Abstract
Ovarian cancer represents a major health concern for the female population: there is no obvious cause, it is frequently misdiagnosed, and it is characterized by a poor prognosis. Additionally, patients are inclined to recurrences because of metastasis and poor treatment tolerance. Combining innovative therapeutic techniques with established approaches can aid in improving treatment outcomes. Because of their multi-target actions, long application history, and widespread availability, natural compounds have particular advantages in this connection. Thus, effective therapeutic alternatives with improved patient tolerance hopefully can be identified within the world of natural and nature-derived products. Moreover, natural compounds are generally perceived to have more limited adverse effects on healthy cells or tissues, suggesting their potential role as valid treatment alternatives. In general, the anticancer mechanisms of such molecules are connected to the reduction of cell proliferation and metastasis, autophagy stimulation and improved response to chemotherapeutics. This review aims at discussing the mechanistic insights and possible targets of natural compounds against ovarian cancer, from the perspective of medicinal chemists. In addition, an overview of the pharmacology of natural products studied to date for their potential application towards ovarian cancer models is presented. The chemical aspects as well as available bioactivity data are discussed and commented on, with particular attention to the underlying molecular mechanism(s).
Keywords: ovarian cancer, natural compounds, semi-synthetic compounds, medicinal chemistry, anti-metastasis, apoptosis
1. Introduction
Among gynecologic cancers, ovarian cancer is categorized as the third most prevalent cancer after cervical and uterine cancer, having high mortality rates in female subjects [1]. Epithelial ovarian malignancies, which include serous, mucinous, endometrioid, metastatic and clear cell carcinoma, represent the majority of ovarian diseases [2]. Intracavitary implantation, hematic and lymphatic pathways can all be exploited to transmit epithelial ovarian cancer, and the main route of spread is intraperitoneal metastases [3,4]. In the initial phases of the disease, patients are commonly asymptomatic, and 70% of patients are diagnosed at a later stage [5].
Nowadays, cytoreductive surgeries followed by platinum/paclitaxel-based chemotherapy are being considered as first-line approaches. Patients who receive this treatment, on the other hand, are prone to develop chemotherapeutic resistance and cumulative adverse effects, including nephrotoxicity [6]. To date, treatment of ovarian cancer is considered among the most challenging tasks in the field of oncology owing to its low survival rate (5 years < 40%) [7]. Consequently, novel drugs and alternative therapeutics for treatment or prevention of progression of ovarian cancer are needed.
Due to the adverse side effects associated with standard anticancer treatment, plant-derived products, alone and/or in combination with conventional anticancer agents, are being explored nowadays as adjuvant treatment to minimize adverse side effects [8].
Recently, several ovarian cancer prevention and early detection strategies have not shown expected or satisfactory results, which is partially attributable to the disease’s heterogeneity [9]. Increased DNA lesion repair, aberrant intracellular signal transmission, and drug metabolic inactivation are all promoted by genetic changes. Complete remission has instead been achieved by combining surgical intervention with genetic analysis [10]. In this context, the PARP inhibitor olaparib is administered to patients with BRCA1 or BRCA2 mutations [11]. It is also common practice to treat patients who have experienced a relapse after receiving platinum-based chemotherapy. Due to rapid tumor development and chemotherapy resistance, the period between treatments decreases progressively after a relapse.
As anticipated, to increase the survival quality of patients undergoing chemotherapeutic treatment, novel approaches are required. Botanical components are naturally occurring antioxidants or alkaloids with a long history in ethnopharmacology and characterized by the potential of being employed as therapeutic resources [12,13,14]. Natural products derived from plants are commonly thought of as nutritional supplements [15], meanwhile, plant-based constituents and products may be used as adjuvant therapies against ovarian cancer and for reduction of metastatic tumor size, and some examples have been reported in the literature.
With this review, we aim at highlighting the beneficial impacts of natural products, as single molecules and in combination, on ovarian cancer. Several scientific databases (Google Scholar, PubMed, Embase, etc.) were searched for records published from 2000 onwards by using the following keywords: ovarian cancer, etiology, risk of ovarian cancer incidence, natural products and ovarian cancer, ovarian cancer progression and chemopreventive potential of natural compounds [16,17,18,19,20,21,22,23,24,25,26,27]. The review is organized into sections covering etiology, risk factors and molecular mechanisms of ovarian cancer development. Then, cellular events and biochemical pathways targeted by natural compounds are discussed. Eventually, a focus on some relevant and widely studied molecules are presented.
2. Etiology of Ovarian Cancer
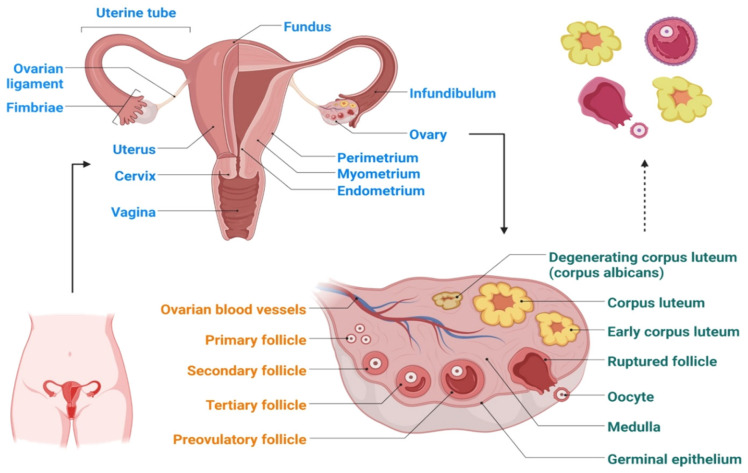
Each ovary is approximately 3.5 cm long, 2 cm wide and 1 cm thick. It has an oval, solid structure that is about the size of an almond. The ovaries are located in ovarian fossae, which are small depressions on either side of the uterus in the lateral walls of the pelvic cavity. Characterizing the variation in the ovarian surface epithelium (OSE) in accordance with pre-cancer lesions (intraepithelial neoplasia) is quite difficult owing to the intra-abdominal localization of the ovaries (Figure 1) and prevalence of disease [28]. Therefore, knowledge regarding earlier genetic and molecular events that are linked with ovarian cancer is still very limited. As a result, the causes of ovarian cancer are not very clear, and this is particularly true for epithelial ovarian cancer. The alterations in the OSE are a contributing factor in ovarian cancer, as shown by the following evidence: (1) the OCP, a widely used strategy of ovarian cancer prevention, triggers cancer-preventive molecular pathways in the OSE [29]; (2) evidence of dysplastic, premalignant alterations in the OSE can be detected using conventional techniques [30]; (3) colocalization of dysplastic specimens in the OSE of ovaries with loss of cancer-suppressing action or overexpression of cyclooxygenase 2 [31]; and (4) evolution from a nonmalignant to a cancerous OSE in a some early ovarian malignancies [32].
Figure 1.
Schematic representation of the ovary structure.
Another hypothesis postulates that the cells that develop in the fallopian tube serve as the foundation for ovarian cancer growth [33]. This hypothesis, while it is still only a theory, is supported by the fact that the majority of ovarian cancer cells show histological features similar to those of the fallopian tube itself. Additionally, an abnormally high incidence of histologic and molecular markers linked to dysplasia at the fimbriated end of the fallopian tube is observed in preventive oophorectomy cases from high-risk women [34]. The probability of fallopian tube cancer development is noticeably increased in women who have a BRCA-related inherent ovarian disease risk. Furthermore, a thorough examination of the fallopian tubes in women with serous pelvic cancer has revealed a high likelihood of endosalpinx inclusion or concurrent tubal carcinomas. Similarly, p53 changes can be retrieved in both the pelvic and fallopian tube lesions, which suggests the possible hereditary character of the disease [35,36]. Additionally, p53 markers have been found in fallopian tubes removed for non-carcinogenic causes in women within a population bearing risk factors of ovarian cancer [37]. The fimbriated end of the fallopian chamber may evolve toward neoplasia when dysplastic cells shed from the OSE, or even when taking into consideration ovarian stromal materials provided during ovulation [38].
3. Risk Factors for Ovarian Cancer
Because of the rate of ovulatory cycles, it has been demonstrated that women who have early menarche (age < 12) and late menopause (age > 50) have a greater risk of ovarian cancer. In particular, early menarche and late menopause enhance the possibility of disease development by 1.1 to 1.5 times and 1.4–4.6 times, respectively. Breastfeeding, pregnancy, and the usage of ovulation-restricting oral contraceptives also all represent risk factors [39,40]. Endometriosis and ovarian cancer have been linked in epidemiological research, however the mechanism is uncertain [41]. Family history for ovarian cancer is known to be one of the most significant risk factors. BRCA1 and BRCA2 mutations have been associated with a high risk of ovarian and breast cancer development [39]. More specifically, women having mutations in BRCA1 and BRCA2 are thought to have elevated risk for the development of ovarian cancer [42]. Located on chromosome 17q21, BRCA1 is an onco-suppressor gene, while BRCA2 is located on chromosome 13q [39]. The codon is prematurely terminated when these genes are removed or inserted, resulting in a shortened protein. The mutation of such genes promotes uncontrolled cell proliferation because they play a role in chromatin remodeling. More specifically, BRCA1 and BRCA2 mutations have been linked to an increased risk of developing ovarian cancer by 50% and 20%, respectively [40,42,43,44,45,46,47,48,49,50,51]
4. Ovarian Cancer Carcinogenesis and Progression: Molecular Mechanisms
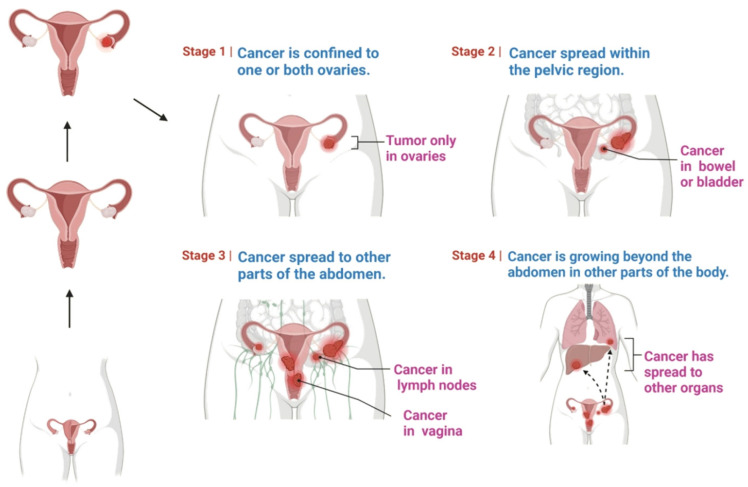
The stages of cancer progression are demonstrated in Figure 2: a higher number, such as stage 4, denotes that the cancer has progressed more widely. Several hypotheses have been formulated to explain the mechanisms underlying disease onset and progression.
Figure 2.
Stages of ovarian cancer, which vary from stage 1 to stage 4.
In this context, the cancer stem cell hypothesis deserves particular attention as it has been introduced to explain many cancer complications, resulting in drug resistance, metastases, and recurrence, that are related to disease progression. Cancer stem cells are a small population of tumor cells that contribute to the formation of phenotypically diverse tumors. Their hallmarks have been recently demonstrated to be targeted also by natural compounds to combat cell invasion and recurrence [52,53,54].
Several other hypotheses have been proposed to clarify the mechanism of ovarian cancer progression. Repeated ovulation, when associated with repetitive ovarian epithelial damage and repair, raises the risk of DNA damage and carcinogenesis, according to the so-called ovulation theory [55]. As a result, having a higher number of ovulations raises the risk of ovarian cancer. In rats, hyper-ovulation raises the chance of ovarian cancer progression substantially. According to experimental studies, ovulation may produce carcinogenesis by stimulating multiple cellular actions [56]. Therefore, incessant ovulation increases the risk of mutagenicity due to transformation of injured OSE cells. Bradykinin and other vasoactive mediators, as well as leukocytes and prostaglandins, are stimulated during ovulation [57].
The gonadotrophin hypothesis suggests that increased levels of gonadotrophins drive epithelial neoplastic change either straightforwardly or by implication through steroidogenesis [58]. On the other hand, it has been noted that progestins can induce apoptotic pathways and decrease the chance of growth alterations, while estrogens can promote the development of the disease [59]. In this context, carcinogenesis may also likewise connected to the use of conceptive therapeutics [60].
Epithelial ovarian cancer cells can relocate to the peritoneal cavity, bringing about ascites and, potentially, immunosuppression that favors cancer development. Lysophosphatidic acid inhibits TNF receptor apoptosis-inducing ligand (TRAIL)-induced apoptosis by activating the Pl3K/Akt pathway [61]. In ascites and plasma samples from epithelial ovarian cancer specimens, a recent report found a huge change in cytokines, demonstrating in particular a unique variety in ascites cytokines [62]. Additionally, it has been noted that protein kinase C (PKC), Akt, lysophosphatidyl acid (LPA), and interleukin-6 (IL-6) are increased in ovarian cancer [63]. According to another report, ovarian cancer cells use the Akt/nuclear factor kappa B (NF-kB) pathway to produce IL-6, IL-8, and VEGF [64]. PKC likewise plays a critical role in the regulation of various pathways. More specifically, in ovarian cancer patients, PKC dysregulation has been related to carcinogenesis and resistance to treatments [65]. The abovementioned inflammatory agents and pathways result in increased ovarian cancer-related inflammation. Generally, inflammation then induces the production of various toxic oxidants that cause direct harm to DNA, proteins, and lipids, enhancing carcinogenesis [66]. In addition to this, inflammation is linked to increased cellular proliferation. Excessive cellular divisions then result in DNA repair replication errors, causing increasing mutagenesis [67]. Ovarian cancer cells release several inflammation mediators, including cytokines and interleukins [68]. In ovarian cancers, elevated levels of prostaglandins are observed as compared with normal cells [69], and prostaglandins promote cancer cell invasion at high concentrations [70]. Oxidative stress is another significant event associated with ovarian cancer. Compared with healthy women, patients with ovarian cancer show decreased antioxidant species and increased levels of oxidative stress [71]. More specifically, in ovarian cancer epithelial cells, some studies have reported oxidative stress conditions, with decreased concentrations of antioxidative enzymes. In addition to defective apoptosis, nitric oxide (NO), myeloperoxidase (MPO), NAD(P)H oxidase, and extended combinations of these enzymes have all been observed in ovarian cancer tissues. Besides, ovarian cancers have more elevated levels of caspase-3 nitrosylation, bringing about a huge decrease in caspase-3 capacity. MPO is a significantly relevant pro-oxidant chemical forming NO [72,73,74]. According to several experimental reports, high MPO levels have been detected in ovarian cancer cells [75]. At the molecular level, MPO directs apoptosis, severe reactions, and drug resistance [76]. MPO prompts the formation of reactive oxygen species (ROS), causing oxidative stress and influencing iron redox balance [72]. As a result, oxidative stress may play a crucial role in the progression of ovarian cancer [77].
5. Molecular Mechanisms Underlying Bioactivity of Natural Products
Mounting evidence demonstrates that plant-derived natural components like phytochemicals can have a role as adjuvants to conventional chemotherapy and may represent promising options for the future development of treatments against ovarian cancer [78,79].
The interest of researchers in the identification of small molecules acting as anticancer agents towards ovarian cancer is constantly growing, and this is testified by the increasing number of contributions in the field. In the 2019–2021 timeframe, some relevant reviews on this topic were published. Shafabakhsh and Asemi as well as Vafadar et al. reviewed the antiproliferative potential of one of the most widely studied natural compounds, quercetin, in the context of ovarian cancer [80,81]. On the other hand, Kubczak et al. reviewed the molecular targets for anticancer natural compounds identified so far, and organized their contribution into sections according to chemical classes [82]. Eventually, Wu et al. focused their attention on ovarian cancer, and classified the studied compounds according to the mechanisms by which natural molecules may act [83].
In this part of the review, we aim at providing a comprehensive and updated overview of natural compounds studied as anticancer agents in the context of ovarian cancer. With respect to previous contributions in the field, we expanded the list of possible molecular mechanisms according to the latest reports. Moreover, in the following sections, we provide a focus on the most promising compounds for which a higher amount of data can be retrieved in the recent literature. Eventually, we discuss the potential of semi-synthetic derivatives of natural compounds with enhanced anticancer activity.
More specifically, the current section briefly reports the role of natural constituents against ovarian cancer, and their proposed mode of action is also be discussed herein. In general, natural compounds potentially modulate chemotherapeutic resistance, autophagy, inflammation, propagation, and apoptosis [84]. A brief overview of the several cellular events is reported below. The studied molecules have been grouped according to the proposed mechanism of action.
5.1. Compounds Inducing Apoptosis and Cytotoxicity and Inhibiting Proliferation
Apoptosis is a kind of organized cell death, and it represents a crucial process for maintenance of homeostasis [85]. The induction of apoptosis and inhibition of cell proliferation are the main general mechanisms through which several natural compounds exert their anticancer role [86,87], and the main examples in the field of ovarian cancer are reported below.
Pro-apoptotic activity in ovarian cancer cell lines has been reported for procyanidins from cocoa [88], zeylenone from Uvaria grandiflora Roxb [89], and sanguiin H-6, a natural constituent present in red raspberry [90].
Similarly, methyl lucidone from L. erythrocarpa has cytotoxic effects and induced apoptosis in SKOV-3 and OVCAR-8 cell lines [91], while tanshinones from Salvia miltiorrhiza (Danshen), such as cryptotanshinone, tanshinone-I (Tan-I) and tanshinone-IIA (TII-A), were reported to induce apoptosis by interaction with TNF receptors. In particular, TII-A showed the highest activity [92].
Sulforafane (SFN) is a biologically relevant component found in cruciferous vegetables, including broccoli, and it suppressed cell growth by downregulating the cell cycle regulators cyclin D1 and cyclin-dependent kinases 4 and 6 [93].
Additionally, dihydroartemisinin (DHA), traditionally used to treat fever symptoms and recently investigated as a potential tool against severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) [94,95], can be found in Artemisia annua [96] and induced apoptosis in ovarian cancer cells [97].
Reduced cell proliferation was also achieved with use of berbamine, an alkaloid obtained from Berberis amurensis, through the involvement of the Wnt/catenin signaling pathway [98].
Epigallocatechin gallate (EGCG), one of the main catechins found in green tea, inhibited the development and proliferation of OVCAR3 [99], as well as Pulchrin A from Enicosanthellum pulchrum [100].
Kadsuphilactone B, a nortriterpenoid from Schisandra chinensis (Turcz) B. [101], resveratrol [102] and curcumin [103], which will be discussed in a separate section of the review, represent other examples of compounds promoting ovarian cancer cell death.
Other naturally occurring mixtures, such as those containing silybin analogs, demonstrated a potential inhibitory effect on cancer development, including inhibition of elongation, pro-apoptotic effects, and cytotoxicity [104]. For a detailed list of extracts, the reader should refer to the review by Wu et al. [83].
Overall, the main involved mechanisms targeted by the abovementioned compounds include induction of DNA damage, caspase-3, reduction of Janus family tyrosine kinase (p-JAK), Akt phosporilation and SERCA, increased apoptosis-inducing factor (AIF), PARP and Bcl-2 family proteins.
5.2. Interference with Reactive Oxygen Species (ROS) Damage and with Nucleic Acid Repair
Excessive oxidative stress is generally believed to play a role in a wide range of diseases, from inflammation to cancer. Carcinogenesis has been connected to enhanced ROS formation and damage [105], and several studies have highlighted the involvement of antioxidant and radical scavenger properties of natural and synthetic compounds [106,107].
In various experiments, the abovementioned antioxidant SFN induced apoptosis in the OVCAR3, OVCAR4, OVCAR5, and SKOV3 cell lines and diminished cancer development in vivo [108].
Several flavones, including quercetin [109], and isoflavones have been previously reported to show antiproliferative activity [110]. Quercetin is a relevant natural compound that has been widely studied, and the properties of this molecule will be overviewed in another section of this review. It has been demonstrated that the isoflavone formononetin (FMN), which is found in red clovers and soy, has anticancer and cancer-preventive actions in a variety of cell types. FMN combats ROS and cell division [83,111].
DNA can be harmed directly or indirectly by events such as oxidative stress, radiations, alkylating agents, and a range of other chemotherapeutic techniques, but the capability of ovarian cancer cells to repair DNA damage is believed to be a crucial element in determining the resistance to chemotherapy [112].
In this context, sideroxylin from Callistemon lanceolatus induced apoptosis and reduced proliferation in ovarian cancer cells by influencing lipid peroxidation and ROS activity [113].
Additionally, berberine, another example of a common alkaloid that can be retrieved from several natural sources [114], which has been proven to stop cell division by interfering with DNA repair processes, inhibited the effects of PARP1, which is involved in oxidative states of damaged DNA [115].
Besides, alone or in combination with cisplatin, the abovementioned compound WFA induced the formation of reactive oxygen species (ROS) in A2780 ovarian cancer cells, which caused DNA harm. The compound acted in a synergistic cytotoxic manner with cisplatin, which formed DNA adducts [116].
On the other hand, in the context of the role played by nucleic acid sequences as targets for anticancer agents, aberrant RNAs have been discovered to play critical oncogenic roles in several human cancers. For example, astragalus polysaccharide (APS), a bioactive substance from Astragalus membranaceus, increased apoptosis while decreasing cell invasion targeting such sequences [117].
5.3. Modulation of Inflammation
It is now widely accepted that inflammation has a direct association with carcinogenesis as it contributes in initiation, proliferation, invasion, and metastasis [118]. Pro-inflammatory cytokines like TNF-α and IL-6 are blocked by anti-inflammatory compounds including baicalein, apigenin, curcumin, EGCG, genistein, luteolin, and wogonin [83]. Alongside, signal transducer and activator of transcription 3 (STAT-3) prevention, cyclooxygenase-2 (COX-2) inhibition, and nitric oxide synthase (iNOS) downregulation are considered as the main anti-inflammatory mechanisms of phytochemicals [119].
5.4. Suppression of Events Related to Disease Progression: Cell Migration and Angiogenesis
Cell migration and invasion are among the hallmarks of disease progression, and some natural compounds have been reported to target such events.
Among these, tetramethylpyrazine (TMP) from Ligusticum wallichil decreased cell viability and motility in SKOV-3 cells [120], and emodin, which is contained in several preparations of Chinese herbs, was found to suppress cell division, invasion, and migration by hindering the ILK/GSK-3β pathway [121].
Another event that contributes to disease progression is angiogenesis. BLP, the abovementioned mixture containing proanthocyanidins from Chinese bayberry leaves, is probably the most promising in this context, as it demonstrated an anti-angiogenic effect in the IOSE-364 ovarian cell line due to an inhibition of vascular endothelial growth factor (VEGF) [122].
Similarly, Tan-IIA, already mentioned above, interfered with disease progression in an A2780 xenograft model. Concerning the underlying mechanism of action, Tan-IIA promoted antiangiogenetic effects, mediated by the interference with VEGF, and induced apoptosis in the ID-8 and A2780 cell lines [123].
Several natural flavonoids were also reported to act on the EGF/VEGF pathway, including apigenin, taxifolin, luteolin, quercetin, genistein, kaempferol [124], harmine [125], and cranberry proanthocyanidin-1 [126].
5.5. Regulation of Tumor Micro Environment
The tumor microenvironment is a complex and dynamic combination of elements in which cancer cells are embedded. It comprises nonmalignant cells, the extracellular matrix and several cytokines, chemokines, and growth factors. Considering their multi-target action, natural compounds can modulate several aspects of the microenvironment. In particular, Dias et al. highlighted how natural derivatives can influence metabolic crosstalk to “re-educate” tumor microenvironment cells towards potential anticancer activity. In particular, curcumin, resveratrol, EGCG, shikonin, and phloretin were reported to alter the metabolism of stromal cells [127].
The abovementioned effect is achieved through the modulation of the expression of cancer-associated genes by the natural products, and this mechanism has also been reported to explain the anticancer activity of quercetin, berberine, and tanshinones [128].
In addition, β-escin was recently reported to combat ovarian cancer metastasis by targeting both cancer and stromal cells in the tumor microenvironment [129].
5.6. Other Mechanisms Related to Dysregulation of Cell Cycle
Dysregulation of the cell cycle is a relevant contributing factor in the carcinogenesis of ovarian cancer, and interference with the G0/G1 stages is the most commonly reported mechanism of natural compounds with an anticancer role targeting this process [130]. This mechanism was reported for asiatic acid from Centella asiatica [131], mentoflavone from Selaginella tamariscina [132], proanthocyanidins from Chinese bayberry leaves (BLPs) [133], and pulchrin A [134], which were found to combat cell proliferation and cancer progression, in particular by targeting such phases of the cell cycle.
Moreover, co-treatment with herbal extracts from Fritillaria cirrhosa (FC) and Scutellaria baicalensis (SB) resulted in G0/G1 stage cell cycle arrest also in OVCA 420 and OVCA 429 ovarian cancer cells [135].
Additionally, cucurbitacin-A, isolated from Momordica charantia L., was found to show anticancer potential, causing cell cycle arrest in the G2/M phase [136].
In this context, licorice plants contain large amounts of the flavonoid isoliquiritigenin (ISL). In OVCAR-5 and ES-2 cell lines, ISL also decreased cell proliferation in a dose- and time-dependent manner, targeting the G2/M phase of the cell cycle [137].
Autophagy is another physiological cell process that contributes to the maintenance of a normal cell cycle. According to increasing evidence, autophagy and ovarian cancer also appear to be connected [138]. Thus, natural compounds that help in modulating autophagy may find an application in ovarian cancer treatment. Among the natural constituents reported to act against ovarian cancer through this mechanism, Emblica officinalis (Amla) extracts [8], resveratrol [139], withaferin A (WFA) [140], and grifolin [141] were reported.
Moreover, Tan-I, a compound from the class of tanshinones, cited above, increased levels of the autophagy-related proteins beclin1, ATG7, and p62 as well as LC3II/LC3I and caspase-3 in A2780 and ID8, boosting apoptosis and inducing autophagy [142,143].
Finally, genistein promoted autophagy of caspase-independent cells [144] and induced apoptosis in cisplatin-sensitive and resistant ovarian cancer cells (A2780/CaOV3, ES-2).
5.7. Natural Constituents Modulating Resistance to Chemotherapeutic Agents
In ovarian cancer cells, plant-derived constituents were found to enhance sensitivity to chemotherapeutics, an aspect which, as anticipated, is crucial in this pathology.
For example, pre-treatment with either ellagic acid or resveratrol 48-h before cisplatin administration was reported to increase cytotoxicity of cisplatin itself in A2780CisR cisplatin-resistant cells, while synergistic treatment with either cisplatin–ellagic acid or cisplatin–resveratrol for 26 weekly cycles completely prevented cisplatin resistance in A2780 cells [145].
Moreover, in A2780 cells, SFN diminished the xenobiotic-reaction component (XRE). SFN also interferes with cell pH regulation and migration, and in this context it has been proposed as an agent to combat chemoresistance [146].
In doxorubicin-resistant human ovarian cancer cell lines (NCI/ADR-RES), treatment with RCM, also known as Korean dark raspberry, led to apoptosis through phosphorylation of c-Jun N-terminal kinase (JNK) [147]. In the same model, ellagic acid and quercetin, two phytochemicals also found in RCM as well as in many other natural sources, were shown to influence JNK and Akt phosphorylation, thus inducing apoptosis [148].
Finally, since therapy with WFA and doxorubicin reduced cell proliferation in xenograft mice models of ovarian cancer more effectively than WFA or doxorubicin alone, it has been postulated that WFA may be thought of as an adjuvant to standard doxorubicin therapy to minimize adverse effects [140].
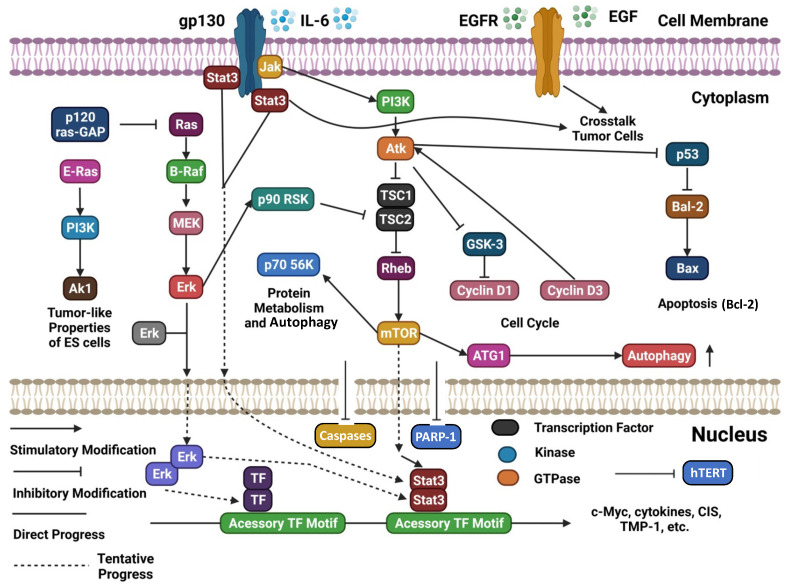
A schematic representation and summary of the pathways targeted by natural compounds and mentioned in this section are reported in Figure 3. Moreover, Table 1 summarizes the most recently reported updates on the molecular mechanisms underlying the activity of natural compounds and their derivatives in the context of ovarian cancer.
Figure 3.
Schematic representation of several cellular signaling pathways potentially targeted by natural compounds (adapted and updated from [83]).
Table 1.
Overview of natural substances showing anticancer properties against ovarian cancer models. This table is intended as an addendum to the one reported by Wu et al. [83], thus updated records were included. The reader is invited to refer to the abovementioned review for a more comprehensive overview with the corresponding references. The table also includes semi-synthetic derivatives of natural compounds that showed antiproliferative activity and that are discussed in Section 6.5 of the current review.
| Compound | Source | Chemical Structure of the Representative Component | Classification | Model | Mechanism of Action | References |
|---|---|---|---|---|---|---|
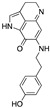
| Aminoalkyl derivatives of cycleanine | Triclisia subcordata |
 (Cycleanine) |
Bisbenzylisoquinoline macrocyclic alkaloid | Cell lines | activation of caspases 3/7, cleavage of PARP | [149] |
| Berberine | European barberry, goldenseal, goldthread, Oregon grape, phellodendron, and tree turmeric |

|
Alkaloid | A2780, HEY, HO8910 | Triggering oxidative DNA damage, targeting of cancer stem cells | [52,115] |
| Epigallocatechin gallate (EGCG) | Green tea |

|
Flavonoid | SKOV3-ip1, SKOV3TR-ip2 | Reduction of hTERT and Bcl-2, alteration of the metabolism of stromal cells | [99,127,150] |
| FBA-TPQ (derivative of makaluvamines) | Zyzzya sponges |
 (Makaluvamine scaffold) |
Pyrroloiminoquinone alkaloid | in vitro and in vivo (xenograft) | ROS species, p53-MDM2 and PI3K-Akt pathways | [151] |
| Phloretin | Apple tree leaves |

|
Dihydrochalcone | in vitro | Alteration of the metabolism of stromal cells | [127] |
| Semi-synthetic derivatives of celastrol | Tripterygium species |
 (Celastrol) |
Nortriterpen quinone | in vitro | STAT-3 pathway, induction of apoptosis, reduction of cell migration | [152] |
| Shikonin | Alkanna tinctoria |

|
Naphthoquinone | A278 cells, in vitro | Alteration of the metabolism of stromal cells | [127,153] |
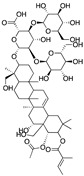
| Tanshinones |
Salvia miltiorrhiza |
 (Tanshinone IIA) |
Terpenoid/Abietane |
A-549, TOV-21G | Growth capacity is inhibited by reducing cell viability, alteration of the microenvironment | [92,123,128,143] |
| Verticillin H esters | Fungi |

|
Verticillins | OVCAR-3 | Reduced cell proliferation | [154] |
| β-escin | horse chestnut seed |
|
Pentacyclic triterpenoid saponin | in vitro and in vivo | Alteration of the microenvironment | [129] |
6. A Focus on Selected Natural Compounds with Promising Activity against Ovarian Cancer
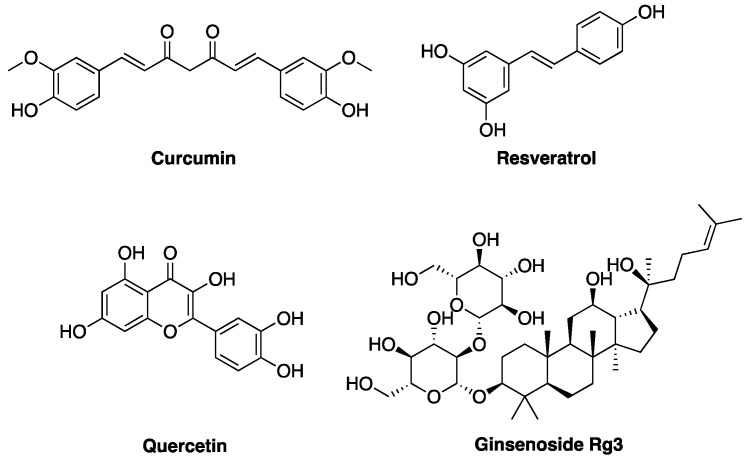
In the following part of the review, we focus on some of the most widely studied natural compounds, some of which have already been mentioned in previous paragraphs, with reported activity against ovarian cancer models (Figure 4). The compounds are presented to the reader according to a classification related to their chemical structure and natural origin. In particular, their potential as antiproliferative and anti-apoptotic agents, as well as the evidence concerning their anti-metastatic activity, are discussed. Eventually, a focus on semi-synthetic derivatives of natural compounds, designed to achieve improved anticancer activity, is presented.
Figure 4.
Chemical structures of curcumin, resveratrol, quercetin, and ginsenoside Rg3, the most promising natural compounds discussed in the review.
6.1. Curcumin
The primary ingredient in South Asian and Indian curries is turmeric, which comes from the root of Curcuma longa. Turmeric has a long history of usage in India and China as a traditional medicine [155]. Curcumin and two others related curcuminoids, namely demethoxycurcumin and bisdemethoxycurcumin, are well-known and widely studied compounds contained in this plant. As indicated by several reports published throughout the years, curcumin and curcuminoids have strong anticancer effects due to the interaction with a combination of intracellular targets [156].
6.1.1. Antiproliferative and Proapoptotic Activity
Excessive proliferation and unbalanced apoptosis are two signs of uncontrolled cell growth, and these events also occur in ovarian cancer, as discussed in the first part of this review. The protein kinase B/phosphatidylinositol 3-kinase (Akt/PI3K) signaling pathway is overactivated in ovarian cancer cells and supports cell proliferation and invasion [157].
In ovarian cancer cells, curcumin decreased Bcl-2 expression while it increased Bax and caspase-3, causing cell cycle arrest in the G2/M stage and consequent cell death [158]. According to Watson et al., curcumin activates caspase-8 and caspase-9 first, and then caspase-3 to exert this activity [159]. Moreover, the authors found that curcumin decreased Akt phosphorylation, Bcl-2, and survivin, an anti-apoptotic protein. When phosphorylated, STAT-3 advanced malignant growth by promoting cell proliferation and hindering apoptosis [160]. According to Saydmohammed et al., curcumin also reduced STAT-3 phosphorylation, which regulates the growth of ovarian cancer cells [161]. Curcumin regulated STAT-3 phosphorylation and enhanced interleukin (IL)-6 and IL-8 release, which decreased ovarian cell motility [162]. Seo et al. reported that curcumin influenced Ca2+ homeostasis in ovarian cancer cells [103]. Curcumin also interferes with miRNAs, short non-coding RNA sequences regulating target genes post-transcriptionally [163]. According to Du et al., treatment with dimethoxy-curcumin sustained the levels of miR-551a, inducing apoptosis in ovarian cancer cells [164]. Additionally, when dihydroartemisinin and curcumin were combined, miR-124 was upregulated and its target, midkine, which promotes carcinogenesis and is overexpressed in infections, was downregulated [165], causing cell cycle arrest and apoptosis. Additionally, curcumin increased apoptosis and stopped the growth of ovarian cancer cells by targeting miR-9 [166].
Thus, as can be deduced from the results of the high number of reports concerning curcumin published in this context, it can be postulated that the compound may act through a combination of mechanisms at the molecular level to exert its antiproliferative activity.
6.1.2. Anti-Metastatic Activity
Unregulated cancer cells, also in the case of ovarian cancer, can spread to different organs [4], and in this context matrix metalloproteinases (MMPs), a type of proteolytic protein, promote the development of ovarian cancer [167]. By reducing the phosphorylation of FAK, MMP-9, and Rab coupling protein, curcumin inhibited SKOV3 cell invasion [168]. Moreover, bisdemethoxycurcumin reduced metastasis-related proteins such as MMP-2, MMP-9, and vascular cell bond particle 1 (VCAM-1) in SKOV3 cells by controlling oxidative stress and inactivating the NF-κB pathway [169]. The cooperation of VCAM-1 and integrin has been shown to play a role in ovarian cancer cell intrusion and metastasis [170].
6.2. Resveratrol
Resveratrol is a polyphenolic compound that can be found in grapes, peanuts, and plants such as Polygonum cuspidatum [171]. Resveratrol improves heart disease and conditions affecting the nervous system and kidneys, and it is reported to have several other beneficial properties [172,173]. This compound has been widely studied throughout the years for its biological roles, and it has been cited previously in the current review. In this section, a brief overview of the reports concerning its antiproliferative and anti-metastatic activities are reported.
6.2.1. Antiproliferative and Proapoptotic Activity
In a mouse model, resveratrol diminished glucose uptake by cancer cells [174]. Resveratrol influenced GSK3β in ovarian cancer cells, reducing protein glycosylation [175]. GSK3β phosphorylated and deactivated glycogen synthase, thus regulating glucose storage [176]. Tino et al. [177] found that the combined use of resveratrol and acetyl resveratrol efficiently retarded the growth of ovarian cancer cells, and that this effect was accomplished by decreased NF-κB protein [177]. Besides GSK3, in ovarian cancer cells, resveratrol reduced the phosphorylation of Akt, and increased the extracellular signal-coordinating kinase (ERK) [102].
6.2.2. Anti-Metastatic Activity
By reducing integrin levels, resveratrol has been shown to hinder the ability of ovarian cancer cells to invade the peritoneal mesothelium, thus preventing metastasis [178]. Resveratrol may limit the interaction between ovarian cancer cells and mesothelial cells by preventing the motility of the firsts, and, in particular, downregulation of VEGF in hypoxic conditions appears to be involved [179]. In fact, increased VEGF production has been shown to be related to metastasis in ovarian cancer cells [180].
6.3. Ginsenosides
The major pharmacologically active components of ginseng, ginsenosides, have antioxidant and anticancer properties [173,181]. Ginsenoside Rg3 and Rb1 especially have been reported to display anticancer activity [182].
6.3.1. Antiproliferative and Proapoptotic Activity
According to Li et al., ginsenoside Rg3 decreased ovarian disease cell glycolysis by downregulating phospho-STAT-3 [183]. Additionally, the compound triggered the upregulation of miR-603 in ovarian cancer cells by inhibiting DNA methylation. The same natural molecule also influenced hexokinase-2 activity [184].
However, the use of ginsenoside Rg3 is a rather debated issue, as recent reports showed that the use of low concentrations of the compound stimulated cell proliferation, while high concentrations were needed to achieve anticancer effects [185].
6.3.2. Anti-Metastatic Activity
HIF-1α is a dimeric protein that plays a role in hypoxic conditions and metastasis [186]. Epithelial–mesenchymal transition (EMT), which is related to cell–cell adhesion, frequently takes place prior to the onset of ovarian cancer. Liu et al. observed that ginsenoside 20(S)-Rg3 counteracted EMT and downregulated HIF-1 through interference with the ubiquitin–proteasome pathway [183]. Additionally, it was discovered that ginsenoside Rg3 increased prolyl hydroxylase protein 1 and resulted in HIF-1α degradation [187]. Moreover, a reduction in cell intrusion capability was observed upon treatment with this compound [184].
Furthermore, ginsenoside Rb1 reduced hypoxia-induced EMT in ovarian cancer cells by downregulating miR-25. More specifically, it prevented the production of EP300, a transcriptional activator of E-cadherin, a crucial molecule for epithelial cell attachment, from being suppressed by miR-25, which would have had an anti-metastatic impact [188]. By interaction with actin microfilaments in the cytoplasm through α- and β-catenin, E-cadherin is associated with the adhesion of epithelial cells [189].
6.4. Quercetin
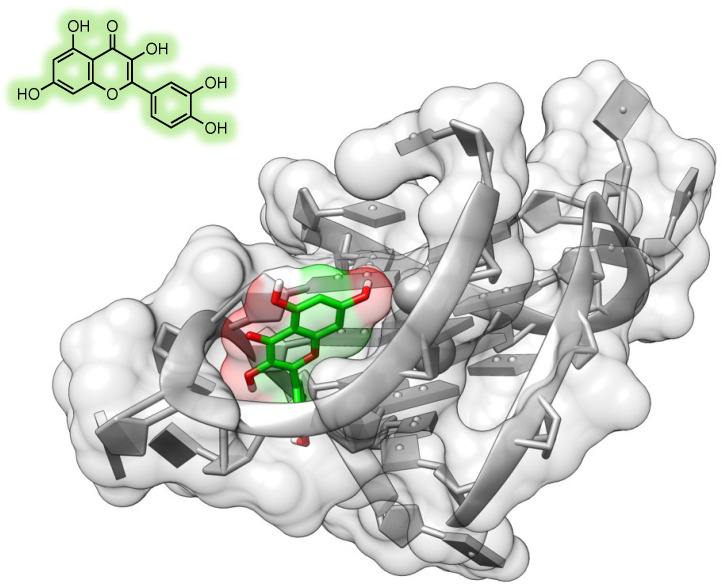
Quercetin is one of the most widely studied naturally occurring flavonoids, which is known to possess a plethora of biological properties through several mechanisms including interaction with DNA (Figure 5) and several protein targets [190], and this section of the review is focused on the reports on anticancer activity of this compound in ovarian cancer models. Shafabakhsh and Asemi [93] and by Vafadar et al. [94] recently reviewed the anticancer properties of quercetin, and the reader is invited to refer to these reviews for a more comprehensive overview of the molecular mechanisms of this compound.
Figure 5.
Quercetin structure and predicted binging mode to a G-quadruplex DNA sequence (Protein Data Bank ID: 3CE5; adapted from [190]). The artwork was produced using UCSF Chimera [191].
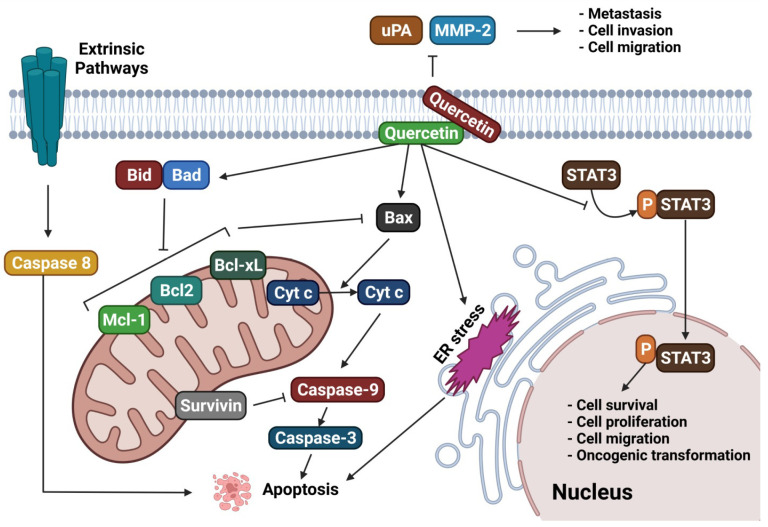
Liu et al. examined the effects of quercetin on apoptosis in an ovarian cancer mice xenograft model and demonstrated that quercetin caused mitochondrial apoptosis [192]. Furthermore, by causing endoplasmic reticulum (ER) stress, quercetin triggered mitochondria-mediated apoptosis in ovarian cancer cells. Quercetin affected ER stress, apoptosis, and autophagy via the p-STAT3/Bcl-2 center. In general, quercetin downregulates the growth of metastatic ovarian cancer cells through the induction of apoptotic conditions. In particular, the flavonoid increases the activity of apoptotic species including caspase-3, caspase-9, and cytochrome c. Moreover, pro-apoptotic proteins Bid, Bax, and Bad are also involved. Concerning this biomolecular mechanism, Bad and Bid promote the oligomerization of Bax and of the protein Bak, and this event triggers the permeabilization of the outer mitochondrial wall. Bid can directly trigger apoptosis, while Bad interacts with anti-apoptotic Bcl-2 proteins, thus lowering the threshold for induction of apoptosis. As a result, their equilibrium has an effect on the neoplastic shift in the human endometrium [193]. Like curcumin, quercetin causes mitochondrial-mediated apoptosis and thus limits the proliferation of metastatic ovarian cancer cells [194]. Moreover, our group recently demonstrated that quercetin, as well as its glycoside rutin, can target specific DNA sequences and arrangements in vitro, demonstrating that the compound could influence gene expression [190].
As for natural compounds and drugs in general, the bioavailability and formulation/delivery system may be crucial for obtaining the biological effects. In this context, another study investigated the antiproliferative potential of a quercetin-based nano-formulation. Both in vitro and in mice xenograft models, this specific form of quercetin reduced the development of ovarian cancer cells. Furthermore, it has been noted that quercetin from the nano-formulation activated caspase-3, caspase-9, and Bax while inhibiting MCL-1 and Bcl-2 to enhance apoptosis [195].
Additionally, several studies were aimed at understanding the synergistic benefits of quercetin when used in combination with various chemotherapeutics. In an in vitro/in vivo investigation, Gong et al. [196] examined the effects of quercetin combined with radiation on ovarian cancer. Exposure of quercetin made ovarian cancer cells undergo ER stress, and there was also an increase in p53, p21, and Bax expression, a reduction of Bcl-2 expression, and an increase in DNA damage.
Quercetin coupled with radiation dramatically decreased the growth of cancer cells and activated p53 in a xenograft ovarian cancer model. In another study, pretreatment with quercetin sustained the cytotoxic activity of cisplatin in ovarian cancer patients. In particular, quercetin increased ER stress, decreased STAT3 phosphorylation, and decreased Bcl-2 expression. Quercetin supported the anticancer impacts of cisplatin also in a xenograft mice model, suggesting a potential role for quercetin as a promising adjuvant medication for ovarian cancer treatment [197].
Other formulations of quercetin, such as PEGylated liposomal quercetin (lipo-quercetin), were tested in vitro and in vivo in models of both cisplatin-sensitive and cisplatin-resistant human ovarian cancer. Studies conducted in vitro revealed that the presence of lipo-quercetin caused cell cycle arrest and apoptosis in both kinds of cancer cells. Moreover, lipo-quercetin was more effective than free quercetin in mice xenograft models [198]. Several studies examined the impact of quercetin on cell cycle progression [199], and it was reported that the compound regulated 1-phosphatidylinositol 4-kinase (PI kinase) activity and lowered inositol-1,4,5-triphosphate (IP3) levels, thus confirming its effect on the cell cycle [200]. Moreover, quercetin was recently studied as an anti-metastatic agent in the context of ovarian cancer [201].
In the context of quercetin derivatives, an in vitro study examined the effects of 3,4′,7-O-trimethylquercetin (34′7TMQ) on the growth and progression of ovarian cancer cells, and the compound diminished ovarian cancer cell invasion [202].
Importantly, recent studies showed that quercetin can help in mitigating the side effects of chemotherapeutic agents including cisplatin, 5-fluorouracil, taxol, and pirarubicin. While other, less recent, research reports showed quercetin to be directly effective in the treatment of ovarian cancer, especially when paired with other drugs; it has been later demonstrated that low doses of quercetin increase antioxidant enzymes and reduce ROS-mediated anti-neoplastic drug toxicity [203]. In this context, another in vitro study in ovarian cancer cells supported the synergistic effect of quercetin when administered in combination with cisplatin [204].
The findings reported in this section suggest that quercetin and its formulations have anticancer potential against ovarian cancer through a combination of several mechanisms, which are outlined in Figure 6. Table 2 reports an update on findings concerning the potential of quercetin as an anticancer agent, in particular in the context of ovarian cancer. As can be noted from the records reported in the table, great efforts are currently focused on improving drug-likeness features and delivery strategies for this compound, together with the investigation of synergistic and potentiation effects with respect to traditional anticancer agents.
Figure 6.
Quercetin targets several signaling pathways within the cells, representing a potential therapeutic agent against ovarian cancer (adapted from [80]).
Table 2.
Update on experimental data reported in the literature for the activity of quercetin in the ovarian cancer model. This table is intended as an addendum to the ones reported by Shafabakhsh and Asemi [80] and by Vafadar et al. [81], thus updated records were included. The reader is invited to refer to the abovementioned reviews for a more comprehensive overview, with the corresponding references.
| Compound/Formulation | Ovarian Cancer Model | Type of Study | Major Findings and Mechanisms | Reference |
|---|---|---|---|---|
| Graphene oxide polyvinylpyrrolidone-quercetin-gefitinib (GO-PVP-QSR-GEF) | Ovarian cancer cells | In vitro | Synergistic cytotoxic effect | [205] |
| Micellar(nanostructures) resveratrol (R):quercetin (Q) (mRQ) | Xenograft model | In vivo | Improvement of the efficacy of adriamycin | [206] |
| Quercetin | - | In vitro | Human telomeric G-quadruplex stabilization | [190] |
| Quercetin | Ovarian cancer cells | In vitro | Attenuation of metastatic ability | [201] |
| Quercetin micelle and thermosensitive hydrogel drug delivery system | SKOV-3 cells and animal model | In vitro and in vivo | Enhanced cytotoxicity | [207] |
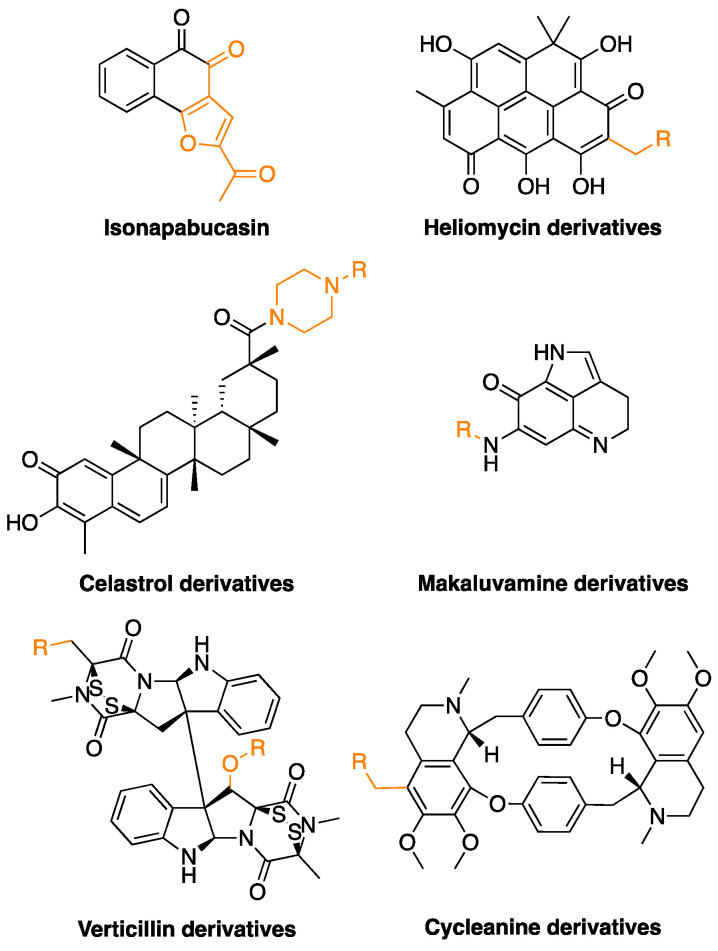
6.5. Semi-Synthetic Compounds
As anticipated, natural compounds are endowed with unique features in terms of chemical diversity and are often characterized, as highlighted by the overview presented in the previous sections of this review, by the capability of targeting a combination of biochemical pathways within the cell. Nevertheless, such compounds may also be characterized by poor bioavailability, lack of drug-likeness features, limited availability from natural sources, and poor specificity. Thus, research has recently focused on the design of semi-synthetic or synthetic derivatives of natural compounds with improved performances to address these issues [208].
Several examples of semi-synthetic investigational anticancer agents are presented in the literature. Napabucasin and other derivatives of naphthoquinones from Handroanthus impetiginosus were tested against cancer cells. The compounds inhibited STAT3, induced apoptosis, and stimulated ROS production [209]. Another example is represented by the paper from Nadysev et al. that reported the synthesis and characterized the biological activity profile of 4-aminomethyl derivatives of heliomycin, a metabolite from Actinomyces flavochromogenes var. heliomycini and Streptomyces resistomycificus. The molecules were tested against a set of cell lines and showed improved water solubility and antiproliferative efficacy with respect to the natural compound [210].
More specifically, concerning therapeutic approaches against ovarian cancer, Li et al. very recently reported a set of derivatives of celastrol, a compound isolated from Tripterygium species. This molecule has promising anticancer properties, but it is endowed with suboptimal pharmacological properties due to poor water stability, low bioavailability, and toxicity. The authors modified the structure to obtain drug-like compounds targeting the STAT3 pathway and showing anti-proliferative activity through induction of apoptosis and reduction of cell migration [152].
Previously, Chen et al. studied the synthetic compound FBA-TPQ, a derivative of the marine pyrroloiminoquinone alkaloid makaluvamine, which is isolated from sponges of the genera Zyzzya. FBA-TPQ exhibited anticancer activity against OVCAR-3 ovarian cancer cells through ROS species, p53-MDM2, and PI3K-Akt pathways. Moreover, minimal toxicity was observed in non-tumorigenic human IOSE-144 cells, and in vitro data were supported by in vivo studies in xenograft models [151].
Verticillins are another class of fungal metabolites, and several ester derivatives of verticillin H were prepared and tested against a panel of cancer cell lines, including OVCAR-3. The compounds showed cytotoxic activity in the nanomolar range [154].
Cycleanine is a bisbenzylisoquinoline macrocyclic alkaloid from Triclisia subcordata. Uche et al. synthesized a small pool of aminoalkyl derivatives that were tested against ovarian cancer cells. The molecules showed anticancer activity through activation of caspases 3/7 and cleavage of PARP [149].
The chemical structures of the most promising semi-synthetic compounds are shown in Figure 7, and the main findings in this context are outlined in Table 1.
Figure 7.
Chemical structures of the discussed semi-synthetic derivatives of natural compounds. The parts of the molecules that have been modified are highlighted in orange.
7. The Point of View of the Medicinal Chemist
Although it is widely established that first-line conventional chemotherapy has a therapeutic effect in many ovarian cancer patients, drug resistance typically limits the efficacy of treatment regimens. Natural products have been investigated in ovarian cancer models both per se and in adjuvant treatment, with positive outcomes in several cases, as overviewed in the previous paragraphs. As laid out in the reported studies, such compounds, belonging to several different chemical classes and acting through a combination of mechanisms, may effectively hinder cancer progression according to in vitro and in vivo studies. Importantly, moreover, natural compounds alone or in combination, boost chemotherapy efficacy while lowering toxic and side effects, potentially allowing a more promising outcome.
Three major observations can be drawn from this literature overview, considering the topic from the point of view of the medicinal chemist. First, the multi-target mechanism of natural compounds represents a valuable resource, but the lack of selectivity may represent a drawback for the development of novel therapeutic approaches. Second, it must be noted how many natural compounds, besides showing anticancer activity per se, also possess potentiating/synergistic properties with respect to other drugs. Additionally, they can help in re-sensitizing resistant cancer cells. Eventually, it must be considered that natural compounds should represent the starting point for compound optimization, as testified by the growing interest towards semi-synthetic derivatives with enhanced drug-likeness and performances. In fact, as overviewed in Section 6 of this review, the development of semi-synthetic compounds is pushing the efficacy of nature-derived molecules in the nanomolar range, even if every case is peculiar. Moreover, the efforts of medicinal chemists, besides improving antiproliferative activity, are pointed towards improving water solubility, stability, bioavailability, and toxicity profiles.
However, a major pitfall is still present and must not be ruled out, as very limited data support the clinical use of the natural compounds discussed in this paper. In fact, few clinical studies have assessed the anticancer effects of natural molecules, even for the most studied ones such as quercetin, particularly in the field of ovarian cancer [81,211]. In other cases, compounds that have been demonstrated to be effective in in vivo models of ovarian cancer were tested in clinical trials, but with different anticancer indications. This is, for example, the case for β-escin [212]. Nevertheless, there are also compounds that have been more widely studied in clinical trials such as resveratrol, which, anyway, is affected by limitations in terms of bioavailability [213].
8. Conclusions and Future Perspectives
This review overviewed and summarized the anticancer potential of plant-derived molecules in ovarian cancer models. The compounds discussed in this paper bear a variety of different chemical scaffolds, as can be expected for molecules of natural origin. In this connection, the main classes comprise phenolic components, flavonoids, steroid glycosides, terpenoids, chalcones, and several alkaloids.
Similarly, the underlying molecular mechanisms for the different compounds are very diverse, and they include autophagy and apoptosis induction, ROS activity, inhibition of cell invasion, angiogenesis, and metastasis [214]. Most importantly, natural molecules often act through a combination of the abovementioned mechanisms.
Nevertheless, more exploration is required to estimate and understand the effective potential of natural substances in pre-clinical and clinical trials. In particular, some major points must be addressed, including (i) assessment of dose for use of natural compounds in ovarian cancer; (ii) usage of natural compounds as co-treatments with chemotherapy, radiotherapy, and other immunotherapies [215]; (iii) use of a combination of natural compounds acting through different and ideally synergistic mechanisms; and (iv) advanced formulation studies to improve bioavailability of the molecules, thus paving the way for the potential application of natural and nature-inspired compounds as antiproliferative agents against ovarian cancer.
Author Contributions
Conceptualization, A.R. and G.R.; investigation, M.R.I., M.M.R., P.S.D., F.T.N., N.S., M.A. and A.A.K.; writing—original draft preparation, M.R.I., M.M.R., P.S.D., F.T.N., N.S., M.A. and A.A.K.; writing—review and editing, A.R., A.G. and G.R.; funding acquisition, A.R., A.G. and G.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable. No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was funded by University of Brescia.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Duska L.R., Kohn E.C. The New Classifications of Ovarian, Fallopian Tube, and Primary Peritoneal Cancer and Their Clinical Implications. Ann. Oncol. 2017;28:viii8–viii12. doi: 10.1093/annonc/mdx445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yousefi M., Dehghani S., Nosrati R., Ghanei M., Salmaninejad A., Rajaie S., Hasanzadeh M., Pasdar A. Current Insights into the Metastasis of Epithelial Ovarian Cancer—Hopes and Hurdles. Cell. Oncol. 2020;43:515–538. doi: 10.1007/s13402-020-00513-9. [DOI] [PubMed] [Google Scholar]
- 4.Weidle U.H., Birzele F., Kollmorgen G., Rueger R. Mechanisms and Targets Involved in Dissemination of Ovarian Cancer. Cancer Genom. Proteom. 2016;13:407–424. doi: 10.21873/cgp.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falzone L., Scandurra G., Lombardo V., Gattuso G., Lavoro A., Distefano A.B., Scibilia G., Scollo P. A Multidisciplinary Approach Remains the Best Strategy to Improve and Strengthen the Management of Ovarian Cancer (Review) Int. J. Oncol. 2021;59:53. doi: 10.3892/ijo.2021.5233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang S.F., Wang X.Y., Fu Z.Q., Peng Q.H., Zhang J.Y., Ye F., Fu Y.F., Zhou C.Y., Lu W.G., Cheng X.D., et al. TXNDC17 Promotes Paclitaxel Resistance via Inducing Autophagy in Ovarian Cancer. Autophagy. 2015;11:225–238. doi: 10.1080/15548627.2014.998931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang M.-F., Lou Y.-L., Liu S.-S., Wang S.-S., Yin C.-H., Cheng X.-H., Huang O.-P. Capn4 Overexpression Indicates Poor Prognosis of Ovarian Cancer Patients. J. Cancer. 2018;9:304–309. doi: 10.7150/jca.22004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De A., De A., Papasian C., Hentges S., Banerjee S., Haque I., Banerjee S.K. Emblica Officinalis Extract Induces Autophagy and Inhibits Human Ovarian Cancer Cell Proliferation, Angiogenesis, Growth of Mouse Xenograft Tumors. PLoS ONE. 2013;8:e72748. doi: 10.1371/journal.pone.0072748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurman R.J., Shih I.-M. The Origin and Pathogenesis of Epithelial Ovarian Cancer-a Proposed Unifying Theory. Am. J. Surg. Pathol. 2010;34:433–443. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ottevanger P.B. Ovarian Cancer Stem Cells More Questions than Answers. Semin. Cancer Biol. 2017;44:67–71. doi: 10.1016/j.semcancer.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Akilli H., Rahatli S., Tohma Y.A., Karakas L.A., Altundag O., Ayhan A. Effect of Increased Number of Neoadjuvant Chemotherapy Cycles on Tumor Resectability and Pathologic Response in Advanced Stage Epithelial Ovarian Cancer. J. BUON. 2018;23:111–115. [PubMed] [Google Scholar]
- 12.Ribaudo G. Synthesis of Flavonoids or Other Nature-Inspired Small Molecules. Molbank. 2022;2022:M1313. doi: 10.3390/M1313. [DOI] [Google Scholar]
- 13.Sharifi-Rad J., Rajabi S., Martorell M., López M.D., Toro M.T., Barollo S., Armanini D., Fokou P.V.T., Zagotto G., Ribaudo G., et al. Plant Natural Products with Anti-Thyroid Cancer Activity. Fitoterapia. 2020;146:104640. doi: 10.1016/j.fitote.2020.104640. [DOI] [PubMed] [Google Scholar]
- 14.Zorzan M., Collazuol D., Ribaudo G., Ongaro A., Scaroni C., Zagotto G., Armanini D., Barollo S., Galeotti F., Volpi N., et al. Biological Effects and Potential Mechanisms of Action of Pistacia Lentiscus Chios Mastic Extract in Caco-2 Cell Model. J. Funct. Foods. 2019;54:92–97. doi: 10.1016/j.jff.2019.01.007. [DOI] [Google Scholar]
- 15.Povolo C., Foschini A., Ribaudo G. Optimization of the Extraction of Bioactive Molecules from Lycium Barbarum Fruits and Evaluation of the Antioxidant Activity: A Combined Study. Nat. Prod. Res. 2018;33:2694–2698. doi: 10.1080/14786419.2018.1460835. [DOI] [PubMed] [Google Scholar]
- 16.Dutta R., Khalil R., Green R., Mohapatra S.S., Mohapatra S. Withania Somnifera (Ashwagandha) and Withaferin A: Potential in Integrative Oncology. Int. J. Mol. Sci. 2019;20:5310. doi: 10.3390/ijms20215310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mominur Rahman M., Islam F., Saidur Rahaman M., Sultana N.A., Fahim N.F., Ahmed M. Studies on the Prevalence of HIV/AIDS in Bangladesh Including Other Developing Countries. Adv. Tradit. Med. 2021:1–12. doi: 10.1007/s13596-021-00610-6. [DOI] [Google Scholar]
- 18.Rahman M.M., Islam M.R., Akash S., Shohag S., Ahmed L., Supti F.A., Rauf A., Aljohani A.S.M., Al Abdulmonem W., Khalil A.A., et al. Naphthoquinones and Derivatives as Potential Anticancer Agents: An Updated Review. Chem. Biol. Interact. 2022;368:110198. doi: 10.1016/j.cbi.2022.110198. [DOI] [PubMed] [Google Scholar]
- 19.Islam M.R., Akash S., Rahman M.M., Nowrin F.T., Akter T., Shohag S., Rauf A., Aljohani A.S.M., Simal-Gandara J. Colon Cancer and Colorectal Cancer: Prevention and Treatment by Potential Natural Products. Chem. Biol. Interact. 2022;368:110170. doi: 10.1016/j.cbi.2022.110170. [DOI] [PubMed] [Google Scholar]
- 20.Rahman M.M., Wang X., Islam M.R., Akash S., Supti F.A., Mitu M.I., Harun-Or-Rashid M., Aktar M.N., Khatun Kali M.S., Jahan F.I., et al. Multifunctional Role of Natural Products for the Treatment of Parkinson’s Disease: At a Glance. Front. Pharmacol. 2022;13:4207. doi: 10.3389/fphar.2022.976385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mukerjee N., Al-Khafaji K., Maitra S., Suhail Wadi J., Sachdeva P., Ghosh A., Buchade R.S., Chaudhari S.Y., Jadhav S.B., Das P., et al. Recognizing Novel Drugs against Keap1 in Alzheimer’s Disease Using Machine Learning Grounded Computational Studies. Front. Mol. Neurosci. 2022;15:638. doi: 10.3389/fnmol.2022.1036552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Semwal P., Painuli S., Anand J., Martins N.C., Machado M., Sharma R., Batiha G.E.S., Yaro C.A., Lorenzo J.M., Rahman M.M. The Neuroprotective Potential of Endophytic Fungi and Proposed Molecular Mechanism: A Current Update. Evid. Based Complement. Altern. Med. 2022;2022:6214264. doi: 10.1155/2022/6214264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garg S., Singla R.K., Rahman M.M., Sharma R., Mittal V. Evaluation of Ulcer Protective Activity of Morus alba L. Extract-Loaded Chitosan Microspheres in Ethanol-Induced Ulcer in Rat Model. Evid. Based Complement. Altern. Med. 2022;2022:4907585. doi: 10.1155/2022/4907585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahman M.M., Sarker M.T., Alam Tumpa M.A., Yamin M., Islam T., Park M.N., Islam M.R., Rauf A., Sharma R., Cavalu S., et al. Exploring the Recent Trends in Perturbing the Cellular Signaling Pathways in Cancer by Natural Products. Front. Pharmacol. 2022;13:3609. doi: 10.3389/fphar.2022.950109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman M.M., Islam M.R., Emran T. Bin Impact of Nutrition in Brain Function and Development: Potential Brain Foods. Int. J. Surg. 2022;106:106908. doi: 10.1016/j.ijsu.2022.106908. [DOI] [PubMed] [Google Scholar]
- 26.Rahman M.M., Islam M.R., Akash S., Harun-Or-Rashid M., Ray T.K., Rahaman M.S., Islam M., Anika F., Hosain M.K., Aovi F.I., et al. Recent Advancements of Nanoparticles Application in Cancer and Neurodegenerative Disorders: At a Glance. Biomed. Pharmacother. 2022;153:113305. doi: 10.1016/j.biopha.2022.113305. [DOI] [PubMed] [Google Scholar]
- 27.Rahman M.M., Islam M.R., Mim S.A., Sultana N., Chellappan D.K., Dua K., Kamal M.A., Sharma R., Emran T. Bin Insights into the Promising Prospect of G Protein and GPCR-Mediated Signaling in Neuropathophysiology and Its Therapeutic Regulation. Oxid. Med. Cell. Longev. 2022;2022:8425640. doi: 10.1155/2022/8425640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soong T.R., Dinulescu D.M., Xian W., Crum C.P. Frontiers in the Pathology and Pathogenesis of Ovarian Cancer: Cancer Precursors and “Precursor Escape”. Hematol. Oncol. Clin. N. Am. 2018;32:915–928. doi: 10.1016/j.hoc.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 29.Kotsopoulos J., Gronwald J., McCuaig J.M., Karlan B.Y., Eisen A., Tung N., Bordeleau L., Senter L., Eng C., Couch F., et al. Breastfeeding and the Risk of Epithelial Ovarian Cancer among Women with a BRCA1 or BRCA2 Mutation. Gynecol. Oncol. 2020;159:820–826. doi: 10.1016/j.ygyno.2020.09.037. [DOI] [PubMed] [Google Scholar]
- 30.Shih I.M., Wang Y., Wang T.L. The Origin of Ovarian Cancer Species and Precancerous Landscape. Am. J. Pathol. 2021;191:26–39. doi: 10.1016/j.ajpath.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang D.H., Smith E.R., Cohen C., Wu H., Patriotis C., Godwin A.K., Hamilton T.C., Xu X.X. Molecular Events Associated with Dysplastic Morphologic Transformation and Initiation of Ovarian Tumorigenicity. Cancer. 2002;94:2380–2392. doi: 10.1002/cncr.10497. [DOI] [PubMed] [Google Scholar]
- 32.Imai Y., Hasegawa K., Matsushita H., Fujieda N., Sato S., Miyagi E., Kakimi K., Fujiwara K. Expression of Multiple Immune Checkpoint Molecules on t Cells in Malignant Ascites from Epithelial Ovarian Carcinoma. Oncol. Lett. 2018;15:6457–6468. doi: 10.3892/ol.2018.8101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crum C.P., Drapkin R., Kindelberger D., Medeiros F., Miron A., Lee Y. Lessons from BRCA: The Tubal Fimbria Emerges as an Origin for Pelvic Serous Cancer. Clin. Med. Res. 2007;5:35–44. doi: 10.3121/cmr.2007.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roh M.H., Yassin Y., Miron A., Mehra K.K., Mehrad M., Monte N.M., Mutter G.L., Nucci M.R., Ning G., McKeon F.D., et al. High-Grade Fimbrial-Ovarian Carcinomas Are Unified by Altered P53, PTEN and PAX2 Expression. Mod. Pathol. 2010;23:1316–1324. doi: 10.1038/modpathol.2010.119. [DOI] [PubMed] [Google Scholar]
- 35.Kindelberger D.W., Lee Y., Miron A., Hirsch M.S., Feltmate C., Medeiros F., Callahan M.J., Garner E.O., Gordon R.W., Birch C., et al. Intraepithelial Carcinoma of the Fimbria and Pelvic Serous Carcinoma: Evidence for a Causal Relationship. Am. J. Surg. Pathol. 2007;31:161–169. doi: 10.1097/01.pas.0000213335.40358.47. [DOI] [PubMed] [Google Scholar]
- 36.Chivukula M., Niemeier L.A., Edwards R., Nikiforova M., Mantha G., McManus K., Carter G. Carcinomas of Distal Fallopian Tube and Their Association with Tubal Intraepithelial Carcinoma: Do They Share a Common “Precursor” Lesion? Loss of Heterozygosity and Immunohistochemical Analysis Using PAX 2, WT-1, and P53 Markers. ISRN Obstet. Gynecol. 2011;2011:858647. doi: 10.5402/2011/858647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaw P.A., Rouzbahman M., Pizer E.S., Pintilie M., Begley H. Candidate Serous Cancer Precursors in Fallopian Tube Epithelium of BRCA1/2 Mutation Carriers. Mod. Pathol. 2009;22:1133–1138. doi: 10.1038/modpathol.2009.89. [DOI] [PubMed] [Google Scholar]
- 38.Hunn J., Rodriguez G.C. Ovarian Cancer: Etiology, Risk Factors, and Epidemiology. Clin. Obstet. Gynecol. 2012;55:3–23. doi: 10.1097/GRF.0b013e31824b4611. [DOI] [PubMed] [Google Scholar]
- 39.Koh S.C.L., Chan Y.H., Lutan D., Marpuang J., Ketut S., Budiana N.G., Saleh A.Z., Aziz M.F., Winarto H., Pradjatmo H., et al. Combined Panel of Serum Human Tissue Kallikreins and CA-125 for the Detection of Epithelial Ovarian Cancer. J. Gynecol. Oncol. 2012;23:175–181. doi: 10.3802/jgo.2012.23.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Budiana I.N.G., Angelina M., Pemayun T.G.A. Ovarian Cancer: Pathogenesis and Current Recommendations for Prophylactic Surgery. J. Turk. Ger. Gynecol. Assoc. 2019;20:47–54. doi: 10.4274/jtgga.galenos.2018.2018.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Worley M.J., Welch W.R., Berkowitz R.S., Ng S.W. Endometriosis-Associated Ovarian Cancer: A Review of Pathogenesis. Int. J. Mol. Sci. 2013;14:5367–5379. doi: 10.3390/ijms14035367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mai P.L., Loud J.T., Greene M.H. A Major Step Forward for BRCA1/2-Related Cancer Risk Management. J. Clin. Oncol. 2014;32:1531–1533. doi: 10.1200/JCO.2013.54.8925. [DOI] [PubMed] [Google Scholar]
- 43.Akash S., Kumer A., Rahman M.M., Emran T.B., Sharma R., Singla R.K., Alhumaydhi F.A., Khandaker M.U., Park M.N., Idris A.M., et al. Development of New Bioactive Molecules to Treat Breast and Lung Cancer with Natural Myricetin and Its Derivatives: A Computational and SAR Approach. Front. Cell. Infect. Microbiol. 2022;12:1400. doi: 10.3389/fcimb.2022.952297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akash S., Rahman M.M., Islam M.R., Sharma R. Emerging Global Concern of Langya Henipavirus: Pathogenicity, Virulence, Genomic Features, and Future Perspectives. J. Med. Virol. 2023;95:e28127. doi: 10.1002/jmv.28127. [DOI] [PubMed] [Google Scholar]
- 45.Rani N., Singla R.K., Narwal S., Tanushree, Kumar N., Mominur Rahman M. Medicinal Plants Used as an Alternative to Treat Gingivitis and Periodontitis. Evid. Based Complement. Altern. Med. 2022;2022:2327641. doi: 10.1155/2022/2327641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kazi M.A., Sahito R., Abbas Q., Ullah S., Majid A., Phull A.R., Rahman M.M., Kim S.J. The Inhibitory Effect of Polyphenon 60 from Green Tea on Melanin and Tyrosinase in Zebrafish and A375 Human Melanoma Cells. Evid. Based Complement. Altern. Med. 2022;2022:7739023. doi: 10.1155/2022/7739023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rhaman M., Islam R., Akash S., Mim M., Noor A., Nepovimova E., Valis M., Kuca K., Sharma R. Exploring the Role of Nanomedicines for the Therapeutic Approach of Central Nervous System Dysfunction: At a Glance. Front. Cell Dev. Biol. 2022;10:1780. doi: 10.3389/fcell.2022.989471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shohag S., Akhter S., Islam S., Sarker T., Sifat M.K., Rahman M.M., Islam M.R., Sharma R. Perspectives on the Molecular Mediators of Oxidative Stress and Antioxidant Strategies in the Context of Neuroprotection and Neurolongevity: An Extensive Review. Oxid. Med. Cell. Longev. 2022;2022:7743705. doi: 10.1155/2022/7743705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rahman M.M., Islam M.R., Yamin M., Islam M.M., Sarker M.T., Meem A.F.K., Akter A., Emran T.B., Cavalu S., Sharma R. Emerging Role of Neuron-Glia in Neurological Disorders: At a Glance. Oxid. Med. Cell. Longev. 2022;2022:3201644. doi: 10.1155/2022/3201644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rauf A., Rahman M.M. Potential Therapeutics against Neurological Disorders: Natural Products-Based Drugs. Front. Pharmacol. 2022;13:3178. doi: 10.3389/fphar.2022.950457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rahman M.M., Islam M.R., Rahman F., Rahaman M.S., Khan M.S., Abrar S., Ray T.K., Uddin M.B., Kali M.S.K., Dua K., et al. Emerging Promise of Computational Techniques in Anti-Cancer Research: At a Glance. Bioengineering. 2022;9:335. doi: 10.3390/bioengineering9080335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taylor W.F., Jabbarzadeh E. The Use of Natural Products to Target Cancer Stem Cells. Am. J. Cancer Res. 2017;7:1588–1605. [PMC free article] [PubMed] [Google Scholar]
- 53.Walcher L., Kistenmacher A.-K., Suo H., Kitte R., Dluczek S., Strauß A., Blaudszun A.-R., Yevsa T., Fricke S., Kossatz-Boehlert U. Cancer Stem Cells—Origins and Biomarkers: Perspectives for Targeted Personalized Therapies. Front. Immunol. 2020;11:1280. doi: 10.3389/fimmu.2020.01280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Telang N. Stem Cell Models for Cancer Therapy. Int. J. Mol. Sci. 2022;23:7055. doi: 10.3390/ijms23137055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jia D., Nagaoka Y., Katsumata M., Orsulic S. Inflammation Is a Key Contributor to Ovarian Cancer Cell Seeding. Sci. Rep. 2018;8:12394. doi: 10.1038/s41598-018-30261-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yamulla R.J., Nalubola S., Flesken-Nikitin A., Nikitin A.Y., Schimenti J.C. Most Commonly Mutated Genes in High-Grade Serous Ovarian Carcinoma Are Nonessential for Ovarian Surface Epithelial Stem Cell Transformation. Cell Rep. 2020;32:108086. doi: 10.1016/j.celrep.2020.108086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saed G.M., Diamond M.P., Fletcher N.M. Updates of the Role of Oxidative Stress in the Pathogenesis of Ovarian Cancer. Gynecol. Oncol. 2017;145:595–602. doi: 10.1016/j.ygyno.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 58.Li H., Liu Y., Wang Y., Zhao X., Qi X. Hormone Therapy for Ovarian Cancer: Emphasis on Mechanisms and Applications (Review) Oncol. Rep. 2021;46:223. doi: 10.3892/or.2021.8174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Risch H.A. Hormonal Etiology of Epithelial Ovarian Cancer, with a Hypothesis Concerning the Role of Androgens and Progesterone. J. Natl. Cancer Inst. 1998;90:1774–1786. doi: 10.1093/jnci/90.23.1774. [DOI] [PubMed] [Google Scholar]
- 60.Browning L., Patel M.R., Horvath E.B., Tawara K., Jorcyk C.L. IL-6 and Ovarian Cancer: Inflammatory Cytokines in Promotion of Metastasis. Cancer Manag. Res. 2018;10:6685–6693. doi: 10.2147/CMAR.S179189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kang Y.C., Kim K.M., Lee K.S., Namkoong S., Lee S.J., Han J.A., Jeoung D., Ha K.S., Kwon Y.G., Kim Y.M. Serum Bioactive Lysophospholipids Prevent TRAIL-Induced Apoptosis via PI3K/Akt-Dependent CFLIP Expression and Bad Phosphorylation. Cell Death Differ. 2004;11:1287–1298. doi: 10.1038/sj.cdd.4401489. [DOI] [PubMed] [Google Scholar]
- 62.Giuntoli R.L., Webb T.J., Zoso A., Rogers O., Diaz-Montes T.P., Bristow R.E., Oelke M. Ovarian Cancer-Associated Ascites Demonstrates Altered Immune Environment-2009. Anticancer Res. 2009;29:2875–2884. [PubMed] [Google Scholar]
- 63.Bast R.C., Hennessy B., Mills G.B. The Biology of Ovarian Cancer: New Opportunities for Translation. Nat. Rev. Cancer. 2009;9:415–428. doi: 10.1038/nrc2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chou C.H., Wei L.H., Kuo M.L., Huang Y.J., Lai K.P., Chen C.A., Hsieh C.Y. Up-Regulation of Interleukin-6 in Human Ovarian Cancer Cell via a Gi/PI3K-Akt/NF-ΚB Pathway by Lysophosphatidic Acid, an Ovarian Cancer-Activating Factor. Carcinogenesis. 2005;26:45–52. doi: 10.1093/carcin/bgh301. [DOI] [PubMed] [Google Scholar]
- 65.Mackay H.J., Twelves C.J. Targeting the Protein Kinase C Family: Are We There Yet? Nat. Rev. Cancer. 2007;7:554–562. doi: 10.1038/nrc2168. [DOI] [PubMed] [Google Scholar]
- 66.Kumari S., Badana A.K., Murali Mohan G., Shailender G., Malla R.R. Reactive Oxygen Species: A Key Constituent in Cancer Survival. Biomark. Insights. 2018;13:1177271918755391. doi: 10.1177/1177271918755391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wong R.S.Y. Role of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) in Cancer Prevention and Cancer Promotion. Adv. Pharmacol. Sci. 2019;2019:3418975. doi: 10.1155/2019/3418975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen S.N., Chang R., Lin L.T., Chern C.U., Tsai H.W., Wen Z.H., Li Y.H., Li C.J., Tsui K.H. MicroRNA in Ovarian Cancer: Biology, Pathogenesis, and Therapeutic Opportunities. Int. J. Environ. Res. Public Health. 2019;16:1510. doi: 10.3390/ijerph16091510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Serhan K., Gartung A., Panigrahy D. Drawing a Link between the Thromboxane A2 Pathway and the Role of Platelets and Tumor Cells in Ovarian Cancer. Prostaglandins Other Lipid Mediat. 2018;137:40–45. doi: 10.1016/j.prostaglandins.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 70.Rajagopal C., Lankadasari M.B., Aranjani J.M., Harikumar K.B. Targeting Oncogenic Transcription Factors by Polyphenols: A Novel Approach for Cancer Therapy. Pharmacol. Res. 2018;130:273–291. doi: 10.1016/j.phrs.2017.12.034. [DOI] [PubMed] [Google Scholar]
- 71.Senthil K., Aranganathan S., Nalini N. Evidence of Oxidative Stress in the Circulation of Ovarian Cancer Patients. Clin. Chim. Acta. 2004;339:27–32. doi: 10.1016/j.cccn.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 72.Fletcher N.M., Jiang Z., Ali-Fehmi R., Levin N.K., Belotte J., Tainsky M.A., Diamond M.P., Abu-Soud H.M., Saed G.M. Myeloperoxidase and Free Iron Levels: Potential Biomarkers for Early Detection and Prognosis of Ovarian Cancer. Cancer Biomark. 2012;10:267–275. doi: 10.3233/CBM-2012-0255. [DOI] [PubMed] [Google Scholar]
- 73.Jiang Z., Fletcher N.M., Ali-Fehmi R., Diamond M.P., Abu-Soud H.M., Munkarah A.R., Saed G.M. Modulation of Redox Signaling Promotes Apoptosis in Epithelial Ovarian Cancer Cells. Gynecol. Oncol. 2011;122:418–423. doi: 10.1016/j.ygyno.2011.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Benhar M. Roles of Mammalian Glutathione Peroxidase and Thioredoxin Reductase Enzymes in the Cellular Response to Nitrosative Stress. Free Radic. Biol. Med. 2018;127:160–164. doi: 10.1016/j.freeradbiomed.2018.01.028. [DOI] [PubMed] [Google Scholar]
- 75.Castillo-Tong D.C., Pils D., Heinze G., Braicu I., Sehouli J., Reinthaller A., Schuster E., Wolf A., Watrowski R., Maki R.A., et al. Association of Myeloperoxidase with Ovarian Cancer. Tumor Biol. 2014;35:141–148. doi: 10.1007/s13277-013-1017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Saed G.M., Ali-Fehmi R., Jiang Z.L., Fletcher N.M., Diamond M.P., Abu-Soud H.M., Munkarah A.R. Myeloperoxidase Serves as a Redox Switch That Regulates Apoptosis in Epithelial Ovarian Cancer. Gynecol. Oncol. 2010;116:276–281. doi: 10.1016/j.ygyno.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kusriani H., Subarnas A., Diantini A., Iskandar Y. Cytotoxicity of Quercetin and Quercetin-3-O-Rhamnoside of Etlingera Elatior (Jack) RM Sm. Leaves against HeLa Cervical Cancer Cells. J. App. Pharm. Sci. 2021;11:85–90. [Google Scholar]
- 78.Rais J., Jafri A., Siddiqui S., Tripathi M., Arshad M. Phytochemicals in the Treatment of Ovarian Cancer. Front. Biosci. 2017;9:67–75. doi: 10.2741/e786. [DOI] [PubMed] [Google Scholar]
- 79.Hosein Farzaei M., Bahramsoltani R., Rahimi R. Phytochemicals as Adjunctive with Conventional Anticancer Therapies. Curr. Pharm. Des. 2016;22:4201–4218. doi: 10.2174/1381612822666160601100823. [DOI] [PubMed] [Google Scholar]
- 80.Shafabakhsh R., Asemi Z. Quercetin: A Natural Compound for Ovarian Cancer Treatment. J. Ovarian Res. 2019;12:55. doi: 10.1186/s13048-019-0530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vafadar A., Shabaninejad Z., Movahedpour A., Fallahi F., Taghavipour M., Ghasemi Y., Akbari M., Shafiee A., Hajighadimi S., Moradizarmehri S., et al. Quercetin and Cancer: New Insights into Its Therapeutic Effects on Ovarian Cancer Cells. Cell Biosci. 2020;10:32. doi: 10.1186/s13578-020-00397-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kubczak M., Szustka A., Rogalińska M. Molecular Targets of Natural Compounds with Anti-Cancer Properties. Int. J. Mol. Sci. 2021;22:13659. doi: 10.3390/ijms222413659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu J., Zhou T., Wang Y., Jiang Y., Wang Y. Mechanisms and Advances in Anti-Ovarian Cancer with Natural Plants Component. Molecules. 2021;26:5949. doi: 10.3390/molecules26195949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pistollato F., Calderón Iglesias R., Ruiz R., Aparicio S., Crespo J., Dzul Lopez L., Giampieri F., Battino M. The Use of Natural Compounds for the Targeting and Chemoprevention of Ovarian Cancer. Cancer Lett. 2017;411:191–200. doi: 10.1016/j.canlet.2017.09.050. [DOI] [PubMed] [Google Scholar]
- 85.Cheng X., Ferrell J.E. Apoptosis Propagates through the Cytoplasm as Trigger Waves. Science. 2018;361:607–612. doi: 10.1126/science.aah4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rajabi S., Maresca M., Yumashev A.V., Choopani R., Hajimehdipoor H. The Most Competent Plant-Derived Natural Products for Targeting Apoptosis in Cancer Therapy. Biomolecules. 2021;11:534. doi: 10.3390/biom11040534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu C., Zeng Y., Wen Y., Huang X., Liu Y. Natural Products Modulate Cell Apoptosis: A Promising Way for the Treatment of Ulcerative Colitis. Front. Pharmacol. 2022;13:806148. doi: 10.3389/fphar.2022.806148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Taparia S.S., Khanna A. Procyanidin-Rich Extract of Natural Cocoa Powder Causes ROS-Mediated Caspase-3 Dependent Apoptosis and Reduction of pro-MMP-2 in Epithelial Ovarian Carcinoma Cell Lines. Biomed. Pharmacother. 2016;83:130–140. doi: 10.1016/j.biopha.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 89.Xu X., Shi J., Gao H., Li Q. Zeylenone Inhibits Proliferation and Promotes Apoptosis in Ovarian Carcinoma Cells via Janus Kinase 2 / Signal Transducers and Activators of Transcription 3 Pathways. J. Obstet. Gynaecol. Res. 2018;44:1451–1457. doi: 10.1111/jog.13690. [DOI] [PubMed] [Google Scholar]
- 90.Lee D., Ko H., Kim Y.J., Kim S.N., Choi K.C., Yamabe N., Kim K.H., Kang K.S., Kim H.Y., Shibamoto T. Inhibition of A2780 Human Ovarian Carcinoma Cell Proliferation by a Rubus Component, Sanguiin H-6. J. Agric. Food Chem. 2016;64:801–805. doi: 10.1021/acs.jafc.5b05461. [DOI] [PubMed] [Google Scholar]
- 91.Yoon J.H., Shin J.W., Pham T.H., Choi Y.J., Ryu H.W., Oh S.R., Oh J.W., Yoon D.Y. Methyl Lucidone Induces Apoptosis and G2/M Phase Arrest via the PI3K/Akt/NF-ΚB Pathway in Ovarian Cancer Cells. Pharm. Biol. 2020;58:51–59. doi: 10.1080/13880209.2019.1701044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chang C.-C., Kuan C.-P., Lin J.-Y., Lai J.-S., Ho T.-F. Tanshinone IIA Facilitates TRAIL Sensitization by Up-Regulating DR5 through the ROS-JNK-CHOP Signaling Axis in Human Ovarian Carcinoma Cell Lines. Chem. Res. Toxicol. 2015;28:1574–1583. doi: 10.1021/acs.chemrestox.5b00150. [DOI] [PubMed] [Google Scholar]
- 93.Taheri M., Roudbari N.H., Amidi F., Parivar K. The Protective Effect of Sulforaphane against Oxidative Stress in Granulosa Cells of Patients with Polycystic Ovary Syndrome (PCOS) through Activation of AMPK/AKT/NRF2 Signaling Pathway. Reprod. Biol. 2021;21:100563. doi: 10.1016/j.repbio.2021.100563. [DOI] [PubMed] [Google Scholar]
- 94.Ribaudo G., Coghi P., Yang L.J., Ng J.P.L., Mastinu A., Memo M., Wong V.K.W., Gianoncelli A. Computational and Experimental Insights on the Interaction of Artemisinin, Dihydroartemisinin and Chloroquine with SARS-CoV-2 Spike Protein Receptor-Binding Domain (RBD) Nat. Prod. Res. 2022;36:5358–5363. doi: 10.1080/14786419.2021.1925894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coghi P., Yang L.J., Ng J.P.L., Haynes R.K., Memo M., Gianoncelli A., Wong V.K.W., Ribaudo G. A Drug Repurposing Approach for Antimalarials Interfering with SARS-CoV-2 Spike Protein Receptor Binding Domain (RBD) and Human Angiotensin-Converting Enzyme 2 (ACE2) Pharmaceuticals. 2021;14:954. doi: 10.3390/ph14100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Abate G., Zhang L., Pucci M., Morbini G., Mac Sweeney E., Maccarinelli G., Ribaudo G., Gianoncelli A., Uberti D., Memo M., et al. Phytochemical Analysis and Anti-Inflammatory Activity of Different Ethanolic Phyto-Extracts of Artemisia Annual. Biomolecules. 2021;11:975. doi: 10.3390/biom11070975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu Y., Gao S., Zhu J., Zheng Y., Zhang H., Sun H. Dihydroartemisinin Induces Apoptosis and Inhibits Proliferation, Migration, and Invasion in Epithelial Ovarian Cancer via Inhibition of the Hedgehog Signaling Pathway. Cancer Med. 2018;7:5704–5715. doi: 10.1002/cam4.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang H., Jiao Y., Shi C., Song X., Chang Y., Ren Y., Shi X. Berbamine Suppresses Cell Proliferation and Promotes Apoptosis in Ovarian Cancer Partially via the Inhibition of Wnt/β-Catenin Signaling. Acta Biochim. Biophys. Sin. 2018;50:532–539. doi: 10.1093/abbs/gmy036. [DOI] [PubMed] [Google Scholar]
- 99.Wang F., Chang Z., Fan Q., Wang L. Epigallocatechin-3-Gallate Inhibits the Proliferation and Migration of Human Ovarian Carcinoma Cells by Modulating P38 Kinase and Matrix Metalloproteinase-2. Mol. Med. Rep. 2014;9:1085–1089. doi: 10.3892/mmr.2014.1909. [DOI] [PubMed] [Google Scholar]
- 100.Ahmed O.H., Hamad M.N., Jaafar N.S. Phytochemical Investigation of Chenopodium Murale (Family: Chenopodiaceae) Cultivated in Iraq, Isolation and Identification of Scopoletin and Gallic Acid. Asian J. Pharm. Clin. Res. 2017;10:70–77. doi: 10.22159/ajpcr.2017.v10i11.20504. [DOI] [Google Scholar]
- 101.Jeong M., Kim H.M., Kim H.J., Choi J.-H., Jang D.S. Kudsuphilactone B, a Nortriterpenoid Isolated from Schisandra Chinensis Fruit, Induces Caspase-Dependent Apoptosis in Human Ovarian Cancer A2780 Cells. Arch. Pharmacal Res. 2017;40:500–508. doi: 10.1007/s12272-017-0902-5. [DOI] [PubMed] [Google Scholar]
- 102.Vergara D., Simeone P., Toraldo D., Del Boccio P., Vergaro V., Leporatti S., Pieragostino D., Tinelli A., De Domenico S., Alberti S., et al. Resveratrol Downregulates Akt/GSK and ERK Signalling Pathways in OVCAR-3 Ovarian Cancer Cells. Mol. Biosyst. 2012;8:1078–1087. doi: 10.1039/c2mb05486h. [DOI] [PubMed] [Google Scholar]
- 103.Seo J.-A., Kim B., Dhanasekaran D.N., Tsang B.K., Song Y.S. Curcumin Induces Apoptosis by Inhibiting Sarco/Endoplasmic Reticulum Ca2+ ATPase Activity in Ovarian Cancer Cells. Cancer Lett. 2016;371:30–37. doi: 10.1016/j.canlet.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 104.Manivannan E., Amawi H., Hussein N., Karthikeyan C., Fetcenko A., Narayana Moorthy N.S.H., Trivedi P., Tiwari A.K. Design and Discovery of Silybin Analogues as Antiproliferative Compounds Using a Ring Disjunctive—Based, Natural Product Lead Optimization Approach. Eur. J. Med. Chem. 2017;133:365–378. doi: 10.1016/j.ejmech.2017.03.033. [DOI] [PubMed] [Google Scholar]
- 105.Jiao R., Liu Y., Gao H., Xiao J., So K.F. The Anti-Oxidant and Antitumor Properties of Plant Polysaccharides. Am. J. Chin. Med. 2016;44:463–488. doi: 10.1142/S0192415X16500269. [DOI] [PubMed] [Google Scholar]
- 106.Xu D.-P., Li Y., Meng X., Zhou T., Zhou Y., Zheng J., Zhang J.-J., Li H.-B. Natural Antioxidants in Foods and Medicinal Plants: Extraction, Assessment and Resources. IJMS. 2017;18:96. doi: 10.3390/ijms18010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ribaudo G., Bortoli M., Pavan C., Zagotto G., Orian L. Antioxidant Potential of Psychotropic Drugs: From Clinical Evidence to In Vitro and In Vivo Assessment and toward a New Challenge for in Silico Molecular Design. Antioxidants. 2020;9:714. doi: 10.3390/antiox9080714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kwon Y. Food-Derived Polyphenols Inhibit the Growth of Ovarian Cancer Cells Irrespective of Their Ability to Induce Antioxidant Responses. Heliyon. 2018;4:e00753. doi: 10.1016/j.heliyon.2018.e00753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sunil C., Xu B. An Insight into the Health-Promoting Effects of Taxifolin (Dihydroquercetin) Phytochemistry. 2019;166:112066. doi: 10.1016/j.phytochem.2019.112066. [DOI] [PubMed] [Google Scholar]
- 110.Ribaudo G., Coghi P., Zanforlin E., Law B.Y.K., Wu Y.Y.J., Han Y., Qiu A.C., Qu Y.Q., Zagotto G., Wong V.K.W. Semi-Synthetic Isoflavones as BACE-1 Inhibitors against Alzheimer’s Disease. Bioorg. Chem. 2019;87:474–483. doi: 10.1016/j.bioorg.2019.03.034. [DOI] [PubMed] [Google Scholar]
- 111.Park S., Bazer F.W., Lim W., Song G. The O-Methylated Isoflavone, Formononetin, Inhibits Human Ovarian Cancer Cell Proliferation by Sub G0/G1 Cell Phase Arrest through PI3K/AKT and ERK1/2 Inactivation. J. Cell. Biochem. 2018;119:7377–7387. doi: 10.1002/jcb.27041. [DOI] [PubMed] [Google Scholar]
- 112.Ai Z., Lu Y., Qiu S., Fan Z. Overcoming Cisplatin Resistance of Ovarian Cancer Cells by Targeting HIF-1-Regulated Cancer Metabolism. Cancer Lett. 2016;373:36–44. doi: 10.1016/j.canlet.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Park S., Lim W., Jeong W., Bazer F.W., Lee D., Song G. Sideroxylin (Callistemon lanceolatus) Suppressed Cell Proliferation and Increased Apoptosis in Ovarian Cancer Cells Accompanied by Mitochondrial Dysfunction, the Generation of Reactive Oxygen Species, and an Increase of Lipid Peroxidation. J. Cell. Physiol. 2018;233:8597–8604. doi: 10.1002/jcp.26540. [DOI] [PubMed] [Google Scholar]
- 114.Ribaudo G., Zanforlin E., Canton M., Bova S., Zagotto G. Preliminary Studies of Berberine and Its Semi-Synthetic Derivatives as a Promising Class of Multi-Target Anti-Parkinson Agents. Nat. Prod. Res. 2018;32:1395–1401. doi: 10.1080/14786419.2017.1350669. [DOI] [PubMed] [Google Scholar]
- 115.Hou D., Xu G., Zhang C., Li B., Qin J., Hao X., Liu Q., Zhang X., Liu J., Wei J., et al. Berberine Induces Oxidative Dna Damage and Impairs Homologous Recombination Repair in Ovarian Cancer Cells to Confer Increased Sensitivity to Parp Inhibition. Cell Death Dis. 2017;8:e3070. doi: 10.1038/cddis.2017.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kakar S.S., Jala V.R., Fong M.Y. Synergistic Cytotoxic Action of Cisplatin and Withaferin A on Ovarian Cancer Cell Lines. Biochem. Biophys. Res. Commun. 2012;423:819–825. doi: 10.1016/j.bbrc.2012.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Guo Y., Zhang Z., Wang Z., Liu G., Liu Y., Wang H. Astragalus Polysaccharides Inhibit Ovarian Cancer Cell Growth via MicroRNA-27a/FBXW7 Signaling Pathway. Biosci. Rep. 2020;40:BSR20193396. doi: 10.1042/BSR20193396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fernandes J.V., Cobucci R.N.O., Jatobá C.A.N., de Medeiros Fernandes T.A.A., de Azevedo J.W.V., de Araújo J.M.G. The Role of the Mediators of Inflammation in Cancer Development. Pathol. Oncol. Res. 2015;21:527–534. doi: 10.1007/s12253-015-9913-z. [DOI] [PubMed] [Google Scholar]
- 119.Kim M.K., Kim K., Han J.Y., Lim J.M., Song Y.S. Modulation of Inflammatory Signaling Pathways by Phytochemicals in Ovarian Cancer. Genes Nutr. 2011;6:109–115. doi: 10.1007/s12263-011-0209-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yin J., Yu C., Yang Z., He J.L., Chen W.J., Liu H.Z., Li W.M., Liu H.T., Wang Y.X. Tetramethylpyrazine Inhibits Migration of SKOV3 Human Ovarian Carcinoma Cells and Decreases the Expression of Interleukin-8 via the ERK1/2, P38 and AP-1 Signaling Pathways. Oncol. Rep. 2011;26:671–679. doi: 10.3892/or.2011.1334. [DOI] [PubMed] [Google Scholar]
- 121.Lu J., Xu Y., Wei X., Zhao Z., Xue J., Liu P. Emodin Inhibits the Epithelial to Mesenchymal Transition of Epithelial Ovarian Cancer Cells via ILK/GSK-3 β /Slug Signaling Pathway. BioMed Res. Int. 2016;2016:6253280. doi: 10.1155/2016/6253280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Y., Chen S., Wei C., Rankin G.O., Rojanasakul Y., Ren N., Ye X., Chen Y.C. Dietary Compound Proanthocyanidins from Chinese Bayberry (Myrica Rubra Sieb. et Zucc.) Leaves Inhibit Angiogenesis and Regulate Cell Cycle of Cisplatin-Resistant Ovarian Cancer Cells via Targeting Akt Pathway. J. Funct. Foods. 2018;40:573–581. doi: 10.1016/j.jff.2017.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhou J., Jiang Y.-Y., Wang X.-X., Wang H.-P., Chen H., Wu Y.-C., Wang L., Pu X., Yue G.-Z., Zhang L. Tanshinone IIA Suppresses Ovarian Cancer Growth through Inhibiting Malignant Properties and Angiogenesis. Ann. Transl. Med. 2020;8:1295. doi: 10.21037/atm-20-5741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Liskova A., Koklesova L., Samec M., Varghese E., Abotaleb M., Samuel S.M., Smejkal K., Biringer K., Petras M., Blahutova D., et al. Implications of Flavonoids as Potential Modulators of Cancer Neovascularity. J. Cancer Res. Clin. Oncol. 2020;146:3079–3096. doi: 10.1007/s00432-020-03383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gao J., Zhu H., Wan H., Zou X., Ma X., Gao G. Harmine Suppresses the Proliferation and Migration of Human Ovarian Cancer Cells through Inhibiting ERK/CREB Pathway. Oncol. Rep. 2017;38:2927–2934. doi: 10.3892/or.2017.5952. [DOI] [PubMed] [Google Scholar]
- 126.Kim K.K., Singh A.P., Singh R.K., DeMartino A., Brard L., Vorsa N., Lange T.S., Moore R.G. Anti-Angiogenic Activity of Cranberry Proanthocyanidins and Cytotoxic Properties in Ovarian Cancer Cells. Int. J. Oncol. 2012;40:227–235. doi: 10.3892/ijo.2011.1198. [DOI] [PubMed] [Google Scholar]
- 127.Dias A.S., Helguero L., Almeida C.R., Duarte I.F. Natural Compounds as Metabolic Modulators of the Tumor Microenvironment. Molecules. 2021;26:3494. doi: 10.3390/molecules26123494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang W., Li S., Li C., Li T., Huang Y. Remodeling Tumor Microenvironment with Natural Products to Overcome Drug Resistance. Front. Immunol. 2022;13:1051998. doi: 10.3389/fimmu.2022.1051998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kenny H.A., Hart P.C., Kordylewicz K., Lal M., Shen M., Kara B., Chen Y.-J., Grassl N., Alharbi Y., Pattnaik B.R., et al. The Natural Product β-Escin Targets Cancer and Stromal Cells of the Tumor Microenvironment to Inhibit Ovarian Cancer Metastasis. Cancers. 2021;13:3931. doi: 10.3390/cancers13163931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Di W., Zhang L., Yi H., Han X., Zhang Y., Xin L. Exopolysaccharides Produced by Lactobacillus Strains Suppress HT-29 Cell Growth via Induction of G0/G1 Cell Cycle Arrest and Apoptosis. Oncol. Lett. 2018;16:3577–3586. doi: 10.3892/ol.2018.9129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ren L., Cao Q.X., Zhai F.R., Yang S.Q., Zhang H.X. Asiatic Acid Exerts Anticancer Potential in Human Ovarian Cancer Cells via Suppression of PI3K/Akt/MTOR Signalling. Pharm. Biol. 2016;54:2377–2382. doi: 10.3109/13880209.2016.1156709. [DOI] [PubMed] [Google Scholar]
- 132.Yu S., Yan H., Zhang L., Shan M., Chen P., Ding A., Li S.F.Y. A Review on the Phytochemistry, Pharmacology, and Pharmacokinetics of Amentoflavone, a Naturally-Occurring Biflavonoid. Molecules. 2017;22:299. doi: 10.3390/molecules22020299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang Y., Chen S., Wei C., Rankin G.O., Ye X., Chen Y.C. Dietary Compound Proanthocyanidins from Chinese Bayberry (Myrica Rubra Sieb. et Zucc.) Leaves Attenuate Chemotherapy-Resistant Ovarian Cancer Stem Cell Traits via Targeting the Wnt/β-Catenin Signaling Pathway and Inducing G1 Cell Cycle Arrest. Food Funct. 2018;9:525–533. doi: 10.1039/C7FO01453H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Nordin N., Fadaeinasab M., Mohan S., Hashim N.M., Othman R., Karimian H., Iman V., Ramli N., Ali H.M., Majid N.A. Pulchrin A, a New Natural Coumarin Derivative of Enicosanthellum Pulchrum, Induces Apoptosis in Ovarian Cancer Cells via Intrinsic Pathway. PLoS ONE. 2016;11:e0154023. doi: 10.1371/journal.pone.0154023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kavandi L., Lee L.R., Bokhari A.A., Pirog J.E., Jiang Y., Ahmad K.A., Syed V. The Chinese Herbs Scutellaria Baicalensis and Fritillaria Cirrhosa Target NFκB to Inhibit Proliferation of Ovarian and Endometrial Cancer Cells. Mol. Carcinog. 2015;54:368–378. doi: 10.1002/mc.22107. [DOI] [PubMed] [Google Scholar]
- 136.Jia S., Shen M., Zhang F., Xie J. Recent Advances in Momordica Charantia: Functional Components and Biological Activities. Int. J. Mol. Sci. 2017;18:2555. doi: 10.3390/ijms18122555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen H.Y., Huang T.C., Shieh T.M., Wu C.H., Lin L.C., Hsia S.M. Isoliquiritigenin Induces Autophagy and Inhibits Ovarian Cancer Cell Growth. Int. J. Mol. Sci. 2017;18:2025. doi: 10.3390/ijms18102025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhan L., Zhang Y., Wang W., Song E., Fan Y., Li J., Wei B. Autophagy as an Emerging Therapy Target for Ovarian Carcinoma. Oncotarget. 2016;7:83476–83487. doi: 10.18632/oncotarget.13080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang H.Y., Peng Y., Wang J., Gu A.X., Li Q., Mao D.W., Guo L.Y. Effect of Autophagy on the Resveratrol-Induced Apoptosis of Ovarian Cancer SKOV3 Cells. J. Cell. Biochem. 2019;120:7788–7793. doi: 10.1002/jcb.28053. [DOI] [PubMed] [Google Scholar]
- 140.Fong M.Y., Jin S., Rane M., Singh R.K., Gupta R., Kakar S.S. Withaferin a Synergizes the Therapeutic Effect of Doxorubicin through ROS-Mediated Autophagy in Ovarian Cancer. PLoS ONE. 2012;7:e42265. doi: 10.1371/journal.pone.0042265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Che X., Yan H., Sun H., Dongol S., Wang Y., Lv Q., Jiang J. Grifolin Induces Autophagic Cell Death by Inhibiting the Akt/MTOR/S6K Pathway in Human Ovarian Cancer Cells. Oncol. Rep. 2016;36:1041–1047. doi: 10.3892/or.2016.4840. [DOI] [PubMed] [Google Scholar]
- 142.Lin L., Baehrecke E.H. Autophagy, Cell Death, and Cancer. Mol. Cell. Oncol. 2015;2:e985913. doi: 10.4161/23723556.2014.985913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhou J., Jiang Y.-Y., Chen H., Wu Y.-C., Zhang L. Tanshinone I Attenuates the Malignant Biological Properties of Ovarian Cancer by Inducing Apoptosis and Autophagy via the Inactivation of PI3K/AKT/MTOR Pathway. Cell Prolif. 2020;53:e12739. doi: 10.1111/cpr.12739. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 144.Gossner G., Choi M., Tan L., Fogoros S., Griffith K.A., Kuenker M., Liu J.R. Genistein-Induced Apoptosis and Autophagocytosis in Ovarian Cancer Cells. Gynecol. Oncol. 2007;105:23–30. doi: 10.1016/j.ygyno.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 145.Engelke L.H., Hamacher A., Proksch P., Kassack M.U. Ellagic Acid and Resveratrol Prevent the Development of Cisplatin Resistance in the Epithelial Ovarian Cancer Cell Line A2780. J. Cancer. 2016;7:353–363. doi: 10.7150/jca.13754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pastorek M., Simko V., Takacova M., Barathova M., Bartosova M., Hunakova L., Sedlakova O., Hudecova S., Krizanova O., Dequiedt F., et al. Sulforaphane Reduces Molecular Response to Hypoxia in Ovarian Tumor Cells Independently of Their Resistance to Chemotherapy. Int. J. Oncol. 2015;47:51–60. doi: 10.3892/ijo.2015.2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kim Y., Lee S.M., Kim J.H. Unripe Rubus Coreanus Miquel Suppresses Migration and Invasion of Human Prostate Cancer Cells by Reducing Matrix Metalloproteinase Expression. Biosci. Biotechnol. Biochem. 2014;78:1402–1411. doi: 10.1080/09168451.2014.921550. [DOI] [PubMed] [Google Scholar]
- 148.Kim M.K., Choi H.S., Cho S.G., Shin Y.C., Ko S.G. Rubus Coreanus Miquel Extract Causes Apoptosis of Doxorubicin-Resistant NCI/ADR-RES Ovarian Cancer Cells via JNK Phosphorylation. Mol. Med. Rep. 2016;13:4065–4072. doi: 10.3892/mmr.2016.4996. [DOI] [PubMed] [Google Scholar]
- 149.Uche F.I., McCullagh J., Claridge T.W.D., Richardson A., Li W.-W. Synthesis of (Aminoalkyl)Cycleanine Analogues: Cytotoxicity, Cellular Uptake, and Apoptosis Induction in Ovarian Cancer Cells. Bioorg. Med. Chem. Lett. 2018;28:1652–1656. doi: 10.1016/j.bmcl.2018.03.038. [DOI] [PubMed] [Google Scholar]
- 150.Chen H., Landen C.N., Li Y., Alvarez R.D., Tollefsbol T.O. Epigallocatechin Gallate and Sulforaphane Combination Treatment Induce Apoptosis in Paclitaxel-Resistant Ovarian Cancer Cells through HTERT and Bcl-2 down-Regulation. Exp. Cell Res. 2013;319:697–706. doi: 10.1016/j.yexcr.2012.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Chen T., Xu Y., Guo H., Liu Y., Hu P., Yang X., Li X., Ge S., Velu S.E., Nadkarni D.H., et al. Experimental Therapy of Ovarian Cancer with Synthetic Makaluvamine Analog: In Vitro and In Vivo Anticancer Activity and Molecular Mechanisms of Action. PLoS ONE. 2011;6:e20729. doi: 10.1371/journal.pone.0020729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Li N., Li C., Zhang J., Jiang Q., Wang Z., Nie S., Gao Z., Li G., Fang H., Ren S., et al. Discovery of Semisynthetic Celastrol Derivatives Exhibiting Potent Anti-Ovarian Cancer Stem Cell Activity and STAT3 Inhibition. Chem. Biol. Interact. 2022;366:110172. doi: 10.1016/j.cbi.2022.110172. [DOI] [PubMed] [Google Scholar]
- 153.Beretta G.L., Ribaudo G., Menegazzo I., Supino R., Capranico G., Zunino F., Zagotto G. Synthesis and Evaluation of New Naphthalene and Naphthoquinone Derivatives as Anticancer Agents: Naphthalene and Naphthoquinone Derivatives as Anticancer Agents. Arch. Pharm. Chem. Life Sci. 2017;350:e1600286. doi: 10.1002/ardp.201600286. [DOI] [PubMed] [Google Scholar]
- 154.Amrine C.S.M., Huntsman A.C., Doyle M.G., Burdette J.E., Pearce C.J., Fuchs J.R., Oberlies N.H. Semisynthetic Derivatives of the Verticillin Class of Natural Products through Acylation of the C11 Hydroxy Group. ACS Med. Chem. Lett. 2021;12:625–630. doi: 10.1021/acsmedchemlett.1c00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Prasad S., Aggarwal B.B. Herbal Medicine: Biomolecular and Clinical Aspects. 2nd ed. CRC Press; Boca Raton, FL, USA: 2011. Turmeric, the Golden Spice. [Google Scholar]
- 156.Zhou H., Beevers C.S., Huang S. The Targets of Curcumin. Curr. Drug Targets. 2012;12:332–347. doi: 10.2174/138945011794815356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dobbin Z.C., Landen C.N. The Importance of the PI3K/AKT/MTOR Pathway in the Progression of Ovarian Cancer. Int. J. Mol. Sci. 2013;14:8213–8227. doi: 10.3390/ijms14048213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Yu Z., Wan Y., Liu Y., Yang J., Li L., Zhang W. Curcumin Induced Apoptosis via PI3K/Akt-Signalling Pathways in SKOV3 Cells. Pharm. Biol. 2016;54:2026–2032. doi: 10.3109/13880209.2016.1139601. [DOI] [PubMed] [Google Scholar]
- 159.Watson J.L., Greenshields A., Hill R., Hilchie A., Lee P.W., Giacomantonio C.A., Hoskin D.W. Curcumin-Induced Apoptosis in Ovarian Carcinoma Cells Is P53-Independent and Involves P38 Mitogen-Activated Protein Kinase Activation and Downregulation of Bcl-2 and Survivin Expression and Akt Signaling. Mol. Carcinog. 2010;49:13–24. doi: 10.1002/mc.20571. [DOI] [PubMed] [Google Scholar]
- 160.Bowman T., Garcia R., Turkson J., Jove R. STATs in Oncogenesis. Oncogene. 2000;19:2474–2488. doi: 10.1038/sj.onc.1203527. [DOI] [PubMed] [Google Scholar]
- 161.Saydmohammed M., Joseph D., Syed V. Curcumin Suppresses Constitutive Activation of STAT-3 by up-Regulating Protein Inhibitor of Activated STAT-3 (PIAS-3) in Ovarian and Endometrial Cancer Cells. J. Cell. Biochem. 2010;110:447–456. doi: 10.1002/jcb.22558. [DOI] [PubMed] [Google Scholar]
- 162.Seo J.H., Jeong K.J., Oh W.J., Sul H.J., Sohn J.S., Kim Y.K., Cho D.Y., Kang J.K., Park C.G., Lee H.Y. Lysophosphatidic Acid Induces STAT3 Phosphorylation and Ovarian Cancer Cell Motility: Their Inhibition by Curcumin. Cancer Lett. 2010;288:50–56. doi: 10.1016/j.canlet.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 163.Kinose Y., Sawada K., Nakamura K., Kimura T. The Role of MicroRNAs in Ovarian Cancer. BioMed Res. Int. 2014;2014:249393. doi: 10.1155/2014/249393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Du Z., Sha X. Demethoxycurcumin Inhibited Human Epithelia Ovarian Cancer Cells’ Growth via up-Regulating MiR-551a. Tumor Biol. 2017;39:1010428317694302. doi: 10.1177/1010428317694302. [DOI] [PubMed] [Google Scholar]
- 165.Takei Y., Kadomatsu K., Muramatsu T., Matsuo S., Itoh H., Nakazawa K., Kubota S. Antisense Oligodeoxynucleotide Targeted to Midkine, a Heparin-Binding Growth Factor, Suppresses Tumorigenicity of Mouse Rectal Carcinoma Cells. Cancer Res. 2001;61:8486–8491. [PubMed] [Google Scholar]
- 166.Zhao S.F., Zhang X., Zhang X.J., Shi X.Q., Yu Z.J., Kan Q.C. Induction of MicroRNA-9 Mediates Cytotoxicity of Curcumin against SKOV3 Ovarian Cancer Cells. Asian Pac. J. Cancer Prev. 2014;15:3363–3368. doi: 10.7314/APJCP.2014.15.8.3363. [DOI] [PubMed] [Google Scholar]
- 167.Al-Alem L., Curry T.E., Jr. Ovarian Cancer: Involvement of the Matrix Metalloproteinases. Reproduction. 2015;150:R55. doi: 10.1530/REP-14-0546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lv J., Shao Q., Wang H., Shi H., Wang T., Gao W., Song B., Zheng G., Kong B., Qu X. Effects and Mechanisms of Curcumin and Basil Polysaccharide on the Invasion of SKOV3 Cells and Dendritic Cells. Mol. Med. Rep. 2013;8:1580–1586. doi: 10.3892/mmr.2013.1695. [DOI] [PubMed] [Google Scholar]
- 169.Pei H., Yang Y., Cui L., Yang J., Li X., Yang Y., Duan H. Bisdemethoxycurcumin Inhibits Ovarian Cancer via Reducing Oxidative Stress Mediated MMPs Expressions. Sci. Rep. 2016;6:28773. doi: 10.1038/srep28773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Slack-Davis J.K., Atkins K.A., Harrer C., Daniel Hershey E., Conaway M. Vascular Cell Adhesion Molecule-1 Is a Regulator of Ovarian Cancer Peritoneal Metastasis. Cancer Res. 2009;69:1469–1476. doi: 10.1158/0008-5472.CAN-08-2678. [DOI] [PubMed] [Google Scholar]
- 171.Daleprane J.B., Abdalla D.S. Emerging Roles of Propolis: Antioxidant, Cardioprotective, and Antiangiogenic Actions. Evid.-Based Complement. Altern. Med. 2013;2013:175135. doi: 10.1155/2013/175135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Baur J.A., Sinclair D.A. Therapeutic Potential of Resveratrol: The in Vivo Evidence. Nat. Rev. Drug Discov. 2006;5:493–506. doi: 10.1038/nrd2060. [DOI] [PubMed] [Google Scholar]
- 173.Pavan V., Mucignat-Caretta C., Redaelli M., Ribaudo G., Zagotto G. The Old Made New: Natural Compounds against Erectile Dysfunction: Natural Compounds against Erectile Dysfunction. Arch. Pharm. Chem. Life Sci. 2015;348:607–614. doi: 10.1002/ardp.201500075. [DOI] [PubMed] [Google Scholar]
- 174.Tan L., Wang W., He G., Kuick R.D., Gossner G., Kueck A.S., Wahl H., Opipari A.W., Liu J.R. Resveratrol Inhibits Ovarian Tumor Growth in an in Vivo Mouse Model. Cancer. 2016;122:722–729. doi: 10.1002/cncr.29793. [DOI] [PubMed] [Google Scholar]
- 175.Gwak H., Kim S., Dhanasekaran D.N., Song Y.S. Resveratrol Triggers ER Stress-Mediated Apoptosis by Disrupting N-Linked Glycosylation of Proteins in Ovarian Cancer Cells. Cancer Lett. 2016;371:347–353. doi: 10.1016/j.canlet.2015.11.032. [DOI] [PubMed] [Google Scholar]
- 176.Majewska E., Szeliga M. AKT/GSK3β Signaling in Glioblastoma. Neurochem. Res. 2017;42:918–924. doi: 10.1007/s11064-016-2044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Tino A.B., Chitcholtan K., Sykes P.H., Garrill A. Resveratrol and Acetyl-Resveratrol Modulate Activity of VEGF and IL-8 in Ovarian Cancer Cell Aggregates via Attenuation of the NF-ΚB Protein. J. Ovarian Res. 2016;9:84. doi: 10.1186/s13048-016-0293-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mikuła-Pietrasik J., Sosińska P., Książek K. Resveratrol Inhibits Ovarian Cancer Cell Adhesion to Peritoneal Mesothelium in Vitro by Modulating the Production of A5β1 Integrins and Hyaluronic Acid. Gynecol. Oncol. 2014;134:624–630. doi: 10.1016/j.ygyno.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 179.Park S.Y., Jeong K.J., Lee J., Yoon D.S., Choi W.S., Kim Y.K., Han J.W., Kim Y.M., Kim B.K., Lee H.Y. Hypoxia Enhances LPA-Induced HIF-1α and VEGF Expression: Their Inhibition by Resveratrol. Cancer Lett. 2007;258:63–69. doi: 10.1016/j.canlet.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 180.Sopo M., Anttila M., Hämäläinen K., Kivelä A., Ylä-Herttuala S., Kosma V.M., Keski-Nisula L., Sallinen H. Expression Profiles of VEGF-A, VEGF-D and VEGFR1 Are Higher in Distant Metastases than in Matched Primary High Grade Epithelial Ovarian Cancer. BMC Cancer. 2019;19:584. doi: 10.1186/s12885-019-5757-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Nag S.A., Qin J.J., Wang W., Wang M.H., Wang H., Zhang R. Ginsenosides as Anticancer Agents: In Vitro and in Vivo Activities, Structure-Activity Relationships, and Molecular Mechanisms of Action. Front. Pharmacol. 2012;3:25. doi: 10.3389/fphar.2012.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Ahuja A., Kim J.H., Kim J.-H., Yi Y.-S., Cho J.Y. Functional Role of Ginseng-Derived Compounds in Cancer. J. Ginseng Res. 2018;42:248–254. doi: 10.1016/j.jgr.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Li J., Liu T., Zhao L., Chen W., Hou H., Ye Z., Li X. Ginsenoside 20(S)-Rg3 Inhibits the Warburg Effect through STAT3 Pathways in Ovarian Cancer Cells. Int. J. Oncol. 2015;46:775–781. doi: 10.3892/ijo.2014.2767. [DOI] [PubMed] [Google Scholar]
- 184.Lu J., Wang L., Chen W., Wang Y., Zhen S., Chen H., Cheng J., Zhou Y., Li X., Zhao L. MiR-603 Targeted Hexokinase-2 to Inhibit the Malignancy of Ovarian Cancer Cells. Arch. Biochem. Biophys. 2019;661:1–9. doi: 10.1016/j.abb.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 185.Liu W., Zhang S.-X., Ai B., Pan H.-F., Zhang D., Jiang Y., Hu L.-H., Sun L.-L., Chen Z.-S., Lin L.-Z. Ginsenoside Rg3 Promotes Cell Growth Through Activation of MTORC1. Front. Cell Dev. Biol. 2021;9:730309. doi: 10.3389/fcell.2021.730309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Li J., Xi W., Li X., Sun H., Li Y. Advances in Inhibition of Protein-Protein Interactions Targeting Hypoxia-Inducible Factor-1 for Cancer Therapy. Bioorg. Med. Chem. 2019;27:1145–1158. doi: 10.1016/j.bmc.2019.01.042. [DOI] [PubMed] [Google Scholar]
- 187.Liu T., Zhao L., Hou H., Ding L., Chen W., Li X. Ginsenoside 20(S)-Rg3 Suppresses Ovarian Cancer Migration via Hypoxia-Inducible Factor 1 Alpha and Nuclear Factor-Kappa B Signals. Tumor Biol. 2017;39:1010428317692225. doi: 10.1177/1010428317692225. [DOI] [PubMed] [Google Scholar]
- 188.Liu D., Liu T., Teng Y., Chen W., Zhao L., Li X. Ginsenoside Rb1 Inhibits Hypoxia-Induced Epithelial-Mesenchymal Transition in Ovarian Cancer Cells by Regulating MicroRNA-25. Exp. Ther. Med. 2017;14:2895–2902. doi: 10.3892/etm.2017.4889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lengyel E. Ovarian Cancer Development and Metastasis. Am. J. Pathol. 2010;177:1053–1064. doi: 10.2353/ajpath.2010.100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ribaudo G., Oselladore E., Ongaro A., Zagotto G., Memo M., Gianoncelli A. Enhanced G-Quadruplex Selectivity of Flavonoid Glycoside Rutin over Quercetin. Nat. Prod. Res. 2020;36:3469–3473. doi: 10.1080/14786419.2020.1859505. [DOI] [PubMed] [Google Scholar]
- 191.Petrescu I., Lamotte-Brasseur J., Chessa J.P., Ntarima P., Claeyssens M., Devreese B., Marino G., Gerday C. Xylanase from the Psychrophilic Yeast Cryptococcus Adeliae. Extremophiles. 2000;4:137–144. doi: 10.1007/s007920070028. [DOI] [PubMed] [Google Scholar]
- 192.Liu Y., Gong W., Yang Z.Y., Zhou X.S., Gong C., Zhang T.R., Wei X., Ma D., Ye F., Gao Q.L. Quercetin Induces Protective Autophagy and Apoptosis through ER Stress via the P-STAT3/Bcl-2 Axis in Ovarian Cancer. Apoptosis. 2017;22:544–557. doi: 10.1007/s10495-016-1334-2. [DOI] [PubMed] [Google Scholar]
- 193.Driak D., Dvorska M., Bolehovska P., Svandova I., Novotny J., Halaska M. Bad and Bid—Potential Background Players in Preneoplastic to Neoplastic Shift in Human Endometrium. Neo. 2014;61:411–415. doi: 10.4149/neo_2014_050. [DOI] [PubMed] [Google Scholar]
- 194.Kemp K., Griffiths J., Campbell S., Lovell K. An Exploration of the Follow-up up Needs of Patients with Inflammatory Bowel Disease. J. Crohn’s Colitis. 2013;7:e386–e395. doi: 10.1016/j.crohns.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 195.Gao X., Wang B., Wei X., Men K., Zheng F., Zhou Y., Zheng Y., Gou M., Huang M., Guo G., et al. Anticancer Effect and Mechanism of Polymer Micelle-Encapsulated Quercetin on Ovarian Cancer. Nanoscale. 2012;4:7021–7030. doi: 10.1039/c2nr32181e. [DOI] [PubMed] [Google Scholar]
- 196.Gong C., Yang Z., Zhang L., Wang Y., Gong W., Liu Y. Quercetin Suppresses DNA Double-Strand Break Repair and Enhances the Radiosensitivity of Human Ovarian Cancer Cells via P53-Dependent Endoplasmic Reticulum Stress Pathway. OncoTargets Ther. 2018;11:17–27. doi: 10.2147/OTT.S147316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yang Z., Liu Y., Liao J., Gong C., Sun C., Zhou X., Wei X., Zhang T., Gao Q., Ma D., et al. Quercetin Induces Endoplasmic Reticulum Stress to Enhance CDDP Cytotoxicity in Ovarian Cancer: Involvement of STAT3 Signaling. FEBS J. 2015;282:1111–1125. doi: 10.1111/febs.13206. [DOI] [PubMed] [Google Scholar]
- 198.Long Q., Xie Y., Huang Y., Wu Q., Zhang H.C., Xiong S., Liu Y., Chen L., Wei Y., Zhao X., et al. Induction of Apoptosis and Inhibition of Angiogenesis by PEGylated Liposomal Quercetin in Both Cisplatin-Sensitive and Cisplatin-Resistant Ovarian Cancers. J. Biomed. Nanotechnol. 2013;9:965–975. doi: 10.1166/jbn.2013.1596. [DOI] [PubMed] [Google Scholar]
- 199.Catanzaro D., Ragazzi E., Vianello C., Caparrotta L., Montopoli M. Effect of Quercetin on Cell Cycle and Cyclin Expression in Ovarian Carcinoma and Osteosarcoma Cell Lines. Nat. Prod. Commun. 2015;10:1365–1368. doi: 10.1177/1934578X1501000813. [DOI] [PubMed] [Google Scholar]
- 200.Rashidi Z., Khosravizadeh Z., Talebi A., Khodamoradi K., Ebrahimi R., Amidi F. Overview of Biological Effects of Quercetin on Ovary. Phytother. Res. 2021;35:33–49. doi: 10.1002/ptr.6750. [DOI] [PubMed] [Google Scholar]
- 201.Dhanaraj T., Mohan M., Arunakaran J. Quercetin Attenuates Metastatic Ability of Human Metastatic Ovarian Cancer Cells via Modulating Multiple Signaling Molecules Involved in Cell Survival, Proliferation, Migration and Adhesion. Arch. Biochem. Biophys. 2021;701:108795. doi: 10.1016/j.abb.2021.108795. [DOI] [PubMed] [Google Scholar]
- 202.Yamauchi K., Afroze S.H., Mitsunaga T., McCormick T.C., Kuehl T.J., Zawieja D.C., Uddin M.N. 3,4′,7-O-Trimethylquercetin Inhibits Invasion and Migration of Ovarian Cancer Cells. Anticancer Res. 2017;37:2823–2829. doi: 10.21873/anticanres.11633. [DOI] [PubMed] [Google Scholar]
- 203.Li N., Sun C., Zhou B., Xing H., Ma D., Chen G., Weng D. Low Concentration of Quercetin Antagonizes the Cytotoxic Effects of Anti-Neoplastic Drugs in Ovarian Cancer. PLoS ONE. 2014;9:e100314. doi: 10.1371/journal.pone.0100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Scambia G., Ranelletti F.O., Benedetti Panici P., Bonanno G., De Vincenzo R., Piantelli M., Mancuso S. Synergistic Antiproliferative Activity of Quercetin and Cisplatin on Ovarian Cancer Cell Growth. Anti-Cancer Drugs. 1990;1:45–48. doi: 10.1097/00001813-199010000-00008. [DOI] [PubMed] [Google Scholar]
- 205.Tiwari H., Karki N., Pal M., Basak S., Verma R.K., Bal R., Kandpal N.D., Bisht G., Sahoo N.G. Functionalized Graphene Oxide as a Nanocarrier for Dual Drug Delivery Applications: The Synergistic Effect of Quercetin and Gefitinib against Ovarian Cancer Cells. Colloids Surf. B Biointerfaces. 2019;178:452–459. doi: 10.1016/j.colsurfb.2019.03.037. [DOI] [PubMed] [Google Scholar]
- 206.Fatease A.A., Shah V., Nguyen D.X., Cote B., LeBlanc N., Rao D.A., Alani A.W.G. Chemosensitization and Mitigation of Adriamycin-Induced Cardiotoxicity Using Combinational Polymeric Micelles for Co-Delivery of Quercetin/Resveratrol and Resveratrol/Curcumin in Ovarian Cancer. Nanomed. Nanotechnol. Biol. Med. 2019;19:39–48. doi: 10.1016/j.nano.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 207.Xu G., Li B., Wang T., Wan J., Zhang Y., Huang J., Shen Y. Enhancing the Anti-Ovarian Cancer Activity of Quercetin Using a Self-Assembling Micelle and Thermosensitive Hydrogel Drug Delivery System. RSC Adv. 2018;8:21229–21242. doi: 10.1039/C8RA03274B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Palanisamy C.P., Cui B., Zhang H., Panagal M., Paramasivam S., Chinnaiyan U., Jeyaraman S., Murugesan K., Rostagno M., Sekar V., et al. Anti-Ovarian Cancer Potential of Phytocompound and Extract from South African Medicinal Plants and Their Role in the Development of Chemotherapeutic Agents. Am. J. Cancer Res. 2021;11:1828–1844. [PMC free article] [PubMed] [Google Scholar]
- 209.Löcken H., Clamor C., Müller K. Napabucasin and Related Heterocycle-Fused Naphthoquinones as STAT3 Inhibitors with Antiproliferative Activity against Cancer Cells. J. Nat. Prod. 2018;81:1636–1644. doi: 10.1021/acs.jnatprod.8b00247. [DOI] [PubMed] [Google Scholar]
- 210.Shchekotikhin A.E., Nadysev G.Y., Tikhomirov A.S., Dezhenkova L.G. Semi-Synthetic Derivatives of Heliomycin with an Antiproliferative Potency. PRA. 2018;13:469–472. doi: 10.2174/1574892813666180723150542. [DOI] [PubMed] [Google Scholar]
- 211.Ferry D.R., Smith A., Malkhandi J., Fyfe D.W., deTakats P.G., Anderson D., Baker J., Kerr D.J. Phase I Clinical Trial of the Flavonoid Quercetin: Pharmacokinetics and Evidence for in Vivo Tyrosine Kinase Inhibition. Clin. Cancer Res. 1996;2:659–668. [PubMed] [Google Scholar]
- 212.Mei J.-Y., Zhang M.-J., Wang Y.-Y., Liu Y.-H. The Positive Clinical Therapeutically Effects of Escin on Advanced Thyroid Cancer. Cancer Med. 2017;6:937–943. doi: 10.1002/cam4.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Berman A.Y., Motechin R.A., Wiesenfeld M.Y., Holz M.K. The Therapeutic Potential of Resveratrol: A Review of Clinical Trials. NPJ Precis. Oncol. 2017;1:35. doi: 10.1038/s41698-017-0038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Budisan L., Gulei D., Zanoaga O.M., Irimie A.I., Sergiu C., Braicu C., Gherman C.D., Berindan-Neagoe I. Dietary Intervention by Phytochemicals and Their Role in Modulating Coding and Non-Coding Genes in Cancer. Int. J. Mol. Sci. 2017;18:1178. doi: 10.3390/ijms18061178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yan Y.B., Tian Q., Zhang J.F., Xiang Y. Antitumor Effects and Molecular Mechanisms of Action of Natural Products in Ovarian Cancer (Review) Oncol. Lett. 2020;20:141. doi: 10.3892/ol.2020.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable. No new data were created or analyzed in this study.