Abstract
Motivated behaviours are thought to lead to enhanced performances. In the neurorehabilitation field, motivation has been demonstrated to be a link between cognition and motor performance, therefore playing an important role upon rehabilitation outcome determining factors. While motivation-enhancing interventions have been frequently investigated, a common and reliable motivation assessment strategy has not been established yet. This review aims to systematically explore and provide a comparison among the existing motivation assessment tools concerning stroke rehabilitation. For this purpose, a literature search (PubMed and Google Scholar) was performed, using the following Medical Subject Headings terms: “assessment” OR “scale” AND “motivation” AND “stroke” AND “rehabilitation”. In all, 31 randomized clinical trials and 15 clinical trials were examined. The existing assessment tools can be grouped into two categories: the first mirroring the trade-off between patients and rehabilitation, the latter reflecting the link between patients and interventions. Furthermore, we presented assessment tools which reflect participation level or apathy, as an indirect index of motivation. In conclusion, we are left to put forth a possible common motivation assessment strategy, which might provide valuable incentive to investigate in future research.
Keywords: motivation, participation, apathy, stroke, neurorehabilitation, performance
1. Introduction
Although the concept of motivation may intuitively seem clear and simple, it poses some hidden pitfalls. What do we mean when we say that a certain treatment “motivates” patients? Is motivation a measurable parameter? Can we turn to motivation as it was a clinical parameter? Despite intense research about this topic, these questions remain probably open. In fact, motivation is a complex, multifaceted psychological construct, resulting from the interplay of several factors. Up to now, indirect measurements, which may provide a quantification of motivation, are available.
Motivation has been didactically defined as an orientation for which humans and other animals activate and sustain behaviour toward a goal [1]. This definition can be applied to several daily life scenarios. Motivation and its related aspects have been the subject of numerous research studies and several competing theories, concerning the content of motivated behaviours, have been regularly proposed. Among incentive theories, a distinction between extrinsic and intrinsic motivation occurs frequently [2]. While intrinsic motivation is related to the joy or to the interest by doing a certain activity, extrinsic motivation occurs when the goal of an activity is an external reward, which is separated from the activity itself. Research on motivation has been employed in multiple areas, including applications in business [3,4,5], educational [6,7], and wellness fields [8]. A specific branch of medical research focused on determining factors which improve recovery from diseases. In this context, motivation is of particular interest to neurologists, neuropsychologists, and experts in neurorehabilitation since it is closely related to therapy outcome. Not surprisingly, highly motivated patients are prone to reach a better recovery than low motivated patients [9]. In the field of clinical research, a common measurement strategy of motivation represents an unmet need.
This review aims at first to illustrate an overview of the most important general motivation theories and, second, to place them with regard to the stroke rehabilitation literature. Moreover, we investigated and compared motivation assessments, which have been used in the last years in interventional studies on stroke patients in the rehabilitative setting. Finally, at the light of the literature, we discussed how to assess motivation, which might be helpful in further clinical research.
1.1. Theories on Motivation: An Overview
An academic, valid distinction between process and content theories about motivation has been established: while process theories try to explain how and why motivation influences behaviours, content theories attempt to define needs that motivate peoples’ actions. Among process theories, self-determination theory (SDT), social-cognitive theory (SCT), and goal orientation theory (GOT) have been deeply investigated. All the above-mentioned theories have been developed in different fields, in particular in the learning-field. Some of these (especially the SDT, but also GOT and SCT) have been further extended to re-learning processes, applying them in the neurorehabilitation setting. SDT represents a macro theory of human motivation [3]. The concept of SD refers to the person’s faculty to make choices, having a great impact on motivation. In fact, people feel more motivated to act (“to make something”) if they observe an effect on the outcome of their own action. According to Deci and Ryan [10], people tend to be driven in their actions by a need to grow and gain fulfilment. In the cognitive evaluation theory, a sub-theory of SDT, a subject becomes self-determined when needs for competence, connection, and autonomy are satisfied. While autonomy refers to the human need to feel in control of behaviours, competence means feeling confident with different task-related skills. Consequently, a person who is confident to reach a goal is also more prone to take actions. Connection is linked to the concept of relatedness. In this sense, a person needs to feel a sense of belonging to the community. In the SDT, three main motivation domains were identified: amotivation (lack of motivation), extrinsic motivation, and intrinsic motivation. While in the intrinsic motivation an action is the result of an intrinsic will regulation, i.e., a person makes something only for the enjoyment of the action, amotivation results in inaction or action without real will. Inside extrinsic motivation many different levels of regulation are related to different types of external value and to action’s consequences (punishments/rewards).
In the SCT, motivation is the result of a cognitive process which is influenced by personal, behavioural, and environmental factors. An essential role in this theory is played by the subject’s faculty to change and manipulate the environment to reach personal goals. This faculty is strongly influenced by the subject’s beliefs about their own capabilities. The most important belief in the SCT is the (perceived) self-efficacy, defined by Albert Bandura as “people’s judgment of their capabilities to organize and execute courses of action required to attain designated types of performances. It is concerned (…) with judgments of what one can do with whatever skills one possesses” [11].
The term goal orientation (GO) refers to the cognition of the achievement and its implications on the behaviour responses [12]. GO influences the individual’s cognitive or emotional tendency toward events, which in turn will trigger behavioural responses. Within GO theories, orientation to achieve goals differs individually and it is related to a subconscious subject’s predisposition. While some subjects show motivated behaviours in task completing exclusively to align themselves with the community’s expectancy (performance goal orientation), a mastery goals orientation leads to motivated behaviours, principally through intrinsic values of related actions. The most important difference with performance goal orientation consists in the conviction that the required ability for task completing can improve through skills training. A summary of these theories is reported in Table 1. In the next paragraph, it will be presented how the most prominent aspects of these theories have been applied in the field of neurorehabilitation.
Table 1.
Summary of contemporary motivation theories.
| SDT | SCT | GOT | |
|---|---|---|---|
| Main Concept | People are driven in their actions by a need to grow and gain fulfilment. SDT is focused on the role played by both intrinsic and extrinsic motivation. While intrinsic motivation is related to the interest by doing a certain activity, extrinsic motivation occurs when the goal of an activity is an external reward. Intrinsic and internalized motivations are promoted by feelings of competence, autonomy, and relatedness. |
Motivation is the result of a cognitive process which is influenced by personal, behavioural, and environmental factors. The subject’s judgment of their own capabilities to reach a specified level in the performance (Self-efficacy) is the main driver of motivated action. |
The term goal orientation (GO) refers to the cognition of the achievement on the behaviour responses. Achievement goals are defined as the terminal point towards which one’s efforts are directed. Two different GOs have been described: In the performance GO (PGO), the subjects show motivated behaviours only to align him/herself with the community’s expectancy. In the mastery GO (MGO), motivated behaviours are characterized by intrinsic values of related actions. In the MGO, the required ability for task completing is supposed to improve through skills training. In PGO, the required task’s ability is a congenital fixed trait (entity mindset): in this case, the real motivation in task’s completing consists in showing to the community that the one is enough able to |
| Keywords | Competence, autonomy, relatedness | Self-efficacy | Mastery goal orientation, performance goal orientation |
| Main references |
Deci and Ryan [2,3,13,14] | Bandura [11,15] | Locke and Latham [12,16]; Dweck [17] |
Abbreviations: SDT: self-determination theory; SCT: social-cognitive theory; GOT: goal orientation theory; MGO: mastery goal orientation; PGO: performance goal orientation.
1.2. Motivation in Neurorehabilitation
Several descriptive studies and reviews describe stroke as a sudden interruption of what was otherwise expected to be a normal life [18,19]. According to the WHO definition [20], rehabilitation in patients with disabilities should be considered as the “process aimed to reach and maintain optimal physical, sensory, intellectual, psychological and social functional levels”. With reference to the rehabilitative setting, motivation may be defined as the reason why patients activate sustained efforts toward the recovery. However, a gap exists in the rehabilitation literature about the nature of motivation. Maclean and Pound [9] divided the global literature about this topic into three broad groups: the first group (the prevalent one) describes motivation as a purely internal quality of the patient; the second group indicates motivation mainly as a social driven factor; and the last group sees motivation as a combination of social factors and individual clinical characteristics, such as personality. A first pitfall about the psychological conceptualization of motivation in rehabilitation could be the differentiation between internal and external motivation. From a mere cognitive point of view, the achievement of a motor functional improvement could be seen as an external reward factor motivating the patient, but from a behavioural point of view, it is an intrinsic factor because it is internal to the patient/person. This aspect has been deeply treated in some studies focused on patients with stroke, for whom motor and cognitive deficits are strictly intertwined.
Focus on Motivation in Stroke
Most of the studies regarding motivation in neurorehabilitation are focused on stroke. Among these studies, many researchers turn to motivation as a process of the SDT [21]. Focusing on the role played by both intrinsic and extrinsic motivation, SDT longs to provide a comprehensive explanation of internal and external influences on human behaviours. In particular, as proposed by Yoshida et al. [22], motivation in subacute stroke patients is mainly influenced by extrinsic reward factors (e.g., positive feedback provided by therapists, praises by medical staff or relatives, etc.). Then, if the self-regulation is, also partially, reached through the satisfaction of basic psychological needs (autonomy, competence, and relatedness), one’s motivation moves from an extrinsic level to an intrinsic one [23]. Therefore, in case of a valid functional improvement, the patient may attend the rehabilitation almost exclusively supported by intrinsic motivation. In addition, the importance of internalization of regulations in fostering rehabilitation and physical activity has been demonstrated, indicating that an enhanced competence for exercise is a positive predictive of more adaptive exercise behavioural outcomes [24]. Moreover, the process of internalization of behavioural regulations has been shown to be the basis for long-term improvement after conclusion of treatment [25]. According to SDT, motivation, especially in stroke rehabilitation, is a dynamic phenomenon. If the purpose of tailoring interventions to extrinsic factors is essential in maintaining patients’ motivation (at least in the subacute phase) [22], clinicians should promote anyways the process of internalization. In this context, sharing an appropriate amount of information about rehabilitation and avoiding “mixed messages” [26] are useful strategies. However, it should be finally noted that both intrinsic and extrinsic motivation are important in fostering actions: the relationship between the two motivation types is not conflictual but addictive, as suggested by Cerasoli et al. [27].
According to the original works of Locke and Latham [12,16], a recent, comprehensive review [28] on GOT identified a triad of different goal types with regard to neurorehabilitation. These are represented by performance goals (where patients use previously learned strategies to perform tasks), process-oriented or learning goals (where required skills for improving performance have to be learned), and outcome goals (which are related to the performance of competitors; this type of goal has not been investigated so far, but a deep research study about this topic is in progress, e.g., [29,30]). The goal setting should represent a milestone of the neurorehabilitation setting [31], although no single guideline has been established [32]. In fact, a recent review [33] identified at least 12 different approaches to goal setting. Among these, two common features have been identified: having measurable goals and patients’ involvement in goal setting. Within the GOT literature, a ‘patient-centered’ approach to establish goals for rehabilitation is universally accepted. Although evidence to support its efficacy is weak [34], a patient-centered approach is supposed to improve self-perceived participation, performance itself, and functional outcomes [35,36] in stroke patients. Furthermore, GO instructions may result in significant increases in the rate of repetitions of exercise in stroke rehabilitation [37].
With regard to SCT principles, personal and environmental factors reciprocally interact influencing motivated behaviour: in this sense, the individual exerts an influence on the environment, which, in turn, influences him/her. A high level of self-efficacy is directly related to the quality of life in stroke patients [38] and to the amount of daily physical activity [39]. Stewart et al. [40] found self-efficacy to be a significant predictor of the performance of the affected arm in chronic stroke patients with mild motor impairment. The authors concluded that self-efficacy may serve as a target for interventions to improve proximal arm control after stroke. Another study [41] demonstrated that self-efficacy for walking, and in general, to perform physical exercise, predicts higher exercise adherences in individuals with chronic stroke.
2. Materials and Methods
A systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A literature search (PubMed and Google Scholar) was performed on 22 August 2022, and we selected articles published in the timeframe 1 January 2010 to 30 Juny 2022, using the following Medical Subject Headings (MeSH) terms: “Assessment” OR “Scale” AND “motivation” AND “stroke” AND “rehabilitation”. In addition, a backward search (checking the bibliography of identified papers) was conducted to identify any studies that were not retrieved using the main search strategy. The inclusion criteria were (1) articles published in English language; (2) interventional studies in stroke patients in rehabilitation setting, which examine the direct effect of the intervention on motivation, measured by specifically designed assessment tools; (3) original research examining the indirect effect of an intervention on motivation (in this case, the motivating effect of the intervention is measured by indirect motivation assessment tools, such those specifically designed to assess participation or depression); and (4) studies conducted in the above-reported period. In the main search strategy, the following exclusion criteria were adopted: (1) article types such as letters to the editor, case reports, reviews, and meta-analyses; (2) studies for which the complete text could not be found; and (3) articles not in English.
Two authors independently performed all searches and removed duplicate records. Finally, a third author performed a quality assessment.
2.1. Quality Assessment
To assess the quality of our review, we have used a qualitative approach. This approach is reasonable because we are investigating phenomena (motivation assessment), in which the assessment’s choice in the examined studies was arbitrary. Thus, we used the qualitative methodological checklist of the National Institute of Clinical Nursing (NICE) [42]. According to the NICE checklist, ++ means that all or most of the checklist criteria have been fulfilled, + means that some of the checklist criteria have been fulfilled, and—means that few or no checklist criteria have been fulfilled.
2.2. Data Extraction
The data extraction form developed for this study aimed to carry out study characteristics (title, first author, study design, geographical location, study setting, and aim of the study with description of the adopted motivation assessment tool, including frequency of assessment). Two authors, who conducted the study selection independently, performed the data extraction. If necessary, any disagreements were discussed with a third review author.
2.3. Ethics Statement
This study is a systematic review and does not deal with human participants.
3. Results
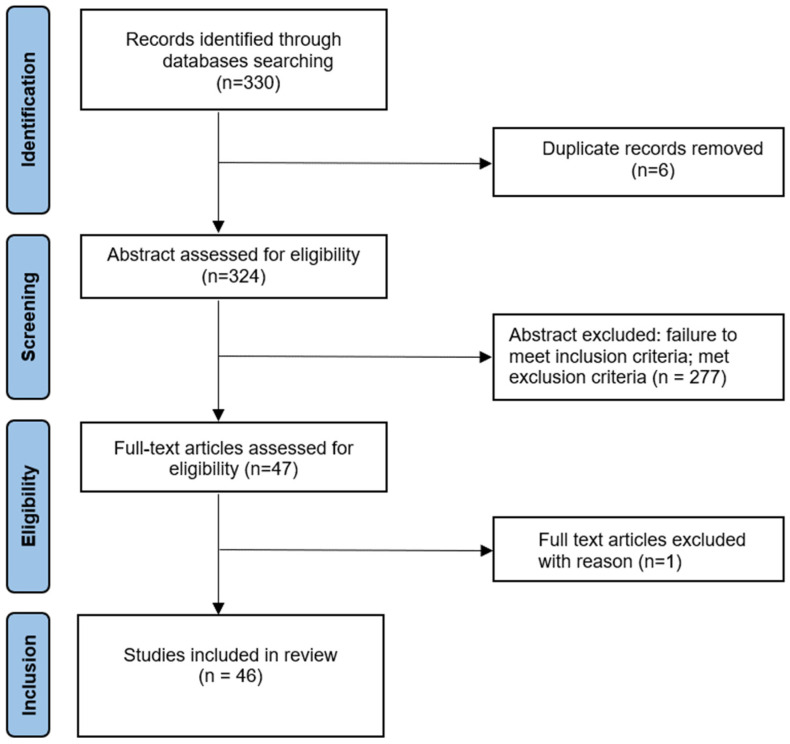
Electronic and additional sources identified 330 references. Duplicate articles were removed, leaving a total of 324 articles. A total of 278 of these were excluded after assessing their abstract, as they did not meet the inclusion criteria. Another study [43] was removed after reading, because, although it has met inclusion criteria, the trial was not completed at the time of writing this article. Thus, a total of 46 articles [44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89] published between 2011 and 2022 were assessed for eligibility after reading the full text (Figure 1) and underwent the quality control.
Figure 1.
Flow diagram of study inclusion.
The 46 selected studies were published between 2010 and 2022. The review includes 31 RCTs and 15 CTs. Of the 46 studies, 25 were carried out in Europe, 12 in Asia, 8 in America (7 in the USA and 1 in Brazil), and 1 in Australia (Table 2).
Table 2.
Motivation-assessing interventional studies in stroke patients in rehabilitation setting.
| First Author | Year | Study Design | Study Location | Stroke Setting | Aim of the Study | Motivation Assessment Tool | Assessment Frequency |
|---|---|---|---|---|---|---|---|
| Bergmann J [44] | 2018 | RCT | Germany | SA | To evaluate the acceptability of robot-assisted gait training with and without virtual reality | IMI | After the 1st, 6th, and 12th week and after the crossover therapy session |
| Winter C [45] | 2021 | RCT | Germany | C | To evaluate the acceptability of robot-assisted gait training in each of three different experimental conditions (VR via HMD, VR via monitor, and treadmill training without VR) | IMI | After every condition |
| Guillén-Climent S [46] | 2021 | CT | Spain | DS | To assess the usability of a robotic device combined with a telecare platform, in which the training is based on serious games for upper limb rehabilitation in the home environment | IMI | On the last day of treatment |
| Navarro MD [47] | 2020 | RCT | Spain | C | To investigate the effectiveness and motivation of a group-based intervention, combining conventional and computerized multi-touch exercises, when administered in either a competitive or non-competitive manner | IMI | Before and after each intervention |
| Swinnen E [48] | 2017 | CT | Belgium | C | To examine stroke patients’ motivation and expectations of robot-assisted gait training (RAGT), and therapists’ perspectives on the usability of RAGT | IMI | Once |
| Prange GB [49] | 2015 | RCT | Netherlands | SA | To examine the effect of weight-supported arm training combined with computerized exercises on arm function and capacity, compared with dose-matched conventional reach training | IMI | Once (post-training) |
| Johar MN [50] | 2022 | RCT | Malaysia | C | To assess the effectiveness of game-based circuit exercise in comparison to conventional circuit exercise on functional outcome (lower limb strength, postural stability, and aerobic endurance), motivation level, self-efficacy, and quality of life. | IMI | Baseline, after 12 and 24 weeks |
| Hung NT [51] | 2021 | CT | USA (Illinois) | C | To assess tolerability and feasibility of home-based, high-dose “myoelectric interface for neurorehabilitation training” therapy | IMI | At the end of the 6th training week |
| Thielbar KO [52] | 2020 | RCT | USA (Illinois) | C | To compare participation and subjective experience of participants in both home-based multiuser virtual reality (VR) therapy and home-based single-user (SU) VR therapy | IMI | 2 and 4 weeks after beginning of the intervention |
| Nijenhuis SM [53] | 2015 | CT | Netherlands, United Kingdom, Italy | C | To assess the feasibility and potential clinical changes associated with a technology-supported arm and hand training system at home for patients with chronic stroke | IMI | After intervention |
| Nijenhuis SM [54] | 2017 | RCT | Netherlands | C | To compare user acceptance and arm and hand function changes after technology-supported training at home with conventional exercises | IMI | After intervention |
| Subramanim S [55] | 2014 | CT | USA (Illinois) | C | To assess adherence and intervention-related effects of gaming to improve balance control and decrease cognitive-motor interference | IMI | Pre- and post- intervention |
| Friedman N [56] | 2014 | RCT | USA (California) | C | To compare the effect of training with a specific robotic glove to conventional hand therapy | IMI | After each session |
| Lloréns R [57] | 2015 | RCT | Spain | C | To evaluate the clinical effectiveness of a virtual reality (VR)-based telerehabilitation program. | IMI | After treatment |
| Knippenberg E [58] | 2021 | CT | Belgium | SA + C | To evaluate the usability, credibility, and treatment expectancy of i-ACT (intelligent activity-based client-centred task-oriented training) and the motivation towards i-ACT use in rehabilitation over time | IMI | At baseline or after one training session with i-ACT, after 2 weeks, 4 weeks, and 6 weeks of training, and 9 weeks after the cessation of training |
| Popović MD [59] | 2014 | RCT | Serbia | SA | To investigate whether feedback-mediated exercise (FME) of the affected arm of hemiplegic patients increases patient motivation and promotes greater improvement of motor function, compared to no-feedback exercise | IMI | Baseline and after three weeks of treatment |
| Novak D [60] | 2014 | RCT | Switzerland | C | To explore the potential of two-player game, played using two robotic devices designed for arm rehabilitation. Three game modes were tested: single-player (competing against computer), competitive (competing against human), and cooperative (cooperating with human against computer) | IMI | After each game mode |
| Chen L [61] | 2019 | RCT | China | DS | To compare the efficacy of motor relearning program versus Bobath approach | AES | After 1, 3, 6, 9, and 12 months |
| Radder B [62] | 2018 | CT | The Netherlands | C | To investigate the feasibility of a wearable, soft-robotic glove system developed to combine assistive support in daily life with performing therapeutic exercises on a computer at home | IMI | Once (at end of Phase 2) |
| Ahmad MA [63] | 2019 | RCT | Malaysia | C | To examine the effectiveness of VR games as an adjunct to standard physiotherapy in improving upper limb (UL) function and general health. | IMI | Before and after 8 interventional weeks |
| Rapolienė J [64] | 2018 | RCT | Lithuania | A | To evaluate the effectiveness of occupational therapy on motivation. | MHLC | Before first occupational treatment and after 20 occupational therapy procedures |
| Lin FH [65] | 2019 | RCT | Taiwan | C | To investigate the effects of routine rehabilitation activities and additional social support and health education by functional therapists on motivation and post-stroke depression | CES-D10 | At the 2nd week, 4th week, 8th week, and 4 weeks after the end of the study |
| Hung JW [66] | 2016 | CT | USA (Illinois) | C | To investigate the feasibility and potential efficacy of the video-controlled biofeedback system for balance training | IMI | At the end of the 6-week training |
| LaPiana N [67] | 2020 | CT | USA Washington | A | To assess the acceptability of a smartphone-based augmented reality game | Ad hoc developed questionnaire | At the end of the final gaming session |
| Huber SK [68] | 2021 | CT | Switzerland | C | To investigate the feasibility of a rehabilitation approach using user-centered exergames | BREQ-3 and the SMSC | At baseline and after 8 weeks |
| Graven C [69] | 2011 | RCT | Australia | DS | To assess the efficacy of an integrated approach (including written provision at discharge, additional phone contacts, and home visits) to facilitate patient goal achievement in the first year post-stroke | GDS-15 | At baseline and six and twelve months post-stroke |
| Morice E [70] | 2020 | RCT | Switzerland | SA | To assess the effects of dance program on patients’ balance control, cognitive function, strength, coordination, functional status, balance confidence, quality of life, and motivation | MAPS | Before and after eight weeks of intervention |
| An HJ [71] | 2021 | RCT | Republic of Korea | C | To investigate the effect of animal-assisted therapy on gait performance, pulmonary function, and psychological variables | SRMS | Before and after eight weeks of intervention |
| Adhikari SP [72] | 2018 | RCT | Nepal | SA | To examine the immediate effect of “action-observation-execution” with accelerated skill acquisition program (ASAP) on dexterity | SRMS | At baseline, after training, and during one-week follow-up |
| Thompson N [73] | 2022 | CT | United Kingdom | SA | To assess the feasibility and acceptability of delivering neurologic music therapy one day-per-week | Ad hoc developed questionnaire | Before and after each single session |
| Street AJ [74] | 2018 | RCT | United Kingdom | SA + C | To evaluate music therapy as a home-based intervention for arm hemiparesis | Ad hoc developed questionnaire | After 1, 6, 9, and 15 weeks |
| Morone G [75] | 2015 | CT | Italy | DS | To evaluate the feasibility of brain–computer interface-assisted motor imagery training to support hand/arm motor rehabilitation | QCM | At the end of each training session |
| Deguchi K [76] | 2013 | RCT | Japan | DS | To assess the usefulness of a novel computerized touch panel-type screening test | AES -VI | Unknown |
| Seregni A [77] | 2021 | CT | Italy, Spain | C | To assess the efficacy of a novel virtual coach system in assisting and counselling patients during home rehabilitation activities | Ad hoc developed questionnaire | Unknown |
| Chen HM [78] | 2020 | CT | Taiwan | A + SA | To determine whether motivational interviewing (MI) improves the performance of activities of daily living and enhances motivation for rehabilitation among first-stroke patients | RMS | Baseline, 6 weeks, and three months after the intervention |
| Aramaki AL [79] | 2019 | CT | Brasil | SA + C | To analyse the feasibility of a rehabilitation protocol using client-centered VR and to evaluate changes in occupational performance and social participation | PS | Baseline and after treatment (12 weeks) |
| Wissink KS [80] | 2014 | CT | The Netherlands | C | To determine therapy intensity of and motivation for physical therapy of geriatric stroke patients in nursing homes, its correlates, and the effect on discharge destination | PRPS | During three interventional weeks |
| Chowdhury A [81] | 2015 | RCT | India | C | To assess the validity of a rehabilitation protocol, characterized by a combination of mental practice (MP) and physical practice (PP), using a hand exoskeleton and brain-computer interface (BCI) | VAS scale | After each session |
| Song HS [82] | 2019 | RCT | Republic of Korea | C | To determine the difference in self-satisfaction by comparing class-based task-oriented circuit training and individual-based task-oriented circuit training | MRS | Pre- and post-intervention |
| Park JS [83] | 2019 | RCT | Republic of Korea | SA | To investigate the effect of game-based exercise on hand strength, motor function, and compliance | VAS scale | After every training session |
| Alhirsan SM [84] | 2021 | RCT | USA (Alabama) | C | To demonstrate the different effects of augmented feedback, simple VR, and exergaming applications on motivation and walking speed performance | IMI | After each condition |
| Grau-Sánchez J [85] | 2021 | RCT | Spain | C | To assess the efficacy of enriched music-supported therapy on cognitive functions, emotional well-being, and quality of life | IMI + AES | IMI: during intervention; AES: baseline, pre-, and post-intervention |
| Zhang L [86] | 2022 | RCT | China | C | To explore whether coaching-based teleoccupational guidance will help stroke survivors and caregivers to obtain satisfactory outcomes | IMI | Baseline and after 3 and 6 months |
| Rozevink SG [87] | 2021 | RCT | The Netherlands | C | To investigate the effect of robotic device combined with a telecare platform on the upper limb function of patients with unilateral upper limb paresis | IMI | Once (post-treatment) |
| Skidmore ER. [88] | 2015 | RCT | USA (Pennsyl-vania) | A | To examine the effects of a behavioural intervention, used to augment usual inpatient rehabilitation, on apathy symptoms | AES | Baseline and after 3 and 6 months |
| Cano-Mañas MJ [89] | 2020 | RCT | Spain | SA | To determine the effect of a structured protocol using commercial video games on balance, postural control, functionality, quality of life, and level of motivation. | Ad hoc developed questionnaire | Pre- and post-treatment |
Abbreviations: Study design—CT: clinical trial; RCT: randomized clinical trial. Stroke setting—A: acute; SA: subacute; C: chronic; DS: different stages. Motivation assessment tool—IMI: Intrinsic Motivation Inventory; AES: Apathy Evaluation Scale; MHLC: Multidimensional Health Locus of Control scale; CES-D10: 10-item Center for the Epidemiological Studies of Depression Short Form; BREQ-3: Behavioural Regulation in Exercise Questionnaire; SMSC: Sport- and Movement-Specific Self-Concordance Scale; GDS-15: Geriatric Depression Scale—15 items; MAPS: echelle de Motivation envers l’Activité Physique en contexte de Santé; SRMS: Stroke Rehabilitation Motivation Scale; QCM: Questionnaire for Current Motivation; VI: Vitality Index; RMS: Rehabilitation Motivation Scale; PS: Participation Scale; MRS: Motivation of Rehabilitation Scale; VAS: Visual Analogic Scale; PRPS: Pittsburgh Rehabilitation Participation Scale.
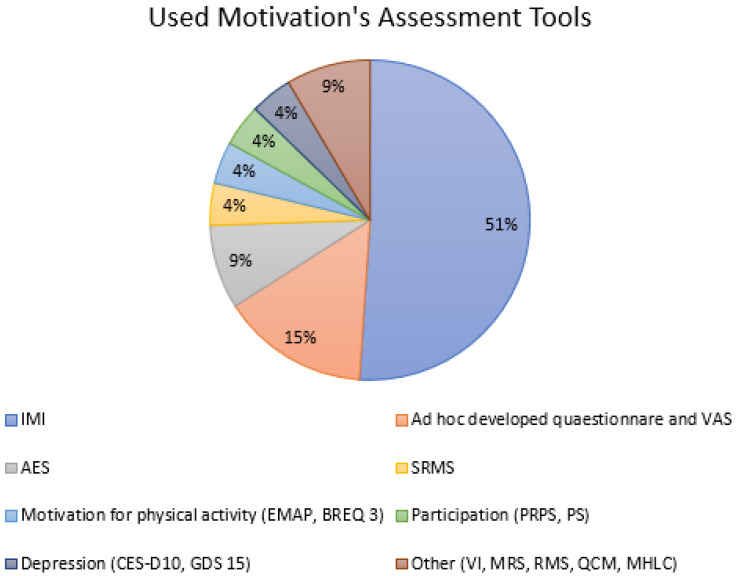
Most of the trials are dealing with robotic therapy, exergames, and virtual reality. In the remaining studies, different types of interventions such as feedback-mediated exercises; occupational therapy; specific physiotherapy approaches; integrated social and educational approach; music, dance, and pet therapy; and competitive rehabilitative strategies are included. Interestingly, we have not found any study regarding drugs, such as antidepressants or stimulants, and effect on motivation in this patient target. The setting in which the intervention was applied was in most cases the chronic phase of stroke (>6 months from stroke onset). The Intrinsic Motivation Inventory [90] represents the most-used motivation assessment tool in our review (see Figure 2). The frequency of motivation assessments appears to be extremely variable in the different studies. The quality control, performed according to the NICE guidelines, is reported in Appendix A (Table A1).
Figure 2.
Used motivation assessment tools. Abbreviations: IMI: Intrinsic Motivation Inventory; AES: Apathy Evaluation Scale; MHLC: Multidimensional Health Locus of Control scale; CES-D10: 10-item Center for the Epidemiological Studies of Depression Short Form; BREQ-3: Behavioural Regulation in Exercise Questionnaire; SMSC: Sport- and Movement-Specific Self-Concordance Scale; GDS-15: Geriatric Depression Scale—15 items; MAPS: echelle de Motivation envers l’Activité Physique en context de Santé; SRMS: Stroke Rehabilitation Motivation Scale; QCM: Questionnaire for Current Motivation; VI: Vitality Index; RMS: Rehabilitation Motivation Scale; PRPS: Pittsburgh Rehabilitation Participation Scale; PS: Participation Scale; MRS: Motivation of Rehabilitation Scale; VAS: Visual Analogic Scale.
4. Discussion
There are many ways to define motivation for rehabilitation. The reason for this is rather simple: the concept of motivation is in practice poorly understood and, as suggested by Maclean et al., also the adopted criteria among professionals to recognize motivation have been shown to have blurred boundaries [91]. In this context, one possible approach in motivation’s definition refers to the orientation for which patients activate sustained efforts toward the recovery [22]. Moreover, the idea of motivation might be also referred to the patient’s self-involvement within the rehabilitation context (rehabilitation-motivation). It should be noted that a motivation questionnaire which investigates how motivation is influenced by a treatment (e.g., the Intrinsic Motivation Inventory) does not quantify the global motivation for rehabilitation per se, but almost exclusively the subject’s predisposition/inclination to the specific treatment. In the different types of studies, it is often implied which meaning of motivation assessment (rehabilitation or intervention motivation) is intended, but such for a dichotomy has not previously been explicit in the literature we reviewed. Furthermore, in some studies of our review, motivation has been also indirectly quantified by depression or participation-related assessments [61,65,69,76,79,80,85,88].
4.1. Motivation Assessment Scales in Stroke-Rehabilitation
To our knowledge, three patient-rated scales, specifically designed for stroke patients in rehabilitation, are available: the Stroke Rehabilitation Motivation Scale (SRMS) [92], the Motivation for Rehabilitation scale (MORE scale) [93] and the Adapted Achievement Motivation Questionnaire (AAMQ) [94]. Another questionnaire to assess motivation in stroke survivors was developed by Hallams and Baker [95], but the questionnaire’s reliability could not be determined because of the small size of the examined sample. The MORE scale, recently developed by Yoshida et al. [93], is a promising motivation assessment tool in stroke patients. It consists of 17 items and explores both extrinsic and intrinsic motivation by referring to 2 types of factors (personal and social-relationship factors). The Cronbach’s alpha coefficient, evaluated for assessing internal consistency, was excellent (0.948). With regard to test–retest reliability, a moderate correlation was found between scores at the beginning and one month after hospitalization (rho = 0.612. p < 0.001). Furthermore, a strength of this tool is its relative independence from some confounding factors, e.g., depression or apathy. The SRMS [92], based on the SDT, has been adapted to be suitable among stroke patients from the Sports Motivation Scale [96], a motivation assessment tool used in sports. The SRMS consists of 28 items exploring 3 domains (amotivation, extrinsic motivation, and intrinsic motivation). A shorter 7-item SRMS version was proved to have good reliability among the rest of the 28 items. In the 28-item version, motivation is quantified through 7 subscales (extrinsic motivation (EM)-introjected; EM-regulation; EM-identification; amotivation; intrinsic motivation (IM)-knowledge; IM-stimulation; and IM-accomplishment). Each subscale includes more questions. A major limitation of the original version of the SRMS consists in the absence of a comparison with similar scales at the time of its validation, due to the fact that none existed yet. However, its validity has been indirectly proved in translation studies in other languages [97], whereby the K-SRMS includes only 24 items of the original SRMS. The first difference between the SRMS and the MORE consists in the item formulations, which are questions in the SRMS and statements in the MORE. Regardless of this psychometric difference, in some cases, the MORE and the SRMS share items or items have the same contents (MORE items: #5, #4, respectively, with SRMS items: #12, #8). In other cases, items of both scales are similar (MORE items: #6, #17, #9, respectively, with SRMS items: #24, #21 and #1, #18). The categories “goal setting”, “influence from supporters”, and “resilience against obstacles”, originally identified in the MORE scale, are well represented also in the SRMS. The category “success experience”, which is related to stroke patients’ functional improvement [98,99], is better represented in the MORE scale (items #11, #12, 13#) than in the SRMS. The intrinsic psychological effect of rehabilitation is conversely more investigated by the SRMS (items #5, #6, #15, #20). Finally, as mentioned above, the MORE seems to be not influenced by depressive symptoms, while the SRMS did not show predictive validity with mood-relevant measurements (such as anxiety, depression, and stress, as measured by Park et al. [97]). Finally, the AAMQ [94] consists of 28 items, shows an interesting internal consistency (Cronbach’s alpha coefficient: 0.946), and was regionally validated for examining the motivational level of Iranian stroke survivors. The content validity was approved by an expert panel. It was not possible to determine neither the criterion validity (there was no regionally standardized measure for comparison at the time of the pilot study) nor the construct validity (a factorial analysis could not be performed due to the small sample size). The main characteristics of the three above-reported scales are summarized in Table 3.
Table 3.
Specifically designed for stroke patients in rehabilitation motivation scales.
| AAMQ | MORE | 28-SRMS | |
|---|---|---|---|
| First Author | Derakh-shanrad SA [94] | Yoshida T [93] | White GN [92] |
| Year | 2016 | 2022 | 2012 |
| Questionnaire was developed from | The Persian version of Hermans Achievement Motivation Questionnaire (PHAMQ) | An item pool, created by nine rehabilitation professionals | Sports Motivation Scale (SMS) |
| Number of enrolled patients in the scale development | 25 | 201 | 18 |
| Number of items | 28 | 17 | 28 |
| Response format | 4-point scale | 7-point scale | 5-point scale |
| Internal consistency (Cronbach’s alpha coefficient) | 0.946 | 0.948 | 0.5 |
| Validity | Content validity was approved by an expert panel. Criterion validity could not be assessed because there was no regionally standardized comparison measure. A factorial analysis (construct validity) could not be performed due to the small sample size. | Construct validity was investigated using exploratory factor analysis, confirmatory factor analysis, and item response theory analysis. Criterion validity was investigated through Spearman’s rho, calculated between the MORE scale and the Apathy Scale (AS), Self-rating Depression Scale (SDS), and Visual Analogue Scale (VAS). | The scale’s validity could not be proved in the original version. |
| Notes (questionnaire dimensions, subscales, etc.) | Although a factorial analysis was not performed, the authors suggest the possibility of latent construct of the scale, which is based on the following factors: perseverance, self-esteem, time perception, seeking opportunities, diligence, competency, high ambition, and foresight. | The factor analysis suggests a one-factor structure (it was impossible to separate the motivation-related factors from the relevant item). | 7 factors have been identified: EM-introjected; EM-regulation; EM-identification; amotivation; IM-knowledge; IM-stimulation; IM-accomplishment. |
Abbreviations: AAMQ: Adapted Achievement Motivation Questionnaire; SRMS: Stroke Rehabilitation Motivation Scale; MORE: Motivation for Rehabilitation scale; EM: extrinsic motivation; IM: intrinsic motivation.
In the stroke rehabilitation literature, many other motivation assessment tools have been used. In addition, several interventional studies provided a motivation assessment, which is primarily based on self-report scales and questionnaires. In our review, the Intrinsic Motivation Inventory (IMI) [90] is the most used motivation assessment tool. The IMI aims to measure the levels of intrinsic motivation as the outcome of a set of subscales (interest/enjoyment, perceived competence, effort, value/usefulness, pressure/tension, relatedness, and perceived choice) and shows, in the original version, a good internal consistency with a Cronbach’s alpha coefficient of 0.85 [90]. The original scale consists of 45 items. The authors of the IMI have suggested that different sets of the original scale can be used, depending on subscales’ relevance to the issues researchers are exploring. Items can also be removed if they “sound” redundant. In the overall inventory, the interest/enjoyment subscale is considered the most direct self-report measure of intrinsic motivation. The Vitality Index (VI) [100] is an easy to administrate, medical staff-rated scale to assess vitality with regard to activities of daily living. It consists of 5 items (waking up, communication, feeding, on and off toilet, and rehabilitation/activity) and all items are answered with a 3-point scale. The presence of item #5 (rehabilitation/activity) in its framework justifies the use of VI as an indirect motivation measurement instrument [76]. The reliability of the VI was examined by determining test–retest reliability (0.98), interrater reliability (0.14), and internal consistency (Cronbach α: 0.88). In other studies of our review, scales concerning the motivation for physical activity have been used. The Echelle de Motivation envers l’Activité Physique (EMAP) [101] consists of 18 items, which cover the 6 forms of motivation underlined by SDT, and can be considered as a valid, reliable, and patient-rated tool to assess motivation in the rehabilitation context. In a validation study of the EMAP in the Spanish population [102], the factor analysis confirmed the original six dimensions of EMAP. A validation of the EMAP in the English language has not yet been performed. Finally, the Behavioural Regulation in Exercise Questionnaire [BREQ], proposed in the original version by Mullan et al. [103], was a first attempt to develop an instrument able to quantify the behavioural regulation in the exercise domain. The BREQ-3 [104,105], is a patient-rated scale which investigates the reasons underlying peoples’ decisions to engage in physical exercise. It consists of 24 items with a 5-point Likert scale and includes six subscales, assessing amotivation, external, introjected, identified, integrated regulation, and intrinsic motivation. Its validity was confirmed by several validation studies in other languages and, recently, it has been proved to be invariant across very different age groups [106].
4.2. Motivation, Depressive Features and Participation in Stroke Patients
Motivational deficits are prevalent in several psychiatric disorders including depression, where a persistent lack of motivation is a pivotal symptom. In the post-stroke depression (PSD), which occurs in approximately one in three stroke-surviving patients [107], motivational impairments have been previously described. The importance of diagnosis and treatment of this disease is crucial because of its negative impact on the rehabilitation outcome [108]. In fact, as shown in a retrospective, case-control study, PSD was demonstrated to be an additional disabling factor which is responsible for ~15% of the increased disability [109]. In a factor analysis of the PSDRS [110], an assessment scale specifically developed for PSD, Quaranta et al. [111] identified a factor, named “Reduced Motivation”, resulting from the combination of apathy and anhedonia. Anhedonia, defined as an inability to experience pleasure, is one of the core symptoms of major depressive disorder (MDD) [112] and, as feature of PSD, has been associated with increased levels of depression at hospital discharge [113]. Anhedonia has been related to cognitive deficits, including executive dysfunction [114], and has been associated with the disruption of neural circuits and neuroendocrine impairments in stroke patients [115]. Although anhedonia is well known to play a relevant role in motivational aspects of (selected) post-stroke patients, very few studies concerning its role in rehabilitation is available, while many studies investigated the role of apathy. Apathy is defined as a lack of motivation relative to the patient’s previous level of functioning, accompanied by a quantitative reduction of goal-directed behaviour and cognition [116]. Starkstein et al. [117] found that 18 of 80 consecutive patients (22.5%) with an acute cerebrovascular lesion met this criterion for apathy. In addition, Santa et al. [118] observed that 14 patients (21%) among 67 subacute stroke subjects were apathetic. As expected, these patients, if compared with non-apathetic patients, showed less improvement in functional independence. Although often associated with depression and cognitive impairment, apathy may occur independently of both [119], but may often be misdiagnosed as depression due to symptom overlap [120]. In general, it is well known that cognitive impairments in depression are strictly connected to impairments in motivational processes [121]. As an example, Kanellopoulos et al. found in a sample of 135 older adults (age ≥ 50) with PSD that apathy is the only symptom cluster of PSD with a significant relationship to cognitive impairment across several neuropsychological domains [122].
In the literature, several tools to assess PSD are available. In addition to the above-mentioned PSDRS [110], the Beck’s Depression Inventory (BDI-II) [123], the Hamilton Depression Rating Scale (HAM-D) [124], the Montgomery-Åsberg Depression Rating Scale (MADRS) [125], and the Zung Self-Rating Depression Scale (ZSRDS) [126] are widely used, providing an adequate measure of depression in stroke patients [127]. Anyways, it should be noted that a PSD assessment in toto may provide an indirect motivation assessment. In fact, these scales are designed to investigate all aspects of depression and do not directly address the motivational features. In our review, some studies have used valid PSD assessment tools, such as the 10-item Center for the Epidemiological Studies of Depression Short Form (CES-D10) [128], the Apathy Evaluation Scale (AES) [129], and the Geriatric Depression Scale—15 items (GDS-15) [130]. Among these tools, we believe that AES, because of its intrinsic nature focused on apathy, could probably be considered as the most suitable motivation assessment tool. This consideration is also supported from other studies concerning this scale and success in rehabilitation [131,132].
With regard to learning theories, participation can be defined as the degree of active involvement of a student in classroom learning activities. Similarly, we consider participation in the neurorehabilitation setting as the process that drives patients to be an active part of the decisions and of the activities that influence their recovery. Engagement in rehabilitation and active involvement in the rehabilitation program are in fact crucial for recovery. A qualitative study using semi-structured interviews [26] found differences among 22 stroke patients, identified by professionals as having either “high” or “low” motivation in rehabilitation. In contrast to low motivation patients, high motivation patients were more involved, more likely to understand the purpose of the neurorehabilitation, and more aligned to the aims and methods of rehabilitation professionals.
Motivation and participation are strictly linked, e.g., motivational deficits trigger unavoidable consequences at the participation level [133]. In this sense, participation assessment can be considered as a surrogate to assess the motivation level. Based on the rating of medical staff, the Pittsburgh Rehabilitation Participation Scale (PRPS) [134,135] evaluates indirectly the patients’ motivation. It consists of a single item. The examinator rates, on a scale from 1 to 6, the patient’s participation (effort and motivation as perceived by the examinator) in the therapy session. As it is based on the clinicians’ observation without any patient self-report, the PRPS might not reflect the patients’ real motivation. The revised Patient Participation in Rehabilitation Questionnaire (PPRQ) [136] is a 20-item questionnaire, developed for patients with various neurological diseases (including stroke), which rates patients’ experiences of participation in neurological rehabilitation. This scale evaluates five participation aspects, including the motivation domain. Finally, the Participation Scale (P-scale) [137] is a participation assessment tool, developed by an international team, which measures (social) participation for use in rehabilitation, stigma reduction, and social integration programs. In our review, the P-scale was used by [79].
5. Limitations
The findings of this review are limited by inclusion dates. We chose to report on tools used in the past 12 years, due to the significant progress of the concept of patient motivation in rehabilitation over the last decade. For example, the two most promising assessment tools (SMRS and MORE), specifically designed for stroke patients in rehabilitation, were developed, respectively, in 2012 and 2022. We expect that other assessment tools, eventually characterized by the presence of some “adjustment factors” (i.e., for patients’ age, for initial impairment severity, etc.), will be developed in the future.
6. Conclusions and Recommendations for Future Studies
Due to its role in rehabilitation as a determining factor of outcome, a reliable validated instrument to measure motivation is paramount. As highlighted in this review, in the stroke literature, several motivation assessments tools have been developed. These are grouped into two categories: the first including tools exploring the relationship between patient and rehabilitation and the latter reflecting the trade-off between patient and intervention. An indirect estimation of the motivation level can be also obtained through assessment tools specifically designed to measure participation or apathy. We believe that the simultaneous administration of combined patient- and medical staff-rated motivation assessments may provide an overall measurement tool of motivation and reduce bias. Finally, motivation represents a dynamic phenomenon, whose level can be enhanced or diminished, sometimes in short timelapses, by several factors. For this reason, motivation should be regularly assessed, especially in rehabilitation, where the clinical course may be long lasting and prone to multiple changes. A frequent assessment might be helpful to identify possible motivation decreases and, potentially, to react appropriately by adapting therapeutic strategies.
Appendix A
Table A1.
Quality control.
| First Author | Quality Check |
|---|---|
| Bergmann J [44] | ++ |
| Winter C [45] | ++ |
| Guillén-Climent S [46] | + |
| Navarro MD [47] | ++ |
| Swinnen E [48] | + |
| Prange GB [49] | + |
| Johar MN [50] | ++ |
| Hung NT [51] | + |
| Thielbar KO [52] | ++ |
| Nijenhuis SM [53] | ++ |
| Nijenhuis SM [54] | ++ |
| Subramaniam S [55] | ++ |
| Friedman N [56] | ++ |
| Lloréns R [57] | ++ |
| Knippenberg E [58] | ++ |
| Popović MD [59] | ++ |
| Novak D [60] | ++ |
| Chen L [61] | ++ |
| Radder B [62] | + |
| Ahmad MA [63] | ++ |
| Rapolienė J [64] | ++ |
| Lin FH [65] | + |
| Hung JW [66] | ++ |
| LaPiana N [67] | + |
| Huber SK [68] | ++ |
| Graven C [69] | + |
| Morice E [70] | ++ |
| An HJ [71] | ++ |
| Adhikari SP [72] | ++ |
| Thompson N [73] | + |
| Street AJ [74] | + |
| Morone G [75] | ++ |
| Deguchi K [76] | - |
| Seregni A [77] | - |
| Chen HM [78] | ++ |
| Aramaki AL [79] | ++ |
| Wissink KS [80] | ++ |
| Chowdhury A [81] | ++ |
| Song HS [82] | ++ |
| Park JS [83] | ++ |
| Alhirsan SM [84] | ++ |
| Grau-Sánchez J [85] | ++ |
| Zhang L [86] | ++ |
| Rozevink SG [87] | + |
| Skidmore ER [88] | ++ |
| Cano-Mañas MJ [89] | + |
Author Contributions
Conceptualization, G.V. and M.I.; methodology, C.R., G.V. and G.L.; validation, C.R., G.L. and D.D.B.; data curation, G.V. and G.L.; writing—original draft preparation: all authors; writing—review and editing, C.R. and G.V.; supervision, M.I. and D.D.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Schunk D.H., Meece J.L., Pintrich P.R. Motivation in Education: Theory, Research, and Applications. 4th ed. Pearson; Upper Saddle River, NJ, USA: 2014. [Google Scholar]
- 2.Ryan R.M., Deci E. Intrinsic and Extrinsic Motivations: Classic Definitions and New Directions. Contemp. Educ. Psychol. 2000;25:54–67. doi: 10.1006/ceps.1999.1020. [DOI] [PubMed] [Google Scholar]
- 3.Deci E.L., Olafsen A.H., Ryan R.M. Self-Determination Theory in Work Organizations: The State of a Science. Annu. Rev. Organ. Psychol. Organ. Behav. 2017;4:19–43. doi: 10.1146/annurev-orgpsych-032516-113108. [DOI] [Google Scholar]
- 4.Steers R.M., Mowday R.T., Shapiro D.L. Introduction to Special Topic Forum: The Future of Work Motivation Theory. Acad. Manag. Rev. 2004;29:379–387. doi: 10.2307/20159049. [DOI] [Google Scholar]
- 5.Latham G.P. Work Motivation: History, Theory, Research, and Practice. Sage Publications, Inc.; Newbury Park, CA, USA: 2007. [Google Scholar]
- 6.Tohidi H., Jabbari M.M. The effects of motivation in education. Procedia-Soc. Behav. Sci. 2012;31:820–824. doi: 10.1016/j.sbspro.2011.12.148. [DOI] [Google Scholar]
- 7.Stirling D. Motivation in Education. Aichi Univ. Engl. Educ. Res. J. 2013;29:51–72. [Google Scholar]
- 8.Gillison F.B., Rouse P., Standage M., Sebire S.J., Ryan R.M. A meta-analysis of techniques to promote motivation for health behaviour change from a self-determination theory perspective. Health Psychol. Rev. 2019;13:110–130. doi: 10.1080/17437199.2018.1534071. [DOI] [PubMed] [Google Scholar]
- 9.Maclean N., Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc. Sci. Med. 2000;50:495–506. doi: 10.1016/s0277-9536(99)00334-2. [DOI] [PubMed] [Google Scholar]
- 10.Deci E.L., Ryan R.M. Motivation, personality, and development within embedded social contexts: An overview of self-determination theory. In: Ryan R.M., editor. The Oxford Handbook of Human Motivation. Oxford University Press; New York, NY, USA: 2012. pp. 85–107. [Google Scholar]
- 11.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Perspective. Princeton-Hall; Princeton, NJ, USA: 1986. p. 391. [Google Scholar]
- 12.Locke E.A., Latham G.P. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. Am. Psychol. 2002;57:705–717. doi: 10.1037/0003-066X.57.9.705. [DOI] [PubMed] [Google Scholar]
- 13.Deci E., Ryan R.M. Intrinsic Motivation and Self-Determination in Human Behavior. Plenum; New York, NY, USA: 1985. [Google Scholar]
- 14.Ryan R.M., Deci E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2020;55:68–78. doi: 10.1037/0003-066X.55.1.68. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Self-Efficacy: The Exercise of Control. W. H. Freeman and Company; New York, NY, USA: 1997. [Google Scholar]
- 16.Locke E.A., Latham G.P. New Developments in Goal Setting and Task Performance. 1st ed. Routledge; New York, NY, USA: 2012. [DOI] [Google Scholar]
- 17.Dweck C.S., Leggett E.L. A social-cognitive approach to motivation and personality. Psychol. Rev. 1988;95:256–273. doi: 10.1037/0033-295X.95.2.256. [DOI] [Google Scholar]
- 18.Salter K., Hellings C., Foley N., Teasell R. The experience of living with stroke: A qualitative meta-synthesis. J. Rehabil. Med. 2008;40:595–602. doi: 10.2340/16501977-0238. [DOI] [PubMed] [Google Scholar]
- 19.Hafsteinsdottir T., Grypdonck M. Being a stroke patient: A review of the literature. J. Adv. Nurs. 1997;26:580–588. doi: 10.1046/j.1365-2648.1997.t01-19-00999.x. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Health Topics: Rehabilitation. [(accessed on 1 August 2022)]. Available online: https://www.who.int/rehabilitation/en/
- 21.Kusec A., Velikonja D., DeMatteo C., Harris J.E. Motivation in rehabilitation and acquired brain injury: Can theory help us understand it? Disabil. Rehabil. 2018;41:2343–2349. doi: 10.1080/09638288.2018.1467504. [DOI] [PubMed] [Google Scholar]
- 22.Yoshida T., Otaka Y., Osu R., Kumagai M., Kitamura S., Yaeda J. Motivation for Rehabilitation in Patients With Subacute Stroke: A Qualitative Study. Front. Rehabil. Sci. 2021;2:664758. doi: 10.3389/fresc.2021.664758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oh S.Y., Hwang S.Y., Chung M.L., Lennie T.A. A Prediction Model of Rehabilitation Motivation in Middle-Aged Survivors of Stroke in Rehabilitation Facilities in Korea. J. Cardiovasc. Nurs. 2020;35:475–482. doi: 10.1097/JCN.0000000000000656. [DOI] [PubMed] [Google Scholar]
- 24.Teixeira P.J., Carraça E.V., Markland D., Silva M.N., Ryan R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012;9:78. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Silva M.N., Markland D., Carraça E., Vieira P.N., Coutinho S.R., Minderico C., de Matos M.G., Sardinha L., Teixeira P. Exercise Autonomous Motivation Predicts 3-yr Weight Loss in Women. Med. Sci. Sports Exerc. 2011;43:728–737. doi: 10.1249/MSS.0b013e3181f3818f. [DOI] [PubMed] [Google Scholar]
- 26.Maclean N., Pound P., Wolfe C., Rudd A. Qualitative analysis of stroke patients’ motivation for rehabilitation. BMJ. 2000;321:1051–1054. doi: 10.1136/bmj.321.7268.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cerasoli C.P., Nicklin J.M., Ford M.T. Intrinsic motivation and extrinsic incentives jointly predict performance: A 40-year meta-analysis. Psychol. Bull. 2014;140:980–1008. doi: 10.1037/a0035661. [DOI] [PubMed] [Google Scholar]
- 28.Leonardi M., Fheodoroff K. Goal Setting with ICF (International Classification of Functioning, Disability and Health) and Multidisciplinary Team Approach in Stroke Rehabilitation. In: Platz T., editor. Clinical Pathways in Stroke Rehabil.: Evidence-Based Clinical Practice Recommendations. Springer; Cham, Switzerland: 2021. [PubMed] [Google Scholar]
- 29.Studer B., Van Dijk H., Handermann R., Knecht S. Increasing self-directed training in neurorehabilitation patients through competition. Prog. Brain Res. 2016;229:367–388. doi: 10.1016/bs.pbr.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 30.Baur K., Schättin A., de Bruin E.D., Riener R., Duarte J.E., Wolf P. Trends in robot-assisted and virtual reality-assisted neuromuscular therapy: A systematic review of health-related multiplayer games. J. Neuroeng. Rehabil. 2018;15:107. doi: 10.1186/s12984-018-0449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siegert R.J., Taylor W.J. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil. Rehabil. 2004;26:1–8. doi: 10.1080/09638280410001644932. [DOI] [PubMed] [Google Scholar]
- 32.Playford E.D., Siegert R., Levack W., Freeman J. Areas of consensus and controversy about goal setting in rehabilitation: A conference report. Clin. Rehabil. 2009;23:334–344. doi: 10.1177/0269215509103506. [DOI] [PubMed] [Google Scholar]
- 33.Levack W.M., Weatherall M., Hay-Smith E.J.C., Dean S.G., McPherson K., Siegert R.J. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst. Rev. 2015;2015:CD009727. doi: 10.1002/14651858.CD009727.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosewilliam S., Roskell C.A., Pandyan A. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin. Rehabil. 2011;25:501–514. doi: 10.1177/0269215510394467. [DOI] [PubMed] [Google Scholar]
- 35.Wressle E., Eeg-Olofsson A.-M., Marcusson J., Henriksson C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J. Rehabil. Med. 2002;34:5–11. doi: 10.1080/165019702317242640. [DOI] [PubMed] [Google Scholar]
- 36.Combs S.A., Kelly S.P., Barton R., Ivaska M., Nowak K. Effects of an intensive, task-specific rehabilitation program for individuals with chronic stroke: A case series. Disabil. Rehabil. 2010;32:669–678. doi: 10.3109/09638280903242716. [DOI] [PubMed] [Google Scholar]
- 37.Hillig T., Ma H., Dorsch S. Goal-oriented instructions increase the intensity of practice in stroke rehabilitation compared with non-specific instructions: A within-participant, repeated measures experimental study. J. Physiother. 2019;65:95–98. doi: 10.1016/j.jphys.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 38.Frost Y., Weingarden H., Zeilig G., Nota A., Rand D. Self-Care Self-Efficacy Correlates with Independence in Basic Activities of Daily Living in Individuals with Chronic Stroke. J. Stroke Cerebrovasc. Dis. 2015;24:1649–1655. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.054. [DOI] [PubMed] [Google Scholar]
- 39.Bailey R.R. Self-Efficacy, Self-Regulation, Social Support, and Outcomes Expectations for Daily Physical Activity in Adults with Chronic Stroke: A Descriptive, Exploratory Study. Occup. Ther. Health Care. 2019;33:129–141. doi: 10.1080/07380577.2018.1558326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stewart J.C., Lewthwaite R., Rocktashel J., Winstein C. Self-efficacy and Reach Performance in Individuals With Mild Motor Impairment Due to Stroke. Neurorehabilit. Neural Repair. 2019;33:319–328. doi: 10.1177/1545968319836231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caetano L.C.G., Pacheco B.D., Samora G.A.R., Teixeira-Salmela L.F., Scianni A.A. Self-Efficacy to Engage in Physical Exercise and Walking Ability Best Predicted Exercise Adherence after Stroke. Stroke Res. Treat. 2020;2020:2957623. doi: 10.1155/2020/2957623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Institute for Health and Care Excellence. [(accessed on 10 October 2022)]. Available online: https://www.nice.org.uk/process/pmg4/chapter/appendix-h-quality-appraisal-checklist-qualitative-studies.
- 43.Bessa N.P.O.S., Filho B.F.D.L., De Medeiros C.S.P., Ribeiro T.S., Campos T.F., Cavalcanti F.A.D.C. Effects of exergames training on postural balance in patients who had a chronic stroke: Study protocol for a randomised controlled trial. BMJ Open. 2020;10:e038593. doi: 10.1136/bmjopen-2020-038593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bergmann J., Krewer C., Bauer P., Koenig A., Riener R., Müller F. Virtual reality to augment robot-assisted gait training in non-ambulatory patients with a subacute stroke: A pilot randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018;54:397–407. doi: 10.23736/S1973-9087.17.04735-9. [DOI] [PubMed] [Google Scholar]
- 45.Winter C., Kern F., Gall D., Latoschik M.E., Pauli P., Käthner I. Immersive virtual reality during gait rehabilitation increases walking speed and motivation: A usability evaluation with healthy participants and patients with multiple sclerosis and stroke. J. Neuroeng. Rehabil. 2021;18:68. doi: 10.1186/s12984-021-00848-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guillén-Climent S., Garzo A., Muñoz-Alcaraz M.N., Casado-Adam P., Arcas-Ruiz-Ruano J., Mejías-Ruiz M., Mayordomo-Riera F.J. A usability study in patients with stroke using MERLIN, a robotic system based on serious games for upper limb rehabilitation in the home setting. J. Neuroeng. Rehabil. 2021;18:41. doi: 10.1186/s12984-021-00837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Navarro M.D., Llorens R., Borrego A., Alcañiz M., Noé E., Ferri J. Competition Enhances the Effectiveness and Motivation of Attention Rehabilitation After Stroke. A Randomized Controlled Trial. Front. Hum. Neurosci. 2020;14:575403. doi: 10.3389/fnhum.2020.575403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Swinnen E., Lefeber N., Willaert W., De Neef F., Bruyndonckx L., Spooren A., Michielsen M., Ramon T., Kerckhofs E. Motivation, expectations, and usability of a driven gait orthosis in stroke patients and their therapists. Top. Stroke Rehabil. 2017;24:299–308. doi: 10.1080/10749357.2016.1266750. [DOI] [PubMed] [Google Scholar]
- 49.Prange G.B., Kottink A.I.R., Buurke J.H., Eckhardt M.M.E.M., Van Keulen-Rouweler B.J., Ribbers G.M., Rietman J.S. The Effect of Arm Support Combined With Rehabilitation Games on Upper-Extremity Function in Subacute Stroke: A randomized controlled trial. Neurorehabilit. Neural Repair. 2015;29:174–182. doi: 10.1177/1545968314535985. [DOI] [PubMed] [Google Scholar]
- 50.Johar M.N.M., Nordin N.A.M., Aziz A.F.A. The effect of game-based in comparison to conventional circuit exercise on functions, motivation level, self-efficacy and quality of life among stroke survivors. Medicine. 2022;101:e28580. doi: 10.1097/MD.0000000000028580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hung N.T., Paul V., Prakash P., Kovach T., Tacy G., Tomic G., Park S., Jacobson T., Jampol A., Patel P., et al. Wearable myoelectric interface enables high-dose, home-based training in severely impaired chronic stroke survivors. Ann. Clin. Transl. Neurol. 2021;8:1895–1905. doi: 10.1002/acn3.51442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thielbar K.O., Triandafilou K.M., Barry A., Yuan N., Nishimoto A., Johnson J., Stoykov M.E., Tsoupikova D., Kamper D.G. Home-based Upper Extremity Stroke Therapy Using a Multiuser Virtual Reality Environment: A Randomized Trial. Arch. Phys. Med. Rehabil. 2020;101:196–203. doi: 10.1016/j.apmr.2019.10.182. [DOI] [PubMed] [Google Scholar]
- 53.Nijenhuis S.M., Prange G.B., Amirabdollahian F., Sale P., Infarinato F., Nasr N., Mountain G., Hermens H.J., Stienen A.H.A., Buurke J.H., et al. Feasibility study into self-administered training at home using an arm and hand device with motivational gaming environment in chronic stroke. J. Neuroeng. Rehabil. 2015;12:89. doi: 10.1186/s12984-015-0080-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nijenhuis S.M., Prange-Lasonder G.B., Stienen A.H., Rietman J.S., Buurke J.H. Effects of training with a passive hand orthosis and games at home in chronic stroke: A pilot randomised controlled trial. Clin. Rehabil. 2017;31:207–216. doi: 10.1177/0269215516629722. [DOI] [PubMed] [Google Scholar]
- 55.Subramaniam S., Hui-Chan C.W.-Y., Bhatt T. A Cognitive-Balance Control Training Paradigm Using Wii Fit to Reduce Fall Risk in Chronic Stroke Survivors. J. Neurol. Phys. Ther. 2014;38:216–225. doi: 10.1097/NPT.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 56.Friedman N., Chan V., Reinkensmeyer A.N., Beroukhim A., Zambrano G.J., Bachman M., Reinkensmeyer D.J. Retraining and assessing hand movement after stroke using the MusicGlove: Comparison with conventional hand therapy and isometric grip training. J. Neuroeng. Rehabil. 2014;11:76. doi: 10.1186/1743-0003-11-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lloréns R., Noé E., Colomer C., Alcañiz M. Effectiveness, Usability, and Cost-Benefit of a Virtual Reality–Based Telerehabilitation Program for Balance Recovery After Stroke: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2015;96:418–425.e2. doi: 10.1016/j.apmr.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 58.Knippenberg E., Lamers I., Timmermans A., Spooren A. Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study. Int. J. Environ. Res. Public Health. 2021;18:7641. doi: 10.3390/ijerph18147641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Popović M.D., Kostić M.D., Rodić S.Z., Konstantinović L.M. Feedback-Mediated Upper Extremities Exercise: Increasing Patient Motivation in Poststroke Rehabilitation. BioMed Res. Int. 2014;2014:520374. doi: 10.1155/2014/520374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Novak D., Nagle A., Keller U., Riener R. Increasing motivation in robot-aided arm rehabilitation with competitive and cooperative gameplay. J. Neuroeng. Rehabil. 2014;11:64. doi: 10.1186/1743-0003-11-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen L., Xiong S., Liu Y., Lin M., Zhu L., Zhong R., Zhao J., Liu W., Wang J., Shang X. Comparison of Motor Relearning Program versus Bobath Approach for Prevention of Poststroke Apathy: A Randomized Controlled Trial. J. Stroke Cerebrovasc. Dis. 2019;28:655–664. doi: 10.1016/j.jstrokecerebrovasdis.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 62.Radder B., Prange-Lasonder G., Kottink A., Melendez-Calderon A., Buurke J., Rietman J. Feasibility of a wearable soft-robotic glove to support impaired hand function in stroke patients. J. Rehabil. Med. 2018;50:598–606. doi: 10.2340/16501977-2357. [DOI] [PubMed] [Google Scholar]
- 63.Ahmad M.A., Singh D.K.A., Nordin N.A.M., Nee K.H., Ibrahim N. Virtual Reality Games as an Adjunct in Improving Upper Limb Function and General Health among Stroke Survivors. Int. J. Environ. Res. Public Health. 2019;16:5144. doi: 10.3390/ijerph16245144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rapolienė J., Endzelytė E., Jasevičienė I., Savickas R. Stroke Patients Motivation Influence on the Effectiveness of Occupational Therapy. Rehabil. Res. Pract. 2018;2018:9367942. doi: 10.1155/2018/9367942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lin F.-H., Yih D.N., Shih F.-M., Chu C.-M. Effect of social support and health education on depression scale scores of chronic stroke patients. Medicine. 2019;98:e17667. doi: 10.1097/MD.0000000000017667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hung J.-W., Yu M.-Y., Chang K.-C., Lee H.-C., Hsieh Y.-W., Chen P.-C. Feasibility of Using Tetrax Biofeedback Video Games for Balance Training in Patients With Chronic Hemiplegic Stroke. PM&R. 2016;8:962–970. doi: 10.1016/j.pmrj.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 67.LaPiana N., Duong A., Lee A., Alschitz L., Silva R.M.L., Early J., Bunnell A., Mourad P. Acceptability of a Mobile Phone–Based Augmented Reality Game for Rehabilitation of Patients With Upper Limb Deficits from Stroke: Case Study. JMIR Rehabil. Assist. Technol. 2020;7:e17822. doi: 10.2196/17822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Huber S.K., Held J.P.O., de Bruin E.D., Knols R.H. Personalized Motor-Cognitive Exergame Training in Chronic Stroke Patients—A Feasibility Study. Front. Aging Neurosci. 2021;13:730801. doi: 10.3389/fnagi.2021.730801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Graven C., Brock K., Hill K., Ames D., Cotton S., Joubert L. From rehabilitation to recovery: Protocol for a randomised controlled trial evaluating a goal-based intervention to reduce depression and facilitate participation post-stroke. BMC Neurol. 2011;11:73. doi: 10.1186/1471-2377-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morice E., Moncharmont J., Jenny C., Bruyneel A.-V. Dancing to improve balance control, cognitive-motor functions and quality of life after stroke: A study protocol for a randomised controlled trial. BMJ Open. 2020;10:e037039. doi: 10.1136/bmjopen-2020-037039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.An H.-J., Park S.-J. Effects of Animal-Assisted Therapy on Gait Performance, Respiratory Function, and Psychological Variables in Patients Post-Stroke. Int. J. Environ. Res. Public Health. 2021;18:5818. doi: 10.3390/ijerph18115818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Adhikari S.P., Tretriluxana J., Chaiyawat P., Jalayondeja C. Enhanced Upper Extremity Functions with a Single Session of Action-Observation-Execution and Accelerated Skill Acquisition Program in Subacute Stroke. Stroke Res. Treat. 2018;2018:1490692. doi: 10.1155/2018/1490692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thompson N., Bloska J., Abington A., Masterson A., Whitten D., Street A. The Feasibility and Acceptability of Neurologic Music Therapy in Subacute Neurorehabilitation and Effects on Patient Mood. Brain Sci. 2022;12:497. doi: 10.3390/brainsci12040497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Street A.J., Magee W.L., Bateman A., Parker M., Odell-Miller H., Fachner J. Home-based neurologic music therapy for arm hemiparesis following stroke: Results from a pilot, feasibility randomized controlled trial. Clin. Rehabil. 2018;32:18–28. doi: 10.1177/0269215517717060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Morone G., Pisotta I., Pichiorri F., Kleih S., Paolucci S., Molinari M., Cincotti F., Kübler A., Mattia D. Proof of Principle of a Brain-Computer Interface Approach to Support Poststroke Arm Rehabilitation in Hospitalized Patients: Design, Acceptability, and Usability. Arch. Phys. Med. Rehabil. 2015;96((Suppl. 3)):S71–S78. doi: 10.1016/j.apmr.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 76.Deguchi K., Kono S., Deguchi S., Morimoto N., Kurata T., Ikeda Y., Abe K. A Novel Useful Tool of Computerized Touch Panel–Type Screening Test for Evaluating Cognitive Function of Chronic Ischemic Stroke Patients. J. Stroke Cerebrovasc. Dis. 2013;22:e197–e206. doi: 10.1016/j.jstrokecerebrovasdis.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 77.Seregni A., Tricomi E., Tropea P., Del Pino R., Gómez-Esteban J.C., Gabilondo I., Díez-Cirarda M., Schlieter H., Gand K., Corbo M. Virtual Coaching for Rehabilitation: The Participatory Design Experience of the vCare Project. Front. Public Health. 2021;9:748307. doi: 10.3389/fpubh.2021.748307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen H.-M., Lee H.-L., Yang F.-C., Chiu Y.-W., Chao S.-Y. Effectiveness of Motivational Interviewing in Regard to Activities of Daily Living and Motivation for Rehabilitation among Stroke Patients. Int. J. Environ. Res. Public Health. 2020;17:2755. doi: 10.3390/ijerph17082755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aramaki A.L., Sampaio R.F., Cavalcanti A., Dutra F.C.M.S.E. Use of client-centered virtual reality in rehabilitation after stroke: A feasibility study. Arq. Neuro-Psiquiatr. 2019;77:622–631. doi: 10.1590/0004-282x20190103. [DOI] [PubMed] [Google Scholar]
- 80.Wissink K.S., Eijk M.S.-V., Buijck B.I., Koopmans R.T.C.M., Zuidema S.U. CVA-revalidatie in het verpleeghuis: Therapie-intensiteit van en motivatie voor fysiotherapie [Stroke rehabilitation in nursing homes: Intensity of and motivation for physiotherapy] Tijdschr. Gerontol. Geriatr. 2014;45:144–153. doi: 10.1007/s12439-014-0072-6. [DOI] [PubMed] [Google Scholar]
- 81.Chowdhury A., Meena Y.K., Raza H., Bhushan B., Uttam A.K., Pandey N., Hashmi A.A., Bajpai A., Dutta A., Prasad G. Active Physical Practice Followed by Mental Practice Using BCI-Driven Hand Exoskeleton: A Pilot Trial for Clinical Effectiveness and Usability. IEEE J. Biomed. Health Inform. 2018;22:1786–1795. doi: 10.1109/JBHI.2018.2863212. [DOI] [PubMed] [Google Scholar]
- 82.Song H.S., Kim J.Y., Park S.D. The effect of class-based task-oriented circuit training on the self-satisfaction of patients with chronic stroke. J. Phys. Ther. Sci. 2015;27:127–129. doi: 10.1589/jpts.27.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Park J.-S., Lee G., Choi J.-B., Hwang N.-K., Jung Y.-J. Game-based hand resistance exercise versus traditional manual hand exercises for improving hand strength, motor function, and compliance in stroke patients: A multi-center randomized controlled study. Neurorehabilitation. 2019;45:221–227. doi: 10.3233/NRE-192829. [DOI] [PubMed] [Google Scholar]
- 84.Alhirsan S.M., Capó-Lugo C.E., Brown D.A. Effects of different types of augmented feedback on intrinsic motivation and walking speed performance in post-stroke: A study protocol. Contemp. Clin. Trials Commun. 2021;24:100863. doi: 10.1016/j.conctc.2021.100863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Grau-Sánchez J., Segura E., Sanchez-Pinsach D., Raghavan P., Münte T.F., Palumbo A.M., Turry A., Duarte E., Särkämö T., Cerquides J., et al. Enriched Music-supported Therapy for chronic stroke patients: A study protocol of a randomised controlled trial. BMC Neurol. 2021;21:19. doi: 10.1186/s12883-020-02019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang L., Yan Y., Sun Z., Ge X., Qin X., Lin K.-C. Coaching-Based Teleoccupational Guidance for Home-Based Stroke Survivors and Their Family Caregivers: Study Protocol for a Superior Randomized Controlled Trial. Evid.-Based Complement. Altern. Med. 2022;2022:9123498. doi: 10.1155/2022/9123498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rozevink S.G., van der Sluis C.K., Garzo A., Keller T., Hijmans J.M. HoMEcare aRm rehabiLItatioN (MERLIN): Telerehabilitation using an unactuated device based on serious games improves the upper limb function in chronic stroke. J. Neuroeng. Rehabil. 2021;18:48. doi: 10.1186/s12984-021-00841-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Skidmore E.R., Whyte E.M., Butters M.A., Terhorst L., Reynolds C.F., III Strategy Training During Inpatient Rehabilitation May Prevent Apathy Symptoms After Acute Stroke. PM&R. 2015;7:562–570. doi: 10.1016/j.pmrj.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cano-Mañas M.J., Collado-Vázquez S., Hernández J.R., Villena A.J.M., Cano-De-La-Cuerda R. Effects of Video-Game Based Therapy on Balance, Postural Control, Functionality, and Quality of Life of Patients with Subacute Stroke: A Randomized Controlled Trial. J. Health Eng. 2020;2020:5480315. doi: 10.1155/2020/5480315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McAuley E., Duncan T., Tammen V.V. Psychometric Properties of the Intrinsic Motivation Inventory in a Competitive Sport Setting: A Confirmatory Factor Analysis. Res. Q. Exerc. Sport. 1989;60:48–58. doi: 10.1080/02701367.1989.10607413. [DOI] [PubMed] [Google Scholar]
- 91.Maclean N., Pound P., Wolfe C., Rudd A. The Concept of Patient Motivation: A qualitative analysis of. Stroke professionals’ attitudes. Stroke. 2002;33:444–448. doi: 10.1161/hs0202.102367. [DOI] [PubMed] [Google Scholar]
- 92.White G.N., Cordato D.J., O’Rourke F., Mendis R.L., Ghia D., Chan D. Validation of the stroke rehabilitation motivation scale: A pilot study. Asian J. Gerontol. Geriatr. 2012;7:80–87. [Google Scholar]
- 93.Yoshida T., Otaka Y., Kitamura S., Ushizawa K., Kumagai M., Kurihara Y., Yaeda J., Osu R. Development and validation of new evaluation scale for measuring stroke patients’ motivation for rehabilitation in rehabilitation wards. PLoS ONE. 2022;17:e0265214. doi: 10.1371/journal.pone.0265214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Derakhshanrad S.A., Piven E. Modification of the Persian version of Hermans Achievement Motivation Questionnaire to develop an adapted scale for measuring motivation of post-stroke survivors in Iran. Iran. J. Neurol. 2016;15:189–194. [PMC free article] [PubMed] [Google Scholar]
- 95.Hallams S., Baker K. The development of a questionnaire to assess motivation in stroke survivors: A pilot study. N. Z. J. Physiother. 2009;37:55–61. [Google Scholar]
- 96.Pelletier L.G., Tuson K.M., Fortier M.S., Vallerand R.J., Briére N.M., Blais M.R. Toward a New Measure of Intrinsic Motivation, Extrinsic Motivation, and Amotivation in Sports: The Sport Motivation Scale (SMS) J. Sport Exerc. Psychol. 1995;17:35–53. doi: 10.1123/jsep.17.1.35. [DOI] [Google Scholar]
- 97.Park M., Lee J.-Y., Ham Y., Oh S.-W., Shin J.-H. Korean Version of the Stroke Rehabilitation Motivation Scale: Reliability and Validity Evaluation. Ann. Rehabil. Med. 2020;44:11–19. doi: 10.5535/arm.2020.44.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kuroda A., Setoguchi M., Uchino Y., Nagata K., Hokonohara D. Effect of rivastigmine on plasma butyrylcholine esterase activity and plasma ghrelin levels in patients with dementia in Alzheimer’s disease. Geriatr. Gerontol. Int. 2018;18:886–891. doi: 10.1111/ggi.13275. [DOI] [PubMed] [Google Scholar]
- 99.Fujita T., Sato A., Tsuchiya K., Ohashi T., Yamane K., Yamamoto Y., Iokawa K., Ohira Y., Otsuki K., Tozato F. Relationship between Grooming Performance and Motor and Cognitive Functions in Stroke Patients with Receiver Operating Characteristic Analysis. J. Stroke Cerebrovasc. Dis. 2017;26:2828–2833. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.054. [DOI] [PubMed] [Google Scholar]
- 100.Toba K., Nakai R., Akishita M., Iijima S., Nishinaga M., Mizoguchi T., Yamada S., Yumita K., Ouchi Y. Vitality Index as a useful tool to assess elderly with dementia. Geriatr. Gerontol. Int. 2002;2:23–29. doi: 10.1046/j.1444-1586.2002.00016.x. [DOI] [Google Scholar]
- 101.Boiché J., Gourlan M., Trouilloud D., Sarrazin P. Development and validation of the ‘Echelle de Motivation envers l’Activité Physique en contexte de Santé’: A motivation scale towards health-oriented physical activity in French. J. Health Psychol. 2019;24:386–396. doi: 10.1177/1359105316676626. [DOI] [PubMed] [Google Scholar]
- 102.González-García H., Martinent G., Vega-Díaz M. Validation of the motivation scale towards Health-Oriented physical activity (EMAPS) in Spanish Population. Curr. Psychol. 2022. pp. 1–13. Epub ahead of print . [DOI] [PMC free article] [PubMed]
- 103.Mullan E., Markland D., Ingledew D.K. A graded conceptualisation of self-determination in the regulation of exercise behaviour: Development of a measure using confirmatory factor analytic procedures. Pers. Individ. Differ. 1997;23:745–752. doi: 10.1016/S0191-8869(97)00107-4. [DOI] [Google Scholar]
- 104.Markland D., Tobin V. A modification of the Behavioral Regulation in Exercise Questionnaire to include an assessment of amotivation. J. Sport Exerc. Psychol. 2004;26:191–196. doi: 10.1123/jsep.26.2.191. [DOI] [Google Scholar]
- 105.Wilson P.M., Rodgers W.M., Loitz C.C., Scime G. “It’s who I am…really!” The importance of integrated regulation in exercise contexts. J. Biobehav. Res. 2006;11:79–104. doi: 10.1111/j.1751-9861.2006.tb00021.x. [DOI] [Google Scholar]
- 106.Cavicchiolo E., Sibilio M., Lucidi F., Cozzolino M., Chirico A., Girelli L., Manganelli S., Giancamilli F., Galli F., Diotaiuti P., et al. The Psychometric Properties of the Behavioural Regulation in Exercise Questionnaire (BREQ-3): Factorial Structure, Invariance and Validity in the Italian Context. Int. J. Environ. Res. Public Health. 2022;19:1937. doi: 10.3390/ijerph19041937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Das J., G.K. R. Post stroke depression: The sequelae of cerebral stroke. Neurosci. Biobehav. Rev. 2018;90:104–114. doi: 10.1016/j.neubiorev.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 108.Gainotti G., Antonucci G., Marra C., Paolucci S. Relation between depression after stroke, antidepressant therapy, and functional recovery. J. Neurol. Neurosurg. Psychiatry. 2001;71:258–261. doi: 10.1136/jnnp.71.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Paolucci S., Iosa M., Coiro P., Venturiero V., Savo A., DE Angelis D., Morone G. Post-stroke Depression Increases Disability More Than 15% in Ischemic Stroke Survivors: A Case-Control Study. Front. Neurol. 2019;10:926. doi: 10.3389/fneur.2019.00926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gainotti G., Azzoni A., Razzano C., Lanzillotta M., Marra C., Gasparini F. The Post-Stroke depression rating scale: A test specifically devised to investigate affective disorders of stroke patients. J. Clin. Exp. Neuropsychol. 1997;19:340–356. doi: 10.1080/01688639708403863. [DOI] [PubMed] [Google Scholar]
- 111.Quaranta D., Marra C., Gainotti G. Post-stroke depression: Main phenomenological clusters and their relationships with clinical measures. Behav. Neurol. 2012;25:303–310. doi: 10.1155/2012/501979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; Arlington, VA, USA: 2013. [Google Scholar]
- 113.Sibon I., Lassalle-Lagadec S., Renou P., Swendsen J. Evolution of Depression Symptoms following Stroke: A Prospective Study Using Computerized Ambulatory Monitoring. Cerebrovasc. Dis. 2012;33:280–285. doi: 10.1159/000334663. [DOI] [PubMed] [Google Scholar]
- 114.Piamarta F., Iurlaro S., Isella V., Atzeni L., Grimaldi M., Russo A.G., Forapani E., Appollonio I. Unconventional affective symptoms and executive functions after stroke in the elderly. Arch. Gerontol. Geriatr. 2004;38:315–323. doi: 10.1016/j.archger.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 115.Terroni L., Amaro E., Jr., Iosifescu D.V., Mattos P., Yamamoto F.I., Tinone G., Conforto A., Sobreiro M.F., Delgado V.D., De Lucia M.C.S., et al. The association of post-stroke anhedonia with salivary cortisol levels and stroke lesion in hippocampal/parahippocampal region. Neuropsychiatr. Dis. Treat. 2015;11:233–242. doi: 10.2147/NDT.S73722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Marin R.S. Apathy: A neuropsychiatric syndrome. J. Neuropsychiatry Clin. Neurosci. 1991;3:243–254. doi: 10.1176/jnp.3.3.243. [DOI] [PubMed] [Google Scholar]
- 117.Starkstein S.E., Fedoroff J.P., Price T.R., Leiguarda R., Robinson R.G. Apathy following cerebrovascular lesions. Stroke. 1993;24:1625–1630. doi: 10.1161/01.STR.24.11.1625. [DOI] [PubMed] [Google Scholar]
- 118.Santa N., Sugimori H., Kusuda K., Yamashita Y., Ibayashi S., Iida M. Apathy and functional recovery following first-ever stroke. Int. J. Rehabil. Res. 2008;31:321–326. doi: 10.1097/MRR.0b013e3282fc0f0e. [DOI] [PubMed] [Google Scholar]
- 119.Jorge R.E., Starkstein S.E., Robinson R.G. Apathy following Stroke. Can. J. Psychiatry. 2010;55:350–354. doi: 10.1177/070674371005500603. [DOI] [PubMed] [Google Scholar]
- 120.Borgi M., Caccamo F., Giuliani A., Piergentili A., Sessa S., Reda E., Alleva E., Cirulli F., Miraglia F. Validation of the Italian version of the Apathy Evaluation Scale (AES-I) in institutionalized geriatric patients. Ann. Ist. Super. Sanita. 2016;52:249–255. doi: 10.4415/ANN_16_02_17. [DOI] [PubMed] [Google Scholar]
- 121.Crocker L.D., Heller W., Warren S.L., O’Hare A.J., Infantolino Z.P., Miller G.A. Relationships among cognition, emotion, and motivation: Implications for intervention and neuroplasticity in psychopathology. Front. Hum. Neurosci. 2013;7:261. doi: 10.3389/fnhum.2013.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kanellopoulos D., Wilkins V., Avari J., Oberlin L., Arader L., Chaplin M., Banerjee S., Alexopoulos G.S. Dimensions of Poststroke Depression and Neuropsychological Deficits in Older Adults. Am. J. Geriatr. Psychiatry. 2020;28:764–771. doi: 10.1016/j.jagp.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Beck A., Steer R., Brown G. BDI-II: Beck Depression Inventory Manual. 2nd ed. Psychological Corporation; San Antonio, TX, USA: 1996. [Google Scholar]
- 124.Hamilton M. A rating scale for depression. J. Neurol. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Montgomery S.A., Åsberg M. A New Depression Scale Designed to be Sensitive to Change. Br. J. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 126.Zung W.W.K. A Self-Rating Depression Scale. Arch. Gen. Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 127.Turner-Stokes L., Hassan N. Depression after stroke: A review of the evidence base to inform the development of an integrated care pathway. Part 1: Diagnosis, frequency and impact. Clin. Rehabil. 2002;16:231–247. doi: 10.1191/0269215502cr487oa. [DOI] [PubMed] [Google Scholar]
- 128.Andresen E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994;10:77–84. doi: 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- 129.Marin R.S., Biedrzycki R.C., Firinciogullari S. Reliability and validity of the apathy evaluation scale. Psychiatry Res. 1991;38:143–162. doi: 10.1016/0165-1781(91)90040-V. [DOI] [PubMed] [Google Scholar]
- 130.Sheikh J., Yesavage J. Geriatric depression scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health. 1986;5:165–173. [Google Scholar]
- 131.Resnick B., Zimmerman S.I., Magaziner J., Adelman A. Use of the Apathy Evaluation Scale as a Measure of Motivation in Elderly People. Rehabil. Nurs. 1998;23:141–147. doi: 10.1002/j.2048-7940.1998.tb01766.x. [DOI] [PubMed] [Google Scholar]
- 132.Graves R., Connor L.T., Nicholas M.L. Apathy and residual neurological impairment are associated with community reintegration after mild stroke. Neuropsychol. Rehabil. 2021:1–14. doi: 10.1080/09602011.2021.2019059. Epub ahead of print . [DOI] [PubMed] [Google Scholar]
- 133.Palmisano S., Fasotti L., Bertens D. Neurobehavioral Initiation and Motivation Problems After Acquired Brain Injury. Front. Neurol. 2020;11:23. doi: 10.3389/fneur.2020.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lenze E.J., Munin M.C., Quear T., Dew M.A., Rogers J.C., Begley A.E., Reynolds C.F., III The Pittsburgh Rehabilitation Participation Scale: Reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch. Phys. Med. Rehabil. 2004;85:380–384. doi: 10.1016/j.apmr.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 135.Iosa M., Galeoto G., De Bartolo D., Russo V., Ruotolo I., Spitoni G., Ciancarelli I., Tramontano M., Antonucci G., Paolucci S., et al. Italian Version of the Pittsburgh Rehabilitation Participation Scale: Psychometric Analysis of Validity and Reliability. Brain Sci. 2021;11:626. doi: 10.3390/brainsci11050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Melin J., Årestedt K. The Patient Participation in Rehabilitation Questionnaire (PPRQ): Psychometric evaluation and revision for use in neurological rehabilitation. Disabil. Rehabil. 2020;42:1454–1461. doi: 10.1080/09638288.2018.1528303. [DOI] [PubMed] [Google Scholar]
- 137.Van Brakel W.H., Anderson A.M., Mutatkar R.K., Bakirtzief Z., Nicholls P.G., Raju M.S., Das-Pattanayak R.K. The Participation Scale: Measuring a key concept in public health. Disabil. Rehabil. 2006;28:193–203. doi: 10.1080/09638280500192785. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.