Abstract
Cancer stem cells (CSCs) have drawn much attention as important tumour-initiating cells that may also be crucial for recurrence after chemotherapy. Although the activity of CSCs in various forms of cancer is complex and yet to be fully elucidated, opportunities for therapies targeting CSCs exist. CSCs are molecularly distinct from bulk tumour cells, so they can be targeted by exploiting their signature molecular pathways. Inhibiting stemness has the potential to reduce the risk posed by CSCs by limiting or eliminating their capacity for tumorigenesis, proliferation, metastasis, and recurrence. Here, we briefly described the role of CSCs in tumour biology, the mechanisms involved in CSC therapy resistance, and the role of the gut microbiota in cancer development and treatment, to then review and discuss the current advances in the discovery of microbiota-derived natural compounds targeting CSCs. Collectively, our overview suggests that dietary intervention, toward the production of those identified microbial metabolites capable of suppressing CSC properties, is a promising approach to support standard chemotherapy.
Keywords: cancer stem cells (CSCs), drug resistance, gut microbiota, microbiota-derived metabolites, bioactive compounds, natural products
1. Introduction
Nowadays, several highly successful cancer therapies are available, with the majority of regimens combining surgery, radiotherapy, and medicine, which includes chemotherapy, targeted therapy [1], and most recently, immunotherapy [2]. The type and stage of the cancer being treated determine which techniques should be employed. One of the most important goals in cancer biology is to discover cells and signalling pathways that are essential for tumour regression, thus developing novel drugs that can abrogate the growth and metastasis of malignant tumours. Among medications, conventional cancer chemotherapy remains one of the most widely used approaches. Traditional chemotherapy is an aggressive form of cytotoxic drug therapy that destroys all rapidly proliferating cells, whether they are malignant or not. Thus, this method also destroys perfectly healthy cells. On the contrary, mechanism-based therapies, such as targeted therapy and immunotherapy, are designed to find and slow the growth of cells that possess a specific cancerous phenotype. Compared to the scatter-gun approach of chemotherapy, targeted therapy appears more sniper-like, accurately destroying its target without causing any collateral harm to otherwise healthy cells. Because targeted therapies only target cancer cells, some patients report fewer side effects than those with chemotherapy, which in turn presents many bottlenecks, including a lack of specificity, which has an impact on healthy tissues, as anticipated, but also rapid drug metabolism and both intrinsic and acquired drug resistance, all contributing to decreased efficacy [3,4]. In this scenario, understanding the molecular mechanisms of cancer and tumour cell biology represents an area of investigation that poses a unique challenge to clinical oncologists and cancer researchers. Here, after introducing CSCs and their role in cancer biology, we briefly describe the mechanisms involved in CSC therapy resistance. Next, we focus our attention on the gut microbiota and its relationship with cancer development and treatment. The main purpose of our review is to provide a comprehensive summary of the currently available literature describing microbiota-derived natural compounds targeting CSCs.
2. Role of Cancer Stem Cells in Tumour Cell Biology
CSCs describe a class of stem-like cells of tumour origin that behave similarly to normal stem cells in their ability to regulate their cell cycle by switching between a quiescent and a differentiation state. This includes key stem cell features, such as self-renewal [5] and the capability to differentiate into parental tumour cells. Moreover, CSCs participate in fundamental processes of tumour growth and progression, including cancer cell proliferation, metastatic spread, and immune evasion. According to the literature, CSCs exist in most haematological and solid tumours. A cluster of differentiation (CD)133+ CSC population was revealed in colorectal cancer (CRC) in 2007 [6,7] after CSCs were first identified in 1994 in acute myeloid leukaemia (AML) [8]. Since then, their significance in solid cancer has been thoroughly researched. To date, the advent of modern flow cytometry and cell sorting techniques has allowed for the identification of cell populations with CSC features, based on their expression of specific markers. Indeed, human CSCs were recognised in other solid tumours, including breast [9], brain [10], prostate [11,12], lung [13], and pancreatic [14,15] tumours. Notably, in non-obese diabetic/severe combined immunodeficient (NOD/SCID) mice, as few as 100 CSCs were sufficient to produce tumours [9]. Nowadays, CSCs are identified and classified according to the markers they express, including cell surface antigens, stemness-related markers (OCT4, SOX2, and NANOG), or high aldehyde dehydrogenase (ALDH) activity. To complicate the picture, CSC surface marker expression varies by tissue type and even by tumour subtype. For example, CD44+CD24−/low and ALDH+ CSCs were characterised in breast cancer [16,17], along with CD133+CD44+ in colon [18,19], brain [20], and lung [21] cancer; CD34+CD8− in leukaemia [22]; CD44+ in head and neck tumours [23]; CD90+ in liver cancer [24]; and CD44+/CD24+/ESA+ in pancreatic cancer [25]. CSCs were at first thought to make up only a small portion of a solid tumour’s overall cell population; however, according to some estimates, up to 25% of cancer cells may display CSC characteristics [26]. Regarding the genesis of CSCs, a variety of theories have been proposed. According to one theory, CSCs develop from healthy stem/progenitor cells when they undergo a specific genetic mutation or environmental change that confers to them the capacity to cause tumours. In terms of cellular characteristics, phenotype, activity, and also cell surface markers, certain CSCs exhibit similarities to typical stem/progenitor cells, thus lending credence to this notion [27]. A second explanation describing the origin of CSCs contends that they originate from healthy somatic cells that undergo genetic and/or heterotypic changes to develop stem-like properties and malignant behaviour. Emerging data showing that CSCs are resistant to standard chemotherapy and radiation treatment and are very likely to be the cause of cancer recurrence and metastasis have enhanced the clinical significance of CSCs [5,28,29].
3. Therapy-Resistant Nature of Cancer Stem Cells
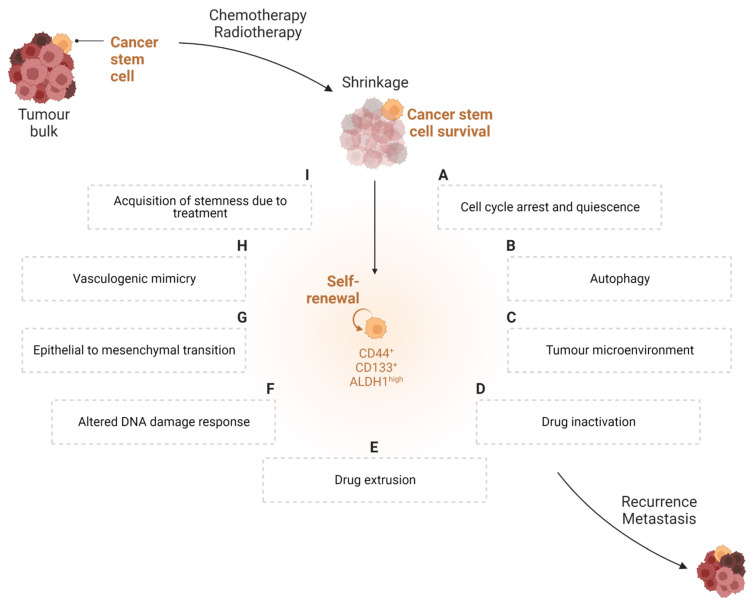
Chemoresistance, recurrence, and metastasis remain the primary causes of cancer mortality, advances in therapeutic development notwithstanding. Numerous investigations have revealed that a small subgroup of cancer cells, called CSCs, is the cause of the tumour’s recurrence. Some regulatory signalling pathways, including the Wnt/β-catenin, Sonic Hedgehog (SHH), and Notch pathways, which are important in the self-renewal process, are shared by CSCs and regular stem cells [30]. Accumulating evidence has shown that the expression of markers related to stemness is crucial for tumour maintenance and that these molecules also mediate cancer therapy resistance. Furthermore, resistant CSCs might cause metastasis at a distant site, resulting in the formation of a metastatic tumour [31]. The mechanisms through which CSCs adapt to escape cancer therapy are summarised in Figure 1 and further discussed below.
Figure 1.
Schematic representation of the different mechanisms applied by CSCs to escape cancer therapy. A small number of cancer cells, known as cancer stem cells (CSCs), have a significant role in the failure of cancer treatment. Despite chemotherapy successfully eliminating a significant amount of the tumour bulk, the main factor for tumour recurrence and metastasis is the existence of CSCs that are resistant to chemotherapy and can regenerate themselves. CSC-mediated therapy resistance appears to be attributed to different mechanisms: cell cycle arrest and quiescence (A), autophagy (B), interactions with the tumour microenvironment (C), drug inactivation (D) and extrusion (E), alteration of the DNA damage response (F), epithelial-to-mesenchymal transition (G), and vasculogenic mimicry (H). Moreover, stemness-related therapy resistance could be induced by cancer treatment itself (I).
3.1. Cell Cycle Arrest and Quiescence
Strong proof of a connection among CSCs, tumour cell plasticity, cell-cycle quiescence, and immune suppression in cancer originates from a wide range of publications. Several studies have shown that CSCs can conceal themselves from the immune system at the onset, avoiding detection during the immunosurveillance phase. Cell cycle is a multi-phased, intricate, and tightly regulated process. Cell cycle control requires the phase-specific transcription of cell cycle genes. Mutations in cell cycle genes can make healthy cells more inclined to acquire a malignant phenotype [32]. In a very elegant study, Agudo et al. [33]. demonstrated that fast-cycling cells, such as Lgr5+ stem cells detected in the stomach, ovaries, and mammary glands, experienced immune clearance. Conversely, slow-cycling stem cells, such as those in muscle and hair follicles, were resistant to just EGFP death-inducing (Jedi) T-cell eradication. Furthermore, the ability of latent stem cells to autonomously downregulate the antigen-presentation pathway via the transactivator NLRC5 is crucial for immunological escape. Notably, the process is reversible once stem cells enter the cell cycle [34]. It has been speculated that cancer cells use the characteristics of dormant stem cells to evade immune cell identification (Figure 1A). In this regard, it was recently shown that CSCs have immune-evasive properties when they enter quiescence [35]. Accordingly, in xenotransplant investigations, leukaemia CSCs were discovered to be chemotherapy-resistant and to be in the G0 (resting) phase of the cell cycle [36]. We can therefore envisage that the immunologically privileged status of CSCs is dependent on their capacity to adopt a quiescent state. Indeed, CSCs’ pharmacological resistance results from a mismatch between their relatively slow cell cycle [37] and the rapidly proliferating cancer cells that multiple chemotherapeutic treatments are designed to target.
3.2. Autophagy
Organelles, protein aggregates, and intracellular pathogens are the types of cellular cargo that are engulfed by double-membraned vesicles called autophagosomes during the evolutionarily conserved catabolic process known as autophagy, which results in their destruction and recycling after fusion with the lysosome [38]. CSCs exhibit autophagy reliance equal to that in tissue-resident stem cells (Figure 1B). For example, it was demonstrated that the secretion of interleukin (IL)-6 from CD44+/CD24low/− breast cancer cells is dependent on autophagy and necessary for CSC maintenance [39]. In addition, autophagy is induced by a wide range of cancer therapies. For example, Imatinib™, a small molecule tyrosine kinase inhibitor used to treat metastatic gastrointestinal stromal tumour (GIST), causes the induction of autophagy in GIST cells [40]. According to preclinical data, stress-induced autophagy helps CSCs survive, while blocking autophagy can help in overcoming CSC resistance [41]. In the case of Imatinib™-treated GIST cells, tumour cell apoptosis was induced by inhibiting autophagy, using the lysosomotropic drug chloroquine (CQ) [40]. Moreover, in prostate cancer, clomipramine (CMI), CQ, or metformin treatment enhanced apoptosis and dramatically reduced cell viability by blocking autophagy in enzalutamide-resistant cells, overcoming the resistance to enzalutamide, an inhibitor of the androgen receptor signalling pathway used for the treatment of metastatic castration-resistant prostate cancer [42].
3.3. Tumour Microenvironment
As per normal stem cells, CSCs are frequently found in anatomically separate locations, hidden niches within the tumour microenvironment (TME) that provide a protective physical and chemical environment from direct contact with drugs and the host immune system. In tumour niches, intricate interactions between cells and the extracellular matrix (ECM) create a complex environment that determines stem cell resilience and the preservation of stemness. ECM remodelling also impacts CSC survival (Figure 1C). On one hand, a physical barrier created by enhanced ECM stiffness can protect CSCs from chemotherapeutic drugs. On the other hand, ECM degradation by matrix metalloproteinases (MMPs) can allow for the release of cytokines and growth factors that enhance tumour cell invasion, metastasis, and angiogenesis [43]. Moreover, solid tumours are commonly affected by hypoxia. The capacity of the pre-existing blood vessels to meet the oxygen requirement is frequently exceeded in cases of uncontrolled cell multiplication [44]. When under hypoxic and therapeutic stress, CSCs use a variety of signalling pathways that are modulated by hypoxia-inducible factor (HIF) signalling to modulate their stemness. HIF-induced gene products include epithelial-to-mesenchymal transition (EMT) programmers, glycolysis-associated molecules, drug resistance-associated molecules, miRNAs, and VEGF [45]. Therefore, by maintaining CSCs in their undifferentiated stem cell state, which enables self-renewal and the accumulation of epigenetic and genetic mutations, hypoxic environments may promote the formation of malignant clones [46]. In addition, the TME has been shown to have an acidic extracellular pH, which is a consequence of lactate accumulation via increased anaerobic glycolysis in hypoxic conditions [47]. In that respect, it was recently demonstrated that extracellular acidosis may cause cancer cells to develop stem-like characteristics and aid in the proliferation of the CSC subpopulation [48]. Lastly, tumour cells, inflammatory cells, cancer-associated fibroblasts, and CSCs are just a few of the cell types that belong to the specialised microenvironment known as the perivascular niche, which is found right next to blood vessels. Here, the stemness features of CSCs, such as their capacity for self-renewal, multipotency, and tumorigenic potential, are maintained by molecular interactions among various cell types [49].
3.4. Drug Inactivation
CSC chemoresistance has also been linked to intracellular drug inactivation (Figure 1D). A class of detoxifying enzymes known as ALDHs is frequently upregulated in cancer cells leading to treatment resistance. ALDHs are overexpressed in cancer cell clusters with stem-like characteristics, where they contribute to the defence of cancer cells by converting harmful aldehydes into more soluble and less reactive carboxylic acids [50]. For example, ALDH is crucial for contrasting the effects of diverse chemotherapeutic agents, such as cyclophosphamide, irinotecan, temozolomide, paclitaxel, doxorubicin (DOX), and epirubicin [51,52,53,54,55]. In addition, ALDH has been a widely used marker for CSC identification. Increased metabolic activity, along with conventional anticancer drugs, leads to aldehyde generation, which results in DNA double-strand breaks (DSBs) via reactive oxygen species (ROS) and lipid peroxidation. Thus, the overexpression of ALDH is essential for CSC survival. Moreover, it can inhibit immunogenic cell death (ICD) and cause the activation and growth of immunosuppressive regulatory T cells (Tregs), thus influencing immune cell activity in the TME [50]. Additionally, in NOD/SCID mice, acute myeloid leukemic cells that possess increased ALDH activity seem to have more capacity for engraftment compared to their ALDH-negative counterparts [56]. Moreover, the epigenetic inhibition of thymidine phosphorylase has been observed in CSCs, resulting in the therapeutically inefficient transformation of active 5-fluorouracil (5-FU) and methotrexate [55,57,58]. Finally, CSCs use thiol glutathione to inactivate platinum [59].
3.5. Drug Extrusion
One of the primary defence mechanisms for CSCs is the transcription of multifunctional efflux transporters from the ATP-binding cassette (ABC) gene family (Figure 1E) [60]. By using the energy of ATP hydrolysis to adenosine diphosphate (ADP) [61], these transporters actively efflux peptides, inorganic anions, amino acids, polysaccharides, proteins, vitamins, and metallic ions [62]. Intrinsic CSC-chemoresistance has been associated with their ability to express proteins of the family of ABC transporters, which results in drug extrusion and loss of effectiveness. Increased ABC transporter expression, including ABCB1 (P-glycoprotein/MDR1), ABCC1 (MRP1), and ABCG2 (BCRP), is one of the most well-established strategies for cancer cells to acquire multidrug resistance (MDR) [63]. A plethora of drugs that modulate MDR-ABC transporters have been developed during the past years, and some of them have also demonstrated significant efficacy in clinical trials [63]. However, one must bear in mind that in addition to promoting the growth of tumours, stem cell-driven tissue repopulation also promotes the growth of adult-specific normal tissues, such as the bone marrow, digestive tract, and hair follicles; thus, the complete inhibition of ABC transporters could have severe drawbacks.
3.6. Altered DNA Damage Response (DDR)
A large number of chemotherapy treatments, including platinum-based drugs and radiation, kill cancer cells by causing DNA damage. Studies have demonstrated that CSCs are incredibly effective in repairing DNA damage (Figure 1F) [64]. CSCs’ resistance to DNA-damaging therapies is thought to be caused by this enhanced DNA damage response (DDR). DDR is an extremely intricate network made up of numerous pathways, each of which exhibits cross-talk both within the network and with other signalling pathways [65]. When compared to non-stem tumour cells, CSCs have a higher capability for DNA repair either through increased DNA repair pathways or through delayed cell-cycle progression [66]. The MRE11–RAD50–NBS1 (MRN) protein complex, a major sensor of DNA double-strand breaks, is expressed in both normal and cancerous cells, as well as CSCs. However, the MRN function is improved in CSCs through interactions with the CSC-related molecules Notch1, ALDH1A1, CD44, SHH, and BMI1, in contrast to that in non-stem tumour cells [67], or through CD171, which boosts CSCs’ radioresistance and selectively triggers the DNA damage checkpoint [68]. The resting activation status of checkpoint kinases could serve as a crucial defence mechanism for CSCs against genotoxic chemicals when coupled with the induction of DNA repair. Not unexpectedly, several DDR-inhibitory drugs are currently undergoing pre-clinical and clinical testing [66]. In addition, stem cells regulate self-renewal and differentiation via differential configurations of the chromatin structure; thus, it is expected that histone changes and chromatin remodelling following DNA damage differ between stem cells and developed cells. In recent years, it has been evident that chromatin’s epigenetic dysregulation plays a significant role in CSCs development and frequently plays a crucial part in CSCs’ self-renewal throughout tumour growth [69].
3.7. Epithelial-to-Mesenchymal Transition (EMT)
Several fundamental features of cellular physiology undergo modifications as a result of the epithelial-to-mesenchymal transition (EMT) program, including alterations to cell morphology, which are related to changes in the cytoskeletal organisation; the dissolution of epithelial cell-cell junctions; loss of apical-basal polarity and concomitant gain of front-rear polarity; acquisition of the ability to breakdown and reorganise the ECM, thus enhancing motility and allowing cell invasion; and alterations to the expression patterns of at least 400 different genes [70]. The relationship between the EMT program and the CSC state raises the possibility that non-CSCs can become CSCs by enacting this program (Figure 1G) [71,72]. Indeed, EMT has been also linked to chemoresistance [73,74]. Worthy of note, an EMT-associated gene-expression signature has been strongly linked with treatment resistance, based on examinations of the relationships between the clinical outcomes of individuals and the gene-expression profiles of the associated tumour samples [75,76]. Moreover, by activating the EMT program, cancer cells can form metastatic colonies [74,77]. More specifically, according to recent studies, cells undergoing partial EMT may exhibit hybrid E/M phenotypes, possess more stem cell-like features, and exhibit more resistance to drugs than cells undergoing complete EMT. Additionally, partial EMT facilitates collective cell movement as clusters of circulating tumour cells or emboli, enhancing cancer cells’ capacity for metastasis and tumour genesis at the secondary regions [78].
3.8. Vasculogenic Mimicry
There is a unanimous understanding that solid tumours require a sufficient blood supply to grow. The term vasculogenic mimicry (VM), first coined by Maniotis [79], describes the ability of aggressive cancer cells to form de novo perfusable, matrix-rich, vasculogenic-like networks in a way that differs from traditional tumour angiogenesis in that it does not rely on endothelial cells. These new patterns of tumour microcirculation assist in perfusing rapidly growing tumours, removing fluid from leaky arteries, and/or integrating with the body’s endothelial-lined normal vessels [80]. The link between VM and poor clinical outcomes in patient malignancies suggests that VM confers a survival advantage to the aggressive tumour cell phenotype [81,82]. Additionally, preclinical pharmacological studies have shown that VM is connected to anticancer therapy resistance [83]. A significant amount of data suggests that CSCs aid in the development of VM (Figure 1H) [84]. The VM phenotype of tumour cells has a molecular signature that includes upregulated expression of genes related to embryonic progenitors, endothelial cells, vessel formation, matrix remodelling, and coagulation inhibitors, as well as downregulated expression of genes primarily related to lineage-specific phenotype markers [80,85].
3.9. Acquisition of Stemness Due to Treatment
It has been shown that chemotherapy and radiation both foster CSC traits in non-stem cancer cells and might even cause non-stem cancer cells to become CSCs [86,87] (Figure 1I); thus, the issue of CSCs not responding to conventional cancer treatments goes beyond the simple inability of these treatments to eradicate CSCs. The plasticity of cancer cells enables the transient acquisition of stemness-related traits. After receiving carboplatin treatment, hepatocellular carcinoma cells developed stem-like characteristics, including the ability to self-renew and the expression of stemness-related genes (SOX2 and OCT3/4), which demonstrated the potential for chemotherapy to generate stemness [88]. Moreover, after being exposed to the chemotherapeutic drug 5-FU, human gastric cancer cell lines demonstrated resistance to 5-FU, as well as characteristics of stemness, such as tumorigenicity and the ability to self-renew [89].
Despite chemotherapy substantially eliminating a large portion of the tumour volume, there cannot be a noticeable clinical improvement if CSCs have not been eradicated to provide long-term disease-free survival. Therefore, CSCs are thought to be a significant target for the development of new anticancer drugs, being that CSC-focused therapy is a key driver for any effective anticancer strategy. In addition to synthetic drugs targeting CSC pathways (reviewed in [30]), dietary components, mostly (poly)phenolic compounds, have shown the ability to inhibit tumour progression [90] and angiogenesis [91]. Nearly all of these naturally occurring phytochemicals with chemopreventive activities also have antioxidant and anti-inflammatory effects. Interestingly, several mechanisms involved in the anticancer effects of dietary phytochemicals target pathways involved in CSC stemness maintenance [92]. Of note, human-ingested nutrients can be transformed by the gut microbiota into useful microbial compounds that closely link diet to cancer [93]. Indeed, the microbiota-derived metabolome has the potential to encourage or prevent carcinogenesis in organs distant from the gut. An emerging field in anticancer research examines the intricate interactions between particular gut microbial metabolites and the advancement or inhibition of cancer cell proliferation [94].
4. Role of the Gut Microbiota in Cancer
The gut microbiota comprises a multitude of microorganisms, mainly bacteria across over 500 species, of which the number reaches 1013–1014, similar to the number of cells in an adult human [95,96]. The majority of them (about 90%) is represented by two bacterial phyla, the Gram-positive Firmicutes (Bacillus spp., Lactobacillus spp., and Clostridium spp.) and the Gram-negative Bacteroidetes (Bacteroides spp. and Prevotella spp.) [97,98]. In their entirety, gut bacteria have several functions, including food fermentation, vitamin production, protection against pathogens, and immune response stimulation; thus, the intestinal microbial balance is highly relevant to human health [99]. It has been established that the breakdown of the host’s and gut microbiota’s symbiotic relationship can facilitate the onset of numerous disorders, including autoimmune disease [100,101] and cancer [102]. In this scenario, the molecular basis of various long-established epidemiological relationships between certain bacteria and cancer are presently being studied [103]. For instance, the correlation between Helicobacter pylori and the risk of the development and progression of gastric cancer, but also the case of Fusobacterium nucleatum, of which the role in the setting of CRC has been extensively studied [104,105,106,107,108,109,110]. Bacterial infections were associated with cancer stemness in both cases. In the former case, Bessède et al. observed that following H. pylori infection, gastric epithelial cells overexpressed CD44 and acquired CSC features, while in the latter case, Cavallucci et al. revealed that F. nucleatum can contribute to the microbiota-driven colorectal carcinogenesis by directly stimulating colorectal CSCs [111,112]. Additionally, Ha and colleagues provide evidence that EMT and cancer stemness acquisition are induced in oral cancer cells by prolonged infection with Porphyromonas gingivalis [113].
Moreover, there have been documented indirect effects of the gut microbiota on the growth of tumours in tissues outside of the gastrointestinal tract [110]. It is fascinating to note that the gut microbiota, by releasing bacterial products that can enter the bloodstream, can practically influence all host organs and systems and eventually affect cancer progression. This expanding knowledge points out that intestinal dysbiosis may cause carcinogenesis in localised gastric and intestinal cancers and tumours located in distant regions of the body [103,110]. For instance, lipopolysaccharide (LPS), a component of the Gram-negative bacterial cell wall, which is recognised by Toll-like Receptor 4 (TLR4), is one of the molecules derived from gut bacteria that has been demonstrated to promote cancer [110]. In a model of chronic injury-induced liver cancer, LPS-induced TLR4 stimulation increased the expression of the hepatomitogen epiregulin in stellate cells, which had a pro-tumorigenic effect [114]. Additionally, deoxycholic acid (DCA), a metabolite produced by gut bacteria, has also been linked to an increased risk of developing hepatocellular carcinoma when its level is increased due to dietary- or hereditary obesity-induced shifts in the gut microbiota composition [115].
On the other side of the coin, recent studies have observed that the gut microbiota can also exert immunomodulatory and anti-tumoral effects in cancers. For instance, in a rat model, the probiotic bacteria Lactobacillus acidophilus have been found to decrease the occurrence of CRC [116]. Moreover, exopolysaccharides from Lactobacillus spp. were able to slow down cell division in a time-dependent fashion and trigger apoptosis by upregulating the expression of Bax and caspase 3 and 9, while downregulating Bcl-2 and survivin, in a colon cancer cell line (HT-29) [117]. Abdelghani et al. provided a comprehensive list of anti-cancer compounds derived from microbial metabolism and their anticancer activities, which range from apoptotic, anti-proliferative, and cytotoxic activity to chemosensitisation to 5-FU [118].
Along with the investigation of the links between the gut microbiota and cancer, the microbiota of tumours themselves has received some consideration. Interestingly, more research into the microbiota revealed that it was also present within tumour tissues that were previously assumed to be sterile [119]. Furthermore, the local microenvironment and the tumour immunological context seem to interact with the tumour-associated microbiota, or microbial communities found in the tumour or inside its body compartment, ultimately affecting cancer growth and the response to therapy [120]. The intratumoral microbial community further complicates the cancer–microbiota–immune axis, which significantly impacts T-cell-mediated killing and anti-tumour immune surveillance [121]. Recently, Zhou et al. reviewed the hitherto neglected but significant impacts of the small molecules derived from tumour microbiota metabolism on the TME and their essential roles in cancer development [122]. Not only that, numerous instances of the microbiota altering drug metabolism and interfering with immunotherapy have been reported [123,124,125,126], and it is expected that research in this area will continue.
From the perspective of “therapeutic microbiology”, the host’s health status can be improved through a variety of approaches: (a) by introducing living, beneficial bacteria (known as probiotics), influencing the microbial composition (probiotics) [127]; (b) providing non-digestible substances, such oligofructose, oligosaccharides, inulin, raffinose, and stachyose (known as prebiotics), which are fermented by endogenous colonised probiotics in the large intestine (colon), promoting the establishment of beneficial microbiota [128]; (c) administering microbial metabolites with low molecular weights (<50, 50–100, and <100 kDa) that have positive effects on health (postbiotics) [129,130]. A significant number of published studies that discuss the capability of postbiotics to regulate different cellular processes and metabolic pathways have been published in the literature and reviewed elsewhere [130,131]. However, the microbiota remains an untapped avenue for finding small-molecule drugs for cancer treatment.
5. Microbiota-Derived Metabolites with Activity towards CSCs
Diet and environmental exposures, as well as lifestyle, have a major role in influencing the human gut microbiota composition and its metabolic activity, which can have an impact on health [132,133,134]. CSCs are very dependent on their surroundings for their energy supply; thus, nutrients play a pivotal role in modulating CSC growth or stemness. Over the past few decades, numerous studies have attempted to clarify the processes governing CSCs’ response to diet [135]. The anaerobic microbial population ferments undigested dietary components and host products, primarily mucin, to produce a remarkably wide range of metabolites that reflect both the chemical diversity of the dietary substrates and the microbiota’s unique metabolism [136]. As outlined above, microbiota metabolites, defined as intermediate end products of microbial metabolism, are key players in the microbiota–cancer relationship. These metabolites can be categorised based on two different parameters: origin (intracellular or extracellular) and function (primary or secondary), respectively. While secondary metabolites are produced close to the stationary phase of growth and are not essential for growth, reproduction, or development, primary metabolites are required for the optimal growth of bacteria. Several studies were conducted to assess the health-promoting effects of microbial products; in those cases, researchers described them as ‘biogenic’, ‘cell-free supernatant’, ‘abiotic’, ‘metabiotic’, ‘paraprobiotic’, ‘ghost probiotics’, ‘pseudoprobiotic’, ‘supernatant’, etc. [137]. Only in 2013, the term “postbiotics” was created to describe soluble components secreted by living bacteria or released following bacterial lysis, including enzymes, peptides, teichoic acids, muropeptides derived from peptidoglycan, polysaccharides, cell surface proteins, and organic acids [129]. This definition also gained support from further reports [138,139]. A detailed and exhaustive description of the range of metabolites produced by gut microbial metabolic activity and their roles in health and diseases is beyond the scope of this review and can be found elsewhere [140]. Here, we focus exclusively on the documented effects of microbiota-derived metabolites that specifically target CSCs and their features.
Traditional approaches to identifying novel bioactive natural products include extraction, fractionation or isolation, chemical characterisation, and, ultimately, an assessment of the potential beneficial effect through the execution of biological assays [141]. In this connection, cell-free supernatant (CFS), a solution that contains metabolites produced as a result of microbial growth, represents an invaluable metabolite-rich source. For instance, the antioxidant, antimicrobial, and anticancer properties of CFS have been demonstrated [142,143,144]. In 2016, An and Ha showed that the expression of particular CSC markers, CD44, CD133, CD166, and ALDH1, can be inhibited by Lactobacillus plantarum (LP) supernatant. Besides that, combined treatment with LP supernatant and 5-FU: (1) prevented CRCs from surviving and caused cell death by inducing caspase-3 activity; (2) prompted an antitumor mechanism by inactivating the Wnt/β-catenin signalling pathway in chemoresistant CRC cells; and (3) decreased the formation and volume of colonospheres [145]. Later in 2020, the same authors also demonstrated that in 5-FU-resistant CRC cells (HCT-116/5FUR), Lactobacillus plantarum-derived metabolites (LDMs) boost drug sensitivity and have antimetastatic effects as well. By reducing the expression of claudin-1 (CLDN-1), co-treatment of HCT-116/5FUR with LDMs and 5-FU decreased chemoresistance and metastatic activity. Their findings suggested that targeting 5-FU-resistant cells with LDMs and 5-FU cotreatments can be effective [146]. Moreover, Maghsood et al. treated human colon cancer stem-like cells enriched from an E-cadherin shRNA-engineered HT-29 cell line (HT29-ShE) with size-fractionated Lactobacillus reuteri CFS. Their results showed that crude and >50 kDa fractions of CFS significantly decreased the expression of COX-2, a crucial factor in the maintenance and function of CSCs. In addition, they demonstrated that colon cancer stem-like cell apoptosis and cell proliferation were both suppressed by L. reuteri CFS [147].
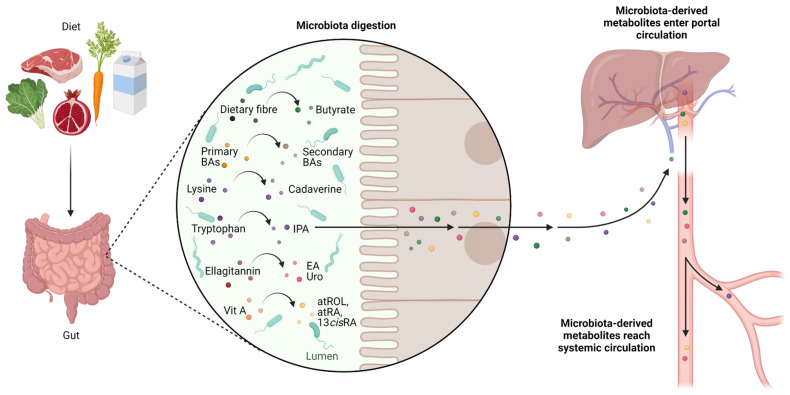
Diet plays a major role in cancer aetiology and prevention; thus, a healthy diet can be a game-changer factor [148,149,150,151,152]. Moreover, food is a significant source of substrates for the production of microbial metabolites. Amongst the vastness of microbiota-derived metabolites, some have been identified as potential CSC-targeting molecules (Figure 2).
Figure 2.
Schematic representation of the metabolites produced via microbiota digestion of dietary compounds that have the potential to target CSCs. The gut microbiota plays a role in digestion by metabolising indigestible macronutrients. The host’s metabolic capability is increased by the large enzymatic repertoire of the microbial population, which integrates the function of mammalian enzymes and allows the host to metabolise a variety of food substrates. Numerous bacterial metabolites are produced by the intestinal microbiota’s metabolic activities toward the available substrates and may accumulate in the lumen. Microbiota-derived metabolites possess enhanced or even different bioactivities compared to their parental compounds. Moreover, they can access circulation and potentially diffuse systemically. Specific products of microbial digestion, highlighted in the zoomed callout, have been found to target CSC features. BAs, biliary acids; IPA, indolepropionic acid; EA, ellagic acid; Uro, urolithins; atROL, all-trans-retinol; atRA, all-trans retinoic acid; 13cisRA, 13-cis-retinoic acid.
5.1. Butyrate
Non-digestible carbohydrates, including resistant starch, non-starch polysaccharides, and certain soluble oligosaccharides, reach the large intestine without undergoing any digestion, because of the upper intestine tract lacks certain food-digesting enzymes [153,154]. Short-chain fatty acids (SCFAs) and gases are produced through the anaerobic degradation of such non-digestible fibres by gut microorganisms. SCFAs are aliphatic carbon-based acids, with acetate (C2), propionate (C3), and butyrate (C4) being the most abundant [155]. Several studies have found a link between a high-fibre diet and a lower risk of colon cancer [156,157,158]; this drove scientists toward the investigation of SCFA’s role in carcinogenesis prevention. However, when studying butyrate, researchers faced a contradictory effect: if butyrate effectively inhibited the proliferation of undifferentiated, highly proliferative adenocarcinoma cells while promoting differentiation and death, butyrate treatment did not affect the normal proliferation and regeneration of the injured epithelium in healthy cells, differentiated cultures, or in vivo experiments [159]. This phenomenon was dubbed “the butyrate paradox” [160,161,162]. Later, a possible explanation was suggested by the disclosure of the butyrate molecular mechanism which comprises the following: (a) activation of the G protein-coupled receptor 109a (GPR109a)–AKT signalling pathway, which leads to the remarkable inhibition of glucose metabolism and DNA synthesis in CRC cells, via reducing the amount of membrane G6PD and GLUT1 [163]; (b) the inhibition of AKT/ERK signalling in a histone deacetylase (HDAC)-dependent manner [164]. In malignant colonocytes, where glycolytic metabolism prevails over oxidative phosphorylation, butyrate accumulates and functions as an HDAC inhibitor, slowing the cell cycle progression through altered gene expression [165]. Thus, distinct metabolic pathways for cellular energy in differentiated and undifferentiated colonocytes are likely to be responsible for ‘the butyrate paradox’ [166]. During the coevolution of the microbiota with its hosts, mammalian crypt architecture has been developed to protect stem/progenitor cell proliferation from the potentially harmful effect of microbially derived butyrate; differentiated colonocytes establish a metabolic barrier that uses butyrate to produce a butyrate gradient [167]. Interestingly, butyrate, but not propionate or acetate, had a significant inhibitory effect on stem cell proliferation. This may be the reason why colonocytes, to protect intestinal stem cells, preferentially break down butyrate over the other SCFAs propionate and acetate, which are also present in high concentrations in the colon [167]. According to the mentioned theories, Lee et al. found out that metformin-butyrate (MFB), a new metformin derivative, showed more effective targeting of the CD44+/high/CD24−/low CSC-like (undifferentiated) population in breast cancer in vitro and in vivo and the inhibition of mammosphere formation, compared to that with metformin [168]. Of note, when butyrate and 5-FU were administered together, the chemotherapeutic effectiveness of 5-FU on CRC cells increased, suggesting a role of butyrate in sensitising CRC cells to chemotherapy [163]. Moreover, in 3D-cultured organoids derived from CRC patients, when compared to that with the administration of radiation alone, butyrate dramatically increased radiation’s ability to cause cell death and improve therapeutic effects [169].
5.2. Secondary Biliary Acids
Dietary fatty acids may increase the ability of intestinal stem cells and progenitor cells to self-renew, as well as their capability to initiate tumours [170]. Bile acids are crucial signalling molecules that aid in the digestion and absorption of dietary lipids by acting as emulsifiers [171]. Cholic acid and chenodeoxycholic acid, the two primary biliary acids (BAs), are produced from cholesterol via a series of enzymatic processes that occur mostly in the liver. After being synthesised, these BAs are conjugated with glycine or taurine and subsequently secreted and stored in the gallbladder. Less than 5% of the BA pool enters the colon each day in humans due to an active transport mechanism that predominantly recycles BAs in the terminal ileum. The gastrointestinal microbiota metabolises BAs that enter the colon, converting primary BAs into secondary BAs, deoxycholic acid (DOC or DCA), and lithocholic acid (LCA). Hence, the circulating BA pool comprises approximately 30 to 40% of cholic acid and chenodeoxycholic acid, 20 to 30% of DOC, and less than 5% of LCA (in the conjugated form when it leaves the gallbladder and subsequently de-conjugated after it enters the colon via the action of bacterial enzymes) [172]. Secondary BAs are potent signal molecules that regulate a variety of processes (both physiological and pathological), through the modulation of several signalling pathways. Gut dysbiosis can alter the homeostatic levels of primary and secondary bile acid pools and produce distinct pathophysiological bile acid profiles [173]. Moreover, the gut microbiota–bile acid axis can control immune cells to indirectly promote tumours. Secondary BAs can inhibit the function of anti-tumour immune cells, such as macrophages, dendritic cells, B cells, and natural killer (NK) cells, while enhancing the function of Tregs, which are known to encourage the development of immunosuppressive microenvironments and the growth of tumours [174]. According to Bayerdorffer et al., there is a positive association between the colon-derived unconjugated fraction of DCA and colorectal adenoma formation, which are the precursors of CRC. The finding of this connection provided evidence in favour of the theory that DCA has a detrimental impact on colon cancer development [175]. Later, the mechanisms through which secondary BAs control carcinogenesis were described by Farhana et al. [176]. They discovered that the unconjugated secondary bile acids, notably DCA and LCA, alter muscarinic acetylcholine receptor M3 (M3R) and Wnt/β-catenin signalling promoting cancer stemness in colonic epithelial cells. Moreover, according to another study, secondary BAs can encourage the development of CSCs from both cancer and non-cancerous cells [174]. Farnesoid X receptor (FXR) is the nuclear receptor responsible for the negative feedback control of bile acid synthesis in the ileum and liver. Besides this role, FXR is also a crucial regulator of the proliferation of intestinal stem cells. In 2019, Fu et al. demonstrated that DCA and tauro-β-muricholic acid (T-βMCA) antagonise intestinal FXR, functioning as strong promoters of CSC proliferation able to induce DNA damage [177]. In their study, the authors also suggest that FXR activation could potentially impede tumour progression. They used the FXR agonist drug Fexaramine D to prove their theory, showing that when intestinal FXR is specifically activated, adenomas and adenocarcinomas in treated mice develop more slowly. A few years earlier, another research group identified two bacterial strains capable of directly modulating the activation of intestinal FXR [178]. They demonstrated that Bacteroides dorei and Eubacterium limosum cell-free supernatants trigger FXR activity and the expression of FXR-dependent genes in in vitro cell-based reporter assays and diet-induced obese (DIO) mice. Taken together, these results suggest that those two bacterial strains could have a beneficial role as probiotics, especially in those cases in which the (high-fat) diet is responsible for an imbalance in the BA pool that could favour CRC onset. A recent report suggests that in the presence of metastatic lesions, a healthy diet and/or proper pharmacological intervention aimed at re-establishing physiological bile acid levels could reduce cancer cell invasion, migration, and adhesion [173].
5.3. Cadaverine and Indolepropionic Acid
Lysine decarboxylase (LDC), a peculiar microbial enzyme, catalyses the decarboxylation of lysine to produce the bacterial metabolite cadaverine. Although cadaverine can also be produced by human cells, it appears that bacterial cadaverine production predominates over human biosynthesis [179]. Kovács et al. administered cadaverine in breast cancer cell lines within the standard range for serum (100–800 nM) and found that cadaverine exposure prevented mesenchymal-to-epithelial transition, inhibited invasion, and decreased mitochondrial oxidation, all hallmarks of stemness. Moreover, smaller and lower-grade primary tumours, together with reduced metastasis, were generated in Balb/c female mice transplanted with 4T1 breast cancer cells and treated with cadaverine [179].
L-tryptophan (Trp) is one of the nine essential amino acids for humans, and therefore, it must be introduced with the diet. Trp and other amino acids are released from dietary and endogenous luminal protein by bacterial proteases and peptidases. Three rate-limiting enzymes convert the Trp into kynurenine (Kyn): liver tryptophan-2,3-dioxygenase (TDO) and peripheral tissue indoleamine 2,3-dioxygenase 1/2 (IDO1/IDO2) [180]. Through the action of the bacterial enzyme tryptophanase, the intestinal microbiota mostly converts Trp into indole [181]. For human health, Trp metabolism through the Kyn pathway and gut microbial metabolism to indolic compounds is essential. For instance, breast cancer and breast cancer survival are strongly correlated with Trp and indole metabolism. In this regard, tumour TDO/IDO overexpression is a marker of poor prognosis [182,183]. Indeed, patients with breast cancer benefit from indole derivatives in terms of survival; of note, the levels of indole derivatives decrease with disease progression [184]. Reduced activity of the indolic pathway was seen in colon cancer, which also exhibits alterations in microbial indole synthesis [185]. As per Kovács et al., Sári and colleagues also employed the Aldefluor Stem Cell kit to measure the impact of treatment with indolepropionic acid (IPA), a bacterial Trp metabolite, on ALDH activity in 4T1 cells. What they discovered was a reduction in the percentage of aldehyde dehydrogenase-positive cells together with induced mesenchymal-to-epithelial transition (MET) in IPA-treated cells [184].
5.4. Ellagic Acid and Urolithins
The health-promoting potential of plant extracts and plant-derived secondary metabolites is widely recognised [186,187,188]. Numerous beneficial effects of polyphenols on human health, such as antioxidant [189,190,191,192,193], anti-inflammatory [194,195,196], immunomodulatory [197,198,199], cardioprotective [200,201,202], neuroprotective [203,204,205], anti-carcinogenic [206,207,208], and prebiotic properties [209], have been reported. Thanks to the plethora of chemical structures they exhibit, natural anticancer compounds may act as cytotoxic agents [210,211,212], anti-mitotic agents [213], angiogenesis inhibitors [214,215], topoisomerase inhibitors [216], apoptosis inducers [217] and cancer invasion [218], migration [219] and proliferation inhibitors [220,221,222]. The identification of plant-derived secondary metabolites that could target CSCs’ peculiar signalling has received much attention in current anticancer drug discovery approaches [223,224,225,226,227,228,229,230,231,232,233,234,235,236,237]. Very recently, a growing understanding of the impact of secondary polyphenol metabolites derived from gut microbial metabolism in the context of carcinogenesis has emerged. It is worth noting that the portion of dietary polyphenol that is absorbed at the small intestine level and enters the blood circulation is estimated at around 10%. Hence, many ingested polyphenols reach the large intestine, where intestinal bacteria convert them to phenolic acids [238].
Lactobacillus rhamnosus, an obligatory anaerobic homofermentative lactic acid producer, has been identified as predominant bacteria in the human gut [239]. The fermentation of polyphenol-rich dried black chokeberry (Aronia melanocarpa) powder using L. rhamnosus led Choi et al. to the isolation of a CSC inhibitor of which the structure was established as 1,2-dihydroxybenzene, also known as catechol [240]. In particular, they found that catechol inhibits proliferation and mammosphere formation in the human breast cancer cell lines MCF-7 and MDA-MB-231. Moreover, the percentage of breast cancer cells expressing CD44high/CD24low, as well as the protein and transcript levels of signal transducer and activator of transcription 3 (STAT3) and IL-6, are reduced by catechol treatment. Finally, catechol was found to reduce the expression of self-renewal genes, such as NANOG, SOX2, and OCT4, in CSCs, hence reducing their stemness and proliferative capacity.
Urolithins are secondary polyphenol metabolites generated via the activity of gut bacteria on ellagitannins (ET) and ellagic acid-rich foods, such as pomegranates, raspberries, strawberries, and walnuts [241]. The acid hydrolysis of ellagitannins releases free ellagic acid [242], which is further processed by gut microbiota that converts ellagic acid into urolithins [238]. The composition of a person’s gut microbiota affects how ellagitannins and ellagic acid are metabolised into urolithins; accordingly, individuals can be categorised into three groups of polyphenol-metabolising phenotypes called metabotypes [243]. Núñez-Sánchez and colleagues evaluated the effects of mixed ET-derived colonic metabolites on colon CSC-associated markers [244]. The authors investigated the ability of two separate mixtures of compounds—ET metabolites, ellagic acid (EA), and the gut microbiota-derived urolithins (Uro)—that, in proportion and concentration, mimic those detected in vivo in individuals with metabotype-A or metabotype-B. According to their study, the mixture resembling the metabotype-A that contains mostly Uro-A (85% Uro-A, 10% Uro-C, 5% EA) was more successful at suppressing CSCs’ molecular (ALDH activity) and phenotypic (number and size of colonospheres) traits, whereas the mixture mimicking the metabotype-B containing less Uro-A but IsoUro-A and Uro-B (30% Uro-A, 50% IsoUro-A, 10% Uro-B, 5% Uro-C, 5% EA) seemed to have some effects on colonosphere size and number, but not on ALDH activity levels. Uro-A, the predominant metabolite in the metabotype-A mixture, may be the main factor causing the discrepancies seen between the two mixtures. Interestingly, González-Sarrías et al. also reported that Uro-A is a substrate of drug efflux transporter breast cancer resistance protein (ABCG2/BCRP), highlighting the role of Uro-A in targeting CSCs [245]. In addition, the finding that the anticancer activity of 5-FU can be enhanced by Uro-A in human colon cancer cells supports the hypothesis that using phytochemicals in combination with traditional cytotoxic drugs to target CSCs may be a new cancer treatment approach [246].
5.5. Retinoids
Diet is the primary source of vitamin A since it cannot be synthesised by animal tissue and has to be introduced with food. Retinoids (including vitamin A, all-trans retinoic acid, and related signalling molecules) were shown to promote the differentiation of diverse stem cell types [247]. Retinoic acid (RA), a well-known vitamin A metabolite, regulates the fate of neighbouring cells. The availability of vitamin A (retinol), the activity of the enzymes necessary for RA synthesis (retinol dehydrogenases and aldehyde dehydrogenases), and the catabolism of RA by CYP26 enzymes all affect the levels of RA [248]. Retinoid signalling is frequently impaired early in carcinogenesis, suggesting that a decrease in retinoid signalling may be essential for tumour growth [249]. Although RA has frequently been regarded as a cell differentiation inducer, depending on the type of cell, RA might prevent cell differentiation and induce stemness [248]. Recent discoveries of retinoids as chemo-preventive and molecular-targeted antitumour agents reveal that RA agents may be considered efficient therapies for treating human solid tumours [250]. Among retinoids, all-trans retinoic acid (atRA) was found to be a promising therapeutic compound capable of targeting CSCs in different cancer settings, such as gastric [251], brain [252], head and neck [253], and breast [254] cancer. For instance, a significantly improved anti-cancer effect towards breast cancer was achieved when atRA and DOX were simultaneously delivered, encapsulated in the same nanoparticle [255]. This combinational drug delivery system aims to target both non-CSCs and CSCs. With their studies in vitro and in vivo, Sun et al. demonstrated that the atRA-induced differentiation of CSCs into non-CSCs can decrease their capacity for self-renewal and enhance their sensitivity to DOX, improving the inhibition of tumour growth while simultaneously decreasing the incidence of CSCs. Moreover, in A549GSC and H1650GSC cells, treatment with atRA was shown to dramatically lower the IC50 values for gefitinib, an ATP-competitive EGFR tyrosine kinase inhibitor used in non-small cells lung cancer (NSCLC) treatment, and the high expression of ALDH 1 family member A1 (ALDH1A1) and CD44 [256]. Additionally, conventional PKC inhibitor (Gö6976) and atRA combined treatment reduced tumour growth, metastatic dissemination, and the frequency of breast CSCs in vivo while impairing the proliferation, self-renewal, and clonogenicity ability of breast CSCs [257]. Interestingly, both products and substrates of the RA pathway, 5 μM atRA and 1 μM ROL, respectively, were shown to inhibit ALDH1+ CSC populations in cisplatin-resistant NSCLC cells [258]. Recently, Bonakdar et al. showed the importance of gut bacteria and their ability to metabolise vitamin A to produce a variety of retinoids with pharmacological activity [259]. In particular, they compared the retinoid metabolomes from caecal contents from germ-free (GF), conventional (CV), and antibiotic-treated mice (CV + Abx) and demonstrated that (1) GF mice had notably reduced amounts of all-trans-retinol (atROL), atRA, and 13-cis-retinoic acid (13cisRA) compared with those in CV mice and (2) when compared to that in control mice, CV animals treated with an antibiotic cocktail displayed a marked decrease in concentrations of all vitamin A metabolites except for RE. These results indicate that dietary vitamin A can be converted into ROL and its active metabolites, atRA and 13cisRA, by the gut microbiota. Besides the above-mentioned anticancer potential of atRA, it is worth noting that 13cisRA, also known as isotretinoin, is a key treatment for treating high-risk neuroblastoma and for dermatology. The presence of 13cisRA in the mouse caecum of CV mice but not GF or CV + Abx mice, as well as its in vitro production by caecal bacteria, indicates that 13cisRA is a particular retinoid derived exclusively from microorganism metabolism [259].
6. Conclusions
The identification of CSCs as a significant contributor to and driver of cancer development mechanisms, such as tumour growth, recurrence, metastasis, and therapy resistance, constitutes a significant advancement in the study of cancer and offers researchers the opportunity to develop new CSC-centric approaches for cancer treatment. The failure of cancer therapy is mostly due to CSC cell-mediated drug resistance. Characterising the differences between non-neoplastic tissue stem-cell programs and those of neoplastic tissue stem cells will be critical in developing therapeutic strategies to selectively target CSCs without negatively affecting non-neoplastic tissue stem cells. The development of mechanism-based methods for cancer drug discovery, including targeted therapies and immunotherapies, has been aided by remarkable improvements in our understanding of the molecular basis of cancer and tumour cell biology. However, there is a pressing need for the development of therapeutic approaches that are more successful in overcoming CSC cell-mediated resistance. In this regard, efforts are currently being made to find effective, affordable, and safe anticancer medicines of natural origin. There are now several strong connections among the host’s nutrition, the composition of the gut microbiota, and the host’s physiology. Particularly, numerous reports have underlined the key role of diet in cancer prevention [260,261]. For instance, it has been proven that the Mediterranean diet regimen significantly lowers the risk of several cancers, particularly colorectal and aerodigestive [262,263,264], gastric [265], pancreatic [266], breast [267,268,269], nasopharyngeal [270], lung [271], prostate [272], and bladder cancer [273].
The impact of the human microbiota on both short- and long-term human health has been amply shown during the last few decades [274,275,276,277,278]. In recent years, growing evidence has indicated the causal relationship between intestinal microbial dysbiosis and colorectal cancer aetiology [279]. In this perspective, to reverse established microbial dysbiosis, a range of approaches has been employed, including probiotics, prebiotics, postbiotics, antibiotics, and faecal microbiota transplantation (FMT) [280]. Currently, the small molecular weight compounds (postbiotics) released by the microbiota, which provide the host with many physiological health benefits, are given much attention. The host’s biochemical versatility is increased by the large metabolic repertoire of the microbial population, which supports the activity of mammalian enzymes and allows the host to metabolise a variety of food substrates [281]. This diet–microbial metabolism feedforward loop modulates a broad spectrum of events. Here, we reviewed the emerging roles of microbiota-derived metabolites as CSC-targeting anticancer agents. The body of evidence provided suggests that postbiotics, bioactive substances derived from gut beneficial microbiota, might be considered novel promising agents to be used in personalised medicine approaches to re-establish gut eubiosis while also targeting CSCs. This strategy may encompass the steering of diet–microbiota interactions toward the production of certain metabolites that could maximise health benefits. Furthermore, the synergistic effect of diverse microbial products with standard anticancer agents may suggest their further employment to sensitise CSCs in chemo-/radiotherapy regimens. In this perspective, postbiotics are superior to probiotics for industrial production because they are easier to use and store, have a longer shelf life, are stable across a wide pH and temperature range, and do not produce bioamine. However, before postbiotics can be employed as probiotic substitutes, more investigation is needed into the production, distribution mechanisms, and safety standards of medicines and functional foods [137]. Moreover, a crucial aspect to take into account from the viewpoint of postbiotic-based therapeutics is their targeted delivery in vivo. Indeed, it is crucial to ensure that a biomolecule given orally, intravenously, or topically can be transferred to its site of action without being altered via pharmacokinetics or digestive processes. In this regard, a recent summary of possible methods for the in vivo delivery of postbiotics was provided by Abbassi et al. [131]. In conclusion, the reviewed literature highlights that the microbiota is a valuable resource for the discovery of novel small-molecule drugs, and metabolites originating from the microbiota may find extensive use in the treatment of cancer, thanks to their ability to target CSCs. In this respect, further study of the pharmacological interaction between conventional chemotherapeutic drugs and gut microbiota-derived compounds will undoubtedly be necessary for the development of improved therapeutic approaches to eliminate CSCs.
7. Data Collection
For the current review, data were gathered from English-language scientific publications using different combinations of the following keywords: ‘cancer stem cells’, ‘cancer’, ‘stemness’, ‘signalling pathway’, ‘microbial products’, ‘microbiota metabolites’, ‘bacterial products’, ‘bacterial metabolites’, ‘probiotic ghosts’, ‘postbiotics’ as keywords in search queries of different databases and electronic search engines. Publications addressing CSC-associated mechanisms of therapeutic resistance, and articles describing the activity of gut microbiota bioactive metabolites toward CSC features were selected.
Acknowledgments
Figures present in this review were created with BioRender.com accessed on 25 January 2023.
Abbreviations
| 13cisRA | 13-cis-retinoic acid |
| 5-FU | 5-fluorouracil |
| ABC | ATP-binding cassette |
| ABCG2 | ATP binding cassette subfamily G member 2 |
| AKT | serine/threonine kinase |
| ALDH | aldehyde dehydrogenase |
| AML | acute myeloid leukaemia |
| atRA | all-trans-retinoic acid |
| atROL | all-trans-retinol |
| Bax | Bcl-2-associated X protein |
| Bcl | B-cell lymphoma 2 |
| BCRP | breast cancer resistance protein |
| BMI1 | polycomb complex protein BMI-1 |
| CFS | cell-free supernatant |
| CLDN-1 | claudin-1 |
| CMI | clomipramine |
| CQ | chloroquine |
| CSC | cancer stem cells |
| CYP26 | cytochrome P450 26A1 |
| DDR | DNA damage response |
| DIO | diet-induced obese |
| DOC or DCA | deoxycholic acid |
| DOX | doxorubicin |
| DSB | double-strand breaks |
| EA | ellagic acid |
| EGFR | epidermal growth factor receptor |
| EMT | epithelial-to-mesenchymal transition |
| ERK | extracellular signal-regulated kinase |
| FMT | faecal microbiota transplantation |
| FXR | farnesoid X receptor |
| GIST | gastrointestinal stromal tumour |
| GLUT1 | glucose transporter 1 |
| gp130 | glycoprotein 130 |
| GPR109a | G protein-coupled receptor 109a |
| HDAC | histone deacetylase |
| SHH | sonic hedgehog |
| HIF | hypoxia-inducible factor |
| ICD | immunogenic cell death |
| IDO1 | indoleamine 2,3-dioxygenase 1 |
| IDO2 | indoleamine 2,3-dioxygenase 2 |
| IPA | indolepropionic acid |
| JAK | Janus kinase |
| LCA | lithocholic acid |
| LDC | lysine decarboxylase |
| Lgr5 | leucine-rich repeat-containing G-protein coupled receptor 5 |
| M3R | muscarinic acetylcholine receptor M3 |
| MDR | multidrug resistance |
| MET | mesenchymal-to-epithelial transition |
| MFB | metformin-butyrate |
| miRNA | micro-RNA |
| MRN | MRE11–RAD50–NBS1 protein complex |
| NLRC5 | NLR family CARD Domain Containing 5 |
| NOD/SCID | non-obese diabetic/severe combined immunodeficient |
| Notch1 | neurogenic locus notch homolog protein 1 |
| OCT3 | octamer-binding transcription factor 3 |
| OCT4 | octamer-binding transcription factor 4 |
| PKC | protein kinase C |
| RA | retinoic acid |
| SCFA | short-chain fatty acid |
| SOX2 | (sex determining region Y)-box 2 |
| STAT3 | signal transducer and activator of transcription 3 |
| TDO | tryptophan 2,3-dioxygenase |
| TLR4 | Toll-like receptor 4 |
| T-βMCA | tauro-β-muricholic acid |
| Uro | urolithin |
| VEGF | vascular-endothelial growth factor |
| VM | vasculogenic mimicry |
| Wnt | Wingless/Integrated |
Author Contributions
V.A. conceived and designed the review, performed the literature search, wrote the manuscript, and produced figures; L.C. participated in review drafting and supported the literature search; L.M., F.P. and A.B. critically revised the manuscript. L.M. and A.B. provided funds. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created. Data sharing is not applicable to this review.
Conflicts of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding Statement
This work was funded by FAR 2022 to A.B. and by FAR 2022 to L.M. A.B. is funded by the Ricerca Corrente, IRCCS MultiMedica. A.B. is the recipient of a Research Grant funded by the Italian Association for Cancer Research (AIRC-MFAG, ID 22818), a Research Grant funded by the Cariplo Foundation (ID 2019-1609), and a Research Grant funded by Ricerca Corrente Rete Cardiologica IRCCS 2022 (ID RCR-2022-23682288).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Baudino T.A. Targeted Cancer Therapy: The Next Generation of Cancer Treatment. Curr. Drug Discov. Technol. 2015;12:3–20. doi: 10.2174/1570163812666150602144310. [DOI] [PubMed] [Google Scholar]
- 2.Waldman A.D., Fritz J.M., Lenardo M.J. A Guide to Cancer Immunotherapy: From T Cell Basic Science to Clinical Practice. Nat. Rev. Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baldo B.A., Pagani M. Adverse Events to Nontargeted and Targeted Chemotherapeutic Agents: Emphasis on Hypersensitivity Responses. Immunol. Allergy Clin. N. Am. 2014;34:565–596, viii. doi: 10.1016/j.iac.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Carvalho A., Fernandes A.R., Baptista P.V. Applications of Targeted Nano Drugs and Delivery Systems. Elsevier; Amsterdam, The Netherlands: 2019. Nanoparticles as Delivery Systems in Cancer Therapy; pp. 257–295. [Google Scholar]
- 5.Chang J.C. Cancer Stem Cells: Role in Tumor Growth, Recurrence, Metastasis, and Treatment Resistance. Medicine. 2016;95:S20–S25. doi: 10.1097/MD.0000000000004766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ricci-Vitiani L., Lombardi D.G., Pilozzi E., Biffoni M., Todaro M., Peschle C., De Maria R. Identification and Expansion of Human Colon-Cancer-Initiating Cells. Nature. 2007;445:111–115. doi: 10.1038/nature05384. [DOI] [PubMed] [Google Scholar]
- 7.O’Brien C.A., Pollett A., Gallinger S., Dick J.E. A Human Colon Cancer Cell Capable of Initiating Tumour Growth in Immunodeficient Mice. Nature. 2007;445:106–110. doi: 10.1038/nature05372. [DOI] [PubMed] [Google Scholar]
- 8.Lapidot T., Sirard C., Vormoor J., Murdoch B., Hoang T., Caceres-Cortes J., Minden M., Paterson B., Caligiuri M.A., Dick J.E. A Cell Initiating Human Acute Myeloid Leukaemia after Transplantation into SCID Mice. Nature. 1994;367:645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 9.Al-Hajj M., Wicha M.S., Benito-Hernandez A., Morrison S.J., Clarke M.F. Prospective Identification of Tumorigenic Breast Cancer Cells. Proc. Natl. Acad. Sci. USA. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh S.K., Clarke I.D., Terasaki M., Bonn V.E., Hawkins C., Squire J., Dirks P.B. Identification of a Cancer Stem Cell in Human Brain Tumors. Cancer Res. 2003;63:5821–5828. [PubMed] [Google Scholar]
- 11.Lin X., Farooqi A.A., Qureshi M.Z., Romero M.A., Tabassum S., Ismail M. Prostate Cancer Stem Cells: Viewing Signaling Cascades at a Finer Resolution. Arch. Immunol. Ther. Exp. 2016;64:217–223. doi: 10.1007/s00005-016-0383-0. [DOI] [PubMed] [Google Scholar]
- 12.Zhang K., Zhou S., Wang L., Wang J., Zou Q., Zhao W., Fu Q., Fang X. Current Stem Cell Biomarkers and Their Functional Mechanisms in Prostate Cancer. Int. J. Mol. Sci. 2016;17:1163. doi: 10.3390/ijms17071163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardavella G., George R., Sethi T. Lung Cancer Stem Cells-Characteristics, Phenotype. Transl. Lung Cancer Res. 2016;5:272–279. doi: 10.21037/tlcr.2016.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heiler S., Wang Z., Zöller M. Pancreatic Cancer Stem Cell Markers and Exosomes-the Incentive Push. World J. Gastroenterol. 2016;22:5971–6007. doi: 10.3748/wjg.v22.i26.5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sancho P., Alcala S., Usachov V., Hermann P.C., Sainz B., Jr. The Ever-Changing Landscape of Pancreatic Cancer Stem Cells. Pancreatology. 2016;16:489–496. doi: 10.1016/j.pan.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Gangopadhyay S., Nandy A., Hor P., Mukhopadhyay A. Breast Cancer Stem Cells: A Novel Therapeutic Target. Clin. Breast Cancer. 2013;13:7–15. doi: 10.1016/j.clbc.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 17.García Bueno J.M., Ocaña A., Castro-García P., Gil Gas C., Sánchez-Sánchez F., Poblet E., Serrano R., Calero R., Ramírez-Castillejo C. An Update on the Biology of Cancer Stem Cells in Breast Cancer. Clin. Transl. Oncol. 2008;10:786–793. doi: 10.1007/s12094-008-0291-9. [DOI] [PubMed] [Google Scholar]
- 18.Cherciu I., Bărbălan A., Pirici D., Mărgăritescu C., Săftoiu A. Stem Cells, Colorectal Cancer and Cancer Stem Cell Markers Correlations. Curr. Health Sci. J. 2014;40:153–161. doi: 10.12865/CHSJ.40.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson B.J., Schatton T., Frank M.H., Frank N.Y. Colorectal Cancer Stem Cells: Biology and Therapeutic Implications. Curr. Color. Cancer Rep. 2011;7:128–135. doi: 10.1007/s11888-011-0093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erhart F., Blauensteiner B., Zirkovits G., Printz D., Soukup K., Klingenbrunner S., Fischhuber K., Reitermaier R., Halfmann A., Lötsch D., et al. Gliomasphere Marker Combinatorics: Multidimensional Flow Cytometry Detects CD44+/CD133+/ITGA6+/CD36+ Signature. J. Cell. Mol. Med. 2019;23:281–292. doi: 10.1111/jcmm.13927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prabavathy D., Swarnalatha Y., Ramadoss N. Lung Cancer Stem Cells-Origin, Characteristics and Therapy. Stem Cell Investig. 2018;5:6. doi: 10.21037/sci.2018.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang L., Gao L., Xu S., Gong S., Chen L., Lü S., Chen J., Qiu H., Xu X., Ni X., et al. FISH+CD34+CD38- Cells Detected in Newly Diagnosed Acute Myeloid Leukemia Patients Can Predict the Clinical Outcome. J. Hematol. Oncol. 2013;6:85. doi: 10.1186/1756-8722-6-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trapasso S., Allegra E. Role of CD44 as a Marker of Cancer Stem Cells in Head and Neck Cancer. Biologics. 2012;6:379–383. doi: 10.2147/BTT.S37906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Z.F., Ho D.W., Ng M.N., Lau C.K., Yu W.C., Ngai P., Chu P.W.K., Lam C.T., Poon R.T.P., Fan S.T. Significance of CD90+ Cancer Stem Cells in Human Liver Cancer. Cancer Cell. 2008;13:153–166. doi: 10.1016/j.ccr.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 25.Wei H.-J., Yin T., Zhu Z., Shi P.-F., Tian Y., Wang C.-Y. Expression of CD44, CD24 and ESA in Pancreatic Adenocarcinoma Cell Lines Varies with Local Microenvironment. Hepatobiliary Pancreat. Dis. Int. 2011;10:428–434. doi: 10.1016/S1499-3872(11)60073-8. [DOI] [PubMed] [Google Scholar]
- 26.Kelly P.N., Dakic A., Adams J.M., Nutt S.L., Strasser A. Tumor Growth Need Not Be Driven by Rare Cancer Stem Cells. Science. 2007;317:337. doi: 10.1126/science.1142596. [DOI] [PubMed] [Google Scholar]
- 27.Kim W.-T., Ryu C.J. Cancer Stem Cell Surface Markers on Normal Stem Cells. BMB Rep. 2017;50:285–298. doi: 10.5483/BMBRep.2017.50.6.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ayob A.Z., Ramasamy T.S. Cancer Stem Cells as Key Drivers of Tumour Progression. J. Biomed. Sci. 2018;25:20. doi: 10.1186/s12929-018-0426-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Islam F., Gopalan V., Smith R.A., Lam A.K.-Y. Translational Potential of Cancer Stem Cells: A Review of the Detection of Cancer Stem Cells and Their Roles in Cancer Recurrence and Cancer Treatment. Exp. Cell Res. 2015;335:135–147. doi: 10.1016/j.yexcr.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 30.Yang L., Shi P., Zhao G., Xu J., Peng W., Zhang J., Zhang G., Wang X., Dong Z., Chen F., et al. Targeting Cancer Stem Cell Pathways for Cancer Therapy. Signal Transduct. Target. Ther. 2020;5:8. doi: 10.1038/s41392-020-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou H.-M., Zhang J.-G., Zhang X., Li Q. Targeting Cancer Stem Cells for Reversing Therapy Resistance: Mechanism, Signaling, and Prospective Agents. Signal Transduct. Target. Ther. 2021;6:62. doi: 10.1038/s41392-020-00430-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caglar H.O., Biray Avci C. Alterations of Cell Cycle Genes in Cancer: Unmasking the Role of Cancer Stem Cells. Mol. Biol. Rep. 2020;47:3065–3076. doi: 10.1007/s11033-020-05341-6. [DOI] [PubMed] [Google Scholar]
- 33.Agudo J., Park E.S., Rose S.A., Alibo E., Sweeney R., Dhainaut M., Kobayashi K.S., Sachidanandam R., Baccarini A., Merad M., et al. Quiescent Tissue Stem Cells Evade Immune Surveillance. Immunity. 2018;48:271–285.e5. doi: 10.1016/j.immuni.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bruschini S., Ciliberto G., Mancini R. The Emerging Role of Cancer Cell Plasticity and Cell-Cycle Quiescence in Immune Escape. Cell Death Dis. 2020;11:471. doi: 10.1038/s41419-020-2669-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malladi S., Macalinao D.G., Jin X., He L., Basnet H., Zou Y., de Stanchina E., Massagué J. Metastatic Latency and Immune Evasion through Autocrine Inhibition of WNT. Cell. 2016;165:45–60. doi: 10.1016/j.cell.2016.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Visvader J.E., Lindeman G.J. Cancer Stem Cells in Solid Tumours: Accumulating Evidence and Unresolved Questions. Nat. Rev. Cancer. 2008;8:755–768. doi: 10.1038/nrc2499. [DOI] [PubMed] [Google Scholar]
- 37.Mitra A., Mishra L., Li S. EMT, CTCs and CSCs in Tumor Relapse and Drug-Resistance. Oncotarget. 2015;6:10697–10711. doi: 10.18632/oncotarget.4037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mizushima N., Komatsu M. Autophagy: Renovation of Cells and Tissues. Cell. 2011;147:728–741. doi: 10.1016/j.cell.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 39.Maycotte P., Jones K.L., Goodall M.L., Thorburn J., Thorburn A. Autophagy Supports Breast Cancer Stem Cell Maintenance by Regulating IL6 Secretion. Mol. Cancer Res. 2015;13:651–658. doi: 10.1158/1541-7786.MCR-14-0487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gupta A., Roy S., Lazar A.J.F., Wang W.-L., McAuliffe J.C., Reynoso D., McMahon J., Taguchi T., Floris G., Debiec-Rychter M., et al. Autophagy Inhibition and Antimalarials Promote Cell Death in Gastrointestinal Stromal Tumor (GIST) Proc. Natl. Acad. Sci. USA. 2010;107:14333–14338. doi: 10.1073/pnas.1000248107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ojha R., Bhattacharyya S., Singh S.K. Autophagy in Cancer Stem Cells: A Potential Link Between Chemoresistance, Recurrence, and Metastasis. Biores. Open Access. 2015;4:97–108. doi: 10.1089/biores.2014.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nguyen H.G., Yang J.C., Kung H.-J., Shi X.-B., Tilki D., Lara P.N., DeVere White R.W., Gao A.C., Evans C.P. Targeting Autophagy Overcomes Enzalutamide Resistance in Castration-Resistant Prostate Cancer Cells and Improves Therapeutic Response in a Xenograft Model. Oncogene. 2014;33:4521–4530. doi: 10.1038/onc.2014.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Plaks V., Kong N., Werb Z. The Cancer Stem Cell Niche: How Essential Is the Niche in Regulating Stemness of Tumor Cells? Cell Stem Cell. 2015;16:225–238. doi: 10.1016/j.stem.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vaupel P., Kallinowski F., Okunieff P. Blood Flow, Oxygen and Nutrient Supply, and Metabolic Microenvironment of Human Tumors: A Review. Cancer Res. 1989;49:6449–6465. [PubMed] [Google Scholar]
- 45.Emami Nejad A., Najafgholian S., Rostami A., Sistani A., Shojaeifar S., Esparvarinha M., Nedaeinia R., Haghjooy Javanmard S., Taherian M., Ahmadlou M., et al. The Role of Hypoxia in the Tumor Microenvironment and Development of Cancer Stem Cell: A Novel Approach to Developing Treatment. Cancer Cell Int. 2021;21:62. doi: 10.1186/s12935-020-01719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yun Z., Lin Q. Hypoxia and Regulation of Cancer Cell Stemness. Adv. Exp. Med. Biol. 2014;772:41–53. doi: 10.1007/978-1-4614-5915-6_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kato Y., Ozawa S., Miyamoto C., Maehata Y., Suzuki A., Maeda T., Baba Y. Acidic Extracellular Microenvironment and Cancer. Cancer Cell Int. 2013;13:89. doi: 10.1186/1475-2867-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andreucci E., Peppicelli S., Ruzzolini J., Bianchini F., Biagioni A., Papucci L., Magnelli L., Mazzanti B., Stecca B., Calorini L. The Acidic Tumor Microenvironment Drives a Stem-like Phenotype in Melanoma Cells. J. Mol. Med. 2020;98:1431–1446. doi: 10.1007/s00109-020-01959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ritchie K.E., Nör J.E. Perivascular Stem Cell Niche in Head and Neck Cancer. Cancer Lett. 2013;338:41–46. doi: 10.1016/j.canlet.2012.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zanoni M., Bravaccini S., Fabbri F., Arienti C. Emerging Roles of Aldehyde Dehydrogenase Isoforms in Anti-Cancer Therapy Resistance. Front. Med. 2022;9:795762. doi: 10.3389/fmed.2022.795762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Croker A.K., Allan A.L. Inhibition of Aldehyde Dehydrogenase (ALDH) Activity Reduces Chemotherapy and Radiation Resistance of Stem-like ALDHhiCD44+ Human Breast Cancer Cells. Breast Cancer Res. Treat. 2012;133:75–87. doi: 10.1007/s10549-011-1692-y. [DOI] [PubMed] [Google Scholar]
- 52.Dylla S.J., Beviglia L., Park I.-K., Chartier C., Raval J., Ngan L., Pickell K., Aguilar J., Lazetic S., Smith-Berdan S., et al. Colorectal Cancer Stem Cells Are Enriched in Xenogeneic Tumors Following Chemotherapy. PLoS ONE. 2008;3:e2428. doi: 10.1371/annotation/2aa6a20a-e63c-49b6-aeea-aae62435617f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Januchowski R., Wojtowicz K., Zabel M. The Role of Aldehyde Dehydrogenase (ALDH) in Cancer Drug Resistance. Biomed. Pharmacother. 2013;67:669–680. doi: 10.1016/j.biopha.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 54.Schäfer A., Teufel J., Ringel F., Bettstetter M., Hoepner I., Rasper M., Gempt J., Koeritzer J., Schmidt-Graf F., Meyer B., et al. Aldehyde Dehydrogenase 1A1—a New Mediator of Resistance to Temozolomide in Glioblastoma. Neuro Oncol. 2012;14:1452–1464. doi: 10.1093/neuonc/nos270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tanei T., Morimoto K., Shimazu K., Kim S.J., Tanji Y., Taguchi T., Tamaki Y., Noguchi S. Association of Breast Cancer Stem Cells Identified by Aldehyde Dehydrogenase 1 Expression with Resistance to Sequential Paclitaxel and Epirubicin-Based Chemotherapy for Breast Cancers. Clin. Cancer Res. 2009;15:4234–4241. doi: 10.1158/1078-0432.CCR-08-1479. [DOI] [PubMed] [Google Scholar]
- 56.Cheung A.M.S., Wan T.S.K., Leung J.C.K., Chan L.Y.Y., Huang H., Kwong Y.L., Liang R., Leung A.Y.H. Aldehyde Dehydrogenase Activity in Leukemic Blasts Defines a Subgroup of Acute Myeloid Leukemia with Adverse Prognosis and Superior NOD/SCID Engrafting Potential. Leukemia. 2007;21:1423–1430. doi: 10.1038/sj.leu.2404721. [DOI] [PubMed] [Google Scholar]
- 57.Houghton J.A., Houghton P.J. Elucidation of Pathways of 5-Fluorouracil Metabolism in Xenografts of Human Colorectal Adenocarcinoma. Eur. J. Cancer Clin. Oncol. 1983;19:807–815. doi: 10.1016/0277-5379(83)90013-5. [DOI] [PubMed] [Google Scholar]
- 58.Schwartz P.M., Moir R.D., Hyde C.M., Turek P.J., Handschumacher R.E. Role of Uridine Phosphorylase in the Anabolism of 5-Fluorouracil. Biochem. Pharmacol. 1985;34:3585–3589. doi: 10.1016/0006-2952(85)90737-3. [DOI] [PubMed] [Google Scholar]
- 59.Meijer C., Mulder N.H., Timmer-Bosscha H., Sluiter W.J., Meersma G.J., de Vries E.G. Relationship of Cellular Glutathione to the Cytotoxicity and Resistance of Seven Platinum Compounds. Cancer Res. 1992;52:6885–6889. [PubMed] [Google Scholar]
- 60.Wu C.-P., Calcagno A.M., Ambudkar S.V. Reversal of ABC Drug Transporter-Mediated Multidrug Resistance in Cancer Cells: Evaluation of Current Strategies. Curr. Mol. Pharmacol. 2008;1:93–105. doi: 10.2174/1874467210801020093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Davidson A.L., Dassa E., Orelle C., Chen J. Structure, Function, and Evolution of Bacterial ATP-Binding Cassette Systems. Microbiol. Mol. Biol. Rev. 2008;72:317–364. doi: 10.1128/MMBR.00031-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Begicevic R.-R., Falasca M. ABC Transporters in Cancer Stem Cells: Beyond Chemoresistance. Int. J. Mol. Sci. 2017;18 doi: 10.3390/ijms18112362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kathawala R.J., Gupta P., Ashby C.R., Jr., Chen Z.-S. The Modulation of ABC Transporter-Mediated Multidrug Resistance in Cancer: A Review of the Past Decade. Drug Resist. Updat. 2015;18:1–17. doi: 10.1016/j.drup.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 64.Nathansen J., Meyer F., Müller L., Schmitz M., Borgmann K., Dubrovska A. Beyond the Double-Strand Breaks: The Role of DNA Repair Proteins in Cancer Stem-Cell Regulation. Cancers. 2021;13:4818. doi: 10.3390/cancers13194818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Andrés-León E., Cases I., Arcas A., Rojas A.M. DDRprot: A Database of DNA Damage Response-Related Proteins. Database. 2016;2016:baw123. doi: 10.1093/database/baw123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Abad E., Graifer D., Lyakhovich A. DNA Damage Response and Resistance of Cancer Stem Cells. Cancer Lett. 2020;474:106–117. doi: 10.1016/j.canlet.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 67.Anuranjani, Bala M. Concerted Action of Nrf2-ARE Pathway, MRN Complex, HMGB1 and Inflammatory Cytokines-Implication in Modification of Radiation Damage. Redox Biol. 2014;2:832–846. doi: 10.1016/j.redox.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cheng L., Wu Q., Huang Z., Guryanova O.A., Huang Q., Shou W., Rich J.N., Bao S. L1CAM Regulates DNA Damage Checkpoint Response of Glioblastoma Stem Cells through NBS1. EMBO J. 2011;30:800–813. doi: 10.1038/emboj.2011.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Völker-Albert M., Bronkhorst A., Holdenrieder S., Imhof A. Histone Modifications in Stem Cell Development and Their Clinical Implications. Stem Cell Rep. 2020;15:1196–1205. doi: 10.1016/j.stemcr.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taube J.H., Herschkowitz J.I., Komurov K., Zhou A.Y., Gupta S., Yang J., Hartwell K., Onder T.T., Gupta P.B., Evans K.W., et al. Core Epithelial-to-Mesenchymal Transition Interactome Gene-Expression Signature Is Associated with Claudin-Low and Metaplastic Breast Cancer Subtypes. Proc. Natl. Acad. Sci. USA. 2010;107:15449–15454. doi: 10.1073/pnas.1004900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mani S.A., Guo W., Liao M.-J., Eaton E.N., Ayyanan A., Zhou A.Y., Brooks M., Reinhard F., Zhang C.C., Shipitsin M., et al. The Epithelial-Mesenchymal Transition Generates Cells with Properties of Stem Cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Morel A.-P., Lièvre M., Thomas C., Hinkal G., Ansieau S., Puisieux A. Generation of Breast Cancer Stem Cells through Epithelial-Mesenchymal Transition. PLoS ONE. 2008;3:e2888. doi: 10.1371/journal.pone.0002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beck B., Blanpain C. Unravelling Cancer Stem Cell Potential. Nat. Rev. Cancer. 2013;13:727–738. doi: 10.1038/nrc3597. [DOI] [PubMed] [Google Scholar]
- 74.Shibue T., Weinberg R.A. EMT, CSCs, and Drug Resistance: The Mechanistic Link and Clinical Implications. Nat. Rev. Clin. Oncol. 2017;14:611–629. doi: 10.1038/nrclinonc.2017.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Farmer P., Bonnefoi H., Anderle P., Cameron D., Wirapati P., Becette V., André S., Piccart M., Campone M., Brain E., et al. A Stroma-Related Gene Signature Predicts Resistance to Neoadjuvant Chemotherapy in Breast Cancer. Nat. Med. 2009;15:68–74. doi: 10.1038/nm.1908. [DOI] [PubMed] [Google Scholar]
- 76.Byers L.A., Diao L., Wang J., Saintigny P., Girard L., Peyton M., Shen L., Fan Y., Giri U., Tumula P.K., et al. An Epithelial-Mesenchymal Transition Gene Signature Predicts Resistance to EGFR and PI3K Inhibitors and Identifies Axl as a Therapeutic Target for Overcoming EGFR Inhibitor Resistance. Clin. Cancer Res. 2013;19:279–290. doi: 10.1158/1078-0432.CCR-12-1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mukherjee S., Manna A., Bhattacharjee P., Mazumdar M., Saha S., Chakraborty S., Guha D., Adhikary A., Jana D., Gorain M., et al. Non-Migratory Tumorigenic Intrinsic Cancer Stem Cells Ensure Breast Cancer Metastasis by Generation of CXCR4(+) Migrating Cancer Stem Cells. Oncogene. 2016;35:4937–4948. doi: 10.1038/onc.2016.26. [DOI] [PubMed] [Google Scholar]
- 78.Saxena K., Jolly M.K., Balamurugan K. Hypoxia, Partial EMT and Collective Migration: Emerging Culprits in Metastasis. Transl. Oncol. 2020;13:100845. doi: 10.1016/j.tranon.2020.100845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maniotis A.J., Folberg R., Hess A., Seftor E.A., Gardner L.M., Pe’er J., Trent J.M., Meltzer P.S., Hendrix M.J. Vascular Channel Formation by Human Melanoma Cells in Vivo and in Vitro: Vasculogenic Mimicry. Am. J. Pathol. 1999;155:739–752. doi: 10.1016/S0002-9440(10)65173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Seftor R.E.B., Hess A.R., Seftor E.A., Kirschmann D.A., Hardy K.M., Margaryan N.V., Hendrix M.J.C. Tumor Cell Vasculogenic Mimicry: From Controversy to Therapeutic Promise. Am. J. Pathol. 2012;181:1115–1125. doi: 10.1016/j.ajpath.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yang J.P., Liao Y.D., Mai D.M., Xie P., Qiang Y.Y., Zheng L.S., Wang M.Y., Mei Y., Meng D.F., Xu L., et al. Tumor Vasculogenic Mimicry Predicts Poor Prognosis in Cancer Patients: A Meta-Analysis. Angiogenesis. 2016;19:191–200. doi: 10.1007/s10456-016-9500-2. [DOI] [PubMed] [Google Scholar]
- 82.Liu R., Yang K., Meng C., Zhang Z., Xu Y. Vasculogenic Mimicry Is a Marker of Poor Prognosis in Prostate Cancer. Cancer Biol. Ther. 2012;13:527–533. doi: 10.4161/cbt.19602. [DOI] [PubMed] [Google Scholar]
- 83.Hori A., Shimoda M., Naoi Y., Kagara N., Tanei T., Miyake T., Shimazu K., Kim S.J., Noguchi S. Vasculogenic Mimicry Is Associated with Trastuzumab Resistance of HER2-Positive Breast Cancer. Breast Cancer Res. 2019;21:88. doi: 10.1186/s13058-019-1167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Murugesan A., Sekar B., Saranyan R., Manivannan E., Rajmohan M. A Review on Cancer Stem Cells in Vasculogenic Mimicry Formation: A New Dimension for Targeted Therapy. J. Adv. Oral Res. 2021;12:34–41. doi: 10.1177/2320206820960862. [DOI] [Google Scholar]
- 85.Bittner M., Meltzer P., Chen Y., Jiang Y., Seftor E., Hendrix M., Radmacher M., Simon R., Yakhini Z., Ben-Dor A., et al. Molecular Classification of Cutaneous Malignant Melanoma by Gene Expression Profiling. Nature. 2000;406:536–540. doi: 10.1038/35020115. [DOI] [PubMed] [Google Scholar]
- 86.Wang Y., Li W., Patel S.S., Cong J., Zhang N., Sabbatino F., Liu X., Qi Y., Huang P., Lee H., et al. Blocking the Formation of Radiation-Induced Breast Cancer Stem Cells. Oncotarget. 2014;5:3743–3755. doi: 10.18632/oncotarget.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lagadec C., Vlashi E., Della Donna L., Dekmezian C., Pajonk F. Radiation-Induced Reprogramming of Breast Cancer Cells. Stem Cells. 2012;30:833–844. doi: 10.1002/stem.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hu X., Ghisolfi L., Keates A.C., Zhang J., Xiang S., Lee D.-K., Li C.J. Induction of Cancer Cell Stemness by Chemotherapy. Cell Cycle. 2012;11:2691–2698. doi: 10.4161/cc.21021. [DOI] [PubMed] [Google Scholar]
- 89.Xu Z.-Y., Tang J.-N., Xie H.-X., Du Y.-A., Huang L., Yu P.-F., Cheng X.-D. 5-Fluorouracil Chemotherapy of Gastric Cancer Generates Residual Cells with Properties of Cancer Stem Cells. Int. J. Biol. Sci. 2015;11:284–294. doi: 10.7150/ijbs.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nosrati N., Bakovic M., Paliyath G. Molecular Mechanisms and Pathways as Targets for Cancer Prevention and Progression with Dietary Compounds. Int. J. Mol. Sci. 2017;18:2050. doi: 10.3390/ijms18102050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bhat T.A., Singh R.P. Tumor Angiogenesis—a Potential Target in Cancer Chemoprevention. Food Chem. Toxicol. 2008;46:1334–1345. doi: 10.1016/j.fct.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 92.Liskova A., Kubatka P., Samec M., Zubor P., Mlyncek M., Bielik T., Samuel S.M., Zulli A., Kwon T.K., Büsselberg D. Dietary Phytochemicals Targeting Cancer Stem Cells. Molecules. 2019;24:899. doi: 10.3390/molecules24050899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schwabe R.F., Jobin C. The Microbiome and Cancer. Nat. Rev. Cancer. 2013;13:800–812. doi: 10.1038/nrc3610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jaye K., Li C.G., Chang D., Bhuyan D.J. The Role of Key Gut Microbial Metabolites in the Development and Treatment of Cancer. Gut Microbes. 2022;14:2038865. doi: 10.1080/19490976.2022.2038865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hsiao W.W.L., Metz C., Singh D.P., Roth J. The Microbes of the Intestine: An Introduction to Their Metabolic and Signaling Capabilities. Endocrinol. Metab. Clin. N. Am. 2008;37:857–871. doi: 10.1016/j.ecl.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pabst O. Correlation, Consequence, and Functionality in Microbiome-Immune Interplay. Immunol. Rev. 2017;279:4–7. doi: 10.1111/imr.12584. [DOI] [PubMed] [Google Scholar]
- 97.Śliżewska K., Markowiak-Kopeć P., Śliżewska W. The Role of Probiotics in Cancer Prevention. Cancers. 2020;13 doi: 10.3390/cancers13010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rinninella E., Raoul P., Cintoni M., Franceschi F., Miggiano G.A.D., Gasbarrini A., Mele M.C. What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7:14. doi: 10.3390/microorganisms7010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hillman E.T., Lu H., Yao T., Nakatsu C.H. Microbial Ecology along the Gastrointestinal Tract. Microbes Environ. 2017;32:300–313. doi: 10.1264/jsme2.ME17017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Xu H., Liu M., Cao J., Li X., Fan D., Xia Y., Lu X., Li J., Ju D., Zhao H. The Dynamic Interplay between the Gut Microbiota and Autoimmune Diseases. J. Immunol. Res. 2019;2019:7546047. doi: 10.1155/2019/7546047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Khan M.F., Wang H. Environmental Exposures and Autoimmune Diseases: Contribution of Gut Microbiome. Front. Immunol. 2019;10:3094. doi: 10.3389/fimmu.2019.03094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sadrekarimi H., Gardanova Z.R., Bakhshesh M., Ebrahimzadeh F., Yaseri A.F., Thangavelu L., Hasanpoor Z., Zadeh F.A., Kahrizi M.S. Emerging Role of Human Microbiome in Cancer Development and Response to Therapy: Special Focus on Intestinal Microflora. J. Transl. Med. 2022;20:301. doi: 10.1186/s12967-022-03492-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Goodman B., Gardner H. The Microbiome and Cancer. J. Pathol. 2018;244:667–676. doi: 10.1002/path.5047. [DOI] [PubMed] [Google Scholar]
- 104.Kuipers E.J. Review Article: Exploring the Link between Helicobacter Pylori and Gastric Cancer. Aliment. Pharmacol. Ther. 1999;13((Suppl. S1)):3–11. doi: 10.1046/j.1365-2036.1999.00002.x. [DOI] [PubMed] [Google Scholar]
- 105.Wroblewski L.E., Peek R.M., Jr., Wilson K.T. Helicobacter Pylori and Gastric Cancer: Factors That Modulate Disease Risk. Clin. Microbiol. Rev. 2010;23:713–739. doi: 10.1128/CMR.00011-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Polk D.B., Peek R.M., Jr. Helicobacter Pylori: Gastric Cancer and Beyond. Nat. Rev. Cancer. 2010;10:403–414. doi: 10.1038/nrc2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Nosho K., Sukawa Y., Adachi Y., Ito M., Mitsuhashi K., Kurihara H., Kanno S., Yamamoto I., Ishigami K., Igarashi H., et al. Association of Fusobacterium Nucleatum with Immunity and Molecular Alterations in Colorectal Cancer. World J. Gastroenterol. 2016;22:557–566. doi: 10.3748/wjg.v22.i2.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shang F.-M., Liu H.-L. Fusobacterium Nucleatum and Colorectal Cancer: A Review. World J. Gastrointest. Oncol. 2018;10:71–81. doi: 10.4251/wjgo.v10.i3.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hashemi Goradel N., Heidarzadeh S., Jahangiri S., Farhood B., Mortezaee K., Khanlarkhani N., Negahdari B. Fusobacterium Nucleatum and Colorectal Cancer: A Mechanistic Overview. J. Cell. Physiol. 2019;234:2337–2344. doi: 10.1002/jcp.27250. [DOI] [PubMed] [Google Scholar]
- 110.Matson V., Chervin C.S., Gajewski T.F. Cancer and the Microbiome-Influence of the Commensal Microbiota on Cancer, Immune Responses, and Immunotherapy. Gastroenterology. 2021;160:600–613. doi: 10.1053/j.gastro.2020.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bessède E., Staedel C., Acuña Amador L.A., Nguyen P.H., Chambonnier L., Hatakeyama M., Belleannée G., Mégraud F., Varon C. Helicobacter Pylori Generates Cells with Cancer Stem Cell Properties via Epithelial–Mesenchymal Transition-like Changes. Oncogene. 2013;33:4123–4131. doi: 10.1038/onc.2013.380. [DOI] [PubMed] [Google Scholar]
- 112.Cavallucci V., Palucci I., Fidaleo M., Mercuri A., Masi L., Emoli V., Bianchetti G., Fiori M.E., Bachrach G., Scaldaferri F., et al. Proinflammatory and Cancer-Promoting Pathobiont Fusobacterium Nucleatum Directly Targets Colorectal Cancer Stem Cells. Biomolecules. 2022;12:1256. doi: 10.3390/biom12091256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ha N.H., Woo B.H., Kim D.J., Ha E.S., Choi J.I., Kim S.J., Park B.S., Lee J.H., Park H.R. Prolonged and Repetitive Exposure to Porphyromonas Gingivalis Increases Aggressiveness of Oral Cancer Cells by Promoting Acquisition of Cancer Stem Cell Properties. Tumour Biol. 2015;36:9947–9960. doi: 10.1007/s13277-015-3764-9. [DOI] [PubMed] [Google Scholar]
- 114.Dapito D.H., Mencin A., Gwak G.-Y., Pradere J.-P., Jang M.-K., Mederacke I., Caviglia J.M., Khiabanian H., Adeyemi A., Bataller R., et al. Promotion of Hepatocellular Carcinoma by the Intestinal Microbiota and TLR4. Cancer Cell. 2012;21:504–516. doi: 10.1016/j.ccr.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yoshimoto S., Loo T.M., Atarashi K., Kanda H., Sato S., Oyadomari S., Iwakura Y., Oshima K., Morita H., Hattori M., et al. Obesity-Induced Gut Microbial Metabolite Promotes Liver Cancer through Senescence Secretome. Nature. 2013;499:97–101. doi: 10.1038/nature12347. [DOI] [PubMed] [Google Scholar]
- 116.McIntosh G.H., Royle P.J., Playne M.J. A Probiotic Strain of L. Acidophilus Reduces DMH-Induced Large Intestinal Tumors in Male Sprague-Dawley Rats. Nutr. Cancer. 1999;35:153–159. doi: 10.1207/S15327914NC352_9. [DOI] [PubMed] [Google Scholar]
- 117.Tukenmez U., Aktas B., Aslim B., Yavuz S. The Relationship between the Structural Characteristics of Lactobacilli-EPS and Its Ability to Induce Apoptosis in Colon Cancer Cells in Vitro. Sci. Rep. 2019;9:8268. doi: 10.1038/s41598-019-44753-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Abdelghani Z., Hourani N., Zaidan Z., Dbaibo G., Mrad M., Hage-Sleiman R. Therapeutic Applications and Biological Activities of Bacterial Bioactive Extracts. Arch. Microbiol. 2021;203:4755–4776. doi: 10.1007/s00203-021-02505-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.McAllister F., Khan M.A.W., Helmink B., Wargo J.A. The Tumor Microbiome in Pancreatic Cancer: Bacteria and Beyond. Cancer Cell. 2019;36:577–579. doi: 10.1016/j.ccell.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 120.Oliva M., Mulet-Margalef N., Ochoa-De-Olza M., Napoli S., Mas J., Laquente B., Alemany L., Duell E.J., Nuciforo P., Moreno V. Tumor-Associated Microbiome: Where Do We Stand? Int. J. Mol. Sci. 2021;22:1446. doi: 10.3390/ijms22031446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Aghamajidi A., Maleki Vareki S. The Effect of the Gut Microbiota on Systemic and Anti-Tumor Immunity and Response to Systemic Therapy against Cancer. Cancers. 2022;14:3563. doi: 10.3390/cancers14153563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou X., Kandalai S., Hossain F., Zheng Q. Tumor Microbiome Metabolism: A Game Changer in Cancer Development and Therapy. Front. Oncol. 2022;12:933407. doi: 10.3389/fonc.2022.933407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.To K.K.W., Cho W.C.S. Drug Repurposing in Cancer Therapy: Approaches and Applications. Academic Press; Cambridge, MA, USA: 2020. [Google Scholar]
- 124.Wallace B.D., Wang H., Lane K.T., Scott J.E., Orans J., Koo J.S., Venkatesh M., Jobin C., Yeh L.-A., Mani S., et al. Alleviating Cancer Drug Toxicity by Inhibiting a Bacterial Enzyme. Science. 2010;330:831–835. doi: 10.1126/science.1191175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Matson V., Fessler J., Bao R., Chongsuwat T., Zha Y., Alegre M.-L., Luke J.J., Gajewski T.F. The Commensal Microbiome Is Associated with Anti–PD-1 Efficacy in Metastatic Melanoma Patients. Science. 2018;359:104–108. doi: 10.1126/science.aao3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.West N.R., Powrie F. Immunotherapy Not Working? Check Your Microbiota. Cancer Cell. 2015;28:687–689. doi: 10.1016/j.ccell.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 127.Azad M.A.K., Sarker M., Li T., Yin J. Probiotic Species in the Modulation of Gut Microbiota: An Overview. BioMed Res. Int. 2018;2018:9478630. doi: 10.1155/2018/9478630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bindels L.B., Delzenne N.M., Cani P.D., Walter J. Towards a More Comprehensive Concept for Prebiotics. Nat. Rev. Gastroenterol. Hepatol. 2015;12:303–310. doi: 10.1038/nrgastro.2015.47. [DOI] [PubMed] [Google Scholar]
- 129.Tsilingiri K., Rescigno M. Postbiotics: What Else? Benef. Microbes. 2013;4:101–107. doi: 10.3920/BM2012.0046. [DOI] [PubMed] [Google Scholar]
- 130.Rad A.H., Abbasi A., Kafil H.S., Ganbarov K. Potential Pharmaceutical and Food Applications of Postbiotics: A Review. Curr. Pharm. Biotechnol. 2020;21:1576–1587. doi: 10.2174/1389201021666200516154833. [DOI] [PubMed] [Google Scholar]
- 131.Abbasi A., Hajipour N., Hasannezhad P., Baghbanzadeh A., Aghebati-Maleki L. Potential in Vivo Delivery Routes of Postbiotics. Crit. Rev. Food Sci. Nutr. 2022;62:3345–3369. doi: 10.1080/10408398.2020.1865260. [DOI] [PubMed] [Google Scholar]
- 132.Conlon M.A., Bird A.R. The Impact of Diet and Lifestyle on Gut Microbiota and Human Health. Nutrients. 2014;7:17–44. doi: 10.3390/nu7010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sheflin A.M., Melby C.L., Carbonero F., Weir T.L. Linking Dietary Patterns with Gut Microbial Composition and Function. Gut Microbes. 2017;8:113–129. doi: 10.1080/19490976.2016.1270809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Leeming E.R., Johnson A.J., Spector T.D., Le Roy C.I. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients. 2019;11:2862. doi: 10.3390/nu11122862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Puca F., Fedele M., Rasio D., Battista S. Role of Diet in Stem and Cancer Stem Cells. Int. J. Mol. Sci. 2022;23:8108. doi: 10.3390/ijms23158108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Louis P., Hold G.L., Flint H.J. The Gut Microbiota, Bacterial Metabolites and Colorectal Cancer. Nat. Rev. Microbiol. 2014;12:661–672. doi: 10.1038/nrmicro3344. [DOI] [PubMed] [Google Scholar]
- 137.Salminen S., Collado M.C., Endo A., Hill C., Lebeer S., Quigley E.M.M., Sanders M.E., Shamir R., Swann J.R., Szajewska H., et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) Consensus Statement on the Definition and Scope of Postbiotics. Nat. Rev. Gastroenterol. Hepatol. 2021;18:649–667. doi: 10.1038/s41575-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Patel R.M., Denning P.W. Therapeutic Use of Prebiotics, Probiotics, and Postbiotics to Prevent Necrotizing Enterocolitis: What Is the Current Evidence? Clin. Perinatol. 2013;40:11–25. doi: 10.1016/j.clp.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Aguilar-Toalá J.E., Garcia-Varela R., Garcia H.S., Mata-Haro V., González-Córdova A.F., Vallejo-Cordoba B., Hernández-Mendoza A. Postbiotics: An Evolving Term within the Functional Foods Field. Trends Food Sci. Technol. 2018;75:105–114. doi: 10.1016/j.tifs.2018.03.009. [DOI] [Google Scholar]
- 140.Liu J., Tan Y., Cheng H., Zhang D., Feng W., Peng C. Functions of Gut Microbiota Metabolites, Current Status and Future Perspectives. Aging Dis. 2022;13:1106–1126. doi: 10.14336/AD.2022.0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhang L., Song J., Kong L., Yuan T., Li W., Zhang W., Hou B., Lu Y., Du G. The Strategies and Techniques of Drug Discovery from Natural Products. Pharmacol. Ther. 2020;216:107686. doi: 10.1016/j.pharmthera.2020.107686. [DOI] [PubMed] [Google Scholar]
- 142.Noori S.M.A., Behfar A., Saadat A., Ameri A., Atashi Yazdi S.S., Siahpoosh A. Antimicrobial and Antioxidant Properties of Natural Postbiotics Derived from Five Lactic Acid Bacteria. Jundishapur J. Nat. Pharm. Prod. 2022 doi: 10.5812/jjnpp-130785. in Press . [DOI] [Google Scholar]
- 143.Zin N.M., Abd Rashid A.N., Zulkhairi N.A., Ridzman N.A. Isolation of Lactic Acid Bacteria from Cocoa Bean Fermentation as Potential Antibacterial Agent against ESKAPE Pathogens. Sains Malays. 2022;51:3401–3414. [Google Scholar]
- 144.Ryu S.W., Kim J.-S., Oh B.S., Choi W.J., Yu S.Y., Bak J.E., Park S.-H., Kang S.W., Lee J., Jung W.Y., et al. Gut Microbiota Eubacterium Callanderi Exerts Anti-Colorectal Cancer Activity. Microbiol. Spectr. 2022;10:e0253122. doi: 10.1128/spectrum.02531-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.An J., Ha E.-M. Combination Therapy of Lactobacillus Plantarum Supernatant and 5-Fluouracil Increases Chemosensitivity in Colorectal Cancer Cells. J. Microbiol. Biotechnol. 2016;26:1490–1503. doi: 10.4014/jmb.1605.05024. [DOI] [PubMed] [Google Scholar]
- 146.An J., Ha E.-M. Lactobacillus-Derived Metabolites Enhance the Antitumor Activity of 5-FU and Inhibit Metastatic Behavior in 5-FU-Resistant Colorectal Cancer Cells by Regulating Claudin-1 Expression. J. Microbiol. 2020;58:967–977. doi: 10.1007/s12275-020-0375-y. [DOI] [PubMed] [Google Scholar]
- 147.Maghsood F., Johari B., Rohani M., Madanchi H., Saltanatpour Z., Kadivar M. Anti-Proliferative and Anti-Metastatic Potential of High Molecular Weight Secretory Molecules from Probiotic Lactobacillus Reuteri Cell-Free Supernatant Against Human Colon Cancer Stem-Like Cells (HT29-ShE) Int. J. Pept. Res. Ther. 2020;26:2619–2631. doi: 10.1007/s10989-020-10049-z. [DOI] [Google Scholar]
- 148.Manson M.M. Cancer Prevention—the Potential for Diet to Modulate Molecular Signalling. Trends Mol. Med. 2003;9:11–18. doi: 10.1016/S1471-4914(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 149.Key T.J., Schatzkin A., Willett W.C., Allen N.E., Spencer E.A., Travis R.C. Diet, Nutrition and the Prevention of Cancer. Public Health Nutr. 2004;7:187–200. doi: 10.1079/PHN2003588. [DOI] [PubMed] [Google Scholar]
- 150.Mayne S.T., Playdon M.C., Rock C.L. Diet, Nutrition, and Cancer: Past, Present and Future. Nat. Rev. Clin. Oncol. 2016;13:504–515. doi: 10.1038/nrclinonc.2016.24. [DOI] [PubMed] [Google Scholar]
- 151.Bail J., Meneses K., Demark-Wahnefried W. Nutritional Status and Diet in Cancer Prevention. Semin. Oncol. Nurs. 2016;32:206–214. doi: 10.1016/j.soncn.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 152.Chen X., Ding J., Li H., Carr P.R., Hoffmeister M., Brenner H. The Power of a Healthy Lifestyle for Cancer Prevention: The Example of Colorectal Cancer. Cancer Biol. Med. 2022;19:1586–1597. doi: 10.20892/j.issn.2095-3941.2022.0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ali R., Staub H., Coccodrilli G., Jr., Schanbacher L. Nutritional Significance of Dietary Fiber: Effect on Nutrient Bioavailability and Selected Gastrointestinal Functions. J. Agric. Food Chem. 1981;29:465–472. doi: 10.1021/jf00105a007. [DOI] [PubMed] [Google Scholar]
- 154.Jones J.M. CODEX-Aligned Dietary Fiber Definitions Help to Bridge the “Fiber Gap”. Nutr. J. 2014;13:34. doi: 10.1186/1475-2891-13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.den Besten G., van Eunen K., Groen A.K., Venema K., Reijngoud D.-J., Bakker B.M. The Role of Short-Chain Fatty Acids in the Interplay between Diet, Gut Microbiota, and Host Energy Metabolism. J. Lipid Res. 2013;54:2325–2340. doi: 10.1194/jlr.R036012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Aune D., Chan D.S.M., Lau R., Vieira R., Greenwood D.C., Kampman E., Norat T. Dietary Fibre, Whole Grains, and Risk of Colorectal Cancer: Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. BMJ. 2011;343:d6617. doi: 10.1136/bmj.d6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kunzmann A.T., Coleman H.G., Huang W.-Y., Kitahara C.M., Cantwell M.M., Berndt S.I. Dietary Fiber Intake and Risk of Colorectal Cancer and Incident and Recurrent Adenoma in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Am. J. Clin. Nutr. 2015;102:881–890. doi: 10.3945/ajcn.115.113282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Masrul M., Nindrea R.D. Dietary Fibre Protective against Colorectal Cancer Patients in Asia: A Meta-Analysis. Open Access Maced. J. Med. Sci. 2019;7:1723–1727. doi: 10.3889/oamjms.2019.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Comalada M., Bailón E., de Haro O., Lara-Villoslada F., Xaus J., Zarzuelo A., Gálvez J. The Effects of Short-Chain Fatty Acids on Colon Epithelial Proliferation and Survival Depend on the Cellular Phenotype. J. Cancer Res. Clin. Oncol. 2006;132:487–497. doi: 10.1007/s00432-006-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gibson P.R., Moeller I., Kagelari O., Folino M., Young G.P. Contrasting Effects of Butyrate on the Expression of Phenotypic Markers of Differentiation in Neoplastic and Non-Neoplastic Colonic Epithelial Cells in Vitro. J. Gastroenterol. Hepatol. 1992;7:165–172. doi: 10.1111/j.1440-1746.1992.tb00956.x. [DOI] [PubMed] [Google Scholar]
- 161.Gibson P.R., Rosella O., Wilson A.J., Mariadason J.M., Rickard K., Byron K., Barkla D.H. Colonic Epithelial Cell Activation and the Paradoxical Effects of Butyrate. Carcinogenesis. 1999;20:539–544. doi: 10.1093/carcin/20.4.539. [DOI] [PubMed] [Google Scholar]
- 162.Lupton J.R. Microbial Degradation Products Influence Colon Cancer Risk: The Butyrate Controversy. J. Nutr. 2004;134:479–482. doi: 10.1093/jn/134.2.479. [DOI] [PubMed] [Google Scholar]
- 163.Geng H.-W., Yin F.-Y., Zhang Z.-F., Gong X., Yang Y. Butyrate Suppresses Glucose Metabolism of Colorectal Cancer Cells via GPR109a-AKT Signaling Pathway and Enhances Chemotherapy. Front. Mol. Biosci. 2021;8:634874. doi: 10.3389/fmolb.2021.634874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li Q., Ding C., Meng T., Lu W., Liu W., Hao H., Cao L. Butyrate Suppresses Motility of Colorectal Cancer Cells via Deactivating Akt/ERK Signaling in Histone Deacetylase Dependent Manner. J. Pharmacol. Sci. 2017;135:148–155. doi: 10.1016/j.jphs.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 165.Donohoe D.R., Collins L.B., Wali A., Bigler R., Sun W., Bultman S.J. The Warburg Effect Dictates the Mechanism of Butyrate-Mediated Histone Acetylation and Cell Proliferation. Mol. Cell. 2012;48:612–626. doi: 10.1016/j.molcel.2012.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Salvi P.S., Cowles R.A. Butyrate and the Intestinal Epithelium: Modulation of Proliferation and Inflammation in Homeostasis and Disease. Cells. 2021;10:1775. doi: 10.3390/cells10071775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kaiko G.E., Ryu S.H., Koues O.I., Collins P.L., Solnica-Krezel L., Pearce E.J., Pearce E.L., Oltz E.M., Stappenbeck T.S. The Colonic Crypt Protects Stem Cells from Microbiota-Derived Metabolites. Cell. 2016;165:1708–1720. doi: 10.1016/j.cell.2016.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lee K.-M., Lee M., Lee J., Kim S.W., Moon H.-G., Noh D.-Y., Han W. Enhanced Anti-Tumor Activity and Cytotoxic Effect on Cancer Stem Cell Population of Metformin-Butyrate Compared with Metformin HCl in Breast Cancer. Oncotarget. 2016;7:38500–38512. doi: 10.18632/oncotarget.9522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Park M., Kwon J., Shin H.-J., Moon S.M., Kim S.B., Shin U.S., Han Y.-H., Kim Y. Butyrate Enhances the Efficacy of Radiotherapy via FOXO3A in Colorectal Cancer Patient-derived Organoids. Int. J. Oncol. 2020;57:1307–1318. doi: 10.3892/ijo.2020.5132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Beyaz S., Mana M.D., Roper J., Kedrin D., Saadatpour A., Hong S.-J., Bauer-Rowe K.E., Xifaras M.E., Akkad A., Arias E., et al. High-Fat Diet Enhances Stemness and Tumorigenicity of Intestinal Progenitors. Nature. 2016;531:53–58. doi: 10.1038/nature17173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Staels B., Fonseca V.A. Bile Acids and Metabolic Regulation: Mechanisms and Clinical Responses to Bile Acid Sequestration. Diabetes Care. 2009;32((Suppl. S2)):S237–S245. doi: 10.2337/dc09-S355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hofmann A.F. The Continuing Importance of Bile Acids in Liver and Intestinal Disease. Arch. Intern. Med. 1999;159:2647–2658. doi: 10.1001/archinte.159.22.2647. [DOI] [PubMed] [Google Scholar]
- 173.Phelan J.P., Reen F.J., Caparros-Martin J.A., O’Connor R., O’Gara F. Rethinking the Bile Acid/Gut Microbiome Axis in Cancer. Oncotarget. 2017;8:115736–115747. doi: 10.18632/oncotarget.22803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yang R., Qian L. Research on Gut Microbiota-Derived Secondary Bile Acids in Cancer Progression. Integr. Cancer Ther. 2022;21 doi: 10.1177/15347354221114100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bayerdörffer E., Mannes G.A., Ochsenkühn T., Dirschedl P., Wiebecke B., Paumgartner G. Unconjugated Secondary Bile Acids in the Serum of Patients with Colorectal Adenomas. Gut. 1995;36:268–273. doi: 10.1136/gut.36.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Farhana L., Nangia-Makker P., Arbit E., Shango K., Sarkar S., Mahmud H., Hadden T., Yu Y., Majumdar A.P.N. Bile Acid: A Potential Inducer of Colon Cancer Stem Cells. Stem Cell Res. Ther. 2016;7:181. doi: 10.1186/s13287-016-0439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fu T., Coulter S., Yoshihara E., Oh T.G., Fang S., Cayabyab F., Zhu Q., Zhang T., Leblanc M., Liu S., et al. FXR Regulates Intestinal Cancer Stem Cell Proliferation. Cell. 2019;176:1098–1112.e18. doi: 10.1016/j.cell.2019.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhang X., Osaka T., Tsuneda S. Bacterial Metabolites Directly Modulate Farnesoid X Receptor Activity. Nutr. Metab. 2015;12:48. doi: 10.1186/s12986-015-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kovács T., Mikó E., Vida A., Sebő É., Toth J., Csonka T., Boratkó A., Ujlaki G., Lente G., Kovács P., et al. Cadaverine, a Metabolite of the Microbiome, Reduces Breast Cancer Aggressiveness through Trace Amino Acid Receptors. Sci. Rep. 2019;9:1300. doi: 10.1038/s41598-018-37664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ball H.J., Jusof F.F., Bakmiwewa S.M., Hunt N.H., Yuasa H.J. Tryptophan-Catabolizing Enzymes—Party of Three. Front. Immunol. 2014;5:485. doi: 10.3389/fimmu.2014.00485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Tennoune N., Andriamihaja M., Blachier F. Production of Indole and Indole-Related Compounds by the Intestinal Microbiota and Consequences for the Host: The Good, the Bad, and the Ugly. Microorganisms. 2022;10:930. doi: 10.3390/microorganisms10050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Sakurai K., Amano S., Enomoto K., Kashio M., Saito Y., Sakamoto A., Matsuo S., Suzuki M., Kitajima A., Hirano T., et al. Study of indoleamine 2,3-dioxygenase expression in patients with breast cancer. Gan Kagaku Ryoho. Cancer Chemother. 2005;32:1546–1549. [PubMed] [Google Scholar]
- 183.Liu Q., Zhai J., Kong X., Wang X., Wang Z., Fang Y., Wang J. Comprehensive Analysis of the Expressionand Prognosis for TDO2 in Breast Cancer. Mol. Ther. Oncolytics. 2020;17:153–168. doi: 10.1016/j.omto.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Sári Z., Mikó E., Kovács T., Jankó L., Csonka T., Lente G., Sebő É., Tóth J., Tóth D., Árkosy P., et al. Indolepropionic Acid, a Metabolite of the Microbiome, Has Cytostatic Properties in Breast Cancer by Activating AHR and PXR Receptors and Inducing Oxidative Stress. Cancers. 2020;12:2411. doi: 10.3390/cancers12092411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wyatt M., Greathouse K.L. Targeting Dietary and Microbial Tryptophan-Indole Metabolism as Therapeutic Approaches to Colon Cancer. Nutrients. 2021;13:1189. doi: 10.3390/nu13041189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhao Y., Wu Y., Wang M. Bioactive Substances of Plant Origin. In: Cheung P.C.K., Mehta B.M., editors. Handbook of Food Chemistry. Springer; Berlin/Heidelberg, Germany: 2015. pp. 967–1008. [Google Scholar]
- 187.Samtiya M., Aluko R.E., Dhewa T., Moreno-Rojas J.M. Potential Health Benefits of Plant Food-Derived Bioactive Components: An Overview. Foods. 2021;10:839. doi: 10.3390/foods10040839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bié J., Sepodes B., Fernandes P.C.B., Ribeiro M.H.L. Polyphenols in Health and Disease: Gut Microbiota, Bioaccessibility, and Bioavailability. Compounds. 2023;3:40–72. doi: 10.3390/compounds3010005. [DOI] [Google Scholar]
- 189.Park J.-H., Choi J.W., Ju E.J., Pae A.N., Park K.D. Antioxidant and Anti-Inflammatory Activities of a Natural Compound, Shizukahenriol, through Nrf2 Activation. Molecules. 2015;20:15989–16003. doi: 10.3390/molecules200915989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Diniz do Nascimento L., Barbosa de Moraes A.A., Santana da Costa K., Pereira Galúcio J.M., Taube P.S., Costa C.M.L., Neves Cruz J., de Aguiar Andrade E.H., Guerreiro de Faria L.J. Bioactive Natural Compounds and Antioxidant Activity of Essential Oils from Spice Plants: New Findings and Potential Applications. Biomolecules. 2020;10:988. doi: 10.3390/biom10070988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Silva A.M., Martins-Gomes C., Souto E.B., Schäfer J., Santos J.A., Bunzel M., Nunes F.M. Thymus Zygis Subsp. Zygis an Endemic Portuguese Plant: Phytochemical Profiling, Antioxidant, Anti-Proliferative and Anti-Inflammatory Activities. Antioxidants. 2020;9:482. doi: 10.3390/antiox9060482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Abraão A.S., Fernandes N., Silva A.M., Domínguez-Perles R., Barros A. Prunus lusitanica L. Fruits as a Novel Source of Bioactive Compounds with Antioxidant Potential: Exploring the Unknown. Antioxidants. 2022;11:1738. doi: 10.3390/antiox11091738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Rivas-Chacón L.d.M., Yanes-Díaz J., de Lucas B., Riestra-Ayora J.I., Madrid-García R., Sanz-Fernández R., Sánchez-Rodríguez C. Cocoa Polyphenol Extract Inhibits Cellular Senescence via Modulation of SIRT1 and SIRT3 in Auditory Cells. Nutrients. 2023;15:544. doi: 10.3390/nu15030544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tomas-Hernandez S., Garcia-Vallvé S., Pujadas G., Valls C., Ojeda-Montes M.J., Gimeno A., Cereto-Massagué A., Roca-Martinez J., Suárez M., Arola L., et al. Anti-Inflammatory and Proapoptotic Properties of the Natural Compound o-Orsellinaldehyde. J. Agric. Food Chem. 2018;66:10952–10963. doi: 10.1021/acs.jafc.8b00782. [DOI] [PubMed] [Google Scholar]
- 195.Li Y., Deng W., Wu L., Chen S., Zheng Z., Song H. Anti-Inflammatory Effects of Polyphenols from Plum (Prunus Salicina Lindl) on RAW264.7 Macrophages Induced by Monosodium Urate and Potential Mechanisms. Foods. 2023;12:254. doi: 10.3390/foods12020254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhou Z., He W., Tian H., Zhan P., Liu J. Thyme (Thymus Vulgaris L.) Polyphenols Ameliorate DSS-Induced Ulcerative Colitis of Mice by Mitigating Intestinal Barrier Damage, Regulating Gut Microbiota, and Suppressing TLR4/NF-ΚB-NLRP3 Inflammasome Pathways. Food Funct. 2023;14:1113–1132. doi: 10.1039/D2FO02523J. [DOI] [PubMed] [Google Scholar]
- 197.Artusa V., Ciaramelli C., D’Aloia A., Facchini F.A., Gotri N., Bruno A., Costa B., Palmioli A., Airoldi C., Peri F. Green and Roasted Coffee Extracts Inhibit Interferon-β Release in LPS-Stimulated Human Macrophages. Front. Pharmacol. 2022;13:806010. doi: 10.3389/fphar.2022.806010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Jia B., Shang J., Zeng H., Wang X., Fang M., Xu L., Liu X., Wu K., Gong Z., Yang Q. Hepatoprotective Effects of Rosmarinic Acid on Ovalbumin-Induced Intestinal Food Allergy Mouse Model. Molecules. 2023;28:788. doi: 10.3390/molecules28020788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Neves B.R.O., de Freitas S., Borelli P., Rogero M.M., Fock R.A. Delphinidin-3-O-Glucoside in Vitro Suppresses NF-ΚB and Changes the Secretome of Mesenchymal Stem Cells Affecting Macrophage Activation. Nutrition. 2023;105:111853. doi: 10.1016/j.nut.2022.111853. [DOI] [PubMed] [Google Scholar]
- 200.Daskalova E., Delchev S., Peeva Y., Vladimirova-Kitova L., Kratchanova M., Kratchanov C., Denev P. Antiatherogenic and Cardioprotective Effects of Black Chokeberry (Aronia Melanocarpa) Juice in Aging Rats. Evid. Based Complement. Altern. Med. 2015;2015:717439. doi: 10.1155/2015/717439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Humeniuk E., Adamczuk G., Kubik J., Adamczuk K., Józefczyk A., Korga-Plewko A. Cardioprotective Effect of Centaurea Castriferrei Borbás & Waisb Extract against Doxorubicin-Induced Cardiotoxicity in H9c2 Cells. Molecules. 2023;28:420. doi: 10.3390/molecules28010420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Li L., Ma H., Zhang Y., Jiang H., Xia B., Sberi H.A., Elhefny M.A., Lokman M.S., Kassab R.B. Protocatechuic Acid Reverses Myocardial Infarction Mediated by β-Adrenergic Agonist via Regulation of Nrf2/HO-1 Pathway, Inflammatory, Apoptotic, and Fibrotic Events. J. Biochem. Mol. Toxicol. 2023:e23270. doi: 10.1002/jbt.23270. [DOI] [PubMed] [Google Scholar]
- 203.D’Aloia A., Molteni L., Gullo F., Bresciani E., Artusa V., Rizzi L., Ceriani M., Meanti R., Lecchi M., Coco S., et al. Palmitoylethanolamide Modulation of Microglia Activation: Characterization of Mechanisms of Action and Implication for Its Neuroprotective Effects. Int. J. Mol. Sci. 2021;22:3054. doi: 10.3390/ijms22063054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Samani P., Costa S., Cai S. Neuroprotective Effects of Blueberries through Inhibition on Cholinesterase, Tyrosinase, Cyclooxygenase-2, and Amyloidogenesis. Nutraceuticals. 2023;3:39–57. doi: 10.3390/nutraceuticals3010004. [DOI] [Google Scholar]
- 205.An L., Li M., Zou C., Wang K., Zhang W., Huang X., Wang Y. Walnut Polyphenols and the Active Metabolite Urolithin A Improve Oxidative Damage in SH-SY5Y Cells by up-Regulating PKA/CREB/BDNF Signaling. Food Funct. 2023 doi: 10.1039/D2FO03310K. [DOI] [PubMed] [Google Scholar]
- 206.Laghezza Masci V., Bernini R., Villanova N., Clemente M., Cicaloni V., Tinti L., Salvini L., Taddei A.R., Tiezzi A., Ovidi E. In Vitro Anti-Proliferative and Apoptotic Effects of Hydroxytyrosyl Oleate on SH-SY5Y Human Neuroblastoma Cells. Int. J. Mol. Sci. 2022;23:12348. doi: 10.3390/ijms232012348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Luz J.R.D.d., López J.A., Ferreira M.P., de Sousa R.M., Silva S.V.e., Almeida M. das G.; Araujo-Silva, G. In Vitro Antithrombotic, Antitumor and Antiangiogenic Activities of Green Tea Polyphenols and Its Main Constituent Epigallocatechin-3-Gallate. Processes. 2022;11:76. doi: 10.3390/pr11010076. [DOI] [Google Scholar]
- 208.Cuciniello R., Di Meo F., Sulli M., Demurtas O.C., Tanori M., Mancuso M., Villano C., Aversano R., Carputo D., Baldi A., et al. Aglianico Grape Seed Semi-Polar Extract Exerts Anticancer Effects by Modulating MDM2 Expression and Metabolic Pathways. Cells. 2023;12:210. doi: 10.3390/cells12020210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Foti P., Ballistreri G., Timpanaro N., Rapisarda P., Romeo F.V. Prebiotic Effects of Citrus Pectic Oligosaccharides. Nat. Prod. Res. 2022;36:3173–3176. doi: 10.1080/14786419.2021.1948845. [DOI] [PubMed] [Google Scholar]
- 210.Nisa S., Bibi Y., Masood S., Ali A., Alam S., Sabir M., Qayyum A., Ahmed W., Alharthi S., Santali E.Y., et al. Isolation, Characterization and Anticancer Activity of Two Bioactive Compounds from Arisaema Flavum (Forssk.) Schott. Molecules. 2022;27:7932. doi: 10.3390/molecules27227932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.NK T., MP R. Biologically Active Naneoicglycolate of Aristolochia Littoralis Parodi Seed Extract with Anti-Bacterial Activity Induces Cytotoxicity and Apoptosis in A431 Human Skin Cancer Cell Line. Indian J. Nat. Prod. Resour. (IJNPR) [Former. Nat. Prod. Radiance (NPR)] 2022;13:301–309. doi: 10.56042/ijnpr.v13i3.53169. [DOI] [Google Scholar]
- 212.Ibrahim A., Siswandono S., Prajogo B.E.W. Anticancer Activity of Peronema Canescens Jack Leaves Extracts against Human Cells: HT-29 and HeLa in Vitro. Res. J. Pharm. Technol. Raipur. 2022;15:4739–4745. doi: 10.52711/0974-360X.2022.00796. [DOI] [Google Scholar]
- 213.Molina L., Williams D.E., Andersen R.J., Golsteyn R.M. Isolation of a Natural Product with Anti-Mitotic Activity from a Toxic Canadian Prairie Plant. Heliyon. 2021;7:e07131. doi: 10.1016/j.heliyon.2021.e07131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Gallo C., Dallaglio K., Bassani B., Rossi T., Rossello A., Noonan D.M., D’Uva G., Bruno A., Albini A. Hop Derived Flavonoid Xanthohumol Inhibits Endothelial Cell Functions via AMPK Activation. Oncotarget. 2016;7:59917–59931. doi: 10.18632/oncotarget.10990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Baci D., Gallazzi M., Cascini C., Tramacere M., De Stefano D., Bruno A., Noonan D.M., Albini A. Downregulation of Pro-Inflammatory and Pro-Angiogenic Pathways in Prostate Cancer Cells by a Polyphenol-Rich Extract from Olive Mill Wastewater. Int. J. Mol. Sci. 2019;20:307. doi: 10.3390/ijms20020307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Grynberg N.F., Carvalho M.G., Velandia J.R., Oliveira M.C., Moreira I.C., Braz-Filho R., Echevarria A. DNA Topoisomerase Inhibitors: Biflavonoids from Ouratea Species. Braz. J. Med. Biol. Res. 2002;35:819–822. doi: 10.1590/S0100-879X2002000700009. [DOI] [PubMed] [Google Scholar]
- 217.Rani V., BC R., GS M., Deshpande S., Venkatesan J., Appana Dalavi P., Prabhu A. Cytotoxic and Apoptotic Efficacy of Alkanna Tinctoria on Glioma Cells. Nat. Prod. Res. 2022:1–5. doi: 10.1080/14786419.2022.2155644. [DOI] [PubMed] [Google Scholar]
- 218.Sigstedt S.C., Hooten C.J., Callewaert M.C., Jenkins A.R., Romero A.E., Pullin M.J., Kornienko A., Lowrey T.K., Van Slambrouck S., Steelant W.F.A. Evaluation of Aqueous Extracts of Taraxacum Officinale on Growth and Invasion of Breast and Prostate Cancer Cells. Int. J. Oncol. 2008;32:1085–1090. doi: 10.3892/ijo.32.5.1085. [DOI] [PubMed] [Google Scholar]
- 219.Matić I.Z., Aljancić I., Vajs V., Jadranin M., Gligorijević N., Milosavljević S., Juranić Z.D. Cancer-Suppressive Potential of Extracts of Endemic Plant Helichrysum Zivojinii: Effects on Cell Migration, Invasion and Angiogenesis. Nat. Prod. Commun. 2013;8:1291–1296. doi: 10.1177/1934578X1300800927. [DOI] [PubMed] [Google Scholar]
- 220.Albini A., Festa M.M.G., Ring N., Baci D., Rehman M., Finzi G., Sessa F., Zacchigna S., Bruno A., Noonan D.M. A Polyphenol-Rich Extract of Olive Mill Wastewater Enhances Cancer Chemotherapy Effects, While Mitigating Cardiac Toxicity. Front. Pharmacol. 2021;12:694762. doi: 10.3389/fphar.2021.694762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Benedetto N., Calabrone L., Gutmańska K., Macrì N., Cerrito M.G., Ricotta R., Pelosi G., Bruno A., Noonan D.M., Albini A. An Olive Oil Mill Wastewater Extract Improves Chemotherapeutic Activity Against Breast Cancer Cells While Protecting From Cardiotoxicity. Front. Cardiovasc. Med. 2022;9:867867. doi: 10.3389/fcvm.2022.867867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Li M., Zhang H., Hu X., Liu Y., Liu Y., Song M., Wu R., Wu J. Isolation of a New Polysaccharide from Dandelion Leaves and Evaluation of Its Antioxidant, Antibacterial, and Anticancer Activities. Molecules. 2022;27:7641. doi: 10.3390/molecules27217641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Efferth T. Stem Cells, Cancer Stem-like Cells, and Natural Products. Planta Med. 2012;78:935–942. doi: 10.1055/s-0031-1298540. [DOI] [PubMed] [Google Scholar]
- 224.Moselhy J., Srinivasan S., Ankem M.K., Damodaran C. Natural Products That Target Cancer Stem Cells. Anticancer Res. 2015;35:5773–5788. [PMC free article] [PubMed] [Google Scholar]
- 225.Pistollato F., Giampieri F., Battino M. The Use of Plant-Derived Bioactive Compounds to Target Cancer Stem Cells and Modulate Tumor Microenvironment. Food Chem. Toxicol. 2015;75:58–70. doi: 10.1016/j.fct.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 226.Scarpa E.-S., Ninfali P. Phytochemicals as Innovative Therapeutic Tools against Cancer Stem Cells. Int. J. Mol. Sci. 2015;16:15727–15742. doi: 10.3390/ijms160715727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Taylor W.F., Jabbarzadeh E. The Use of Natural Products to Target Cancer Stem Cells. Am. J. Cancer Res. 2017;7:1588–1605. [PMC free article] [PubMed] [Google Scholar]
- 228.Palermo R., Ghirga F., Piccioni M.G., Bernardi F., Zhdanovskaya N., Infante P., Mori M. Natural Products Inspired Modulators of Cancer Stem Cells-Specific Signaling Pathways Notch and Hedgehog. Curr. Pharm. Des. 2018;24:4251–4269. doi: 10.2174/1381612825666190111124822. [DOI] [PubMed] [Google Scholar]
- 229.Das P.K., Zahan T., Abdur Rakib M., Khanam J.A., Pillai S., Islam F. Natural Compounds Targeting Cancer Stem Cells: A Promising Resource for Chemotherapy. Anticancer Agents Med. Chem. 2019;19:1796–1808. doi: 10.2174/1871520619666190704111714. [DOI] [PubMed] [Google Scholar]
- 230.Ganesan K., Jayachandran M., Xu B. Diet-Derived Phytochemicals Targeting Colon Cancer Stem Cells and Microbiota in Colorectal Cancer. Int. J. Mol. Sci. 2020;21:3976. doi: 10.3390/ijms21113976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Rahman M.A., Saha S.K., Rahman M.S., Uddin M.J., Uddin M.S., Pang M.-G., Rhim H., Cho S.-G. Molecular Insights Into Therapeutic Potential of Autophagy Modulation by Natural Products for Cancer Stem Cells. Front. Cell Dev. Biol. 2020;8:283. doi: 10.3389/fcell.2020.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Gairola K., Gururani S., Bahuguna A., Garia V., Pujari R., Dubey S.K. Natural Products Targeting Cancer Stem Cells: Implications for Cancer Chemoprevention and Therapeutics. J. Food Biochem. 2021;45:e13772. doi: 10.1111/jfbc.13772. [DOI] [PubMed] [Google Scholar]
- 233.Gupta P.K., Saraff M., Gahtori R., Negi N., Tripathi S.K., Kumar J., Kumar S., Aldhayan S.H., Dhanasekaran S., Abomughaid M.M., et al. Phytomedicines Targeting Cancer Stem Cells: Therapeutic Opportunities and Prospects for Pharmaceutical Development. Pharmaceuticals. 2021;14:676. doi: 10.3390/ph14070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Meerson A., Khatib S., Mahajna J. Natural Products Targeting Cancer Stem Cells for Augmenting Cancer Therapeutics. Int. J. Mol. Sci. 2021;22:13044. doi: 10.3390/ijms222313044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Hashem S., Ali T.A., Akhtar S., Nisar S., Sageena G., Ali S., Al-Mannai S., Therachiyil L., Mir R., Elfaki I., et al. Targeting Cancer Signaling Pathways by Natural Products: Exploring Promising Anti-Cancer Agents. Biomed. Pharmacother. 2022;150:113054. doi: 10.1016/j.biopha.2022.113054. [DOI] [PubMed] [Google Scholar]
- 236.Singh D., Pandey H., Singh V. Handbook of Research on Natural Products and Their Bioactive Compounds as Cancer Therapeutics. IGI Global; Hershey, PA, USA: 2022. Natural Products That Target Cancer Stem Cells; pp. 169–186. [Google Scholar]
- 237.Bonuccelli G., Sotgia F., Lisanti M.P. Identification of Natural Products and FDA-Approved Drugs for Targeting Cancer Stem Cell (CSC) Propagation. Aging. 2022;14:9466–9483. doi: 10.18632/aging.204412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Kawabata K., Yoshioka Y., Terao J. Role of Intestinal Microbiota in the Bioavailability and Physiological Functions of Dietary Polyphenols. Molecules. 2019;24:370. doi: 10.3390/molecules24020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Nishiyama K., Sugiyama M., Mukai T. Adhesion Properties of Lactic Acid Bacteria on Intestinal Mucin. Microorganisms. 2016;4:34. doi: 10.3390/microorganisms4030034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Choi H.S., Kim J.-H., Kim S.-L., Deng H.-Y., Lee D., Kim C.S., Yun B.-S., Lee D.-S. Catechol Derived from Aronia Juice through Lactic Acid Bacteria Fermentation Inhibits Breast Cancer Stem Cell Formation via Modulation Stat3/IL-6 Signaling Pathway. Mol. Carcinog. 2018;57:1467–1479. doi: 10.1002/mc.22870. [DOI] [PubMed] [Google Scholar]
- 241.Cerdá B., Tomás-Barberán F.A., Espín J.C. Metabolism of Antioxidant and Chemopreventive Ellagitannins from Strawberries, Raspberries, Walnuts, and Oak-Aged Wine in Humans: Identification of Biomarkers and Individual Variability. J. Agric. Food Chem. 2005;53:227–235. doi: 10.1021/jf049144d. [DOI] [PubMed] [Google Scholar]
- 242.Seeram N.P., Henning S.M., Zhang Y., Suchard M., Li Z., Heber D. Pomegranate Juice Ellagitannin Metabolites Are Present in Human Plasma and Some Persist in Urine for up to 48 Hours. J. Nutr. 2006;136:2481–2485. doi: 10.1093/jn/136.10.2481. [DOI] [PubMed] [Google Scholar]
- 243.Cortés-Martín A., Selma M.V., Tomás-Barberán F.A., González-Sarrías A., Espín J.C. Where to Look into the Puzzle of Polyphenols and Health? The Postbiotics and Gut Microbiota Associated with Human Metabotypes. Mol. Nutr. Food Res. 2020;64:e1900952. doi: 10.1002/mnfr.201900952. [DOI] [PubMed] [Google Scholar]
- 244.Núñez-Sánchez M.Á., Karmokar A., González-Sarrías A., García-Villalba R., Tomás-Barberán F.A., García-Conesa M.T., Brown K., Espín J.C. In Vivo Relevant Mixed Urolithins and Ellagic Acid Inhibit Phenotypic and Molecular Colon Cancer Stem Cell Features: A New Potentiality for Ellagitannin Metabolites against Cancer. Food Chem. Toxicol. 2016;92:8–16. doi: 10.1016/j.fct.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 245.González-Sarrías A., Miguel V., Merino G., Lucas R., Morales J.C., Tomás-Barberán F., Alvarez A.I., Espín J.C. The Gut Microbiota Ellagic Acid-Derived Metabolite Urolithin A and Its Sulfate Conjugate Are Substrates for the Drug Efflux Transporter Breast Cancer Resistance Protein (ABCG2/BCRP) J. Agric. Food Chem. 2013;61:4352–4359. doi: 10.1021/jf4007505. [DOI] [PubMed] [Google Scholar]
- 246.González-Sarrías A., Tomé-Carneiro J., Bellesia A., Tomás-Barberán F.A., Espín J.C. The Ellagic Acid-Derived Gut Microbiota Metabolite, Urolithin A, Potentiates the Anticancer Effects of 5-Fluorouracil Chemotherapy on Human Colon Cancer Cells. Food Funct. 2015;6:1460–1469. doi: 10.1039/C5FO00120J. [DOI] [PubMed] [Google Scholar]
- 247.Cañestro C., Catchen J.M., Rodríguez-Marí A., Yokoi H., Postlethwait J.H. Consequences of Lineage-Specific Gene Loss on Functional Evolution of Surviving Paralogs: ALDH1A and Retinoic Acid Signaling in Vertebrate Genomes. PLoS Genet. 2009;5:e1000496. doi: 10.1371/journal.pgen.1000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Mezquita B., Mezquita C. Two Opposing Faces of Retinoic Acid: Induction of Stemness or Induction of Differentiation Depending on Cell-Type. Biomolecules. 2019;9:567. doi: 10.3390/biom9100567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Tang X.-H., Gudas L.J. Retinoids, Retinoic Acid Receptors, and Cancer. Annu. Rev. Pathol. 2011;6:345–364. doi: 10.1146/annurev-pathol-011110-130303. [DOI] [PubMed] [Google Scholar]
- 250.Hunsu V.O., Facey C.O.B., Fields J.Z., Boman B.M. Retinoids as Chemo-Preventive and Molecular-Targeted Anti-Cancer Therapies. Int. J. Mol. Sci. 2021;22:7731. doi: 10.3390/ijms22147731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Bouriez D., Giraud J., Gronnier C., Varon C. Efficiency of All-Trans Retinoic Acid on Gastric Cancer: A Narrative Literature Review. Int. J. Mol. Sci. 2018;19:3388. doi: 10.3390/ijms19113388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Karsy M., Albert L., Tobias M.E., Murali R., Jhanwar-Uniyal M. All-Trans Retinoic Acid Modulates Cancer Stem Cells of Glioblastoma Multiforme in an MAPK-Dependent Manner. Anticancer Res. 2010;30:4915–4920. [PubMed] [Google Scholar]
- 253.Lim Y.C., Kang H.J., Kim Y.S., Choi E.C. All-Trans-Retinoic Acid Inhibits Growth of Head and Neck Cancer Stem Cells by Suppression of Wnt/β-Catenin Pathway. Eur. J. Cancer. 2012;48:3310–3318. doi: 10.1016/j.ejca.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 254.Li R.-J., Ying X., Zhang Y., Ju R.-J., Wang X.-X., Yao H.-J., Men Y., Tian W., Yu Y., Zhang L., et al. All-Trans Retinoic Acid Stealth Liposomes Prevent the Relapse of Breast Cancer Arising from the Cancer Stem Cells. J. Control. Release. 2011;149:281–291. doi: 10.1016/j.jconrel.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 255.Sun R., Liu Y., Li S.-Y., Shen S., Du X.-J., Xu C.-F., Cao Z.-T., Bao Y., Zhu Y.-H., Li Y.-P., et al. Co-Delivery of All-Trans-Retinoic Acid and Doxorubicin for Cancer Therapy with Synergistic Inhibition of Cancer Stem Cells. Biomaterials. 2015;37:405–414. doi: 10.1016/j.biomaterials.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 256.Yao W., Wang L., Huang H., Li X., Wang P., Mi K., Cheng J., Liu H., Gu C., Huang L., et al. All-Trans Retinoic Acid Reduces Cancer Stem Cell-like Cell-Mediated Resistance to Gefitinib in NSCLC Adenocarcinoma Cells. BMC Cancer. 2020;20:315. doi: 10.1186/s12885-020-06818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Berardi D.E., Ariza Bareño L., Amigo N., Cañonero L., Pelagatti M.d.L.N., Motter A.N., Taruselli M.A., Díaz Bessone M.I., Cirigliano S.M., Edelstein A., et al. All-Trans Retinoic Acid and Protein Kinase C α/Β1 Inhibitor Combined Treatment Targets Cancer Stem Cells and Impairs Breast Tumor Progression. Sci. Rep. 2021;11:6044. doi: 10.1038/s41598-021-85344-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.MacDonagh L., Santiago R.M., Gray S.G., Breen E., Cuffe S., Finn S.P., O’Byrne K.J., Barr M.P. Exploitation of the Vitamin A/Retinoic Acid Axis Depletes ALDH1-Positive Cancer Stem Cells and Re-Sensitises Resistant Non-Small Cell Lung Cancer Cells to Cisplatin. Transl. Oncol. 2021;14:101025. doi: 10.1016/j.tranon.2021.101025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Bonakdar M., Czuba L.C., Han G., Zhong G., Luong H., Isoherrannen N., Vaishnava S. Gut Commensals Expand Vitamin A Metabolic Capacity of the Mammalian Host. Cell Host Microbe. 2022;30:1084–1092.e5. doi: 10.1016/j.chom.2022.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Ubago-Guisado E., Rodríguez-Barranco M., Ching-López A., Petrova D., Molina-Montes E., Amiano P., Barricarte-Gurrea A., Chirlaque M.-D., Agudo A., Sánchez M.-J. Evidence Update on the Relationship between Diet and the Most Common Cancers from the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: A Systematic Review. Nutrients. 2021;13:3582. doi: 10.3390/nu13103582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Kamal N., Ilowefah M.A., Hilles A.R., Anua N.A., Awin T., Alshwyeh H.A., Aldosary S.K., Jambocus N.G.S., Alosaimi A.A., Rahman A., et al. Genesis and Mechanism of Some Cancer Types and an Overview on the Role of Diet and Nutrition in Cancer Prevention. Molecules. 2022;27:1794. doi: 10.3390/molecules27061794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Bamia C., Lagiou P., Buckland G., Grioni S., Agnoli C., Taylor A.J., Dahm C.C., Overvad K., Olsen A., Tjønneland A., et al. Mediterranean Diet and Colorectal Cancer Risk: Results from a European Cohort. Eur. J. Epidemiol. 2013;28:317–328. doi: 10.1007/s10654-013-9795-x. [DOI] [PubMed] [Google Scholar]
- 263.Schwingshackl L., Hoffmann G. Adherence to Mediterranean Diet and Risk of Cancer: A Systematic Review and Meta-Analysis of Observational Studies. Int. J. Cancer. 2014;135:1884–1897. doi: 10.1002/ijc.28824. [DOI] [PubMed] [Google Scholar]
- 264.Rosato V., Guercio V., Bosetti C., Negri E., Serraino D., Giacosa A., Montella M., La Vecchia C., Tavani A. Mediterranean Diet and Colorectal Cancer Risk: A Pooled Analysis of Three Italian Case-Control Studies. Br. J. Cancer. 2016;115:862–865. doi: 10.1038/bjc.2016.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Praud D., Bertuccio P., Bosetti C., Turati F., Ferraroni M., La Vecchia C. Adherence to the Mediterranean Diet and Gastric Cancer Risk in Italy. Int. J. Cancer. 2014;134:2935–2941. doi: 10.1002/ijc.28620. [DOI] [PubMed] [Google Scholar]
- 266.Bosetti C., Turati F., Dal Pont A., Ferraroni M., Polesel J., Negri E., Serraino D., Talamini R., La Vecchia C., Zeegers M.P. The Role of Mediterranean Diet on the Risk of Pancreatic Cancer. Br. J. Cancer. 2013;109:1360–1366. doi: 10.1038/bjc.2013.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Demetriou C.A., Hadjisavvas A., Loizidou M.A., Loucaides G., Neophytou I., Sieri S., Kakouri E., Middleton N., Vineis P., Kyriacou K. The Mediterranean Dietary Pattern and Breast Cancer Risk in Greek-Cypriot Women: A Case-Control Study. BMC Cancer. 2012;12:113. doi: 10.1186/1471-2407-12-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Turati F., Carioli G., Bravi F., Ferraroni M., Serraino D., Montella M., Giacosa A., Toffolutti F., Negri E., Levi F., et al. Mediterranean Diet and Breast Cancer Risk. Nutrients. 2018;10:326. doi: 10.3390/nu10030326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Laudisio D., Castellucci B., Barrea L., Pugliese G., Savastano S., Colao A., Muscogiuri G. Mediterranean Diet and Breast Cancer Risk: A Narrative Review. Minerva Endocrinol. 2021;46:441–452. doi: 10.23736/S2724-6507.20.03266-6. [DOI] [PubMed] [Google Scholar]
- 270.Turati F., Bravi F., Polesel J., Bosetti C., Negri E., Garavello W., Taborelli M., Serraino D., Libra M., Montella M., et al. Adherence to the Mediterranean Diet and Nasopharyngeal Cancer Risk in Italy. Cancer Causes Control. 2017;28:89–95. doi: 10.1007/s10552-017-0850-x. [DOI] [PubMed] [Google Scholar]
- 271.Fortes C., Forastiere F., Farchi S., Mallone S., Trequattrinni T., Anatra F., Schmid G., Perucci C.A. The Protective Effect of the Mediterranean Diet on Lung Cancer. Nutr. Cancer. 2003;46:30–37. doi: 10.1207/S15327914NC4601_04. [DOI] [PubMed] [Google Scholar]
- 272.Itsiopoulos C., Hodge A., Kaimakamis M. Can the Mediterranean Diet Prevent Prostate Cancer? Mol. Nutr. Food Res. 2009;53:227–239. doi: 10.1002/mnfr.200800207. [DOI] [PubMed] [Google Scholar]
- 273.Bravi F., Spei M.-E., Polesel J., Di Maso M., Montella M., Ferraroni M., Serraino D., Libra M., Negri E., La Vecchia C., et al. Mediterranean Diet and Bladder Cancer Risk in Italy. Nutrients. 2018;10:1061. doi: 10.3390/nu10081061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Botero L.E., Delgado-Serrano L., Cepeda Hernandez M.L., Del Portillo Obando P., Zambrano Eder M.M. The Human Microbiota: The Role of Microbial Communities in Health and Disease. Acta Biológica Colomb. 2016;21:5–15. [Google Scholar]
- 275.Karkman A., Lehtimäki J., Ruokolainen L. The Ecology of Human Microbiota: Dynamics and Diversity in Health and Disease. Ann. N. Y. Acad. Sci. 2017;1399:78–92. doi: 10.1111/nyas.13326. [DOI] [PubMed] [Google Scholar]
- 276.Wang B., Yao M., Lv L., Ling Z., Li L. The Human Microbiota in Health and Disease. Engineering. 2017;3:71–82. doi: 10.1016/J.ENG.2017.01.008. [DOI] [Google Scholar]
- 277.Tungland B. Human Microbiota in Health and Disease: From Pathogenesis to Therapy. Academic Press; Cambridge, MA, USA: 2018. [Google Scholar]
- 278.Martínez J.E., Vargas A., Pérez-Sánchez T., Encío I.J., Cabello-Olmo M., Barajas M. Human Microbiota Network: Unveiling Potential Crosstalk between the Different Microbiota Ecosystems and Their Role in Health and Disease. Nutrients. 2021;13:2905. doi: 10.3390/nu13092905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Artemev A., Naik S., Pougno A., Honnavar P., Shanbhag N.M. The Association of Microbiome Dysbiosis With Colorectal Cancer. Cureus. 2022;14:e22156. doi: 10.7759/cureus.22156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Fong W., Li Q., Yu J. Gut Microbiota Modulation: A Novel Strategy for Prevention and Treatment of Colorectal Cancer. Oncogene. 2020;39:4925–4943. doi: 10.1038/s41388-020-1341-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Rowland I., Gibson G., Heinken A., Scott K., Swann J., Thiele I., Tuohy K. Gut Microbiota Functions: Metabolism of Nutrients and Other Food Components. Eur. J. Nutr. 2018;57:1–24. doi: 10.1007/s00394-017-1445-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created. Data sharing is not applicable to this review.