Abstract
Context:
Nano-calcium hydroxide (NCH) has been proven to have several advantages over normal calcium hydroxide, supporting in its possible use as an intracanal medicament.
Aim:
The aim is to evaluate and compare calcium ion release and pH change using NCH with different vehicles as intracanal medicament.
Subjects and Methods:
Sixty freshly extracted premolars were decoronated at the cementoenamel junction level and the length was standardized. Canals were enlarged to F3 size using protaper rotary system. The samples were divided into three groups (n = 20), namely NCH + distilled water (Group 1), NCH + propylene glycol (Group 2), and NCH + chitosan (CT) (Group 3). Each sample was suspended in 6 ml of distilled water using silicone putty with only the apical third of the roots immersed. The pH and calcium ions were assessed at 24 h, 7 days, 15 days, and 30 days using a pH meter and ultraviolet spectrophotometer, respectively.
Statistical Analysis:
Comparison of mean calcium release and pH change was made using Kruskal–Wallis ANOVA with post-hoc Dunn's test. The level of significance was set at 5%.
Results:
A significant difference was seen in the calcium ion release and pH change among the three groups at 24 h, 7 days, 15 days, and 30 days.
Conclusions:
NCH mixed with propylene glycol showed alkaline pH and adequate release of calcium ions till 30 days. NCH mixed with CT exhibited a high pH at the end of 30 days. Both combinations proved their efficacy as intracanal medicaments.
Keywords: Calcium ion release, chitosan, nano-calcium hydroxide, propylene glycol
INTRODUCTION
Intracanal medicament (ICM) is recommended for various reasons when treating infected root canals. It eradicates residual bacteria after root canal preparation, reduces pulpal and periapical tissue inflammation, neutralizes tissue debris and renders canal contents inert, prevents leakage by acting as a barrier along with the temporary filling, and aids in the drying of persistently wet canals.[1] Hence, ICM is a prerequisite for obtaining a microbe-free environment before obturation of the root canal to achieve optimal healing of periapical tissues.[2,3]
Calcium hydroxide (CH) is a widely used ICM in endodontics. It has been used during many clinical procedures, including root canal cleaning, ceasing inflammatory root resorption, and promoting apexification.[4] CH kills bacteria while reducing the effectiveness of the remaining cell wall components like lipopolysaccharides by eliminating fatty acids.[5] The mode of action is directly related to its propensity to dissociate into calcium and hydroxyl ions, leading to elevated pH.[6] Since CH dissolves rapidly in an aqueous solution and releases hydroxyl ions, the pH remains high after setting. In the absence of bacterial infection, the high pH stimulates the tooth to repair itself. The vehicle by which CH is delivered plays a crucial role as it controls the rate of ionic dissociation, which causes the periapical tissues within the canal to solubilize and resorb the paste at different speeds.[7]
The vehicles can be water-soluble (saline, distilled water (DW), local anesthesia, Ringer's solution); viscous [Glycerin, Propylene glycol (PG), Polyethylene glycol (PEG)]; or oil-based (eugenol, silicone oil, olive oil, metacresylacetate, camphor).[4,8,9] The aqueous vehicle encourages solubilization, while viscous vehicles can slowly liberate ions over time. They release calcium ions (Ca) slowly over extended periods,[8] minimizing the number of replacement sessions required.[9] It has been reported that Ca ions permeate through the apex and alter the pH, facilitated by the carrier utilized.[10]
PG is a colorless liquid, dihydric alcohol with a sweet taste and a faintly pungent odor.[11] PG is less cytotoxic and has antibacterial properties that are useful in endodontic therapy compared to other vehicles for ICM.[12]
Chitosan (CT) is a polysaccharide used as a pharmaceutical excipient. It is synthesized by partially deacetylating chitin, a product of the arthropod exoskeleton. It is made up of glucosamine and N-acetyl glucosamine copolymers.[13] It has various biological properties, including hypercholesterolemic, antibacterial, wound healing, mucoadhesive, and sustained release properties.[14]
Nano-calcium hydroxide (NCH) has been recently introduced in the field of endodontics. They are gaining popularity in dentistry and medicine as antibacterial agents. Nanoparticles are microscopic particles that are less than 100 μm in size. As these materials have a larger surface-to-volume ratio and charge density, they interact more with the environment and hence have more antibacterial activity. Endodontic bacteria found in dentinal tubules are killed by calcium hydroxide nanoparticles. Previous studies have highlighted the advantages of NCH over CH, which include fewer surface alterations, better penetration into deeper layers of dentin, and superior antimicrobial activity against high pH-resistant Enterococcus fecalis.[15] Hence, they have the capability to be employed as an intracanal medication in root canal therapy.
Studies have looked at the long-term release of Calcium (Ca) ions from CH combined with various vehicles. However, in the endodontic literature, no studies compare sustained Ca ion release from NCH combined with various vehicles (DW, PG, CT). This study was thus performed to evaluate Ca ion release and pH change by combining NCH with various vehicles (DW, PG, CT).
SUBJECTS AND METHODS
Specimen selection and preparation
This in-vitro study was reviewed by the institutional ethical committee for its ethical integrity and applications (859–2019). The power of the study was 95%, the level of significance was P < 0.05, and a sample size of 60 was estimated. Freshly extracted mandibular premolars with comparable root diameter, length, and taper were obtained, cleaned mechanically using an ultrasonic scaler and kept at room temperature in normal saline. Diamond discs were used to decoronate the teeth at the cementoenamel junction under water spray and the length was set to 15 mm. Patency of the canal was achieved using a 10-k file and the working length was calculated by deducting one mm from the exit of the file at the apex.
Canal preparation
Standardized cleaning and shaping procedures were done using Protaper rotary instruments up to size F3. After each instrumentation, 2 mL of 2.5% NaOCl for 1 min was used for passive irrigation, utilizing a beveled 27G stainless steel needle positioned one mm short of the working length. After 1 min of final irrigation with 2 mL of 17% ethylene diamine tetra acetic acid solution, the canal was washed with DW (5 ml) to eliminate any precipitate. Sterile paper points were used to dry the canals. The specimens were randomly split into three groups: NCH mixed with DW (Group 1; n = 20), NCH mixed with PG (Group 2; n = 20), and NCH mixed with CT (Group 3; n = 20).
Nano-calcium hydroxide paste preparation
As per the manufacturer's instructions, 150mg of NCH powder was mixed with 0.15 ml of the different vehicles for the first two groups to form a paste. For the third group, 150 mg of NCH powder was mixed with 0.20 ml of 3%(w/v) CT solution resulting in a thick paste placed into the root canal using lentulo spirals. Hand pluggers were used for the compaction of paste into the canals. While placing the medication, sufficient care was taken to ensure that no traces of the drug adhered to the external surface. Sealing of the orifice was done using glass ionomer cement. Silicone putty was used to suspend the teeth in glass vials containing 6 ml of DW, such that only the apical third was submerged [Figure 1]. The calcium ion concentration and pH were then assessed.
Figure 1.
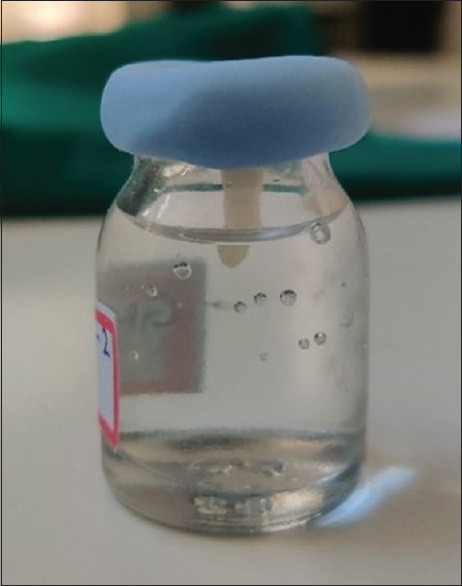
Apical third of the tooth suspended in the glass vial using silicone putty
Measurement of calcium ion concentration
One milliliters of DW from the glass vials was withdrawn periodically after 24 h, 7 days, 15 days, and 30 days from each group, each time replenishing with fresh DW. The solution was then analyzed using a ultraviolet (UV) spectrophotometer (1601 PC, Shimadzu, Japan) at 220 nm to determine the Ca ion concentration, which was then calculated using a reference calibration curve formulated with water.
pH measurement
pH change of DW was measured using a pH meter (Systronics limited, Mumbai) at intervals of 24 h, 7, 15, and 30 days. The pH change of each formulation was assessed by dropping the electrode into DW with a pH meter, swirling the solution for 5 s to equally distribute the hydroxyl ions, and measuring the pH at each time interval. The electrode was cleansed with DW and dried using sterile tissue paper between readings.
Statistical analysis
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) software version 20 (IBM SPSS corp. Released 2011). The normality of the data was checked using the Shapiro–Wilk test. Data showed non-normal distribution. A comparison of mean calcium release and pH was made using Kruskal–Wallis ANOVA with post hoc Dunns test. A value of P < 0.05 was considered statistically significant.
RESULTS
A significant difference in the mean calcium ion concentration was noted among the three groups at all the four time intervals (P < 0.001, <0.001, <0.001, and <0.001), respectively. The post-hoc test showed that group 2 had higher mean calcium ions than others at 24 h, 7, 15, and 30 days, respectively. The lowest concentration of calcium ions was seen in group 3 at 15 and 30 days [Table 1].
Table 1.
Intergroup comparison of mean calcium ion release and pH change at different time intervals
| Mean±SD | P† -value | Post-hoc test | |||
|---|---|---|---|---|---|
|
| |||||
| Group 1 | Group 2 | Group 3 | |||
| Calcium ion release | |||||
| 24 h | 9.85±0.6 | 13.62±0.88 | 11.36±0.8 | <0.001 | 2>3>1 |
| 7 days | 22.82±1.08 | 30.85±1.86 | 23.95±1.03 | <0.001 | 2>1,3 |
| 15 days | 36.12±1.56 | 53.55±1.57 | 33.45±1.61 | <0.001 | 2>1>3 |
| 30 days | 61.63±1.08 | 73.21±1.67 | 52.62±1.78 | <0.001 | 2>1>3 |
| pH change | |||||
| 24 h | 7.43±0.17 | 7.78±0.71 | 7.4±0.13 | 0.113 | - |
| 7 days | 7.71±0.53 | 7.79±0.67 | 7.86±0.61 | 0.881 | - |
| 15 days | 8.44±0.42 | 8.31±0.51 | 8.35±0.53 | 0.651 | - |
| 30 days | 10.21±0.29 | 10.23±0.18 | 10.88±0.55 | <0.001 | 3>1,2 |
SD: Standard deviation. P-value <0.05 was considered statistically significant
There was no statistically significant difference in the mean pH among the three groups at 24 h, 7, and 15 days (P = 0.113, 0.881, and 0.651), respectively. However, there was a significant difference in the mean pH at 30 days among the three groups. The post-hoc test showed that Group 3 had the highest pH, followed by Groups 2 and 1 [Table 1].
DISCUSSION
NCH, because of its smaller size and high surface area, penetrates into the deeper layers of dentin and effectively kills endodontic bacteria in the dentinal tubules.[15] NCH has also been shown to cause fewer changes in the dentin microhardness than CH when used as an intracanal medication for 4 weeks.[16] Several studies have evaluated the association of CH with various carriers.[8,9,10] Previous studies have shown the sustained release property of PG and CT when used as a carrier with CH.[10,14,17] Hence, in this study, PG and CT and DW were selected as a carrier for NCH in determining its effectiveness as an alternative intracanal medicament.
Change in pH of radicular dentin over 4 weeks has been examined previously and deemed an appropriate period for CH-based materials to provide therapeutic advantages.[18] However, some CH preparations show Ca ion release for only a shorter period. From a clinical outlook, this means that the root canal must be redressed numerous times until the intended effect is obtained, resulting in an increase in the number of appointments.[19] Therefore, drug release and pH change were compared for varying time intervals for 30 days.
This study employed human extracted teeth, consistent with a previous study.[14,17] Diffusion of NCH from the canal orifice was inhibited by submerging only apical one-third of the tooth in DW, simulating a clinical setting. Precise assessment of Ca ions release can be done using a calorimetric method, flame photometry, atomic absorption spectrophotometry, and UV spectrophotometer.[20] In the present study, an UV spectrophotometer was utilized because the analysis is quick and less expensive than other techniques.[14]
On intergroup comparison, the highest Ca ion release was seen with Group 2 at the end of 30 days. This is in accordance with the previous studies[14] and could be due to PG's hygroscopic character, which allows water absorption and provides a good, sustained release of CH for longer than a paste containing DW. Another benefit is its consistency, which enhances the paste's handling properties. It induces the most favorable release of hydroxyl and Ca ions compared to other vehicles.[21] The sudden Ca ion release by Group 1 after 7 days can be attributed to the aqueous nature of DW, which promoted a rapid ion release and should be utilized in clinical situations such as dental replantation and intense exudative cases. This characteristic of rapid release is beneficial in clinical situations requiring short-term inter-appointment disinfection.[10]
CT showed a biphasic release pattern, with an initial spurt of release, followed by a constant release over time. Due to the presence of free amino groups in CT-based delivery methods, an early burst effect is common. On mixing, the drug present on the surface of the polymer is immediately released into the surrounding media. First, swelling of the polymer takes place, which results in the release of the active ingredient and subsequent drug diffusion. Ionic interactions between CT chains influence drug release, depending on the cross-linking density determined during matrix network formation.[14,22] Prolonged release is useful in clinical conditions such as inflammatory root resorption, healing large periapical lesions, and reducing the frequency of canal re-dressing.[18,23]
All three experimental groups demonstrated a considerable rise in pH (pH >10) of the surrounding medium comparable with previous studies.[14] Group 3 revealed a high pH at the end of 30 days. Similarly, in an earlier study,[24] a high alkaline pH of 11 was observed with Chitosan-based accelerated Portland cement that used varying concentrations of CT solution. CT's increased alkalinity is due to the protonation of its amino groups, causing a rise in pH.[24]
Further studies can be conducted to evaluate the antimicrobial activity using different NCH formulations. The duration of action and the dentinal tubular penetration depth of various NCH formulations also can be investigated and compared to corroborate the efficacy of NCH as an effective intracanal medicament.
CONCLUSIONS
Within the limitations of this study, it could be concluded that NCH with PG showed alkaline pH and adequate release of calcium ions till 30 days. CT exhibited a high pH with NCH at the end of 30 days. NCH could be considered an alternate intracanal medication to calcium hydroxide.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
We would like to express our gratitude to Dr. Usha Nayak, Associate Professor, Department of Pharmaceutics, Manipal College of Pharmaceutical Sciences, Manipal for letting out the department facilities for the evaluation of calcium ion release and pH change.
REFERENCES
- 1.Chong BS, Pitt Ford TR. The role of intracanal medication in root canal treatment. Int Endod J. 1992;25:97–106. doi: 10.1111/j.1365-2591.1992.tb00743.x. [DOI] [PubMed] [Google Scholar]
- 2.Fabricius L, Dahlén G, Sundqvist G, Happonen RP, Möller AJ. Influence of residual bacteria on periapical tissue healing after chemomechanical treatment and root filling of experimentally infected monkey teeth. Eur J Oral Sci. 2006;114:278–85. doi: 10.1111/j.1600-0722.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 3.Kawashima N, Wadachi R, Suda H, Yeng T, Parashos P. Root canal medicaments. Int Dent J. 2009;59:5–11. [PubMed] [Google Scholar]
- 4.Fava LR, Saunders WP. Calcium hydroxide pastes: Classification and clinical indications. Int Endod J. 1999;32:257–82. doi: 10.1046/j.1365-2591.1999.00232.x. [DOI] [PubMed] [Google Scholar]
- 5.Safavi KE, Nichols FC. Alteration of biological properties of bacterial lipopolysaccharide by calcium hydroxide treatment. J Endod. 1994;20:127–9. doi: 10.1016/S0099-2399(06)80057-9. [DOI] [PubMed] [Google Scholar]
- 6.Tronstad L, Andreasen JO, Hasselgren G, Kristerson L, Riis I. PH changes in dental tissues after root canal filling with calcium hydroxide. J Endod. 1981;7:17–21. doi: 10.1016/S0099-2399(81)80262-2. [DOI] [PubMed] [Google Scholar]
- 7.Robert GH, Liewehr FR, Buxton TB, McPherson JC., 3rd Apical diffusion of calcium hydroxide in an in vitro model. J Endod. 2005;31:57–60. doi: 10.1097/01.don.0000134211.85578.38. [DOI] [PubMed] [Google Scholar]
- 8.Gomes BP, Ferraz CC, Vianna ME, Rosalen PL, Zaia AA, Teixeira FB, et al. In vitro antimicrobial activity of calcium hydroxide pastes and their vehicles against selected microorganisms. Braz Dent J. 2002;13:155–61. doi: 10.1590/s0103-64402002000300002. [DOI] [PubMed] [Google Scholar]
- 9.Duarte MA, Midena RZ, Zeferino MA, Vivan RR, Weckwerth PH, Dos Santos F, et al. Evaluation of pH and calcium ion release of calcium hydroxide pastes containing different substances. J Endod. 2009;35:1274–7. doi: 10.1016/j.joen.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Anthony DR, Gordon TM, del Rio CE. The effect of three vehicles on the pH of calcium hydroxide. Oral Surg Oral Med Oral Pathol. 1982;54:560–5. doi: 10.1016/0030-4220(82)90195-5. [DOI] [PubMed] [Google Scholar]
- 11.Srinivas S, Jibhkate NG, Baranwal R, Avinash A, Rathi S. Propylene glycol: A new alternative for an intracanal medicament. J Int Oral Health. 2016;8:611. [Google Scholar]
- 12.Bhat KS, Walkevar SV. Evaluation of bactericidal property of propylene glycol for its possible use in endodontics. Arogya J Health Sci. 1975;1:54–9. [Google Scholar]
- 13.Paul W, Sharma CP. Chitosan, a drug carrier for the 21st century: A review. STP J Pharma Sci. 2000;10:5–22. [Google Scholar]
- 14.Ballal NV, Shavi GV, Kumar R, Kundabala M, Bhat KS. In vitro sustained release of calcium ions and pH maintenance from different vehicles containing calcium hydroxide. J Endod. 2010;36:862–6. doi: 10.1016/j.joen.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Dianat O, Saedi S, Kazem M, Alam M. Antimicrobial activity of nanoparticle calcium hydroxide against enterococcus faecalis: An in vitro study. Iran Endod J. 2015;10:39–43. [PMC free article] [PubMed] [Google Scholar]
- 16.Naseri M, Eftekhar L, Gholami F, Atai M, Dianat O. The effect of calcium hydroxide and Nano-calcium hydroxide on microhardness and superficial chemical structure of root canal dentin: An ex vivo study. J Endod. 2019;45:1148–54. doi: 10.1016/j.joen.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Grover C, Shetty N. Evaluation of calcium ion release and change in pH on combining calcium hydroxide with different vehicles. Contemp Clin Dent. 2014;5:434–9. doi: 10.4103/0976-237X.142803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nerwich A, Figdor D, Messer HH. PH changes in root dentin over a 4-week period following root canal dressing with calcium hydroxide. J Endod. 1993;19:302–6. doi: 10.1016/s0099-2399(06)80461-9. [DOI] [PubMed] [Google Scholar]
- 19.Jain A, Bhadoria K, Hada HS. Spectrophotometric evaluation of calcium ion release from different calcium hydroxide preparations: An in-vitro study. J Oral Res. 2017;6:61–3. [Google Scholar]
- 20.Robertson WG, Marshall RW. Calcium measurements in serum and plasma – total and ionized. CRC Crit Rev Clin Lab Sci. 1979;11:271–304. doi: 10.3109/10408367909105859. [DOI] [PubMed] [Google Scholar]
- 21.Simon ST, Bhat KS, Francis R. Effect of four vehicles on the pH of calcium hydroxide and the release of calcium ion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:459–64. doi: 10.1016/s1079-2104(05)80371-3. [DOI] [PubMed] [Google Scholar]
- 22.Berger J, Reist M, Mayer JM, Felt O, Gurny R. Structure and interactions in chitosan hydrogels formed by complexation or aggregation for biomedical applications. Eur J Pharm Biopharm. 2004;57:35–52. doi: 10.1016/s0939-6411(03)00160-7. [DOI] [PubMed] [Google Scholar]
- 23.Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44:697–730. doi: 10.1111/j.1365-2591.2011.01886.x. [DOI] [PubMed] [Google Scholar]
- 24.Subhi H, Husein A, Mohamad D, Nurul AA. Physicochemical, mechanical and cytotoxicity evaluation of chitosan-based accelerated portland cement. J Mater Res Technol. 2020;9:11574–86. [Google Scholar]


