n = 47). The HER2-low phenotype was represented more frequently in secondary metastases than in de-novo metastases (60.0% vs. 54.7%) (Tables S6 and S7). The discordance rate was lower in the PMBC than in the SMBC cohort [30.2% (Kappa 0.48, 95%CI 0.27–0.69) vs. 50.5% (Kappa 0.14, 95% CI −0.03–0.32)]. In the de-novo cohort, the increase almost corresponded to the loss of HER2 expression (11.3% vs. 13.2%), whereas in the SMBC cohort, the change from HER2-zero to HER2-low clearly predominated (29.5% vs. 11.6%) (Figure 4, Tables S6 and S7).
Figure 4.
Change of HER2 status between primary tumor and metastasis in the de-novo cohort (n = 53).
4. Discussion
In our retrospective analysis, we showed a relevant discordance rate of HER2 status between primary breast cancer and distant metastases, with the conversion from HER2-zero to HER2-low observed most frequently. Recently published studies have addressed the heterogeneity of HER2-negative breast cancer, focusing on the HER2-negative cohort [17,19,20,28]. The need to relativize the traditional dichotomization between HER2-positive and HER2-negative appeared at the latest with the results of the DESTINY-Breast04 trial, which demonstrated the superiority of trastuzumab-deruxtecan (T-DXd) vs. chemotherapy of the physician’s choice in patients with advanced HER2-low breast cancer [37]. In addition, other HER2-targeting ADCs like trastuzumab duocarmazine showed promising activity in early studies [58]. In our previous study, we reported a rate of 48.3% HER2-low tumors, which was within the range of approximately half of HER2-negative breast cancer patients (31.0% to 60.6%) reported by Prat and coworkers in a recent review article [20,58]. Since 80–85% of all breast cancer tumors have a HER2-negative phenotype, which was 85.2% in our study, a better understanding of this cohort has potential therapeutic implications for the majority of breast cancer patients. In this context, the aspect of the evolution of HER2 expression from early to advanced breast cancer is important. In the present study, we demonstrated a discordance rate between HER2 status of primarytumors and associated distant metastases within the HER2-negative cohort of 49.6% (Kappa −0.003, 95%CI −0.15–0.15). The development of HER2-low occurred frequently (40.9%), particularly with a switch from HER2-zero to HER2-low (26.8%). Discordance rates from our study were slightly higher than in other studies (38.0% and 40.9%, respectively [52,59]. However, all studies showed an increase in HER2 expression from HER2-zero to HER2-low during disease progression. Our results of additional metastatic biopsies compared with initial metastatic biopsies point in the same direction, with a discordance rate of 57.9%. There are several hypotheses for low HER2 stability (e.g., genetic drift and clonal evolution during tumor progression, intratumoral heterogeneity, and the selective effect of administered therapies) leading to the enrichment of HER2 expression [41,60,61,62,63,64,65,66]. Our study cohort showed heterogeneity in terms of time to metastasis, with a significantly longer time in the HER2-zero cohort than in the HER2-low cohort [median 44 months (0–150) vs. 14 months (0–121)] and in terms of systemic treatments given. Neo-/adjuvant chemotherapy was significantly more common in the HER2-zero than in the HER2-low cohort (71.4% vs. 38.5%, p < 0.001). Both aspects may have an impact on the increase of HER2-low from a primary tumor to distant metastases. In our study, there were no significant differences in HER2-low expression depending on the metastatic site (p = 0.349). Comparable to our results, Tarantino and coworkers also found no significant difference in HER2-low expression at different metastatic sites (p = 0.88), even when they divided biopsy sites into visceral (liver, lung, and pleura) and nonvisceral (skin and soft tissues, lymph nodes, bone, other) (p = 0.56) [32]. Miglietta et al. examined locoregional recurrences in addition to HER2-low prevalence in various distant metastases, also with similar results for HER2-low [52]. However, in Miglietta′s cohort, a significant difference in discordance rates was observed between the different metastases (p = 0.001), with the greatest HER2 instability in liver and bone metastases and the greatest concordance in lung and CNS metastases. Lung/pleural metastases also had the strongest concordance in our study. In the HER2-negative cohort, discordance rates ranged from 40.9% (liver) to 80.0% (CNS). The HER2 score changed from HER2-zero to HER2-low most frequently at metastatic biopsy, except for bone metastases, which is in contrast to the results of Lin et al. [66]. Overall, the aspects of similar HER2 expression levels at different metastatic sites and the different discordance rates are of clinical importance when a metastatic site has to be selected for biopsy to decide on targeted therapies that are also effective in HER2-low tumors. Another objective of our study was to analyze whether discordance rates depend on the molecular subtype of the primary BC. Recently published studies that examined discordance rates as a function of the molecular subtype of the primary tumor showed that HER2-low was more common in HR-positive tumors than in triple-negative tumors [22,32,52,59,67,68]. Similarly, the HR-positive subtype was associated with a higher discordance rate, most frequently switching from HER2-zero to HER2-low [32,52]. In our study, HER2-low was also significantly more common in luminal-like tumors than in triple-negative tumors, although the difference was much greater than in the above studies.
A particular aspect of our study was the evaluation of PMBC, which we assessed for HER2-low prevalence and discordance rates. Compared to SMBC, PMBC had a significantly lower discordance rate between the PT and matched metastases [30.2% (Kappa 0.48, 95%CI 0.27–0.69) versus 50.5% (Kappa 0.14, 95% CI −0.03–0.32)]. While an increase in HER2 expression between primary tumor and distant metastases was observed across the cohort in our study, this trend was not observed in PMBC, supporting the hypothesis of HER2 enrichment during tumor progression. Overall, not all studies clearly addressed PMBC [52], excluded de-novo tumors, or applied various de-novo definitions (e.g., <6 months) [32,59]. Therefore, a comparison between our results and those of other studies is difficult. Although the de novo cohort of our study was small (n = 53), the aspect of low HER2 instability should also receive attention in de novo metastatic BC. In this regard, further studies with larger study cohorts are needed.
Our study has several limitations, such as the retrospective and unicenter setting. Another limitation is the lack of a central pathology assessment given the low interobserver reproducibility, especially in HER2-low and HER2-zero [69]. In addition, we did not investigate a possible prognostic impact of HER2 discordance between the primary tumor and the corresponding distant metastases. However, the consecutive inclusion of matched pairs is a strength. In addition, we examined the impact of both the site of distant metastases and molecular subtypes and took a closer look at the PMBC group.
5. Conclusions
In summary, we have shown in our study that there is a significant discordance rate between HER2-negative primary breast cancer and the corresponding metastases, with HER2-zero tumors more likely to become HER2-low tumors at advanced stages. In contrast, there is less discordance in PMBC. This evolution of HER2 expression is a clinically relevant rationale for metastatic biopsy and offers patients the opportunity to receive an effective treatment such as trastuzumab-deruxtecan.
Acknowledgments
This work contains parts of the doctoral thesis of Lisa Krauthauser.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15051413/s1, Table S1: Change of HER2 status between primary tumor and metastasis in the HER2-negative cohort (n = 127); Table S2: Change of HER2 status between primary tumor and metastasis in the entire cohort (n = 148); Table S3: Change of HER2 status in different metastatic sites in the HER2-negative cohort (n = 127); Table S4: Change of HER2 status in different metastatic sites (n = 148); Table S5: Change of HER-2 in different molecular subtypes (luminal-like and triple-negative) (n = 127); Table S6: Change of HER2 status between primary tumor and metastasis in the de-novo cohort (n = 53); Table S7: Change of HER2 status between primary tumor and metastasis in the secondary metastastic breast cancer cohort (n = 95); Figure S1: Change of HER2 status between primary tumor and metastasis in the entire cohort (n = 148); Figure S2: Change of HER2 status in different metastatic sites (n = 148); Figure S3: Change of HER-2 in different molecular subtypes (luminal-like and triple-negative) (n = 127).
Author Contributions
Conceptualization, K.A. (Katrin Almstedt) and M.S.; methodology, K.A. (Katrin Almstedt), F.K., J.R. and M.S.; validation, K.A. (Katrin Almstedt) and M.S.; formal analysis, K.A. (Katrin Almstedt), L.K., F.K., D.-C.W., J.R., W.R. and M.S.; investigation, D.-C.W., W.R. and M.S.; resources, W.B., A.H. and M.S.; data curation, K.A. (Katrin Almstedt), F.K., J.R., K.S. and M.S.; writing—original draft preparation, K.A. (Katrin Almstedt) and M.S.; writing—review and editing, K.A. (Katrin Almstedt), L.K., F.K., D.-C.W., A.-S.H., M.J.B., K.A. (Katharina Anic), S.K., A.L., R.S., W.B., W.W., J.R., J.G.H., W.R., A.H., K.S. and M.S.; visualization, K.A. (Katrin Almstedt) and F.K.; supervision, M.S.; project administration, K.A. (Katrin Almstedt). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Rhineland-Palatinate Medical Association, Germany (2021-15657, ethical approval date 08.04.2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset analyzed during the current study is available from the corresponding author upon reasonable request.
Conflicts of Interest
K.A. received speaker honoraria from Roche Pharma AG, Pfizer Pharma GmbH, Seagen, Med publico GmbH, and Astra Zeneca. D.-C.W. received speaker honoraria from Roche, BMS, MSD, and Janssen. He received funded research from Roche and BMS. A.-S.H. received speaker honoraria from Pfizer Pharma GmbH and honoraria from Medupdate GmbH. M.J.B. received honoraria and expenses from Astra Zeneca, Clovis Oncology, GSK, MSD, Pharma Mar, Roche, and Tesaro Bio Germany GmbH. He is a consultant to Eisai, GSK, MSD, Pharma Mar, Roche Pharma AG, and Tesaro Bio Germany GmbH. He received funded research from Astra Zeneca, Clovis Oncology, MSD, and Novartis. S.K. received speaker honoraria from Roche Pharma AG and Novartis Pharma GmbH Germany, research funding from Novartis Pharma GmbH Germany, and travel reimbursement from Pharma Mar and Novartis Pharma GmbH Germany. A.H. received honoraria from Astra Zeneca, Celgene, MedConcept Gm, Med update GmbH, Medicultus, Pfizer, Promedicis GmbH, Pierre Fabre, Softconsult, Roche Pharma AG, Streamedup!GmbH and Tesaro Bio Germany GmbH. She is a member of the advisory board of Pharma Mar, Promedicis GmbH, Pierre Fabre Pharma GmbH, Roche Pharma AG, and Tesaro Bio Germany GmbH. She received research funding from Celgene. M.S. reports personal fees from Astra Zeneca, BioNTech, Daiichi Sankyo, Eisai, Lilly, MSD, Novartis, Pantarhei Bioscience, Pfizer, Roche, and SeaGen outside the submitted work. Institutional research funding from Astra Zeneca, BioNTech, Eisai, Genentech, German Breast Group, Novartis, Palleos, Pantarhei Bioscience, Pierre Fabre, and SeaGen. In addition, Marcus Schmidt has a patent for EP 2390370 B1 issued and a patent for EP 2951317 B1 issued. All other authors declare that they have no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Slamon D.J., Clark G.M., Wong S.G., Levin W.J., Ullrich A., McGuire W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–182. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 2.Slamon D.J., Godolphin W., Jones L.A., Holt J.A., Wong S.G., Keith D.E., Levin W.J., Stuart S.G., Udove J., Ullrich A. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244:707–712. doi: 10.1126/science.2470152. [DOI] [PubMed] [Google Scholar]
- 3.Slamon D.J., Leyland-Jones B., Shak S., Fuchs H., Paton V., Bajamonde A., Fleming T., Eiermann W., Wolter J., Pegram M., et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N. Engl. J. Med. 2001;344:783–792. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 4.Baselga J., Cortés J., Kim S.-B., Im S.-A., Hegg R., Im Y.-H., Roman L., Pedrini J.L., Pienkowski T., Knott A., et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N. Engl. J. Med. 2012;366:109–119. doi: 10.1056/NEJMoa1113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geyer C.E., Forster J., Lindquist D., Chan S., Romieu C.G., Pienkowski T., Jagiello-Gruszfeld A., Crown J., Chan A., Kaufman B., et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N. Engl. J. Med. 2006;355:2733–2743. doi: 10.1056/NEJMoa064320. [DOI] [PubMed] [Google Scholar]
- 6.Murthy R.K., Loi S., Okines A., Paplomata E., Hamilton E., Hurvitz S.A., Lin N.U., Borges V., Abramson V., Anders C., et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2020;382:597–609. doi: 10.1056/NEJMoa1914609. [DOI] [PubMed] [Google Scholar]
- 7.Cortés J., Kim S.-B., Chung W.-P., Im S.-A., Park Y.H., Hegg R., Kim M.H., Tseng L.-M., Petry V., Chung C.-F., et al. Trastuzumab Deruxtecan versus Trastuzumab Emtansine for Breast Cancer. N. Engl. J. Med. 2022;386:1143–1154. doi: 10.1056/NEJMoa2115022. [DOI] [PubMed] [Google Scholar]
- 8.Verma S., Miles D., Gianni L., Krop I.E., Welslau M., Baselga J., Pegram M., Oh D.-Y., Diéras V., Guardino E., et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N. Engl. J. Med. 2012;367:1783–1791. doi: 10.1056/NEJMoa1209124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trastuzumab for early-stage, HER2-positive breast cancer: A meta-analysis of 13 864 women in seven randomised trials. Lancet Oncol. 2021;22:1139–1150. doi: 10.1016/S1470-2045(21)00288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paik S., Kim C., Wolmark N. HER2 status and benefit from adjuvant trastuzumab in breast cancer. N. Engl. J. Med. 2008;358:1409–1411. doi: 10.1056/NEJMc0801440. [DOI] [PubMed] [Google Scholar]
- 11.Perez E.A., Reinholz M.M., Hillman D.W., Tenner K.S., Schroeder M.J., Davidson N.E., Martino S., Sledge G.W., Harris L.N., Gralow J.R., et al. HER2 and chromosome 17 effect on patient outcome in the N9831 adjuvant trastuzumab trial. J. Clin. Oncol. 2010;28:4307–4315. doi: 10.1200/JCO.2009.26.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fehrenbacher L., Cecchini R.S., Geyer C.E., Rastogi P.J.R., Costantino J.P., Atkins J.N., Crown J.P., Polikoff J., Boileau J.-F., Provencher L., et al. NSABP B-47/NRG Oncology Phase III Randomized Trial Comparing Adjuvant Chemotherapy With or Without Trastuzumab in High-Risk Invasive Breast Cancer Negative for HER2 by FISH and With IHC 1+ or 2. J. Clin. Oncol. 2020;38:444–453. doi: 10.1200/JCO.19.01455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gianni L., Pienkowski T., Im Y.-H., Tseng L.-M., Liu M.-C., Lluch A., Starosławska E., de La Haba-Rodriguez J., Im S.-A., Pedrini J.L., et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): A multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17:791–800. doi: 10.1016/S1470-2045(16)00163-7. [DOI] [PubMed] [Google Scholar]
- 14.von Minckwitz G., Procter M., de Azambuja E., Zardavas D., Benyunes M., Viale G., Suter T., Arahmani A., Rouchet N., Clark E., et al. Adjuvant Pertuzumab and Trastuzumab in Early HER2-Positive Breast Cancer. N. Engl. J. Med. 2017;377:122–131. doi: 10.1056/NEJMoa1703643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan A., Delaloge S., Holmes F.A., Moy B., Iwata H., Harvey V.J., Robert N.J., Silovski T., Gokmen E., von Minckwitz G., et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): A multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17:367–377. doi: 10.1016/S1470-2045(15)00551-3. [DOI] [PubMed] [Google Scholar]
- 16.von Minckwitz G., Huang C.-S., Mano M.S., Loibl S., Mamounas E.P., Untch M., Wolmark N., Rastogi P., Schneeweiss A., Redondo A., et al. Trastuzumab Emtansine for Residual Invasive HER2-Positive Breast Cancer. N. Engl. J. Med. 2019;380:617–628. doi: 10.1056/NEJMoa1814017. [DOI] [PubMed] [Google Scholar]
- 17.Li Y., Abudureheiyimu N., Mo H., Guan X., Lin S., Wang Z., Chen Y., Chen S., Li Q., Cai R., et al. In Real Life, Low-Level HER2 Expression May Be Associated With Better Outcome in HER2-Negative Breast Cancer: A Study of the National Cancer Center, China. Front. Oncol. 2021;11:774577. doi: 10.3389/fonc.2021.774577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mutai R., Barkan T., Moore A., Sarfaty M., Shochat T., Yerushalmi R., Stemmer S.M., Goldvaser H. Prognostic impact of HER2-low expression in hormone receptor positive early breast cancer. Breast. 2021;60:62–69. doi: 10.1016/j.breast.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denkert C., Seither F., Schneeweiss A., Link T., Blohmer J.-U., Just M., Wimberger P., Forberger A., Tesch H., Jackisch C., et al. Clinical and molecular characteristics of HER2-low-positive breast cancer: Pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol. 2021;22:1151–1161. doi: 10.1016/S1470-2045(21)00301-6. [DOI] [PubMed] [Google Scholar]
- 20.Almstedt K., Heimes A.-S., Kappenberg F., Battista M.J., Lehr H.-A., Krajnak S., Lebrecht A., Gehrmann M., Stewen K., Brenner W., et al. Long-term prognostic significance of HER2-low and HER2-zero in node-negative breast cancer. Eur. J. Cancer. 2022;173:10–19. doi: 10.1016/j.ejca.2022.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Rosso C., Voutsadakis I.A. Characteristics, Clinical Differences and Outcomes of Breast Cancer Patients with Negative or Low HER2 Expression. Clin. Breast Cancer. 2022;22:391–397. doi: 10.1016/j.clbc.2022.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Tan R.S.Y.C., Ong W.S., Lee K.-H., Lim A.H., Park S., Park Y.H., Lin C.-H., Lu Y.-S., Ono M., Ueno T., et al. HER2 expression, copy number variation and survival outcomes in HER2-low non-metastatic breast cancer: An international multicentre cohort study and TCGA-METABRIC analysis. BMC Med. 2022;20:105. doi: 10.1186/s12916-022-02284-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tarantino P., Niman S.M., Erick T.K., Priedigkeit N., Harrison B.T., Giordano A., Nakhlis F., Bellon J.R., Parker T., Strauss S., et al. HER2-low inflammatory breast cancer: Clinicopathologic features and prognostic implications. Eur. J. Cancer. 2022;174:277–286. doi: 10.1016/j.ejca.2022.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Chen M., Chen W., Liu D., Chen W., Shen K., Wu J., Zhu L. Prognostic values of clinical and molecular features in HER2 low-breast cancer with hormonal receptor overexpression: Features of HER2-low breast cancer. Breast Cancer. 2022;29:844–853. doi: 10.1007/s12282-022-01364-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Douganiotis G., Kontovinis L., Markopoulou E., Ainali A., Zarampoukas T., Natsiopoulos I., Papazisis K. Prognostic Significance of Low HER2 Expression in Patients With Early Hormone Receptor Positive Breast Cancer. Cancer Diagn. Progn. 2022;2:316–323. doi: 10.21873/cdp.10111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horisawa N., Adachi Y., Takatsuka D., Nozawa K., Endo Y., Ozaki Y., Sugino K., Kataoka A., Kotani H., Yoshimura A., et al. The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer. 2021;29:234–241. doi: 10.1007/s12282-021-01303-3. [DOI] [PubMed] [Google Scholar]
- 27.Jacot W., Maran-Gonzalez A., Massol O., Sorbs C., Mollevi C., Guiu S., Boissière-Michot F., Ramos J. Prognostic Value of HER2-Low Expression in Non-Metastatic Triple-Negative Breast Cancer and Correlation with Other Biomarkers. Cancers. 2021;13:6059. doi: 10.3390/cancers13236059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agostinetto E., Rediti M., Fimereli D., Debien V., Piccart M., Aftimos P., Sotiriou C., de Azambuja E. HER2-Low Breast Cancer: Molecular Characteristics and Prognosis. Cancers (Basel) 2021;13:2824. doi: 10.3390/cancers13112824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schettini F., Chic N., Brasó-Maristany F., Paré L., Pascual T., Conte B., Martínez-Sáez O., Adamo B., Vidal M., Barnadas E., et al. Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer. 2021;7:1. doi: 10.1038/s41523-020-00208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shao Y., Yu Y., Luo Z., Guan H., Zhu F., He Y., Chen Q., Liu C., Nie B., Liu H. Clinical, Pathological Complete Response, and Prognosis Characteristics of HER2-Low Breast Cancer in the Neoadjuvant Chemotherapy Setting: A Retrospective Analysis. Ann. Surg. Oncol. 2022;29:8026–8034. doi: 10.1245/s10434-022-12369-4. [DOI] [PubMed] [Google Scholar]
- 31.Shu L., Tong Y., Li Z., Chen X., Shen K. Can HER2 1+ Breast Cancer Be Considered as HER2-Low Tumor? A Comparison of Clinicopathological Features, Quantitative HER2 mRNA Levels, and Prognosis among HER2-Negative Breast Cancer. Cancers. 2022;14:4250. doi: 10.3390/cancers14174250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarantino P., Gandini S., Nicolò E., Trillo P., Giugliano F., Zagami P., Vivanet G., Bellerba F., Trapani D., Marra A., et al. Evolution of low HER2 expression between early and advanced-stage breast cancer. Eur. J. Cancer. 2022;163:35–43. doi: 10.1016/j.ejca.2021.12.022. [DOI] [PubMed] [Google Scholar]
- 33.van den Ende N.S., Smid M., Timmermans A., van Brakel J.B., Hansum T., Foekens R., Trapman A.M.A.C., Heemskerk-Gerritsen B.A.M., Jager A., Martens J.W.M., et al. HER2-low breast cancer shows a lower immune response compared to HER2-negative cases. Sci. Rep. 2022;12:12974. doi: 10.1038/s41598-022-16898-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Won H.S., Ahn J., Kim Y., Kim J.S., Song J.-Y., Kim H.-K., Lee J., Park H.K., Kim Y.-S. Clinical significance of HER2-low expression in early breast cancer: A nationwide study from the Korean Breast Cancer Society. Breast Cancer Res. 2022;24:22. doi: 10.1186/s13058-022-01519-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu H., Han Y., Wu Y., Wang Y., Li Q., Zhang P., Yuan P., Luo Y., Fan Y., Chen S., et al. Clinicopathological Characteristics and Prognosis of HER2-Low Early-Stage Breast Cancer: A Single-Institution Experience. Front. Oncol. 2022;12:906011. doi: 10.3389/fonc.2022.906011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gampenrieder S.P., Dezentjé V., Lambertini M., de Nonneville A., Marhold M., Le Du F., Cortés Salgado A., Alpuim Costa D., Vaz Batista M., Chic Ruché N., et al. Influence of HER2 expression on prognosis in metastatic triple-negative breast cancer-results from an international, multicenter analysis coordinated by the AGMT Study Group. ESMO Open. 2022;8:100747. doi: 10.1016/j.esmoop.2022.100747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Modi S., Jacot W., Yamashita T., Sohn J., Vidal M., Tokunaga E., Tsurutani J., Ueno N.T., Prat A., Chae Y.S., et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N. Engl. J. Med. 2022;387:9–20. doi: 10.1056/NEJMoa2203690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moy B., Rumble R.B., Carey L.A. Chemotherapy and Targeted Therapy for Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer That Is Either Endocrine-Pretreated or Hormone Receptor-Negative: ASCO Guideline Rapid Recommendation Update. J. Clin. Oncol. 2022;40:3088–3090. doi: 10.1200/JCO.22.01533. [DOI] [PubMed] [Google Scholar]
- 39.ESMO EMA Recommends Extension of Therapeutic Indications for Trastuzumab Deruxtecan. European Society for Medical Oncology (ESMO) [Online] Dec 22, 2022. [(accessed on 4 January 2023)]. Available online: https://www.esmo.org/oncology-news/ema-recommends-extension-of-therapeutic-indications-for-trastuzumab-deruxtecan2.
- 40.Wolff A.C., Hammond M.E.H., Allison K.H., Harvey B.E., Mangu P.B., Bartlett J.M.S., Bilous M., Ellis I.O., Fitzgibbons P., Hanna W., et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J. Clin. Oncol. 2018;36:2105–2122. doi: 10.1200/JCO.2018.77.8738. [DOI] [PubMed] [Google Scholar]
- 41.Grassini D., Cascardi E., Sarotto I., Annaratone L., Sapino A., Berrino E., Marchiò C. Unusual Patterns of HER2 Expression in Breast Cancer: Insights and Perspectives. Pathobiology. 2022;89:278–296. doi: 10.1159/000524227. [DOI] [PubMed] [Google Scholar]
- 42.Denkert C., Lebeau A., Schildhaus H.U., Jackisch C., Rüschoff J. New treatment options for metastatic HER2-low breast cancer: Consequences for histopathological diagnosis. Pathologie (Heidelb) 2022 doi: 10.1007/s00292-022-01139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schrijver W.A.M.E., Suijkerbuijk K.P.M., van Gils C.H., van der Wall E., Moelans C.B., van Diest P.J. Receptor Conversion in Distant Breast Cancer Metastases: A Systematic Review and Meta-analysis. J. Natl. Cancer Inst. 2018;110:568–580. doi: 10.1093/jnci/djx273. [DOI] [PubMed] [Google Scholar]
- 44.Chen R., Qarmali M., Siegal G.P., Wei S. Receptor conversion in metastatic breast cancer: Analysis of 390 cases from a single institution. Mod. Pathol. 2020;33:2499–2506. doi: 10.1038/s41379-020-0615-z. [DOI] [PubMed] [Google Scholar]
- 45.Aurilio G., Disalvatore D., Pruneri G., Bagnardi V., Viale G., Curigliano G., Adamoli L., Munzone E., Sciandivasci A., de Vita F., et al. A meta-analysis of oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 discordance between primary breast cancer and metastases. Eur. J. Cancer. 2014;50:277–289. doi: 10.1016/j.ejca.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 46.Guarneri V., Dieci M.V., Barbieri E., Piacentini F., Omarini C., Ficarra G., Bettelli S., Conte P.F. Loss of HER2 positivity and prognosis after neoadjuvant therapy in HER2-positive breast cancer patients. Ann. Oncol. 2013;24:2990–2994. doi: 10.1093/annonc/mdt364. [DOI] [PubMed] [Google Scholar]
- 47.Mittendorf E.A., Wu Y., Scaltriti M., Meric-Bernstam F., Hunt K.K., Dawood S., Esteva F.J., Buzdar A.U., Chen H., Eksambi S., et al. Loss of HER2 amplification following trastuzumab-based neoadjuvant systemic therapy and survival outcomes. Clin Cancer Res. 2009;15:7381–7388. doi: 10.1158/1078-0432.CCR-09-1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tural D., Karaca M., Zirtiloglu A., Hacioglu B.M., Sendur M.A., Ozet A. Receptor discordances after neoadjuvant chemotherapy and their effects on survival. J. BUON. 2019;24:20–25. [PubMed] [Google Scholar]
- 49.Wang R.-X., Chen S., Jin X., Chen C.-M., Shao Z.-M. Weekly paclitaxel plus carboplatin with or without trastuzumab as neoadjuvant chemotherapy for HER2-positive breast cancer: Loss of HER2 amplification and its impact on response and prognosis. Breast Cancer Res. Treat. 2017;161:259–267. doi: 10.1007/s10549-016-4064-9. [DOI] [PubMed] [Google Scholar]
- 50.Ignatov T., Gorbunow F., Eggemann H., Ortmann O., Ignatov A. Loss of HER2 after HER2-targeted treatment. Breast Cancer Res. Treat. 2019;175:401–408. doi: 10.1007/s10549-019-05173-4. [DOI] [PubMed] [Google Scholar]
- 51.Branco F.P., Machado D., Silva F.F., André S., Catarino A., Madureira R., Pinto J.M., Godinho J.P., Simões P.D., Brito M., et al. Loss of HER2 and disease prognosis after neoadjuvant treatment of HER2+ breast cancer. Am. J. Transl. Res. 2019;11:6110–6116. [PMC free article] [PubMed] [Google Scholar]
- 52.Miglietta F., Griguolo G., Bottosso M., Giarratano T., Lo Mele M., Fassan M., Cacciatore M., Genovesi E., de Bartolo D., Vernaci G., et al. Evolution of HER2-low expression from primary to recurrent breast cancer. NPJ Breast Cancer. 2021;7:137. doi: 10.1038/s41523-021-00343-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andre F., Slimane K., Bachelot T., Dunant A., Namer M., Barrelier A., Kabbaj O., Spano J.P., Marsiglia H., Rouzier R., et al. Breast cancer with synchronous metastases: Trends in survival during a 14-year period. J. Clin. Oncol. 2004;22:3302–3308. doi: 10.1200/JCO.2004.08.095. [DOI] [PubMed] [Google Scholar]
- 54.Barinoff J., Schmidt M., Schneeweiss A., Schoenegg W., Thill M., Keitel S., Lattrich C.R., Hinke A., Kutscheidt A., Jackisch C. Primary metastatic breast cancer in the era of targeted therapy—Prognostic impact and the role of breast tumour surgery. Eur. J. Cancer. 2017;83:116–124. doi: 10.1016/j.ejca.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 55.Allison K.H., Hammond M.E.H., Dowsett M., McKernin S.E., Carey L.A., Fitzgibbons P.L., Hayes D.F., Lakhani S.R., Chavez-MacGregor M., Perlmutter J., et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 2020;38:1346–1366. doi: 10.1200/JCO.19.02309. [DOI] [PubMed] [Google Scholar]
- 56.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 57.R Core Team R: A Language and Environment for Statistical Computing. [(accessed on 5 October 2022)]. Available online: https://www.R-project.org/
- 58.Prat A., Bardia A., Curigliano G., Hammond M.E.H., Loibl S., Tolaney S.M., Viale G. An Overview of Clinical Development of Agents for Metastatic or Advanced Breast Cancer Without ERBB2 Amplification (HER2-Low) JAMA Oncol. 2022;8:1676–1687. doi: 10.1001/jamaoncol.2022.4175. [DOI] [PubMed] [Google Scholar]
- 59.de Calbiac O., Lusque A., Mailliez A., Bachelot T., Uwer L., Mouret-Reynier M.-A., Emile G., Jouannaud C., Gonçalves A., Patsouris A., et al. Comparison of Management and Outcomes in ERBB2 -Low vs ERBB2 -Zero Metastatic Breast Cancer in France. JAMA Netw. Open. 2022;5:e2231170. doi: 10.1001/jamanetworkopen.2022.31170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marchiò C., Annaratone L., Marques A., Casorzo L., Berrino E., Sapino A. Evolving concepts in HER2 evaluation in breast cancer: Heterogeneity, HER2-low carcinomas and beyond. Semin. Cancer Biol. 2021;72:123–135. doi: 10.1016/j.semcancer.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 61.Shah S.P., Morin R.D., Khattra J., Prentice L., Pugh T., Burleigh A., Delaney A., Gelmon K., Guliany R., Senz J., et al. Mutational evolution in a lobular breast tumour profiled at single nucleotide resolution. Nature. 2009;461:809–813. doi: 10.1038/nature08489. [DOI] [PubMed] [Google Scholar]
- 62.Kan S., Koido S., Okamoto M., Hayashi K., Ito M., Kamata Y., Komita H., Ishidao T., Nagasaki E., Homma S. Gemcitabine treatment enhances HER2 expression in low HER2-expressing breast cancer cells and enhances the antitumor effects of trastuzumab emtansine. Oncol. Rep. 2015;34:504–510. doi: 10.3892/or.2015.3974. [DOI] [PubMed] [Google Scholar]
- 63.Knowlden J.M., Hutcheson I.R., Jones H.E., Madden T., Gee J.M.W., Harper M.E., Barrow D., Wakeling A.E., Nicholson R.I. Elevated levels of epidermal growth factor receptor/c-erbB2 heterodimers mediate an autocrine growth regulatory pathway in tamoxifen-resistant MCF-7 cells. Endocrinology. 2003;144:1032–1044. doi: 10.1210/en.2002-220620. [DOI] [PubMed] [Google Scholar]
- 64.Cao N., Li S., Wang Z., Ahmed K.M., Degnan M.E., Fan M., Dynlacht J.R., Li J.J. NF-kappaB-mediated HER2 overexpression in radiation-adaptive resistance. Radiat. Res. 2009;171:9–21. doi: 10.1667/RR1472.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scaltriti M., Verma C., Guzman M., Jimenez J., Parra J.L., Pedersen K., Smith D.J., Landolfi S., Ramon y Cajal S., Arribas J., et al. Lapatinib, a HER2 tyrosine kinase inhibitor, induces stabilization and accumulation of HER2 and potentiates trastuzumab-dependent cell cytotoxicity. Oncogene. 2009;28:803–814. doi: 10.1038/onc.2008.432. [DOI] [PubMed] [Google Scholar]
- 66.Lin M., Jin Y., Lv H., Hu X., Zhang J. Incidence and prognostic significance of receptor discordance between primary breast cancer and paired bone metastases. Int. J. Cancer. 2022;152:1476–1489. doi: 10.1002/ijc.34365. [DOI] [PubMed] [Google Scholar]
- 67.Denkert C., Nekljudova V., Loibl S. HER2-low-positive breast cancer from four neoadjuvant clinical trials—Authors’ reply. Lancet Oncol. 2021;22:e427. doi: 10.1016/S1470-2045(21)00548-9. [DOI] [PubMed] [Google Scholar]
- 68.Miglietta F., Griguolo G., Bottosso M., Giarratano T., Lo Mele M., Fassan M., Cacciatore M., Genovesi E., de Bartolo D., Vernaci G., et al. HER2-low-positive breast cancer: Evolution from primary tumor to residual disease after neoadjuvant treatment. NPJ Breast Cancer. 2022;8:66. doi: 10.1038/s41523-022-00434-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fernandez A.I., Liu M., Bellizzi A., Brock J., Fadare O., Hanley K., Harigopal M., Jorns J.M., Kuba M.G., Ly A., et al. Examination of Low ERBB2 Protein Expression in Breast Cancer Tissue. JAMA Oncol. 2022;8:607–610. doi: 10.1001/jamaoncol.2021.7239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset analyzed during the current study is available from the corresponding author upon reasonable request.