Abstract
Simple Summary
Immune-checkpoint inhibitors (ICIs) are increasingly used in the treatment of cancer, but they cause immune-related adverse events (irAEs) in around 40% of patients treated. Identifying biomarkers predictive of irAEs has become a priority for the optimal management of patients on ICIs. Herein, we review the state of the art regarding the most relevant biomarkers for predicting irAEs, distinguishing between biomarkers already clinically available and those under investigation. Although none of these biomarkers has been validated in prospective studies, there is growing evidence supporting their use for irAE prediction and clinical characterization, which depend on cancer type, ICI agent and organ affected by the toxicity. A better understanding of the pathogenic mechanisms underlying irAEs and the combination of different emerging biomarkers would allow us to improve the risk-benefit balance for patients who are candidates for ICI therapy.
Abstract
Immune-checkpoint inhibitors (ICIs) are antagonists of inhibitory receptors in the immune system, such as the cytotoxic T-lymphocyte-associated antigen-4, the programmed cell death protein-1 and its ligand PD-L1, and they are increasingly used in cancer treatment. By blocking certain suppressive pathways, ICIs promote T-cell activation and antitumor activity but may induce so-called immune-related adverse events (irAEs), which mimic traditional autoimmune disorders. With the approval of more ICIs, irAE prediction has become a key factor in improving patient survival and quality of life. Several biomarkers have been described as potential irAE predictors, some of them are already available for clinical use and others are under development; examples include circulating blood cell counts and ratios, T-cell expansion and diversification, cytokines, autoantibodies and autoantigens, serum and other biological fluid proteins, human leucocyte antigen genotypes, genetic variations and gene profiles, microRNAs, and the gastrointestinal microbiome. Nevertheless, it is difficult to generalize the application of irAE biomarkers based on the current evidence because most studies have been retrospective, time-limited and restricted to a specific type of cancer, irAE or ICI. Long-term prospective cohorts and real-life studies are needed to assess the predictive capacity of different potential irAE biomarkers, regardless of the ICI type, organ involved or cancer site.
Keywords: immune-related adverse events, immune-checkpoint inhibitors, biomarkers, prediction, diagnosis
1. Introduction
In recent years, treatment with immune checkpoint inhibitors (ICIs) has led to a paradigm shift in the treatment of various types of cancer [1,2]. The mechanism of action of ICIs consists of blocking certain inhibitory receptors in the immune system, such as the cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed death cell protein 1 (PD-1), and PD ligand 1 (PD-L1). By blocking these inhibitory pathways, ICIs induce an enhanced T-cell-mediated response aimed at eliminating tumor cells. As a result of this immune overactivation, ICIs may also trigger a wide range of toxic effects known as immune-related adverse events (irAEs) [3], which mimic traditional autoimmune disorders. In practical terms, an irAE can be defined as any symptom, sign, syndrome, or disease caused or exacerbated by an immune-activating mechanism during the administration of an ICI once other causes such as infectious diseases or tumor progression have been ruled out [4]. The burden of irAEs is high because they are common and, not infrequently, severe complications impact the quality of life and prognosis of patients receiving ICIs [5]. Furthermore, it remains unclear how best to manage irAEs without interfering with ICI-related antitumor response and long-term patient survival [6]. Indeed, patients who develop irAEs have a better cancer-related prognosis [7,8,9]. Therefore, it is of great interest to assess the individual risk of toxicity in advance, allowing earlier management of irAEs, which would help maintain ICIs in these patients susceptible to immune-mediated complications but who, paradoxically, benefit more from therapy.
With the progressive expansion of ICI use in the oncology field, there is an increasing need for reliable and validated biomarkers able to predict irAEs [10]. In accordance with FDA guidelines, a biomarker is “a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes or responses to an exposure or intervention” [11]. In line with this, a predictive biomarker can be defined as a factor that is “used to identify individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or an environmental agent” [12]. Recent years have seen a proliferation of studies on predictive biomarkers for irAEs. Nonetheless, the clinical benefit of reported biomarkers still needs to be confirmed by long-term prospective studies, preferably within randomized clinical trials or real-life studies.
To date, most research on irAE biomarkers has had similar shortcomings: a short follow-up time, retrospective design, and a restricted focus on specific types of irAE, ICI or cancer. That is, there is a lack of long-term, multicenter, and prospective studies encompassing pan-tumor cohorts of patients treated with different ICI agents. Moreover, a cross-sectional use of generic predictors aimed at different tumors, irAEs and ICIs is not feasible because each organ or system damaged by immune toxicity is related to a specific biomarker. For instance, it is well known that the risk of developing nivolumab-induced destructive thyroiditis is higher in patients with antithyroid antibodies pre-treatment [13]. Strikingly, some studies have suggested that certain specific autoantibodies, such as antithyroid antibodies, may herald the risk of irAEs at other anatomic sites [14]. Overall, current knowledge gaps on the pathogenesis of irAEs prevent us from estimating individual patients’ risk of ICI-mediated toxicity and motivate us to search for more effective predictive biomarkers.
Among the wide range of potentially useful biomarkers, we can distinguish between biomarkers that, though not validated, are available for routine clinical use and investigational biomarkers [15]. The aim of this paper is to review the literature on predictive biomarkers for irAEs from a practical approach, differentiating between biomarkers already available for use in daily practice and those still at the research stage.
2. Material and Methods
The search strategy is detailed in Supplementary Materials (Figure S1).
3. Results
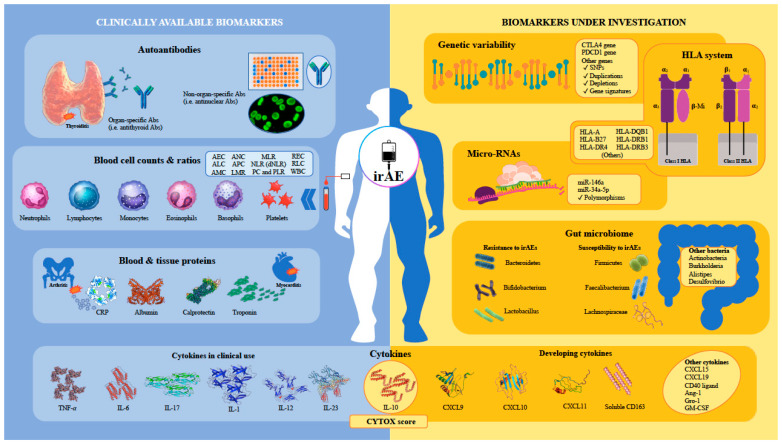
First, it should be noted that no biomarkers have yet been validated as an irAE predictor in asymptomatic patients treated with ICIs [16]. Taking a pragmatic, clinically based approach, we have classified potentially predictive irAE biomarkers as those currently available for clinical use and those still under investigation (Figure 1). Within this classification, clinically available biomarkers would be easily accessible to attending physicians if validated for this purpose, while those still under investigation would require implementation in clinical practice in addition to validation.
Figure 1.
Graphical representation of different families of predictive biomarkers for immune-related adverse events in patients receiving immune-checkpoint inhibitors. Abbreviations in alphabetical order: Abs, antibodies; AEC, absolute eosinophil count; ALC, absolute lymphocyte count; AMC, absolute monocyte count; ANC, absolute neutrophil count; Ang-1, angiopoietin-1; APC, absolute platelet count; CD40, cluster of differentiation 40; CRP, C-reactive protein; CTLA4, cytotoxic T-lymphocyte-associated antigen 4; CXCL, chemokine ligand; dNLR, derived neutrophil-to-lymphocyte ratio; GM-CSF, granulocyte-macrophage colony-stimulating factor; gro-1, growth-regulated oncogene-1; HLA, human leucocyte antigen; IL, interleukin; irAE, immune-related adverse event; LMR, lymphocyte-to-monocyte ratio; miR, micro-RNA; MLR, monocyte-to-lymphocyte ratio; NLR, neutrophil-to-lymphocyte ratio; PC, platelet count; PDCD1, programmed cell death protein 1; PLR, platelet-to-lymphocyte ratio; REC, relative eosinophil count; RLC, relative lymphocyte count; sCD163, soluble cluster of differentiation 163; SNP, single nucleotide polymorphism; TNF-α, tumor necrosis factor-alpha; WBC, white blood cell.
3.1. Biomarkers Available for Clinical Use
3.1.1. Autoantibodies
The potential use of autoantibodies as predictive biomarkers of irAEs has become an expanding field of research [17,18]. Currently, guidelines do not recommend testing every patient for autoantibodies before ICI initiation as this indicator has not been validated for irAE screening [19]. The association between autoantibodies and irAEs is, however, well documented in the case of organ-specific irAEs and the autoantibodies related to such events [20,21,22]. For instance, the risk of suffering ICI-induced thyroiditis is higher in patients with pre-existing antithyroid antibodies [13,23,24]. That is, on the one hand, some organ-specific autoantibodies are only useful for organ-specific irAEs, although not all reported irAEs have been paired with a specific autoantibody. On the other, generic and routinely available autoantibodies, such as antinuclear antibodies (ANA) or rheumatoid factor, may be useful in screening for any type of irAE, regardless of the tissue involved [25]. Furthermore, even certain organ-specific autoantibodies such as antithyroid antibodies, traditionally linked to the prognosis of immunogenic tumors [26], could also be useful in predicting irAEs at any site, indicating a marked overlap between generic and specific autoantibodies [14,25]. Nevertheless, the clinical heterogeneity and complex and diverse pathogenesis, as well as the generally low rates of autoantibody seropositivity associated with these events, mean that current autoantibody panels are not applicable to all patients developing ICI-related toxicity.
In recent years, research on autoantibodies as irAE indicators has moved from retrospective towards prospective methods (Table 1) [14,25,27,28,29,30,31,32,33,34,35,36,37,38,39]. While testing positive for autoantibodies at baseline was considered a risk factor for irAE development in preliminary studies, the most recent reports have provided greater insight into changes in antibody levels over time. For example, a retrospective study by Toi et al. suggested that patients with pre-treatment ANAs, rheumatoid factor or antithyroid antibodies were at increased risk of developing irAEs [27]. De Moel et al. showed an association between seroconversion of any autoantibody included in a battery of 23 autoantibodies and irAEs during follow-up, especially when focusing on specific irAEs related to the battery under study; however, the presence of autoantibodies before ICI initiation was not associated with irAEs [30]. The value of autoantibody seroconversion was also highlighted by Giannicola et al., who found a higher risk of irAEs in patients who became positive for ANAs, anti-extractable nuclear antigens antibodies or anti-smooth muscle antibodies after starting nivolumab administration [31].
Table 1.
Summary of studies on the clinical use of autoantibodies as predictive biomarkers for immune-related adverse events regardless of the specific organ-autoantibody pairing.
| Type of Parameter | Design (No. Patients) |
Type of Tumor | Type of irAE | Main Findings | Reference |
|---|---|---|---|---|---|
| ANA, RF and ATA (detected before ICI initiation) |
Retrospective (n = 137) |
NSCLC | All types | Autoantibodies were associated with a higher risk of irAEs (OR 3.25, p = 0.001) |
Toi Y. JAMA Oncol 2019 [27] |
| ANA (detected before ICI initiation) |
Retrospective (n = 83) |
NSCLC | All types | ANA were not associated with irAEs, though the risk of irAEs tended to be higher with higher titers of ANAs | Yoneshima Y. Lung Cancer 2019 [28] |
| ANA (detected before ICI initiation) |
Retrospective (n = 191) |
Pan-tumor | All types | ANA were not associated with irAEs, except for colitis (22% vs. 1.6%, p = 0.002) | Sakakida T. Clin Transl Oncol 2020 [29] |
| ANA, anti-dsDNA antibody, ENA *, RF, ACPA, ASMA, AMA, anti-LKM antibody and ATA (developing after ICI initiation) |
Retrospective (n = 133) |
Melanoma | All types | The association between irAEs and seroconversions was nonsignificant considering all irAEs and any autoantibody (OR 2.92, p = 0.12), but became significant when focusing on irAEs related to the autoantibodies tested (OR 3.64, p = 0.04) | de Moel EC. Cancer Immunol Res 2019 [30] |
| ANA, ENA and ASMA (developing after ICI initiation, within 30 days) | Retrospective (n = 92) |
NSCLC | All types | Early detection of autoantibodies was associated with a higher risk of irAEs (HR not available, p = 0.002) | Giannicola R. Mol Clin Oncol 2019 [31] |
| ATA (titer increase from baseline) |
Prospective (n = 78) |
Pan-tumor | All types | Increases in anti-Tg and anti-TPO titers ≥ 1.5 from baseline were associated with irAE occurrence (OR 17.4, p = 0.015; OR 6.1, p = 0.035; respectively) |
Music M. F1000Res 2020 [14] |
| ANA, RF, ATA and ANCA (before and after ICI initiation) |
Retrospective (n = 69) |
Pan-tumor | All types | Positivity for any autoantibody was associated with a higher risk of irAEs (OR 46.61, p = 0.010) |
Les I. Ann Med 2021 [25] |
| ANA (detected before ICI initiation) |
Retrospective (n = 68) |
Urothelial carcinoma | All types | Patients with ANA positivity at a titer >1:160 developed irAEs more frequently (p = 0.029) and earlier (p = 0.052) | Castel-Ajgal Z. Clin Genitourin Cancer 2022 [32] |
| ANA, ENA **, RF, ACPA, autoimmune hepatopathy profile # and myopathy profile † (detected before ICI initiation) |
Prospective (n = 44) |
Pan-cancer | All types | The frequency of irAEs did not differ as a function of positivity for any autoantibody (OR 0.62, p = 0.480) or ANA titers (OR 0.79, p = 0.529) | Barth DA. Cancer Med 2022 [33] |
| ANA and ATA (detected before ICI initiation) |
Retrospective (n = 159) |
NSCLC | All types | ANA titer ≥ 1:320 was related to irAEs (OR 4.9, p = 0.01), especially to skin subtypes (9.7% in patients with ANA <1:320 vs. 32% in patients with ANA ≥ 1:320, p = 0.003) | Zhang D. Transl Lung Cancer Res 2022 [34] |
| ANA, anti-Ro52 and ATA (detected before ICI initiation) |
Retrospective (n = 177) |
Pan-tumor | All types | ANA and anti-Ro52 positivity was not associated with a higher risk of irAEs. ATA positivity was more common in patients with than without thyroiditis (75% vs. 13.8%, p < 0.001) | Tang H. Front Immunol 2022 [35] |
| ANA, ATA, AGAD, AChR and PA-IgG (detected before ICI initiation) |
Retrospective (n = 275) |
Pan-tumor | All types | There were no associations between autoantibodies and irAEs, except between ATA and thyroiditis (39.5% in anti-Tg-positive vs. 12.5% in anti-Tg-negative patients, p < 0.01) | Izawa N. ESMO 2022 [36] |
| ANA (detected before ICI initiation) |
Retrospective (n = 266) |
NSCLC | All types | There were no significant differences in the frequency of irAEs between positive and negative ANA patients and between high and low ANA titers | Mouri A. Front Oncol 2021 [37] |
| ANA (before and after ICI initiation) |
Prospective (n = 152) |
Pan-tumor | All types | There was no association between irAEs and ANA at baseline or developing. Patients who became ANA-positive during follow-up were more likely to have severe irAEs than those who were ANA-positive at baseline and ANA-negative patients (42.8% vs. 26.1% vs. 9.1%, p = 0.05) | Alserawan L. Int J Mol Sci 2022 [38] |
| ANA, RF and ACPA (before and 6 weeks after ICI initiation) |
Prospective (n = 60) |
Melanoma | All types | There was no association between baseline seropositivity for ANA/RF/ACPA and time to first irAE (p = 0.39). ANA/RF/ACPA-negative patients experienced more thyroid irAEs than ANA/RF/ACPA-positive patients (p = 0.006) |
Gosh N. J Immunother Cancer 2022 [39] |
* Included anti-U1RNP, anti-SS-A/Ro, anti-SS-B/La, anti-centromere protein B, anti-Scl-70, anti-Jo-1, and anti-Sm. ** Included anti-centromere protein B, anti-double strand DNA, anti-SS-B/La, anti-PM100, anti-PM75, anti-RNP70, anti-SS-A/Ro, anti-Scl-70, and anti-U1RNP. # Included anti-GP210, anti-LKM1, anti-M2, anti-SP100, anti-SLA-LP, anti-LC1, and anti-F-Actin. † Included anti-EJ, anti-Jo-1, anti-Ku, anti-MDA5, anti-MI2a, anti-MI2b, anti-NXP2, anti-Oj, anti-PL-12, anti-PL-7, anti-SAE, anti-SRP, and anti-TIF-1γ. Abbreviations in alphabetical order: ACPA, anti-citrullinated peptide antibody; AGAD, anti-glutamic acid decarboxylase antibody; AChR, anti-acetylcholinesterase receptor antibody; ALKM, anti-liver-kidney microsomal; AMA, anti-mitochondrial antibody; ANA, antinuclear antibody; ANCA, antineutrophil cytoplasmic antibody; ASMA, anti-smooth muscle antibody; ATA, antithyroid antibody; dsDNA, double-stranded DNA antibody; ENA, extractable nuclear antigen antibody; HR, hazard ratio; ICI, immune-checkpoint inhibitor; irAE, immune-related adverse event; NSCLC, non-small lung cancer; OR, odds ratio; PA-Ig, platelet-associated immunoglobulin G; RF, rheumatoid factor; Tg, thyroglobulin; TPO, thyroid peroxidase.
Confirming the significance of dynamic changes in autoantibody titer, a sub-study from a phase II clinical trial identified a low autoantibody titer at baseline and greater fold change in autoantibody titer after ICI initiation as independent risk factors for irAEs [39], in contrast with the pre-formed autoantibody theory. Moreover, Alsewaran et al. demonstrated that pre-treatment ANA positivity was not associated with irAE development. On the contrary, patients experiencing seroconversion to ANA positivity after ICI initiation developed more severe irAEs than patients who remained ANA-negative and patients who were ANA-positive before ICI initiation. This humoral response in the form of ANA seroconversion could be related to early B-cell changes induced by ICIs, namely a decline in circulating B cells and an increase in CD21 B cells and plasmablasts, which have been associated with a higher frequency of irAEs [40]. Furthermore, in up to 83% of patients with severe irAEs, modifications in ANA patterns preceded irAE onset [38]. In addition to ANA positivity, ANA patterns determined by immunofluorescence may be useful for discriminating between primary autoimmune diseases and irAEs. Although no studies designed to compare autoantibody profiles have yet been reported, patients who develop irAEs may be less likely to express disease-specific ANA patterns than patients with the corresponding classical autoimmune disease. In contrast, a nuclear speckled pattern may be more indicative of immune-related toxicity [38].
3.1.2. Blood Cell Counts and Ratios
The use of blood cell counts for the early detection of irAEs may be of great interest to clinicians due to their wide availability, low cost, and easy interpretation. Although not completely consistent, there is supportive evidence suggesting that baseline absolute neutrophil, lymphocyte, monocyte, eosinophil and basophil counts, platelet counts, and increases in white blood cell, lymphocyte and eosinophil counts during follow-up are associated with a higher risk of irAEs (Table 2) [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60]. In addition, several blood cell ratios, the most common being the neutrophil-to-lymphocyte ratio (NLR) and derived NLR (calculated as absolute neutrophil count/[white blood cell count–absolute neutrophil count]), could help to predict irAEs before and after ICI initiation. In a systematic review and meta-analysis including 6696 patients on ICIs from 25 studies, a high NLR was identified as an independent risk factor for developing irAEs [51]. In a prospective study including 1187 patients, an elevated NLR at the beginning of ICI therapy was predictive of very severe irAEs (grades 4 and 5) [42].
Table 2.
Summary of studies on the clinical use of blood cell counts and ratios as predictive biomarkers for immune-related adverse events.
| At Baseline (Before Immune-Checkpoint Inhibitor Initiation) | |||||
|---|---|---|---|---|---|
| Type of Parameter |
Study Design (No. Patients) |
Type of Tumor | Type of irAE | Main Findings | Reference |
| ALC | Retrospective (n = 167) |
Pan-tumor | All types | Grade ≥ 2 irAEs were associated with ALC > 2000/μL (OR 1.996, p < 0.05) |
Diehl A. Oncotarget 2017 [41] |
| AEC | Retrospective (n = 45) |
Melanoma | Endocrine irAEs | irAEs were associated with AEC > 240/μL (OR 1.601, p = 0.045) |
Nakamura Y. Jpn J Clin Oncol 2019 [42] |
| AEC | Retrospective (n = 95) |
Pan-tumor | All types | AEC > 0.045 × 109/L was predictive of irAEs (OR 4.114, p = 0.014) |
Ma Y. World J Surg Oncol 2022 [43] |
| NLR | Prospective (n = 1187) |
Pan-tumor (blood and solid organ cancers) | All types | NLR > 4.78 was predictive of grade 4 and 5 irAEs (OR not available, p = 0.0137) * |
Ruste V. Eur J Cancer 2021 [44] |
| NLR and PLR | Retrospective (n = 184) |
NSCLC | All types | PLR < 180 was the only independent predictor of irAEs (OR 2.3, p = 0.017) |
Pavan A. Oncologist 2019 [45] |
| dNLR | Retrospective (n = 391) |
Pan-tumor | All types | dNLR ≥ 3 was protective against irAEs (OR 0.37, p = 0.012) |
Eun Y. Sci Rep 2019 [46] |
| ANC, PC, NLR and PLR | Retrospective (n = 150) |
NSCLC | All types | Grade 3–4 irAEs were associated with ANC (p = 0.009), PC (p = 0.023), NLR (p= 0.023) and PLR (p = 0.0016) * (cut-off values and ORs not provided) |
Liu W. Cancer Manag Res 2021 [47] |
| RLC and AEC | Retrospective (n = 105) |
Pan-tumor | All types | irAEs were associated with RLC < 28.5% (OR 3.60, p = 0.027) and AEC > 0.175 × 109/L (OR 3.44, p = 0.020) | Bai R. Cancer Biol Med 2021 [48] |
| NLR | Retrospective (n = 115) |
NSCLC | All types | irAEs were associated with NLR < 2.86 (OR 2.69, p = 0.016) |
Fujimoto A. Thorac Cancer 2021 [49] |
| ALC, AMC, APC, NLR, MLR and PLR | Retrospective (n = 470) |
Pan-tumor | All types | irAEs were associated with ALC > 2.6 K/μL (aOR 4.3, p = 0.002), AMC > 0.29 K/μL (aOR 2.34, p = 0.03), PC > 145 K/μL (aOR 2.23, p = 0.03), NLR ≤ 5.3 (aOR 2.07, p = 0.01), MLR ≤ 0.76 (aOR 2.96, p = 0.01) and PLR ≤ 534 (aOR 5.05, p = 0.04) ** | Michailidou D. Sci Rep 2021 [50] |
| NLR | Metanalysis #
(n = 6696) |
NSCLC | All types | irAEs were associated with NLR ≥ 5 (OR = 1.046, p = 0.026) |
Suazo-Zepeda E. Cancer Immunol Immunother 2021 [51] |
| ALC, LMR, NLR and PLR | Retrospective (n = 92) |
NSCLC | All types | ALC > 1450/mm3 (aOR 0.24, p = 0.003) and LMR > 1.6 (OR 0.12, p = 0.004) were associated with a lower risk of irAEs. NLR > 2.3 (aOR 5.99, p = 0.005) and PLR > 165 (OR = 2.87, p = 0.022) were associated with a higher risk of irAEs † |
Egami S. J Cancer 2021 [52] |
| ALC | Retrospective (n = 667) |
NSCLC | All types | ALC was positively associated with irAE risk (OR 2.556, p = 0.001; ALC cut-off value not provided) |
Xu H. Exp Cell Res 2022 [53] |
| NLR | Retrospective (n = 147) |
Pan-tumor | All types | NLR < 3 was associated with a higher rate of irAE (aOR 2.27, p = 0.034) |
Lee PY. Cancers (Basel) 2021 [54] |
| AEC | Retrospective (n = 300) |
NSCLC | Pneumonitis | Pneumonitis was associated with AEC ≥ 0.125 × 109/L (HR 2.825, p < 0.001) |
Chu X. Lung Cancer 2020 [55] |
| ALC | Retrospective (n = 110) |
Pan-tumor | Myocarditis | ALC 1.6 K/μL in myocarditis group vs. 1.3 K/μL in non-myocarditis group (p = 0.02) * | Drobni ZD. J Am Heart Assoc 2020 [56] |
| NLR | Retrospective (n = 73) |
Gastric and renal cancers | Grade 3 and 4 irAEs | NLR < 4.3 was associated with lower risk of grade 3–4 irAEs (OR 0.024, p = 0.014) |
Takada S. Asian Pac J Cancer Prev 2022 [57] |
| During Follow-Up (After Immune-Checkpoint Inhibitor Initiation) | |||||
| Type of Parameter |
Study Design | Type of Tumor | Type of irAE | Main Findings | Reference |
| WBC RLC (on the day of irAE detection) |
Retrospective (n =101) |
Melanoma | Lung and gastrointestinal irAEs | 59.1% increase in WBC (OR = 6.04, p = 0.014) and 32.3% decrease in RLC (OR = 5.01, p = 0.012) were predictive of irAEs |
Fujisawa Y. J Dermatol Sci 2017 [58] |
| ALC at 1 month | Retrospective (n = 167) |
Pan-tumor | All types | Grade ≥ 2 irAEs were associated with ALC > 2000/μL (OR = 1.813, p < 0.05) |
Diehl A. Oncotarget 2017 [41] |
| REC at 1 month WBC at 1 month |
Retrospective (n = 45) |
Melanoma | Endocrine irAEs and vitiligo | REC > 3.2% was predictive of irAEs (OR = 5.111, p = 0.025) *. A summative increase in WBC by 100 was protective against vitiligo (OR = 0.823, p = 0.0023). |
Nakamura Y. Jpn J Clin Oncol 2019 [42] |
| ANC NLR PLR (treatment cycle before onset of the irAE) |
Retrospective (n = 150) |
NSCLC | All types | Multiple univariate associations were described, namely, between *: 1.91 × 109/L decrease in ANC and grade 1–2 irAEs (p = 0.013) 1.11 × 109/L decrease in ANC and grade 3–4 irAEs (p = 0.003) 0.62 decrease in NLR and grade 1–2 irAEs (p = 0.013) 0.76 decrease in NLR and grade 3–4 irAEs (p = 0.011) 89.26 decrease in PLR and grade 1–2 irAEs (p = 0.011) (comparative data between baseline and pre-irAE cycle) |
Liu W. Cancer Manag Res 2021 [47] |
| ALC at 2 weeks | Retrospective (n = 171) |
NSCLC | All types | Early onset of irAEs was associated with ALC > 820/mm3
(aOR = 3.58, p = 0.07) † |
Egami S. Front Oncol 2021 [59] |
| NLR at second course (2 to 3 weeks after the first dose) | Retrospective (n = 243) |
Esophageal, gastric and colon cancer | All types | irAEs (any grade) were associated with NLR < 3 (OR = 0.894, p= 0.044) |
Zhang Z. Cancers (Basel) 2022 [60] |
| ALC NLR (from baseline to last ICI dose; and from baseline to myocarditis onset) |
Retrospective (n = 110) |
Pan-tumor | Myocarditis | irAEs were associated with a decrease in ALC (1.6 K/μL to 1.4 K/μL to 1.1 K/μL, p < 0.001) and an increase in NLR (3.5 to 4.1 to 6.6, p < 0.001) * |
Drobni ZD. J Am Heart Assoc 2020 [56] |
| NLR (at the onset of the irAE) | Retrospective (n = 73) |
Gastric and renal cancers | Grade 3 and 4 irAEs | ∆NLR >120% was associated with increased risk of irAEs (OR = 10.48, p = 0.033) |
Takada S. Asian Pac J Cancer Prev 2022 [57] |
* Only in the univariate analysis. ** All odds ratios adjusted for age, sex, smoking history, cancer type (hematological malignancy vs. solid tumor), Eastern Cooperative Oncology Group performance status, concomitant systemic therapy, personal or family history of autoimmune disease, personal history of chronic infection, systemic steroid treatment at the time of ICI initiation. # Including randomized controlled trials, cohort and case-control studies. Abbreviations in alphabetical order: AEC: absolute eosinophil count; ALC: absolute lymphocyte count; AMC: absolute monocyte count; ANC: absolute neutrophil count; APC: absolute platelet count; dNLR (calculated as absolute neutrophil count/[white blood cell count–absolute neutrophil count]): derived neutrophil-to-lymphocyte ratio; LMR: lymphocyte-to-monocyte ratio; MLR: monocyte-to-lymphocyte ratio; NLR: neutrophil-to-lymphocyte ratio; NSCLC, non-small cell lung cancer; PC: platelet count; PLR: platelet-to-lymphocyte ratio; REC: relative eosinophil count; RLC: relative lymphocyte count; WBC: white blood cell. † All odds ratios adjusted for age and PD-L1 expression (≥50%). ∆: rate of change.
Similarly, it has been reported that peripheral CD8 T-cell expansion and diversification after ipilimumab initiation, as surrogate markers of autoreactivity against tissue self-antigens at the systemic level, allows us to predict irAE onset with very high sensitivity [61]. This diversification occurs early in follow-up, within the first two weeks after ICI administration [62]. Furthermore, patients experiencing ipilimumab-induced colitis showed higher absolute counts of peripheral CD4+ T cells and lower percentages of regulatory T cells at baseline [63]. Likewise, it has been suggested that changes in the percentage of peripheral CD4+ CD25+ Foxp3+ regulatory T cells, a cell subset in charge of maintaining immune tolerance in the tumor microenvironment, may be predictive of irAEs [64]. Recently, elevated levels of circulating low-density neutrophils, a myeloid subpopulation with immunosuppressive properties, have been associated with a poor response to pembrolizumab mediated by T-cell cytotoxicity down-regulation in patients with non-small cell lung cancer [65]. As in tumor response, different subpopulations may play a role in the pathogenesis of ICI toxicity.
Despite these promising findings, most published studies on blood cell counts and ratios have been retrospective, time-limited (usually considering only baseline data or short follow-up periods) and constrained to either a specific type of cancer, irAE or ICI agent (Table 2). Notably, to date, few prospective studies have assessed the clinical value of blood cell count fluctuations for predicting irAEs in the long term.
3.1.3. Serum and Other Biological Fluid Proteins
Baseline levels of thyroid-stimulating hormone in serum have been shown to predict immune-related thyroiditis before ICI initiation [66,67,68]. Likewise, thyroid stimulating hormone is the most efficient biomarker for monitoring thyroid dysfunction in patients on ICI therapy [6]. Similarly, serial measurements of serum brain natriuretic peptide and troponin, together with new-onset electrocardiographic abnormalities, help anticipate cardiovascular irAEs [69]. Fecal lactoferrin and calprotectin are commonly used as screening tools for ICI-induced colitis [70], calprotectin being a good non-invasive indicator for assessing treatment response and avoiding repetitive endoscopic procedures [71].
Among generic biomarkers, raised C-reactive protein levels correlate well with the risk of developing irAEs [51], in parallel with serum interleukin-6 (IL-6) levels [72]. With different cut-offs, high serum albumin levels have also been associated with irAEs [48,73]. In addition, elevated blood lactate dehydrogenase levels predispose patients to irAEs [74], especially high-severity events (grade ≥ 3) [48]. In contrast, a decrease in serum leptin levels at four weeks from ICI initiation was more common in patients who experienced irAEs than in irAE-free patients [75]. Levels of these generic proteins, which are acute-phase reactants or tumor burden-related markers, are relatively easy to interpret in patients with an indication for adjuvant treatment. In contrast, it may be less appropriate to use them as irAE biomarkers in patients with metastatic disease since cancer, especially in progressive phases, may alter protein levels. Interestingly, a reduction over time in the level of certain serum tumor markers, such as the melanoma-inhibitory activity protein, could help discriminate between toxicity and progression in patients with metastatic melanoma [72,76].
3.1.4. Cytokine Profiles and Dynamics
In recent years, the interest in cytokines to predict irAE susceptibility has grown steadily [77]. Certain cytokine profiles at baseline and dynamic fluctuations in cytokine levels over time have been associated with a higher risk of developing irAEs and better treatment outcomes [78]. Moreover, the uncoupled effect achieved by some anti-cytokine drugs in preclinical studies, consisting of decreased ICI-induced toxicity without sacrificing antitumor activity, makes it a priority to improve our understanding of the pathogenic role of cytokines [79,80]. Unfortunately, not all cytokines are currently assessed in clinical practice for diagnostic purposes. In addition, the cytokines involved in a particular irAE can differ from the corresponding autoimmune manifestation and with the ICI agent administered [81].
Tumor necrosis factor-α (TNF-α) is one of the most studied biomarkers in the field of irAE research [82]. Low baseline TNF-α levels may predispose patients to better antitumor immunity [83], while it is unknown whether fluctuations in TNF-α levels over time can anticipate irAE onset. In any case, various TNF-α blockers, such as infliximab, etanercept, adalimumab and certolizumab, have been used as rescue therapy for steroid-refractory cases of ICI-induced colitis, arthritis and pneumonitis [84,85,86,87]. Two concerns arising from TNF-α antagonism are the attenuation of antitumor immunity and promotion of tumorigenesis by anti-TNF-α drugs [88], which may depend on the dose and duration of treatment. Indeed, it is accepted that short courses of TNF-α inhibitors given at regular doses are safe for patients undergoing ICI therapy [89]. Moreover, preclinical data suggesting an antitumor benefit in mice combining ICIs and TNF-α inhibitors warrant the undertaking of clinical trials assessing this hypothesis (NCT03293784) [90,91].
Considered a “usual suspect”, IL-6 is a proinflammatory cytokine that is potentially involved in the pathogenesis of several immune-mediated disorders [92]. Low baseline levels of IL-6 were strongly associated with irAEs [93,94]. Combined with C-reactive protein, IL-6 has also been proposed as an early biomarker for irAE detection during follow-up [72,83]. Even in patients with elevated C-reactive protein, regardless of serum IL-6 levels, IL-6 blockade with tocilizumab has been tested as a therapeutic and pre-emptive drug for irAEs [95]. Recently, an uncoupled effect on induced toxicity and antitumor immunity exerted by immunotherapy has been achieved by the blockade of IL-6 in a murine model [96], which has warranted the launching of a phase II clinical trial to assess the efficacy of tocilizumab in patients receiving ICIs (NCT04940299). The favorable safety profile of tocilizumab and other anti-IL-6 agents, widely available in the clinical setting due to the SARS-CoV-2 pandemic, makes IL-6 a promising therapeutic target [97].
Interleukin-17 (IL-17) is another pro-inflammatory cytokine involved in the pathogenesis of inflammatory bowel disease, psoriasis, psoriatic arthritis, other types of spondyloarthritis, and even interstitial lung disease [98,99]. Unlike TNF-α and IL-6, high serum levels of IL-17 at baseline have been associated with severe colitis in patients on ipilimumab [100]. An increase in serum IL-17 levels was demonstrated following CTLA-4 blockade with ipilimumab in patients developing colitis, consistent with CTLA-4 inhibiting the production of IL-17 by type 17 T helper (Th17) cells [101,102]. These findings support the central role of IL-17 in the pathogenesis of irAEs involving Th17 cell-enriched tissues, such as colitis, psoriasiform dermatitis, pneumonitis and neuroendocrine toxicity [103,104,105]. Correspondingly, IL-17 antagonists have shown a clinical benefit in IL-17-dependent irAEs, opening the door to targeted anti-cytokine therapies [106].
The case of IL-1 is revealing and may represent a new therapeutic target. There is evidence suggesting that baseline elevated levels of IL-1β are related to thyroid dysfunction [107]. In a retrospective series, IL-1α was significantly elevated in patients who developed ICI-induced myositis [108]. Notably, patients treated with a combination of anti-CTLA-4 and anti-PD-1 drugs who developed ICI-induced colitis overexpressed mucosal IL-1β (as well as IL-17), but not TNF-α, with a higher abundance of Bacteroides intestinalis [109]. Moreover, fecal microbiota transplant of large numbers of Bacteroides intestinalis bacteria to mice induced overexpression of IL-1β after ICI administration [5]. These findings on the role of IL-1 regardless of TNF-α activity in immune-mediated colitis could be related to the subgroup of patients with inflammatory bowel disease who are refractory to standard therapy with TNF-α blockers [110]. In addition, IL-1β has been identified as an independent risk factor for irAEs in patients on PD-(L)1 inhibitors [111].
The pro-inflammatory interleukins IL-12 and IL-23 belong to the IL-12 family and are characterized by sharing a p40 subunit. Blocking both IL-12 and IL-23 with ustekinumab has been shown to be effective in ICI-induced refractory colitis [112]. On the other hand, interfering with the IL-12-dependent pathway may alter the antitumor effect associated with ICI therapy [113,114]. The use of guselkumab, a specific anti-IL-23 agent, has been proposed as a way of inhibiting both the pro-tumor and pro-inflammatory effects attributed to IL-23 without affecting the IL-12 pathway, although this hypothesis needs further testing [115].
Regarding IL-10, an anti-inflammatory interleukin with homeostatic properties [116], a retrospective study revealed that high baseline IL-10 levels and increases in these levels after the first cycle of ICI were the only independent factors predicting irAEs among a broad battery of cytokines [117]. Further insight is required into the mechanisms by which IL-10 may promote immune tolerance and their relationship with toxicity modulation [118].
Other potential cytokine-related biomarkers are being studied, such as the serum soluble IL-2 receptor, a biomarker of hyper-inflammatory status available in daily clinical practice [119]. In addition, low baseline values and decreases in interferon-γ release, commonly used for the detection of Mycobacterium tuberculosis (latent) infection, have been associated with ICI-induced pneumonitis [120].
3.2. Biomarkers under Investigation
3.2.1. Other Cytokines and Serum Proteins under Development
The chemokine ligand 15 (CXCL15) and the soluble protein cluster of differentiation 163 (sCD163), as surrogate indicators of Th17 cell and tumor-associated macrophage activation, respectively, have been proposed as biomarkers for irAE prediction [121]. Lower levels of CXCL9, CXCL10, CXCL11 and CXCL19 at baseline and greater increases in CXCL9 and CXCL10 levels have been reported in patients who experienced irAEs [122]. Other biomarkers under investigation are angiopoietin-1 (Ang-1) and CD40 ligand, whose baseline high levels have been related to dermatitis [78]. Early decreases in granulocyte colony-stimulating factor have been associated with several irAEs, while lower baseline levels of this growth factor may predispose patients to colitis [78,107]. High baseline growth-regulated oncogene-1 and granulocyte macrophage colony-stimulating factor levels have been associated with generic irAEs and specifically with thyroid dysfunction and dermatitis, respectively [75,107]. Other organ-specific irAEs were associated with stem cell factor (colitis), leukemia inhibitory factor and placental growth factor (both with myositis), and B and T-lymphocyte attenuator (dermatitis) [108].
In addition, the pathogenic role and predictive value of other cytokines such as IL-2, IL-4, IL-5, IL-15, IL-27, IL-35, and interferon-α remain to be clarified [107,108,123,124].
Overall, the incorporation of several cytokines, both those available routinely and those under development, into already-designed toxicity risk scores such as the CYTOX score might provide a useful tool for irAE prediction [125]. We are currently witnessing a surge in precision medicine approaches based on personalized cytokine profiles depending on individual, pharmacologic and tissue-related factors, without undermining the antitumor response. Such molecular-focused strategies yield therapies focused on specific cytokine signatures rather than the targeted organ [126].
3.2.2. Genetic Variations and Gene Expression Profiling
Monogenic mutations leading to autoimmune diseases have been identified for years [127]. For instance, we know about the existence of cases of systemic lupus erythematosus caused by monogenic mutations in the C1qA, B, C, C1R, DNASE1, DNASE1L3, and ACP5 genes [128], among many other predisposing genetic variations [129]. Furthermore, certain germline CTLA4 and PDCD1 (encoding for PD-1 protein) gene polymorphisms have been associated with both the development of autoimmune diseases and susceptibility to ICI-induced endocrine irAEs [130] (Table 3) [131,132,133,134,135,136,137,138,139,140,141,142,143,144]. In the same vein, two different PDCD1 gene single-nucleotide polymorphisms (SNPs), namely rs2227981 and rs10204525, have been identified as protective and susceptibility biomarkers for irAEs, respectively [135,136]; these apparently paradoxical findings are explained by the polymorphism in question, which determines the level of PD-1 expression (low in the case of rs2227981 and high in the case of rs10204525). In a comprehensive study, Abdel-Wahab et al. described as many as 30 SNPs related to irAEs, of which twelve led to a higher irAE risk, eighteen to a lower irAE risk, and nine involved genes associated with autoimmune or inflammatory diseases (GABRP, DSC2, BAZ2B, SEMA5A, ANKRD42, PACRG, FAR2, ROBO1 and GLIS3) [132]. These SNPs add to others previously described as isolated risk factors for irAEs or combined predictors of irAEs and autoimmune diseases [133,145].
In addition, genetic alterations other than SNPs such as small sequence variations and copy number variations (namely, duplications and depletions) have been detected in 16 genes (AIRE, TERT, SH2B3, LRRK2, IKZF1, SMAD3, JAK2, PRDM1, CTLA4, TSHR, FAN1, SLCO1B1, PDCD1, IL1RN, CD274, and UNG) and linked to irAEs affecting different organs and systems [131]. Moreover, patients showing modifications of CEBPA, FGFR4, MET or KMT2B genes detected in circulating tumor DNA before ICI initiation are at higher risk of experiencing irAEs [134].
Another gene-related biomarker for ICI-mediated toxicity is the expression of specific gene signatures. For example, Friedlander et al. proposed a 16-gene signature (involving CARD12, CCL3, CCR3, CXCL1, F5, FAM210B, GADD45A, IL18bp, IL2RA, IL5, IL8, MMP9, PTGS2, SOCS3, TLR9 and UBE2c genes) to discriminate between low- and high-grade tremelimumab-induced diarrhea [139]. Clinically relevant pathways, such as those of the inflammasome in ICI-induced myocarditis or the neutrophil activation cascade in gastrointestinal irAEs, have been identified through the overexpression of type 5 and 6 guanylate binding proteins and CD177 and CEACAM1 genes, respectively [140,141]. More specifically, IFI27 gene expression, related to the interferon-α pathway, has allowed ICI-associated T cell-mediated rejection to be distinguished from ICI-associated acute interstitial nephritis in kidney transplant patients [142].
With the assistance of pharmacovigilance, other over-represented genes in patients with irAEs have been identified through integrated bioinformatic analysis [143], molecular multi-omics data [144], and transcriptomic information of messenger RNA and alternative splicing features [146,147] (Table 3). Again, further studies are needed to validate these promising results in clinical practice.
3.2.3. Human Leucocyte Antigen Genotyping
Among the genes most influential in irAEs are those in the major histocompatibility complex, also known as the human leucocyte antigen (HLA) system, which is a group of genes encoding for surface glycoproteins involved in antigen presentation that has been widely related to susceptibility to immune-mediated diseases and cancer [148,149]. Although clinically available, the use of HLA genotyping for diagnostic purposes is constrained to specific disorders such as celiac disease or axial spondyloarthritis [150,151]. Despite other confirmed genotypic-phenotypic associations, testing is not recommended for entities with more reliable diagnostic methods, because HLA variants indicate a genetic susceptibility rather than a diagnosis of certainty.
The potential association between certain HLA genotypes and polymorphisms and the risk of immune-related toxicity has been mainly assessed in the context of endocrinologic irAEs, such as ICI-induced diabetes (overall, the irAE most studied from the point of view of the HLA system) [152], thyroid dysfunction and hypophysitis [13,153]. For instance, the development of ICI-induced type 1 diabetes mellitus [154,155], thyroiditis [156] and even autoimmune polyglandular syndrome type 2 [157] was observed in patients with HLA-DR4 more often than in patients with another HLA haplotype. Notably, Delivanis et al. demonstrated that ICI therapy can increase HLA-DR surface expression in activated monocytes leading to pembrolizumab-induced thyroiditis [158].
Other relevant associations of HLA alleles or proteins with irAEs previously reported are those of HLA-DRB1*04:05 with inflammatory arthritis [159], HLA-B27*05 with autoimmune encephalitis [160], HLA-Cw12 with hypophysitis [153,161], HLA-DQB1*03:01 with colitis [162], HLA-DRB3*01:01 with thrombocytopenia [163], HLA-A03 with pneumonitis [164], and HLA DRB*04:01, HLA-DRB1*15:01 and HLA-DQB1*06:02 with hepatitis [165] (Table 3) [74,131,152,153,154,155,156,157,159,160,161,162,164,165,166,167,168,169]. By contrast, some studies have reached negative results regarding the connection between irAEs and the HLA system [170,171].
Due to its growing availability, HLA genotyping could be considered an irAE biomarker on the boundary between clinical and investigational.
3.2.4. Micro-RNAs
A micro-RNA (miR) is a non-coding molecule of single-stranded RNA containing between 20 and 25 nucleotides, which can regulate the post-transcriptional expression of genes by blocking translation of targeted messenger RNA through a process known as ribo-interference [172]. Like CTLA-4 and PD-1, certain miRs, such as miR-146a, promote down-regulation of both innate and adaptive immune responses and may impact ICI-related survival [173], in part by counteracting cell escape mechanisms in the tumor microenvironment [174]. Indeed, the first phase 1 clinical trial which evaluated a liposomal mimic of miR-34a was halted early due to severe irAEs in participating patients [175].
Among the most relevant miRs (Table 3) [176,177,178], miR-146a is a miR family whose modified expression has been involved in the pathogenesis of several autoimmune diseases, including rheumatoid arthritis, psoriasis, and laboratory-induced colitis [179,180,181]. Moreover, specific miR-146a SNPs, such as rs2910164, predispose patients on ICIs to a higher risk of developing severe irAEs and reduced progression-free survival [177]. By contrast, exogenous administration of a miR-146a mimic may mitigate irAE intensity assessed by histopathologic criteria in mice [176].
Table 3.
Summary of studies on reported associations between immune-related adverse events and HLA system antigens, genetic variants and signatures and micro-RNAs.
| Genetic Variants and Gene Expression Profiles | |||||
|---|---|---|---|---|---|
| Reference | Study Design (No. Patients) |
Type of Tumor | Type of irAE | Associations | |
| Wölffer M. [131] | Prospective (n = 95) |
Melanoma | All types | VARs on SMAD3 gene | Pancreatitis |
| CNVs on IL1RN and deletions on PRDM1 genes | Higher risk of irAEs | ||||
| Duplications on CD274 and CNVs on SLCO1B1 genes | Hepatitis | ||||
| CNVs on PRDM1 and CD274 genes | Encephalitis | ||||
| CNVs on PRDM1, CD274, TSHR and FAN1 genes | Myositis | ||||
| Abdel-Wahab N. [132] | Retrospective | Melanoma | All types | Several SNPs on GABRP, DSC2, BAZ2B, SEMA5A, OSBPL6, AGPS and LOC102724355, and near CFAP65 and LOC100129175 genes | Higher risk of irAEs |
| (n = 89) | Several SNPs on LOC105377125, RGMA, ANKRD42, PACRG, FAR2, LOC105374140, ROBO1, GLIS3, PVT1, PACRG and PREX2 genes | Lower risk of irAEs | |||
| Refae S. [133] | Retrospective (n = 94) |
Pan-tumor | All types | Several SNPs on UNG, IFNW1, PD-L1, IFBL4 and CTLA-4 genes | Higher risk of irAEs |
| Jin Y. [134] | Retrospective (n = 46) |
Gastric cancer | All types | Alterations in CEBPA, FGFR4, MET or KMT2B genes # | Higher risk of irAEs |
| Bins S. [135] | Retrospective (n = 322) |
NSCLC | All types | Homozygous 804C > T (rs2227981) SNP on PDCD1 gene | Lower risk of any grade of irAEs |
| Kobayashi M. [136] | Retrospective (n = 106) |
Renal cell cancer | All types | PD-1.6 SNP (G allele) on PDCD1 gene (rs10204525) | Higher risk of severe and multiple irAEs |
| Khan Z. [137] | Retrospective (n = 479) |
Bladder cancer | Skin irAEs | Genetic variants related to vitiligo and psoriasis, assessed by a polygenic risk score |
Higher risk of irAEs and better survival |
| Khan Z. [138] | Retrospective (n = 6075) |
Pan-tumor | Thyroid dysfunction | Genetic variants related to autoimmune hypothyroidism, assessed by a polygenic risk score |
Higher risk of irAEs and better survival |
| Friedlander P. [139] | Prospective (n = 150) |
Melanoma | Diarrhea/colitis | Gene signature composed of 16 inflammation-related genes (CARD12, CCL3, CCR3, CXCL1, F5, FAM210B, GADD45A, IL18bp, IL2RA, IL5, IL8, MMP9, PTGS2, SOCS3, TLR9, UBE2C) |
Differentiation between grade 0–1 and grade 2–4 diarrhea |
| Sahabi V. [140] | Prospective (n = 162) |
Melanoma | Gastrointestinal irAEs | Increase in expression of CD177, CEACAM1 and immunoglobulin-related genes (IGHA1, IGHA2, IGHG1, and IGHV4–31) | Higher risk of gastrointestinal irAEs |
| Finke D. [141] | Retrospective (n = 19) |
All types | Myocarditis | Upregulation of 3784 genes with overexpression of interferon-γ and inflammasome-regulating proteins (GBP5 and 6) | Higher risk of myocarditis |
| Adam BA. [142] | Retrospective (n = 75) * |
All types | AIN | Overexpression of IFI27 gene (related to interferon-α) | Discrimination between AIN and TCMR |
| Zhang Y. [143] | Preclinical study (n not applicable) |
Not applicable | Thyroid dysfunction | Overexpression of ALB, MAPK1, SPP1, PPARG and MIF genes | Hypothyroidism |
| Overexpression of ALB, FCGR2B, CD44, LCN2, and CD74 genes | Hyperthyroidism | ||||
| Jing Y. [144] | Retrospective (n = 18,706) |
Pan-tumor (26 types) |
General irAEs | Overexpression of LCP1 and ADPGK genes | Higher risk of irAEs |
| HLA Antigens | |||||
| Reference | Study Design (No. Patients) |
Type of Tumor | Type of irAE | Associations | |
| Kobayashi T. [161] | Retrospective (n = 62) |
All types | Endocrine irAEs | HLA-Cw12, HLA DR-15, HLA-DQ7 and HLA DPw9 | ACTH deficiency |
| HLA-Cw12 and HLA-DR15 | Hypophysitis | ||||
| HLA-DRB3*01:01 | Thrombocytopenia | ||||
| Jiang N. [163] | Retrospective (n = 530) |
Pan-tumor | All types | HLA-DPB1*04:02 | Hypokalemia, hyponatremia, leukopenia and anemia |
| HLA-A*26:01 | Hyperbilirubinemia | ||||
| Capelli LC. [159] | Retrospective (n = 26) |
Pan-tumor | Articular irAEs | HLA-DRB1*04:05 | Inflammatory arthritis |
| Correale P. [166] | Retrospective (n = 256, 29 with pneumonitis) |
Pan-tumor | Lung irAEs | HLA-B*35 and HLA-DRB1*11 | Pneumonitis |
| Wölffer M. [131] | Prospective (n = 95) |
Melanoma | All types | HLA class I homozygosity | Hepatitis |
| Stamatouli AM. [154] | Retrospective (n = 27) |
Pan-tumor | Endocrine irAEs | HLA-DR4 | T1DM |
| Lo Preiato V. [155] | Retrospective ** (n =200) |
Pan-tumor | All types | HLA-DR4 | T1DM |
| Inaba H. [167] | Retrospective (n = 25) |
Pan-tumor | All types | HLA-B*46:01, HLA-C*14:02, HLA-DPA1*0103 and HLA-DPB1*02:01 |
Higher risk of thyroid dysfunction |
| HLA-DPB1*05:01 | Lower risk of thyroid dysfunction | ||||
| Inaba H. [168] | Retrospective (n = 871, 7 with T1DM) |
Pan-tumor | T1DM | HLA-DPA1*02:02, HLA-DPB1*05:01 and HLA-DRB1*04:05 | T1DM |
| Shi Y. [157] | Retrospective ** (n = 26) |
Pan-tumor | APST2 | HLA-DR4 | APST2 |
| Chang H. [160] | Prospective (n = 290, 7 with encephalitis) |
Breast and bladder cancer |
Encephalitis | HLA-B*27:05 | Encephalitis |
| Yano S. [153] | Retrospective (n = 11) |
Pan-tumor | Pituitary irAEs | HLA-DR15, HLA-B52 and HLA-Cw12 | Hypophysitis |
| Abed A. [164] | Retrospective (n = 179) |
NSCLC | All types | HLA class I (but not class II) homozygosity | Lower risk of irAEs, especially pneumonitis |
| HLA-A03 | Higher risk of irAEs | ||||
| Hasan Ali O. [162] | Prospective (n = 102) |
NSCLC Melanoma |
All types | HLA-DRB1*11:01 | Pruritus |
| HLA-DQB1*03:01 | Colitis | ||||
| Kotwal A. [156] | Prospective (n = 10) |
Pan-tumor | Endocrine irAEs | HLA-DR4-DR53 and HLA-DR15 | Thyroiditis |
| Purde MT. [165] | Prospective (n = 131, 11 hepatitis) |
NSCLC Melanoma |
Hepatitis | HLA- DRB1*04:01 and HLA- DRB1*15:01-DQB1*06:02 | Hepatitis |
| Clotman K. [152] | Retrospective ** (n = 42) |
Pan-tumor | T1DM | HLA-DR3-DQ2, HLA-DRB1*04, HLA-DQB1*03:02, HLA-DR4, HLA-A2 and HLA-DR3DQ3, among others |
T1DM |
| Magis Q. [169] | Retrospective (n = 163, 5 with T1DM) |
Not available | T1DM | HLA-DRB01*03 or HLA-DRB01*04 | T1DM |
| Micro-RNAs | |||||
| Reference | Study Design (Sample Size) |
Type of Tumor | Type of irAE | Associations | |
| Marschner D. [176] | Prospective (n = 179) |
Pan-tumor | All types | Underexpression of miR-146a by SNP on MIR146A gene (rs2910164) |
Higher risk of severe irAEs |
| Ivanova E. [177] | Prospective (n = 86) |
ccRCC | All types | Underexpression of miR-146a by SNP on MIR146A gene (rs2910164) |
Higher risk of severe irAEs |
| Xia W. [178] | Mouse model | Not applicable | Myocarditis | Overexpression of miR-34a-5p induced by PD-1 inhibitor-treated macrophages led to cardiac senescence | Higher risk of myocarditis |
* The study included 75 kidney biopsies. ** The study consisted of a literature review. # All of them with a p = 0.09. Abbreviations in alphabetical order (except for gene designations): ACTH, adrenocorticotropic hormone; AIN, acute interstitial nephritis; APST2, autoimmune polyglandular syndrome type 2; ccRCC, clear cell renal cell carcinoma; CNV, copy number variation; GBP5, guanylate binding protein 5; GBP6, guanylate binding protein 6; HLA, human leukocyte antigen; irAE, immune-related adverse event; miR, micro-RNA; No, number; NSCLC, non-small cell lung cancer; SNP, single nucleotide polymorphism; TCMR, T cell-mediated rejection; T1DM, type 1 diabetes mellitus; VARs, small variations.
Another micro-RNA called miR-34a-5p, related to cardiac injury by doxorubicin and cardiac senescence [182], was found to be involved in ICI-induced cardiotoxicity in an animal model [178]. Interestingly, miR-34a-5p has been shown to modulate the response of M1 macrophages, CD4+ and CD8+ T cells by downregulation of chemokine signaling, specifically of CXCR3 and its ligands CXCL10 and CXCL11 [183].
3.2.5. Gastrointestinal Microbiome
The term gastrointestinal, or gut, microbiome refers to a complex system of microorganisms, mainly bacteria, that inhabit the intestine establishing a symbiotic relationship with the host and participating in several homeostatic processes that contribute to the host’s health [184]. Already known to be involved in the pathogenesis of several immune-based disorders, especially those related to inflammatory bowel diseases [185,186,187], the gut microbiome has also been shown to modulate both intestinal and non-intestinal irAEs [188]. Gut dysbiosis, characterized by a reduction in microbiome diversity and resulting dominance of certain bacteria in the gut, may increase or decrease the anti-tumoral response and the risk of developing irAEs induced by ICIs [189]. As with other irAEs, patients experiencing ICI-induced colitis appear to have better antitumor responses and cancer-related prognosis [190]. An abundance of Bacteroidetes phylum has long been known to be a feature of colitis-resistant patients [191], while a microbiome rich in Faecalibacterium and other members of Firmicutes is associated with an elevated risk of ICI-related colitis [63]. Recently, a well-designed cohort study has confirmed the impact of specific microbial signatures, enriched with Lachnospiraceae spp. and Streptococcaceae spp., on certain irAEs [192]. In another prospective cohort study, Chau et al. found that the gut microbiome of patients not developing irAEs was relatively enriched with Bifidobacterium and Desulfovibrio species [193]. Indeed, over recent years, the collection of intestinal commensal micro-organisms potentially related to irAEs has expanded (Table 4) [63,109,186,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204].
Table 4.
Summary of gut microbiome members related to the risk of developing immune-related adverse events.
| Type of Taxonomic Category or Microorganism | Type of Effect | Type of irAE Assessed | Related References |
|---|---|---|---|
| Bacteroidetes phylum * | Protective factor | Colitis | Dubin K. Nat Commun 2016 [191] Chaput N. Ann Oncol 2019 [63] Liu T. Immunotherapy 2019 [194] Sakai K. Front Oncol 2021 [186] Liu W. Front Immunol 2021 [195] |
| Bacteroidetes phylum | Protective factor | Pancreatic irAEs | Tan B. Thorac Cancer 2021 [196] |
|
Bacteroides dorei
Bacteroides vulgatus |
Risk factor Protective factor |
General irAEs | Usyk M. Genome Med 2021 [197] |
|
Bacteroides fragilis
Bacteroides thetaiotaomicron |
Protective factor | Colitis (in mice) | Vétizou M. Science 2015 [198] |
|
Bacteroides thetaiotaomicron
Bacteroides faecis |
Risk factor | Myocarditis | Gil-Cruz C. Science 2019 [199] |
| Bacteroides intestinalis | Risk factor | General irAEs (grade ≥ 3) |
Andrews MC. Nat Med 2021 [109] |
| Prevotellamassilia timonensis (from Bacteroidetes phylum) | Risk factor | Severe colitis | Mao J. J Immunother Cancer 2021 [190] |
| Firmicutes phylum ** | Risk factor | Colitis | Dubin K. Nat Commun 2016 [191] Chaput N. Ann Oncol 2019 [63] Gopalakrishnan V. Science 2018 [188] Liu T. Immunotherapy 2019 [194] |
| Firmicutes phylum | Risk factor | Pancreatic irAEs | Tan B. Thorac Cancer 2021 [196] |
| Phascolarctobacterium genus (from Firmicutes phylum) | Protective factor | Colitis | Liu T. Immunotherapy 2019 [194] |
| Faecalibacterium genus (from Firmicutes phylum) | Protective factor | Absent or grade 0–2 colitis |
Liu W. Front Immunol 2021 [195] |
|
Bifidobacterium
Bifidobacterium breve # |
Protective factor | Colitis (in mice) | Wang F. Proc Natl Acad Sci USA 2018 [200] Sun S. Proc Natl Acad Sci USA 2020 [201] |
| Bifidobacterium | Protective factor | General irAEs | Chau J. J Clin Oncol 2021 [193] |
| Lactobacillus rhamnosum | Protective factor | Colitis (in mice) | Sun S. Proc Natl Acad Sci USA 2020 [201] |
|
Lactobacillaceae family Raoultella genus Akkermansia species Agathobacter genus |
Protective factor Protective factor Protective factor Risk factor |
Low-grade irAEs Low-grade irAEs Low-grade irAEs High-grade irAEs |
Hakozaki T. Cancer Immunol Res 2020 [202] |
| Enterobacteriaceae family † | Protective factor (remission of colitis) |
Colitis | Sakurai T. Mol Oncol 2022 [189] |
|
Intestinibacter barlettii
Anaerotignum lactatifermentans Dorea formicigenerans |
Risk factor Protective factor Protective factor |
General irAEs (grade ≥ 3) |
Andrews MC. Nat Med 2021 [109] |
|
Streptococcus genus Paecalibacterium genus Stenotrophomonas genus |
Risk factor | General irAEs (grade ≥ 3) |
Liu W. Front Immunol 2021 [195] |
|
Lachnospiraceae species Streptococcaceae species |
Risk factor | General irAEs | McCulloch JA. Nat Med 2022 [192] |
| Akkermansia muciniphila | Protective factor | Colitis | Wang L. Gut 2020 [203] |
| Alispides genus | Protective factor | Pancreatic irAEs | Tan B. Thorac Cancer 2021 [196] |
| Lachnospiraceae genus | Risk factor | Pancreatic irAEs | Tan B. Thorac Cancer 2021 [196] |
| Burkholderia cepacia | Protective factor | Colitis in mice | Vétizou M. Science 2015 [198] |
| Proteobacteria phylum | |||
| Desulfovibrio | Protective factor | General irAEs | Chau J. J Clin Oncol 2021 [193] |
| Veillonela | Risk factor | Colitis | Liu T. Immunotherapy 2019 [194] |
| Staphylococcus epidermidis | Risk factor | Dermatitis (in mice) | Hu ZI. Proc Natl Acad Sci USA 2022 [204] |
* Including Bacteroidaceae, Rikenellaceae and Barnesiellaceae families. ** Including Ruminococcaceae, Clostridium cluster XIVa, Blautia, and Faecalibacterium. # Only for Bifidobacterium breve, but not for other Bifidobacterium strains. † Including operational taxonomic units classified as Shigella flexneri, Citrobacter, Klebsiella pneumoniae, Enterobacter cloacae, and other unclassified Enterobacteriaceae. Abbreviations in alphabetical order: irAE, immune-related adverse event.
There are many hypothetical underlying mechanisms, likely interconnected, explaining the contribution of the gut microbiome to immune-related toxicity: dysregulation between pro-inflammatory (i.e., IL-6) and anti-inflammatory (i.e., IL-10) interleukins at local and distant tissues [198]; differentiation, expansion and migration of gut mucosal Th17 cells; inactivation of gut-associated regulatory T cells leading to exacerbation of T-cell effector activities [205]; a role of microbiome metabolites such as short-chain fatty acids [205], polyamine transport system and group B vitamins [181], and microbial fragments such as polysaccharide A [206]. As already mentioned in the “Cytokine” section, overexpression of IL-1β and IL-17, but not of TNF-α, has been demonstrated by two independent groups in samples from patients with ICI-induced colitis [5,109]. All these findings open the door to gut microbiota manipulation using various strategies, such as the administration of antibiotics [86], prebiotics, probiotics, or postbiotics [196,201], or fecal microbiota transplantation [200,207,208,209,210], as well as cytokine-targeted therapies for specific irAEs [211]. Nonetheless, many questions remain unanswered in the complex phenomenon of interaction between the gut microbiome and ICI-related toxicity.
3.2.6. Upcoming Biomarkers for irAE Prediction
Neoantigens are immunogenic peptides derived from tumor-specific genetic alterations and presented to T cells only on the malignant cell surface in the presence of the HLA system [212]. Nowadays, the detection of neoantigens, which are tumor and individual-specific, is being used as a way to design targeted therapies based on T-cell-mediated cytotoxicity with a low incidence of irAEs [213]. One of these neoantigens, namely, napsin A, has already been identified as a lung tumor self-antigen present in both lung malignant cells and ICI-induced inflammatory lung lesions [214]. Furthermore, Tahir et al. conducted a serological analysis of recombinant cDNA expression, a technique designed to identify tumor antigens, resulting in the detection of specific anti-CD74 autoantibodies related to pneumonitis, and anti-GNAL and anti-ITM2B autoantibodies related to hypophysitis [215].
In addition, autoantibody signatures profiled using the HuProt human proteome microarray system, which tests a massive number of proteins, may become a prominent tool for predicting toxicity [216], or even efficacy and toxicity simultaneously [217], in the short-to-medium term. Likewise, by means of a microarray autoantigen panel including 120 autoantibodies, Ghosh et al. showed that patients most likely to experience irAEs had lower baseline autoantibody titers and larger increases in these titers over time [39].
Given the complex nature of irAEs and the difficulty of predicting their onset, an approach based on the combination of different omics disciplines, including radiomics [218], together with real-time big data exploitation is on the horizon [219].
4. Conclusions
The field of ICI-related toxicity is evolving rapidly [220]. Nowadays, we are witnessing rapid growth in publications on potentially predictive irAE biomarkers [208]. Despite this boom in research, no biomarkers have yet been validated for clinical use. Except for routine laboratory testing, such as complete blood cell count with differential, glucose, renal and liver function tests and thyroid-stimulating hormone measurements, analysis of other laboratory parameters is not recommended before starting ICI therapy [221,222].
Hence, the first question is, Are any known biomarkers capable of predicting toxicity? and the answer is no, at least for most patients. In certain clinical scenarios, we can use some biomarkers for decision-making. Specifically, in the case of patients with a pre-existing autoimmune disease who would benefit from an ICI, measurement of autoantibodies known to be useful in assessing autoimmune disease activity may be indicated [19]. For instance, a high titer of anti-double-stranded DNA antibodies could represent a risk factor for developing a flare in a patient diagnosed with lupus before starting ICI therapy. Likewise, a progressive increase in anti-double-stranded DNA antibody titers could anticipate a lupus flare once an ICI has been initiated.
The identification of versatile biomarkers is also made more complex by the pathogenic mechanisms involved in irAEs, which are diverse and heterogeneous [223]. Hence, not all biomarkers under study are equally applicable to all patients. A pragmatic approach would be to design risk toxicity scores that are cross-sectionally applicable to different settings and include accessible and understandable biomarkers [125,217]. To our knowledge, there are currently no multi-factor prediction models combining baseline patient characteristics with autoantibody titers, blood cell counts or ratios, and levels of easily measurable cytokines. Besides static predictive models, longitudinal data on biomarker fluctuations, such as blood cell counts, autoantibodies, and cytokines, may provide a more reliable approach to assessing the individual risk of experiencing irAEs. Moreover, incorporation into standard practice of more sophisticated but increasingly widespread diagnostic tools, such as HLA genotyping, and measurement of micro-RNA expression, genetic variation and gene expression, and gut microbiome signatures, will depend on their future validation and availability. In this regard, results from emerging research based on artificial intelligence, big data and machine learning as methods for creating predictive models of toxicity are particularly promising [219,224,225].
From a practical point of view, another question that arises is, Once toxicity appears in a particular patient treated with ICIs, would any of these potential biomarkers be reliable for categorizing this toxicity as immune-mediated? If that were to be the case, biomarkers could be recommended as a support tool for the differential diagnosis of a particular complication. In this clinical situation, certain hormone profiles already represent a valuable test for the identification of immune-related endocrinopathies in routine practice. In addition, some biomarkers such as fecal lactoferrin and calprotectin might suggest an immune-mediated process underlies new-onset diarrhea and reduce the number of endoscopic procedures, especially during the recovery phase from colitis. In a more general sense, the elevation of acute phase reactants, such as C-reactive protein, could also point to an immune-related etiology when faced with a nonspecific clinical picture without a clear diagnosis. Nonetheless, such generic biomarkers of inflammation can be difficult to interpret in the context of advanced cancer or concomitant infection.
In conclusion, a better understanding of the pathogenic mechanisms linked to immune-mediated toxicity and the implementation of long-term, prospective, and real-life studies on irAEs are needed to confirm the validity of numerous biomarkers under investigation and enable their adoption in practice in a wide range of clinical scenarios.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15051629/s1, Figure S1. Diagram flow of studies identified via PubMed, screened, and finally included in the review, based on the PRISMA 2020 statement. References [226,227] are cited in supplementary materials.
Author Contributions
Conceptualization, I.L. and M.M.; writing—original draft preparation, I.L., M.M. and V.A.; writing—review and editing, I.P.-F., M.C., L.T., N.T., A.C.-C., I.E., G.K. and D.E.; supervision, G.K. and D.E. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research is supported by a grant for Health Research and Development Projects 2020 from the Basque Government (reference number: 2020111056).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Postow M.A., Callahan M.K., Wolchok J.D. Immune Checkpoint Blockade in Cancer Therapy. J. Clin. Oncol. 2015;33:1974–1982. doi: 10.1200/JCO.2014.59.4358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson R.A.M., Evans T.R.J., Fraser A.R., Nibbs R.J.B. Immune Checkpoint Inhibitors: New Strategies to Checkmate Cancer. Clin. Exp. Immunol. 2018;191:133–148. doi: 10.1111/cei.13081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postow M.A., Sidlow R., Hellmann M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018;378:158–168. doi: 10.1056/NEJMra1703481. [DOI] [PubMed] [Google Scholar]
- 4.Les I., Pérez-Francisco I., Cabero M., Sánchez C., Hidalgo M., Teijeira L., Arrazubi V., Domínguez S., Anaut P., Eguiluz S., et al. Prediction of Immune-Related Adverse Events Induced by Immune Checkpoint Inhibitors with a Panel of Autoantibodies: Protocol of a Multicenter, Prospective, Observational Cohort Study. Front. Pharmacol. 2022;13:894550. doi: 10.3389/fphar.2022.894550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poto R., Troiani T., Criscuolo G., Marone G., Ciardiello F., Tocchetti C.G., Varricchi G. Holistic Approach to Immune Checkpoint Inhibitor-Related Adverse Events. Front. Immunol. 2022;13:804597. doi: 10.3389/fimmu.2022.804597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneider B.J., Naidoo J., Santomasso B.D., Lacchetti C., Adkins S., Anadkat M., Atkins M.B., Brassil K.J., Caterino J.M., Chau I., et al. Management of Immune-Related Adverse Events in Patients Treated with Immune Checkpoint Inhibitor Therapy: ASCO Guideline Update. J. Clin. Oncol. 2021;39:4073–4126. doi: 10.1200/JCO.21.01440. [DOI] [PubMed] [Google Scholar]
- 7.Petrelli F., Grizzi G., Ghidini M., Ghidini A., Ratti M., Panni S., Cabiddu M., Ghilardi M., Borgonovo K., Parati M.C., et al. Immune-Related Adverse Events and Survival in Solid Tumors Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. J. Immunother. 2020;43:1–7. doi: 10.1097/CJI.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 8.Zhou X., Yao Z., Yang H., Liang N., Zhang X., Zhang F. Are Immune-Related Adverse Events Associated with the Efficacy of Immune Checkpoint Inhibitors in Patients with Cancer? A Systematic Review and Meta-Analysis. BMC Med. 2020;18:87. doi: 10.1186/s12916-020-01549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park R., Lopes L., Saeed A. Anti-PD-1/L1-Associated Immune-Related Adverse Events as Harbinger of Favorable Clinical Outcome: Systematic Review and Meta-Analysis. Clin. Transl. Oncol. 2021;23:100–109. doi: 10.1007/s12094-020-02397-5. [DOI] [PubMed] [Google Scholar]
- 10.Chennamadhavuni A., Abushahin L., Jin N., Presley C.J., Manne A. Risk Factors and Biomarkers for Immune-Related Adverse Events: A Practical Guide to Identifying High-Risk Patients and Rechallenging Immune Checkpoint Inhibitors. Front. Immunol. 2022;13:779691. doi: 10.3389/fimmu.2022.779691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Food and Drug Administration. National Institutes of Health . BEST (Biomarkers, EndpointS and Other Tools) Resource. FDA-NIH Biomarker Working Group; Silver Spring, MD, USA: 2016. [PubMed] [Google Scholar]
- 12.Califf R.M. Biomarker Definitions and Their Applications. Exp. Biol. Med. 2018;243:213–221. doi: 10.1177/1535370217750088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kobayashi T., Iwama S., Yasuda Y., Okada N., Tsunekawa T., Onoue T., Takagi H., Hagiwara D., Ito Y., Morishita Y., et al. Patients with Antithyroid Antibodies Are Prone to Develop Destructive Thyroiditis by Nivolumab: A Prospective Study. J. Endocr. Soc. 2018;2:241–251. doi: 10.1210/js.2017-00432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Music M., Iafolla M., Soosaipillai A., Batruch I., Prassas I., Pintilie M., Hansen A.R., Bedard P.L., Lheureux S., Spreafico A., et al. Predicting Response and Toxicity to PD-1 Inhibition Using Serum Autoantibodies Identified from Immuno-Mass Spectrometry. F1000Research. 2020;9:337. doi: 10.12688/f1000research.22715.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Itzstein M.S., Khan S., Gerber D.E. Investigational Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Event Prediction and Diagnosis. Clin. Chem. 2020;66:779–793. doi: 10.1093/clinchem/hvaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glehr G., Riquelme P., Yang Zhou J., Cordero L., Schilling H.-L., Kapinsky M., Schlitt H.J., Geissler E.K., Burkhardt R., Schmidt B., et al. External Validation of Biomarkers for Immune-Related Adverse Events after Immune Checkpoint Inhibition. Front. Immunol. 2022;13:1011040. doi: 10.3389/fimmu.2022.1011040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghosh N., Chan K.K., Jivanelli B., Bass A.R. Autoantibodies in Patients with Immune-Related Adverse Events from Checkpoint Inhibitors: A Systematic Literature Review. JCR J. Clin. Rheumatol. 2022;28:e498–e505. doi: 10.1097/RHU.0000000000001777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salim A., Tapia Rico G., Shaikh A., Brown M. A Systematic Review of Immune Checkpoint Inhibitor-Related Neurological Adverse Events and Association with Anti-Neuronal Autoantibodies. Expert Opin. Biol. Ther. 2021;21:1237–1251. doi: 10.1080/14712598.2021.1897101. [DOI] [PubMed] [Google Scholar]
- 19.Kostine M., Finckh A., Bingham C.O., Visser K., Leipe J., Schulze-Koops H., Choy E.H., Benesova K., Radstake T.R.D.J., Cope A.P., et al. EULAR Points to Consider for the Diagnosis and Management of Rheumatic Immune-Related Adverse Events due to Cancer Immunotherapy with Checkpoint Inhibitors. Ann. Rheum. Dis. 2021;80:36–48. doi: 10.1136/annrheumdis-2020-217139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mammen A.L., Rajan A., Pak K., Lehky T., Casciola-Rosen L., Donahue R.N., Lepone L.M., Zekeridou A., Pittock S.J., Hassan R., et al. Pre-Existing Antiacetylcholine Receptor Autoantibodies and B Cell Lymphopaenia Are Associated with the Development of Myositis in Patients with Thymoma Treated with Avelumab, an Immune Checkpoint Inhibitor Targeting Programmed Death-Ligand 1. Ann. Rheum. Dis. 2019;78:150–152. doi: 10.1136/annrheumdis-2018-213777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasan Ali O., Bomze D., Ring S.S., Berner F., Fässler M., Diem S., Abdou M.-T., Hammers C., Emtenani S., Braun A., et al. BP180-Specific IgG Is Associated with Skin Adverse Events, Therapy Response, and Overall Survival in Non-Small Cell Lung Cancer Patients Treated with Checkpoint Inhibitors. J. Am. Acad. Dermatol. 2020;82:854–861. doi: 10.1016/j.jaad.2019.08.045. [DOI] [PubMed] [Google Scholar]
- 22.Seki M., Kitano S., Suzuki S. Neurological Disorders Associated with Immune Checkpoint Inhibitors: An Association with Autoantibodies. Cancer Immunol. Immunother. 2022;71:769–775. doi: 10.1007/s00262-021-03053-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osorio J.C., Ni A., Chaft J.E., Pollina R., Kasler M.K., Stephens D., Rodriguez C., Cambridge L., Rizvi H., Wolchok J.D., et al. Antibody-Mediated Thyroid Dysfunction during T-Cell Checkpoint Blockade in Patients with Non-Small-Cell Lung Cancer. Ann. Oncol. 2017;28:583–589. doi: 10.1093/annonc/mdw640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basak E.A., van der Meer J.W.M., Hurkmans D.P., Schreurs M.W.J., Oomen-de Hoop E., van der Veldt A.A.M., Bins S., Joosse A., Koolen S.L.W., Debets R., et al. Overt Thyroid Dysfunction and Anti-Thyroid Antibodies Predict Response to Anti-PD-1 Immunotherapy in Cancer Patients. Thyroid. 2020;30:966–973. doi: 10.1089/thy.2019.0726. [DOI] [PubMed] [Google Scholar]
- 25.Les I., Martínez M., Narro A., Pérez I., Sánchez C., Puntí L., Anaut P., Eguiluz S., Herrera A., Domínguez S. Association of Immune-Related Adverse Events Induced by Nivolumab with a Battery of Autoantibodies. Ann. Med. 2021;53:762–769. doi: 10.1080/07853890.2021.1931956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gogas H., Stavropoulou-Giokas C., Tsoutsos D., Papadopoulos O., Markopoulos C., Pectasides D., Kirkwood J.M. Prognostic Significance of Autoimmunity during Treatment of Melanoma with Interferon. N. Engl. J. Med. 2006;354:709–718. doi: 10.1056/NEJMoa053007. [DOI] [PubMed] [Google Scholar]
- 27.Toi Y., Sugawara S., Sugisaka J., Ono H., Kawashima Y., Aiba T., Kawana S., Saito R., Aso M., Tsurumi K., et al. Profiling Preexisting Antibodies in Patients Treated with Anti-PD-1 Therapy for Advanced Non-Small Cell Lung Cancer. JAMA Oncol. 2019;5:376. doi: 10.1001/jamaoncol.2018.5860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoneshima Y., Tanaka K., Shiraishi Y., Hata K., Watanabe H., Harada T., Otsubo K., Iwama E., Inoue H., Masuda S., et al. Safety and Efficacy of PD-1 Inhibitors in Non-Small Cell Lung Cancer Patients Positive for Antinuclear Antibodies. Lung Cancer. 2019;130:5–9. doi: 10.1016/j.lungcan.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 29.Sakakida T., Ishikawa T., Chihara Y., Harita S., Uchino J., Tabuchi Y., Komori S., Asai J., Narukawa T., Arai A., et al. Safety and Efficacy of PD-1/PD-L1 Blockade in Patients with Preexisting Antinuclear Antibodies. Clin. Transl. Oncol. 2020;22:919–927. doi: 10.1007/s12094-019-02214-8. [DOI] [PubMed] [Google Scholar]
- 30.De Moel E.C., Rozeman E.A., Kapiteijn E.H., Verdegaal E.M.E., Grummels A., Bakker J.A., Huizinga T.W.J., Haanen J.B., Toes R.E.M., van der Woude D. Autoantibody Development under Treatment with Immune-Checkpoint Inhibitors. Cancer Immunol. Res. 2019;7:6–11. doi: 10.1158/2326-6066.CIR-18-0245. [DOI] [PubMed] [Google Scholar]
- 31.Giannicola R., D’Arrigo G., Botta C., Agostino R., Del Medico P., Falzea A., Barbieri V., Staropoli N., Del Giudice T., Pastina P., et al. Early Blood Rise in Auto-antibodies to Nuclear and Smooth Muscle Antigens Is Predictive of Prolonged Survival and Autoimmunity in Metastatic-non-small Cell Lung Cancer Patients Treated with PD-1 Immune-check Point Blockade by Nivolumab. Mol. Clin. Oncol. 2019;11:81–90. doi: 10.3892/mco.2019.1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Castel-Ajgal Z., Goulvestre C., Zaibet S., Arrondeau J., Bretagne M., Peyromaure M., Batteux F., Alexandre J., Goldwasser F., Huillard O. Preexisting Autoantibodies and Immune Related Adverse Events in Metastatic Urothelial Carcinoma Patients Treated by Pembrolizumab. Clin. Genitourin. Cancer. 2022;20:e362–e368. doi: 10.1016/j.clgc.2022.04.002. [DOI] [PubMed] [Google Scholar]
- 33.Barth D.A., Stanzer S., Spiegelberg J., Bauernhofer T., Absenger G., Posch F., Lipp R., Halm M., Szkandera J., Balic M., et al. Evaluation of Autoantibodies as Predictors of Treatment Response and Immune-related Adverse Events during the Treatment with Immune Checkpoint Inhibitors: A Prospective Longitudinal Pan-cancer Study. Cancer Med. 2022;11:3074–3083. doi: 10.1002/cam4.4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang D., Shi Y., Liu X., Liu J., Xu Y., Zhao J., Zhong W., Käsmann L., Hakozaki T., Provencio M., et al. Safety and Efficacy of Immune Checkpoint Inhibitors in Non-Small Cell Lung Cancer Patients with Preexisting Antinuclear Antibodies: A Retrospective Cohort Study. Transl. Lung Cancer Res. 2022;11:1420–1433. doi: 10.21037/tlcr-22-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang H., Geng R., Xu X., Wang Y., Zhou J., Zhang S., Zhao L., Guan M., Bai C. Safety and Efficacy of PD-1/PD-L1 Inhibitors in Cancer Patients with Preexisting Autoantibodies. Front. Immunol. 2022;13:893179. doi: 10.3389/fimmu.2022.893179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Izawa N., Shiokawa H., Onuki R., Hamaji K., Morikawa K., Saji H., Ohashi H., Kasugai S., Hayakawa N., Ohara T., et al. The Clinical Utility of Comprehensive Measurement of Autoimmune Disease-Related Antibodies in Patients with Advanced Solid Tumors Receiving Immune Checkpoint Inhibitors: A Retrospective Study. ESMO Open. 2022;7:100415. doi: 10.1016/j.esmoop.2022.100415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mouri A., Kaira K., Yamaguchi O., Hashimoto K., Miura Y., Shiono A., Shinomiya S., Akagami T., Imai H., Kobayashi K., et al. Efficacy and Feasibility of Programmed Death-1/Programmed Death Ligand-1 Blockade Therapy in Non-Small Cell Lung Cancer Patients with High Antinuclear Antibody Titers. Front. Oncol. 2021;11:610952. doi: 10.3389/fonc.2021.610952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alserawan L., Anguera G., Zamora Atenza C., Serra López J., Martínez-Martínez L., Riudavets Melià M., Sullivan I., Barba Joaquin A., Majem Tarruella M., Vidal S. Association between Changes in the Patterns of Antinuclear Autoantibodies during Immune Checkpoint Inhibition Therapy and the Development of Severe Immune Related Adverse Events. Int. J. Mol. Sci. 2022;23:12641. doi: 10.3390/ijms232012641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghosh N., Postow M., Zhu C., Jannat-Khah D., Li Q.-Z., Vitone G., Chan K.K., Bass A.R. Lower Baseline Autoantibody Levels Are Associated with Immune-Related Adverse Events from Immune Checkpoint Inhibition. J. Immunother. Cancer. 2022;10:e004008. doi: 10.1136/jitc-2021-004008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Das R., Bar N., Ferreira M., Newman A.M., Zhang L., Bailur J.K., Bacchiocchi A., Kluger H., Wei W., Halaban R., et al. Early B Cell Changes Predict Autoimmunity Following Combination Immune Checkpoint Blockade. J. Clin. Investig. 2018;128:715–720. doi: 10.1172/JCI96798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diehl A., Yarchoan M., Hopkins A., Jaffee E., Grossman S.A. Relationships between Lymphocyte Counts and Treatment-Related Toxicities and Clinical Responses in Patients with Solid Tumors Treated with PD-1 Checkpoint Inhibitors. Oncotarget. 2017;8:114268–114280. doi: 10.18632/oncotarget.23217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakamura Y., Tanaka R., Maruyama H., Ishitsuka Y., Okiyama N., Watanabe R., Fujimoto M., Fujisawa Y. Correlation between Blood Cell Count and Outcome of Melanoma Patients Treated with Anti-PD-1 Antibodies. Jpn. J. Clin. Oncol. 2019;49:431–437. doi: 10.1093/jjco/hyy201. [DOI] [PubMed] [Google Scholar]
- 43.Ma Y., Ma X., Wang J., Wu S., Wang J., Cao B. Absolute Eosinophil Count May Be an Optimal Peripheral Blood Marker to Identify the Risk of Immune-Related Adverse Events in Advanced Malignant Tumors Treated with PD-1/PD-L1 Inhibitors: A Retrospective Analysis. World J. Surg. Oncol. 2022;20:242. doi: 10.1186/s12957-022-02695-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ruste V., Goldschmidt V., Laparra A., Messayke S., Danlos F.-X., Romano-Martin P., Champiat S., Voisin A.-L., Baldini C., Massard C., et al. The Determinants of Very Severe Immune-Related Adverse Events Associated with Immune Checkpoint Inhibitors: A Prospective Study of the French REISAMIC Registry. Eur. J. Cancer. 2021;158:217–224. doi: 10.1016/j.ejca.2021.08.048. [DOI] [PubMed] [Google Scholar]
- 45.Pavan A., Calvetti L., Dal Maso A., Attili I., Del Bianco P., Pasello G., Guarneri V., Aprile G., Conte P., Bonanno L. Peripheral Blood Markers Identify Risk of Immune-Related Toxicity in Advanced Non-Small Cell Lung Cancer Treated with Immune-Checkpoint Inhibitors. Oncologist. 2019;24:1128–1136. doi: 10.1634/theoncologist.2018-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eun Y., Kim I.Y., Sun J.-M., Lee J., Cha H.-S., Koh E.-M., Kim H., Lee J. Risk Factors for Immune-Related Adverse Events Associated with Anti-PD-1 Pembrolizumab. Sci. Rep. 2019;9:14039. doi: 10.1038/s41598-019-50574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu W., Liu Y., Ma F., Sun B., Wang Y., Luo J., Liu M., Luo Z. Peripheral Blood Markers Associated with Immune-Related Adverse Effects in Patients Who Had Advanced Non-Small Cell Lung Cancer Treated with PD-1 Inhibitors. Cancer Manag. Res. 2021;13:765–771. doi: 10.2147/CMAR.S293200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bai R., Chen N., Chen X., Li L., Song W., Li W., Zhao Y., Zhang Y., Han F., Lyu Z., et al. Analysis of Characteristics and Predictive Factors of Immune Checkpoint Inhibitor-Related Adverse Events. Cancer Biol. Med. 2021;18:1118–1133. doi: 10.20892/j.issn.2095-3941.2021.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fujimoto A., Toyokawa G., Koutake Y., Kimura S., Kawamata Y., Fukuishi K., Yamazaki K., Takeo S. Association between Pretreatment Neutrophil-to-lymphocyte Ratio and Immune-related Adverse Events Due to Immune Checkpoint Inhibitors in Patients with Non-small Cell Lung Cancer. Thorac. Cancer. 2021;12:2198–2204. doi: 10.1111/1759-7714.14063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Michailidou D., Khaki A.R., Morelli M.P., Diamantopoulos L., Singh N., Grivas P. Association of Blood Biomarkers and Autoimmunity with Immune Related Adverse Events in Patients with Cancer Treated with Immune Checkpoint Inhibitors. Sci. Rep. 2021;11:9029. doi: 10.1038/s41598-021-88307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suazo-Zepeda E., Bokern M., Vinke P.C., Hiltermann T.J.N., de Bock G.H., Sidorenkov G. Risk Factors for Adverse Events Induced by Immune Checkpoint Inhibitors in Patients with Non-Small-Cell Lung Cancer: A Systematic Review and Meta-Analysis. Cancer Immunol. Immunother. 2021;70:3069–3080. doi: 10.1007/s00262-021-02996-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Egami S., Kawazoe H., Hashimoto H., Uozumi R., Arami T., Sakiyama N., Ohe Y., Nakada H., Aomori T., Ikemura S., et al. Peripheral Blood Biomarkers Predict Immune-Related Adverse Events in Non-Small Cell Lung Cancer Patients Treated with Pembrolizumab: A Multicenter Retrospective Study. J. Cancer. 2021;12:2105–2112. doi: 10.7150/jca.53242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xu H., Feng H., Zhang W., Wei F., Zhou L., Liu L., Zhao Y., Lv Y., Shi X., Zhang J., et al. Prediction of Immune-Related Adverse Events in Non-Small Cell Lung Cancer Patients Treated with Immune Checkpoint Inhibitors Based on Clinical and Hematological Markers: Real-World Evidence. Exp. Cell Res. 2022;416:113157. doi: 10.1016/j.yexcr.2022.113157. [DOI] [PubMed] [Google Scholar]
- 54.Lee P.Y., Oen K.Q.X., Lim G.R.S., Hartono J.L., Muthiah M., Huang D.Q., Teo F.S.W., Li A.Y., Mak A., Chandran N.S., et al. Neutrophil-to-Lymphocyte Ratio Predicts Development of Immune-Related Adverse Events and Outcomes from Immune Checkpoint Blockade: A Case-Control Study. Cancers. 2021;13:1308. doi: 10.3390/cancers13061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chu X., Zhao J., Zhou J., Zhou F., Jiang T., Jiang S., Sun X., You X., Wu F., Ren S., et al. Association of Baseline Peripheral-Blood Eosinophil Count with Immune Checkpoint Inhibitor-Related Pneumonitis and Clinical Outcomes in Patients with Non-Small Cell Lung Cancer Receiving Immune Checkpoint Inhibitors. Lung Cancer. 2020;150:76–82. doi: 10.1016/j.lungcan.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 56.Drobni Z.D., Zafar A., Zubiri L., Zlotoff D.A., Alvi R.M., Lee C., Hartmann S., Gilman H.K., Villani A., Nohria A., et al. Decreased Absolute Lymphocyte Count and Increased Neutrophil/Lymphocyte Ratio with Immune Checkpoint Inhibitor-Associated Myocarditis. J. Am. Heart Assoc. 2020;9:e018306. doi: 10.1161/JAHA.120.018306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takada S., Murooka H., Tahatsu K., Yanase M., Umehara K., Hashishita H., Toru H., Satoru M., Sagawa T., Fujikawa K., et al. Identifying Early Predictive Markers for Immune-Related Adverse Events in Nivolumab-Treated Patients with Renal Cell Carcinoma and Gastric Cancer. Asian Pac. J. Cancer Prev. 2022;23:695–701. doi: 10.31557/APJCP.2022.23.2.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fujisawa Y., Yoshino K., Otsuka A., Funakoshi T., Fujimura T., Yamamoto Y., Hata H., Gosho M., Tanaka R., Yamaguchi K., et al. Fluctuations in Routine Blood Count Might Signal Severe Immune-Related Adverse Events in Melanoma Patients Treated with Nivolumab. J. Dermatol. Sci. 2017;88:225–231. doi: 10.1016/j.jdermsci.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 59.Egami S., Kawazoe H., Hashimoto H., Uozumi R., Arami T., Sakiyama N., Ohe Y., Nakada H., Aomori T., Ikemura S., et al. Absolute Lymphocyte Count Predicts Immune-Related Adverse Events in Patients with Non-Small-Cell Lung Cancer Treated with Nivolumab Monotherapy: A Multicenter Retrospective Study. Front. Oncol. 2021;11:618570. doi: 10.3389/fonc.2021.618570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang Z., Xie T., Qi C., Zhang X., Shen L., Peng Z. Peripheral Blood Biomarkers Predictive of Efficacy Outcome and Immune-Related Adverse Events in Advanced Gastrointestinal Cancers Treated with Checkpoint Inhibitors. Cancers. 2022;14:3736. doi: 10.3390/cancers14153736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Subudhi S.K., Aparicio A., Gao J., Zurita A.J., Araujo J.C., Logothetis C.J., Tahir S.A., Korivi B.R., Slack R.S., Vence L., et al. Clonal Expansion of CD8 T Cells in the Systemic Circulation Precedes Development of Ipilimumab-Induced Toxicities. Proc. Natl. Acad. Sci. USA. 2016;113:11919–11924. doi: 10.1073/pnas.1611421113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oh D.Y., Cham J., Zhang L., Fong G., Kwek S.S., Klinger M., Faham M., Fong L. Immune Toxicities Elicted by CTLA-4 Blockade in Cancer Patients Are Associated with Early Diversification of the T-Cell Repertoire. Cancer Res. 2017;77:1322–1330. doi: 10.1158/0008-5472.CAN-16-2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chaput N., Lepage P., Coutzac C., Soularue E., Le Roux K., Monot C., Boselli L., Routier E., Cassard L., Collins M., et al. Baseline Gut Microbiota Predicts Clinical Response and Colitis in Metastatic Melanoma Patients Treated with Ipilimumab. Ann. Oncol. 2017;28:1368–1379. doi: 10.1093/annonc/mdx108. [DOI] [PubMed] [Google Scholar]
- 64.Granito A., Muratori L., Lalanne C., Quarneti C., Ferri S., Guidi M., Lenzi M., Muratori P. Hepatocellular Carcinoma in Viral and Autoimmune Liver Diseases: Role of CD4+ CD25+ Foxp3+ Regulatory T Cells in the Immune Microenvironment. World J. Gastroenterol. 2021;27:2994–3009. doi: 10.3748/wjg.v27.i22.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arasanz H., Bocanegra A.I., Morilla I., Fernández-Irigoyen J., Martínez-Aguillo M., Teijeira L., Garnica M., Blanco E., Chocarro L., Ausin K., et al. Circulating Low Density Neutrophils Are Associated with Resistance to First Line Anti-PD1/PDL1 Immunotherapy in Non-Small Cell Lung Cancer. Cancers. 2022;14:3846. doi: 10.3390/cancers14163846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Muir C.A., Clifton-Bligh R.J., Long G.V., Scolyer R.A., Lo S.N., Carlino M.S., Tsang V.H.M., Menzies A.M. Thyroid Immune-Related Adverse Events Following Immune Checkpoint Inhibitor Treatment. J. Clin. Endocrinol. Metab. 2021;106:e3704–e3713. doi: 10.1210/clinem/dgab263. [DOI] [PubMed] [Google Scholar]
- 67.Yoon J.H., Hong A.R., Kim H.K., Kang H.-C. Characteristics of Immune-Related Thyroid Adverse Events in Patients Treated with PD-1/PD-L1 Inhibitors. Endocrinol. Metab. 2021;36:413–423. doi: 10.3803/EnM.2020.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Luongo C., Morra R., Gambale C., Porcelli T., Sessa F., Matano E., Damiano V., Klain M., Schlumberger M., Salvatore D. Higher Baseline TSH Levels Predict Early Hypothyroidism during Cancer Immunotherapy. J. Endocrinol. Investig. 2021;44:1927–1933. doi: 10.1007/s40618-021-01508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Isawa T., Toi Y., Sugawara S., Taguri M., Toyoda S. Incidence, Clinical Characteristics and Predictors of Cardiovascular Immune-Related Adverse Events Associated with Immune Checkpoint Inhibitors. Oncologist. 2022;27:e410–e419. doi: 10.1093/oncolo/oyac056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gong Z., Wang Y. Immune Checkpoint Inhibitor–Mediated Diarrhea and Colitis: A Clinical Review. JCO Oncol. Pract. 2020;16:453–461. doi: 10.1200/OP.20.00002. [DOI] [PubMed] [Google Scholar]
- 71.Zou F., Wang X., Glitza Oliva I.C., McQuade J.L., Wang J., Zhang H.C., Thompson J.A., Thomas A.S., Wang Y. Fecal Calprotectin Concentration to Assess Endoscopic and Histologic Remission in Patients with Cancer with Immune-Mediated Diarrhea and Colitis. J. Immunother. Cancer. 2021;9:e002058. doi: 10.1136/jitc-2020-002058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Husain B., Kirchberger M.C., Erdmann M., Schüpferling S., Abolhassani A.-R., Fröhlich W., Berking C., Heinzerling L. Inflammatory Markers in Autoimmunity Induced by Checkpoint Inhibitors. J. Cancer Res. Clin. Oncol. 2021;147:1623–1630. doi: 10.1007/s00432-021-03550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shimozaki K., Sukawa Y., Sato Y., Horie S., Chida A., Tsugaru K., Togasaki K., Kawasaki K., Hirata K., Hayashi H., et al. Analysis of Risk Factors for Immune-Related Adverse Events in Various Solid Tumors Using Real-World Data. Future Oncol. 2021;17:2593–2603. doi: 10.2217/fon-2020-0861. [DOI] [PubMed] [Google Scholar]
- 74.Zhao L., Li Y., Jiang N., Song X., Xu J., Zhu X., Chen C., Kong C., Wang X., Zong D., et al. Association of Blood Biochemical Indexes and Antibiotic Exposure with Severe Immune-Related Adverse Events in Patients with Advanced Cancers Receiving PD-1 Inhibitors. J. Immunother. 2022;45:210–216. doi: 10.1097/CJI.0000000000000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Oyanagi J., Koh Y., Sato K., Mori K., Teraoka S., Akamatsu H., Kanai K., Hayata A., Tokudome N., Akamatsu K., et al. Predictive Value of Serum Protein Levels in Patients with Advanced Non-Small Cell Lung Cancer Treated with Nivolumab. Lung Cancer. 2019;132:107–113. doi: 10.1016/j.lungcan.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 76.Tas F., Yasasever V., Duranyildiz D., Camlica H., Ustuner Z., Aydiner A., Topuz E. Clinical Value of Protein S100 and Melanoma-Inhibitory Activity (MIA) in Malignant Melanoma. Am. J. Clin. Oncol. 2004;27:225–228. doi: 10.1097/01.COC.0000054895.39558.DB. [DOI] [PubMed] [Google Scholar]
- 77.Kang J.H., Bluestone J.A., Young A. Predicting and Preventing Immune Checkpoint Inhibitor Toxicity: Targeting Cytokines. Trends Immunol. 2021;42:293–311. doi: 10.1016/j.it.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 78.Tyan K., Baginska J., Brainard M., Giobbie-Hurder A., Severgnini M., Manos M., Haq R., Buchbinder E.I., Ott P.A., Hodi F.S., et al. Cytokine Changes during Immune-Related Adverse Events and Corticosteroid Treatment in Melanoma Patients Receiving Immune Checkpoint Inhibitors. Cancer Immunol. Immunother. 2021;70:2209–2221. doi: 10.1007/s00262-021-02855-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bertrand F., Montfort A., Marcheteau E., Imbert C., Gilhodes J., Filleron T., Rochaix P., Andrieu-Abadie N., Levade T., Meyer N., et al. TNFα Blockade Overcomes Resistance to Anti-PD-1 in Experimental Melanoma. Nat. Commun. 2017;8:2256. doi: 10.1038/s41467-017-02358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Perez-Ruiz E., Minute L., Otano I., Alvarez M., Ochoa M.C., Belsue V., de Andrea C., Rodriguez-Ruiz M.E., Perez-Gracia J.L., Marquez-Rodas I., et al. Prophylactic TNF Blockade Uncouples Efficacy and Toxicity in Dual CTLA-4 and PD-1 Immunotherapy. Nature. 2019;569:428–432. doi: 10.1038/s41586-019-1162-y. [DOI] [PubMed] [Google Scholar]
- 81.Yoshino K., Nakayama T., Ito A., Sato E., Kitano S. Severe Colitis after PD-1 Blockade with Nivolumab in Advanced Melanoma Patients: Potential Role of Th1-Dominant Immune Response in Immune-Related Adverse Events: Two Case Reports. BMC Cancer. 2019;19:1019. doi: 10.1186/s12885-019-6138-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Luoma A.M., Suo S., Williams H.L., Sharova T., Sullivan K., Manos M., Bowling P., Hodi F.S., Rahma O., Sullivan R.J., et al. Molecular Pathways of Colon Inflammation Induced by Cancer Immunotherapy. Cell. 2020;182:655–671.e22. doi: 10.1016/j.cell.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tanaka R., Okiyama N., Okune M., Ishitsuka Y., Watanabe R., Furuta J., Ohtsuka M., Otsuka A., Maruyama H., Fujisawa Y., et al. Serum Level of Interleukin-6 Is Increased in Nivolumab-Associated Psoriasiform Dermatitis and Tumor Necrosis Factor-α Is a Biomarker of Nivolumab Recativity. J. Dermatol. Sci. 2017;86:71–73. doi: 10.1016/j.jdermsci.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 84.Oke A.R., Wheater M., Karydis I., Wallis D. Successful Use of Adalimumab in Immune Checkpoint Inhibitor-Associated Inflammatory Arthritis. Rheumatol. Adv. Pract. 2018;2:rky001. doi: 10.1093/rap/rky001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Badran Y.R., Cohen J.V., Brastianos P.K., Parikh A.R., Hong T.S., Dougan M. Concurrent Therapy with Immune Checkpoint Inhibitors and TNFα Blockade in Patients with Gastrointestinal Immune-Related Adverse Events. J. Immunother. Cancer. 2019;7:226. doi: 10.1186/s40425-019-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Abu-Sbeih H., Ali F.S., Wang X., Mallepally N., Chen E., Altan M., Bresalier R.S., Charabaty A., Dadu R., Jazaeri A., et al. Early Introduction of Selective Immunosuppressive Therapy Associated with Favorable Clinical Outcomes in Patients with Immune Checkpoint Inhibitor–Induced Colitis. J. Immunother. Cancer. 2019;7:93. doi: 10.1186/s40425-019-0577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gao J., Miao J., Sun H., Fu X., Zhang P., Chen Z., Zhu P. TNF-α Inhibitor Ameliorates Immune-Related Arthritis and Pneumonitis in Humanized Mice. Front. Immunol. 2022;13:955812. doi: 10.3389/fimmu.2022.955812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Verheijden R.J., May A.M., Blank C.U., Aarts M.J.B., van den Berkmortel F.W.P.J., van den Eertwegh A.J.M., de Groot J.W.B., Boers-Sonderen M.J., van der Hoeven J.J.M., Hospers G.A., et al. Association of Anti-TNF with Decreased Survival in Steroid Refractory Ipilimumab and Anti-PD1–Treated Patients in the Dutch Melanoma Treatment Registry. Clin. Cancer Res. 2020;26:2268–2274. doi: 10.1158/1078-0432.CCR-19-3322. [DOI] [PubMed] [Google Scholar]
- 89.Chen A.Y., Wolchok J.D., Bass A.R. TNF in the Era of Immune Checkpoint Inhibitors: Friend or Foe? Nat. Rev. Rheumatol. 2021;17:213–223. doi: 10.1038/s41584-021-00584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alvarez M., Otano I., Minute L., Ochoa M.C., Perez-Ruiz E., Melero I., Berraondo P. Impact of Prophylactic TNF Blockade in the Dual PD-1 and CTLA-4 Immunotherapy Efficacy and Toxicity. Cell Stress. 2019;3:236–239. doi: 10.15698/cst2019.07.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Montfort A., Filleron T., Virazels M., Dufau C., Milhès J., Pagès C., Olivier P., Ayyoub M., Mounier M., Lusque A., et al. Combining Nivolumab and Ipilimumab with Infliximab or Certolizumab in Patients with Advanced Melanoma: First Results of a Phase Ib Clinical Trial. Clin. Cancer Res. 2021;27:1037–1047. doi: 10.1158/1078-0432.CCR-20-3449. [DOI] [PubMed] [Google Scholar]
- 92.Hunter C.A., Jones S.A. Erratum: Corrigendum: IL-6 as a Keystone Cytokine in Health and Disease. Nat. Immunol. 2017;18:1271. doi: 10.1038/ni1117-1271b. [DOI] [PubMed] [Google Scholar]
- 93.Valpione S., Pasquali S., Campana L.G., Piccin L., Mocellin S., Pigozzo J., Chiarion-Sileni V. Sex and Interleukin-6 Are Prognostic Factors for Autoimmune Toxicity Following Treatment with Anti-CTLA4 Blockade. J. Transl. Med. 2018;16:94. doi: 10.1186/s12967-018-1467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kang D.H., Park C.-K., Chung C., Oh I.-J., Kim Y.-C., Park D., Kim J., Kwon G.C., Kwon I., Sun P., et al. Baseline Serum Interleukin-6 Levels Predict the Response of Patients with Advanced Non-Small Cell Lung Cancer to PD-1/PD-L1 Inhibitors. Immune Netw. 2020;20:e27. doi: 10.4110/in.2020.20.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dimitriou F., Hogan S., Menzies A.M., Dummer R., Long G.V. Interleukin-6 Blockade for Prophylaxis and Management of Immune-Related Adverse Events in Cancer Immunotherapy. Eur. J. Cancer. 2021;157:214–224. doi: 10.1016/j.ejca.2021.08.031. [DOI] [PubMed] [Google Scholar]
- 96.Hailemichael Y., Johnson D.H., Abdel-Wahab N., Foo W.C., Bentebibel S.-E., Daher M., Haymaker C., Wani K., Saberian C., Ogata D., et al. Interleukin-6 Blockade Abrogates Immunotherapy Toxicity and Promotes Tumor Immunity. Cancer Cell. 2022;40:509–523.e6. doi: 10.1016/j.ccell.2022.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Campochiaro C., Farina N., Tomelleri A., Ferrara R., Lazzari C., De Luca G., Bulotta A., Signorelli D., Palmisano A., Vignale D., et al. Tocilizumab for the Treatment of Immune-Related Adverse Events: A Systematic Literature Review and a Multicentre Case Series. Eur. J. Intern. Med. 2021;93:87–94. doi: 10.1016/j.ejim.2021.07.016. [DOI] [PubMed] [Google Scholar]
- 98.McGeachy M.J., Cua D.J., Gaffen S.L. The IL-17 Family of Cytokines in Health and Disease. Immunity. 2019;50:892–906. doi: 10.1016/j.immuni.2019.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lo C.-Y., Wang C.-H., Wang C.-W., Chen C.-J., Huang H.-Y., Chung F.-T., Huang Y.-C., Lin C.-W., Lee C.-S., Lin C.-Y., et al. Increased Interleukin-17 and Glucocorticoid Receptor-β Expression in Interstitial Lung Diseases and Corticosteroid Insensitivity. Front. Immunol. 2022;13:905727. doi: 10.3389/fimmu.2022.905727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tarhini A.A., Zahoor H., Lin Y., Malhotra U., Sander C., Butterfield L.H., Kirkwood J.M. Baseline Circulating IL-17 Predicts Toxicity While TGF-Β1 and IL-10 Are Prognostic of Relapse in Ipilimumab Neoadjuvant Therapy of Melanoma. J. Immunother. Cancer. 2015;3:39. doi: 10.1186/s40425-015-0081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li D., Gál I., Vermes C., Alegre M.-L., Chong A.S.F., Chen L., Shao Q., Adarichev V., Xu X., Koreny T., et al. Cutting Edge: Cbl-b: One of the Key Molecules Tuning CD28- and CTLA-4-Mediated T Cell Costimulation. J. Immunol. 2004;173:7135–7139. doi: 10.4049/jimmunol.173.12.7135. [DOI] [PubMed] [Google Scholar]
- 102.Bouguermouh S., Fortin G., Baba N., Rubio M., Sarfati M. CD28 Co-Stimulation Down Regulates Th17 Development. PLoS ONE. 2009;4:e5087. doi: 10.1371/journal.pone.0005087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Johnson D., Patel A.B., Uemura M.I., Trinh V.A., Jackson N., Zobniw C.M., Tetzlaff M.T., Hwu P., Curry J.L., Diab A. IL17A Blockade Successfully Treated Psoriasiform Dermatologic Toxicity from Immunotherapy. Cancer Immunol. Res. 2019;7:860–865. doi: 10.1158/2326-6066.CIR-18-0682. [DOI] [PubMed] [Google Scholar]
- 104.Mazzarella L., Giugliano S., D’Amico P., Belli C., Duso B.A., Rescigno M., Curigliano G. Evidence for Interleukin 17 Involvement in Severe Immune-Related Neuroendocrine Toxicity. Eur. J. Cancer. 2020;141:218–224. doi: 10.1016/j.ejca.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 105.Yin J., Wu Y., Yang X., Gan L., Xue J. Checkpoint Inhibitor Pneumonitis Induced by Anti-PD-1/PD-L1 Therapy in Non-Small-Cell Lung Cancer: Occurrence and Mechanism. Front. Immunol. 2022;13:830631. doi: 10.3389/fimmu.2022.830631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Esfahani K., Miller W.H. Reversal of Autoimmune Toxicity and Loss of Tumor Response by Interleukin-17 Blockade. N. Engl. J. Med. 2017;376:1989–1991. doi: 10.1056/NEJMc1703047. [DOI] [PubMed] [Google Scholar]
- 107.Kurimoto C., Inaba H., Ariyasu H., Iwakura H., Ueda Y., Uraki S., Takeshima K., Furukawa Y., Morita S., Yamamoto Y., et al. Predictive and Sensitive Biomarkers for Thyroid Dysfunctions during Treatment with Immune-checkpoint Inhibitors. Cancer Sci. 2020;111:1468–1477. doi: 10.1111/cas.14363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang Y., Zou J., Li Y., Jiao X., Wang Y., Zhuo N., Gao M., Gong J., Li J., Zhang X., et al. Serological Biomarkers Predict Immune-Related Adverse Events and Clinical Benefit in Patients with Advanced Gastrointestinal Cancers. Front. Immunol. 2022;13:987568. doi: 10.3389/fimmu.2022.987568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Andrews M.C., Duong C.P.M., Gopalakrishnan V., Iebba V., Chen W.-S., Derosa L., Khan M.A.W., Cogdill A.P., White M.G., Wong M.C., et al. Gut Microbiota Signatures Are Associated with Toxicity to Combined CTLA-4 and PD-1 Blockade. Nat. Med. 2021;27:1432–1441. doi: 10.1038/s41591-021-01406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Friedrich M., Pohin M., Jackson M.A., Korsunsky I., Bullers S.J., Rue-Albrecht K., Christoforidou Z., Sathananthan D., Thomas T., Ravindran R., et al. IL-1-Driven Stromal–Neutrophil Interactions Define a Subset of Patients with Inflammatory Bowel Disease That Does Not Respond to Therapies. Nat. Med. 2021;27:1970–1981. doi: 10.1038/s41591-021-01520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schindler H., Lusky F., Daniello L., Elshiaty M., Gaissmaier L., Benesova K., Souto-Carneiro M., Angeles A.K., Janke F., Eichhorn F., et al. Serum Cytokines Predict Efficacy and Toxicity, but Are Not Useful for Disease Monitoring in Lung Cancer Treated with PD-(L)1 Inhibitors. Front. Oncol. 2022;12:1010660. doi: 10.3389/fonc.2022.1010660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Thomas A.S., Ma W., Wang Y. Ustekinumab for Refractory Colitis Associated with Immune Checkpoint Inhibitors. N. Engl. J. Med. 2021;384:581–583. doi: 10.1056/NEJMc2031717. [DOI] [PubMed] [Google Scholar]
- 113.Ngiow S.F., Young A., Blake S.J., Hill G.R., Yagita H., Teng M.W.L., Korman A.J., Smyth M.J. Agonistic CD40 MAb-Driven IL12 Reverses Resistance to Anti-PD1 in a T-Cell–Rich Tumor. Cancer Res. 2016;76:6266–6277. doi: 10.1158/0008-5472.CAN-16-2141. [DOI] [PubMed] [Google Scholar]
- 114.Garris C.S., Arlauckas S.P., Kohler R.H., Trefny M.P., Garren S., Piot C., Engblom C., Pfirschke C., Siwicki M., Gungabeesoon J., et al. Successful Anti-PD-1 Cancer Immunotherapy Requires T Cell-Dendritic Cell Crosstalk Involving the Cytokines IFN-γ and IL-12. Immunity. 2018;49:1148–1161.e7. doi: 10.1016/j.immuni.2018.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Langowski J.L., Zhang X., Wu L., Mattson J.D., Chen T., Smith K., Basham B., McClanahan T., Kastelein R.A., Oft M. IL-23 Promotes Tumour Incidence and Growth. Nature. 2006;442:461–465. doi: 10.1038/nature04808. [DOI] [PubMed] [Google Scholar]
- 116.Saraiva M., Vieira P., O’Garra A. Biology and Therapeutic Potential of Interleukin-10. J. Exp. Med. 2020;217:e20190418. doi: 10.1084/jem.20190418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang H., Zhou F., Zhao C., Cheng L., Zhou C., Qiao M., Li X., Chen X. Interleukin-10 Is a Promising Marker for Immune-Related Adverse Events in Patients with Non-Small Cell Lung Cancer Receiving Immunotherapy. Front. Immunol. 2022;13:840313. doi: 10.3389/fimmu.2022.840313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wei X., Zhang J., Gu Q., Huang M., Zhang W., Guo J., Zhou X. Reciprocal Expression of IL-35 and IL-10 Defines Two Distinct Effector Treg Subsets That Are Required for Maintenance of Immune Tolerance. Cell Rep. 2017;21:1853–1869. doi: 10.1016/j.celrep.2017.10.090. [DOI] [PubMed] [Google Scholar]
- 119.Takai R., Funakoshi Y., Suto H., Nagatani Y., Imamura Y., Toyoda M., Yakushijin K., Kiyota N., Harada K.-I., Yamashita K., et al. Serum Soluble Interleukin-2 Receptor as a Potential Biomarker for Immune-Related Adverse Events. Anticancer Res. 2021;41:1021–1026. doi: 10.21873/anticanres.14857. [DOI] [PubMed] [Google Scholar]
- 120.Hirashima T., Kanai T., Suzuki H., Yoshida H., Matsushita A., Kawasumi H., Samejima Y., Noda Y., Nasu S., Tanaka A., et al. The Levels of Interferon-Gamma Release as a Biomarker for Non-Small-Cell Lung Cancer Patients Receiving Immune Checkpoint Inhibitors. Anticancer Res. 2019;39:6231–6240. doi: 10.21873/anticanres.13832. [DOI] [PubMed] [Google Scholar]
- 121.Fujimura T., Sato Y., Tanita K., Kambayashi Y., Otsuka A., Fujisawa Y., Yoshino K., Matsushita S., Funakoshi T., Hata H., et al. Serum Levels of Soluble CD163 and CXCL5 May Be Predictive Markers for Immune-Related Adverse Events in Patients with Advanced Melanoma Treated with Nivolumab: A Pilot Study. Oncotarget. 2018;9:15542–15551. doi: 10.18632/oncotarget.24509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Khan S., Khan S.A., Luo X., Fattah F.J., Saltarski J., Gloria-McCutchen Y., Lu R., Xie Y., Li Q., Wakeland E., et al. Immune Dysregulation in Cancer Patients Developing Immune-Related Adverse Events. Br. J. Cancer. 2019;120:63–68. doi: 10.1038/s41416-018-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhao N., Yi Y., Cao W., Fu X., Mei N., Li C. Serum Cytokine Levels for Predicting Immune-Related Adverse Events and the Clinical Response in Lung Cancer Treated with Immunotherapy. Front. Oncol. 2022;12:923531. doi: 10.3389/fonc.2022.923531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ciecko A.E., Foda B., Barr J.Y., Ramanathan S., Atkinson M.A., Serreze D.V., Geurts A.M., Lieberman S.M., Chen Y.-G. Interleukin-27 Is Essential for Type 1 Diabetes Development and Sjögren Syndrome-like Inflammation. Cell Rep. 2019;29:3073–3086.e5. doi: 10.1016/j.celrep.2019.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lim S.Y., Lee J.H., Gide T.N., Menzies A.M., Guminski A., Carlino M.S., Breen E.J., Yang J.Y.H., Ghazanfar S., Kefford R.F., et al. Circulating Cytokines Predict Immune-Related Toxicity in Melanoma Patients Receiving Anti-PD-1-Based Immunotherapy. Clin. Cancer Res. 2019;25:1557–1563. doi: 10.1158/1078-0432.CCR-18-2795. [DOI] [PubMed] [Google Scholar]
- 126.Schett G., McInnes I.B., Neurath M.F. Reframing Immune-Mediated Inflammatory Diseases through Signature Cytokine Hubs. N. Engl. J. Med. 2021;385:628–639. doi: 10.1056/NEJMra1909094. [DOI] [PubMed] [Google Scholar]
- 127.McGonagle D., McDermott M.F. A Proposed Classification of the Immunological Diseases. PLoS Med. 2006;3:e297. doi: 10.1371/journal.pmed.0030297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Omarjee O., Picard C., Frachette C., Moreews M., Rieux-Laucat F., Soulas-Sprauel P., Viel S., Lega J.-C., Bader-Meunier B., Walzer T., et al. Monogenic Lupus: Dissecting Heterogeneity. Autoimmun. Rev. 2019;18:102361. doi: 10.1016/j.autrev.2019.102361. [DOI] [PubMed] [Google Scholar]
- 129.Yin X., Kim K., Suetsugu H., Bang S.-Y., Wen L., Koido M., Ha E., Liu L., Sakamoto Y., Jo S., et al. Meta-Analysis of 208370 East Asians Identifies 113 Susceptibility Loci for Systemic Lupus Erythematosus. Ann. Rheum. Dis. 2021;80:632–640. doi: 10.1136/annrheumdis-2020-219209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chye A., Allen I., Barnet M., Burnett D.L. Insights into the Host Contribution of Endocrine Associated Immune-Related Adverse Events to Immune Checkpoint Inhibition Therapy. Front. Oncol. 2022;12:894015. doi: 10.3389/fonc.2022.894015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wölffer M., Battke F., Schulze M., Feldhahn M., Flatz L., Martus P., Forschner A. Biomarkers Associated with Immune-Related Adverse Events under Checkpoint Inhibitors in Metastatic Melanoma. Cancers. 2022;14:302. doi: 10.3390/cancers14020302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Abdel-Wahab N., Diab A., Yu R.K., Futreal A., Criswell L.A., Tayar J.H., Dadu R., Shannon V., Shete S.S., Suarez-Almazor M.E. Genetic Determinants of Immune-Related Adverse Events in Patients with Melanoma Receiving Immune Checkpoint Inhibitors. Cancer Immunol. Immunother. 2021;70:1939–1949. doi: 10.1007/s00262-020-02797-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Refae S., Gal J., Ebran N., Otto J., Borchiellini D., Peyrade F., Chamorey E., Brest P., Milano G., Saada-Bouzid E. Germinal Immunogenetics Predict Treatment Outcome for PD-1/PD-L1 Checkpoint Inhibitors. Invest. New Drugs. 2020;38:160–171. doi: 10.1007/s10637-019-00845-w. [DOI] [PubMed] [Google Scholar]
- 134.Jin Y., Chen D.-L., Wang F., Yang C., Chen X.-X., You J., Huang J.-S., Shao Y., Zhu D.-Q., Ouyang Y.-M., et al. The Predicting Role of Circulating Tumor DNA Landscape in Gastric Cancer Patients Treated with Immune Checkpoint Inhibitors. Mol. Cancer. 2020;19:154. doi: 10.1186/s12943-020-01274-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bins S., Basak E.A., el Bouazzaoui S., Koolen S.L.W., de Hoop E.O., van der Leest C.H., van der Veldt A.A.M., Sleijfer S., Debets R., van Schaik R.H.N., et al. Association between Single-Nucleotide Polymorphisms and Adverse Events in Nivolumab-Treated Non-Small Cell Lung Cancer Patients. Br. J. Cancer. 2018;118:1296–1301. doi: 10.1038/s41416-018-0074-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kobayashi M., Numakura K., Hatakeyama S., Muto Y., Sekine Y., Sasagawa H., Kashima S., Yamamoto R., Koizumi A., Nara T., et al. Severe Immune-Related Adverse Events in Patients Treated with Nivolumab for Metastatic Renal Cell Carcinoma Are Associated with PDCD1 Polymorphism. Genes. 2022;13:1204. doi: 10.3390/genes13071204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Khan Z., Di Nucci F., Kwan A., Hammer C., Mariathasan S., Rouilly V., Carroll J., Fontes M., Ley Acosta S., Guardino E., et al. Polygenic Risk for Skin Autoimmunity Impacts Immune Checkpoint Blockade in Bladder Cancer. Proc. Natl. Acad. Sci. USA. 2020;117:12288–12294. doi: 10.1073/pnas.1922867117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Khan Z., Hammer C., Carroll J., Di Nucci F., Acosta S.L., Maiya V., Bhangale T., Hunkapiller J., Mellman I., Albert M.L., et al. Genetic Variation Associated with Thyroid Autoimmunity Shapes the Systemic Immune Response to PD-1 Checkpoint Blockade. Nat. Commun. 2021;12:3355. doi: 10.1038/s41467-021-23661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Friedlander P., Wood K., Wassmann K., Christenfeld A.M., Bhardwaj N., Oh W.K. A Whole-Blood RNA Transcript-Based Gene Signature Is Associated with the Development of CTLA-4 Blockade-Related Diarrhea in Patients with Advanced Melanoma Treated with the Checkpoint Inhibitor Tremelimumab. J. Immunother. Cancer. 2018;6:90. doi: 10.1186/s40425-018-0408-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Shahabi V., Berman D., Chasalow S.D., Wang L., Tsuchihashi Z., Hu B., Panting L., Jure-Kunkel M., Ji R.-R. Gene Expression Profiling of Whole Blood in Ipilimumab-Treated Patients for Identification of Potential Biomarkers of Immune-Related Gastrointestinal Adverse Events. J. Transl. Med. 2013;11:75. doi: 10.1186/1479-5876-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Finke D., Heckmann M., Salatzki J., Riffel J., Herpel E., Heinzerling L., Meder B., Völkers M., Müller O., Frey N., et al. Comparative Transcriptomics of Immune Checkpoint Inhibitor Myocarditis Identifies Guanylate Binding Protein 5 and 6 Dysregulation. Cancers. 2021;13:2498. doi: 10.3390/cancers13102498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Adam B.A., Murakami N., Reid G., Du K., Jasim R., Boils C.L., Bu L., Hill P.D., Murray A.G., Renaudin K., et al. Gene Expression Profiling in Kidney Transplants with Immune Checkpoint Inhibitor–Associated Adverse Events. Clin. J. Am. Soc. Nephrol. 2021;16:1376–1386. doi: 10.2215/CJN.00920121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhang Y., Garofano F., Wu X., Schmid M., Krawitz P., Essler M., Schmidt-Wolf I.G.H. Integrative Analysis of Key Candidate Genes and Signaling Pathways in Autoimmune Thyroid Dysfunction Related to Anti-CTLA-4 Therapy by Bioinformatics. Investig. New Drugs. 2020;38:1717–1729. doi: 10.1007/s10637-020-00952-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jing Y., Liu J., Ye Y., Pan L., Deng H., Wang Y., Yang Y., Diao L., Lin S.H., Mills G.B., et al. Multi-Omics Prediction of Immune-Related Adverse Events during Checkpoint Immunotherapy. Nat. Commun. 2020;11:4946. doi: 10.1038/s41467-020-18742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Queirolo P., Dozin B., Morabito A., Banelli B., Carosio R., Fontana V., Ferrucci P.F., Martinoli C., Cocorocchio E., Ascierto P.A., et al. CTLA-4 Gene Variant -1661A>G May Predict the Onset of Endocrine Adverse Events in Metastatic Melanoma Patients Treated with Ipilimumab. Eur. J. Cancer. 2018;97:59–61. doi: 10.1016/j.ejca.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 146.Curry J.L., Reuben A., Szczepaniak-Sloane R., Ning J., Milton D.R., Lee C.H., Hudgens C., George S., Torres-Cabala C., Johnson D., et al. Gene Expression Profiling of Lichenoid Dermatitis Immune-related Adverse Event from Immune Checkpoint Inhibitors Reveals Increased CD14+ and CD16+ Monocytes Driving an Innate Immune Response. J. Cutan. Pathol. 2019;46:627–636. doi: 10.1111/cup.13454. [DOI] [PubMed] [Google Scholar]
- 147.He X., Yu J., Shi H. Pan-Cancer Analysis Reveals Alternative Splicing Characteristics Associated with Immune-Related Adverse Events Elicited by Checkpoint Immunotherapy. Front. Pharmacol. 2021;12:797852. doi: 10.3389/fphar.2021.797852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Martín-Villa J.M., Vaquero-Yuste C., Molina-Alejandre M., Juarez I., Suárez-Trujillo F., López-Nares A., Palacio-Gruber J., Barrera-Gutiérrez L., Fernández-Cruz E., Rodríguez-Sainz C., et al. HLA-G: Too Much or Too Little? Role in Cancer and Autoimmune Disease. Front. Immunol. 2022;13:796054. doi: 10.3389/fimmu.2022.796054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Bodis G., Toth V., Schwarting A. Role of Human Leukocyte Antigens (HLA) in Autoimmune Diseases. Rheumatol. Ther. 2018;5:5–20. doi: 10.1007/s40744-018-0100-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Brown N.K., Guandalini S., Semrad C., Kupfer S.S. A Clinician’s Guide to Celiac Disease HLA Genetics. Am. J. Gastroenterol. 2019;114:1587–1592. doi: 10.14309/ajg.0000000000000310. [DOI] [PubMed] [Google Scholar]
- 151.Diaconu A.-D., Ceasovschih A., Șorodoc V., Pomîrleanu C., Lionte C., Șorodoc L., Ancuța C. Practical Significance of Biomarkers in Axial Spondyloarthritis: Updates on Diagnosis, Disease Activity, and Prognosis. Int. J. Mol. Sci. 2022;23:11561. doi: 10.3390/ijms231911561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Clotman K., Janssens K., Specenier P., Weets I., De Block C.E.M. Programmed Cell Death-1 Inhibitor–Induced Type 1 Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2018;103:3144–3154. doi: 10.1210/jc.2018-00728. [DOI] [PubMed] [Google Scholar]
- 153.Yano S., Ashida K., Sakamoto R., Sakaguchi C., Ogata M., Maruyama K., Sakamoto S., Ikeda M., Ohe K., Akasu S., et al. Human Leucocyte Antigen DR15, a Possible Predictive Marker for Immune Checkpoint Inhibitor–Induced Secondary Adrenal Insufficiency. Eur. J. Cancer. 2020;130:198–203. doi: 10.1016/j.ejca.2020.02.049. [DOI] [PubMed] [Google Scholar]
- 154.Stamatouli A.M., Quandt Z., Perdigoto A.L., Clark P.L., Kluger H., Weiss S.A., Gettinger S., Sznol M., Young A., Rushakoff R., et al. Collateral Damage: Insulin-Dependent Diabetes Induced with Checkpoint Inhibitors. Diabetes. 2018;67:1471–1480. doi: 10.2337/dbi18-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lo Preiato V., Salvagni S., Ricci C., Ardizzoni A., Pagotto U., Pelusi C. Diabetes Mellitus Induced by Immune Checkpoint Inhibitors: Type 1 Diabetes Variant or New Clinical Entity? Review of the Literature. Rev. Endocr. Metab. Disord. 2021;22:337–349. doi: 10.1007/s11154-020-09618-w. [DOI] [PubMed] [Google Scholar]
- 156.Kotwal A., Gustafson M.P., Bornschlegl S., Kottschade L., Delivanis D.A., Dietz A.B., Gandhi M., Ryder M. Immune Checkpoint Inhibitor-Induced Thyroiditis Is Associated with Increased Intrathyroidal T Lymphocyte Subpopulations. Thyroid. 2020;30:1440–1450. doi: 10.1089/thy.2020.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shi Y., Shen M., Zheng X., Chen Y., Zhao R., Gu Y., Yang T. ICPis-Induced Autoimmune Polyendocrine Syndrome Type 2: A Review of the Literature and a Protocol for Optimal Management. J. Clin. Endocrinol. Metab. 2020;105:e4208–e4218. doi: 10.1210/clinem/dgaa553. [DOI] [PubMed] [Google Scholar]
- 158.Delivanis D.A., Gustafson M.P., Bornschlegl S., Merten M.M., Kottschade L., Withers S., Dietz A.B., Ryder M. Pembrolizumab-Induced Thyroiditis: Comprehensive Clinical Review and Insights into Underlying Involved Mechanisms. J. Clin. Endocrinol. Metab. 2017;102:2770–2780. doi: 10.1210/jc.2017-00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cappelli L.C., Dorak M.T., Bettinotti M.P., Bingham C.O., Shah A.A. Association of HLA-DRB1 Shared Epitope Alleles and Immune Checkpoint Inhibitor-Induced Inflammatory Arthritis. Rheumatology. 2019;58:476–480. doi: 10.1093/rheumatology/key358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chang H., Shin Y., Keam B., Kim M., Im S., Lee S. HLA-B27 Association of Autoimmune Encephalitis Induced by PD-L1 Inhibitor. Ann. Clin. Transl. Neurol. 2020;7:2243–2250. doi: 10.1002/acn3.51213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kobayashi T., Iwama S., Sugiyama D., Yasuda Y., Okuji T., Ito M., Ito S., Sugiyama M., Onoue T., Takagi H., et al. Anti-Pituitary Antibodies and Susceptible Human Leukocyte Antigen Alleles as Predictive Biomarkers for Pituitary Dysfunction Induced by Immune Checkpoint Inhibitors. J. Immunother. Cancer. 2021;9:e002493. doi: 10.1136/jitc-2021-002493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hasan Ali O., Berner F., Bomze D., Fässler M., Diem S., Cozzio A., Jörger M., Früh M., Driessen C., Lenz T.L., et al. Human Leukocyte Antigen Variation Is Associated with Adverse Events of Checkpoint Inhibitors. Eur. J. Cancer. 2019;107:8–14. doi: 10.1016/j.ejca.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 163.Jiang N., Yu Y., Zhang M., Tang Y., Wu D., Wang S., Fang Y., Zhang Y., Meng L., Li Y., et al. Association between Germ-Line HLA and Immune-Related Adverse Events. Front. Immunol. 2022;13:952099. doi: 10.3389/fimmu.2022.952099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Abed A., Law N., Calapre L., Lo J., Bhat V., Bowyer S., Millward M., Gray E.S. Human Leucocyte Antigen Genotype Association with the Development of Immune-Related Adverse Events in Patients with Non-Small Cell Lung Cancer Treated with Single Agent Immunotherapy. Eur. J. Cancer. 2022;172:98–106. doi: 10.1016/j.ejca.2022.05.021. [DOI] [PubMed] [Google Scholar]
- 165.Purde M.-T., Niederer R., Wagner N.B., Diem S., Berner F., Hasan Ali O., Hillmann D., Bergamin I., Joerger M., Risch M., et al. Presence of Autoantibodies in Serum Does Not Impact the Occurrence of Immune Checkpoint Inhibitor-Induced Hepatitis in a Prospective Cohort of Cancer Patients. J. Cancer Res. Clin. Oncol. 2022;148:647–656. doi: 10.1007/s00432-021-03870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Correale P., Saladino R.E., Giannarelli D., Sergi A., Mazzei M.A., Bianco G., Giannicola R., Iuliano E., Forte I.M., Calandruccio N.D., et al. HLA Expression Correlates to the Risk of Immune Checkpoint Inhibitor-Induced Pneumonitis. Cells. 2020;9:1964. doi: 10.3390/cells9091964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Inaba H., Kaido Y., Ito S., Hirobata T., Inoue G., Sugita T., Yamamoto Y., Jinnin M., Kimura H., Kobayashi T., et al. Human Leukocyte Antigens and Biomarkers in Type 1 Diabetes Mellitus Induced by Immune-Checkpoint Inhibitors. Endocrinol. Metab. 2022;37:84–95. doi: 10.3803/EnM.2021.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Inaba H., Ariyasu H., Iwakura H., Kurimoto C., Takeshima K., Morita S., Furuta H., Hotomi M., Akamizu T. Distinct Clinical Features and Prognosis between Persistent and Temporary Thyroid Dysfunctions by Immune-Checkpoint Inhibitors. Endocr. J. 2021;68:231–241. doi: 10.1507/endocrj.EJ20-0371. [DOI] [PubMed] [Google Scholar]
- 169.Magis Q., Gaudy-Marqueste C., Basire A., Loundou A., Malissen N., Troin L., Monestier S., Mallet S., Hesse S., Richard M.-A., et al. Diabetes and Blood Glucose Disorders Under Anti-PD1. J. Immunother. 2018;41:232–240. doi: 10.1097/CJI.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 170.Iafolla M.A.J., Yang C., Chandran V., Pintilie M., Li Q., Bedard P.L., Hansen A., Lheureux S., Spreafico A., Razak A.A., et al. Predicting Toxicity and Response to Pembrolizumab Through Germline Genomic HLA Class 1 Analysis. JNCI Cancer Spectr. 2021;5:pkaa115. doi: 10.1093/jncics/pkaa115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Berman D., Parker S.M., Siegel J., Chasalow S.D., Weber J., Galbraith S., Targan S.R., Wang H.L. Ipilimumab efficacy and safety in patients with advanced melanoma: A retrospective analysis of HLA subtype from four trials. Cancer Immun. 2010;10:6. [PMC free article] [PubMed] [Google Scholar]
- 172.Rusca N., Monticelli S. MiR-146a in Immunity and Disease. Mol. Biol. Int. 2011;2011:437301. doi: 10.4061/2011/437301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Rajakumar T., Horos R., Jehn J., Schenz J., Muley T., Pelea O., Hofmann S., Kittner P., Kahraman M., Heuvelman M., et al. A Blood-Based MiRNA Signature with Prognostic Value for Overall Survival in Advanced Stage Non-Small Cell Lung Cancer Treated with Immunotherapy. NPJ Precis. Oncol. 2022;6:19. doi: 10.1038/s41698-022-00262-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Mastroianni J., Stickel N., Andrlova H., Hanke K., Melchinger W., Duquesne S., Schmidt D., Falk M., Andrieux G., Pfeifer D., et al. MiR-146a Controls Immune Response in the Melanoma Microenvironment. Cancer Res. 2019;79:183–195. doi: 10.1158/0008-5472.CAN-18-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hong D.S., Kang Y.-K., Borad M., Sachdev J., Ejadi S., Lim H.Y., Brenner A.J., Park K., Lee J.-L., Kim T.-Y., et al. Phase 1 Study of MRX34, a Liposomal MiR-34a Mimic, in Patients with Advanced Solid Tumours. Br. J. Cancer. 2020;122:1630–1637. doi: 10.1038/s41416-020-0802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Marschner D., Falk M., Javorniczky N.R., Hanke-Müller K., Rawluk J., Schmitt-Graeff A., Simonetta F., Haring E., Dicks S., Ku M., et al. MicroRNA-146a Regulates Immune-Related Adverse Events Caused by Immune Checkpoint Inhibitors. JCI Insight. 2020;5:e132334. doi: 10.1172/jci.insight.132334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Ivanova E., Asadullina D., Rakhimov R., Izmailov A., Izmailov A., Gilyazova G., Galimov S., Pavlov V., Khusnutdinova E., Gilyazova I. Exosomal MiRNA-146a Is Downregulated in Clear Cell Renal Cell Carcinoma Patients with Severe Immune-Related Adverse Events. Non-Coding RNA Res. 2022;7:159–163. doi: 10.1016/j.ncrna.2022.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Xia W., Chen H., Chen D., Ye Y., Xie C., Hou M. PD-1 Inhibitor Inducing Exosomal MiR-34a-5p Expression Mediates the Cross Talk between Cardiomyocyte and Macrophage in Immune Checkpoint Inhibitor–Related Cardiac Dysfunction. J. Immunother. Cancer. 2020;8:e001293. doi: 10.1136/jitc-2020-001293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Runtsch M.C., Hu R., Alexander M., Wallace J., Kagele D., Petersen C., Valentine J.F., Welker N.C., Bronner M.P., Chen X., et al. MicroRNA-146a Constrains Multiple Parameters of Intestinal Immunity and Increases Susceptibility to DSS Colitis. Oncotarget. 2015;6:28556–28572. doi: 10.18632/oncotarget.5597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bogunia-Kubik K., Wysoczańska B., Piątek D., Iwaszko M., Ciechomska M., Świerkot J. Significance of Polymorphism and Expression of MiR-146a and NFkB1 Genetic Variants in Patients with Rheumatoid Arthritis. Arch. Immunol. Ther. Exp. 2016;64:131–136. doi: 10.1007/s00005-016-0443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Srivastava A., Nikamo P., Lohcharoenkal W., Li D., Meisgen F., Xu Landén N., Ståhle M., Pivarcsi A., Sonkoly E. MicroRNA-146a Suppresses IL-17–Mediated Skin Inflammation and Is Genetically Associated with Psoriasis. J. Allergy Clin. Immunol. 2017;139:550–561. doi: 10.1016/j.jaci.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 182.Pantazi D., Tselepis A.D. Cardiovascular Toxic Effects of Antitumor Agents: Pathogenetic Mechanisms. Thromb. Res. 2022;213:S95–S102. doi: 10.1016/j.thromres.2021.12.017. [DOI] [PubMed] [Google Scholar]
- 183.Hart M., Nickl L., Walch-Rueckheim B., Krammes L., Rheinheimer S., Diener C., Taenzer T., Kehl T., Sester M., Lenhof H.-P., et al. Wrinkle in the Plan: MiR-34a-5p Impacts Chemokine Signaling by Modulating CXCL10/CXCL11/CXCR3-Axis in CD4+, CD8+ T Cells and M1 Macrophages. J. Immunother. Cancer. 2020;8:e001617. doi: 10.1136/jitc-2020-001617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Dixit K., Chaudhari D., Dhotre D., Shouche Y., Saroj S. Restoration of Dysbiotic Human Gut Microbiome for Homeostasis. Life Sci. 2021;278:119622. doi: 10.1016/j.lfs.2021.119622. [DOI] [PubMed] [Google Scholar]
- 185.Chassaing B., Darfeuille–Michaud A. The Commensal Microbiota and Enteropathogens in the Pathogenesis of Inflammatory Bowel Diseases. Gastroenterology. 2011;140:1720–1728.e3. doi: 10.1053/j.gastro.2011.01.054. [DOI] [PubMed] [Google Scholar]
- 186.Sakai K., Sakurai T., De Velasco M.A., Nagai T., Chikugo T., Ueshima K., Kura Y., Takahama T., Hayashi H., Nakagawa K., et al. Intestinal Microbiota and Gene Expression Reveal Similarity and Dissimilarity Between Immune-Mediated Colitis and Ulcerative Colitis. Front. Oncol. 2021;11:763468. doi: 10.3389/fonc.2021.763468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bellaguarda E., Hanauer S. Checkpoint Inhibitor-Induced Colitis. Am. J. Gastroenterol. 2020;115:202–210. doi: 10.14309/ajg.0000000000000497. [DOI] [PubMed] [Google Scholar]
- 188.Gopalakrishnan V., Spencer C.N., Nezi L., Reuben A., Andrews M.C., Karpinets T.V., Prieto P.A., Vicente D., Hoffman K., Wei S.C., et al. Gut Microbiome Modulates Response to Anti–PD-1 Immunotherapy in Melanoma Patients. Science. 2018;359:97–103. doi: 10.1126/science.aan4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sakurai T., De Velasco M.A., Sakai K., Nagai T., Nishiyama H., Hashimoto K., Uemura H., Kawakami H., Nakagawa K., Ogata H., et al. Integrative Analysis of Gut Microbiome and Host Transcriptomes Reveals Associations between Treatment Outcomes and Immunotherapy-induced Colitis. Mol. Oncol. 2022;16:1493–1507. doi: 10.1002/1878-0261.13062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mao J., Wang D., Long J., Yang X., Lin J., Song Y., Xie F., Xun Z., Wang Y., Wang Y., et al. Gut Microbiome Is Associated with the Clinical Response to Anti-PD-1 Based Immunotherapy in Hepatobiliary Cancers. J. Immunother. Cancer. 2021;9:e003334. doi: 10.1136/jitc-2021-003334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Dubin K., Callahan M.K., Ren B., Khanin R., Viale A., Ling L., No D., Gobourne A., Littmann E., Huttenhower C., et al. Intestinal Microbiome Analyses Identify Melanoma Patients at Risk for Checkpoint-Blockade-Induced Colitis. Nat. Commun. 2016;7:10391. doi: 10.1038/ncomms10391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.McCulloch J.A., Davar D., Rodrigues R.R., Badger J.H., Fang J.R., Cole A.M., Balaji A.K., Vetizou M., Prescott S.M., Fernandes M.R., et al. Intestinal Microbiota Signatures of Clinical Response and Immune-Related Adverse Events in Melanoma Patients Treated with Anti-PD-1. Nat. Med. 2022;28:545–556. doi: 10.1038/s41591-022-01698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Chau J., Yadav M., Liu B., Furqan M., Dai Q., Shahi S., Gupta A., Nace Mercer K., Eastman E., Abu Hejleh T., et al. Prospective Correlation between the Patient Microbiome with Response to and Development of Immune-Mediated Adverse Effects to Immunotherapy in Lung Cancer. J. Clin. Oncol. 2021;39:e21024. doi: 10.1200/JCO.2021.39.15_suppl.e21024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Liu T., Xiong Q., Li L., Hu Y. Intestinal Microbiota Predicts Lung Cancer Patients at Risk of Immune-Related Diarrhea. Immunotherapy. 2019;11:385–396. doi: 10.2217/imt-2018-0144. [DOI] [PubMed] [Google Scholar]
- 195.Liu W., Ma F., Sun B., Liu Y., Tang H., Luo J., Chen H., Luo Z. Intestinal Microbiome Associated with Immune-Related Adverse Events for Patients Treated with Anti-PD-1 Inhibitors, a Real-World Study. Front. Immunol. 2021;12:756872. doi: 10.3389/fimmu.2021.756872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Tan B., Liu Y., Tang H., Chen D., Xu Y., Chen M., Li Y., Wang M., Qian J. Gut Microbiota Shed New Light on the Management of Immune-Related Adverse Events. Thorac. Cancer. 2022;13:2681–2691. doi: 10.1111/1759-7714.14626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Usyk M., Pandey A., Hayes R.B., Moran U., Pavlick A., Osman I., Weber J.S., Ahn J. Bacteroides Vulgatus and Bacteroides Dorei Predict Immune-Related Adverse Events in Immune Checkpoint Blockade Treatment of Metastatic Melanoma. Genome Med. 2021;13:160. doi: 10.1186/s13073-021-00974-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Vétizou M., Pitt J.M., Daillère R., Lepage P., Waldschmitt N., Flament C., Rusakiewicz S., Routy B., Roberti M.P., Duong C.P.M., et al. Anticancer Immunotherapy by CTLA-4 Blockade Relies on the Gut Microbiota. Science. 2015;350:1079–1084. doi: 10.1126/science.aad1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gil-Cruz C., Perez-Shibayama C., De Martin A., Ronchi F., van der Borght K., Niederer R., Onder L., Lütge M., Novkovic M., Nindl V., et al. Microbiota-Derived Peptide Mimics Drive Lethal Inflammatory Cardiomyopathy. Science. 2019;366:881–886. doi: 10.1126/science.aav3487. [DOI] [PubMed] [Google Scholar]
- 200.Wang F., Yin Q., Chen L., Davis M.M. Bifidobacterium Can Mitigate Intestinal Immunopathology in the Context of CTLA-4 Blockade. Proc. Natl. Acad. Sci. USA. 2018;115:157–161. doi: 10.1073/pnas.1712901115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Sun S., Luo L., Liang W., Yin Q., Guo J., Rush A.M., Lv Z., Liang Q., Fischbach M.A., Sonnenburg J.L., et al. Bifidobacterium Alters the Gut Microbiota and Modulates the Functional Metabolism of T Regulatory Cells in the Context of Immune Checkpoint Blockade. Proc. Natl. Acad. Sci. USA. 2020;117:27509–27515. doi: 10.1073/pnas.1921223117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hakozaki T., Richard C., Elkrief A., Hosomi Y., Benlaïfaoui M., Mimpen I., Terrisse S., Derosa L., Zitvogel L., Routy B., et al. The Gut Microbiome Associates with Immune Checkpoint Inhibition Outcomes in Patients with Advanced Non-Small Cell Lung Cancer. Cancer Immunol. Res. 2020;8:1243–1250. doi: 10.1158/2326-6066.CIR-20-0196. [DOI] [PubMed] [Google Scholar]
- 203.Wang L., Tang L., Feng Y., Zhao S., Han M., Zhang C., Yuan G., Zhu J., Cao S., Wu Q., et al. A Purified Membrane Protein from Akkermansia Muciniphila or the Pasteurised Bacterium Blunts Colitis Associated Tumourigenesis by Modulation of CD8+ T Cells in Mice. Gut. 2020;69:1988–1997. doi: 10.1136/gutjnl-2019-320105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hu Z.I., Link V.M., Lima-Junior D.S., Delaleu J., Bouladoux N., Han S.-J., Collins N., Belkaid Y. Immune Checkpoint Inhibitors Unleash Pathogenic Immune Responses against the Microbiota. Proc. Natl. Acad. Sci. USA. 2022;119:e2200348119. doi: 10.1073/pnas.2200348119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Pham F., Moinard-Butot F., Coutzac C., Chaput N. Cancer and Immunotherapy: A Role for Microbiota Composition. Eur. J. Cancer. 2021;155:145–154. doi: 10.1016/j.ejca.2021.06.051. [DOI] [PubMed] [Google Scholar]
- 206.Wang Q., McLoughlin R.M., Cobb B.A., Charrel-Dennis M., Zaleski K.J., Golenbock D., Tzianabos A.O., Kasper D.L. A Bacterial Carbohydrate Links Innate and Adaptive Responses through Toll-like Receptor 2. J. Exp. Med. 2006;203:2853–2863. doi: 10.1084/jem.20062008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Park R., Umar S., Kasi A. Immunotherapy in Colorectal Cancer: Potential of Fecal Transplant and Microbiota-Augmented Clinical Trials. Curr. Colorectal Cancer Rep. 2020;16:81–88. doi: 10.1007/s11888-020-00456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Zhang Y., Zhang X., Li W., Du Y., Hu W., Zhao J. Biomarkers and Risk Factors for the Early Prediction of Immune-Related Adverse Events: A Review. Hum. Vaccines Immunother. 2022;18:2018894. doi: 10.1080/21645515.2021.2018894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Luo B., Zhang Y., Zhang C., Liu X., Shi C. Intestinal Microbiota: A Potential Target for Enhancing the Antitumor Efficacy and Reducing the Toxicity of Immune Checkpoint Inhibitors. Cancer Lett. 2021;509:53–62. doi: 10.1016/j.canlet.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 210.Dai Z., Fu J., Peng X., Tang D., Song J. Intestinal Microbiota: The Driving Force behind Advances in Cancer Immunotherapy. Cancers. 2022;14:4796. doi: 10.3390/cancers14194796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Holmstroem R.B., Nielsen O.H., Jacobsen S., Riis L.B., Theile S., Bjerrum J.T., Vilmann P., Johansen J.S., Boisen M.K., Eefsen R.H.L., et al. COLAR: Open-Label Clinical Study of IL-6 Blockade with Tocilizumab for the Treatment of Immune Checkpoint Inhibitor-Induced Colitis and Arthritis. J. Immunother. Cancer. 2022;10:e005111. doi: 10.1136/jitc-2022-005111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zamora A.E., Crawford J.C., Thomas P.G. Hitting the Target: How T Cells Detect and Eliminate Tumors. J. Immunol. 2018;200:392–399. doi: 10.4049/jimmunol.1701413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Bethune M.T., Joglekar A.V. Personalized T Cell-Mediated Cancer Immunotherapy: Progress and Challenges. Curr. Opin. Biotechnol. 2017;48:142–152. doi: 10.1016/j.copbio.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 214.Berner F., Bomze D., Lichtensteiger C., Walter V., Niederer R., Ali O.H., Wyss N., Bauer J., Freudenmann L.K., Marcu A., et al. Autoreactive Napsin A-Specific T Cells Are Enriched in Lung Tumors and Inflammatory Lung Lesions during Immune Checkpoint Blockade. Sci. Immunol. 2022;7:eabn9644. doi: 10.1126/sciimmunol.abn9644. [DOI] [PubMed] [Google Scholar]
- 215.Tahir S.A., Gao J., Miura Y., Blando J., Tidwell R.S.S., Zhao H., Subudhi S.K., Tawbi H., Keung E., Wargo J., et al. Autoimmune Antibodies Correlate with Immune Checkpoint Therapy-Induced Toxicities. Proc. Natl. Acad. Sci. USA. 2019;116:22246–22251. doi: 10.1073/pnas.1908079116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Gowen M.F., Giles K.M., Simpson D., Tchack J., Zhou H., Moran U., Dawood Z., Pavlick A.C., Hu S., Wilson M.A., et al. Baseline Antibody Profiles Predict Toxicity in Melanoma Patients Treated with Immune Checkpoint Inhibitors. J. Transl. Med. 2018;16:82. doi: 10.1186/s12967-018-1452-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Johannet P., Liu W., Fenyo D., Wind-Rotolo M., Krogsgaard M., Mehnert J.M., Weber J.S., Zhong J., Osman I. Baseline Serum Autoantibody Signatures Predict Recurrence and Toxicity in Melanoma Patients Receiving Adjuvant Immune Checkpoint Blockade. Clin. Cancer Res. 2022;28:4121–4130. doi: 10.1158/1078-0432.CCR-22-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Colen R.R., Fujii T., Bilen M.A., Kotrotsou A., Abrol S., Hess K.R., Hajjar J., Suarez-Almazor M.E., Alshawa A., Hong D.S., et al. Radiomics to Predict Immunotherapy-Induced Pneumonitis: Proof of Concept. Investig. New Drugs. 2018;36:601–607. doi: 10.1007/s10637-017-0524-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Jing Y., Yang J., Johnson D.B., Moslehi J.J., Han L. Harnessing Big Data to Characterize Immune-Related Adverse Events. Nat. Rev. Clin. Oncol. 2022;19:269–280. doi: 10.1038/s41571-021-00597-8. [DOI] [PubMed] [Google Scholar]
- 220.Ramos-Casals M., Brahmer J.R., Callahan M.K., Flores-Chávez A., Keegan N., Khamashta M.A., Lambotte O., Mariette X., Prat A., Suárez-Almazor M.E. Immune-Related Adverse Events of Checkpoint Inhibitors. Nat. Rev. Dis. Primer. 2020;6:38. doi: 10.1038/s41572-020-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Puzanov I., Diab A., Abdallah K., Bingham C.O., 3rd, Brogdon C., Dadu R., Hamad L., Kim S., Lacouture M.E., LeBoeuf N.R., et al. Managing Toxicities Associated with Immune Checkpoint Inhibitors: Consensus Recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J. Immunother. Cancer. 2017;5:95. doi: 10.1186/s40425-017-0300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Brahmer J.R., Abu-Sbeih H., Ascierto P.A., Brufsky J., Cappelli L.C., Cortazar F.B., Gerber D.E., Hamad L., Hansen E., Johnson D.B., et al. Society for Immunotherapy of Cancer (SITC) Clinical Practice Guideline on Immune Checkpoint Inhibitor-Related Adverse Events. J. Immunother. Cancer. 2021;9:e002435. doi: 10.1136/jitc-2021-002435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Morad G., Helmink B.A., Sharma P., Wargo J.A. Hallmarks of Response, Resistance, and Toxicity to Immune Checkpoint Blockade. Cell. 2021;184:5309–5337. doi: 10.1016/j.cell.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zhou J.-G., Wong A.H.-H., Wang H., Tan F., Chen X., Jin S.-H., He S.-S., Shen G., Wang Y.-J., Frey B., et al. Elucidation of the Application of Blood Test Biomarkers to Predict Immune-Related Adverse Events in Atezolizumab-Treated NSCLC Patients Using Machine Learning Methods. Front. Immunol. 2022;13:862752. doi: 10.3389/fimmu.2022.862752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Iivanainen S., Ekstrom J., Virtanen H., Kataja V.V., Koivunen J.P. Electronic Patient-Reported Outcomes and Machine Learning in Predicting Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapies. BMC Med. Inform. Decis. Mak. 2021;21:205. doi: 10.1186/s12911-021-01564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Grant M.J., Booth A. A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies: A Typology of Reviews. Maria J. Grant Andrew Booth. Health Inf. Libr. J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 227.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.